Novel Antidiabetic Agents and Their Effects on Lipid Profile: A Single Shot for Several Cardiovascular Targets
Abstract
1. Introduction
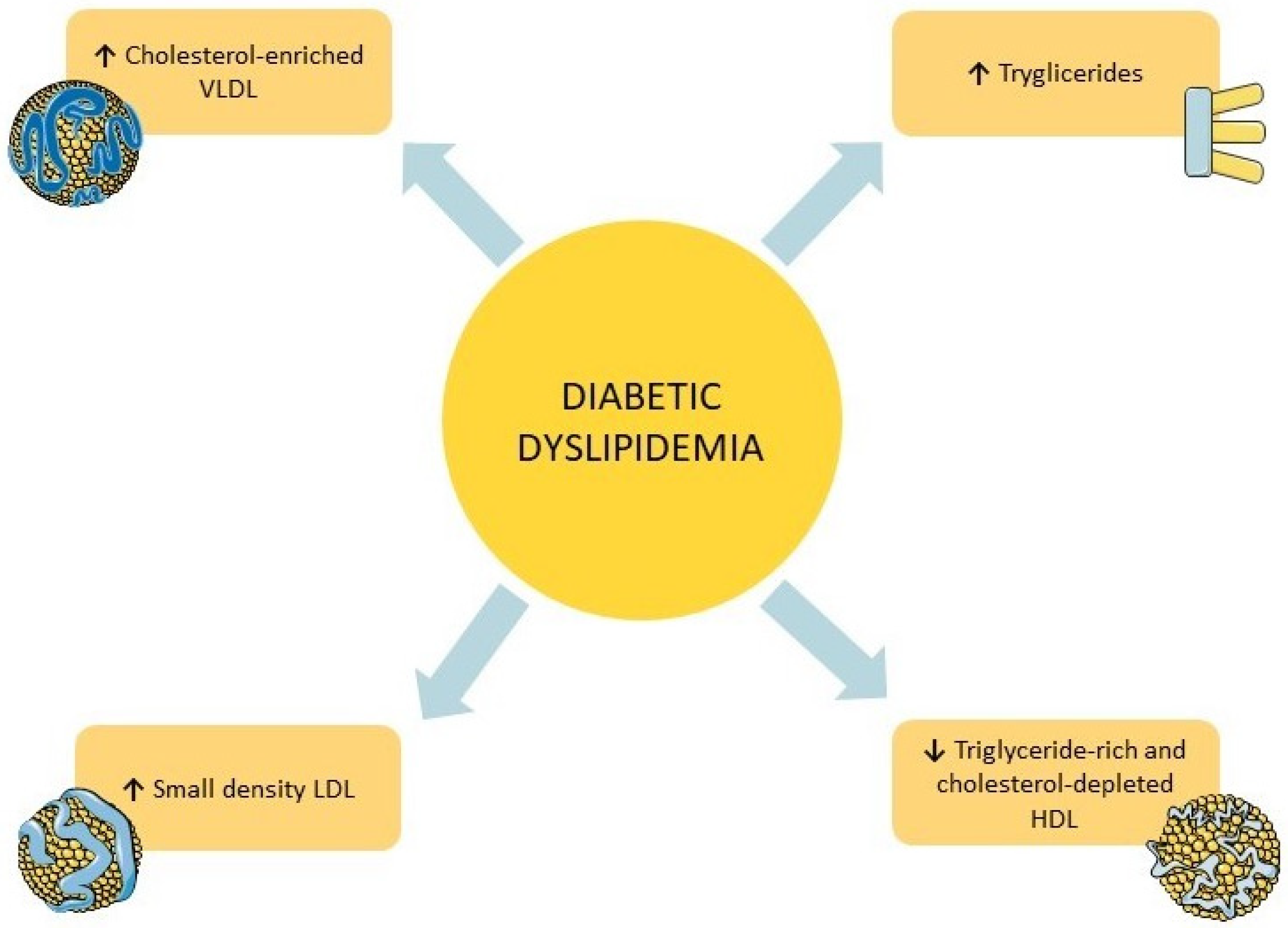
2. Diabetic Dyslipidemia
3. Novel Anti-Diabetic Drugs
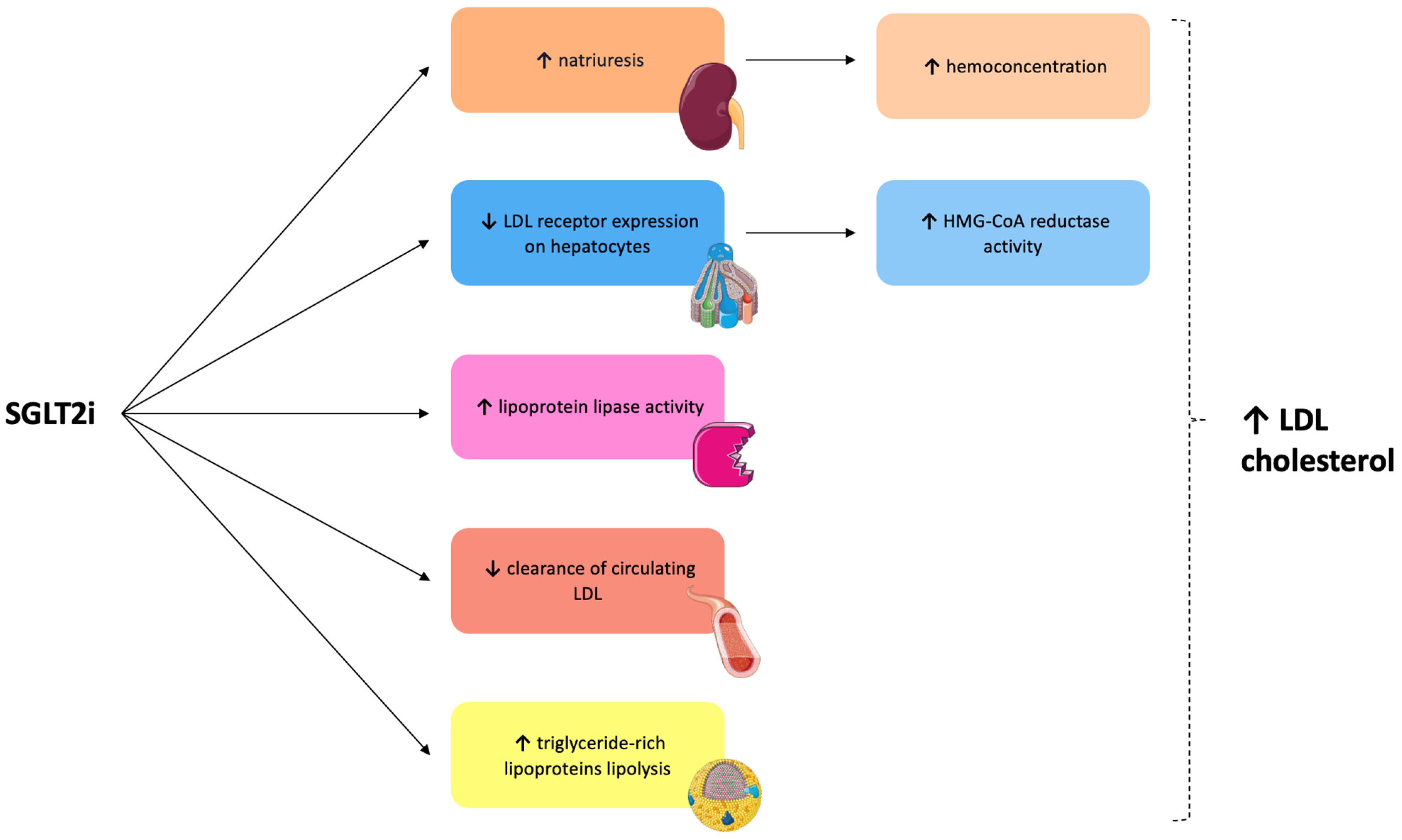
3.1. Sodium-Glucose Cotransporter 2 Inhibitors
3.1.1. Mechanisms of Action and Pre-Clinical Evidence
3.1.2. Clinical Evidence
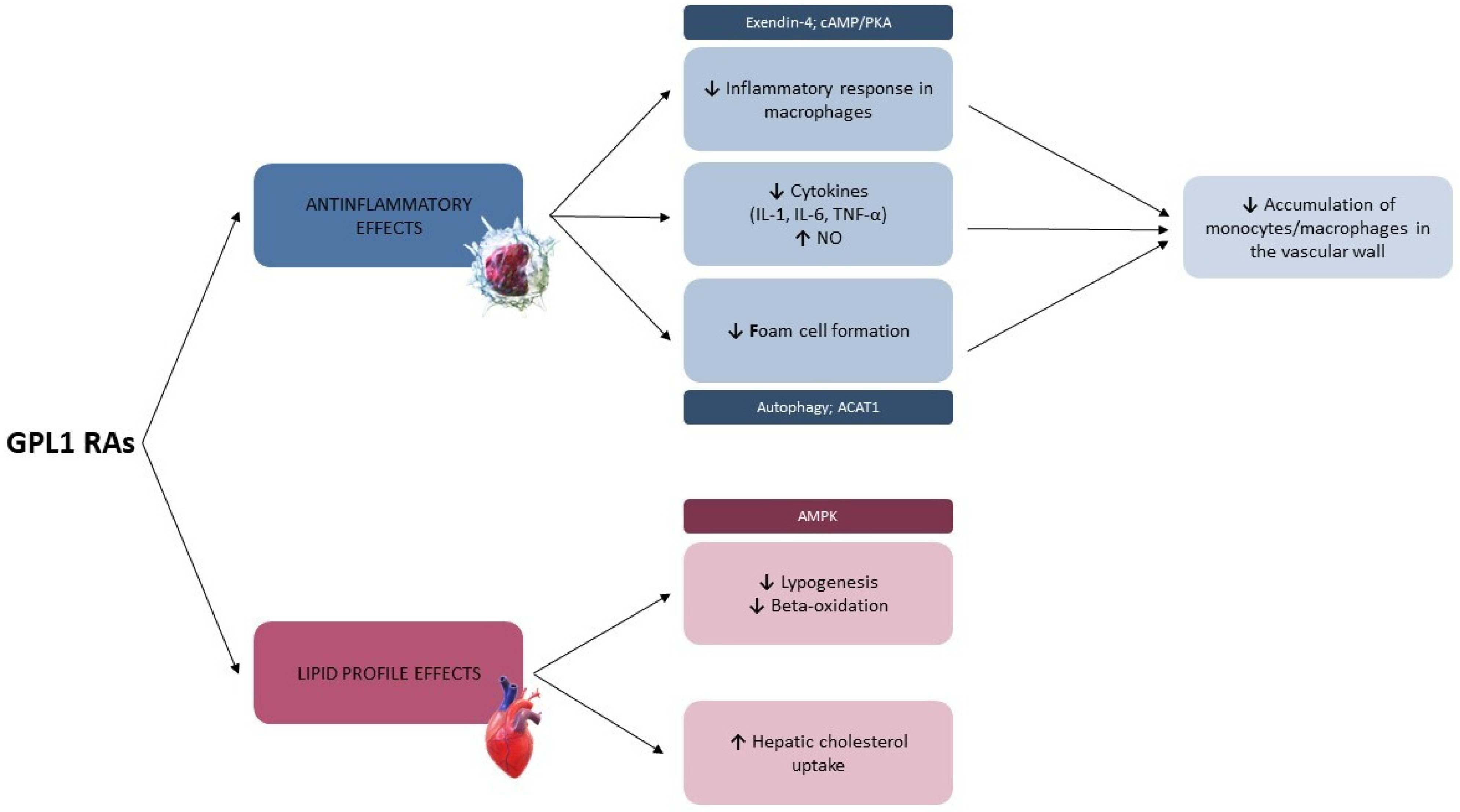
3.2. Glucagon-like Peptide-1 Receptor Agonists
3.2.1. Mechanisms of Action and Pre-Clinical Evidence
3.2.2. Clinical Evidence
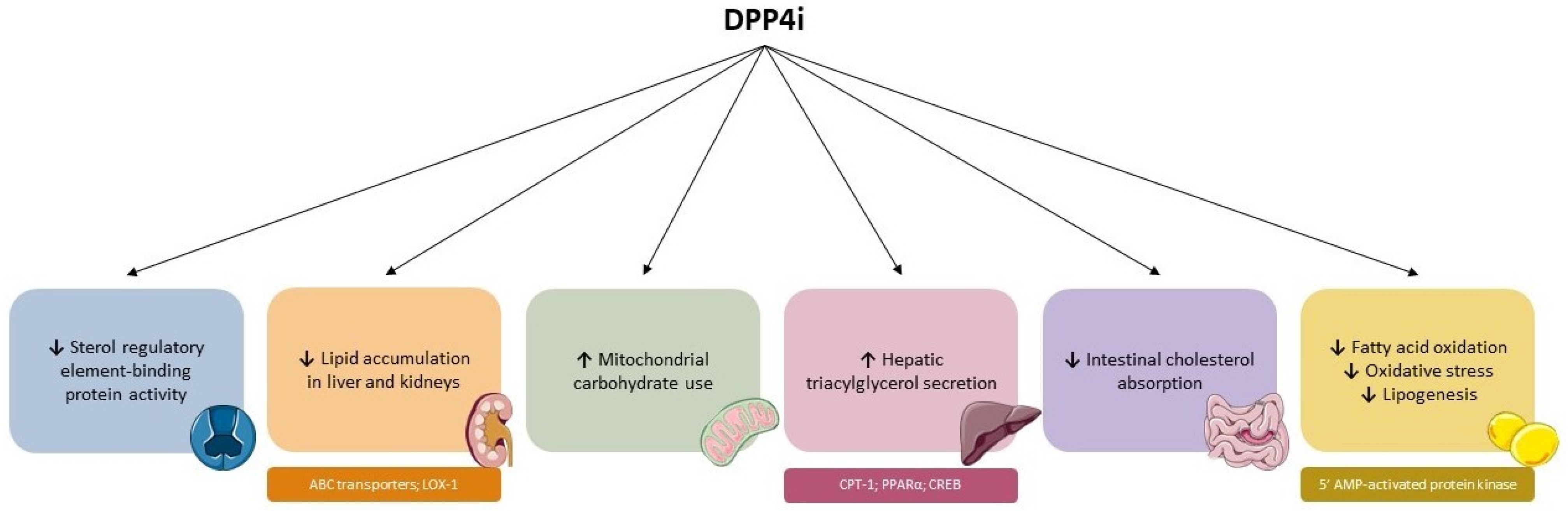
3.3. Dipeptidyl Peptidase-4 Inhibitors
3.3.1. Mechanisms of Action and Pre-Clinical Evidence
3.3.2. Clinical Evidence
4. Effects of Combination Therapy
5. Novel Cholesterol-Lowering Drugs
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef]
- Piccirillo, F.; Miano, N.; Goffredo, C.; Nusca, A.; Mangiacapra, F.; Khazrai, Y.M.; De Gara, L.; Ussia, G.P.; Grigioni, F. Impact of Mediterranean diet on metabolic and inflammatory status of patients with polyvascular atherosclerotic disease. Nutr. Metab. Cardiovasc. Dis. NMCD 2022, 32, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2022, 45, 2753–2786. [Google Scholar] [CrossRef] [PubMed]
- Gerstein, H.C.; Miller, M.E.; Byington, R.P.; Goff, D.C., Jr.; Bigger, J.T.; Buse, J.B.; Cushman, W.C.; Genuth, S.; Ismail-Beigi, F.; Grimm, R.H., Jr.; et al. Effects of intensive glucose lowering in type 2 diabetes. N. Engl. J. Med. 2008, 358, 2545–2559. [Google Scholar] [CrossRef] [PubMed]
- Nusca, A.; Bernardini, F.; Mangiacapra, F.; Maddaloni, E.; Melfi, R.; Ricottini, E.; Piccirillo, F.; Manfrini, S.; Ussia, G.P.; Grigioni, F. Ranolazine Improves Glycemic Variability and Endothelial Function in Patients with Diabetes and Chronic Coronary Syndromes: Results from an Experimental Study. J. Diabetes Res. 2021, 2021, 4952447. [Google Scholar] [CrossRef]
- Nusca, A.; Tuccinardi, D.; Albano, M.; Cavallaro, C.; Ricottini, E.; Manfrini, S.; Pozzilli, P.; Di Sciascio, G. Glycemic variability in the development of cardiovascular complications in diabetes. Diabetes/Metab. Res. Rev. 2018, 34, e3047. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Parhofer, K.G. Diabetic dyslipidemia. Metab. Clin. Exp. 2014, 63, 1469–1479. [Google Scholar] [CrossRef]
- Arca, M.; Pigna, G.; Favoccia, C. Mechanisms of diabetic dyslipidemia: Relevance for atherogenesis. Curr. Vasc. Pharmacol. 2012, 10, 684–686. [Google Scholar] [CrossRef]
- Secrest, M.H.; Udell, J.A.; Filion, K.B. The cardiovascular safety trials of DPP-4 inhibitors, GLP-1 agonists, and SGLT2 inhibitors. Trends Cardiovasc. Med. 2017, 27, 194–202. [Google Scholar] [CrossRef]
- Nusca, A.; Piccirillo, F.; Bernardini, F.; De Filippis, A.; Coletti, F.; Mangiacapra, F.; Ricottini, E.; Melfi, R.; Gallo, P.; Cammalleri, V.; et al. Glycaemic Control in Patients Undergoing Percutaneous Coronary Intervention: What Is the Role for the Novel Antidiabetic Agents? A Comprehensive Review of Basic Science and Clinical Data. Int. J. Mol. Sci. 2022, 23, 7261. [Google Scholar] [CrossRef]
- Patti, A.M.; Giglio, R.V.; Papanas, N.; Rizzo, M.; Rizvi, A.A. Future perspectives of the pharmacological management of diabetic dyslipidemia. Expert Rev. Clin. Pharmacol. 2019, 12, 129–143. [Google Scholar] [CrossRef]
- Gupta, M.; Tummala, R.; Ghosh, R.K.; Blumenthal, C.; Philip, K.; Bandyopadhyay, D.; Ventura, H.; Deedwania, P. An update on pharmacotherapies in diabetic dyslipidemia. Prog. Cardiovasc. Dis. 2019, 62, 334–341. [Google Scholar] [CrossRef]
- Bahiru, E.; Hsiao, R.; Phillipson, D.; Watson, K.E. Mechanisms and Treatment of Dyslipidemia in Diabetes. Curr. Cardiol. Rep. 2021, 23, 26. [Google Scholar] [CrossRef]
- Marušić, M.; Paić, M.; Knobloch, M.; Liberati Pršo, A.M. NAFLD, Insulin Resistance, and Diabetes Mellitus Type 2. Can. J. Gastroenterol. Hepatol. 2021, 2021, 6613827. [Google Scholar] [CrossRef] [PubMed]
- Morigny, P.; Houssier, M.; Mouisel, E.; Langin, D. Adipocyte lipolysis and insulin resistance. Biochimie 2016, 125, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Parhofer, K.G. Interaction between Glucose and Lipid Metabolism: More than Diabetic Dyslipidemia. Diabetes Metab. J. 2015, 39, 353–362. [Google Scholar] [CrossRef]
- Martin, S.S.; Khokhar, A.A.; May, H.T.; Kulkarni, K.R.; Blaha, M.J.; Joshi, P.H.; Toth, P.P.; Muhlestein, J.B.; Anderson, J.L.; Knight, S.; et al. HDL cholesterol subclasses, myocardial infarction, and mortality in secondary prevention: The Lipoprotein Investigators Collaborative. Eur. Heart J. 2015, 36, 22–30. [Google Scholar] [CrossRef]
- Steven, S.; Oelze, M.; Hanf, A.; Kröller-Schön, S.; Kashani, F.; Roohani, S.; Welschof, P.; Kopp, M.; Gödtel-Armbrust, U.; Xia, N.; et al. The SGLT2 inhibitor empagliflozin improves the primary diabetic complications in ZDF rats. Redox Biol. 2017, 13, 370–385. [Google Scholar] [CrossRef]
- Fonseca-Correa, J.I.; Correa-Rotter, R. Sodium-Glucose Cotransporter 2 Inhibitors Mechanisms of Action: A Review. Front. Med. 2021, 8, 777861. [Google Scholar] [CrossRef]
- Abdul-Ghani, M.A.; DeFronzo, R.A.; Norton, L. Novel hypothesis to explain why SGLT2 inhibitors inhibit only 30–50% of filtered glucose load in humans. Diabetes 2013, 62, 3324–3328. [Google Scholar] [CrossRef] [PubMed]
- Rahmoune, H.; Thompson, P.W.; Ward, J.M.; Smith, C.D.; Hong, G.; Brown, J. Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non-insulin-dependent diabetes. Diabetes 2005, 54, 3427–3434. [Google Scholar] [CrossRef] [PubMed]
- DeFronzo, R.A.; Hompesch, M.; Kasichayanula, S.; Liu, X.; Hong, Y.; Pfister, M.; Morrow, L.A.; Leslie, B.R.; Boulton, D.W.; Ching, A.; et al. Characterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetes. Diabetes Care 2013, 36, 3169–3176. [Google Scholar] [CrossRef] [PubMed]
- Ferrannini, E.; Muscelli, E.; Frascerra, S.; Baldi, S.; Mari, A.; Heise, T.; Broedl, U.C.; Woerle, H.J. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J. Clin. Investig. 2014, 124, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Filippas-Ntekouan, S.; Tsimihodimos, V.; Filippatos, T.; Dimitriou, T.; Elisaf, M. SGLT-2 inhibitors: Pharmacokinetics characteristics and effects on lipids. Expert Opin. Drug Metab. Toxicol. 2018, 14, 1113–1121. [Google Scholar] [CrossRef]
- Li, C.; Zhang, J.; Xue, M.; Li, X.; Han, F.; Liu, X.; Xu, L.; Lu, Y.; Cheng, Y.; Li, T.; et al. SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart. Cardiovasc. Diabetol. 2019, 18, 15. [Google Scholar] [CrossRef]
- Briand, F.; Mayoux, E.; Brousseau, E.; Burr, N.; Urbain, I.; Costard, C.; Mark, M.; Sulpice, T. Empagliflozin, via Switching Metabolism toward Lipid Utilization, Moderately Increases LDL Cholesterol Levels through Reduced LDL Catabolism. Diabetes 2016, 65, 2032–2038. [Google Scholar] [CrossRef]
- Yaribeygi, H.; Maleki, M.; Reiner, Ž.; Jamialahmadi, T.; Sahebkar, A. Mechanistic View on the Effects of SGLT2 Inhibitors on Lipid Metabolism in Diabetic Milieu. J. Clin. Med. 2022, 11, 6544. [Google Scholar] [CrossRef]
- Lauritsen, K.M.; Voigt, J.H.; Pedersen, S.B.; Hansen, T.K.; Møller, N.; Jessen, N.; Gormsen, L.C.; Søndergaard, E. Effects of SGLT2 inhibition on lipid transport in adipose tissue in type 2 diabetes. Endocr. Connect. 2022, 11, e210558. [Google Scholar] [CrossRef]
- Jojima, T.; Tomotsune, T.; Iijima, T.; Akimoto, K.; Suzuki, K.; Aso, Y. Empagliflozin (an SGLT2 inhibitor), alone or in combination with linagliptin (a DPP-4 inhibitor), prevents steatohepatitis in a novel mouse model of non-alcoholic steatohepatitis and diabetes. Diabetol. Metab. Syndr. 2016, 8, 45. [Google Scholar] [CrossRef]
- Osataphan, S.; Macchi, C.; Singhal, G.; Chimene-Weiss, J.; Sales, V.; Kozuka, C.; Dreyfuss, J.M.; Pan, H.; Tangcharoenpaisan, Y.; Morningstar, J.; et al. SGLT2 inhibition reprograms systemic metabolism via FGF21-dependent and -independent mechanisms. JCI Insight 2019, 4, e123130. [Google Scholar] [CrossRef]
- Hawley, S.A.; Ford, R.J.; Smith, B.K.; Gowans, G.J.; Mancini, S.J.; Pitt, R.D.; Day, E.A.; Salt, I.P.; Steinberg, G.R.; Hardie, D.G. The Na+/Glucose Cotransporter Inhibitor Canagliflozin Activates AMPK by Inhibiting Mitochondrial Function and Increasing Cellular AMP Levels. Diabetes 2016, 65, 2784–2794. [Google Scholar] [CrossRef]
- Xing, Y.J.; Liu, B.H.; Wan, S.J.; Cheng, Y.; Zhou, S.M.; Sun, Y.; Yao, X.M.; Hua, Q.; Meng, X.J.; Cheng, J.H.; et al. A SGLT2 Inhibitor Dapagliflozin Alleviates Diabetic Cardiomyopathy by Suppressing High Glucose-Induced Oxidative Stress In Vivo and In Vitro. Front. Pharmacol. 2021, 12, 708177. [Google Scholar] [CrossRef]
- Kimura, Y.; Kuno, A.; Tanno, M.; Sato, T.; Ohno, K.; Shibata, S.; Nakata, K.; Sugawara, H.; Abe, K.; Igaki, Y.; et al. Canagliflozin, a sodium-glucose cotransporter 2 inhibitor, normalizes renal susceptibility to type 1 cardiorenal syndrome through reduction of renal oxidative stress in diabetic rats. J. Diabetes Investig. 2019, 10, 933–946. [Google Scholar] [CrossRef] [PubMed]
- Oshima, H.; Miki, T.; Kuno, A.; Mizuno, M.; Sato, T.; Tanno, M.; Yano, T.; Nakata, K.; Kimura, Y.; Abe, K.; et al. Empagliflozin, an SGLT2 Inhibitor, Reduced the Mortality Rate after Acute Myocardial Infarction with Modification of Cardiac Metabolomes and Antioxidants in Diabetic Rats. J. Pharmacol. Exp. Ther. 2019, 368, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Kern, M.; Klöting, N.; Mark, M.; Mayoux, E.; Klein, T.; Blüher, M. The SGLT2 inhibitor empagliflozin improves insulin sensitivity in db/db mice both as monotherapy and in combination with linagliptin. Metab. Clin. Exp. 2016, 65, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Merovci, A.; Solis-Herrera, C.; Daniele, G.; Eldor, R.; Fiorentino, T.V.; Tripathy, D.; Xiong, J.; Perez, Z.; Norton, L.; Abdul-Ghani, M.A.; et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J. Clin. Investig. 2014, 124, 509–514. [Google Scholar] [CrossRef]
- Wallenius, K.; Kroon, T.; Hagstedt, T.; Löfgren, L.; Sörhede-Winzell, M.; Boucher, J.; Lindén, D.; Oakes, N.D. The SGLT2 inhibitor dapagliflozin promotes systemic FFA mobilization, enhances hepatic β-oxidation, and induces ketosis. J. Lipid Res. 2022, 63, 100176. [Google Scholar] [CrossRef]
- Herring, R.A.; Shojaee-Moradie, F.; Stevenage, M.; Parsons, I.; Jackson, N.; Mendis, J.; Middleton, B.; Umpleby, A.M.; Fielding, B.A.; Davies, M.; et al. The SGLT2 Inhibitor Dapagliflozin Increases the Oxidation of Ingested Fatty Acids to Ketones in Type 2 Diabetes. Diabetes Care 2022, 45, 1408–1415. [Google Scholar] [CrossRef]
- Yokono, M.; Takasu, T.; Hayashizaki, Y.; Mitsuoka, K.; Kihara, R.; Muramatsu, Y.; Miyoshi, S.; Tahara, A.; Kurosaki, E.; Li, Q.; et al. SGLT2 selective inhibitor ipragliflozin reduces body fat mass by increasing fatty acid oxidation in high-fat diet-induced obese rats. Eur. J. Pharmacol. 2014, 727, 66–74. [Google Scholar] [CrossRef]
- Trnovska, J.; Svoboda, P.; Pelantova, H.; Kuzma, M.; Kratochvilova, H.; Kasperova, B.J.; Dvorakova, I.; Rosolova, K.; Malinska, H.; Huttl, M.; et al. Complex Positive Effects of SGLT-2 Inhibitor Empagliflozin in the Liver, Kidney and Adipose Tissue of Hereditary Hypertriglyceridemic Rats: Possible Contribution of Attenuation of Cell Senescence and Oxidative Stress. Int. J. Mol. Sci. 2021, 22, 10606. [Google Scholar] [CrossRef]
- Suzuki, M.; Takeda, M.; Kito, A.; Fukazawa, M.; Yata, T.; Yamamoto, M.; Nagata, T.; Fukuzawa, T.; Yamane, M.; Honda, K.; et al. Tofogliflozin, a sodium/glucose cotransporter 2 inhibitor, attenuates body weight gain and fat accumulation in diabetic and obese animal models. Nutr. Diabetes 2014, 4, e125. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Nagata, N.; Nagashimada, M.; Zhuge, F.; Ni, Y.; Chen, G.; Mayoux, E.; Kaneko, S.; Ota, T. SGLT2 Inhibition by Empagliflozin Promotes Fat Utilization and Browning and Attenuates Inflammation and Insulin Resistance by Polarizing M2 Macrophages in Diet-induced Obese Mice. eBioMedicine 2017, 20, 137–149. [Google Scholar] [CrossRef]
- Sato, D.; Nakamura, T.; Amarume, J.; Yano, M.; Umehara, Y.; Nishina, A.; Tsutsumi, K.; Feng, Z.; Kusunoki, M. Effects of Dapagliflozin on Adipose and Liver Fatty Acid Composition and mRNA Expression Involved in Lipid Metabolism in High-Fat-Fed Rats. Endocr. Metab. Immune Disord. Drug Targets 2022, 22, 944–953. [Google Scholar] [CrossRef]
- Xu, L.; Nagata, N.; Chen, G.; Nagashimada, M.; Zhuge, F.; Ni, Y.; Sakai, Y.; Kaneko, S.; Ota, T. Empagliflozin reverses obesity and insulin resistance through fat browning and alternative macrophage activation in mice fed a high-fat diet. BMJ Open Diabetes Res. Care 2019, 7, e000783. [Google Scholar] [CrossRef]
- Sánchez-García, A.; Simental-Mendía, M.; Millán-Alanís, J.M.; Simental-Mendía, L.E. Effect of sodium-glucose co-transporter 2 inhibitors on lipid profile: A systematic review and meta-analysis of 48 randomized controlled trials. Pharmacol. Res. 2020, 160, 105068. [Google Scholar] [CrossRef] [PubMed]
- Basu, D.; Huggins, L.A.; Scerbo, D.; Obunike, J.; Mullick, A.E.; Rothenberg, P.L.; Di Prospero, N.A.; Eckel, R.H.; Goldberg, I.J. Mechanism of Increased LDL (Low-Density Lipoprotein) and Decreased Triglycerides with SGLT2 (Sodium-Glucose Cotransporter 2) Inhibition. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 2207–2216. [Google Scholar] [CrossRef] [PubMed]
- Cha, S.A.; Park, Y.M.; Yun, J.S.; Lim, T.S.; Song, K.H.; Yoo, K.D.; Ahn, Y.B.; Ko, S.H. A comparison of effects of DPP-4 inhibitor and SGLT2 inhibitor on lipid profile in patients with type 2 diabetes. Lipids Health Dis. 2017, 16, 58. [Google Scholar] [CrossRef] [PubMed]
- Jiang, A.; Feng, Z.; Yuan, L.; Zhang, Y.; Li, Q.; She, Y. Effect of sodium-glucose co-transporter-2 inhibitors on the levels of serum asprosin in patients with newly diagnosed type 2 diabetes mellitus. Diabetol. Metab. Syndr. 2021, 13, 34. [Google Scholar] [CrossRef]
- Fadini, G.P.; Bonora, B.M.; Zatti, G.; Vitturi, N.; Iori, E.; Marescotti, M.C.; Albiero, M.; Avogaro, A. Effects of the SGLT2 inhibitor dapagliflozin on HDL cholesterol, particle size, and cholesterol efflux capacity in patients with type 2 diabetes: A randomized placebo-controlled trial. Cardiovasc. Diabetol. 2017, 16, 42. [Google Scholar] [CrossRef]
- Bosch, A.; Ott, C.; Jung, S.; Striepe, K.; Karg, M.V.; Kannenkeril, D.; Dienemann, T.; Schmieder, R.E. How does empagliflozin improve arterial stiffness in patients with type 2 diabetes mellitus? Sub analysis of a clinical trial. Cardiovasc. Diabetol. 2019, 18, 44. [Google Scholar] [CrossRef]
- Toyama, T.; Neuen, B.L.; Jun, M.; Ohkuma, T.; Neal, B.; Jardine, M.J.; Heerspink, H.L.; Wong, M.G.; Ninomiya, T.; Wada, T.; et al. Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: A systematic review and meta-analysis. Diabetes Obes. Metab. 2019, 21, 1237–1250. [Google Scholar] [CrossRef] [PubMed]
- Nusca, A.; Piccirillo, F.; Viscusi, M.M.; Giannone, S.; Mangiacapra, F.; Melfi, R.; Ricottini, E.; Ussia, G.P.; Grigioni, F. Contrast-induced Acute Kidney Injury in Diabetic Patients and SGLT-2 Inhibitors: A Preventive Opportunity or Promoting Element? J. Cardiovasc. Pharmacol. 2022, 80, 661–671. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Calapkulu, M.; Cander, S.; Gul, O.O.; Ersoy, C. Lipid profile in type 2 diabetic patients with new dapagliflozin treatment; actual clinical experience data of six months retrospective lipid profile from single center. Diabetes Metab. Syndr. 2019, 13, 1031–1034. [Google Scholar] [CrossRef]
- Bays, H.E.; Sartipy, P.; Xu, J.; Sjöström, C.D.; Underberg, J.A. Dapagliflozin in patients with type II diabetes mellitus, with and without elevated triglyceride and reduced high-density lipoprotein cholesterol levels. J. Clin. Lipidol. 2017, 11, 450–458.e1. [Google Scholar] [CrossRef]
- Matthaei, S.; Bowering, K.; Rohwedder, K.; Grohl, A.; Parikh, S. Dapagliflozin improves glycemic control and reduces body weight as add-on therapy to metformin plus sulfonylurea: A 24-week randomized, double-blind clinical trial. Diabetes Care 2015, 38, 365–372. [Google Scholar] [CrossRef]
- Hayashi, T.; Fukui, T.; Nakanishi, N.; Yamamoto, S.; Tomoyasu, M.; Osamura, A.; Ohara, M.; Yamamoto, T.; Ito, Y.; Hirano, T. Dapagliflozin decreases small dense low-density lipoprotein-cholesterol and increases high-density lipoprotein 2-cholesterol in patients with type 2 diabetes: Comparison with sitagliptin. Cardiovasc. Diabetol. 2017, 16, 8. [Google Scholar] [CrossRef]
- Yanai, H.; Hakoshima, M.; Adachi, H.; Kawaguchi, A.; Waragai, Y.; Harigae, T.; Masui, Y.; Kakuta, K.; Hamasaki, H.; Katsuyama, H.; et al. Effects of Six Kinds of Sodium-Glucose Cotransporter 2 Inhibitors on Metabolic Parameters, and Summarized Effect and Its Correlations with Baseline Data. J. Clin. Med. Res. 2017, 9, 605–612. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Tikkanen, I.; Narko, K.; Zeller, C.; Green, A.; Salsali, A.; Broedl, U.C.; Woerle, H.J. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care 2015, 38, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Liakos, A.; Karagiannis, T.; Athanasiadou, E.; Sarigianni, M.; Mainou, M.; Papatheodorou, K.; Bekiari, E.; Tsapas, A. Efficacy and safety of empagliflozin for type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes. Metab. 2014, 16, 984–993. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.; Perkovic, V.; Mahaffey, K.W.; de Zeeuw, D.; Fulcher, G.; Erondu, N.; Shaw, W.; Law, G.; Desai, M.; Matthews, D.R. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 644–657. [Google Scholar] [CrossRef] [PubMed]
- Bode, B.; Stenlöf, K.; Harris, S.; Sullivan, D.; Fung, A.; Usiskin, K.; Meininger, G. Long-term efficacy and safety of canagliflozin over 104 weeks in patients aged 55–80 years with type 2 diabetes. Diabetes Obes. Metab. 2015, 17, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Nauck, M.A.; Quast, D.R.; Wefers, J.; Meier, J.J. GLP-1 receptor agonists in the treatment of type 2 diabetes—State-of-the-art. Mol. Metab. 2021, 46, 101102. [Google Scholar] [CrossRef] [PubMed]
- Htike, Z.Z.; Zaccardi, F.; Papamargaritis, D.; Webb, D.R.; Khunti, K.; Davies, M.J. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: A systematic review and mixed-treatment comparison analysis. Diabetes Obes. Metab. 2017, 19, 524–536. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Liu, Z.; Ilyas, I.; Little, P.J.; Kamato, D.; Sahebka, A.; Chen, Z.; Luo, S.; Zheng, X.; Weng, J.; et al. GLP-1 receptor agonists (GLP-1RAs): Cardiovascular actions and therapeutic potential. Int. J. Biol. Sci. 2021, 17, 2050–2068. [Google Scholar] [CrossRef] [PubMed]
- Rakipovski, G.; Rolin, B.; Nøhr, J.; Klewe, I.; Frederiksen, K.S.; Augustin, R.; Hecksher-Sørensen, J.; Ingvorsen, C.; Polex-Wolf, J.; Knudsen, L.B. The GLP-1 Analogs Liraglutide and Semaglutide Reduce Atherosclerosis in ApoE(−/−) and LDLr(−/−) Mice by a Mechanism That Includes Inflammatory Pathways. JACC. Basic Transl. Sci. 2018, 3, 844–857. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, M.; Mita, T.; Azuma, K.; Ebato, C.; Goto, H.; Nomiyama, T.; Fujitani, Y.; Hirose, T.; Kawamori, R.; Watada, H. Inhibition of monocyte adhesion to endothelial cells and attenuation of atherosclerotic lesion by a glucagon-like peptide-1 receptor agonist, exendin-4. Diabetes 2010, 59, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Bułdak, Ł.; Machnik, G.; Bułdak, R.J.; Łabuzek, K.; Bołdys, A.; Okopień, B. Exenatide and metformin express their anti-inflammatory effects on human monocytes/macrophages by the attenuation of MAPKs and NFκB signaling. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2016, 389, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Matsuo, Y.; Yamakage, H.; Masuda, S.; Terada, Y.; Muranaka, K.; Wada, H.; Hasegawa, K.; Shimatsu, A.; Satoh-Asahara, N. Differential effects of GLP-1 receptor agonist on foam cell formation in monocytes between non-obese and obese subjects. Metab. Clin. Exp. 2016, 65, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, Y.; Sato, K.; Watanabe, T.; Nohtomi, K.; Terasaki, M.; Nagashima, M.; Hirano, T. A glucagon-like peptide-1 analog liraglutide suppresses macrophage foam cell formation and atherosclerosis. Peptides 2014, 54, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Osto, E.; Doytcheva, P.; Corteville, C.; Bueter, M.; Dörig, C.; Stivala, S.; Buhmann, H.; Colin, S.; Rohrer, L.; Hasballa, R.; et al. Rapid and body weight-independent improvement of endothelial and high-density lipoprotein function after Roux-en-Y gastric bypass: Role of glucagon-like peptide-1. Circulation 2015, 131, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Piccirillo, F.; Carpenito, M.; Verolino, G.; Chello, C.; Nusca, A.; Lusini, M.; Spadaccio, C.; Nappi, F.; Di Sciascio, G.; Nenna, A. Changes of the coronary arteries and cardiac microvasculature with aging: Implications for translational research and clinical practice. Mech. Ageing Dev. 2019, 184, 111161. [Google Scholar] [CrossRef] [PubMed]
- Ariel, D.; Kim, S.H.; Abbasi, F.; Lamendola, C.A.; Liu, A.; Reaven, G.M. Effect of liraglutide administration and a calorie-restricted diet on lipoprotein profile in overweight/obese persons with prediabetes. Nutr. Metab. Cardiovasc. Dis. NMCD 2014, 24, 1317–1322. [Google Scholar] [CrossRef] [PubMed]
- Parlevliet, E.T.; Wang, Y.; Geerling, J.J.; Schröder-Van der Elst, J.P.; Picha, K.; O’Neil, K.; Stojanovic-Susulic, V.; Ort, T.; Havekes, L.M.; Romijn, J.A.; et al. GLP-1 receptor activation inhibits VLDL production and reverses hepatic steatosis by decreasing hepatic lipogenesis in high-fat-fed APOE*3-Leiden mice. PLoS ONE 2012, 7, e49152. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.J.; Joharapurkar, A.A.; Shah, G.B.; Jain, M.R. Effect of GLP-1 based therapies on diabetic dyslipidemia. Curr. Diabetes Rev. 2014, 10, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, S.; Zvibel, I.; Shnell, M.; Shlomai, A.; Chepurko, E.; Halpern, Z.; Barzilai, N.; Oren, R.; Fishman, S. Glucagon-like peptide-1 reduces hepatic lipogenesis via activation of AMP-activated protein kinase. J. Hepatol. 2011, 54, 1214–1223. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.R.; Shi, X.Y.; Ma, C.Y.; Zhang, Y.; Xu, R.X.; Li, J.J. Liraglutide improves lipid metabolism by enhancing cholesterol efflux associated with ABCA1 and ERK1/2 pathway. Cardiovasc. Diabetol. 2019, 18, 146. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Cao, H.; Chen, Z.; Gu, H.; Guo, W.; Lin, B.; Weng, J. Short-term GLP-1 receptor agonist exenatide ameliorates intramyocellular lipid deposition without weight loss in ob/ob mice. Int. J. Obes. 2020, 44, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.J.; Hull, D.; Guo, K.; Barton, D.; Hazlehurst, J.M.; Gathercole, L.L.; Nasiri, M.; Yu, J.; Gough, S.C.; Newsome, P.N.; et al. Glucagon-like peptide 1 decreases lipotoxicity in non-alcoholic steatohepatitis. J. Hepatol. 2016, 64, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Gastaldelli, A.; Gaggini, M.; Daniele, G.; Ciociaro, D.; Cersosimo, E.; Tripathy, D.; Triplitt, C.; Fox, P.; Musi, N.; DeFronzo, R.; et al. Exenatide improves both hepatic and adipose tissue insulin resistance: A dynamic positron emission tomography study. Hepatol. 2016, 64, 2028–2037. [Google Scholar] [CrossRef]
- Lee, J.; Hong, S.W.; Chae, S.W.; Kim, D.H.; Choi, J.H.; Bae, J.C.; Park, S.E.; Rhee, E.J.; Park, C.Y.; Oh, K.W.; et al. Exendin-4 improves steatohepatitis by increasing Sirt1 expression in high-fat diet-induced obese C57BL/6J mice. PLoS ONE 2012, 7, e31394. [Google Scholar] [CrossRef]
- Trevaskis, J.L.; Griffin, P.S.; Wittmer, C.; Neuschwander-Tetri, B.A.; Brunt, E.M.; Dolman, C.S.; Erickson, M.R.; Napora, J.; Parkes, D.G.; Roth, J.D. Glucagon-like peptide-1 receptor agonism improves metabolic, biochemical, and histopathological indices of nonalcoholic steatohepatitis in mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 302, G762–G772. [Google Scholar] [CrossRef] [PubMed]
- Jendle, J.; Hyötyläinen, T.; Orešič, M.; Nyström, T. Pharmacometabolomic profiles in type 2 diabetic subjects treated with liraglutide or glimepiride. Cardiovasc. Diabetol. 2021, 20, 237. [Google Scholar] [CrossRef] [PubMed]
- Seghieri, M.; Rebelos, E.; Gastaldelli, A.; Astiarraga, B.D.; Casolaro, A.; Barsotti, E.; Pocai, A.; Nauck, M.; Muscelli, E.; Ferrannini, E. Direct effect of GLP-1 infusion on endogenous glucose production in humans. Diabetologia 2013, 56, 156–161. [Google Scholar] [CrossRef]
- Viswanathan, P.; Chaudhuri, A.; Bhatia, R.; Al-Atrash, F.; Mohanty, P.; Dandona, P. Exenatide therapy in obese patients with type 2 diabetes mellitus treated with insulin. Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2007, 13, 444–450. [Google Scholar] [CrossRef]
- Schwartz, E.A.; Koska, J.; Mullin, M.P.; Syoufi, I.; Schwenke, D.C.; Reaven, P.D. Exenatide suppresses postprandial elevations in lipids and lipoproteins in individuals with impaired glucose tolerance and recent onset type 2 diabetes mellitus. Atherosclerosis 2010, 212, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Hori, M.; Nakagami, T.; Harada-Shiba, M.; Uchigata, Y. Glucagon-like peptide-1 receptor agonists reduced the low-density lipoprotein cholesterol in Japanese patients with type 2 diabetes mellitus treated with statins. J. Clin. Lipidol. 2018, 12, 62–69.e1. [Google Scholar] [CrossRef] [PubMed]
- Pi-Sunyer, X.; Astrup, A.; Fujioka, K.; Greenway, F.; Halpern, A.; Krempf, M.; Lau, D.C.; le Roux, C.W.; Violante Ortiz, R.; Jensen, C.B.; et al. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N. Engl. J. Med. 2015, 373, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Wu, S.; Wang, J.; Guo, S.; Chai, S.; Yang, Z.; Li, L.; Zhang, Y.; Ji, L.; Zhan, S. Effect of glucagon-like peptide-1 receptor agonists on lipid profiles among type 2 diabetes: A systematic review and network meta-analysis. Clin. Ther. 2015, 37, 225–241.e8. [Google Scholar] [CrossRef]
- Buse, J.B.; Nauck, M.; Forst, T.; Sheu, W.H.; Shenouda, S.K.; Heilmann, C.R.; Hoogwerf, B.J.; Gao, A.; Boardman, M.K.; Fineman, M.; et al. Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): A randomised, open-label study. Lancet 2013, 381, 117–124. [Google Scholar] [CrossRef]
- Buse, J.B.; Rosenstock, J.; Sesti, G.; Schmidt, W.E.; Montanya, E.; Brett, J.H.; Zychma, M.; Blonde, L. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: A 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 2009, 374, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Yu, J.; Tian, T.; Miao, J.; Shang, W. Meta-analysis of the efficacy of liraglutide in patients with type 2 diabetes accompanied by incipient nephropathy. Exp. Ther. Med. 2019, 18, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Sorli, C.; Harashima, S.I.; Tsoukas, G.M.; Unger, J.; Karsbøl, J.D.; Hansen, T.; Bain, S.C. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): A double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 2017, 5, 251–260. [Google Scholar] [CrossRef]
- Aroda, V.R.; Bain, S.C.; Cariou, B.; Piletič, M.; Rose, L.; Axelsen, M.; Rowe, E.; DeVries, J.H. Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-naive patients with type 2 diabetes (SUSTAIN 4): A randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol. 2017, 5, 355–366. [Google Scholar] [CrossRef]
- Ahmann, A.J.; Capehorn, M.; Charpentier, G.; Dotta, F.; Henkel, E.; Lingvay, I.; Holst, A.G.; Annett, M.P.; Aroda, V.R. Efficacy and Safety of Once-Weekly Semaglutide Versus Exenatide ER in Subjects With Type 2 Diabetes (SUSTAIN 3): A 56-Week, Open-Label, Randomized Clinical Trial. Diabetes Care 2018, 41, 258–266. [Google Scholar] [CrossRef]
- Chiquette, E.; Toth, P.P.; Ramirez, G.; Cobble, M.; Chilton, R. Treatment with exenatide once weekly or twice daily for 30 weeks is associated with changes in several cardiovascular risk markers. Vasc. Health Risk Manag. 2012, 8, 621–629. [Google Scholar] [CrossRef]
- Song, X.; Jia, H.; Jiang, Y.; Wang, L.; Zhang, Y.; Mu, Y.; Liu, Y. Anti-atherosclerotic effects of the glucagon-like peptide-1 (GLP-1) based therapies in patients with type 2 Diabetes Mellitus: A meta-analysis. Sci. Rep. 2015, 5, 10202. [Google Scholar] [CrossRef] [PubMed]
- Dar, S.; Siddiqi, A.K.; Alabduladhem, T.O.; Rashid, A.M.; Sarfraz, S.; Maniya, T.; Menezes, R.G.; Almas, T. Effects of novel glucose-lowering drugs on the lipid parameters: A systematic review and meta-analysis. Ann. Med. Surg. 2022, 77, 103633. [Google Scholar] [CrossRef]
- Li, C.; Luo, J.; Jiang, M.; Wang, K. The Efficacy and Safety of the Combination Therapy with GLP-1 Receptor Agonists and SGLT-2 Inhibitors in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis. Front. Pharmacol. 2022, 13, 838277. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Allison, D.; Birkenfeld, A.L.; Blicher, T.M.; Deenadayalan, S.; Jacobsen, J.B.; Serusclat, P.; Violante, R.; Watada, H.; Davies, M. Effect of Additional Oral Semaglutide vs Sitagliptin on Glycated Hemoglobin in Adults with Type 2 Diabetes Uncontrolled with Metformin Alone or with Sulfonylurea: The PIONEER 3 Randomized Clinical Trial. JAMA 2019, 321, 1466–1480. [Google Scholar] [CrossRef] [PubMed]
- Niman, S.; Hardy, J.; Goldfaden, R.F.; Reid, J.; Sheikh-Ali, M.; Sutton, D.; Choksi, R. A Review on the Efficacy and Safety of Oral Semaglutide. Drugs RD 2021, 21, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Pirro, V.; Roth, K.D.; Lin, Y.; Willency, J.A.; Milligan, P.L.; Wilson, J.M.; Ruotolo, G.; Haupt, A.; Newgard, C.B.; Duffin, K.L. Effects of Tirzepatide, a Dual GIP and GLP-1 RA, on Lipid and Metabolite Profiles in Subjects with Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2022, 107, 363–378. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.M.; Nikooienejad, A.; Robins, D.A.; Roell, W.C.; Riesmeyer, J.S.; Haupt, A.; Duffin, K.L.; Taskinen, M.R.; Ruotolo, G. The dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist, tirzepatide, improves lipoprotein biomarkers associated with insulin resistance and cardiovascular risk in patients with type 2 diabetes. Diabetes Obes. Metab. 2020, 22, 2451–2459. [Google Scholar] [CrossRef] [PubMed]
- Thornberry, N.A.; Gallwitz, B. Mechanism of action of inhibitors of dipeptidyl-peptidase-4 (DPP-4). Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Yano, W.; Inoue, N.; Ito, S.; Itou, T.; Yasumura, M.; Yoshinaka, Y.; Hagita, S.; Goto, M.; Nakagawa, T.; Inoue, K.; et al. Mechanism of lipid-lowering action of the dipeptidyl peptidase-4 inhibitor, anagliptin, in low-density lipoprotein receptor-deficient mice. J. Diabetes Investig. 2017, 8, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Rufinatscha, K.; Radlinger, B.; Dobner, J.; Folie, S.; Bon, C.; Profanter, E.; Ress, C.; Salzmann, K.; Staudacher, G.; Tilg, H.; et al. Dipeptidyl peptidase-4 impairs insulin signaling and promotes lipid accumulation in hepatocytes. Biochem. Biophys. Res. Commun. 2017, 485, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, A.M.; Hamdy, N.M.; Abdel-Rahman, S.Z.; El-Mesallamy, H.O. Effect of vildagliptin and pravastatin combination on cholesterol efflux in adipocytes. IUBMB Life 2016, 68, 535–543. [Google Scholar] [CrossRef] [PubMed]
- Aroor, A.R.; Habibi, J.; Ford, D.A.; Nistala, R.; Lastra, G.; Manrique, C.; Dunham, M.M.; Ford, K.D.; Thyfault, J.P.; Parks, E.J.; et al. Dipeptidyl peptidase-4 inhibition ameliorates Western diet-induced hepatic steatosis and insulin resistance through hepatic lipid remodeling and modulation of hepatic mitochondrial function. Diabetes 2015, 64, 1988–2001. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, N.; Zhu, L.; Liu, Y.; Pei, Z.; Wang, G.; Luo, L.; Liu, H. The Dipeptidyl Peptidase-4 Inhibitor Teneligliptin Reduces Aortic Damage from Hypercholesterolaemia in Apolipoprotein E-Deficient Mice. Biomed. Hub 2017, 2, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Shen, T.; Chen, L.; Xia, J.; Zhang, C.; Wang, H.; Yu, M.; Lei, T. The Effect of Sitagliptin on Lipid Metabolism of Fatty Liver Mice and Related Mechanisms. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Kutoh, E.; Wada, A.; Hayashi, J. Regulation of free fatty acid by sitagliptin monotherapy in drug-naïve subjects with type 2 diabetes. Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2018, 24, 1063–1072. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Xu, L.; Xing, M.; Xu, X.; Wei, J.; Wang, J.; Kang, W. Trelagliptin succinate: DPP-4 inhibitor to improve insulin resistance in adipocytes. Biomed. Pharmacother. Biomed. Pharmacother. 2020, 125, 109952. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Chae, Y.N.; Ahn, G.J.; Shin, C.Y.; Choi, S.H.; Yang, E.K.; Sohn, Y.S.; Son, M.H. Prevention and treatment effect of evogliptin on hepatic steatosis in high-fat-fed animal models. Arch. Pharmacal Res. 2017, 40, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.; Frahm, J.; Kersten, S.; Meyer, U.; Rehage, J.; Piechotta, M.; Meyerholz, M.; Breves, G.; Reiche, D.; Sauerwein, H.; et al. Effects of Inhibiting Dipeptidyl Peptidase-4 (DPP4) in Cows with Subclinical Ketosis. PLoS ONE 2015, 10, e0136078. [Google Scholar] [CrossRef] [PubMed]
- Briand, F.; Thieblemont, Q.; Burcelin, R.; Sulpice, T. Sitagliptin promotes macrophage-to-faeces reverse cholesterol transport through reduced intestinal cholesterol absorption in obese insulin resistant CETP-apoB100 transgenic mice. Diabetes Obes. Metab. 2012, 14, 662–665. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Leem, J.; Park, S.; Lee, C.K.; Park, K.G.; Lee, I.K. Gemigliptin ameliorates Western-diet-induced metabolic syndrome in mice. Can. J. Physiol. Pharmacol. 2017, 95, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Rameshrad, M.; Razavi, B.M.; Ferns, G.A.A.; Hosseinzadeh, H. Pharmacology of dipeptidyl peptidase-4 inhibitors and its use in the management of metabolic syndrome: A comprehensive review on drug repositioning. Daru J. Fac. Pharm. Tehran Univ. Med. Sci. 2019, 27, 341–360. [Google Scholar] [CrossRef] [PubMed]
- Monami, M.; Lamanna, C.; Desideri, C.M.; Mannucci, E. DPP-4 inhibitors and lipids: Systematic review and meta-analysis. Adv. Ther. 2012, 29, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, Y.; Takenaka, Y.; Saito, D.; Shimada, A.; Inoue, I. Anagliptin Monotherapy for Six Months in Patients with Type 2 Diabetes Mellitus and Hyper-Low-Density Lipoprotein Cholesterolemia Reduces Plasma Levels of Fasting Low-Density Lipoprotein Cholesterol and Lathosterol: A Single-Arm Intervention Trial. J. Clin. Med. Res. 2021, 13, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Nishida, Y.; Takahashi, Y.; Tezuka, K.; Akimoto, H.; Nakayama, T.; Asai, S. Comparative effect of dipeptidyl-peptidase 4 inhibitors on laboratory parameters in patients with diabetes mellitus. BMC Pharmacol. Toxicol. 2020, 21, 28. [Google Scholar] [CrossRef]
- Kusunoki, M.; Sato, D.; Nakamura, T.; Oshida, Y.; Tsutsui, H.; Natsume, Y.; Tsutsumi, K.; Miyata, T. The Beneficial Effects of the DPP-4 Inhibitor Alogliptin on Hemoglobin A1c and Serum Lipids in Japanese Patients with Type 2 Diabetes. Drug Res. 2016, 66, 18–22. [Google Scholar] [CrossRef]
- Monami, M.; Vitale, V.; Ambrosio, M.L.; Bartoli, N.; Toffanello, G.; Ragghianti, B.; Monami, F.; Marchionni, N.; Mannucci, E. Effects on lipid profile of dipeptidyl peptidase 4 inhibitors, pioglitazone, acarbose, and sulfonylureas: Meta-analysis of placebo-controlled trials. Adv. Ther. 2012, 29, 736–746. [Google Scholar] [CrossRef]
- Homma, K.; Yoshizawa, J.; Shiina, Y.; Ozawa, H.; Igarashi, M.; Matsuoka, T.; Sasaki, J.; Yoshizawa, M.; Homma, Y. A Dipeptidyl Peptidase-4 Inhibitor, Teneligliptin, Decreases Plasma Triglyceride-Rich Lipoprotein Remnants in Diabetic Patients with Chronic Kidney Disease Undergoing Hemodialysis. Drugs RD 2017, 17, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, A.J.; Lamarche, B.; Kelly, I.; Charest, A.; Lépine, M.C.; Droit, A.; Couture, P. Effect of sitagliptin therapy on triglyceride-rich lipoprotein kinetics in patients with type 2 diabetes. Diabetes Obes. Metab. 2014, 16, 1223–1229. [Google Scholar] [CrossRef] [PubMed]
- Kakuda, H.; Kobayashi, J.; Kakuda, M.; Yamakawa, J.; Takekoshi, N. The effect of anagliptin treatment on glucose metabolism and lipid metabolism, and oxidative stress in fasting and postprandial states using a test meal in Japanese men with type 2 diabetes. Endocrine 2015, 48, 1005–1009. [Google Scholar] [CrossRef]
- Cheng, L.; Fu, Q.; Zhou, L.; Fan, Y.; Liu, F.; Fan, Y.; Zhang, X.; Lin, W.; Wu, X. Dapagliflozin, metformin, monotherapy or both in patients with metabolic syndrome. Sci. Rep. 2021, 11, 24263. [Google Scholar] [CrossRef]
- Bolinder, J.; Ljunggren, Ö.; Kullberg, J.; Johansson, L.; Wilding, J.; Langkilde, A.M.; Sugg, J.; Parikh, S. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J. Clin. Endocrinol. Metab. 2012, 97, 1020–1031. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.Y.; Weng, S.F.; Hsu, C.H.; Huang, C.L.; Lin, Y.P.; Yeh, M.C.; Han, A.Y.; Hsieh, Y.S. Effect of metformin monotherapy and dual or triple concomitant therapy with metformin on glycemic control and lipid profile management of patients with type 2 diabetes mellitus. Front. Med. 2022, 9, 995944. [Google Scholar] [CrossRef] [PubMed]
- Frías, J.P.; Guja, C.; Hardy, E.; Ahmed, A.; Dong, F.; Öhman, P.; Jabbour, S.A. Exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy (DURATION-8): A 28 week, multicentre, double-blind, phase 3, randomised controlled trial. Lancet. Diabetes Endocrinol. 2016, 4, 1004–1016. [Google Scholar] [CrossRef]
- Jabbour, S.A.; Frías, J.P.; Guja, C.; Hardy, E.; Ahmed, A.; Öhman, P. Effects of exenatide once weekly plus dapagliflozin, exenatide once weekly, or dapagliflozin, added to metformin monotherapy, on body weight, systolic blood pressure, and triglycerides in patients with type 2 diabetes in the DURATION-8 study. Diabetes Obes. Metab. 2018, 20, 1515–1519. [Google Scholar] [CrossRef]
- 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis 2019, 290, 140–205. [CrossRef] [PubMed]
- Vinci, P.; Panizon, E.; Tosoni, L.M.; Cerrato, C.; Pellicori, F.; Mearelli, F.; Biasinutto, C.; Fiotti, N.; Di Girolamo, F.G.; Biolo, G. Statin-Associated Myopathy: Emphasis on Mechanisms and Targeted Therapy. Int. J. Mol. Sci. 2021, 22, 11687. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Suo, Y.; Yang, L.; Zhang, X.; Yu, Q.; Zeng, M.; Zhang, W.; Jiang, X.; Wang, Y. Effect of PCSK9 Inhibitor on Blood Lipid Levels in Patients with High and Very-High CVD Risk: A Systematic Review and Meta-Analysis. Cardiol. Res. Pract. 2022, 2022, 8729003. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wen, D.; Chen, Y.; Ma, L.; You, C. PCSK9 inhibitors for secondary prevention in patients with cardiovascular diseases: A bayesian network meta-analysis. Cardiovasc. Diabetol. 2022, 21, 107. [Google Scholar] [CrossRef]
- Leiter, L.A.; Teoh, H.; Kallend, D.; Wright, R.S.; Landmesser, U.; Wijngaard, P.L.J.; Kastelein, J.J.P.; Ray, K.K. Inclisiran Lowers LDL-C and PCSK9 Irrespective of Diabetes Status: The ORION-1 Randomized Clinical Trial. Diabetes Care 2019, 42, 173–176. [Google Scholar] [CrossRef]
- Biolo, G.; Vinci, P.; Mangogna, A.; Landolfo, M.; Schincariol, P.; Fiotti, N.; Mearelli, F.; Di Girolamo, F.G. Mechanism of action and therapeutic use of bempedoic acid in atherosclerosis and metabolic syndrome. Front. Cardiovasc. Med. 2022, 9, 1028355. [Google Scholar] [CrossRef]
- Pinkosky, S.L.; Filippov, S.; Srivastava, R.A.; Hanselman, J.C.; Bradshaw, C.D.; Hurley, T.R.; Cramer, C.T.; Spahr, M.A.; Brant, A.F.; Houghton, J.L.; et al. AMP-activated protein kinase and ATP-citrate lyase are two distinct molecular targets for ETC-1002, a novel small molecule regulator of lipid and carbohydrate metabolism. J. Lipid Res. 2013, 54, 134–151. [Google Scholar] [CrossRef]
- Gutierrez, M.J.; Rosenberg, N.L.; Macdougall, D.E.; Hanselman, J.C.; Margulies, J.R.; Strange, P.; Milad, M.A.; McBride, S.J.; Newton, R.S. Efficacy and safety of ETC-1002, a novel investigational low-density lipoprotein-cholesterol-lowering therapy for the treatment of patients with hypercholesterolemia and type 2 diabetes mellitus. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 676–683. [Google Scholar] [CrossRef]
- Leiter, L.A.; Banach, M.; Catapano, A.L.; Duell, P.B.; Gotto, A.M., Jr.; Laufs, U.; Mancini, G.B.J.; Ray, K.K.; Hanselman, J.C.; Ye, Z.; et al. Bempedoic acid in patients with type 2 diabetes mellitus, prediabetes, and normoglycaemia: A post hoc analysis of efficacy and glycaemic control using pooled data from phase 3 clinical trials. Diabetes Obes. Metab. 2022, 24, 868–880. [Google Scholar] [CrossRef]

| Type of Study | Molecule | N° of Patients | Time of Follow-Up | Main Results | |
|---|---|---|---|---|---|
| Calapkulu et al., 2019 [54] | Retrospective study | Dapaglifozin 10 mg | 31 patients | 3 and 6 months | At three months:
|
| Bays et al., 2017 [55] | Post-hoc analysis | Dapaglifozin 10 mg | 4401 patients | 6 months | ↑ LDL ↑ HDL ↑ total cholesterol ↓ triglycerides |
| Matthaei et al., 2015 [56] | Phase 3b study | Dapaglifozin 10 mg | 219 patients | 6 months | ↑ LDL ↑ HDL ↑ total cholesterol |
| Hayashi et al., 2017 [57] | Prospective study | Dapaglifozin 10 mg | 80 patients | 3 months | ↑ LDL (0.5%) ↑ HDL (10.5%) ↑ total cholesterol (2.5%) ↓ triglycerides (12.4%) |
| Yanai et al., 2017 [58] | Retrospective study | Dapaglifozin 10 mg | 249 patients (69 treated with dapaglifozin) | 3 and 6 months | At three months: non-significant changes At six months:
|
| Zinman et al., 2015 [59] | Randomized controlled trial | Empaglifozin 10 or 25 mg | 7028 patients | 3 years | ↑ LDL ↓ HDL |
| Tikkanen et al., 2015 [60] | Phase 3 study | Empaglifozin 10 or 25 mg | 825 patients | 14 weeks | With 10 mg:
|
| Sánchez-García et al., 2020 [45] | Meta-analysis of 48 randomized controlled trials | Empaglifozin 10 or 25 mg AND Canagliflozin 100 or 300 mg | 24,782 patients | Variable | ↑ LDL ↑ HDL ↑ total cholesterol ↓ triglycerides |
| Liakos et al., 2014 [61] | Meta-analysis of 10 randomized controlled trials | Empaglifozin 10 or 25 mg | 6203 patients | Variable | ↑ LDL (4.5–6.5%) |
| Neal et al., 2014 [62] | Randomized controlled trial | Canaglifozin 100 or 300 mg | 10,142 patients | Up to 78 weeks | ↑ LDL ↑ HDL |
| Bode et al., 2015 [63] | Phase 3 study | Canaglifozin 100 or 300 mg | 714 patients | 104 weeks | ↑ LDL ↑ HDL ↓ triglycerides |
| Type of Study | Molecule | N° of Patients | Time of Follow-Up | Main Results | |
|---|---|---|---|---|---|
| Ariel et al., 2014 [74] | Prospective study | Liraglutide | 50 patients | 14 weeks | ↓ LDL ↓ non-HDL ↓ total cholesterol ↓ triglycerides ↓ apo-B ↓ apo-B/apo-A1 ratio shift of small LDL lipoproteins towards larger |
| Viswanathan et al., 2007 [86] | Retrospective study | Exenatide 5 mcg | 52 patients | 26 weeks | ↓ total cholesterol ↓ triglycerides |
| Schwartz et al., 2010 [87] | Double-blinded, randomized, placebo-controlled study | Exenatide 10 mcg | 35 patients | Up to 3 weeks | ↓ RLP-cholesterol ↓ RLP triglycerides ↓ triglycerides ↓ apo-B48 ↓ apo-CIII |
| Hasegawa et al., 2018 [88] | Retrospective study | Various | 317 patients | 119 days | ↓ LDL |
| Pi-Sunyer et al., 2015 [89] | Randomized controlled trial | Liraglutide 3.0 mg | 3731 patients | 56 weeks | ↑ HDL ↓ total cholesterol ↓ triglycerides |
| Sun et al., 2015 [90] | Meta-analysis of 35 trials | Exenatide, Liraglutide, and Taspoglutide | 14,340 patients | Al least 8 weeks | ↓ LDL ↓ total cholesterol |
| Buse et al., 2009 [92] (LEAD-6) | Randomized controlled trial | Liraglutide and Exenatide | 464 patients | 26 weeks | ↓ LDL ↓ HDL ↓ total cholesterol ↓ triglycerides ↑ VLDL |
| Buse et al., 2013 [91] (DURATION-6) | Randomized controlled trial | Liraglutide and Exenatide | 911 patients (450 liraglutide, 461 exenatide) | 26 weeks | ↓ LDL ↑ HDL ↓ non-HDL ↓ total cholesterol |
| Liu et al., 2019 [93] | Meta-analysis of 13 trials | Liraglutide | 1187 patients | At least 8 weeks | ↓ triglycerides |
| Sorli et al., 2017 [94] (SUSTAIN 1) | Double-blind randomized trial | Semaglutide 0.5 mg Semaglutide 1.0 mg | 388 patients | 30 weeks | ↓ LDL ↓ total cholesterol ↓ free fatty acids |
| Aroda et al., 2017 [95] (SUSTAIN 4) | Double-blind randomized trial | Semaglutide 0.5 mg Semaglutide 1.0 mg | 1089 patients | 30 weeks | ↓ LDL ↓ total cholesterol ↓ triglycerides |
| Ahmann et al., 2018 [96] (SUSTAIN 3) | Double-blind randomized trial | Semaglutide 1.0 mg Exenatide | 813 patients | 56 weeks | (semaglutide > exenatide) ↓ triglycerides ↓ VLDL cholesterol ↓ free fatty acids |
| Chiquette et al., 2012 [97] (DURATION-1) | Post hoc analysis | Exenatide | 211 patients | 30 weeks | ↓ triglycerides ↓ VLDL cholesterol ↓ apolipoprotein B (apoB) ↓ apo B/apo A ratio |
| Song et al., 2015 [98] | Meta-analysis of 31 trials | Various | Variable | Up to 52 weeks | ↓ LDL ↓ total cholesterol ↓ triglycerides |
| Dar et al., 2022 [99] | Meta-analysis of 57 trials | Various | Variable | Between 12 weeks and 312 weeks | ↑ HDL ↓ total cholesterol |
| Li et al., 2022 [100] | Meta-analysis of 8 trials | Various | 1895 patients | At least 12 weeks | ↓ LDL |
| Type of Study | Molecule | N° of Patients | Time of Follow-Up | Main Results | |
|---|---|---|---|---|---|
| Monami et al., 2012 [119] | Meta-analysis of 17 trials | Alogliptin, Dutogliptin, Linagliptin, Saxagliptin, Sitagliptin, Vildagliptin | Variable | Variable | ↓ total cholesterol ↓ triglycerides |
| Ikegami et al., 2021 [120] | Single-arm trial | Anagliptin | 14 patients | 6 months | ↓ LDL ↓ lathosterol |
| Nishida et al., 2020 [121] | Retrospective study | Sitagliptin, Vildagliptin, Teneligliptin, Alogliptin and Linagliptin | 1809 patients | 3 and 12 months | ↓ HDL (in sitagliptin and vildagliptin users) ↓ total cholesterol and triglycerides (in sitagliptin, vildagliptin, and alogliptin users) |
| Kusunoki et al., 2016 [122] | Prospective study | Alogliptin 25 mg Sitagliptin 100 mg | 129 patients 6 patients | 6 months 12 months | ↓ LDL ↓ total cholesterol ↓ triglycerides non-significant changes in LDL, HDL, and total cholesterol |
| Monami et al., 2012 [123] | Meta-analysis of 18 trials | Alogliptin, Dutogliptin, Linagliptin, Saxagliptin, Sitagliptin, Vildagliptin | Variable | Variable | ↓ total cholesterol ↓ triglycerides vildagliptin > sitagliptin and alogliptin |
| Homma et al., 2017 [124] | Prospective study | Teneligliptin 20 mg | 25 patients | 12 months | ↓ RLP cholesterol ↓ FPG |
| Tremblay et al., 2014 [125] | Randomized controlled trial | Sitagliptin 100 mg | 22 patients | 6 weeks | ↓ triglycerides ↓ apoB-48 ↓ free fatty acids |
| Kakuda et al., 2015 [126] | Prospective study | Anagliptin 200 mg | - | 12 weeks | ↓ LDL ↓ non-HDL cholesterol ↓ RLP cholesterol ↓ total cholesterol ↓ triglycerides ↓ apoB-48 |
| Dar et al., 2022 [99] | Meta-analysis of 57 trials | Variable | Variable | Variable | ↑ HDL Non-significant changes in LDL, total cholesterol, and triglycerides |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piccirillo, F.; Mastroberardino, S.; Nusca, A.; Frau, L.; Guarino, L.; Napoli, N.; Ussia, G.P.; Grigioni, F. Novel Antidiabetic Agents and Their Effects on Lipid Profile: A Single Shot for Several Cardiovascular Targets. Int. J. Mol. Sci. 2023, 24, 10164. https://doi.org/10.3390/ijms241210164
Piccirillo F, Mastroberardino S, Nusca A, Frau L, Guarino L, Napoli N, Ussia GP, Grigioni F. Novel Antidiabetic Agents and Their Effects on Lipid Profile: A Single Shot for Several Cardiovascular Targets. International Journal of Molecular Sciences. 2023; 24(12):10164. https://doi.org/10.3390/ijms241210164
Chicago/Turabian StylePiccirillo, Francesco, Sara Mastroberardino, Annunziata Nusca, Lorenzo Frau, Lorenzo Guarino, Nicola Napoli, Gian Paolo Ussia, and Francesco Grigioni. 2023. "Novel Antidiabetic Agents and Their Effects on Lipid Profile: A Single Shot for Several Cardiovascular Targets" International Journal of Molecular Sciences 24, no. 12: 10164. https://doi.org/10.3390/ijms241210164
APA StylePiccirillo, F., Mastroberardino, S., Nusca, A., Frau, L., Guarino, L., Napoli, N., Ussia, G. P., & Grigioni, F. (2023). Novel Antidiabetic Agents and Their Effects on Lipid Profile: A Single Shot for Several Cardiovascular Targets. International Journal of Molecular Sciences, 24(12), 10164. https://doi.org/10.3390/ijms241210164







