Non-Coeliac Wheat Sensitivity: Symptoms in Search of a Mechanism, or a Distinct Well-Defined Clinical Entity? A Narrative Review
Abstract
1. Introduction
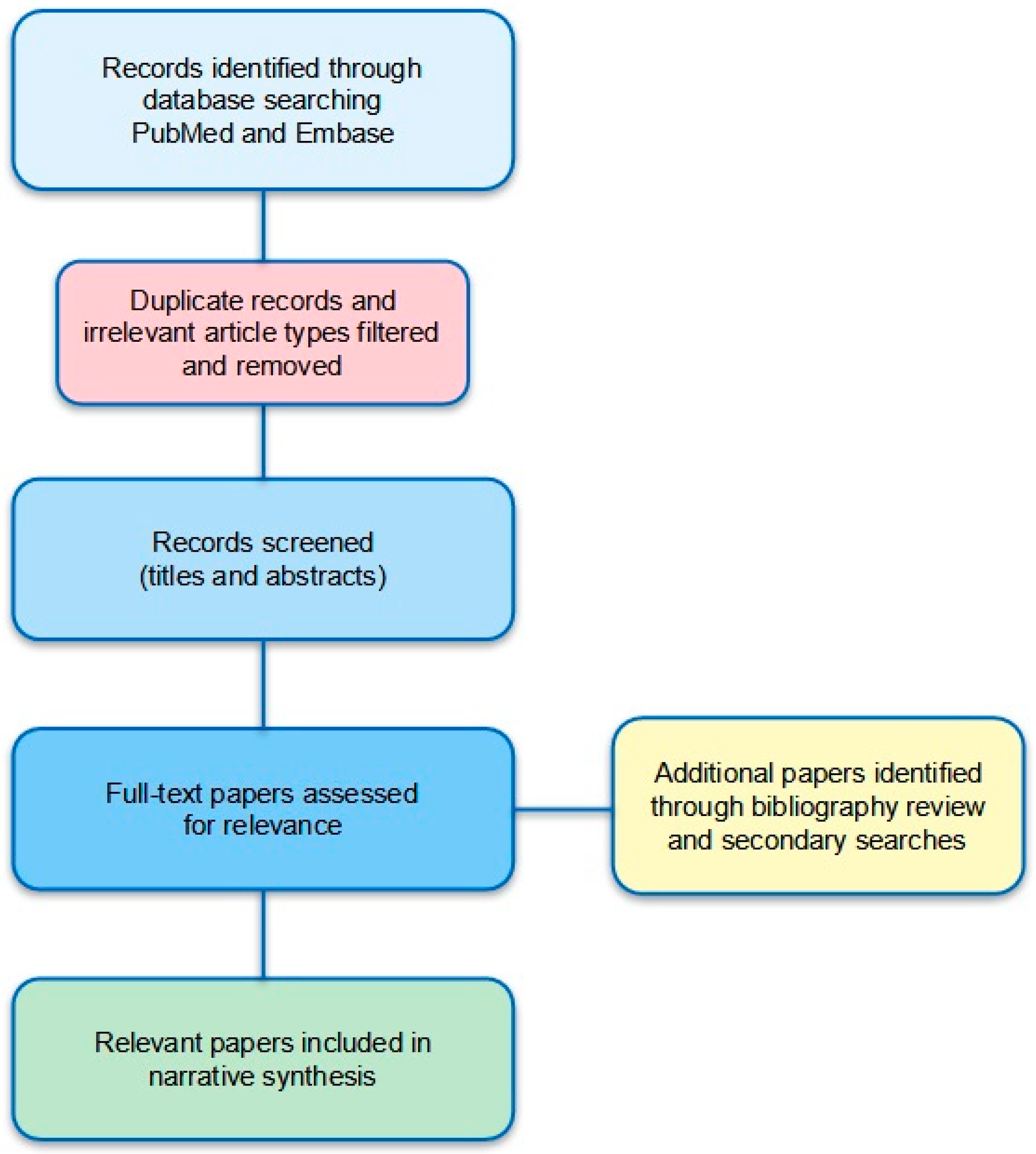
2. Methods
2.1. Epidemiology
Factors Contributing to Geographic and Temporal Variation in Prevalence
2.2. Clinical Presentation
2.3. Associated Conditions
2.4. Pathophysiology
2.4.1. Experimental Models and In Vitro Evidence
2.4.2. Immune Mechanisms
2.4.3. Gut Barrier Function and Microbial Translocation
2.4.4. Gut Microbiota
2.4.5. Genetic Factors
2.4.6. Neuro-Immune Interactions
2.4.7. The Role of Gluten, Placebo, and Nocebo
2.4.8. FODMAPs (Fermentable Oligo-, Di-, Monosaccharides, and Polyols)
2.4.9. Other Wheat Factors
2.5. Challenges in Diagnosis and Differential Diagnosis
2.5.1. The Role and Limitations of Gluten Challenge
2.5.2. Distinguishing NCWS from IBS
2.5.3. Histological Findings
2.6. Biomarkers
2.7. Management
3. Limitations
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AGA | Anti-gliadin antibodies |
| AMPK | AMP-activated protein kinase |
| ATI | Amylase-trypsin inhibitors |
| AUC | Area Under the Curve |
| BMI | Body Mass Index |
| CD | Coeliac disease |
| DBPCC | Double-blind, placebo-controlled challenge |
| DEG | Differentially expressed gene |
| DGP | Deamidated gliadin peptide |
| EMA | Endomysial antibodies |
| ER | Endoplasmic reticulum |
| FC | Faecal calprotectin |
| FDA | Food and Drug Administration |
| FODMAP | Fermentable oligo-, di-, monosaccharides, and polyols |
| GFD | Gluten-free diet |
| GPR | G protein-coupled receptor |
| HLA | Human leukocyte antigen |
| IBD | Inflammatory bowel disease |
| IBS | Irritable bowel syndrome |
| I-FABP | Intestinal fatty acid-binding protein |
| IFN-γ | Interferon-gamma |
| IgG | Immunoglobulin G |
| IL | Interleukin |
| IEL | Intraepithelial lymphocyte |
| KIR | Killer-cell immunoglobulin-like receptor |
| LBP | Lipopolysaccharide-binding protein |
| LPS | Lipopolysaccharide |
| NCWS | Non-coeliac wheat sensitivity |
| NF-kB | Nuclear factor-kappa B |
| NLRP3 | NLR Family Pyrin Domain Containing 3 |
| PAR-2 | Protease-activated receptor 2 |
| sCD14 | Soluble CD14 |
| SCFA | Short-chain fatty acid |
| TCR | T-cell receptor |
| TLR4 | Toll-like receptor 4 |
| TNF | Tumour Necrosis Factor |
| tTG | Tissue transglutaminase antibodies |
| WA | Wheat allergy |
References
- Cooper, B.T.; Holmes, G.K.; Fperguson, R.; Thompson, R.; Cooke, W.T. Proceedings: Chronic diarrhoea and gluten sensitivity. Gut 1976, 17, 398. [Google Scholar]
- Ellis, A.; Linaker, B.D. Non-coeliac gluten sensitivity? Lancet 1978, 1, 1358–1359. [Google Scholar] [CrossRef] [PubMed]
- Sapone, A.; Lammers, K.M.; Mazzarella, G.; Mikhailenko, I.; Cartenì, M.; Casolaro, V.; Fasano, A. Differential mucosal IL-17 expression in two gliadin-induced disorders: Gluten sensitivity and the autoimmune enteropathy celiac disease. Int. Arch. Allergy Immunol. 2010, 152, 75–80. [Google Scholar] [CrossRef]
- Sapone, A.; Bai, J.C.; Ciacci, C.; Dolinsek, J.; Green, P.H.; Hadjivassiliou, M.; Kaukinen, K.; Rostami, K.; Sanders, D.S.; Schumann, M.; et al. Spectrum of gluten-related disorders: Consensus on new nomenclature and classification. BMC Med. 2012, 10, 13. [Google Scholar] [CrossRef]
- Biesiekierski, J.R.; Newnham, E.D.; Irving, P.M.; Barrett, J.S.; Haines, M.; Doecke, J.D.; Shepherd, S.J.; Muir, J.G.; Gibson, P.R. Gluten causes gastrointestinal symptoms in subjects without celiac disease: A double-blind randomized placebo-controlled trial. Am. J. Gastroenterol. 2011, 106, 508–514. [Google Scholar] [CrossRef]
- Biesiekierski, J.R.; Peters, S.L.; Newnham, E.D.; Rosella, O.; Muir, J.G.; Gibson, P.R. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 2013, 145, e1–e3. [Google Scholar] [CrossRef]
- Carroccio, A.; Rini, G.; Mansueto, P. Non-celiac wheat sensitivity is a more appropriate label than non-celiac gluten sensitivity. Gastroenterology 2014, 146, 320–321. [Google Scholar] [CrossRef] [PubMed]
- Uhde, M.; Ajamian, M.; Caio, G.; De Giorgio, R.; Indart, A.; Green, P.H.; Verna, E.C.; Volta, U.; Alaedini, A. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut 2016, 65, 1930–1937. [Google Scholar] [CrossRef]
- Volta, U.; Caio, G.; Karunaratne, T.B.; Alaedini, A.; De Giorgio, R. Non-coeliac gluten/wheat sensitivity: Advances in knowledge and relevant questions. Expert. Rev. Gastroenterol. Hepatol. 2017, 11, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Sergi, C.; Villanacci, V.; Carroccio, A. Non-celiac wheat sensitivity: Rationality and irrationality of a gluten-free diet in individuals affected with non-celiac disease: A review. BMC Gastroenterol. 2021, 21, 5. [Google Scholar] [CrossRef]
- Manza, F.; Lungaro, L.; Costanzini, A.; Caputo, F.; Carroccio, A.; Mansueto, P.; Seidita, A.; Raju, S.A.; Volta, U.; De Giorgio, R.; et al. Non-Celiac Gluten/Wheat Sensitivity-State of the Art: A Five-Year Narrative Review. Nutrients 2025, 17, 220. [Google Scholar] [CrossRef]
- Catassi, C.; Elli, L.; Bonaz, B.; Bouma, G.; Carroccio, A.; Castillejo, G.; Cellier, C.; Cristofori, F.; de Magistris, L.; Dolinsek, J.; et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients 2015, 7, 4966–4977. [Google Scholar] [CrossRef]
- Mansueto, P.; Seidita, A.; D’Alcamo, A.; Carroccio, A. Non-celiac gluten sensitivity: Literature review. J. Am. Coll. Nutr. 2014, 33, 39–54. [Google Scholar] [CrossRef]
- Elli, L.; Branchi, F.; Tomba, C.; Villalta, D.; Norsa, L.; Ferretti, F.; Roncoroni, L.; Bardella, M.T. Diagnosis of gluten related disorders: Celiac disease, wheat allergy and non-celiac gluten sensitivity. World J. Gastroenterol. 2015, 21, 7110–7119. [Google Scholar] [CrossRef] [PubMed]
- Catassi, C.; Bai, J.C.; Bonaz, B.; Bouma, G.; Calabrò, A.; Carroccio, A.; Castillejo, G.; Ciacci, C.; Cristofori, F.; Dolinsek, J.; et al. Non-Celiac Gluten sensitivity: The new frontier of gluten related disorders. Nutrients 2013, 5, 3839–3853. [Google Scholar] [CrossRef]
- Barbaro, M.R.; Cremon, C.; Wrona, D.; Fuschi, D.; Marasco, G.; Stanghellini, V.; Barbara, G. Non-Celiac Gluten Sensitivity in the Context of Functional Gastrointestinal Disorders. Nutrients 2020, 12, 3735. [Google Scholar] [CrossRef]
- Makharia, A.; Catassi, C.; Makharia, G.K. The Overlap between Irritable Bowel Syndrome and Non-Celiac Gluten Sensitivity: A Clinical Dilemma. Nutrients 2015, 7, 10417–10426. [Google Scholar] [CrossRef]
- Borrelli DE Andreis, F.; Schiepatti, A.; Gibiino, G.; Fabbri, C.; Baiardi, P.; Biagi, F. Is it time to rethink the burden of non-coeliac gluten sensitivity? A systematic review. Minerva Gastroenterol. 2022, 68, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Vasagar, B.; Cox, J.; Herion, J.T.; Ivanoff, E. World epidemiology of non-celiac gluten sensitivity. Minerva Gastroenterol. Dietol. 2017, 63, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Francavilla, R.; Cristofori, F.; Verzillo, L.; Gentile, A.; Castellaneta, S.; Polloni, C.; Giorgio, V.; Verduci, E.; D’Angelo, E.; Dellatte, S.; et al. Randomized Double-Blind Placebo-Controlled Crossover Trial for the Diagnosis of Non-Celiac Gluten Sensitivity in Children. Am. J. Gastroenterol. 2018, 113, 421–430. [Google Scholar] [CrossRef]
- Carroccio, A.; Giambalvo, O.; Blasca, F.; Iacobucci, R.; D’Alcamo, A.; Mansueto, P. Self-Reported Non-Celiac Wheat Sensitivity in High School Students: Demographic and Clinical Characteristics. Nutrients 2017, 9, 771. [Google Scholar] [CrossRef]
- Elli, L.; Tomba, C.; Branchi, F.; Roncoroni, L.; Lombardo, V.; Bardella, M.T.; Conte, D.; Valiante, F.; Fini, L.; Forti, E.; et al. Evidence for the Presence of Non-Celiac Gluten Sensitivity in Patients with Functional Gastrointestinal Symptoms: Results from a Multicenter Randomized Double-Blind Placebo-Controlled Gluten Challenge. Nutrients 2016, 8, 84. [Google Scholar] [CrossRef] [PubMed]
- Potter, M.; Jones, M.P.; Walker, M.M.; Koloski, N.A.; Keely, S.; Holtmann, G.; Talley AC, N.J. Incidence and prevalence of self-reported non-coeliac wheat sensitivity and gluten avoidance in Australia. Med. J. Aust. 2020, 212, 126–131. [Google Scholar] [CrossRef]
- Aziz, I.; Lewis, N.R.; Hadjivassiliou, M.; Winfield, S.N.; Rugg, N.; Kelsall, A.; Newrick, L.; Sanders, D.S. A UK study assessing the population prevalence of self-reported gluten sensitivity and referral characteristics to secondary care. Eur. J. Gastroenterol. Hepatol. 2014, 26, 33–39. [Google Scholar] [CrossRef]
- Brindicci, V.F.; Franceschini, S.; Gnasso, I.; Alcini, P.; Tassi, E.A.; Santarelli, L.; Cristofori, F.; Dargenio, V.N.; Castellaneta, S.; Francavilla, R.; et al. Self-Reported Nonceliac Gluten Sensitivity in Italian Young Adults: A Cross-Sectional Study. A Dietary Fad? Am. J. Gastroenterol. 2024, 119, 2114–2121. [Google Scholar] [CrossRef] [PubMed]
- van Gils, T.; Nijeboer, P.; IJssennagger, C.E.; Sanders, D.S.; Mulder, C.J.; Bouma, G. Prevalence and Characterization of Self-Reported Gluten Sensitivity in The Netherlands. Nutrients 2016, 8, 714. [Google Scholar] [CrossRef]
- Jansson-Knodell, C.L.; White, M.; Lockett, C.; Xu, H.; Rubio-Tapia, A.; Shin, A. Self-Reported Gluten Intolerance Is Prevalent, but Not All Gluten-Containing Foods Are Equal. Dig. Dis. Sci. 2023, 68, 1364–1368. [Google Scholar] [CrossRef]
- Cabrera-Chávez, F.; Dezar, G.V.; Islas-Zamorano, A.P.; Espinoza-Alderete, J.G.; Vergara-Jiménez, M.J.; Magaña-Ordorica, D.; Ontiveros, N. Prevalence of Self-Reported Gluten Sensitivity and Adherence to a Gluten-Free Diet in Argentinian Adult Population. Nutrients 2017, 9, 81. [Google Scholar] [CrossRef]
- Ontiveros, N.; Real-Delor, R.E.; Mora-Melgem, J.A.; Beltrán-Cárdenas, C.E.; Figueroa-Salcido, O.G.; Vergara-Jiménez, M.J.; Cárdenas-Torres, F.I.; Flores-Mendoza, L.K.; Arámburo-Gálvez, J.G.; Cabrera-Chávez, F. Prevalence of Wheat/Gluten-Related Disorders and Gluten-Free Diet in Paraguay: An Online Survey-Based Study. Nutrients 2021, 13, 396. [Google Scholar] [CrossRef] [PubMed]
- Ontiveros, N.; Rodríguez-Bellegarrigue, C.I.; Galicia-Rodríguez, G.; Vergara-Jiménez, M.J.; Zepeda-Gómez, E.M.; Arámburo-Galvez, J.G.; Gracia-Valenzuela, M.H.; Cabrera-Chávez, F. Prevalence of Self-Reported Gluten-Related Disorders and Adherence to a Gluten-Free Diet in Salvadoran Adult Population. Int. J. Environ. Res. Public Health 2018, 15, 786. [Google Scholar] [CrossRef]
- Arámburo-Gálvez, J.G.; Beltrán-Cárdenas, C.E.; Geralda André, T.; Carvalho Gomes, I.; Macêdo-Callou, M.A.; Braga-Rocha, É.M.; Mye-Takamatu-Watanabe, E.A.; Rahmeier-Fietz, V.; Figueroa-Salcido, O.G.; Vergara-Jiménez, M.J.; et al. Prevalence of Adverse Reactions to Gluten and People Going on a Gluten-Free Diet: A Survey Study Conducted in Brazil. Medicina 2020, 56, 163. [Google Scholar] [CrossRef]
- Lionetti, E.; Pulvirenti, A.; Vallorani, M.; Catassi, G.; Verma, A.K.; Gatti, S.; Catassi, C. Re-challenge Studies in Non-celiac Gluten Sensitivity: A Systematic Review and Meta-Analysis. Front. Physiol. 2017, 8, 621. [Google Scholar] [CrossRef]
- Dale, H.F.; Hatlebakk, J.G.; Hovdenak, N.; Ystad, S.O.; Lied, G.A. The effect of a controlled gluten challenge in a group of patients with suspected non-coeliac gluten sensitivity: A randomized, double-blind placebo-controlled challenge. Neurogastroenterol. Motil. 2018, 30, e13332. [Google Scholar] [CrossRef] [PubMed]
- Barone, M.; Gemello, E.; Viggiani, M.T.; Cristofori, F.; Renna, C.; Iannone, A.; Di Leo, A.; Francavilla, R. Evaluation of Non-Celiac Gluten Sensitivity in Patients with Previous Diagnosis of Irritable Bowel Syndrome: A Randomized Double-Blind Placebo-Controlled Crossover Trial. Nutrients 2020, 12, 705. [Google Scholar] [CrossRef] [PubMed]
- Zanini, B.; Baschè, R.; Ferraresi, A.; Ricci, C.; Lanzarotto, F.; Marullo, M.; Villanacci, V.; Hidalgo, A.; Lanzini, A. Randomised clinical study: Gluten challenge induces symptom recurrence in only a minority of patients who meet clinical criteria for non-coeliac gluten sensitivity. Aliment. Pharmacol. Ther. 2015, 42, 968–976. [Google Scholar] [CrossRef] [PubMed]
- de Graaf, M.C.G.; Lawton, C.L.; Croden, F.; Smolinska, A.; Winkens, B.; Hesselink, M.A.M.; van Rooy, G.; Weegels, P.L.; Shewry, P.R.; Houghton, L.A.; et al. The effect of expectancy versus actual gluten intake on gastrointestinal and extra-intestinal symptoms in non-coeliac gluten sensitivity: A randomised, double-blind, placebo-controlled, international, multicentre study. Lancet Gastroenterol. Hepatol. 2024, 9, 110–123. [Google Scholar] [CrossRef]
- Ahmed, A.; Dixit, K.; Singh, A.; Agarwal, A.; Mehtab, W.; Prasad, S.; Rajput, M.S.; Chauhan, A.; Agarwal, A.; Mehta, S.; et al. Sieving out non-celiac gluten sensitivity amongst patients with irritable bowel syndrome. Dig. Liver Dis. 2024, 56, 451–457. [Google Scholar] [CrossRef]
- Shahbazkhani, B.; Sadeghi, A.; Malekzadeh, R.; Khatavi, F.; Etemadi, M.; Kalantri, E.; Rostami-Nejad, M.; Rostami, K. Non-Celiac Gluten Sensitivity Has Narrowed the Spectrum of Irritable Bowel Syndrome: A Double-Blind Randomized Placebo-Controlled Trial. Nutrients 2015, 7, 4542–4554. [Google Scholar] [CrossRef]
- Shahbazkhani, B.; Fanaeian, M.M.; Farahvash, M.J.; Aletaha, N.; Alborzi, F.; Elli, L.; Shahbazkhani, A.; Zebardast, J.; Rostami-Nejad, M. Prevalence of Non-Celiac Gluten Sensitivity in Patients with Refractory Functional Dyspepsia: A Randomized Double-blind Placebo Controlled Trial. Sci. Rep. 2020, 10, 2401. [Google Scholar] [CrossRef]
- Hadjivassiliou, M.; Rao, D.G.; Grünewald, R.A.; Aeschlimann, D.P.; Sarrigiannis, P.G.; Hoggard, N.; Aeschlimann, P.; Mooney, P.D.; Sanders, D.S. Neurological Dysfunction in Coeliac Disease and Non-Coeliac Gluten Sensitivity. Am. J. Gastroenterol. 2016, 111, 561–567. [Google Scholar] [CrossRef]
- Carroccio, A.; Soresi, M.; Chiavetta, M.; La Blasca, F.; Compagnoni, S.; Giuliano, A.; Fayer, F.; Mandreucci, F.; Castellucci, D.; Seidita, A.; et al. Frequency and Clinical Aspects of Neurological and Psychiatric Symptoms in Patients with Non-Celiac Wheat Sensitivity. Nutrients 2021, 13, 1971. [Google Scholar] [CrossRef]
- Rodrigo, L.; Hernández-Lahoz, C.; Lauret, E.; Rodriguez-Peláez, M.; Soucek, M.; Ciccocioppo, R.; Kruzliak, P. Gluten ataxia is better classified as non-celiac gluten sensitivity than as celiac disease: A comparative clinical study. Immunol. Res. 2016, 64, 558–564. [Google Scholar] [CrossRef]
- Croall, I.D.; Hoggard, N.; Aziz, I.; Hadjivassiliou, M.; Sanders, D.S. Brain fog and non-coeliac gluten sensitivity: Proof of concept brain MRI pilot study. PLoS ONE 2020, 15, e0238283. [Google Scholar] [CrossRef]
- Mansueto, P.; Seidita, A.; Soresi, M.; Giuliano, A.; Riccio, G.; Volta, U.; Caio, G.; La Blasca, F.; Disclafani, R.; De Giorgio, R.; et al. Anemia in non-celiac wheat sensitivity: Prevalence and associated clinical and laboratory features. Dig. Liver Dis. 2023, 55, 735–742. [Google Scholar] [CrossRef]
- Peters, S.L.; Biesiekierski, J.R.; Yelland, G.W.; Muir, J.G.; Gibson, P.R. Randomised clinical trial: Gluten may cause depression in subjects with non-coeliac gluten sensitivity—An exploratory clinical study. Aliment. Pharmacol. Ther. 2014, 39, 1104–1112. [Google Scholar] [CrossRef]
- Brottveit, M.; Vandvik, P.O.; Wojniusz, S.; Løvik, A.; Lundin, K.E.; Boye, B. Absence of somatization in non-coeliac gluten sensitivity. Scand. J. Gastroenterol. 2012, 47, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Bonciolini, V.; Bianchi, B.; Del Bianco, E.; Verdelli, A.; Caproni, M. Cutaneous Manifestations of Non-Celiac Gluten Sensitivity: Clinical Histological and Immunopathological Features. Nutrients 2015, 7, 7798–7805. [Google Scholar] [CrossRef] [PubMed]
- Soresi, M.; Incandela, S.; Mansueto, P.; Incandela, G.; La Blasca, F.; Fayer, F.; D’Alcamo, A.; Florena, A.M.; Carroccio, A. Gynecological Disorders in Patients with Non-celiac Wheat Sensitivity. Dig. Dis. Sci. 2021, 66, 167–174. [Google Scholar] [CrossRef] [PubMed]
- D’Alcamo, A.; Mansueto, P.; Soresi, M.; Iacobucci, R.; Blasca, F.; Geraci, G.; Cavataio, F.; Fayer, F.; Arini, A.; Di Stefano, L.; et al. Contact Dermatitis Due to Nickel Allergy in Patients Suffering from Non-Celiac Wheat Sensitivity. Nutrients 2017, 9, 103. [Google Scholar] [CrossRef]
- Carroccio, A.; Soresi, M.; D’Alcamo, A.; Sciumè, C.; Iacono, G.; Geraci, G.; Brusca, I.; Seidita, A.; Adragna, F.; Carta, M.; et al. Risk of low bone mineral density and low body mass index in patients with non-celiac wheat-sensitivity: A prospective observation study. BMC Med. 2014, 12, 230. [Google Scholar] [CrossRef]
- Aziz, I.; Branchi, F.; Pearson, K.; Priest, J.; Sanders, D.S. A study evaluating the bidirectional relationship between inflammatory bowel disease and self-reported non-celiac gluten sensitivity. Inflamm. Bowel Dis. 2015, 21, 847–853. [Google Scholar] [CrossRef]
- Cha, R.R.; Kim, J.H.; Koo, H.S.; Jung, K.W.; Min, Y.W.; Choi, C.H.; Ryu, H.S.; Kwon, Y.H.; Cho, D.H.; Kwon, J.G.; et al. Self-reported Non-celiac Gluten Sensitivity in the Korean Population: Demographic and Clinical Characteristics. J. Neurogastroenterol. Motil. 2022, 28, 283–290. [Google Scholar] [CrossRef]
- Isasi, C.; Stadnitsky, A.; Casco, F.; Tejerina, E.; Royuela, A.; Esteban, B.; Puga, N.F. Non-celiac gluten sensitivity and chronic refractory low back pain with spondyloarthritis features. Med. Hypotheses 2020, 140, 109646. [Google Scholar] [CrossRef]
- Mansueto, P.; Soresi, M.; Candore, G.; Garlisi, C.; Fayer, F.; Gambino, C.M.; La Blasca, F.; Seidita, A.; D’Alcamo, A.; Lo Sasso, B.; et al. Autoimmunity Features in Patients With Non-Celiac Wheat Sensitivity. Am. J. Gastroenterol. 2021, 116, 1015–1023. [Google Scholar] [CrossRef]
- Isasi, C.; Colmenero, I.; Casco, F.; Tejerina, E.; Fernandez, N.; Serrano-Vela, J.I.; Castro, M.J.; Villa, L.F. Fibromyalgia and non-celiac gluten sensitivity: A description with remission of fibromyalgia. Rheumatol. Int. 2014, 34, 1607–1612. [Google Scholar] [CrossRef]
- Almirall, M.; Casellas, F.; Dot, J.; de Torres, I.; Segurola, H.; Marsal, S. Prevalence of non-coeliac gluten sensitivity and assessment of the response to gluten-free diet in a cohort of patients with fibromyalgia. Rheumatology 2023, 62, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Caio, G.; Riegler, G.; Patturelli, M.; Facchiano, A.; DEMagistris, L.; Sapone, A. Pathophysiology of non-celiac gluten sensitivity: Where are we now? Minerva Gastroenterol. Dietol. 2017, 63, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Schuppan, D.; Pickert, G.; Ashfaq-Khan, M.; Zevallos, V. Non-celiac wheat sensitivity: Differential diagnosis, triggers and implications. Best Pract. Res. Clin. Gastroenterol. 2015, 29, 469–476. [Google Scholar] [CrossRef]
- Junker, Y.; Zeissig, S.; Kim, S.J.; Barisani, D.; Wieser, H.; Leffler, D.A.; Zevallos, V.; Libermann, T.A.; Dillon, S.; Freitag, T.L.; et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J. Exp. Med. 2012, 209, 2395–2408. [Google Scholar] [CrossRef] [PubMed]
- Koumbi, L.; Giouleme, O.; Vassilopoulou, E. Non-Celiac Gluten Sensitivity and Irritable Bowel Disease: Looking for the Culprits. Curr. Dev. Nutr. 2020, 4, nzaa176. [Google Scholar] [CrossRef]
- Barbaro, M.R.; Cremon, C.; Morselli-Labate, A.M.; Di Sabatino, A.; Giuffrida, P.; Corazza, G.R.; Di Stefano, M.; Caio, G.; Latella, G.; Ciacci, C.; et al. Serum zonulin and its diagnostic performance in non-coeliac gluten sensitivity. Gut 2020, 69, 1966–1974. [Google Scholar] [CrossRef]
- Hollon, J.; Puppa, E.L.; Greenwald, B.; Goldberg, E.; Guerrerio, A.; Fasano, A. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients 2015, 7, 1565–1576. [Google Scholar] [CrossRef] [PubMed]
- Naseri, K.; Dabiri, H.; Olfatifar, M.; Shahrbaf, M.A.; Yadegar, A.; Soheilian-Khorzoghi, M.; Sadeghi, A.; Saadati, S.; Rostami-Nejad, M.; Verma, A.K.; et al. Evaluation of gut microbiota of iranian patients with celiac disease, non-celiac wheat sensitivity, and irritable bowel syndrome: Are there any similarities? BMC Gastroenterol. 2023, 23, 15. [Google Scholar] [CrossRef] [PubMed]
- Ponzo, V.; Ferrocino, I.; Goitre, I.; Pellegrini, M.; Bruno, M.; Astegiano, M.; Cadario, G.; Castellana, E.; Bioletto, F.; Corvaglia, M.R.; et al. Non-Celiac Gluten/Wheat Sensitivity: Clinical Characteristics and Microbiota and Mycobiota Composition by Response to the Gluten Challenge Test. Nutrients 2021, 13, 1260. [Google Scholar] [CrossRef]
- Dieterich, W.; Schuppan, D.; Schink, M.; Schwappacher, R.; Wirtz, S.; Agaimy, A.; Neurath, M.F.; Zopf, Y. Influence of low FODMAP and gluten-free diets on disease activity and intestinal microbiota in patients with non-celiac gluten sensitivity. Clin. Nutr. 2019, 38, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Skodje, G.I.; Sarna, V.K.; Minelle, I.H.; Rolfsen, K.L.; Muir, J.G.; Gibson, P.R.; Veierød, M.B.; Henriksen, C.; Lundin, K.E.A. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology 2018, 154, 529–539.e2. [Google Scholar] [CrossRef]
- Giancola, F.; Volta, U.; Repossi, R.; Latorre, R.; Beeckmans, D.; Carbone, F.; Van den Houte, K.; Bianco, F.; Bonora, E.; Gori, A.; et al. Mast cell-nerve interactions correlate with bloating and abdominal pain severity in patients with non-celiac gluten/wheat sensitivity. Neurogastroenterol. Motil. 2020, 32, e13814. [Google Scholar] [CrossRef]
- Brottveit, M.; Beitnes, A.C.; Tollefsen, S.; Bratlie, J.E.; Jahnsen, F.L.; Johansen, F.E.; Sollid, L.M.; Lundin, K.E. Mucosal cytokine response after short-term gluten challenge in celiac disease and non-celiac gluten sensitivity. Am. J. Gastroenterol. 2013, 108, 842–850. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Rodal, A.I.; Furuzawa-Carballeda, J.; Peláez-Luna, M.; Castro-Gómez, J.; López-Vidal, Y.; Uscanga, L. More fuel to the fire: Some patients with non-celiac self-reported wheat sensitivity exhibit adaptive immunological responses in duodenal mucosa. BMC Gastroenterol. 2020, 20, 414. [Google Scholar] [CrossRef]
- Gupta, K.B.; Dhiman, M.; Mantha, A.K. Gliadin induced oxidative stress and altered cellular responses in human intestinal cells: An in-vitro study to understand the cross-talk between the transcription factor Nrf-2 and multifunctional APE1 enzyme. J. Biochem. Mol. Toxicol. 2022, 36, e23096. [Google Scholar] [CrossRef]
- Ferrari, E.; Monzani, R.; Saverio, V.; Gagliardi, M.; Pańczyszyn, E.; Raia, V.; Villella, V.R.; Bona, G.; Pane, M.; Amoruso, A.; et al. Probiotics Supplements Reduce ER Stress and Gut Inflammation Associated with Gliadin Intake in a Mouse Model of Gluten Sensitivity. Nutrients 2021, 13, 1221. [Google Scholar] [CrossRef] [PubMed]
- Pickert, G.; Wirtz, S.; Matzner, J.; Ashfaq-Khan, M.; Heck, R.; Rosigkeit, S.; Thies, D.; Surabattula, R.; Ehmann, D.; Wehkamp, J.; et al. Wheat Consumption Aggravates Colitis in Mice via Amylase Trypsin Inhibitor-mediated Dysbiosis. Gastroenterology 2020, 159, 257–272.e17. [Google Scholar] [CrossRef]
- Zevallos, V.F.; Raker, V.; Tenzer, S.; Jimenez-Calvente, C.; Ashfaq-Khan, M.; Rüssel, N.; Pickert, G.; Schild, H.; Steinbrink, K.; Schuppan, D. Nutritional Wheat Amylase-Trypsin Inhibitors Promote Intestinal Inflammation via Activation of Myeloid Cells. Gastroenterology 2017, 152, 1100–1113.e12. [Google Scholar] [CrossRef] [PubMed]
- Krouch, D.; Vreeke, G.J.C.; America, A.H.P.; Mes, J.J.; Wierenga, P.A.; Vincken, J.P.; Bastiaan-Net, S.; Weegels, P.L. Amylase trypsin inhibitors activation of toll-like receptor 4 revisited: The dominance of lipopolysaccharides contamination. Int. J. Biol. Macromol. 2025, 310, 143378. [Google Scholar] [CrossRef] [PubMed]
- Bellinghausen, I.; Weigmann, B.; Zevallos, V.; Maxeiner, J.; Reißig, S.; Waisman, A.; Schuppan, D.; Saloga, J. Wheat amylase-trypsin inhibitors exacerbate intestinal and airway allergic immune responses in humanized mice. J. Allergy Clin. Immunol. 2019, 143, 201–212.e4. [Google Scholar] [CrossRef]
- Zevallos, V.F.; Raker, V.K.; Maxeiner, J.; Scholtes, P.; Steinbrink, K.; Schuppan, D. Dietary wheat amylase trypsin inhibitors exacerbate murine allergic airway inflammation. Eur. J. Nutr. 2019, 58, 1507–1514. [Google Scholar] [CrossRef]
- Esmaeili, P.; Rostami, E.; Akbarijavar, A.; Akbari Meyestani, A.; Bashiri, H.; Rezaee, M.A.; Fakhari, S. Effects of Gliadin on Autoimmune Responses of Central Nervous System of C57BL/6 Mice. Iran. J. Allergy Asthma Immunol. 2021, 20, 188–197. [Google Scholar] [CrossRef]
- Zingone, F.; Maimaris, S.; Auricchio, R.; Caio, G.P.I.; Carroccio, A.; Elli, L.; Galliani, E.; Montagnani, M.; Valiante, F.; Biagi, F. Guidelines of the Italian societies of gastroenterology on the diagnosis and management of coeliac disease and dermatitis herpetiformis. Dig. Liver Dis. 2022, 54, 1304–1319. [Google Scholar] [CrossRef]
- Volta, U.; Caio, G.; Tovoli, F.; De Giorgio, R. Non-celiac gluten sensitivity: Questions still to be answered despite increasing awareness. Cell Mol. Immunol. 2013, 10, 383–392. [Google Scholar] [CrossRef]
- Talley, N.J.; Holtmann, G.J.; Jones, M.; Koloski, N.A.; Walker, M.M.; Burns, G.; Potter, M.D.E.; Shah, A.; Keely, S. Zonulin in serum as a biomarker fails to identify the IBS, functional dyspepsia and non-coeliac wheat sensitivity. Gut 2020, 69, 1719–1722. [Google Scholar] [CrossRef] [PubMed]
- Ajamian, M.; Rosella, G.; Newnham, E.D.; Biesiekierski, J.R.; Muir, J.G.; Gibson, P.R. Effect of Gluten Ingestion and FODMAP Restriction on Intestinal Epithelial Integrity in Patients with Irritable Bowel Syndrome and Self-Reported Non-Coeliac Gluten Sensitivity. Mol. Nutr. Food Res. 2021, 65, e1901275. [Google Scholar] [CrossRef]
- Transeth, E.L.; Dale, H.F.; Lied, G.A. Comparison of gut microbiota profile in celiac disease, non-celiac gluten sensitivity and irritable bowel syndrome: A systematic review. Turk. J. Gastroenterol. 2020, 31, 735–745. [Google Scholar] [CrossRef]
- Haro, C.; Villatoro, M.; Vaquero, L.; Pastor, J.; Giménez, M.J.; Ozuna, C.V.; Sánchez-León, S.; García-Molina, M.D.; Segura, V.; Comino, I.; et al. The Dietary Intervention of Transgenic Low-Gliadin Wheat Bread in Patients with Non-Celiac Gluten Sensitivity (NCGS) Showed No Differences with Gluten Free Diet (GFD) but Provides Better Gut Microbiota Profile. Nutrients 2018, 10, 1964. [Google Scholar] [CrossRef] [PubMed]
- Nobel, Y.R.; Rozenberg, F.; Park, H.; Freedberg, D.E.; Blaser, M.J.; Green, P.H.R.; Uhlemann, A.C.; Lebwohl, B. Lack of Effect of Gluten Challenge on Fecal Microbiome in Patients With Celiac Disease and Non-Celiac Gluten Sensitivity. Clin. Transl. Gastroenterol. 2021, 12, e00441. [Google Scholar] [CrossRef]
- Garcia-Mazcorro, J.F.; Rivera-Gutierrez, X.; Cobos-Quevedo, O.J.; Grube-Pagola, P.; Meixueiro-Daza, A.; Hernandez-Flores, K.; Cabrera-Jorge, F.J.; Vivanco-Cid, H.; Dowd, S.E.; Remes-Troche, J.M. First Insights into the Gut Microbiota of Mexican Patients with Celiac Disease and Non-Celiac Gluten Sensitivity. Nutrients 2018, 10, 1641. [Google Scholar] [CrossRef]
- Herfindal, A.M.; Nilsen, M.; Aspholm, T.E.; Schultz, G.I.G.; Valeur, J.; Rudi, K.; Thoresen, M.; Lundin, K.E.A.; Henriksen, C.; Bøhn, S.K. Effects of fructan and gluten on gut microbiota in individuals with self-reported non-celiac gluten/wheat sensitivity—A randomised controlled crossover trial. BMC Med. 2024, 22, 358. [Google Scholar] [CrossRef]
- Gambino, C.M.; Agnello, L.; Vidali, M.; Lo Sasso, B.; Mansueto, P.; Seidita, A.; Giuliano, A.; Scazzone, C.; Massa, D.; Masucci, A.; et al. The role of Killer immunoglobulin-like receptors (KIRs) in the genetic susceptibility to non-celiac wheat sensitivity (NCWS). Clin. Chem. Lab. Med. 2024, 62, 1814–1823. [Google Scholar] [CrossRef]
- Efthymakis, K.; Clemente, E.; Marchioni, M.; Di Nicola, M.; Neri, M.; Sallese, M. An Exploratory Gene Expression Study of the Intestinal Mucosa of Patients with Non-Celiac Wheat Sensitivity. Int. J. Mol. Sci. 2020, 21, 1969. [Google Scholar] [CrossRef]
- Clemente, E.; Efthymakis, K.; Carletti, E.; Capone, V.; Sperduti, S.; Bologna, G.; Marchisio, M.; Di Nicola, M.; Neri, M.; Sallese, M. An explorative study identifies miRNA signatures for the diagnosis of non-celiac wheat sensitivity. PLoS ONE 2019, 14, e0226478. [Google Scholar] [CrossRef] [PubMed]
- Sallese, M.; Efthymakis, K.; Marchioni, M.; Neri, B.; Dufrusine, B.; Dainese, E.; Di Nicola, M.; Neri, M. Gene Expression Profiling in Coeliac Disease Confirmed the Key Role of the Immune System and Revealed a Molecular Overlap with Non-Celiac Gluten Sensitivity. Int. J. Mol. Sci. 2023, 24, 7769. [Google Scholar] [CrossRef] [PubMed]
- Sazzini, M.; De Fanti, S.; Cherubini, A.; Quagliariello, A.; Profiti, G.; Martelli, P.L.; Casadio, R.; Ricci, C.; Campieri, M.; Lanzini, A.; et al. Ancient pathogen-driven adaptation triggers increased susceptibility to non-celiac wheat sensitivity in present-day European populations. Genes Nutr. 2016, 11, 15. [Google Scholar] [CrossRef]
- Leccioli, V.; Oliveri, M.; Romeo, M.; Berretta, M.; Rossi, P. A New Proposal for the Pathogenic Mechanism of Non-Coeliac/Non-Allergic Gluten/Wheat Sensitivity: Piecing Together the Puzzle of Recent Scientific Evidence. Nutrients 2017, 9, 1203. [Google Scholar] [CrossRef] [PubMed]
- Mumolo, M.G.; Rettura, F.; Melissari, S.; Costa, F.; Ricchiuti, A.; Ceccarelli, L.; de Bortoli, N.; Marchi, S.; Bellini, M. Is Gluten the Only Culprit for Non-Celiac Gluten/Wheat Sensitivity? Nutrients 2020, 12, 3785. [Google Scholar] [CrossRef] [PubMed]
- Moleski, S.M.; Shah, A.; Durney, P.; Matthews, M.; Kaushal, G.; Smith, C.; Koons, K.C.; Rubin, E.; Casey, P.; Miller, R.; et al. Symptoms of gluten ingestion in patients with non-celiac gluten sensitivity: A randomized clinical trial. Nutrition 2021, 81, 110944. [Google Scholar] [CrossRef]
- Di Sabatino, A.; Volta, U.; Salvatore, C.; Biancheri, P.; Caio, G.; De Giorgio, R.; Di Stefano, M.; Corazza, G.R. Small Amounts of Gluten in Subjects With Suspected Nonceliac Gluten Sensitivity: A Randomized, Double-Blind, Placebo-Controlled, Cross-Over Trial. Clin. Gastroenterol. Hepatol. 2015, 13, 1604–1612.e3. [Google Scholar] [CrossRef]
- An, C.; Yang, J.; Pinto-Sanchez, M.I.; Verdu, E.F.; Lebwohl, B.; Green, P.H.; Alaedini, A. Molecular Triggers of Non-celiac Wheat Sensitivity: A Scoping Review and Analysis. Am. J. Gastroenterol. 2025, 120, 1998–2008. [Google Scholar] [CrossRef] [PubMed]
- Roncoroni, L.; Bascuñán, K.A.; Vecchi, M.; Doneda, L.; Bardella, M.T.; Lombardo, V.; Scricciolo, A.; Branchi, F.; Elli, L. Exposure to Different Amounts of Dietary Gluten in Patients with Non-Celiac Gluten Sensitivity (NCGS): An Exploratory Study. Nutrients 2019, 11, 136. [Google Scholar] [CrossRef]
- Rabinowitz, L.G.; Zylberberg, H.M.; Levinovitz, A.; Stockwell, M.S.; Green, P.H.R.; Lebwohl, B. Skepticism Regarding Vaccine and Gluten-Free Food Safety Among Patients with Celiac Disease and Non-celiac Gluten Sensitivity. Dig. Dis. Sci. 2018, 63, 1158–1164. [Google Scholar] [CrossRef]
- Fardet, A. Wheat-based foods and non celiac gluten/wheat sensitivity: Is drastic processing the main key issue? Med. Hypotheses 2015, 85, 934–939. [Google Scholar] [CrossRef]
- Ianiro, G.; Rizzatti, G.; Napoli, M.; Matteo, M.V.; Rinninella, E.; Mora, V.; Fanali, C.; Leonetti, A.; Benedettelli, S.; Mele, M.C.; et al. A Durum Wheat Variety-Based Product Is Effective in Reducing Symptoms in Patients with Non-Celiac Gluten Sensitivity: A Double-Blind Randomized Cross-Over Trial. Nutrients 2019, 11, 712. [Google Scholar] [CrossRef]
- Seidita, A.; Mansueto, P.; Giuliano, A.; Chiavetta, M.; Mandreucci, F.; Soresi, M.; Pistone, M.; Compagnoni, S.; Castellucci, D.; Bisso, G.; et al. Potential tolerability of ancient grains in non-celiac wheat sensitivity patients: A preliminary evaluation. Front. Med. 2022, 9, 995019. [Google Scholar] [CrossRef]
- Catassi, G.; Catassi, C. An overview of progress in establishing a diagnostic tool for non-celiac gluten sensitivity. Expert. Rev. Mol. Diagn. 2025, 25, 59–66. [Google Scholar] [CrossRef]
- Størdal, K.; Kurppa, K. Celiac disease, non-celiac wheat sensitivity, wheat allergy—Clinical and diagnostic aspects. Semin. Immunol. 2025, 77, 101930. [Google Scholar] [CrossRef]
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K.E.A. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613. [Google Scholar] [CrossRef]
- Maimaris, S.; Schiepatti, A.; Saracino, M.; Ongarelli, L.; Torres, D.I.C.; Scarcella, C.; Minerba, P.; Biagi, F. Diagnostic outcomes after gluten challenge in adult patients with unconfirmed coeliac disease already on a gluten-free diet: A 20-year retrospective cohort study. Dig. Liver Dis. 2025, 57, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Ventoso, M.; Ignatiev, J.H.; Shin, S.; Krishnareddy, S.; Lewis, S.; Green, P.H.R.; Lebwohl, B. Yield of Gluten Challenge in Patients on Self-Prescribed Gluten-Free Diets. Dig. Dis. Sci. 2024, 69, 2916–2921. [Google Scholar] [CrossRef]
- Ford, A.C.; Sperber, A.D.; Corsetti, M.; Camilleri, M. Irritable bowel syndrome. Lancet 2020, 396, 1675–1688. [Google Scholar] [CrossRef]
- Carroccio, A.; Mansueto, P.; Iacono, G.; Soresi, M.; D’Alcamo, A.; Cavataio, F.; Brusca, I.; Florena, A.M.; Ambrosiano, G.; Seidita, A.; et al. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: Exploring a new clinical entity. Am. J. Gastroenterol. 2012, 107, 1898–1906. [Google Scholar] [CrossRef] [PubMed]
- Infantino, M.; Meacci, F.; Grossi, V.; Macchia, D.; Manfredi, M. Anti-gliadin antibodies in non-celiac gluten sensitivity. Minerva Gastroenterol. Dietol. 2017, 63, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Infantino, M.; Manfredi, M.; Meacci, F.; Grossi, V.; Severino, M.; Benucci, M.; Bellio, E.; Bellio, V.; Nucci, A.; Zolfanelli, F.; et al. Diagnostic accuracy of anti-gliadin antibodies in Non Celiac Gluten Sensitivity (NCGS) patients: A dual statistical approach. Clin. Chim. Acta 2015, 451, 135–141. [Google Scholar] [CrossRef]
- Rostami, K.; Ensari, A.; Marsh, M.N.; Srivastava, A.; Villanacci, V.; Carroccio, A.; Asadzadeh Aghdaei, H.; Bai, J.C.; Bassotti, G.; Becheanu, G.; et al. Gluten Induces Subtle Histological Changes in Duodenal Mucosa of Patients with Non-Coeliac Gluten Sensitivity: A Multicentre Study. Nutrients 2022, 14, 2487. [Google Scholar] [CrossRef] [PubMed]
- Kirmizi, A.; Salman, F.G.; Savas, B.; Kalkan, C.; Soykan, I.; Ensari, A. Histopathology of non-coeliac gluten sensitivity. Virchows Arch. 2022, 480, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Carroccio, A.; Giannone, G.; Mansueto, P.; Soresi, M.; La Blasca, F.; Fayer, F.; Iacobucci, R.; Porcasi, R.; Catalano, T.; Geraci, G.; et al. Duodenal and Rectal Mucosa Inflammation in Patients With Non-celiac Wheat Sensitivity. Clin. Gastroenterol. Hepatol. 2019, 17, 682–690.e3. [Google Scholar] [CrossRef]
- Zanini, B.; Villanacci, V.; Marullo, M.; Cadei, M.; Lanzarotto, F.; Bozzola, A.; Ricci, C. Duodenal histological features in suspected non-celiac gluten sensitivity: New insights into a still undefined condition. Virchows Arch. 2018, 473, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Figueroa-Salcido, O.G.; Ontiveros, N.; Cabrera-Chavez, F. Gluten Vehicle and Placebo for Non-Celiac Gluten Sensitivity Assessment. Medicina 2019, 55, 117. [Google Scholar] [CrossRef]
- Barmeyer, C.; Schumann, M.; Meyer, T.; Zielinski, C.; Zuberbier, T.; Siegmund, B.; Schulzke, J.D.; Daum, S.; Ullrich, R. Long-term response to gluten-free diet as evidence for non-celiac wheat sensitivity in one third of patients with diarrhea-dominant and mixed-type irritable bowel syndrome. Int. J. Color. Dis. 2017, 32, 29–39. [Google Scholar] [CrossRef]
- Corazza, G.R.; Villanacci, V. Coeliac disease. J. Clin. Pathol. 2005, 58, 573–574. [Google Scholar] [CrossRef]
- Di Liberto, D.; Mansueto, P.; D’Alcamo, A.; Lo Pizzo, M.; Lo Presti, E.; Geraci, G.; Fayer, F.; Guggino, G.; Iacono, G.; Dieli, F.; et al. Predominance of Type 1 Innate Lymphoid Cells in the Rectal Mucosa of Patients With Non-Celiac Wheat Sensitivity: Reversal After a Wheat-Free Diet. Clin. Transl. Gastroenterol. 2016, 7, e178. [Google Scholar] [CrossRef]
- Caio, G.; Volta, U.; Tovoli, F.; De Giorgio, R. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol. 2014, 14, 26. [Google Scholar] [CrossRef]
- Dale, H.F.; Johannessen, J.C.H.; Brønstad, I.; Lied, G.A. Assessment of Markers of Gut Integrity and Inflammation in Non-Celiac Gluten Sensitivity After a Gluten Free-Diet. Int. J. Gen. Med. 2021, 14, 9459–9470. [Google Scholar] [CrossRef]
- Masaebi, F.; Azizmohammad Looha, M.; Rostami-Nejad, M.; Pourhoseingholi, M.A.; Mohseni, N.; Samasca, G.; Lupan, I.; Rezaei-Tavirani, M.; Zali, M.R. The Predictive Value of Serum Cytokines for Distinguishing Celiac Disease from Non-Celiac Gluten Sensitivity and Healthy Subjects. Iran. Biomed. J. 2020, 24, 340–346. [Google Scholar] [CrossRef]
- Heydari, F.; Rostami-Nejad, M.; Moheb-Alian, A.; Mollahoseini, M.H.; Rostami, K.; Pourhoseingholi, M.A.; Aghamohammadi, E.; Zali, M.R. Serum cytokines profile in treated celiac disease compared with non-celiac gluten sensitivity and control: A marker for differentiation. J. Gastrointest. Liver Dis. 2018, 27, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Seidita, A.; Giuliano, A.; Soresi, M.; Chiavetta, M.; Nardi, E.; Mogavero, G.; Giannone, G.; Carroccio, A.; Mansueto, P. Fecal calprotectin levels in patients with non-celiac wheat sensitivity: A proof of concept. Intern. Emerg. Med. 2024, 19, 1255–1266. [Google Scholar] [CrossRef] [PubMed]
- Martín-Cardona, A.; Carrasco, A.; Arau, B.; Vidal, J.; Tristán, E.; Ferrer, C.; Gonzalez-Puglia, G.; Pallarès, N.; Tebé, C.; Farrais, S.; et al. γδ+ T-Cells Is a Useful Biomarker for the Differential Diagnosis between Celiac Disease and Non-Celiac Gluten Sensitivity in Patients under Gluten Free Diet. Nutrients 2024, 16, 2294. [Google Scholar] [CrossRef]
- Vignoli, A.; Luchinat, C.; Segata, N.; Renzi, D.; Tenori, L.; Calabrò, A.S. Serum metabolomics and lipoproteomics discriminate celiac disease and non-celiac gluten sensitivity patients. Clin. Nutr. 2025, 45, 31–35. [Google Scholar] [CrossRef]
- Di Stefano, M.; Pesatori, E.V.; Manfredi, G.F.; De Amici, M.; Grandi, G.; Gabriele, A.; Iozzi, D.; Di Fede, G. Non-Celiac Gluten Sensitivity in patients with severe abdominal pain and bloating: The accuracy of ALCAT 5. Clin. Nutr. ESPEN 2018, 28, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Tovoli, F.; Granito, A.; Negrini, G.; Guidetti, E.; Faggiano, C.; Bolondi, L. Long term effects of gluten-free diet in non-celiac wheat sensitivity. Clin. Nutr. 2019, 38, 357–363. [Google Scholar] [CrossRef]
- Skodje, G.I.; Minelle, I.H.; Rolfsen, K.L.; Iacovou, M.; Lundin, K.E.A.; Veierød, M.B.; Henriksen, C. Dietary and symptom assessment in adults with self-reported non-coeliac gluten sensitivity. Clin. Nutr. ESPEN 2019, 31, 88–94. [Google Scholar] [CrossRef]
- Di Pierro, F.; Bergomas, F.; Marraccini, P.; Ingenito, M.R.; Ferrari, L.; Vigna, L. Pilot study on non-celiac gluten sensitivity: Effects of Bifidobacterium longum ES1 co-administered with a gluten-free diet. Minerva Gastroenterol. Dietol. 2020, 66, 187–193. [Google Scholar] [CrossRef]
- Ido, H.; Matsubara, H.; Kuroda, M.; Takahashi, A.; Kojima, Y.; Koikeda, S.; Sasaki, M. Combination of Gluten-Digesting Enzymes Improved Symptoms of Non-Celiac Gluten Sensitivity: A Randomized Single-blind, Placebo-controlled Crossover Study. Clin. Transl. Gastroenterol. 2018, 9, 181. [Google Scholar] [CrossRef]
- Scricciolo, A.; Lombardo, V.; Elli, L.; Bascuñán, K.A.; Doneda, L.; Rinaldi, F.; Pinto, D.; Araya, M.; Costantino, A.; Vecchi, M.; et al. Use of a proline-specific endopeptidase to reintroduce gluten in patients with non-coeliac gluten sensitivity: A randomized trial. Clin. Nutr. 2022, 41, 2025–2030. [Google Scholar] [CrossRef]
- Løvik, A.; Skodje, G.; Bratlie, J.; Brottveit, M.; Lundin, K.E. Diet adherence and gluten exposure in coeliac disease and self-reported non-coeliac gluten sensitivity. Clin. Nutr. 2017, 36, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Cotton, C.; Raju, S.A.; Ahmed, H.; Webster, G.; Hallam, R.; Croall, I.; Coleman, S.; Trott, N.; Rej, A.; Shiha, M.G.; et al. Does a Gluten-Free Diet Improve Quality of Life and Sleep in Patients with Non-Coeliac Gluten/Wheat Sensitivity? Nutrients 2023, 15, 3461. [Google Scholar] [CrossRef] [PubMed]
- Maimaris, S.; Schiepatti, A.; Biagi, F. Systematic review with meta-analysis: Cause-specific and all-cause mortality trends across different coeliac disease phenotypes. Aliment. Pharmacol. Ther. 2024, 59, 592–605. [Google Scholar] [CrossRef] [PubMed]
| Category | Symptoms |
|---|---|
| Gastrointestinal | Abdominal pain, bloating, altered bowel habits (diarrhoea/constipation), flatulence, dyspepsia [16,17,37,38,39]. Symptoms often overlap with irritable bowel syndrome. |
| Extra-intestinal/Systemic | Fatigue, lethargy (‘brain fog’), headaches (often migraine-like), musculoskeletal pain (fibromyalgia-like), anaemia [40,41,42,43,44]. |
| Neurological/Psychiatric | Cognitive disturbances, peripheral neuropathy, ataxia, anxiety, depression [40,41,42,43,45,46]. |
| Dermatological | Eczema-like or psoriasis-like skin rashes, dermatitis herpetiformis-like lesions [47]. |
| Other Associations | Gynaecological issues (menstrual irregularities, recurrent vaginitis) [48], increased prevalence of atopy and nickel allergy [49], reduced bone mineral density (osteopenia/osteoporosis) [50]. |
| Mechanism | Hypothesised Effect | Key Evidence/Mediators |
|---|---|---|
| Innate Immune Activation | Wheat components trigger an innate immune response in the gut mucosa, leading to low-grade inflammation. | Amylase-trypsin inhibitors activating toll-like receptor 4 [58,59]; increased pro-inflammatory cytokines (e.g., TNF-α, IL-8) [58,60]. |
| Increased Intestinal Permeability | A compromised gut barrier (“leaky gut”) allows microbial products and dietary antigens to cross into circulation, causing immune activation. | Increased serum zonulin in some studies [61]; ex vivo studies showing increased permeability upon gliadin exposure [62]. |
| Gut Microbiota Dysbiosis | Alterations in the composition and function of the gut microbiome contribute to symptoms and inflammation. | Altered Firmicutes/Bacteroidetes ratio; reduced Bifidobacterium; changes in microbial profiles vs. controls and CD patients [63,64,65]. |
| FODMAP Intolerance | Fermentation of short-chain carbohydrates (especially fructans from wheat) by gut bacteria leads to gas, bloating, and pain. | DBPCC trials showing fructans induce more symptoms than gluten in some self-reported NCWS individuals [6,66]. |
| Neuro-immune Interactions | Increased interaction between immune cells (mast cells) and the enteric nervous system enhances visceral hypersensitivity. | Increased mast cell density in close proximity to submucosal nerve fibres, correlating with pain and bloating severity [67]. |
| Mild Adaptive Immunity | A low-level adaptive immune response, distinct from and less intense than that seen in CD. | Presence of IgG-AGA in some patients [37]; slight increase in Th1/Th17-related cytokines and duodenal IFN-γ mRNA [68,69]. |
| Challenge | Key Findings | Implications for Diagnosis and Research |
|---|---|---|
| High Placebo and Nocebo Effects | A significant portion of patients report symptom recurrence when given a placebo they believe contains gluten. | Complicates interpretation of DBPCCs; highlights the strong psychological component and symptom anticipation [33,35]. |
| Power of Expectation | The mere expectation of consuming gluten can cause a greater increase in symptoms than covertly consuming gluten itself. | The nocebo effect may be a greater driver of symptoms than gluten in many individuals, clouding diagnostic clarity [36]. |
| Inability to Distinguish | In several blinded trials, patients as a group could not reliably distinguish gluten from placebo, sometimes reporting worse symptoms on placebos. | Questions the specificity of gluten as the sole trigger in a large subset of self-diagnosed NCWS patients [33]. |
| Inconsistent DBPCC Results | Meta-analyses show high variability in gluten relapse rates (7–77%) and often no significant difference from the placebo unless strict criteria are used. | Standardisation of DBPCC protocols (e.g., Salerno Criteria) is critical to obtain reliable and comparable results [32]. |
| Methodological Variation | Wide variation in participant selection, gluten/placebo vehicle, challenge dose, and outcome measures across studies. | Lack of standardisation hinders the ability to compare studies and draw firm conclusions on gluten’s pathogenetic role [96]. |
| Feature | Non-Coeliac Wheat Sensitivity | Coeliac Disease | Wheat Allergy | Irritable Bowel Syndrome |
|---|---|---|---|---|
| Pathophysiology | Innate immunity [58,79], barrier dysfunction [61,62], microbial dysbiosis suspected [60]. | HLA-DQ2/DQ8 associated adaptive T-cell response to gluten [78,104]. | IgE-mediated or non-IgE-mediated reaction to wheat proteins [103]. | Visceral hypersensitivity, altered motility, gut–brain axis dysfunction [107]. |
| Key Symptoms | IBS-like GI symptoms + diverse extra-intestinal (fatigue, ‘brain fog’, headache, pain) [16,17,38,40,41,42,43]. | GI symptoms (diarrhoea, malabsorption) + extra-intestinal [78,104]. | Rapid onset (mins–hrs) urticaria, angioedema, asthma; or delayed GI symptoms [103]. | Recurrent abdominal pain related to defecation, change in stool frequency/form [107]. |
| Symptom Onset | Hours to days after ingestion [9,13]. | Variable, can be delayed [78,104]. | IgE-mediated: minutes to 2 h. Non-IgE: hours to days [103]. | Chronic, fluctuating; can be triggered by food (incl. wheat), stress [107]. |
| Serology | Negative CD/WA serology. IgG AGA may be positive (~50%) [108,109,110]. | Positive anti-tTG, anti-EMA, anti-DGP IgA [78,104]. | Positive wheat-specific IgE (for IgE-mediated WA) [103]. | Negative for specific markers [107]. |
| Genetics (HLA) | HLA-DQ2/DQ8 in ~50% (vs ~30% in general population) [41]. | Strong association with HLA-DQ2/DQ8 (>95%) [78,104]. | No specific HLA association [103]. | No specific HLA association [107]. |
| Histology (Duodenum) | Normal or minimal changes (Marsh 0-I), mild IEL increase, eosinophils [68,108,111,112,113,114]. | Villous atrophy, crypt hyperplasia, significant IEL increase (Marsh III) [78,104]. | Usually normal [103]. | Usually normal [107]. |
| Diagnosis | Exclusion of CD/WA, followed by DBPCC (Salerno criteria) [12]. | Positive serology + duodenal biopsy showing villous atrophy [78,104]. | Clinical history + positive IgE tests or skin prick tests [103]. | Symptom-based criteria (Rome IV) after excluding organic disease [107]. |
| Primary Trigger | Gluten, fructans, ATIs, other wheat components [32,58,66]. | Gluten [78,104]. | Wheat proteins (gluten and others) [103]. | Various foods (FODMAPs), stress, visceral sensitivity [107]. |
| Biomarker | Proposed Role | Key Findings and Limitations |
|---|---|---|
| IgG Anti-Gliadin Antibodies | Serological marker of gluten exposure/reaction. | Positive in ~50% of NCWS, but low sensitivity and specificity [108,109,110]. Not diagnostic. Tend to normalise on GFD [119]. |
| Zonulin | Marker of intestinal permeability. | Controversial. Some studies show higher levels vs. IBS [61], others find no difference [62]. Not reliable for diagnosis. |
| I-FABP, LBP, sCD14 | Markers of epithelial barrier integrity and microbial translocation. | No significant differences found between NCWS, IBS, and healthy controls in most studies [81,120]. |
| Serum Cytokines (e.g., IL-6, IL-8) | Markers of systemic inflammation. | Some studies show different profiles vs. CD/controls, but findings are inconsistent and not validated for diagnostic use [121,122]. |
| Faecal Calprotectin (FC) | Marker of intestinal inflammation. | One study found elevated FC in ~31% of NCWS patients (vs. 0% in IBS) [123], suggesting potential but requiring validation. |
| Duodenal Histology (IELs, Eosinophils) | Quantifying subtle mucosal inflammation. | Slight increases in IELs and eosinophils reported, but overlap with controls is large [68,108,111,112,113,114]. Not useful for individual diagnosis. |
| Flow Cytometry (TCRγδ + IELs) | Differentiating CD from NCWS in patients on GFD. | Promising results in one study to exclude CD (even on GFD), but not a positive marker for NCWS [124]. Needs validation. |
| Metabolomics/Lipoprotein Profiles | Identifying unique metabolic signatures. | Pilot study suggested potential to distinguish NCWS from CD, but still preliminary and requires validation [125]. |
| ALCAT 5 Test | In vitro food sensitivity testing. | One pilot study showed 64% concordance with DBPCC. Not validated and has low accuracy for clinical use [126]. |
| Genetic Markers (KIR, CXCL10/11) | Identifying genetic predisposition. | Research findings of associations exist [85,89], but these are not diagnostic markers for clinical practice. |
| Intervention | Description | State of Evidence |
|---|---|---|
| Gluten-Free Diet (GFD) | Strict elimination of wheat, barley, rye, and related grains. | Primary Treatment. Most patients improve, but response rates vary and mild symptoms may persist [18,127,128]. |
| Low-FODMAP Diet | Restriction of fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. | Evidence for Symptom Control. Effective, especially as wheat is a major source of fructans (a FODMAP) [6,34,65,81]. May be combined with GFD. |
| ‘Ancient’ Wheat Grains | Consumption of older wheat varieties (e.g., Senatore Cappelli, Khorasan). | Limited Evidence. Some studies suggest better tolerability in a subset of patients, but not a substitute for GFD in sensitive individuals [100,101]. |
| Probiotics | Supplementation with specific bacterial strains (Bifidobacterium longum ES1). | Preliminary Evidence. One open-label pilot study showed improved symptoms when combined with a GFD [129]. More research needed. |
| Enzyme Supplements | Oral enzymes designed to break down gluten peptides in the gut. | Mixed/Weak Evidence. Some small studies show modest benefit [130], while others show no effect compared to placebo [131]. Not a validated treatment. |
| Domain | Finding | Primary Study Types | Level of Evidence * |
|---|---|---|---|
| Epidemiology | High prevalence of self-reported wheat sensitivity (~5–15%). | Cross-sectional surveys. | Low |
| Only a minority (<30%) of self-reported cases are confirmed by DBPCC. | Meta-analysis of DBPCCs, individual DBPCCs. | High | |
| Clinical Presentation | Extensive symptom overlap with IBS. | DBPCCs in IBS cohorts, reviews, comparative studies. | Moderate |
| Extra-intestinal symptoms (e.g., fatigue, “brain fog”, headache) are common. | Observational studies (retrospective, cross-sectional), case series. | Low | |
| Pathogenesis: Triggers, Placebo, Nocebo | The nocebo/placebo effect is a major confounder in symptom reporting. | Rigorous DBPCCs designed to assess expectancy effects, meta-analyses. | High |
| Fructans (a FODMAP in wheat) trigger more symptoms than gluten in many self-reported cases. | Rigorous DBPCC crossover trials. | High | |
| Pathogenesis: Biological Mechanisms | Innate immune system activation is implicated. | In vitro cellular assays, animal models, ex vivo biopsy studies. | Pre-clinical |
| Intestinal permeability (“leaky gut”) may be increased, but evidence is conflicting. | Observational studies measuring biomarkers (e.g., zonulin), ex vivo experiments. | Low/Pre-clinical | |
| Gut microbiota composition may be altered compared to controls. | Cross-sectional comparative 16S rRNA/metagenomic studies. | Low | |
| Diagnosis and Management | No validated biomarkers currently exist for diagnosis. | Numerous biomarker discovery studies (observational) with conflicting results. | Low |
| A gluten-free diet is the primary management for symptom control. | Observational studies, run-in phases of DBPCCs (indirect evidence). | Moderate | |
| A low-FODMAP diet is also effective for symptom control in many individuals. | DBPCCs, comparative dietary trials. | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maimaris, S.; Scarcella, C.; Memoli, G.A.; Crisciotti, C.; Schiepatti, A.; Biagi, F. Non-Coeliac Wheat Sensitivity: Symptoms in Search of a Mechanism, or a Distinct Well-Defined Clinical Entity? A Narrative Review. Int. J. Mol. Sci. 2025, 26, 11174. https://doi.org/10.3390/ijms262211174
Maimaris S, Scarcella C, Memoli GA, Crisciotti C, Schiepatti A, Biagi F. Non-Coeliac Wheat Sensitivity: Symptoms in Search of a Mechanism, or a Distinct Well-Defined Clinical Entity? A Narrative Review. International Journal of Molecular Sciences. 2025; 26(22):11174. https://doi.org/10.3390/ijms262211174
Chicago/Turabian StyleMaimaris, Stiliano, Chiara Scarcella, Giusi Aurora Memoli, Carlotta Crisciotti, Annalisa Schiepatti, and Federico Biagi. 2025. "Non-Coeliac Wheat Sensitivity: Symptoms in Search of a Mechanism, or a Distinct Well-Defined Clinical Entity? A Narrative Review" International Journal of Molecular Sciences 26, no. 22: 11174. https://doi.org/10.3390/ijms262211174
APA StyleMaimaris, S., Scarcella, C., Memoli, G. A., Crisciotti, C., Schiepatti, A., & Biagi, F. (2025). Non-Coeliac Wheat Sensitivity: Symptoms in Search of a Mechanism, or a Distinct Well-Defined Clinical Entity? A Narrative Review. International Journal of Molecular Sciences, 26(22), 11174. https://doi.org/10.3390/ijms262211174





