Abstract
Sanguinarine (1) is a natural product with significant pharmacological effects. However, the application of sanguinarine has been limited due to its toxic side effects and a lack of clarity regarding its molecular mechanisms. To reduce the toxic side effects of sanguinarine, its cyanide derivative (1a) was first designed and synthesized in our previous research. In this study, we confirmed that 1a presents lower toxicity than sanguinarine but shows comparable anti-leukemia activity. Further biological studies using RNA-seq, lentiviral transfection, Western blotting, and flow cytometry analysis first revealed that both compounds 1 and 1a inhibited the proliferation and induced the apoptosis of leukemic cells by regulating the transcription of c-MET and then suppressing downstream pathways, including the MAPK, PI3K/AKT and JAK/STAT pathways. Collectively, the data indicate that 1a, as a potential anti-leukemia lead compound regulating c-MET transcription, exhibits better safety than 1 while maintaining cytostatic activity through the same mechanism as 1.
1. Introduction
Sanguinarine (1) (Figure 1) is an active natural product isolated from many medicinal plants []. Its pharmacological effects include antitumor, antibacterial, antiviral, and anti-inflammatory effects [,,,]. Antitumor studies on sanguinarine have mainly focused on several major human cancers, including lung, breast, and bladder cancer, and other solid tumors []. Previous studies indicated that the toxicity of sanguinarine is the main factor limiting its clinical application in cancer therapy [,]. Therefore, it is necessary to perform structural optimization to reduce toxicity.
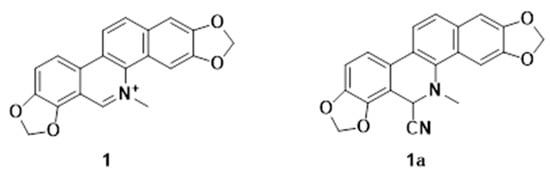
Figure 1.
Structures of Sanguinarine and its cyanide derivative.
To improve the cytostatic activity of 1 and reduce its toxic effects on normal cells, in our previous work we carried out structural modification and assessed the anti-leukemia activities of its derivatives []. We found that the activity of 1 was mainly dependent on the following structural features: the fusion of the B/C ring, hydroxylation patterns, N-methyl substitutions, and planar configuration []. Most notably, the cyanide derivative (1a) (Figure 1) showed comparable anti-leukemic activity and lower normal hepatic stellate cell cytotoxicity than 1; however, the molecular mechanisms of the anti-leukemic effect remain to be explored.
According to previous research, 1 exerts its cytostatic effects mainly by inducing the apoptosis of tumor cells through regulatory proteins and signaling pathways, including the mitogen-activated protein kinase (MAPK) [], PI3K/AKT [], JAK2/STAT3, and P53 pathways [,]. However, it is not clear how these signaling pathways and proteins are regulated by 1. Therefore, it is crucial to further explore the underlying anticancer mechanism or targets of 1. Upstream proteins such as c-MET, EGFR, and HER2 are involved in compound-1-mediated regulation of the MAPK, PI3K/AKT, and STAT3 signaling pathways [,,]. The c-MET receptor, a receptor tyrosine kinase (RTK), is the cell surface receptor for hepatocyte growth factor (HGF) encoded by the MET proto-oncogene []. It plays essential roles in controlling a number of critical cellular processes []. Aberrant activation of c-MET can lead to tumor progression, invasive growth, angiogenesis, metastasis, and resistance to therapies, and plays a vital role in the treatment of tumors, especially hepatocellular carcinoma; therefore, c-MET has become a popular target for tumor treatment [].
To date, there are no reports about the effect of 1 on c-MET. In this work, we investigated the effects of 1 and its derivative 1a on c-MET at the transcript and protein levels. This study might reveal a new antitumor mechanism and provide a solid theoretical basis for the development and utilization of 1 in tumor therapy.
2. Results and Discussion
2.1. Compounds 1 and 1a Inhibited the Proliferation of Human Erythroid Leukemia Cells
Leukemia is a class of clonal malignant diseases involving the abnormal expansion of hepatic stellate cells []. At present, the treatment of leukemia is still a major challenge, and most of the drugs used clinically for the treatment of leukemia have various degrees of adverse effects []. There is an urgent need for effective lead compounds for the treatment of leukemia. Compound 1 is a natural product isolated from Zanthoxylum nitidum (Roxb.) DC with significant inhibitory activity against leukemia cells but obvious cytotoxicity against normal cells. To improve the cytostatic activity of 1 and reduce its toxic effects, a series of derivatives were synthesized (Figure S1), and the cytostatic activity of the derivatives including 1a was screened (Table S1). Notably, the cytostatic activity of 1a was comparable to that of 1 (Figure 2A), but 1a was less cytotoxic than 1 to normal LX-2 hepatic stellate cells (Figure 2B). To further investigate whether the molecular mechanisms of compound 1a were the same as those of the lead compound (compound 1), 0.75 μM, 1.50 μM, and 3.00 μM, and 1.00 μM, 2.00 μM, and 4.00 μM were separately selected as experimental concentrations for 1 and 1a.
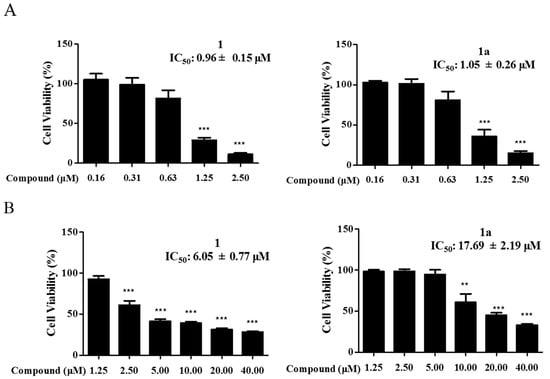
Figure 2.
Compounds 1 and 1a inhibit the proliferation of HEL cells and LX-2 cells. (A) HEL cells were incubated with 1 and 1a. (B) LX-2 cells were incubated with 1 and 1a. Cell activity was assessed using the CCK-8 kit. Data were collected from three independent experiments. Error bars represent standard deviation. Two-tailed p values were derived from unpaired Student’s t test. “**”, p < 0.01; “***”, p < 0.001.
2.2. The Effect of 1 and 1a on Cell Apoptosis
The induction of apoptosis is considered to be one of the major mechanisms of 1′s inhibition of tumor cells []. To assess the effect of 1 on the apoptosis of HEL cells, cells were stained with Hoechst 33258 []. As shown in Figure 3A, the intensity of bright blue fluorescence was enhanced with increasing concentrations after treatment with 1 and 1a, and the fluorescence spots were evenly distributed. Compared with that of the blank control group, the fluorescence intensity of the treatment group was significantly higher. Meanwhile, TUNEL staining showed that treatment with 1 and 1a significantly induced cell apoptosis (Figure 3B) []. The above results demonstrate that both 1 and 1a could induce the apoptosis of HEL cells in a dose-dependent manner.

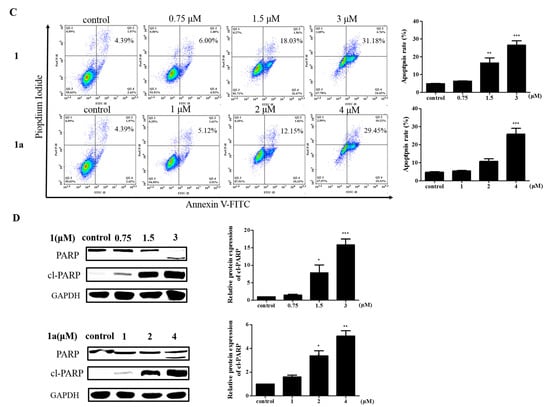
Figure 3.
The effect of 1 and 1a on cell apoptosis. (A) Hoechst 33258 staining of HEL cells. Bright blue fluorescence increases in a dose-dependent manner Scale bar: 300 μm (n = 3). (B) TUNEL staining and the average data of HEL cells. Scale bar: 200 μm (n = 3). (C) Different concentrations of 1 or 1a were used to treat HEL cells. The rate of apoptosis was assessed with an Annexin V-FITC/PI kit. (D) The expression levels of apoptosis-related proteins from HEL cells treated with 1 and 1a were analyzed by Western blotting. “*”, p < 0.05; “**”, p < 0.01; “***”, p < 0.001.
To further explore the effect of 1 and 1a on the viability of HEL cells, an Annexin V-FITC/propidium iodide (PI) double-staining apoptosis kit was used to measure the apoptosis rate of HEL cells []. HEL cells were treated with different concentrations of the compounds, and the staining results showed that the compounds increased the apoptosis rate of HEL cells in a dose-dependent manner (Figure 3C). Then, Western blotting was used to analyze the changes in apoptotic proteins after the treatment of HEL cells with the compounds []. The results showed that the compounds increased the levels of cl-PARP protein in a dose-dependent manner (Figure 3D). PARP is a DNA repair enzyme that plays an important role in DNA damage repair and apoptosis, and PARP shearing is considered to be an important indicator of apoptosis []. Overall, these results clearly confirmed that 1 and 1a can induce HEL cell apoptosis.
2.3. Compounds 1 and 1a Exerted Pharmacological Antitumor Effects by Blocking MAPK Signaling
To elucidate the molecular mechanisms of 1 and 1a in leukemia, RNA-seq analysis was used to detect differential gene expression after compound treatment (Table S2) [], and the twenty most significantly enriched pathways were identified by KEGG enrichment analysis []. The MAPK signaling pathway was the most significantly enriched pathway in both 1-treated cells and 1a-treated cells vs. controls cells (Figure 4A). The MAPK family is a group of serine/threonine protein kinases that mediate intracellular signaling and are important transmitters of signals from the cell surface to the interior of the nucleus. The MAPK signaling pathway consists of three main MAPK subfamilies, including MAPK14, the c-Jun N-terminal kinase or stress-activated protein kinase (JNK or SAPK), and the extracellular signal-regulated kinases (ERK MAPK, Ras/Raf1/MEK/ERK). There is increasing evidence that activation of the ERK MAPK pathway is involved in the pathogenesis and progression of human cancers and is one of the most important pathways for cell proliferation [].
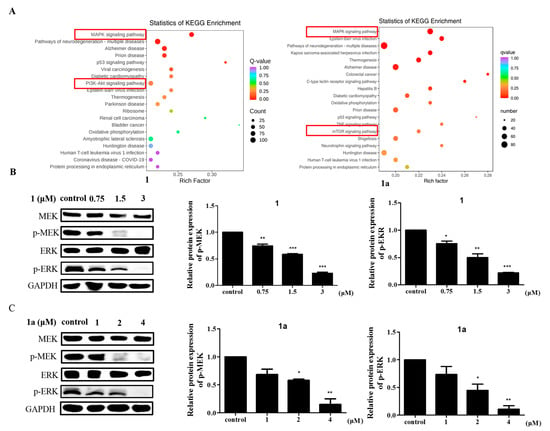
Figure 4.
Compounds 1 and 1a inhibit HEL cell activity by blocking MAPK signaling pathways. (A) RNA-seq was performed in HEL cells pretreated with DMSO, 1 (3 μM), or 1a (4 μM), and KEGG enrichment analysis was used to analyze the most significantly enriched signaling pathways. The vertical coordinate represents the KEGG pathway, and the horizontal coordinate represents the rich factor. The larger the rich factor is, the greater the enrichment level. The larger the dot is, the greater the number of differential genes enriched in the pathway. The redder the color of the dot is, the more significant the enrichment. (B,C) The expression of intrinsic MAPK-signaling-pathway-related proteins in HEL cells was measured by Western blotting. “*”, p < 0.05; “**”, p < 0.01; “***”, p < 0.001.
To further confirm the role of the MAPK signaling pathway in the mechanisms of action of 1 and 1a on cells, we examined the protein expression levels of MEK and ERK and their phosphorylation levels of key factors in the MAPK signaling pathway by Western blotting. Western blotting results showed that treatment with 1 and 1a reduced p-MEK and p-ERK expression in a concentration-dependent manner (Figure 4B,C). These results revealed an antagonistic relationship between 1/1a and MAPK signaling in HEL cells. In addition, we found that both 1 and 1a significantly decreased the protein levels of c-MET, an upstream target protein of the MAPK signaling pathway [].
2.4. Compounds 1 and 1a Antagonize the MAPK Signaling Pathway to Induce Apoptosis by Inhibiting c-MET Protein Expression
c-MET is an upstream protein of the MAPK signaling pathway, and it has been reported in the literature that c-MET activates Ras through the GRB2-SOS complex [], which in turn activates RAF and activates the downstream MAPK pathway. In addition, the binding of the receptor c-MET to hepatocyte growth factor (HGF) activates several signaling pathways, such as the PI3K/AKT, NF-κB and STAT3/5 pathways []. Thus, the overexpression of HGF and the overactivation of c-MET play key roles in tumorigenesis []. Another study showed that there is high expression of c-MET and its sole ligand HGF in HEL cells [], and in view of this, it is reasonable to suspect that in HEL cells, 1 and 1a induce apoptosis by mediating c-MET activation of the MAPK signaling pathway. Therefore, we analyzed the protein expression of c-MET after compound treatment of HEL cells. The experiments showed that both 1 and 1a reduced the expression levels of c-MET protein in a time-dependent and dose-dependent manner (Figure 5A,B). This suggests that the expression of c-MET was suppressed after treatment with the compounds, and the RNA-seq analysis also showed that the PI3K/AKT/mTOR signaling pathway, a downstream signaling pathway of c-MET, was one of the most significantly changed signaling pathways in cells treated with 1 or 1a vs. control cells (Figure 4A) []. We speculate that the alteration of the MAPK signaling pathway is likely to be mediated by c-MET. To test this hypothesis, we further validated the protein expression levels of the c-MET downstream pathway components PI3K/AKT/mTOR and JAK2/STAT3. As expected, the Western blotting results showed that both 1 and 1a reduced the protein expression levels of p-PI3K, p-mTOR, and p-STAT3 in a dose-dependent manner (Figure 5C,D). This result further confirms that the molecular mechanism by which 1 and 1a act on HEL cells may be mediated through c-MET.
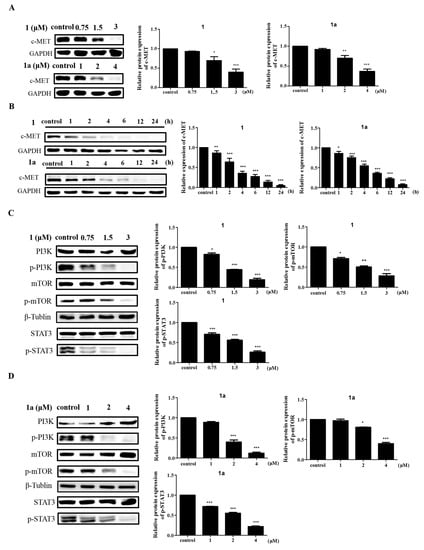
Figure 5.
Compounds 1 and 1a induce HEL cell apoptosis via the c-MET signaling pathway. (A) Both 1 and 1a decrease c-MET protein expression in a dose-dependent manner. (B) Both 1 and 1a decrease c- MET protein expression in a time-dependent manner. (C,D) Both 1 and 1a decrease the phosphorylation levels of downstream proteins in the c-MET signaling pathway in a dose-dependent manner. “*”, p < 0.05; “**”, p < 0.01; “***”, p < 0.001.
2.5. Compounds 1 and 1a Suppress the MAPK, PI3K/AKT, and STAT3 Signaling Pathways by Decreasing the mRNA and Protein Levels of c-MET
To confirm the mechanism by which the downstream signaling pathways MAPK, PI3K/AKT, and STAT3 are mediated by 1 and 1a via c-MET, overexpression of c-MET was performed in HEL cells (Table S3, Figure S2) []. According to Western blotting validation experiments, the decrease in the protein levels of c-MET caused by treatment with 1 and 1a could be attenuated by MET transient transfection, indicating the essential role of MET in the antiproliferative activity of these compounds. This result was verified by assessment of the protein expression levels of p-MEK, p-ERK, p-mTOR, and p-STAT3, which are key targets in the downstream signaling pathway (Figure 6A,B). To further explore how c-MET protein expression levels were affected by 1 and 1a, we examined the mRNA expression levels of c- MET by RT q-PCR after compound treatment []. Intriguingly, c-MET mRNA levels in HEL cells were reduced in a dose-dependent manner with compound treatment, indicating that c-MET expression is subject to pretranscriptional regulation (Figure 6C); this indicates that c-MET and its downstream pathways are repressed, at least in part, through c-MET pretranscriptional regulation after treatment with 1 and 1a.

Figure 6.
Compounds 1 and 1a decrease the mRNA and protein levels of c-MET. (A, B) Overexpression of c-MET by lentiviral infection of HEL cells and detection of c-MET-signaling-pathway-related protein expression by Western blotting. (C) After treatment with 1 and 1a, the mRNA levels of c-MET were detected by RT q-PCR. “ns”, no significance; “*”, p < 0.05; “**”, p < 0.01; “***” p < 0.001, “****”, p < 0.0001.
These data indicated that in HEL cells, 1 and 1a exert their cytostatic effects at least in part by decreasing the mRNA and protein levels of c-MET and subsequently inhibiting the MAPK, PI3K/AKT, and STAT3 signaling pathways as shown in Figure 7.
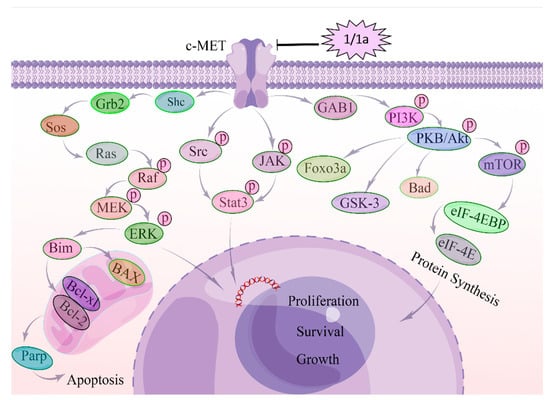
Figure 7.
Molecular mechanism of c-MET regulating HEL cells after the treatment with compounds 1 and 1a. c-MET is overactivated in human erythroid leukemia cell cells (HEL). After the treatment with 1 and 1a, the mRNA expression level and protein expression level of c-MET were suppressed, and subsequently, the c-MET homodimerization and autophosphorylation were affected. Then, GAB-1, Shc, Grb-2, and STAT3 were suppressed. Grb2 inhibits SOS, SOS suppresses RAS, and then RAS inhibits RAF, MEK, and ERK/MAPK. Suppressed ERK/MAPK can modulate transcription factors to regulate cell behaviors. Suppressed GAB-1 inhibits AKT, PKB, and mTOR to regulate transcription factors.
In this study, we found that both 1 and 1a effectively decreased the viability of HEL in leukemic cells in a dose-dependent manner, and 1 and 1a mainly decreased c-MET mRNA and protein levels in a time-dependent and dose-dependent manner, thereby inhibiting the phosphorylation of its downstream signaling components MAPK, PI3K/mTOR, and STAT3 and subsequently inducing apoptosis. Our study clarified that the molecular mechanisms of compound 1a were the same as those of lead compound 1 and that c-MET was involved in the regulatory effects of 1 and 1a on signaling pathways, including the MAPK, PI3K/mTOR, and STAT3 pathways, which is a new antitumor mechanism of 1. This study provides a solid theoretical basis for the development and utilization of 1 in tumor therapy and provides more drug candidates for the treatment of leukemia and a theoretical basis for applying such treatments. Certainly, there are some limitations to this research. For example, the mechanism by which 1 and 1a decrease the mRNA level of c-MET needs to be further explored; this will be addressed in future studies.
3. Materials and Methods
3.1. Cell Lines and Culture
For this study, the HEL cell line was obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA), and the cells were cultured in 1640 medium (Gibco, Grand Island, NYC, New York, NY, USA) supplemented with 100 U/mL penicillin, 0.1 mg/mL streptomycin, 0.25 µg/mL amphotericin B, and 10% heat-inactivated fetal bovine serum, at 37 °C in a humidified atmosphere with 5% CO2.
3.2. Cell Viability Assays
A total of 5 × 103 cells were added to each well of the 96-well plate and treated with 0.1625, 0.3125, 0.625, 1.25, 2.5, and 5 μM test compounds or DMSO (Beijing Solarbio Science & Technology Co., Ltd. Beijing, China) for 48 h. Then, 10 μL of MTT (5 mg/mL, in PBS) (Beijing Solarbio Science & Technology Co., Ltd. Beijing, China) or CCK-8 (Beijing Solarbio Science & Technology Co., Ltd. Beijing, China) was added into each well and further incubated for 4 h. For MTT, the samples were centrifuged at 2000 r/min for 15 min, the supernatant was removed, and 10 μL of DMSO was added to each well. Then, the cells were incubated for 10 min, and the absorbance value was measured at 490 nm using a microplate reader (Bio-Tek, Winooski, VT, USA). For CCK8, after incubation, the absorbance of the plates was measured directly at 450 nm.
3.3. Apoptosis Analysis
HEL cells were incubated in 6-well plates at 4 × 105 per well and after 24 h different concentrations of compounds were added, and the incubation was continued for 6 h. Then, the cells were collected and washed twice with PBS. The cells were stained with reagents from an Annexin V-FITC/PI apoptosis kit (Shanghai Yishan Biotech Co., Ltd. Shanghai, China, AP001). Apoptosis was determined by flow cytometry (ACEA Biosciences, San Diego, CA, USA).
3.4. Hoechst 33258 Staining
HEL cells were incubated in 6-well plates at 4 × 105 cells/well and cultured for 24 h. Then, the cells were incubated in the presence of different concentrations of compounds for 6 h. According to the Hoechst 33258 kit (Beijing Solarbio Science & Technology Co., Ltd., Beijing, China, C0020) instructions, Hoechst 33258 staining solution was added directly to the sample; the sample was incubated for 25 min and then gently washed twice with PBS. Finally, cell morphology was assessed under a fluorescence microscope (Leica, Wetzlar, Hessian, Germany).
3.5. TUNEL Staining
After fixation of the cells with 4% paraformaldehyde, the TUNEL staining procedure was performed according to the instructions of YF® 488 TUNEL Kit (US Everbright® Inc. Suzhou, China, T6013S), the DAPI dye solution used was purchased from Beyotime Institute of Biotechnology (Beyotime Biotech Inc. Shanghai, China, P0131), and the cells were then observed under a fluorescence microscope (Leica, Wetzlar, Hessian, Germany). The number of TUNEL-positive cells and total cells in each field was determined. The apoptosis rate was shown as the average percentage of TUNEL-positive cells among the total cells in the three fields selected for each section.
3.6. Western Blotting
HEL cells were treated with different concentrations of 1, 1a, or 0.1% DMSO for 6 h and collected. After washing twice with PBS, cells were treated with a RIPA lysis buffer (Beyotime Biotech Inc. Shanghai, China) solution containing protease inhibitors to extract the total proteins and then the protein concentration was determined by BCA protein assay (Solarbio Science Technology, Beijing, China, PC0020). The proteins (40–60 μg per lane) were separated using 10% SDS-PAGE (Beyotime Biotech Inc. Shanghai, China), wet-transferred to PVDF membranes, and blotted with primary antibodies specific for GAPDH (Proteintech, Chicago, Illinois, USA, #21800-1-AP), c-MET (Proteintech, Chicago, Illinois, USA, 25869-1-AP), MEK (Proteintech, Chicago, Illinois, USA, 11049-1-AP), p-MEK (Cell Signaling Technology, Inc, Boston, MA, USA, #914), ERK1/2 (Proteintech, 16443-1-AP), p-ERK (Cell Signaling Technology, Inc, Boston, MA, USA, #4370S), STAT3 (Proteintech, Chicago, IL, USA, 10253-2-AP), p-STAT3 (Cell Signaling Technology, Inc, Boston, Massachusetts, USA, #9145), p-PI3K (Affinity, AF3242), PI3K (Affinity, Melbourne, Victoria, Australia, AF5112), mTOR (Proteintech, Chicago, IL, USA, 2065AP), p-mTOR (Cell Signaling Technology, Inc, Boston, Massachusetts, USA, #5536), PARP (Cell Signaling Technology, Inc, Boston, MA, USA, #9532), and cleaved PARP (Cell Signaling Technology, Inc, Boston, MA, USA, #94885) at 4 °C. After 12 h, the membranes were washed three times with TBST, and then HRP-conjugated secondary antibodies were applied for 2 h. The previous cleaning procedure was repeated. Later, color development was performed with Smart-ECL Enhanced reagent (Changzhou Smart-Lifesciences Biotechnology Co., Ltd., Changzhou, China), and band intensities were quantified using Image Lab 5.1 (Bio-Rad Laboratories Inc, Hercules, CA, USA) and normalized to those of GAPDH.
3.7. RNA-Sequencing (RNA-Seq) Experiment and Analysis
After treatments, RNA samples were extracted and sequenced by Metware Biotechnology Co., Ltd. (Wuhan, China), and the cDNA libraries were sequenced on the Illumina sequencing platform by Metware Biotechnology Co., Ltd. (Wuhan, China). Bioinformatics analysis was performed on the Metware Cloud platform (Metware Biotechnology Co., Ltd., Wuhan, China).
3.8. Overexpression of c-MET
The MET (NM_000245) plasmid and its lentivirus were generated by GeneChem (Shanghai GeneChem CO., Ltd., Shanghai, China). The GV513 vector was used to construct a full-length c-MET plasmid and to complete the packaging of the lentivirus with Helper 1.0 and Helper 2.0 (Shanghai GeneChem CO., Ltd., Shanghai, China). Then, transfection of the lentivirus was conducted using HitransG A (Shanghai Genechem CO., Ltd., Shanghai, China), and the negative control virus CON335 (Ubi-MCS-CBh-gcGFP-IRES-puromycin, provided by Shanghai Genechem CO., Ltd., Shanghai, China) was used as a negative control virus. Cells were collected for further experiments 24 h after transfection, following the manufacturer’s recommendations. The sequences are listed in the additional Table S2.
3.9. Real-Time q-PCR
After treatments, total RNA was extracted from cells using the RNA isolation reagent TRIzol (Beijing Solarbio Science & Technology Co., Ltd., Beijing, China) and transcribed into cDNA using Hifair® III 1st Strand cDNA Synthesis SuperMix for q-PCR (gDNA digester plus, Yeasen Biotechnology (Shanghai) Co., Ltd., Shanghai, China). Then, cDNA was used for qRT-PCR analysis with Hieff UNICON® Universal Blue q-PCR SYBR Green Master Mix (Yeasen Biotechnology (Shanghai) Co., Ltd., Shanghai, China), and the reaction mixtures were incubated for 2 min at 95 °C followed by 40 cycles of 10 s at 95 °C and 30 s at 60 °C. The 2−ΔΔCt method was used to calculate relative gene expression, and the mRNA level of the gene of interest was normalized to that of GAPDH. The primers used for the q-PCR were as follows:
c-MET, forward 5′-AGCAATGGGGAGTGTAAAGAGG-3′,
reverse 5′-CCCAGTCTTGTACTCAGCAAC-3′;
GAPDH, forward 5′-CATCAAGAAGGTGGTGAAGCA-3′;
reverse 5′-TCAAAGGTGGAGGAGTGGGT-3′.
3.10. Statistical Analysis
All data were obtained from three independent experiments. Statistical analysis was performed using GraphPad Prism 8 (GraphPad Software, La Jolla, CA, USA). Student’s t test was applied to assess the significance of differences between two groups. The data are displayed as the mean ± SD, and the threshold for significance was set to p < 0.05.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijms24098113/s1.
Author Contributions
X.X. and L.D. contributed equally to this paper. All authors contributed to the study conception and design. X.X.: methodology, data curation, software, writing—original draft preparation. L.D.: methodology, investigation, visualization. Y.T.: investigation, data curation, formal analysis. J.L.: investigation. T.Z.: software. X.H.: formal analysis. Y.F.: resources, validation, supervision. S.M.: conceptualization, resources, supervision, writing, original draft preparation, reviewing and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (U1812403-3, 22067003 and 31760097), the Science and Technology Projects of Guizhou Province (QKH Foundation-ZK (2021) General 516), the Technological Talents in Colleges and Universities of Guizhou Province (Qian Ke He KY (2021) 181), and the Science and Technology Program of Guizhou Province (QKH-JC [2019]1430).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data of RNA-seq from this study were submitted to the NCBI database under SRA, ID: SUB12932460.
Acknowledgments
We would also like to thank the Guizhou Provincial Key Laboratory of Chemistry for Natural Products. We are grateful to Wuhan Metware Biotechnology Co., Ltd. for assisting in the sequencing and bioinformatics analysis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lou, G.; Wang, J.; Hu, J.; Gan, Q.; Peng, C.; Xiong, H.; Huang, Q. Sanguinarine: A Double-Edged Sword of Anticancer and Carcinogenesis and Its Future Application Prospect. Anti-Cancer Agents Med. Chem. 2021, 21, 2100–2110. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.; Guan, G.; Wang, H. The Anticancer Effect of Sanguinarine: A Review. Curr. Pharm. Des. 2018, 24, 2760–2764. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Zhang, N.; Kou, S.; Gao, L.; Peng, B.; Dai, Y.; Zheng, J. Sanguinarine synergistically potentiates aminoglycoside-mediated bacterial killing. Microb. Biotechnol. 2022, 15, 2055–2070. [Google Scholar] [CrossRef] [PubMed]
- Jena, A.B.; Kanungo, N.; Chainy, G.B.N.; Devaraji, V.; Das, S.K.; Dandapat, J. A Computational Insight on the Inhibitory Potential of 8-Hydroxydihydr of Sanguinarine (8-HDS), a Pyridone Containing Analog of Sanguinarine, Against SARS CoV2. Chem Biodivers. 2022, 19, e202200266. [Google Scholar] [CrossRef] [PubMed]
- Niu, X.; Fan, T.; Li, W.; Huang, H. The Anti-inflammatory Effects of Sanguinarine and Its Modulation of in Flammatory Mediators from Peritoneal Macrophages. Eur. J. Pharmacol. 2012, 689, 262–269. [Google Scholar] [CrossRef]
- Khan, A.Q.; Rashid, K.; AlAmodi, A.A.; Agha, M.V.; Akhtar, S.; Hakeem, I.; Raza, S.S.; Uddin, S. Reactive oxygen species (ROS) in cancer pathogenesis and therapy: An update on the role of ROS in anticancer action of benzophenanthridine alkaloids. Biomed. Pharmacother. 2021, 143, 112142. [Google Scholar] [CrossRef]
- Wang, X.; Yang, X.; Wang, J.; Li, L.; Zhang, Y.; Jin, M.; Chen, X.; Sun, C.; Wang, R.; Liu, K. Cardiotoxicity of sanguinarine via regulating apoptosis and MAPK pathways in zebrafish and HL1 cardiomyocytes. Comp. Biochem. Physiol. Part C Toxicol. Pharmacol. 2021, 252, 109228. [Google Scholar] [CrossRef]
- Singh, N.; Sharma, B. Toxicological Effects of Berberine and Sanguinarine. Front. Mol. Biosci. 2018, 5, 21. [Google Scholar] [CrossRef]
- Tang, Y.; Xu, X.; Li, J.; Deng, L.; Mu, S. Synthesis and Antileukemia Activity Evaluation of Benzophenanthridine Alkaloid Derivatives. Molecules 2022, 27, 3934. [Google Scholar] [CrossRef]
- Laines-Hidalgo, J.I.; Muñoz-Sánchez, J.A.; Loza-Müller, L.; Vázquez-Flota, F. An Update of the Sanguinarine and Benzophenanthridine Alkaloids’ Biosynthesis and Their Applications. Molecules 2022, 27, 1378. [Google Scholar] [CrossRef]
- Yu, C.; Li, P.; Wang, Y.-X.; Zhang, K.-G.; Zheng, Z.-C.; Liang, L.-S. Sanguinarine Attenuates Neuropathic Pain by Inhibiting P38 MAPK Activated Neuroinflammation in Rat Model. Drug Des. Dev. Ther. 2020, 14, 4725–4733. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Leng, T.; Zhang, Q.; Nie, X.; Yang, L. Sanguinarine Inhibits Epithelial Ovarian Cancer Development via Regulating Long Non-coding RNA CASC2-EIF4A3 Axis and/or Inhibiting NF-κB Signaling or PI3K/AKT/mTOR Pathway. Biomed. Pharmacother. 2018, 102, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, S.; Achkar, I.W.; Siveen, K.S.; Khan, A.Q.; Ahmed, E.I.; Sahir, F.; Jerobin, J.; Raza, A.; Merhi, M.; Elsabah, H.M.; et al. Sanguinarine Induces Apoptosis Pathway in Multiple Myeloma Cell Lines via Inhibition of the JAK2/STAT3 Signaling. Front Oncol. 2019, 9, 285. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Wang, X.; Deng, J.; Zheng, H.; Liu, W.; Chen, S.; Tian, J.; Wang, F. p53-dependent upregulation of miR-16-2 by sanguinarine induces cell cycle arrest and apoptosis in hepatocellular carcinoma. Cancer Lett. 2019, 459, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Ye, W.; Wang, Y.-D.; Chen, W.-D. HGF/c-Met: A Key Promoter in Liver Regeneration. Front. Pharmacol. 2022, 13, 808855. [Google Scholar] [CrossRef]
- Stefani, C.; Miricescu, D.; Stanescu, I.; Nica, R.I.; Greabu, M.; Totan, A.R.; Jinga, M. (Growth Factors, PI3K/AKT/mTOR and MAPK Signaling Pathways in Colorectal Cancer Pathogenesis: Where Are we Now? Int. J. Mol. Sci. 2021, 22, 10260. [Google Scholar] [CrossRef]
- Blangé, D.; Stroes, C.I.; Derks, S.; Bijlsma, M.F.; van Laarhoven, H.W. Resistance Mechanisms to HER2-targeted Therapy in Aastroesophageal Adenocarcinoma: A Systematic Review. Cancer Treat. Rev. 2022, 108, 102418. [Google Scholar] [CrossRef]
- Uchikawa, E.; Chen, Z.; Xiao, G.-Y.; Zhang, X.; Bai, X.-C. Structural basis of the activation of c-MET receptor. Nat. Commun. 2021, 12, 1–14. [Google Scholar] [CrossRef]
- Damghani, T.; Elyasi, M.; Pirhadi, S.; Haghighijoo, Z.; Ghazi, S. Type II c-Met inhibitors: Molecular insight into crucial interactions for effective inhibition. Mol. Divers. 2021, 26, 1411–1423. [Google Scholar] [CrossRef]
- Wang, H.; Rao, B.; Lou, J.; Li, J.; Liu, Z.; Li, A.; Cui, G.; Ren, Z.; Yu, Z. The Function of the HGF/c-Met Axis in Hepatocellular Carcinoma. Front. Cell Dev. Biol. 2020, 8, 55. [Google Scholar] [CrossRef]
- Ci, T.; Zhang, W.; Qiao, Y.; Li, H.; Zang, J.; Li, H.; Feng, N.; Gu, Z. Delivery strategies in treatments of leukemia. Chem. Soc. Rev. 2022, 51, 2121–2144. [Google Scholar] [CrossRef] [PubMed]
- Roloff, G.W.; Odenike, O.; Bajel, A.; Wei, A.H.; Foley, N.; Uy, G.L. Contemporary Approach to Acute Myeloid Leukemia Therapy in 2022. Am. Soc. Clin. Oncol. Educ. Book 2022, 568–583. [Google Scholar] [CrossRef]
- Cao, X.; Fu, M.; Bi, R.; Zheng, X.; Fu, B.; Tian, S.; Liu, C.; Li, Q.; Liu, J. Cadmium induced BEAS-2B cells apoptosis and mitochondria damage via MAPK signaling pathway. Chemosphere 2020, 263, 128346. [Google Scholar] [CrossRef]
- Feng, H.; Hu, L.; Zhu, H.; Tao, L.; Wu, L.; Zhao, Q.; Gao, Y.; Gong, Q.; Mao, F.; Li, X.; et al. Repurposing antimycotic ciclopirox olamine as a promising anti-ischemic stroke agent. Acta Pharm. Sin. B 2019, 10, 434–446. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.L.; Zhang, Y.J.; Lei, J.; Li, S.Q.; He, L.J.; Tang, D.Y.; Xu, C.; Zhang, L.T.; Wen, J.; Lin, H.K.; et al. Discovery of Fused Benzimidazole-imidazole Autophagic Flux Inhibitors for Treatment of Triple-negative Treast Cancer. Eur. J. Med. Chem. 2022, 240, 114565. [Google Scholar] [CrossRef] [PubMed]
- Zaky, M.Y.; Liu, X.; Wang, T.; Wang, S.; Liu, F.; Wang, D.; Wu, Y.; Zhang, Y.; Guo, D.; Sun, Q.; et al. Dynasore potentiates c-Met inhibitors against hepatocellular carcinoma through destabilizing c-Met. Arch. Biochem. Biophys. 2020, 680, 108239. [Google Scholar] [CrossRef]
- Rose, M.; Burgess, J.T.; O’byrne, K.; Richard, D.J.; Bolderson, E. PARP Inhibitors: Clinical Relevance, Mechanisms of Action and Tumor Resistance. Front. Cell Dev. Biol. 2020, 8, 564601. [Google Scholar] [CrossRef]
- Wang, C.; Liu, H.; Yang, M.; Bai, Y.; Ren, H.; Zou, Y.; Yao, Z.; Zhang, B.; Li, Y. RNA-Seq Based Transcriptome Analysis of Endothelial Differentiation of Bone Marrow Mesenchymal Stem Cells. Eur. J. Vasc. Endovasc. Surg. 2019, 59, 834–842. [Google Scholar] [CrossRef]
- Lu, S.; Zhu, N.; Guo, W.; Wang, X.; Li, K.; Yan, J.; Jiang, C.; Han, S.; Xiang, H.; Xiaohan, W.; et al. RNA-Seq revealed a circular RNA-microRNA-mRNA Regulatory Network in Hantaan Virus Infection. Front. Cell Infect. Microbiol. 2022, 10, 97. [Google Scholar] [CrossRef]
- Fang, J.Y.; Richardson, B.C. The MAPK signalling pathways and colorectal cancer. Lancet Oncol. 2005, 6, 322–327. [Google Scholar] [CrossRef]
- Raj, S.; Kesari, K.K.; Kumar, A.; Rathi, B.; Sharma, A.; Gupta, P.K.; Jha, S.K.; Jha, N.K.; Slama, P.; Roychoudhury, S.; et al. Molecular mechanism(s) of regulation(s) of c-MET/HGF signaling in head and neck cancer. Mol. Cancer 2022, 21, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Besser, D.; Bardelli, A.; Didichenko, S.; Thelen, M.; Comoglio, P.M.; Ponzetto, C.; Nagamine, Y. Regulation of the urokinase-type plasminogen activator gene by the oncogene Tpr-Met involves GRB2. Oncogene 1997, 14, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Inagaki, Y.; Song, P.; Qu, X.; Kokudo, N.; Tang, W. Targeting c-Met as a promising strategy for the treatment of hepatocellular carcinoma. Pharmacol. Res. 2012, 65, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Pons, E.; Uphoff, C.; Drexler, H. Expression of hepatocyte growth factor and its receptor c-met in human leukemia-lymphoma cell lines. Leuk. Res. 1998, 22, 797–804. [Google Scholar] [CrossRef]
- Paiva, R.S.; Gomes, I.; Casimiro, S.; Fernandes, I.; Costa, L. c-Met expression in renal cell carcinoma with bone metastases. J. Bone Oncol. 2020, 25, 100315. [Google Scholar] [CrossRef]
- Hu, Y.; Gong, C.; Li, Z.; Liu, J.; Chen, Y.; Huang, Y.; Luo, Q.; Wang, S.; Hou, Y.; Yang, S.; et al. Demethylase ALKBH5 suppresses invasion of gastric cancer via PKMYT1 m6A modification. Mol. Cancer 2022, 21, 1–15. [Google Scholar] [CrossRef]
- Sheng, W.; Guo, W.; Lu, F.; Liu, H.; Xia, R.; Dong, F. Upregulation of Linc00284 Promotes Lung Cancer Progression by Regulating the miR-205-3p/c-Met Axis. Front. Genet. 2021, 12, 694571. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).