Laboratory Findings and Biomarkers in Long COVID: What Do We Know So Far? Insights into Epidemiology, Pathogenesis, Therapeutic Perspectives and Challenges
Abstract
1. Introduction
2. Epidemiology of Long COVID and Risk Factors
3. Clinical Manifestations of Long COVID
4. Are Clinical Manifestations and Pathogenesis Unique to SARS-CoV-2 Infection?
5. Pathogenesis of Long COVID
6. Laboratory Findings and Biomarkers in Long COVID
6.1. Biomarkers of Systemic Inflammation
6.2. Immune Profiling in Long COVID
6.3. Biomarkers Reflecting SARS-CoV-2 Persistence
6.4. Humoral and Cellular Response against SARS-CoV-2 in Long COVID
6.5. Biomarkers Reflecting Reactivation of Latent Viruses
6.6. Biomarkers Reflecting Autoimmunity
6.7. Endothelial or Vascular Biomarkers
6.8. Biomarkers of Coagulation and Fibrinolysis
6.9. Hormonal and Metabolic Biomarkers
6.10. Various Proteins as Biomarkers
6.11. Metabolites as Biomarkers
6.12. Microbiota Alterations in Long COVID
6.13. Cerebrospinal Fluid Biomarkers
7. Biomarkers Classifying Clinical Manifestations in Long COVID
7.1. Candidate Biomarkers for General Symptoms and Fatigue
7.2. Candidate Biomarkers for Neurological Symptoms
7.3. Candidate Biomarkers for Respiratory Symptoms
7.4. Candidate Biomarkers for Gastrointestinal and Other Specific Symptoms
8. Limitations of Studies and Challenges
9. Therapeutic Perspectives and Challenges
10. Concluding Remarks-Quo Vadis?
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 7 June 2023).
- Lee, W.E.; Woo Park, S.; Weinberger, D.M.; Olson, D.; Simonsen, L.; Grenfell, B.T.; Viboud, C. Direct and indirect mortality impacts of the COVID-19 pandemic in the United States, 1 March 2020 to 1 January 2022. Elife 2023, 12, e77562. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Tsilingiris, D.; Vallianou, N.G.; Karampela, I.; Liu, J.; Dalamaga, M. Potential implications of lipid nanoparticles in the pathogenesis of myocarditis associated with the use of mRNA vaccines against SARS-CoV-2. Metab. Open 2022, 13, 100159. [Google Scholar] [CrossRef] [PubMed]
- Marzianο, V.; Guzzetta, G.; Menegale, F.; Sacco, C.; Petrone, D.; Urdiales, A.; del Manso, M.; Bella, A.; Fabiani, M.; Vescio, M.; et al. The decline of COVID-19 severity and lethality over two years of pandemic. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Sigal, A. Milder disease with Omicron: Is it the virus or the pre-existing immunity? Nat. Rev. Immunol. 2022, 22, 69–71. [Google Scholar] [CrossRef]
- Mahase, E. COVID-19: What do we know about XBB.1.5 and should we be worried? BMJ 2023, 380, 153. [Google Scholar] [CrossRef]
- WHO. XBB.1.5 Updated Risk Assessment, 24 February 2023. Available online: https://www.who.int/docs/default-source/coronaviruse/22022024xbb.1.5ra.pdf (accessed on 15 May 2023).
- Siddiqui, S.; Alhamdi, H.W.S.; Alghamdi, H.A. Recent Chronology of COVID-19 Pandemic. Front. Public Health 2022, 10, 778037. [Google Scholar] [CrossRef]
- Líška, D.; Liptaková, E.; Babičová, A.; Batalik, L.; Baňárová, P.S.; Dobrodenková, S. What is the quality of life in patients with long COVID compared to a healthy control group? Front. Public Health 2022, 10, 975992. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef]
- WHO: Post COVID-19 Condition (Long COVID). Available online: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition#:~:text=It%20is%20defined%20as%20the,months%20with%20no%20other%20explanation (accessed on 6 June 2023).
- NICE: COVID-19 Rapid Guideline: Managing the Longterm Effects of COVID-19. Available online: https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742#:~:text=In%20addition%20to%20the%20clinical,)%20and%20post%E2%80%91COVID%E2%80%9119 (accessed on 6 June 2023).
- CDC: Long COVID or Post-COVID Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html#:~:text=Long%20COVID%20is%20broadly%20defined,with%20CDC%20and%20other%20partners (accessed on 6 June 2023).
- Robert Koch Institute: RKI Information Portal on Long COVID. Available online: https://www.rki.de/EN/Content/infections/epidemiology/outbreaks/COVID-19/Long-COVID/content-total.html (accessed on 6 June 2023).
- Government of Canada: Post COVID-19 Condition (Long COVID). Available online: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/symptoms/post-covid-19-condition.html (accessed on 6 June 2023).
- Jennings, G.; Monaghan, A.; Xue, F.; Mockler, D.; Romero-Ortuño, R. A Systematic Review of Persistent Symptoms and Residual Abnormal Functioning following Acute COVID-19: Ongoing Symptomatic Phase vs. Post-COVID-19 Syndrome. J. Clin. Med. 2021, 10, 5913. [Google Scholar] [CrossRef]
- WHO: Expanding Our Understanding of Post COVID-19 Condition. Report of a WHO Webinar, 9 February 2021. Available online: https://www.who.int/publications/i/item/9789240025035 (accessed on 6 June 2023).
- Roe, K. The Symptoms and Clinical Manifestations Observed in COVID-19 Patients/Long COVID-19 Symptoms that Parallel Toxoplasma gondii Infections. J. Neuroimmune Pharmacol. 2021, 16, 513–516. [Google Scholar] [CrossRef]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef]
- Castanares-Zapatero, D.; Chalon, P.; Kohn, L.; Dauvrin, M.; Detollenaere, J.; Maertens de Noordhout, C.; Primus-de Jong, C.; Cleemput, I.; Van den Heede, K. Pathophysiology and mechanism of long COVID: A comprehensive review. Ann. Med. 2022, 54, 1473–1487. [Google Scholar] [CrossRef]
- Dalamaga, M.; Karmaniolas, K.; Matekovits, A.; Migdalis, I.; Papadavid, E. Cutaneous manifestations in relation to immunologic parameters in a cohort of primary myelodysplastic syndrome patients. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 543–548. [Google Scholar] [CrossRef]
- Mentis, A.A.; Dalamaga, M.; Lu, C.; Polissiou, M.G. Saffron for “toning down” COVID-19-related cytokine storm: Hype or hope? A mini-review of current evidence. Metab. Open 2021, 11, 100111. [Google Scholar] [CrossRef]
- Varghese, J.; Sandmann, S.; Ochs, K.; Schrempf, I.M.; Frömmel, C.; Dugas, M.; Schmidt, H.H.; Vollenberg, R.; Tepasse, P.R. Persistent symptoms and lab abnormalities in patients who recovered from COVID-19. Sci. Rep. 2021, 11, 12775. [Google Scholar] [CrossRef]
- Espín, E.; Yang, C.; Shannon, C.P.; Assadian, S.; He, D.; Tebbutt, S.J. Cellular and molecular biomarkers of long COVID: A scoping review. EBioMedicine 2023, 91, 104552. [Google Scholar] [CrossRef]
- Lai, Y.J.; Liu, S.H.; Manachevakul, S.; Lee, T.A.; Kuo, C.T.; Bello, D. Biomarkers in long COVID-19: A systematic review. Front. Med. 2023, 10, 1085988. [Google Scholar] [CrossRef]
- Nasserie, T.; Hittle, M.; Goodman, S.N. Assessment of the Frequency and Variety of Persistent Symptoms among Patients with COVID-19: A Systematic Review. JAMA Netw. Open 2021, 4, e2111417. [Google Scholar] [CrossRef]
- Mizrahi, B.; Sudry, T.; Flaks-Manov, N.; Yehezkelli, Y.; Kalkstein, N.; Akiva, P.; Ekka-Zohar, A.; Ben David, S.S.; Lerner, U.; Bivas-Benita, M.; et al. Long COVID outcomes at one year after mild SARS-CoV-2 infection: Nationwide cohort study. BMJ 2023, 380, e072529. [Google Scholar] [CrossRef]
- UK Office for National Statistics. Prevalence of Ongoing Symptoms Following Coronavirus (COVID-19) Infection in the UK. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/alldatarelatingtoprevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk (accessed on 17 May 2023).
- Ahmad, F.B.; Anderson, R.N.; Cisewski, J.A.; Sutton, P.D. Identification of Deaths with Post-Acute Sequelae of COVID-19 from death Certificate Literal Text: United States, 1 January 2020–30 June 2022; CDC: Atlanta, GA, USA, 2022. [Google Scholar] [CrossRef]
- Du, M.; Ma, Y.; Deng, J.; Liu, M.; Liu, J. Comparison of Long COVID-19 Caused by Different SARS-CoV-2 Strains: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 16010. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, M.; Pujol, J.C.; Spector, T.D.; Ourselin, S.; Steves, C.J. Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2. Lancet 2022, 399, 2263–2264. [Google Scholar] [CrossRef]
- Nehme, M.; Vetter, P.; Chappuis, F.; Kaiser, L.; Guessous, I. Prevalence of Post-Coronavirus Disease Condition 12 Weeks after Omicron Infection Compared with Negative Controls and Association with Vaccination Status. Clin. Infect. Dis. 2023, 76, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Ballouz, T.; Menges, D.; Kaufmann, M.; Amati, R.; Frei, A.; von Wyl, V.; Fehr, J.S.; Albanese, E.; Puhan, M.A. Post COVID-19 condition after Wildtype, Delta, and Omicron SARS-CoV-2 infection and prior vaccination: Pooled analysis of two population-based cohorts. PLoS ONE 2023, 18, e0281429. [Google Scholar] [CrossRef] [PubMed]
- Levy, N.; Koppel, J.H.; Kaplan, O.; Yechiam, H.; Shahar-Nissan, K.; Cohen, N.K.; Shavit, I. Severity and Incidence of Multisystem Inflammatory Syndrome in Children during 3 SARS-CoV-2 Pandemic Waves in Israel. JAMA 2022, 327, 2452–2454. [Google Scholar] [CrossRef]
- Amanatidou, E.; Gkiouliava, A.; Pella, E.; Serafidi, M.; Tsilingiris, D.; Vallianou, N.G.; Karampela, I.; Dalamaga, M. Breakthrough infections after COVID-19 vaccination: Insights, perspectives and challenges. Metab. Open 2022, 14, 100180. [Google Scholar] [CrossRef]
- Dalamaga, M.; Nasiri-Ansari, N.; Spyrou, N. Perspectives and Challenges of COVID-19 with Obesity-Related Cancers. Cancers 2023, 15, 1771. [Google Scholar] [CrossRef]
- Tsilingiris, D.; Nasiri-Ansari, N.; Spyrou, N.; Magkos, F.; Dalamaga, M. Management of Hematologic Malignancies in the Era of COVID-19 Pandemic: Pathogenetic Mechanisms, Impact of Obesity, Perspectives, and Challenges. Cancers 2022, 14, 2494. [Google Scholar] [CrossRef]
- Syriga, M.; Karampela, I.; Dalamaga, M.; Karampelas, M. The effect of COVID-19 pandemic on the attendance and clinical outcomes of patients with ophthalmic disease: A mini-review. Metab. Open 2021, 12, 100131. [Google Scholar] [CrossRef]
- Kikkenborg Berg, S.; Palm, P.; Nygaard, U.; Bundgaard, H.; Petersen, M.N.S.; Rosenkilde, S.; Thorsted, A.B.; Ersbøll, A.K.; Thygesen, L.C.; Nielsen, S.D.; et al. Long COVID symptoms in SARS-CoV-2-positive children aged 0-14 years and matched controls in Denmark (LongCOVIDKidsDK): A national, cross-sectional study. Lancet. Child Adolesc. Health 2022, 6, 614–623. [Google Scholar] [CrossRef]
- Sørensen, A.I.V.; Spiliopoulos, L.; Bager, P.; Nielsen, N.M.; Hansen, J.V.; Koch, A.; Meder, I.K.; Ethelberg, S.; Hviid, A. A nationwide questionnaire study of post-acute symptoms and health problems after SARS-CoV-2 infection in Denmark. Nat. Commun. 2022, 13, 4213. [Google Scholar] [CrossRef]
- Roessler, M.; Tesch, F.; Batram, M.; Jacob, J.; Loser, F.; Weidinger, O.; Wende, D.; Vivirito, A.; Toepfner, N.; Ehm, F.; et al. Post-COVID-19-associated morbidity in children, adolescents, and adults: A matched cohort study including more than 157,000 individuals with COVID-19 in Germany. PLoS Med. 2022, 19, e1004122. [Google Scholar] [CrossRef]
- Edlow, A.G.; Castro, V.M.; Shook, L.L.; Kaimal, A.J.; Perlis, R.H. Neurodevelopmental Outcomes at 1 Year in Infants of Mothers Who Tested Positive for SARS-CoV-2 during Pregnancy. JAMA Netw. Open 2022, 5, e2215787. [Google Scholar] [CrossRef]
- Vella, L.A.; Rowley, A.H. Current Insights Into the Pathophysiology of Multisystem Inflammatory Syndrome in Children. Curr. Pediatr. Rep. 2021, 9, 83–92. [Google Scholar] [CrossRef]
- Melgar, M.; Lee, E.H.; Miller, A.D.; Lim, S.; Brown, C.M.; Yousaf, A.R.; Zambrano, L.D.; Belay, E.D.; Godfred-Cato, S.; Abrams, J.Y.; et al. Council of State and Territorial Epidemiologists/CDC Surveillance Case Definition for Multisystem Inflammatory Syndrome in Children Associated with SARS-CoV-2 Infection—United States. MMWR. Recomm. Rep. 2022, 71, 1–14. [Google Scholar] [CrossRef]
- Tsampasian, V.; Elghazaly, H.; Chattopadhyay, R.; Debski, M.; Naing, T.K.P.; Garg, P.; Clark, A.; Ntatsaki, E.; Vassiliou, V.S. Risk Factors Associated with Post-COVID-19 Condition: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2023, 183, 566–580. [Google Scholar] [CrossRef]
- Asadi-Pooya, A.A.; Akbari, A.; Emami, A.; Lotfi, M.; Rostamihosseinkhani, M.; Nemati, H.; Barzegar, Z.; Kabiri, M.; Zeraatpisheh, Z.; Farjoud-Kouhanjani, M.; et al. Risk Factors Associated with Long COVID Syndrome: A Retrospective Study. Iran. J. Med. Sci. 2021, 46, 428–436. [Google Scholar] [CrossRef]
- Subramanian, A.; Nirantharakumar, K.; Hughes, S.; Myles, P.; Williams, T.; Gokhale, K.M.; Taverner, T.; Chandan, J.S.; Brown, K.; Simms-Williams, N.; et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med. 2022, 28, 1706–1714. [Google Scholar] [CrossRef]
- Rao, S.; Lee, G.M.; Razzaghi, H.; Lorman, V.; Mejias, A.; Pajor, N.M.; Thacker, D.; Webb, R.; Dickinson, K.; Bailey, L.C.; et al. Clinical Features and Burden of Postacute Sequelae of SARS-CoV-2 Infection in Children and Adolescents. JAMA Pediatr. 2022, 176, 1000–1009. [Google Scholar] [CrossRef]
- Morello, R.; Mariani, F.; Mastrantoni, L.; De Rose, C.; Zampino, G.; Munblit, D.; Sigfrid, L.; Valentini, P.; Buonsenso, D. Risk factors for post-COVID-19 condition (Long COVID) in children: A prospective cohort study. EClinicalMedicine 2023, 59, 101961. [Google Scholar] [CrossRef]
- Yu, Z.; Ekström, S.; Bellander, T.; Ljungman, P.; Pershagen, G.; Eneroth, K.; Kull, I.; Bergström, A.; Georgelis, A.; Stafoggia, M.; et al. Ambient air pollution exposure linked to long COVID among young adults: A nested survey in a population-based cohort in Sweden. Lancet Reg. Health. Eur. 2023, 28, 100608. [Google Scholar] [CrossRef] [PubMed]
- Merzon, E.; Weiss, M.; Krone, B.; Cohen, S.; Ilani, G.; Vinker, S.; Cohen-Golan, A.; Green, I.; Israel, A.; Schneider, T.; et al. Clinical and Socio-Demographic Variables Associated with the Diagnosis of Long COVID Syndrome in Youth: A Population-Based Study. Int. J. Environ. Res. Public Health 2022, 19, 5993. [Google Scholar] [CrossRef] [PubMed]
- Ayoubkhani, D.; Bosworth, M.L.; King, S.; Pouwels, K.B.; Glickman, M.; Nafilyan, V.; Zaccardi, F.; Khunti, K.; Alwan, N.A.; Walker, A.S. Risk of Long COVID in People Infected with Severe Acute Respiratory Syndrome Coronavirus 2 After 2 Doses of a Coronavirus Disease 2019 Vaccine: Community-Based, Matched Cohort Study. Open Forum Infect. Dis. 2022, 9, ofac464. [Google Scholar] [CrossRef] [PubMed]
- Al-Aly, Z.; Bowe, B.; Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. 2022, 28, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
- Antar, A.A.R.; Yu, T.; Demko, Z.O.; Hu, C.; Tornheim, J.A.; Blair, P.W.; Thomas, D.L.; Manabe, Y.C. Long COVID brain fog and muscle pain are associated with longer time to clearance of SARS-CoV-2 RNA from the upper respiratory tract during acute infection. medRxiv 2023. [Google Scholar] [CrossRef]
- Tsuchida, T.; Hirose, M.; Inoue, Y.; Kunishima, H.; Otsubo, T.; Matsuda, T. Relationship between changes in symptoms and antibody titers after a single vaccination in patients with Long COVID. J. Med. Virol. 2022, 94, 3416–3420. [Google Scholar] [CrossRef]
- Nguyen, N.N.; Nguyen, Y.N.; Hoang, V.T.; Million, M.; Gautret, P. SARS-CoV-2 Reinfection and Severity of the Disease: A Systematic Review and Meta-Analysis. Viruses 2023, 15, 967. [Google Scholar] [CrossRef]
- Bowe, B.; Xie, Y.; Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. 2022, 28, 2398–2405. [Google Scholar] [CrossRef]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Izquierdo-Pujol, J.; Moron-Lopez, S.; Dalmau, J.; Gonzalez-Aumatell, A.; Carreras-Abad, C.; Mendez, M.; Rodrigo, C.; Martinez-Picado, J. Post COVID-19 Condition in Children and Adolescents: An Emerging Problem. Front. Pediatr. 2022, 10, 894204. [Google Scholar] [CrossRef]
- Gonzalez-Aumatell, A.; Bovo, M.V.; Carreras-Abad, C.; Cuso-Perez, S.; Domènech Marsal, È.; Coll-Fernández, R.; Goicoechea Calvo, A.; Giralt-López, M.; Enseñat Cantallops, A.; Moron-Lopez, S.; et al. Social, Academic, and Health Status Impact of Long COVID on Children and Young People: An Observational, Descriptive, and Longitudinal Cohort Study. Children 2022, 9, 1677. [Google Scholar] [CrossRef]
- Fonseca, A.; Lima, R.; Ladeira, I.; Guimarães, M. Evaluation of pulmonary function in post-COVID-19 patients—When and how should we do it? J. Bras. De Pneumol. 2021, 47, e20210065. [Google Scholar] [CrossRef]
- Fortini, A.; Rosso, A.; Cecchini, P.; Torrigiani, A.; Lo Forte, A.; Carrai, P.; Alessi, C.; Fabbrizzi, F.; Lovicu, E.; Sbaragli, S.; et al. One-year evolution of DLCO changes and respiratory symptoms in patients with post COVID-19 respiratory syndrome. Infection 2022, 50, 513–517. [Google Scholar] [CrossRef]
- Kanne, J.P.; Little, B.P.; Schulte, J.J.; Haramati, A.; Haramati, L.B. Long-term Lung Abnormalities Associated with COVID-19 Pneumonia. Radiology 2023, 306, e221806. [Google Scholar] [CrossRef]
- Michelen, M.; Manoharan, L.; Elkheir, N.; Cheng, V.; Dagens, A.; Hastie, C.; O’Hara, M.; Suett, J.; Dahmash, D.; Bugaeva, P.; et al. Characterising long COVID: A living systematic review. BMJ Glob. Health 2021, 6, e005427. [Google Scholar] [CrossRef]
- Canas, L.S.; Molteni, E.; Deng, J.; Sudre, C.H.; Murray, B.; Kerfoot, E.; Antonelli, M.; Chen, L.; Rjoob, K.; Pujol, J.C.; et al. Profiling post-COVID syndrome across different variants of SARS-CoV-2. medRxiv 2022. [Google Scholar] [CrossRef]
- Dennis, A.; Cuthbertson, D.J.; Wootton, D.; Crooks, M.; Gabbay, M.; Eichert, N.; Mouchti, S.; Pansini, M.; Roca-Fernandez, A.; Thomaides-Brears, H.; et al. Multi-organ impairment and long COVID: A 1-year prospective, longitudinal cohort study. J. R. Soc. Med. 2023, 116, 97–112. [Google Scholar] [CrossRef]
- Fedorowski, A.; Sutton, R. Autonomic dysfunction and postural orthostatic tachycardia syndrome in post-acute COVID-19 syndrome. Nat. Rev. Cardiol. 2023, 20, 281–282. [Google Scholar] [CrossRef]
- Espinosa-Gonzalez, A.B.; Master, H.; Gall, N.; Halpin, S.; Rogers, N.; Greenhalgh, T. Orthostatic tachycardia after COVID-19. BMJ 2023, 380, e073488. [Google Scholar] [CrossRef]
- Agashe, S.; Petak, S. Cardiac Autonomic Neuropathy in Diabetes Mellitus. Methodist DeBakey Cardiovasc. J. 2018, 14, 251–256. [Google Scholar] [CrossRef]
- Guo, B.; Zhao, C.; He, M.Z.; Senter, C.; Zhou, Z.; Peng, J.; Li, S.; Fitzpatrick, A.L.; Lindström, S.; Stebbins, R.C.; et al. Long-term cardiac symptoms following COVID-19: A systematic review and meta-analysis. medRxiv 2023. [Google Scholar] [CrossRef]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Harding, J.L.; Oviedo, S.A.; Ali, M.K.; Ofotokun, I.; Gander, J.C.; Patel, S.A.; Magliano, D.J.; Patzer, R.E. The bidirectional association between diabetes and long-COVID-19—A systematic review. Diabetes Res. Clin. Pract. 2023, 195, 110202. [Google Scholar] [CrossRef] [PubMed]
- Nassar, M.; Daoud, A.; Nso, N.; Medina, L.; Ghernautan, V.; Bhangoo, H.; Nyein, A.; Mohamed, M.; Alqassieh, A.; Soliman, K.; et al. Diabetes Mellitus and COVID-19: Review Article. Diabetes Metab. Syndr. 2021, 15, 102268. [Google Scholar] [CrossRef]
- Karampela, I.; Vallianou, N.; Magkos, F.; Apovian, C.M.; Dalamaga, M. Obesity, Hypovitaminosis D, and COVID-19: The Bermuda Triangle in Public Health. Curr. Obes. Rep. 2022, 11, 116–125. [Google Scholar] [CrossRef]
- Dalamaga, M.; Christodoulatos, G.S.; Karampela, I.; Vallianou, N.; Apovian, C.M. Understanding the Co-Epidemic of Obesity and COVID-19: Current Evidence, Comparison with Previous Epidemics, Mechanisms, and Preventive and Therapeutic Perspectives. Curr. Obes. Rep. 2021, 10, 214–243. [Google Scholar] [CrossRef]
- Vallianou, N.G.; Evangelopoulos, A.; Kounatidis, D.; Stratigou, T.; Christodoulatos, G.S.; Karampela, I.; Dalamaga, M. Diabetes Mellitus and SARS-CoV-2 Infection: Pathophysiologic Mechanisms and Implications in Management. Curr. Diabetes Rev. 2021, 17, e123120189797. [Google Scholar] [CrossRef]
- Al-Aly, Z. Diabetes after SARS-CoV-2 infection. Lancet. Diabetes Endocrinol. 2023, 11, 11–13. [Google Scholar] [CrossRef]
- Kendall, E.K.; Olaker, V.R.; Kaelber, D.C.; Xu, R.; Davis, P.B. Association of SARS-CoV-2 Infection with New-Onset Type 1 Diabetes among Pediatric Patients from 2020 to 2021. JAMA Netw. Open 2022, 5, e2233014. [Google Scholar] [CrossRef]
- Tsilingiris, D.; Dalamaga, M.; Liu, J. SARS-CoV-2 adipose tissue infection and hyperglycemia: A further step towards the understanding of severe COVID-19. Metab. Open 2022, 13, 100163. [Google Scholar] [CrossRef]
- Tansey, C.M.; Louie, M.; Loeb, M.; Gold, W.L.; Muller, M.P.; de Jager, J.; Cameron, J.I.; Tomlinson, G.; Mazzulli, T.; Walmsley, S.L.; et al. One-year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Arch. Intern. Med. 2007, 167, 1312–1320. [Google Scholar] [CrossRef]
- Lam, M.H.; Wing, Y.K.; Yu, M.W.; Leung, C.M.; Ma, R.C.; Kong, A.P.; So, W.Y.; Fong, S.Y.; Lam, S.P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: Long-term follow-up. Arch. Intern. Med. 2009, 169, 2142–2147. [Google Scholar] [CrossRef]
- Lee, S.H.; Shin, H.S.; Park, H.Y.; Kim, J.L.; Lee, J.J.; Lee, H.; Won, S.D.; Han, W. Depression as a Mediator of Chronic Fatigue and Post-Traumatic Stress Symptoms in Middle East Respiratory Syndrome Survivors. Psychiatry Investig. 2019, 16, 59–64. [Google Scholar] [CrossRef]
- Moldofsky, H.; Patcai, J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011, 11, 37. [Google Scholar] [CrossRef]
- Fukuda, K.; Straus, S.E.; Hickie, I.; Sharpe, M.C.; Dobbins, J.G.; Komaroff, A.; International Chronic Fatigue Syndrome Study Group. The chronic fatigue syndrome: A comprehensive approach to its definition and study. Ann. Intern. Med. 1994, 121, 953–959. [Google Scholar] [CrossRef]
- CDC. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Symptoms. Available online: https://www.cdc.gov/me-cfs/symptoms-diagnosis/symptoms.html (accessed on 17 May 2023).
- Magnus, P.; Gunnes, N.; Tveito, K.; Bakken, I.J.; Ghaderi, S.; Stoltenberg, C.; Hornig, M.; Lipkin, W.I.; Trogstad, L.; Håberg, S.E. Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is associated with pandemic influenza infection, but not with an adjuvanted pandemic influenza vaccine. Vaccine 2015, 33, 6173–6177. [Google Scholar] [CrossRef]
- Wilson, H.W.; Amo-Addae, M.; Kenu, E.; Ilesanmi, O.S.; Ameme, D.K.; Sackey, S.O. Post-Ebola Syndrome among Ebola Virus Disease Survivors in Montserrado County, Liberia 2016. BioMed Res. Int. 2018, 2018, 1909410. [Google Scholar] [CrossRef]
- Garcia, M.N.; Hause, A.M.; Walker, C.M.; Orange, J.S.; Hasbun, R.; Murray, K.O. Evaluation of prolonged fatigue post-West Nile virus infection and association of fatigue with elevated antiviral and proinflammatory cytokines. Viral Immunol. 2014, 27, 327–333. [Google Scholar] [CrossRef]
- Shikova, E.; Reshkova, V.; Kumanova, A.; Raleva, S.; Alexandrova, D.; Capo, N.; Murovska, M. Cytomegalovirus, Epstein-Barr virus, and human herpesvirus-6 infections in patients with myalgic encephalomyelitis/chronic fatigue syndrome. J. Med. Virol. 2020, 92, 3682–3688. [Google Scholar] [CrossRef]
- Lim, E.J.; Ahn, Y.C.; Jang, E.S.; Lee, S.W.; Lee, S.H.; Son, C.G. Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J. Transl. Med. 2020, 18, 100. [Google Scholar] [CrossRef]
- Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: A prospective observational study. Lancet. Respir. Med. 2022, 10, 761–775. [CrossRef] [PubMed]
- Kritas, S.K.; Ronconi, G.; Caraffa, A.; Gallenga, C.E.; Ross, R.; Conti, P. Mast cells contribute to coronavirus-induced inflammation: New anti-inflammatory strategy. J. Biol. Regul. Homeost. Agents 2020, 34, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Turner, S.; Khan, M.A.; Putrino, D.; Woodcock, A.; Kell, D.B.; Pretorius, E. Long COVID: Pathophysiological factors and abnormalities of coagulation. Trends Endocrinol. Metab. 2023, 34, 321–344. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.; Chen, F.; Ou, Z.; Fan, Q.; Tan, X.; Wang, Y.; Pan, Y.; Ke, B.; Li, L.; Guan, Y.; et al. A compromised specific humoral immune response against the SARS-CoV-2 receptor-binding domain is related to viral persistence and periodic shedding in the gastrointestinal tract. Cell. Mol. Immunol. 2020, 17, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Phetsouphanh, C.; Darley, D.R.; Wilson, D.B.; Howe, A.; Munier, C.M.L.; Patel, S.K.; Juno, J.A.; Burrell, L.M.; Kent, S.J.; Dore, G.J.; et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 2022, 23, 210–216. [Google Scholar] [CrossRef]
- Pinho, J.R.R.; Oliveira, K.G.; Sitnik, R.; Maluf, M.M.; Rodrigues, P.H.S.; Santana, R.A.F.; Welter, E.R.; Irony, O. Long term persistence of coronavirus SARS-CoV-2 infection. Einstein 2021, 19, eRC6369. [Google Scholar] [CrossRef]
- Stein, S.R.; Ramelli, S.C.; Grazioli, A.; Chung, J.Y.; Singh, M.; Yinda, C.K.; Winkler, C.W.; Sun, J.; Dickey, J.M.; Ylaya, K.; et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature 2022, 612, 758–763. [Google Scholar] [CrossRef]
- Karn, V.; Ahmed, S.; Tsai, L.W.; Dubey, R.; Ojha, S.; Singh, H.N.; Kumar, M.; Gupta, P.K.; Sadhu, S.; Jha, N.K.; et al. Extracellular Vesicle-Based Therapy for COVID-19: Promises, Challenges and Future Prospects. Biomedicines 2021, 9, 1373. [Google Scholar] [CrossRef]
- Vojdani, A.; Vojdani, E.; Saidara, E.; Maes, M. Persistent SARS-CoV-2 Infection, EBV, HHV-6 and Other Factors May Contribute to Inflammation and Autoimmunity in Long COVID. Viruses 2023, 15, 400. [Google Scholar] [CrossRef]
- García-Abellán, J.; Padilla, S.; Fernández-González, M.; García, J.A.; Agulló, V.; Andreo, M.; Ruiz, S.; Galiana, A.; Gutiérrez, F.; Masiá, M. Antibody Response to SARS-CoV-2 is Associated with Long-term Clinical Outcome in Patients with COVID-19: A Longitudinal Study. J. Clin. Immunol. 2021, 41, 1490–1501. [Google Scholar] [CrossRef]
- Spatola, M.; Nziza, N.; Jung, W.; Deng, Y.; Yuan, D.; Dinoto, A.; Bozzetti, S.; Chiodega, V.; Ferrari, S.; Lauffenburger, D.A.; et al. Neurologic sequelae of COVID-19 are determined by immunologic imprinting from previous coronaviruses. Brain 2023. [Google Scholar] [CrossRef]
- Proal, A.D.; VanElzakker, M.B. Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front. Microbiol. 2021, 12, 698169. [Google Scholar] [CrossRef]
- Sausen, D.G.; Basith, A.; Muqeemuddin, S. EBV and Lymphomagenesis. Cancers 2023, 15, 2133. [Google Scholar] [CrossRef]
- Lupo, J.; Truffot, A.; Andreani, J.; Habib, M.; Epaulard, O.; Morand, P.; Germi, R. Virological Markers in Epstein-Barr Virus-Associated Diseases. Viruses 2023, 15, 656. [Google Scholar] [CrossRef]
- Lanz, T.V.; Brewer, R.C.; Ho, P.P.; Moon, J.S.; Jude, K.M.; Fernandez, D.; Fernandes, R.A.; Gomez, A.M.; Nadj, G.S.; Bartley, C.M.; et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature 2022, 603, 321–327. [Google Scholar] [CrossRef]
- Du Toit, A. EBV linked to multiple sclerosis. Nat. Rev. Microbiol. 2022, 20, 189. [Google Scholar] [CrossRef]
- Vallianou, N.G.; Tsilingiris, D.; Karampela, I.; Liu, J.; Dalamaga, M. Herpes zoster following COVID-19 vaccination in an immunocompetent and vaccinated for herpes zoster adult: A two-vaccine related event? Metab. Open 2022, 13, 100171. [Google Scholar] [CrossRef]
- Argyrakopoulou, G.; Dalamaga, M.; Spyrou, N.; Kokkinos, A. Gender Differences in Obesity-Related Cancers. Curr. Obes. Rep. 2021, 10, 100–115. [Google Scholar] [CrossRef]
- O’Leary, K. Mounting evidence for EBV links to multiple sclerosis. Nat. Med. 2022, 28, 2450. [Google Scholar] [CrossRef]
- Nekoua, M.P.; Alidjinou, E.K.; Hober, D. Persistent coxsackievirus B infection and pathogenesis of type 1 diabetes mellitus. Nat. Rev. Endocrinol. 2022, 18, 503–516. [Google Scholar] [CrossRef]
- Wang, L.; Cao, Z.M.; Zhang, L.L.; Dai, X.C.; Liu, Z.J.; Zeng, Y.X.; Li, X.Y.; Wu, Q.J.; Lv, W.L. Helicobacter Pylori and Autoimmune Diseases: Involving Multiple Systems. Front. Immunol. 2022, 13, 833424. [Google Scholar] [CrossRef] [PubMed]
- Zangiabadian, M.; Mirsaeidi, M.; Pooyafar, M.H.; Goudarzi, M.; Nasiri, M.J. Associations of Yersinia Enterocolitica Infection with Autoimmune Thyroid Diseases: A Systematic Review and Meta-Analysis. Endocr. Metab. Immune Disord. Drug Targets 2021, 21, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, A.; Putrino, D. Why we need a deeper understanding of the pathophysiology of long COVID. Lancet. Infect. Dis. 2023, 23, 393–395. [Google Scholar] [CrossRef] [PubMed]
- Lake, C.M.; Breen, J.J. Sequence similarity between SARS-CoV-2 nucleocapsid and multiple sclerosis-associated proteins provides insight into viral neuropathogenesis following infection. Sci. Rep. 2023, 13, 389. [Google Scholar] [CrossRef] [PubMed]
- Tsilingiris, D.; Vallianou, N.G.; Karampela, I.; Dalamaga, M. Vaccine induced thrombotic thrombocytopenia: The shady chapter of a success story. Metab. Open 2021, 11, 100101. [Google Scholar] [CrossRef]
- Brogna, C.; Brogna, B.; Bisaccia, D.R.; Lauritano, F.; Marino, G.; Montano, L.; Cristoni, S.; Prisco, M.; Piscopo, M. Could SARS-CoV-2 Have Bacteriophage Behavior or Induce the Activity of Other Bacteriophages? Vaccines 2022, 10, 708. [Google Scholar] [CrossRef]
- Zuo, T.; Zhang, F.; Lui, G.C.Y.; Yeoh, Y.K.; Li, A.Y.L.; Zhan, H.; Wan, Y.; Chung, A.C.K.; Cheung, C.P.; Chen, N.; et al. Alterations in Gut Microbiota of Patients with COVID-19 during Time of Hospitalization. Gastroenterology 2020, 159, 944–955.e948. [Google Scholar] [CrossRef]
- Vallianou, N.; Kounatidis, D.; Christodoulatos, G.S.; Panagopoulos, F.; Karampela, I.; Dalamaga, M. Mycobiome and Cancer: What Is the Evidence? Cancers 2021, 13, 3149. [Google Scholar] [CrossRef]
- Spyrou, N.; Vallianou, N.; Kadillari, J.; Dalamaga, M. The interplay of obesity, gut microbiome and diet in the immune check point inhibitors therapy era. Semin. Cancer Biol. 2021, 73, 356–376. [Google Scholar] [CrossRef]
- Vallianou, N.; Dalamaga, M.; Stratigou, T.; Karampela, I.; Tsigalou, C. Do Antibiotics Cause Obesity Through Long-term Alterations in the Gut Microbiome? A Review of Current Evidence. Curr. Obes. Rep. 2021, 10, 244–262. [Google Scholar] [CrossRef]
- Tsigalou, C.; Vallianou, N.; Dalamaga, M. Autoantibody Production in Obesity: Is There Evidence for a Link Between Obesity and Autoimmunity? Curr. Obes. Rep. 2020, 9, 245–254. [Google Scholar] [CrossRef]
- Koliaki, C.; Liatis, S.; Dalamaga, M.; Kokkinos, A. The Implication of Gut Hormones in the Regulation of Energy Homeostasis and Their Role in the Pathophysiology of Obesity. Curr. Obes. Rep. 2020, 9, 255–271. [Google Scholar] [CrossRef]
- Ahamed, J.; Laurence, J. Long COVID endotheliopathy: Hypothesized mechanisms and potential therapeutic approaches. J. Clin. Investig. 2022, 132, 2133. [Google Scholar] [CrossRef]
- Paniz-Mondolfi, A.; Bryce, C.; Grimes, Z.; Gordon, R.E.; Reidy, J.; Lednicky, J.; Sordillo, E.M.; Fowkes, M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J. Med. Virol. 2020, 92, 699–702. [Google Scholar] [CrossRef]
- Fox, S.E.; Li, G.; Akmatbekov, A.; Harbert, J.L.; Lameira, F.S.; Brown, J.Q.; Vander Heide, R.S. Unexpected Features of Cardiac Pathology in COVID-19 Infection. Circulation 2020, 142, 1123–1125. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. Jama 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Kassi, E.; Dalamaga, M.; Hroussalas, G.; Kazanis, K.; Merantzi, G.; Zachari, A.; Giamarellos-Bourboulis, E.J.; Dionyssiou-Asteriou, A. Adipocyte factors, high-sensitive C-reactive protein levels and lipoxidative stress products in overweight postmenopausal women with normal and impaired OGTT. Maturitas 2010, 67, 72–77. [Google Scholar] [CrossRef]
- Hroussalas, G.; Kassi, E.; Dalamaga, M.; Delimaris, I.; Zachari, A.; Dionyssiou-Asteriou, A. Leptin, soluble leptin receptor, adiponectin and resistin in relation to OGTT in overweight/obese postmenopausal women. Maturitas 2008, 59, 339–349. [Google Scholar] [CrossRef]
- Tsilingiris, D.; Tzeravini, E.; Koliaki, C.; Dalamaga, M.; Kokkinos, A. The Role of Mitochondrial Adaptation and Metabolic Flexibility in the Pathophysiology of Obesity and Insulin Resistance: An Updated Overview. Curr. Obes. Rep. 2021, 10, 191–213. [Google Scholar] [CrossRef]
- Kassi, E.; Dalamaga, M.; Faviou, E.; Hroussalas, G.; Kazanis, K.; Nounopoulos, C.; Dionyssiou-Asteriou, A. Circulating oxidized LDL levels, current smoking and obesity in postmenopausal women. Atherosclerosis 2009, 205, 279–283. [Google Scholar] [CrossRef]
- Nunes, J.M.; Kruger, A.; Proal, A.; Kell, D.B.; Pretorius, E. The Occurrence of Hyperactivated Platelets and Fibrinaloid Microclots in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Pharmaceuticals 2022, 15, 931. [Google Scholar] [CrossRef] [PubMed]
- Xiang, M.; Wu, X.; Jing, H.; Novakovic, V.A.; Shi, J. The intersection of obesity and (long) COVID-19: Hypoxia, thrombotic inflammation, and vascular endothelial injury. Front. Cardiovasc. Med. 2023, 10, 1062491. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Laubscher, G.J.; Pretorius, E. A central role for amyloid fibrin microclots in long COVID/PASC: Origins and therapeutic implications. Biochem. J. 2022, 479, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Bansal, R.; Gubbi, S.; Koch, C.A. COVID-19 and chronic fatigue syndrome: An endocrine perspective. J. Clin. Transl. Endocrinol. 2022, 27, 100284. [Google Scholar] [CrossRef] [PubMed]
- Wheatland, R. Molecular mimicry of ACTH in SARS—Implications for corticosteroid treatment and prophylaxis. Med. Hypotheses 2004, 63, 855–862. [Google Scholar] [CrossRef]
- Al-Hakeim, H.K.; Al-Rubaye, H.T.; Jubran, A.S.; Almulla, A.F.; Moustafa, S.R.; Maes, M. Increased insulin resistance due to Long COVID is associated with depressive symptoms and partly predicted by the inflammatory response during acute infection. Braz. J. Psychiatry 2023. [Google Scholar] [CrossRef]
- Dodd, S.; Sominsky, L.; Siskind, D.; Bortolasci, C.C.; Carvalho, A.F.; Maes, M.; Walker, A.J.; Walder, K.; Yung, A.R.; Williams, L.J.; et al. The role of metformin as a treatment for neuropsychiatric illness. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2022, 64, 32–43. [Google Scholar] [CrossRef]
- Scherer, P.E.; Kirwan, J.P.; Rosen, C.J. Post-acute sequelae of COVID-19: A metabolic perspective. eLife 2022, 11, e78200. [Google Scholar] [CrossRef]
- Tan, D.X.; Reiter, R.J. Mechanisms and clinical evidence to support melatonin’s use in severe COVID-19 patients to lower mortality. Life Sci. 2022, 294, 120368. [Google Scholar] [CrossRef]
- Cardinali, D.P.; Brown, G.M.; Pandi-Perumal, S.R. Possible Application of Melatonin in Long COVID. Biomolecules 2022, 12, 1646. [Google Scholar] [CrossRef]
- Etter, M.M.; Martins, T.A.; Kulsvehagen, L.; Pössnecker, E.; Duchemin, W.; Hogan, S.; Sanabria-Diaz, G.; Müller, J.; Chiappini, A.; Rychen, J.; et al. Severe Neuro-COVID is associated with peripheral immune signatures, autoimmunity and neurodegeneration: A prospective cross-sectional study. Nat. Commun. 2022, 13, 6777. [Google Scholar] [CrossRef]
- Spudich, S.; Nath, A. Nervous system consequences of COVID-19. Science 2022, 375, 267–269. [Google Scholar] [CrossRef]
- Leng, A.; Shah, M.; Ahmad, S.A.; Premraj, L.; Wildi, K.; Li Bassi, G.; Pardo, C.A.; Choi, A.; Cho, S.M. Pathogenesis Underlying Neurological Manifestations of Long COVID Syndrome and Potential Therapeutics. Cells 2023, 12, 816. [Google Scholar] [CrossRef]
- Raj, S.R.; Bourne, K.M.; Stiles, L.E.; Miglis, M.G.; Cortez, M.M.; Miller, A.J.; Freeman, R.; Biaggioni, I.; Rowe, P.C.; Sheldon, R.S.; et al. Postural orthostatic tachycardia syndrome (POTS): Priorities for POTS care and research from a 2019 National Institutes of Health Expert Consensus Meeting—Part 2. Auton. Neurosci. Basic Clin. 2021, 235, 102836. [Google Scholar] [CrossRef]
- Wallukat, G.; Hohberger, B.; Wenzel, K.; Fürst, J.; Schulze-Rothe, S.; Wallukat, A.; Hönicke, A.S.; Müller, J. Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J. Transl. Autoimmun. 2021, 4, 100100. [Google Scholar] [CrossRef]
- Sinaei, R.; Nejadbiglari, H.; Sinaei, R.; Zeinaly, M.; Pezeshki, S.; Jafari, M. Finding positive SARS-CoV-2 RT-PCR in cerebrospinal fluid of two pediatric patients with severe COVID-19: A brief case report. BMC Pediatr. 2023, 23, 49. [Google Scholar] [CrossRef]
- Jarius, S.; Pache, F.; Körtvelyessy, P.; Jelčić, I.; Stettner, M.; Franciotta, D.; Keller, E.; Neumann, B.; Ringelstein, M.; Senel, M.; et al. Cerebrospinal fluid findings in COVID-19: A multicenter study of 150 lumbar punctures in 127 patients. J. Neuroinflamm. 2022, 19, 19. [Google Scholar] [CrossRef]
- Díaz-Resendiz, K.J.G.; Benitez-Trinidad, A.B.; Covantes-Rosales, C.E.; Toledo-Ibarra, G.A.; Ortiz-Lazareno, P.C.; Girón-Pérez, D.A.; Bueno-Durán, A.Y.; Pérez-Díaz, D.A.; Barcelos-García, R.G.; Girón-Pérez, M.I. Loss of mitochondrial membrane potential (ΔΨ(m)) in leucocytes as post-COVID-19 sequelae. J. Leukoc. Biol. 2022, 112, 23–29. [Google Scholar] [CrossRef]
- Guntur, V.P.; Nemkov, T.; de Boer, E.; Mohning, M.P.; Baraghoshi, D.; Cendali, F.I.; San-Millán, I.; Petrache, I.; D’Alessandro, A. Signatures of Mitochondrial Dysfunction and Impaired Fatty Acid Metabolism in Plasma of Patients with Post-Acute Sequelae of COVID-19 (PASC). Metabolites 2022, 12, 1026. [Google Scholar] [CrossRef]
- Twomey, R.; DeMars, J.; Franklin, K.; Culos-Reed, S.N.; Weatherald, J.; Wrightson, J.G. Chronic Fatigue and Postexertional Malaise in People Living with Long COVID: An Observational Study. Phys. Ther. 2022, 102, pzac005. [Google Scholar] [CrossRef]
- Heerdt, P.M.; Shelley, B.; Singh, I. Impaired systemic oxygen extraction long after mild COVID-19: Potential perioperative implications. Br. J. Anaesth. 2022, 128, e246–e249. [Google Scholar] [CrossRef] [PubMed]
- Paul, B.D.; Lemle, M.D.; Komaroff, A.L.; Snyder, S.H. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proc. Natl. Acad. Sci. USA 2021, 118, e2024358118. [Google Scholar] [CrossRef] [PubMed]
- de Boer, E.; Petrache, I.; Goldstein, N.M.; Olin, J.T.; Keith, R.C.; Modena, B.; Mohning, M.P.; Yunt, Z.X.; San-Millán, I.; Swigris, J.J. Decreased Fatty Acid Oxidation and Altered Lactate Production during Exercise in Patients with Post-acute COVID-19 Syndrome. Am. J. Respir. Crit. Care Med. 2022, 205, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Terpos, E.; Ntanasis-Stathopoulos, I.; Elalamy, I.; Kastritis, E.; Sergentanis, T.N.; Politou, M.; Psaltopoulou, T.; Gerotziafas, G.; Dimopoulos, M.A. Hematological findings and complications of COVID-19. Am. J. Hematol. 2020, 95, 834–847. [Google Scholar] [CrossRef]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020, 130, 2620–2629. [Google Scholar] [CrossRef]
- Kotecha, T.; Knight, D.S.; Razvi, Y.; Kumar, K.; Vimalesvaran, K.; Thornton, G.; Patel, R.; Chacko, L.; Brown, J.T.; Coyle, C.; et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur. Heart J. 2021, 42, 1866–1878. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Fagot Gandet, F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef]
- Karampela, I.; Christodoulatos, G.S.; Vallianou, N.; Tsilingiris, D.; Chrysanthopoulou, E.; Skyllas, G.; Antonakos, G.; Marinou, I.; Vogiatzakis, E.; Armaganidis, A.; et al. Circulating Chemerin and Its Kinetics May Be a Useful Diagnostic and Prognostic Biomarker in Critically Ill Patients with Sepsis: A Prospective Study. Biomolecules 2022, 12, 301. [Google Scholar] [CrossRef]
- Karampela, I.; Christodoulatos, G.S.; Dalamaga, M. The Role of Adipose Tissue and Adipokines in Sepsis: Inflammatory and Metabolic Considerations, and the Obesity Paradox. Curr. Obes. Rep. 2019, 8, 434–457. [Google Scholar] [CrossRef]
- Dalamaga, M.; Karmaniolas, K.; Nikolaidou, A.; Papadavid, E. Hypocalcemia, hypomagnesemia, and hypokalemia following hydrofluoric acid chemical injury. J. Burn Care Res. Off. Publ. Am. Burn Assoc. 2008, 29, 541–543. [Google Scholar] [CrossRef]
- Karampela, I.; Kandri, E.; Antonakos, G.; Vogiatzakis, E.; Christodoulatos, G.S.; Nikolaidou, A.; Dimopoulos, G.; Armaganidis, A.; Dalamaga, M. Kinetics of circulating fetuin-A may predict mortality independently from adiponectin, high molecular weight adiponectin and prognostic factors in critically ill patients with sepsis: A prospective study. J. Crit. Care 2017, 41, 78–85. [Google Scholar] [CrossRef]
- Shaw, B.H.; Stiles, L.E.; Bourne, K.; Green, E.A.; Shibao, C.A.; Okamoto, L.E.; Garland, E.M.; Gamboa, A.; Diedrich, A.; Raj, V.; et al. The face of postural tachycardia syndrome—Insights from a large cross-sectional online community-based survey. J. Intern. Med. 2019, 286, 438–448. [Google Scholar] [CrossRef]
- Houben-Wilke, S.; Goërtz, Y.M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.; van Herck, M.; Burtin, C.; Posthuma, R.; Franssen, F.M.; et al. The Impact of Long COVID-19 on Mental Health: Observational 6-Month Follow-Up Study. JMIR Ment. Health 2022, 9, e33704. [Google Scholar] [CrossRef]
- Naidu, S.B.; Shah, A.J.; Saigal, A.; Smith, C.; Brill, S.E.; Goldring, J.; Hurst, J.R.; Jarvis, H.; Lipman, M.; Mandal, S. The high mental health burden of “Long COVID” and its association with on-going physical and respiratory symptoms in all adults discharged from hospital. Eur. Respir. J. 2021, 57, 2004364. [Google Scholar] [CrossRef]
- Roca-Fernandez, A.; Wamil, M.; Telford, A.; Carapella, V.; Borlotti, A.; Monteiro, D.; Thomaides-Brears, H.; Kelly, M.; Dennis, A.; Banerjee, R.; et al. Cardiac abnormalities in Long COVID 1-year post-SARS-CoV-2 infection. Open Heart 2023, 10, e002241. [Google Scholar] [CrossRef]
- Hughes, S.E.; Haroon, S.; Subramanian, A.; McMullan, C.; Aiyegbusi, O.L.; Turner, G.M.; Jackson, L.; Davies, E.H.; Frost, C.; McNamara, G.; et al. Development and validation of the symptom burden questionnaire for long COVID (SBQ-LC): Rasch analysis. BMJ 2022, 377, e070230. [Google Scholar] [CrossRef]
- Jamal, S.M.; Landers, D.B.; Hollenberg, S.M.; Turi, Z.G.; Glotzer, T.V.; Tancredi, J.; Parrillo, J.E. Prospective Evaluation of Autonomic Dysfunction in Post-Acute Sequela of COVID-19. J. Am. Coll. Cardiol. 2022, 79, 2325–2330. [Google Scholar] [CrossRef]
- Stavileci, B.; Özdemir, E.; Özdemir, B.; Ereren, E.; Cengiz, M. De-novo development of fragmented QRS during a six-month follow-up period in patients with COVID-19 disease and its cardiac effects. J. Electrocardiol. 2022, 72, 44–48. [Google Scholar] [CrossRef]
- Grist, J.T.; Collier, G.J.; Walters, H.; Kim, M.; Chen, M.; Abu Eid, G.; Laws, A.; Matthews, V.; Jacob, K.; Cross, S.; et al. Lung Abnormalities Detected with Hyperpolarized (129)Xe MRI in Patients with Long COVID. Radiology 2022, 305, 709–717. [Google Scholar] [CrossRef]
- Bateman, L.; Bested, A.C.; Bonilla, H.F.; Chheda, B.V.; Chu, L.; Curtin, J.M.; Dempsey, T.T.; Dimmock, M.E.; Dowell, T.G.; Felsenstein, D.; et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management. Mayo Clin. Proc. 2021, 96, 2861–2878. [Google Scholar] [CrossRef]
- Yong, S.J.; Halim, A.; Halim, M.; Liu, S.; Aljeldah, M.; Al Shammari, B.R.; Alwarthan, S.; Alhajri, M.; Alawfi, A.; Alshengeti, A.; et al. Inflammatory and vascular biomarkers in post-COVID-19 syndrome: A systematic review and meta-analysis of over 20 biomarkers. Rev. Med. Virol. 2023, 33, e2424. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.X.; Agbana, Y.L.; Sun, Z.S.; Fei, S.W.; Zhao, H.Q.; Zhou, X.N.; Chen, J.H.; Kassegne, K. Increased interleukin-6 is associated with long COVID-19: A systematic review and meta-analysis. Infect. Dis. Poverty 2023, 12, 43. [Google Scholar] [CrossRef] [PubMed]
- Klein, J.; Wood, J.; Jaycox, J.; Lu, P.; Dhodapkar, R.M.; Gehlhausen, J.R.; Tabachnikova, A.; Tabacof, L.; Malik, A.A.; Kamath, K.; et al. Distinguishing features of Long COVID identified through immune profiling. medRxiv 2022. [Google Scholar] [CrossRef]
- Haunhorst, S.; Bloch, W.; Javelle, F.; Krüger, K.; Baumgart, S.; Drube, S.; Lemhöfer, C.; Reuken, P.; Stallmach, A.; Müller, M.; et al. A scoping review of regulatory T cell dynamics in convalescent COVID-19 patients—Indications for their potential involvement in the development of Long COVID? Front. Immunol. 2022, 13, 1070994. [Google Scholar] [CrossRef]
- Galán, M.; Vigón, L.; Fuertes, D.; Murciano-Antón, M.A.; Casado-Fernández, G.; Domínguez-Mateos, S.; Mateos, E.; Ramos-Martín, F.; Planelles, V.; Torres, M.; et al. Persistent Overactive Cytotoxic Immune Response in a Spanish Cohort of Individuals with Long-COVID: Identification of Diagnostic Biomarkers. Front. Immunol. 2022, 13, 848886. [Google Scholar] [CrossRef]
- Utrero-Rico, A.; Ruiz-Ruigómez, M.; Laguna-Goya, R.; Arrieta-Ortubay, E.; Chivite-Lacaba, M.; González-Cuadrado, C.; Lalueza, A.; Almendro-Vazquez, P.; Serrano, A.; Aguado, J.M.; et al. A Short Corticosteroid Course Reduces Symptoms and Immunological Alterations Underlying Long-COVID. Biomedicines 2021, 9, 1540. [Google Scholar] [CrossRef]
- Patterson, B.K.; Guevara-Coto, J.; Yogendra, R.; Francisco, E.B.; Long, E.; Pise, A.; Rodrigues, H.; Parikh, P.; Mora, J.; Mora-Rodríguez, R.A. Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning. Front. Immunol. 2021, 12, 700782. [Google Scholar] [CrossRef]
- Swank, Z.; Senussi, Y.; Manickas-Hill, Z.; Yu, X.G.; Li, J.Z.; Alter, G.; Walt, D.R. Persistent Circulating Severe Acute Respiratory Syndrome Coronavirus 2 Spike Is Associated with Post-acute Coronavirus Disease 2019 Sequelae. Clin. Infect. Dis. 2023, 76, e487–e490. [Google Scholar] [CrossRef]
- Natarajan, A.; Zlitni, S.; Brooks, E.F.; Vance, S.E.; Dahlen, A.; Hedlin, H.; Park, R.M.; Han, A.; Schmidtke, D.T.; Verma, R.; et al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med 2022, 3, 371–387.e379. [Google Scholar] [CrossRef]
- Tejerina, F.; Catalan, P.; Rodriguez-Grande, C.; Adan, J.; Rodriguez-Gonzalez, C.; Muñoz, P.; Aldamiz, T.; Diez, C.; Perez, L.; Fanciulli, C.; et al. Post-COVID-19 syndrome. SARS-CoV-2 RNA detection in plasma, stool, and urine in patients with persistent symptoms after COVID-19. BMC Infect. Dis. 2022, 22, 211. [Google Scholar] [CrossRef]
- Zollner, A.; Koch, R.; Jukic, A.; Pfister, A.; Meyer, M.; Rössler, A.; Kimpel, J.; Adolph, T.E.; Tilg, H. Postacute COVID-19 is Characterized by Gut Viral Antigen Persistence in Inflammatory Bowel Diseases. Gastroenterology 2022, 163, 495–506.e498. [Google Scholar] [CrossRef]
- Yonker, L.M.; Gilboa, T.; Ogata, A.F.; Senussi, Y.; Lazarovits, R.; Boribong, B.P.; Bartsch, Y.C.; Loiselle, M.; Rivas, M.N.; Porritt, R.A.; et al. Multisystem inflammatory syndrome in children is driven by zonulin-dependent loss of gut mucosal barrier. J. Clin. Investig. 2021, 131. [Google Scholar] [CrossRef]
- Files, J.K.; Sarkar, S.; Fram, T.R.; Boppana, S.; Sterrett, S.; Qin, K.; Bansal, A.; Long, D.M.; Sabbaj, S.; Kobie, J.J.; et al. Duration of post-COVID-19 symptoms is associated with sustained SARS-CoV-2-specific immune responses. JCI Insight 2021, 6, e151544. [Google Scholar] [CrossRef]
- Augustin, M.; Schommers, P.; Stecher, M.; Dewald, F.; Gieselmann, L.; Gruell, H.; Horn, C.; Vanshylla, K.; Cristanziano, V.D.; Osebold, L.; et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: A longitudinal prospective cohort study. Lancet Reg. Health. Eur. 2021, 6, 100122. [Google Scholar] [CrossRef]
- Blomberg, B.; Mohn, K.G.; Brokstad, K.A.; Zhou, F.; Linchausen, D.W.; Hansen, B.A.; Lartey, S.; Onyango, T.B.; Kuwelker, K.; Sævik, M.; et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. 2021, 27, 1607–1613. [Google Scholar] [CrossRef]
- Peluso, M.J.; Deitchman, A.N.; Torres, L.; Iyer, N.S.; Munter, S.E.; Nixon, C.C.; Donatelli, J.; Thanh, C.; Takahashi, S.; Hakim, J.; et al. Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms. Cell Rep. 2021, 36, 109518. [Google Scholar] [CrossRef]
- Peluso, M.J.; Deveau, T.M.; Munter, S.E.; Ryder, D.; Buck, A.; Beck-Engeser, G.; Chan, F.; Lu, S.; Goldberg, S.A.; Hoh, R.; et al. Chronic viral coinfections differentially affect the likelihood of developing long COVID. J. Clin. Investig. 2023, 133. [Google Scholar] [CrossRef]
- Zubchenko, S.; Kril, I.; Nadizhko, O.; Matsyura, O.; Chopyak, V. Herpesvirus infections and post-COVID-19 manifestations: A pilot observational study. Rheumatol. Int. 2022, 42, 1523–1530. [Google Scholar] [CrossRef]
- Su, Y.; Yuan, D.; Chen, D.G.; Ng, R.H.; Wang, K.; Choi, J.; Li, S.; Hong, S.; Zhang, R.; Xie, J.; et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 2022, 185, 881–895.e820. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.E.; Okyay, R.A.; Licht, W.E.; Hurley, D.J. Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation. Pathogens 2021, 10, 763. [Google Scholar] [CrossRef]
- Muri, J.; Cecchinato, V.; Cavalli, A.; Shanbhag, A.A.; Matkovic, M.; Biggiogero, M.; Maida, P.A.; Moritz, J.; Toscano, C.; Ghovehoud, E.; et al. Autoantibodies against chemokines post-SARS-CoV-2 infection correlate with disease course. Nat. Immunol. 2023, 24, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Bodansky, A.; Wang, C.Y.; Saxena, A.; Mitchell, A.; Takahashi, S.; Anglin, K.; Huang, B.; Hoh, R.; Lu, S.; Goldberg, S.A.; et al. Autoantigen profiling reveals a shared post-COVID signature in fully recovered and Long COVID patients. medRxiv 2023. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Jamil, R.; Chowdhury, A.; Mukherjee, M.; Venegas, C.; Miyasaki, K.; Zhang, K.; Patel, Z.; Salter, B.; Yuen, A.C.Y.; et al. Circulating anti-nuclear autoantibodies in COVID-19 survivors predict long COVID symptoms. Eur. Respir. J. 2023, 61, 2200970. [Google Scholar] [CrossRef] [PubMed]
- Franke, C.; Boesl, F.; Goereci, Y.; Gerhard, A.; Schweitzer, F.; Schroeder, M.; Foverskov-Rasmussen, H.; Heine, J.; Quitschau, A.; Kandil, F.I.; et al. Association of cerebrospinal fluid brain-binding autoantibodies with cognitive impairment in post-COVID-19 syndrome. Brain Behav. Immun. 2023, 109, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Peluso, M.J.; Mitchell, A.; Wang, C.Y.; Takahashi, S.; Hoh, R.; Tai, V.; Durstenfeld, M.S.; Hsue, P.Y.; Kelly, J.D.; Martin, J.N.; et al. Low Prevalence of Interferon α Autoantibodies in People Experiencing Symptoms of Post-Coronavirus Disease 2019 (COVID-19) Conditions, or Long COVID. J. Infect. Dis. 2023, 227, 246–250. [Google Scholar] [CrossRef]
- Rojas, M.; Rodríguez, Y.; Acosta-Ampudia, Y.; Monsalve, D.M.; Zhu, C.; Li, Q.Z.; Ramírez-Santana, C.; Anaya, J.M. Autoimmunity is a hallmark of post-COVID syndrome. J. Transl. Med. 2022, 20, 129. [Google Scholar] [CrossRef]
- Patel, M.A.; Knauer, M.J.; Nicholson, M.; Daley, M.; Van Nynatten, L.R.; Martin, C.; Patterson, E.K.; Cepinskas, G.; Seney, S.L.; Dobretzberger, V.; et al. Elevated vascular transformation blood biomarkers in Long-COVID indicate angiogenesis as a key pathophysiological mechanism. Mol. Med. 2022, 28, 122. [Google Scholar] [CrossRef]
- Haffke, M.; Freitag, H.; Rudolf, G.; Seifert, M.; Doehner, W.; Scherbakov, N.; Hanitsch, L.; Wittke, K.; Bauer, S.; Konietschke, F.; et al. Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS). J. Transl. Med. 2022, 20, 138. [Google Scholar] [CrossRef]
- Tong, M.; Yan, X.; Jiang, Y.; Jin, Z.; Zhu, S.; Zou, L.; Liu, Y.; Zheng, Q.; Chen, G.; Gu, R.; et al. Endothelial Biomarkers in Patients Recovered from COVID-19 One Year after Hospital Discharge: A Cross-Sectional Study. Mediterr. J. Hematol. Infect. Dis. 2022, 14, e2022033. [Google Scholar] [CrossRef]
- Constantinescu-Bercu, A.; Kessler, A.; de Groot, R.; Dragunaite, B.; Heightman, M.; Hillman, T.; Price, L.C.; Brennan, E.; Sivera, R.; Vanhoorelbeke, K.; et al. Analysis of thrombogenicity under flow reveals new insights into the prothrombotic state of patients with post-COVID syndrome. J. Thromb. Haemost. JTH 2023, 21, 94–100. [Google Scholar] [CrossRef]
- Di Gennaro, L.; Valentini, P.; Sorrentino, S.; Ferretti, M.A.; De Candia, E.; Basso, M.; Lancellotti, S.; De Cristofaro, R.; De Rose, C.; Mariani, F.; et al. Extended coagulation profile of children with Long COVID: A prospective study. Sci. Rep. 2022, 12, 18392. [Google Scholar] [CrossRef]
- Kruger, A.; Vlok, M.; Turner, S.; Venter, C.; Laubscher, G.J.; Kell, D.B.; Pretorius, E. Proteomics of fibrin amyloid microclots in long COVID/post-acute sequelae of COVID-19 (PASC) shows many entrapped pro-inflammatory molecules that may also contribute to a failed fibrinolytic system. Cardiovasc. Diabetol. 2022, 21, 190. [Google Scholar] [CrossRef]
- Pretorius, E.; Vlok, M.; Venter, C.; Bezuidenhout, J.A.; Laubscher, G.J.; Steenkamp, J.; Kell, D.B. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021, 20, 172. [Google Scholar] [CrossRef]
- di Filippo, L.; Frara, S.; Nannipieri, F.; Cotellessa, A.; Locatelli, M.; Rovere Querini, P.; Giustina, A. Low vitamin D levels are associated with Long COVID syndrome in COVID-19 survivors. J. Clin. Endocrinol. Metab. 2023. [Google Scholar] [CrossRef]
- Mohamed Hussein, A.A.R.; Galal, I.; Amin, M.T.; Moshnib, A.A.; Makhlouf, N.A.; Makhlouf, H.A.; Abd-Elaal, H.K.; Kholief, K.M.S.; Abdel Tawab, D.A.; Kamal Eldin, K.A.; et al. Prevalence of vitamin D deficiency among patients attending Post COVID-19 follow-up clinic: A cross-sectional study. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 3038–3045. [Google Scholar] [CrossRef]
- Sunada, N.; Honda, H.; Nakano, Y.; Yamamoto, K.; Tokumasu, K.; Sakurada, Y.; Matsuda, Y.; Hasegawa, T.; Otsuka, Y.; Obika, M.; et al. Hormonal trends in patients suffering from long COVID symptoms. Endocr. J. 2022, 69, 1173–1181. [Google Scholar] [CrossRef]
- Townsend, L.; Dyer, A.H.; McCluskey, P.; O’Brien, K.; Dowds, J.; Laird, E.; Bannan, C.; Bourke, N.M.; Cheallaigh, C.N.; Byrne, D.G.; et al. Investigating the Relationship between Vitamin D and Persistent Symptoms Following SARS-CoV-2 Infection. Nutrients 2021, 13, 2430. [Google Scholar] [CrossRef]
- Captur, G.; Moon, J.C.; Topriceanu, C.C.; Joy, G.; Swadling, L.; Hallqvist, J.; Doykov, I.; Patel, N.; Spiewak, J.; Baldwin, T.; et al. Plasma proteomic signature predicts who will get persistent symptoms following SARS-CoV-2 infection. EBioMedicine 2022, 85, 104293. [Google Scholar] [CrossRef]
- López-Hernández, Y.; Oropeza-Valdez, J.J.; García Lopez, D.A.; Borrego, J.C.; Murgu, M.; Valdez, J.; López, J.A.; Monárrez-Espino, J. Untargeted analysis in post-COVID-19 patients reveals dysregulated lipid pathways two years after recovery. Front. Mol. Biosci. 2023, 10, 1100486. [Google Scholar] [CrossRef]
- López-Hernández, Y.; Aquino, J.M.; López, D.A.G.; Zheng, J.; Borrego, J.C.; Torres-Calzada, C.; Elizalde-Díaz, J.P.; Mandal, R.; Berjanskii, M.; Martínez-Martínez, E.; et al. The plasma metabolome of long COVID-19 patients two years after infection. medRxiv 2023. [Google Scholar] [CrossRef]
- Cysique, L.A.; Jakabek, D.; Bracken, S.G.; Allen-Davidian, Y.; Heng, B.; Chow, S.; Dehhaghi, M.; Pires, A.S.; Darley, D.R.; Byrne, A.; et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: A longitudinal observational study. medRxiv 2022. [Google Scholar] [CrossRef]
- Zhang, D.; Zhou, Y.; Ma, Y.; Chen, P.; Tang, J.; Yang, B.; Li, H.; Liang, M.; Xue, Y.; Liu, Y.; et al. Gut Microbiota Dysbiosis Correlates with Long COVID-19 at One-Year After Discharge. J. Korean Med. Sci. 2023, 38, e120. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Mak, J.W.Y.; Su, Q.; Yeoh, Y.K.; Lui, G.C.; Ng, S.S.S.; Zhang, F.; Li, A.Y.L.; Lu, W.; Hui, D.S.; et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut 2022, 71, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Apple, A.C.; Oddi, A.; Peluso, M.J.; Asken, B.M.; Henrich, T.J.; Kelly, J.D.; Pleasure, S.J.; Deeks, S.G.; Allen, I.E.; Martin, J.N.; et al. Risk factors and abnormal cerebrospinal fluid associate with cognitive symptoms after mild COVID-19. Ann. Clin. Transl. Neurol. 2022, 9, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Guasp, M.; Muñoz-Sánchez, G.; Martínez-Hernández, E.; Santana, D.; Carbayo, Á.; Naranjo, L.; Bolós, U.; Framil, M.; Saiz, A.; Balasa, M.; et al. CSF Biomarkers in COVID-19 Associated Encephalopathy and Encephalitis Predict Long-Term Outcome. Front. Immunol. 2022, 13, 866153. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, B.; Cosme, J.; Dupuis, C.; Coupez, E.; Adda, M.; Calvet, L.; Fabre, L.; Saint-Sardos, P.; Bereiziat, M.; Vidal, M.; et al. Severe COVID-19 is characterized by the co-occurrence of moderate cytokine inflammation and severe monocyte dysregulation. EBioMedicine 2021, 73, 103622. [Google Scholar] [CrossRef]
- Montazersaheb, S.; Hosseiniyan Khatibi, S.M.; Hejazi, M.S.; Tarhriz, V.; Farjami, A.; Ghasemian Sorbeni, F.; Farahzadi, R.; Ghasemnejad, T. COVID-19 infection: An overview on cytokine storm and related interventions. Virol. J. 2022, 19, 92. [Google Scholar] [CrossRef]
- Low, R.N.; Low, R.J.; Akrami, A. A review of cytokine-based pathophysiology of Long COVID symptoms. Front. Med. 2023, 10, 1011936. [Google Scholar] [CrossRef]
- Peluso, M.J.; Lu, S.; Tang, A.F.; Durstenfeld, M.S.; Ho, H.E.; Goldberg, S.A.; Forman, C.A.; Munter, S.E.; Hoh, R.; Tai, V.; et al. Markers of Immune Activation and Inflammation in Individuals with Postacute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 Infection. J. Infect. Dis. 2021, 224, 1839–1848. [Google Scholar] [CrossRef]
- Littlefield, K.M.; Watson, R.O.; Schneider, J.M.; Neff, C.P.; Yamada, E.; Zhang, M.; Campbell, T.B.; Falta, M.T.; Jolley, S.E.; Fontenot, A.P.; et al. SARS-CoV-2-specific T cells associate with inflammation and reduced lung function in pulmonary post-acute sequalae of SARS-CoV-2. PLoS Pathog. 2022, 18, e1010359. [Google Scholar] [CrossRef]
- Cortellini, A.; Gennari, A.; Pommeret, F.; Patel, G.; Newsom-Davis, T.; Bertuzzi, A.; Viladot, M.; Aguilar-Company, J.; Mirallas, O.; Felip, E.; et al. COVID-19 Sequelae and the Host Proinflammatory Response: An Analysis from the OnCovid Registry. J. Natl. Cancer Inst. 2022, 114, 979–987. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.J.; Weng, Z.C. [Influence of stimulation of the skin receptive field on evoked discharges of the polymodal nociceptors in rats]. Sheng Li Xue Bao 1988, 40, 437–443. [Google Scholar] [PubMed]
- Queiroz, M.A.F.; Neves, P.; Lima, S.S.; Lopes, J.D.C.; Torres, M.; Vallinoto, I.; Bichara, C.D.A.; Dos Santos, E.F.; de Brito, M.; da Silva, A.L.S.; et al. Cytokine Profiles Associated with Acute COVID-19 and Long COVID-19 Syndrome. Front. Cell. Infect. Microbiol. 2022, 12, 922422. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Castañeda, A.; Lu, P.; Geraghty, A.C.; Song, E.; Lee, M.H.; Wood, J.; Yalçın, B.; Taylor, K.R.; Dutton, S.; Acosta-Alvarez, L.; et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. bioRxiv 2022. [Google Scholar] [CrossRef]
- Venkataramani, V.; Winkler, F. Cognitive Deficits in Long COVID-19. New Engl. J. Med. 2022, 387, 1813–1815. [Google Scholar] [CrossRef]
- da Silva, R.; de Sarges, K.M.L.; Cantanhede, M.H.D.; da Costa, F.P.; Dos Santos, E.F.; Rodrigues, F.B.B.; de Nazaré do Socorro de Almeida Viana, M.; de Meira Leite, M.; da Silva, A.L.S.; de Brito, M.T.M.; et al. Thrombophilia and Immune-Related Genetic Markers in Long COVID. Viruses 2023, 15, 885. [Google Scholar] [CrossRef]
- Hornig, M.; Montoya, J.G.; Klimas, N.G.; Levine, S.; Felsenstein, D.; Bateman, L.; Peterson, D.L.; Gottschalk, C.G.; Schultz, A.F.; Che, X.; et al. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci. Adv. 2015, 1, e1400121. [Google Scholar] [CrossRef]
- Glynne, P.; Tahmasebi, N.; Gant, V.; Gupta, R. Long COVID following mild SARS-CoV-2 infection: Characteristic T cell alterations and response to antihistamines. J. Investig. Med. 2022, 70, 61–67. [Google Scholar] [CrossRef]
- Cheung, C.C.L.; Goh, D.; Lim, X.; Tien, T.Z.; Lim, J.C.T.; Lee, J.N.; Tan, B.; Tay, Z.E.A.; Wan, W.Y.; Chen, E.X.; et al. Residual SARS-CoV-2 viral antigens detected in GI and hepatic tissues from five recovered patients with COVID-19. Gut 2022, 71, 226–229. [Google Scholar] [CrossRef]
- Gaebler, C.; Wang, Z.; Lorenzi, J.C.C.; Muecksch, F.; Finkin, S.; Tokuyama, M.; Cho, A.; Jankovic, M.; Schaefer-Babajew, D.; Oliveira, T.Y.; et al. Evolution of antibody immunity to SARS-CoV-2. Nature 2021, 591, 639–644. [Google Scholar] [CrossRef]
- Sigal, G.B.; Novak, T.; Mathew, A.; Chou, J.; Zhang, Y.; Manjula, N.; Bathala, P.; Joe, J.; Padmanabhan, N.; Romero, D.; et al. Measurement of Severe Acute Respiratory Syndrome Coronavirus 2 Antigens in Plasma of Pediatric Patients with Acute Coronavirus Disease 2019 or Multisystem Inflammatory Syndrome in Children Using an Ultrasensitive and Quantitative Immunoassay. Clin. Infect. Dis. 2022, 75, 1351–1358. [Google Scholar] [CrossRef]
- Yang, C.; Zhao, H.; Espín, E.; Tebbutt, S.J. Association of SARS-CoV-2 infection and persistence with long COVID. Lancet. Respir. Med. 2023, 11, 504–506. [Google Scholar] [CrossRef]
- Barouch, D.H. COVID-19 Vaccines—Immunity, Variants, Boosters. New Engl. J. Med. 2022, 387, 1011–1020. [Google Scholar] [CrossRef]
- Banko, A.; Miljanovic, D.; Cirkovic, A. Systematic review with meta-analysis of active herpesvirus infections in patients with COVID-19: Old players on the new field. Int. J. Infect. Dis. 2023, 130, 108–125. [Google Scholar] [CrossRef]
- Manoharan, S.; Ying, L.Y. Epstein Barr Virus Reactivation during COVID-19 Hospitalization Significantly Increased Mortality/Death in SARS-CoV-2(+)/EBV(+) than SARS-CoV-2(+)/EBV(−) Patients: A Comparative Meta-Analysis. Int. J. Clin. Pract. 2023, 2023, 1068000. [Google Scholar] [CrossRef]
- Ruiz-Pablos, M.; Paiva, B.; Montero-Mateo, R.; Garcia, N.; Zabaleta, A. Epstein-Barr Virus and the Origin of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome. Front. Immunol. 2021, 12, 656797. [Google Scholar] [CrossRef]
- Apostolou, E.; Rizwan, M.; Moustardas, P.; Sjögren, P.; Bertilson, B.C.; Bragée, B.; Polo, O.; Rosén, A. Saliva antibody-fingerprint of reactivated latent viruses after mild/asymptomatic COVID-19 is unique in patients with myalgic-encephalomyelitis/chronic fatigue syndrome. Front. Immunol. 2022, 13, 949787. [Google Scholar] [CrossRef]
- Suurmond, J.; Diamond, B. Autoantibodies in systemic autoimmune diseases: Specificity and pathogenicity. J. Clin. Investig. 2015, 125, 2194–2202. [Google Scholar] [CrossRef]
- Knight, J.S.; Caricchio, R.; Casanova, J.L.; Combes, A.J.; Diamond, B.; Fox, S.E.; Hanauer, D.A.; James, J.A.; Kanthi, Y.; Ladd, V.; et al. The intersection of COVID-19 and autoimmunity. J. Clin. Investig. 2021, 131, e154886. [Google Scholar] [CrossRef]
- Wang, E.Y.; Mao, T.; Klein, J.; Dai, Y.; Huck, J.D.; Jaycox, J.R.; Liu, F.; Zhou, T.; Israelow, B.; Wong, P.; et al. Diverse functional autoantibodies in patients with COVID-19. Nature 2021, 595, 283–288. [Google Scholar] [CrossRef]
- Bastard, P.; Gervais, A.; Le Voyer, T.; Rosain, J.; Philippot, Q.; Manry, J.; Michailidis, E.; Hoffmann, H.H.; Eto, S.; Garcia-Prat, M.; et al. Autoantibodies neutralizing type I IFNs are present in ~4% of uninfected individuals over 70 years old and account for ~20% of COVID-19 deaths. Sci. Immunol. 2021, 6, eabl4340. [Google Scholar] [CrossRef] [PubMed]
- Manry, J.; Bastard, P.; Gervais, A.; Le Voyer, T.; Rosain, J.; Philippot, Q.; Michailidis, E.; Hoffmann, H.H.; Eto, S.; Garcia-Prat, M.; et al. The risk of COVID-19 death is much greater and age dependent with type I IFN autoantibodies. Proc. Natl. Acad. Sci. USA 2022, 119, e2200413119. [Google Scholar] [CrossRef] [PubMed]
- Eto, S.; Nukui, Y.; Tsumura, M.; Nakagama, Y.; Kashimada, K.; Mizoguchi, Y.; Utsumi, T.; Taniguchi, M.; Sakura, F.; Noma, K.; et al. Neutralizing Type I Interferon Autoantibodies in Japanese Patients with Severe COVID-19. Res. Sq. 2022. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Bastard, P.; Cobat, A.; Casanova, J.L. Human genetic and immunological determinants of critical COVID-19 pneumonia. Nature 2022, 603, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Peluso, M.J.; Thomas, I.J.; Munter, S.E.; Deeks, S.G.; Henrich, T.J. Lack of Antinuclear Antibodies in Convalescent Coronavirus Disease 2019 Patients with Persistent Symptoms. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2022, 74, 2083–2084. [Google Scholar] [CrossRef]
- Arthur, J.M.; Forrest, J.C.; Boehme, K.W.; Kennedy, J.L.; Owens, S.; Herzog, C.; Liu, J.; Harville, T.O. Development of ACE2 autoantibodies after SARS-CoV-2 infection. PLoS ONE 2021, 16, e0257016. [Google Scholar] [CrossRef]
- Fogarty, H.; Townsend, L.; Morrin, H.; Ahmad, A.; Comerford, C.; Karampini, E.; Englert, H.; Byrne, M.; Bergin, C.; O’Sullivan, J.M.; et al. Persistent endotheliopathy in the pathogenesis of long COVID syndrome. J. Thromb. Haemost. JTH 2021, 19, 2546–2553. [Google Scholar] [CrossRef]
- Jarrott, B.; Head, R.; Pringle, K.G.; Lumbers, E.R.; Martin, J.H. “LONG COVID”-A hypothesis for understanding the biological basis and pharmacological treatment strategy. Pharmacol. Res. Perspect. 2022, 10, e00911. [Google Scholar] [CrossRef]
- Fan, B.E.; Wong, S.W.; Sum, C.L.L.; Lim, G.H.; Leung, B.P.; Tan, C.W.; Ramanathan, K.; Dalan, R.; Cheung, C.; Lim, X.R.; et al. Hypercoagulability, endotheliopathy, and inflammation approximating 1 year after recovery: Assessing the long-term outcomes in COVID-19 patients. Am. J. Hematol. 2022, 97, 915–923. [Google Scholar] [CrossRef]
- Kell, D.B.; Pretorius, E. The potential role of ischaemia-reperfusion injury in chronic, relapsing diseases such as rheumatoid arthritis, Long COVID, and ME/CFS: Evidence, mechanisms, and therapeutic implications. Biochem. J. 2022, 479, 1653–1708. [Google Scholar] [CrossRef]
- Pretorius, E.; Venter, C.; Laubscher, G.J.; Kotze, M.J.; Oladejo, S.O.; Watson, L.R.; Rajaratnam, K.; Watson, B.W.; Kell, D.B. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC). Cardiovasc. Diabetol. 2022, 21, 148. [Google Scholar] [CrossRef]
- Du, W.N.; Zhang, Y.; Yu, Y.; Zhang, R.M. D-dimer levels is associated with severe COVID-19 infections: A meta-analysis. Int. J. Clin. Pract. 2021, 75, e14031. [Google Scholar] [CrossRef]
- Rushworth, R.L.; Torpy, D.J.; Falhammar, H. Adrenal Crisis. New Engl. J. Med. 2019, 381, 852–861. [Google Scholar] [CrossRef]
- Demitrack, M.A.; Dale, J.K.; Straus, S.E.; Laue, L.; Listwak, S.J.; Kruesi, M.J.; Chrousos, G.P.; Gold, P.W. Evidence for impaired activation of the hypothalamic-pituitary-adrenal axis in patients with chronic fatigue syndrome. J. Clin. Endocrinol. Metab. 1991, 73, 1224–1234. [Google Scholar] [CrossRef]
- Lin, Y.J.; Ko, Y.C.; Chow, L.H.; Hsiao, F.J.; Liu, H.Y.; Wang, P.N.; Chen, W.T. Salivary cortisol is associated with cognitive changes in patients with fibromyalgia. Sci. Rep. 2021, 11, 1311. [Google Scholar] [CrossRef]
- Leow, M.K.; Kwek, D.S.; Ng, A.W.; Ong, K.C.; Kaw, G.J.; Lee, L.S. Hypocortisolism in survivors of severe acute respiratory syndrome (SARS). Clin. Endocrinol. 2005, 63, 197–202. [Google Scholar] [CrossRef]
- Choy, K.W. Cortisol concentrations and mortality from COVID-19. Lancet. Diabetes Endocrinol. 2020, 8, 808. [Google Scholar] [CrossRef]
- Kedor, C.; Freitag, H.; Meyer-Arndt, L.; Wittke, K.; Hanitsch, L.G.; Zoller, T.; Steinbeis, F.; Haffke, M.; Rudolf, G.; Heidecker, B.; et al. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat. Commun. 2022, 13, 5104. [Google Scholar] [CrossRef]
- Bonilla, H.; Quach, T.C.; Tiwari, A.; Bonilla, A.E.; Miglis, M.; Yang, P.C.; Eggert, L.E.; Sharifi, H.; Horomanski, A.; Subramanian, A.; et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome is common in post-acute sequelae of SARS-CoV-2 infection (PASC): Results from a post-COVID-19 multidisciplinary clinic. Front. Neurol. 2023, 14, 1090747. [Google Scholar] [CrossRef]
- Dalamaga, M.; Christodoulatos, G.S. Adiponectin as a biomarker linking obesity and adiposopathy to hematologic malignancies. Horm. Mol. Biol. Clin. Investig. 2015, 23, 5–20. [Google Scholar] [CrossRef]
- Dalamaga, M.; Karmaniolas, K.; Chamberland, J.; Nikolaidou, A.; Lekka, A.; Dionyssiou-Asteriou, A.; Mantzoros, C.S. Higher fetuin-A, lower adiponectin and free leptin levels mediate effects of excess body weight on insulin resistance and risk for myelodysplastic syndrome. Metabolism 2013, 62, 1830–1839. [Google Scholar] [CrossRef] [PubMed]
- Dalamaga, M.; Crotty, B.H.; Fargnoli, J.; Papadavid, E.; Lekka, A.; Triantafilli, M.; Karmaniolas, K.; Migdalis, I.; Dionyssiou-Asteriou, A.; Mantzoros, C.S. B-cell chronic lymphocytic leukemia risk in association with serum leptin and adiponectin: A case-control study in Greece. Cancer Causes Control. CCC 2010, 21, 1451–1459. [Google Scholar] [CrossRef] [PubMed]
- Dalamaga, M.; Karmaniolas, K.; Nikolaidou, A.; Chamberland, J.; Hsi, A.; Dionyssiou-Asteriou, A.; Mantzoros, C.S. Adiponectin and resistin are associated with risk for myelodysplastic syndrome, independently from the insulin-like growth factor-I (IGF-I) system. Eur. J. Cancer 2008, 44, 1744–1753. [Google Scholar] [CrossRef] [PubMed]
- Dalamaga, M.; Nikolaidou, A.; Karmaniolas, K.; Hsi, A.; Chamberland, J.; Dionyssiou-Asteriou, A.; Mantzoros, C.S. Circulating adiponectin and leptin in relation to myelodysplastic syndrome: A case-control study. Oncology 2007, 73, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Marouga, A.; Dalamaga, M.; Kastania, A.N.; Antonakos, G.; Thrasyvoulides, A.; Kontelia, G.; Dimas, C.; Vlahakos, D.V. Correlates of serum resistin in elderly, non-diabetic patients with chronic kidney disease. Clin. Lab. 2013, 59, 1121–1128. [Google Scholar] [CrossRef]
- Papadavid, E.; Gazi, S.; Dalamaga, M.; Stavrianeas, N.; Ntelis, V. Palmoplantar and scalp psoriasis occurring during anti-tumour necrosis factor-alpha therapy: A case series of four patients and guidelines for management. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 380–382. [Google Scholar] [CrossRef]
- Papadavid, E.; Vlami, K.; Dalamaga, M.; Giatrakou, S.; Theodoropoulos, K.; Gyftopoulos, S.; Stavrianeas, N.; Papiris, S.; Rigopoulos, D. Sleep apnea as a comorbidity in obese psoriasis patients: A cross-sectional study. Do psoriasis characteristics and metabolic parameters play a role? J. Eur. Acad. Dermatol. Venereol. 2013, 27, 820–826. [Google Scholar] [CrossRef]
- Papadavid, E.; Dalamaga, M.; Vlami, K.; Koumaki, D.; Gyftopoulos, S.; Christodoulatos, G.S.; Papiris, S.; Rigopoulos, D. Psoriasis is associated with risk of obstructive sleep apnea independently from metabolic parameters and other comorbidities: A large hospital-based case-control study. Sleep Breath. Schlaf Atm. 2017, 21, 949–958. [Google Scholar] [CrossRef]
- Pavlidou, A.; Dalamaga, M.; Kroupis, C.; Konstantoudakis, G.; Belimezi, M.; Athanasas, G.; Dimas, K. Survivin isoforms and clinicopathological characteristics in colorectal adenocarcinomas using real-time qPCR. World J. Gastroenterol. 2011, 17, 1614–1621. [Google Scholar] [CrossRef]
- Dalamaga, M.; Karmaniolas, K.; Lekka, A.; Antonakos, G.; Thrasyvoulides, A.; Papadavid, E.; Spanos, N.; Dionyssiou-Asteriou, A. Platelet markers correlate with glycemic indices in diabetic, but not diabetic-myelodysplastic patients with normal platelet count. Dis. Mrk. 2010, 29, 55–61. [Google Scholar] [CrossRef]
- Bramante, C.T.; Buse, J.B.; Liebovitz, D.; Nicklas, J.; Puskarich, M.A.; Cohen, K.; Belani, H.; Anderson, B.; Huling, J.D.; Tignanelli, C.; et al. Outpatient treatment of COVID-19 with metformin, ivermectin, and fluvoxamine and the development of Long COVID over 10-month follow-up. medRxiv 2022. [Google Scholar] [CrossRef]
- Dissanayake, H.A.; de Silva, N.L.; Sumanatilleke, M.; de Silva, S.D.N.; Gamage, K.K.K.; Dematapitiya, C.; Kuruppu, D.C.; Ranasinghe, P.; Pathmanathan, S.; Katulanda, P. Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-analysis. J. Clin. Endocrinol. Metab. 2022, 107, 1484–1502. [Google Scholar] [CrossRef]
- Akbar, M.R.; Wibowo, A.; Pranata, R.; Setiabudiawan, B. Corrigendum: Low Serum 25-hydroxyvitamin D (Vitamin D) Level Is Associated with Susceptibility to COVID-19, Severity, and Mortality: A Systematic Review and Meta-Analysis. Front. Nutr. 2021, 8, 754539. [Google Scholar] [CrossRef]
- Bilezikian, J.P.; Bikle, D.; Hewison, M.; Lazaretti-Castro, M.; Formenti, A.M.; Gupta, A.; Madhavan, M.V.; Nair, N.; Babalyan, V.; Hutchings, N.; et al. MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19. Eur. J. Endocrinol. 2020, 183, R133–r147. [Google Scholar] [CrossRef]
- Moukayed, M. A Narrative Review on the Potential Role of Vitamin D(3) in the Prevention, Protection, and Disease Mitigation of Acute and Long COVID-19. Curr. Nutr. Rep. 2023, 12, 215–223. [Google Scholar] [CrossRef]
- Bader-Larsen, K.S.; Larson, E.A.; Dalamaga, M.; Magkos, F. A Narrative Review of the Safety of Anti-COVID-19 Nutraceuticals for Patients with Cancer. Cancers 2021, 13, 6094. [Google Scholar] [CrossRef]
- Garcia, M.; Seelaender, M.; Sotiropoulos, A.; Coletti, D.; Lancha, A.H., Jr. Vitamin D, muscle recovery, sarcopenia, cachexia, and muscle atrophy. Nutrition 2019, 60, 66–69. [Google Scholar] [CrossRef]
- Gáll, Z.; Székely, O. Role of Vitamin D in Cognitive Dysfunction: New Molecular Concepts and Discrepancies between Animal and Human Findings. Nutrients 2021, 13, 3672. [Google Scholar] [CrossRef]
- Dalamaga, M.; Muscogiuri, G.; Paganitsa, G.; Parvouleskou, G.; Syriou, V.; Karagkoynis, P.; Stratigou, T.; Vallianou, N.; Christodoulatos, G.S.; Karampela, I.; et al. Adherence to the Mediterranean diet is an independent predictor of circulating vitamin D levels in normal weight and non-smoker adults: An observational cross-sectional study. Int. J. Food Sci. Nutr. 2021, 72, 848–860. [Google Scholar] [CrossRef]
- Jolliffe, D.A.; Camargo, C.A., Jr.; Sluyter, J.D.; Aglipay, M.; Aloia, J.F.; Ganmaa, D.; Bergman, P.; Bischoff-Ferrari, H.A.; Borzutzky, A.; Damsgaard, C.T.; et al. Vitamin D supplementation to prevent acute respiratory infections: A systematic review and meta-analysis of aggregate data from randomised controlled trials. Lancet. Diabetes Endocrinol. 2021, 9, 276–292. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Rainsbury, J.; Kimball, S.M. Vitamin D Supplementation, Serum 25(OH)D Concentrations and Cardiovascular Disease Risk Factors: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2018, 5, 87. [Google Scholar] [CrossRef] [PubMed]
- Karampela, I.; Sakelliou, A.; Vallianou, N.; Christodoulatos, G.S.; Magkos, F.; Dalamaga, M. Vitamin D and Obesity: Current Evidence and Controversies. Curr. Obes. Rep. 2021, 10, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.L.; Sales, L.P.; Santos, M.D.; Caparbo, V.F.; Murai, I.H.; Pereira, R.M.R. Persistent or new symptoms 1 year after a single high dose of vitamin D(3) in patients with moderate to severe COVID-19. Front. Nutr. 2022, 9, 979667. [Google Scholar] [CrossRef] [PubMed]
- Galluzzo, V.; Ciciarello, F.; Tosato, M.; Zazzara, M.B.; Pais, C.; Savera, G.; Calvani, R.; Picca, A.; Marzetti, E.; Landi, F. Association between vitamin D status and physical performance in COVID-19 survivors: Results from the Gemelli against COVID-19 post-acute care project. Mech. Ageing Dev. 2022, 205, 111684. [Google Scholar] [CrossRef]
- Bruzzone, C.; Conde, R.; Embade, N.; Mato, J.M.; Millet, O. Metabolomics as a powerful tool for diagnostic, pronostic and drug intervention analysis in COVID-19. Front. Mol. Biosci. 2023, 10, 1111482. [Google Scholar] [CrossRef]
- König, R.S.; Albrich, W.C.; Kahlert, C.R.; Bahr, L.S.; Löber, U.; Vernazza, P.; Scheibenbogen, C.; Forslund, S.K. The Gut Microbiome in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS). Front. Immunol. 2021, 12, 628741. [Google Scholar] [CrossRef]
- Vallianou, N.G.; Kounatidis, D.; Tsilingiris, D.; Panagopoulos, F.; Christodoulatos, G.S.; Evangelopoulos, A.; Karampela, I.; Dalamaga, M. The Role of Next-Generation Probiotics in Obesity and Obesity-Associated Disorders: Current Knowledge and Future Perspectives. Int. J. Mol. Sci. 2023, 24, 6755. [Google Scholar] [CrossRef]
- Papavasileiou, G.; Tsilingiris, D.; Spyrou, N.; Vallianou, N.G.; Karampela, I.; Magkos, F.; Dalamaga, M. Obesity and main urologic cancers: Current systematic evidence, novel biological mechanisms, perspectives and challenges. Semin. Cancer Biol. 2023, 91, 70–98. [Google Scholar] [CrossRef]
- Yeoh, Y.K.; Zuo, T.; Lui, G.C.; Zhang, F.; Liu, Q.; Li, A.Y.; Chung, A.C.; Cheung, C.P.; Tso, E.Y.; Fung, K.S.; et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 2021, 70, 698–706. [Google Scholar] [CrossRef]
- Zhang, F.; Lau, R.I.; Liu, Q.; Su, Q.; Chan, F.K.L.; Ng, S.C. Gut microbiota in COVID-19: Key microbial changes, potential mechanisms and clinical applications. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 323–337. [Google Scholar] [CrossRef]
- de Almeida, V.M.; Engel, D.; Ricci, M.F.; Cruz, C.S.; Lopes, I.S.; Alves, D.A.; Auriol, M.D.; Magalhães, J.; Zuccoli, G.S.; Smith, B.J.; et al. Gut microbiota from patients with mild COVID-19 cause alterations in mice that resemble post-COVID syndrome. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Dalamaga, M.; Karmaniolas, K.; Arsenis, G.; Pantelaki, M.; Daskalopoulou, K.; Papadavid, E.; Migdalis, I. Cedecea lapagei bacteremia following cement-related chemical burn injury. Burns 2008, 34, 1205–1207. [Google Scholar] [CrossRef]
- Papadavid, E.; Dalamaga, M.; Kapniari, I.; Pantelidaki, E.; Papageorgiou, S.; Pappa, V.; Tsirigotis, P.; Dervenoulas, I.; Stavrianeas, N.; Rigopoulos, D. Lobomycosis: A case from Southeastern Europe and review of the literature. J. Dermatol. Case Rep. 2012, 6, 65–69. [Google Scholar] [CrossRef]
- Giron, L.B.; Peluso, M.J.; Ding, J.; Kenny, G.; Zilberstein, N.F.; Koshy, J.; Hong, K.Y.; Rasmussen, H.; Miller, G.E.; Bishehsari, F.; et al. Markers of fungal translocation are elevated during post-acute sequelae of SARS-CoV-2 and induce NF-κB signaling. JCI Insight 2022, 7, e160989. [Google Scholar] [CrossRef]
- Domingues, R.B.; Leite, F.; Senne, C. Cerebrospinal fluid analysis in patients with COVID-19-associated central nervous system manifestations: A systematic review. Arq. De Neuro-Psiquiatr. 2022, 80, 296–305. [Google Scholar] [CrossRef]
- Perrin, P.; Collongues, N.; Baloglu, S.; Bedo, D.; Bassand, X.; Lavaux, T.; Gautier-Vargas, G.; Keller, N.; Kremer, S.; Fafi-Kremer, S.; et al. Cytokine release syndrome-associated encephalopathy in patients with COVID-19. Eur. J. Neurol. 2021, 28, 248–258. [Google Scholar] [CrossRef]
- Chaumont, H.; Kaczorowski, F.; San-Galli, A.; Michel, P.P.; Tressières, B.; Roze, E.; Quadrio, I.; Lannuzel, A. Cerebrospinal fluid biomarkers in SARS-CoV-2 patients with acute neurological syndromes. Rev. Neurol. 2023, 179, 208–217. [Google Scholar] [CrossRef]
- Guillot, F.; Garcia, A.; Salou, M.; Brouard, S.; Laplaud, D.A.; Nicot, A.B. Transcript analysis of laser capture microdissected white matter astrocytes and higher phenol sulfotransferase 1A1 expression during autoimmune neuroinflammation. J. Neuroinflammation 2015, 12, 130. [Google Scholar] [CrossRef]
- Peluso, M.J.; Sans, H.M.; Forman, C.A.; Nylander, A.N.; Ho, H.E.; Lu, S.; Goldberg, S.A.; Hoh, R.; Tai, V.; Munter, S.E.; et al. Plasma Markers of Neurologic Injury and Inflammation in People with Self-Reported Neurologic Postacute Sequelae of SARS-CoV-2 Infection. Neurol. (R) Neuroimmunol. Neuroinflamm. 2022, 9, e200003. [Google Scholar] [CrossRef]
- Magdy, R.; Eid, R.A.; Fathy, W.; Abdel-Aziz, M.M.; Ibrahim, R.E.; Yehia, A.; Sheemy, M.S.; Hussein, M. Characteristics and Risk Factors of Persistent Neuropathic Pain in Recovered COVID-19 Patients. Pain Med. 2022, 23, 774–781. [Google Scholar] [CrossRef]
- Peluso, M.J.; Deeks, S.G.; Mustapic, M.; Kapogiannis, D.; Henrich, T.J.; Lu, S.; Goldberg, S.A.; Hoh, R.; Chen, J.Y.; Martinez, E.O.; et al. SARS-CoV-2 and Mitochondrial Proteins in Neural-Derived Exosomes of COVID-19. Ann. Neurol. 2022, 91, 772–781. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Tang, L.; Ma, Y.; Li, Y.; Zhang, D.; Li, Q.; Mei, H.; Hu, Y. Immunological Profiling of COVID-19 Patients with Pulmonary Sequelae. mBio 2021, 12, e0159921. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Apostolo, D.; D’Onghia, D.; Tonello, S.; Minisini, R.; Baricich, A.; Gramaglia, C.; Patrucco, F.; Zeppegno, P.; Acquaviva, A.; Balbo, P.E.; et al. Decreased Gas6 and sAxl Plasma Levels Are Associated with Hair Loss in COVID-19 Survivors. Int. J. Mol. Sci. 2023, 24, 6257. [Google Scholar] [CrossRef] [PubMed]
- Haslam, A.; Olivier, T.; Prasad, V. The definition of long COVID used in interventional studies. Eur. J. Clin. Investig. 2023, e13989. [Google Scholar] [CrossRef]
- Fawzy, N.A.; Abou Shaar, B.; Taha, R.M.; Arabi, T.Z.; Sabbah, B.N.; Alkodaymi, M.S.; Omrani, O.A.; Makhzoum, T.; Almahfoudh, N.E.; Al-Hammad, Q.A.; et al. A systematic review of trials currently investigating therapeutic modalities for post-acute COVID-19 syndrome and registered on WHO International Clinical Trials Platform. Clin. Microbiol. Infect. 2023, 29, 570–577. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Sivan, M.; Delaney, B.; Evans, R.; Milne, R. Long COVID-an update for primary care. BMJ 2022, 378, e072117. [Google Scholar] [CrossRef]
- Chadda, K.R.; Blakey, E.E.; Huang, C.L.; Jeevaratnam, K. Long COVID-19 and Postural Orthostatic Tachycardia Syndrome—Is Dysautonomia to Be Blamed? Front. Cardiovasc. Med. 2022, 9, 860198. [Google Scholar] [CrossRef]
- Geng, L.N.; Bonilla, H.F.; Shafer, R.W.; Miglis, M.G.; Yang, P.C. The Use of Nirmatrelvir-ritonavir in a Case of Breakthrough Long COVID. Explor. Res. Hypothesis Med. 2023. [Google Scholar] [CrossRef]
- Xie, Y.; Choi, T.; Al-Aly, Z. Association of Treatment with Nirmatrelvir and the Risk of Post-COVID-19 Condition. JAMA Intern. Med. 2023, 183, 554–564. [Google Scholar] [CrossRef]
- Bajema, K.L.; Berry, K.; Streja, E.; Rajeevan, N.; Li, Y.; Yan, L.; Cunningham, F.; Hynes, D.M.; Rowneki, M.; Bohnert, A.; et al. Effectiveness of COVID-19 treatment with nirmatrelvir-ritonavir or molnupiravir among U.S. Veterans: Target trial emulation studies with one-month and six-month outcomes. medRxiv 2022. [Google Scholar] [CrossRef]
- Durstenfeld, M.S.; Peluso, M.J.; Lin, F.; Peyser, N.D.; Isasi, C.; Carton, T.W.; Henrich, T.J.; Deeks, S.G.; Olgin, J.E.; Pletcher, M.J.; et al. Association of Nirmatrelvir/Ritonavir Treatment with Long COVID Symptoms in an Online Cohort of Non-Hospitalized Individuals Experiencing Breakthrough SARS-CoV-2 Infection in the Omicron Era. medRxiv 2023. [Google Scholar] [CrossRef]
- Parthasarathy, H.; Tandel, D.; Siddiqui, A.H.; Harshan, K.H. Metformin suppresses SARS-CoV-2 in cell culture. Virus Res. 2022, 323, 199010. [Google Scholar] [CrossRef]
- Ventura-López, C.; Cervantes-Luevano, K.; Aguirre-Sánchez, J.S.; Flores-Caballero, J.C.; Alvarez-Delgado, C.; Bernaldez-Sarabia, J.; Sánchez-Campos, N.; Lugo-Sánchez, L.A.; Rodríguez-Vázquez, I.C.; Sander-Padilla, J.G.; et al. Treatment with metformin glycinate reduces SARS-CoV-2 viral load: An in vitro model and randomized, double-blind, Phase IIb clinical trial. Biomed. Pharmacother. Biomed. Pharmacother. 2022, 152, 113223. [Google Scholar] [CrossRef]
- Daou, N.; Viader, A.; Cokol, M.; Nitzel, A.; Chakravarthy, M.V.; Afeyan, R.; Tramontin, T.; Marukian, S.; Hamill, M.J. A novel, multitargeted endogenous metabolic modulator composition impacts metabolism, inflammation, and fibrosis in nonalcoholic steatohepatitis-relevant primary human cell models. Sci. Rep. 2021, 11, 11861. [Google Scholar] [CrossRef]
- Finnigan, L.E.M.; Cassar, M.P.; Koziel, M.J.; Pradines, J.; Lamlum, H.; Azer, K.; Kirby, D.; Montgomery, H.; Neubauer, S.; Valkovič, L.; et al. Efficacy and tolerability of an endogenous metabolic modulator (AXA1125) in fatigue-predominant long COVID: A single-centre, double-blind, randomised controlled phase 2a pilot study. eClinicalMedicine 2023, 59, 101946. [Google Scholar] [CrossRef]
- Available online: https://clinicaltrials.gov/ (accessed on 15 May 2023).
- Kritis, P.; Karampela, I.; Kokoris, S.; Dalamaga, M. The combination of bromelain and curcumin as an immune-boosting nutraceutical in the prevention of severe COVID-19. Metab. Open 2020, 8, 100066. [Google Scholar] [CrossRef]
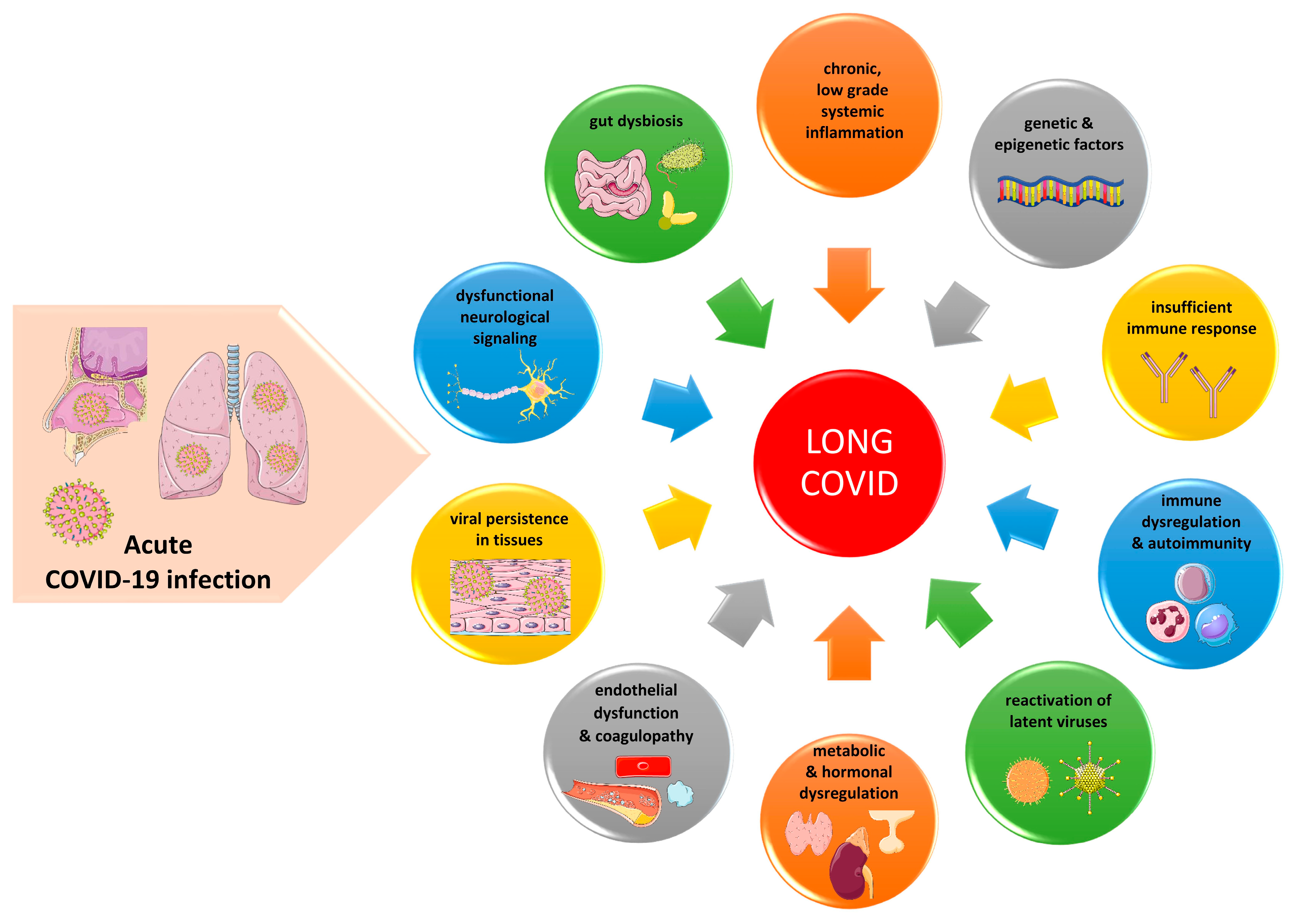
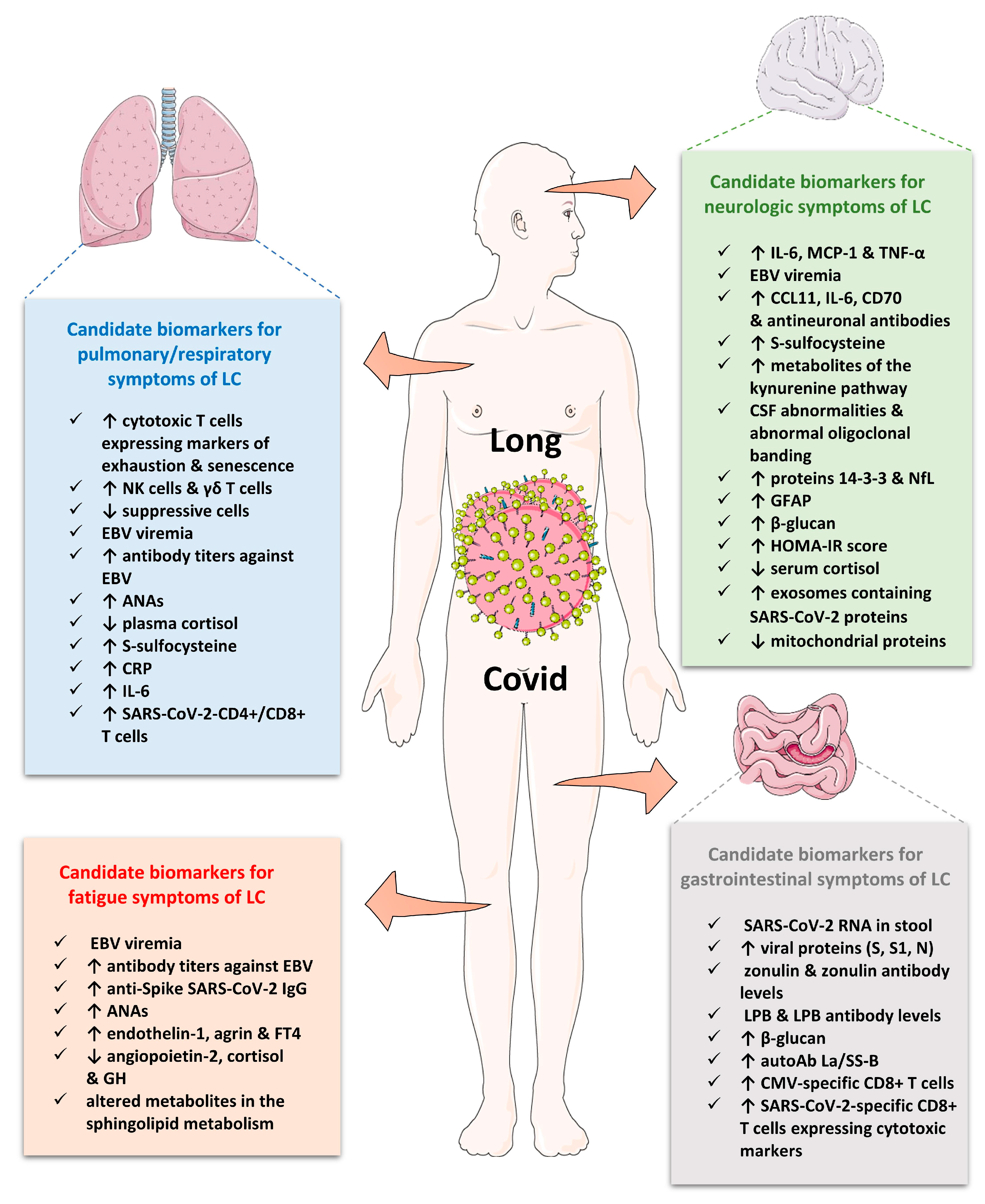
| Source | Used Terms | Definition |
|---|---|---|
| World Health Organization (WHO) [12] | Post-COVID condition or long COVID | The continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection lasting for at least 2 months with no other explanation. |
| National Institute for Clinical Excellence (NICE) [13] | Long COVID, ongoing symptomatic COVID-19, post-COVID | Long COVID: Signs and symptoms that continue or develop after acute COVID-19. It includes both ongoing symptomatic COVID-19 and post-COVID. Ongoing symptomatic COVID-19: signs and symptoms of COVID-19 lasting from 4 weeks up to 12 weeks. Post-COVID: Signs and symptoms that develop during or after COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis. This diagnosis may be considered before 12 weeks while the possibility of an alternative underlying disease is also being assessed. |
| Centers for Disease Control and Prevention [14] | Long COVID or post-COVID conditions | Signs, symptoms and conditions that continue or develop (at least 4 weeks) after initial COVID-19 infection. |
| Robert Koch Institute [15] | Long COVID, post-COVID condition or post-COVID syndrome | Longer-term health impairments following a SARS-CoV-2 infection that are present beyond the acute phase of the sickness phase of four weeks. Post-COVID condition/post-COVID syndrome: the presence of symptoms for at least 12 weeks after the acute infection or symptoms that appear anew after this period and cannot be explained otherwise. |
| Government of Canada [16] | Post-COVID condition or long COVID | Symptoms of COVID-19 persisting for more than 12 weeks after the infection. |
| Main Characteristics | Acute Severe COVID-19 | Long COVID |
|---|---|---|
| Age | Older age | ↑ % of diagnoses between the ages of 36 and 50 years |
| Gender | More frequent in males | More frequent in females |
| Predisposing factors and comorbidities | - Older age, obesity, T2DM, CVD, asthma or chronic lung disease, sickle cell disease, immunocompromised patients, hematologic malignancies, chronic kidney disease, patients under immunosuppressive treatments - Racial and ethnic minority groups - People with low income - Unvaccinated individuals | - Obesity, T2DM, connective tissue disorders, allergic rhinitis, ADHD - More frequent in Black and Hispanic Americans - People with a low income - Poor rest in the early period after COVID-19 - ↑ risk after severe COVID-19 - Most cases involve non-hospitalized patients with a mild acute COVID-19 |
| Laboratory findings and biomarkers | Lymphopenia, ↑ CRP, ↑ neutrophils, ↑ IL-6, ↑ IL-10, ↑ D-dimer, ↑ LDH, ↑ ferritin | The following factors are present in certain patients: ↑ IL-6, ↑ CRP, ↑ D-dimer, detectable SARS-CoV-2 RNA in stool or gut mucosa, biomarkers of EBV reactivation, anti-IFN-α2 or anti-IFN-λAbs, ↑ ET-1 and ↓ Ang-2, ↓ cortisol, metabolites of mitochondrial dysfunction, ↑ % of CSF abnormalities and ↑ biomarkers of neuronal damage |
| CVD features | Pulmonary embolism, deep vein thrombosis, AMI, heart failure | Chest pain, palpitations, myocarditis, cardiac impairment, POTS |
| Neurologic features | Headache, ischemic stroke, ataxia, seizures, anosmia, ageusia | Brain fog, fatigue, musculoskeletal pain, cognitive impairment, paresthesia, sleep disorder, dizziness, memory loss, dysautonomia, tinnitus |
| Pulmonary features | Cough, dyspnea, hypoxia, bilateral lung infiltrates | Cough, dyspnea, abnormal gas exchange, ground glass lung |
| Gastrointestinal features | Abdominal pain, nausea, vomiting, diarrhea, T1DM,↑ transaminases | Abdominal pain, nausea |
| Endocrine abnormalities | ↑ T1DM, ↑ T2DM thyroiditis | Diabetes, hypocortisolism |
| Dermatologic findings | Skin rashes (maculopapular, chilblain-like, urticarial, vesicular, livedoid and petechial lesions), hair loss | Most commonly alopecia, various skin rashes |
| Renal manifestations | Acute Kidney Injury, Acute Tubular Necrosis | ↓ eGFR |
| Manifestations from the reproductive system | Menstrual irregularities, ↑ urinary frequency and nocturia | Menstrual irregularities, ↑ premenstrual symptoms, erectile dysfunction, ↓ sperm count |
| General Laboratory Work-Up |
|---|
| Complete blood count |
| Erythrocyte sedimentation rate |
| General biochemical tests: glucose, HbA1c, urea, creatinine, electrolytes (sodium, potassium, calcium, phosphate) |
| Indices of hepatic function: AST, ALT, γ-GT, ALP |
| CPK, ferritin, LDH |
| Indices of cardiac function: troponin, BNP or NT-proBNP |
| Indices of thyroid function: TSH, fT4 |
| Indices of coagulation and fibrinolysis: D-dimer, fibrinogen, PT, aPTT |
| Indices of inflammation: CRP, IL-6 |
| Vitamins: 25-OHD, B12 |
| Autoantibodies and complements: RF, anti-CCP, ANA, ENA, ACA, autoantibodies against central nervous system antigens, C3, C4 |
| Imaging and Other Function Tests |
| High-resolution Chest Computed Tomography |
| Computed Tomography Pulmonary Angiogram (CTPA) |
| Pulmonary function tests (spirometry, diffusion capacity, lung volumes) |
| Pulse oxymetry |
| Six-minute walk test (6MWT) |
| Electrocardiogram |
| Cardiac ultrasound |
| Cardiac magnetic resonance |
| Cardiopulmonary exercise testing (CPET) |
| Brain magnetic resonance |
| Questionnaires and Clinical Tests |
| Tilt table test for POTS or 10-Minute NASA Lean Test for orthostatic intolerance |
| Dyspnea scales (mMRC, NYHA) |
| Questionnaire SBQ-LC |
| Questionnaires for anxiety: BAI, HAM-A, GAD-7 |
| Questionnaires for depression: BDI, HAM-D, PHQ-2,-9 |
| Some Promising Tests |
| Cortisol/four-point salivary cortisol test |
| IgG, IgA, IgM |
| Natural killer cell function tests |
| Panels for reactivated herpesviruses (EBV, CMV, VZV, HHV-6) |
| SARS-CoV-2 RNA in stool or gut mucosa |
| Endothelin-1 and Angiopoietin-2 |
| Hyperpolarized gas magnetic resonance of the lungs |
| Study, Year | Study Design/Population | Main Findings | Utility |
|---|---|---|---|
| Biomarkers of systemic inflammation | |||
| Yong, S.J. et al., 2023 [172] | Meta-analysis of 23 studies (14 prospective and 9 retrospective case control) with 18 meta-analyzed biomarkers | - ↑ CRP, D-dimer, LDH and leukocytes in LC patients than those without LC - ↑ lymphocytes and IL-6 in LC patients than those without LC - ↑ IL-8 in LC than healthy controls | - Diagnostic utility in LC; however, the effects are small; - ↑ D-dimer, LDH and lymphocytes in patients with organ abnormalities - ↑ IL-6 in patients with symptom persistence - ↑ LDH, leucocytes and NT-pro-BNP in patients with duration of symptoms < 6 months - ↑ D-dimer in patients with duration of symptoms ≥ 6 months |
| Yin, J.X. et al., 2022 [173] | Meta-analysis of 22 case-control observational studies | - ↑ IL-6 levels in LC patients than controls - ↑ IL-6 levels in LC patients than those with non-post acute sequelae of severe COVID-19 - ↑ IL-6 levels in patients with acute COVID-19 than patients with LC | - IL-6 may predict LC; - IL-6 may characterize an early stage of LC. |
| Lopez-Leon, S. et al., 2021 [20] | A total of 21 meta-analyses on the prevalence of long-term effects in LC, 15 studies, 47,910 patients (age: 17–87 years). | - ↑ CRP in 8% of patients (95% CI: 5–12) - ↑ ferritin in 8% of patients (95% CI: 4–14) - ↑ procalcitonin in 4% of patients (95% CI: 2–9) - ↑ IL-6 in 3% of patients (95% CI: 1–7) | Limited evidence for systemic inflammation after approximately 4 months post-viral-infection. |
| Immune profiling in long COVID | |||
| Klein, J. et al., 2022 [174] | A total of 220 participants (101 LC, 41 CC, 41 HC and 37 HCW) at >400-days post-infection, cross-sectional study | LC is characterized by the following: ↑ non-classical monocytes; ↑ activated B cells; ↑ double-negative B cells; ↑ exhausted T cells; ↑ IL-4/IL-6 secreting CD4 T cells; ↓ conventional DC1; ↓ central memory CD4 T cells. | The integration of immune phenotyping data into machine learning models may identify distinguishing features in the classification of LC. |
| Haunhorst, S. et al., 2022 [175] | Scoping review of three studies examining Tregs in LC | - Galán M et al. [176] found a 2.5X ↑ Tregs in LC compared to subjects that recovered completely. - Utrero-Rico et al. [177] ↓ Tregs in LC compared to subjects that recovered completely - ↓ Tregs in LC compared to seronegative controls [178] | No firm conclusions can be drawn about Treg alterations in LC. |
| Phetsouphanh, C. et al., 2022 [96] | LC group (n = 31) and asymptomatic matched controls (MC) (n = 31) compared to individuals infected with common cold coronavirus (HCoV) (n = 25) and unexposed healthy donors (n = 13) | ↑ activated innate immune cells, ↓ naive T and B cells ↑ expression of type I IFN (IFN-β) and type III IFN (IFN-λ1) that remained persistently high at 8 months after infection | |
| Patterson, B.K. et al., 2021 [178] | Case-control and longitudinal study, 121 cases with LC, 29 healthy controls, 26 cases with mild–moderate COVID-19, 48 cases with severe COVID-19 | -↑ B cells in LC compared to HC - ↑ inflammatory monocytes CD14+, CD16+ and CCR5+ compared to HC - ↓CD4+ and CD8+ T cells expressing PD-1 (exhausted lymphocytes) and T-reg in LC compared to HC | - ↑ inflammatory monocytes and ↓ exhausted lymphocytes detected in patients who later developed LC (predictive biomarkers) - ↑ inflammatory monocytes and ↑ exhausted lymphocytes in the convalescence period of LC |
| Biomarkers reflecting SARS-CoV-2 persistence | |||
| Swank, Z. et al., 2022 [179] | A total of 63 individuals previously infected with SARS-CoV-2, 37 of whom were diagnosed with LC | ↑ circulating spike protein in LC cases but not in convalescent controls up to 12 months | SARS-CoV-2 viral reservoirs may persist in the body. |
| Natarajan, A. et al., 2022 [180] | A total of 113 individuals with mild to moderate COVID-19, longitudinal study | - SARS-CoV-2 RNA in the feces at 4 months after diagnosis (12.7%) - SARS-CoV-2 RNA in the feces at 7 months after diagnosis (3.8%) | GI symptoms (abdominal pain, nausea, vomiting) are related to fecal shedding of SARS-CoV-2 RNA. |
| Stein, S.R. et al., 2022 [98] | Autopsies on 44 patients who died with COVID-19 | - Persistent SARS-CoV-2 RNA in multiple anatomic sites, including throughout the brain, as late as 230 days - A proportion of ≥50% of late cases had persistent RNA in the myocardium and lymph nodes from the head and neck and from the thorax, sciatic nerve, ocular tissue and in all sampled regions of the CNS, except the dura mater. | SARS-CoV-2 can cause systemic infection and persist in the body for months in certain patients. |
| Tejerina, F. et al., 2022 [181] | Cohort of 29 patients who reported persistent symptoms at least 4 w after COVID-19 | - A total of 45% had positive plasma RT-PCR results -A total of 51% were positive in at least one RT-PCR sample (plasma, urine or stool) | Potential systemic viral persistence associated with persistent symptoms |
| Zollner, A. et al., 2022 [182] | Cohort of 46 patients with IBD 219 days (range, 94–257) after confirmed COVID-19 | - SARS-CoV-2 RNA in the gut mucosa ∼7 months after mild acute COVID-19 in 69.5% - Nucleocapsid protein persisted in 52.2% of patients in gut epithelium and CD8+ T cells - No detectable viral antigens in stool | - Viral persistence markers associated with symptoms of LC |
| Yonker, L.M. et al., 2021 [183] | A total of 19 children with MIS-C, 26 with acute COVID-19 and 55 controls. | - A total of 89% of cases with MIS-C had GI symptoms versus 27% of children with acute COVID-19 - Detectable viral loads in the stool (1.5 × 102 to 2.5 × 107 RNA copies/mL) in the majority of cases - ↑ plasma zonulin and LBP compared to controls - ↑ SARS-CoV-2 spike, S1 and nucleocapsid antigens compared to controls | - Prolonged exposure to SARS-CoV-2 in the GI tract of children with MIS -Loss of mucosal barrier integrity - SARS-CoV-2 antigenemia may trigger the hyperinflammatory responses defining MIS-C |
| Humoral and cellular response against SARS-CoV-2 in long COVID | |||
| Klein, J. et al., 2022 [174] | A total of 220 participants (101 LC, 41 CC, 41 HC and 37 HCW) at >400-days post-infection; cross-sectional study | ↑ IgG against spike and S1 in LC compared to vaccination-matched controls | - Potential predictive biomarker of LC |
| Files, J.K. et al., 2021 [184] | A longitudinal study of 50 cases with COVID-19: - Total of 20 with persistent symptoms (30–208 days); - Total of 30 with symptom resolution within 20 days. | The following were found in patients with persistent symptoms: - ↑ IgG avidity to SARS-CoV-2 spike protein; - sustained T cell response magnitudes; - ↑ antigen-specific CD4+ T cell responses against spike (late phase); - ↑ antigen-specific CD8+ T cell populations. | ↑ T cell response magnitude in individuals with prolonged symptoms |
| García-Abellán, J. et al., 2021 [101] | Prospective, longitudinal study of 146 hospitalized COVID-19 patients | ↓ peak IgG against spike-associated with LC symptoms at 6 months | - Potential predictive biomarker of LC |
| Augustin, M. et al., 2021 [185] | A longitudinal prospective cohort study of 958 non-hospitalized patients with confirmed COVID-19 | ↓ baseline levels of IgG against S1 domain of the spike associated with long-term symptoms | - Potential predictive biomarker of LC |
| Blomberg, B. et al., 2021 [186] | A prospective cohort study of 312 patients (247 home-isolated and 65 hospitalized) | - ↑ IgG against spike protein and ↑ microneutralizing antibody titers detected after 2 months independently associated with both persistent fatigue and total number of symptoms at 6 months | - Increased antibody titers is a predictive biomarker of LC symptoms |
| Peluso, M.J. et al., 2021 [187] | A prospective cohort study of 70 individuals with PCR-confirmed COVID-19 | - No significant differences in early and late (1 and 4 months) antibody levels (IgG against SARS-CoV-2 Spike, RBD and two preparations of the N protein) between cases with and without persistent symptoms - No differences in T cell responses at initial time point between cases with and without persistent symptoms - ↓ CD8+ T cells expressing CD107a against N peptide in cases with LC -↓ N-specific interferon-γ-producing CD8+ T cells in cases with LC | |
| Biomarkers reflecting reactivation of latent viruses | |||
| Peluso, M.J. et al., 2023 [188] | A cohort of 280 adults with prior COVID-19 | - ↑ early antigen-diffuse EBV IgG positivity associated with fatigue at 4 m - ↑ IgG against EBNA associated with fatigue and neurocognitive dysfunction, at 4 m after infection | Reactivation of EBV is associated with fatigue and cognitive dysfunction in LC |
| Klein, J. et al., 2022 [174] | A total of 220 participants (101 LC, 41 CC, 41 HC and 37 HCW) at >400-days post-infection; cross-sectional study | ↑ titers of anti-EBV antibodies, even though overall seroprevalence is not different from HC or CC | Altered humoral responses to distinct herpesviruses in LC as a predictive biomarker |
| Zubchenko, S. et al., 2022 [189] | A total of 88 patients with LC | - EBV reactivation in 42.6% - HHV6 reactivation in 25.0% - EBV plus HHV6 reactivation in 32.4% | Reactivation was associated with ↑ slight fever temperature, headache, psycho-neurological disorders, pulmonary abnormalities and myalgia, liver enzymes, CRP and D-dimer and ↓ cellular immune response |
| Su, Y. et al., 2022 [190] | A cohort of 309 COVID-19 patients from initial diagnosis to convalescence (2–3 months later), 457 HC | - EBV viremia at T1 was associated with LC (fatigue and respiratory symptoms) at 3 m post-infection. | - EBV viremia may be a predictive biomarker of LC. |
| Gold, J.E. et al., 2021 [191] | A cohort of randomly 185 surveyed COVID-19 patients, 56 developed LC | - ↑ EBV early antigen-diffuse IgG or ↑EBV viral capsid antigen (VCA) IgM in 66.7% of LC versus 10% of controls | - EBV reactivation may be a predictive biomarker of LC. |
| Biomarkers reflecting autoimmunity | |||
| Muri, J. et al., 2023 [192] | A cohort of 71 COVID-19 convalescent patients at month 6 (on average) after disease onset, 23 HC | - IgG antibodies against chemokines CCL21, CXCL13 and CXCL16 at month 6 distinguished LC from no LC groups. - Levels of CCL21, CXCL13 and CXCL16 predicted the absence of persistent symptoms with 77.8% accuracy. | - Ab against specific chemokines were associated with a favorable disease outcome and negatively correlated with the development of LC at 1-year post-infection. |
| Bodansky, A. et al., 2023 [193] | A cohort of 121 individuals with LC, 64 with prior COVID-19 and full recovery, and 57 pre-COVID controls. | - Significant differences in autoreactivity between COVID-19 patients and pre-COVID controls - No patterns of autoreactivity that separated individuals with LC from individuals fully recovered from COVID-19 | Absence of LC-specific autoreactivities |
| Son, K. et al., 2023 [194] | A cohort of 106 convalescent COVID-19 patients with varying acute phase severities at 3-, 6- and 12-months post-recovery, 22 HCs and 34 with other respiratory infections | - Abs to U1-snRNP and anti-SS-B/La were both positively associated with persistent symptoms of fatigue and dyspnea. - Pro-inflammatory cytokines such as TNF-α and CRP predicted ↑ ANAs at 12 months. | Persistently positive ANAs at 12-months post-COVID are associated with persisting symptoms and inflammation in a subset of COVID-19 survivors. |
| Franke, C. et al., 2023 [195] | A prospective study of 50 patients with reported cognitive problems | - A total of 92% had normal routine CSF parameters. - A total of 52% had antineuronal Abs (n = 9 in serum only, n = 3 in CSF only and n = 14 in both, including those against myelin, Yo, Ma2/Ta, GAD65 and the NMDA receptor along with a variety of undetermined epitopes on brain sections). | An abnormal cognitive status is associated with antineuronal Abs in CSF. |
| Peluso, M.J. et al., 2022 [196] | A prospective study of 215 participants with convalescent COVID-19 tested over 394 time points, including 121 people with LC | - An amount of 2 out of 215 had IFN-α2-specific autoantibodies across all sample time points. | No detectable anti-IFN-α2 antibodies in LC |
| Klein, J. et al., 2022 [174] | A total of 220 participants (101 LC, 41 CC, 41 HC and 37 HCW), cross-sectional study | No significant differences in the total number of autoantibody reactivities per participant across groups using REAP, a high throughput method for the measurement of Ab reactivity against >6000 extracellular and secreted human proteins | No specific autoAbs that could differentiate participants with LC from controls |
| Su, Y. et al., 2022 [190] | A cohort of 309 COVID-19 patients from initial diagnosis to convalescence (2–3 months later), 457 HC Determination of an auto-Ab panel: anti-IFN-α2 and 5 antinuclear auto-Abs (Ro/SS-A, La/SS-B, U1-snRNP, Jo-1 and P1) at clinical diagnosis and convalescence | - Patients with autoAbs at convalescence (44%) already exhibited mature (class-switched) auto-Abs as early as at diagnosis (56%). - Inverse correlations between SARS-CoV-2 IgGs (class-switched) and autoAbs | - IFN-α2 autoAbs uniquely associated with respiratory symptoms of LC - ↑ multiple autoAbs at convalescence are associated with GI symptoms and the sputum production of LC. |
| Rojas, M. et al., 2022 [197] | Case-control study: 100 patients with LC with a median post-COVID time of 219 (IQR: 143 to 258) days, 30 prepandemic HC | - Latent autoimmunity in 83% of patients - Polyautoimmunity in 62% of patients - Anti-IFN autoAbs in 5–10% of patients - Anti-SARS-CoV-2 IgG correlated with autoAbs | - IgG anti-IFN-λ Abs were associated with the persistence of respiratory symptoms. - Latent autoimmunity correlates with an Ab response against SARS-CoV-2. |
| Endothelial or vascular biomarkers | |||
| Patel, M.A. et al., 2022 [198] | A case-control study of 23 LC patients, one- to six-months post-infection, and 23 ward COVID patients, 23 ICU COVID patients and 23 HCs | - Angiogenesis markers (ANG-1 and P-SEL) had excellent sensitivity and specificity for LC status (AUC = 1.00) among 16 blood biomarkers of vascular transformation. - ANG-1 levels were associated with female sex and a lack of disease interventions at follow-up | - Diagnostic utility and classification of LC status (accuracy: 96%) |
| Haffke, M. et al., 2022 [199] | A case-control study of 30 LC patients with persistent fatigue and exertion intolerance (14 with 14 post-COVID ME/CFS) and 15 age- and sex matched seronegative HCs | - ↑ ET-1 concentration in both ME/CFS and LC patients compared to HCs and post-convalescent controls - ↓ Ang-2 in both LC patients and post-convalescent controls compared to HCs | - LC patients with fatigue present ↑ ET-1 and ↓ Ang-2 - Ang-2 levels exclusively in LC could be a differentiation biomarker betweenPCS and ME/CFS |
| Tong, M. et al., 2022 [200] | A cross-sectional study of 345 COVID-19 (39% had LC symptoms) and 119 age and gender-matched HCWs | - No significant differences in vascular biomarkers (serum levels of VCAM-1, ICAM-1, P-selectin) between COVID-19 survivors and controls | |
| Biomarkers of coagulation and fibrinolysis | |||
| Yong, S.J. et al., 2023 [172] | Meta-analysis of 23 studies (14 prospective and 9 retrospective case control) with 18 meta-analyzed biomarkers | - ↑ D-dimer, CRP, LDH and leukocytes in LC patients than those without LC - ↑ lymphocytes and IL-6 in LC patients than those without LC - ↑ IL-8 in LC than healthy controls | - Diagnostic utility in LC; however, the effects are small - ↑ D-dimer, LDH and lymphocytes in patients with organ abnormalities - ↑ D-dimer in patients with duration of symptoms ≥ 6 months |
| Constantinescu-Bercu, A. et al., 2023 [201] | A cohort of 21 patients with LC with a median time of 23 months of follow-up and controls | - ↑ platelet binding on both collagen and anti-VWF A3 in patients with LC compared with controls, which positively correlated with VWF and VWF(Ag):ADAMTS13 ratio and inversely correlated with ADAMTS13 activity | - LC is a prothrombotic state |
| Di Gennaro, L. et al., 2022 [202] | A case-control study of 75 children with previously confirmed COVID-19 in a pediatric post-COVID unit ≥ 8 weeks after the initial infection | - ↑ D-dimer levels in LC children compared to children that had fully recovered at the 8–12 weeks (p = 0.04) and 12 week follow-ups or more (p = 0.05) and in children with three or more symptoms at 12 weeks (p = 0.002). - No significant differences in other coagulation factors between LC children and controls | Abnormal D-dimer levels in children with LC and more symptoms |
| Kruger et al., 2022 [203] | A case-control study of 99 LC patients and 29 HCs. | - ↑ platelet factor 4 (PF4), VWF and α-2 antiplasmin (α-2-AP) in LC - ↓ plasma kallikrein in LC - Significant platelet hyperactivation was noted in LC. | Failed fibrinolytic system in LC |
| Pretorius, E. et al., 2021 [204] | A cross-sectional study of 11 patients with LC, 13 HCs, 15 with COVID-19 (before treatment) and 10 with T2DM | - Microclots in both acute COVID-19 and LC plasma samples are resistant to fibrinolysis (compared to plasma from controls and T2DM). - ↑ SAA in LC than controls - Platelets from LC patients are hyperactivated. - In the digested clots, ↑ α2 antiplasmin, plasminogen, coagulation factor XIII A chain, vWF, fibrinogen alpha chain, C7 and CRP in LC than controls | Abnormal fibrinolysis and coagulopathy in LC |
| Hormonal and metabolic biomarkers | |||
| di Filippo, L. et al., 2023 [205] | - Total of 50 cases with LC and 50 non-LC subjects matched on a 1:1 basis followed for 6 months. - Follow-up case-control study | - Concentrations of 20.1 vs. 23.2 ng/mL (p = 0.03) in cases with LC vs. controls at follow-up - ↓ 25(OH)D in cases with neurocognitive symptoms at follow-up - ↓ 25(OH)D levels at follow-up were the only significant variable in LC | - ↓ 25(OH)D in LC and particularly in those with brain fog - 25(OH)D levels should be evaluated in cases with COVID-19 after hospital discharge. |
| Mohamed Hussein, A.A.R. et al., 2022 [206] | - A total of 219 post-COVID cases - A cross-sectional, single-center study of all cases attending a post-COVID follow-up clinic | - A proportion of 84% had deficient vitamin D levels (<20 ng/dL). - A proportion of 11.4% had insufficient levels (20–30 ng/dL). - Only 4.9% had normal levels. | - ↑ prevalence of vitamin D deficiency - No association between vitamin D levels and post-COVID symptoms. |
| Su, Y. et al., 2022 [190] | A cohort of 309 COVID-19 patients from initial diagnosis to convalescence (2–3 months later), 457 HC | - ↓ cortisol and cortisone in patients with LC at convalescence - ↑ proteins associated with the negative regulation of the circadian sleep/wake cycle in patients with neurological symptoms | - Patients with respiratory symptoms at convalescence exhibited ↓ cortisol and cortisone. |
| Klein, J. et al., 2022 [174] | A total of 220 participants (101 LC, 41 CC, 41 HC and 37 HCW), cross-sectional study | ↓ serum cortisol in LC, ↑ in healthy (uninfected) controls, ↓ in convalescent controls and ↓↓ in cases with LC | - Serum cortisol was the most significant individual predictor of LC. |
| Sunada, N. et al., 2022 [207] | - A total of 186 patients with LC - Retrospective analysis | - ↓ serum GH and ↑ serum FT4 in patients with general fatigue - ↓cortisol in patients with dysosmia/dysgeusia -↑ serum TSH and ↓ ratio of FT4/TSH in initial severe LC cases | |
| Townsend, L. et al., 2021 [208] | A cohort of 149 patients at a median of 79 days after COVID-19 illness. | - Median vitamin D was 62 nmol/L, with 24% having levels of 30–49 nmol/L (insufficiency) and 9% with levels < 30 nmol/L (deficiency) | - No association between vitamin D and persistent fatigue or decreased exercise tolerance |
| Other proteins as biomarkers | |||
| The PHOSP-COVID Collaborative Group, 2022 [92] | A prospective, longitudinal cohort study: 2320 participants discharged from hospital; 807 (34.7%) participants completed 5-month and 1-year visits. | The plasma proteome data for 296 protein features is as follows: - ↑ of 13 proteins in the severe group of LC. | - ↑ IL-6 and CD70 in cognitive impairment cluster compared with the mild cluster |
| Captur, G. et al., 2022 [209] | A nested longitudinal proteomic case-control study of 156 healthcare workers | Differentially abundant proteins in HCW with persistent symptoms (>6 w): proteins with lipid, atherosclerosis and cholesterol metabolism pathways, complement and coagulation cascades, autophagy and lysosomal function | Potential predictive value for LC at the time of seroconversion |
| Metabolites as biomarkers | |||
| López-Hernández, Y. et al., 2023 [210] | A longitudinal retrospective analysis of COVID-19 patients (n = 22), LC patients (n = 25) and controls (n = 15) | - Fatigue (59%) and musculoskeletal issues (50%) were most relevant and persistent symptoms. - Sterols, bile acids, isoprenoids and fatty esters were affected in both COVID-19 and post-COVID patients. - ↑ species of phosphatidylcholines and sphingomyelins in LC compared to controls | - Dysregulation in sphingolipid metabolism could be associated with fatigue and muscular pain. |
| López-Hernández, Y. et al., 2023 [211] | A retrospective longitudinal analysis of 108 participants (HC, COVID-19 and LC patients) | - ↑ Lactic acid, lactate/pyruvate ratio, ornithine/citrulline ratio, sarcosine and arginine in LC - ↑ IL-17 in LC | - Mitochondrial dysfunction, redox state imbalance, impaired energy metabolism and chronic immune dysregulation in LC |
| Guntur, V.P. et al., 2022 [150] | Case-control study of 29 patients with LC, 16 CC and 30 HC | - ↑ free- and carnitine-conjugated mono-, poly- and highly unsaturated fatty acids and ↓ levels of mono-, di- and tricarboxylates, polyamines (spermine) and taurine in LC - Milder disturbances in fatty acid metabolism and ↑ spermine and taurine in recovered patients - Tryptophan depletion not normalized in LC | - Altered fatty acid metabolism and dysfunctional mitochondria-dependent lipid catabolism associated with mitochondrial dysfunction during exercise |
| Cysique, L.A. et al., 2022 [212] | A prospective study of 128 SARS-CoV-2-positive patients | - ↑ quinolinic acid, 3-hydroxyanthranilic acid and kynurenine were significantly associated with cognitive decline. | The kynurenine pathway metabolites are potential therapeutic targets for COVID-19-related cognitive impairment. |
| Microbiota alterations in long COVID | |||
| Zhang, D. et al., 2023 [213] | A prospective follow-up study of 187 recovered subjects; 84 reported LC symptoms at one-year after discharge; 32 HCs, 16S rRNA sequencing of stool samples | - Gut microbiota dysbiosis in symptomatic recovered patients - ↓ bacterial diversities in LC - ↓ relative abundance of SCFA-producing salutary symbionts, such as Eubacterium hallii, Subdoligranulum, Ruminococcus, Dorea, Coprococcus and Eubacterium_ventriosum groups in LC | - Gut microbiota dysbiosis in recovered patients at one-year after discharge - Gut microbiota dysbiosis in LC |
| Liu, Q. et al., 2022 [214] | A prospective study of 106 patients with a spectrum of COVID-19 severity from admission to 6 months and 68 non-COVID-19 controls | - ↑ Ruminococcus gnavus, Bacteroides vulgatus in LC - ↓ Faecalibacterium prausnitzii in LC - ↓ Butyrate-producing bacteria in LC | - Gut microbiota composition at admission was predictive of LC occurrence. |
| Cerebrospinal fluid biomarkers | |||
| Etter, M.M. et al., 2022 [142] | A cohort study of 40 neuro-COVID patients; 25 HCs and 25 non-MS inflammatory neurological disease controls | - CSF levels: ↑ pro-inflammatory proteins (TNFRSF9, IFN-γ) and ↓ anti-inflammatory mediators (TRANCE(RANKL), TRAIL) are predictive for LC. - plasma CLM-6, MCP-3 and ST1A1 may predict LC. | - Prediction of LC |
| Apple, A.C. et al., 2022 [215] | A case-control study of 22 participants with cognitive LC and 10 cognitive controls within the prospective study LIINC | - CSF abnormality in 77% of LC patients versus 0% of cognitive controls - Normal values for CSF white blood cells, glucose, calculated CSF/serum albumin ratio, IgG index, CSF IgG level and serum IgG level in all participants - Abnormal oligoclonal banding in 69% of LC patients versus 0% of cognitive controls | - ↑% of CSF abnormalities in patients with LC and cognitive impairment after mild COVID-19 |
| Guasp, M. et al., 2022 [216] | A prospective study of 60 hospitalized neuro-COVID patients, 25 of them with encephalopathy and 14 with encephalitis. A total of 46 serum samples from HCs and 24 CSF samples from subjects with mild subjective cognitive complaints. Follow-up: 18 months | - ↑ IL-18, IL-6 and IL-8 in both serum and CSF in neuro-COVID patients compared to HCs - ↑ 14-3-3, NfL, IL-18, IL-1RA and IL-8 are associated with acute COVID-19 severity - ↑ CSF 14-3-3 and NfL correlate with the degree of neurologic disability in the daily activities at 18 months | - ↑ CSF levels of neuronal damage biomarkers during the acute phase of COVID-19 are prognostic biomarkers of worse long-term clinical outcomes of patients. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsilingiris, D.; Vallianou, N.G.; Karampela, I.; Christodoulatos, G.S.; Papavasileiou, G.; Petropoulou, D.; Magkos, F.; Dalamaga, M. Laboratory Findings and Biomarkers in Long COVID: What Do We Know So Far? Insights into Epidemiology, Pathogenesis, Therapeutic Perspectives and Challenges. Int. J. Mol. Sci. 2023, 24, 10458. https://doi.org/10.3390/ijms241310458
Tsilingiris D, Vallianou NG, Karampela I, Christodoulatos GS, Papavasileiou G, Petropoulou D, Magkos F, Dalamaga M. Laboratory Findings and Biomarkers in Long COVID: What Do We Know So Far? Insights into Epidemiology, Pathogenesis, Therapeutic Perspectives and Challenges. International Journal of Molecular Sciences. 2023; 24(13):10458. https://doi.org/10.3390/ijms241310458
Chicago/Turabian StyleTsilingiris, Dimitrios, Natalia G. Vallianou, Irene Karampela, Gerasimos Socrates Christodoulatos, Georgios Papavasileiou, Dimitra Petropoulou, Faidon Magkos, and Maria Dalamaga. 2023. "Laboratory Findings and Biomarkers in Long COVID: What Do We Know So Far? Insights into Epidemiology, Pathogenesis, Therapeutic Perspectives and Challenges" International Journal of Molecular Sciences 24, no. 13: 10458. https://doi.org/10.3390/ijms241310458
APA StyleTsilingiris, D., Vallianou, N. G., Karampela, I., Christodoulatos, G. S., Papavasileiou, G., Petropoulou, D., Magkos, F., & Dalamaga, M. (2023). Laboratory Findings and Biomarkers in Long COVID: What Do We Know So Far? Insights into Epidemiology, Pathogenesis, Therapeutic Perspectives and Challenges. International Journal of Molecular Sciences, 24(13), 10458. https://doi.org/10.3390/ijms241310458










