Mitochondrial Biomarkers in the Omics Era: A Clinical-Pathophysiological Perspective
Abstract
1. Introduction
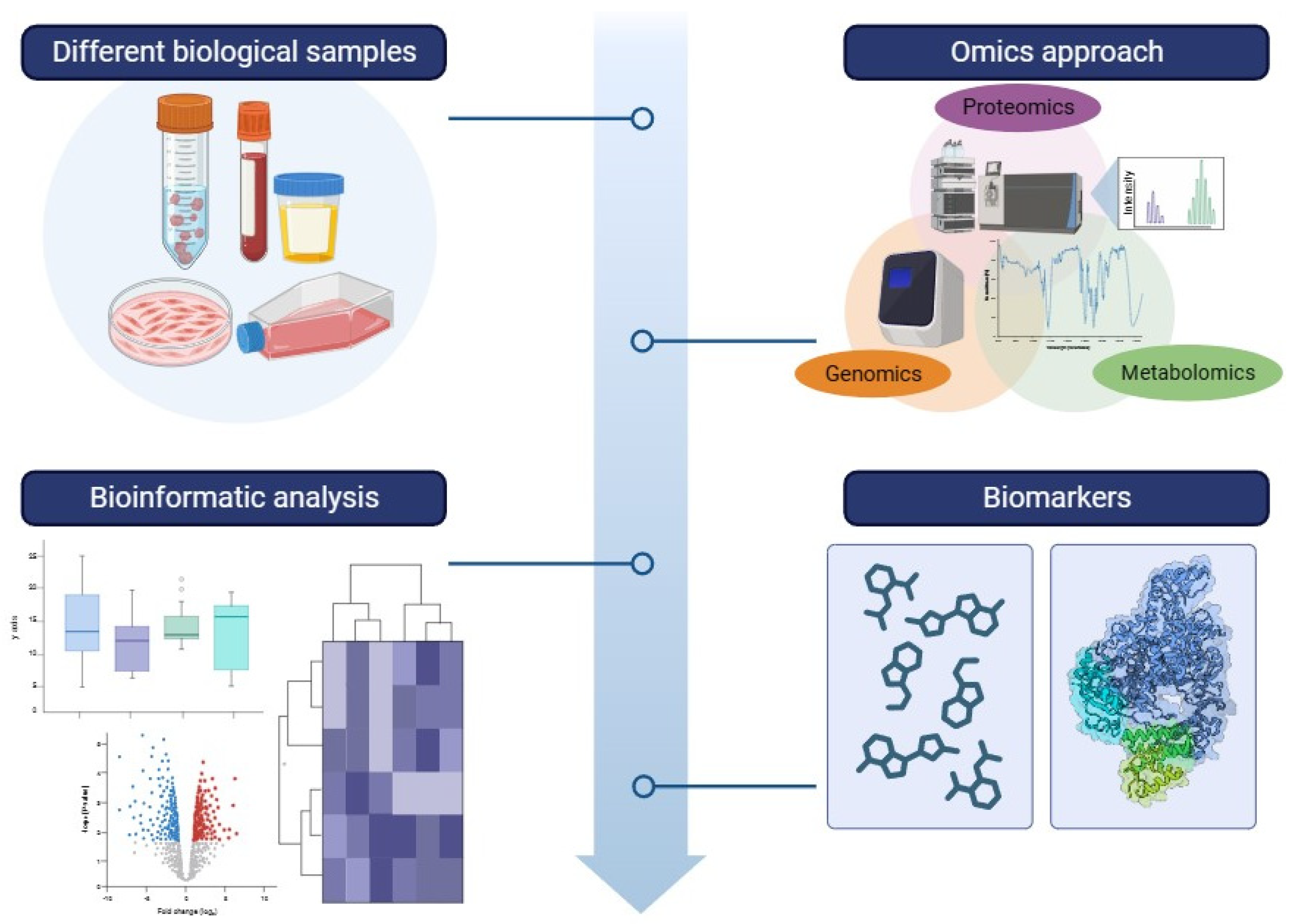
2. Metabolomics and Proteomics in Mitochondrial Disease Biomarkers
2.1. Contribution to Identifying Clinical Biomarkers
2.2. Contribution in Unraveling Pathophysiological Mechanisms of Disease
3. Discussion
4. Materials and Methods
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Spinelli, J.B.; Haigis, M.C. The multifaceted contributions of mitochondria to cellular metabolism. Nat. Cell Biol. 2018, 20, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Chinnery, P.F. Mitochondrial disease in adults: What’s old and what’s new? EMBO Mol. Med. 2015, 12, 1503–1512. [Google Scholar] [CrossRef]
- Chakrabarty, R.P.; Navdeep, S.C. Beyond ATP, new roles of mitochondria. Biochemist 2022, 44, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Luft, R.; Ikkos, D.; Palmieri, G.; Ernster, L.; Afzelius, B. A case of severe hypermetabolism of nonthy-roid origin with a defect in the maintenance of mitochondrial respiratory control: A correlated clinical, biochemical, and morphological study. J. Clin. Investig. 1962, 41, 1776–1804. [Google Scholar] [CrossRef] [PubMed]
- Luft, R. The development of mitochondrial medicine. Proc. Natl. Acad. Sci. USA 1994, 13, 8731–8738. [Google Scholar] [CrossRef] [PubMed]
- Collier, J.J.; Oláhová, M.; McWilliams, T.G.; Taylor, R.W. Mitochondrial signalling and homeostasis: From cell biology to neurological disease. Trends Neurosci. 2023, 46, 137–152. [Google Scholar] [CrossRef] [PubMed]
- Di Mauro, S.; Schon, E.A.; Carelli, V.; Hirano, M. The clinical maze of mitochondrial neurology. Nat. Rev. Neurol. 2013, 9, 429–444. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.S.; Bindoff, L.A.; Gorman, G.S.; Klopstock, T.; Kornblum, C.; Mancuso, M.; McFarland, R.; Sue, C.M.; Suomalainen, A.; Taylor, R.W.; et al. Mitochondrial disease in adults: Recent advances and future promise. Lancet Neurol. 2021, 20, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Di Mauro, S. Mitochondrial encephalomyopathies fifty years on: The Robert Wartenberg Lecture. Neurology 2013, 81, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Battersby, B.J. Mitochondrial diseases: The contribution of organelle stress responses to pathology. Nat. Rev. Mol. Cell Biol. 2018, 19, 77–92. [Google Scholar] [CrossRef]
- Gorman, G.S.; Schaefer, A.M.; Ng, Y.; Gomez, N.; Blakely, E.L.; Alston, C.L.; Feeney, C.; Horvath, R.; Yu-Wai-Man, P.; Chinnery, P.F.; et al. Prevalence of nuclear and mitochondrial DNA mutations related to adult mitochondrial disease. Ann. Neurol. 2015, 77, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Skladal, D.; Halliday, J.; Thorburn, D.R. Minimum birth prevalence of mitochondrial respiratory chain disorders in children. Brain 2003, 126, 1905–1912. [Google Scholar] [CrossRef]
- Rahman, S. Mitochondrial disease in children. J. Intern. Med. 2020, 287, 609–633. [Google Scholar] [CrossRef]
- Grier, J.; Hirano, M.; Karaa, A.; Shepard, E.; Thompson, J.L.P. Diagnostic odyssey of patients with mitochondrial disease: Results of a survey. Neurol. Genet. 2018, 26, e230. [Google Scholar] [CrossRef] [PubMed]
- Stenton, S.L.; Prokisch, H. Genetics of mitochondrial diseases: Identifying mutations to help diagnosis. EBioMedicine 2020, 56, 102784. [Google Scholar] [CrossRef] [PubMed]
- Schon, K.R.; Ratnaike, T.; van den Ameele, J.; Horvath, R.; Chinnery, P.F. Mitochondrial Diseases: A Diagnostic Revolution. Trends Genet. 2020, 36, 702–717. [Google Scholar] [CrossRef]
- Alston, C.L.; Stenton, S.L.; Hudson, G.; Prokisch, H.; Taylor, R.W. The genetics of mitochondrial disease: Dissecting mitochondrial pathology using multi-omic pipelines. J. Pathol. 2021, 254, 430–442. [Google Scholar] [CrossRef]
- Hubens, W.H.G.; Vallbona-Garcia, A.; de Coo, I.F.M.; van Tienen, F.H.J.; Webers, C.A.B.; Smeets, H.J.M.; Gorgels, T.G.M.F. Blood biomarkers for assessment of mitochondrial dysfunction: An expert review. Mitochondrion 2022, 62, 187–204. [Google Scholar] [CrossRef] [PubMed]
- Pickett, S.J.; Grady, J.P.; Ng, Y.S.; Gorman, G.S.; Schaefer, A.M.; Wilson, I.J.; Cordell, H.J.; Turnbull, D.M.; Taylor, R.W.; McFarland, R. Phenotypic heterogeneity in m.3243A>G mitochondrial disease: The role of nuclear factors. Ann. Clin. Transl. Neurol. 2018, 5, 333–345. [Google Scholar] [CrossRef]
- Nesbitt, V.; Pitceathly, R.D.; Turnbull, D.M.; Taylor, R.W.; Sweeney, M.G.; Mudanohwo, E.E.; Rahman, S.; Hanna, M.G.; McFarland, R. The UK MRC Mitochondrial Disease Patient Cohort Study: Clinical phenotypes associated with the m.3243A>G mutation--implications for diagnosis and management. J. Neurol. Neurosurg. Psychiatry 2013, 84, 936–938. [Google Scholar] [CrossRef]
- Russell, O.M.; Gorman, G.S.; Lightowlers, R.N.; Turnbull, D.M. Mitochondrial Diseases: Hope for the Future. Cell 2020, 181, 168–188. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Wang, X.; Li, M.; Ji, D.; Liang, D.; Liang, C.; Liu, Y.; Zhang, Z.; Cao, Y.; Zou, W.W. Mitochondrial Unfolded Protein Response and Integrated Stress Response as Promising Therapeutic Targets for Mitochondrial Diseases. Cells 2023, 12, 20. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ince-Dunn, G.; Suomalainen, A.; Elo, L.L. Integrative omics approaches provide biological and clinical insights: Examples from mitochondrial diseases. J. Clin. Investig. 2020, 130, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Reinstadler, B.; Engelstad, K.; Skinner, O.S.; Stackowitz, E.; Haller, R.G.; Clish, C.B.; Pierce, K.; Walker, M.A.; Fryer, R.; et al. Circulating markers of NADH-reductive stress correlate with mitochondrial disease severity. J. Clin. Investig. 2021, 131, e136055. [Google Scholar] [CrossRef] [PubMed]
- Tragni, V.; Primiano, G.; Tummolo, A.; Cafferati Beltrame, L.; La Piana, G.; Sgobba, M.N.; Cavalluzzi, M.M.; Paterno, G.; Gorgoglione, R.; Volpicella, M.; et al. Personalized Medicine in Mitochondrial Health and Disease: Molecular Basis of Therapeutic Approaches Based on Nutritional Supplements and Their Analogs. Molecules 2022, 27, 3494. [Google Scholar] [CrossRef] [PubMed]
- Lindon, J.C.; Nicholson, J.K. Analytical technologies for metabonomics and metabolomics, and multi-omic information recovery. TrAC Trends Anal. Chem. 2008, 27, 194–204. [Google Scholar] [CrossRef]
- Gucek, M.; Sack, M.N. Proteomic and metabolomic advances uncover biomarkers of mitochondrial disease pathophysology and severity. J. Clin. Investig. 2021, 131, e145158. [Google Scholar] [CrossRef] [PubMed]
- Rahman, J.; Rahman, S. Mitochondrial medicine in the omics era. Lancet 2018, 391, 2560–2574. [Google Scholar] [CrossRef] [PubMed]
- Roberts, L.D.; Souza, A.L.; Gerszten, R.E.; Clish, C.B. Targeted metabolomics. Curr. Protoc. Mol. Biol. 2012, 98, 30.2.1–30.2.24. [Google Scholar] [CrossRef]
- Schrimpe-Rutledge, A.C.; Codreanu, S.G.; Sherrod, S.D.; McLean, J.A. Untargeted Metabolomics Strategies-Challenges and Emerging Directions. J. Am. Soc. Mass. Spectrom. 2016, 27, 1897–1905. [Google Scholar] [CrossRef]
- Esterhuizen, K.; Lindeque, J.Z.; Mason, S.; van der Westhuizen, F.H.; Rodenburg, R.J.; de Laat, P.; Smeitink, J.A.M.; Janssen, M.C.H.; Louw, R. One mutation, three phenotypes: Novel metabolic insights on MELAS, MIDD and myopathy caused by the m.3243A > G mutation. Metabolomics 2021, 17, 10. [Google Scholar] [CrossRef]
- Gervasoni, J.; Primiano, A.; Marini, F.; Sabino, A.; Biancolillo, A.; Calvani, R.; Picca, A.; Marzetti, E.; Persichilli, S.; Urbani, A.; et al. Fourier-Transform Infrared Spectroscopy of Skeletal Muscle Tissue: Expanding Biomarkers in Primary Mitochondrial Myopathies. Genes 2020, 11, 1522. [Google Scholar] [CrossRef] [PubMed]
- Alix, J.J.P.; Plesia, M.; Lloyd, G.R.; Dudgeon, A.P.; Kendall, C.A.; Hewamadduma, C.; Hadjivassiliou, M.; McDermott, C.J.; Gorman, G.S.; Taylor, R.W.; et al. Rapid identification of human muscle disease with fibre optic Raman spectroscopy. Analyst 2022, 147, 2533–2540. [Google Scholar] [CrossRef]
- Bocca, C.; Le Paih, V.; Chao de la Barca, J.M.; Kouassy Nzoughet, J.; Amati-Bonneau, P.; Blanchet, O.; Védie, B.; Géromin, D.; Simard, G.; Procaccio, V.; et al. A plasma metabolomic signature of Leber hereditary optic neuropathy showing taurine and nicotinamide deficiencies. Hum. Mol. Genet. 2021, 30, 21–29. [Google Scholar]
- Ruiz, M.; Cuillerier, A.; Daneault, C.; Deschênes, S.; Frayne, I.R.; Bouchard, B.; Forest, A.; Legault, J.T.; LSFCConsortium Vaz, F.M.; Rioux, J.D.; et al. Lipidomics unveils lipid dyshomeostasis and low circulating plasmalogens as biomarkers in a monogenic mitochondrial disorder. JCI Insight 2019, 4, e123231. [Google Scholar] [CrossRef] [PubMed]
- Thompson Legault, J.; Strittmatter, L.; Tardif, J.; Sharma, R.; Tremblay-Vaillancourt, V.; Aubut, C.; Boucher, G.; Clish, C.B.; Cyr, D.; Daneault, C.; et al. Metabolic Signature of Mitochondrial Dysfunction Revealed through a Monogenic Form of Leigh Syndrome. Cell Rep. 2015, 13, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Pastore, A.; Petrillo, S.; Tozzi, G.; Carrozzo, R.; Martinelli, D.; Dionisi-Vici, C.; Di Giovamberardino, G.; Ceravolo, F.; Klein, M.B.; Miller, G.; et al. Glutathione: A redox signature in monitoring EPI-743 therapy in children with mitochondrial encephalomyopathies. Mol. Gen. Met. 2013, 2, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Suárez-Rivero, J.M.; Pastor-Maldonado, C.J.; Povea-Cabello, S.; Álvarez-Córdoba, M.; Villalón-García, I.; Munuera-Cabeza, M.; Suárez-Carrillo, A.; Talaverón-Rey, M.; Sánchez-Alcázar, J.A. Coenzyme Q10 Analogues: Benefits and Challenges for Therapeutics. Antioxidants 2021, 10, 236. [Google Scholar] [CrossRef]
- Buzkova, J.; Nikkanen, J.; Ahola, S.; Hakonen, H.A.; Sevastianova, K.; Hovinen, T.; Yki-Järvinen, H.; Pietiläinen, K.H.; Lönnqvist, T.; Velagapudi, V.; et al. Metabolomes of mitochondrial diseases and inclusion body myositis patients: Treatment targets and biomarkers. EMBO Mol. Med. 2018, 10, e9091. [Google Scholar] [CrossRef]
- Delaney, N.F.; Sharma, R.; Tadvalkar, L.; Clish, C.B.; Haller, R.G.; Mootha, V.K. Metabolic profiles of exercise in patients with McArdle disease or mitochondrial myopathy. Proc. Natl. Acad. Sci. USA 2017, 31, 8402–8407. [Google Scholar] [CrossRef]
- Shaham, O.; Slate, N.G.; Goldberger, O.; Xu, Q.; Ramanathan, A.; Souza, A.L.; Clish, C.B.; Sims, K.B.; Mootha, V.K. A plasma signature of human mitochondrial disease revealed through metabolic profiling of spent media from cultured muscle cells. Proc. Natl. Acad. Sci. USA 2010, 107, 1571–1575. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.M.; Vilasi, A.; Garcia-Perez, I.; Lapsley, M.; Alston, C.L.; Pitceathly, R.D.S.; McFarland, R.; Schaefer, A.M.; Turnbull, D.M.; Beaumont, N.J.; et al. The urinary proteome and metabonome differ from normal in adults with mitochondrial disease. Kidney Int. 2015, 87, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Southwell, N.; Primiano, G.; Nadkarni, V.; Attarwala, N.; Beattie, E.; Miller, D.; Alam, S.; Liparulo, I.; Shurbor, Y.; Valentino, M.L.; et al. A coordinated multiorgan metabolic response contributes to human mitochondrial myopathy. EMBO Mol. Med. 2023, 15, e16951. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Snyder, M. Promise of personalized omics to precision medicine. Wiley Interdiscip. Rev. Syst. Biol. Med. 2012, 5, 73–82. [Google Scholar] [CrossRef]
- Rotroff, D.M.; Motsinger-Reif, A.A. Embracing integrative multiomics approaches. Int. J. Genom. 2016, 2016, 1715985. [Google Scholar] [CrossRef]
| Authors | Year | No Pt | Phenotype | Genotype | Techniques | Tissues Analyzed |
|---|---|---|---|---|---|---|
| Shaham et al. [41] | 2010 | 16; 14 | PEO, MELAS; MERRF; PMM; ME | sDel, mDel, mtDNA depletion m.3243A>G, m.8344A>G, m.8993T>G | LC-MS/MS; Proton NMR spectroscopy | media of cultured mouse muscle cell, patient plasma |
| Pastore et al. [37] | 2013 | 10 | LS | m.3697G>A, m.13513G>A, m.14487T>C, SUCLA2, ETHE1, EARS2, SURF1 | HPLC-FL, spectrophotometric assay, colorimetric analysis, fluorometric assay | plasma; leukocytes and erythrocytes |
| Legault et al. [36] | 2015 | 9 | LSFC | LRPPRC | GC-MS and LC-MS | plasma, urine |
| Delaney et al. [40] | 2017 | 21 | PMM | sDel, mDel, m.3243A>G, m.10010T>C, m.12261T>C, m.4281A>G, m.8344A>G, m.5543T>C, MT-CYB, ISCU | LC-MS | plasma |
| Hall et al. [42] | 2015 | 117 | MELAS; MIDD; MERRF | m.3243G>A, m.8344A>G, single large scale mtDNA deletion, POLG, C10orf2/PEO, COX10, multiple mtDNA deletions | LC–MS/MS, Proton NMR spectroscopy | urine, serum |
| Buzkova et al. [39] | 2018 | 26 | ANS, PEO, MELAS, MIDD, IOSCA | sDel, m.3243A>G, POLG, TWNK | LC-MS/MS | serum/plasma, muscle |
| Ruiz et al. [35] | 2019 | 9 | LSFC | LRPPRC | untargeted and targeted lipidomics LC-MS (LC-QTOF and LC-QQQ) | plasma |
| Gervasoni et al. [32] | 2020 | 16 | PEO | sDel, POLG | FTIR | muscle |
| Sharma et al. [24] | 2021 | 102; 16 | MELAS, non-MELAS m.3243A>G | m.3243A>G | SOMAscan proteomic analysis, LC-MS | plasma |
| Esterhuizen et al. [31] | 2021 | 57 | MELAS, MIDD, PMM | m.3243A>G | GC-TOF-MS, LC-MS/MS, NMR | urine |
| Bocca et al. [34] | 2021 | 18 | LHON | m.3460G>A, m.11778G>A, m.14482C>A | untargeted metabolomics UHPLC/HRMS2 | plasma |
| Southwell et al. [43] | 2023 | 10 | MERRF | m.8344A>G | untargeted metabolomics LC/MS, tandem LC–MS/MS | plasma/serum, muscle |
| References | Proteins and Metabolites | Main Results | Field |
|---|---|---|---|
| Esterhuizen et al. [31] | In total, 54 significantly altered metabolites were discovered: 27 for the MELAS phenotype, 22 for MIDD, and 5 for myopathy. | Data highlighted an altered glucose metabolism in the MIDD phenotype, while an altered fatty acid synthesis in the MELAS patients. Hypothesized to be disturbed in all the phenotypes also the branched-chain amino acid (BCAA) metabolism. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Bocca et al. [34] | Found discriminating metabolites related to the diet (nicotinamide, taurine, choline, 1-methylhistidine and hippurate), mitochondrial energetic substrates (acetoacetate, glutamate and fumarate), and purine metabolism (inosine). | The study documents possible new therapeutic targets, in particular taurine and nicotinamide, due to their neuroprotective role. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Ruiz et al. [35] | The analysis revealed higher circulating levels of various acylcarnitines (ACs), saturated and unsaturated long-chain acylcarnitines (LCACs), changes in plasma and/or hepatic levels of plasmalogens, very-long-chain acylcarnitines (VLCACs), and primary bile acids conjugates in LSFC patients. | The study unveiled perturbations in fatty acid (FA) metabolism in mitochondria and major lipid dyshomeostasis in LSFC phenotype. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Buzkova et al. [39] | MDs and IBM showed transsulfuration pathway changes, creatine and niacinamide depletion in NMDs, IBM, and infantile-onset spinocerebellar ataxia (IOSCA). Low blood and muscle arginine in patients with m.3243A>G mutation. A group of four-metabolite (sorbitol, alanine, myoinositol, cystathionine) could distinguish primary MDs from others. | A disease-specific metabolomic fingerprint was highlighted for mitochondrial myopathy, infantile-onset spinocerebellar ataxia, inclusion body myositis, and non-mitochondrial neuromuscular diseases. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Delaney et al. [40] | In total, 9 metabolites levels differed between patient and control groups. In total, 10 metabolites levels differed between peak of exercise and rest and 17 metabolites levels differed between post-exercise and rest. The metabolites identified were associated with pyruvate metabolism, the TCA cycle, the urea cycle, and the purine nucleotide cycle. | Both at rest and exercise conditions highlight biochemical alterations that can be linked to the symptoms of the patients enrolled. In particular, lactate and pyruvate are examples of metabolites which variate across disease groups and exercise conditions. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Shaham et al. [41] | Detected 32 altered metabolites in culture media and 68 metabolites in plasma, 26 of which were had in common. | Elevated levels of lactate, alanine, creatine, and uridine were observed in patients compared with controls. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Hall et al. [42] | Metabolomics analysis highlighted low urine levels N-methylnicotinamide, hippurate, and creatinine in MDs patients respect to controls. Proteomics analysis revealed a decrease in the abundance of uromodulin, collagen fragments, apolipoprotein E, megalin, and cubilin. | The metabolomics and proteomics analysis showed variations in the urinary metabolites and proteins of mitochondrial patients compared to healthy controls. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Southwell et al. [43] | Altered TCA cycle, catabolism of glutamate, and lipid metabolism. | The study unveiled a metabolic remodeling in the cohort of MDs, characterized by catabolic signaling, lipid store mobilization and intramuscular lipid accumulation. | Biomarkers and pathological mechanisms: alteration in metabolic pathways |
| Legault et al. [36] | The analysis identified 45 relevant metabolites that distinguished patients from controls. | Redox status, b-hydroxybutyrate/acetoacetate ratio, acylcarnitines, citric acid cycle reaction, lipid and amino acid metabolism were altered in the disease condition. | Biomarkers and pathological mechanisms: alteration in metabolic, alteration in redox pathways |
| Sharma et al. [24] | Proteomic analysis revealed 3 possible novel protein markers (sE-selectin, sulfate 6-O-sulfotransferase 1, receptor tyrosine kinase). Metabolomic analysis identified N-lactoyl-amino acids, Beta-Hydroxy Fatty Acids (BOHFAs), and Beta-Hydroxy Acylcarnitines (BOHCAs) as new families of m.3243A>G markers. | The new biomarkers are associated with NADH-reductive stress, revealing an intriguing condition of metabolic adaptation focused on NADH redox imbalance that could lead to the activation of the integrated stress response. | Biomarkers and pathological mechanisms: alteration in redox pathways |
| Pastore et al. [37] | Glutathione forms levels and glutathione peroxidase activity were object of study. | MDs present a decrease of total and reduced glutathione (GSH), associated with high levels of all oxidized glutathione forms and a decreased of glutathione peroxidase activity. Glutathione is here defined as a “redox blood signature” and pathogenic factor in primary mitochondrial disorders. | Biomarkers and pathological mechanisms: alteration in redox pathways |
| Gervasoni et al. [32] | Found few peaks which can be considered putative markers for the disease discrimination. | FTIR spectroscopy emerges as a sensitive and specific diagnostic technique for PEO, revealing distinct biochemical profiles between participants with a single mtDNA deletion and those with pathogenic variants in POLG by. | New potential diagnostic approaches: spectroscopy analysis |
| Alix et al. [33] | Peaks assigned to proteins and various metabolites show differences in muscle disease vs. no muscle disease and between different muscle diseases. | Results demonstrated that spontaneous fiber-optic Raman spectroscopy could be applied to identify muscle disease in human samples and to discriminate between two different classes of muscle disease. | New potential diagnostic approaches: spectroscopy analysis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gervasoni, J.; Primiano, A.; Cicchinelli, M.; Santucci, L.; Servidei, S.; Urbani, A.; Primiano, G.; Iavarone, F. Mitochondrial Biomarkers in the Omics Era: A Clinical-Pathophysiological Perspective. Int. J. Mol. Sci. 2024, 25, 4855. https://doi.org/10.3390/ijms25094855
Gervasoni J, Primiano A, Cicchinelli M, Santucci L, Servidei S, Urbani A, Primiano G, Iavarone F. Mitochondrial Biomarkers in the Omics Era: A Clinical-Pathophysiological Perspective. International Journal of Molecular Sciences. 2024; 25(9):4855. https://doi.org/10.3390/ijms25094855
Chicago/Turabian StyleGervasoni, Jacopo, Aniello Primiano, Michela Cicchinelli, Lavinia Santucci, Serenella Servidei, Andrea Urbani, Guido Primiano, and Federica Iavarone. 2024. "Mitochondrial Biomarkers in the Omics Era: A Clinical-Pathophysiological Perspective" International Journal of Molecular Sciences 25, no. 9: 4855. https://doi.org/10.3390/ijms25094855
APA StyleGervasoni, J., Primiano, A., Cicchinelli, M., Santucci, L., Servidei, S., Urbani, A., Primiano, G., & Iavarone, F. (2024). Mitochondrial Biomarkers in the Omics Era: A Clinical-Pathophysiological Perspective. International Journal of Molecular Sciences, 25(9), 4855. https://doi.org/10.3390/ijms25094855






