A Wearable Sensor System to Measure Step-Based Gait Parameters for Parkinson’s Disease Rehabilitation
Abstract
1. Introduction
2. Materials and Methods
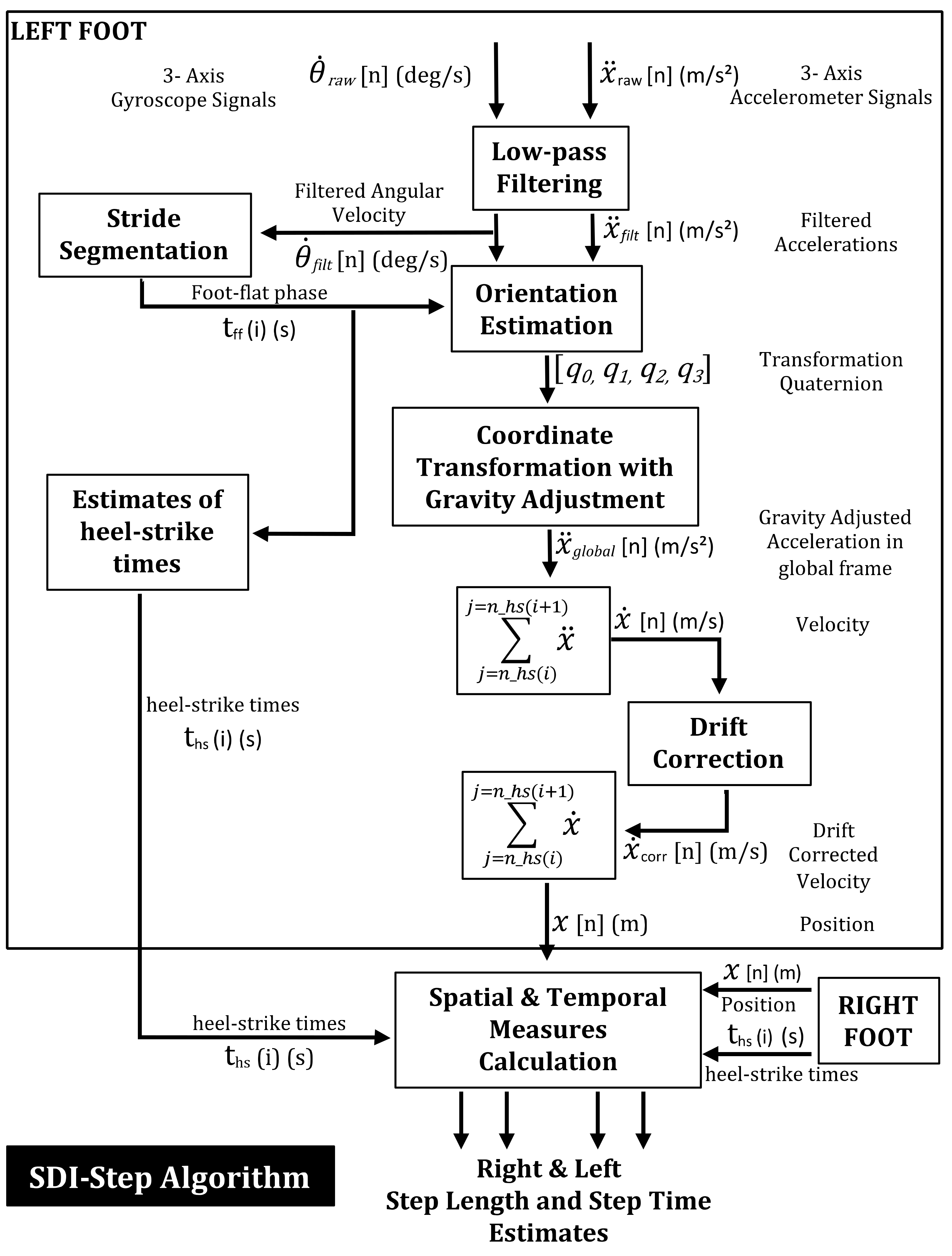
2.1. Segmented Double Integration-Step Algorithm
- Stride segmentation: The IMU data was then segmented into two phases of gait movements–stationary (foot-flat) phase and non-stationary (swing phase). The time point at which the filtered angular velocity signal crossed a pre-specified threshold (20 degrees/s) was used to detect the onset of swing phase as this threshold was observed to be the lowest value that avoided false positive identification of swing phase initiation. Segmentation was performed to obtain the start and end times of each phase.
- Orientation estimation: A complementary filter [36] was used for orientation estimation, which fuses the static low-frequency linear movements from the accelerometer with the dynamic high-frequency angular movements of the gyroscope.
- Coordinate transformation with gravity adjustment: The acceleration vector of the sensor was transformed to the global coordinate system using the estimated orientation function and the gravitational component of the transformed acceleration was removed.
- Heel-strike detection: The heel-strike events were identified by determining the minima of the angular velocity vector within an average estimate of stride duration for the population.
- Velocity estimation: The velocity of each swing phase was obtained by numerically integrating the gravity-adjusted acceleration between two consecutive heel strikes for each foot.
- Drift correction: Drift in the computed velocity was corrected using a zero velocity update algorithm [37]. The average amount of drift during the foot-flat phase was subtracted from the subsequent swing phase for each step to obtain the drift-corrected velocity.
- Position estimation: The drift-corrected velocity signal was numerically integrated between two consecutive heel strikes to estimate the location (in three dimensions) of each foot at each heel strike.
- Step length and step time calculation: The step length and step times for each foot were obtained using the estimated positions and timings of subsequent heel-strikes.
2.2. Participants
2.3. Measurement Systems and Calculation of Gait Parameters
2.4. Gait Assessment Protocol
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bugané, F.; Benedetti, M.G.; Casadio, G.; Attala, S.; Biagi, F.; Manca, M.; Leardini, A. Estimation of spatial-temporal gait parameters in level walking based on a single accelerometer: Validation on normal subjects by standard gait analysis. Comput. Methods Programs Biomed. 2012, 108, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Byun, S.; Han, J.W.; Kim, T.H.; Kim, K.W. Test-Retest Reliability and Concurrent Validity of a Single Tri-Axial Accelerometer-Based Gait Analysis in Older Adults with Normal Cognition. PLoS ONE 2016, 11, e0158956. [Google Scholar] [CrossRef] [PubMed]
- Del Din, S.; Godfrey, A.; Rochester, L. Validation of an Accelerometer to Quantify a Comprehensive Battery of Gait Characteristics in Healthy Older Adults and Parkinson’s Disease: Toward Clinical and at Home Use. IEEE J. Biomed. Health Inform. 2016, 20, 838–847. [Google Scholar] [CrossRef]
- Hsu, Y.L.; Chung, P.C.; Wang, W.H.; Pai, M.C.; Wang, C.Y.; Lin, C.W.; Wu, H.L.; Wang, J.S. Gait and balance analysis for patients with Alzheimer’s disease using an inertial-sensor-based wearable instrument. IEEE J. Biomed. Health Inform 2014, 18, 1822–1830. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois, A.B.; Mariani, B.; Aminian, K.; Zambelli, P.Y.; Newman, C.J. Spatio-temporal gait analysis in children with cerebral palsy using, foot-worn inertial sensors. Gait Posture 2014, 39, 436–442. [Google Scholar] [CrossRef]
- Mariani, B.; Hoskovec, C.; Rochat, S.; Büla, C.; Penders, J.; Aminian, K. 3D gait assessment in young and elderly subjects using foot-worn inertial sensors. J. Biomech. 2010, 43, 2999–3006. [Google Scholar] [CrossRef]
- Salarian, A.; Russmann, H.; Vingerhoets, F.J.; Dehollain, C.; Blanc, Y.; Burkhard, P.R.; Aminian, K. Gait assessment in Parkinson’s disease: Toward an ambulatory system for long-term monitoring. IEEE Trans. Biomed. Eng. 2004, 51, 1434–1443. [Google Scholar] [CrossRef]
- Esser, P.; Dawes, H.; Collett, J.; Feltham, M.G.; Howells, K. Assessment of spatio-temporal gait parameters using inertial measurement units in neurological populations. Gait Posture 2011, 34, 558–560. [Google Scholar] [CrossRef]
- Mariani, B.; Jiménez, M.C.; Vingerhoets, F.J.; Aminian, K. On-shoe wearable sensors for gait and turning assessment of patients with Parkinson’s disease. IEEE Trans. Biomed. Eng. 2013, 60, 155–158. [Google Scholar] [CrossRef]
- Gray, P.; Hildebrand, K. Fall risk factors in Parkinson’s disease. J. Neurosci. Nurs. 2000, 32, 222–228. [Google Scholar] [CrossRef]
- Xu, J.; Bao, T.; Lee, U.H.; Kinnaird, C.; Carender, W.; Huang, Y.; Sienko, K.H.; Shull, P.B. Configurable, wearable sensing and vibrotactile feedback system for real-time postural balance and gait training: Proof-of-concept. J. Neuroeng. Rehabil. 2017, 14, 102. [Google Scholar] [CrossRef]
- Studer, V.; Maestri, R.; Clerici, I.; Spina, L.; Zivi, I.; Ferrazzoli, D.; Frazzitta, G. Treadmill Training with Cues and Feedback Improves Gait in People with More Advanced Parkinson’s Disease. J. Parkinsons Dis. 2017, 7, 729–739. [Google Scholar] [CrossRef]
- Jellish, J.; Abbas, J.J.; Ingalls, T.M.; Mahant, P.; Samanta, J.; Ospina, M.C.; Krishnamurthi, N. A System for Real-Time Feedback to Improve Gait and Posture in Parkinson’s Disease. IEEE J. Biomed. Health Inform. 2015, 19, 1809–1819. [Google Scholar] [CrossRef]
- Mancini, M.; Smulders, K.; Harker, G.; Stuart, S.; Nutt, J.G. Assessment of the ability of open- and closed-loop cueing to improve turning and freezing in people with Parkinson’s disease. Sci. Rep. 2018, 8, 12773. [Google Scholar] [CrossRef]
- Muthukrishnan, N.; Abbas, J.J.; Shill, H.A.; Krishnamurthi, N. Cueing Paradigms to Improve Gait and Posture in Parkinson’s Disease: A Narrative Review. Sensors 2019, 19, 5468. [Google Scholar] [CrossRef]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef]
- Sabatini, A.M. Quaternion-based extended Kalman filter for determining orientation by inertial and magnetic sensing. IEEE Trans. Biomed. Eng. 2006, 53, 1346–1356. [Google Scholar] [CrossRef]
- Yun, X.; Calusdian, J.; Bachmann, E.R.; McGhee, R.B. Estimation of Human Foot Motion During Normal Walking Using Inertial and Magnetic Sensor Measurements. IEEE Trans. Instrum. Meas. 2012, 61, 2059–2072. [Google Scholar] [CrossRef]
- Song, M.; Kim, J. An Ambulatory Gait Monitoring System with Activity Classification and Gait Parameter Calculation Based on a Single Foot Inertial Sensor. IEEE Trans. Biomed. Eng. 2018, 65, 885–893. [Google Scholar] [CrossRef]
- Hannink, J.; Kautz, T.; Pasluosta, C.F.; Gaßmann, K.G.; Klucken, J.; Eskofier, B.M. Sensor-Based Gait Parameter Extraction With Deep Convolutional Neural Networks. IEEE J. Biomed. Health Inform. 2017, 21, 85–93. [Google Scholar] [CrossRef]
- Hu, B.; Dixon, P.C.; Jacobs, J.V.; Dennerlein, J.T.; Schiffman, J.M. Machine learning algorithms based on signals from a single wearable inertial sensor can detect surface- and age-related differences in walking. J. Biomech. 2018, 71, 37–42. [Google Scholar] [CrossRef]
- Rogers, M.W. Disorders of posture, balance, and gait in Parkinson’s disease. Clin. Geriatr. Med. 1996, 12, 825–845. [Google Scholar] [CrossRef]
- Nieuwboer, A.; Dom, R.; De Weerdt, W.; Desloovere, K.; Fieuws, S.; Broens-Kaucsik, E. Abnormalities of the spatiotemporal characteristics of gait at the onset of freezing in Parkinson’s disease. Mov. Disord. 2001, 16, 1066–1075. [Google Scholar] [CrossRef]
- Fasano, A.; Plotnik, M.; Bove, F.; Berardelli, A. The neurobiology of falls. Neurol. Sci. 2012, 33, 1215–1223. [Google Scholar] [CrossRef]
- Morris, R.; Stuart, S.; McBarron, G.; Fino, P.C.; Mancini, M.; Curtze, C. Validity of Mobility Lab (version 2) for gait assessment in young adults, older adults and Parkinson’s disease. Physiol. Meas. 2019, 40, 095003. [Google Scholar] [CrossRef]
- Baram, Y.; Aharon-Peretz, J.; Badarny, S.; Susel, Z.; Schlesinger, I. Closed-loop auditory feedback for the improvement of gait in patients with Parkinson’s disease. J. Neurol. Sci. 2016, 363, 104–106. [Google Scholar] [CrossRef]
- Ginis, P.; Nieuwboer, A.; Dorfman, M.; Ferrari, A.; Gazit, E.; Canning, C.G.; Rocchi, L.; Chiari, L.; Hausdorff, J.M.; Mirelman, A. Feasibility and effects of home-based smartphone-delivered automated feedback training for gait in people with Parkinson’s disease: A pilot randomized controlled trial. Parkinsonism Relat. Disord. 2016, 22, 28–34. [Google Scholar] [CrossRef]
- Aich, S.; Pradhan, P.M.; Park, J.; Sethi, N.; Vathsa, V.S.; Kim, H.C. A Validation Study of Freezing of Gait (FoG) Detection and Machine-Learning-Based FoG Prediction Using Estimated Gait Characteristics with a Wearable Accelerometer. Sensors 2018, 18, 3287. [Google Scholar] [CrossRef]
- Yang, S.; Li, Q. Inertial sensor-based methods in walking speed estimation: A systematic review. Sensors 2012, 12, 6102–6116. [Google Scholar] [CrossRef]
- Song, Y.; Shin, S.; Kim, S.; Lee, D.; Lee, K.H. Speed estimation from a tri-axial accelerometer using neural networks. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 23–26 August 2007; pp. 3224–3227. [Google Scholar]
- Miyazaki, S. Long-term unrestrained measurement of stride length and walking velocity utilizing a piezoelectric gyroscope. IEEE Trans. Biomed. Eng. 1997, 44, 753–759. [Google Scholar] [CrossRef]
- Zhu, S.; Anderson, H.; Wang, Y. A Real-Time On-Chip Algorithm for IMU-Based Gait Measurement. In Advances in Multimedia Information Processing; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Yang, S.; Li, Q. IMU-based ambulatory walking speed estimation in constrained treadmill and overground walking. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 313–322. [Google Scholar]
- Tong, K.; Granat, M.H. A practical gait analysis system using gyroscopes. Med. Eng. Phys. 1999, 21, 87–94. [Google Scholar] [PubMed]
- Greene, B.R.; McGrath, D.; O’Neill, R.; O’Donovan, K.J.; Burns, A.; Caulfield, B. An adaptive gyroscope-based algorithm for temporal gait analysis. Med. Biol. Eng. Comput. 2010, 48, 1251–1260. [Google Scholar] [PubMed]
- Tian, Y.; Wei, H.; Tan, J. An adaptive-gain complementary filter for real-time human motion tracking with MARG sensors in free-living environments. IEEE Trans. Neural. Syst. Rehabil. Eng. 2013, 21, 254–264. [Google Scholar] [CrossRef]
- Ma, M.; Song, Q.; Gu, Y.; Li, Y.; Zhou, Z. An Adaptive Zero Velocity Detection Algorithm Based on Multi-Sensor Fusion for a Pedestrian Navigation System. Sensors 2018, 18, 3261. [Google Scholar] [CrossRef]
- Pierleoni, P.; Pinti, F.; Belli, A.; Palma, L. A dataset for wearable sensors validation in gait analysis. Data Brief 2020, 31, 105918. [Google Scholar] [CrossRef]
- Vítečková, S.; Horáková, H.; Poláková, K.; Krupička, R.; Růžička, E.; Brožová, H. Agreement between the GAITRite((R)) System and the Wearable Sensor BTS G-Walk((R)) for measurement of gait parameters in healthy adults and Parkinson’s disease patients. PeerJ 2020, 8, e8835. [Google Scholar]
- Passing, H.; Bablok, W. A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, Part I. J. Clin. Chem. Clin. Biochem. 1983, 21, 709–720. [Google Scholar]
- Bilić-Zulle, L. Comparison of methods: Passing and Bablok regression. Biochem. Med. 2011, 21, 49–52. [Google Scholar] [CrossRef]
- Giavarina, D. Understanding Bland Altman analysis. Biochem. Med. 2015, 25, 141–151. [Google Scholar]
- Senn, S. Review of Fleiss, statistical methods for rates and proportions. Res. Synth. Methods 2011, 2, 221–222. [Google Scholar] [PubMed]
- Allseits, E.; Agrawal, V.; Lučarević, J.; Gailey, R.; Gaunaurd, I.; Bennett, C. A practical step length algorithm using lower limb angular velocities. J. Biomech. 2018, 66, 137–144. [Google Scholar] [PubMed]
- Hartmann, A.; Luzi, S.; Murer, K.; de Bie, R.A.; de Bruin, E.D. Concurrent validity of a trunk tri-axial accelerometer system for gait analysis in older adults. Gait Posture 2009, 29, 444–448. [Google Scholar] [PubMed]
- Tunca, C.; Pehlivan, N.; Ak, N.; Arnrich, B.; Salur, G.; Ersoy, C. Inertial Sensor-Based Robust Gait Analysis in Non-Hospital Settings for Neurological Disorders. Sensors 2017, 17, 825. [Google Scholar]

| Descriptive and Statistical Measures | Step Length | Step Time | ||||
|---|---|---|---|---|---|---|
| PD (n = 211 steps) | YA1 (n = 222 steps) | YA2 (n = 160 steps) | PD (n = 211 steps) | YA1 (n = 222 steps) | YA2 (n = 160 steps) | |
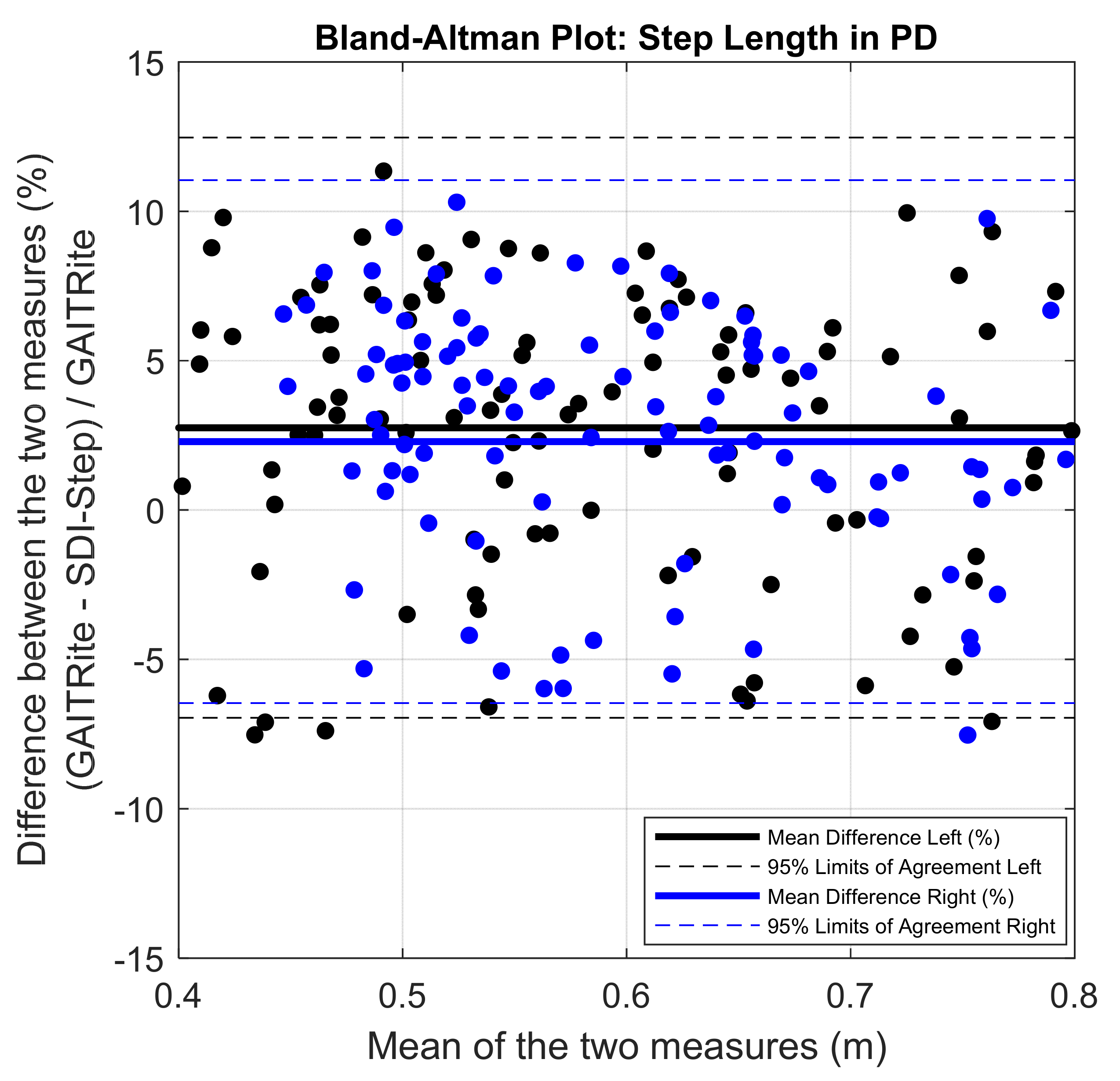
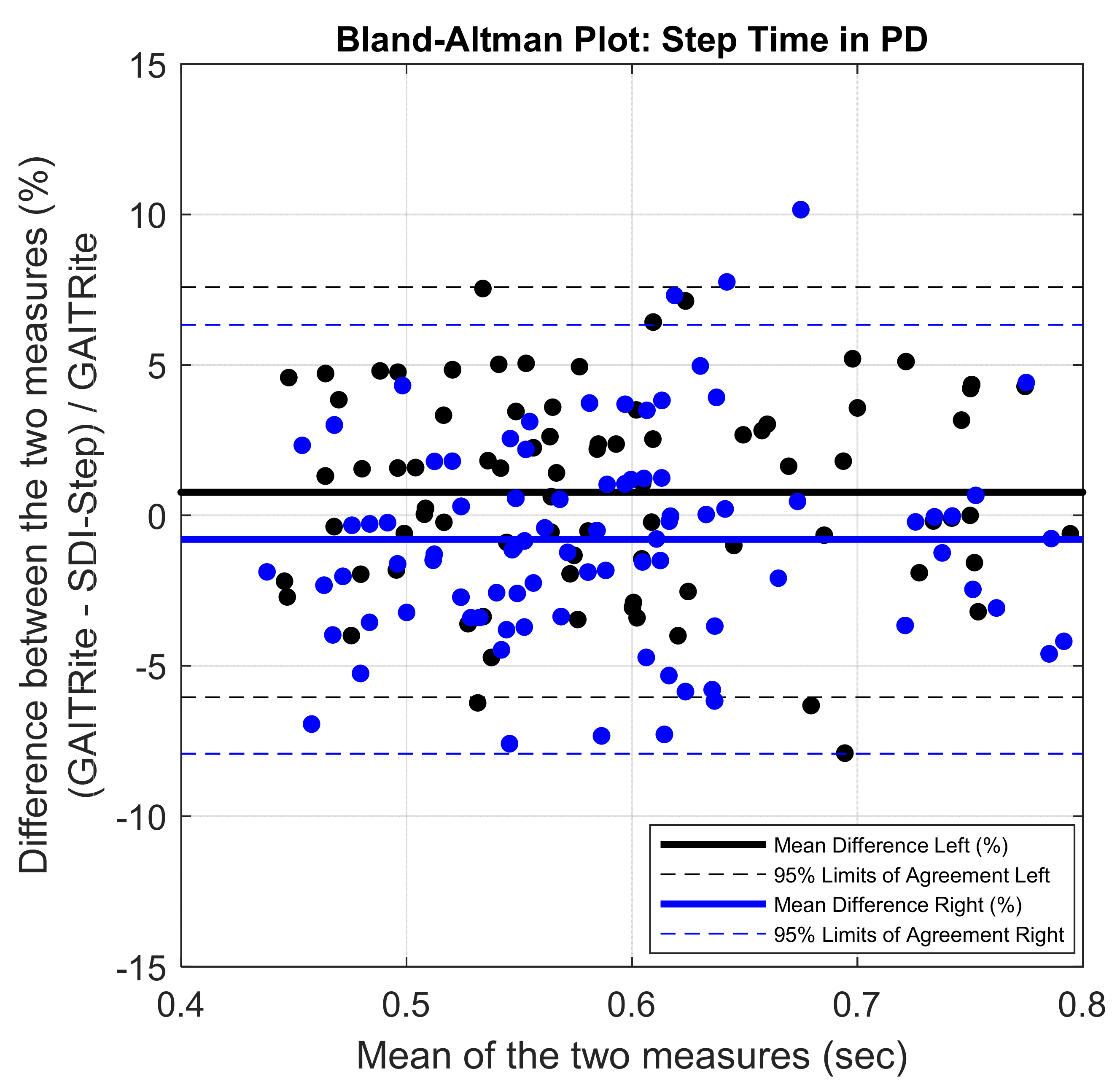
| Mean (SD) Lab-based system | 0.59 (0.11) | 0.68 (0.09) | 0.67 (0.05) | 0.73 (0.26) | 0.59 (0.06) | 0.64 (0.05) |
| Mean (SD) IMU SDI-Step | 0.58 (0.12) | 0.66 (0.09) | 0.66 (0.05) | 0.73 (0.27) | 0.59 (0.08) | 0.64 (0.05) |
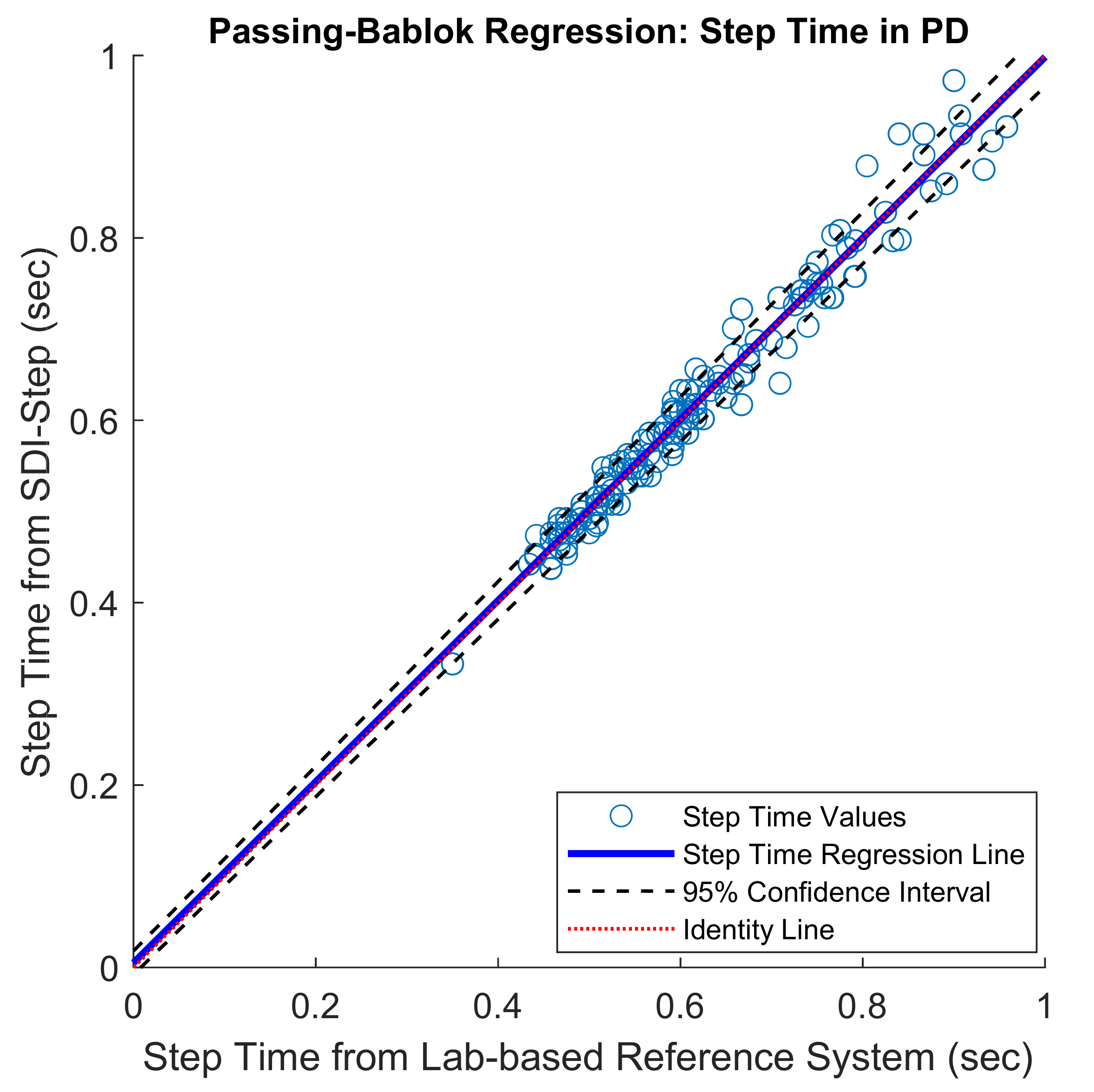
| PB Slope (95% CI) | 1.05 (1–1.17) | 0.99 (0.94–1.06) | 0.94 (0.74–1.12) | 1 (1–1.16) | 0.99 (0.97–1.01) | 1 (0.91–1.09) |
| PB Intercept (95% CI) | −0.05 (−0.01–0.1) | 0.03 (−0.03–0.05) | 0.03 (−0.09–0.17) | 0 (−0.09–0) | 0.003 (−0.01–0.02) | 0.005 (−0.05–0.06) |
| ICC (2,1) (95% CI) | 0.97 (0.93–0.98) | 0.9 (0.83–0.95) | 0.84 (0.81–0.90) | 0.98 (0.98–0.99) | 0.94 (0.91–0.95) | 0.94 (0.88–0.96) |
| BA–bias (95% LoA) | 0.02 (−0.04–0.07) | 0.02 (−0.06–0.09) | 0.01 (−0.05–0.08) | 0.01 (−0.05–0.06) | 0 (−0.05–0.05) | 0.01 (−0.04–0.06) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muthukrishnan, N.; Abbas, J.J.; Krishnamurthi, N. A Wearable Sensor System to Measure Step-Based Gait Parameters for Parkinson’s Disease Rehabilitation. Sensors 2020, 20, 6417. https://doi.org/10.3390/s20226417
Muthukrishnan N, Abbas JJ, Krishnamurthi N. A Wearable Sensor System to Measure Step-Based Gait Parameters for Parkinson’s Disease Rehabilitation. Sensors. 2020; 20(22):6417. https://doi.org/10.3390/s20226417
Chicago/Turabian StyleMuthukrishnan, Niveditha, James J. Abbas, and Narayanan Krishnamurthi. 2020. "A Wearable Sensor System to Measure Step-Based Gait Parameters for Parkinson’s Disease Rehabilitation" Sensors 20, no. 22: 6417. https://doi.org/10.3390/s20226417
APA StyleMuthukrishnan, N., Abbas, J. J., & Krishnamurthi, N. (2020). A Wearable Sensor System to Measure Step-Based Gait Parameters for Parkinson’s Disease Rehabilitation. Sensors, 20(22), 6417. https://doi.org/10.3390/s20226417




