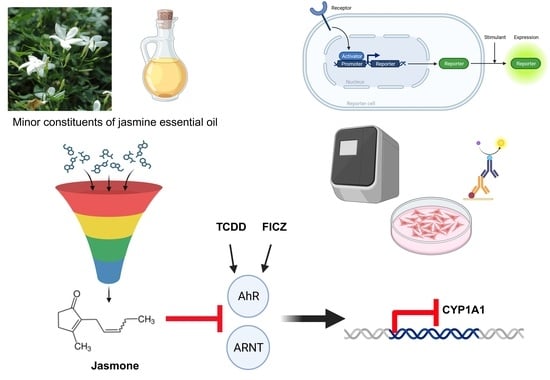
Jasmone Is a Ligand-Selective Allosteric Antagonist of Aryl Hydrocarbon Receptor (AhR)
Abstract
:1. Introduction
2. Results
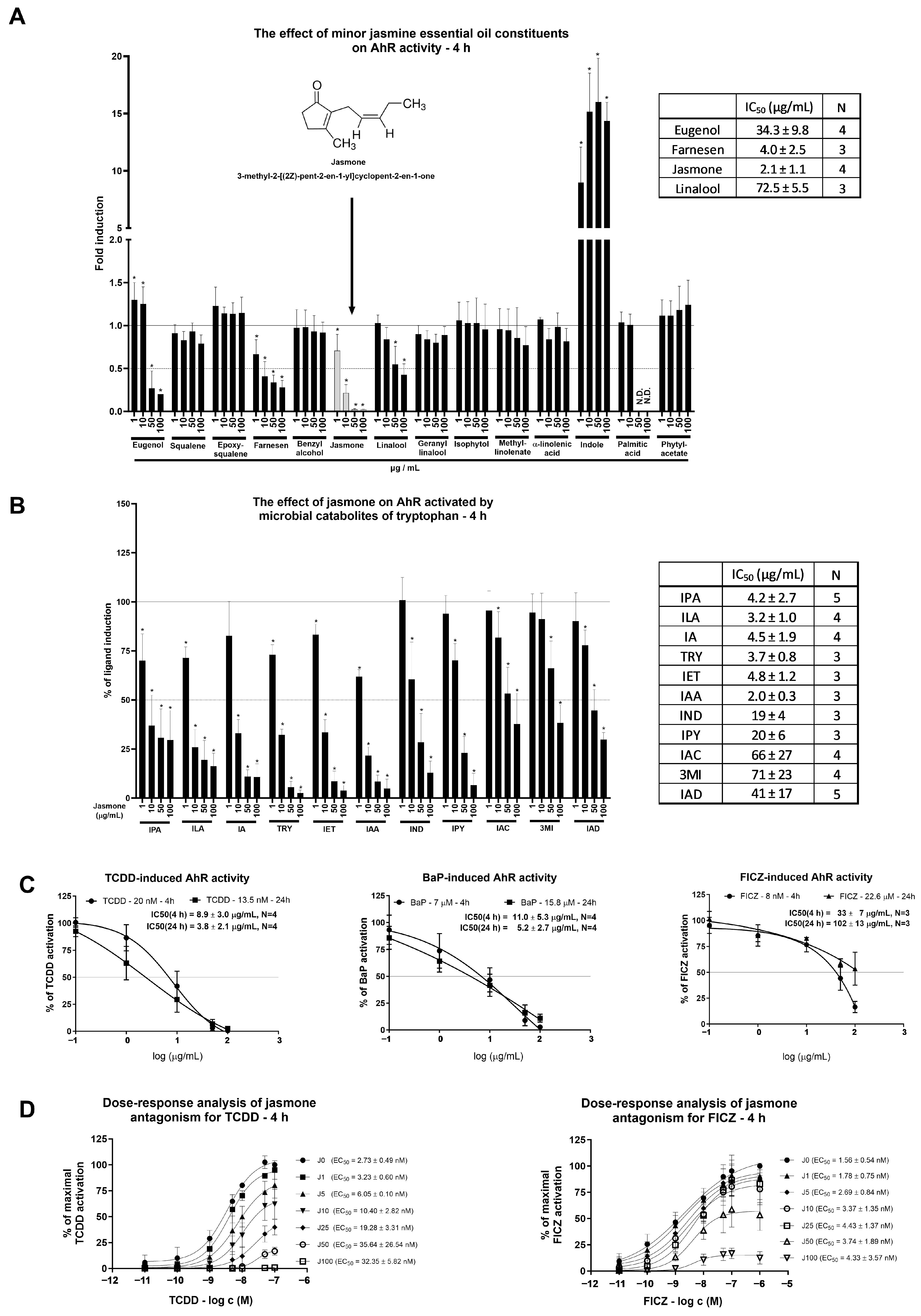
2.1. Jasmone Is an AhR Antagonist
2.2. Jasmone Suppresses Ligand-Triggered AhR-Regulated Genes
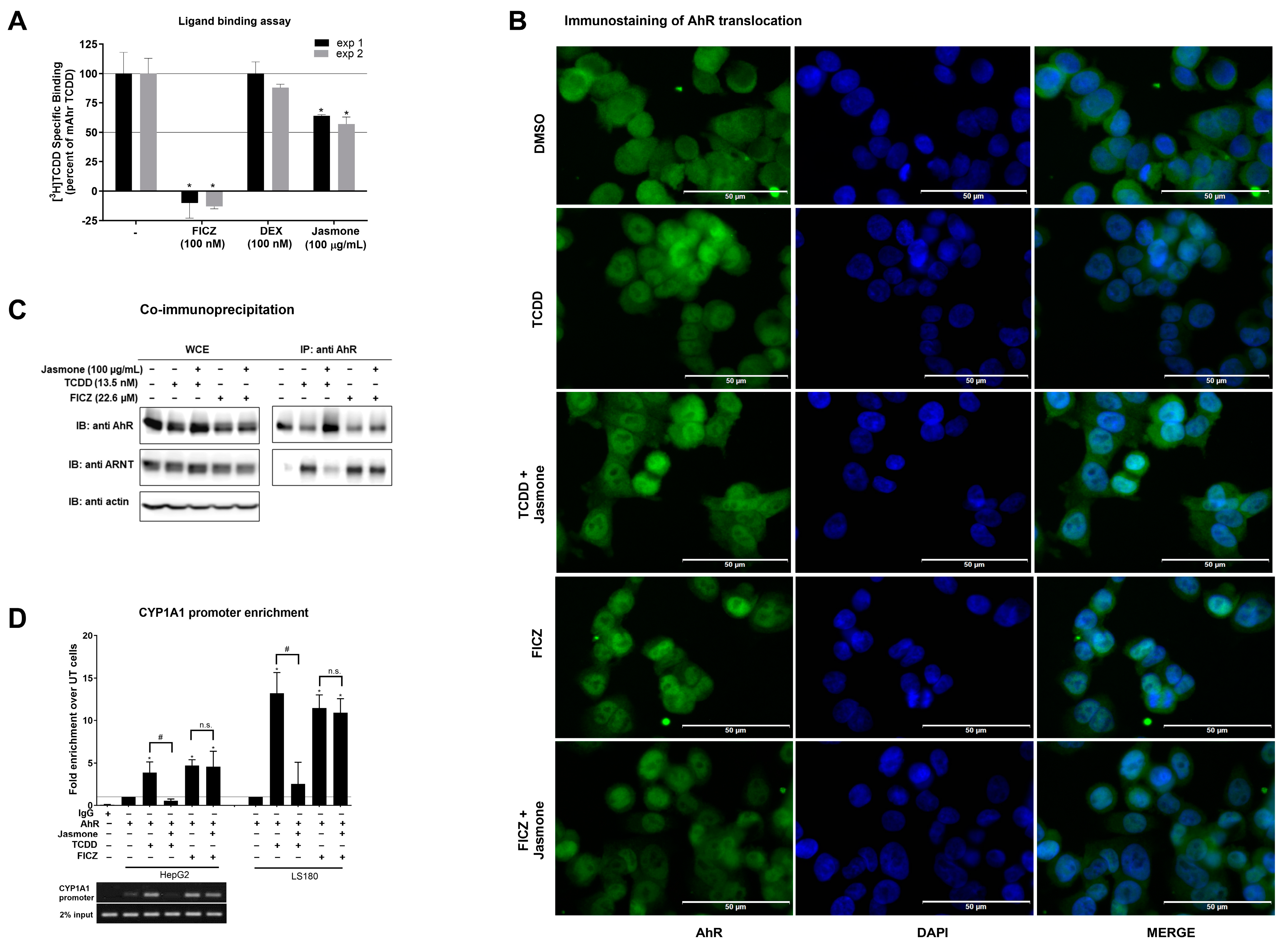
2.3. Jasmone Affects the Process of Dimerization in Ligand-Triggered AhR Signaling
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Cell Cultures
4.3. Human Hepatocytes
4.4. Immunostaining of AhR Translocation
4.5. Co-Immunoprecipitation (Co-IP)
4.6. SDS-PAGE and Western Blotting
4.7. Reporter Gene Assays (RGAs)
4.8. Chromatin Immunoprecipitation Assay (ChIP)
4.9. RNA Isolation, Reverse Transcription, and PCR
4.10. Radioligand Binding Assay
4.11. P450-Glo CYP1A1 Assay
4.12. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gu, Y.Z.; Hogenesch, J.B.; Bradfield, C.A. The PAS superfamily: Sensors of environmental and developmental signals. Annu. Rev. Pharmacol. Toxicol. 2000, 40, 519–561. [Google Scholar] [CrossRef] [PubMed]
- Poland, A.; Glover, E.; Kende, A.S. Stereospecific, high affinity binding of 2,3,7,8-tetrachlorodibenzo-p-dioxin by hepatic cytosol. Evidence that the binding species is receptor for induction of aryl hydrocarbon hydroxylase. J. Biol. Chem. 1976, 251, 4936–4946. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, J.; Ihara, K.; Nakayama, H.; Hikino, S.; Satoh, K.; Kubo, N.; Iida, T.; Fujii, Y.; Hara, T. Characteristic expression of aryl hydrocarbon receptor repressor gene in human tissues: Organ-specific distribution and variable induction patterns in mononuclear cells. Life Sci. 2004, 74, 1039–1049. [Google Scholar] [CrossRef]
- Kazlauskas, A.; Poellinger, L.; Pongratz, I. Two distinct regions of the immunophilin-like protein XAP2 regulate dioxin receptor function and interaction with hsp90. J. Biol. Chem. 2002, 277, 11795–11801. [Google Scholar] [CrossRef] [PubMed]
- Kazlauskas, A.; Poellinger, L.; Pongratz, I. Evidence that the co-chaperone p23 regulates ligand responsiveness of the dioxin (Aryl hydrocarbon) receptor. J. Biol. Chem. 1999, 274, 13519–13524. [Google Scholar] [CrossRef] [PubMed]
- Veldhoen, M.; Hirota, K.; Westendorf, A.M.; Buer, J.; Dumoutier, L.; Renauld, J.C.; Stockinger, B. The aryl hydrocarbon receptor links TH17-cell-mediated autoimmunity to environmental toxins. Nature 2008, 453, 106–109. [Google Scholar] [CrossRef]
- Haas, K.; Weighardt, H.; Deenen, R.; Kohrer, K.; Clausen, B.; Zahner, S.; Boukamp, P.; Bloch, W.; Krutmann, J.; Esser, C. Aryl Hydrocarbon Receptor in Keratinocytes Is Essential for Murine Skin Barrier Integrity. J. Investig. Dermatol. 2016, 136, 2260–2269. [Google Scholar] [CrossRef]
- Nebert, D.W.; Roe, A.L.; Dieter, M.Z.; Solis, W.A.; Yang, Y.; Dalton, T.P. Role of the aromatic hydrocarbon receptor and [Ah] gene battery in the oxidative stress response, cell cycle control, and apoptosis. Biochem. Pharmacol. 2000, 59, 65–85. [Google Scholar] [CrossRef]
- Davarinos, N.A.; Pollenz, R.S. Aryl hydrocarbon receptor imported into the nucleus following ligand binding is rapidly degraded via the cytosplasmic proteasome following nuclear export. J. Biol. Chem. 1999, 274, 28708–28715. [Google Scholar] [CrossRef]
- Denison, M.S.; Nagy, S.R. Activation of the aryl hydrocarbon receptor by structurally diverse exogenous and endogenous chemicals. Annu. Rev. Pharmacol. Toxicol. 2003, 43, 309–334. [Google Scholar] [CrossRef]
- Xue, Z.; Li, D.; Yu, W.; Zhang, Q.; Hou, X.; He, Y.; Kou, X. Mechanisms and therapeutic prospects of polyphenols as modulators of the aryl hydrocarbon receptor. Food Funct. 2017, 8, 1414–1437. [Google Scholar] [CrossRef]
- Hubbard, T.D.; Murray, I.A.; Perdew, G.H. Indole and Tryptophan Metabolism: Endogenous and Dietary Routes to Ah Receptor Activation. Drug Metab. Dispos. 2015, 43, 1522–1535. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.P.; Bradfield, C.A. The search for endogenous activators of the aryl hydrocarbon receptor. Chem. Res. Toxicol. 2008, 21, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Rannug, U.; Rannug, A.; Sjoberg, U.; Li, H.; Westerholm, R.; Bergman, J. Structure elucidation of two tryptophan-derived, high affinity Ah receptor ligands. Chem. Biol. 1995, 2, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, A.K.; Kerkvliet, N.I. Is chronic AhR activation by rapidly metabolized ligands safe for the treatment of immune-mediated diseases? Curr. Opin. Toxicol. 2017, 2, 72–78. [Google Scholar] [CrossRef]
- Giovannoni, F.; Li, Z.; Remes-Lenicov, F.; Davola, M.E.; Elizalde, M.; Paletta, A.; Ashkar, A.A.; Mossman, K.L.; Dugour, A.V.; Figueroa, J.M.; et al. AHR signaling is induced by infection with coronaviruses. Nat. Commun. 2021, 12, 5148. [Google Scholar] [CrossRef]
- Tongnuanchan, P.; Benjakul, S. Essential oils: Extraction, bioactivities, and their uses for food preservation. J. Food Sci. 2014, 79, R1231–R1249. [Google Scholar] [CrossRef]
- Bartonkova, I.; Dvorak, Z. Essential oils of culinary herbs and spices display agonist and antagonist activities at human aryl hydrocarbon receptor AhR. Food Chem. Toxicol. 2018, 111, 374–384. [Google Scholar] [CrossRef]
- Rotem, R.; Heyfets, A.; Fingrut, O.; Blickstein, D.; Shaklai, M.; Flescher, E. Jasmonates: Novel anticancer agents acting directly and selectively on human cancer cell mitochondria. Cancer Res. 2005, 65, 1984–1993. [Google Scholar] [CrossRef]
- Vyhlidalova, B.; Krasulova, K.; Pecinkova, P.; Marcalikova, A.; Vrzal, R.; Zemankova, L.; Vanco, J.; Travnicek, Z.; Vondracek, J.; Karasova, M.; et al. Gut Microbial Catabolites of Tryptophan Are Ligands and Agonists of the Aryl Hydrocarbon Receptor: A Detailed Characterization. Int. J. Mol. Sci. 2020, 21, 2614. [Google Scholar] [CrossRef]
- Vrzalova, A.; Pecinkova, P.; Illes, P.; Gurska, S.; Dzubak, P.; Szotkowski, M.; Hajduch, M.; Mani, S.; Dvorak, Z. Mixture Effects of Tryptophan Intestinal Microbial Metabolites on Aryl Hydrocarbon Receptor Activity. Int. J. Mol. Sci. 2022, 23, 10825. [Google Scholar] [CrossRef]
- Modoux, M.; Rolhion, N.; Lefevre, J.H.; Oeuvray, C.; Nadvornik, P.; Illes, P.; Emond, P.; Parc, Y.; Mani, S.; Dvorak, Z.; et al. Butyrate acts through HDAC inhibition to enhance aryl hydrocarbon receptor activation by gut microbiota-derived ligands. Gut Microbes 2022, 14, 2105637. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.W.; Dong, F.; Annalora, A.; Murray, I.A.; Wolfe, T.; Erickson, R.; Gowda, K.; Amin, S.G.; Petersen, K.S.; Kris-Etherton, P.M.; et al. Contribution of circulating host and microbial tryptophan metabolites towards Ah receptor activation. bioRxiv 2023. [Google Scholar] [CrossRef] [PubMed]
- Ondrova, K.; Zuvalova, I.; Vyhlidalova, B.; Krasulova, K.; Mikova, E.; Vrzal, R.; Nadvornik, P.; Nepal, B.; Kortagere, S.; Kopecna, M.; et al. Monoterpenoid aryl hydrocarbon receptor allosteric antagonists protect against ultraviolet skin damage in female mice. Nat. Commun. 2023, 14, 2728. [Google Scholar] [CrossRef] [PubMed]
- Giani Tagliabue, S.; Faber, S.C.; Motta, S.; Denison, M.S.; Bonati, L. Modeling the binding of diverse ligands within the Ah receptor ligand binding domain. Sci. Rep. 2019, 9, 10693. [Google Scholar] [CrossRef] [PubMed]
- Harper, P.A.; Giannone, J.V.; Okey, A.B.; Denison, M.S. In vitro transformation of the human Ah receptor and its binding to a dioxin response element. Mol. Pharmacol. 1992, 42, 603–612. [Google Scholar]
- Aarts, J.M.; Denison, M.S.; Cox, M.A.; Schalk, M.A.; Garrison, P.M.; Tullis, K.; de Haan, L.H.; Brouwer, A. Species-specific antagonism of Ah receptor action by 2,2′,5,5′-tetrachloro- and 2,2′,3,3′4,4′-hexachlorobiphenyl. Eur. J. Pharmacol. 1995, 293, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Boitano, A.E.; Wang, J.; Romeo, R.; Bouchez, L.C.; Parker, A.E.; Sutton, S.E.; Walker, J.R.; Flaveny, C.A.; Perdew, G.H.; Denison, M.S.; et al. Aryl hydrocarbon receptor antagonists promote the expansion of human hematopoietic stem cells. Science 2010, 329, 1345–1348. [Google Scholar] [CrossRef]
- Kalmes, M.; Blomeke, B. Impact of eugenol and isoeugenol on AhR translocation, target gene expression, and proliferation in human HaCaT keratinocytes. J. Toxicol. Environ. Health Part A 2012, 75, 478–491. [Google Scholar] [CrossRef]
- Yeruva, L.; Pierre, K.J.; Carper, S.W.; Elegbede, J.A.; Toy, B.J.; Wang, R.C. Jasmonates induce apoptosis and cell cycle arrest in non-small cell lung cancer lines. Exp. Lung Res. 2006, 32, 499–516. [Google Scholar] [CrossRef]
- Yeruva, L.; Elegbede, J.A.; Carper, S.W. Methyl jasmonate decreases membrane fluidity and induces apoptosis through tumor necrosis factor receptor 1 in breast cancer cells. Anticancer. Drugs 2008, 19, 766–776. [Google Scholar] [CrossRef]
- Yeruva, L.; Pierre, K.J.; Bathina, M.; Elegbede, A.; Carper, S.W. Delayed cytotoxic effects of methyl jasmonate and cis-jasmone induced apoptosis in prostate cancer cells. Cancer Investig. 2008, 26, 890–899. [Google Scholar] [CrossRef] [PubMed]
- Dong, F.; Annalora, A.J.; Murray, I.A.; Tian, Y.; Marcus, C.B.; Patterson, A.D.; Perdew, G.H. Endogenous Tryptophan-Derived Ah Receptor Ligands are Dissociated from CYP1A1/1B1-Dependent Negative-Feedback. Int. J. Tryptophan Res. 2023, 16, 11786469231182508. [Google Scholar] [CrossRef] [PubMed]
- Sanmarco, L.M.; Chao, C.C.; Wang, Y.C.; Kenison, J.E.; Li, Z.; Rone, J.M.; Rejano-Gordillo, C.M.; Polonio, C.M.; Gutierrez-Vazquez, C.; Piester, G.; et al. Identification of environmental factors that promote intestinal inflammation. Nature 2022, 611, 801–809. [Google Scholar] [CrossRef]
- Pichard-Garcia, L.; Gerbal-Chaloin, S.; Ferrini, J.B.; Fabre, J.M.; Maurel, P. Use of long-term cultures of human hepatocytes to study cytochrome P450 gene expression. Methods Enzymol. 2002, 357, 311–321. [Google Scholar] [PubMed]
- Vrzal, R.; Zenata, O.; Doricakova, A.; Dvorak, Z. Environmental pollutants parathion, paraquat and bisphenol A show distinct effects towards nuclear receptors-mediated induction of xenobiotics-metabolizing cytochromes P450 in human hepatocytes. Toxicol. Lett. 2015, 238, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Novotna, A.; Pavek, P.; Dvorak, Z. Novel stably transfected gene reporter human hepatoma cell line for assessment of aryl hydrocarbon receptor transcriptional activity: Construction and characterization. Environ. Sci. Technol. 2011, 45, 10133–10139. [Google Scholar] [CrossRef]
- Stepankova, M.; Bartonkova, I.; Jiskrova, E.; Vrzal, R.; Mani, S.; Kortagere, S.; Dvorak, Z. Methylindoles and Methoxyindoles are Agonists and Antagonists of Human Aryl Hydrocarbon Receptor. Mol. Pharmacol. 2018, 93, 631–644. [Google Scholar] [CrossRef]
- Zenata, O.; Dvorak, Z.; Vrzal, R. Profiling of bisphenol S towards nuclear receptors activities in human reporter cell lines. Toxicol. Lett. 2017, 281, 10–19. [Google Scholar] [CrossRef]
- Zenata, O.; Vrzalova, A.; Bachleda, P.; Janeckova, J.; Panacek, A.; Kvitek, L.; Vrzal, R. The effect of graphene oxide on signalling of xenobiotic receptors involved in biotransformation. Chemosphere 2020, 253, 126753. [Google Scholar] [CrossRef]

| Name of the Gene | Primer Sequences (F/R) | UPL Number |
|---|---|---|
| CYP1A1 | CCAGGCTCCAAGAGTCCA GATCTTGGAGGTGGCTGCT | 33 |
| CYP1A2 | ACAACCCTGCCAATCTCAAG GGGAACAGACTGGGACAATG | 34 |
| CYP1B1 | ACGTACCGGCCACTATCACT CTCGAGTCTGCACATCAGGA | 20 |
| AhRR | CAAAACCCAGAGCAGACACC CAGTTCCGATTCGCACAGA | 77 |
| GAPDH | CTCTGCTCCTCCTGTTCGAC ACGACCAAATCCGTTGACTC | 60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vrzal, R.; Marcalíková, A.; Krasulová, K.; Zemánková, L.; Dvořák, Z. Jasmone Is a Ligand-Selective Allosteric Antagonist of Aryl Hydrocarbon Receptor (AhR). Int. J. Mol. Sci. 2023, 24, 15655. https://doi.org/10.3390/ijms242115655
Vrzal R, Marcalíková A, Krasulová K, Zemánková L, Dvořák Z. Jasmone Is a Ligand-Selective Allosteric Antagonist of Aryl Hydrocarbon Receptor (AhR). International Journal of Molecular Sciences. 2023; 24(21):15655. https://doi.org/10.3390/ijms242115655
Chicago/Turabian StyleVrzal, Radim, Adéla Marcalíková, Kristýna Krasulová, Lenka Zemánková, and Zdeněk Dvořák. 2023. "Jasmone Is a Ligand-Selective Allosteric Antagonist of Aryl Hydrocarbon Receptor (AhR)" International Journal of Molecular Sciences 24, no. 21: 15655. https://doi.org/10.3390/ijms242115655
APA StyleVrzal, R., Marcalíková, A., Krasulová, K., Zemánková, L., & Dvořák, Z. (2023). Jasmone Is a Ligand-Selective Allosteric Antagonist of Aryl Hydrocarbon Receptor (AhR). International Journal of Molecular Sciences, 24(21), 15655. https://doi.org/10.3390/ijms242115655