Fli1 and Tissue Fibrosis in Various Diseases
Abstract
1. Introduction
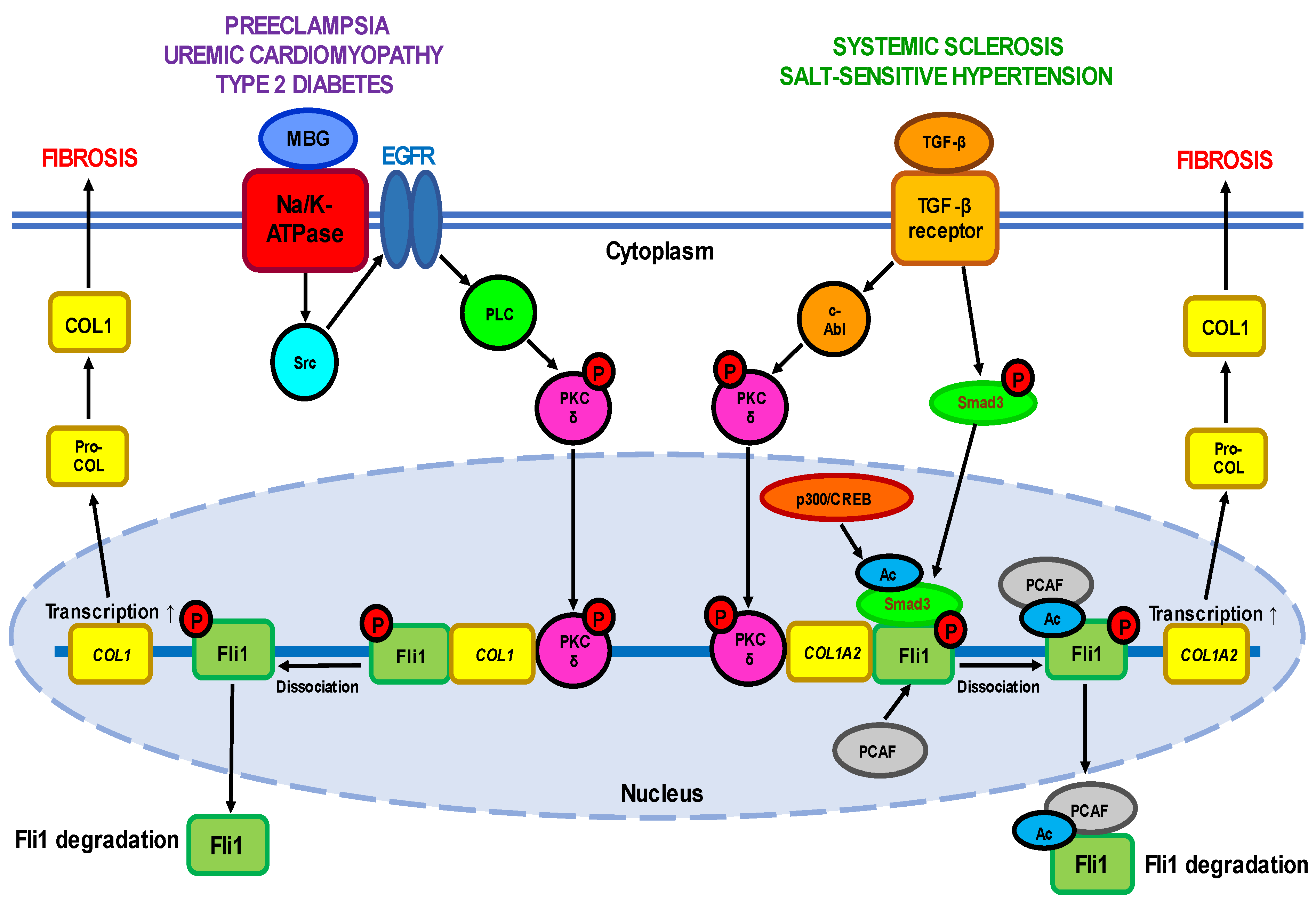
2. Diseases Associated with Fli1 Deficiency
2.1. Fli1 in Systemic Sclerosis
2.2. Fli1 in Uremic Cardiomyopathy
2.3. Fli1 in Preeclampsia
2.4. Fli1 as a Common Causative Factor of Hypertension
| Expression | Effect | Experimental System | References | |
|---|---|---|---|---|
| Fli1 repressors | ||||
| TGF-β | ↑ | Activation of TGF-β receptors | Human dermal fibroblasts; rat diabetes model; rat hypertension model | [25,29,32,38,39,79,80,81] |
| c-Abl | ↑ | PKC-δ phosphorylation | Human normal and SSc dermal fibroblasts | [40,41,47,51] |
| PKC-δ | ↑ | Fli1 phosphorylation | Human normal and SSc dermal fibroblasts; FLI1-transfected HEK293T cells; FLI1 silencing in human UA | [37,39,42,47,77] |
| Endothelin-1 | ↑ | Fli1 activation | Human normal and SSc dermal fibroblasts; BLM-treated mice | [42] |
| PCAF | ↑ | Fli1 acetylation | Human dermal fibroblasts; FLI1-transfected HEK293T cells | [38] |
| CXCL4 | ↑ | Vasculopathy | HUVECs | [51] |
| MBG | ↑ | PKC-δ activation; Fli1 suppression | Wild-type and FLI1-knockdown mice; rat CKD model; rat cardiac fibroblasts; human cardiac fibroblasts; human renal fibroblasts; FLI1-transfected renal fibroblasts; rat diabetes model; rat hypertension model; rat PE model | [16,66,67,68,73,74,75,76,77,79,80,81] |
| Fli1-deficiency targets | ||||
| COL1 | ↑ | Collagen synthesis | FLI1-transfected human dermal fibroblasts; human normal and SSc dermal fibroblasts; murine Fli11−/−, Fli1+/− and Fli1+/+ fibroblasts; wild-type and FLI1-knockdown mice; rat CKD model; rat cardiac fibroblasts; human cardiac fibroblasts; human renal fibroblasts; FLI1-transfected renal fibroblasts; rat diabetes model; rat hypertension model; rat PE model; human PE UA; FLI1 silencing in human UA; human MBG-treated UA | [8,16,25,29,32,38,66,67,68,73,74,75,76,77,79,80,81] |
| CTGF(CCN2) | ↑ | COL1A1 and COL1A2 upregulation; MMP-1 downregulation | FLI1-transfected human dermal fibroblasts; human SSc fibroblasts | [32,33] |
| MMP-1 | ↓ | Increased production of EMC components | FLI1-transfected human dermal fibroblasts; human SSc fibroblasts | [32,33] |
| Fibronectin | ↑ | Fibrosis | Human CD14+ monocytes and CD14+ macrophages | [23] |
| Chemerin | ↑ | Impaired angiogenesis | Human SSc dermal vessels and HDMECs; murine Fli1+/− dermal blood vessels; | [35] |
| S100A12 | ↑ | Skin sclerosis | Human SSc skin; | [36] |
| RALDH1 | ↓ | Fibrosis | Human dermal dendritic cells; BLM-treated Fli1+/− mice | [30] |
| Cathepsin B | ↑ ↓ | Vasculopathy Increased production of EMC components | FLI1 silencing in HDMECs; Fli1+/− mice; human dcSSc dermal fibroblasts, early dcSSc dermal fibroblasts | [43] |
| Cathepsin L | ↑ ↓ | Vasculopathy Increased production of EMC components | FLI1 silencing in HDMECs; human SS dermal vessels and skin; FLI1-knockout mice; skin of BLM-treated mice | [45] |
| Cathepsin V | ↓ | Increased production of EMC components | FLI1 silencing in HDMECs; human dcSSc dermal fibroblasts, microvascular ECs, dcSSc and lcSSc skin keratinocytes | [44] |
| PGRN | ↑ | Inflammation; skin sclerosis; fibrosis | Human SSc dermal fibroblasts; Fli-1+/− mice; BLM-treated mice; human LSc skin lesions | [46,47] |
| TNF-α | ↑ | Inflammation; fibrosis | Human LSc skin lesions; | [47] |
| CXCL5 | ↓ | Vasculopathy | Human dcSSc dermal blood vessels; FLI1 silencing in HDMECs; dermal vessels of Fli1 knockout mice | [48] |
| CXCL6 | ↑ | Tissues fibrosis; vasculopathy | Human SSc dermal fibroblasts; FLI1 silencing in HDMECs | [49] |
| CCL20 | ↑ | Fibrosis | Human early dcSSc | [52] |
| CCL6 | ↑ | Vasculopathy | Human SSc dermal vessels; FLI1 silencing in HDMECs | [52] |
| EPCR | ↓ | Impaired vascular homeostasis | Human SSc dermal vessels; Fli1+/− mice; FLI1 silencing in HDMECs | [53] |
| VE-cadherin | ↓ | Impaired vascular homeostasis | MDMECs of Fli1 CKO mice; MDMECs of Fli1+/− mice; FLI1 silencing in HDMECs | [34] |
| PECAM-1 | ↓ | Impaired vascular homeostasis | MDMECs of Fli1 CKO mice; MDMECs of Fli1+/− mice; FLI1 silencing in HDMECs | [34] |
| MMP-9 | ↓ | Impaired vascular homeostasis | MDMECs of Fli1 CKO mice; MDMECs of Fli1+/− mice; FLI1 silencing in HDMECs | [34] |
| PDGF-B | ↓ | Impaired vascular homeostasis | MDMECs of Fli1 CKO mice; MDMECs of Fli1+/− mice; FLI1 silencing in HDMECs | [34] |
| S1P1 | ↓ | Impaired vascular homeostasis | MDMECs of Fli1 CKO mice; MDMECs of Fli1+/− mice; FLI1 silencing in HDMECs | [34] |
| Adipsin | ↑ | Vascular hypertension | Human SSc dermal vessels; FLI1 silencing in HDMECs | [54] |
| Genetic and epigenetic factors | ||||
| (GA)n alleles | ↑ | Increased susceptibility to SSc | Human SSc peripheral blood | [56] |
| Acetylation of histones H3 and H4 in the FLI1 gene promoter | ↓ | FLI1 suppression; increased collagen synthesis | Human skin, normal and dcSSc fibroblasts | [57] |
| HDAC-1 and 6 | ↑ | FLI1 suppression | Human skin, normal and dcSSc fibroblasts | [57] |
| MBD-1 and 2, MeCP2 | ↑ | DNA methylation | Human skin, normal and dcSSc fibroblasts | [57] |
| Methylation of CpG islands in the FLI1 promoter | ↑ | FLI1 suppression; increased Collagen synthesis | Human skin, normal and dcSSc fibroblasts | [57] |
| DNMT1 | ↑ | FLI1 suppression | Human skin, normal and dcSSc fibroblasts | [33,57] |
| COL23A1, COL4A2 methylation | ↓ | Increased collagen synthesis | Human dcSSc and lcSSc dermal fibroblasts | [58] |
| ITGA9 methylation | ↓ | TGF-β upregulation | Human dcSSc and lcSSc dermal fibroblasts | [58] |
| ADAM12 methylation | ↓ | TGF-β upregulation | Human dcSSc and lcSSc dermal fibroblasts | [58] |
| miRNA-26a | ↑ | FLI1 suppression | Primary SSc skin fibroblasts | [31] |
| miRNA-21 | ↑ | TGF-β upregulation; collagen synthesis | Human dcSSc and TGF-β treated normal fibroblasts | [59] |
| miRNA-29a | ↓ | TGF-β upregulation; collagen synthesis | Human dcSSc and TGF-β treated normal fibroblasts | [59] |
3. Fli1 Overexpression as a Cause of Ewing’s Sarcoma
4. Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ben-David, Y.; Giddens, E.B.; Bernstein, A. Identification and mapping of a common proviral integration site Fli-1 in erythroleukemia cells induced by Friend murine leukemia virus. Proc. Natl. Acad. Sci. USA 1990, 87, 1332–1336. [Google Scholar] [CrossRef] [PubMed]
- Ben-David, Y.; Giddens, E.B.; Letwin, K.; Bernstein, A. Erythroleukemia induction by Friend murine leukemia virus: Insertional activation of a new member of the ets gene family, Fli-1, closely linked to c-ets-1. Genes Dev. 1991, 5, 908–918. [Google Scholar] [CrossRef] [PubMed]
- He, Y.S.; Yang, X.K.; Hu, Y.Q.; Xiang, K.; Pan, H.F. Emerging role of Fli1 in autoimmune diseases. Int. Immunopharmacol. 2021, 90, 107127. [Google Scholar] [CrossRef] [PubMed]
- Ben-David, Y.; Babu Gajendran, B.; Klarke, M.; Sample, K.M.; Zacksenhaus, E. Current insights into the role of Fli-1 in hematopoiesis and malignant transformation. Cell. Mol. Life Sci. 2022, 79, 163. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y. Role of ETS family transcription factors in vascular development and angiogenesis. Cell Struct. Funct. 2001, 26, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Ferdous, A.; Singh, S.; Luo, Y.; Abedin, M.J.; Jiang, N.; Perry, C.E.; Evers, B.M.; Gillette, T.G.; Kyba, M.; Trojanowska, M.; et al. Fli1 Promotes Vascular Morphogenesis by Regulating Endothelial Potential of Multipotent Myogenic Progenitors. Circ. Res. 2021, 129, 949–964. [Google Scholar] [CrossRef]
- Spyropoulos, D.D.; Pharr, P.N.; Lavenburg, K.R.; Jackers, P.; Papas, T.S.; Ogawa, M.; Watson, D.K. Hemorrhage, impaired hematopoiesis, and lethality in mouse embryos carrying a targeted disruption of the Fli1 transcription factor. Mol. Cell. Biol. 2000, 20, 5643–5652. [Google Scholar] [CrossRef]
- Asano, Y.J. What can we learn from Fli1-deficient mice, new animal models of systemic sclerosis? Scleroderma Relat. Disord. 2018, 3, 6–13. [Google Scholar] [CrossRef]
- Pimanda, J.E.; Chan, W.Y.; Donaldson, I.J.; Bowen, M.; Green, A.R.; Göttgens, B. Endoglin expression in the endothelium is regulated by Fli-1, Erg, and Elf-1 acting on the promoter and a −8-kb enhancer. Blood 2006, 107, 4737–4745. [Google Scholar] [CrossRef]
- Le Bras, A.; Samson, C.; Trentini, M.; Caetano, B.; Lelievre, E.; Mattot, V.; Beermann, F.; Soncin, F. VE-statin/egfl7 expression in endothelial cells is regulated by a distal enhancer and a proximal promoter under the direct control of Erg and GATA-2. PLoS ONE 2010, 5, e12156. [Google Scholar] [CrossRef]
- Soncin, F.; Mattot, V.; Lionneton, F.; Spruyt, N.; Lepretre, F.; Begue, A.; Stehelin, D. VE-statin, an endothelial repressor of smooth muscle cell migration. EMBO J. 2003, 22, 5700–5711. [Google Scholar] [CrossRef] [PubMed]
- Lelièvre, E.; Lionneton, F.; Mattot, V.; Spruyt, N.; Soncin, F. Ets-1 regulates fli-1 expression in endothelial cells. Identification of ETS binding sites in the fli-1 gene promoter. J. Biol. Chem. 2002, 277, 25143–25151. [Google Scholar] [CrossRef]
- Li, L.; Yu, J.; Cheng, S.; Peng, Z.; Luo, H. Transcription factor Fli-1 as a new target for antitumor drug development. Int. J. Biol. Macromol. 2022, 209 Pt A, 1155–1168. [Google Scholar] [CrossRef]
- Gargallo, P.; Yáñez, Y.; Juan, A.; Segura, V.; Balaguer, J.; Torres, B.; Oltra, S.; Castel, V.; Cañete, A. Review: Ewing Sarcoma Predisposition. Pathol. Oncol. Res. 2020, 26, 2057–2066. [Google Scholar] [CrossRef] [PubMed]
- Qian, C.; Li, D.; Chen, Y. ETS factors in prostate cancer. Cancer Lett. 2022, 530, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Elkareh, J.; Periyasamy, S.M.; Shidyak, A.; Vetteth, S.; Schroeder, J.; Raju, V.; Hariri, I.M.; El-Okdi, N.; Gupta, S.; Fedorova, L.; et al. Marinobufagenin induces increases in procollagen expression in a process involving protein kinase C and Fli-1: Implications for uremic cardiomyopathy. Am. J. Physiol. Renal Physiol. 2009, 296, F1219–F1226. [Google Scholar] [CrossRef]
- Agalakova, N.I.; Kolodkin, N.I.; Adair, C.D.; Trashkov, A.P.; Bagrov, A.Y. Preeclampsia: Cardiotonic Steroids, Fibrosis, Fli1 and Hint to Carcinogenesis. Int. J. Mol. Sci. 2021, 22, 1941. [Google Scholar] [CrossRef]
- Toyama, T.; Asano, Y.; Miyagawa, T.; Nakamura, K.; Hirabayashi, M.; Yamashita, T.; Saigusa, R.; Miura, S.; Ichimura, Y.; Takahashi, T.; et al. The impact of transcription factor Fli1 deficiency on the regulation of angiogenesis. Exp. Dermatol. 2017, 26, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y. Epigenetic suppression of Fli1, a potential predisposing factor in the pathogenesis of systemic sclerosis. Int. J. Biochem. Cell Biol. 2015, 67, 86–91. [Google Scholar] [CrossRef]
- Fioretto, B.S.; Rosa, I.; Romano, E.; Wang, Y.; Guiducci, S.; Zhang, G.; Manetti, M.; Matucci-Cerinic, M. The contribution of epigenetics to the pathogenesis and gender dimorphism of systemic sclerosis: A comprehensive overview. Ther. Adv. Musculoskelet. Dis. 2020, 12, 1759720X20918456. [Google Scholar] [CrossRef]
- Yu, J.; Tang, R.; Ding, K. Epigenetic Modifications in the Pathogenesis of Systemic Sclerosis. Int. J. Gen. Med. 2022, 15, 3155–3166. [Google Scholar] [CrossRef]
- Kowalska-Kępczyńska, A.J. Systemic Scleroderma-Definition, Clinical Picture and Laboratory Diagnostics. Clin. Med. 2022, 11, 2299. [Google Scholar] [CrossRef] [PubMed]
- Rudnik, M.; Hukara, A.; Kocherova, I.; Jordan, S.; Schniering, J.; Milleret, V.; Ehrbar, M.; Klingel, K.; Feghali-Bostwick, C.; Distler, O.; et al. Elevated Fibronectin Levels in Profibrotic CD14+ Monocytes and CD14+ Macrophages in Systemic Sclerosis. Front. Immunol. 2021, 12, 642891. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, S.; Midwood, K.S.; Varga, J. Tenascin-C in fibrosis in multiple organs: Translational implications. Semin. Cell Dev. Biol. 2022, 128, 130–136. [Google Scholar] [CrossRef]
- Czuwara-Ladykowska, J.; Shirasaki, F.; Jackers, P.; Watson, D.K.; Trojanowska, M.J. Fli-1 inhibits collagen type I production in dermal fibroblasts via an Sp1-dependent pathway. Biol. Chem. 2001, 276, 20839–20848. [Google Scholar] [CrossRef] [PubMed]
- Manetti, M. Fli1 deficiency and beyond: A unique pathway linking peripheral vasculopathy and dermal fibrosis in systemic sclerosis. Exp. Dermatol. 2015, 24, 256–257. [Google Scholar] [CrossRef]
- Takahashi, T.; Asano, Y.; Sugawara, K.; Yamashita, T.; Nakamura, K.; Saigusa, R.; Ichimura, Y.; Toyama, T.; Taniguchi, T.; Akamata, K.; et al. Epithelial Fli1 deficiency drives systemic autoimmunity and fibrosis: Possible roles in scleroderma. J. Exp. Med. 2017, 214, 1129–1151. [Google Scholar] [CrossRef]
- Asano, Y.J. The Pathogenesis of Systemic Sclerosis: An Understanding Based on a Common Pathologic Cascade across Multiple Organs and Additional Organ-Specific Pathologies. Clin. Med. 2020, 9, 2687. [Google Scholar] [CrossRef]
- Kubo, M.; Czuwara-Ladykowska, J.; Moussa, O.; Markiewicz, M.; Smith, E.; Silver, R.M.; Jablonska, S.; Blaszczyk, M.; Watson, D.K.; Trojanowska, M. Persistent down-regulation of Fli1, a suppressor of collagen transcription, in fibrotic scleroderma skin. Am. J. Pathol. 2003, 163, 571–581. [Google Scholar] [CrossRef]
- Miura, S.; Watanabe, Y.; Saigusa, R.; Yamashita, T.; Nakamura, K.; Hirabayashi, M.; Miyagawa, T.; Yoshizaki, A.; Trojanowska, M.; Sato, S.; et al. Fli1 deficiency suppresses RALDH1 activity of dermal dendritic cells and related induction of regulatory T cells: A possible role in scleroderma. Arthritis Res. Ther. 2021, 23, 137. [Google Scholar] [CrossRef]
- Cheng, Z.; Zhang, J.; Deng, W.; Lin, S.; Li, D.; Zhu, K.; Qi, Q. Bushen Yijing Decoction (BSYJ) exerts an anti-systemic sclerosis effect via regulating MicroRNA-26a/FLI1 axis. Bioengineered 2021, 12, 1212–1225. [Google Scholar] [CrossRef]
- Nakerakanti, S.S.; Kapanadze, B.; Yamasaki, M.; Markiewicz, M.; Trojanowska, M. Fli1 and Ets1 have distinct roles in connective tissue growth factor/CCN2 gene regulation and induction of the profibrotic gene program. J. Biol. Chem. 2006, 281, 25259–25269. [Google Scholar] [CrossRef]
- Bujor, A.M.; Haines, P.; Padilla, C.; Christmann, R.B.; Junie, M.; Sampaio-Barros, P.D.; Lafyatis, R.; Trojanowska, M. Ciprofloxacin has antifibrotic effects in scleroderma fibroblasts via downregulation of Dnmt1 and upregulation of Fli1. Int. J. Mol. Med. 2012, 30, 1473–1480. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Stawski, L.; Hant, F.; Highland, K.; Silver, R.; Szalai, G.; Watson, D.K.; Trojanowska, M. Endothelial Fli1 deficiency impairs vascular homeostasis: A role in scleroderma vasculopathy. Am. J. Pathol. 2010, 176, 1983–1998. [Google Scholar] [CrossRef] [PubMed]
- Akamata, K.; Asano, Y.; Taniguchi, T.; Yamashita, T.; Saigusa, R.; Nakamura, K.; Noda, S.; Aozasa, N.; Toyama, T.; Takahashi, T.; et al. Increased expression of chemerin in endothelial cells due to Fli1 deficiency may contribute to the development of digital ulcers in systemic sclerosis. Rheumatology 2015, 54, 1308–1316. [Google Scholar] [CrossRef]
- Omatsu, J.; Saigusa, R.; Miyagawa, T.; Fukui, Y.; Toyama, S.; Awaji, K.; Ikawa, T.; Norimatsu, Y.; Yoshizaki, A.; Sato, S.; et al. Serum S100A12 levels: Possible association with skin sclerosis and interstitial lung disease in systemic sclerosis. Exp. Dermatol. 2021, 30, 409–415. [Google Scholar] [CrossRef]
- Jinnin, M.; Ihn, H.; Yamane, K.; Mimura, Y.; Asano, Y.; Tamaki, K. Alpha2(I) collagen gene regulation by protein kinase C signaling in human dermal fibroblasts. Nucleic Acids Res. 2005, 33, 1337–1351. [Google Scholar] [CrossRef]
- Asano, Y.; Czuwara, J.; Trojanowska, M. Transforming growth factor-beta regulates DNA binding activity of transcription factor Fli1 by p300/CREB-binding protein-associated factor-dependent acetylation. J. Biol. Chem. 2007, 282, 34672–34683. [Google Scholar] [CrossRef]
- Asano, Y.; Trojanowska, M. Phosphorylation of Fli1 at threonine 312 by protein kinase C delta promotes its interaction with p300⁄CREB-binding protein-associated factor and subsequent acetylation in response to transforming growth factor beta. Mol. Cell. Biol. 2009, 29, 1882–1894. [Google Scholar] [CrossRef]
- Bujor, A.M.; Asano, Y.; Haines, P.; Lafyatis, R.; Trojanowska, M. The c-Abl tyrosine kinase controls protein kinase Cδ-induced Fli-1 phosphorylation in human dermal fibroblasts. Arthritis Rheum. 2011, 63, 1729–1737. [Google Scholar] [CrossRef] [PubMed]
- Noda, S.; Asano, Y.; Akamata, K.; Aozasa, N.; Taniguchi, T.; Takahashi, T.; Ichimura, Y.; Toyama, T.; Sumida, H.; Yanaba, K.; et al. Constitutive activation of c-Abl/protein kinase C-δ/Fli1 pathway in dermal fibroblasts derived from patients with localized scleroderma. Br. J. Dermatol. 2012, 167, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Akamata, K.; Asano, Y.; Aozasa, N.; Noda, S.; Taniguchi, T.; Takahashi, T.; Ichimura, Y.; Toyama, T.; Sato, S. Bosentan reverses the pro-fibrotic phenotype of systemic sclerosis dermal fibroblasts via increasing DNA binding ability of transcription factor Fli1. Arthritis Res. Ther. 2014, 16, R86. [Google Scholar] [CrossRef] [PubMed]
- Noda, S.; Asano, Y.; Akamata, K.; Aozasa, N.; Taniguchi, T.; Takahashi, T.; Ichimura, Y.; Toyama, T.; Sumida, H.; Yanaba, K.; et al. A possible contribution of altered cathepsin B expression to the development of skin sclerosis and vasculopathy in systemic sclerosis. PLoS ONE 2012, 7, e32272. [Google Scholar] [CrossRef]
- Noda, S.; Asano, Y.; Takahashi, T.; Akamata, K.; Aozasa, N.; Taniguchi, T.; Ichimura, Y.; Toyama, T.; Sumida, H.; Kuwano, Y.; et al. Decreased cathepsin V expression due to Fli1 deficiency contributes to the development of dermal fibrosis and proliferative vasculopathy in systemic sclerosis. Rheumatology 2013, 52, 790–799. [Google Scholar] [CrossRef]
- Yamashita, T.; Asano, Y.; Taniguchi, T.; Nakamura, K.; Saigusa, R.; Takahashi, T.; Ichimura, Y.; Toyama, T.; Yoshizaki, A.; Miyagaki, T.; et al. A potential contribution of altered cathepsin L expression to the development of dermal fibrosis and vasculopathy in systemic sclerosis. Exp. Dermatol. 2016, 25, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Ichimura, Y.; Asano, Y.; Akamata, K.; Noda, S.; Taniguchi, T.; Takahashi, T.; Toyama, T.; Tada, Y.; Sugaya, M.; Sato, S.; et al. Progranulin Overproduction Due to Fli-1 Deficiency Contributes to the Resistance of Dermal Fibroblasts to Tumor Necrosis Factor in Systemic Sclerosis. Arthritis Rheumatol. 2015, 67, 3245–3255. [Google Scholar] [CrossRef]
- Miyagawa, T.; Ichimura, Y.; Nakamura, K.; Hirabayashi, M.; Yamashita, T.; Saigusa, R.; Miura, S.; Takahashi, T.; Toyama, T.; Taniguchi, T.; et al. Progranulin overproduction due to constitutively activated c-Abl/PKC-δ/Fli1 pathway contributes to the resistance of dermal fibroblasts to the anti-fibrotic effect of tumor necrosis factor-α in localized scleroderma. Dermatol. Sci. 2018, 92, 207–214. [Google Scholar] [CrossRef]
- Ichimura, Y.; Asano, Y.; Akamata, K.; Takahashi, T.; Noda, S.; Taniguchi, T.; Toyama, T.; Aozasa, N.; Sumida, H.; Kuwano, Y.; et al. Fli1 deficiency contributes to the suppression of endothelial CXCL5 expression in systemic sclerosis. Arch. Dermatol. Res. 2014, 306, 331–338. [Google Scholar] [CrossRef]
- Taniguchi, T.; Asano, Y.; Nakamura, K.; Yamashita, T.; Saigusa, R.; Ichimura, Y.; Takahashi, T.; Toyama, T.; Yoshizaki, A.; Sato, S. Fli1 Deficiency Induces CXCL6 Expression in Dermal Fibroblasts and Endothelial Cells, Contributing to the Development of Fibrosis and Vasculopathy in Systemic Sclerosis. J. Rheumatol. 2017, 44, 1198–1205. [Google Scholar] [CrossRef]
- Taniguchi, T.; Miyagawa, T.; Toyama, S.; Yamashita, T.; Nakamura, K.; Saigusa, R.; Ichimura, Y.; Takahashi, T.; Toyama, T.; Yoshizaki, A.; et al. CXCL13 produced by macrophages due to Fli1 deficiency may contribute to the development of tissue fibrosis, vasculopathy and immune activation in systemic sclerosis. Exp. Dermatol. 2018, 27, 1030–1037. [Google Scholar] [CrossRef]
- Jiang, Z.; Chen, C.; Yang, S.; He, H.; Zhu, X.; Liang, M. Contribution to the peripheral vasculopathy and endothelial cell dysfunction by CXCL4 in Systemic Sclerosis. J. Dermatol. Sci. 2021, 104, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Ikawa, T.; Miyagawa, T.; Fukui, Y.; Toyama, S.; Omatsu, J.; Awaji, K.; Norimatsu, Y.; Watanabe, Y.; Yoshizaki, A.; Sato, S.; et al. Endothelial CCR6 expression due to FLI1 deficiency contributes to vasculopathy associated with systemic sclerosis. Arthritis Res. Ther. 2021, 23, 283. [Google Scholar] [CrossRef] [PubMed]
- Saigusa, R.; Asano, Y.; Yamashita, T.; Taniguchi, T.; Takahashi, T.; Ichimura, Y.; Toyama, T.; Yoshizaki, A.; Miyagaki, T.; Sugaya, M.; et al. Fli1 deficiency contributes to the downregulation of endothelial protein C receptor in systemic sclerosis: A possible role in prothrombotic conditions. Br. J. Dermatol. 2016, 174, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Miyagawa, T.; Taniguchi, T.; Saigusa, R.; Fukayama, M.; Takahashi, T.; Yamashita, T.; Hirabayashi, M.; Miura, S.; Nakamura, K.; Yoshizaki, A.; et al. Fli1 deficiency induces endothelial adipsin expression, contributing to the onset of pulmonary arterial hypertension in systemic sclerosis. Rheumatology 2020, 59, 2005–2015. [Google Scholar] [CrossRef]
- Mayes, M.D.; Trojanowska, M. Genetic factors in systemic sclerosis. Arthritis Res. Ther. 2007, 9, S5. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, K.; Kawasaki, A.; Matsushita, T.; Furukawa, H.; Kondo, Y.; Okiyama, N.; Nagaoka, S.; Shimada, K.; Sugii, S.; Katayama, M.; et al. Association of functional (GA)n microsatellite polymorphism in the FLI1 gene with susceptibility to human systemic sclerosis. Rheumatology 2020, 59, 3553–3562. [Google Scholar] [CrossRef]
- Wang, Y.; Fan, P.S.; Kahaleh, B. Association between enhanced type I collagen expression and epigenetic repression of the FLI1 gene in scleroderma fibroblasts. Arthritis Rheum. 2006, 54, 2271–2279. [Google Scholar] [CrossRef]
- Altorok, N.; Tsou, P.S.; Coit, P.; Khanna, D.; Sawalha, A.H. Genome-wide DNA methylation analysis in dermal fibroblasts from patients with diffuse and limited systemic sclerosis reveals common and subset-specific DNA methylation aberrancies. Ann. Rheum. Dis. 2015, 74, 1612–1620. [Google Scholar] [CrossRef]
- Jafarinejad-Farsangi, S.; Gharibdoost, F.; Farazmand, A.; Kavosi, H.; Jamshidi, A.; Karimizadeh, E.; Noorbakhsh, F.; Mahmoudi, M. MicroRNA-21 and microRNA-29a modulate the expression of collagen in dermal fibroblasts of patients with systemic sclerosis. Autoimmunity 2019, 52, 108–116. [Google Scholar] [CrossRef]
- Maurer, B.; Stanczyk, J.; Jüngel, A.; Akhmetshina, A.; Trenkmann, M.; Brock, M.; Kowal-Bielecka, O.; Gay, R.E.; Michel, B.A.; Distler, J.H.; et al. MicroRNA-29, a key regulator of collagen expression in systemic sclerosis. Arthritis Rheum. 2010, 62, 1733–1743. [Google Scholar] [CrossRef]
- Makino, K.; Jinnin, M.; Hirano, A.; Yamane, K.; Eto, M.; Kusano, T.; Honda, N.; Kajihara, I.; Makino, T.; Sakai, K.; et al. The downregulation of miR-let-7a contributes to the excessive expression of type I collagen in systemic and localized scleroderma. J. Immunol. 2013, 190, 3905–3915. [Google Scholar] [CrossRef]
- Makino, T.; Jinnin, M.; Etoh, M.; Yamane, K.; Kajihara, I.; IMakino, H.; Ichihara, A.; Igata, T.; Sakai, K.; Fukushima, S.; et al. Downregulation of microRNA-196a in the sera and involved skin of localized scleroderma patients. Eur. J. Dermatol. 2014, 24, 470–476. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, S.; Ciechomska, M.; Fullard, N.; Przyborski, S.; van Laar, J.M. IL-13 mediates collagen deposition via STAT6 and microRNA-135b: A role for epigenetics. Sci. Rep. 2016, 6, 25066. [Google Scholar] [CrossRef]
- Garikapati, K.; Goh, D.; Khanna, S.; Echampati, K. Uraemic Cardiomyopathy: A Review of Current Literature. Clin. Med. Insights Cardiol. 2021, 15, 1179546821998347. [Google Scholar] [CrossRef]
- Zhang, L.; Eddy, A.; Teng, Y.T.; Fritzler, M.; Kluppel, M.; Melet, F.; Bernstein, A. An immunological renal disease in transgenic mice that overexpress Fli-1, a member of the ets family of transcription factor genes. Mol. Cell. Biol. 1995, 15, 6961–6970. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, D.J.; Vetteth, S.; Periyasamy, S.M.; Kanj, M.; Fedorova, L.; Khouri, S.; Kahaleh, M.B.; Xie, Z.; Malhotra, D.; Kolodkin, N.I.; et al. Central role for the cardiotonic steroid marinobufagenin in the pathogenesis of experimental uremic cardiomyopathy. Hypertension 2006, 47, 488–495. [Google Scholar] [CrossRef]
- Elkareh, J.; Kennedy, D.J.; Yashaswi, B.; Vetteth, S.; Shidyak, A.; Kim, E.G.; Smaili, S.; Periyasamy, S.M.; Hariri, I.M.; Fedorova, L.; et al. Marinobufagenin stimulates fibroblast collagen production and causes fibrosis in experimental uremic cardiomyopathy. Hypertension 2007, 49, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Haller, S.T.; Kennedy, D.J.; Shidyak, A.; Budny, G.V.; Malhotra, D.; Fedorova, O.V.; Shapiro, J.I.; Bagrov, A.Y. Monoclonal antibody against marinobufagenin reverses cardiac fibrosis in rats with chronic renal failure. Am. J. Hypertens. 2012, 25, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Reznik, V.A.; Kashkin, V.A.; Agalakova, N.I.; Adair, C.D.; Bagrov, A.Y. Endogenous Bufadienolides, Fibrosis and Preeclampsia. Cardiol. Res. Pract. 2019, 2019, 5019287. [Google Scholar] [CrossRef] [PubMed]
- Dennehy, N.; Lees, C. Preeclampsia: Maternal cardiovascular function and optimising outcomes. Early Hum. Dev. 2022, 174, 105669. [Google Scholar] [CrossRef]
- Tossetta, G.; Fantone, S.; Muti, N.D.; Balercia, G.; Ciavattini, A.; Giannubilo, S.R.; Marzioni, D. Preeclampsia and severe acute respiratory syndrome coronavirus 2 infection: A systematic review. J. Hypertens. 2022, 40, 629–1638. [Google Scholar] [CrossRef] [PubMed]
- Opichka, M.A.; Rappelt, M.W.; Gutterman, D.D.; Grobe, J.L.; McIntosh, J.J. Vascular Dysfunction in Preeclampsia. Cells 2021, 10, 3055. [Google Scholar] [CrossRef] [PubMed]
- Nikitina, E.R.; Mikhailov, A.V.; Nikandrova, E.S.; Frolova, E.V.; Fadeev, A.V.; Shman, V.V.; Shilova, V.Y.; Tapilskaya, N.I.; Shapiro, J.I.; Fedorova, O.V.; et al. In preeclampsia endogenous cardiotonic steroids induce vascular fibrosis and impair relaxation of umbilical arteries. J. Hypertens. 2011, 29, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Fedorova, O.V.; Ishkaraeva, V.V.; Grigorova, Y.N.; Reznik, V.A.; Kolodkin, N.I.; Zazerskaya, I.E.; Zernetkina, V.; Agalakova, N.I.; Tapilskaya, N.I.; Adair, C.D.; et al. Antibody to Marinobufagenin Reverses Placenta-Induced Fibrosis of Umbilical Arteries in Preeclampsia. Int. J. Mol. Sci. 2018, 19, 2377. [Google Scholar] [CrossRef]
- Agalakova, N.I.; Grigorova, Y.N.; Ershov, I.A.; Reznik, V.A.; Mikhailova, E.V.; Nadei, O.V.; Samuilovskaya, L.; Romanova, L.A.; Adair, C.D.; Romanova, I.V.; et al. Canrenone Restores Vasorelaxation Impaired by Marinobufagenin in Human Preeclampsia. Int. J. Mol. Sci. 2022, 23, 3336. [Google Scholar] [CrossRef]
- Agalakova, N.I.; Reznik, V.A.; Nadei, O.V.; Ershov, I.A.; Rassokha, O.S.; Vasyutina, M.L.; Ivanov, D.O.; Adair, C.D.; Galagudza, M.M.; Bagrov, A.Y. Antibody against Na/K-ATPase Inhibitor Lowers Blood Pressure and Increases Vascular Fli1 in Experimental Preeclampsia. Am. J. Hypertens. 2020, 33, 514–519. [Google Scholar] [CrossRef]
- Agalakova, N.I.; Reznik, V.A.; Ershov, I.A.; Lupanova, E.A.; Nadei, O.V.; Ivanov, D.O.; Adair, C.D.; Bagrov, A.Y. Silencing of Fli1 Gene Mimics Effects of Preeclampsia and Induces Collagen Synthesis in Human Umbilical Arteries. Am. J. Hypertens. 2022, 35, 828–832. [Google Scholar] [CrossRef]
- Kolmakova, E.V.; Haller, S.T.; Kennedy, D.J.; Isachkina, A.N.; Budny, G.V.; Frolova, E.V.; Nikitina, E.R.; Piecha, G.; Malhotra, D.; Fedorova, O.V.; et al. Endogenous cardiotonic steroids in chronic renal failure. Nephrol. Dial. Transplant. 2011, 26, 2912–2919. [Google Scholar] [CrossRef]
- Fedorova, O.V.; Fadeev, A.V.; Grigorova, Y.N.; Agalakova, N.I.; Konradi, A.O.; Bagrov, A.Y. Marinobufagenin induces vascular fibrosis via a pressure-independent mechanism in NaCl-loaded diabetic rats. J. Cardiovasc. Pharmacol. 2019, 74, 436–442. [Google Scholar] [CrossRef]
- Zhang, Y.; Wei, W.; Shilova, V.; Petrashevskaya, N.N.; Zernetkina, V.I.; Grigorova, Y.N.; Marshall, C.A.; Fenner, R.C.; Lehrmann, E.; Wood, W.H., III; et al. Monoclonal Antibody to Marinobufagenin Downregulates TGFβ Profibrotic Signaling in Left Ventricle and Kidney and Reduces Tissue Remodeling in Salt-Sensitive Hypertension. J. Am. Heart Assoc. 2019, 8, e012138. [Google Scholar] [CrossRef]
- Grigorova, Y.N.; Juhasz, O.; Zernetkina, V.; Fishbein, K.W.; Fedorova, O.V.; Bagrov, A.Y. Monoclonal antibody to an endogenous sodium pump inhibitor marinobufagenin reverses aortic remodeling and stiffness in normotensive rats on a high salt intake. Am. J. Hypertens. 2016, 29, 641–646. [Google Scholar] [CrossRef]
- Grünewald, T.G.P.; Cidre-Aranaz, F.; Surdez, D.; Tomazou, E.M.; de Álava, E.; Kovar, H.; Sorensen, P.H.; Delattre, O.; Dirksen, U. Ewing sarcoma. Nat. Rev. Dis. Primers 2018, 4, 5. [Google Scholar] [CrossRef]
- Riggi, N.; Suvà, M.L.; Stamenkovic, I. Ewing’s Sarcoma. N. Eng. J. Med. 2021, 384, 154–164. [Google Scholar] [CrossRef]
- Uren, A.; Toretsky, J.A. Ewing’s sarcoma oncoprotein EWS-FLI1: The perfect target without a therapeutic agent. Future Oncol. 2005, 1, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Ban, J.; Siligan, C.; Kreppel, M.; Aryee, D.; Kovar, H. EWS-FLI1 in Ewing’s sarcoma: Real targets and collateral damage. Adv. Exp. Med. Biol. 2006, 587, 41–52. [Google Scholar] [CrossRef]
- Watanabe, G.; Nishimori, H.; Irifune, H.; Sasaki, Y.; Ishida, S.; Zembutsu, H.; Tanaka, T.; Kawaguchi, S.; Wada, T.; Hata, J.; et al. Induction of tenascin-C by tumor-specific EWS-ETS fusion genes. Genes Chromosomes Cancer 2003, 36, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Vasileva, E.; Warren, M.; Triche, T.J.; Amatruda, J.F. Dysregulated heparan sulfate proteoglycan metabolism promotes Ewing sarcoma tumor growth. eLife 2022, 11, e69734. [Google Scholar] [CrossRef]
- Bailly, R.A.; Bosselut, R.; Zucman, J.; Cormier, F.; Delattre, O.; Roussel, M.; Thomas, G.; Ghysdael, J. DNA-binding and transcriptional activation properties of the EWS-FLI-1 fusion protein resulting from the t(11;22) translocation in Ewing sarcoma. Mol. Cell. Biol. 1994, 14, 3230–3241. [Google Scholar] [PubMed]
- Lessnick, S.L.; Braun, B.S.; Denny, C.T.; May, W.A. Multiple domains mediate transformation by the Ewing’s sarcoma EWS/FLI-1 fusion gene. Oncogene 1995, 10, 423–431. [Google Scholar]
- Goldman, L.; Cecil, R.L.; Schafer, A.I. Goldman’s Cecil Medicine, 24th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2012. [Google Scholar]
- Johnson, K.M.; Taslim, C.; Saund, R.S.; Lessnick, S.L. Identification of two types of GGAA-microsatellites and their roles in EWS/FLI binding and gene regulation in Ewing sarcoma. PLoS ONE 2017, 12, e0186275. [Google Scholar] [CrossRef]
- Johnson, K.M.; Mahler, N.R.; Saund, R.S.; Theisen, E.R.; Taslim, C.; Callender, N.W.; Crow, J.C.; Miller, K.R.; Lessnick, S.L. Role for the EWS domain of EWS/FLI in binding GGAA-microsatellites required for Ewing sarcoma anchorage independent growth. Proc. Natl. Acad. Sci USA 2017, 114, 9870–9875. [Google Scholar] [CrossRef]
- Li, M.; Chen, C.W. Epigenetic and Transcriptional Signaling in Ewing Sarcoma-Disease Etiology and Therapeutic Opportunities. Biomedicines 2022, 10, 1325. [Google Scholar] [CrossRef]
- He, S.; Huang, Q.; Hu, J.; Li, L.; Xiao, Y.; Yu, H.; Han, Z.; Wang, T.; Zhou, W.; Wei, H.; et al. EWS-FLI1-mediated tenascin-C expression promotes tumor progression by targeting MALAT1 through integrin α5β1-mediated YAP activation in Ewing sarcoma. Br. J. Cancer 2019, 121, 922–933. [Google Scholar] [CrossRef] [PubMed]
- Silvany, R.E.; Eliazer, S.; Wolff, N.C.; Ilaria, R.L. Interference with the constitutive activation of ERK1 and ERK2 impairs EWS/FLI-1-dependent transformation. Oncogene 2000, 19, 4523–4530. [Google Scholar] [CrossRef]
- Lagares-Tena, L.; García-Monclús, S.; López-Alemany, R.; Almacellas-Rabaiget, O.; Huertas-Martínez, J.; Sáinz-Jaspeado, M.; Mateo-Lozano, S.; Rodríguez-Galindo, C.; Rello-Varona, S.; Herrero-Martín, D.; et al. Caveolin-1 promotes Ewing sarcoma metastasis regulating MMP-9 expression through MAPK/ERK pathway. Oncotarget 2016, 7, 56889–56903. [Google Scholar] [CrossRef]
- Agra, N.; Cidre, F.; García-García, L.; de la Parra, J.; Alonso, J. Lysyl oxidase is downregulated by the EWS/FLI1 oncoprotein and its propeptide domain displays tumor suppressor activities in Ewing sarcoma cells. PLoS ONE 2013, 8, e66281. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, A.G.; Pedersen, E.A.; Treichel, S.; Temprine, K.; Sperring, C.; Read, J.A.; Magnuson, B.; Chugh, R.; Lawlor, E.R. Wnt/β-catenin-activated Ewing sarcoma cells promote the angiogenic switch. JCI Insight 2020, 5, e135188. [Google Scholar] [CrossRef]
- Riggi, N.; Knoechel, B.; Gillespie, S.M.; Rheinbay, E.; Boulay, G.; Suvà, M.L.; Rossetti, N.E.; Boonseng, W.E.; Oksuz, O.; Cook, E.B.; et al. EWS-FLI1 utilizes divergent chromatin remodeling mechanisms to directly activate or repress enhancer elements in Ewing sarcoma. Cancer Cell 2014, 26, 668–681. [Google Scholar] [CrossRef] [PubMed]
- Montoya, C.; Rey, L.; Rodríguez, J.; Fernández, M.J.; Troncoso, D.; Cañas, A.; Moreno, O.; Henríquez, B.; Rojas, A. Epigenetic control of the EWS-FLI1 promoter in Ewing’s sarcoma. Oncol. Rep. 2020, 43, 1199–1207. [Google Scholar] [CrossRef]
- Matsumoto, Y.; Tanaka, K.; Nakatani, F.; Matsunobu, T.; Matsuda, S.; Iwamoto, Y. Downregulation and forced expression of EWS-Fli1 fusion gene results in changes in the expression of G(1)regulatory genes. Br. J. Cancer 2001, 84, 768–775. [Google Scholar] [CrossRef]
- Richter, G.H.; Plehm, S.; Fasan, A.; Rossler, S.; Unland, R.; Bennani-Baiti, I.M.; Hotfilder, M.; Lowel, D.; von Luettichau, I.; Mossbrugger, I.; et al. EZH2 is a mediator of EWS/FLI1 driven tumor growth and metastasis blocking endothelial and neuro-ectodermal differentiation. Proc. Natl. Acad. Sci. USA 2009, 106, 5324–5329. [Google Scholar] [CrossRef] [PubMed]
- Svoboda, L.K.; Harris, A.; Bailey, N.J.; Schwentner, R.; Tomazou, E.; von Levetzow, C.; Magnuson, B.; Ljungman, M.; Kovar, H.; Lawlor, E.R. Overexpression of HOX genes is prevalent in Ewing sarcoma and is associated with altered epigenetic regulation of developmental transcription programs. Epigenetics 2014, 12, 1613–1625. [Google Scholar] [CrossRef]
- Riggi, N.; Suvà, M.L.; De Vito, C.; Provero, P.; Stehle, J.C.; Baumer, K.; Cironi, L.; Janiszewska, M.; Petricevic, T.; Suvà, D.; et al. EWS-FLI-1 modulates miRNA145 and SOX2 expression to initiate mesenchymal stem cell reprogramming toward Ewing sarcoma cancer stem cells. Genes Dev. 2010, 24, 916–932. [Google Scholar] [CrossRef] [PubMed]
- Parrish, J.K.; Sechler, M.; Winn, R.A.; Jedlicka, P. The histone demethylase KDM3A is a microRNA-22-regulated tumor promoter in Ewing Sarcoma. Oncogene 2015, 34, 257–262. [Google Scholar] [CrossRef]
- De Feo, A.; Pazzaglia, L.; Ciuffarin, L.; Mangiagli, F.; Pasello, M.; Simonetti, E.; Pellegrini, E.; Ferrari, C.; Bianchi, G.; Spazzoli, B.; et al. miR-214-3p is commonly downregulated by EWS-FLI1 and by CD99 and its restoration limits Ewing sarcoma aggressiveness. Cancers 2022, 14, 1762. [Google Scholar] [CrossRef]
- De Vito, C.; Riggi, N.; Suvà, M.L.; Janiszewska, M.; Horlbeck, J.; Baumer, K.; Provero, P.; Stamenkovic, I. Let-7a is a direct EWS-FLI-1 target implicated in Ewing’s sarcoma development. PLoS ONE 2011, 6, e23592. [Google Scholar] [CrossRef]
- Daley, J.D.; Olson, A.C.; Bailey, K.M. Harnessing immunomodulation during DNA damage in Ewing sarcoma. Front. Oncol. 2022, 12, 1048705. [Google Scholar] [CrossRef]
- Brenner, J.C.; Feng, F.Y.; Han, S.; Patel, S.; Goyal, S.V.; Bou-Maroun, L.M.; Liu, M.; Lonigro, R.; Prensner, J.R.; Tomlins, S.A.; et al. PARP-1 inhibition as a targeted strategy to treat Ewing’s sarcoma. Cancer Res. 2012, 72, 1608–1613. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Huo, X.; Yang, Y.; Mo, Y.; Kollipara, R.K.; Kittler, R. Ablation of EWS-FLI1 by USP9X inhibition suppresses cancer cell growth in Ewing sarcoma. Cancer Lett. 2023, 552, 215984. [Google Scholar] [CrossRef]
- Erkizan, H.V.; Kong, Y.; Merchant, M.; Schlottmann, S.; Barber-Rotenberg, J.S.; Yuan, L.; Abaan, O.D.; Chou, T.H.; Dakshanamurthy, S.; Brown, M.L.; et al. A small molecule blocking oncogenic protein EWS-FLI1 interaction with RNA helicase A inhibits growth of Ewing’s sarcoma. Nat. Med. 2009, 15, 750–756. [Google Scholar] [CrossRef]
- Ludwig, J.A.; Federman, N.C.; Anderson, P.M.; Macy, M.E.; Riedel, R.F.; Davis, L.E.; Daw, N.C.; Wulff, J.; Kim, A.; Ratan, R.; et al. TK216 for relapsed/refractory Ewing sarcoma: Interim phase 1/2 results. J. Clin. Oncol. 2021, 39, 11500. [Google Scholar] [CrossRef]
- Hölting, T.L.B.; Cidre-Aranaz, F.; Matzek, D.; Popper, B.; Jacobi, S.J.; Funk, C.M.; Geyer, F.H.; Li, J.; Piseddu, I.; Cadilha, B.L.; et al. Neomorphic DNA-binding enables tumor-specific therapeutic gene expression in fusion-addicted childhood sarcoma. Mol. Cancer 2022, 21, 199. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, T.; Asano, Y.; Taniguchi, T.; Nakamura, K.; Saigusa, R.; Miura, S.; Toyama, T.; Takahashi, T.; Ichimura, Y.; Yoshizaki, A.; et al. Glycyrrhizin Ameliorates Fibrosis, Vasculopathy, and Inflammation in Animal Models of Systemic Sclerosis. J. Investig. Dermatol. 2017, 137, 631–640. [Google Scholar] [CrossRef]
- Yamashita, T.; Asano, Y.; Saigusa, R.; Taniguchi, T.; Hirabayashi, M.; Miyagawa, T.; Nakamura, K.; Miura, S.; Yoshizaki, A.; Trojanowska, M.; et al. Cyclophosphamide Pulse Therapy Normalizes Vascular Abnormalities in a Mouse Model of Systemic Sclerosis Vasculopathy. J. Investig. Dermatol. 2019, 139, 1150–1160. [Google Scholar] [CrossRef] [PubMed]
| Expression | Effect | Experimental System | References | |
|---|---|---|---|---|
| Tenascin-C (TNC) | ↑ | ECM growth | FLI1 transfection of human fibrosarcoma HT-1080 cells; human primary ES tumors; TNC-knockout cell lines; murine xenografts | [86,87,94] |
| ERK1/2 protein kinases | ↑ | Tumor growth; metastases; dysregulation of EMC metabolism | NIH-3T3 cells; human ES cell lines | [87,95] |
| Caveolin-1 (CAV1) | ↑ | Tumor growth; metastases; | Human ES cell lines; CAV1 silencing; murine xenografts | [96] |
| MMP-9 | ↑ | Tumor growth; metastases; dysregulation of EMC metabolism | Human ES cell lines; CAV1 silencing; murine xenografts | [96] |
| LOX | ↓ | Tumorigenesis | Human ES cell lines; murine xenografts | [97] |
| Wnt/β-catenin/TGF-β/SMAD | ↑ | Altered synthesis of ECM proteins; promotion of angiogenesis in local TME | Human ES cells; HUVECs; FLI1 knockdown | [98] |
| DNA methylation | ↓ | Tumorigenesis | Human ES cell lines; primary pediatric MSC; FLI1 knockdown; in vivo tumorigenesis | [99] |
| Histone acetylation, H3K4Me3, H3K9ac, H3K27ac markers at the FLI1 promoter | ↑ | FLI1 transcriptional activation; tumorigenesis | Human ES cell lines; primary pediatric MSC; primary tumor cells; FLI1 knockdown; in vivo tumorigenesis | [99,100] |
| Acetyltransferase p300 | ↑ | Tumorigenesis | Human ES cell lines; primary pediatric MSC; FLI1 knockdown; in vivo tumorigenesis | [99] |
| Cyclin G1, Cyclin D1 | ↑ | Tumorigenesis | Human SK-N-MC and PNKT-1 cell lines; murine xenografts; FLI1 transfected NIH3T3 cell | [101] |
| NR0B1 | ↑ | Increased ES susceptibility | ES A673 and HEK 293EBNA cell lines; FLI1 knockdown | [92] |
| Histone methyltransferase EZH2 | ↑ | Tumor development; metastases growth | ES and neuroblastoma cell lines; murine xenografts; RNA interference; FLI1 transfection | [102] |
| HOX genes | ↑ | Aberrant differentiation; tumorigenesis | ES cell lines; HeLa, neuroblastoma, HEK293FT, NCSC, BM-MSCs; FLI1 transduction of NCSC | [103] |
| miRNA-145 | ↓ | Tumorigenesis | hpMSCs; MSC; ES cell lines; mouse xenografts | [104] |
| miRNA-22 | ↓ | Tumor growth | ES A673 cells; miRNA-22 overexpression; murine xenografts | [105] |
| miRNA-214-3p | ↓ | Tumor growth | ES cell lines; human BM-MSCs; human ES primary tumors and metastases; FLI1 silencing | [106] |
| miRNA-let-7g | ↓ | Tumorigenesis | MSCs; ES cell lines; murine xenografts; FLI1 knockdown | [107] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mikhailova, E.V.; Romanova, I.V.; Bagrov, A.Y.; Agalakova, N.I. Fli1 and Tissue Fibrosis in Various Diseases. Int. J. Mol. Sci. 2023, 24, 1881. https://doi.org/10.3390/ijms24031881
Mikhailova EV, Romanova IV, Bagrov AY, Agalakova NI. Fli1 and Tissue Fibrosis in Various Diseases. International Journal of Molecular Sciences. 2023; 24(3):1881. https://doi.org/10.3390/ijms24031881
Chicago/Turabian StyleMikhailova, Elena V., Irina V. Romanova, Alexei Y. Bagrov, and Natalia I. Agalakova. 2023. "Fli1 and Tissue Fibrosis in Various Diseases" International Journal of Molecular Sciences 24, no. 3: 1881. https://doi.org/10.3390/ijms24031881
APA StyleMikhailova, E. V., Romanova, I. V., Bagrov, A. Y., & Agalakova, N. I. (2023). Fli1 and Tissue Fibrosis in Various Diseases. International Journal of Molecular Sciences, 24(3), 1881. https://doi.org/10.3390/ijms24031881









