New Approaches in Early-Stage NSCL Management: Potential Use of PARP Inhibitors and Immunotherapy Combination
Abstract
1. Non-Small Cell Lung Cancer Management
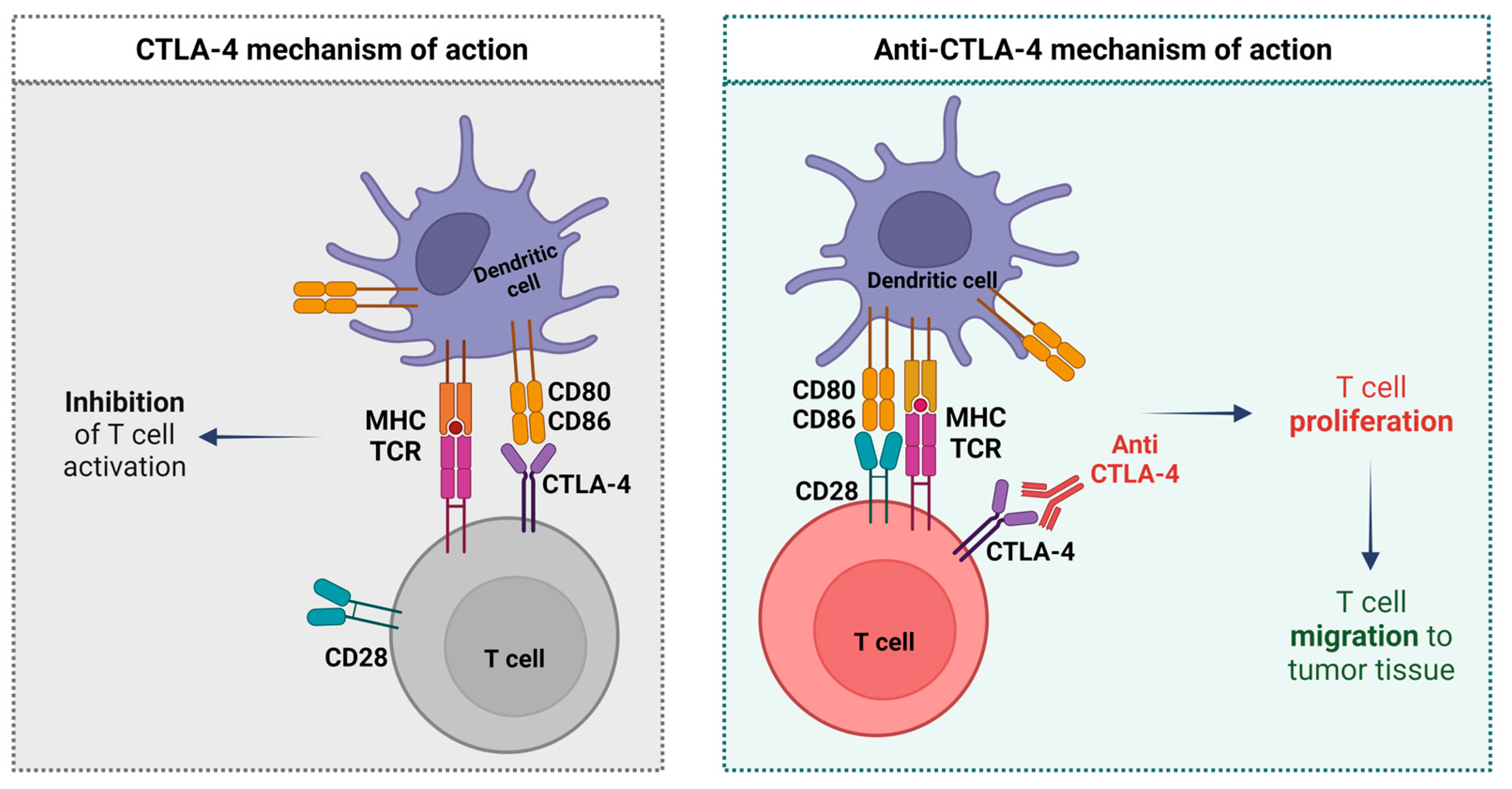
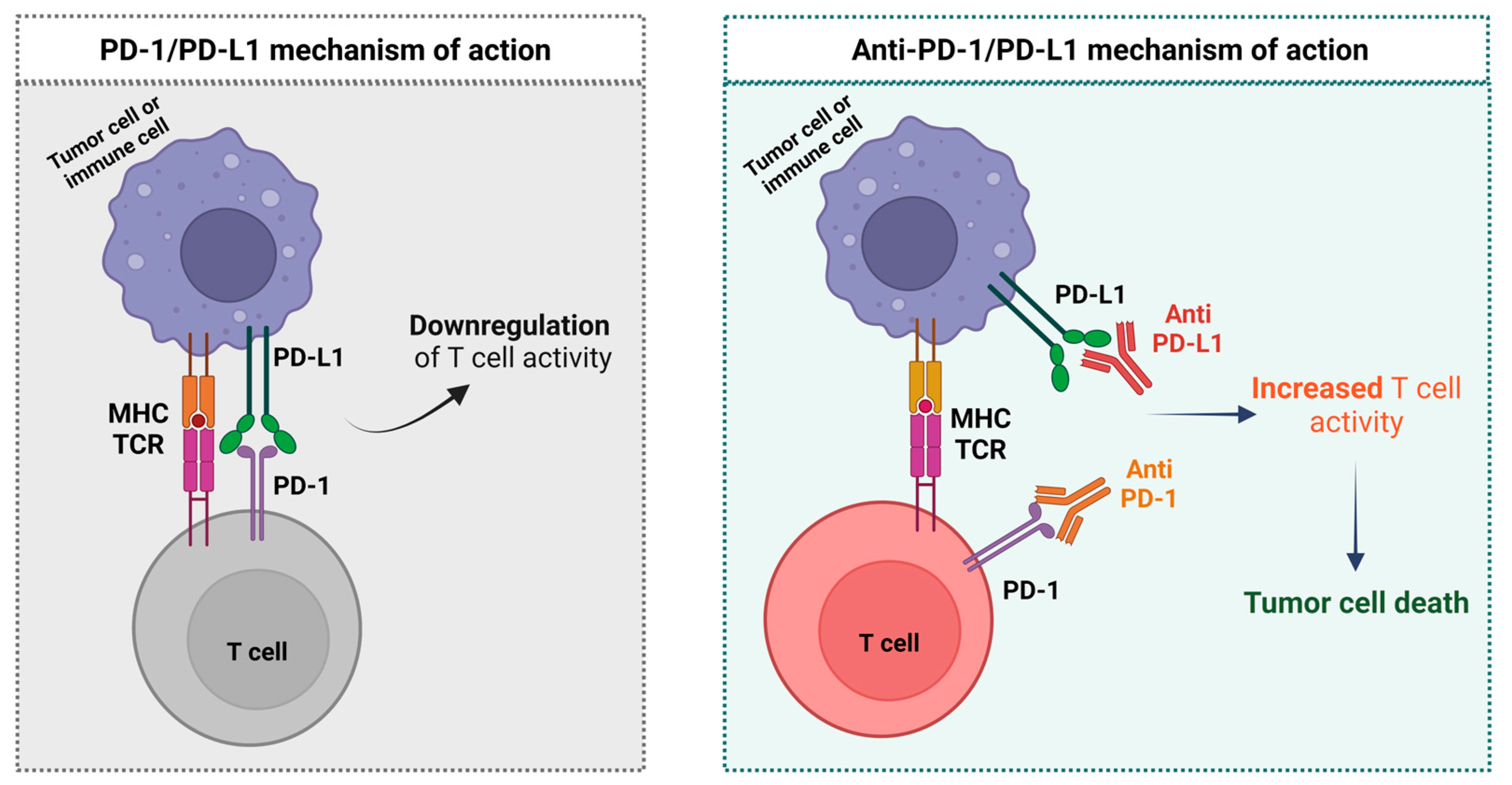
2. Immunotherapy
Neoadjuvant ICI in NSCLC
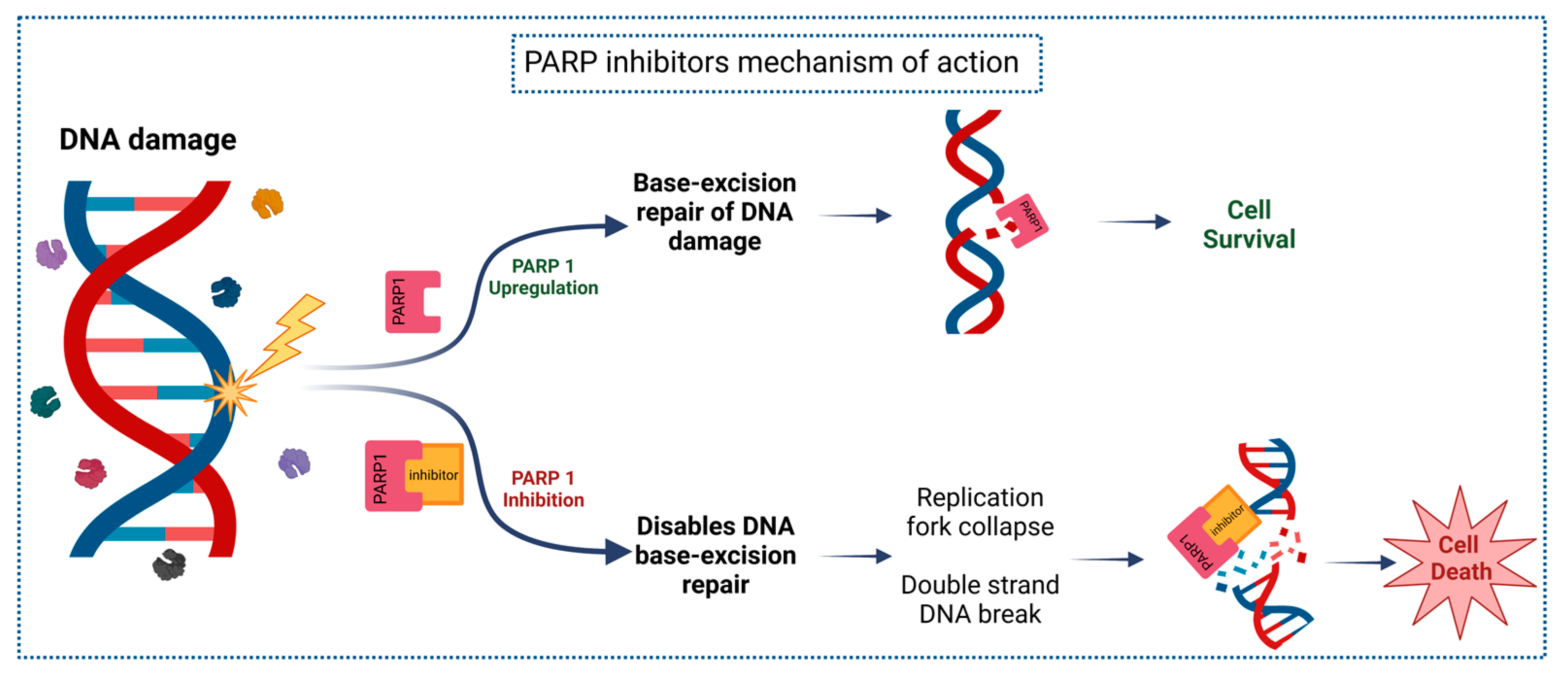
3. PARP Inhibitors
3.1. PARPi in NSCLC
3.2. PARPi in the Neoadjuvant Setting
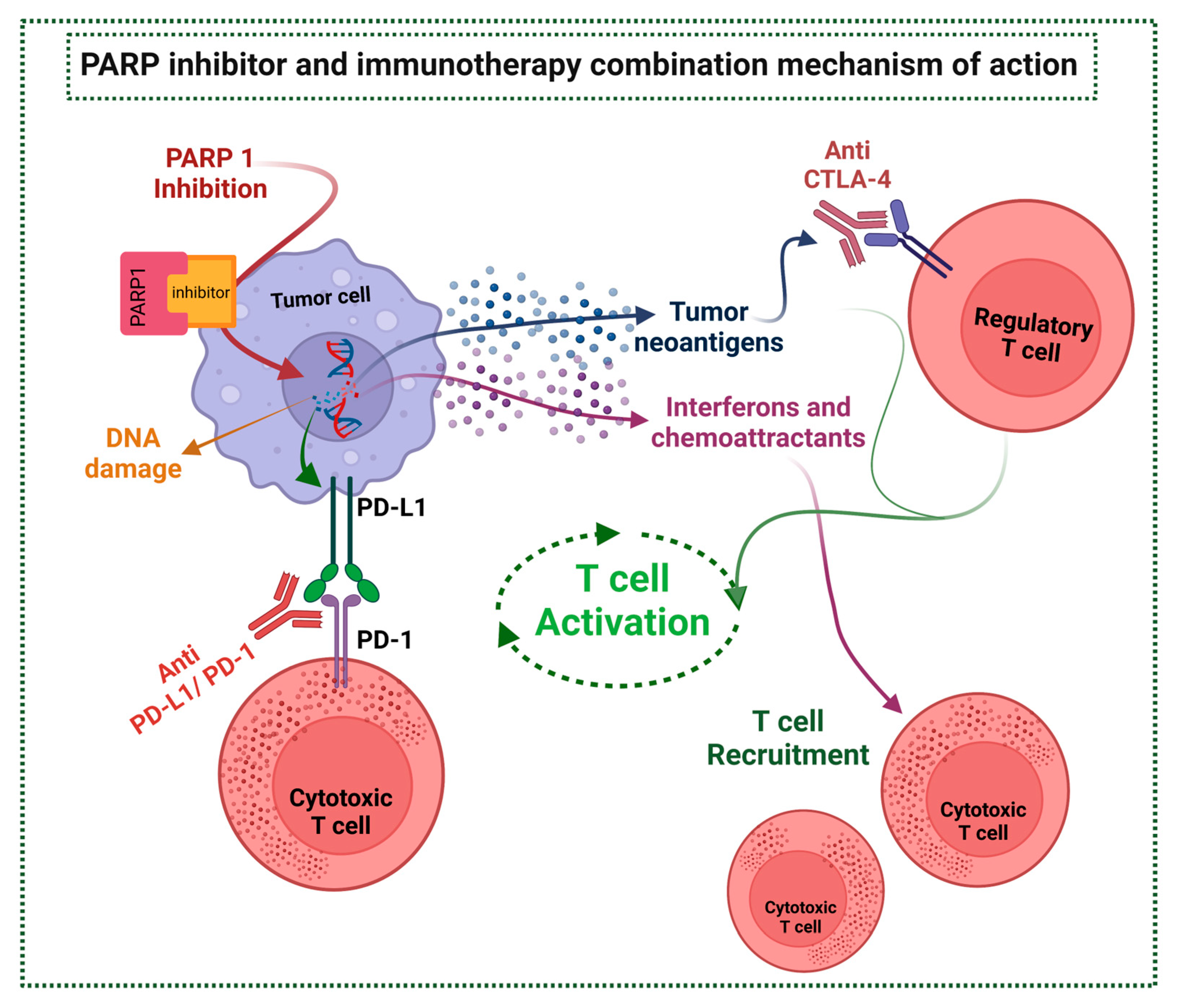
4. Combination of ICI and PARPi
ICI and PARPi Combination Trials
| Trial | NCT02657889 (TOPACIO/ KEYNOTE-162) | NCT02734004 (MEDIOLA) | NCT03308942 (JASPER) | NCT03330405 (JAVELIN PARP Medley) |
|---|---|---|---|---|
| Phase | I-II | II | II | Ib-II |
| Status | Complete | In progress | Complete | Complete |
| Drugs | Niraparib + Pembrolizumab | Olaparib + Durvalumab | Niraparib + Pembrolizumab | Talazoparib + Avelumab |
| Tumor types | TNBC Ovarian cancer | mBC (gBRCAm HER2-) Ovarian cancer SCLC Gastric cancer | NSCLC Cohort 1—PD-L1 ≥50% Cohort 2—PD-L1 <50% | NSCLC Breast Ovarian Prostate Solid Tumors |
| Patients (N) | 55 TNBC 60 Ovarian cancer Total—115 | 34 mBC 32 Ovarian Cancer gBRCAm 32 Ovarian Cancer BRCAwt 39 Gastric cancer 38 SCLC Total—175 | 16 Cohort 1 16 Cohort 2 Total—38 | 42 NSCLC 5 DDR + NSCLC 23 HR+, HER2–, DDR+ mBC 22 TNBC 20 Ovarian cancer 11 Ovarian cancer BRCAm Total—123 |
| Outcomes | Ovarian: ORR 18% DCR 65% PFS 3.4m sAE 37.7% irsAE 6% TNBC ORR 21% DCR 49% PFS 2.3m sAE 20% irsAE 4% | mBC: ORR 56% DCR 47% PFS 6.7m sAE 32% Ovarian gBRCAm: ORR 63% DCR 81% PFS 11.1m Ovarian non-gBRCAm: ORR 31.3% DCR 28.1% PFS 5.5m Gastric: ORR 10% DCR 26% sAE 48% SCLC: DCR 29% sAE 34.2% | Cohort 1 ORR 56,3% DCR 87% PFS 8.4m OS NR sAE 88.2% Cohort 2 ORR 20% DCR 70% PFS 4.2m OS 7.7m sAE 85.7% | NSCLC ORR 16.7% DDR + NSCLC ORR 20% TNBC ORR 18.2% DoR 11.1m DDR+ TNBC ORR 34.8% DoR 15.7m Ovarian ORR 20% BRCAm Ovarian ORR 63.6% DoR NR All tumors sAE—33.6% |
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Rolf, A.; Stahel, S.P. Thoracic Tumours: Essentials for Clinicians, 2nd ed.; Marina Chiara Garassino, Ed.; ESMO Press: Lugano, Switzerland, 2019. [Google Scholar]
- Hoffman, P.C.; Mauer, A.M.; Vokes, E.E. Lung cancer. Lancet 2000, 355, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Szeto, C.H.; Shalata, W.; Yakobson, A.; Agbarya, A. Neoadjuvant and Adjuvant Immunotherapy in Early-Stage Non-Small-Cell Lung Cancer, Past, Present, and Future. J. Clin. Med. 2021, 10, 5614. [Google Scholar] [CrossRef] [PubMed]
- Alexander, M.; Kim, S.Y.; Cheng, H. Update 2020: Management of Non-Small Cell Lung Cancer. Lung 2020, 198, 897–907. [Google Scholar] [CrossRef]
- Mielgo-Rubio, X.; Montemuiño, S.; Jiménez, U.; Luna, J.; Cardeña, A.; Mezquita, L.; Martín, M.; Couñago, F. Management of Resectable Stage III-N2 Non-Small-Cell Lung Cancer (NSCLC) in the Age of Immunotherapy. Cancers 2021, 13, 4811. [Google Scholar] [CrossRef]
- Majeed, U.; Manochakian, R.; Zhao, Y.; Lou, Y. Targeted therapy in advanced non-small cell lung cancer: Current advances and future trends. J. Hematol. Oncol. 2021, 14, 108. [Google Scholar] [CrossRef]
- Sharma, P.; Siddiqui, B.A.; Anandhan, S.; Yadav, S.S.; Subudhi, S.K.; Gao, J.; Goswami, S.; Allison, J.P. The Next Decade of Immune Checkpoint Therapy. Cancer Discov. 2021, 11, 838–857. [Google Scholar] [CrossRef]
- Saw, S.P.L.; Ong, B.H.; Chua, K.L.M.; Takano, A.; Tan, D.S.W. Revisiting neoadjuvant therapy in non-small-cell lung cancer. Lancet Oncol. 2021, 22, e501–e516. [Google Scholar] [CrossRef]
- Group, N.-s.C.L.C.C. Chemotherapy in non-small cell lung cancer: A meta-analysis using updated data on individual patients from 52 randomised clinical trials. Non-small Cell Lung Cancer Collaborative Group. BMJ 1995, 311, 899–909. [Google Scholar]
- Liang, Y.; Wakelee, H.A. Adjuvant chemotherapy of completely resected early stage non-small cell lung cancer (NSCLC). Transl. Lung Cancer Res. 2013, 2, 403–410. [Google Scholar]
- Uramoto, H.; Tanaka, F. Recurrence after surgery in patients with NSCLC. Transl. Lung Cancer Res. 2014, 3, 242–249. [Google Scholar] [CrossRef]
- Paoletti, L.; Pastis, N.J.; Denlinger, C.E.; Silvestri, G.A. A decade of advances in treatment of early-stage lung cancer. Clin. Chest. Med. 2011, 32, 827–838. [Google Scholar] [CrossRef]
- Bai, R.; Li, L.; Chen, X.; Chen, N.; Song, W.; Cui, J. Neoadjuvant and Adjuvant Immunotherapy: Opening New Horizons for Patients With Early-Stage Non-small Cell Lung Cancer. Front. Oncol. 2020, 10, 2048. [Google Scholar] [CrossRef]
- Eichhorn, F.; Klotz, L.V.; Kriegsmann, M.; Bischoff, H.; Schneider, M.A.; Muley, T.; Kriegsmann, K.; Haberkorn, U.; Heussel, C.P.; Savai, R.; et al. Neoadjuvant anti-programmed death-1 immunotherapy by pembrolizumab in resectable non-small cell lung cancer: First clinical experience. Lung Cancer 2021, 153, 150–157. [Google Scholar] [CrossRef]
- Forde, P.M.; Spicer, J.; Lu, S.; Provencio, M.; Mitsudomi, T.; Awad, M.M.; Felip, E.; Broderick, S.R.; Brahmer, J.R.; Swanson, S.J.; et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N. Engl. J. Med. 2022, 386, 1973–1985. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, M.; Weder, W.; Escriu, C.; Blakely, C.; He, J.; Dacic, S.; Yatabe, Y.; Zeng, L.; Walding, A.; Chaft, J.E. Neoadjuvant osimertinib with/without chemotherapy versus chemotherapy alone for EGFR-mutated resectable non-small-cell lung cancer: NeoADAURA. Future Oncol. 2021, 17, 4045–4055. [Google Scholar] [CrossRef] [PubMed]
- Uprety, D.; Mandrekar, S.J.; Wigle, D.; Roden, A.C.; Adjei, A.A. Neoadjuvant Immunotherapy for NSCLC: Current Concepts and Future Approaches. J. Thorac. Oncol. 2020, 15, 1281–1297. [Google Scholar] [CrossRef]
- Disis, M.L. Mechanism of action of immunotherapy. Semin. Oncol. 2014, 41 (Suppl. S5), S3–S13. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, F.; De Giovanni, C.; Nanni, P.; Forni, G.; Lollini, P.L. 2011: The immune hallmarks of cancer. Cancer Immunol. Immunother. 2011, 60, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Mortezaee, K. Immune escape: A critical hallmark in solid tumors. Life Sci. 2020, 258, 118110. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.C.; Santos, J.M.O.; Gil da Costa, R.M.; Medeiros, R. Impact of immune cells on the hallmarks of cancer: A literature review. Crit. Rev. Oncol./Hematol. 2021, 168, 103541. [Google Scholar] [CrossRef] [PubMed]
- Paul, D. The systemic hallmarks of cancer. J. Cancer Metastasis Treat. 2020, 6, 29. [Google Scholar] [CrossRef]
- Zagozdzon, R.; Winiarska, M.; Firczuk, M. Immune Evasion as the Main Challenge for Immunotherapy of Cancer. Cancers 2022, 14, 3622. [Google Scholar] [CrossRef]
- Akinleye, A.; Rasool, Z. Immune checkpoint inhibitors of PD-L1 as cancer therapeutics. J. Hematol. Oncol. 2019, 12, 92. [Google Scholar] [CrossRef]
- Seidel, J.A.; Otsuka, A.; Kabashima, K. Anti-PD-1 and Anti-CTLA-4 Therapies in Cancer: Mechanisms of Action, Efficacy, and Limitations. Front. Oncol. 2018, 8, 86. [Google Scholar] [CrossRef]
- Gajewski, T.F.; Corrales, L.; Williams, J.; Horton, B.; Sivan, A.; Spranger, S. Cancer Immunotherapy Targets Based on Understanding the T Cell-Inflamed Versus Non-T Cell-Inflamed Tumor Microenvironment. Adv. Exp. Med. Biol. 2017, 1036, 19–31. [Google Scholar] [CrossRef]
- Hodi, F.S.; Mihm, M.C.; Soiffer, R.J.; Haluska, F.G.; Butler, M.; Seiden, M.V.; Davis, T.; Henry-Spires, R.; MacRae, S.; Willman, A.; et al. Biologic activity of cytotoxic T lymphocyte-associated antigen 4 antibody blockade in previously vaccinated metastatic melanoma and ovarian carcinoma patients. Proc. Natl. Acad. Sci. USA 2003, 100, 4712–4717. [Google Scholar] [CrossRef]
- Phan, G.Q.; Yang, J.C.; Sherry, R.M.; Hwu, P.; Topalian, S.L.; Schwartzentruber, D.J.; Restifo, N.P.; Haworth, L.R.; Seipp, C.A.; Freezer, L.J.; et al. Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc. Natl. Acad. Sci. USA 2003, 100, 8372–8377. [Google Scholar] [CrossRef]
- Hoos, A.; Ibrahim, R.; Korman, A.; Abdallah, K.; Berman, D.; Shahabi, V.; Chin, K.; Canetta, R.; Humphrey, R. Development of ipilimumab: Contribution to a new paradigm for cancer immunotherapy. Semin. Oncol. 2010, 37, 533–546. [Google Scholar] [CrossRef]
- Tang, S.; Qin, C.; Hu, H.; Liu, T.; He, Y.; Guo, H.; Yan, H.; Zhang, J.; Tang, S.; Zhou, H. Immune Checkpoint Inhibitors in Non-Small Cell Lung Cancer: Progress, Challenges, and Prospects. Cells 2022, 11, 320. [Google Scholar] [CrossRef]
- Hodi, F.S.; O’Day, S.J.; McDermott, D.F.; Weber, R.W.; Sosman, J.A.; Haanen, J.B.; Gonzalez, R.; Robert, C.; Schadendorf, D.; Hassel, J.C.; et al. Improved Survival with Ipilimumab in Patients with Metastatic Melanoma. N. Engl. J. Med. 2010, 363, 711–723. [Google Scholar] [CrossRef]
- Chiu, L.-C.; Lin, S.-M.; Lo, Y.-L.; Kuo, S.C.-H.; Yang, C.-T.; Hsu, P.-C. Immunotherapy and Vaccination in Surgically Resectable Non-Small Cell Lung Cancer (NSCLC). Vaccines 2021, 9, 689. [Google Scholar] [CrossRef]
- Walia, H.K.; Sharma, P.; Singh, N.; Sharma, S. Immunotherapy in Small Cell Lung Cancer Treatment: A Promising Headway for Future Perspective. Curr. Treat. Options Oncol. 2022, 23, 268–294. [Google Scholar] [CrossRef] [PubMed]
- Alard, E.; Butnariu, A.-B.; Grillo, M.; Kirkham, C.; Zinovkin, D.; Newnham, L.; Macciochi, J.; Pranjol, Z. Advances in Anti-Cancer Immunotherapy: Car-T Cell, Checkpoint Inhibitors, Dendritic Cell Vaccines, and Oncolytic Viruses, and Emerging Cellular and Molecular Targets. Cancers 2020, 12, 1826. [Google Scholar] [CrossRef] [PubMed]
- Vikas, P.; Borcherding, N.; Chennamadhavuni, A.; Garje, R. Therapeutic Potential of Combining PARP Inhibitor and Immunotherapy in Solid Tumors. Front. Oncol. 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Schadendorf, D.; Hodi, F.S.; Robert, C.; Weber, J.S.; Margolin, K.; Hamid, O.; Patt, D.; Chen, T.-T.; Berman, D.M.; Wolchok, J.D. Pooled Analysis of Long-Term Survival Data From Phase II and Phase III Trials of Ipilimumab in Unresectable or Metastatic Melanoma. J. Clin. Oncol. 2015, 33, 1889–1894. [Google Scholar] [CrossRef]
- Johnson, M.L.; Cho, B.C.; Luft, A.; Alatorre-Alexander, J.; Geater, S.L.; Laktionov, K.; Kim, S.-W.; Ursol, G.; Hussein, M.; Lim, F.L.; et al. Durvalumab With or Without Tremelimumab in Combination With Chemotherapy as First-Line Therapy for Metastatic Non–Small-Cell Lung Cancer: The Phase III POSEIDON Study. J. Clin. Oncol. 2023, 41, 1213–1227. [Google Scholar] [CrossRef]
- Goldman, J.W.; Dvorkin, M.; Chen, Y.; Reinmuth, N.; Hotta, K.; Trukhin, D.; Statsenko, G.; Hochmair, M.J.; Özgüroğlu, M.; Ji, J.H.; et al. Durvalumab, with or without tremelimumab, plus platinum–etoposide versus platinum–etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): Updated results from a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 51–65. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Chan, S.L.; Kudo, M.; Lau, G.; Kelley, R.K.; Furuse, J.; Sukeepaisarnjaroen, W.; Kang, Y.-K.; Dao, T.V.; Toni, E.N.D.; et al. Phase 3 randomized, open-label, multicenter study of tremelimumab (T) and durvalumab (D) as first-line therapy in patients (pts) with unresectable hepatocellular carcinoma (uHCC): HIMALAYA. J. Clin. Oncol. 2022, 40, 379. [Google Scholar] [CrossRef]
- Jiang, Y.; Chen, M.; Nie, H.; Yuan, Y. PD-1 and PD-L1 in cancer immunotherapy: Clinical implications and future considerations. Hum. Vaccines Immunother. 2019, 15, 1111–1122. [Google Scholar] [CrossRef] [PubMed]
- Rotte, A. Combination of CTLA-4 and PD-1 blockers for treatment of cancer. J. Exp. Clin. Cancer Res. 2019, 38, 255. [Google Scholar] [CrossRef] [PubMed]
- Keir, M.E.; Butte, M.J.; Freeman, G.J.; Sharpe, A.H. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 2008, 26, 677–704. [Google Scholar] [CrossRef]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef]
- Gettinger, S.; Horn, L.; Jackman, D.; Spigel, D.; Antonia, S.; Hellmann, M.; Powderly, J.; Heist, R.; Sequist, L.V.; Smith, D.C.; et al. Five-Year Follow-Up of Nivolumab in Previously Treated Advanced Non-Small-Cell Lung Cancer: Results From the CA209-003 Study. J. Clin. Oncol. 2018, 36, 1675–1684. [Google Scholar] [CrossRef]
- Forde, P.M.; Chaft, J.E.; Smith, K.N.; Anagnostou, V.; Cottrell, T.R.; Hellmann, M.D.; Zahurak, M.; Yang, S.C.; Jones, D.R.; Broderick, S.; et al. Neoadjuvant PD-1 Blockade in Resectable Lung Cancer. N. Engl. J. Med. 2018, 378, 1976–1986. [Google Scholar] [CrossRef]
- Rusch, V.W.; Chaft, J.E.; Johnson, B.; Wistuba, I.I.; Kris, M.G.; Lee, J.M.; Bunn, P.A.; Kwiatkowski, D.J.; Reckamp, K.L.; Finley, D.J.; et al. Neoadjuvant atezolizumab in resectable non-small cell lung cancer (NSCLC): Initial results from a multicenter study (LCMC3). J. Clin. Oncol. 2018, 36, 8541. [Google Scholar] [CrossRef]
- Cascone, T.; William, W.N., Jr.; Weissferdt, A.; Leung, C.H.; Lin, H.Y.; Pataer, A.; Godoy, M.C.B.; Carter, B.W.; Federico, L.; Reuben, A.; et al. Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: The phase 2 randomized NEOSTAR trial. Nat. Med. 2021, 27, 504–514. [Google Scholar] [CrossRef]
- Gatteschi, L.; Iannopollo, M.; Gonfiotti, A. Neoadjuvant Immunotherapy in Resectable Non-Small Cell Lung Cancer. A Narrative Review. Life 2021, 11, 1036. [Google Scholar] [CrossRef]
- Provencio, M.; Nadal, E.; Insa, A.; García-Campelo, M.R.; Casal-Rubio, J.; Dómine, M.; Majem, M.; Rodríguez-Abreu, D.; Martínez-Martí, A.; De Castro Carpeño, J.; et al. Neoadjuvant chemotherapy and nivolumab in resectable non-small-cell lung cancer (NADIM): An open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020, 21, 1413–1422. [Google Scholar] [CrossRef] [PubMed]
- Besse, B.; Adam, J.; Cozic, N.; Chaput-Gras, N.; Planchard, D.; Mezquita, L.; Masip, J.R.; Lavaud, P.; Naltet, C.; Gazzah, A.; et al. 1215O-SC Neoadjuvant atezolizumab (A) for resectable non-small cell lung cancer (NSCLC): Results from the phase II PRINCEPS trial. Ann. Oncol. 2020, 31, S794–S795. [Google Scholar] [CrossRef]
- Shu, C.A.; Gainor, J.F.; Awad, M.M.; Chiuzan, C.; Grigg, C.M.; Pabani, A.; Garofano, R.F.; Stoopler, M.B.; Cheng, S.K.; White, A.; et al. Neoadjuvant atezolizumab and chemotherapy in patients with resectable non-small-cell lung cancer: An open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020, 21, 786–795. [Google Scholar] [CrossRef] [PubMed]
- Tong, B.C.; Gu, L.; Wang, X.; Wigle, D.A.; Phillips, J.D.; Harpole, D.H., Jr.; Klapper, J.A.; Sporn, T.; Ready, N.E.; D’Amico, T.A. Perioperative outcomes of pulmonary resection after neoadjuvant pembrolizumab in patients with non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2022, 163, 427–436. [Google Scholar] [CrossRef]
- Rothschild, S.I.; Zippelius, A.; Eboulet, E.I.; Savic Prince, S.; Betticher, D.; Bettini, A.; Früh, M.; Joerger, M.; Lardinois, D.; Gelpke, H.; et al. SAKK 16/14: Durvalumab in Addition to Neoadjuvant Chemotherapy in Patients With Stage IIIA(N2) Non-Small-Cell Lung Cancer-A Multicenter Single-Arm Phase II Trial. J. Clin. Oncol. 2021, 39, 2872–2880. [Google Scholar] [CrossRef]
- Zhao, Z.R.; Yang, C.P.; Chen, S.; Yu, H.; Lin, Y.B.; Lin, Y.B.; Qi, H.; Jin, J.T.; Lian, S.S.; Wang, Y.Z.; et al. Phase 2 trial of neoadjuvant toripalimab with chemotherapy for resectable stage III non-small-cell lung cancer. Oncoimmunology 2021, 10, 1996000. [Google Scholar] [CrossRef]
- Chaft, J.E.; Oezkan, F.; Kris, M.G.; Bunn, P.A.; Wistuba, I.I.; Kwiatkowski, D.J.; Owen, D.H.; Tang, Y.; Johnson, B.E.; Lee, J.M.; et al. Neoadjuvant atezolizumab for resectable non-small cell lung cancer: An open-label, single-arm phase II trial. Nat. Med. 2022, 28, 2155–2161. [Google Scholar] [CrossRef]
- Hamada, A.; Soh, J.; Hata, A.; Nakamatsu, K.; Shimokawa, M.; Yatabe, Y.; Oizumi, H.; Tsuboi, M.; Horinouchi, H.; Yoshino, I.; et al. Phase II Study of Neoadjuvant Concurrent Chemo-immuno-radiation Therapy Followed by Surgery and Adjuvant Immunotherapy for Resectable Stage IIIA-B (Discrete N2) Non-small-cell Lung Cancer: SQUAT trial (WJOG 12119L). Clin. Lung Cancer 2021, 22, 596–600. [Google Scholar] [CrossRef]
- Heymach, J.V.; Mitsudomi, T.; Harpole, D.; Aperghis, M.; Jones, S.; Mann, H.; Fouad, T.M.; Reck, M. Design and Rationale for a Phase III, Double-Blind, Placebo-Controlled Study of Neoadjuvant Durvalumab + Chemotherapy Followed by Adjuvant Durvalumab for the Treatment of Patients With Resectable Stages II and III non-small-cell Lung Cancer: The AEGEAN Trial. Clin. Lung Cancer 2022, 23, e247–e251. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Neoadjuvant Durvalumab Alone or in Combination With Novel Agents in Resectable Non-Small Cell Lung Cancer. NCT03794544. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03794544. (accessed on 1 December 2022).
- Sepesi, B.; Zhou, N.; William, W.N., Jr.; Lin, H.Y.; Leung, C.H.; Weissferdt, A.; Mitchell, K.G.; Pataer, A.; Walsh, G.L.; Rice, D.C.; et al. Surgical outcomes after neoadjuvant nivolumab or nivolumab with ipilimumab in patients with non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2022, 164, 1327–1337. [Google Scholar] [CrossRef]
- Langelier, M.F.; Eisemann, T.; Riccio, A.A.; Pascal, J.M. PARP family enzymes: Regulation and catalysis of the poly(ADP-ribose) posttranslational modification. Curr. Opin. Struct. Biol. 2018, 53, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Farmer, H.; McCabe, N.; Lord, C.J.; Tutt, A.N.J.; Johnson, D.A.; Richardson, T.B.; Santarosa, M.; Dillon, K.J.; Hickson, I.; Knights, C.; et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 2005, 434, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.J.; Ashworth, A. PARP inhibitors: Synthetic lethality in the clinic. Science 2017, 355, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Khaddour, K.; Felipe Fernandez, M.; Khabibov, M.; Garifullin, A.; Dressler, D.; Topchu, I.; Patel, J.D.; Weinberg, F.; Boumber, Y. The Prognostic and Therapeutic Potential of DNA Damage Repair Pathway Alterations and Homologous Recombination Deficiency in Lung Cancer. Cancers 2022, 14, 5305. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.-C.; Chang, Y.-H.; Chang, G.-C.; Ho, B.-C.; Yuan, S.-S.; Li, Y.-C.; Zeng, J.-W.; Yu, S.-L.; Li, K.-C.; Yang, P.-C.; et al. Tumor mutation burden and recurrent tumors in hereditary lung cancer. Cancer Med. 2019, 8, 2179–2187. [Google Scholar] [CrossRef]
- Maiorano, B.A.; Lorusso, D.; Maiorano, M.F.P.; Ciardiello, D.; Parrella, P.; Petracca, A.; Cormio, G.; Maiello, E. The Interplay between PARP Inhibitors and Immunotherapy in Ovarian Cancer: The Rationale behind a New Combination Therapy. Int. J. Mol. Sci. 2022, 23, 3871. [Google Scholar] [CrossRef]
- Dias, M.P.; Moser, S.C.; Ganesan, S.; Jonkers, J. Understanding and overcoming resistance to PARP inhibitors in cancer therapy. Nat. Rev. Clin. Oncol. 2021, 19, 773–791. [Google Scholar] [CrossRef]
- Lord, C.J.; Ashworth, A. BRCAness revisited. Nat. Rev. Cancer 2016, 16, 110–120. [Google Scholar] [CrossRef]
- Yang, P.S.; Chao, Y.T.; Lung, C.F.; Liu, C.L.; Chang, Y.C.; Li, K.C.; Hsu, Y.C. Association of Pathway Mutations With Survival in Taiwanese Breast Cancers. Front. Oncol. 2022, 12, 819555. [Google Scholar] [CrossRef]
- Ricciuti, B.; Recondo, G.; Spurr, L.F.; Li, Y.Y.; Lamberti, G.; Venkatraman, D.; Umeton, R.; Cherniack, A.D.; Nishino, M.; Sholl, L.M.; et al. Impact of DNA Damage Response and Repair (DDR) Gene Mutations on Efficacy of PD-(L)1 Immune Checkpoint Inhibition in Non-Small Cell Lung Cancer. Clin. Cancer Res. 2020, 26, 4135–4142. [Google Scholar] [CrossRef]
- Kim, D.-S.; Camacho, C.V.; Kraus, W.L. Alternate therapeutic pathways for PARP inhibitors and potential mechanisms of resistance. Exp. Mol. Med. 2021, 53, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Rose, M.; Burgess, J.T.; O’Byrne, K.; Richard, D.J.; Bolderson, E. PARP Inhibitors: Clinical Relevance, Mechanisms of Action and Tumor Resistance. Front. Cell Dev. Biol. 2020, 8, 564601. [Google Scholar] [CrossRef] [PubMed]
- Dizon, S.D.; Powell, M.A. Perspectives on PARP Inhibitors in Ovarian Cancer: Has the Time Come for Individualized Care? 2014. Available online: https://www.medscape.org/viewarticle/830282_2 (accessed on 1 December 2022).
- Ledermann, J.; Harter, P.; Gourley, C.; Friedlander, M.; Vergote, I.; Rustin, G.; Scott, C.L.; Meier, W.; Shapira-Frommer, R.; Safra, T.; et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: A preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 2014, 15, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Pujade-Lauraine, E.; Ledermann, J.A.; Selle, F.; Gebski, V.; Penson, R.T.; Oza, A.M.; Korach, J.; Huzarski, T.; Poveda, A.; Pignata, S.; et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): A double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017, 18, 1274–1284. [Google Scholar] [CrossRef]
- Swisher, E.M.; Lin, K.K.; Oza, A.M.; Scott, C.L.; Giordano, H.; Sun, J.; Konecny, G.E.; Coleman, R.L.; Tinker, A.V.; O’Malley, D.M.; et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): An international, multicentre, open-label, phase 2 trial. Lancet Oncol. 2017, 18, 75–87. [Google Scholar] [CrossRef]
- de Bono, J.; Mateo, J.; Fizazi, K.; Saad, F.; Shore, N.; Sandhu, S.; Chi, K.N.; Sartor, O.; Agarwal, N.; Olmos, D.; et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2020, 382, 2091–2102. [Google Scholar] [CrossRef]
- Chi, J.; Chung, S.Y.; Prasad, S.; Saif, M.W. The Role of Olaparib in Metastatic Pancreatic Cancer. Cancer Med. J. 2021, 4, 89–91. [Google Scholar]
- Dréan, A.; Williamson, C.T.; Brough, R.; Brandsma, I.; Menon, M.; Konde, A.; Garcia-Murillas, I.; Pemberton, H.N.; Frankum, J.; Rafiq, R.; et al. Modeling Therapy Resistance in BRCA1/2-Mutant Cancers. Mol. Cancer Ther. 2017, 16, 2022–2034. [Google Scholar] [CrossRef]
- Brown, J.S.; Kaye, S.B.; Yap, T.A. PARP inhibitors: The race is on. Br. J. Cancer 2016, 114, 713–715. [Google Scholar] [CrossRef]
- Fennell, D.A.; Lester, J.F.; Danson, S.; Blackhall, F.H.; Nicolson, M.; Nixon, L.S.; Porter, C.; Gardner, G.M.; White, A.; Griffiths, G.O.; et al. A randomized phase II trial of olaparib maintenance versus placebo monotherapy in patients with chemosensitive advanced non-small cell lung cancer. J. Clin. Oncol. 2020, 38, e21649. [Google Scholar] [CrossRef]
- Riess, J.W.; Redman, M.W.; Wheatley-Price, P.; Faller, B.A.; Villaruz, L.C.; Corum, L.R.; Gowda, A.C.; Srkalovic, G.; Osarogiagbon, R.U.; Baumgart, M.A.; et al. A phase II study of rucaparib in patients with high genomic LOH and/or BRCA 1/2 mutated stage IV non-small cell lung cancer (Lung-MAP Sub-Study, S1900A). J. Clin. Oncol. 2021, 39, 9024. [Google Scholar] [CrossRef]
- Eikesdal, H.P.; Yndestad, S.; Elzawahry, A.; Llop-Guevara, A.; Gilje, B.; Blix, E.S.; Espelid, H.; Lundgren, S.; Geisler, J.; Vagstad, G.; et al. Olaparib monotherapy as primary treatment in unselected triple negative breast cancer. Ann. Oncol. 2021, 32, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Spring, L.M.; Han, H.; Liu, M.C.; Hamilton, E.; Irie, H.; Santa-Maria, C.A.; Reeves, J.; Pan, P.; Shan, M.; Tang, Y.; et al. Neoadjuvant study of niraparib in patients with HER2-negative, BRCA-mutated, resectable breast cancer. Nat. Cancer 2022, 3, 927–931. [Google Scholar] [CrossRef] [PubMed]
- Fasching, P.A.; Link, T.; Hauke, J.; Seither, F.; Jackisch, C.; Klare, P.; Schmatloch, S.; Hanusch, C.; Huober, J.; Stefek, A.; et al. Neoadjuvant paclitaxel/olaparib in comparison to paclitaxel/carboplatinum in patients with HER2-negative breast cancer and homologous recombination deficiency (GeparOLA study). Ann. Oncol. 2021, 32, 49–57. [Google Scholar] [CrossRef]
- Litton, J.K.; Scoggins, M.E.; Hess, K.R.; Adrada, B.E.; Murthy, R.K.; Damodaran, S.; DeSnyder, S.M.; Brewster, A.M.; Barcenas, C.H.; Valero, V.; et al. Neoadjuvant Talazoparib for Patients With Operable Breast Cancer With a Germline BRCA Pathogenic Variant. J. Clin. Oncol. 2020, 38, 388–394. [Google Scholar] [CrossRef]
- Pusztai, L.; Yau, C.; Wolf, D.M.; Han, H.S.; Du, L.; Wallace, A.M.; String-Reasor, E.; Boughey, J.C.; Chien, A.J.; Elias, A.D.; et al. Durvalumab with olaparib and paclitaxel for high-risk HER2-negative stage II/III breast cancer: Results from the adaptively randomized I-SPY2 trial. Cancer Cell 2021, 39, 989–998.e985. [Google Scholar] [CrossRef]
- Loibl, S.; O’Shaughnessy, J.; Untch, M.; Sikov, W.M.; Rugo, H.S.; McKee, M.D.; Huober, J.; Golshan, M.; von Minckwitz, G.; Maag, D.; et al. Addition of the PARP inhibitor veliparib plus carboplatin or carboplatin alone to standard neoadjuvant chemotherapy in triple-negative breast cancer (BrighTNess): A randomised, phase 3 trial. Lancet Oncol. 2018, 19, 497–509. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Abemaciclib and Niraparib before Surgery for the Treatment of Hormone Receptor Positive HER2 Negative Breast Cancer. NCT04481113. Available online: https://clinicaltrials.gov/ct2/show/NCT04481113?term=niraparib+neoadjuvant&draw=2&rank=6. (accessed on 1 December 2022).
- ClinicalTrials.gov. Genomic Biomarker-Selected Umbrella Neoadjuvant Study for High Risk Localized Prostate Cancer (GUNS). NCT04812366. Available online: https://clinicaltrials.gov/ct2/show/NCT04812366?term=niraparib+neoadjuvant&draw=2&rank=9. (accessed on 1 December 2022).
- ClinicalTrials.gov. Platinum and Polyadenosine 5′Diphosphoribose Polymerisation Inhibitor for Neoadjuvant Treatment of Triple Negative Breast Cancer and/or Germline BRCA Positive Breast Cancer (PARTNER). NCT03150576. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03150576?term=olaparib+neoadjuvant&draw=2&rank=3. (accessed on 1 December 2022).
- ClinicalTrials.gov. A Study of Olaparib Prior to Surgery and Chemotherapy in Ovarian, Primary Peritoneal, and Fallopian Tube Cancer (NEO). NCT02489006. Available online: https://clinicaltrials.gov/ct2/show/results/NCT02489006?term=olaparib+neoadjuvant&draw=2&rank=8. (accessed on 1 December 2022).
- ClinicalTrials.gov. Study of Neoadjuvant PARP Inhibition Followed by Radical Prostatectomy in Patients With Unfavorable Intermediate-Risk or High-Risk Prostate Cancer With BRCA1/2 Gene Alterations (NePtune). NCT05498272. Available online: https://clinicaltrials.gov/ct2/show/study/NCT05498272?term=olaparib+neoadjuvant&draw=2&rank=10. (accessed on 1 December 2022).
- ClinicalTrials.gov. The NUVOLA TRIAL: Neoadjuvant Chemotherapy in Unresectable oVarian Cancer With OLAparib and Weekly Carboplatin Plus Paclitaxel: A Phase II Open-label Multicentre Study. NCT04261465. Available online: https://clinicaltrials.gov/ct2/show/NCT04261465?term=olaparib+neoadjuvant&draw=3&rank=13. (accessed on 1 December 2022).
- Peyraud, F.; Italiano, A. Combined PARP Inhibition and Immune Checkpoint Therapy in Solid Tumors. Cancers 2020, 12, 1502. [Google Scholar] [CrossRef]
- Li, A.; Yi, M.; Qin, S.; Chu, Q.; Luo, S.; Wu, K. Prospects for combining immune checkpoint blockade with PARP inhibition. J. Hematol. Oncol. 2019, 12. [Google Scholar] [CrossRef]
- Wu, Z.; Cui, P.; Tao, H.; Zhang, S.; Ma, J.; Liu, Z.; Wang, J.; Qian, Y.; Chen, S.; Huang, Z.; et al. The Synergistic Effect of PARP Inhibitors and Immune Checkpoint Inhibitors. Clin. Med. Insights Oncol. 2021, 15, 1179554921996288. [Google Scholar] [CrossRef]
- Sato, H.; Niimi, A.; Yasuhara, T.; Permata, T.B.M.; Hagiwara, Y.; Isono, M.; Nuryadi, E.; Sekine, R.; Oike, T.; Kakoti, S.; et al. DNA double-strand break repair pathway regulates PD-L1 expression in cancer cells. Nat. Commun. 2017, 8, 1751. [Google Scholar] [CrossRef] [PubMed]
- Tangutoori, S.; Baldwin, P.; Sridhar, S. PARP inhibitors: A new era of targeted therapy. Maturitas 2015, 81, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Mouw, K.W.; Goldberg, M.S.; Konstantinopoulos, P.A.; D’Andrea, A.D. DNA Damage and Repair Biomarkers of Immunotherapy Response. Cancer Discov. 2017, 7, 675–693. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, M.S.; Bartelink, I.H.; Aggarwal, R.R.; Leng, J.; Zhang, J.Z.; Pawlowska, N.; Terranova-Barberio, M.; Grabowsky, J.A.; Gewitz, A.; Chien, A.J.; et al. Differential Toxicity in Patients with and without DNA Repair Mutations: Phase I Study of Carboplatin and Talazoparib in Advanced Solid Tumors. Clin. Cancer Res. 2017, 23, 6400–6410. [Google Scholar] [CrossRef] [PubMed]
- Konstantinopoulos, P.A.; Waggoner, S.E.; Vidal, G.A.; Mita, M.M.; Fleming, G.F.; Holloway, R.W.; Van Le, L.; Sachdev, J.C.; Chapman-Davis, E.; Colon-Otero, G.; et al. TOPACIO/Keynote-162 (NCT02657889): A phase 1/2 study of niraparib + pembrolizumab in patients (pts) with advanced triple-negative breast cancer or recurrent ovarian cancer (ROC)—Results from ROC cohort. J. Clin. Oncol. 2018, 36, 106. [Google Scholar] [CrossRef]
- Vinayak, S.; Tolaney, S.M.; Schwartzberg, L.; Mita, M.; McCann, G.; Tan, A.R.; Wahner-Hendrickson, A.E.; Forero, A.; Anders, C.; Wulf, G.M.; et al. Open-label Clinical Trial of Niraparib Combined With Pembrolizumab for Treatment of Advanced or Metastatic Triple-Negative Breast Cancer. JAMA Oncol. 2019, 5, 1132–1140. [Google Scholar] [CrossRef] [PubMed]
- Drew, Y.; Kaufman, B.; Banerjee, S.; Lortholary, A.; Hong, S.H.; Park, Y.H.; Zimmermann, S.; Roxburgh, P.; Ferguson, M.; Alvarez, R.H.; et al. Phase II study of olaparib + durvalumab (MEDIOLA): Updated results in germline BRCA-mutated platinum-sensitive relapsed (PSR) ovarian cancer (OC). Ann. Oncol. 2019, 30, v475–v532. [Google Scholar] [CrossRef]
- Bang, Y.-J.; Kaufman, B.; Geva, R.; Stemmer, S.M.; Hong, S.-H.; Lee, J.-S.; Domchek, S.M.; Lanasa, M.C.; Tang, M.; Gresty, C.; et al. An open-label, phase II basket study of olaparib and durvalumab (MEDIOLA): Results in patients with relapsed gastric cancer. J. Clin. Oncol. 2019, 37, 140. [Google Scholar] [CrossRef]
- Ramalingam, S.S.; Thara, E.; Awad, M.M.; Dowlati, A.; Haque, B.; Stinchcombe, T.E.; Dy, G.K.; Spigel, D.R.; Lu, S.; Iyer Singh, N.; et al. JASPER: Phase 2 trial of first-line niraparib plus pembrolizumab in patients with advanced non-small cell lung cancer. Cancer 2022, 128, 65–74. [Google Scholar] [CrossRef]
- Yap, T.A.; Bardia, A.; Dvorkin, M.; Galsky, M.D.; Beck, J.T.; Wise, D.R.; Karyakin, O.; Rubovszky, G.; Kislov, N.; Rohrberg, K.; et al. Avelumab Plus Talazoparib in Patients With Advanced Solid Tumors: The JAVELIN PARP Medley Nonrandomized Controlled Trial. JAMA Oncol. 2022. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. A Phase II Study of Niraparib With Dostarlimab Therapy as Neoadjuvant Treatment for Patients With BRCA-mutated Breast Cancer. NCT04584255. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04584255?term=niraparib+neoadjuvant&draw=2&rank=5. (accessed on 1 December 2022).
- ClinicalTrials.gov. Study of Neoadjuvant Olaparib Monotherapy and Olaparib and Durvalumab Combination in HER2 Negative BRCAm Breast Cancer (OlympiaN). NCT05498155. Available online: https://clinicaltrials.gov/ct2/show/NCT05498155?term=olaparib+neoadjuvant&draw=2. (accessed on 1 December 2022).
- ClinicalTrials.gov. Neoadjuvant and Adjuvant Olaparib Plus Pembrolizumab Following Platinum Based Chemotherapy Plus Pembrolizumab for Germline BRCA Mutated Triple Negative Breast Cancer (WJOG14020B). NCT05485766. Available online: https://clinicaltrials.gov/ct2/show/NCT05485766?term=olaparib+neoadjuvant&draw=2&rank=2. (accessed on 1 December 2022).
- ClinicalTrials.gov. Chemo-free BRCA-targeted Neoadjuvant Strategy. NCT05209529. Available online: https://clinicaltrials.gov/ct2/show/NCT05209529?term=olaparib+neoadjuvant&draw=2&rank=5. (accessed on 12 January 2023).
- ClinicalTrials.gov. Durvalumab Plus Olaparib Administered Prior to Surgery of Resectable Urothelial Bladder Cancer (NEODURVARIB). NCT05203445. Available online: https://clinicaltrials.gov/ct2/show/study/NCT05203445?term=olaparib+neoadjuvant&draw=3&rank=17. (accessed on 12 January 2023).
- ClinicalTrials.gov. Olaparib in Treating Patients With Newly Diagnosed BRCA-Mutant Ovarian, Primary Peritoneal, or Fallopian Cancer Before Surgery. NCT03943173. Available online: https://clinicaltrials.gov/ct2/show/results/NCT03943173?term=olaparib+neoadjuvant&draw=3&rank=18. (accessed on 12 January 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, M.P.; Oliveira, C.; Sousa, H.; Oliveira, J. New Approaches in Early-Stage NSCL Management: Potential Use of PARP Inhibitors and Immunotherapy Combination. Int. J. Mol. Sci. 2023, 24, 4044. https://doi.org/10.3390/ijms24044044
Fernandes MP, Oliveira C, Sousa H, Oliveira J. New Approaches in Early-Stage NSCL Management: Potential Use of PARP Inhibitors and Immunotherapy Combination. International Journal of Molecular Sciences. 2023; 24(4):4044. https://doi.org/10.3390/ijms24044044
Chicago/Turabian StyleFernandes, Marta Pina, Cristina Oliveira, Hugo Sousa, and Júlio Oliveira. 2023. "New Approaches in Early-Stage NSCL Management: Potential Use of PARP Inhibitors and Immunotherapy Combination" International Journal of Molecular Sciences 24, no. 4: 4044. https://doi.org/10.3390/ijms24044044
APA StyleFernandes, M. P., Oliveira, C., Sousa, H., & Oliveira, J. (2023). New Approaches in Early-Stage NSCL Management: Potential Use of PARP Inhibitors and Immunotherapy Combination. International Journal of Molecular Sciences, 24(4), 4044. https://doi.org/10.3390/ijms24044044