Uveal Melanoma Patients Have a Distinct Metabolic Phenotype in Peripheral Blood
Abstract
1. Introduction
2. Results
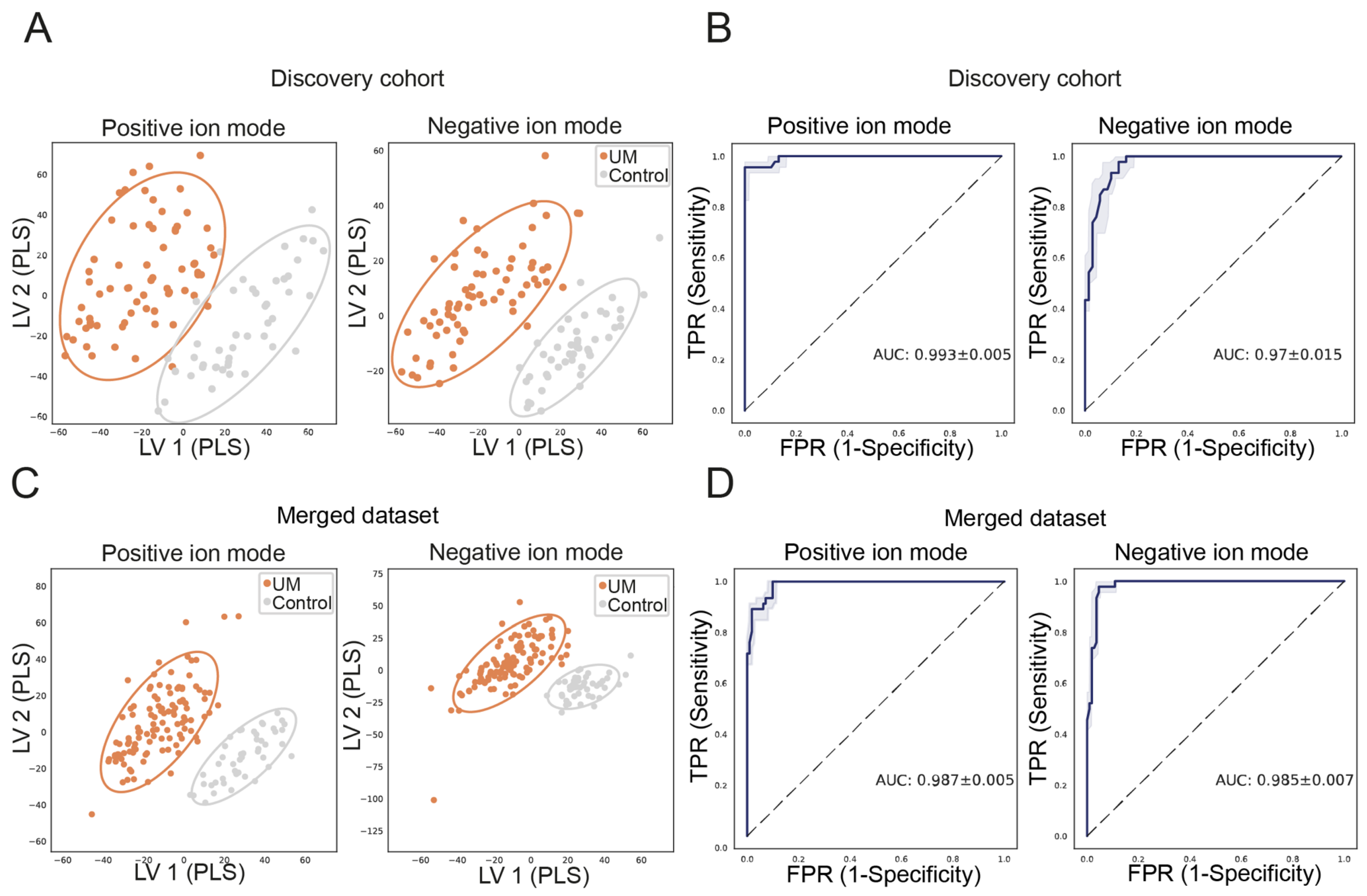
2.1. Untargeted Metabolomics Discriminates UM Patients from Control Participants
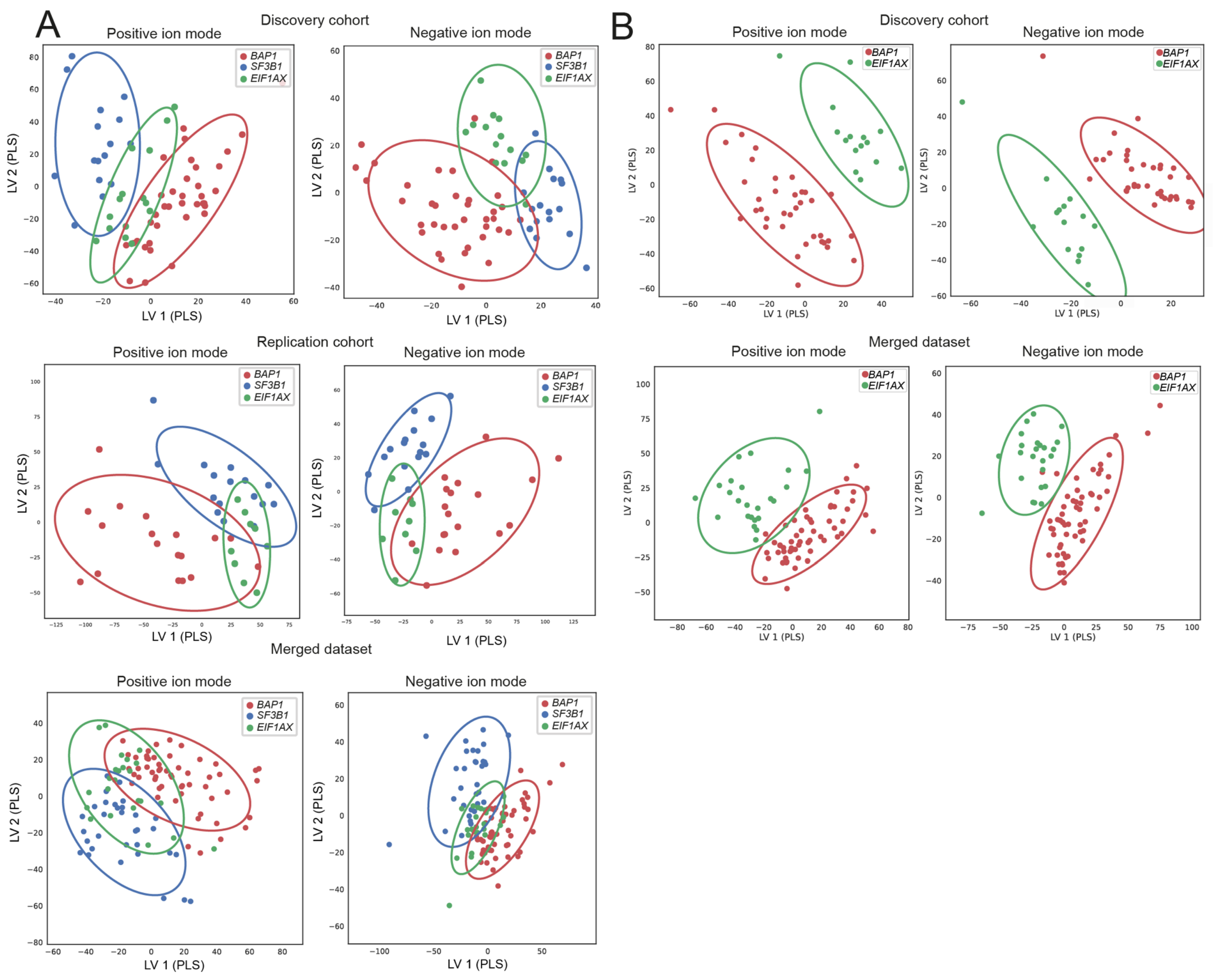
2.2. Metabolic Patterns Do Not Distinguish Prognostic Subtypes at the Time of Diagnosis
2.3. Differentially Expressed Pathways in Peripheral Blood of Uveal Melanoma Patients
3. Discussion
4. Materials and Methods
4.1. Experimental Design
4.2. Patient Selection
4.3. Collection of Blood
4.4. Liquid Chromatography-Mass Spectrometry
4.5. Metabolomics Analyses
Removing Inter—And Intra-Batch Variation
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smit, K.N.; Jager, M.J.; de Klein, A.; Kiliç, E. Uveal melanoma: Towards a molecular understanding. Prog. Retin. Eye Res. 2020, 75, 100800. [Google Scholar] [CrossRef] [PubMed]
- Drabarek, W.; Yavuzyigitoglu, S.; Obulkasim, A.; van Riet, J.; Smit, K.N.; van Poppelen, N.M.; Vaarwater, J.; Brands, T.; Eussen, B.; Verdijk, R.M.; et al. Multi-Modality Analysis Improves Survival Prediction in Enucleated Uveal Melanoma Patients. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3595–3605. [Google Scholar] [CrossRef] [PubMed]
- Yavuzyigitoglu, S.; Koopmans, A.E.; Verdijk, R.M.; Vaarwater, J.; Eussen, B.; Van Bodegom, A.; Paridaens, D.; Kiliç, E.; de Klein, A.; Group, R.O.M.S. Uveal melanomas with SF3B1 mutations: A distinct subclass associated with late-onset metastases. Ophthalmology 2016, 123, 1118–1128. [Google Scholar] [CrossRef]
- Smidt-Nielsen, I.; Bagger, M.; Heegaard, S.; Andersen, K.K.; Kiilgaard, J.F. Posterior uveal melanoma incidence and survival by AJCC tumour size in a 70-year nationwide cohort. Acta Ophthalmol. 2021, 99, e1474–e1482. [Google Scholar] [CrossRef] [PubMed]
- Jager, M.J.; Shields, C.L.; Cebulla, C.M.; Abdel-Rahman, M.H.; Grossniklaus, H.E.; Stern, M.-H.; Carvajal, R.D.; Belfort, R.N.; Jia, R.; Shields, J.A. Uveal melanoma. Nat. Rev. Dis. Prim. 2020, 6, 24. [Google Scholar] [CrossRef] [PubMed]
- de Bruyn, D.P.; Beasley, A.B.; Verdijk, R.M.; van Poppelen, N.M.; Paridaens, D.; de Keizer, R.O.B.; Naus, N.C.; Gray, E.S.; de Klein, A.; Brosens, E.; et al. Is Tissue Still the Issue? The Promise of Liquid Biopsy in Uveal Melanoma. Biomedicines 2022, 10, 506. [Google Scholar] [CrossRef]
- Damato, E.M.; Damato, B.E. Detection and time to treatment of uveal melanoma in the United Kingdom: An evaluation of 2384 patients. Ophthalmology 2012, 119, 1582–1589. [Google Scholar] [CrossRef]
- Beasley, A.; Isaacs, T.; Khattak, M.A.; Freeman, J.B.; Allcock, R.; Chen, F.K.; Pereira, M.R.; Yau, K.; Bentel, J.; Vermeulen, T.; et al. Clinical application of circulating tumor cells and circulating tumor DNA in uveal melanoma. JCO Precis. Oncol. 2018, 2, 1–12. [Google Scholar] [CrossRef]
- Wróblewska, J.P.; Lach, M.S.; Kulcenty, K.; Galus, Ł.; Suchorska, W.M.; Rösel, D.; Brábek, J.; Marszałek, A. The analysis of inflammation-related proteins in a cargo of exosomes derived from the serum of uveal melanoma patients reveals potential biomarkers of disease progression. Cancers 2021, 13, 3334. [Google Scholar] [CrossRef]
- Pavlova, N.N.; Thompson, C.B. The Emerging Hallmarks of Cancer Metabolism. Cell Metab. 2016, 23, 27–47. [Google Scholar] [CrossRef]
- Huang, L.; Wang, L.; Hu, X.; Chen, S.; Tao, Y.; Su, H.; Yang, J.; Xu, W.; Vedarethinam, V.; Wu, S.; et al. Machine learning of serum metabolic patterns encodes early-stage lung adenocarcinoma. Nat. Commun. 2020, 11, 3556. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Sanchez-Espiridion, B.; Lin, M.; White, L.; Mishra, L.; Raju, G.S.; Kopetz, S.; Eng, C.; Hildebrandt, M.A.T.; Chang, D.W.; et al. Global and targeted serum metabolic profiling of colorectal cancer progression. Cancer 2017, 123, 4066–4074. [Google Scholar] [CrossRef] [PubMed]
- Larkin, J.R.; Anthony, S.; Johanssen, V.A.; Yeo, T.; Sealey, M.; Yates, A.G.; Smith, C.F.; Claridge, T.D.W.; Nicholson, B.D.; Moreland, J.A.; et al. Metabolomic Biomarkers in Blood Samples Identify Cancers in a Mixed Population of Patients with Nonspecific Symptoms. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2022, 28, 1651–1661. [Google Scholar] [CrossRef] [PubMed]
- Bongaerts, M.; Bonte, R.; Demirdas, S.; Jacobs, E.H.; Oussoren, E.; van der Ploeg, A.T.; Wagenmakers, M.; Hofstra, R.M.W.; Blom, H.J.; Reinders, M.J.T.; et al. Using Out-of-Batch Reference Populations to Improve Untargeted Metabolomics for Screening Inborn Errors of Metabolism. Metabolites 2020, 11, 8. [Google Scholar] [CrossRef]
- Colijn, J.M.; Buitendijk, G.H.S.; Prokofyeva, E.; Alves, D.; Cachulo, M.L.; Khawaja, A.P.; Cougnard-Gregoire, A.; Merle, B.M.J.; Korb, C.; Erke, M.G.; et al. Prevalence of Age-Related Macular Degeneration in Europe: The Past and the Future. Ophthalmology 2017, 124, 1753–1763. [Google Scholar] [CrossRef] [PubMed]
- Cedrone, C.; Culasso, F.; Cesareo, M.; Mancino, R.; Ricci, F.; Cupo, G.; Cerulli, L. Prevalence and incidence of age-related cataract in a population sample from Priverno, Italy. Ophthalmic Epidemiol. 1999, 6, 95–103. [Google Scholar] [CrossRef]
- Hashemi, H.; Pakzad, R.; Yekta, A.; Aghamirsalim, M.; Pakbin, M.; Ramin, S.; Khabazkhoob, M. Global and regional prevalence of age-related cataract: A comprehensive systematic review and meta-analysis. Eye 2020, 34, 1357–1370. [Google Scholar] [CrossRef]
- Eskelin, S.; Pyrhönen, S.; Summanen, P.; Hahka-Kemppinen, M.; Kivelä, T. Tumor doubling times in metastatic malignant melanoma of the uvea: Tumor progression before and after treatment. Ophthalmology 2000, 107, 1443–1449. [Google Scholar] [CrossRef]
- Piaggio, F.; Croce, M.; Reggiani, F.; Monti, P.; Bernardi, C.; Ambrosio, M.; Banelli, B.; Dogrusöz, M.; Jockers, R.; Bordo, D.; et al. In uveal melanoma Gα-protein GNA11 mutations convey a shorter disease-specific survival and are more strongly associated with loss of BAP1 and chromosomal alterations than Gα-protein GNAQ mutations. Eur. J. Cancer 2022, 170, 27–41. [Google Scholar] [CrossRef]
- Bonte, R.; Bongaerts, M.; Demirdas, S.; Langendonk, J.G.; Huidekoper, H.H.; Williams, M.; Onkenhout, W.; Jacobs, E.H.; Blom, H.J.; Ruijter, G.J.G. Untargeted Metabolomics-Based Screening Method for Inborn Errors of Metabolism using Semi-Automatic Sample Preparation with an UHPLC-Orbitrap-MS Platform. Metabolites 2019, 9, 289. [Google Scholar] [CrossRef]
- Vincent, C.T.; Schneider, R.J. Selective tRNA charging in breast cancer. Nat. Cell Biol. 2022, 24, 287–289. [Google Scholar] [CrossRef]
- Amelio, I.; Cutruzzolá, F.; Antonov, A.; Agostini, M.; Melino, G. Serine and glycine metabolism in cancer. Trends Biochem. Sci. 2014, 39, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Ren, W.; Huang, X.; Deng, J.; Li, T.; Yin, Y. Potential Mechanisms Connecting Purine Metabolism and Cancer Therapy. Front. Immunol. 2018, 9, 1697. [Google Scholar] [CrossRef]
- Lamas, N.J.; Martel, A.; Nahon-Estève, S.; Goffinet, S.; Macocco, A.; Bertolotto, C.; Lassalle, S.; Hofman, P. Prognostic Biomarkers in Uveal Melanoma: The Status Quo, Recent Advances and Future Directions. Cancers 2022, 14, 96. [Google Scholar] [CrossRef] [PubMed]
- Velez, G.; Nguyen, H.V.; Chemudupati, T.; Ludwig, C.A.; Toral, M.; Reddy, S.; Mruthyunjaya, P.; Mahajan, V.B. Liquid biopsy proteomics of uveal melanoma reveals biomarkers associated with metastatic risk. Mol. Cancer 2021, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Azuma, K.; Xiang, H.; Tagami, T.; Kasajima, R.; Kato, Y.; Karakawa, S.; Kikuchi, S.; Imaizumi, A.; Matsuo, N.; Ishii, H.; et al. Clinical significance of plasma-free amino acids and tryptophan metabolites in patients with non-small cell lung cancer receiving PD-1 inhibitor: A pilot cohort study for developing a prognostic multivariate model. J. Immuno Ther. Cancer 2022, 10, e004420. [Google Scholar] [CrossRef]
- Roś-Mazurczyk, M.; Wojakowska, A.; Marczak, Ł.; Polański, K.; Pietrowska, M.; Polanska, J.; Dziadziuszko, R.; Jassem, J.; Rzyman, W.; Widlak, P. Panel of serum metabolites discriminates cancer patients and healthy participants of lung cancer screening—A pilot study. Acta Biochim. Pol. 2017, 64, 513–518. [Google Scholar] [CrossRef]
- Muthubharathi, B.C.; Gowripriya, T.; Balamurugan, K. Metabolomics: Small molecules that matter more. Mol. Omics 2021, 17, 210–229. [Google Scholar] [CrossRef]
- Haid, M.; Muschet, C.; Wahl, S.; Römisch-Margl, W.; Prehn, C.; Möller, G.; Adamski, J. Long-Term Stability of Human Plasma Metabolites during Storage at −80 °C. J. Proteome Res. 2018, 17, 203–211. [Google Scholar] [CrossRef]
- Wagner-Golbs, A.; Neuber, S.; Kamlage, B.; Christiansen, N.; Bethan, B.; Rennefahrt, U.; Schatz, P.; Lind, L. Effects of Long-Term Storage at −80 °C on the Human Plasma Metabolome. Metabolites 2019, 9, 99. [Google Scholar] [CrossRef]
- Hebels, D.G.; Georgiadis, P.; Keun, H.C.; Athersuch, T.J.; Vineis, P.; Vermeulen, R.; Portengen, L.; Bergdahl, I.A.; Hallmans, G.; Palli, D.; et al. Performance in omics analyses of blood samples in long-term storage: Opportunities for the exploitation of existing biobanks in environmental health research. Environ. Health Perspect. 2013, 121, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Pinto, J.; Domingues, M.R.; Galhano, E.; Pita, C.; Almeida Mdo, C.; Carreira, I.M.; Gil, A.M. Human plasma stability during handling and storage: Impact on NMR metabolomics. Analyst 2014, 139, 1168–1177. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Zhai, G.; Singmann, P.; He, Y.; Xu, T.; Prehn, C.; Römisch-Margl, W.; Lattka, E.; Gieger, C.; Soranzo, N.; et al. Human serum metabolic profiles are age dependent. Aging Cell 2012, 11, 960–967. [Google Scholar] [CrossRef]
- Palles, C.; West, H.D.; Chew, E.; Galavotti, S.; Flensburg, C.; Grolleman, J.E.; Jansen, E.A.M.; Curley, H.; Chegwidden, L.; Arbe-Barnes, E.H.; et al. Germline MBD4 deficiency causes a multi-tumor predisposition syndrome. Am. J. Hum. Genet. 2022, 109, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Saint-Ghislain, M.; Derrien, A.C.; Geoffrois, L.; Gastaud, L.; Lesimple, T.; Negrier, S.; Penel, N.; Kurtz, J.E.; Le Corre, Y.; Dutriaux, C.; et al. MBD4 deficiency is predictive of response to immune checkpoint inhibitors in metastatic uveal melanoma patients. Eur. J. Cancer 2022, 173, 105–112. [Google Scholar] [CrossRef]
- Derrien, A.-C.; Rodrigues, M.; Eeckhoutte, A.; Dayot, S.; Houy, A.; Mobuchon, L.; Gardrat, S.; Lequin, D.; Ballet, S.; Pierron, G.; et al. Germline MBD4 Mutations and Predisposition to Uveal Melanoma. JNCI J. Natl. Cancer Inst. 2020, 113, 80–87. [Google Scholar] [CrossRef]
- Rodrigues, M.; Mobuchon, L.; Houy, A.; Alsafadi, S.; Baulande, S.; Mariani, O.; Marande, B.; Ait Rais, K.; Van der Kooij, M.K.; Kapiteijn, E.; et al. Evolutionary Routes in Metastatic Uveal Melanomas Depend on MBD4 Alterations. Clin. Cancer Res. 2019, 25, 5513–5524. [Google Scholar] [CrossRef]
- van den Bosch, Q.C.C.; Nguyen, J.Q.N.; Brands, T.; van den Bosch, T.P.P.; Verdijk, R.M.; Paridaens, D.; Naus, N.C.; de Klein, A.; Kiliç, E.; Brosens, E. FOXD1 Is a Transcription Factor Important for Uveal Melanocyte Development and Associated with High-Risk Uveal Melanoma. Cancers 2022, 14, 3668. [Google Scholar] [CrossRef]
- Pandiani, C.; Strub, T.; Nottet, N.; Cheli, Y.; Gambi, G.; Bille, K.; Husser, C.; Dalmasso, M.; Béranger, G.; Lassalle, S.; et al. Single-cell RNA sequencing reveals intratumoral heterogeneity in primary uveal melanomas and identifies HES6 as a driver of the metastatic disease. Cell Death Differ. 2021, 28, 1990–2000. [Google Scholar] [CrossRef]
- Drabarek, W.; van Riet, J.; Nguyen, J.Q.N.; Smit, K.N.; van Poppelen, N.M.; Jansen, R.; Medico-Salsench, E.; Vaarwater, J.; Magielsen, F.J.; Brands, T.; et al. Identification of Early-Onset Metastasis in SF3B1 Mutated Uveal Melanoma. Cancers 2022, 14, 846. [Google Scholar] [CrossRef]
- Bakhoum, M.F.; Francis, J.H.; Agustinus, A.; Earlie, E.M.; Di Bona, M.; Abramson, D.H.; Duran, M.; Masilionis, I.; Molina, E.; Shoushtari, A.N.; et al. Loss of polycomb repressive complex 1 activity and chromosomal instability drive uveal melanoma progression. Nat. Commun. 2021, 12, 5402. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Barbour, J.A.; Zhu, X.; Wong, J.W. Gene expression is a poor predictor of steady-state metabolite abundance in cancer cells. FASEB J. 2022, 36, e22296. [Google Scholar] [CrossRef]
- Huang, S.Q.; Sun, B.; Xiong, Z.P.; Shu, Y.; Zhou, H.H.; Zhang, W.; Xiong, J.; Li, Q. The dysregulation of tRNAs and tRNA derivatives in cancer. J. Exp. Clin. Cancer Res. 2018, 37, 101. [Google Scholar] [CrossRef] [PubMed]
- Chattopadhyay, C.; Oba, J.; Roszik, J.; Marszalek, J.R.; Chen, K.; Qi, Y.; Eterovic, K.; Gordon Robertson, A.; Burks, J.K.; McCannel, T.A.; et al. Elevated endogenous SDHA drives pathological metabolism in highly metastatic uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2019, 60, 4187–4195. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Chua, V.; Baqai, U.; Purwin, T.J.; Bechtel, N.; Hunter, E.; Tiago, M.; Seifert, E.; Speicher, D.W.; Schug, Z.T.; et al. Pyruvate dehydrogenase inactivation causes glycolytic phenotype in BAP1 mutant uveal melanoma. Oncogene 2022, 41, 1129–1139. [Google Scholar] [CrossRef]
- Han, A.; Purwin, T.J.; Bechtel, N.; Liao, C.; Chua, V.; Seifert, E.; Sato, T.; Schug, Z.T.; Speicher, D.W.; Harbour, J.W. BAP1 mutant uveal melanoma is stratified by metabolic phenotypes with distinct vulnerability to metabolic inhibitors. Oncogene 2021, 40, 618–632. [Google Scholar] [CrossRef]
- Terlizzi, M.; Molino, A.; Colarusso, C.; Somma, P.; De Rosa, I.; Troisi, J.; Scala, G.; Salvi, R.; Pinto, A.; Sorrentino, R. Altered lung tissue lipidomic profile in caspase-4 positive non-small cell lung cancer (NSCLC) patients. Oncotarget 2020, 11, 3515–3525. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V. Scikit-learn: Machine learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Krämer, A.; Green, J.; Pollard, J., Jr.; Tugendreich, S. Causal analysis approaches in Ingenuity Pathway Analysis. Bioinformatics 2014, 30, 523–530. [Google Scholar] [CrossRef]
| BAP1 n = 56 | SF3B1 n = 33 | EIF1AX n = 24 | |||||
|---|---|---|---|---|---|---|---|
| D (n = 37) | R (n = 19) | D (n = 16) | R (n = 17) | D (n = 15) | R (n = 9) | ||
| Age at onset (y) Ns | Mean (SD) | 68.8 (10.7) | 64.4 (12.9) | 54.3 (12.2) | 58.6 (14.7) | 61.3 (12.0) | 62.0 (12.1) |
| Gender | Male | 17 | 12 | 7 | 8 | 8 | 5 |
| Female | 20 | 7 | 9 | 9 | 7 | 4 | |
| MFS (mo) *** | Mean (SD) | 30.0 (29.2) | 38.1 (36.6) | 61.7 (46.5) | 73.0 (61.1) | 70.6 (61.2) | 78.6 (37.5) |
| Primary driver mutation | GNAQ | 7 | 10 | 5 | 7 | 5 | 4 |
| GNA11 | 10 | 9 | 5 | 10 | 5 | 5 | |
| CYSLTR2 | 2 | 0 | 0 | 0 | 0 | 0 | |
| Missing | 18 | 0 | 6 | 0 | 5 | 0 | |
| Tumor location | Choroid | 32 | 16 | 13 | 17 | 14 | 9 |
| CB | 5 | 3 | 3 | 0 | 1 | 0 | |
| T-class | 1 | 3 | 1 66 | 2 | 2 | 2 | 1 |
| 2 | 11 | 6 | 6 | 8 | 5 | 3 | |
| 3 | 18 | 10 | 7 | 6 | 7 | 5 | |
| 4 | 5 | 1 | 1 | 1 | 1 | 0 | |
| Missing | 0 | 1 | 0 | 0 | 0 | 0 | |
| LTD (mm) Ns | mean (SD) | 13.7 (3>3) | 13.9 (3.0) | 14.2 (3.5) | 13.3 (3.0) | 12.5 (3.4) | 12.0 (3.6) |
| Prominence (mm) Ns | mean (SD) | 8.6 (4.1) | 7.8 (3.5) | 6.9 (3.6) | 6.3 (2.3) | 7.1 (2.3) | 7.9 (3.1) |
| Cell type **** | Epithelioid | 9 | 2 | 1 | 0 | 0 | 1 |
| Spindle | 3 | 1 | 7 | 12 | 9 | 6 | |
| Mixed | 21 | 16 | 7 | 5 | 6 | 1 | |
| NE | 4 | 0 | 1 | 0 | 0 | 0 | |
| Inflammatory infiltrate | Yes | 3 | 7 | 2 | 4 | 0 | 1 |
| No | 4 | 12 | 3 | 13 | 4 | 8 | |
| NE | 30 | 0 | 11 | 0 | 11 | 0 | |
| Necrosis * | Yes | 13 | 9 | 4 | 5 | 4 | 1 |
| No | 20 | 10 | 10 | 12 | 9 | 8 | |
| NE | 4 | 0 | 2 | 0 | 2 | 0 | |
| Closed vascular loops * | Yes | 20 | 15 | 5 | 3 | 4 | 1 |
| No | 12 | 4 | 10 | 14 | 9 | 6 | |
| NE | 5 | 0 | 1 | 0 | 2 | 2 | |
| CB involvement | Yes | 13 | 7 | 6 | 2 | 3 | 0 |
| No | 19 | 12 | 8 | 15 | 10 | 7 | |
| NE | 5 | 0 | 2 | 0 | 2 | 2 | |
| (A) | Discovery Cohort UM Patients versus Controls | ||||||
|---|---|---|---|---|---|---|---|
| Negative Ion Mode | Positive Ion Mode | ||||||
| Precision | Recall | F1-Score | Precision | Recall | F1-Score | ||
| UM | 1.000 | 0.794 | 0.885 | UM | 0.955 | 0.941 | 0.948 |
| Control | 0.767 | 1.000 | 0.868 | Control | 0.915 | 0.935 | 0.925 |
| Accuracy | 0.877 | Accuracy | 0.939 | ||||
| (B) | Merged datasets UM patients versus controls | ||||||
| Negative ion mode | Positive ion mode | ||||||
| precision | recall | F1-score | precision | recall | F1-score | ||
| UM | 0.990 | 0.875 | 0.929 | UM | 0.955 | 0.946 | 0.951 |
| Control | 0.763 | 0.978 | 0.857 | Control | 0.872 | 0.891 | 0.882 |
| Accuracy | 0.905 | Accuracy | 0.930 | ||||
| A | Discovery Cohort UM-Subtypes and Controls | ||||||
|---|---|---|---|---|---|---|---|
| Negative Ion Mode | Positive Ion Mode | ||||||
| Precision | Recall | F1-Score | Precision | Recall | F1-Score | ||
| BAP1 | 0.532 | 0.676 | 0.595 | BAP1 | 0.453 | 0.649 | 0.533 |
| SF3B1 | 0 | 0 | 0 | SF3B1 | 0 | 0 | 0 |
| EIF1AX | 0 | 0 | 0 | EIF1AX | 0 | 0 | 0 |
| Control | 0.714 | 0.978 | 0.826 | Control | 0.8 | 0.957 | 0.871 |
| Accuracy | 0.614 | Accuracy | 0.6 | ||||
| B | Replication cohort UM-subtypes | ||||||
| Negative ion mode | Positive ion mode | ||||||
| precision | recall | F1-score | precision | recall | F1-score | ||
| BAP1 | 0.652 | 0.79 | 0.714 | BAP1 | 0.7 | 0.778 | 0.737 |
| SF3B1 | 0.556 | 0.625 | 0.588 | SF3B1 | 0.474 | 0.563 | 0.514 |
| EIF1AX | 0 | 0 | 0 | EIF1AX | 0.75 | 0.333 | 0.462 |
| Accuracy | 0.568 | Accuracy | 0.605 | ||||
| C | Merged datasets UM-subtypes and controls | ||||||
| Negative ion mode | Positive ion mode | ||||||
| precision | recall | F1-score | precision | recall | F1-score | ||
| BAP1 | 0.565 | 0.64 | 0.6 | BAP1 | 0.581 | 0.705 | 0.637 |
| SF3B1 | 0.367 | 0.289 | 0.324 | SF3B1 | 0.5 | 0.289 | 0.367 |
| EIF1AX | 0.41 | 0.321 | 0.36 | EIF1AX | 0.444 | 0.286 | 0.348 |
| Control | 0.78 | 1 | 0.876 | Control | 0.763 | 0.978 | 0.857 |
| Accuracy | 0.601 | Accuracy | 0.618 | ||||
| D | Merged datasets primary driver mutation | ||||||
| Negative ion mode | Positive ion mode | ||||||
| precision | recall | F1-score | precision | recall | F1-score | ||
| GNA11 | 0.571 | 0.571 | 0.571 | GNA11 | 0.571 | 0.571 | 0.571 |
| GNAQ | 0.609 | 0.609 | 0.609 | GNAQ | 0.609 | 0.609 | 0.609 |
| Accuracy | 0.591 | Accuracy | 0.591 | ||||
| E | Merged dataset BAP1 and EIF1AX mutations | ||||||
| Negative ion mode | Positive ion mode | ||||||
| precision | recall | F1-score | precision | recall | F1-score | ||
| BAP1 | 0.571 | 0.632 | 0.6 | BAP1 | 0.636 | 0.778 | 0.7 |
| EIF1AX | 0.417 | 0.357 | 0.385 | EIF1AX | 0 | 0 | 0 |
| Accuracy | 0.515 | Accuracy | 0.538 | ||||
| F | Merged dataset metastatic formation of UM patients | ||||||
| Negative ion mode | Positive ion mode | ||||||
| precision | recall | F1-score | precision | recall | F1-score | ||
| Yes | 0.5 | 0.15 | 0.231 | Yes | 0.333 | 0.1 | 0.154 |
| No | 0.726 | 0.938 | 0.818 | No | 0.71 | 0.917 | 0.8 |
| Accuracy | 0.706 | Accuracy | 0.676 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Bruyn, D.P.; Bongaerts, M.; Bonte, R.; Vaarwater, J.; Meester-Smoor, M.A.; Verdijk, R.M.; Paridaens, D.; Naus, N.C.; de Klein, A.; Ruijter, G.J.G.; et al. Uveal Melanoma Patients Have a Distinct Metabolic Phenotype in Peripheral Blood. Int. J. Mol. Sci. 2023, 24, 5077. https://doi.org/10.3390/ijms24065077
de Bruyn DP, Bongaerts M, Bonte R, Vaarwater J, Meester-Smoor MA, Verdijk RM, Paridaens D, Naus NC, de Klein A, Ruijter GJG, et al. Uveal Melanoma Patients Have a Distinct Metabolic Phenotype in Peripheral Blood. International Journal of Molecular Sciences. 2023; 24(6):5077. https://doi.org/10.3390/ijms24065077
Chicago/Turabian Stylede Bruyn, Daniël P., Michiel Bongaerts, Ramon Bonte, Jolanda Vaarwater, Magda A. Meester-Smoor, Robert M. Verdijk, Dion Paridaens, Nicole C. Naus, Annelies de Klein, George J. G. Ruijter, and et al. 2023. "Uveal Melanoma Patients Have a Distinct Metabolic Phenotype in Peripheral Blood" International Journal of Molecular Sciences 24, no. 6: 5077. https://doi.org/10.3390/ijms24065077
APA Stylede Bruyn, D. P., Bongaerts, M., Bonte, R., Vaarwater, J., Meester-Smoor, M. A., Verdijk, R. M., Paridaens, D., Naus, N. C., de Klein, A., Ruijter, G. J. G., Kiliç, E., & Brosens, E., on behalf of the Rotterdam Ocular Melanoma Study Group (ROMS). (2023). Uveal Melanoma Patients Have a Distinct Metabolic Phenotype in Peripheral Blood. International Journal of Molecular Sciences, 24(6), 5077. https://doi.org/10.3390/ijms24065077







