Computational Prediction of Resistance Induced Alanine-Mutation in ATP Site of Epidermal Growth Factor Receptor
Abstract
1. Introduction
2. Results and Discussion
2.1. Validation of the Simulation Parameters
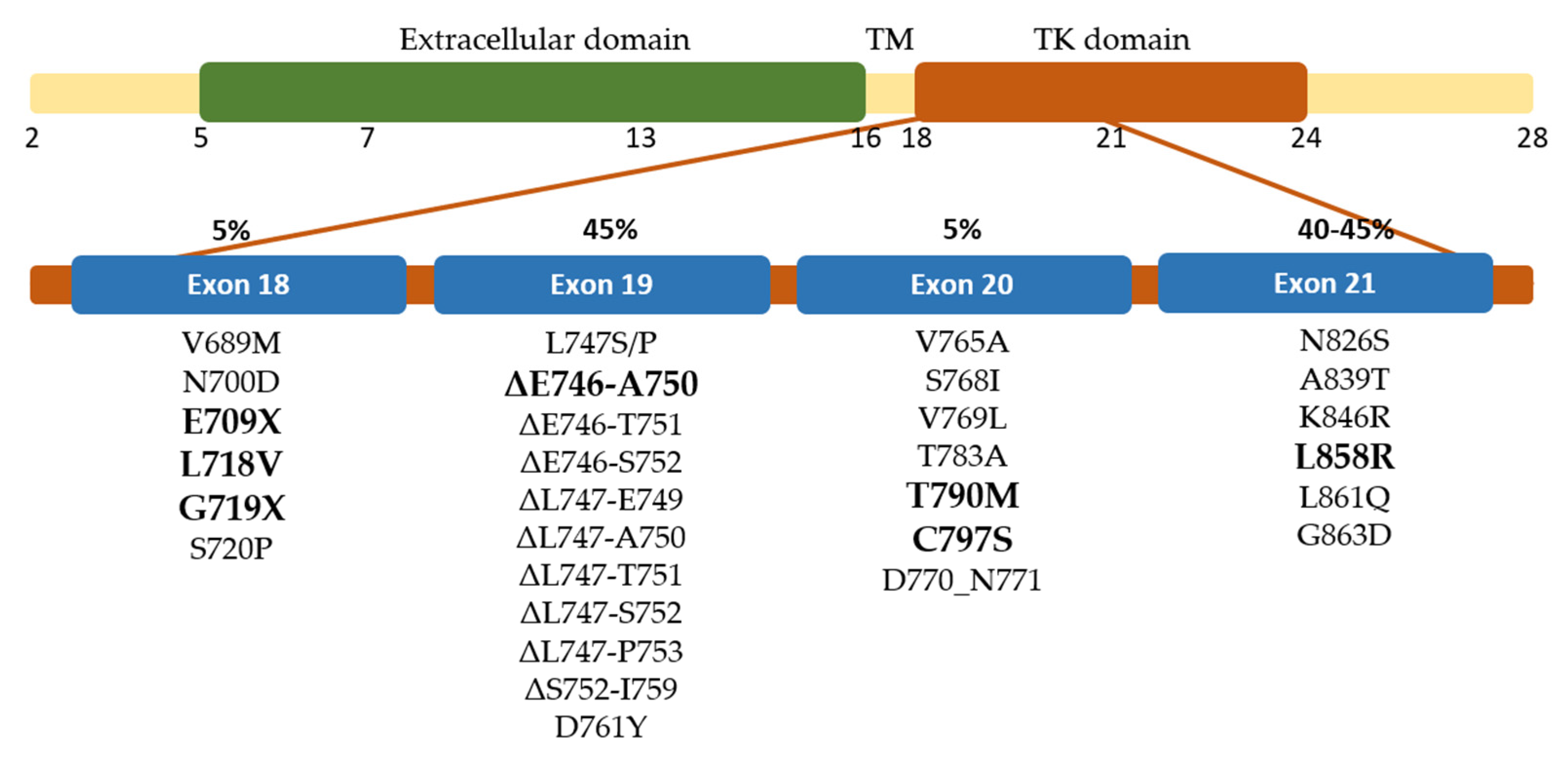
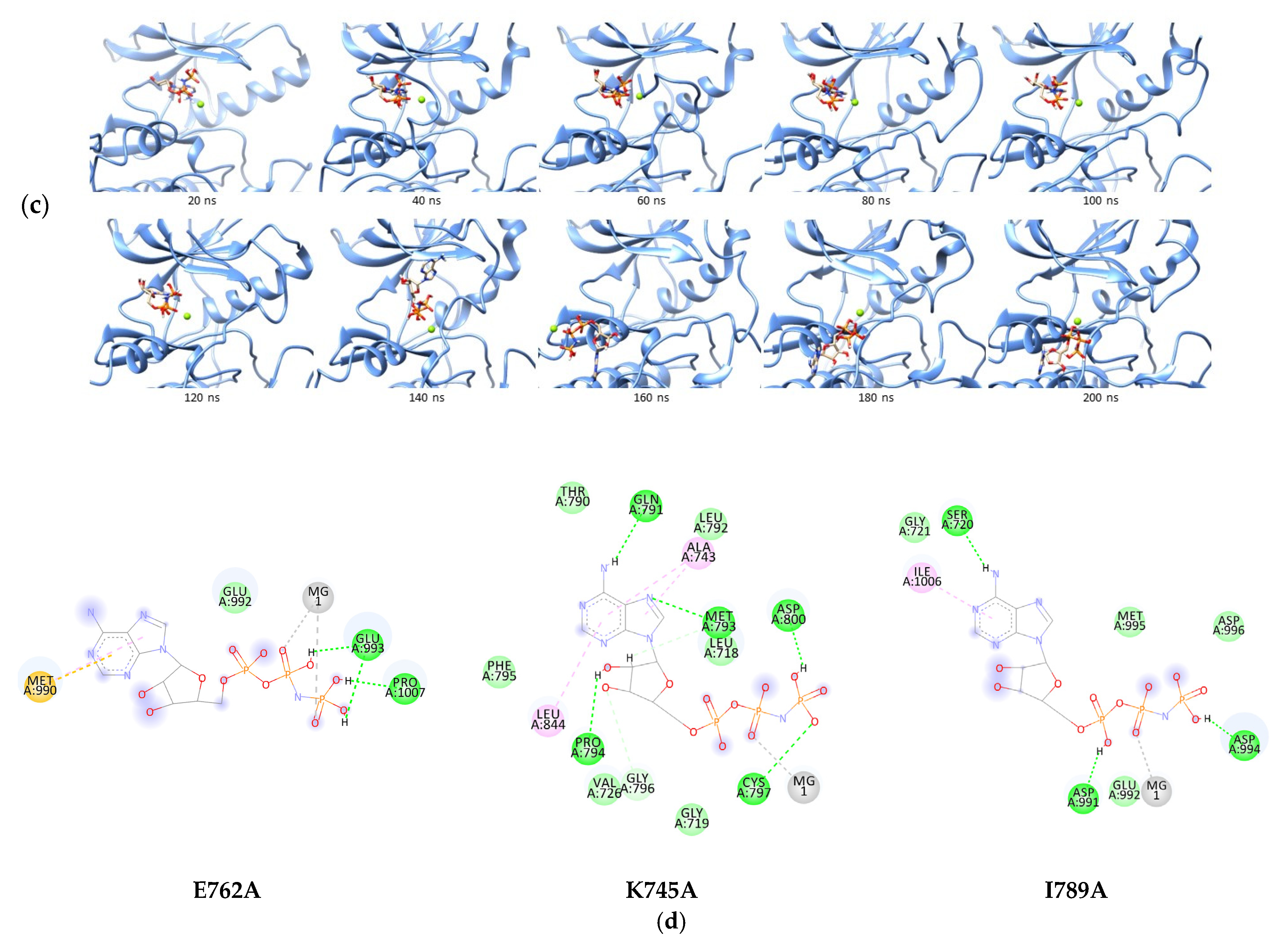
2.2. Interaction Study of ATP Analogue in Well-Known EGFR Mutant
2.3. Binding Study of ATP Analogue in Novel EGFR Mutations
2.4. Binding Study of Erlotinib in Mutated EGFR
3. Materials and Methods
3.1. Macromolecule Preparation
3.2. Ligand Preparation
3.3. Docking Simulation
3.4. Molecular Dynamic (MD) Simulation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Cancer Statistics for the Year 2020: An Overview. Int. J. Cancer 2021, 149, 778–789. [Google Scholar] [CrossRef]
- Cho, J.H. Immunotherapy for Non-Small-Cell Lung Cancer: Current Status and Future Obstacles. Immune. Netw. 2017, 17, 378. [Google Scholar] [CrossRef]
- Howlander, N.; Noone, A.M.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. SEER Cancer Statistics Review, 1975–2018. Available online: https://seer.cancer.gov/csr/1975_2018/ (accessed on 11 September 2022).
- Sharma, S.V.; Bell, D.W.; Settleman, J.; Haber, D.A. Epidermal Growth Factor Receptor Mutations in Lung Cancer. Nat. Rev. Cancer 2007, 7, 169–181. [Google Scholar] [CrossRef]
- Mosseson, Y.; Yarden, Y. Oncogenic Growth Factor Receptors: Implications for Signal Transduction Therapy. Semin. Cancer Biol. 2004, 14, 262–270. [Google Scholar] [CrossRef]
- Yarden, Y.; Sliwkowski, M.X. Untangling the ErbB Signalling Network. Nat. Rev. Mol. Cell Biol. 2001, 2, 127–137. [Google Scholar] [CrossRef]
- de Luca, A.; Carotenuto, A.; Rachiglio, A.; Gallo, M.; Maiello, M.R.; Aldinucci, D.; Pinto, A.; Normanno, N. The Role of the EGFR Signaling in Tumor Microenvironment. J. Cell. Physiol. 2008, 214, 559–567. [Google Scholar] [CrossRef]
- Barker, A.J.; Gibson, K.H.; Grundy, W.; Godfrey, A.A.; Barlow, J.J.; Healy, M.P.; Woodburn, J.R.; Ashton, S.E.; Curry, B.J.; Scarlett, L.; et al. Studies Leading to the Identification of ZD1839 (IressaTM): An Orally Active, Selective Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Targeted to the Treatment of Cancer. Bioorg. Med. Chem. Lett. 2001, 11, 1911–1914. [Google Scholar] [CrossRef]
- Pollack, V.A.; Savage, D.M.; Baker, D.A.; Tsaparikos, K.E.; Sloan, D.E.; Moyer, J.D.; Barbacci, E.G.; Pustilnik, L.R.; Smolarek, T.A.; Davis, J.A.; et al. Inhibition of Epidermal Growth Factor Receptor-Associated Tyrosine Phosphorylation in Human Carcinomas with CP-358,774: Dynamics of Receptor Inhibition in Situ and Antitumor Effects in Athymic Mice. J. Pharmacol. Exp. Ther. 1999, 291, 739–748. [Google Scholar]
- Li, D.; Ambrogio, L.; Shimamura, T.; Kubo, S.; Takahashi, M.; Chirieac, L.R.; Padera, R.F.; Shapiro, G.I.; Baum, A.; Himmelsbach, F.; et al. BIBW2992, an Irreversible EGFR/HER2 Inhibitor Highly Effective in Preclinical Lung Cancer Models. Oncogene 2008, 27, 4702–4711. [Google Scholar] [CrossRef]
- Engelman, J.A.; Zejnullahu, K.; Gale, C.-M.; Lifshits, E.; Gonzales, A.J.; Shimamura, T.; Zhao, F.; Vincent, P.W.; Naumov, G.N.; Bradner, J.E.; et al. PF00299804, an Irreversible Pan-ERBB Inhibitor, Is Effective in Lung Cancer Models with EGFR and ERBB2 Mutations That Are Resistant to Gefitinib. Cancer Res. 2007, 67, 11924–11932. [Google Scholar] [CrossRef]
- Jänne, P.A.; Yang, J.C.-H.; Kim, D.-W.; Planchard, D.; Ohe, Y.; Ramalingam, S.S.; Ahn, M.-J.; Kim, S.-W.; Su, W.-C.; Horn, L.; et al. AZD9291 in EGFR Inhibitor–Resistant Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 372, 1689–1699. [Google Scholar] [CrossRef]
- Riely, G.J.; Pao, W.; Pham, D.; Li, A.R.; Rizvi, N.; Venkatraman, E.S.; Zakowski, M.F.; Kris, M.G.; Ladanyi, M.; Miller, V.A. Clinical Course of Patients with Non–Small Cell Lung Cancer and Epidermal Growth Factor Receptor Exon 19 and Exon 21 Mutations Treated with Gefitinib or Erlotinib. Clin. Cancer Res. 2006, 12, 839–844. [Google Scholar] [CrossRef]
- Kobayashi, S.; Boggon, T.J.; Dayaram, T.; Jänne, P.A.; Kocher, O.; Meyerson, M.; Johnson, B.E.; Eck, M.J.; Tenen, D.G.; Halmos, B. EGFR Mutation and Resistance of Non–Small-Cell Lung Cancer to Gefitinib. New Engl. J. Med. 2005, 352, 786–792. [Google Scholar] [CrossRef]
- Pao, W.; Miller, V.A.; Politi, K.A.; Riely, G.J.; Somwar, R.; Zakowski, M.F.; Kris, M.G.; Varmus, H. Acquired Resistance of Lung Adenocarcinomas to Gefitinib or Erlotinib Is Associated with a Second Mutation in the EGFR Kinase Domain. PLoS Med. 2005, 2, e73. [Google Scholar] [CrossRef]
- Kosaka, T.; Yatabe, Y.; Endoh, H.; Yoshida, K.; Hida, T.; Tsuboi, M.; Tada, H.; Kuwano, H.; Mitsudomi, T. Analysis of Epidermal Growth Factor Receptor Gene Mutation in Patients with Non–Small Cell Lung Cancer and Acquired Resistance to Gefitinib. Clin. Cancer Res. 2006, 12, 5764–5769. [Google Scholar] [CrossRef]
- Harrison, P.T.; Vyse, S.; Huang, P.H. Rare Epidermal Growth Factor Receptor (EGFR) Mutations in Non-Small Cell Lung Cancer. Semin. Cancer Biol. 2020, 61, 167–179. [Google Scholar] [CrossRef]
- Stamos, J.; Sliwkowski, M.X.; Eigenbrot, C. Structure of the Epidermal Growth Factor Receptor Kinase Domain Alone and in Complex with a 4-Anilinoquinazoline Inhibitor. J. Biol. Chem. 2002, 277, 46265–46272. [Google Scholar] [CrossRef]
- Yun, C.-H.; Mengwasser, K.E.; Toms, A.V.; Woo, M.S.; Greulich, H.; Wong, K.-K.; Meyerson, M.; Eck, M.J. The T790M Mutation in EGFR Kinase Causes Drug Resistance by Increasing the Affinity for ATP. Proc. Natl. Acad. Sci. USA 2008, 105, 2070–2075. [Google Scholar] [CrossRef]
- Vikis, H.; Sato, M.; James, M.; Wang, D.; Wang, Y.; Wang, M.; Jia, D.; Liu, Y.; Bailey-Wilson, J.E.; Amos, C.I.; et al. EGFR-T790M Is a Rare Lung Cancer Susceptibility Allele with Enhanced Kinase Activity. Cancer Res. 2007, 67, 4665–4670. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Togashi, Y.; Yatabe, Y.; Mizuuchi, H.; Jangchul, P.; Kondo, C.; Shimoji, M.; Sato, K.; Suda, K.; Tomizawa, K.; et al. EGFR Exon 18 Mutations in Lung Cancer: Molecular Predictors of Augmented Sensitivity to Afatinib or Neratinib as Compared with First- or Third-Generation TKIs. Clin. Cancer Res. 2015, 21, 5305–5313. [Google Scholar] [CrossRef]
- Yun, C.-H.; Boggon, T.J.; Li, Y.; Woo, M.S.; Greulich, H.; Meyerson, M.; Eck, M.J. Structures of Lung Cancer-Derived EGFR Mutants and Inhibitor Complexes: Mechanism of Activation and Insights into Differential Inhibitor Sensitivity. Cancer Cell 2007, 11, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Shan, Y.; Eastwood, M.P.; Zhang, X.; Kim, E.T.; Arkhipov, A.; Dror, R.O.; Jumper, J.; Kuriyan, J.; Shaw, D.E. Oncogenic Mutations Counteract Intrinsic Disorder in the EGFR Kinase and Promote Receptor Dimerization. Cell 2012, 149, 860–870. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.-H.; Yang, C.-T.; Shih, J.-Y.; Huang, M.-S.; Su, W.-C.; Lai, R.-S.; Wang, C.-C.; Hsiao, S.-H.; Lin, Y.-C.; Ho, C.-L.; et al. Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Treatment Response in Advanced Lung Adenocarcinomas with G719X/L861Q/S768I Mutations. J. Thorac. Oncol. 2015, 10, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Morrison, K.L.; Weiss, G.A. Combinatorial Alanine-Scanning. Curr. Opin. Chem. Biol. 2001, 5, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Buelens, F.P.; Leonov, H.; de Groot, B.L.; Grubmüller, H. ATP–Magnesium Coordination: Protein Structure-Based Force Field Evaluation and Corrections. J. Chem. Theory Comput. 2021, 17, 1922–1930. [Google Scholar] [CrossRef]
- Tamirat, M.Z.; Kurppa, K.J.; Elenius, K.; Johnson, M.S. Structural Basis for the Functional Changes by EGFR Exon 20 Insertion Mutations. Cancers 2021, 13, 1120. [Google Scholar] [CrossRef]
- Barlesi, F.; Mazieres, J.; Merlio, J.-P.; Debieuvre, D.; Mosser, J.; Lena, H.; Ouafik, L.; Besse, B.; Rouquette, I.; Westeel, V.; et al. Routine Molecular Profiling of Patients with Advanced Non-Small-Cell Lung Cancer: Results of a 1-Year Nationwide Programme of the French Cooperative Thoracic Intergroup (IFCT). Lancet 2016, 387, 1415–1426. [Google Scholar] [CrossRef]
- Lynch, T.J.; Bell, D.W.; Sordella, R.; Gurubhagavatula, S.; Okimoto, R.A.; Brannigan, B.W.; Harris, P.L.; Haserlat, S.M.; Supko, J.G.; Haluska, F.G.; et al. Activating Mutations in the Epidermal Growth Factor Receptor Underlying Responsiveness of Non–Small-Cell Lung Cancer to Gefitinib. N. Engl. J. Med. 2004, 350, 2129–2139. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.-E.; Jung, J.-W.; Oh, S.-J.; Park, M.-J.; Shon, Y.-J.; Choi, K.-H.; Jeong, E.-T.; Kim, H.-R. Transformation to Small Cell Lung Cancer as an Acquired Resistance Mechanism in EGFR -Mutant Lung Adenocarcinoma: A Case Report of Complete Response to Etoposide and Cisplatin. Tumori J. 2015, 101, e96–e98. [Google Scholar] [CrossRef]
- Sequist, L.V.; Waltman, B.A.; Dias-Santagata, D.; Digumarthy, S.; Turke, A.B.; Fidias, P.; Bergethon, K.; Shaw, A.T.; Gettinger, S.; Cosper, A.K.; et al. Genotypic and Histological Evolution of Lung Cancers Acquiring Resistance to EGFR Inhibitors. Sci. Transl. Med. 2011, 3, 75ra26. [Google Scholar] [CrossRef] [PubMed]
- Jackman, D.; Pao, W.; Riely, G.J.; Engelman, J.A.; Kris, M.G.; Jänne, P.A.; Lynch, T.; Johnson, B.E.; Miller, V.A. Clinical Definition of Acquired Resistance to Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2010, 28, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Reguart, N.; Remon, J. Common EGFR -Mutated Subgroups (Del19/L858R) in Advanced Non-Small-Cell Lung Cancer: Chasing Better Outcomes with Tyrosine Kinase Inhibitors. Future Oncol. 2015, 11, 1245–1257. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Wu, Y.-L.; Chen, G.; Feng, J.; Liu, X.-Q.; Wang, C.; Zhang, S.; Wang, J.; Zhou, S.; Ren, S.; et al. Erlotinib versus Chemotherapy as First-Line Treatment for Patients with Advanced EGFR Mutation-Positive Non-Small-Cell Lung Cancer (OPTIMAL, CTONG-0802): A Multicentre, Open-Label, Randomised, Phase 3 Study. Lancet Oncol. 2011, 12, 735–742. [Google Scholar] [CrossRef]
- Rosell, R.; Carcereny, E.; Gervais, R.; Vergnenegre, A.; Massuti, B.; Felip, E.; Palmero, R.; Garcia-Gomez, R.; Pallares, C.; Sanchez, J.M.; et al. Erlotinib versus Standard Chemotherapy as First-Line Treatment for European Patients with Advanced EGFR Mutation-Positive Non-Small-Cell Lung Cancer (EURTAC): A Multicentre, Open-Label, Randomised Phase 3 Trial. Lancet Oncol. 2012, 13, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Tsao, M.-S.; Sakurada, A.; Cutz, J.-C.; Zhu, C.-Q.; Kamel-Reid, S.; Squire, J.; Lorimer, I.; Zhang, T.; Liu, N.; Daneshmand, M.; et al. Erlotinib in Lung Cancer—Molecular and Clinical Predictors of Outcome. N. Engl. J. Med. 2005, 353, 133–144. [Google Scholar] [CrossRef]
- Kosaka, T.; Yamaki, E.; Mogi, A.; Kuwano, H. Mechanisms of Resistance to EGFR TKIs and Development of a New Generation of Drugs in Non-Small-Cell Lung Cancer. J. Biomed. Biotechnol. 2011, 2011, 165214. [Google Scholar] [CrossRef]
- Oxnard, G.R.; Janjigian, Y.Y.; Arcila, M.E.; Sima, C.S.; Kass, S.L.; Riely, G.J.; Pao, W.; Kris, M.G.; Ladanyi, M.; Azzoli, C.G.; et al. Maintained Sensitivity to EGFR Tyrosine Kinase Inhibitors in EGFR -Mutant Lung Cancer Recurring after Adjuvant Erlotinib or Gefitinib. Clin. Cancer Res. 2011, 17, 6322–6328. [Google Scholar] [CrossRef]
- Nasab, R.; Mansourian, M.; Hassanzadeh, F.; Shahlaei, M. Exploring the Interaction between Epidermal Growth Factor Receptor Tyrosine Kinase and Some of the Synthesized Inhibitors Using Combination of In-Silico and in-Vitro Cytotoxicity Methods. Res. Pharm. Sci. 2018, 13, 509. [Google Scholar] [CrossRef]
- Polychronidou, G.; Papakotoulas, P. Long-Term Treatment with Erlotinib for EGFR Wild-Type Non-Small Cell Lung Cancer: A Case Report. Case Rep. Oncol. 2013, 6, 189–196. [Google Scholar] [CrossRef]
- Amelia, T.; Kartasasmita, R.E.; Ohwada, T.; Tjahjono, D.H. Structural Insight and Development of EGFR Tyrosine Kinase Inhibitors. Molecules 2022, 27, 819. [Google Scholar] [CrossRef] [PubMed]
- Dassault Systèmes, BIOVIA Discovery Studio Visualizer; BIOVIA: San Diego, CA, USA, 2019.
- Jia, Y.; Yun, C.-H.; Park, E.; Ercan, D.; Manuia, M.; Juarez, J.; Xu, C.; Rhee, K.; Chen, T.; Zhang, H.; et al. Overcoming EGFR(T790M) and EGFR(C797S) Resistance with Mutant-Selective Allosteric Inhibitors. Nature 2016, 534, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Frisch, M.J.; Trucks, G.W.; Schlegel, H.B.; Scuseria, G.E.; Robb, M.A.; Cheeseman, J.R.; Scalmani, G.; Barone, V.; Petersson, G.A.; Nakatsuji, H.; et al. Gaussian 09, Revision A.02; Gaussian, Inc.: Wallingford, CT, USA, 2009. [Google Scholar]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated Docking with Selective Receptor Flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef]
- Case, D.S.; Betz, R.M.; Cerutti, D.S.; Cheatham, I.T.E.; Darden, T.A.; Duke, R.E.; Giese, T.J.; Gohlke, H.; Goetz, A.W.; Homeyer, N.; et al. AMBER 2016; University of California: San Fransisco, CA, USA, 2016. [Google Scholar]
- Wang, J.; Wang, W.; Kollman, P.A.; Case, D.A. Automatic Atom Type and Bond Type Perception in Molecular Mechanical Calculations. J. Mol. Graph. Model 2006, 25, 247–260. [Google Scholar] [CrossRef]
- Wang, J.; Wolf, R.M.; Caldwell, J.W.; Kollman, P.A.; Case, D.A. Development and Testing of a General Amber Force Field. J. Comput. Chem. 2004, 25, 1157–1174. [Google Scholar] [CrossRef]
- Maier, J.A.; Martinez, C.; Kasavajhala, K.; Wickstrom, L.; Hauser, K.E.; Simmerling, C. Ff14SB: Improving the Accuracy of Protein Side Chain and Backbone Parameters from Ff99SB. J. Chem. Theory Comput. 2015, 11, 3696–3713. [Google Scholar] [CrossRef] [PubMed]
- Grotz, K.K.; Cruz-León, S.; Schwierz, N. Optimized Magnesium Force Field Parameters for Biomolecular Simulations with Accurate Solvation, Ion-Binding, and Water-Exchange Properties. J. Chem. Theory Comput. 2021, 17, 2530–2540. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.R.; McGee, T.D.; Swails, J.M.; Homeyer, N.; Gohlke, H.; Roitberg, A.E. MMPBSA.Py: An Efficient Program for End-State Free Energy Calculations. J. Chem. Theory Comput. 2012, 8, 3314–3321. [Google Scholar] [CrossRef]
- Sun, H.; Li, Y.; Shen, M.; Tian, S.; Xu, L.; Pan, P.; Guan, Y.; Hou, T. Assessing the Performance of MM/PBSA and MM/GBSA Methods. 5. Improved Docking Performance Using High Solute Dielectric Constant MM/GBSA and MM/PBSA Rescoring. Phys. Chem. Chem. Phys. 2014, 16, 22035–22045. [Google Scholar] [CrossRef]
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-alkyl.
, pi-alkyl.
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-alkyl.
, pi-alkyl.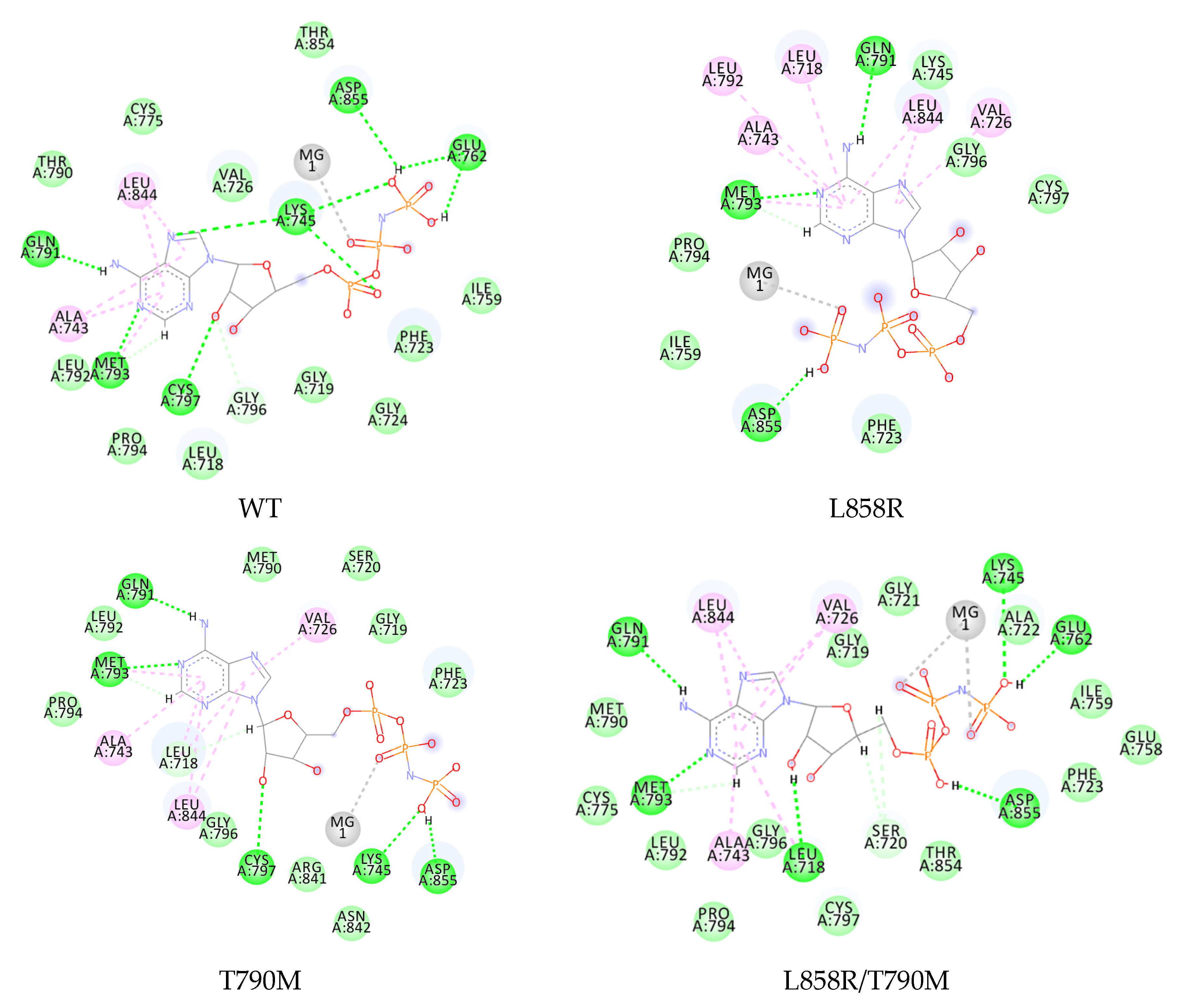
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sigma;
, pi-sigma;  , pi-sulfur;
, pi-sulfur;  , pi-alkyl.
, pi-alkyl.
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sigma;
, pi-sigma;  , pi-sulfur;
, pi-sulfur;  , pi-alkyl.
, pi-alkyl.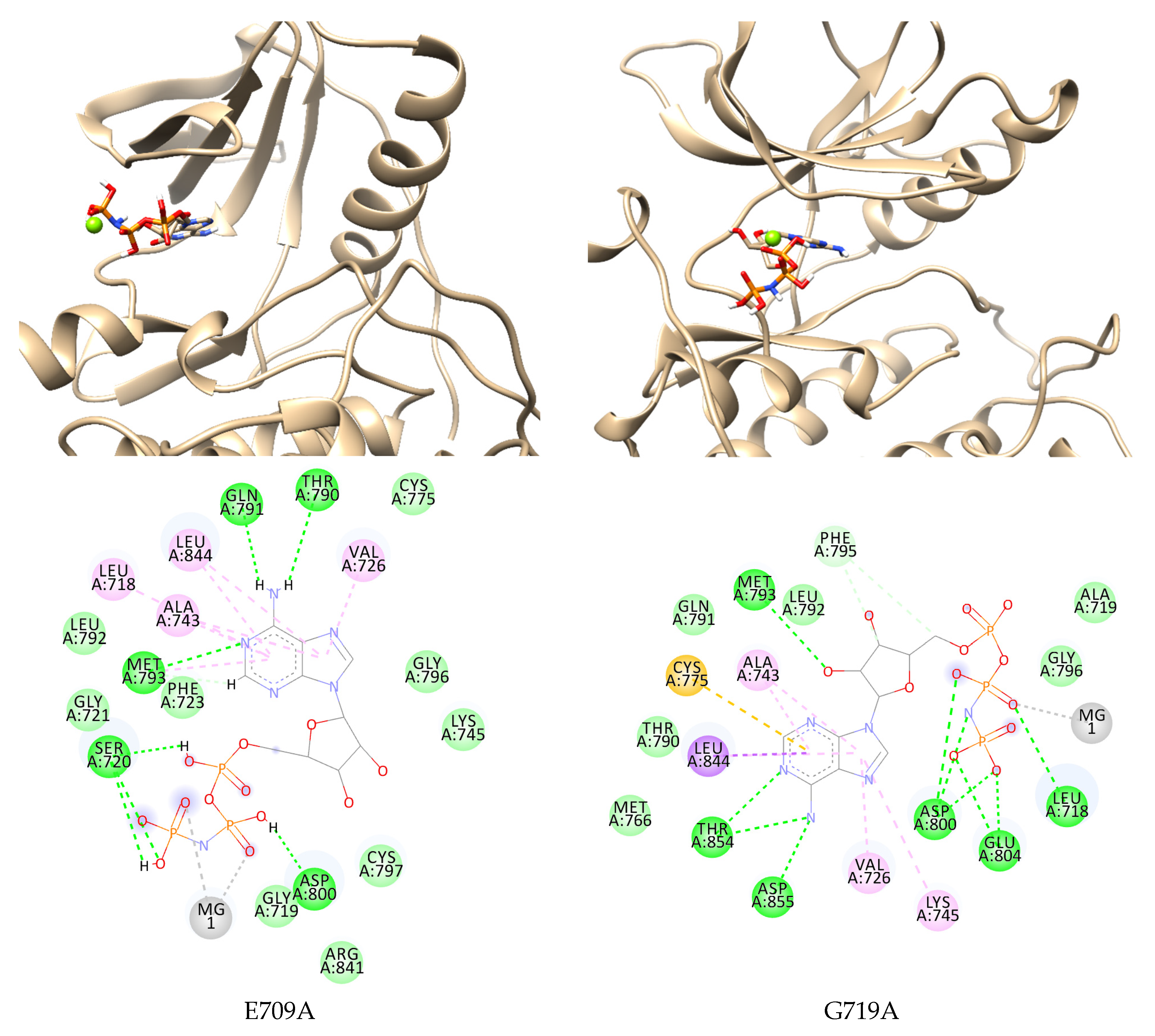

 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sulfur;
, pi-sulfur;  , pi-alkyl.
, pi-alkyl.
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sulfur;
, pi-sulfur;  , pi-alkyl.
, pi-alkyl.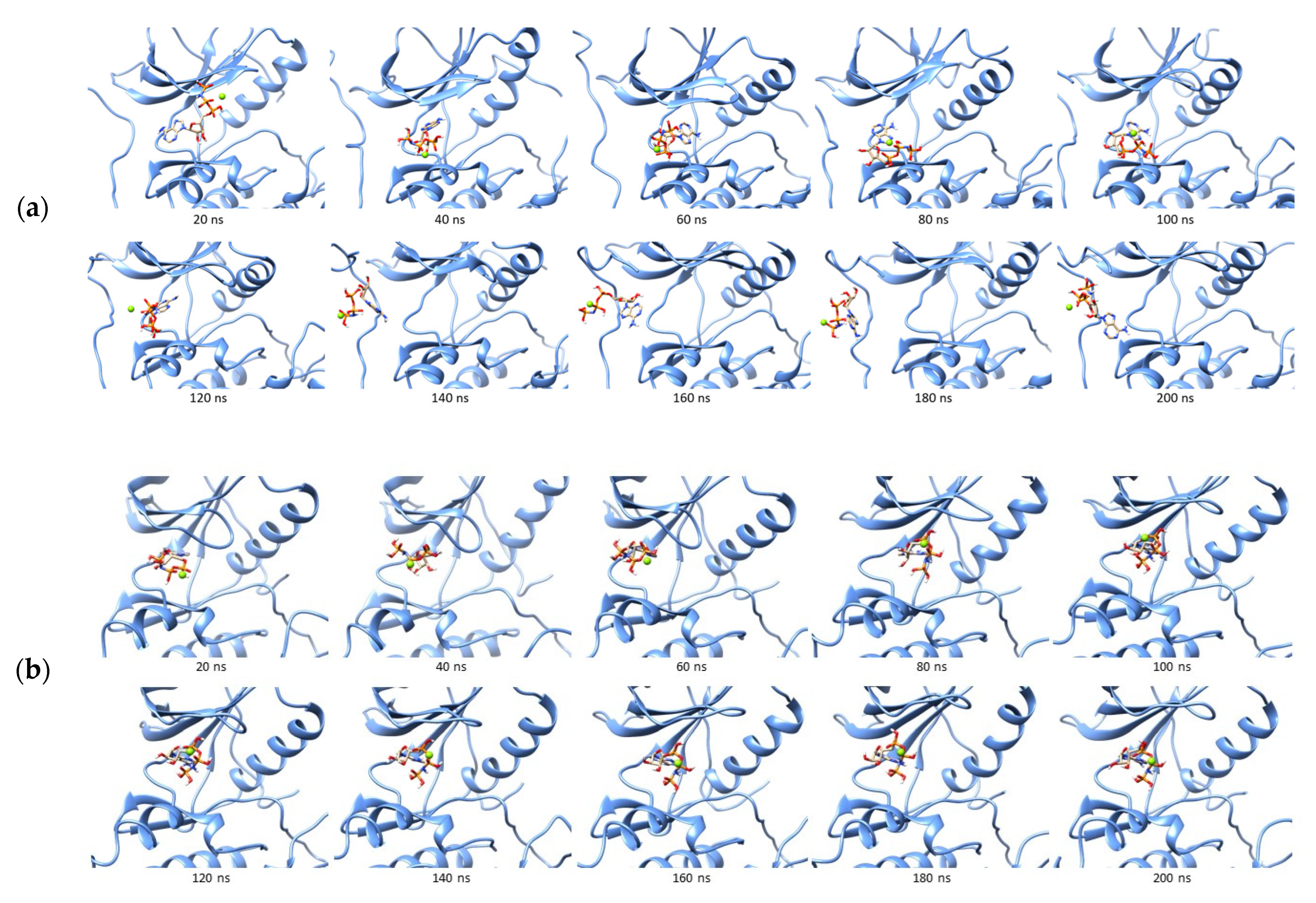
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sigma;
, pi-sigma;  , pi-alkyl.
, pi-alkyl.
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sigma;
, pi-sigma;  , pi-alkyl.
, pi-alkyl.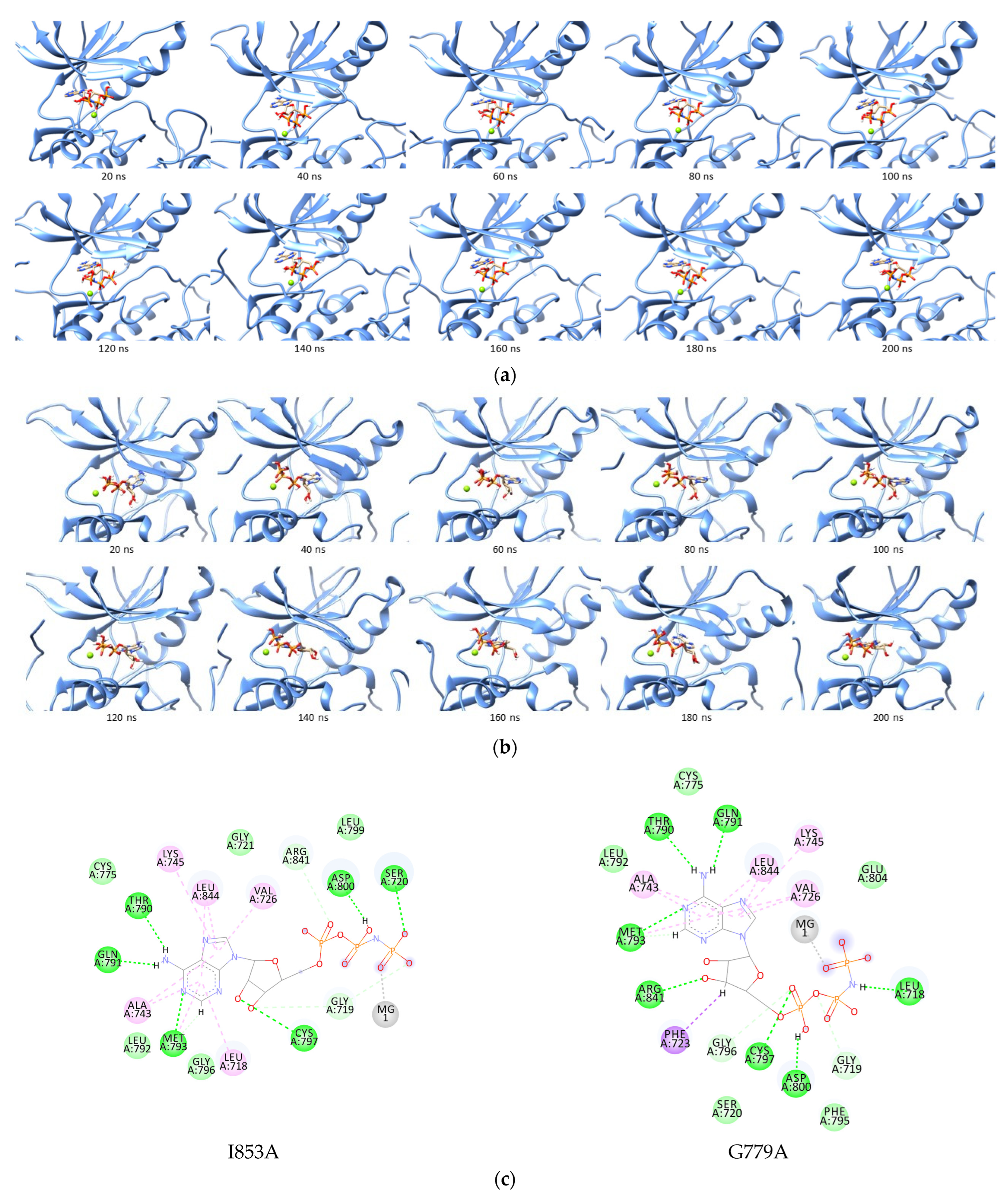
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-alkyl.
, pi-alkyl.
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-alkyl.
, pi-alkyl.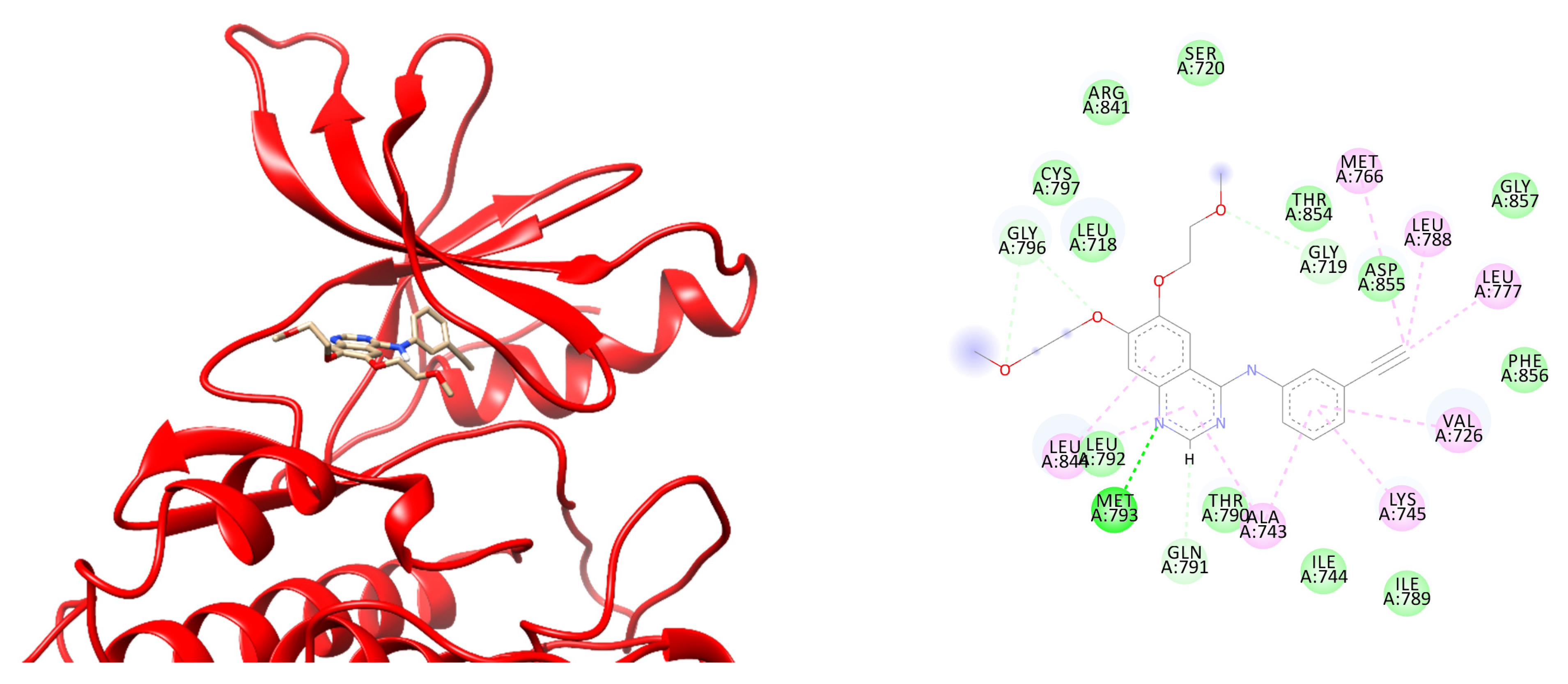
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sulfur;
, pi-sulfur;  , pi-alkyl).
, pi-alkyl).
 , hydrogen bond;
, hydrogen bond;  , van der Waals;
, van der Waals;  , metal acceptor;
, metal acceptor;  , pi-sulfur;
, pi-sulfur;  , pi-alkyl).
, pi-alkyl).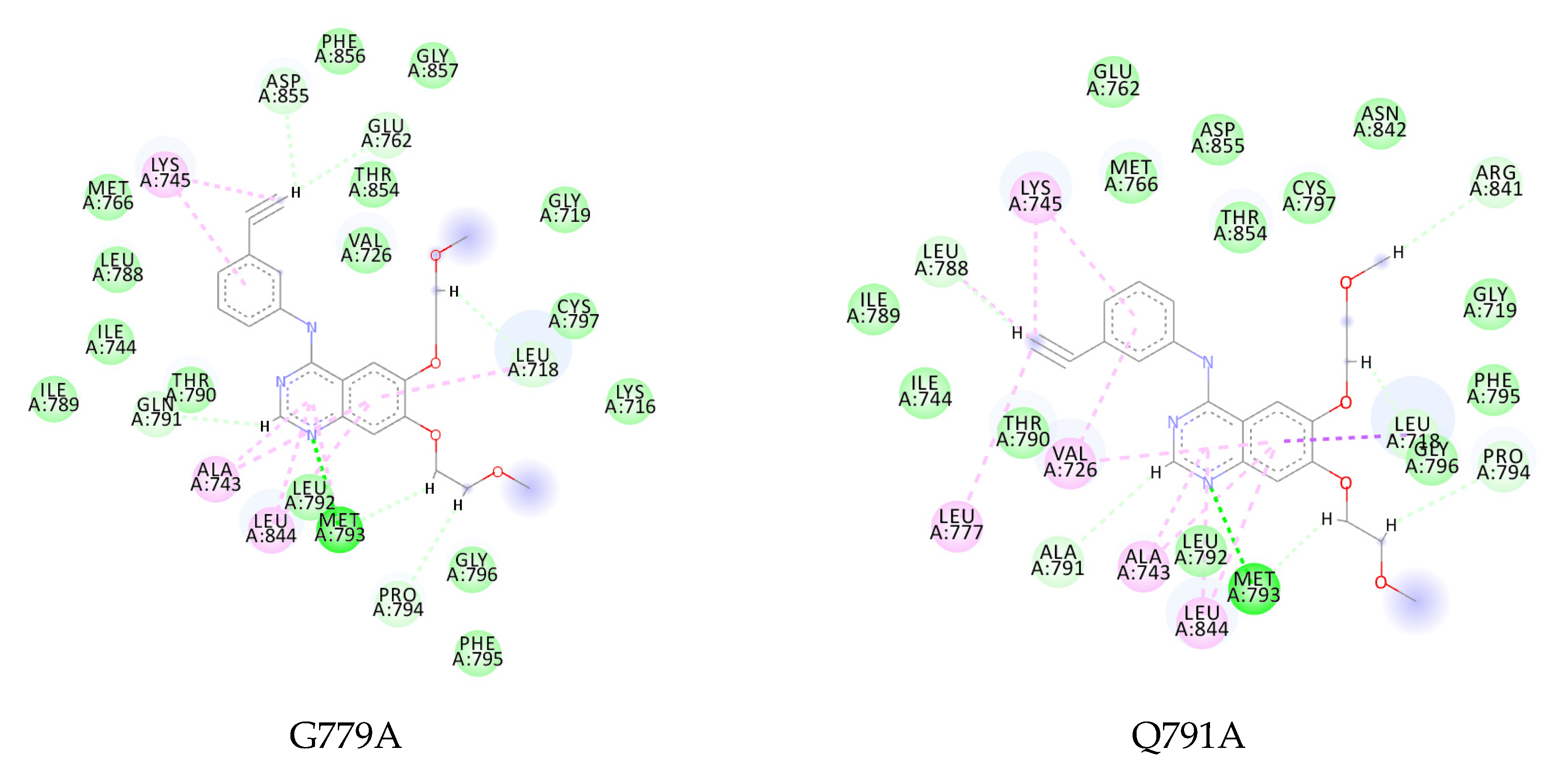

| Ligand | EGFR | ΔG (kcal/mol) | SD | ΔΔG to Wildtype |
|---|---|---|---|---|
| ATP | Wild-type | −27.4416 | 3.3357 | 0 |
| T790M | −29.5109 | 2.9640 | −2.0693 | |
| L858R | −15.5423 | 5.0081 | 11.8993 | |
| L858R-T790M | −26.3177 | 3.8815 | 1.1239 | |
| E709A | −32.1810 | 2.6739 | −4.7394 | |
| G719A | −32.9977 | 3.4104 | −5.5561 |
| EGFR | ΔG * | SD | ΔΔG ** | EGFR | ΔG * | SD | ΔΔG ** | ||
|---|---|---|---|---|---|---|---|---|---|
| V726A | −24.5951 | ± | 6.8073 | 2.8465 | Q791A | −34.8260 | ± | 2.9055 | −7.3844 |
| Y727A | −26.5902 | ± | 2.9467 | 0.8514 | L792A | −30.3337 | ± | 3.0148 | −2.8321 |
| P741A | −23.3618 | ± | 4.0048 | 4.0798 | M793A | −26.1200 | ± | 3.1922 | 1.3216 |
| V742A | −24.4672 | ± | 4.1159 | 2.9744 | F795A | −20.9834 | ± | 3.6914 | 6.4582 |
| K745A | −27.2926 | ± | 2.9010 | 0.1490 | R841A | −29.2160 | ± | 3.3257 | −1.7744 |
| R748A | −25.5706 | ± | 5.4211 | 1.8710 | N842A | −29.4135 | ± | 2.2418 | −1.9719 |
| E762A | −4.2624 | ± | 4.7396 | 23.1792 | V843A | −29.0340 | ± | 2.3082 | −1.5924 |
| C775A | −15.0233 | ± | 4.9797 | 12.4183 | L844A | −26.3112 | ± | 3.7357 | 1.1304 |
| L777A | −8.3795 | ± | 4.8769 | 19.0621 | V845A | −18.5851 | ± | 4.6366 | 8.8565 |
| L778A | −24.5564 | ± | 3.7146 | 2.8852 | K852A | −23.0544 | ± | 4.1278 | 4.3872 |
| G779A | −35.6042 | ± | 3.2002 | −8.1626 | I853A | −36.8969 | ± | 3.2789 | −9.4553 |
| L788A | −11.6746 | ± | 3.5942 | 15.7670 | D855A | −28.6598 | ± | 2.8774 | −1.2182 |
| I789A | −9.6311 | ± | 6.2091 | 17.8105 |
| EGFR | ΔG * | SD | ΔΔG ** | EGFR | ΔG * | SD | ΔΔG ** | ||
|---|---|---|---|---|---|---|---|---|---|
| Wild-type | −33.5815 | ± | 4.4701 | 0 | I789A | −30.2833 | ± | 4.1253 | 3.2982 |
| V726A | −25.3940 | ± | 4.2140 | 8.1875 | Q791A | −29.8615 | ± | 4.3156 | 3.7200 |
| Y727A | −31.0579 | ± | 4.7024 | 2.5236 | L792A | −31.7232 | ± | 4.1862 | 1.8583 |
| P741A | −31.2215 | ± | 4.1350 | 2.3600 | M793A | −25.6215 | ± | 4.1862 | 7.9600 |
| V742A | −19.3823 | ± | 6.4425 | 14.1992 | F795A | −31.0544 | ± | 4.1622 | 2.5271 |
| K745A | −27.3411 | ± | 5.1047 | 6.2404 | R841A | −33.6124 | ± | 4.5257 | −0.0309 |
| R748A | −26.3685 | ± | 3.9220 | 7.2130 | N842A | −29.6648 | ± | 4.0082 | 3.9167 |
| E762A | −29.8702 | ± | 3.9274 | 3.7113 | V843A | −32.1735 | ± | 4.7292 | 1.4080 |
| C775A | −29.7660 | ± | 4.0230 | 3.8155 | L844A | −30.1431 | ± | 3.4659 | 3.4384 |
| L777A | −28.8312 | ± | 3.7831 | 4.7503 | V845A | −32.0817 | ± | 4.6266 | 1.4998 |
| L778A | −29.5240 | ± | 4.2194 | 4.0575 | K852A | −29.8120 | ± | 4.2821 | 3.7695 |
| G779A | −27.8010 | ± | 4.3619 | 5.7805 | I853A | −32.5858 | ± | 4.1526 | 0.9957 |
| L788A | −28.4853 | ± | 5.4903 | 5.0962 | D855A | −27.9652 | ± | 3.7118 | 5.6163 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amelia, T.; Setiawan, A.N.; Kartasasmita, R.E.; Ohwada, T.; Tjahjono, D.H. Computational Prediction of Resistance Induced Alanine-Mutation in ATP Site of Epidermal Growth Factor Receptor. Int. J. Mol. Sci. 2022, 23, 15828. https://doi.org/10.3390/ijms232415828
Amelia T, Setiawan AN, Kartasasmita RE, Ohwada T, Tjahjono DH. Computational Prediction of Resistance Induced Alanine-Mutation in ATP Site of Epidermal Growth Factor Receptor. International Journal of Molecular Sciences. 2022; 23(24):15828. https://doi.org/10.3390/ijms232415828
Chicago/Turabian StyleAmelia, Tasia, Aderian Novito Setiawan, Rahmana Emran Kartasasmita, Tomohiko Ohwada, and Daryono Hadi Tjahjono. 2022. "Computational Prediction of Resistance Induced Alanine-Mutation in ATP Site of Epidermal Growth Factor Receptor" International Journal of Molecular Sciences 23, no. 24: 15828. https://doi.org/10.3390/ijms232415828
APA StyleAmelia, T., Setiawan, A. N., Kartasasmita, R. E., Ohwada, T., & Tjahjono, D. H. (2022). Computational Prediction of Resistance Induced Alanine-Mutation in ATP Site of Epidermal Growth Factor Receptor. International Journal of Molecular Sciences, 23(24), 15828. https://doi.org/10.3390/ijms232415828







