Topical Neuropeptide Y for Ischemic Skin Wounds
Abstract
1. Introduction
2. Results
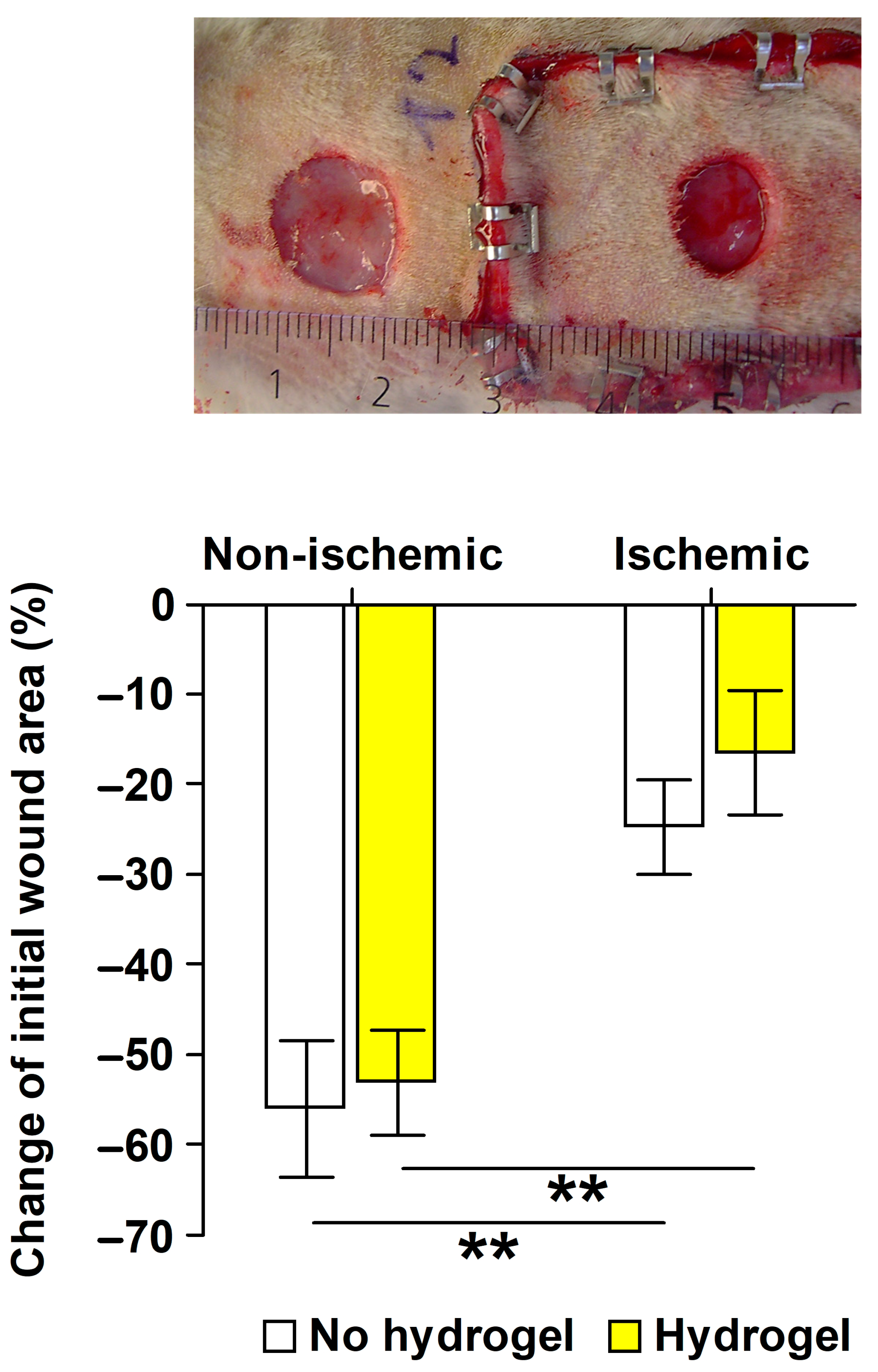
2.1. Validation of the Ischemic Wound Model
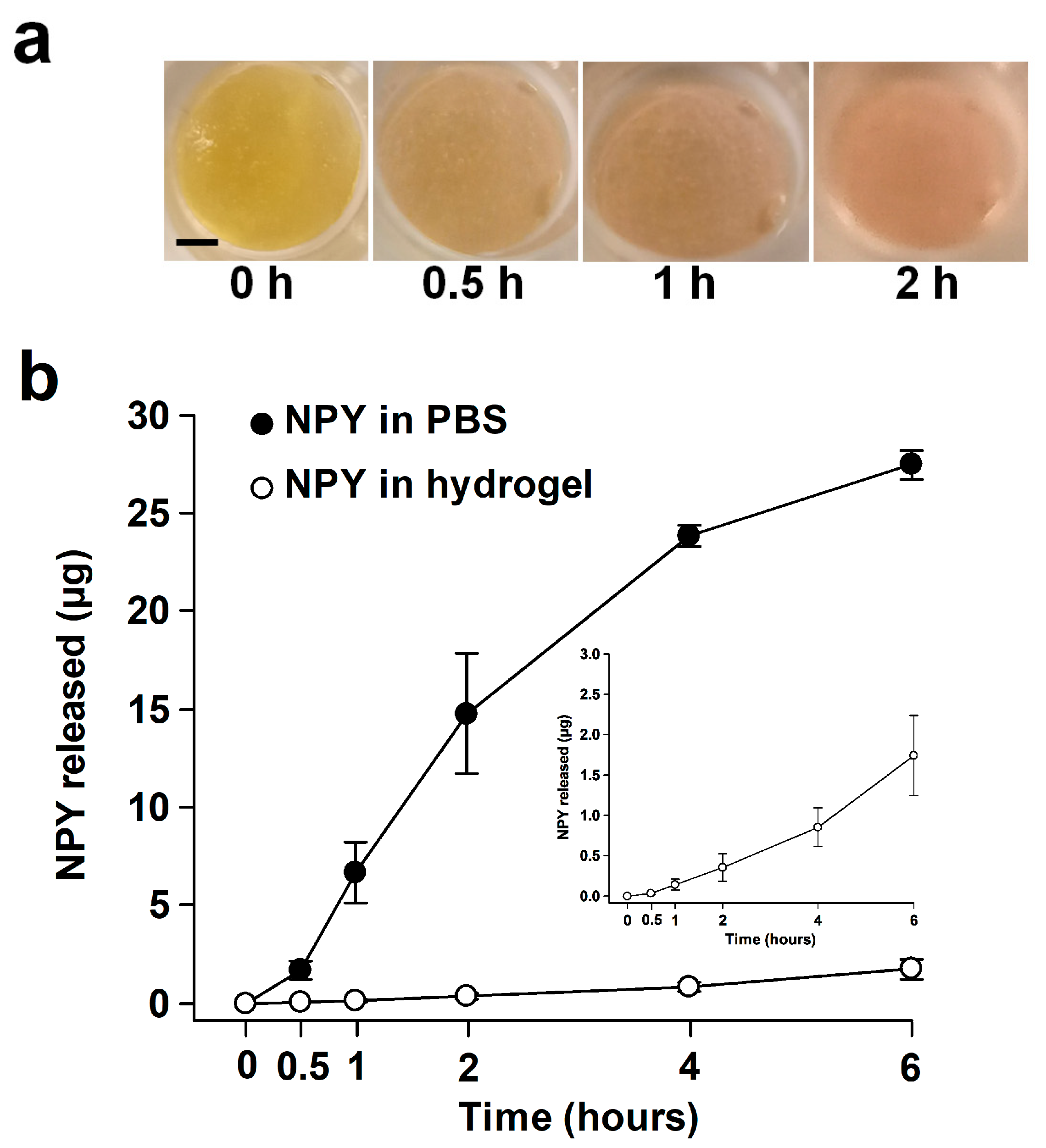
2.2. Release of NPY In Vitro
2.3. Effects of NPY In Vivo
2.3.1. Body Weight Development
2.3.2. Ischemic Wound Healing
2.3.3. In Situ Hybridization for Y2R mRNA
2.3.4. Light Microscopy Examination
3. Discussion
4. Materials and Methods
4.1. Chemicals and Reagents
4.2. In Vitro Release of NPY
4.3. In Vivo Wound Experiments
4.3.1. Animals
4.3.2. Surgery and Wounding Day 0
4.3.3. Validation Study of Ischemic versus Nonischemic Wound Healing
4.3.4. Intervention Study in the Ischemic Wounds
4.3.5. Wound Care, Wound Area Measurements, and Calculation of Relative Wound Area Change
4.3.6. Tissue Harvesting (Intervention Study)
4.3.7. In Situ Hybridization Assay of Y2R mRNA by RNAscope® (Intervention Study)
4.3.8. Histology (Intervention Study)
4.3.9. Blinding
4.4. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BSA | bovine serum albumin |
| CMC | carboxymethyl cellulose |
| FGF | fibroblast growth factor |
| HOAc | acetic acid |
| HUVEC | human umbilical vascular endothelial cell |
| IGF | insulin-like growth factor |
| LC | lymphocytes |
| MC | mast cells |
| NG | neutrophil granulocytes |
| NPY | neuropeptide Y |
| PBS | phosphate-buffered saline |
| PC | plasma cells |
| PDGF | platelet-derived growth factor |
| PP | pancreatic polypeptide |
References
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human skin wounds: A major and snowballing threat to public health and the economy. Wound Repair. Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Sen, C.K. Human wounds and its burden: An updated compendium of estimates. Adv. Wound Care 2019, 8, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Nelson, E.; Bradley, M. Dressings and topical agents for arterial leg ulcers. Cochrane Database Syst. Rev. 2007, CD001836, 1–20. [Google Scholar]
- Barrientos, S.; Stojadinovic, O.; Golinko, M.S.; Brem, H.; Tomic-Canic, M. Growth factors and cytokines in wound healing. Wound Repair. Regen. 2008, 16, 585–601. [Google Scholar] [CrossRef] [PubMed]
- Schäffer, M.; Beiter, T.; Becker, H.D.; Hunt, T.K. Neuropeptides: Mediators of inflammation and tissue repair? Arch. Surg. 1998, 133, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Ashrafi, M.; Baguneid, M.; Bayat, A. The role of neuromediators and innervation in cutaneous wound healing. Acta Derm. Venereol. 2016, 96, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Saraf, R.; Mahmood, F.; Amir, R.; Matyal, R. Neuropeptide Y is an angiogenic factor in cardiovascular regeneration. Eur. J. Pharmacol. 2016, 776, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Pedrazzini, T.; Pralong, F.; Grouzmann, E. Neuropeptide Y: The universal soldier. Cell. Mol. Life Sci. 2003, 60, 350–377. [Google Scholar] [CrossRef]
- Zukowska-Grojec, Z.; Karwatowska-Prokopczuk, E.; Rose, W.; Rone, J.; Movafagh, S.; Ji, H.; Yeh, Y.; Chen, W.T.; Kleinman, H.K.; Grouzmann, E.; et al. Neuropeptide Y: A novel angiogenic factor from the sympathetic nerves and endothelium. Circ. Res. 1998, 83, 187–195. [Google Scholar] [CrossRef]
- Ekstrand, A.J.; Cao, R.; Björndahl, M.; Nyström, S.; Jönsson-Rylander, A.C.; Hassani, H.; Hallberg, B.; Nordlander, M.; Cao, Y. Deletion of neuropeptide Y (NPY) 2 receptor in mice results in blockage of NPY-induced angiogenesis and delayed wound healing. Proc. Natl. Acad. Sci. USA 2003, 100, 6033–6038. [Google Scholar] [CrossRef]
- Movafagh, S.; Hobson, J.P.; Spiegel, S.; Kleinman, H.K.; Zukowska, Z. Neuropeptide Y induces migration, proliferation, and tube formation of endothelial cells bimodally via Y1, Y2, and Y5 receptors. FASEB J. 2006, 20, 1924–1926. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.W.; Grant, D.S.; Movafagh, S.; Zukowska, Z. Impaired angiogenesis in neuropeptide Y (NPY)-Y2 receptor knockout mice. Peptides 2003, 24, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.C.; Liu, Y.B.; Liu, W.F.; Zhou, Y.Y.; He, H.F.; Lin, S. Neuropeptide Y is an immunomodulatory factor: Direct and indirect. Front. Immunol. 2020, 11, 580378. [Google Scholar] [CrossRef] [PubMed]
- Kopp, J.; Collin, O.; Villar, M.; Mullins, D.; Bergh, A.; Hokfelt, T. Regulation of neuropeptide Y Y1 receptors by testosterone in vascular smooth muscle cells in rat testis. Neuroendocrinology 2008, 88, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.Q.; Cox, H.M.; Costa, S.K.; Herzog, H.; Brain, S.D. The ability of neuropeptide Y to mediate responses in the murine cutaneous microvasculature: An analysis of the contribution of Y1 and Y2 receptors. Br. J. Pharmacol. 2003, 140, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Dumont, Y.; Bastianetto, S.; Duranton, A.; Breton, L.; Quirion, R. Immunohistochemical distribution of neuropeptide Y, peptide YY, pancreatic polypeptide-like immunoreactivity and their receptors in the epidermal skin of healthy women. Peptides 2015, 70, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Pradhan Nabzdyk, L.; Kuchibhotla, S.; Guthrie, P.; Chun, M.; Auster, M.E.; Nabzdyk, C.; Deso, S.; Andersen, N.; Gnardellis, C.; LoGerfo, F.W.; et al. Expression of neuropeptides and cytokines in a rabbit model of diabetic neuroischemic wound healing. J. Vasc. Surg. 2013, 58, 766–775. [Google Scholar] [CrossRef]
- Lee, E.W.; Michalkiewicz, M.; Kitlinska, J.; Kalezic, I.; Switalska, H.; Yoo, P.; Sangkharat, A.; Ji, H.; Li, L.; Michalkiewicz, T.; et al. Neuropeptide Y induces ischemic angiogenesis and restores function of ischemic skeletal muscles. J. Clin. Investig. 2003, 111, 1853–1862. [Google Scholar] [CrossRef]
- Zukowska, Z.; Grant, D.S.; Lee, E.W. Neuropeptide Y: A novel mechanism for ischemic angiogenesis. Trends Cardiovasc. Med. 2003, 13, 86–92. [Google Scholar] [CrossRef]
- Puolakkainen, P.A.; Twardzik, D.R.; Ranchalis, J.E.; Pankey, S.C.; Reed, M.J.; Gombotz, W.R. The enhancement in wound healing by transforming growth factor-beta 1 (TGF-beta 1) depends on the topical delivery system. J. Surg. Res. 1995, 58, 321–329. [Google Scholar] [CrossRef]
- Beckert, S.; Hierlemann, H.; Muschenborn, N.; Witte, M.; Ranke, M.; Coerper, S. Experimental ischemic wounds: Correlation of cell proliferation and insulin-like growth factor I expression and its modification by different local IGF-I release systems. Wound Repair. Regen. 2005, 13, 278–283. [Google Scholar] [CrossRef]
- Gainza, G.; Villullas, S.; Pedraz, J.L.; Hernandez, R.M.; Igartua, M. Advances in drug delivery systems (DDSs) to release growth factors for wound healing and skin regeneration. Nanomedicine 2015, 11, 1551–1573. [Google Scholar] [CrossRef]
- Harrison, I.P.; Spada, F. Hydrogels for atopic dermatitis and wound management: A superior drug delivery vehicle. Pharmaceutics 2018, 10, 71. [Google Scholar] [CrossRef]
- Shin, D.Y.; Park, J.U.; Choi, M.H.; Kim, S.; Kim, H.E.; Jeong, S.H. Polydeoxyribonucleotide-delivering therapeutic hydrogel for diabetic wound healing. Sci. Rep. 2020, 10, 16811. [Google Scholar] [CrossRef]
- Ji, J.A.; Liu, J.; Shire, S.J.; Kamerzell, T.J.; Hong, S.; Billeci, K.; Shen, Y.; Wang, Y.J. Characteristics of rhVEGF release from topical hydrogel formulations. Pharm. Res. 2010, 27, 644–654. [Google Scholar] [CrossRef]
- Weinreich, J.; Ågren, M.S.; Bilali, E.; Kleinman, H.K.; Coerper, S.; Königsrainer, A.; Beckert, S. Effects of isoniazid and niacin on experimental wound-healing. Surgery 2010, 147, 780–788. [Google Scholar] [CrossRef]
- Ågren, M.S.; Andersen, T.L.; Andersen, L.; Schiødt, C.B.; Surve, V.; Andreassen, T.T.; Risteli, J.; Franzén, L.E.; Delaissé, J.M.; Heegaard, A.M.; et al. Nonselective matrix metalloproteinase but not tumor necrosis factor-alpha inhibition effectively preserves the early critical colon anastomotic integrity. Int. J. Color. Dis. 2011, 26, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Danielsen, P.L.; Holst, A.V.; Maltesen, H.R.; Bassi, M.R.; Holst, P.J.; Heinemeier, K.M.; Olsen, J.; Danielsen, C.C.; Poulsen, S.S.; Jorgensen, L.N.; et al. Matrix metalloproteinase-8 overexpression prevents proper tissue repair. Surgery 2011, 150, 897–906. [Google Scholar] [CrossRef]
- Parker, S.L.; Balasubramaniam, A. Neuropeptide Y Y2 receptor in health and disease. Br. J. Pharmacol. 2008, 153, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Shi, T.; Holmberg, K.; Landry, M.; Huang, W.; Xiao, H.; Ju, G.; Hökfelt, T. Expression and regulation of the neuropeptide Y Y2 receptor in sensory and autonomic ganglia. Proc. Natl. Acad. Sci. USA 1997, 94, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.P.; Cavadas, C.; Baïsse-Agushi, B.; Spertini, O.; Brunner, H.R.; Grouzmann, E. NPY, NPY receptors, and DPP IV activity are modulated by LPS, TNF-alpha and IFN-gamma in HUVEC. Regul. Pept. 2003, 116, 71–79. [Google Scholar] [CrossRef]
- Chen, C.; Schultz, G.S.; Bloch, M.; Edwards, P.D.; Tebes, S.; Mast, B.A. Molecular and mechanistic validation of delayed healing rat wounds as a model for human chronic wounds. Wound Repair. Regen. 1999, 7, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Amin, Z.A.; Ali, H.M.; Alshawsh, M.A.; Darvish, P.H.; Abdulla, M.A. Application of Antrodia camphorata promotes rat’s wound healing in vivo and facilitates fibroblast cell proliferation in vitro. Evid. Based Complement. Altern. Med. 2015, 2015, 317693. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.G.; Phan, C.W.; Sabaratnam, V.; Abdullah, N.; Abdulla, M.A.; Kuppusamy, U.R. Polysaccharides-rich extract of Ganoderma lucidum (M.A. Curtis:Fr.) P. Karst accelerates wound healing in streptozotocin-induced diabetic rats. Evid. Based Complement. Altern. Med. 2013, 2013, 671252. [Google Scholar] [CrossRef] [PubMed]
- Hajiaghaalipour, F.; Kanthimathi, M.S.; Abdulla, M.A.; Sanusi, J. The effect of Camellia sinensis on wound healing potential in an animal model. Evid. Based Complement. Altern. Med. 2013, 2013, 386734. [Google Scholar] [CrossRef]
- Tan, M.K.; Hasan Adli, D.S.; Tumiran, M.A.; Abdulla, M.A.; Yusoff, K.M. The efficacy of gelam honey dressing towards excisional wound healing. Evid. Based Complement. Altern. Med. 2012, 2012, 805932. [Google Scholar] [CrossRef] [PubMed]
- Albaayit, S.F.; Abba, Y.; Rasedee, A.; Abdullah, N. Effect of Clausena excavata Burm. f. (Rutaceae) leaf extract on wound healing and antioxidant activity in rats. Drug Des. Devel Ther. 2015, 9, 3507–3518. [Google Scholar] [CrossRef]
- Rouhollahi, E.; Moghadamtousi, S.Z.; Hajiaghaalipour, F.; Zahedifard, M.; Tayeby, F.; Awang, K.; Abdulla, M.A.; Mohamed, Z. Curcuma purpurascens BI. rhizome accelerates rat excisional wound healing: Involvement of Hsp70/Bax proteins, antioxidant defense, and angiogenesis activity. Drug Des. Devel Ther. 2015, 9, 5805–5813. [Google Scholar] [CrossRef]
- Thomas, L.; Scheidt, H.A.; Bettio, A.; Beck-Sickinger, A.G.; Huster, D.; Zschörnig, O. The interaction of neuropeptide Y with negatively charged and zwitterionic phospholipid membranes. Eur. Biophys. J. 2009, 38, 663–677. [Google Scholar] [CrossRef]
- Nagashima, R.; Yoshida, N.; Terao, N. Sucralfate, a basic aluminum salt of sucrose sulfate. II. Inhibition of peptic hydrolysis as it results from sucrose sulfate interaction with protein substrate, serum albumins. Arzneimittelforschung 1980, 30, 73–76. [Google Scholar]
- Abid, K.; Rochat, B.; Lassahn, P.G.; Stocklin, R.; Michalet, S.; Brakch, N.; Aubert, J.F.; Vatansever, B.; Tella, P.; De Meester, I.; et al. Kinetic study of neuropeptide Y (NPY) proteolysis in blood and identification of NPY3-35: A new peptide generated by plasma kallikrein. J. Biol. Chem. 2009, 284, 24715–24724. [Google Scholar] [CrossRef]
- Baticic Pucar, L.; Pernjak Pugel, E.; Detel, D.; Varljen, J. Involvement of DPP IV/CD26 in cutaneous wound healing process in mice. Wound Repair. Regen. 2017, 25, 25–40. [Google Scholar] [CrossRef]
- Kanikireddy, V.; Varaprasad, K.; Jayaramudu, T.; Karthikeyan, C.; Sadiku, R. Carboxymethyl cellulose-based materials for infection control and wound healing: A review. Int. J. Biol. Macromol. 2020, 164, 963–975. [Google Scholar] [CrossRef]
- Ågren, M.S.; Franzén, L. Foam cells after treatment with hydrocolloid dressings. Br. J. Dermatol. 1991, 125, 193. [Google Scholar] [CrossRef] [PubMed]
- Ågren, M.S. Matrix metalloproteinases (MMPs) are required for re-epithelialization of cutaneous wounds. Arch. Dermatol. Res. 1999, 291, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Leonardis, M.; Palange, A.; Dornelles, R.F.; Hund, F. Use of cross-linked carboxymethyl cellulose for soft-tissue augmentation: Preliminary clinical studies. Clin. Interv. Aging 2010, 5, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Ågren, M.S. An amorphous hydrogel enhances epithelialisation of wounds. Acta Derm. Venereol. 1998, 78, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Pilakasiri, K.; Molee, P.; Sringernyuang, D.; Sangjun, N.; Channasanon, S.; Tanodekaew, S. Efficacy of chitin-PAA-GTMAC gel in promoting wound healing: Animal study. J. Mater. Sci. Mater. Med. 2011, 22, 2497–2504. [Google Scholar] [CrossRef] [PubMed]
- Ågren, M.S.; Everland, H. Two hydrocolloid dressings evaluated in experimental full-thickness wounds in the skin. Acta Derm. Venereol. 1997, 77, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Mitić, K.; Stanojević, S.; Kuštrimović, N.; Vujic, V.; Dimitrijević, M. Neuropeptide Y modulates functions of inflammatory cells in the rat: Distinct role for Y1, Y2 and Y5 receptors. Peptides 2011, 32, 1626–1633. [Google Scholar] [CrossRef] [PubMed]
- Kastin, A.J.; Kuzemchak, B.; Tompkins, R.G.; Schally, A.V.; Miller, M.C., 3rd. Melanin in the rat brain. Brain Res. Bull. 1976, 1, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Manunta, G.; Cancedda, M. Skins of albino animals contain melanin. Boll. Soc. Ital. Biol. Sper. 1975, 51, 766–770. [Google Scholar] [PubMed]
- Blaszczyk, W.M.; Arning, L.; Hoffmann, K.P.; Epplen, J.T. A Tyrosinase missense mutation causes albinism in the Wistar rat. Pigment. Cell Res. 2005, 18, 144–145. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Nimse, S.B.; Mathew, D.E.; Dhimmar, A.; Sahastrabudhe, H.; Gajjar, A.; Ghadge, V.A.; Kumar, P.; Shinde, P.B. Microbial melanin: Recent advances in biosynthesis, extraction, characterization, and applications. Biotechnol. Adv. 2021, 53, 107773. [Google Scholar] [CrossRef]
- Kjaer, M.; Kristjansdottir, H.; Andersen, L.; Heegaard, A.M.; Ågren, M.S.; Jorgensen, L.N. The effect of gender on early colonic anastomotic wound healing. Int. J. Color. Dis. 2018, 33, 1269–1276. [Google Scholar] [CrossRef]
- Wheater, P.R.; Burkitt, H.G.; Daniels, V.G. Functional Histology: A Text and Colour Atlas; Churchhill Livingstone: Edinburgh, UK, 1979; p. 278. [Google Scholar]




| Group | Angiogenesis 1 | Inflammatory Cell Infiltrate | Neoepithelium (mm) 2 | Foreign Bodies 4 | Giant Cells | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Grade 1 | LC 3 | NG 3 | PC 3 | MC 3 | Ingrowth | Thickness | ||||
| NPY | 3 | 3 | 316 | 85 | 6 | 3 | 1.1 | 0.14 | 1 | 3 |
| IGF-I | 1 | 1 | 144 | 42 | 1 | 0 | 1.4 | 0.061 | 3 | 1 |
| Control | 2 | 1.5 | 247 | 75 | 8 | 3 | 0.88 | 0.10 | 2 | 0 |
| Procedure | Day | |||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 2 | 4 | 6 | 8 | 10 | 12 | 14 | |
| Wounding 1 | ✕ | |||||||
| Treatment 2 | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | |
| Wound tracing 3 | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stangerup, T.; Gjerdrum, L.M.R.; Bzorek, M.; Andersen, L.; Heegaard, A.-M.; Jorgensen, L.N.; Ågren, M.S. Topical Neuropeptide Y for Ischemic Skin Wounds. Int. J. Mol. Sci. 2024, 25, 3346. https://doi.org/10.3390/ijms25063346
Stangerup T, Gjerdrum LMR, Bzorek M, Andersen L, Heegaard A-M, Jorgensen LN, Ågren MS. Topical Neuropeptide Y for Ischemic Skin Wounds. International Journal of Molecular Sciences. 2024; 25(6):3346. https://doi.org/10.3390/ijms25063346
Chicago/Turabian StyleStangerup, Tais, Lise Mette Rahbek Gjerdrum, Michael Bzorek, Line Andersen, Anne-Marie Heegaard, Lars N. Jorgensen, and Magnus S. Ågren. 2024. "Topical Neuropeptide Y for Ischemic Skin Wounds" International Journal of Molecular Sciences 25, no. 6: 3346. https://doi.org/10.3390/ijms25063346
APA StyleStangerup, T., Gjerdrum, L. M. R., Bzorek, M., Andersen, L., Heegaard, A.-M., Jorgensen, L. N., & Ågren, M. S. (2024). Topical Neuropeptide Y for Ischemic Skin Wounds. International Journal of Molecular Sciences, 25(6), 3346. https://doi.org/10.3390/ijms25063346








