Ethnobotanical Survey on Plants Used to Manage Febrile Illnesses among Herbalists in Casablanca, Morocco
Abstract
1. Introduction
2. Material and Methods
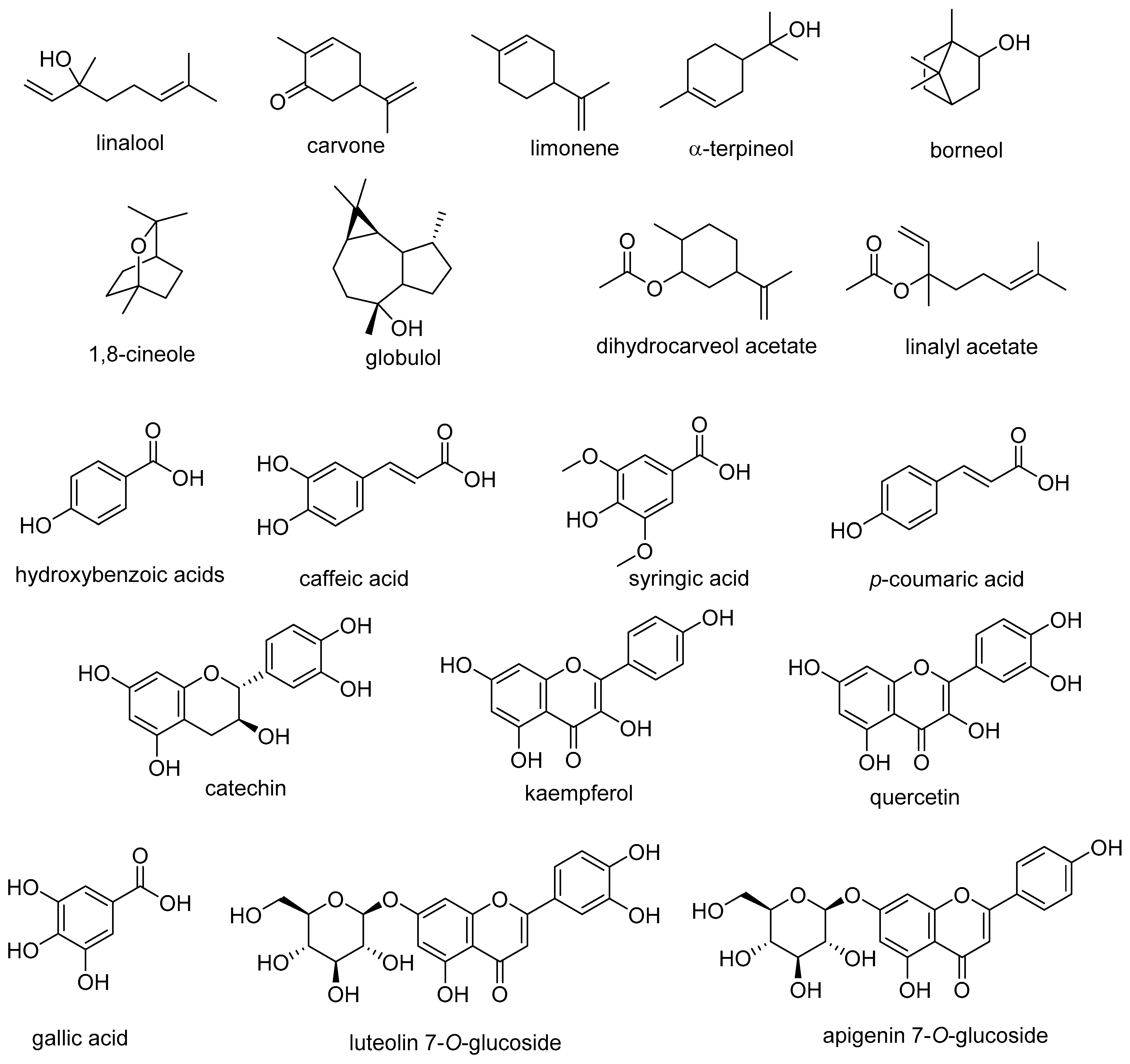
2.1. Study Zone
2.2. Data Gathering
2.3. Data Analysis
2.3.1. Use Value (UV)
2.3.2. Frequency of Citation (FC)
2.3.3. Relative Frequency of Citation (RFC)
2.3.4. Fidelity Level
2.3.5. Informant Consensus Factor
2.4. Bibliographic Review
3. Results
3.1. Socio-Demographic Data
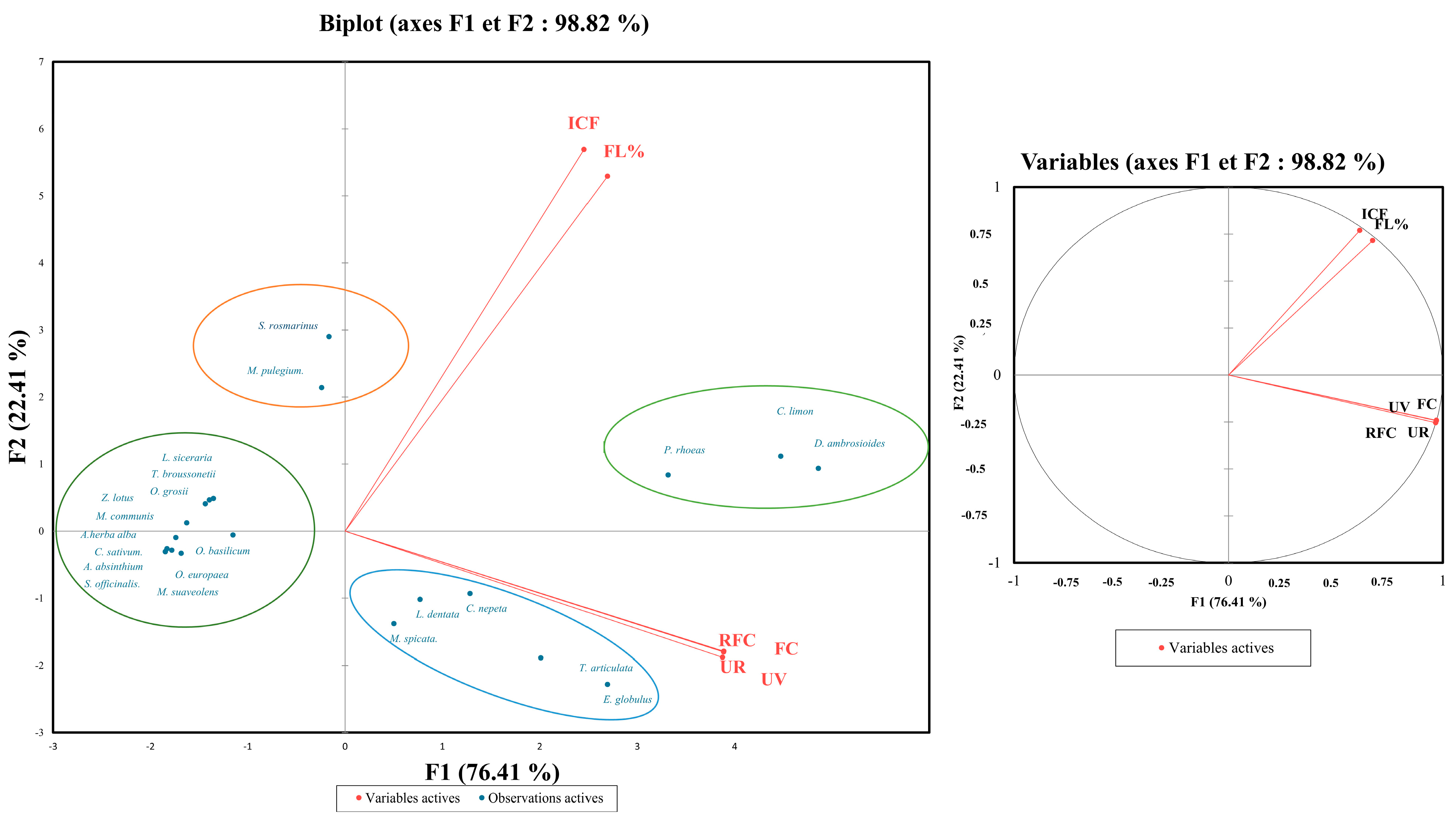
3.2. Quantitative Analysis
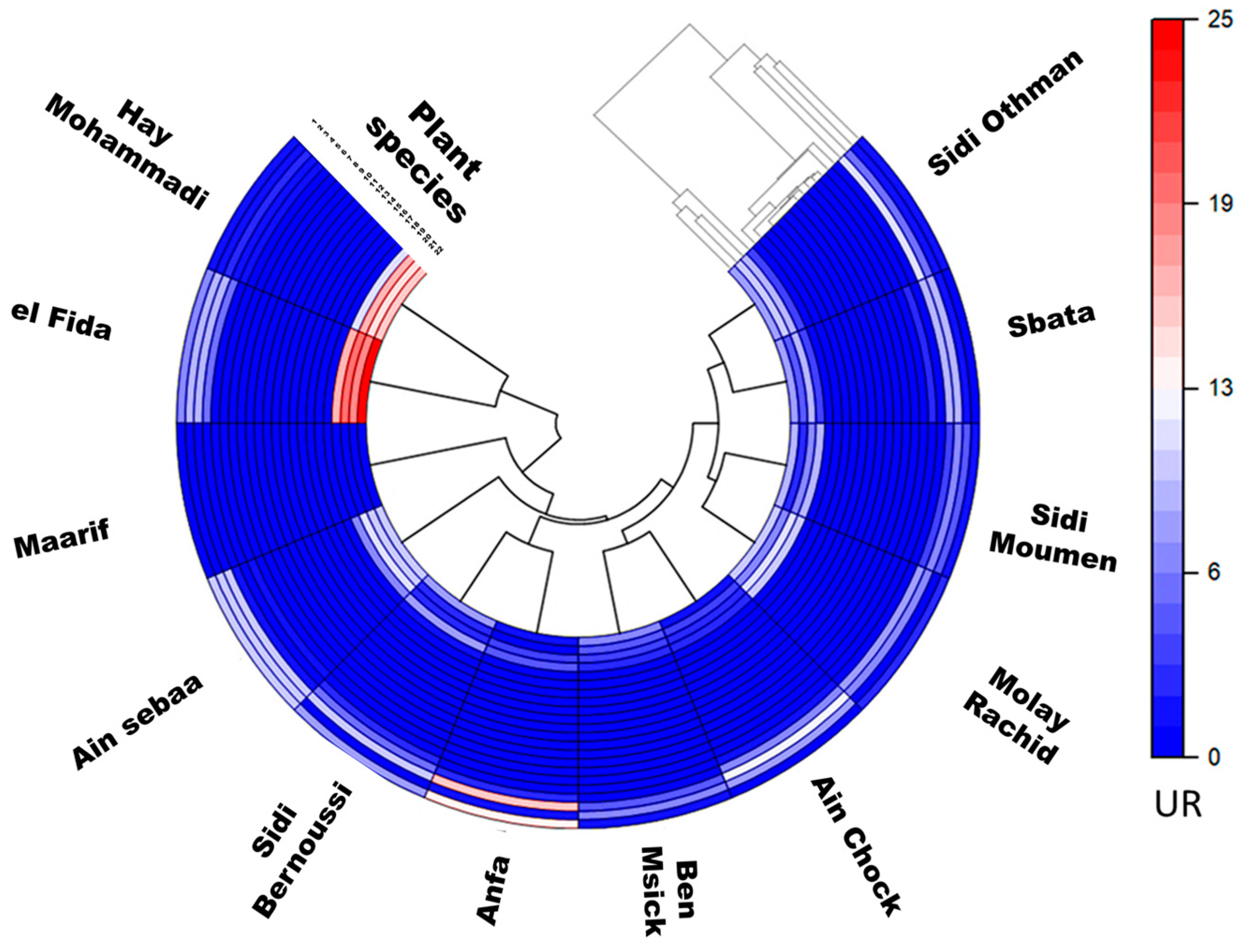
3.3. Relative Frequency of Citation and Use Value
3.4. Fidelity Level
3.5. Informant Consensus Factor
3.6. Method of Administration and Preparation
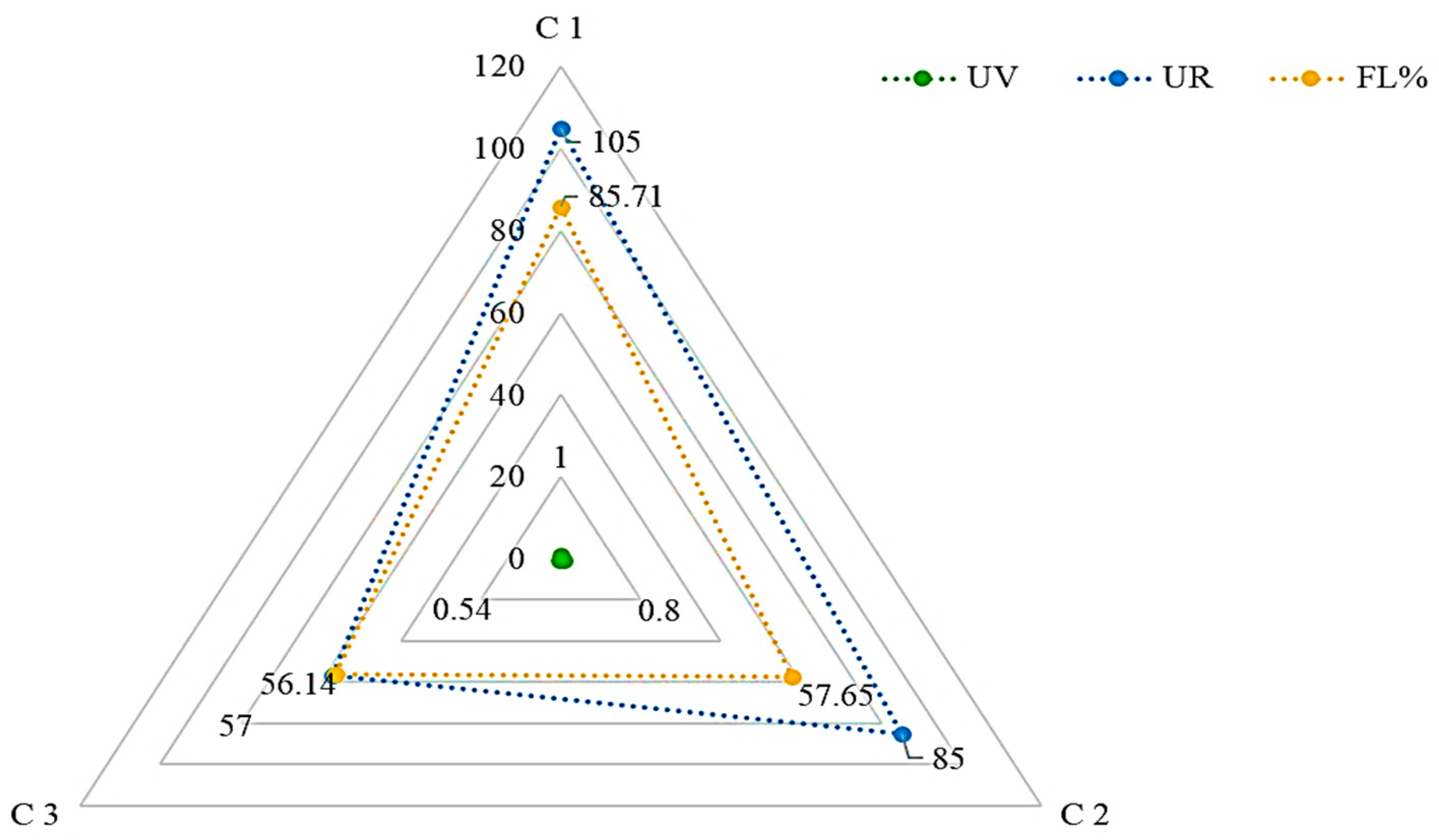
3.7. Medicinal Uses of Combined Plants
4. Discussion
4.1. Limitations of the Study
4.2. Conclusions and Recommendations for Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Walter, E.J.; Hanna-Jumma, S.; Carraretto, M.; Forni, L. The pathophysiological basis and consequences of fever. Crit. Care 2016, 20, 200. [Google Scholar] [CrossRef]
- Roberts, T.; Dahal, P.; Shrestha, P.; Schilling, W.; Shrestha, R.; Ngu, R.; Huong, V.T.L.; van Doorn, H.R.; Phimolsarnnousith, V.; Miliya, T. Antimicrobial resistance patterns in bacteria causing febrile illness in Africa, South Asia and Southeast Asia: A systematic review of published aetiological studies from 1980–2015. Int. J. Infect. Dis. 2022, 122, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Abdel Wahab, M.F.; Younis, T.A.; Fahmy, I.A.; El Gindy, I.M. Parasitic infections presenting as prolonged fevers. J. Egypt. Soc. Parasitol. 1996, 26, 509–516. [Google Scholar] [PubMed]
- Merle, H.; Donnio, A.; Jean-Charles, A.; Guyomarch, J.; Hage, R.; Najioullah, F.; Césaire, R.; Cabié, A. Ocular manifestations of emerging arboviruses: Dengue fever, Chikungunya, Zika virus, West Nile virus, and yellow fever. J. Fr. Ophtalmol. 2018, 41, e235–e243. [Google Scholar] [CrossRef] [PubMed]
- Mayxay, M.; Castonguay-Vanier, J.; Chansamouth, V.; Dubot-Pérès, A.; Paris, D.H.; Phetsouvanh, R.; Tangkhabuanbutra, J.; Douangdala, P.; Inthalath, S.; Souvannasing, P. Causes of non-malarial fever in Laos: A prospective study. Lancet Glob. Health 2013, 1, e46–e54. [Google Scholar] [CrossRef]
- Crump, J.A. Time for a comprehensive approach to the syndrome of fever in the tropics. Trans. R. Soc. Trop. Med. Hyg. 2014, 108, 61–62. [Google Scholar] [CrossRef]
- Ogoina, D. Fever, fever patterns and diseases called ‘fever’—A review. J. Infect. Public Health 2011, 4, 108–124. [Google Scholar] [CrossRef]
- Dinarello, C.A.; Gelfand, J.A. Fever and hyperthermia. Harrisons Princ. Intern. Med. 2005, 16, 104. [Google Scholar]
- Ames, N.J.; Powers, J.H.; Ranucci, A.; Gartrell, K.; Yang, L.; Van Raden, M.; Leidy, N.K.; Wallen, G.R. A systematic approach for studying the signs and symptoms of fever in adult patients: The fever assessment tool (FAST). Health Qual. Life Outcomes 2017, 15, 1–11. [Google Scholar] [CrossRef]
- World Health Organization. Integrated Management of Childhood Illness; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- O’Grady, N.P.; Barie, P.S.; Bartlett, J.G.; Bleck, T.; Carroll, K.; Kalil, A.C.; Linden, P.; Maki, D.G.; Nierman, D.; Pasculle, W. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit. Care Med. 2008, 36, 1330–1349. [Google Scholar] [CrossRef]
- Society of Critical Care Medicine. Available online: https://www.sccm.org/Home (accessed on 15 July 2023).
- Hines, C.B. Herbal Medications Used to Treat Fever. Nurs. Clin. 2021, 56, 91–107. [Google Scholar] [CrossRef] [PubMed]
- Chaachouay, N.; Benkhnigue, O.; Fadli, M.; El Ibaoui, H.; Zidane, L. Ethnobotanical and ethnopharmacological studies of medicinal and aromatic plants used in the treatment of metabolic diseases in the Moroccan Rif. Heliyon 2019, 5, e02191. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for the Treatment of Malaria; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Bellakhdar, J.; Claisse, R.; Fleurentin, J.; Younos, C. Repertory of standard herbal drugs in the Moroccan pharmacopoea. J. Ethnopharmacol. 1991, 35, 123–143. [Google Scholar] [CrossRef]
- Zougagh, S.; Belghiti, A.; Rochd, T.; Zerdani, I.; Mouslim, J. Medicinal and aromatic plants used in traditional treatment of the oral pathology: The ethnobotanical survey in the economic capital Casablanca, Morocco (North Africa). Nat. Prod. Bioprospect. 2019, 9, 35–48. [Google Scholar] [CrossRef]
- Bourhia, M.; Abdelaziz Shahat, A.; Mohammed Almarfadi, O.; Ali Naser, F.; Mostafa Abdelmageed, W.; Ait Haj Said, A.; El Gueddari, F.; Naamane, A.; Benbacer, L.; Khlil, N. Ethnopharmacological survey of herbal remedies used for the treatment of cancer in the greater Casablanca-Morocco. Evid-Based Complement. Altern. Med. 2019, 2019, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yusro, F.; Mariani, Y.; Diba, F.; Ohtani, K. Inventory of medicinal plants for fever used by four Dayak Sub Ethnic in West Kalimantan, Indonesia. Kuroshio Sci. 2014, 8, 33–38. [Google Scholar]
- Zerhouny, M.; Fadil, A.; Hakdaoui, M. Underground space utilization in the urban land-use planning of casablanca (morocco). Land 2018, 7, 143. [Google Scholar] [CrossRef]
- Bolle, H.-J. Climate, climate variability, and impacts in the Mediterranean area: An overview. In Mediterranean Climate; Springer: Berlin/Heidelberg, Germany, 2003; pp. 5–86. [Google Scholar] [CrossRef]
- Deelstra, T.; Girardet, H. Urban agriculture and sustainable cities. In Growing Cities, Growing Food. Urban Agriculture on the Policy Agenda; Bakker, N., Dubbeling, M., Gündel, S., Sabel-Koshella, U., de Zeeuw, H., Eds.; Zentralstelle für Ernährung und Landwirtschaft (ZEL): Feldafing, Germany, 2000; pp. 43–66. [Google Scholar]
- Lwanga, S.K.; Lemeshow, S.; World Health Organization. Sample Size Determination in Health Studies: A Practical Manual; World Health Organization: Geneva, Switzerland, 1991. [Google Scholar]
- Nesbitt, M. Use of herbarium specimens in ethnobotany. In Curating Biocultural Collections; Royal Botanic Gardens: Richmond, UK, 2014; pp. 313–328. [Google Scholar]
- Jain, S. The role of botanist in folklore research. Folklore 1964, 5, 145–150. [Google Scholar]
- Plants of the World Online. Available online: https://powo.science.kew.org/ (accessed on 4 July 2023).
- Phillips, O.; Gentry, A.H.; Reynel, C.; Wilkin, P.; Gálvez-Durand, B.C. Quantitative ethnobotany and Amazonian conservation. Conserv. Biol. 1994, 8, 225–248. [Google Scholar] [CrossRef]
- Suroowan, S.; Mahomoodally, M.F. A comparative ethnopharmacological analysis of traditional medicine used against respiratory tract diseases in Mauritius. J. Ethnopharmacol. 2016, 177, 61–80. [Google Scholar] [CrossRef]
- Alexiades, M.N.; Sheldon, J.W. Selected Guidelines for Ethnobotanical Research: A Field Manual; New York Botanical Garden: Bronx, NY, USA, 1996. [Google Scholar]
- Uddin, M.Z.; Hassan, M.A. Determination of informant consensus factor of ethnomedicinal plants used in Kalenga forest, Bangladesh. Bangladesh J. Plant Taxon. 2014, 21, 83–91. [Google Scholar] [CrossRef]
- Tardío, J.; Pardo-de-Santayana, M. Cultural importance indices: A comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain). Econ. Bot. 2008, 62, 24–39. [Google Scholar] [CrossRef]
- Sreekeesoon, D.P.; Mahomoodally, M.F. Ethnopharmacological analysis of medicinal plants and animals used in the treatment and management of pain in Mauritius. J. Ethnopharmacol. 2014, 157, 181–200. [Google Scholar] [CrossRef]
- Trotter, R.T.; Logan, M.H. Informant consensus: A new approach for identifying potentially effective medicinal plants. In Plants in Indigenous Medicine & Diet; Routledge: Abingdon, UK, 2019; pp. 91–112. [Google Scholar]
- Heinrich, M.; Ankli, A.; Frei, B.; Weimann, C.; Sticher, O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc. Sci. Med. 1998, 47, 1859–1871. [Google Scholar] [CrossRef]
- Pfeiffer, J.M.; Butz, R.J. Assessing cultural and ecological variation in ethnobiological research: The importance of gender. J. Ethnobiol. 2005, 25, 240–278. [Google Scholar]
- Bachiri, L.; Labazi, N.; Daoudi, A.; Ibijbijien, J.; Nassiri, L.; Echchegadda, G.; Mokhtari, F. Etude ethnobotanique de quelques lavandes marocaines spontanées. Int. J. Biol. Chem. Sci. 2015, 9, 1308–1318. [Google Scholar] [CrossRef]
- Harouak, H.; Falaki, K.; Bouiamrine, E.-H.; Oudija, F.; Ibijbijen, J.; Nassiri, L. Ethnobotanical survey of plants used in treatment of oral diseases in the city of Meknes, Morocco. Int. J. Herb. Med. 2018, 6, 46–49. [Google Scholar]
- Idm’hand, E.; Msanda, F.; Cherifi, K. Ethnobotanical study and biodiversity of medicinal plants used in the Tarfaya Province, Morocco. Acta Ecol. Sin. 2020, 40, 134–144. [Google Scholar] [CrossRef]
- Barkaoui, M.; Katiri, A.; Boubaker, H.; Msanda, F. Ethnobotanical survey of medicinal plants used in the traditional treatment of diabetes in Chtouka Ait Baha and Tiznit (Western Anti-Atlas), Morocco. J. Ethnopharmacol. 2017, 198, 338–350. [Google Scholar] [CrossRef]
- Kankara, S.S.; Ibrahim, M.H.; Mustafa, M.; Go, R. Ethnobotanical survey of medicinal plants used for traditional maternal healthcare in Katsina state, Nigeria. S. Afr. J. Bot. 2015, 97, 165–175. [Google Scholar] [CrossRef]
- Bencheikh, N.; Elbouzidi, A.; Kharchoufa, L.; Ouassou, H.; Alami Merrouni, I.; Mechchate, H.; Es-Safi, I.; Hano, C.; Addi, M.; Bouhrim, M. Inventory of Medicinal Plants Used Traditionally to Manage Kidney Diseases in North-Eastern Morocco: Ethnobotanical Fieldwork and Pharmacological Evidence. Plants 2021, 10, 1966. [Google Scholar] [CrossRef] [PubMed]
- Anyinam, C. Ecology and ethnomedicine: Exploring links between current environmental crisis and indigenous medical practices. Soc. Sci. Med. 1995, 40, 321–329. [Google Scholar] [CrossRef]
- Weniger, B. Interest and limitation of a global ethnopharmacological survey. J. Ethnopharmacol. 1991, 32, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Mroczek, A. Phytochemistry and bioactivity of triterpene saponins from Amaranthaceae family. Phytochem. Rev. 2015, 14, 577–605. [Google Scholar] [CrossRef]
- Nebo, L.; Varela, R.M.; Molinillo, J.M.; Sampaio, O.M.; Severino, V.G.; Cazal, C.M.; das Graças Fernandes, M.F.; Fernandes, J.B.; Macías, F.A. Phytotoxicity of alkaloids, coumarins and flavonoids isolated from 11 species belonging to the Rutaceae and Meliaceae families. Phytochem. Lett. 2014, 8, 226–232. [Google Scholar] [CrossRef]
- Najem, M.; Ibijbijen, J.; Nassiri, L. Ethnobotanical treatment of respiratory diseases in the central Middle Atlas (Morocco): Qualitative and quantitative approach. Eur. J. Integr. Med. 2021, 46, 101358. [Google Scholar] [CrossRef]
- Al-Fatimi, M. Ethnobotanical survey of medicinal plants in central Abyan governorate, Yemen. J. Ethnopharmacol. 2019, 241, 111973. [Google Scholar] [CrossRef] [PubMed]
- Slimani, I.; Najem, M.; Belaidi, R.; Bachiri, L.; Bouiamrine, E.H.; Nassiri, L.; Ibijbijen, J. Étude ethnobotanique des plantes médicinales utilisées dans la région de Zerhoun-Maroc-[Ethnobotanical Survey of medicinal plants used in Zerhoun region-Morocco-]. Int. J. Innov. Appl. Stud. 2016, 15, 846. [Google Scholar]
- Tembo, N.; Lampiao, F.; Mwakikunga, A.; Chikowe, I. Ethnobotanical survey of medicinal plants used for cervical cancer management in Zomba District, Malawi. Sci. Afr. 2021, 13, e00941. [Google Scholar] [CrossRef]
- Chakale, M.V.; Asong, J.A.; Struwig, M.; Mwanza, M.; Aremu, A.O. Ethnoveterinary Practices and Ethnobotanical Knowledge on Plants Used against Cattle Diseases among Two Communities in South Africa. Plants 2022, 11, 1784. [Google Scholar] [CrossRef]
- Moichwanetse, B.I.; Ndhlovu, P.T.; Sedupane, G.; Aremu, A.O. Ethno-veterinary plants used for the treatment of retained placenta and associated diseases in cattle among Dinokana communities, North West Province, South Africa. S. Afr. J. Bot. 2020, 132, 108–116. [Google Scholar] [CrossRef]
- Moreki, J.; Tshireletso, K.; Okoli, I. Potential use of ethnoveterinary medicine for retained placenta in cattle in Mogonono, Botswana. J. Anim. Prod. Adv. 2012, 2, 303–309. [Google Scholar]
- Jamila, F.; Mostafa, E. Ethnobotanical survey of medicinal plants used by people in Oriental Morocco to manage various ailments. J. Ethnopharmacol. 2014, 154, 76–87. [Google Scholar] [CrossRef] [PubMed]
- El-Hilaly, J.; Hmammouchi, M.; Lyoussi, B. Ethnobotanical studies and economic evaluation of medicinal plants in Taounate province (Northern Morocco). J. Ethnopharmacol. 2003, 86, 149–158. [Google Scholar] [CrossRef]
- Tene, V.; Malagon, O.; Finzi, P.V.; Vidari, G.; Armijos, C.; Zaragoza, T. An ethnobotanical survey of medicinal plants used in Loja and Zamora-Chinchipe, Ecuador. J. Ethnopharmacol. 2007, 111, 63–81. [Google Scholar] [CrossRef]
- Hadian, F.; Varshochi, M.; Feyzabadi, Z.; Zargaran, A.; Besharat, M.; Mousavi Bazaz, M. Medicinal herbs useful in pediatric fever from the perspective of Persian medicine. Int. J. Pediatr. 2019, 7, 10087–10098. [Google Scholar]
- Dagni, A.; Suharoschi, R.; Heghes, S.C.; Pop, O.L.; Fodor, A.; VULTURAR, R.; Cozma, A.; Vodnar, D.C.; Soukri, A. Essential oils from Dysphania genus: Traditional uses, phytochemistry, toxicology, and health benefits. Front. Pharmacol. 2022, 13, 1024274. [Google Scholar] [CrossRef]
- Kandsi, F.; Elbouzidi, A.; Lafdil, F.Z.; Meskali, N.; Azghar, A.; Addi, M.; Hano, C.; Maleb, A.; Gseyra, N. Antibacterial and antioxidant activity of Dysphania ambrosioides (L.) mosyakin and clemants essential oils: Experimental and computational approaches. Antibiotics 2022, 11, 482. [Google Scholar] [CrossRef]
- Mworia, J.K.; Kibiti, C.M.; Ngugi, M.P.; Ngeranwa, J.N. Antipyretic potential of dichloromethane leaf extract of Eucalyptus globulus (Labill) and Senna didymobotrya (Fresenius) in rats models. Heliyon 2019, 5, e02924. [Google Scholar] [CrossRef]
- Silva, J.; Abebe, W.; Sousa, S.; Duarte, V.; Machado, M.; Matos, F. Analgesic and anti-inflammatory effects of essential oils of Eucalyptus. J. Ethnopharmacol. 2003, 89, 277–283. [Google Scholar] [CrossRef]
- Pereira, A.P.; Ferreira, I.C.; Marcelino, F.; Valentão, P.; Andrade, P.B.; Seabra, R.; Estevinho, L.; Bento, A.; Pereira, J.A. Phenolic compounds and antimicrobial activity of olive (Olea europaea L. Cv. Cobrançosa) leaves. Molecules 2007, 12, 1153–1162. [Google Scholar] [CrossRef]
- Esmaeili-Mahani, S.; Rezaeezadeh-Roukerd, M.; Esmaeilpour, K.; Abbasnejad, M.; Rasoulian, B.; Sheibani, V.; Kaeidi, A.; Hajializadeh, Z. Olive (Olea europaea L.) leaf extract elicits antinociceptive activity, potentiates morphine analgesia and suppresses morphine hyperalgesia in rats. J. Ethnopharmacol. 2010, 132, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Mehmood, T.; Afzal, A.; Anwar, F.; Memon, N.; Memon, A.A.; Qadir, R. Variation in phenolic acids and antibacterial attributes of peel extracts from ripe and unripe [Citrus limon (L.) Osbeck] fruit. J. Food Meas. Charact. 2020, 14, 1325–1332. [Google Scholar] [CrossRef]
- Aleksic, V.; Knezevic, P. Antimicrobial and antioxidative activity of extracts and essential oils of Myrtus communis L. Microbiol. Res. 2014, 169, 240–254. [Google Scholar] [CrossRef]
- Maxia, A.; Frau, M.A.; Falconieri, D.; Karchuli, M.S.; Kasture, S. Essential oil of Myrtus communis inhibits inflammation in rats by reducing serum IL-6 and TNF-α. Nat. Prod. Commun. 2011, 6, 1934578X1100601034. [Google Scholar] [CrossRef]
- Rached, W.; Zeghada, F.Z.; Bennaceur, M.; Barros, L.; Calhelha, R.C.; Heleno, S.; Alves, M.J.; Carvalho, A.M.; Marouf, A.; Ferreira, I.C. Phytochemical analysis and assessment of antioxidant, antimicrobial, anti-inflammatory and cytotoxic properties of Tetraclinis articulata (Vahl) Masters leaves. Ind. Crops Prod. 2018, 112, 460–466. [Google Scholar] [CrossRef]
- Borgi, W.; Recio, M.-C.; Ríos, J.; Chouchane, N. Anti-inflammatory and analgesic activities of flavonoid and saponin fractions from Zizyphus lotus (L.) Lam. S. Afr. J. Bot. 2008, 74, 320–324. [Google Scholar] [CrossRef]
- Arumugam, P.; Priya, N.G.; Subathra, M.; Ramesh, A. Anti-inflammatory activity of four solvent fractions of ethanol extract of Mentha spicata L. investigated on acute and chronic inflammation induced rats. Environ. Toxicol. Pharmacol. 2008, 26, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Algieri, F.; Rodriguez-Nogales, A.; Vezza, T.; Garrido-Mesa, J.; Garrido-Mesa, N.; Utrilla, M.P.; González-Tejero, M.R.; Casares-Porcel, M.; Molero-Mesa, J.; del Mar Contreras, M. Anti-inflammatory activity of hydroalcoholic extracts of Lavandula dentata L. and Lavandula stoechas L. J. Ethnopharmacol. 2016, 190, 142–158. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Kong, D.; Fu, Y.; Sussman, M.R.; Wu, H. The effect of developmental and environmental factors on secondary metabolites in medicinal plants. Plant Physiol. Biochem. 2020, 148, 80–89. [Google Scholar] [CrossRef]
- Mostafa, E.I.; Mohammed, E.; Ali, A.; Adrae, L.; Saadia, B.; Ghizlane, E. Characterization of essential oils from Chenopodium ambrosioides (L.) (Chenopodiaceae) from four regions of Morocco]. J. Mater. Environ. Sci. 2016, 7, 4087–4095. [Google Scholar]
- Alitonou, G.A.; Sessou, P.; Tchobo, P.F.; Noudogbessi, J.P.; Avlessi, F.; Yehouenou, B.; Menut, C.; Villeneuve, P.; Sohounhloue, D.C.K. Chemical composition and biological activities of essential oils of Chenopodium ambrosioides L. collected in two areas of Benin. Int. J. Biosci. 2012, 2, 58–66. [Google Scholar]
- Verma, N.; Shukla, S. Impact of various factors responsible for fluctuation in plant secondary metabolites. J. Appl. Res. Med. Aromat. Plants 2015, 2, 105–113. [Google Scholar] [CrossRef]
- Leonti, M. The relevance of quantitative ethnobotanical indices for ethnopharmacology and ethnobotany. J. Ethnopharmacol. 2022, 288, 115008. [Google Scholar] [CrossRef] [PubMed]
- Israel, G.D. Determining Sample Size; University of Florida Cooperative Extension Service, Institute of Food and Agriculture Sciences: Gainesville, FL, USA, 1992. [Google Scholar]
- Makbli, M.; El Rhaffari, L.; Messaouri, H.; Rhallabi, N.; Ait, M.R.; Mellouki, F. Ethnobotanical study of plants used in the treatment of cutaneous infections in urban areas of the region of Grand Casablanca–Morocco. IOSR J. Env. Sci. Toxicol. Food Tech. 2016, 10, 38–48. [Google Scholar] [CrossRef]
- Kachmar, M.R.; Mrabti, H.N.; Bellahmar, M.; Ouahbi, A.; Haloui, Z.; El Badaoui, K.; Bouyahya, A.; Chakir, S. Traditional knowledge of medicinal plants used in the Northeastern part of Morocco. Evid. Based Complement. Altern. Med. 2021, 2021, 6002949. [Google Scholar] [CrossRef]
- Moussi, M.; Filali, H.; Tazi, A.; Hakkou, F. Ethnobotanical survey of healing medicinal plants traditionally used in the main Moroccan cities. J. Pharmacogn. Phytother. 2015, 7, 164–182. [Google Scholar]
- Eddouks, M.; Maghrani, M.; Lemhadri, A.; Ouahidi, M.-L.; Jouad, H. Ethnopharmacological survey of medicinal plants used for the treatment of diabetes mellitus, hypertension and cardiac diseases in the south-east region of Morocco (Tafilalet). J. Ethnopharmacol. 2002, 82, 97–103. [Google Scholar] [CrossRef]
- Hayat, J.; Akodad, M.; Moumen, A.; Baghour, M.; Skalli, A.; Ezrari, S.; Belmalha, S. Ethnobotanical survey of medicinal plants growing in the region of “Oulad Daoud Zkhanine” (Nador Province), in Northeastern Morocco. Ethnobot. Res. Appl. 2020, 19, 1–12. [Google Scholar]
- Teixidor-Toneu, I.; Martin, G.J.; Ouhammou, A.; Puri, R.K.; Hawkins, J.A. An ethnomedicinal survey of a Tashelhit-speaking community in the High Atlas, Morocco. J. Ethnopharmacol. 2016, 188, 96–110. [Google Scholar] [CrossRef] [PubMed]
- Senouci, F.; Ababou, A.; Chouieb, M. Ethnobotanical survey of the medicinal plants used in the Southern Mediterranean. Case study: The region of Bissa (Northeastern Dahra Mountains, Algeria). Pharmacogn. J. 2019, 11, 647–659. [Google Scholar] [CrossRef]
- Ouhaddou, H.; Boubaker, H.; Msanda, F.; El Mousadik, A. An ethnobotanical study of medicinal plants of the Agadir Ida Ou Tanane province (southwest Morocco). J. Appl. Biosci. 2014, 84, 7707–7722. [Google Scholar] [CrossRef]
- Chaachouay, N.; Benkhnigue, O.; Zidane, L. Ethnobotanical study aimed at investigating the use of medicinal plants to treat nervous system diseases in the Rif of Morocco. J. Chiropr. Med. 2020, 19, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Lemhadri, A.; Achtak, H.; Lamraouhi, A.; Louidani, N.; Benali, T.; Dahbi, A.; Bouyahya, A.; Khouchlaa, A.; Shariati, M.A.; Hano, C.; et al. Diversity of Medicinal Plants Used by the Local Communities of the Coastal Plateau of Safi Province (Morocco). Front. Biosci. Sch. 2023, 15, 1. [Google Scholar] [CrossRef]
- Skalli, S.; Hassikou, R.; Arahou, M. An ethnobotanical survey of medicinal plants used for diabetes treatment in Rabat, Morocco. Heliyon 2019, 5, e01421. [Google Scholar] [CrossRef]
- Youbi, A.E.H.E.; Ouahidi, I.; Mansouri, L.E.; Daoudi, A.; Bousta, D. Ethnopharmacological survey of plants used for immunological diseases in four regions of Morocco. Eur. J. Med. Plants 2016, 13, 1–24. [Google Scholar] [CrossRef]
- Mrabti, H.N.; Jaradat, N.; Kachmar, M.R.; Ed-Dra, A.; Ouahbi, A.; Cherrah, Y.; El Abbes Faouzi, M. Integrative herbal treatments of diabetes in Beni Mellal region of Morocco. J. Integr. Med. 2019, 17, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Abouri, M.; El Mousadik, A.; Msanda, F.; Boubaker, H.; Saadi, B.; Cherifi, K. An ethnobotanical survey of medicinal plants used in the Tata Province, Morocco. Int. J. Med. Plants Res. 2012, 1, 99–123. [Google Scholar]


| Factors | Classes | Frequency | Percentage (%) |
|---|---|---|---|
| Gender | Female | 19 | 18.1 |
| Male | 86 | 81.9 | |
| Age | ≤30 | 17 | 16.2 |
| 31–40 | 18 | 17.1 | |
| 41–50 | 36 | 34.3 | |
| ≥51 | 34 | 32.4 | |
| Educational status | Illiterate | 29 | 27.6 |
| Primary | 44 | 41.9 | |
| Secondary | 28 | 26.7 | |
| University | 4 | 3.8 | |
| Source of Knowledge | Hereditary | 73 | 70 |
| Herbalists | 32 | 30 |
| N° | Scientific Names of Families and Species (Voucher Number) | Local Name | Parts Used | Traditional Dosages | Method of Preparation | Method Administration | UR | UV | FC | RFC |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Amaranthaceae Dysphania ambrosioides (L.) Mosyakin & Clemants (CLA30324) | M’khinza | Leaves | Spoon | Infusion | Internal use External use | 105 | 1 | 15.88 | 0.15 |
| Spoon | Juice | |||||||||
| Handful | Poultice | |||||||||
| 2 | Apiaceae Coriandrum sativum L. (CLA30321) | Kasbour | Leaves | Handful | Juice | Internal use | 4 | 0.038 | 0.60 | 0.005 |
| 3 | Asteraceae Artemisia herba-alba (CLA30310) | Chih | Leaves | Spoon | Decoction | External use | 1 | 0.009 | 0.1 | 0.001 |
| 4 | Artemisia absinthium L. (CLA30323) | Chiba | Aerial parts | Spoon | Infusion | Internal use | 1 | 0.009 | 0.1 | 0.001 |
| 5 | Cupressaceae Tetraclinis articulata (Vahl) Mast. (CLA30320) | El-Aarar | Leaves Bark | Spoon | Decoction | Internal use External use | 80 | 0.76 | 12.10 | 0.11 |
| Handful | Poultice | |||||||||
| 6 | Cucurbitaceae Lagenaria siceraria (Molina) Standl. (CLA30314) | Slawi | Fruit | 1 unit | Juice | Internal use External use | 3 | 0.028 | 0.004 | 0.004 |
| 1 unit | Poultice | |||||||||
| Lamiaceae | ||||||||||
| 7 | Clinopodium nepeta (L.) Kuntze (CLA30307) | Manta | Leaves | Handful | Infusion | Internal use | 59 | 0.56 | 8.92 | 0.085 |
| 8 | Mentha spicata L. (CLA30305) | Naanaa | Whole plant | Handful | Infusion | Internal use | 49 | 0.46 | 7.41 | 0.07 |
| 9 | Lavandula dentata L. (CLA30311) | Khzama | Leaves | Spoon | Infusion | Internal use | 51 | 0.48 | 7.71 | 0.073 |
| 10 | Mentha pulegium L. (CLA30322) | Flio | Whole plant | Spoon | Infusion | Internal use | 10 | 0.09 | 1.51 | 0.01 |
| 11 | Salvia officinalis subsp. officinalis (CLA30309) | Salmiya | Leaves | Handful | Infusion | External use | 1 | 0.009 | 0.151 | 0.001 |
| 12 | Mentha suaveolens Ehrh. (CLA30312) | Timija | Leaves | Spoon | Infusion | External use | 1 | 0.009 | 0.151 | 0.001 |
| 13 | Origanum grosii Pau & Font Quer (CLA30317) | Zàater | Leaves | Handful | Infusion | Internal use External use | 3 | 0.02 | 0.45 | 0.004 |
| Handful | Decoction | |||||||||
| 14 | Salvia rosmarinus Spenn. (CLA30306) | Azir | Leaves and stems | Glass | Infusion | Internal use External use | 4 | 0.038 | 0.6 | 0.005 |
| Glass | Decoction | |||||||||
| 15 | Thymus broussonetii Boiss. (CLA30318) | Ziitra | Leaves | Glass | Infusion | Internal use | 2 | 0.019 | 0.3 | 0.0028 |
| 16 | Ocimum basilicum L. (CLA30325) | hbaq | Leaves and stems | Spoon | Decoction | Internal use | 1 | 0.0095 | 0.151 | 0.001 |
| Spoon | Infusion | |||||||||
| Myrtaceae | ||||||||||
| 17 | Eucalyptus globulus Labill. (CLA30319) | Kalitouse | Leaves/Bark | Handful | Infusion | Internal use External use | 94 | 0.89 | 14.22 | 0.135 |
| Handful | Decoction | |||||||||
| 18 | Myrtus communis L. (CLA30308) | Rihan | Leaves | Handful | Decoction | Internal use | 2 | 0.10 | 1.66 | 0.015 |
| 19 | Oleaceae Olea europaea L. (CLA30316) | Zitoun | Leaves/Bark | Glass | Infusion | Internal use External use | 11 | 0.019 | 0.30 | 0.002 |
| 20 | Papaveraceae Papaver rhoeas L. (CLA30315) | Belâaman | Leaves | Handful | Infusion | Internal use | 81 | 0.77 | 12.25 | 0.11 |
| Handful | Decoction | External use | ||||||||
| 21 | Rhamnaceae Ziziphus lotus (L.) Lam (CLA30326) | Sedra | Leaves/Root -bark | Handful | Infusion | Internal use External use | 1 | 0.009 | 0.151 | 0.001 |
| 22 | Rutaceae Citrus × limon (L.) Osbeck (CLA30313) | Limon | Fruit | 5 units | Juice | Internal use | 97 | 0.92 | 14.67 | 0.139 |
| Diseases | Plant Species | FL% | Nur | Nt | ICF |
|---|---|---|---|---|---|
| Unspecified Fever | D. ambrosioides L. | 100 | 45 | 14 | 0.70 |
| C. limon (L.) Osbeck | 95.23 | ||||
| E. globulus Labill. | 89.52 | ||||
| P. rhoeas L. | 77.14 | ||||
| T. articulata | 76.19 | ||||
| M. pulegium L. | 57.14 | ||||
| L. dentata L. | 48.57 | ||||
| Enteric Fever | D. ambrosioides L. | 100 | 40 | 12 | 0.72 |
| C. limon (L.) Osbeck | 100 | ||||
| S. rosmarinus | 85.71 | ||||
| P. rhoeas L. | 69.52 | ||||
| M. pulegium L. | 56.19 | ||||
| Influenza | D. ambrosioides L. | 100 | 20 | 8 | 0.63 |
| C. limon (L.) Osbeck | 90.47 | ||||
| S. rosmarinus | 88.57 | ||||
| M. spicata L. | 84.76 | ||||
| L. dentata L. | 34.28 | ||||
| Spotted Fever | D. ambrosioides L. | 100 | 12 | 6 | 0.54 |
| C. nepeta | 59.04 | ||||
| E. globulus Labill. | 50.47 | ||||
| C. limon (L.) Osbeck | 28.57 | ||||
| P. rhoeas L. | 38.09 |
| N° | Form | Preparation Method |
|---|---|---|
| C1 | Juice | Some leaves of D. ambrosioides (Handful) were made in juice with 1 cup of C. limon (250 mL). |
| C2 | Juice | Leaves of D. ambrosioides (Spoon), M. communis (Spoon), T. articulata (Spoon), Z. lotus (Spoon), and M. suaveolens (Spoon), mixed with one tablespoon of honey. |
| C3 | Poultice | Leaves of D. ambrosioides (Handful), M. spicata (Handful), and L. dentata (Handful) mixed with 1/2 cup of vinegar (125 mL). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dagni, A.; Suharoschi, R.; Hegheș, S.-C.; Vârban, R.; Lelia Pop, O.; Vulturar, R.; Fodor, A.; Cozma, A.; Soukri, A.; El Khalfi, B. Ethnobotanical Survey on Plants Used to Manage Febrile Illnesses among Herbalists in Casablanca, Morocco. Diversity 2023, 15, 879. https://doi.org/10.3390/d15070879
Dagni A, Suharoschi R, Hegheș S-C, Vârban R, Lelia Pop O, Vulturar R, Fodor A, Cozma A, Soukri A, El Khalfi B. Ethnobotanical Survey on Plants Used to Manage Febrile Illnesses among Herbalists in Casablanca, Morocco. Diversity. 2023; 15(7):879. https://doi.org/10.3390/d15070879
Chicago/Turabian StyleDagni, Amal, Ramona Suharoschi, Simona-Codruta Hegheș, Rodica Vârban, Oana Lelia Pop, Romana Vulturar, Adriana Fodor, Angela Cozma, Abdelaziz Soukri, and Bouchra El Khalfi. 2023. "Ethnobotanical Survey on Plants Used to Manage Febrile Illnesses among Herbalists in Casablanca, Morocco" Diversity 15, no. 7: 879. https://doi.org/10.3390/d15070879
APA StyleDagni, A., Suharoschi, R., Hegheș, S.-C., Vârban, R., Lelia Pop, O., Vulturar, R., Fodor, A., Cozma, A., Soukri, A., & El Khalfi, B. (2023). Ethnobotanical Survey on Plants Used to Manage Febrile Illnesses among Herbalists in Casablanca, Morocco. Diversity, 15(7), 879. https://doi.org/10.3390/d15070879








