Development of User-Friendly Wearable Electronic Textiles for Healthcare Applications
Abstract
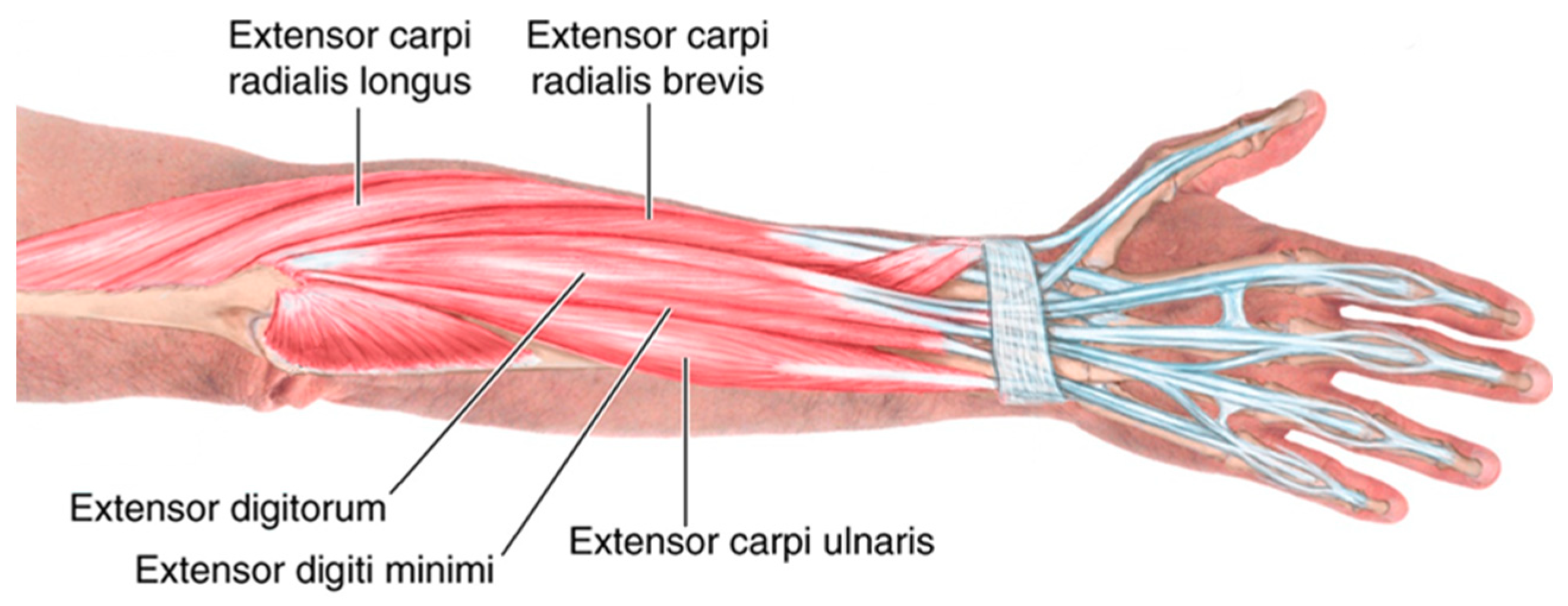
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. E-Sleeve Fabrication Process
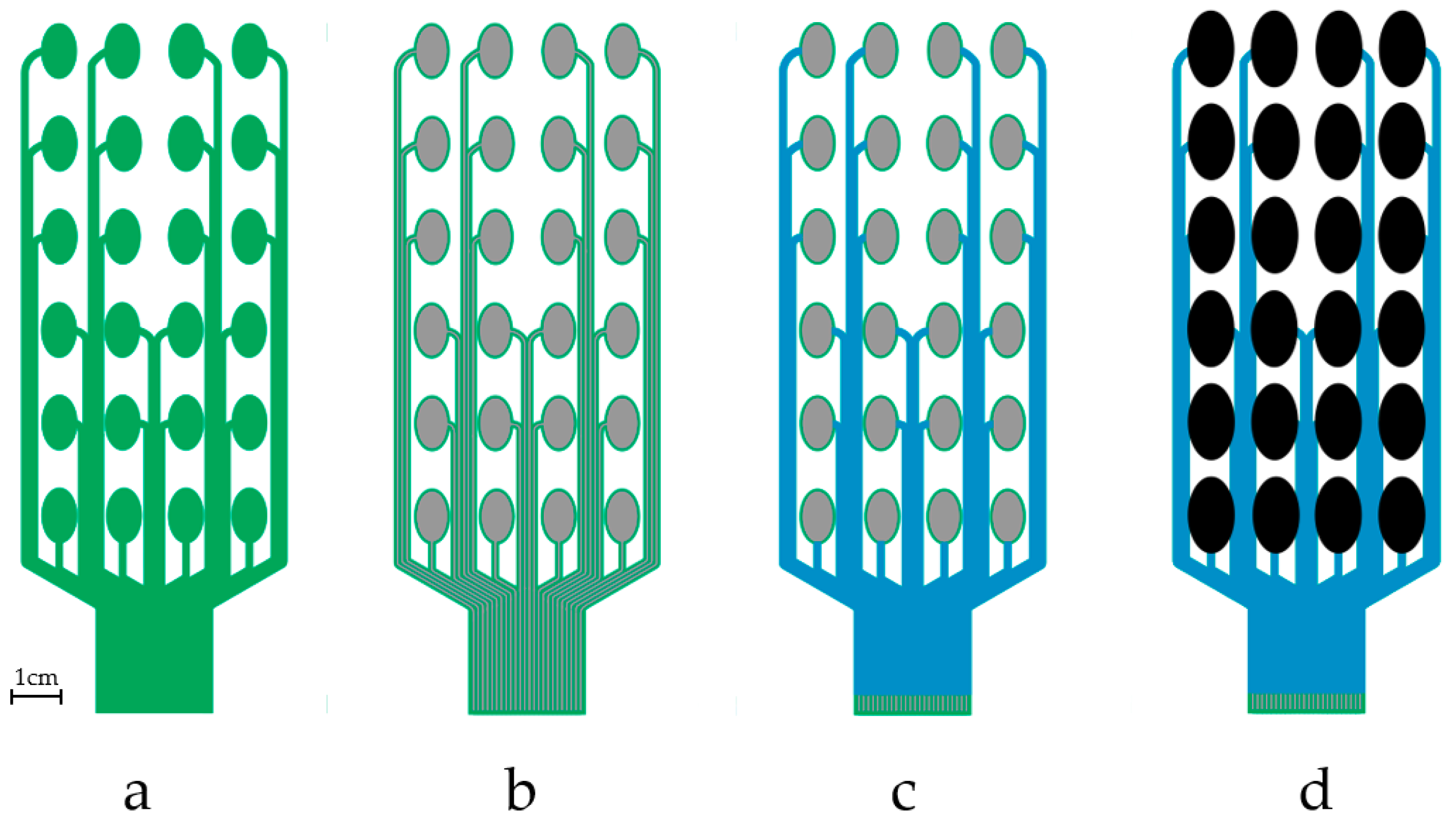
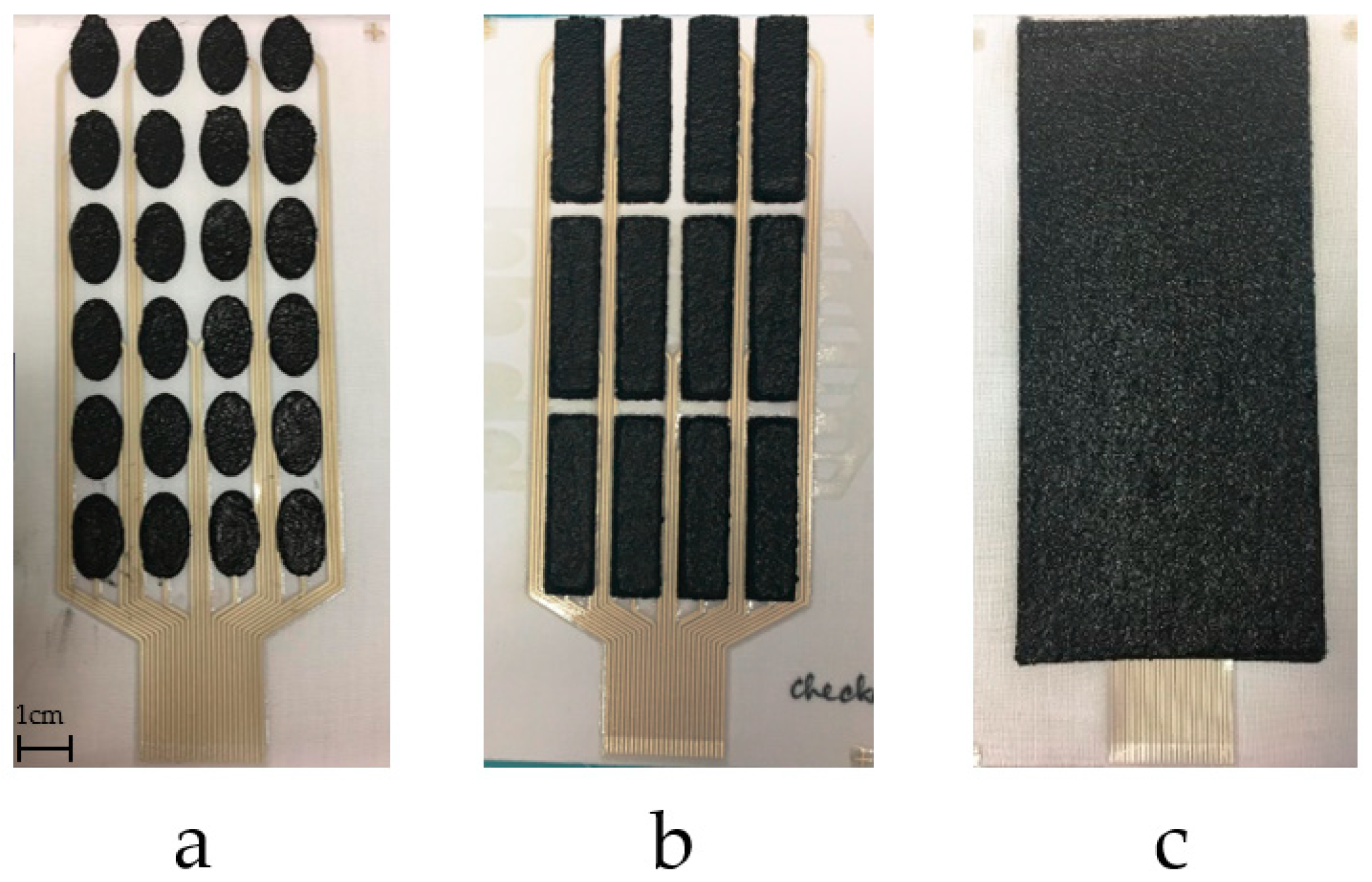
2.2.1. Fabric Electrode Array Fabrication
- (1)
- Print interface layer to create a smooth and flexible surface on to which the silver paste can be printed. A 250 thread/inch stainless steel screen with 40 μm emulsion thickness supplied by MCI Precision Screens Ltd. (Melbourn, UK). was used. The interface layer was formed using two prints of Fabink IF-UV-1039 followed one print of Fabink IF-UV-1004. Using two types of interface provides waterproof properties and details have been published in our previous work [31]. UV curing was applied after each print by exposing the sample to a 400 W mercury (Hg) bulb in a UV cabinet supplied by UV Light Technology Ltd. (Birmingham, UK). The UV curing time was 60 s for Fabink IF-UV-1039 and 30 s for Fabink IF-UV1004. The total thickness of the interface is 170 μm.
- (2)
- Print conductive layer to create the conductive tracks and conductive pads. A 120 thread/cm polyester screen with 10 μm emulsion thickness was used. The conductive layer was formed using one print of Fabink TC-C4007. The paste was cured in a box oven at 130 °C for 25 min. The thickness of the conductive silver layer is 8 μm.
- (3)
- Print encapsulation to protect the conductive tracks and provide electrical insulation. A 250 thread/inch stainless steel screen with 30 μm emulsion thickness was used in the encapsulation layer printing. The encapsulation layer was formed using one print of Fabink IF-UV1004 followed by two print of Fabink IF-UV-1039 and cured as specified before. The thickness of the encapsulation layer is 110 μm.
- (4)
- Print dry electrode to provide interface between the conductive pads and the skin. A thick stainless steel stencil screen was used in the electrode layer printing. The electrode paste was cured in a box oven at 80 °C for 30 min leaving a dry electrode layer with a thickness of 1 mm. In addition to the electrode layout shown in Figure 3d, three other types of electrodes layout were also fabricated and evaluated as discussed later in Section 3.1.
2.2.2. E-Sleeve Co-Design with End Users
2.3. Durability Test
- (1)
- Electrodes were placed in a sterile tube containing tryptone soya broth and autoclaved glass beads.
- (2)
- The tubes were vortex mixed for 2 min to remove any attached bacteria.
- (3)
- Aliquots of 50 μL were spread over tryptone soya agar plates.
- (4)
- Agar plates were incubated at 37 °C, overnight, before colonies were counted.
2.4. Muscle Stimulation Testing
- (1)
- At the beginning of the session, the pulse width applied to a central element in the array is slowly increased until a comfortable limit is found. This is set as the maximum pulse width that that can be applied to any channel for the individual user.
- (2)
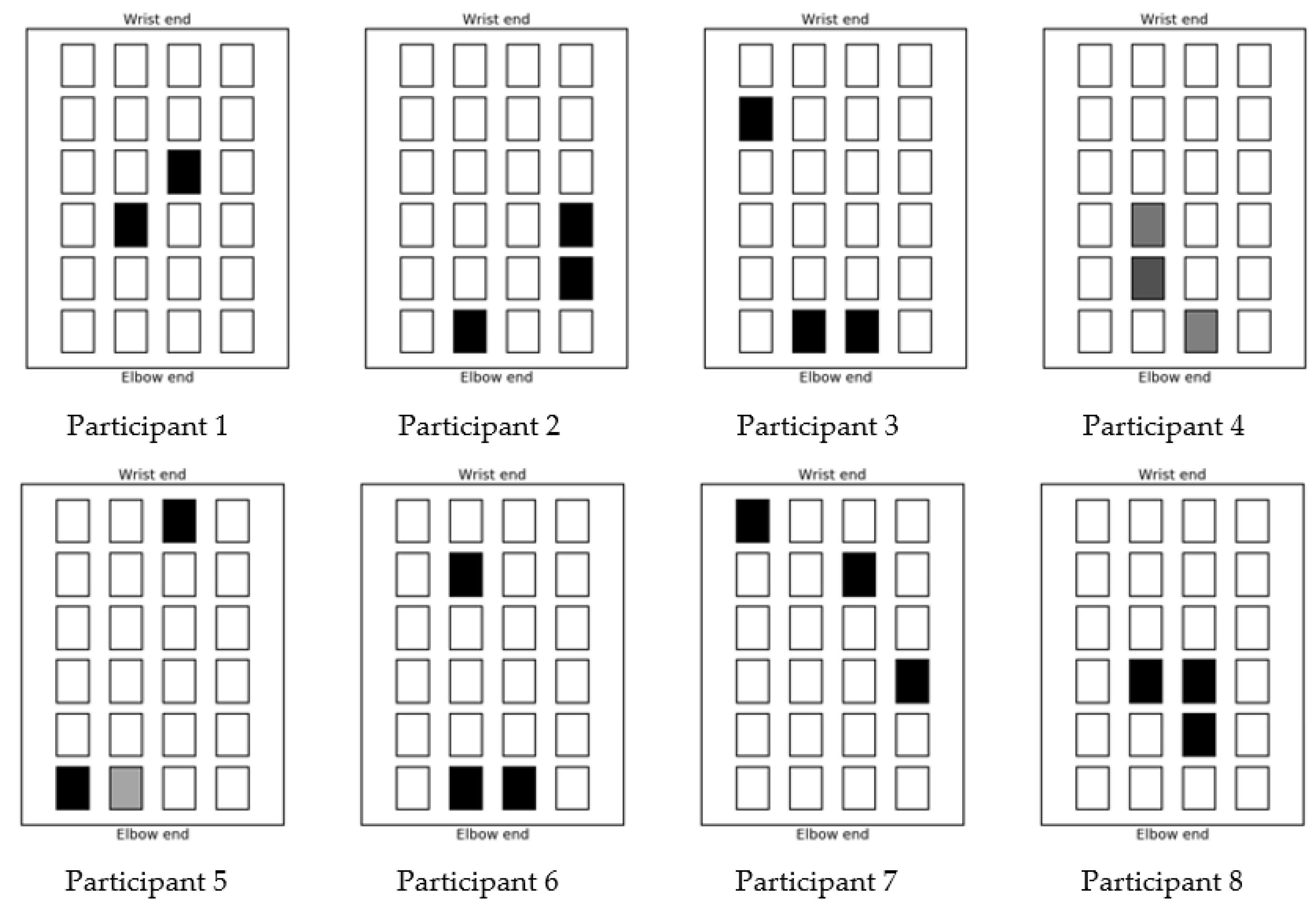
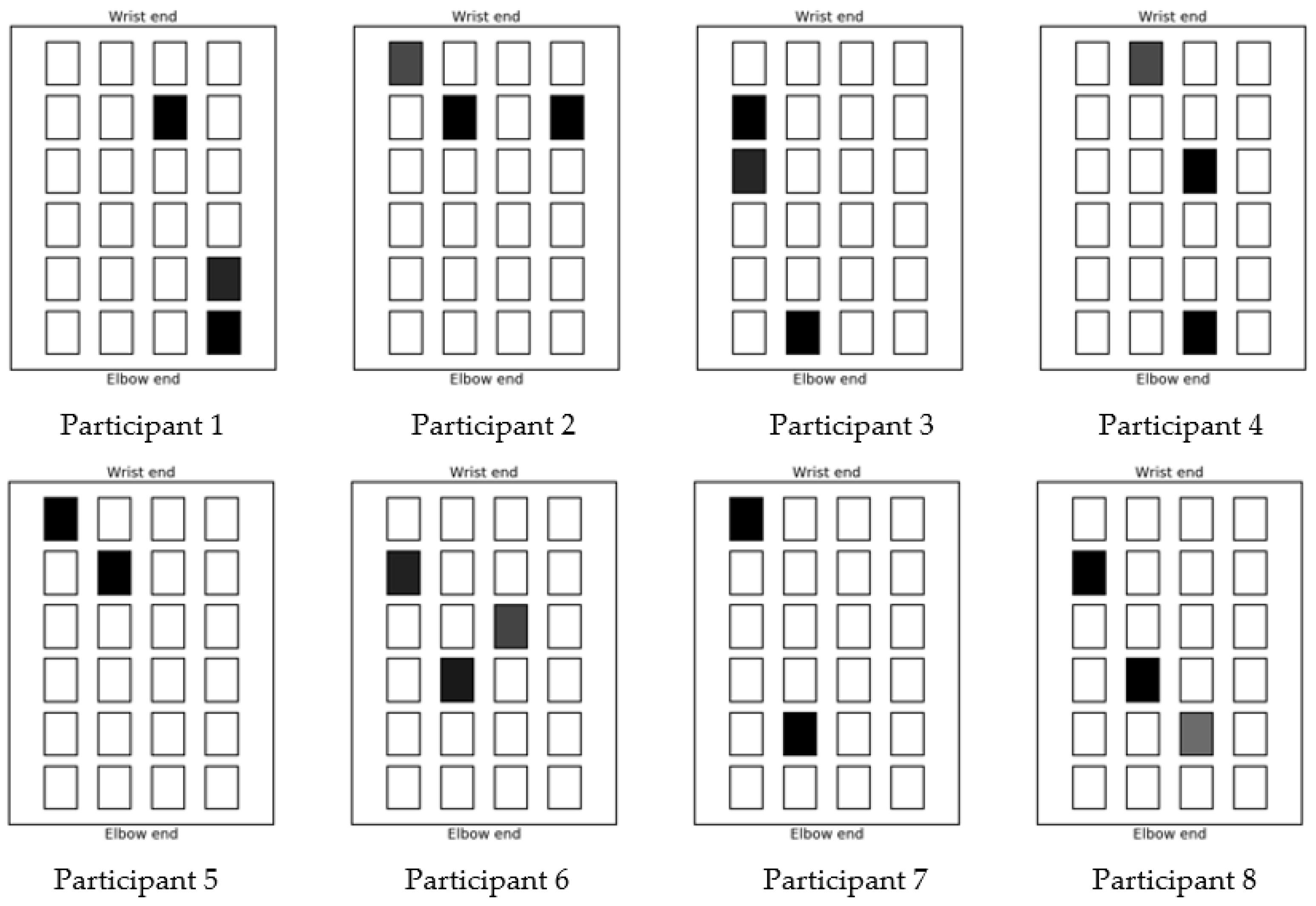
- The control algorithm then applies stimulation to each electrode in turn, using a triangular pulse width profile of 6 s duration. At the end of this profile the stimulation is removed and a further 1 s waiting period is provided to allow the hand to return to its initial position. During each profile, the angular movement produced by the hand and wrist is recorded using the movement sensor. This comprises 2 wrist angles and 10 finger angles. The slope of each joint angle is computed via least-squares fitting. When repeated over the 24 electrodes, this produces a 12 by 24 matrix which captures the static response to stimulation.
- (3)
- For each test, the sensor then records the initial and desired final angular positions for the target gesture (e.g., hand opening, pointing).
- (4)
- The control system then uses the desired movement (from (3)), together with the response matrix (from (2)) to compute a set of array elements and associated pulse width values which is best able to achieve the intended movement. For ease of computation, and to minimize the effect of nonlinearity, a set of only 3 elements is stipulated.
3. Results and Discussion
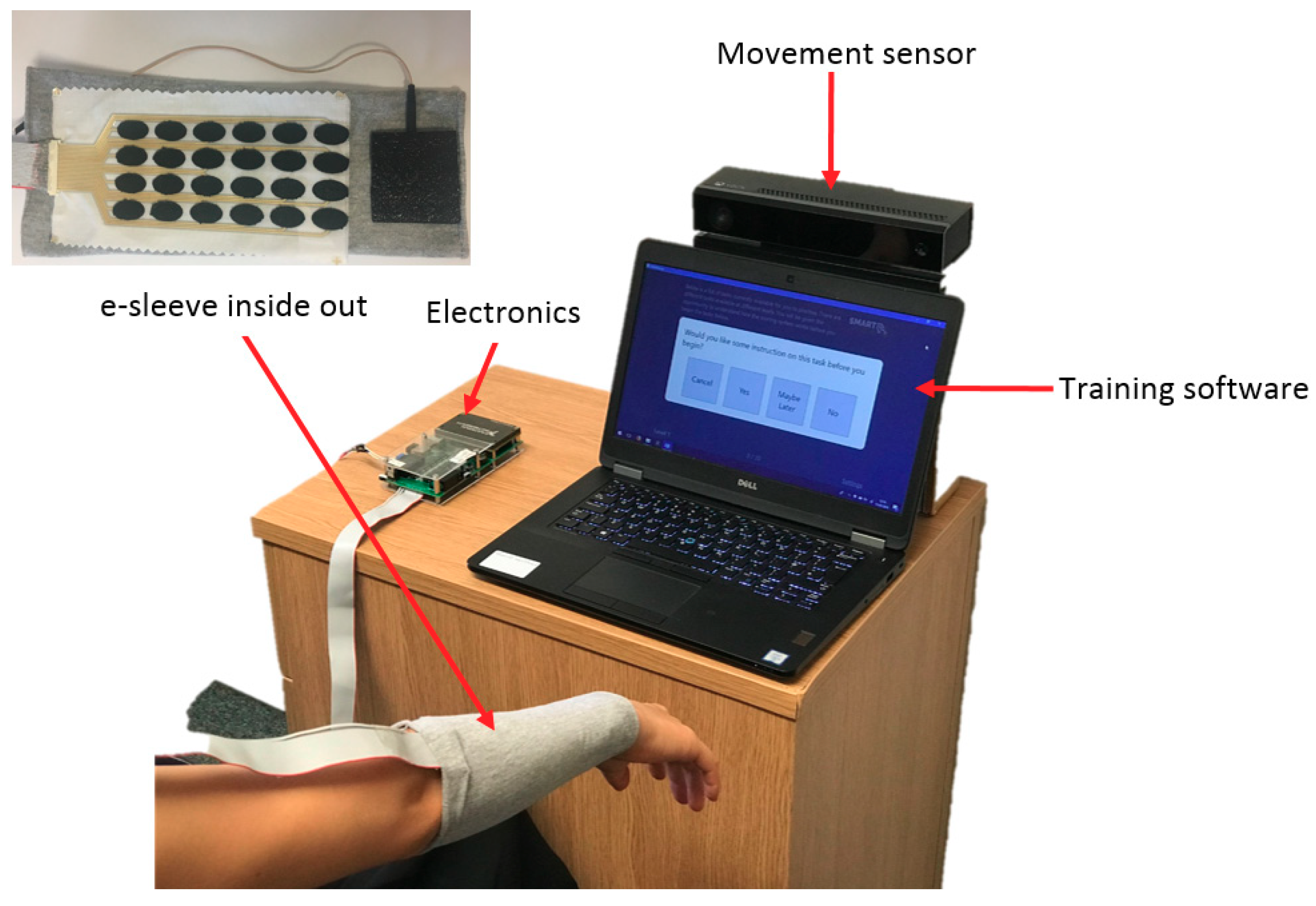
3.1. Fabric Electrode Array and E-Sleeve Fabrication
- (1)
- The electronics was contained in a pocket that was included on the e-sleeve
- (2)
- The electronics was connected via a lead and either clipped onto clothing, placed in a pocket or left on the table.
3.2. Fabric Electrode Array Durability Tests
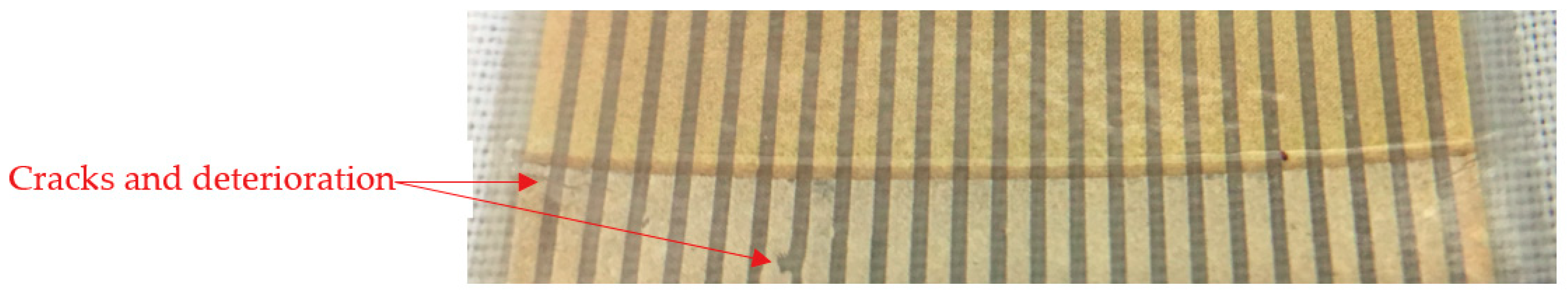
3.2.1. Bending Test
3.2.2. Cleaning Tests
3.3. Muscle Stimulation Test
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lund, A.; van der Velden, N.M.; Persson, N.-K.; Hamedi, M.M.; Müller, C. Electrically conducting fibres for e-textiles: An open playground for conjugated polymers and carbon nanomaterials. Mater. Sci. Eng. R. Rep. 2018, 126, 1–29. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, W.; Jiang, Z.; Yu, D. Low temperature sintering nano-silver conductive ink printed on cotton fabric as printed electronics. Prog. Org. Coat. 2016, 101, 604–611. [Google Scholar] [CrossRef]
- Matsuhisa, N.; Kaltenbrunner, M.; Yokota, T.; Jinno, H.; Kuribara, K.; Sekitani, T.; Someya, T. Printable elastic conductors with a high conductivity for electronic textile applications. Nat. Commun. 2015, 6, 7461. [Google Scholar] [CrossRef] [PubMed]
- Hardy, D.; Moneta, A.; Sakalyte, V.; Connolly, L.; Shahidi, A.; Hughes-Riley, T. Engineering a Costume for Performance Using Illuminated LED-Yarns. Fibers 2018, 6, 35. [Google Scholar] [CrossRef]
- Hughes-Riley, T.; Dias, T. Developing an Acoustic Sensing Yarn for Health Surveillance in a Military Setting. Sensors 2018, 18, 1590. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.J.; Hong, W.G.; Kim, D.Y.; Kim, H.J.; Jun, Y.; Lee, H.-K. E-textile gas sensors composed of molybdenum disulfide and reduced graphene oxide for high response and reliability. Sens. Actuators B Chem. 2017, 248, 829–835. [Google Scholar] [CrossRef]
- Hughes-Riley, T.; Lugoda, P.; Dias, T.; Trabi, C.; Morris, R. A Study of Thermistor Performance within a Textile Structure. Sensors 2017, 17, 1804. [Google Scholar] [CrossRef] [PubMed]
- Katragadda, R.B.; Xu, Y. A novel intelligent textile technology based on silicon flexible skins. Sens. Actuators A Phys. 2008, 143, 169–174. [Google Scholar] [CrossRef]
- Michael, B.; Howard, M. Activity recognition with wearable sensors on loose clothing. PLoS ONE 2017, 12, e0184642. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.K.; Singh, V.K.; Naresh, B. Textile Antenna for Microwave Wireless Power Transmission. Procedia Comput. Sci. 2016, 85, 856–861. [Google Scholar] [CrossRef]
- Grabham, N.J.; Li, Y.; Clare, L.R.; Stark, B.H.; Beeby, S.P. Fabrication techniques for manufacturing flexible coils on textiles for inductive power transfer. IEEE Sens. J. 2018, 18, 2599–2606. [Google Scholar] [CrossRef]
- Carey, T.; Cacovich, S.; Divitini, G.; Ren, J.; Mansouri, A.; Kim, J.M.; Wang, C.; Ducati, C.; Sordan, R.; Torrisi, F. Fully inkjet-printed two-dimensional material field-effect heterojunctions for wearable and textile electronics. Nat. Commun. 2017, 8, 1202. [Google Scholar] [CrossRef] [PubMed]
- Marculescu, D.; Marculescu, R.; Zamora, N.H.; Stanley-Marbell, P.; Khosla, P.K.; Park, S.; Jayaraman, S.; Jung, S.; Lauterbach, C.; Weber, W.; et al. Electronic textiles: A platform for pervasive computing. Proc. IEEE 2003, 91, 1995–2018. [Google Scholar] [CrossRef]
- Sun, F.; Yi, C.; Li, W.; Li, Y. A wearable H-shirt for exercise ECG monitoring and individual lactate threshold computing. Comput. Ind. 2017, 92, 1–11. [Google Scholar] [CrossRef]
- Paul, G.; Torah, R.; Beeby, S.; Tudor, J. Novel active electrodes for ECG monitoring on woven textiles fabricated by screen and stencil printing. Sens. Actuators A Phys. 2015, 221, 60–66. [Google Scholar] [CrossRef]
- Paul, G.M.; Cao, F.; Torah, R.; Yang, K.; Beeby, S.; Tudor, J. A Smart Textile Based Facial EMG and EOG Computer Interface. IEEE Sens. J. 2014, 14, 393–400. [Google Scholar] [CrossRef]
- Wei, Y.; Wu, Y.; Tudor, J. A real-time wearable emotion detection headband based on EEG measurement. Sens. Actuators A Phys. 2017, 263, 614–621. [Google Scholar] [CrossRef]
- Akita, J.; Shinmura, T.; Sakurazawa, S.; Yanagihara, K.; Kunita, M.; Toda, M.; Iwata, K. Wearable electromyography measurement system using cable-free network system on conductive fabric. Artif. Intell. Med. 2008, 42, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Belbasis, A.; Fuss, F.K.; Sidhu, J. Muscle Activity Analysis with a Smart Compression Garment. Procedia Eng. 2015, 112, 163–168. [Google Scholar] [CrossRef]
- Stewart, A.M.; Pretty, C.G.; Chen, X. An Evaluation of the Effect of Stimulation Parameters and Electrode Type on Bicep Muscle Response for a Voltage-controlled Functional Electrical Stimulator. IFAC-PapersOnLine 2017, 50, 15109–15114. [Google Scholar] [CrossRef]
- Zhou, H.; Lu, Y.; Chen, W.; Wu, Z.; Zou, H.; Krundel, L.; Li, G. Stimulating the Comfort of Textile Electrodes in Wearable Neuromuscular Electrical Stimulation. Sensors 2015, 15, 17241. [Google Scholar] [CrossRef] [PubMed]
- State of the Nation Stroke Statistics. Available online: https://www.stroke.org.uk/system/files/sotn_2018.pdf (accessed on 1 June 2018).
- National Clinical Guidelines for Stroke. Available online: https://www.strokeaudit.org/SupportFiles/Documents/Guidelines/2016-National-Clinical-Guideline-for-Stroke-5t-(1).aspx (accessed on 24 June 2018).
- Howlett, O.A.; Lannin, N.A.; Ada, L.; McKinstry, C. Functional Electrical Stimulation Improves Activity after Stroke: A Systematic Review with Meta-Analysis. Arch. Phys. Med. Rehabil. 2015, 96, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Veerbeek, J.M.; van Wegen, E.; van Peppen, R.; van der Wees, P.J.; Hendriks, E.; Rietberg, M.; Kwakkel, G. What Is the Evidence for Physical Therapy Poststroke? A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e87987. [Google Scholar] [CrossRef] [PubMed]
- Popović, D.B. Advances in functional electrical stimulation (FES). J. Electromyogr. Kinesiol. 2014, 24, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, A.; Keller, T.; Micera, S.; Morari, M. Array electrode design for transcutaneous electrical stimulation: A simulation study. Med. Eng. Phys. 2009, 31, 945–951. [Google Scholar] [CrossRef] [PubMed]
- Malešević, N.M.; Maneski, L.Z.P.; Ilić, V.; Jorgovanović, N.; Bijelić, G.; Keller, T.; Popović, D.B. A multi-pad electrode based functional electrical stimulation system for restoration of grasp. J. Neuroeng. Rehabil. 2012, 9, 66. [Google Scholar] [CrossRef] [PubMed]
- Malešević, J.; Dedijer Dujović, S.; Savić, A.M.; Konstantinović, L.; Vidaković, A.; Bijelić, G.; Malešević, N.; Keller, T. A decision support system for electrode shaping in multi-pad FES foot drop correction. J. Neuroeng. Rehabil. 2017, 14, 66. [Google Scholar] [CrossRef] [PubMed]
- Koutsou, A.D.; Moreno, J.C.; del Ama, A.J.; Rocon, E.; Pons, J.L. Advances in selective activation of muscles for non-invasive motor neuroprostheses. J. Neuroeng. Rehabil. 2016, 13, 56. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Torah, R.; Wei, Y.; Beeby, S.; Tudor, J. Waterproof and durable screen printed silver conductive tracks on textiles. Text. Res. J. 2013, 83, 2023–2031. [Google Scholar] [CrossRef]
- Yang, K.; Freeman, C.; Torah, R.; Beeby, S.; Tudor, J. Screen printed fabric electrode array for wearable functional electrical stimulation. Sens. Actuators A Phys. 2014, 213, 108–115. [Google Scholar] [CrossRef]
- Scoones, R. Cleaning Liquid. WO2015028806A1, 29 August 2014. [Google Scholar]
- Freeman, C.T. Electrode array-based electrical stimulation using ILC with restricted input subspace. Control Eng. Pract. 2014, 23, 32–43. [Google Scholar] [CrossRef]
- Freeman, C. Control System Design for Electrical Stimulation in Upper Limb Rehabilitation; Springer International Publishing: Basel, Switzerland, 2016. [Google Scholar]






| Pastes | Functionality | Curing Conditions |
|---|---|---|
| Fabink UV-IF-1004 | Standard interface to create smooth surface on various fabrics | UV light, 30 s |
| Fabink UV-IF-1039 | Waterproof interface and encapsulation suitable for various fabrics | UV light, 60 s |
| Fabink TC-C4007 | Silver ink for printing flexible conductor layer on top of the interface layer | 120–130 °C, 10–25 min |
| Fabink TC-E0002 | Silicone rubber carbon paste for printing dry electrode on top of the conductive layer | 80 °C, 30 min |
| Color | Black | White | Gray | Red | Blue |
|---|---|---|---|---|---|
| Participant No. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Maximum comfort stimulation level | 30 | 65 | 70 | 50 | 50 | 41 | 62 | 100 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, K.; Meadmore, K.; Freeman, C.; Grabham, N.; Hughes, A.-M.; Wei, Y.; Torah, R.; Glanc-Gostkiewicz, M.; Beeby, S.; Tudor, J. Development of User-Friendly Wearable Electronic Textiles for Healthcare Applications. Sensors 2018, 18, 2410. https://doi.org/10.3390/s18082410
Yang K, Meadmore K, Freeman C, Grabham N, Hughes A-M, Wei Y, Torah R, Glanc-Gostkiewicz M, Beeby S, Tudor J. Development of User-Friendly Wearable Electronic Textiles for Healthcare Applications. Sensors. 2018; 18(8):2410. https://doi.org/10.3390/s18082410
Chicago/Turabian StyleYang, Kai, Katie Meadmore, Chris Freeman, Neil Grabham, Ann-Marie Hughes, Yang Wei, Russel Torah, Monika Glanc-Gostkiewicz, Steve Beeby, and John Tudor. 2018. "Development of User-Friendly Wearable Electronic Textiles for Healthcare Applications" Sensors 18, no. 8: 2410. https://doi.org/10.3390/s18082410
APA StyleYang, K., Meadmore, K., Freeman, C., Grabham, N., Hughes, A.-M., Wei, Y., Torah, R., Glanc-Gostkiewicz, M., Beeby, S., & Tudor, J. (2018). Development of User-Friendly Wearable Electronic Textiles for Healthcare Applications. Sensors, 18(8), 2410. https://doi.org/10.3390/s18082410








