Effect of PACAP on Heat Exposure
Abstract
1. Introduction
2. Results
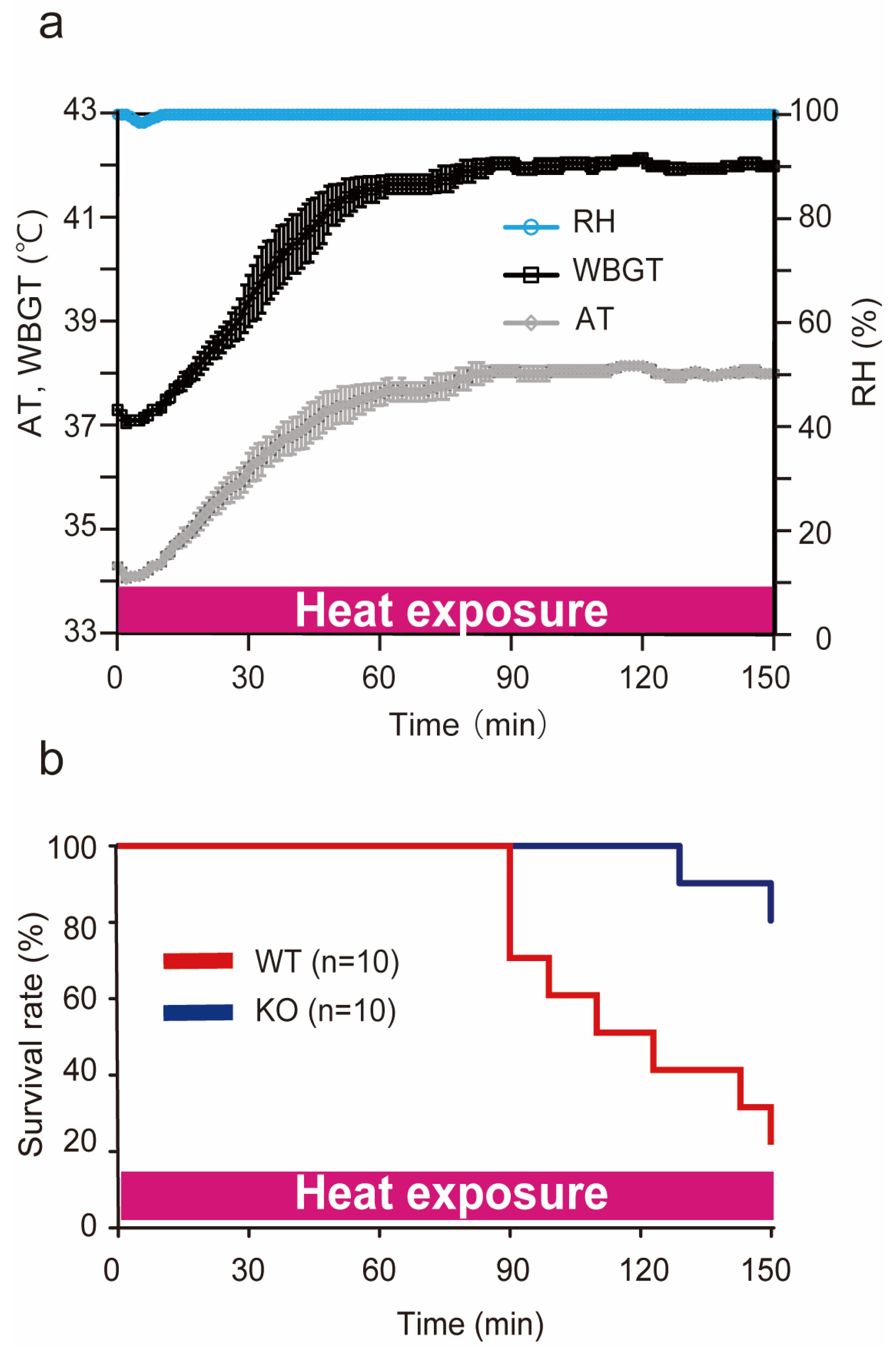
2.1. Conditions of Heat Stroke on ICR Mice
2.2. Survival Rate during Heat Exposure
2.3. Impact of Heat Exposure on Blood Count and Serum Biochemical Parameters
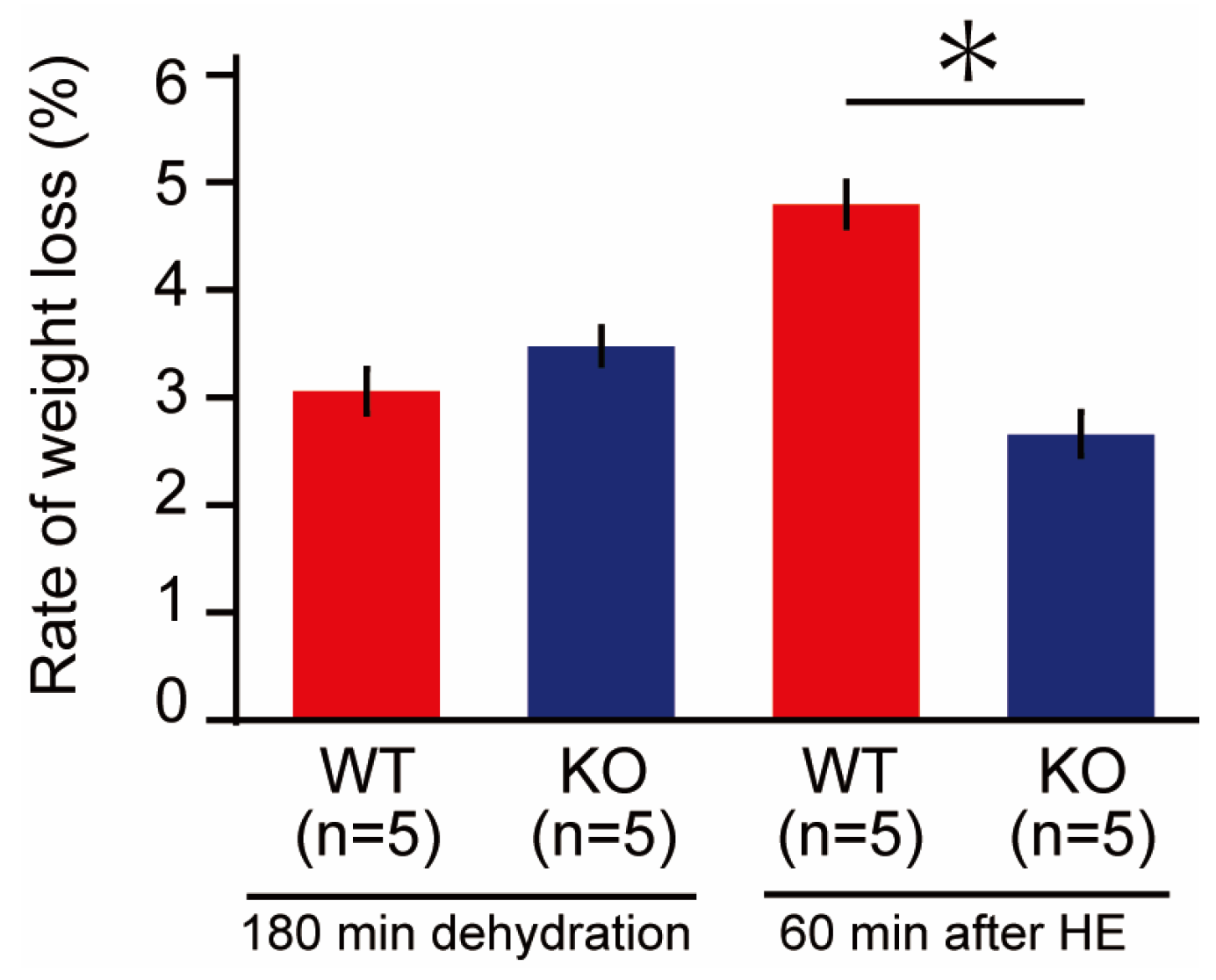
2.4. Weight Loss before and after Heat Exposure
2.5. Morphological Observation in Liver and Kidney after 60 min of Heat Exposure
2.6. Changes in Core Body Temperature in Wild-Type and PACAP KO Mice
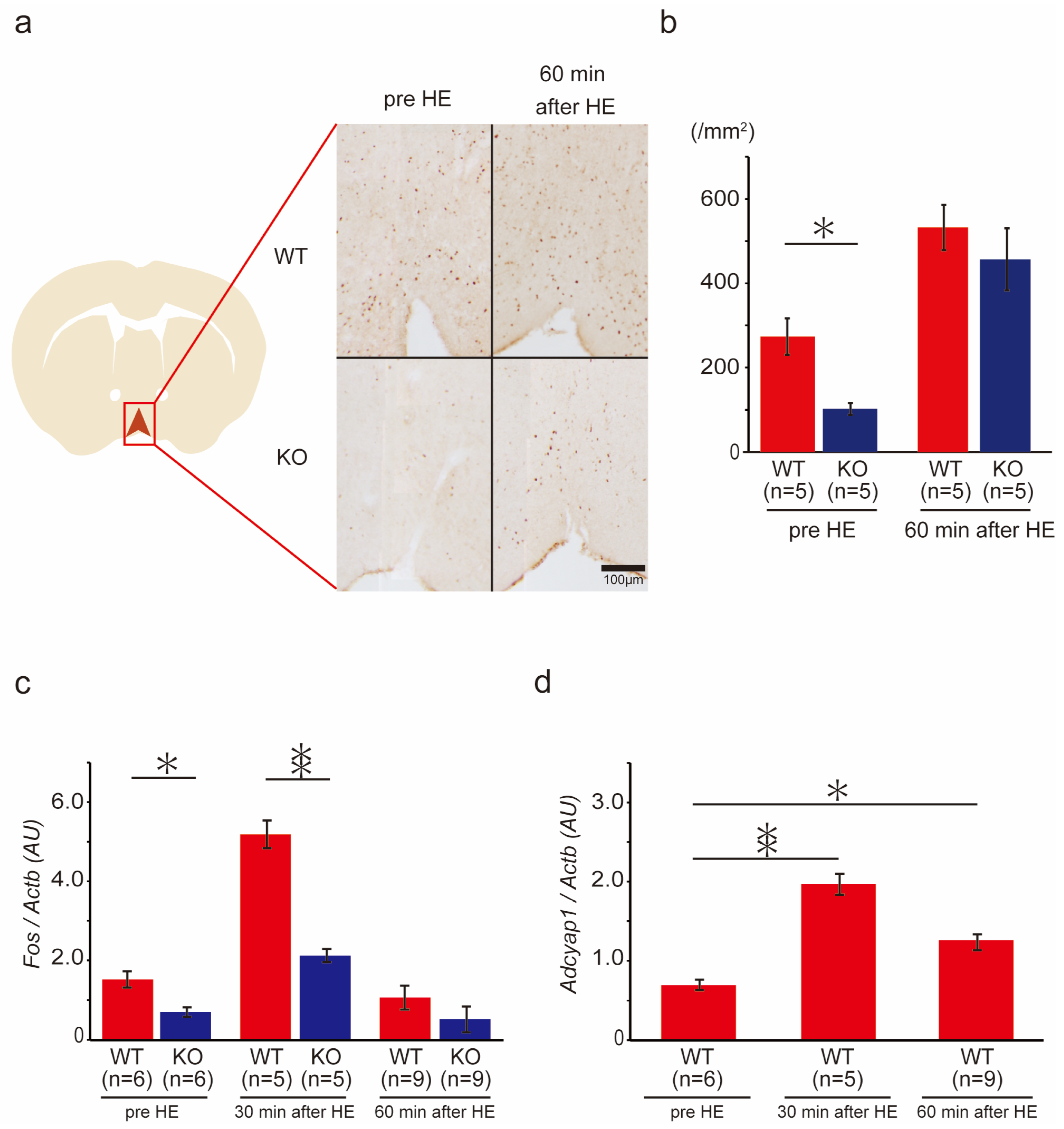
2.7. c-Fos Gene and Protein Expression in the Ventral Medial Preoptic Area (VMPO) of the Hypothalamus in Wild-Type and PACAP KO Mice after Heat Exposure
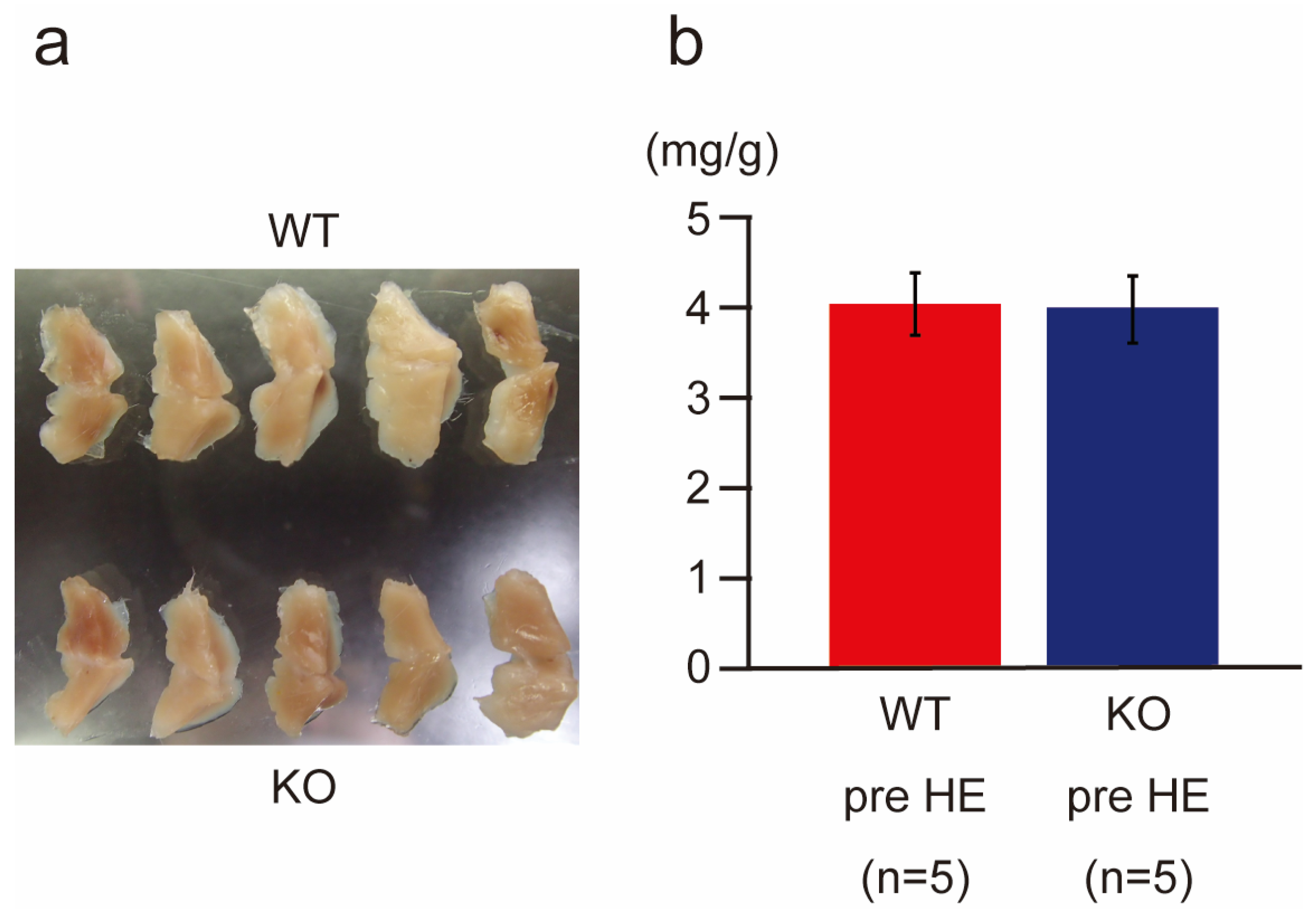
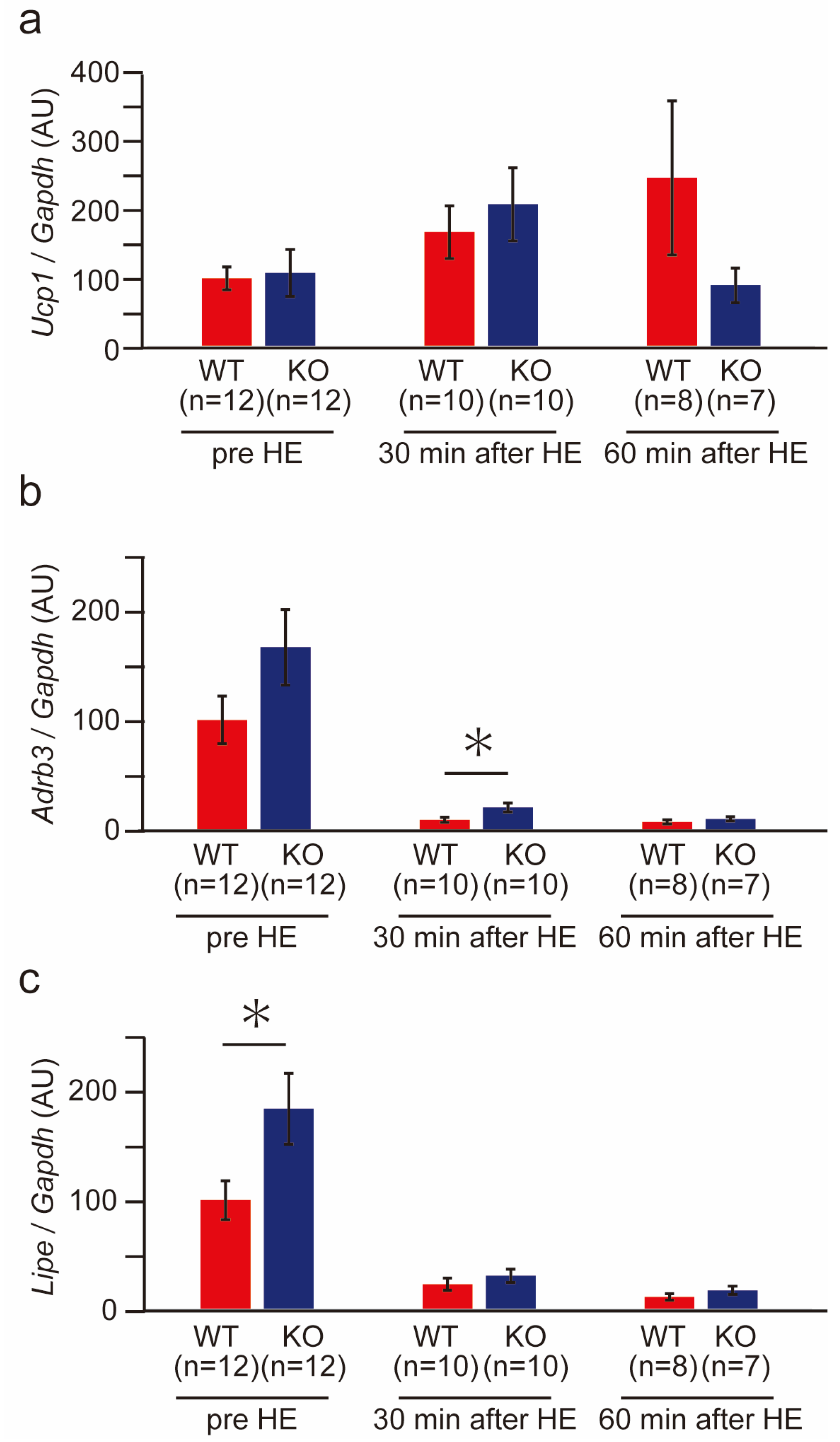
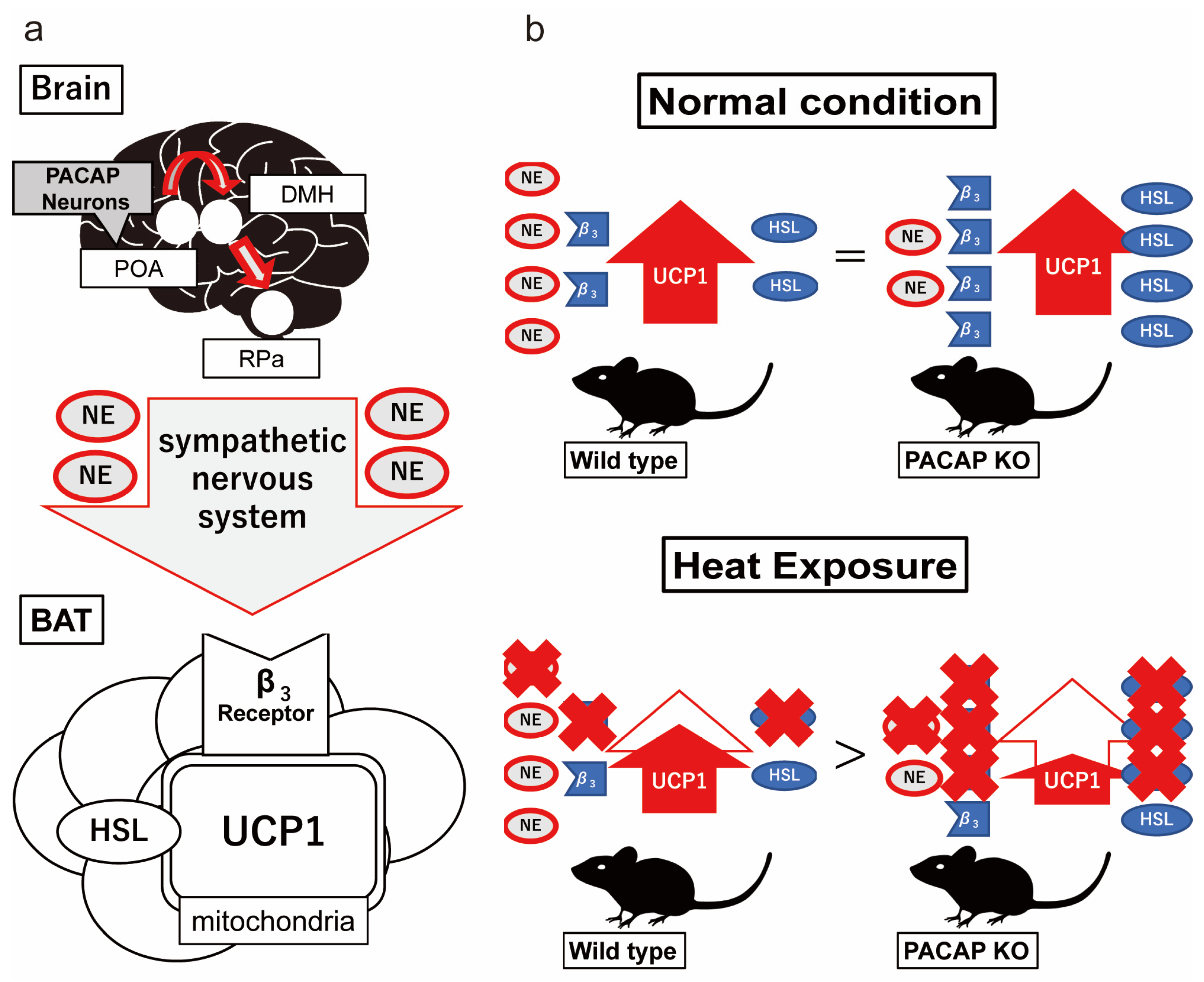
2.8. BAT Weight and Thermogenesis-Related Gene Expression in Wild-Type and PACAP KO Mice after Heat Exposure
3. Discussion
4. Materials and Methods
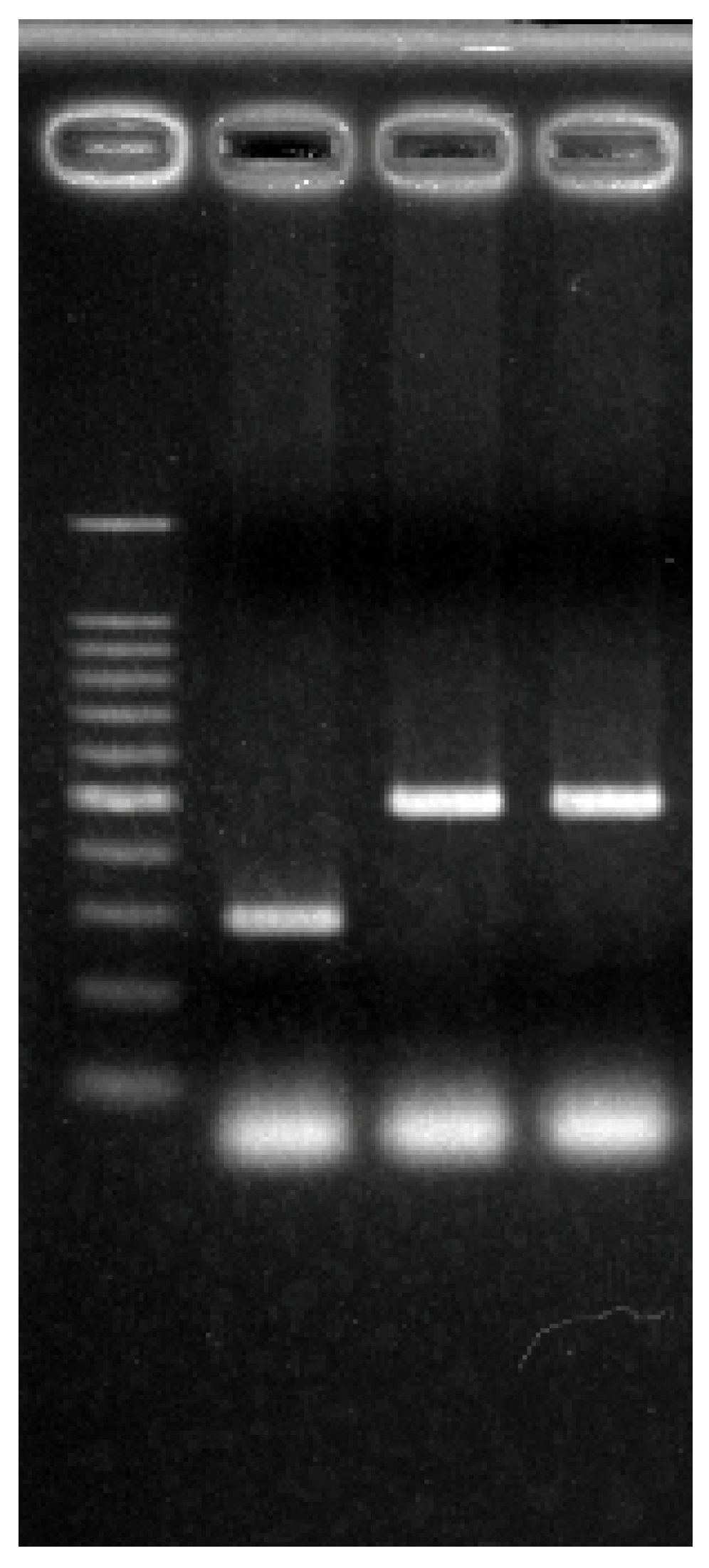
4.1. Animals
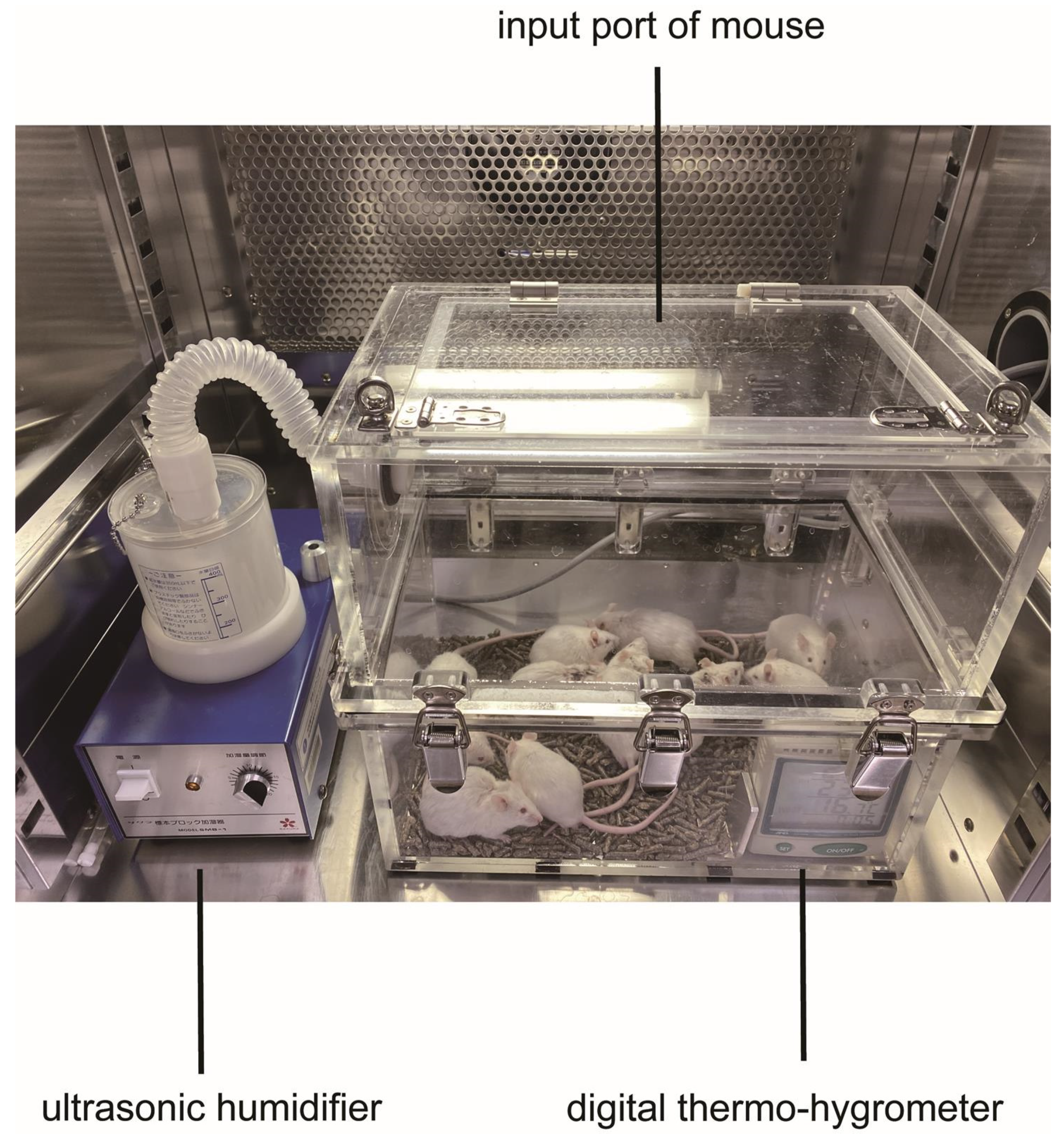
4.2. Heat Stroke Model
4.3. Examination of Survival Rate
4.4. Preparation of Histological Samples and Morphological Observation
4.5. CBC and Biochemical Parameters in Serum
4.6. Measurement of Core Body Temperature
4.7. Immunohistochemistry and Cell Count of Hypothalamus
4.8. Polymerase Chain Reaction (PCR)
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meehl, G.A.; Tebaldi, C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Fujita, M.; Oda, Y.; Todani, M.; Hifumi, T.; Kondo, Y.; Shimazaki, J.; Shiraishi, S.; Hayashida, K.; Yokobori, S.; et al. Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012). Int. J. Environ. Res. Public Health 2018, 15, 1962. [Google Scholar] [CrossRef] [PubMed]
- Bouchama, A.; Knochel, J.P. Heat stroke. N. Engl. J. Med. 2002, 346, 1978–1988. [Google Scholar] [CrossRef] [PubMed]
- Epstein, Y.; Yanovich, R. Heatstroke. N. Engl. J. Med. 2019, 380, 2449–2459. [Google Scholar] [CrossRef]
- Hausmann, J.S.; Berna, R.; Gujral, N.; Ayubi, S.; Hawkins, J.; Brownstein, J.S.; Dedeoglu, F. Using Smartphone Crowdsourcing to Redefine Normal and Febrile Temperatures in Adults: Results from the Feverprints Study. J. Gen. Intern. Med. 2018, 33, 2046–2047. [Google Scholar] [CrossRef]
- Cannon, B.; Nedergaard, J. Brown adipose tissue: Function and physiological significance. Physiol. Rev. 2004, 84, 277–359. [Google Scholar] [CrossRef]
- Bi, S.; Li, L. Browning of white adipose tissue: Role of hypothalamic signaling. Ann. N. Y. Acad. Sci. 2013, 1302, 30–34. [Google Scholar] [CrossRef]
- Miyamoto, K.; Suzuki, K.; Ohtaki, H.; Nakamura, M.; Yamaga, H.; Yagi, M.; Honda, K.; Hayashi, M.; Dohi, K. A novel mouse model of heatstroke accounting for ambient temperature and relative humidity. J. Intensive Care 2021, 9, 35. [Google Scholar] [CrossRef]
- Miyamoto, K.; Nakamura, M.; Ohtaki, H.; Suzuki, K.; Yamaga, H.; Yanagisawa, K.; Maeda, A.; Yagi, M.; Hayashi, M.; Honda, K.; et al. Heatstroke-induced late-onset neurological deficits in mice caused by white matter demyelination, Purkinje cell degeneration, and synaptic impairment in the cerebellum. Sci. Rep. 2022, 12, 10598. [Google Scholar] [CrossRef]
- Miyata, A.; Arimura, A.; Dahl, R.R.; Minamino, N.; Uehara, A.; Jiang, L.; Culler, M.D.; Coy, D.H. Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem. Biophys. Res. Commun. 1989, 164, 567–574. [Google Scholar] [CrossRef]
- Winters, S.J.; Moore, J.P., Jr. PACAP: A regulator of mammalian reproductive function. Mol. Cell. Endocrinol. 2020, 518, 110912. [Google Scholar] [CrossRef]
- Vaudry, D.; Falluel-Morel, A.; Bourgault, S.; Basille, M.; Burel, D.; Wurtz, O.; Fournier, A.; Chow, B.K.C.; Hashimoto, H.; Galas, L.; et al. Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol. Rev. 2009, 61, 283–357. [Google Scholar] [CrossRef] [PubMed]
- Toth, D.; Szabo, E.; Tamas, A.; Juhasz, T.; Horvath, G.; Fabian, E.; Opper, B.; Szabo, D.; Maugeri, G.; D’Amico, A.G.; et al. Protective Effects of PACAP in Peripheral Organs. Front. Endocrinol. 2020, 11, 377. [Google Scholar] [CrossRef]
- Miyamoto, K.; Tsumuraya, T.; Ohtaki, H.; Dohi, K.; Satoh, K.; Xu, Z.; Tanaka, S.; Murai, N.; Watanabe, J.; Sugiyama, K.; et al. PACAP38 suppresses cortical damage in mice with traumatic brain injury by enhancing antioxidant activity. J. Mol. Neurosci. 2014, 54, 370–379. [Google Scholar] [CrossRef]
- Tsumuraya, T.; Ohtaki, H.; Song, D.; Sato, A.; Watanabe, J.; Hiraizumi, Y.; Nakamachi, T.; Xu, Z.; Dohi, K.; Hashimoto, H.; et al. Human mesenchymal stem/stromal cells suppress spinal inflammation in mice with contribution of pituitary adenylate cyclase-activating polypeptide (PACAP). J. Neuroinflamm. 2015, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Ohtaki, H.; Nakamachi, T.; Dohi, K.; Aizawa, Y.; Takaki, A.; Hodoyama, K.; Yofu, S.; Hashimoto, H.; Shintani, N.; Baba, A.; et al. Pituitary adenylate cyclase-activating polypeptide (PACAP) decreases ischemic neuronal cell death in association with IL-6. Proc. Natl. Acad. Sci. USA 2006, 103, 7488–7493. [Google Scholar] [CrossRef] [PubMed]
- Ohtaki, H.; Nakamachi, T.; Dohi, K.; Shioda, S. Role of PACAP in ischemic neural death. J. Mol. Neurosci. 2008, 36, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Mori, H.; Nakamachi, T.; Ohtaki, H.; Yofu, S.; Sato, A.; Endo, K.; Iso, Y.; Suzuki, H.; Takeyama, Y.; Shintani, N.; et al. Cardioprotective effect of endogenous pituitary adenylate cyclase-activating polypeptide on Doxorubicin-induced cardiomyopathy in mice. Circ. J. 2010, 74, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cao, L.; Yi, P.Q.; Xu, C.; Su, J.; Chen, P.Z.; Li, M.; Chen, J.Y. Pituitary adenylate cyclase-activating polypeptide ameliorates radiation-induced cardiac injury. Am. J. Transl. Res. 2019, 11, 6585–6599. [Google Scholar] [CrossRef]
- Ji, H.; Zhang, Y.; Shen, X.D.; Gao, F.; Huang, C.Y.; Abad, C.; Busuttil, R.W.; Waschek, J.A.; Kupiec-Weglinski, J.W. Neuropeptide PACAP in mouse liver ischemia and reperfusion injury: Immunomodulation by the cAMP-PKA pathway. Hepatology 2013, 57, 1225–1237. [Google Scholar] [CrossRef]
- Liu, Y.; Lu, T.; Zhang, C.; Xue, Z.; Xu, J.; Busuttil, R.W.; Xia, Q.; Xu, N.; Kupiec-Weglinski, J.W.; Ji, H. Pituitary Adenylate Cyclase-activating Polypeptides Prevent Hepatocyte Damage by Promoting Yes-associated Protein in Liver Ischemia-Reperfusion Injury. Transplantation 2019, 103, 1639–1648. [Google Scholar] [CrossRef]
- Laszlo, E.; Juhasz, T.; Varga, A.; Czibere, B.; Kovacs, K.; Degrell, P.; Horvath, G.; Jancso, G.; Szakaly, P.; Tamas, A.; et al. Protective Effect of PACAP on Ischemia/Reperfusion-Induced Kidney Injury of Male and Female Rats: Gender Differences. J. Mol. Neurosci. 2019, 68, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Heimesaat, M.M.; Mousavi, S.; Kløve, S.; Genger, C.; Weschka, D.; Tamas, A.; Reglodi, D.; Bereswill, S. Pituitary Adenylate Cyclase-Activating Polypeptide Alleviates Intestinal, Extra-Intestinal and Systemic Inflammatory Responses during Acute Campylobacter jejuni-induced Enterocolitis in Mice. Pathogens 2020, 9, 805. [Google Scholar] [CrossRef]
- Gray, S.L.; Yamaguchi, N.; Vencová, P.; Sherwood, N.M. Temperature-sensitive phenotype in mice lacking pituitary adenylate cyclase-activating polypeptide. Endocrinology 2002, 143, 3946–3954. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.L.; Cooke, E.K.; Leib, D.E.; Lin, Y.C.; Daly, G.E.; Zimmerman, C.A.; Knight, Z.A. Warm-Sensitive Neurons that Control Body Temperature. Cell 2016, 167, 47–59.e15. [Google Scholar] [CrossRef]
- Takahashi, T.M.; Sunagawa, G.A.; Soya, S.; Abe, M.; Sakurai, K.; Ishikawa, K.; Yanagisawa, M.; Hama, H.; Hasegawa, E.; Miyawaki, A.; et al. A discrete neuronal circuit induces a hibernation-like state in rodents. Nature 2020, 583, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Hrvatin, S.; Sun, S.; Wilcox, O.F.; Yao, H.; Lavin-Peter, A.J.; Cicconet, M.; Assad, E.G.; Palmer, M.E.; Aronson, S.; Banks, A.S.; et al. Neurons that regulate mouse torpor. Nature 2020, 583, 115–121. [Google Scholar] [CrossRef]
- Tsukiyama, N.; Saida, Y.; Kakuda, M.; Shintani, N.; Hayata, A.; Morita, Y.; Tanida, M.; Tajiri, M.; Hazama, K.; Ogata, K.; et al. PACAP centrally mediates emotional stress-induced corticosterone responses in mice. Stress 2011, 14, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Diané, A.; Nikolic, N.; Rudecki, A.P.; King, S.M.; Bowie, D.J.; Gray, S.L. PACAP is essential for the adaptive thermogenic response of brown adipose tissue to cold exposure. J. Endocrinol. 2014, 222, 327–339. [Google Scholar] [CrossRef]
- Yaglou, C.P.; Minard, D. Control of heat casualties at military training centers. AMA Arch. Ind. Health 1957, 16, 302–316. [Google Scholar]
- Ramanathan, N.L.; Belding, H.S. Physiologic evaluation of the WBGT index for occupational heat stress. Am. Ind. Hyg. Assoc. J. 1973, 34, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Paxinos, G.; Franklin, K.B.J. The Mouse Brain in Stereotaxic Coordinates, 2nd ed.; Academic Press: San Diego, CA, USA, 2001. [Google Scholar]
- Hifumi, T.; Kondo, Y.; Shimizu, K.; Miyake, Y. Heat stroke. J. Intensive Care 2018, 6, 30. [Google Scholar] [CrossRef]
- Walter, E.J.; Hanna-Jumma, S.; Carraretto, M.; Forni, L. The pathophysiological basis and consequences of fever. Crit. Care 2016, 20, 200. [Google Scholar] [CrossRef]
- Hildebrandt, B.; Wust, P.; Ahlers, O.; Dieing, A.; Sreenivasa, G.; Kerner, T.; Felix, R.; Riess, H. The cellular and molecular basis of hyperthermia. Crit. Rev. Oncol. Hematol. 2002, 43, 33–56. [Google Scholar] [CrossRef] [PubMed]
- Roti Roti, J.L. Cellular responses to hyperthermia (40–46 degrees C): Cell killing and molecular events. Int. J. Hyperth. 2008, 24, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Banki, E.; Pakai, E.; Gaszner, B.; Zsiboras, C.; Czett, A.; Bhuddi, P.R.; Hashimoto, H.; Toth, G.; Tamas, A.; Reglodi, D.; et al. Characterization of the thermoregulatory response to pituitary adenylate cyclase-activating polypeptide in rodents. J. Mol. Neurosci. 2014, 54, 543–554. [Google Scholar] [CrossRef]
- Hashimoto, H.; Shintani, N.; Tanaka, K.; Mori, W.; Hirose, M.; Matsuda, T.; Sakaue, M.; Miyazaki, J.; Niwa, H.; Yamamoto, K.; et al. Altered psychomotor behaviors in mice lacking pituitary adenylate cyclase-activating polypeptide (PACAP). Proc. Natl. Acad. Sci. USA 2001, 98, 13355–13360. [Google Scholar] [CrossRef]
- Derry, D.M.; Daniel, H. Sympathetic nerve development in the brown adipose tissue of the rat. Can. J. Physiol. Pharmacol. 1970, 48, 160–168. [Google Scholar]
- Lowell, B.B.; Spiegelman, B.M. Towards a molecular understanding of adaptive thermogenesis. Nature 2000, 404, 652–660. [Google Scholar] [CrossRef]
- Morrison, S.F.; Nakamura, K. Central Mechanisms for Thermoregulation. Annu. Rev. Physiol. 2019, 81, 285–308. [Google Scholar] [CrossRef]
- Saper, C.B.; Machado, N.L.S. Flipping the Switch on the Body’s Thermoregulatory System. Nature 2020, 583, 34–35. [Google Scholar] [CrossRef] [PubMed]
- Tsay, H.J.; Li, H.Y.; Lin, C.H.; Yang, Y.L.; Yeh, J.Y.; Lin, M.T. Heatstroke induces c-fos expression in the rat hypothalamus. Neurosci. Lett. 1999, 262, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Gray, S.L.; Cummings, K.J.; Jirik, F.R.; Sherwood, N.M. Targeted disruption of the pituitary adenylate cyclase-activating polypeptide gene results in early postnatal death associated with dysfunction of lipid and carbohydrate metabolism. Mol. Endocrinol. 2001, 15, 1739–1747. [Google Scholar] [CrossRef] [PubMed]
- Rudecki, A.P.; Gray, S.L. PACAP in the Defense of Energy Homeostasis. Trends Endocrinol. Metab. 2016, 27, 620–632. [Google Scholar] [CrossRef]
- Adams, B.A.; Gray, S.L.; Isaac, E.R.; Bianco, A.C.; Vidal-Puig, A.J.; Sherwood, N.M. Feeding and metabolism in mice lacking pituitary adenylate cyclase-activating polypeptide. Endocrinology 2008, 149, 1571–1580. [Google Scholar] [CrossRef]
- Filatov, E.; Short, L.I.; Forster, M.A.M.; Harris, S.S.; Schien, E.N.; Hughes, M.C.; Cline, D.L.; Appleby, C.J.; Gray, S.L. Contribution of thermogenic mechanisms by male and female mice lacking pituitary adenylate cyclase-activating polypeptide in response to cold acclimation. Am. J. Physiol. Endocrinol. Metab. 2021, 320, E475–E487. [Google Scholar] [CrossRef]
- Martinez-deMena, R.; Anedda, A.; Cadenas, S.; Obregon, M.J. TSH effects on thermogenesis in rat brown adipocytes. Mol. Cell. Endocrinol. 2015, 404, 151–158. [Google Scholar] [CrossRef]
- Okada, R.; Yamamoto, K.; Ito, Y.; Mochida, H.; Tonon, M.C.; Fournier, A.; Leprince, J.; Vaudry, H.; Kikuyama, S. VIP and PACAP stimulate TSH release from the bullfrog pituitary. Peptides 2007, 28, 1784–1789. [Google Scholar] [CrossRef]
- Watson, R.E., Jr.; Wiegand, S.J.; Clough, R.W.; Hoffman, G.E. Use of cryoprotectant to maintain long-term peptide immunoreactivity and tissue morphology. Peptides 1986, 7, 155–159. [Google Scholar] [CrossRef]


| pre HE | 60 min after HE | |||||
|---|---|---|---|---|---|---|
| WT (n = 5) | KO (n = 5) | p | WT (n = 5) | KO (n = 5) | p | |
| WBC × 106 (/L) | 3.0 ± 1.4 | 1.8 ± 0.6 | 3.3 ± 0.8 | 5.3 ± 3.3 | ||
| RBC × 1012 (/L) | 10.2 ± 0.3 | 9.8 ± 0.2 | 11.4 ± 0.7 | 10.7 ± 0.1 | ||
| Hb (g/dL) | 15.0 ± 0.6 | 14.8 ± 0.4 | 20.0 ± 1.7 | 17.9 ± 0.3 | ||
| Hct (%) | 44.6 ± 1.1 | 44.5 ± 0.6 | 50.5 ± 2.9 | 46.1 ± 0.5 | ||
| Plt × 109 (/L) | 622.0 ± 39.2 | 591.0 ± 27.4 | 176.0 ± 43.0 | 491.0 ± 29.3 | ** | |
| Na (mmol/L) | 151.0 ± 0.9 | 153.0 ± 0.9 | 156.0 ± 2.2 | 151.0 ± 0.7 | ** | |
| K (mmol/L) | 6.6 ± 0.3 | 5.7 ± 0.8 | 6.4 ± 1.0 | 7.6 ± 0.4 | ||
| Cl (mmol/L) | 105.0 ± 1.0 | 106.0 ± 0.7 | 106.0 ± 2.2 | 112.0 ± 1.6 | ||
| TP (g/dL) | 4.7 ± 0.1 | 4.8 ± 0.1 | 5.3 ± 0.2 | 4.6 ± 0.1 | ** | |
| Alb (g/dL) | 2.6 ± 0.0 | 3.0 ± 0.1 | 3.4 ± 0.3 | 2.7 ± 0.1 | * | |
| AST (IU/L) | 68.0 ± 8.5 | 60.0 ± 6.0 | 390.0 ± 96.5 | 143.0 ± 17.9 | ** | |
| ALT (IU/L) | 34.0 ± 7.9 | 30.0 ± 5.8 | 172.0 ± 37.6 | 72.0 ± 22.1 | ||
| ALP (IU/L) | 141.0 ± 14.2 | 212.0 ± 22.2 | 216.0 ± 23.2 | 239.0 ± 21.5 | ||
| LDH (IU/L) | 323.0 ± 310.9 | 921.0 ± 91.2 | 3480.0 ± 1011.3 | 1057.0 ± 74.3 | * | |
| CK (IU/L) | 508.0 ± 147.4 | 747.0 ± 103.7 | 1515.0 ± 134.5 | 1088.0 ± 165.1 | * | |
| BUN (mg/dL) | 27.6 ± 1.1 | 26.5 ± 1.5 | 73.6 ± 5.2 | 30.7 ± 0.8 | ** | |
| Cre (mg/dL) | 0.1 ± 0.0 | 0.2 ± 0.0 | 0.4 ± 0.1 | 0.2 ± 0.0 | ** | |
| Name | Sequence | Size | |
|---|---|---|---|
| Adcyap1 | Forward | AACCCGCTGCAAGACTTCTATGAC | 125 |
| Reverse | TTAAGGATTTCGTGGGCGACA | ||
| Fos | Forward | CGGGTTTCAACGCCGACTA | 165 |
| Reverse | TTGGCACTAGAGACGGACAGA | ||
| Actb | Forward | GGCTGTATTCCCCTCCATCG | 154 |
| Reverse | CCAGTTGGTAACAATGCCATGT | ||
| Ucp1 | Forward | GTCAACAGCAAAAGCCACAA | 206 |
| Reverse | TCTGGGGTCAGAGGAAGAGA | ||
| Lipe | Forward | GGCTCACAGTTACCATCTCACC | 106 |
| Reverse | GAGTACCTTGCTGTCCTGTCC | ||
| Adrb3 | Forward | CAGCCAGCCCTGTTGA | 60 |
| Reverse | CCTTCATAGCCATCAA | ||
| Gapdh | Forward | TGTGTCCGTCGTGGATCTGA | 57 |
| Reverse | CCTGCTTCACCACCTTCTTGAT | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, K.; Yamaga, H.; Ohtaki, H.; Hirako, S.; Miyamoto, K.; Nakamura, M.; Yanagisawa, K.; Shimada, T.; Hosono, T.; Hashimoto, H.; et al. Effect of PACAP on Heat Exposure. Int. J. Mol. Sci. 2023, 24, 3992. https://doi.org/10.3390/ijms24043992
Suzuki K, Yamaga H, Ohtaki H, Hirako S, Miyamoto K, Nakamura M, Yanagisawa K, Shimada T, Hosono T, Hashimoto H, et al. Effect of PACAP on Heat Exposure. International Journal of Molecular Sciences. 2023; 24(4):3992. https://doi.org/10.3390/ijms24043992
Chicago/Turabian StyleSuzuki, Keisuke, Hiroki Yamaga, Hirokazu Ohtaki, Satoshi Hirako, Kazuyuki Miyamoto, Motoyasu Nakamura, Kaoru Yanagisawa, Takuya Shimada, Tomohiko Hosono, Hitoshi Hashimoto, and et al. 2023. "Effect of PACAP on Heat Exposure" International Journal of Molecular Sciences 24, no. 4: 3992. https://doi.org/10.3390/ijms24043992
APA StyleSuzuki, K., Yamaga, H., Ohtaki, H., Hirako, S., Miyamoto, K., Nakamura, M., Yanagisawa, K., Shimada, T., Hosono, T., Hashimoto, H., Honda, K., & Dohi, K. (2023). Effect of PACAP on Heat Exposure. International Journal of Molecular Sciences, 24(4), 3992. https://doi.org/10.3390/ijms24043992







