A Systematic Review on the Risk Modulators of Myocardial Infarction in the “Young”—Implications of Lipoprotein (a)
Abstract
1. Introduction
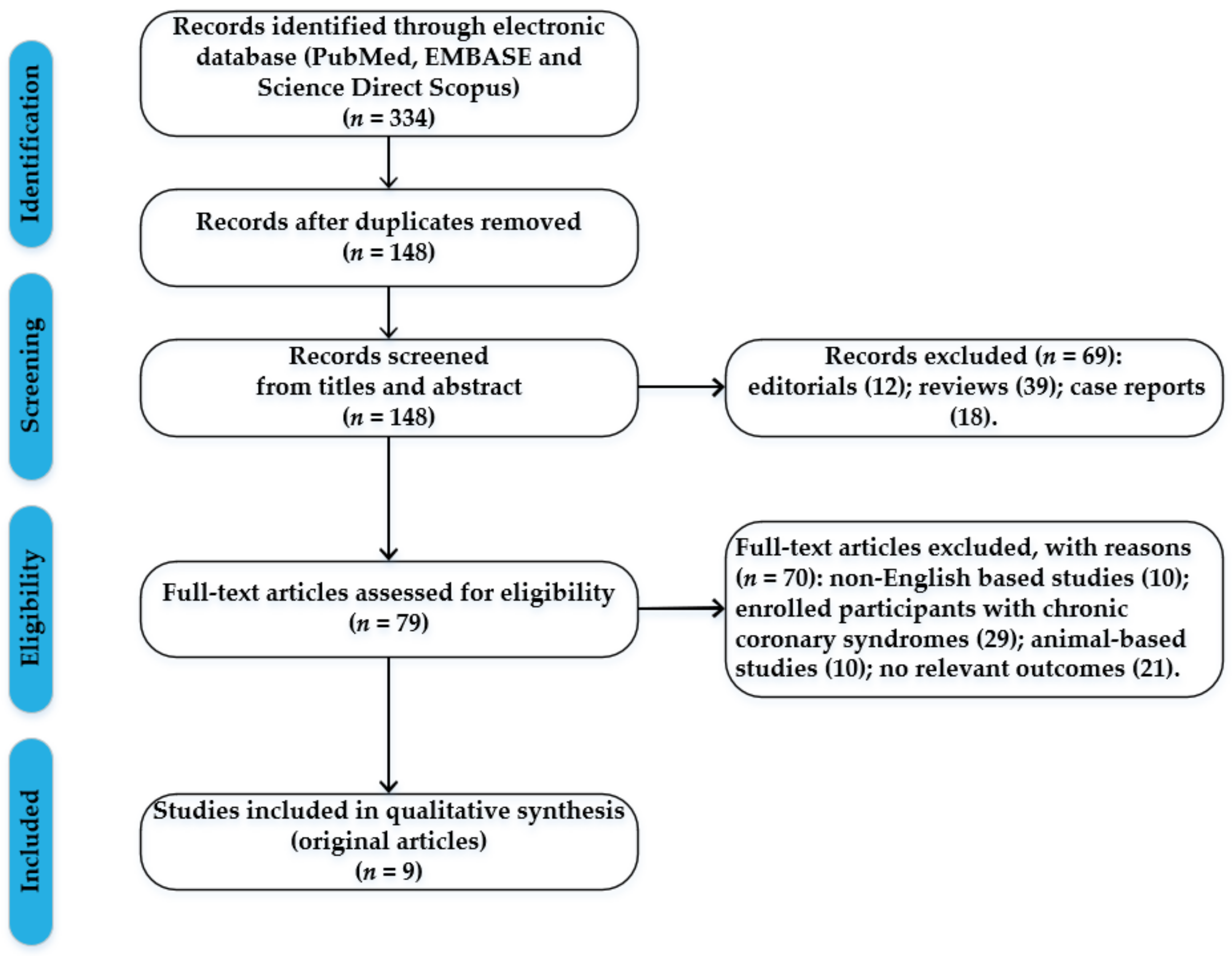
2. Methods
3. Results and Discussion
3.1. Myocardial Infarction Related to Traditional Cardiovascular Risk Factors in Young Patients
3.1.1. Arterial Hypertension
3.1.2. Smoking
3.1.3. Diabetes Mellitus
3.1.4. Obesity
3.1.5. Dyslipidaemia
3.1.6. Gender
3.1.7. Family History
3.1.8. Psychosocial and Environmental Factors
3.2. Lipoprotein (a)
3.2.1. How, When, and What to Look For?
3.2.2. Implications of Lp(a) in Young Patients
3.2.3. Therapeutic Approaches
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kronenberg, F.; Mora, S.; Stroes, E.S.G.; Ference, B.A.; Arsenault, B.J.; Berglund, L.; Dweck, M.R.; Koschinsky, M.; Lambert, G.; Mach, F.; et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: A European Atherosclerosis Society consensus statement. Eur. Heart J. 2022, 43, 3925–3946. [Google Scholar] [CrossRef]
- Writing Committee; Lloyd-Jones, D.M.; Morris, P.B.; Ballantyne, C.M.; Birtcher, K.K.; Covington, A.M.; DePalma, S.M.; Minissian, M.B.; Orringer, C.E.; Smith, S.C., Jr.; et al. 2022 ACC Expert Consensus Decision Pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: A report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2022, 80, 1366–1418. [Google Scholar]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef]
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.K.B.M.; Alkatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.E.A.H.; Alzaabi, M.E.H.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [PubMed]
- Aggarwal, A.; Aggarwal, S.; Goel, A.; Sharma, V.; Dwivedi, S. A retrospective case-control study of modifiable risk factors and cutaneous markers in Indian patients with young coronary artery disease. JRSM Cardiovasc. Dis. 2012, 1, cvd.2012.012010. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, K.; Khare, A.; Shetty, S. Fasting plasma homocysteine levels are increased in young patients with acute myocardial infarction from Western India. Indian Heart J. 2007, 59, 242–245. [Google Scholar]
- Awad-Elkarim, A.A.; Bagger, J.P.; Albers, C.J.; Skinner, J.S.; Adams, P.C.; Hall, R.J. A prospective study of long-term prognosis in young myocardial infarction survivors: The prognostic value of angiography and exercise testing. Heart 2003, 89, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Afshar, M.; Rong, J.; Zhan, Y.; Chen, H.Y.; Engert, J.C.; Sniderman, A.D.; Larson, M.G.; Vasan, R.S.; Thanassoulis, G. Risks of incident cardiovascular disease associated with concomitant elevations in Lipoprotein(a) and low-density lipoprotein cholesterol-the Framingham Heart Study. J. Am. Heart Assoc. 2020, 9, e014711. [Google Scholar] [CrossRef] [PubMed]
- Enas, E.A.; Varkey, B.; Dharmarajan, T.; Pare, G.; Bahl, V.K. Lipoprotein(a): An underrecognized genetic risk factor for malignant coronary artery disease in young Indians. Indian Heart J. 2019, 71, 184–198. [Google Scholar] [CrossRef]
- Chi, G.C.; Kanter, M.H.; Li, B.H.; Qian, L.; Reading, S.R.; Harrison, T.N.; Jacobsen, S.J.; Scott, R.D.; Cavendish, J.J.; Lawrence, J.; et al. Trends in acute myocardial infarction by race and ethnicity. J. Am. Heart Assoc. 2020, 9, e013542. [Google Scholar] [CrossRef]
- Gwon, J.G.; Choi, J.; Kim, S.H.; Kim, S.H.; Ryu, J.J.; Cho, D.H.; Song, I.S. Risk of acute and chronic coronary syndrome in a population with periodontitis: A cohort study. Oral Dis. 2022, 28 (Suppl. S2), 2522–2529. [Google Scholar] [CrossRef] [PubMed]
- Choudry, F.A.; Hamshere, S.M.; Rathod, K.S.; Akhtar, M.M.; Archbold, R.A.; Guttmann, O.P.; Woldman, S.; Jain, A.K.; Knight, C.J.; Baumbach, A.; et al. High thrombus burden in patients with COVID-19 presenting with ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2020, 76, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Konstantinou, K.; Tsioufis, C.; Koumelli, A.; Mantzouranis, M.; Kasiakogias, A.; Doumas, M.; Tousoulis, D. Hypertension and patients with acute coronary syndrome: Putting blood pressure levels into perspective. J. Clin. Hypertens 2019, 21, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Alexander, T.; Kumbhani, D.J.; Subban, V.; Sundar, H.; Nallamothu, B.K.; Mullasari, A.S. Acute ST-Elevation Myocardial Infarction in the Young Compared With Older Patients in the Tamil Nadu STEMI Program. Heart Lung Circ. 2021, 30, 1876–1882. [Google Scholar] [CrossRef]
- Yagel, O.; Shadafny, N.; Eliaz, R.; Dagan, G.; Leibowitz, D.; Tahiroglu, I.; Planer, D.; Amir, O.; Greener, G.E.; Alcalai, R. Long-Term Prognosis in Young Patients with Acute Coronary Syndrome Treated with Percutaneous Coronary Intervention. Vasc. Health Risk Manag. 2021, 17, 53–159. [Google Scholar] [CrossRef]
- Yanase, T.; Sakakura, K.; Taniguchi, Y.; Yamamoto, K.; Tsukui, T.; Seguchi, M.; Wada, H.; Momomura, S.-I.; Fujita, H. Comparison of Clinical Characteristics of Acute Myocardial Infarction Between Young (< 55 Years) and Older (55 to < 70 Years) Patients. Int. Heart J. 2021, 62, 33–41. [Google Scholar]
- Muhammad, A.S.; Ashraf, T.; Mir, A.; Alishan, S.; Farooq, F.; Ammar, A.; Karim, M.; Rizvi, S.N.H.; Saghir, T.; Sial, J.A.; et al. Comparative assessment of clinical profile and outcomes after primary percutaneous coronary intervention in young patients with single vs multivessel disease. World J. Cardiol. 2020, 12, 136–143. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, J.; Ma, Z.; Xu, Z. Clinical Study on Characteristics and Risk Factors of Coronary Artery Lesions in Young Patients with Acute Myocardial Infarction. Evid. Based Complement Altern. Med. 2021, 2021, 5716410. [Google Scholar] [CrossRef]
- Singh, B.; Singh, A.; Goyal, A.; Chhabra, S.; Tandon, R.; Aslam, N.; Mohan, B.; Wander, G.S. The Prevalence, Clinical Spectrum and the Long Term Outcome of ST-segment Elevation Myocardial Infarction in Young—A Prospective Observational Study. Cardiovasc. Revasc. Med. 2019, 20, 387–391. [Google Scholar] [CrossRef]
- Noaman, S.; Dinh, D.; Reid, C.M.; Brennan, A.L.; Clark, D.; Shaw, J.; Freeman, M.; Sebastian, M.; Oqueli, E.; Ajani, A.; et al. Comparison of Outcomes of Coronary Artery Disease Treated by Percutaneous Coronary Intervention in 3 Different Age Groups (<45, 46-65, and >65 Years). Am. J. Cardiol. 2021, 152, 19–26. [Google Scholar]
- Yandrapalli, S.; Nabors, C.; Goyal, A.; Aronow, W.S.; Frishman, W.H. Modifiable Risk Factors in Young Adults with First Myocardial Infarction. J. Am. Coll Cardiol. 2019, 73, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Abed, M.A.; Eshah, N.F.; Moser, D.K. Risk profile of myocardial infarction in young versus older adults. Heart Lung 2018, 47, 226–230. [Google Scholar] [CrossRef]
- Biery, D.W.; Berman, A.N.; Singh, A.; Divakaran, S.; DeFilippis, E.M.; Collins, B.L.; Gupta, A.; Fatima, A.; Qamar, A.; Klein, J.; et al. Association of Smoking Cessation and Survival Among Young Adults With Myocardial Infarction in the Partners YOUNG-MI Registry. JAMA Netw. Open. 2020, 3, e209649. [Google Scholar]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed]
- Winter, M.-P.; Blessberger, H.; Alimohammadi, A.; Pavo, N.; Huber, K.; Wojta, J.; Lang, I.M.; Wiesbauer, F.; Goliasch, G. Long-term outcome and risk assessment in premature acute myocardial infarction: A 10-year follow-up study. Int. J. Cardiol. 2017, 240, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Divakaran, S.; Singh, A.; Biery, D.; Yang, J.; DeFilippis, E.M.; Collins, B.L.; Ramsis, M.; Qamar, A.; Hainer, J.; Klein, J.; et al. Diabetes Is Associated with Worse Long-term Outcomes in Young Adults after Myocardial Infarction: The Partners YOUNG-MI Registry. Diabetes Care 2020, 43, 1843–1850. [Google Scholar] [CrossRef]
- Rawshani, A.; Sattar, N.; Franzén, S.; Rawshani, A.; Hattersley, A.T.; Svensson, A.M.; Eliasson, B.; Gudbjörnsdottir, S. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: A nationwide, register-based cohort study. Lancet 2018, 392, 477–486. [Google Scholar] [CrossRef]
- Bęćkowski, M.; Gierlotka, M.; Gąsior, M.; Poloński, L.; Zdrojewski, T.; Dąbrowski, R.; Karwowski, J.; Kowalik, I.; Drygas, W.; Szwed, H. Risk factors predisposing to acute coronary syndromes in young women ≤45 years of age. Int. J. Cardiol. 2018, 264, 165–169. [Google Scholar] [CrossRef]
- Zhang, M.; Zuo, H.J.; Yang, H.X.; Nan, N.; Song, X.T. Trends in conventional cardiovascular risk factors and myocardial infarction subtypes among young Chinese men with a first acute myocardial infarction. Clin. Cardiol. 2022, 45, 129–135. [Google Scholar]
- Krittanawong, C.; Luo, Y.; Mahtta, D.; Narasimhan, B.; Wang, Z.; Jneid, H.; Tamis-Holland, J.E.; Mahboob, A.; Baber, U.; Mehran, R.; et al. Non-traditional risk factors and the risk of myocardial infarction in the young in the US population-based cohort. Int. J. Cardiol. Heart Vasc. 2020, 30, 100634. [Google Scholar] [CrossRef]
- Zasada, W.; Bobrowska, B.; Plens, K.; Dziewierz, A.; Siudak, Z.; Surdacki, A.; Dudek, D.; Bartuś, S. Acute myocardial infarction in young patients. Kardiol. Pol. 2021, 79, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, S.; Coşansu, K. Prognostic Factors and Outcomes in Young Patients with Presented of Different Types Acute Coronary Syndrome. Angiology 2020, 71, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Jortveit, J.; Pripp, A.H.; Langørgen, J.; Halvorsen, S. Incidence, risk factors and outcome of young patients with myocardial infarction. Heart 2020, 106, 1420–1426. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Itoh, T.; Fusazaki, T.; Matsui, H.; Sugawara, S.; Ogino, Y.; Endo, H.; Kobayashi, K.; Nakamura, M. Low-density Lipoprotein Cholesterol/High-density Lipoprotein Cholesterol Ratio as Predictor of First Acute Myocardial Infarction and Major Adverse Cardiovascular Event after Intervention in Young Males. Chin. Med. J. 2018, 131, 2239–2241. [Google Scholar]
- Arsenescu, C.; Anghel, L. Long term assessment of the biological profile in patients with acute myocardial infarction and left bundle branch block? Rev. Chim. 2017, 68, 2682–2684. [Google Scholar]
- Ivert, T.; Malmström, H.; Hammar, N.; Carlsson, A.C.; Wändell, P.E.; Holzmann, M.J.; Jungner, I.; Ärnlöv, J.; Walldius, G. Cardiovascular events in patients under age fifty with early findings of elevated lipid and glucose levels—The AMORIS study. PLoS ONE 2018, 13, e0201972. [Google Scholar] [CrossRef] [PubMed]
- Kheiri, B.; Simpson, T.F.; Osman, M.; Balla, S.; Rahmouni, H.; Mehta, A.; Pokharel, Y.; Nasir, K.; Fazio, S.; Shapiro, M.D. Familial hypercholesterolaemia related admission for acute coronary syndrome in the United States: Incidence, predictors, and outcomes. J. Clin. Lipidol. 2021, 15, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Ricci, B.; Cenko, E.; Vasiljevic, Z.; Stankovic, G.; Kedev, S.; Kalpak, O.; Vavlukis, M.; Zdravkovic, M.; Hinic, S.; Milicic, D.; et al. Acute Coronary Syndrome: The Risk to Young Women. J. Am. Heart Assoc. 2017, 6, e007519. [Google Scholar] [CrossRef]
- Shehab, A.; Bhagavathula, A.S.; Alhabib, K.F.; Ullah, A.; Suwaidi, J.A.; Almahmeed, W.; AlFaleh, H.; Zubaid, M. Age-Related Sex Differences in Clinical Presentation, Management, and Outcomes in ST-Segment-Elevation Myocardial Infarction: Pooled Analysis of 15 532 Patients from 7 Arabian Gulf Registries. J. Am. Heart Assoc. 2020, 9, e013880. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Ni, L.; Liu, K.; Gao, X.; Yang, J.; Zhang, X.; Ye, Y.; Dong, Q.; Fu, R.; Sun, H.; et al. Clinical Characteristics, Prognosis, and Gender Disparities in Young Patients with Acute Myocardial Infarction. Front. Cardiovasc. Med. 2021, 8, 720378. [Google Scholar] [CrossRef]
- Bandyopadhyay, D.; Chakraborty, S.; Amgai, B.; Patel, N.; Hajra, A.; Heise, L.; Sud, K.; Ghosh, R.K.; Herzog, E.; Aronow, W.S.; et al. Acute myocardial infarction in the young—National Trend Analysis with gender-based difference in outcomes. Int. J. Cardiol. 2020, 301, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Stouffer, G.A.; Kucharska-Newton, A.M.; Qamar, A.; Vaduganathan, M.; Pandey, A.; Porterfield, D.; Blankstein, R.; Rosamond, W.D.; Bhatt, D.L.; et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation 2019, 139, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, C.; Valsdottir, L.; Wasfy, J.H.; Strom, J.B.; Secemsky, E.A.; Wang, Y.; Yeh, R.W. Comparison of 30-Day Readmission Rates After Hospitalization for Acute Myocardial Infarction in Men Versus Women. Am. J. Cardiol. 2017, 120, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Preisler, Y.; Ziv-Baran, T.; Chorin, E.; Margolis, G.; Khoury, S.; Shacham, Y. Family history of coronary artery disease and adverse clinical outcomes in patients suffering from acute ST-segment elevation myocardial infarction. Coron Artery Dis. 2018, 29, 657–662. [Google Scholar] [CrossRef]
- Si, J.H.; Meng, R.R.; Yu, C.Q.; Guo, Y.; Bian, Z.; Tan, Y.L.; Pei, P.; Chen, J.S.; Chen, Z.M.; Lyu, J.; et al. Family history and risk of coronary heart disease. Zhonghua Liu Xing Bing Xue Za Zhi 2018, 39, 173–178. (In Chinese) [Google Scholar]
- Chacko, M.; Sarma, P.S.; Harikrishnan, S.; Zachariah, G.; Jeemon, P. Family history of cardiovascular disease and risk of premature coronary heart disease: A matched case-control study. Wellcome Open Res. 2020, 5, 70. [Google Scholar] [CrossRef]
- Alfaddagh, A.; Khraishah, H.; Rashed, W.; Sharma, G.; Blumenthal, R.S.; Zubaid, M. Clinical characteristics and outcomes of young adults with first myocardial infarction: Results from Gulf COAST. Int. J. Cardiol. Heart Vasc. 2020, 31, 100680. [Google Scholar] [CrossRef]
- Al-Shahrani, M.S.; Katbi, F.A.; Al-Sharydah, A.M.; AlShahrani, S.D.; Alghamdi, T.M.; Al-Sharidah, M.A. Differences in Clinical Nature and Outcome among Young Patients Suffering from an Acute Coronary Syndrome. J. Blood Med. 2021, 12, 1011–1017. [Google Scholar] [CrossRef]
- Levi, A.; Chezar-Azerrad, C.; Hasdai, D.; Beigel, R.; Gottlieb, S.; Eisen, A.; Shlomo, N.; Goldenberg, I.; Landes, U.; Kornowski, R.; et al. Impact of Self-Reported Family History of Premature Cardiovascular Disease on the Outcomes of Patients Hospitalized for Acute Coronary Syndrome (from the Acute Coronary Syndrome Israel Survey [ACSIS] 2000 to 2013). Am. J. Cardiol. 2018, 122, 917–921. [Google Scholar] [CrossRef]
- Waller, C.; Bauersachs, J.; Hoppmann, U.; Höch, J.; Krause, S.; Szabo, F.; Engler, H.; Rottler, E.; Herrmann-Lingen, C.; Gündel, H. Blunted Cortisol Stress Response and Depression-Induced Hypocortisolism Is Related to Inflammation in Patients with CAD. J. Am. Coll. Cardiol. 2016, 67, 1124–1126. [Google Scholar] [CrossRef]
- Valtorta, N.K.; Kanaan, M.; Gilbody, S.; Ronzi, S.; Hanratty, B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart 2016, 102, 1009–1016. [Google Scholar] [CrossRef] [PubMed]
- Xia, N.; Li, H. Loneliness, Social Isolation, and Cardiovascular Health. Antioxid. Redox Signal 2018, 28, 837–851. [Google Scholar] [CrossRef] [PubMed]
- Ladwig, K.H.; Fang, X.; Wolf, K.; Hoschar, S.; Albarqouni, L.; Ronel, J.; Meinertz, T.; Spieler, D.; Laugwitz, K.L.; Schunkert, H. Comparison of Delay Times Between Symptom Onset of an Acute ST-elevation Myocardial Infarction and Hospital Arrival in Men and Women <65 Years Versus ≥65 Years of Age: Findings From the Multicenter Munich Examination of Delay in Patients Experiencing Acute Myocardial Infarction (MEDEA) Study. Am. J. Cardiol. 2017, 120, 2128–2134. [Google Scholar]
- Wahid, A.; Manek, N.; Nichols, M.; Kelly, P.; Foster, C.; Webster, P.; Kaur, A.; Smith, C.F.; Wilkins, E.; Rayner, M.; et al. Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2016, 5, e002495. [Google Scholar] [CrossRef] [PubMed]
- Grigorescu, E.D.; Lăcătușu, C.M.; Floria, M.; Cazac, G.D.; Onofriescu, A.; Ceasovschih, A.; Crețu, I.; Mihai, B.M.; Șorodoc, L. Association of inflammatory and metabolic biomarkers with mitral annular calcification in type 2 diabetes patients. J. Pers. Med. 2022, 12, 1484. [Google Scholar] [CrossRef] [PubMed]
- Tersalvi, G.; Biasco, L.; Radovanovic, D.; Rickli, H.; Roffi, M.; Eberli, F.; Moccetti, M.; Jeger, R.; Moccetti, T.; Erne, P.; et al. Heavy drinking habits are associated with worse in-hospital outcomes in patients with acute coronary syndrome: An insight from the AMIS Plus registry. Cardiology 2020, 145, 757–765. [Google Scholar] [CrossRef]
- Alkhawam, H.; Fabisevich, M.M.; Sogomonian, R.; Lieber, J.; Madanieh, R.; Vittorio, T.; El-Hunjul, M. The role of alcohol abuse and tobacco use in the incidence of early acute coronay syndrome. J. Investig. Med. 2016, 64, 922–923. [Google Scholar] [CrossRef]
- Erqou, S.; Kaptoge, S.; Perry, P.L.; Emerging Risk Factors Collaboration. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA 2009, 302, 412–423. [Google Scholar]
- Finneran, P.; Pampana, A.; Khetarpal, S.A.; Trinder, M.; Patel, A.P.; Paruchuri, K.; Aragam, K.; Peloso, G.M.; Natarajan, P. Lipoprotein(a) and Coronary Artery Disease Risk Without a Family History of Heart Disease. J. Am. Heart Assoc. 2021, 10, e017470. [Google Scholar] [CrossRef]
- Paré, G.; Çaku, A.; McQueen, M.; Anand, S.S.; Enas, E.; Clarke, R.; Boffa, M.B.; Koschinsky, M.; Wang, X.; Yusuf, S.; et al. Lipoprotein(a) Levels and the Risk of Myocardial Infarction among 7 Ethnic Groups. Circulation 2019, 139, 1472–1482. [Google Scholar] [CrossRef]
- Virani, S.S.; Brautbar, A.; Davis, B.C.; Nambi, V.; Hoogeveen, R.C.; Sharrett, A.R.; Coresh, J.; Mosley, T.H.; Morrisett, J.D.; Catellier, D.J.; et al. Associations between lipoprotein (a) levels and cardiovascular outcomes in black and white subjects: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2012, 125, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.P.; Wang, M.; Pirruccello, J.P.; Ellinor, P.T.; Ng, K.; Kathiresan, S.; Khera, A.V. Lp(a) (Lipoprotein[a]) Concentrations and Incident Atherosclerotic Cardiovascular Disease: New Insights from a Large National Biobank. Arter. Thromb. Vasc. Biol. 2021, 41, 465–474. [Google Scholar] [CrossRef]
- Anghel, L.; Prisacariu, C.; Arsenescu, C. Is there a sex difference of cardiovascular risk factors in patients with acute myocardial infarction? Rev. Chim. 2018, 69, 255–258. [Google Scholar] [CrossRef]
- Varvel, S.; McConnell, J.P.; Tsimikas, S. Prevalence of Elevated Lp(a) Mass Levels and Patient Thresholds in 532 359 Patients in the United States. Arter. Thromb. Vasc. Biol. 2016, 36, 2239–2245. [Google Scholar] [CrossRef] [PubMed]
- Ugovšek, S.; Šebeštjen, M. Lipoprotein(a)-The Crossroads of Atherosclerosis, Atherothrombosis and Inflammation. Biomolecules 2021, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Enas, E.A.; Varkey, B.; Dharmarajan, T.S.; Pare, G.; Bahl, V.K. Lipoprotein(a): An independent, genetic, and causal factor for cardiovascular disease and acute myocardial infarction. Indian Heart J. 2019, 71, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Korneva, V.; Kuznetsova, T.; Julius, U. Analysis of lipid metabolism and its impact on the risk of ischaemic heart disease in patients with definite familial hypercholesterolaemia. Atheroscler. Suppl. 2017, 30, 56–62. [Google Scholar] [CrossRef]
- Kronenberg, F.; Utermann, G. Lipoprotein(a): Resurrected by genetics. J. Intern. Med. 2013, 273, 6–30. [Google Scholar] [CrossRef]
- Enkhmaa, B.; Petersen, K.S.; Kris-Etherton, P.M.; Berglund, L. Diet and Lp(a): Does Dietary Change Modify Residual Cardiovascular Risk Conferred by Lp(a)? Nutrients 2020, 12, 2024. [Google Scholar] [CrossRef]
- Kronenberg, F. Causes and consequences of lipoprotein (a) abnormalities in kidney disease. Clin. Exp. Nephrol. 2014, 18, 234–237. [Google Scholar] [CrossRef]
- O’Donoghue, M.L.; Morrow, D.A.; Tsimikas, S.; Sloan, S.; Ren, A.F.; Hoffman, E.B.; Desai, N.R.; Solomon, S.D.; Domanski, M.; Arai, K.; et al. Lipoprotein(a) for risk assessment in patients with established coronary artery disease. J. Am. Coll. Cardiol. 2014, 63, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Madsen, C.M.; Kamstrup, P.R.; Langsted, A.; Varbo, A.; Nordestgaard, B.G. Lipoprotein(a)-Lowering by 50 mg/dL (105 nmol/L) May Be Needed to Reduce Cardiovascular Disease 20% in Secondary Prevention: A Population-Based Study. Arter. Thromb. Vasc. Biol. 2020, 40, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Albers, J.J.; Slee, A.; O’Brien, K.D.; Robinson, J.G.; Kashyap, M.L.; Kwiterovich, P.O.; Xu, P.; Marcovina, S.M. Relationship of apolipoproteins A-1 and B, and lipoprotein (a) to cardiovascular outcomes: The AIM-HIGH trial (Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglyceride and Impact on Global Health Outcomes). J. Am. Coll. Cardiol. 2013, 62, 1575–1579. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T.J.; Grégoire, J.; Pearson, G.J.; Barry, A.R.; Couture, P.; Dawes, M.; Francis, G.A.; Genest, J., Jr.; Grover, S.; Gupta, M.; et al. 2021 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in Adults. Can. J. Cardiol. 2021, 37, 1129–1150. [Google Scholar]
- Rhainds, D.; Brodeur, M.R.; Tardif, J.C. Lipoprotein (a): When to Measure and How to Treat? Curr. Atheroscler. Rep. 2021, 23, 51. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Cegla, J.; France, M.; Marcovina, S.M.; Neely, R.D.G. Lp(a): When and how to measure it. Ann. Clin. Biochem. 2021, 58, 16–21. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; De Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, 3168–3209. [Google Scholar] [CrossRef]
- Wilson, D.P.; Jacobson, T.A.; Jones, P.H.; Koschinsky, M.L.; McNeal, C.J.; Nordestgaard, B.G.; Orringer, C.E. Use of Lipoprotein(a) in clinical practice: A biomarker whose time has come. A scientific statement from the National Lipid Association. J. Clin. Lipidol. 2019, 13, 374–392. [Google Scholar] [CrossRef]
- Anderson, T.J.; Grégoire, J.; Pearson, G.J.; Barry, A.R.; Couture, P.; Dawes, M.; Francis, G.A.; Genest, J., Jr.; Grover, S.; Gupta, M.; et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can. J. Cardiol. 2016, 32, 1263–1282. [Google Scholar] [CrossRef]
- Nave, A.H.; Lange, K.S.; Leonards, C.O.; Siegerink, B.; Doehner, W.; Landmesser, U.; Steinhagen-Thiessen, E.; Endres, M.; Ebinger, M. Lipoprotein (a) as a risk factor for ischaemic stroke: A meta-analysis. Atherosclerosis 2015, 242, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Rallidis, L.S.; Triantafyllis, A.S.; Tsirebolos, G.; Katsaras, D.; Rallidi, M.; Moutsatsou, P.; Lekakis, J. Prevalence of heterozygous familial hypercholesterolaemia and combined hyperlipidaemia phenotype in very young survivors of myocardial infarction and their association with the severity of atheromatous burden. J. Clin. Lipidol. 2019, 13, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Hanif, S.; Akhtar, B.; Afzal, M.N. Serum Lipoprotein (a) levels in acute coronary syndrome; Comparison of younger and elderly patients with healthy controls. Pak. J. Med. Sci. 2019, 35, 1718–1723. [Google Scholar] [CrossRef] [PubMed]
- Jubran, A.; Zetser, A.; Zafrir, B. Lipoprotein(a) screening in young and middle-aged patients presenting with acute coronary syndrome. Cardiol. J. 2019, 26, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Luna, M.; Rodriguez Cordoba, A.; Rodriguez Capitan, J.; Martinez Carmona, J.D.; Diaz Exposito, A.; Marquez Camas, P.; Garcia Rodriguez, L.; Palma Marti, L.; Angullo Gomez, M.; Doncel Abad, M.V.; et al. Analysis of LpA levels in young patients after ACS: Getting to know less famous risk factors. Eur. Heart J. 2021, 42, ehab724.2478. [Google Scholar] [CrossRef]
- Rallidis, L.S.; Pavlakis, G.; Foscolou, A.; Kotakos, C.; Katsimardos, A.; Drosatos, A.; Zolindaki, M.; Panagiotakos, D.B. High levels of lipoprotein (a) and premature acute coronary syndrome. Atherosclerosis 2018, 269, 29–34. [Google Scholar] [CrossRef]
- Schatz, U.; Fischer, S.; Müller, G.; Tselmin, S.; Birkenfeld, A.L.; Julius, U.; März, W.; Bornstein, S.R. Cardiovascular risk factors in patients with premature cardiovascular events attending the University of Dresden Lipid Clinic. Atheroscler. Suppl. 2019, 40, 94–99. [Google Scholar] [CrossRef]
- Reyes-Soffer, G.; Ginsberg, H.N.; Berglund, L.; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Peripheral Vascular Disease. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arter. Thromb. Vasc. Biol. 2022, 42, e48–e60. [Google Scholar] [CrossRef]
- Bittner, V.A.; Szarek, M.; Aylward, P.E.; Bhatt, D.L.; Diaz, R.; Edelberg, J.M.; Fras, Z.; Goodman, S.G.; Halvorsen, S.; Hanotin, C.; et al. Effect of Alirocumab on Lipoprotein(a) and Cardiovascular Risk After Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2020, 75, 133–144. [Google Scholar] [CrossRef]
- de Boer, L.M.; Oorthuys, A.O.; Wiegman, A.; Langendam, M.W.; Kroon, J.; Spijker, R.; Zwinderman, A.H.; Hutten, B.A. Statin therapy and lipoprotein (a) levels: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2022, 29, 779–792. [Google Scholar] [CrossRef] [PubMed]
- Tsimikas, S.; Karwatowska-Prokopczuk, E.; Gouni-Berthold, I.; Tardif, J.C.; Baum, S.J.; Steinhagen-Thiessen, E.; Shapiro, M.D.; Stroes, E.S.; Moriarty, P.M.; Nordestgaard, B.G.; et al. Lipoprotein(a) Reduction in Persons with Cardiovascular Disease. N. Engl. J. Med. 2020, 382, 244–255. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, M.L.; Rosenson, R.S.; Gencer, B.; López, J.A.G.; Lepor, N.E.; Baum, S.J.; Stout, E.; Gaudet, D.; Knusel, B.; Kuder, J.F.; et al. Small interfering RNA to reduce lipoprotein (a) in cardiovascular disease. N. Engl. J. Med. 2022, 387, 1855–1864. [Google Scholar] [CrossRef] [PubMed]
| Traditional Cardiovascular Risk Factor | “Young” Patients | “Old” Patients |
|---|---|---|
| Arterial hypertension |
| |
| Smoking | ||
| Diabetes mellitus |
|
|
| Obesity |
|
|
| Dyslipidaemia |
|
|
| Gender |
| |
| Family history |
|
| Guidelines | Recommendation |
|---|---|
| ESC/EAS (European Society of Cardiology/European Atherosclerosis Society) for the management of dyslipidemias [76] |
|
| HEART UK (Hyperlipidaemia Education and Atherosclerosis Research Trust UK) [77] |
|
| AHA/ACC (American Heart Association/American College of Cardiology) Guideline of the Management of Blood Cholesterol [78] |
|
| NLA (National Lipid Association) [79] |
|
| CCS (Canadian Cardiovascular Society) [80] |
|
| Study | Country | Population | Measurement | High Lp(a) Threshold | Methodology | Results |
|---|---|---|---|---|---|---|
| Afshar et al. [8] | USA | 2606 participants from the Framingham Offspring Cohort (median age of 54, 45% men) | ELISA | ≥100 nmol/L | Prospective cohort study with a median follow-up of 15 years | Elevated levels of Lp(a) were associated with a high incidence of cardiovascular disease |
| Rallidis et al. [82] | Greece | 382 participants ≤ 40 years who suffered an AMI | High sensitivity particle-enhanced immunonephelometry | apoB > 120 mg/dL | Retrospective cohort study | Lp(a) levels were higher in patients with combined hyperlipidaemia phenotype |
| Hanif et al. [83] | Pakistan | 180 participants with ACS (70% male) subdivided into 45 cases aged ≤ 45 years (considered “young”), respectively, 45 aged > 45 years, each group with age-matched healthy controls | Lp(a) assay on Abbott Architect platform ci8200 using a Latex enhanced technique | High risk for ACS: 31–50 mg/dL, very high risk for ACS: >50 mg/dL | Case control study | In young patients, Lp(a) levels were strongly associated with coronary vascular disease, even with comparative values of LDL and HDL between cases and controls |
| Jubran [84] | Israel | 134 patients ≤ 65 years, with a mean age of 52 ± 8 years, 83% male, presenting with ACS | Particle enhanced trubidimetric immunoassay | >30 mg/dL | Retrospective observational cohort analysis | Elevated Lp(a) levels were independently associated with CAD in young and middle-aged patients |
| Luna et al. [85] | Spain | 159 patients (men under 65 years and women under 70 years), who suffered a STEMI or NSTEMI | ELISA | >60 mg/dL | Descriptive and observational study | Mean Lp(a) levels were 41.08 mg/dL, and 24.5% of patients had values greater than 60 mg/dL |
| Rallidis et al. [86] | Greece | 1457 patients with a history of ACS (median age 54.8 ± 13 years, 86% male) and 2090 age- and sex-matched controls with no CAD | High sensitivity particle-enhanced immunonephelometry | >30 mg/dL | Case-control study | In young patients (<45 years), Lp(a) is an independent risk factor for ACS and elevated Lp(a) levels increase this risk threefold; the correlation was not as strong in the 45–60 years category and was not observed at all >60 years |
| Schatz et al. [87] | Germany | 130 patients with a history of cardiovascular events, aged ≤ 50 years | Immune nephelometry | Three groups: <18 mg/dL, 18–50 mg/dL, >50 mg/dL | Prospective observational study | Lp(a) levels >50 mg/dL were associated with premature CAD |
| Finneran et al. [59] | UK | 153 228 patients without prevalent CAD and no family history of heart disease, with a mean age of 58.4 years, of which 52.2% were female with follow-up time of <9 years | Immunoturbidimetric assay | >150 nmol/L | Prospective, observational cohort study | In patients with no personal or familial (first degree) history of CAD, high Lp(a) levels were associated with an increased risk of incident CAD |
| Korneva et al. [67] | Karelia Republic | 81 patients (middle age was 39.1 ± 0.4 years, 33 males, 48 females), with familial hypercholesterolaemia | Immunoturbidimetry | >30 mg/dL | Prospective observational study | Elevated Lp(a) levels were associated with an increased risk of CAD in patients with familial hypercholesterolaemia |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stătescu, C.; Anghel, L.; Benchea, L.-C.; Tudurachi, B.-S.; Leonte, A.; Zăvoi, A.; Zota, I.M.; Prisacariu, C.; Radu, R.; Șerban, I.-L.; et al. A Systematic Review on the Risk Modulators of Myocardial Infarction in the “Young”—Implications of Lipoprotein (a). Int. J. Mol. Sci. 2023, 24, 5927. https://doi.org/10.3390/ijms24065927
Stătescu C, Anghel L, Benchea L-C, Tudurachi B-S, Leonte A, Zăvoi A, Zota IM, Prisacariu C, Radu R, Șerban I-L, et al. A Systematic Review on the Risk Modulators of Myocardial Infarction in the “Young”—Implications of Lipoprotein (a). International Journal of Molecular Sciences. 2023; 24(6):5927. https://doi.org/10.3390/ijms24065927
Chicago/Turabian StyleStătescu, Cristian, Larisa Anghel, Laura-Cătălina Benchea, Bogdan-Sorin Tudurachi, Andreea Leonte, Alexandra Zăvoi, Ioana Mădălina Zota, Cristina Prisacariu, Rodica Radu, Ionela-Lăcrămioara Șerban, and et al. 2023. "A Systematic Review on the Risk Modulators of Myocardial Infarction in the “Young”—Implications of Lipoprotein (a)" International Journal of Molecular Sciences 24, no. 6: 5927. https://doi.org/10.3390/ijms24065927
APA StyleStătescu, C., Anghel, L., Benchea, L.-C., Tudurachi, B.-S., Leonte, A., Zăvoi, A., Zota, I. M., Prisacariu, C., Radu, R., Șerban, I.-L., & Sascău, R. A. (2023). A Systematic Review on the Risk Modulators of Myocardial Infarction in the “Young”—Implications of Lipoprotein (a). International Journal of Molecular Sciences, 24(6), 5927. https://doi.org/10.3390/ijms24065927












