Sensor-to-Segment Calibration Methodologies for Lower-Body Kinematic Analysis with Inertial Sensors: A Systematic Review
Abstract
1. Introduction
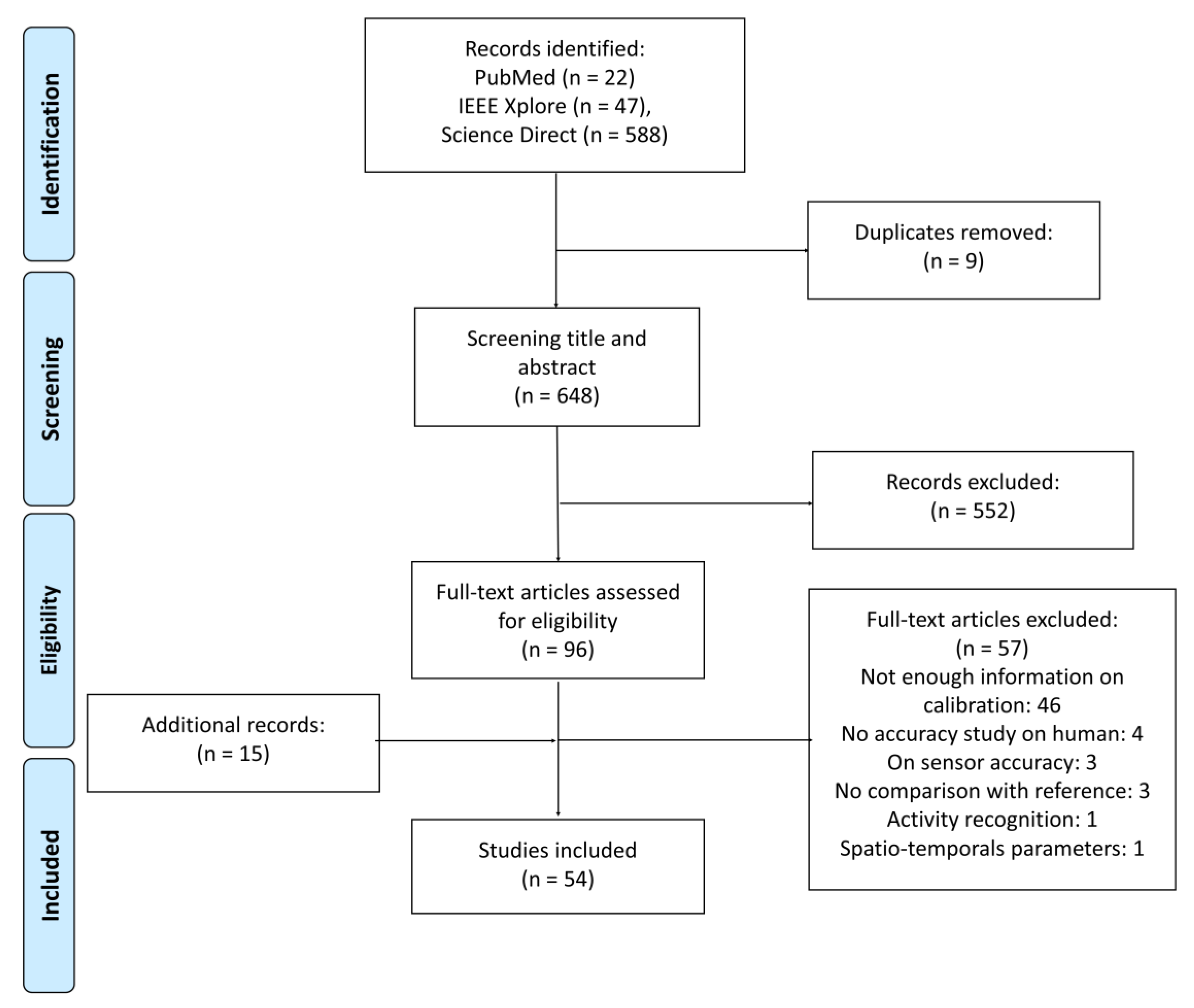
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Sources
2.3. Study Selection
2.4. Results Synthesis
3. Results
3.1. Type of Sensor-to-Segment Calibration
3.1.1. Pelvis Segment Calibration
3.1.2. Femur Segment Calibration
3.1.3. Tibia-Fibula Segment Calibration
3.1.4. Foot-Segment Calibration
3.2. Mathematical Computation of Segment Axes
3.3. Evaluation of the Methods
3.3.1. Method of Reference
3.3.2. Accuracy Assessment by Comparison with a Reference
3.3.3. Repeatability Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Baker, R. Gait analysis methods in rehabilitation. J. Neuroeng. Rehabil. 2006, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Bertucci, W.M.; Betik, A.C.; Duc, S.; Grappe, F. Gross Efficiency and Cycling Economy Are Higher in the Field as Compared with on an Axiom Stationary Ergometer. J. Appl. Biomech. 2012, 28, 636–644. [Google Scholar] [CrossRef]
- Galperin, I.; Hillel, I.; Del Din, S.; Bekkers, E.M.J.; Nieuwboer, A.; Abbruzzese, G.; Avanzino, L.; Nieuwhof, F.; Bloem, B.R.; Rochester, L.; et al. Associations between daily-living physical activity and laboratory-based assessments of motor severity in patients with falls and Parkinson’s disease. Parkinsonism Relat. Disord. 2019, 62, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Tamburini, P.; Storm, F.; Buckley, C.; Bisi, M.C.; Stagni, R.; Mazzà, C. Moving from laboratory to real life conditions: Influence on the assessment of variability and stability of gait. Gait Posture 2018, 59, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Cavanagh, P.R. ISB recommendations for standardization in the reporting of kinematic data. J. Biomech. 1995, 28, 1257–1261. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Cappozzo, A.; Della Croce, U.; Leardini, A.; Chiari, L. Human movement analysis using stereophotogrammetry: Part 1: Theoretical background. Gait Posture 2005, 21, 186–196. [Google Scholar]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.; Chan, Y.-Y.; Fong, D.T.-P.; Chan, Y.-Y. The Use of Wearable Inertial Motion Sensors in Human Lower Limb Biomechanics Studies: A Systematic Review. Sensors 2010, 10, 11556–11565. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; Galán-Mercant, A.; Williams, J.M. The use of inertial sensors system for human motion analysis. Phys. Ther. Rev. 2010, 15, 462–473. [Google Scholar] [CrossRef]
- Caldas, R.; Mundt, M.; Potthast, W.; Buarque de Lima Neto, F.; Markert, B. A systematic review of gait analysis methods based on inertial sensors and adaptive algorithms. Gait Posture 2017, 57, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Sprager, S.; Juric, M.; Sprager, S.; Juric, M.B. Inertial Sensor-Based Gait Recognition: A Review. Sensors 2015, 15, 22089–22127. [Google Scholar] [CrossRef] [PubMed]
- Jarchi, D.; Pope, J.; Lee, T.K.M.; Tamjidi, L.; Mirzaei, A.; Sanei, S. A Review on Accelerometry-Based Gait Analysis and Emerging Clinical Applications. IEEE Rev. Biomed. Eng. 2018, 11, 177–194. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward Pervasive Gait Analysis with Wearable Sensors: A Systematic Review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef]
- Murphy, S.L. Review of physical activity measurement using accelerometers in older adults: Considerations for research design and conduct. Prev. Med. (Baltim.) 2009, 48, 108–114. [Google Scholar] [CrossRef]
- Tao, W.; Liu, T.; Zheng, R.; Feng, H.; Tao, W.; Liu, T.; Zheng, R.; Feng, H. Gait Analysis Using Wearable Sensors. Sensors 2012, 12, 2255–2283. [Google Scholar] [CrossRef]
- Weygers, I.; Kok, M.; Konings, M.; Hallez, H.; De Vroey, H.; Claeys, K. Inertial Sensor-Based Lower Limb Joint Kinematics: A Methodological Systematic Review. Sensors 2020, 20, 673. [Google Scholar] [CrossRef]
- Poitras, I.; Dupuis, F.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.-S. Validity and Reliability of Wearable Sensors for Joint Angle Estimation: A Systematic Review. Sensors 2019, 19, 1555. [Google Scholar] [CrossRef]
- Kalman, R.E. A New Approach to Linear Filtering and Prediction Problems. J. Basic Eng. 1960, 82, 35. [Google Scholar] [CrossRef]
- Sabatini, A.M. Estimating Three-Dimensional Orientation of Human Body Parts by Inertial/Magnetic Sensing. Sensors 2011, 11, 1489–1525. [Google Scholar] [CrossRef]
- Bergamini, E.; Ligorio, G.; Summa, A.; Vannozzi, G.; Cappozzo, A.; Sabatini, A. Estimating Orientation Using Magnetic and Inertial Sensors and Different Sensor Fusion Approaches: Accuracy Assessment in Manual and Locomotion Tasks. Sensors 2014, 14, 18625–18649. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P. 25 years of lower limb joint kinematics by using inertial and magnetic sensors: A review of methodological approaches. Gait Posture 2017, 51, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Murakami, T.; Handa, Y. Preliminary tests of a prototype FES control system for cycling wheelchair rehabilitation. In Proceedings of the IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; pp. 1–6. [Google Scholar]
- Palermo, E.; Rossi, S.; Patanè, F.; Petrarca, M.; Castelli, E.; Cappa, P. Experimental validation of a sensor to segment calibration procedure for MIMU based gait analysis. Gait Posture 2013, 38, S110. [Google Scholar] [CrossRef]
- O’Donovan, K.J.; Kamnik, R.; O’Keeffe, D.T.; Lyons, G.M. An inertial and magnetic sensor based technique for joint angle measurement. J. Biomech. 2007, 40, 2604–2611. [Google Scholar] [CrossRef] [PubMed]
- Favre, J.; Aissaoui, R.; Jolles, B.M.; de Guise, J.A.; Aminian, K. Functional calibration procedure for 3D knee joint angle description using inertial sensors. J. Biomech. 2009, 42, 2330–2335. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P.; Cereatti, A.; Cappozzo, A. Joint kinematics estimate using wearable inertial and magnetic sensing modules. Gait Posture 2008, 28, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Dejnabadi, H.; Jolles, B.M.; Aminian, K. A New Approach to Accurate Measurement of Uniaxial Joint Angles Based on a Combination of Accelerometers and Gyroscopes. IEEE Trans. Biomed. Eng. 2005, 52, 1478–1484. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Catani, F.; Leardini, A.; Pignotti, E.; Giannini, S. Data management in gait analysis for clinical applications. Clin. Biomech. 1998, 13, 204–215. [Google Scholar] [CrossRef]
- Cappozzo, A.; Catani, F.; Della Croce, U.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Fasel, B.; Spörri, J.; Schütz, P.; Lorenzetti, S.; Aminian, K. Validation of functional calibration and strap-down joint drift correction for computing 3D joint angles of knee, hip, and trunk in alpine skiing. PLoS ONE 2017, 12, e0181446. [Google Scholar] [CrossRef]
- Favre, J.; Jolles, B.M.M.; Aissaoui, R.; Aminian, K. Ambulatory measurement of 3D knee joint angle. J. Biomech. 2008, 41, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Nazarahari, M.; Rouhani, H. Semi-Automatic Sensor-to-Body Calibration of Inertial Sensors on Lower Limb Using Gait Recording. IEEE Sens. J. 2019, 19, 12465–12474. [Google Scholar] [CrossRef]
- Cordillet, S.; Bideau, N.; Bideau, B.; Nicolas, G. Estimation of 3D Knee Joint Angles during Cycling Using Inertial Sensors: Accuracy of a Novel Sensor-to-Segment Calibration Procedure Based on Pedaling Motion. Sensors 2019, 19, 2474. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Cutti, A.G.; Ferrari, A.A.; Garofalo, P.; Raggi, M.; Cappello, A.; Ferrari, A.A. ‘Outwalk’’: A protocol for clinical gait analysis based on inertial and magnetic sensors’. Med. Biol. Eng. Comput. 2010, 48, 17–25. [Google Scholar] [CrossRef]
- Ferrari, A.; Cutti, A.G.; Garofalo, P.; Raggi, M.; Heijboer, M.; Cappello, A.; Davalli, A. First in vivo assessment of “outwalk”: A novel protocol for clinical gait analysis based on inertial and magnetic sensors. Med. Biol. Eng. Comput. 2010, 48, 1–15. [Google Scholar] [CrossRef]
- Van Den Noort, J.C.; Ferrari, A.; Cutti, A.G.; Becher, J.G.; Harlaar, J. Gait analysis in children with cerebral palsy via inertial and magnetic sensors. Med. Biol. Eng. Comput. 2013, 51, 377–386. [Google Scholar] [CrossRef]
- Buganè, F.; Benedetti, M.G.; D’Angeli, V.; Leardini, A.; Bugane, F.; Benedetti, M.G.; D’Angeli, V.; Leardini, A.; Buganè, F.; Benedetti, M.G.; et al. Estimation of pelvis kinematics in level walking based on a single inertial sensor positioned close to the sacrum: Validation on healthy subjects with stereophotogrammetric system. Biomed. Eng. Online 2014, 13, 146. [Google Scholar] [CrossRef]
- Hamdi, M.M.; Awad, M.I.; Abdelhameed, M.M.; Tolbah, F.A. Lower limb motion tracking using IMU sensor network. In Proceedings of the Cairo International Biomedical Engineering Conference (CIBEC), Cairo, Egypt, 11–13 December 2014; pp. 28–33. [Google Scholar]
- Tadano, S.; Takeda, R.; Miyagawa, H. Three dimensional gait analysis using wearable acceleration and gyro sensors based on quaternion calculations. Sensors 2013, 13, 9321–9343. [Google Scholar] [CrossRef]
- Vargas-Valencia, L.S.; Elias, A.; Rocon, E.; Bastos-Filho, T.; Frizera, A. An IMU-to-Body Alignment Method Applied to Human Gait Analysis. Sensors 2016, 16, 2090. [Google Scholar] [CrossRef] [PubMed]
- Nazarahari, M.; Noamani, A.; Ahmadian, N.; Rouhani, H. Sensor-to-body calibration procedure for clinical motion analysis of lower limb using magnetic and inertial measurement units. J. Biomech. 2019, 85, 224–229. [Google Scholar] [CrossRef]
- Lebleu, J.; Gosseye, T.; Detrembleur, C.; Mahaudens, P.; Cartiaux, O.; Penta, M. Lower Limb Kinematics Using Inertial Sensors during Locomotion: Accuracy and Reproducibility of Joint Angle Calculations with Different Sensor-to-Segment Calibrations. Sensors 2020, 20, 715. [Google Scholar] [CrossRef] [PubMed]
- Leineweber, M.J.; Gomez Orozco, M.D.; Andrysek, J. Evaluating the feasibility of two post-hoc correction techniques for mitigating posture-induced measurement errors associated with wearable motion capture. Med. Eng. Phys. 2019, 71, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Duong, T.T.H.; Zhang, H.; Lynch, T.S.; Zanotto, D. Improving the Accuracy of Wearable Sensors for Human Locomotion Tracking Using Phase-Locked Regression Models. In Proceedings of the IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 145–150. [Google Scholar]
- Kianifar, R.; Joukov, V.; Lee, A.; Raina, S.; Kulić, D. Inertial measurement unit-based pose estimation: Analyzing and reducing sensitivity to sensor placement and body measures. J. Rehabil. Assist. Technol. Eng. 2019, 6, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Palermo, E.; Rossi, S.; Patanè, F.; Cappa, P. Experimental evaluation of indoor magnetic distortion effects on gait analysis performed with wearable inertial sensors. Physiol. Meas. 2014, 35, 399–415. [Google Scholar] [CrossRef]
- Horenstein, R.E.; Lewis, C.L.; Yan, S.; Halverstadt, A.; Shefelbine, S.J. Validation of magneto-inertial measuring units for measuring hip joint angles. J. Biomech. 2019, 91, 170–174. [Google Scholar] [CrossRef]
- Favre, J.; Luthi, F.; Jolles, B.M.; Siegrist, O.; Najafi, B.; Aminian, K. A new ambulatory system for comparative evaluation of the three-dimensional knee kinematics, applied to anterior cruciate ligament injuries. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 592–604. [Google Scholar] [CrossRef]
- Chen, K.-H.; Chen, P.-C.; Liu, K.-C.; Chan, C.-T. Wearable sensor-based rehabilitation exercise assessment for knee osteoarthritis. Sensors 2015, 15, 4193–4211. [Google Scholar] [CrossRef]
- Liu, K.; Liu, T.; Shibata, K.; Inoue, Y. Ambulatory measurement and analysis of the lower limb 3D posture using wearable sensor system. In Proceedings of the IEEE International Conference on Mechatronics and Automation, ICMA 2009, Changchun, China, 9–12 August 2009; pp. 3065–3069. [Google Scholar]
- Djurić-Jovičić, M.D.; Jovičić, N.S.; Popović, D.B. Kinematics of gait: New method for angle estimation based on accelerometers. Sensors 2011, 11, 10571–10585. [Google Scholar] [CrossRef]
- Chardonnens, J.; Favre, J.; Aminian, K. An effortless procedure to align the local frame of an inertial measurement unit to the local frame of another motion capture system. J. Biomech. 2012, 45, 2297–2300. [Google Scholar] [CrossRef]
- Chardonnens, J.; Favre, J.; Cuendet, F.; Gremion, G.; Aminian, K. A system to measure the kinematics during the entire ski jump sequence using inertial sensors. J. Biomech. 2013, 46, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Chardonnens, J.; Favre, J.; Cuendet, F.; Gremion, G.; Aminian, K. Characterization of lower-limbs inter-segment coordination during the take-off extension in ski jumping. Hum. Mov. Sci. 2013, 32, 741–752. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.W.; Zrenner, M.; Reynolds, D.; Dümler, B.; Eskofier, B.M. Sleeve based knee angle calculation for rehabilitation. In Proceedings of the IEEE 15th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Las Vegas, NV, USA, 4–7 March 2018; pp. 1–4. [Google Scholar]
- Feldhege, F.; Mau-Moeller, A.; Lindner, T.; Hein, A.; Markschies, A.; Zettl, U.K.; Bader, R. Accuracy of a custom physical activity and knee angle measurement sensor system for patients with neuromuscular disorders and gait abnormalities. Sensors 2015, 15, 10734–10752. [Google Scholar] [CrossRef]
- Robert-Lachaine, X.; Parent, G.; Fuentes, A.; Hagemeister, N.; Aissaoui, R. Inertial motion capture validation of 3D knee kinematics at various gait speed on the treadmill with a double-pose calibration. Gait Posture 2020, 77, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Choe, N.; Zhao, H.; Qiu, S.; So, Y. A sensor-to-segment calibration method for motion capture system based on low cost MIMU. Measurement 2019, 131, 490–500. [Google Scholar] [CrossRef]
- Soussé, R.; Verdú, J.; Jauregui, R.; Ferrer-Roca, V.; Balocco, S. Non-rigid alignment pipeline applied to human gait signals acquired with optical motion capture systems and inertial sensors. J. Biomech. 2019, 98, 109429. [Google Scholar] [CrossRef]
- Dejnabadi, H.; Jolles, B.M.; Casanova, E.; Fua, P.; Aminian, K. Estimation and Visualization of Sagittal Kinematics of Lower Limbs Orientation Using Body-Fixed Sensors. IEEE Trans. Biomed. Eng. 2006, 53, 1385–1393. [Google Scholar] [CrossRef]
- Gastaldi, L.; Rosso, V.; Gabola, V.; Agostini, V.; Frutos, M.M.L.; Knaflitz, M.; Takeda, R.; Tadano, S. Technical challenges using magneto-inertial sensors for gait analysis. In Proceedings of the IEEE International Symposium on Medical Measurements and Applications (MeMeA), Benevento, Italy, 15–18 May 2016; pp. 1–6. [Google Scholar]
- Favre, J.; Aissaoui, R.; Jolles, B.; Luthi, F.; de Guise, J.; Aminian, K. Ambulatory inertial system for 3D knee joint angles measurement during gait. J. Biomech. 2006, 39, S74. [Google Scholar] [CrossRef]
- Palermo, E.; Rossi, S.; Marini, F.; Patanè, F.; Cappa, P. Experimental evaluation of accuracy and repeatability of a novel body-to-sensor calibration procedure for inertial sensor-based gait analysis. Measurement 2014, 52, 145–155. [Google Scholar] [CrossRef]
- McGrath, T.; Fineman, R.; Stirling, L. An Auto-Calibrating Knee Flexion-Extension Axis Estimator Using Principal Component Analysis with Inertial Sensors. Sensors 2018, 18, 1882. [Google Scholar] [CrossRef] [PubMed]
- Seel, T.; Raisch, J.J.; Schauer, T. IMU-based joint angle measurement for gait analysis. Sensors 2014, 14, 6891–6909. [Google Scholar] [CrossRef]
- Chardonnens, J.; Favre, J.; Le Callennec, B.; Cuendet, F.; Gremion, G.; Aminian, K. Automatic measurement of key ski jumping phases and temporal events with a wearable system. J. Sports Sci. 2012, 30, 53–61. [Google Scholar] [CrossRef]
- Van den Noort, J.; van der Esch, M.; Steultjens, M.P.M.M.; Dekker, J.; Schepers, M.; Veltink, P.H.; Harlaar, J. Ambulatory measurement of the knee adduction moment in patients with osteoarthritis of the knee. J. Biomech. 2013, 46, 43–49. [Google Scholar] [CrossRef]
- Meng, L.; Martinez-Hernandez, U.; Childs, C.; Dehghani-Sanij, A.A.; Buis, A. A Practical Gait Feedback Method Based on Wearable Inertial Sensors for a Drop Foot Assistance Device. IEEE Sens. J. 2019, 19, 12235–12243. [Google Scholar] [CrossRef]
- Zhou, M.; An, S.; Feng, M.; Li, Z.; Shen, H.; Zhang, K.; Sun, J.; Cao, G. Gait analysis of patients with continuous proximal sciatic nerve blockade in flexion contractures after primary total knee arthroplasty. Gait Posture 2018, 66, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Van den Noort, J.C.; Scholtes, V.A.; Harlaar, J. Evaluation of clinical spasticity assessment in Cerebral palsy using inertial sensors. Gait Posture 2009, 30, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Takeda, R.; Tadano, S.; Natorigawa, A.; Todoh, M.; Yoshinari, S. Gait posture estimation using wearable acceleration and gyro sensors. J. Biomech. 2009, 42, 2486–2494. [Google Scholar] [CrossRef] [PubMed]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Millar, L.J.; Meng, L.; Rowe, P.J. Routine clinical motion analysis: Comparison of a bespoke real-time protocol to current clinical methods. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 149–158. [Google Scholar] [CrossRef]
- Leardini, A.; Cappozzo, A.; Catani, F.; Toksvig-Larsen, S.; Petitto, A.; Sforza, V.; Cassanelli, G.; Giannini, S. Validation of a functional method for the estimation of hip joint centre location. J. Biomech. 1999, 32, 99–103. [Google Scholar] [CrossRef]
- Camomilla, V.; Cereatti, A.; Vannozzi, G.; Cappozzo, A. An optimized protocol for hip joint centre determination using the functional method. J. Biomech. 2006, 39, 1096–1106. [Google Scholar] [CrossRef] [PubMed]
- List, R.; Gülay, T.; Stoop, M.; Lorenzetti, S. List Renate Kinematics of the Trunk and the Lower extremities During Restricted and Inrestricted Squats. J. Strength Cond. Res. 2013, 27, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Hagemeister, N.; Parent, G.; Van De Putte, M.; St-Onge, N.; Duval, N.; De Guise, J. A reproducible method for studying three-dimensional knee kinematics. J. Biomech. 2005, 38, 1926–1931. [Google Scholar] [CrossRef]
- Frigo, C.; Rabuffetti, M.; Kerrigan, D.C.; Deming, L.C.; Pedotti, A. Functionally oriented and clinically feasible quantitative gait analysis method. Med. Biol. Eng. Comput. 1998, 36, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Grood, E.S.; Suntay, W.J. A Joint Coordinate System for the Clinical Description of Three-Dimensional Motions: Application to the Knee. J. Biomech. Eng. 1983, 105, 136. [Google Scholar] [CrossRef]
- Favre, J.; Crevoisier, X.; Jolles, B.M.; Aminian, K. Evaluation of a mixed approach combining stationary and wearable systems to monitor gait over long distance. J. Biomech. 2010, 43, 2196–2202. [Google Scholar] [CrossRef]
- Rabuffetti, M.; Crenna, P. A modular protocol for the analysis of movement in children. Gait Posture 2004, 20, S77–S78. [Google Scholar]
- Leardini, A.; Sawacha, Z.; Paolini, G.; Ingrosso, S.; Nativo, R.; Benedetti, M.G. A new anatomically based protocol for gait analysis in children. Gait Posture 2007, 26, 560–571. [Google Scholar] [CrossRef]
- Picerno, P.; Cereatti, A.; Cappozzo, A. 3D joint kinematics by means of wearable sensors. Gait Posture 2008, 28, S2–S3. [Google Scholar] [CrossRef]
- Frigo, C.; Rabuffetti, M. Multifactorial estimation of hip and knee joint centres for clinical application of gait analysis. Gait Posture 1998, 8, 91–102. [Google Scholar] [CrossRef]
- Watanabe, T.; Saito, H.; Koike, E.; Nitta, K. A preliminary test of measurement of joint angles and stride length with wireless inertial sensors for wearable gait evaluation system. Comput. Intell. Neurosci. 2011, 2011, 975193. [Google Scholar] [CrossRef] [PubMed]
- Morton, L.; Baillie, L.; Ramirez-Iniguez, R. Pose calibrations for inertial sensors in rehabilitation applications. In Proceedings of the International Conference on Wireless and Mobile Computing, Networking and Communications, Lyon, France, 7–9 October 2013; pp. 204–211. [Google Scholar]
- Besier, T.F.; Sturnieks, D.L.; Alderson, J.A.; Lloyd, D.G. Repeatability of gait data using a functional hip joint centre and a mean helical knee axis. J. Biomech. 2003, 36, 1159–1168. [Google Scholar] [CrossRef]
- Marin, F.; Mannel, H.; Claes, L.; Dürselen, L. Correction of axis misalignment in the analysis of knee rotations. Hum. Mov. Sci. 2003, 22, 285–296. [Google Scholar] [CrossRef]
- Bouvier, B.; Duprey, S.; Claudon, L.; Dumas, R.; Savescu, A.; Bouvier, B.; Duprey, S.; Claudon, L.; Dumas, R.; Savescu, A. Upper Limb Kinematics Using Inertial and Magnetic Sensors: Comparison of Sensor-to-Segment Calibrations. Sensors 2015, 15, 18813–18833. [Google Scholar] [CrossRef] [PubMed]
- Reenalda, J.; Maartens, E.; Buurke, J.H.; Gruber, A.H. Kinematics and shock attenuation during a prolonged run on the athletic track as measured with inertial magnetic measurement units. Gait Posture 2019, 68, 155–160. [Google Scholar] [CrossRef]
- Reenalda, J.; Maartens, E.; Homan, L.; Buurke, J.H. Continuous three dimensional analysis of running mechanics during a marathon by means of inertial magnetic measurement units to objectify changes in running mechanics. J. Biomech. 2016, 49, 3362–3367. [Google Scholar] [CrossRef]
- Van den Noort, J.C.; Scholtes, V.A.; Becher, J.G.; Harlaar, J. Evaluation of the Catch in Spasticity Assessment in Children with Cerebral Palsy. Arch. Phys. Med. Rehabil. 2010, 91, 615–623. [Google Scholar] [CrossRef]
- Fradet, L.; Nez, A.; Monnet, T.; Lacouture, P. Which functional movements for sensor-to-segment calibration for lower-limb movement analysis with inertial sensors? Comput. Methods Biomech. Biomed. Eng. 2017, 20, 77–78. [Google Scholar] [CrossRef]
- Kainz, H.; Hajek, M.; Modenese, L.; Saxby, D.J.; Lloyd, D.G.; Carty, C.P. Reliability of functional and predictive methods to estimate the hip joint centre in human motion analysis in healthy adults. Gait Posture 2017, 53, 179–184. [Google Scholar] [CrossRef]
- Assi, A.; Sauret, C.; Massaad, A.; Bakouny, Z.; Pillet, H.; Skalli, W.; Ghanem, I. Validation of hip joint center localization methods during gait analysis using 3D EOS imaging in typically developing and cerebral palsy children. Gait Posture 2016, 48, 30–35. [Google Scholar] [CrossRef]
- Peters, A.; Baker, R.; Morris, M.E.; Sangeux, M. A comparison of hip joint centre localisation techniques with 3-DUS for clinical gait analysis in children with cerebral palsy. Gait Posture 2012, 36, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Della Croce, U.; Leardini, A.; Chiari, L.; Cappozzo, A. Human movement analysis using stereophotogrammetry: Part 4: Assessment of anatomical landmark misplacement and its effects on joint kinematics. Gait Posture 2005, 21, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Leardini, A.; Chiari, L.; Della Croce, U.; Cappozzo, A. Human movement analysis using stereophotogrammetry: Part 3. Soft tissue artifact assessment and compensation. Gait Posture 2005, 21, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, T.; Taetz, B.; Bleser, G. IMU-to-segment assignment and orientation alignment for the lower body using deep learning. Sensors 2018, 18, 302. [Google Scholar] [CrossRef]
- Cockcroft, J.; Muller, J.H.; Scheffer, C. A Novel Complimentary Filter for Tracking Hip Angles During Cycling Using Wireless Inertial Sensors and Dynamic Acceleration Estimation. IEEE Sens. J. 2014, 14, 2864–2871. [Google Scholar] [CrossRef]
- Roetenberg, D.; Luinge, H.; Slycke, P. Xsens MVN: Full 6DOF Human Motion Tracking Using Miniature Inertial Sensors; XSENS Technologies: Enschede, The Netherlands, 2009. [Google Scholar]
- Luinge, H.J.; Veltink, P.H. Inclination Measurement of Human Movement Using a 3-D Accelerometer with Autocalibration. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 112–121. [Google Scholar] [CrossRef]
- Luinge, H.J.; Veltink, P.H. Measuring orientation of human body segments using miniature gyroscopes and accelerometers. Med. Biol. Eng. Comput. 2005, 43, 273–282. [Google Scholar] [CrossRef]
- Foxlin, E. Inertial head-tracker sensor fusion by a complementary separate-bias Kalman filter. In Proceedings of the Virtual Reality Annual International Symposium, Santa Clara, CA, USA, 30 March–3 April 1996; pp. 185–194. [Google Scholar]
- Rehbinder, H.; Hu, X. Drift-free attitude estimation for accelerated rigid bodies. In Proceedings of the International Conference on Robotics & Automation, Seoul, Korea, 21–26 May 2001; Volume 4, pp. 4244–4249. [Google Scholar]
- Zhu, R.; Zhou, Z. A real-time articulated human motion tracking using tri-axis inertial/magnetic sensors package. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 295–302. [Google Scholar] [CrossRef]
- Barshan, B.; Durrant-Whyte, H.F. Inertial Navigation Systems for Mobile Robots. IEEE Trans. Robot. Autom. 1995, 11, 328–342. [Google Scholar] [CrossRef]
- Luis Marins, J.; Yun, X.; Bachmann, E.R.; McGhee, R.B.; Zyda, M.J. An Extended Kalman Filter for Quaternion-Based Orientation Estimation Using MARG Sensors. In Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems, Maui, HI, USA, 29 October–3 November 2001; Volume 4, pp. 2003–2011. [Google Scholar]
| Axis | Manual | Static | Functional | Anatomical | |
|---|---|---|---|---|---|
| Pelvis | Long | [36,37,39,47,72] | [24,34,40,41,42,43,44,45,49] | [46] | - |
| Medio-Lat | [36,37,39,42,47,72] | [24,41,42,43,44,45] | [44,46,49] | [27] | |
| Ant-Post | - | - | - | [27] | |
| Femur | Long | [49,50,51,52,53] | [26,31,32,33,34,36,37,38,40,41,42,43,44,45,49,54,55,56,57,58,59,60,61,65] | - | [27,28,62,63] |
| Medio-Lat | [47,50] | [26,41,42,59,65] | [26,31,33,34,36,37,38,43,44,46,49,54,55,56,57,66,67] | [27] | |
| Ant-Post | - | [34] | [32,34,43,46,57] | - | |
| Tibia-fibula | Long | [50,52,53,61] | [31,32,34,36,37,38,40,41,42,43,44,45,47,54,55,56,57,58,59,60,65,73] | [25] | [27,28,62,63] |
| Medio-Lat | [36,37,38,50,61] | [31,41,42,45,47,65,73] | [25,26,33,34,43,44,54,55,56,57,59,66,67,70] | [27] | |
| Ant-Post | - | [34] | [26,31,43,57] | - | |
| Foot | Long | - | [36,37,38,42,45] | - | [27] |
| Medio-Lat | - | [36,37,38,41,42,65] | [25,33,44,67,70] | - | |
| Ant-Post | [53,63] | [24,33,36,37,38,40,41,42,43,44,45,60] | [25] | [27] |
| Static Method | Functional Method | |||
|---|---|---|---|---|
| Acceleration | Angular Velocity | Acceleration | ||
| Mean | Mean | Principle Component Analysis | Least-Squares Method | Principle Component Analysis |
| [33,41,42,43,44,54,55,56,59,60,65] | [34,36,37,54,55,56,69] | [31,43,44,49,57,66] | [40,67,70] | [44] |
| Direct Kinematics | Optimized Kinematics | ||
|---|---|---|---|
| Conventional Gait Model or Similar | CAST Protocol or Similar | Functional Calibration | Kinematic Chain |
| [24,37,45,54,55,56] (Kadaba et al. [74], Plug In Gait, LAMB [83]) [47] (Motion analysis Cortex Software) [37] | [33,36,37,43,69] (CAST defined in [30]) [70] (Starthclyde functional Cluster Model defined in [75]) [37,39] (Total3D gait protocol defined in [84]) | [41,82] (hip joint centre as in [76]) [85] (hip joint centre as in [77]) [61] (hip joint centre)[37] (hip, knee joint centre [86]) [31] (hip, knee, ankle joint centre as in [78]) [26,59] (knee joint centre as in [79]) | [66] (Opensim) |
| Pelvis | Femur | Tibia-Fibula | Foot | |
|---|---|---|---|---|
| [34] | 10.9 (1.6) | 11.8 (2.8) | ||
| [33] | 6.1 (3.4) * | 17 (4.4) * | 12.2 (1.7) * | |
| [43] | 9.7 (3.44) * | 4.3 (1.7) * | 11 (2.6) * | 9.5 (2.2) * |
| [43] | 9.9 (3.23) * | 14.7 (5.17) * |
| Reference | Pelvis | Hip | Knee | Ankle | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tilt | Obliquity | Rotation | Flex-Ext | Abd-Add | Int-Ext | Flex-Ext | Abd-Add | Rotation | Flex-Ext | Abd-Add | Int-Ext | |
| [73] | 8.72 | 4.96 | 6.79 | |||||||||
| [52] | 4.46 | 3.96 | 3.75 | |||||||||
| [87] | 5.8 (1.8) *,● | 7.0 (4.0) *,● | 5.6 (2.6) *,● | |||||||||
| [53] | 5 (4.2–5.2) *,● | 3.5 (3.9–2.5) *,● | ||||||||||
| [58] | 3.63(1.23) | |||||||||||
| [41] | 10.74 | 7.88 | 9.75 | |||||||||
| [49] | 2.6 (2.0) | 2.7 (2.0) | 6.0 (4.0) | |||||||||
| [61] | 5.33 (2.01) | |||||||||||
| [28] | 1.30 | |||||||||||
| [62] | 1.69 (0.48) | 0.78 (0.17) | ||||||||||
| [27] | 0.8 | 1.5 | 1.8 | 1.9 | 2.8 | 3.6 | 1.2 | 2.2 | 3.5 | |||
| [25] | 0.49 (0.4) ● | 1.6 *,● | 3.33 (1.7) ● | |||||||||
| [26] | 8.1 (5.4) | 6.2 (5.1) | 4.0 (4.7) | |||||||||
| [66] | 9.69 (4.35) | |||||||||||
| [32] | 1.5 (0.4) ◊ | 1.7 (0.5) ◊ | 1.6 (0.5) ◊ | |||||||||
| [38] | 8.8 (4.1) ● | 6.5 (3.5) ● | 13.8 (8.6) ● | 6.2 (2.0) ● | 9.2 (6.0) ● | 16.1 (9.8) ● | 4.6 (3.4) ● | 6.0 (1.1) ● | 11.2 (2.5) ● | |||
| [43] | 3.1 (1.2) | 2.2 (0.7) | 6.9 (1.4) | 2.7 (0.8) | 3.6 (1.0) | 8 (3.3) | 3.2 (1.0) | 2.7 (1.1) | 4.7 (2.0) | |||
| [33] | 2.6 (0.8) | 3.5 (1.0) | 8.1 (3.5) | 3.6 (1.0) | 3.3 (1.4) | 4.7 (1.9) | ||||||
| [34] | 3.74 (2.99) | 5.92 (2.85) | 6.65 (1.94) | |||||||||
| [59] | 3.4 (2.2) | 5.6 (3.3) | 5.5 (5.3) | |||||||||
| [44] | 0.9 (0.5) | 1.1 (0.9) | 1.5 (1.8) | 2.0 (1.2) | 2.7 (2.1) | 2.4 (1.5) | 4.1 (3.1) | 3.6 (2.3) | 3.3 (2.1) | 2.5 (1.7) | 3.3 (2.5) | 2.4 (4.3) |
| [2] | 3.86 | 0.98 | ||||||||||
| [46] | 3.68 | 2.51 | ||||||||||
| [3] | 11.6 (4.8) | 5.3 (1.8) | 8 (3.1) | 6.3 (3.2) | 5.1 (2.1) | 3.6 (1.3) | 3.8 (1.8) |
| Reference | Hip | Knee | Ankle | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Flex-Ext | Abd-Add | Int-Ext | Flex-Ext | Abd-Add | Rotation | Flex-Ext | Abd-Add | Int-Ext | |
| [73] | 0.88 | 0.72 | 0.92 | ||||||
| [52] | 0.92 | 0.91 | 0.91 | ||||||
| [87] | 0.97 | 0.95 | 0.82 | ||||||
| [53] | 0.99 * | 0.92 * | |||||||
| [58] | 0.975 (0.026) | ||||||||
| [41] | 0.98 | 0.97 | 0.78 | ||||||
| [65] | 0.964 | 0.9075 | 0.954 | 0.966 | 0.8675 | 0.707 | 0.954 | ||
| [28] | 0.99 | ||||||||
| [62] | 0.99 | 0.99 | |||||||
| [27] | 0.97 (0.03) | ||||||||
| [26] | 1.00 (0.00) | 0.76 (0.18) | 0.85 (0.11) | ||||||
| [37] | 0.999 | 0.994 | 0.973 | 0.999 | 0.988 | 0.939 | 0.750 | ||
| [46] | 0.96 | 0.83 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pacher, L.; Chatellier, C.; Vauzelle, R.; Fradet, L. Sensor-to-Segment Calibration Methodologies for Lower-Body Kinematic Analysis with Inertial Sensors: A Systematic Review. Sensors 2020, 20, 3322. https://doi.org/10.3390/s20113322
Pacher L, Chatellier C, Vauzelle R, Fradet L. Sensor-to-Segment Calibration Methodologies for Lower-Body Kinematic Analysis with Inertial Sensors: A Systematic Review. Sensors. 2020; 20(11):3322. https://doi.org/10.3390/s20113322
Chicago/Turabian StylePacher, Léonie, Christian Chatellier, Rodolphe Vauzelle, and Laetitia Fradet. 2020. "Sensor-to-Segment Calibration Methodologies for Lower-Body Kinematic Analysis with Inertial Sensors: A Systematic Review" Sensors 20, no. 11: 3322. https://doi.org/10.3390/s20113322
APA StylePacher, L., Chatellier, C., Vauzelle, R., & Fradet, L. (2020). Sensor-to-Segment Calibration Methodologies for Lower-Body Kinematic Analysis with Inertial Sensors: A Systematic Review. Sensors, 20(11), 3322. https://doi.org/10.3390/s20113322





