The Impact of Artificial Intelligence on Lung Cancer Diagnosis and Personalized Treatment
Abstract
1. Introduction
2. Lung Cancer Definition
- Non-Small Cell Lung Cancer (NSCLC): Accounting for approximately 85% of all lung cancers, NSCLC encompasses three primary subtypes:
- -
- Adenocarcinoma: The most common subtype, particularly prevalent among females and non-smokers. It originates from glandular epithelial cells and typically presents in the peripheral regions of the lung.
- -
- Squamous Cell Carcinoma: Strongly associated with smoking, this subtype arises centrally near the bronchial airways.
- -
- Large Cell Carcinoma: A poorly differentiated and aggressive subtype characterized by rapid progression and unfavorable prognosis [2].
- Small Cell Lung Cancer (SCLC): Representing 10–15% of lung cancers, SCLC is distinguished by its neuroendocrine features, rapid proliferation, early metastasis, and strong association with tobacco use. Histologically, SCLC is composed of small cells with minimal cytoplasm and high mitotic activity [3].
3. Pathophysiology
3.1. Genetic Alterations
3.2. Epigenetic Modifications
3.3. Tumor Microenvironment
3.4. Immune Evasion and Tumor Cell Plasticity
4. Artificial Intelligence
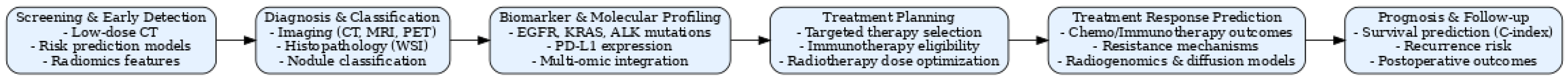
5. AI in Lung Cancer Diagnosis
| Study | Application | Model Architecture | Data Used | Performance | Key Strengths |
|---|---|---|---|---|---|
| Lee et al. [11] | Lung cancer detection on chest radiographs | Deep CNN (Lunit Insight) | Chest radiographs | AUC up to 0.99 Sensitivity 83–90% Specificity 97% | Large real-world cohort; outperformed radiologists in visible cancer detection |
| Zhu et al. [21] | Benign vs. malignant pulmonary nodule classification | Cross-ViT (CNN + Transformer fusion; optional SENet CNN branch) | LUNA16 (subset of LIDC-IDRI), CT images | Cross-ViT: ACC 91.04%, Cross-ViT (SENet): ACC 92.43% | Combines local CNN and global Transformer features via cross-fusion attention; SENet branch further boosts performance over state-of-the-art |
| Safarian et al. [28] | [18F]FDG PET/CT radiomics for lung cancer diagnosis, staging, and treatment planning | Multiple AI architectures (ML, DL, CNN, radiomics integration) | [18F]FDG PET/CT ± clinical, pathological, and molecular data | Diagnostic AUCs up to 0.94 Subtype differentiation AUC ~0.86; Staging AUC up to 0.88 Treatment response prediction ACC up to 93% | Comprehensive review of PET/CT radiomics in NSCLC; covers benign/malignant classification, subtype differentiation, molecular marker prediction, staging, prognosis, and therapy response; highlights integration of imaging with clinical and genomic data |
| Dutta et al. [29] | Lung cancer prediction from symptoms & lifestyle | ML (DT, RF, KNN, NB, AB, LR, SVM) vs. DL (Neural Networks, 1–3 hidden layers | Clinical & lifestyle data set (Kaggle) | Best NN (1 hidden layer, 800 epochs): ACC 92.86%; best ML (KNN): AUC 0.915 | Rigorous preprocessing & feature selection |
6. AI in Personalized Treatment
6.1. AI for Biomarker Prediction
6.2. AI in Predicting Treatment Response
6.3. AI for Prognostic Assessment
6.4. AI for Surgical and Radiotherapy Decision-Making
6.5. AI for Postoperative Outcomes and Healthcare Utilization
| Study | Application | Model Architecture | Data Used | Performance | Key Strengths |
|---|---|---|---|---|---|
| Lu et al. [33] | PD-L1 prediction | Deep learning radiomics (ResNet-50) + clinical fusion | CT + clinical data | AUC 0.91 (combined) | Multimodal fusion improves accuracy |
| Wang et al. [34] | PD-L1 prediction | Multi-source fusion (3D ResNet + radiomics + clinical) | CT + clinical data | AUC 0.950 (low), 0.934 (medium), 0.946 (high); C-index 0.89 | Largest cohort; robust 3-class prediction; adds survival prognostics |
| Cao et al. [40] | EGFR mutation | Radiomics + random forest + clinical features | T1-CE & T2W MRI of brain metastases | AUC 0.931 (train), 0.892 (val) for radiomics; AUC 0.943 (train), 0.936 (val) for DL; AUC 0.938 overall | Non-invasive, high accuracy for BM genotyping, external validation, strong generalization |
| Jia et al. [41] | EGFR mutation | Deep Learning Radiological-Pathological-Clinical (DLRPC) model | Preoperative CT + sex + smoking history | AUC 0.828; sensitivity 60.6%, specificity 85.1% | Widely available CT; high specificity; practical in low-resource setting |
| Yang et al. [50] | Treatment response | Multisequence MRI deep learning radiomics (ResNet34) + radiomics features + stacking fusion | CT scans + H&E-stained biopsy images + clinical data | AUC = 0.8424; Accuracy = 79.8%; Sensitivity = 81.2%; Specificity = 76.4%; PPV = 92.1%, NPV = 61.3% | Multimodal feature fusion captures macro- and microstructure; high PPV supports treatment allocation |
| Zheng et al. [46] | Treatment response | Diffusion MRI models (IVIM & DKI) with histogram analysis (whole-tumor & single-slice ROI) | Pre-treatment 3.0T MRI (IVIM and DKI sequences) | Whole-tumor combined model (Dslow_mean, f_mean, f_90th) AUC = 0.968; best single parameter f_mean AUC = 0.886 | Prospective design; volumetric analysis captures tumor heterogeneity better than single-slice; identifies f_mean as strong non-invasive imaging biomarker |
| Xie et al. [57] | Prognosis | Machine learning (XGBoost, RF, LightGBM, AdaBoost) and deep learning (MLP, TabNet, CNN) | Histopathological nuclear features + clinical data + genetic (mRNA, SNV, CNV) | Subtype: XGBoost AUC = 0.9821 (Acc = 94.0%); OS prediction: RF AUC = 0.9134 (1 yr), 0.8706 (2 yr), 0.8765 (3 yr | First to integrate nuclear morphology with clinical & genetic features; high accuracy across multiple outcomes; large, multi-institution data set |
7. Current Limitation and Future Perspectives
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| ML | Machine Learning |
| DL | Deep Learning |
| CNN | Convolutional Neural Network |
| DCNN | Deep Convolutional Neural Network |
| U-Net | Convolutional Neural Network architecture for image segmentation |
| RNN | Recurrent Neural Network |
| LSTM | Long Short-Term Memory |
| GAN | Generative Adversarial Network |
| ANN | Artificial Neural Network |
| KNN | K-Nearest Neighbors |
| SVM | Support Vector Machine |
| RFNN | Random Forest Neural Network |
| POMDP | Partially Observable Markov Decision Process |
| EDM | Entropy Degradation Method |
| AUC | Area Under the Curve |
| C-index | Concordance Index |
| NSCLC | Non-Small Cell Lung Cancer |
| SCLC | Small Cell Lung Cancer |
| PD-L1 | Programmed Death-Ligand 1 |
| EGFR | Epidermal Growth Factor Receptor |
| KRAS | Kirsten Rat Sarcoma Viral Oncogene Homolog |
| ALK | Anaplastic Lymphoma Kinase |
| BRAF | v-Raf Murine Sarcoma Viral Oncogene Homolog B1 |
| TP53 | Tumor Protein p53 |
| RB1 | Retinoblastoma 1 |
| CDKN2A | Cyclin Dependent Kinase Inhibitor 2A |
| RASSF1A | Ras Association Domain Family Member 1A |
| FHIT | Fragile Histidine Triad Protein |
| miRNA | MicroRNA |
| CT | Computed Tomography |
| PET | Positron Emission Tomography |
| MRI | Magnetic Resonance Imaging |
| [18F]FDG | Fluorodeoxyglucose (radiotracer) |
| IVIM | Intravoxel Incoherent Motion |
| DKI | Diffusion Kurtosis Imaging |
| H&E | Hematoxylin and Eosin |
| PFS | Progression-Free Survival |
| OS | Overall Survival |
| SaMD | Software as a Medical Device |
| CONSORT-AI | Consolidated Standards of Reporting Trials–Artificial Intelligence |
| SPIRIT-AI | Standard Protocol Items: Recommendations for Interventional Trials–Artificial Intelligence |
| TRIPOD | Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis |
References
- Lung Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/lung-cancer (accessed on 30 May 2025).
- Aberle, D.R.; Black, W.C.; Chiles, C.; Church, T.R.; Gareen, I.F.; Gierada, D.S.; Mahon, I.; Miller, E.A.; Pinsky, P.F.; Sicks, J.D. Lung Cancer Incidence and Mortality with Extended Follow-up in the National Lung Screening Trial. J. Thorac. Oncol. 2019, 14, 1732. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC6764895/ (accessed on 30 May 2025). [CrossRef]
- Thandra, K.C.; Barsouk, A.; Saginala, K.; Aluru, J.S.; Barsouk, A. Epidemiology of lung cancer. Contemp. Oncol. 2021, 25, 45–52. [Google Scholar]
- Nana-Sinkam, S.P.; Powell, C.A. Molecular Biology of Lung Cancer. Chest 2013, 143, e30S–e39S. [Google Scholar] [CrossRef] [PubMed]
- Pao, W.; Girard, N. New driver mutations in non-small-cell lung cancer. Lancet Oncol. 2011, 12, 175–180. Available online: https://www.thelancet.com/journals/lancet/article/PIIS1470-2045(10)70087-5/abstract (accessed on 30 May 2025). [CrossRef]
- Sholl, L.M.; Aisner, D.L.; Varella-Garcia, M.; Berry, L.D.; Dias-Santagata, D.; Wistuba, I.I.; Chen, H.; Fujimoto, J.; Kugler, K.; Franklin, W.A.; et al. Multi-institutional oncogenic driver mutation analysis in lung adenocarcinoma. J. Thorac. Oncol. 2015, 10, 768–777. [Google Scholar] [CrossRef]
- Shaul, M.E.; Fridlender, Z.G. Tumour-associated neutrophils in patients with cancer. Nat. Rev. Clin. Oncol. 2019, 16, 601–620. Available online: https://pubmed.ncbi.nlm.nih.gov/31160735/ (accessed on 30 May 2025). [CrossRef]
- Pesapane, F.; Codari, M.; Sardanelli, F. Artificial intelligence and machine learning for medical imaging: A technology review. Phys. Med. 2021, 83, 242–256. Available online: https://www.sciencedirect.com/science/article/pii/S1120179721001733 (accessed on 30 May 2025).
- Setio, A.A.A.; Traverso, A.; de Bel, T.; Berens, M.S.N.; van den Bogaard, C.; Cerello, P.; Chen, H.; Dou, Q.; Fantacci, M.E.; Geurts, B.; et al. Validation, comparison, and combination of algorithms for automatic detection of pulmonary nodules in computed tomography images: The LUNA16 challenge. Med. Image Anal. 2017, 42, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Armato, S.G., 3rd; McLennan, G.; Bidaut, L.; McNitt-Gray, M.F.; Meyer, C.R.; Reeves, A.P.; Zhao, B.; Aberle, D.R.; Henschke, C.I.; Hoffman, E.A.; et al. The Lung Image Database Consortium (LIDC) and Image Database Resource Initiative (IDRI): A completed reference database of lung nodules on CT scans. Med. Phys. 2011, 38, 915–931. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, J.H.; Sun, H.Y.; Park, S.; Kim, H.; Hwang, E.J.; Goo, J.M.; Park, C.M. Performance of a Deep Learning Algorithm Compared with Radiologic Interpretation for Lung Cancer Detection on Chest Radiographs in a Health Screening Population. Radiology 2020, 297, 687–696. [Google Scholar] [CrossRef]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G.; et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019, 25, 954–961, Erratum in Nat. Med. 2019, 25, 1319. [Google Scholar] [CrossRef] [PubMed]
- Pacurari, A.C.; Bhattarai, S.; Muhammad, A.; Avram, C.; Mederle, A.O.; Rosca, O.; Bratosin, F.; Bogdan, I.; Fericean, R.M.; Biris, M.; et al. Diagnostic accuracy of machine learning AI architectures in lung cancer: A systematic review. Diagnostics 2023, 13, 2145. [Google Scholar] [CrossRef] [PubMed]
- Abadia, A.F.; Yacoub, B.; Stringer, N.; Snoddy, M.; Kocher, M.; Schoepf, U.J.; Aquino, G.J.; Kabakus, I.; Dargis, D.; Hoelzer, P.; et al. Diagnostic accuracy and performance of artificial intelligence in detecting lung nodules in patients with complex lung disease: A noninferiority study. J. Thorac. Imaging 2022, 37, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, P.; Xu, H.; Nasir, M.; Shen, L. Deep learning for lung cancer detection: A review. Artif. Intell. Rev. 2024, 57, 3345–3390. Available online: https://link.springer.com/article/10.1007/s10462-024-10807-1 (accessed on 30 May 2025). [CrossRef]
- Shedrawi, G.; Magron, F.; Vigga, B.; Bosserelle, P.; Gislard, S.; Halford, A.R.; Tiitii, S.; Fepuleai, F.; Molai, C.; Rota, M.; et al. Leveraging deep learning and computer vision technologies to enhance management of coastal fisheries in the Pacific region. Sci. Rep. 2024, 14, 20915. Available online: https://pubmed.ncbi.nlm.nih.gov/39245678/ (accessed on 30 May 2025). [CrossRef]
- Azad, R.; Kazerouni, A.; Heidari, M.; Aghdam, E.K.; Molaei, A.; Jia, Y.; Jose, A.; Roy, R.; Merhof, D. Advances in medical image analysis with vision transformers: A comprehensive review. Med. Image Anal. 2024, 91, 103000. [Google Scholar] [CrossRef]
- Gai, L.; Xing, M.; Chen, W.; Zhang, Y.; Qiao, X. Comparing CNN-based and transformer-based models for identifying lung cancer: Which is more effective? Biomed. Signal Process Control. 2024, 91, 105030. [Google Scholar] [CrossRef]
- Durgam, R.; Panduri, B.; Balaji, V.; Khadidos, A.O.; Khadidos, A.l.O.; Selvarajan, S. Enhancing lung cancer detection through integrated deep learning and transformer models. Sci. Rep. 2025, 15, 15614. [Google Scholar] [CrossRef]
- Gould, M.K.; Huang, B.Z.; Tammemagi, M.C.; Kinar, Y.; Shiff, R. Machine learning for early lung cancer identification using routine clinical and laboratory data. Am. J. Respir. Crit. Care Med. 2021, 204, 445–453. [Google Scholar] [CrossRef]
- Zhu, Q.; Fei, L. Cross-ViT based benign and malignant classification of pulmonary nodules. PLoS ONE 2025, 20, e0318670. [Google Scholar] [CrossRef]
- Lin, C.Y.; Guo, S.M.; Lien, J.J.; Lin, W.T.; Liu, Y.S.; Lai, C.H.; Hsu, I.L.; Chang, C.C.; Tseng, Y.L. Combined model integrating deep learning, radiomics, and clinical data to classify lung nodules at chest CT. Radiol. Med. 2024, 129, 56–69. [Google Scholar] [CrossRef]
- Meeradevi, T.; Sasikala, S.; Murali, L.; Manikandan, N.; Ramaswamy, K. Lung cancer detection with machine learning classifiers with multi-attribute decision-making system and deep learning model. Sci. Rep. 2025, 15, 8565. [Google Scholar] [CrossRef]
- Hiraman, A.; Viriri, S.; Gwetu, M. Lung tumor segmentation: A review of the state of the art. Front. Comput. Sci. 2024, 6, 1423693. Available online: https://www.frontiersin.org/articles/10.3389/fcomp.2024.1423693/full (accessed on 30 May 2025). [CrossRef]
- Astley, J.R.; Biancardi, A.M.; Hughes, P.J.C.; Marshall, H.; Smith, L.J.; Collier, G.J.; Eaden, J.A.; Weatherley, N.D.; Hatton, M.Q.; Wild, J.M.; et al. Large-scale investigation of deep learning approaches for ventilated lung segmentation using multi-nuclear hyperpolarized gas MRI. Sci. Rep. 2022, 12, 10566. [Google Scholar] [CrossRef]
- Gao, C.; Wu, L.; Wu, W.; Huang, Y.; Wang, X.; Sun, Z.; Xu, M.; Gao, C. Deep learning in pulmonary nodule detection and segmentation: A systematic review. Eur. Radiol. 2025, 35, 255–266. [Google Scholar] [CrossRef]
- Chavan, M.; Varadarajan, V.; Gite, S.; Kotecha, K. Deep neural network for lung image segmentation on chest X-ray. Technologies 2022, 10, 105. [Google Scholar] [CrossRef]
- Safarian, A.; Mirshahvalad, S.A.; Nasrollahi, H.; Jung, T.; Pirich, C.; Arabi, H.; Beheshti, M. Impact of [18F]FDG PET/CT Radiomics and Artificial Intelligence in Clinical Decision Making in Lung Cancer: Its Current Role. Semin. Nucl. Med. 2025, 55, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Dutta, B. Comparative analysis of machine learning and deep learning models for lung cancer prediction based on symptomatic and lifestyle features. Appl. Sci. 2025, 15, 4507. [Google Scholar] [CrossRef]
- Schuler, M.; Bölükbas, S.; Darwiche, K.; Theegarten, D.; Herrmann, K.; Stuschke, M. Personalized treatment for patients with lung cancer. Dtsch. Arztebl. Int. 2023, 120, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Memmott, R.M.; Wolfe, A.R.; Carbone, D.P.; Williams, T.M. Predictors of response, progression-free survival, and overall survival in patients with lung cancer treated with immune checkpoint inhibitors. J. Thorac. Oncol. 2021, 16, 1086–1098. [Google Scholar] [CrossRef]
- Dia, A.K.; Kolnohuz, A.; Yolchuyeva, S.; Tonneau, M.; Lamaze, F.; Orain, M.; Gagné, A.; Blais, F.; Coulombe, F.; Malo, J.; et al. Computational analysis of whole slide images predicts PD-L1 expression and progression-free survival in immunotherapy-treated non-small cell lung cancer patients. J. Transl. Med. 2025, 23, 510. [Google Scholar] [CrossRef]
- Lu, J.; Liu, X.; Ji, X.; Jiang, Y.; Zuo, A.; Guo, Z.; Yang, S.; Peng, H.; Sun, F.; Lu, D. Predicting PD-L1 status in NSCLC patients using deep learning radiomics based on CT images. Sci. Rep. 2025, 15, 12495. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ma, J.; Shao, J.; Zhang, S.; Li, J.; Yan, J.; Zhao, Z.; Bai, C.; Yu, Y.; Li, W. Non-invasive measurement using deep learning algorithm based on multi-source features fusion to predict PD-L1 expression and survival in NSCLC. Front. Immunol. 2022, 13, 828560. [Google Scholar] [CrossRef] [PubMed]
- Mu, W.; Jiang, L.; Shi, Y.; Tunali, I.; Gray, J.E.; Katsoulakis, E.; Tian, J.; Gillies, R.J.; Schabath, M.B. Non-invasive measurement of PD-L1 status and prediction of immunotherapy response using deep learning of PET/CT images. J. Immunother. Cancer 2021, 9, e002118. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Liu, X.; Chen, Y.; Wang, S.; Jiang, C.; Gong, J. CT-based deep learning radiomics biomarker for programmed cell death ligand 1 expression in non-small cell lung cancer. BMC Med. Imaging 2024, 24, 196. [Google Scholar] [CrossRef]
- Lim, C.H.; Koh, Y.W.; Hyun, S.H.; Lee, S.J. A machine learning approach using PET/CT-based radiomics for prediction of PD-L1 expression in non-small cell lung cancer. Anticancer. Res. 2022, 42, 5875–5884. [Google Scholar] [CrossRef]
- Liang, C.; Zheng, M.; Zou, H.; Han, Y.; Zhan, Y.; Xing, Y.; Liu, C.; Zuo, C.; Zou, J. Deep learning-based image analysis predicts PD-L1 status from 18F-FDG PET/CT images in non-small-cell lung cancer. Front. Oncol. 2024, 14, 1402994. [Google Scholar] [CrossRef]
- Hashimoto, K.; Murakami, Y.; Omura, K.; Takahashi, H.; Suzuki, R.; Yoshioka, Y.; Oguchi, M.; Ichinose, J.; Matsuura, Y.; Nakao, M.; et al. Prediction of tumor PD-L1 expression in resectable non-small cell lung cancer by machine learning models based on clinical and radiological features: Performance comparison with preoperative biopsy. Clin. Lung Cancer 2024, 25, e26–e34.e6. [Google Scholar] [CrossRef]
- Cao, P.; Jia, X.; Wang, X.; Fan, L.; Chen, Z.; Zhao, Y.; Zhu, J.; Wen, Q. Deep learning radiomics for the prediction of epidermal growth factor receptor mutation status based on MRI in brain metastasis from lung adenocarcinoma patients. BMC Cancer 2025, 25, 443. [Google Scholar] [CrossRef]
- Jia, T.Y.; Xiong, J.F.; Li, X.Y.; Yu, W.; Xu, Z.Y.; Cai, X.W.; Ma, J.C.; Ren, Y.C.; Larsson, R.; Zhang, J.; et al. Identifying EGFR mutations in lung adenocarcinoma by noninvasive imaging using radiomics features and random forest modeling. Eur. Radiol. 2019, 29, 4742–4750. [Google Scholar] [CrossRef]
- Hajikarimloo, B.; Mohammadzadeh, I.; Tos, S.M.; Habibi, M.A.; Hashemi, R.; Hezaveh, E.B.; Najari, D.; Hasanzade, A.; Hooshmand, M.; Bana, S. Machine learning in prediction of epidermal growth factor receptor status in non-small cell lung cancer brain metastases: A systematic review and meta-analysis. BMC Cancer 2025, 25, 818. [Google Scholar] [CrossRef]
- Felfli, M.; Liu, Y.; Zerka, F.; Voyton, C.; Thinnes, A.; Jacques, S.; Iannessi, A.; Bodard, S. Systematic review, meta-analysis and radiomics quality score assessment of CT radiomics-based models predicting tumor EGFR mutation status in patients with non-small-cell lung cancer. Int. J. Mol. Sci. 2023, 24, 11433. [Google Scholar] [CrossRef]
- Zuo, Y.; Liu, Q.; Li, N.; Li, P.; Fang, Y.; Bian, L.; Zhang, J.; Song, S. Explainable 18F-FDG PET/CT radiomics model for predicting EGFR mutation status in lung adenocarcinoma: A two-center study. J. Cancer Res. Clin. Oncol. 2024, 150, 469. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.; Liu, Q.; Li, N.; Li, P.; Zhang, J.; Song, S. Optimal 18F-FDG PET/CT radiomics model development for predicting EGFR mutation status and prognosis in lung adenocarcinoma: A multicentric study. Front. Oncol. 2023, 13, 1173355. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhou, L.; Huang, W.; Han, N.; Zhang, J. Histogram analysis of multiple diffusion models for predicting advanced non-small cell lung cancer response to chemoimmunotherapy. Cancer Imaging 2024, 24, 71. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Li, Y.; Zhao, M.; Wang, P.; Xin, J. Combination of 18F-fluorodeoxyglucose PET/CT radiomics and clinical features for predicting epidermal growth factor receptor mutations in lung adenocarcinoma. Korean J. Radiol. 2022, 23, 921–930. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.H.; Le, M.H.N.; Bui, A.T.; Le, N.Q.K. Artificial intelligence in predicting EGFR mutations from whole slide images in lung cancer: A systematic review and meta-analysis. Lung Cancer 2025, 204, 108577. [Google Scholar] [CrossRef]
- Lim, Z.F.; Ma, P.C. Emerging insights of tumor heterogeneity and drug resistance mechanisms in lung cancer targeted therapy. J. Hematol. Oncol. 2019, 12, 134. [Google Scholar] [CrossRef]
- Yang, T.; Wang, X.; Jin, Y.; Yao, X.; Sun, Z.; Chen, P.; Zhou, S.; Zhu, W.; Chen, W. Deep learning radiopathomics predicts targeted therapy sensitivity in EGFR-mutant lung adenocarcinoma. J. Transl. Med. 2025, 23, 482. [Google Scholar] [CrossRef]
- Zheng, L.; Nie, W.; Wang, S.; Yang, L.; Hu, F.; Ma, M.; Cheng, L.; Lu, J.; Zhang, B.; Xu, J.; et al. Metabolomic machine learning-based model predicts efficacy of chemoimmunotherapy for advanced lung squamous cell carcinoma. Front. Immunol. 2025, 16, 1545976. [Google Scholar] [CrossRef]
- Rakaee, M.; Tafavvoghi, M.; Ricciuti, B.; Alessi, J.V.; Cortellini, A.; Citarella, F.; Nibid, L.; Perrone, G.; Adib, E.; Fulgenzi, C.A.M.; et al. Deep learning model for predicting immunotherapy response in advanced non-small cell lung cancer. JAMA Oncol. 2025, 11, 109–118. [Google Scholar] [CrossRef]
- Li, J.; Chen, A.; Liu, Z.; Wei, S.; Zhang, J.; Chen, J.; Shi, C. Machine learning driven prediction of drug efficacy in lung cancer: Based on protein biomarkers and clinical features. Life Sci. 2025, 375, 123706. [Google Scholar] [CrossRef] [PubMed]
- Cai, F.; Guo, Z.; Wang, G.; Luo, F.; Yang, Y.; Lv, M.; He, J.; Xiu, Z.; Tang, D.; Bao, X.; et al. Integration of intratumoral and peritumoral CT radiomic features with machine learning algorithms for predicting induction therapy response in locally advanced non-small cell lung cancer. BMC Cancer 2025, 25, 461. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Ji, Z.; Zhang, L.; Li, L.; Xu, W.; Su, Q. Prediction of pathological complete response to neoadjuvant chemoimmunotherapy in non–small cell lung cancer using 18F-FDG PET radiomics features of primary tumour and lymph nodes. BMC Cancer 2025, 25, 520. [Google Scholar] [CrossRef] [PubMed]
- Sheng, Z.; Ji, S.; Chen, Y.; Mi, Z.; Yu, H.; Zhang, L.; Wan, S.; Song, N.; Shen, Z.; Zhang, P. Machine learning algorithms integrating positron emission tomography/computed tomography features to predict pathological complete response after neoadjuvant chemoimmunotherapy in lung cancer. Eur. J. Cardiothorac. Surg. 2025, 67, ezaf132. [Google Scholar] [CrossRef]
- Xie, B.; Mo, M.; Cui, H.; Dong, Y.; Yin, H.; Lu, Z. Integration of nuclear, clinical, and genetic features for lung cancer subtype classification and survival prediction using ML and deep learning. Diagnostics 2025, 15, 872. [Google Scholar] [CrossRef]
- Hu, X.; Zhao, S.; Li, Y.; Heibi, Y.; Wu, H.; Jiang, Y. Development and validation of a machine learning-based nomogram for predicting prognosis in lung cancer patients with malignant pleural effusion. Sci. Rep. 2025, 15, 9714. [Google Scholar] [CrossRef]
- Nemoto, T.; Takeda, A.; Matsuo, Y.; Kishi, N.; Eriguchi, T.; Kunieda, E.; Kimura, R.; Sanuki, N.; Tsurugai, Y.; Yagi, M.; et al. Applying artificial neural networks to develop a decision support tool for Tis–4N0M0 non–small-cell lung cancer treated with stereotactic body radiotherapy. JCO Clin. Cancer Inform. 2022, 6, e2100176. [Google Scholar] [CrossRef]
- Lou, B.; Doken, S.; Zhuang, T.; Wingerter, D.; Gidwani, M.; Mistry, N.; Ladic, L.; Kamen, A.; Abazeed, M.E. An image-based deep learning framework for individualizing radiotherapy dose. Lancet Digit. Health 2019, 1, e136–e147. [Google Scholar] [CrossRef]
- Hashimoto, Y.; Inoue, N.; Tani, T.; Imai, S. Machine learning for predicting postoperative functional disability and mortality among older patients with cancer: Retrospective cohort study. JMIR Aging 2025, 8, e65898. [Google Scholar] [CrossRef]
- Alsinglawi, B.; Alshari, O.; Alorjani, M.; Mubin, O.; Alnajjar, F.; Novoa, M.; Darwish, O. An explainable machine learning framework for lung cancer hospital length of stay prediction. Sci. Rep. 2022, 12, 607. [Google Scholar] [CrossRef]
- Zhao, X.; Zhao, Y.; Zhang, J.; Zhang, Z.; Liu, L.; Zhao, X. Predicting PD-L1 expression status in patients with non-small cell lung cancer using [18F]FDG PET/CT radiomics. EJNMMI Res. 2023, 13, 4. [Google Scholar] [CrossRef]
- Stüber, A.T.; Heimer, M.M.; Ta, J.; Fabritius, M.P.; Hoppe, B.F.; Sheikh, G.; Brendel, M.; Unterrainer, L.; Jurmeister, P.; Tufman, A.; et al. Replication study of PD-L1 status prediction in NSCLC using PET/CT radiomics. Eur. J. Radiol. 2025, 183, 111825. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Li, Z.; Jiang, T.; Yang, C.; Li, N. Artificial intelligence in lung cancer: Current applications, future perspectives, and challenges. Front. Oncol. 2024, 14, 1486310. [Google Scholar] [CrossRef] [PubMed]
- Ziegelmayer, S.; Graf, M.; Makowski, M.; Gawlitza, J.; Gassert, F. Cost-Effectiveness of AI Support in CT-Based Lung Cancer Screening. Cancers 2022, 14, 1729. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.; Pauling, J.; Keck, A.; Baumbach, J. The economic impact of artificial intelligence in health care: Systematic review. J. Med. Internet Res. 2020, 22, e16866. [Google Scholar] [CrossRef]
- Smiley, A.; Villarreal-Zegarra, D.; Reategui-Rivera, C.M.; Escobar-Agreda, S.; Finkelstein, J. Methodological and reporting quality of machine learning studies on cancer diagnosis, treatment, and prognosis. Front. Oncol. 2025, 15, 1555247. [Google Scholar] [CrossRef]
- Adler-Milstein, J.; Aggarwal, N.; Ahmed, M.; Castner, J.; Evans, B.J.; Gonzalez, A.A.; James, C.A.; Lin, S.; Mandl, K.D.; Matheny, M.E.; et al. Meeting the moment: Addressing barriers and facilitating clinical adoption of artificial intelligence in medical diagnosis. NAM Perspect. 2022, 2022. [Google Scholar] [CrossRef]
- Wubineh, B.Z.; Deriba, F.G.; Woldeyohannis, M.M. Exploring the opportunities and challenges of implementing artificial intelligence in healthcare: A systematic literature review. Urol. Oncol. 2024, 42, 48–56. [Google Scholar] [CrossRef]
- Bashkin, O. Patient perspectives on artificial intelligence in healthcare: A global scoping review of benefits, ethical concerns, and implementation strategies. Int. J. Med. Inform. 2025, 203, 106007. [Google Scholar] [CrossRef]
- Liu, X.; Cruz Rivera, S.; Moher, D.; Calvert, M.J.; Denniston, A.K.; SPIRIT-AI and CONSORT-AI Working Group. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: The CONSORT-AI extension. Lancet Digit. Health 2020, 2, e537–e548. [Google Scholar] [CrossRef]
- Cruz Rivera, S.; Liu, X.; Chan, A.W.; Denniston, A.K.; Calvert, M.J.; SPIRIT-AI and CONSORT-AI Working Group; SPIRIT-AI and CONSORT-AI Steering Group; SPIRIT-AI and CONSORT-AI Consensus Group. Guidelines for clinical trial protocols for interventions involving artificial intelligence: The SPIRIT-AI extension. Nat. Med. 2020, 26, 1351–1363. [Google Scholar] [CrossRef]
- Shahzad, R.; Ayub, B.; Siddiqui, M.A.R. Quality of reporting of randomised controlled trials of artificial intelligence in healthcare: A systematic review. BMJ Open 2023, 13, e061519. [Google Scholar] [CrossRef]
- Smiley, A.; Reategui-Rivera, C.M.; Villarreal-Zegarra, D.; Escobar-Agreda, S.; Finkelstein, J. Exploring AI biases in predictive models for cancer diagnosis. Cancers 2025, 17, 407. [Google Scholar] [CrossRef] [PubMed]
- Palaniappan, K.; Lin, E.Y.T.; Vogel, S. Global regulatory frameworks for the use of artificial intelligence (AI) in the healthcare services sector. Healthcare 2024, 12, 562. [Google Scholar] [CrossRef] [PubMed]
- Palaniappan, K.; Lin, E.Y.T.; Vogel, S.; Lim, J.C.W. Gaps in Global Regulatory Frameworks for AI in Healthcare and Key Recommendations. Healthcare 2024, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Copley, S.J.; Viola, P.; Lu, H.; Aboagye, E.O. Radiomics and artificial intelligence for precision medicine in lung cancer treatment. Semin. Cancer Biol. 2023, 93, 97–113. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.W.L.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized quantitative radiomics for high-throughput image-based phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G.M. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. BMJ 2015, 350, g7594. [Google Scholar] [CrossRef]
| AI Model | Common Architectures |
|---|---|
| Machine Learning | Logistic regression Entropy degradation method (EDM) K-Nearest Neighbors (KNN) Gradient Boosting (XGBoost, LightGBM) Support vector machine (SVM) Partially observable Markov decision Process (POMDP) Random forest neural network (RFNN) |
| Deep Learning | Artificial Neural Networks (ANN) Convolutional neural networks (CNNs) U-Net 3D CNN Recurrent Neural Network (RNN) Transformer Long Short-Term Memory (LSTM) Generative adversarial networks (GANs) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayasa, Y.; Alajrami, D.; Idkedek, M.; Tahayneh, K.; Akar, F.A. The Impact of Artificial Intelligence on Lung Cancer Diagnosis and Personalized Treatment. Int. J. Mol. Sci. 2025, 26, 8472. https://doi.org/10.3390/ijms26178472
Ayasa Y, Alajrami D, Idkedek M, Tahayneh K, Akar FA. The Impact of Artificial Intelligence on Lung Cancer Diagnosis and Personalized Treatment. International Journal of Molecular Sciences. 2025; 26(17):8472. https://doi.org/10.3390/ijms26178472
Chicago/Turabian StyleAyasa, Yaman, Diyar Alajrami, Mayar Idkedek, Kareem Tahayneh, and Firas Abu Akar. 2025. "The Impact of Artificial Intelligence on Lung Cancer Diagnosis and Personalized Treatment" International Journal of Molecular Sciences 26, no. 17: 8472. https://doi.org/10.3390/ijms26178472
APA StyleAyasa, Y., Alajrami, D., Idkedek, M., Tahayneh, K., & Akar, F. A. (2025). The Impact of Artificial Intelligence on Lung Cancer Diagnosis and Personalized Treatment. International Journal of Molecular Sciences, 26(17), 8472. https://doi.org/10.3390/ijms26178472









