Current Review of Increasing Animal Health Threat of Per- and Polyfluoroalkyl Substances (PFAS): Harms, Limitations, and Alternatives to Manage Their Toxicity
Abstract
1. Introduction
1.1. Presence of PFAS Worldwide
1.2. Regulation and Restrictions on PFAS Use
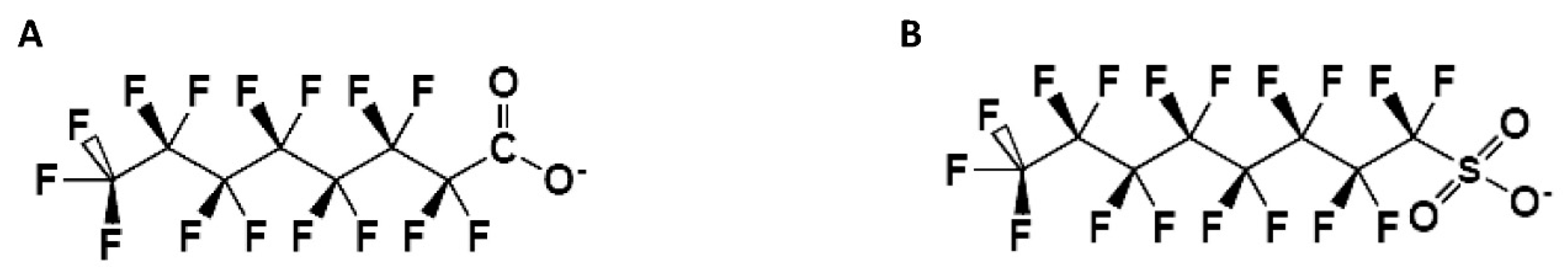
2. PFAS Characteristics
2.1. Structure and Physical Characteristics
2.2. Benefits of Using PFAS
2.3. Mechanisms of Action of PFAS
3. Commercial Uses
3.1. PFAS in Industrial and Consumer Applications
3.2. Do PFAS Present in Alternative Plastic Packaging Migrate into Food?
3.3. PFAS and Pesticides
4. PFAS Exposure: The Risks to Animal Health
4.1. PFOA and PFOS Toxicology
4.2. PFAS in Domestic Environments and the Risk of Exposure to Pets
4.3. PFAS Exposure and the Health Management of Farm Animals
4.4. The Effects of Pre- and Postnatal PFAS Exposure
5. Correlation of Geographic Area and Risk
5.1. Animals
5.2. Human
6. Natural Substances with Low Environmental Impact
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sunderland, E.M.; Hu, X.C.; Dassuncao, C.; Tokranov, A.K.; Wagner, C.C.; Allen, J.G. A review of the pathways of human exposure to poly-and perfluoroalkyl substances (PFASs) and present understanding of health effects. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 131–147. [Google Scholar] [CrossRef] [PubMed]
- Butt, C.M.; Berger, U.; Bossi, R.; Tomy, G.T. Levels and trends of poly-and perfluorinated compounds in the arctic environment. Sci. Total Environ. 2010, 408, 2936–2965. [Google Scholar] [CrossRef] [PubMed]
- Schiavone, A.; Corsolini, S.; Kannan, K.; Tao, L.; Trivelpiece, W.; Torres Jr, D.; Focardi, S. Perfluorinated contaminants in fur seal pups and penguin eggs from South Shetland, Antarctica. Sci. Total Environ. 2009, 407, 3899–3904. [Google Scholar] [CrossRef] [PubMed]
- Foguth, R.; Sepúlveda, M.S.; Cannon, J. Per-and polyfluoroalkyl substances (PFAS) neurotoxicity in sentinel and non-traditional laboratory model systems: Potential utility in predicting adverse outcomes in human health. Toxics 2020, 8, 42. [Google Scholar] [CrossRef] [PubMed]
- Costello, E.; Rock, S.; Stratakis, N.; Eckel, S.P.; Walker, D.I.; Valvi, D.; Cserbik, D.; Jenkins, T.; Xanthakos, S.A.; Kohli, R. Exposure to per-and polyfluoroalkyl substances and markers of liver injury: A systematic review and meta-analysis. Environ. Health Perspect. 2022, 130, 046001. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S.; Vasudevan, N. Impacts of perfluorinated compounds on human health. Bull. Environ. Pharmacol. Life Sci. 2015, 4, 183–191. [Google Scholar]
- Giesy, J.P.; Kannan, K. Global distribution of perfluorooctane sulfonate in wildlife. Environ. Sci. Technol. 2001, 35, 1339–1342. [Google Scholar] [CrossRef]
- Houde, M.; De Silva, A.O.; Muir, D.C.; Letcher, R.J. Monitoring of perfluorinated compounds in aquatic biota: An updated review: PFCs in aquatic biota. Environ. Sci. Technol. 2011, 45, 7962–7973. [Google Scholar] [CrossRef]
- Reiner, J.L.; Place, B.J. Perfluorinated alkyl acids in wildlife. In Toxicological Effects of Perfluoroalkyl and Polyfluoroalkyl Substances; Springer: Basel, Switzerland, 2015; pp. 127–150. [Google Scholar]
- Muir, D.; Bossi, R.; Carlsson, P.; Evans, M.; De Silva, A.; Halsall, C.; Rauert, C.; Herzke, D.; Hung, H.; Letcher, R. Levels and trends of poly-and perfluoroalkyl substances in the Arctic environment–An update. Emerg. Contam. 2019, 5, 240–271. [Google Scholar] [CrossRef]
- Koch, A.; Jonsson, M.; Yeung, L.W.; Karrman, A.; Ahrens, L.; Ekblad, A.; Wang, T. Quantification of biodriven transfer of per-and polyfluoroalkyl substances from the aquatic to the terrestrial environment via emergent insects. Environ. Sci. Technol. 2021, 55, 7900–7909. [Google Scholar] [CrossRef]
- Houde, M.; Martin, J.W.; Letcher, R.J.; Solomon, K.R.; Muir, D.C. Biological monitoring of polyfluoroalkyl substances: A review. Environ. Sci. Technol. 2006, 40, 3463–3473. [Google Scholar] [CrossRef] [PubMed]
- Lindstrom, A.B.; Strynar, M.J.; Libelo, E.L. Polyfluorinated compounds: Past, present, and future. Environ. Sci. Technol. 2011, 45, 7954–7961. [Google Scholar] [CrossRef] [PubMed]
- Surma, M.; Zieliński, H.; Piskuła, M. Levels of contamination by perfluoroalkyl substances in honey from selected European countries. Bull. Environ. Contam. Toxicol. 2016, 97, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Convention, S. All POPs Listed in the Stockholm Convention. Available online: https://chm.pops.int/TheConvention/ThePOPs/ListingofPOPs/tabid/2509/Default.aspx (accessed on 17 July 2023).
- EFSA 2008. Perfluorooctane sulfonate (PFOS), perfluorooctanoic acid (PFOA) and their salts Scientific Opinion of the Panel on Contaminants in the Food chain EFSA J. 2008, 653, 1–131.
- Mandard, S.; Müller, M.; Kersten, S. Peroxisome proliferator-activated receptor α target genes. Cell. Mol. Life Sci. CMLS 2004, 61, 393–416. [Google Scholar] [CrossRef]
- Leonard, R.C.; Kreckmann, K.H.; Sakr, C.J.; Symons, J.M. Retrospective cohort mortality study of workers in a polymer production plant including a reference population of regional workers. Ann. Epidemiol. 2008, 18, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-Y.; Lin, L.-Y.; Chiang, C.-K.; Wang, W.-J.; Su, Y.-N.; Hung, K.-Y.; Chen, P.-C. Investigation of the associations between low-dose serum perfluorinated chemicals and liver enzymes in US adults. Off. J. Am. Coll. Gastroenterol. ACG 2010, 105, 1354–1363. [Google Scholar] [CrossRef] [PubMed]
- Lundin, J.I.; Alexander, B.H.; Olsen, G.W.; Church, T.R. Ammonium perfluorooctanoate production and occupational mortality. Epidemiology 2009, 20, 921–928. [Google Scholar] [CrossRef]
- Kudo, N.; Kawashima, Y. Fish oil-feeding prevents perfluorooctanoic acid-induced fatty liver in mice. Toxicol. Appl. Pharmacol. 1997, 145, 285–293. [Google Scholar] [CrossRef]
- Martin, M.T.; Brennan, R.J.; Hu, W.; Ayanoglu, E.; Lau, C.; Ren, H.; Wood, C.R.; Corton, J.C.; Kavlock, R.J.; Dix, D.J. Toxicogenomic study of triazole fungicides and perfluoroalkyl acids in rat livers predicts toxicity and categorizes chemicals based on mechanisms of toxicity. Toxicol. Sci. 2007, 97, 595–613. [Google Scholar] [CrossRef]
- Kersten, S.; Desvergne, B.; Wahli, W. Roles of PPARs in health and disease. Nature 2000, 405, 421–424. [Google Scholar] [CrossRef] [PubMed]
- la Cour Poulsen, L.; Siersbæk, M.; Mandrup, S. PPARs: Fatty acid sensors controlling metabolism. Proc. Semin. Cell Dev. Biol. 2012, 23, 631–639. [Google Scholar] [CrossRef]
- Elcombe, C.R.; Elcombe, B.M.; Foster, J.R.; Farrar, D.G.; Jung, R.; Chang, S.-C.; Kennedy, G.L.; Butenhoff, J.L. Hepatocellular hypertrophy and cell proliferation in Sprague–Dawley rats following dietary exposure to ammonium perfluorooctanoate occurs through increased activation of the xenosensor nuclear receptors PPARα and CAR/PXR. Arch. Toxicol. 2010, 84, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.B.; Lee, J.S.; Ren, H.; Vallanat, B.; Liu, J.; Waalkes, M.P.; Abbott, B.D.; Lau, C.; Corton, J.C. Toxicogenomic dissection of the perfluorooctanoic acid transcript profile in mouse liver: Evidence for the involvement of nuclear receptors PPARα and CAR. Toxicol. Sci. 2008, 103, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Klaassen, C.D. Perfluorocarboxylic acids induce cytochrome P450 enzymes in mouse liver through activation of PPAR-α and CAR transcription factors. Toxicol. Sci. 2008, 106, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Vanden Heuvel, J.P.; Thompson, J.T.; Frame, S.R.; Gillies, P.J. Differential activation of nuclear receptors by perfluorinated fatty acid analogs and natural fatty acids: A comparison of human, mouse, and rat peroxisome proliferator-activated receptor-α,-β, and-γ, liver X receptor-β, and retinoid X receptor-α. Toxicol. Sci. 2006, 92, 476–489. [Google Scholar] [CrossRef] [PubMed]
- Bjork, J.; Butenhoff, J.; Wallace, K.B. Multiplicity of nuclear receptor activation by PFOA and PFOS in primary human and rodent hepatocytes. Toxicology 2011, 288, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.H.; Rifas-Shiman, S.L.; Calafat, A.M.; Ye, X.; Mora, A.M.; Webster, T.F.; Oken, E.; Sagiv, S.K. Predictors of per-and polyfluoroalkyl substance (PFAS) plasma concentrations in 6–10 year old American children. Environ. Sci. Technol. 2017, 51, 5193–5204. [Google Scholar] [CrossRef]
- Pérez, F.; Nadal, M.; Navarro-Ortega, A.; Fabrega, F.; Domingo, J.L.; Barceló, D.; Farré, M. Accumulation of perfluoroalkyl substances in human tissues. Environ. Int. 2013, 59, 354–362. [Google Scholar] [CrossRef]
- Buck, R.C.; Franklin, J.; Berger, U.; Conder, J.M.; Cousins, I.T.; De Voogt, P.; Jensen, A.A.; Kannan, K.; Mabury, S.A.; van Leeuwen, S.P. Perfluoroalkyl and polyfluoroalkyl substances in the environment: Terminology, classification, and origins. Integr. Environ. Assess. Manag. 2011, 7, 513–541. [Google Scholar] [CrossRef]
- Richard Head JD, M. PFAS regulations: How we got here and how to recover the costs. J. N. Engl. Water Work. Assoc. 2019, 133, 239–242. [Google Scholar]
- Lindström, T.; Larsson, P.T. Alkyl ketene dimer (AKD) sizing–A review. Nord. Pulp Pap. Res. J. 2008, 23, 202–209. [Google Scholar] [CrossRef]
- Dean, W.S.; Adejumo, H.A.; Caiati, A.; Garay, P.M.; Harmata, A.S.; Li, L.; Rodriguez, E.E.; Sundar, S. A Framework for Regulation of New and Existing PFAS by EPA. J. Sci. Policy Gov. 2020, 16, 14. [Google Scholar]
- Sinclair, E.; Kim, S.K.; Akinleye, H.B.; Kannan, K. Quantitation of gas-phase perfluoroalkyl surfactants and fluorotelomer alcohols released from nonstick cookware and microwave popcorn bags. Environ. Sci. Technol. 2007, 41, 1180–1185. [Google Scholar] [CrossRef] [PubMed]
- Begley, T.; Hsu, W.; Noonan, G.; Diachenko, G. Migration of fluorochemical paper additives from food-contact paper into foods and food simulants. Food Addit. Contam. 2008, 25, 384–390. [Google Scholar] [CrossRef]
- Schwartz-Narbonne, H.; Xia, C.; Shalin, A.; Whitehead, H.D.; Yang, D.; Peaslee, G.F.; Wang, Z.; Wu, Y.; Peng, H.; Blum, A. Per-and Polyfluoroalkyl Substances in Canadian Fast Food Packaging. Environ. Sci. Technol. Lett. 2023, 10, 343–349. [Google Scholar] [CrossRef]
- Whitehead, H.D.; Peaslee, G.F. Directly Fluorinated Containers as a Source of Perfluoroalkyl Carboxylic Acids. Environ. Sci. Technol. Lett. 2023, 10, 350–355. [Google Scholar] [CrossRef]
- Glüge, J.; Scheringer, M.; Cousins, I.T.; DeWitt, J.C.; Goldenman, G.; Herzke, D.; Lohmann, R.; Ng, C.A.; Trier, X.; Wang, Z. An overview of the uses of per-and polyfluoroalkyl substances (PFAS). Environ. Sci. Process. Impacts 2020, 22, 2345–2373. [Google Scholar] [CrossRef]
- Lasee, S.; McDermett, K.; Kumar, N.; Guelfo, J.; Payton, P.; Yang, Z.; Anderson, T.A. Targeted analysis and Total Oxidizable Precursor assay of several insecticides for PFAS. J. Hazard. Mater. Lett. 2022, 3, 100067. [Google Scholar] [CrossRef]
- Lasee, S.; Subbiah, S.; Deb, S.; Karnjanapiboonwong, A.; Payton, P.; Anderson, T.A. The effects of soil organic carbon content on plant uptake of soil perfluoro alkyl acids (PFAAs) and the potential regulatory implications. Environ. Toxicol. Chem. 2021, 40, 820–833. [Google Scholar] [CrossRef]
- Lasee, S.; Subbiah, S.; Thompson, W.A.; Karnjanapiboonwong, A.; Jordan, J.; Payton, P.; Anderson, T.A. Plant uptake of per-and polyfluoroalkyl acids under a maximum bioavailability scenario. Environ. Toxicol. Chem. 2019, 38, 2497–2502. [Google Scholar] [CrossRef] [PubMed]
- Di Paola, D.; Natale, S.; Iaria, C.; Crupi, R.; Cuzzocrea, S.; Spanò, N.; Gugliandolo, E.; Peritore, A.F. Environmental Co-Exposure to Potassium Perchlorate and Cd Caused Toxicity and Thyroid Endocrine Disruption in Zebrafish Embryos and Larvae (Danio rerio). Toxics 2022, 10, 198. [Google Scholar] [CrossRef] [PubMed]
- Di Paola, D.; Capparucci, F.; Lanteri, G.; Cordaro, M.; Crupi, R.; Siracusa, R.; D’Amico, R.; Fusco, R.; Impellizzeri, D.; Cuzzocrea, S. Combined toxicity of xenobiotics Bisphenol A and heavy metals on zebrafish embryos (Danio rerio). Toxics 2021, 9, 344. [Google Scholar] [CrossRef]
- Paola, D.D.; Capparucci, F.; Natale, S.; Crupi, R.; Cuzzocrea, S.; Spanò, N.; Gugliandolo, E.; Peritore, A.F. Combined Effects of Potassium Perchlorate and a Neonicotinoid on Zebrafish Larvae (Danio rerio). Toxics 2022, 10, 203. [Google Scholar] [CrossRef]
- Di Paola, D.; Gugliandolo, E.; Capparucci, F.; Cordaro, M.; Iaria, C.; Siracusa, R.; D’Amico, R.; Fusco, R.; Impellizzeri, D.; Cuzzocrea, S. Early Exposure to Environmental Pollutants: Imidacloprid Potentiates Cadmium Toxicity on Zebrafish Retinal Cells Death. Animals 2022, 12, 3484. [Google Scholar] [CrossRef]
- Paola, D.D.; Iaria, C.; Marino, F.; Gugliandolo, E.; Piras, C.; Crupi, R.; Cuzzocrea, S.; Spanò, N.; Britti, D.; Peritore, A.F. Environmental Impact of Pharmaceutical Pollutants: Synergistic Toxicity of Ivermectin and Cypermethrin. Toxics 2022, 10, 388. [Google Scholar] [CrossRef]
- Olsen, G.W.; Burris, J.M.; Ehresman, D.J.; Froehlich, J.W.; Seacat, A.M.; Butenhoff, J.L.; Zobel, L.R. Half-life of serum elimination of perfluorooctanesulfonate, perfluorohexanesulfonate, and perfluorooctanoate in retired fluorochemical production workers. Environ. Health Perspect. 2007, 115, 1298–1305. [Google Scholar] [CrossRef]
- Butenhoff, J.L.; Chang, S.-C.; Olsen, G.W.; Thomford, P.J. Chronic dietary toxicity and carcinogenicity study with potassium perfluorooctanesulfonate in Sprague Dawley rats. Toxicology 2012, 293, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.T.; Adami, H.-O.; Boffetta, P.; Cole, P.; Starr, T.B.; Mandel, J.S. A critical review of perfluorooctanoate and perfluorooctanesulfonate exposure and cancer risk in humans. Crit. Rev. Toxicol. 2014, 44, 1–81. [Google Scholar] [CrossRef]
- United Nations Environment Programme, Chemicals; Global Environment Facility. Regional Reports of the Regionally Based Assessment of Persistent Toxic Substances Programme; United Nations: New York, NY, USA, 2013. [Google Scholar]
- Kudo, N.; Kawashima, Y. Toxicity and toxicokinetics of perfluorooctanoic acid in humans and animals. J. Toxicol. Sci. 2003, 28, 49–57. [Google Scholar] [CrossRef]
- Tsuda, S. Differential toxicity between perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA). J. Toxicol. Sci. 2016, 41, SP27–SP36. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.A. Perfluorooctanoic acid (PFOA). In Understanding Risk to Wildlife from Exposures to Per-and Polyfluorinated Alkyl Substances (PFAS); CRC Press: Boca Raton, FL, USA, 2021; pp. 5–52. [Google Scholar]
- D’eon, J.C.; Mabury, S.A. Exploring indirect sources of human exposure to perfluoroalkyl carboxylates (PFCAs): Evaluating uptake, elimination, and biotransformation of polyfluoroalkyl phosphate esters (PAPs) in the rat. Environ. Health Perspect. 2011, 119, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Whitacre, D.M. Reviews of Environmental Contamination and Toxicology; Springer: Berlin/Heidelberg, Germany, 2008; Volume 202. [Google Scholar]
- Kariuki, M.N.; Nagato, E.G.; Lankadurai, B.P.; Simpson, A.J.; Simpson, M.J. Analysis of sub-lethal toxicity of perfluorooctane sulfonate (PFOS) to Daphnia magna using 1H nuclear magnetic resonance-based metabolomics. Metabolites 2017, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Land, M.; De Wit, C.A.; Bignert, A.; Cousins, I.T.; Herzke, D.; Johansson, J.H.; Martin, J.W. What is the effect of phasing out long-chain per-and polyfluoroalkyl substances on the concentrations of perfluoroalkyl acids and their precursors in the environment? A systematic review. Environ. Evid. 2018, 7, 4. [Google Scholar] [CrossRef]
- Ma, J.; Zhu, H.; Kannan, K. Fecal excretion of perfluoroalkyl and polyfluoroalkyl substances in pets from New York State, United States. Environ. Sci. Technol. Lett. 2020, 7, 135–142. [Google Scholar] [CrossRef]
- Wang, M.; Guo, W.; Gardner, S.; Petreas, M.; Park, J.S. Per-and polyfluoroalkyl substances in Northern California cats: Temporal comparison and a possible link to cat hyperthyroidism. Environ. Toxicol. Chem. 2018, 37, 2523–2529. [Google Scholar] [CrossRef]
- Glenn, G.; Shogren, R.; Jin, X.; Orts, W.; Hart-Cooper, W.; Olson, L. Per-and polyfluoroalkyl substances and their alternatives in paper food packaging. Compr. Rev. Food Sci. Food Saf. 2021, 20, 2596–2625. [Google Scholar] [CrossRef] [PubMed]
- Chain, E.P.o.C.i.t.F.; Schrenk, D.; Bignami, M.; Bodin, L.; Chipman, J.K.; del Mazo, J.; Grasl-Kraupp, B.; Hogstrand, C.; Hoogenboom, L.; Leblanc, J.C. Risk to human health related to the presence of perfluoroalkyl substances in food. EFSA J. 2020, 18, e06223. [Google Scholar]
- Yue, Y.; Li, S.; Qian, Z.; Pereira, R.F.; Lee, J.; Doherty, J.J.; Zhang, Z.; Peng, Y.; Clark, J.M.; Timme-Laragy, A.R. Perfluorooctanesulfonic acid (PFOS) and perfluorobutanesulfonic acid (PFBS) impaired reproduction and altered offspring physiological functions in Caenorhabditis elegans. Food Chem. Toxicol. 2020, 145, 111695. [Google Scholar] [CrossRef] [PubMed]
- Guruge, K.S.; Manage, P.M.; Yamanaka, N.; Miyazaki, S.; Taniyasu, S.; Yamashita, N. Species-specific concentrations of perfluoroalkyl contaminants in farm and pet animals in Japan. Chemosphere 2008, 73, S210–S215. [Google Scholar] [CrossRef]
- Vestergren, R.; Orata, F.; Berger, U.; Cousins, I.T. Bioaccumulation of perfluoroalkyl acids in dairy cows in a naturally contaminated environment. Environ. Sci. Pollut. Res. 2013, 20, 7959–7969. [Google Scholar] [CrossRef]
- Kowalczyk, J.; Ehlers, S.; Fürst, P.; Schafft, H.; Lahrssen-Wiederholt, M. Transfer of perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS) from contaminated feed into milk and meat of sheep: Pilot study. Arch. Environ. Contam. Toxicol. 2012, 63, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, J.; Ehlers, S.; Oberhausen, A.; Tischer, M.; Fürst, P.; Schafft, H.; Lahrssen-Wiederholt, M. Absorption, distribution, and milk secretion of the perfluoroalkyl acids PFBS, PFHxS, PFOS, and PFOA by dairy cows fed naturally contaminated feed. J. Agric. Food Chem. 2013, 61, 2903–2912. [Google Scholar] [CrossRef] [PubMed]
- Lupton, S.J.; Huwe, J.K.; Smith, D.J.; Dearfield, K.L.; Johnston, J.J. Distribution and excretion of perfluorooctane sulfonate (PFOS) in beef cattle (Bos taurus). J. Agric. Food Chem. 2014, 62, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Lupton, S.J.; Dearfield, K.L.; Johnston, J.J.; Wagner, S.; Huwe, J.K. Perfluorooctane sulfonate plasma half-life determination and long-term tissue distribution in beef cattle (Bos taurus). J. Agric. Food Chem. 2015, 63, 10988–10994. [Google Scholar] [CrossRef]
- Zafeiraki, E.; Costopoulou, D.; Vassiliadou, I.; Leondiadis, L.; Dassenakis, E.; Hoogenboom, R.L.; van Leeuwen, S.P. Perfluoroalkylated substances (PFASs) in home and commercially produced chicken eggs from the Netherlands and Greece. Chemosphere 2016, 144, 2106–2112. [Google Scholar] [CrossRef]
- Wilson, T.B.; Stevenson, G.; Crough, R.; de Araujo, J.; Fernando, N.; Anwar, A.; Scott, T.; Quinteros, J.A.; Scott, P.C.; Archer, M.J. Evaluation of Residues in Hen Eggs After Exposure of Laying Hens to Water Containing Per-and Polyfluoroalkyl Substances. Environ. Toxicol. Chem. 2021, 40, 735–743. [Google Scholar] [CrossRef]
- Zafeiraki, E.; Vassiliadou, I.; Costopoulou, D.; Leondiadis, L.; Schafft, H.A.; Hoogenboom, R.L.; van Leeuwen, S.P. Perfluoroalkylated substances in edible livers of farm animals, including depuration behaviour in young sheep fed with contaminated grass. Chemosphere 2016, 156, 280–285. [Google Scholar] [CrossRef]
- Yeung, L.W.; Loi, E.I.; Wong, V.Y.; Guruge, K.S.; Yamanaka, N.; Tanimura, N.; Hasegawa, J.; Yamashita, N.; Miyazaki, S.; Lam, P.K. Biochemical responses and accumulation properties of long-chain perfluorinated compounds (PFOS/PFDA/PFOA) in juvenile chickens (Gallus gallus). Arch. Environ. Contam. Toxicol. 2009, 57, 377–386. [Google Scholar] [CrossRef]
- Yoo, H.; Guruge, K.S.; Yamanaka, N.; Sato, C.; Mikami, O.; Miyazaki, S.; Yamashita, N.; Giesy, J.P. Depuration kinetics and tissue disposition of PFOA and PFOS in white leghorn chickens (Gallus gallus) administered by subcutaneous implantation. Ecotoxicol. Environ. Saf. 2009, 72, 26–36. [Google Scholar] [CrossRef]
- McKinney, J.; Rogers, R. ES&T metal bioavailability. Environ. Sci. Technol. 1992, 26, 1298–1299. [Google Scholar]
- Aylward, L.; Hays, S.; LaKind, J.; Ryan, J. Rapid communication: Partitioning of persistent lipophilic compounds, including dioxins, between human milk lipid and blood lipid: An initial assessment. J. Toxicol. Environ. Health Part A 2003, 66, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Snow, T.A.; Kemper, R.A.; Jepson, G.W. Binding of perfluorooctanoic acid to rat and human plasma proteins. Chem. Res. Toxicol. 2003, 16, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.A.; Ungell, A.-L.; Dolgos, H. Physiologically based pharmacokinetic (PBPK) modeling and simulation: Applications in lead optimization. Curr. Opin. Drug Discov. Dev. 2009, 12, 509–518. [Google Scholar]
- Conder, J.M.; Hoke, R.A.; Wolf, W.d.; Russell, M.H.; Buck, R.C. Are PFCAs bioaccumulative? A critical review and comparison with regulatory criteria and persistent lipophilic compounds. Environ. Sci. Technol. 2008, 42, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Frederiksen, H.; Skakkebaek, N.E.; Andersson, A.M. Metabolism of phthalates in humans. Mol. Nutr. Food Res. 2007, 51, 899–911. [Google Scholar] [CrossRef]
- Kapraun, D.F.; Wambaugh, J.F.; Setzer, R.W.; Judson, R.S. Empirical models for anatomical and physiological changes in a human mother and fetus during pregnancy and gestation. PLoS ONE 2019, 14, e0215906. [Google Scholar] [CrossRef]
- Needham, L.L.; Grandjean, P.; Heinzow, B.; Jørgensen, P.J.; Nielsen, F.; Patterson Jr, D.G.; Sjödin, A.; Turner, W.E.; Weihe, P. Partition of environmental chemicals between maternal and fetal blood and tissues. Environ. Sci. Technol. 2011, 45, 1121–1126. [Google Scholar] [CrossRef]
- Luebker, D.J.; York, R.G.; Hansen, K.J.; Moore, J.A.; Butenhoff, J.L. Neonatal mortality from in utero exposure to perfluorooctanesulfonate (PFOS) in Sprague–Dawley rats: Dose–response, and biochemical and pharamacokinetic parameters. Toxicology 2005, 215, 149–169. [Google Scholar] [CrossRef]
- Lau, C.; Thibodeaux, J.R.; Hanson, R.G.; Narotsky, M.G.; Rogers, J.M.; Lindstrom, A.B.; Strynar, M.J. Effects of perfluorooctanoic acid exposure during pregnancy in the mouse. Toxicol. Sci. 2006, 90, 510–518. [Google Scholar] [CrossRef]
- White, S.S.; Calafat, A.M.; Kuklenyik, Z.; Villanueva, L.; Zehr, R.D.; Helfant, L.; Strynar, M.J.; Lindstrom, A.B.; Thibodeaux, J.R.; Wood, C. Gestational PFOA exposure of mice is associated with altered mammary gland development in dams and female offspring. Toxicol. Sci. 2007, 96, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Johansson, N.; Fredriksson, A.; Eriksson, P. Neonatal exposure to perfluorooctane sulfonate (PFOS) and perfluorooctanoic acid (PFOA) causes neurobehavioural defects in adult mice. Neurotoxicology 2008, 29, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.A.; Hungerbühler, K. Bioconcentration of perfluorinated alkyl acids: How important is specific binding? Environ. Sci. Technol. 2013, 47, 7214–7223. [Google Scholar] [CrossRef]
- MacManus-Spencer, L.A.; Tse, M.L.; Hebert, P.C.; Bischel, H.N.; Luthy, R.G. Binding of perfluorocarboxylates to serum albumin: A comparison of analytical methods. Anal. Chem. 2010, 82, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Porpora, M.G.; Lucchini, R.; Abballe, A.; Ingelido, A.M.; Valentini, S.; Fuggetta, E.; Cardi, V.; Ticino, A.; Marra, V.; Fulgenzi, A.R. Placental transfer of persistent organic pollutants: A preliminary study on mother-newborn pairs. Int. J. Environ. Res. Public Health 2013, 10, 699–711. [Google Scholar] [CrossRef]
- Glynn, A.; Berger, U.; Bignert, A.; Ullah, S.; Aune, M.; Lignell, S.; Darnerud, P.O. Perfluorinated alkyl acids in blood serum from primiparous women in Sweden: Serial sampling during pregnancy and nursing, and temporal trends 1996–2010. Environ. Sci. Technol. 2012, 46, 9071–9079. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Beesoon, S.; Zhu, L.; Martin, J.W. Biomonitoring of perfluoroalkyl acids in human urine and estimates of biological half-life. Environ. Sci. Technol. 2013, 47, 10619–10627. [Google Scholar] [CrossRef] [PubMed]
- Gützkow, K.B.; Haug, L.S.; Thomsen, C.; Sabaredzovic, A.; Becher, G.; Brunborg, G. Placental transfer of perfluorinated compounds is selective–a Norwegian Mother and Child sub-cohort study. Int. J. Hyg. Environ. Health 2012, 215, 216–219. [Google Scholar] [CrossRef]
- Kim, S.; Choi, K.; Ji, K.; Seo, J.; Kho, Y.; Park, J.; Kim, S.; Park, S.; Hwang, I.; Jeon, J. Trans-placental transfer of thirteen perfluorinated compounds and relations with fetal thyroid hormones. Environ. Sci. Technol. 2011, 45, 7465–7472. [Google Scholar] [CrossRef]
- Mamsen, L.S.; Björvang, R.D.; Mucs, D.; Vinnars, M.-T.; Papadogiannakis, N.; Lindh, C.H.; Andersen, C.Y.; Damdimopoulou, P. Concentrations of perfluoroalkyl substances (PFASs) in human embryonic and fetal organs from first, second, and third trimester pregnancies. Environ. Int. 2019, 124, 482–492. [Google Scholar] [CrossRef]
- Chen, M.-H.; Ha, E.-H.; Liao, H.-F.; Jeng, S.-F.; Su, Y.-N.; Wen, T.-W.; Lien, G.-W.; Chen, C.-Y.; Hsieh, W.-S.; Chen, P.-C. Perfluorinated compound levels in cord blood and neurodevelopment at 2 years of age. Epidemiology 2013, 24, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Skogheim, T.S.; Weyde, K.V.F.; Aase, H.; Engel, S.M.; Surén, P.; Øie, M.G.; Biele, G.; Reichborn-Kjennerud, T.; Brantsæter, A.L.; Haug, L.S. Prenatal exposure to per-and polyfluoroalkyl substances (PFAS) and associations with attention-deficit/hyperactivity disorder and autism spectrum disorder in children. Environ. Res. 2021, 202, 111692. [Google Scholar] [CrossRef] [PubMed]
- Braun, J.M.; Kalkbrenner, A.E.; Just, A.C.; Yolton, K.; Calafat, A.M.; Sjödin, A.; Hauser, R.; Webster, G.M.; Chen, A.; Lanphear, B.P. Gestational exposure to endocrine-disrupting chemicals and reciprocal social, repetitive, and stereotypic behaviors in 4-and 5-year-old children: The HOME study. Environ. Health Perspect. 2014, 122, 513–520. [Google Scholar] [CrossRef]
- Long, M.; Ghisari, M.; Kjeldsen, L.; Wielsøe, M.; Nørgaard-Pedersen, B.; Mortensen, E.L.; Abdallah, M.W.; Bonefeld-Jørgensen, E.C. Autism spectrum disorders, endocrine disrupting compounds, and heavy metals in amniotic fluid: A case-control study. Mol. Autism 2019, 10, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Bennett, D.H.; Calafat, A.M.; Tancredi, D.; Roa, D.L.; Schmidt, R.J.; Hertz-Picciotto, I.; Shin, H.-M. Prenatal exposure to per-and polyfluoroalkyl substances in association with autism spectrum disorder in the MARBLES study. Environ. Int. 2021, 147, 106328. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.-M.; Bennett, D.H.; Calafat, A.M.; Tancredi, D.; Hertz-Picciotto, I. Modeled prenatal exposure to per-and polyfluoroalkyl substances in association with child autism spectrum disorder: A case-control study. Environ. Res. 2020, 186, 109514. [Google Scholar] [CrossRef] [PubMed]
- Ode, A.; Källén, K.; Gustafsson, P.; Rylander, L.; Jönsson, B.A.; Olofsson, P.; Ivarsson, S.A.; Lindh, C.H.; Rignell-Hydbom, A. Fetal exposure to perfluorinated compounds and attention deficit hyperactivity disorder in childhood. PLoS ONE 2014, 9, e95891. [Google Scholar] [CrossRef]
- Jensen, D.V.; Christensen, J.; Virtanen, H.E.; Skakkebæk, N.E.; Main, K.M.; Toppari, J.; Veje, C.W.; Andersson, A.-M.; Nielsen, F.; Grandjean, P. No association between exposure to perfluorinated compounds and congenital cryptorchidism: A nested case-control study among 215 boys from Denmark and Finland. Reproduction 2014, 147, 411–417. [Google Scholar] [CrossRef]
- Frazzoli, C.; Bocca, B.; Mantovani, A. The one health perspective in trace elements biomonitoring. J. Toxicol. Environ. Health Part B 2015, 18, 344–370. [Google Scholar] [CrossRef]
- Rock, K.D.; Polera, M.E.; Guillette, T.C.; Starnes, H.M.; Dean, K.; Watters, M.; Stevens-Stewart, D.; Belcher, S.M. Domestic Dogs and Horses as Sentinels of Per-and Polyfluoroalkyl Substance Exposure and Associated Health Biomarkers in Gray’s Creek North Carolina. Environ. Sci. Technol. 2023, 57, 9567–9579. [Google Scholar] [CrossRef]
- Zhao, Z.; Cheng, X.; Hua, X.; Jiang, B.; Tian, C.; Tang, J.; Li, Q.; Sun, H.; Lin, T.; Liao, Y. Emerging and legacy per-and polyfluoroalkyl substances in water, sediment, and air of the Bohai Sea and its surrounding rivers. Environ. Pollut. 2020, 263, 114391. [Google Scholar] [CrossRef] [PubMed]
- Lindstrom, A.B.; Strynar, M.J.; Delinsky, A.D.; Nakayama, S.F.; McMillan, L.; Libelo, E.L.; Neill, M.; Thomas, L. Application of WWTP biosolids and resulting perfluorinated compound contamination of surface and well water in Decatur, Alabama, USA. Environ. Sci. Technol. 2011, 45, 8015–8021. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Duan, J.; Tian, S.; Ji, H.; Zhu, Y.; Wei, Z.; Zhao, D. Short-chain per-and polyfluoroalkyl substances in aquatic systems: Occurrence, impacts and treatment. Chem. Eng. J. 2020, 380, 122506. [Google Scholar] [CrossRef]
- Schultes, L.; Sandblom, O.; Broeg, K.; Bignert, A.; Benskin, J.P. Temporal trends (1981–2013) of per-and polyfluoroalkyl substances and total fluorine in Baltic cod (Gadus morhua). Environ. Toxicol. Chem. 2020, 39, 300–309. [Google Scholar] [CrossRef]
- Hanssen, L.; Herzke, D.; Nikiforov, V.; Moe, B.; Nygård, T.; van Dijk, J.J.; Gabrielsen, G.W.; Fuglei, E.; Yeung, L.; Vogelsang, C. Screening new PFAS compounds 2018. In NILU Rapport; Norwegian Institute for Air Research NILU: Kjeller, Norway, 2019. [Google Scholar]
- Liu, C.; Gin, K.Y.; Chang, V.W.; Goh, B.P.; Reinhard, M. Novel perspectives on the bioaccumulation of PFCs–the concentration dependency. Environ. Sci. Technol. 2011, 45, 9758–9764. [Google Scholar] [CrossRef]
- Liu, C.; Chang, V.W.; Gin, K.Y. Oxidative toxicity of perfluorinated chemicals in green mussel and bioaccumulation factor dependent quantitative structure–activity relationship. Environ. Toxicol. Chem. 2014, 33, 2323–2332. [Google Scholar] [CrossRef]
- Chen, M.; Wang, Q.; Shan, G.; Zhu, L.; Yang, L.; Liu, M. Occurrence, partitioning and bioaccumulation of emerging and legacy per-and polyfluoroalkyl substances in Taihu Lake, China. Sci. Total Environ. 2018, 634, 251–259. [Google Scholar] [CrossRef]
- Bost, P.C.; Strynar, M.J.; Reiner, J.L.; Zweigenbaum, J.A.; Secoura, P.L.; Lindstrom, A.B.; Dye, J.A. US domestic cats as sentinels for perfluoroalkyl substances: Possible linkages with housing, obesity, and disease. Environ. Res. 2016, 151, 145–153. [Google Scholar] [CrossRef]
- Wang, F.; Zhao, C.; Gao, Y.; Fu, J.; Gao, K.; Lv, K.; Wang, K.; Yue, H.; Lan, X.; Liang, Y. Protein-specific distribution patterns of perfluoroalkyl acids in egg yolk and albumen samples around a fluorochemical facility. Sci. Total Environ. 2019, 650, 2697–2704. [Google Scholar] [CrossRef]
- Hitchcock, D.J.; Andersen, T.; Varpe, Ø.; Loonen, M.J.; Warner, N.A.; Herzke, D.; Tombre, I.M.; Griffin, L.R.; Shimmings, P.; Borgå, K. Potential effect of migration strategy on pollutant occurrence in eggs of Arctic breeding barnacle geese (Branta leucopsis). Environ. Sci. Technol. 2019, 53, 5427–5435. [Google Scholar] [CrossRef]
- Løseth, M.E.; Briels, N.; Eulaers, I.; Nygård, T.; Malarvannan, G.; Poma, G.; Covaci, A.; Herzke, D.; Bustnes, J.O.; Lepoint, G. Plasma concentrations of organohalogenated contaminants in white-tailed eagle nestlings–The role of age and diet. Environ. Pollut. 2019, 246, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Rotander, A.; Kärrman, A.; van Bavel, B.; Polder, A.; Rigét, F.; Auðunsson, G.A.; Víkingsson, G.; Gabrielsen, G.W.; Bloch, D.; Dam, M. Increasing levels of long-chain perfluorocarboxylic acids (PFCAs) in Arctic and North Atlantic marine mammals, 1984–2009. Chemosphere 2012, 86, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Zhong, W.; Zhang, L.; Cui, Y.; Chen, M.; Zhu, L. Probing mechanisms for bioaccumulation of perfluoroalkyl acids in carp (Cyprinus carpio): Impacts of protein binding affinities and elimination pathways. Sci. Total Environ. 2019, 647, 992–999. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.C.; Andrews, D.Q.; Lindstrom, A.B.; Bruton, T.A.; Schaider, L.A.; Grandjean, P.; Lohmann, R.; Carignan, C.C.; Blum, A.; Balan, S.A. Detection of poly-and perfluoroalkyl substances (PFASs) in US drinking water linked to industrial sites, military fire training areas, and wastewater treatment plants. Environ. Sci. Technol. Lett. 2016, 3, 344–350. [Google Scholar] [CrossRef]
- Sun, Q.; Zong, G.; Valvi, D.; Nielsen, F.; Coull, B.; Grandjean, P. Plasma concentrations of perfluoroalkyl substances and risk of type 2 diabetes: A prospective investigation among US women. Environ. Health Perspect. 2018, 126, 037001. [Google Scholar] [CrossRef]
- Park, S.K.; Peng, Q.; Ding, N.; Mukherjee, B.; Harlow, S.D. Determinants of per-and polyfluoroalkyl substances (PFAS) in midlife women: Evidence of racial/ethnic and geographic differences in PFAS exposure. Environ. Res. 2019, 175, 186–199. [Google Scholar] [CrossRef] [PubMed]
- De Voogt, P.; Berger, U.; De Coen, W.; De Wolf, W.; Heimstad, E.; MCLachlan, M.; Van Leeuwen, S.; Van Roon, A. Perfluorinated Organic Compounds in the European Environment; Institute for Biodiversity and Ecosystem Dynamics, Universiteit van Amsterdam: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Tromba, C. PFASs pollution in Veneto Region (Northern Italy). After USA, it is the turn of Italy. Epidemiol. Prev. 2017, 41, 232–236. [Google Scholar]
- Patrocinio, R.d.V.; WHO. Keeping Our Water Clean: The Case of Water Contamination in the Veneto Region, Italy; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Mastrantonio, M.; Bai, E.; Uccelli, R.; Cordiano, V.; Screpanti, A.; Crosignani, P. Drinking water contamination from perfluoroalkyl substances (PFAS): An ecological mortality study in the Veneto Region, Italy. Eur. J. Public Health 2018, 28, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, K.T.; Raaschou-Nielsen, O.; McLaughlin, J.K.; Lipworth, L.; Tjønneland, A.; Overvad, K.; Sørensen, M. Association between plasma PFOA and PFOS levels and total cholesterol in a middle-aged Danish population. PLoS ONE 2013, 8, e56969. [Google Scholar] [CrossRef]
- Geiger, S.D.; Xiao, J.; Ducatman, A.; Frisbee, S.; Innes, K.; Shankar, A. The association between PFOA, PFOS and serum lipid levels in adolescents. Chemosphere 2014, 98, 78–83. [Google Scholar] [CrossRef]
- Fletcher, T.; Galloway, T.S.; Melzer, D.; Holcroft, P.; Cipelli, R.; Pilling, L.C.; Mondal, D.; Luster, M.; Harries, L.W. Associations between PFOA, PFOS and changes in the expression of genes involved in cholesterol metabolism in humans. Environ. Int. 2013, 57, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.C.; Johns, L.E.; Meeker, J.D. Serum biomarkers of exposure to perfluoroalkyl substances in relation to serum testosterone and measures of thyroid function among adults and adolescents from NHANES 2011–2012. Int. J. Environ. Res. Public Health 2015, 12, 6098–6114. [Google Scholar] [CrossRef]
- Li, Y.; Xu, Y.; Fletcher, T.; Scott, K.; Nielsen, C.; Pineda, D.; Lindh, C.H.; Olsson, D.S.; Andersson, E.M.; Jakobsson, K. Associations between perfluoroalkyl substances and thyroid hormones after high exposure through drinking water. Environ. Res. 2021, 194, 110647. [Google Scholar] [CrossRef]
- Wang, H.; Du, H.; Yang, J.; Jiang, H.; Karmin, O.; Xu, L.; Liu, S.; Yi, J.; Qian, X.; Chen, Y. PFOS, PFOA, estrogen homeostasis, and birth size in Chinese infants. Chemosphere 2019, 221, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Espinosa, M.-J.; Fletcher, T.; Armstrong, B.; Genser, B.; Dhatariya, K.; Mondal, D.; Ducatman, A.; Leonardi, G. Association of perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS) with age of puberty among children living near a chemical plant. Environ. Sci. Technol. 2011, 45, 8160–8166. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Exposure to Highly Hazardous Pesticides: A Major Public Health Concern; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Cantrell, C.L.; Dayan, F.E.; Duke, S.O. Natural products as sources for new pesticides. J. Nat. Prod. 2012, 75, 1231–1242. [Google Scholar] [CrossRef] [PubMed]
- Kumar, J.; Ramlal, A.; Mallick, D.; Mishra, V. An overview of some biopesticides and their importance in plant protection for commercial acceptance. Plants 2021, 10, 1185. [Google Scholar] [CrossRef]
- Essiedu, J.A.; Adepoju, F.O.; Ivantsova, M.N. Benefits and limitations in using biopesticides: A review. Proc. AIP Conf. Proc. 2020, 2313, 080002. [Google Scholar]
- Chang, J.H.; Choi, J.Y.; Jin, B.R.; Roh, J.Y.; Olszewski, J.A.; Seo, S.J.; O’Reilly, D.R.; Je, Y.H. An improved baculovirus insecticide producing occlusion bodies that contain Bacillus thuringiensis insect toxin. J. Invertebr. Pathol. 2003, 84, 30–37. [Google Scholar] [CrossRef]
- Castagna, F.; Piras, C.; Palma, E.; Musolino, V.; Lupia, C.; Bosco, A.; Rinaldi, L.; Cringoli, G.; Musella, V.; Britti, D. Green veterinary pharmacology applied to parasite control: Evaluation of Punica granatum, Artemisia campestris, Salix caprea aqueous macerates against gastrointestinal nematodes of sheep. Vet. Sci. 2021, 8, 237. [Google Scholar] [CrossRef]
- Castagna, F.; Bava, R.; Piras, C.; Carresi, C.; Musolino, V.; Lupia, C.; Marrelli, M.; Conforti, F.; Palma, E.; Britti, D. Green veterinary pharmacology for honey bee welfare and health: Origanum heracleoticum L. (Lamiaceae) essential oil for the control of the Apis mellifera varroatosis. Vet. Sci. 2022, 9, 124. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, R.; Fusco, R.; Peritore, A.F.; Cordaro, M.; D’Amico, R.; Genovese, T.; Gugliandolo, E.; Crupi, R.; Smeriglio, A.; Mandalari, G. The antioxidant and anti-inflammatory properties of Anacardium occidentale L. cashew nuts in a mouse model of colitis. Nutrients 2020, 12, 834. [Google Scholar] [CrossRef] [PubMed]
- Cordaro, M.; Fusco, R.; D’Amico, R.; Siracusa, R.; Peritore, A.F.; Gugliandolo, E.; Genovese, T.; Crupi, R.; Mandalari, G.; Cuzzocrea, S. Cashew (Anacardium occidentale L.) nuts modulate the Nrf2 and NLRP3 pathways in pancreas and lung after induction of acute pancreatitis by cerulein. Antioxidants 2020, 9, 992. [Google Scholar] [CrossRef]
- D’Amico, R.; Cordaro, M.; Fusco, R.; Peritore, A.F.; Genovese, T.; Gugliandolo, E.; Crupi, R.; Mandalari, G.; Caccamo, D.; Cuzzocrea, S. Consumption of Cashew (Anacardium occidentale L.) Nuts Counteracts Oxidative Stress and Tissue Inflammation in Mild Hyperhomocysteinemia in Rats. Nutrients 2022, 14, 1474. [Google Scholar] [CrossRef]
- Gugliandolo, E.; Fusco, R.; Licata, P.; Peritore, A.F.; D’amico, R.; Cordaro, M.; Siracusa, R.; Cuzzocrea, S.; Crupi, R. Protective Effect of hydroxytyrosol on LPS-induced inflammation and oxidative stress in bovine endometrial epithelial cell line. Vet. Sci. 2020, 7, 161. [Google Scholar] [CrossRef] [PubMed]
- Fusco, R.; Cordaro, M.; Siracusa, R.; Peritore, A.F.; D’Amico, R.; Licata, P.; Crupi, R.; Gugliandolo, E. Effects of hydroxytyrosol against lipopolysaccharide-induced inflammation and oxidative stress in bovine mammary epithelial cells: A natural therapeutic tool for bovine mastitis. Antioxidants 2020, 9, 693. [Google Scholar] [CrossRef]

| PFAS Group | PFAS Acronym | PFAS Name |
|---|---|---|
| Short-chain perfluoroalkyl carboxylic acids (PFCAs) (With less than seven carbons) | PFHpA | Perfluoro-n-heptanoic acid |
| PFHxA | Undecafluorohexanoic acid | |
| PFPeA | Perfluorovaleric acid | |
| PFBA | Perfluorobutanoic acid | |
| Short-chain perfluoroalkyl sulfonic acids (PFSAs) (With less than five carbons) | PFBS | Perfluorobutanesulfonic acid |
| PFPeS | Perfluoropentanesulfonic acid | |
| Long-chain perfluoroalkyl carboxylic acids (PFCAs) (With more than seven carbons) | PFOA | Perfluorooctanoic acid |
| PFNA | Perfluorononan-1-oic acid | |
| PFDA | Nonadecafluorodecanoic acid | |
| PFUnDA | Henicosafluoroundecanoic acid | |
| PFDoDA | Tricosafluorododecanoic acid | |
| Long-chain perfluoroalkyl sulfonic acids (PFSAs) (With more than five carbons) | PFOS | Perfluorooctane sulfonate |
| PFNS | Perfluorononanesulfonic acid | |
| PFDS | Perfluorodecanesulfonic acid |
| Animals | PFAS Acronym | PFAS Concentrations | Location | Studies |
|---|---|---|---|---|
| Cats | PFNA, PFUnDA, PFHxS | 18.0–165 ng/g dw | North Carolina USA | [60,114] |
| Dogs | PFOA, PFNA, PFOS, PFHxS | 21.6–474 ng/g dw | North Carolina USA | [60,105,114] |
| Horses | PFOA, PFOS, | 0.10 ng/mL 1.8 ng/mL | North Carolina USA | [105] |
| Chickens | PFOA, PFOS, PFHxS | 4.75, ng/g ww 25.7 ng/g ww 4.29 ng/g ww | China | [115] |
| Barnacle geese | PFOS | 1.21 ± 2.97 ng/g | Norway, UK | [116] |
| White-tailed eagle nestlings | PFOS | 4.58 e 52.94 ng/mL | Norway, UK | [117] |
| Polar bear | PFOS, PFNA, PFUnDA | 205 ng/mL 37.6 ng/mL 25.5 ng/mL | Greenland, Norwegian Arctic | [10] |
| Cattle | PFOS, | 3.0 ng/ml | Sweden, Japan | [65,66] |
| Sheep | PFOS | 103 and 240 μg/L (Pilot study after exposure to 1.16–1.45 μg/kg bw/d) | Germany, Netherlands | [67] |
| Whales | PFNA, PFDA PFUnD | 50 ng g−1 ww | Faroe Islands | [118] |
| Carps | PFOS, PFHxS | 1.43 nmol/gw 5.20 nmol/gw | China | [119] |
| Aquatic organisms | PFHxS, PFOA | 0.141–74.9 ng/g ww | China | [113] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peritore, A.F.; Gugliandolo, E.; Cuzzocrea, S.; Crupi, R.; Britti, D. Current Review of Increasing Animal Health Threat of Per- and Polyfluoroalkyl Substances (PFAS): Harms, Limitations, and Alternatives to Manage Their Toxicity. Int. J. Mol. Sci. 2023, 24, 11707. https://doi.org/10.3390/ijms241411707
Peritore AF, Gugliandolo E, Cuzzocrea S, Crupi R, Britti D. Current Review of Increasing Animal Health Threat of Per- and Polyfluoroalkyl Substances (PFAS): Harms, Limitations, and Alternatives to Manage Their Toxicity. International Journal of Molecular Sciences. 2023; 24(14):11707. https://doi.org/10.3390/ijms241411707
Chicago/Turabian StylePeritore, Alessio Filippo, Enrico Gugliandolo, Salvatore Cuzzocrea, Rosalia Crupi, and Domenico Britti. 2023. "Current Review of Increasing Animal Health Threat of Per- and Polyfluoroalkyl Substances (PFAS): Harms, Limitations, and Alternatives to Manage Their Toxicity" International Journal of Molecular Sciences 24, no. 14: 11707. https://doi.org/10.3390/ijms241411707
APA StylePeritore, A. F., Gugliandolo, E., Cuzzocrea, S., Crupi, R., & Britti, D. (2023). Current Review of Increasing Animal Health Threat of Per- and Polyfluoroalkyl Substances (PFAS): Harms, Limitations, and Alternatives to Manage Their Toxicity. International Journal of Molecular Sciences, 24(14), 11707. https://doi.org/10.3390/ijms241411707









