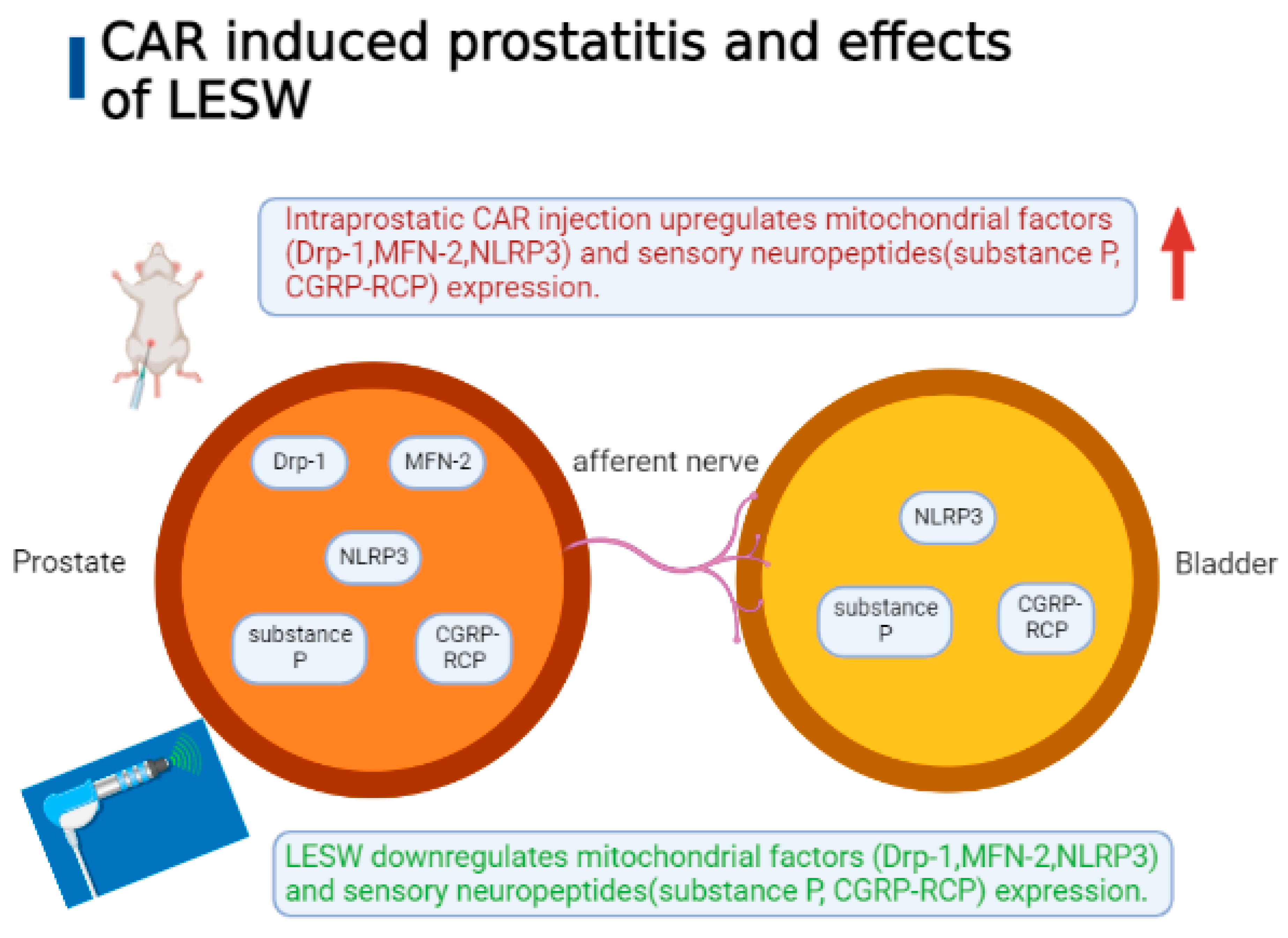
Low-Energy Shock Wave Suppresses Prostatic Pain and Inflammation by Modulating Mitochondrial Dynamics Regulators on a Carrageenan-Induced Prostatitis Model in Rats
Abstract
1. Introduction
2. Results
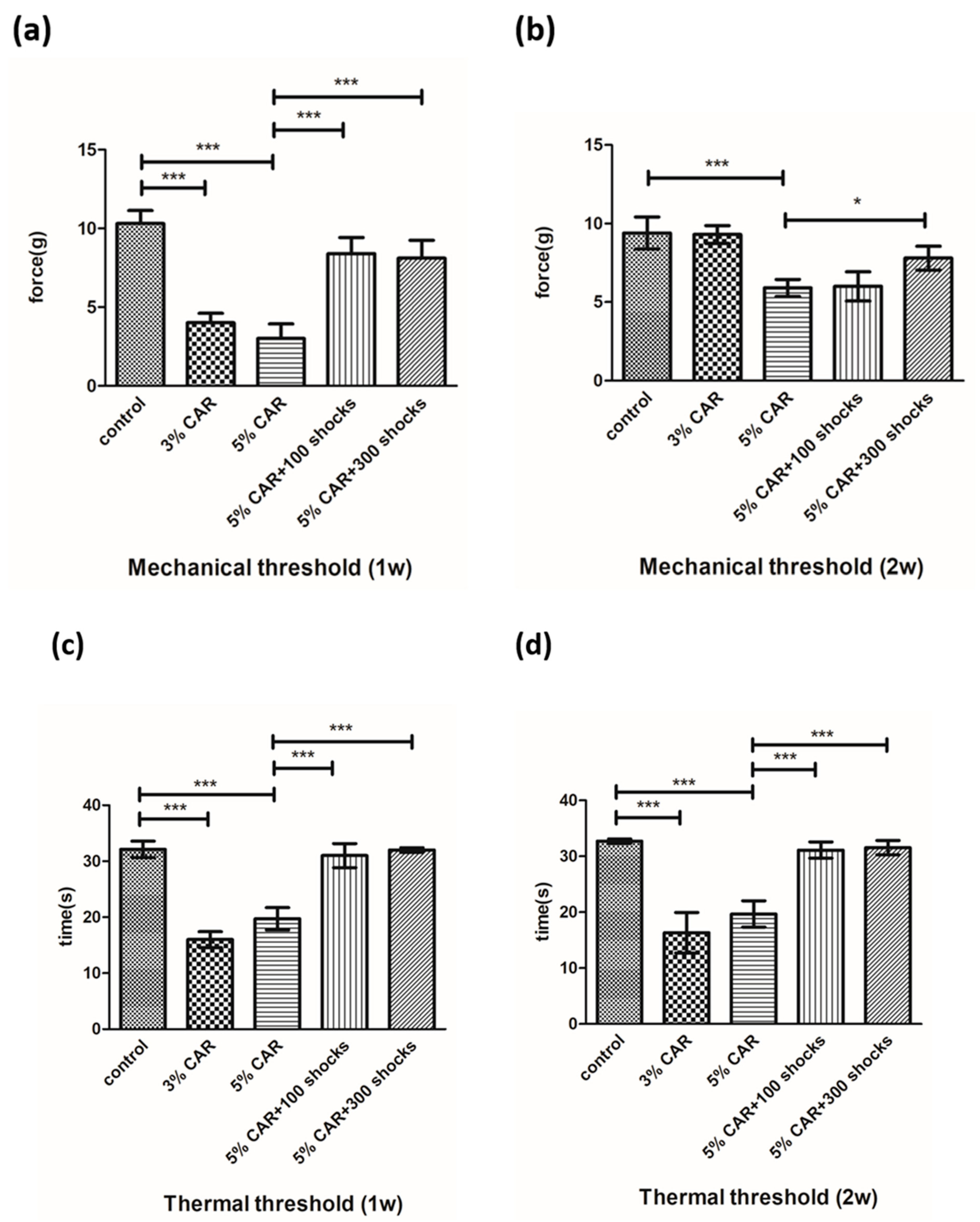
2.1. LESW Treatment Suppressed a Decrease in the Mechanical and Thermal Thresholds Induced by CAR Injection
2.2. LESW Treatment Suppressed an Increase in the Accumulation of Inflammatory Cells in the Bladder and the Prostate
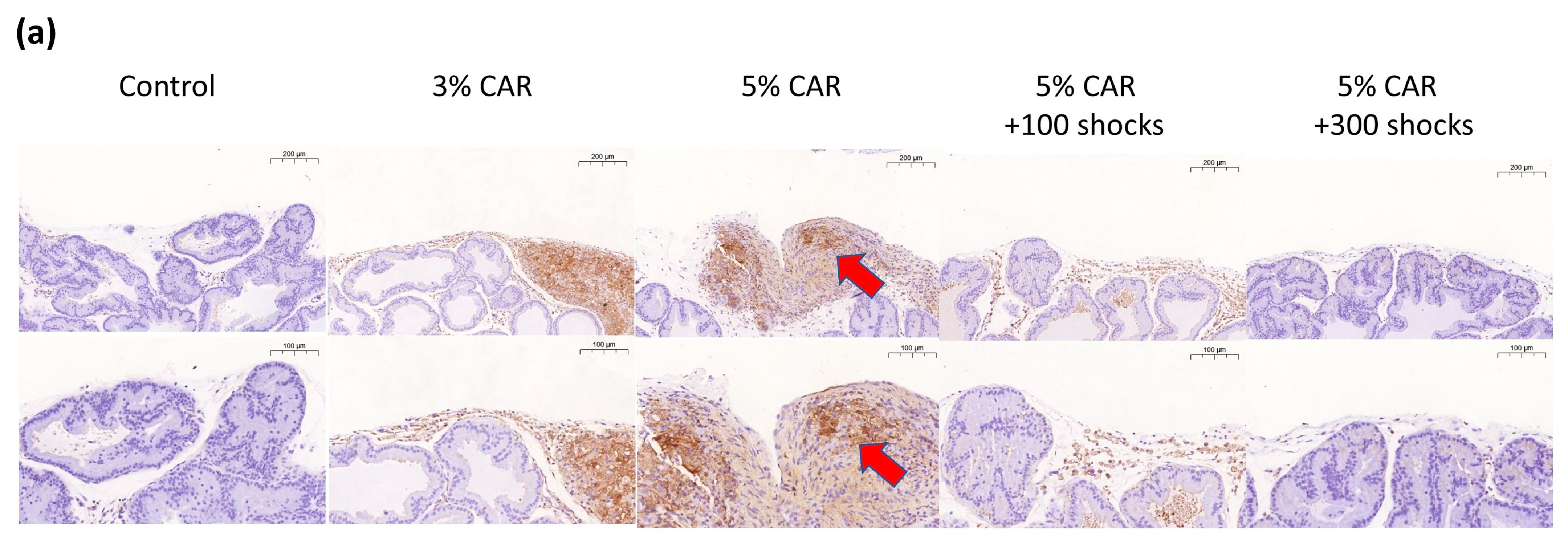
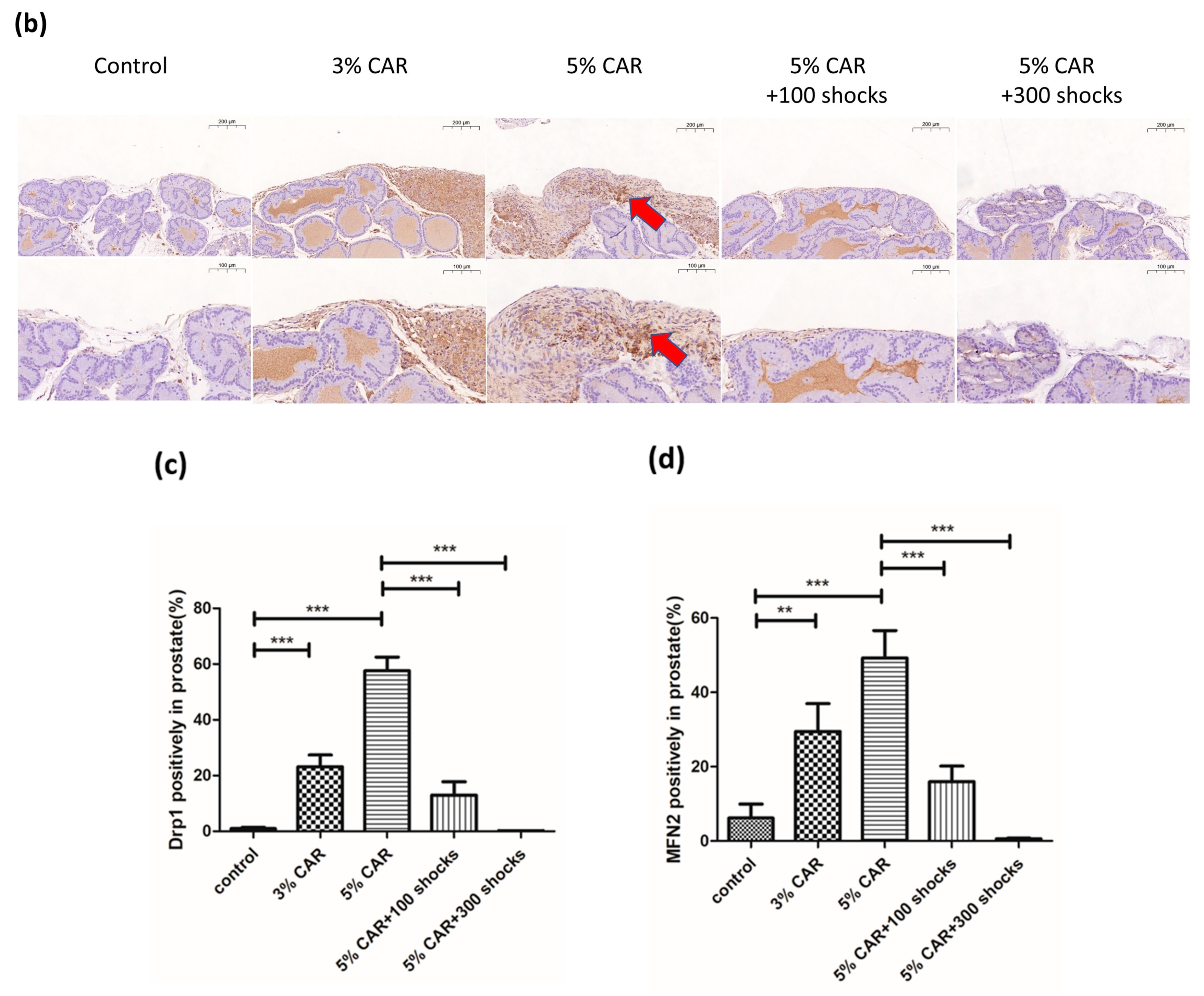
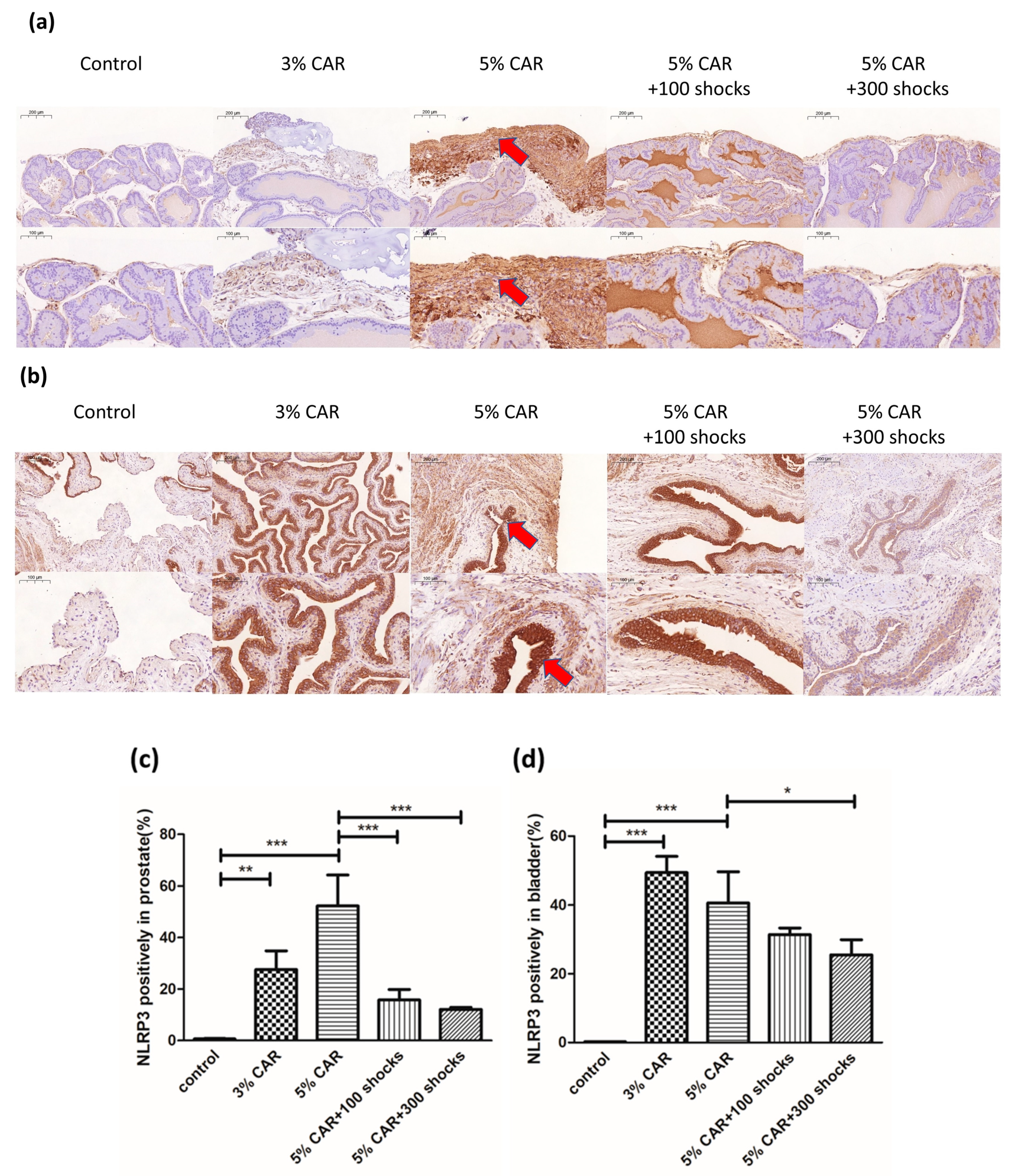
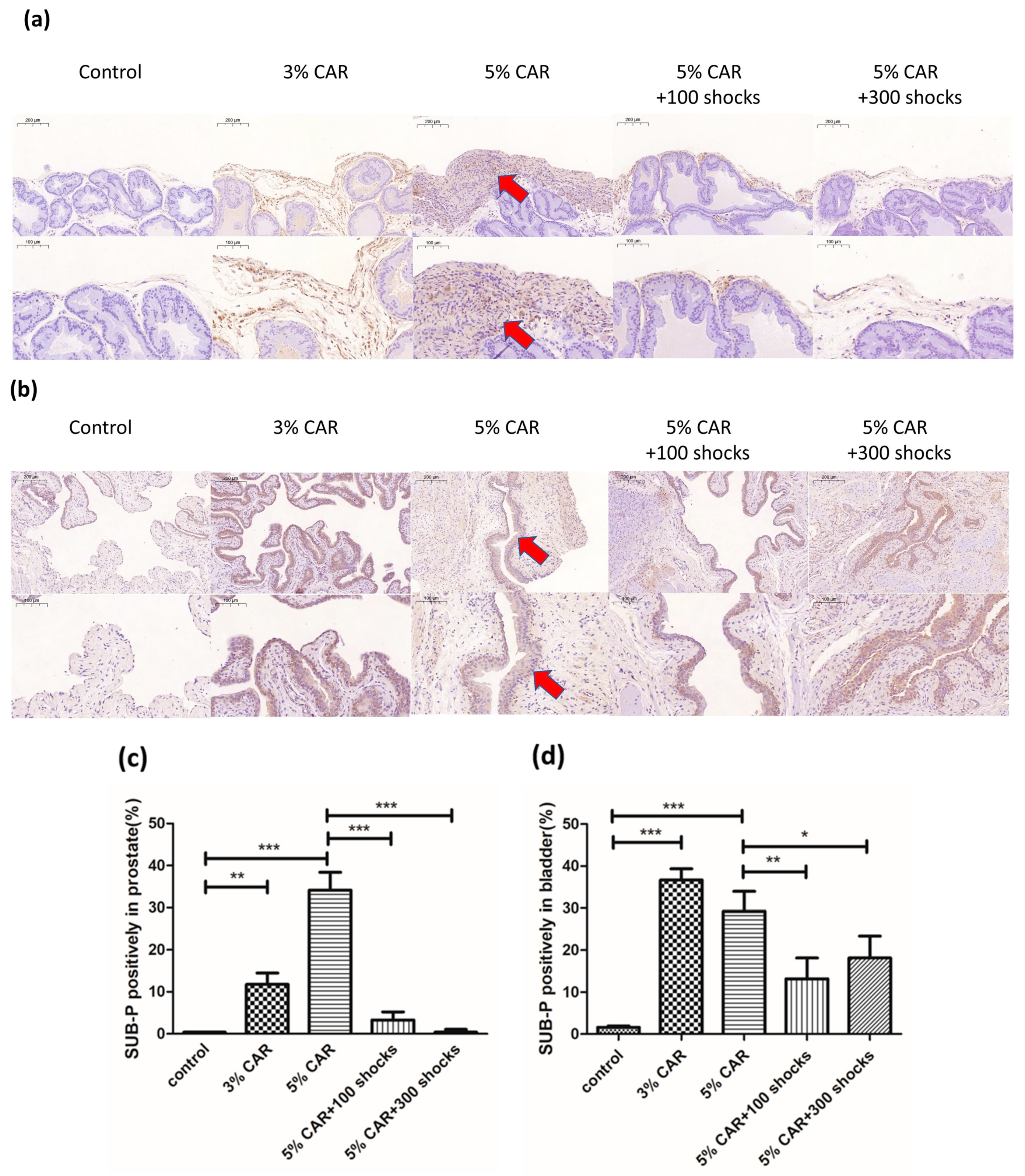
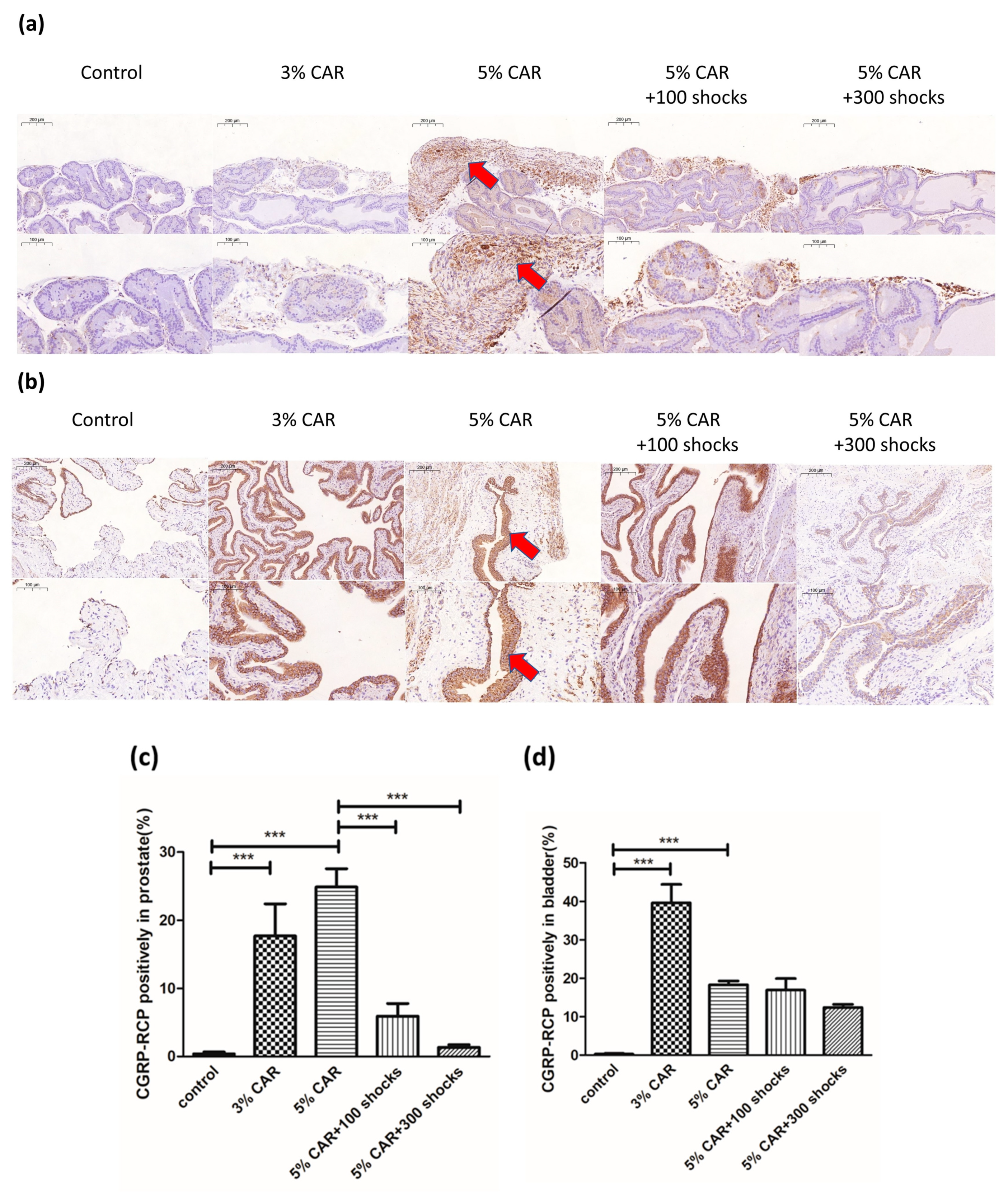
2.3. LESW Treatment Suppressed the Expressions of Mitochondrial-Related Factors (Drp-1, MFN-2, and NLRP3) and Pain-Related Peptides (Substance P and CGRP-RCP) in the Prostate and the Bladder Induced by CAR Injection
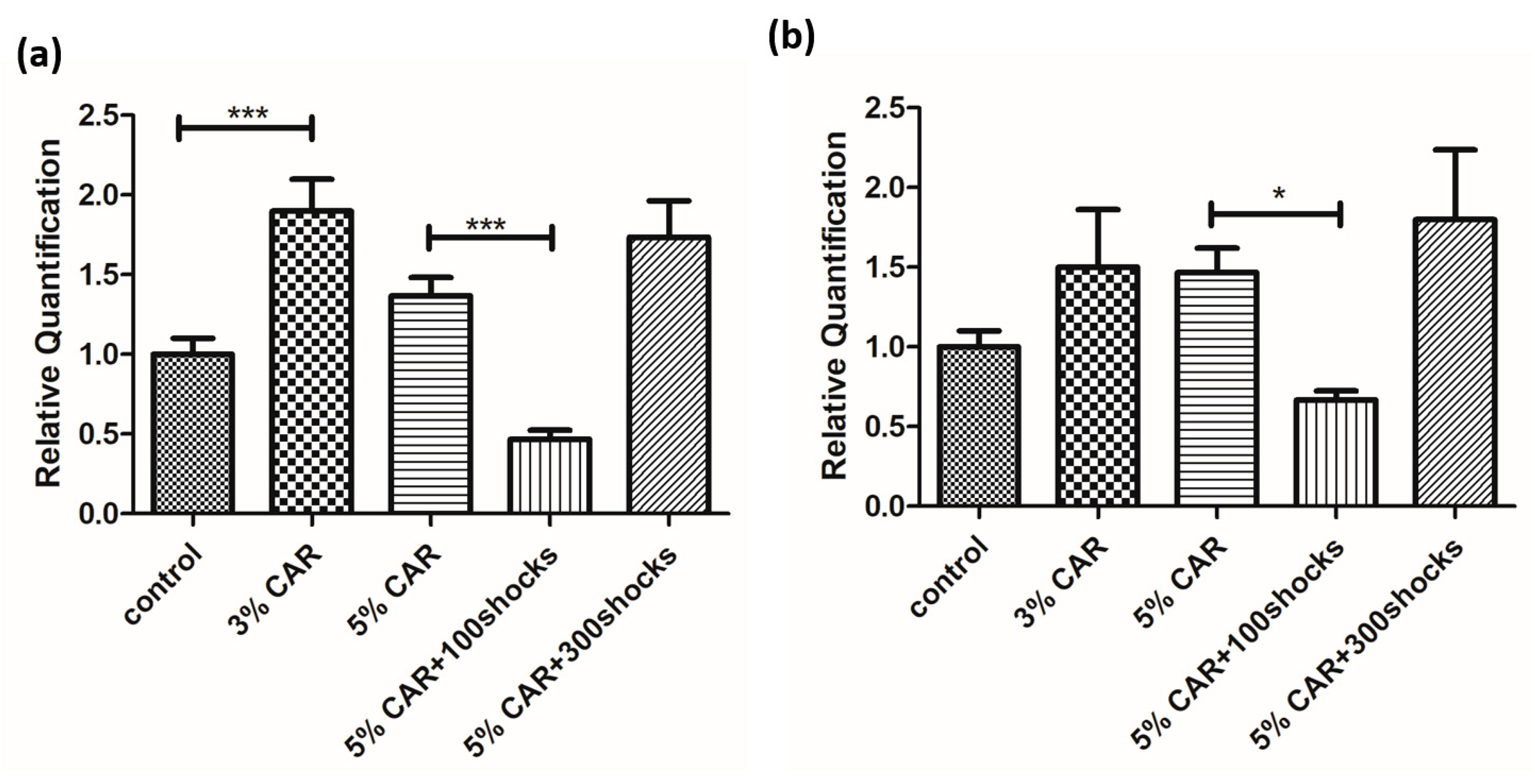
2.4. Drp-1 and MFN-2 Gene Expression in the Prostate Tissue in CAR-Induced Prostatitis with or without LESW Treatment
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. CAR-Induced Prostatitis Model
4.3. LESW Treatment
4.4. Assessment of Pain Behaviors
4.5. Immunohistochemical (IHC) Assay
4.6. Total RNA Extraction and RT-qPCR Analysis
4.7. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, Y.; Mikrani, R.; Xie, D.; Wazir, J.; Shrestha, S.; Ullah, R.; Baig, M.M.F.A.; Ahmed, A.; Srivastava, P.K.; Thapa, K.B.; et al. Chronic prostatitis/chronic pelvic pain syndrome and prostate cancer: Study of immune cells and cytokines. Fundam. Clin. Pharmacol. 2020, 34, 160–172. [Google Scholar] [CrossRef]
- Polackwich, A.S.; Shoskes, D.A. Chronic prostatitis/chronic pelvic pain syndrome: A review of evaluation and therapy. Prostate Cancer Prostatic Dis. 2016, 19, 132–138. [Google Scholar] [CrossRef]
- Igarashi, T.; Tyagi, P.; Mizoguchi, S.; Saito, T.; Furuta, A.; Suzuki, Y.; Egawa, S.; Wang, Z.; Yoshimura, N. Therapeutic effects of nerve growth factor-targeting therapy on bladder overactivity in rats with prostatic inflammation. Prostate 2021, 81, 1303–1309. [Google Scholar] [CrossRef]
- Krieger, J.N.; Riley, D.E.; Cheah, P.Y.; Liong, M.L.; Yuen, K.H. Epidemiology of prostatitis: New evidence for a world-wide problem. World J. Urol. 2003, 21, 70–74. [Google Scholar]
- Hu, M.; Wazir, J.; Ullah, R.; Wang, W.; Cui, X.; Tang, M.; Zhou, X. Phytotherapy and physical therapy in the management of chronic prostatitis–chronic pelvic pain syndrome. Int. Urol. Nephrol. 2019, 51, 1081–1088. [Google Scholar] [CrossRef]
- Mense, S.; Hoheisel, U. Shock wave treatment improves nerve regeneration in the rat. Muscle Nerve 2013, 47, 702–710. [Google Scholar] [CrossRef]
- Ito, K.; Fukumoto, Y.; Shimokawa, H. Extracorporeal shock wave therapy for ischemic cardiovascular disorders. Am. J. Cardiovasc. Drugs 2011, 11, 295–302. [Google Scholar] [CrossRef]
- Maffulli, G.; Padulo, J.; Iuliano, E.; Saxena, A.; Rompe, J.; Maffulli, N. Extracorporeal shock wave therapy in the management of midsubstance Achilles tendinopathy: The ASSERT database. Muscles Ligaments Tendons J. 2019, 2019, 3086910. [Google Scholar] [CrossRef]
- Jin, C.; Zhang, S.; Mo, F.; Zhang, M.; Meng, J.; Bian, Z.; Fu, Z.; Fang, Q.; Kong, X.; Feng, B.; et al. Efficacy and safety evaluation of low-intensity extracorporeal shock wave therapy on prostatitis-like symptoms: An open-label, single-arm trial. Andrologia 2022, 54, e14260. [Google Scholar] [CrossRef]
- Meng, J.; Jin, C.; Li, J.; Zhang, S.; Zhang, M.; Hao, Z.; Chen, X.; Song, Z.; Zhang, L.; Liang, C. Metabolomics Analysis Reveals the Differential Metabolites and Establishes the Therapeutic Effect Prediction Nomogram Among CP/CPPS Patients Who Respond or Do Not Respond to LiST. Front. Immunol. 2022, 13, 953403. [Google Scholar] [CrossRef]
- Vahdatpour, B.; Alizadeh, F.; Moayednia, A.; Emadi, M.; Khorami, M.H.; Haghdani, S. Efficacy of extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome: A randomized, controlled trial. ISRN Urol. 2013, 2013, 972601. [Google Scholar] [CrossRef] [PubMed]
- van Horssen, J.; van Schaik, P.; Witte, M. Inflammation and mitochondrial dysfunction: A vicious circle in neurodegenerative disorders? Neurosci. Lett. 2019, 710, 132931. [Google Scholar] [CrossRef] [PubMed]
- Na, Y.; Woo, J.; Choi, W.I.; Lee, J.H.; Hong, J.; Sung, D. α-Tocopherol-loaded reactive oxygen species-scavenging ferrocene nanocapsules with high antioxidant efficacy for wound healing. Int. J. Pharm. 2021, 596, 120205. [Google Scholar] [CrossRef] [PubMed]
- van den Ameele, J.; Fuge, J.; Pitceathly, R.D.S.; Berry, S.; McIntyre, Z.; Hanna, M.G.; Lee, M.; Chinnery, P.F. Chronic pain is common in mitochondrial disease. Neuromuscul. Disord. 2020, 30, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.J.; Tyagi, P.; Lin, T.K.; Huang, C.C.; Lee, W.C.; Chancellor, M.B.; Chuang, Y.-C. Low Energy Shock Wave Therapy Attenuates Mitochondrial Dysfunction and Improves Bladder Function in HCl induced Cystitis in Rats. Biomed. J. 2021, 45, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.-Q.; Yang, F.-Y.; Wang, M.-S.; Shi, B.-K.; Chen, D.-X.; Chen, D.; Zhou, Q.; He, Q.-B.; Ma, L.-X.; Cheng, W.-L.; et al. Quercetin protects against chronic prostatitis in rat model through NF-κB and MAPK signaling pathways. Prostate 2018, 78, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, H.; Kurita, M.; Okamoto, K.; Kotera, T.; Oka, M. Voiding behavior and chronic pelvic pain in two types of rat nonbacterial prostatitis models: Attenuation of chronic pelvic pain by repeated administration of tadalafil. Prostate 2019, 79, 446–453. [Google Scholar] [CrossRef]
- Kehl, L.J.; Trempe, T.M.; Hargreaves, K.M. A new animal model for assessing mechanisms and management of muscle hyperalgesia. Pain 2000, 85, 333–343. [Google Scholar] [CrossRef]
- Radhakrishnan, R.; Nallu, R.S. Development and characterisation of a novel animal model of prostate inflammation-induced chronic pelvic pain. Inflammopharmacology 2009, 17, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, N.; Yamanishi, T.; Fujita, T. Bladder sensation evaluation of a carrageenan-induced chronic prostatitis model using a direct measurement of the bladder mechanosensitive single-unit afferent nerve activity. Neurourol. Urodyn. 2020, 39, 2111–2119. [Google Scholar] [CrossRef]
- Wang, H.J.; Tyagi, P.; Chen, Y.M.; Chancellor, M.B.; Chuang, Y.C. Low Energy Shock Wave Therapy Inhibits Inflammatory Molecules and Suppresses Prostatic Pain and Hypersensitivity in a Capsaicin Induced Prostatitis Model in Rats. Int. J. Mol. Sci. 2019, 20, 4777. [Google Scholar] [CrossRef]
- Lee, J.C.; Yang, C.C.; Kromm, B.G.; Berger, R.E. Neurophysiologic testing in chronic pelvic pain syndrome: A pilot study. Urology 2001, 58, 246–250. [Google Scholar] [CrossRef]
- Lee, S.; Yang, G.; Xiang, W.; Bushman, W. Retrograde double-labeling demonstrates convergent afferent innervation of the prostate and bladder. Prostate 2016, 76, 767–775. [Google Scholar] [CrossRef]
- Mashaghi, A.; Marmalidou, A.; Tehrani, M.; Grace, P.M.; Pothoulakis, C.; Dana, R. Neuropeptide substance P and the immune response. Cell. Mol. Life Sci. 2016, 73, 4249–4264. [Google Scholar] [CrossRef] [PubMed]
- Yapa, N.M.B.; Lisnyak, V.; Reljic, B.; Ryan, M.T. Mitochondrial dynamics in health and disease. FEBS Lett. 2021, 595, 1184–1204. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.M.; Park, J.; Kim, S.H.; Jung, Y.K. Emerging perspectives on mitochondrial dysfunction and inflammation in Alzheimer’s disease. BMB Rep. 2020, 53, 35–46. [Google Scholar] [CrossRef]
- Chuang, T.-Y.; Chang, T.-W.; Chen, S.-S.; Chang, C.-C.; Cheng, W.-M.; Wei, Y.-H. Mitochondrial dysfunction in patients with urogenital disease. Urol. Sci. 2021, 32, 143–150. [Google Scholar]
- Kelley, N.; Jeltema, D.; Duan, Y.; He, Y. The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int. J. Mol. Sci. 2019, 20, 3328. [Google Scholar] [CrossRef]
- Scaini, G.; Mason, B.L.; Diaz, A.P.; Jha, M.K.; Soares, J.C.; Trivedi, M.H.; Quevedo, J. Dysregulation of mitochondrial dynamics, mitophagy and apoptosis in major depressive disorder: Does inflammation play a role? Mol. Psychiatry 2022, 27, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Wu, Z.; He, Y.; Chen, Z.; Xu, K.; Yu, W.; Fang, W.; Ma, C.; Moqbel, S.; Ran, J.; et al. MFN2 contributes to metabolic disorders and inflammation in the aging of rat chondrocytes and osteoarthritis. Osteoarthr. Cartil. 2020, 28, 1079–1091. [Google Scholar] [CrossRef]
- Nie, L.; Wu, G.; Zhang, W. Correlation of mRNA expression and protein abundance affected by multiple sequence features related to translational efficiency in Desulfovibrio vulgaris: A quantitative analysis. Genetics 2006, 174, 2229–2243. [Google Scholar] [CrossRef] [PubMed]
- Oliveto, S.; Mancino, M.; Manfrini, N.; Biffo, S. Role of microRNAs in translation regulation and cancer. World J. Biol. Chem. 2017, 8, 45–56. [Google Scholar] [CrossRef]
- Deng, G.C.; Lu, M.; Zhao, Y.Y.; Yuan, Y.; Chen, G. Activated spinal astrocytes contribute to the later phase of carrageenan-induced prostatitis pain. J. Neuroinflammation 2019, 16, 189. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, Y.; Chen, J.; Chen, L.; Meng, J.; Yang, C.; Yin, S.; Zhang, X.; Zhang, L.; Hao, Z.; et al. Single-cell multi-omics analysis presents the landscape of peripheral blood T-cell subsets in human chronic prostatitis/chronic pelvic pain syndrome. J. Cell. Mol. Med. 2020, 24, 14099–14109. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Meng, J.; Li, X.; Li, X.; Liu, Y.; Jin, C.; Zhang, L.; Hao, Z.; Chen, X.; Zhang, M.; et al. HA/CD44 Regulates the T Helper 1 Cells Differentiation by Activating Annexin A1/Akt/mTOR Signaling to Drive the Pathogenesis of EAP. Front. Immunol. 2022, 13, 875412. [Google Scholar] [CrossRef]
- Chuang, Y.C.; Tyagi, P.; Luo, H.L.; Lee, W.C.; Wang, H.J.; Huang, C.C.; Chancellor, M.B. Long-term functional change of cryoinjury-induced detrusor underactivity and effects of extracorporeal shock wave therapy in a rat model. Int. Urol. Nephrol. 2019, 51, 617–626. [Google Scholar] [CrossRef]
- Saban, R.; Saban, M.R.; Nguyen, N.-B.; Lu, B.; Gerard, C.; Gerard, N.P.; Hammond, T.G. Neurokinin-1 (NK-1) receptor is required in antigen-induced cystitis. Am. J. Pathol. 2000, 156, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.-C.; Yoshimura, N.; Wu, M.; Chiang, P.-H.; Chancellor, M.B. Intravesical botulinum toxin A administration inhibits COX-2 and EP4 expression and suppresses bladder hyperactivity in cyclophosphamide-induced cystitis in rats. Eur. Urol. 2009, 56, 159–166. [Google Scholar] [CrossRef]
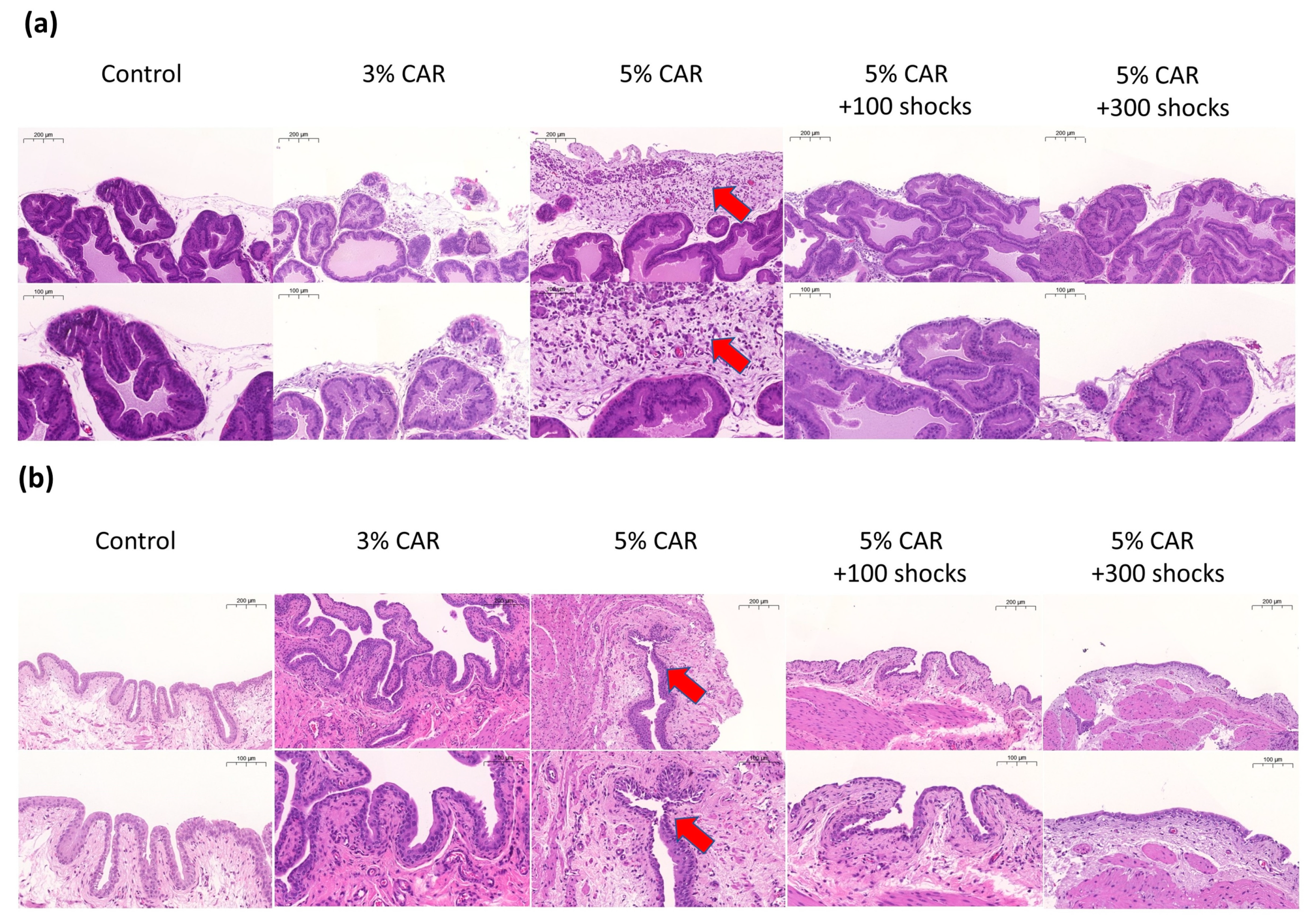
| Prostate | Edema | Inflammatory Cell |
|---|---|---|
| A: Control | 1.33 ± 0.52 | 1.33 ± 0.52 |
| B: 3% CAR | 2.33 ± 0.52 | 1.67 ± 0.52 |
| C: 5% CAR | 2.67 ± 0.52 | 2.67 ± 0.52 |
| D: 5% CAR + 100 shocks | 1.33 ± 0.52 | 1.33 ± 0.52 |
| E: 5% CAR + 300 shocks | 1.33 ± 0.52 | 1.33 ± 0.52 |
| p-value | ||
| A vs. B | 0.02 | 0.796 |
| A vs. C | 0.001 | 0.001 |
| C vs. D | 0.001 | 0.001 |
| C vs. E | 0.001 | 0.001 |
| Data presented as means ± SD | ||
| N = 6 for each group | ||
| Bladder | Edema | Inflammatory Cell |
| A: Control | 1.33 ± 0.58 | 1.33 ± 0.58 |
| B: 3% CAR | 2.33 ± 0.58 | 2.67 ± 0.58 |
| C: 5% CAR | 2.33 ± 0.58 | 2.67 ± 0.58 |
| D: 5% CAR + 100 shocks | 1.33 ± 0.58 | 1.67 ± 0.58 |
| E: 5% CAR + 300 shocks | 1.33 ± 0.58 | 1.33 ± 0.58 |
| p-value | ||
| A vs. B | 0.02 | 0.001 |
| A vs. C | 0.02 | 0.001 |
| C vs. D | 0.02 | 0.02 |
| C vs. E | 0.02 | 0.001 |
| Data presented as means ± SD | ||
| N = 6 for each group | ||
| Gene Primer | Sequence (5’-3’) |
|---|---|
| β-actin-F | AGGCCCCTCTGAACCCTAAG |
| β-actin-R | CAGCCTGGATGGCTACGTACA |
| MFN2-F | AGCACTTTGTCACTGCCAAGAAA |
| MFN2-R | GGACCTGCTCTTCTGTAGTAACTGG |
| Drp1-F | TGAAGGAACGGCAAAGTACATTG |
| Drp1-R | GGATCAACAGATTCTAAGGTTCGC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Z.-S.; Wang, H.-J.; Lee, W.-C.; Luo, H.L.; Lin, T.-K.; Chuang, Y.-C. Low-Energy Shock Wave Suppresses Prostatic Pain and Inflammation by Modulating Mitochondrial Dynamics Regulators on a Carrageenan-Induced Prostatitis Model in Rats. Int. J. Mol. Sci. 2023, 24, 3898. https://doi.org/10.3390/ijms24043898
Wu Z-S, Wang H-J, Lee W-C, Luo HL, Lin T-K, Chuang Y-C. Low-Energy Shock Wave Suppresses Prostatic Pain and Inflammation by Modulating Mitochondrial Dynamics Regulators on a Carrageenan-Induced Prostatitis Model in Rats. International Journal of Molecular Sciences. 2023; 24(4):3898. https://doi.org/10.3390/ijms24043898
Chicago/Turabian StyleWu, Zong-Sheng, Hung-Jen Wang, Wei-Chia Lee, Hou Lun Luo, Tsu-Kung Lin, and Yao-Chi Chuang. 2023. "Low-Energy Shock Wave Suppresses Prostatic Pain and Inflammation by Modulating Mitochondrial Dynamics Regulators on a Carrageenan-Induced Prostatitis Model in Rats" International Journal of Molecular Sciences 24, no. 4: 3898. https://doi.org/10.3390/ijms24043898
APA StyleWu, Z.-S., Wang, H.-J., Lee, W.-C., Luo, H. L., Lin, T.-K., & Chuang, Y.-C. (2023). Low-Energy Shock Wave Suppresses Prostatic Pain and Inflammation by Modulating Mitochondrial Dynamics Regulators on a Carrageenan-Induced Prostatitis Model in Rats. International Journal of Molecular Sciences, 24(4), 3898. https://doi.org/10.3390/ijms24043898






