Abstract
Both physiological and pathological aging processes induce brain alterations especially affecting the speed of processing, working memory, conceptual reasoning and executive functions. Many therapeutic approaches to reduce the impact of brain aging on cognitive functioning have been tested; unfortunately, there are no satisfactory results as a single therapy. As aging is partly contributed by free radical reactions, it has been proposed that exogenous antioxidants could have a positive impact on both aging and its associated manifestations. The aim of this report is to provide a summary and a subsequent review of the literature evidence on the role of antioxidants in preventing and improving cognition in the aging brain. Manipulation of endogenous cellular defense mechanisms through nutritional antioxidants or pharmacological compounds represents an innovative approach to therapeutic intervention in diseases causing brain tissue damage, such as neurodegeneration. Coherently with this notion, antioxidants, especially those derived from the Mediterranean diet such as hydroxytyrosol and resveratrol, seem to be able to delay and modulate the cognitive brain aging processes and decrease the occurrence of its effects on the brain. The potential preventive activity of antioxidants should be evaluated in long-term exposure clinical trials, using preparations with high bioavailability, able to bypass the blood-brain barrier limitation, and that are well standardized.
Keywords:
aging; antioxidants; cognition; epigenetic; hydroxytyrosol; Mediterranean diet; oxidative stress; resveratrol 1. Introduction
It is well established that both the physiological and pathological aging processes induce brain alterations affecting, particularly, some aspects of cognition, especially the speed of processing, working memory, conceptual reasoning, and executive functions [1,2,3]. Even though the majority of the aged people retain relatively well-preserved health, this trend reflects on numerous individuals, especially those with disability and fragility [4,5,6]. However, there is significant heterogeneity among older adults in the rate of decline in some abilities, such as the measures of perceptual reasoning and processing speed [7]. More precisely, age-related brain deterioration results in a scaffolding of new compensatory networks, depending on the factors that positively and negatively influence cognition. This decline is mostly associated with a dysfunction of the pre-frontal cortex, which, being especially vulnerable, tends to atrophy prematurely while aging, causing a reorganization of brain functioning, which often occurs with hemispheric lateralization of the solicited regions with more frequent bilateral brain activation [8,9,10]. Furthermore, many pathologies, such as common comorbidities in elder people, negatively affect cognition, though further studies are required to better understand how aging plays a role and how brain structure and brain function might mediate the relationship between comorbidities and age on cognition [11,12,13].
Many therapeutic approaches (cognitive and physical training, pharmacology, etc.) have been tested in literature to reduce the impact of brain aging on cognitive functioning, but nothing has been proven to bring satisfactory results as a single therapy [4]. As aging is partly contributed by free radical reactions, it has been proposed that exogenous antioxidants should have a positive impact on both aging and its associated manifestations [14,15].
This report aims to provide a summary and a subsequent review of literature evidence on the role of antioxidants in preventing and improving cognition in the aging brain.
2. Aging
2.1. General Mechanisms
Aging is an inevitable time-dependent decline of all biological functions, driven by a genetic program and linked to an increased risk for numerous diseases [16]. It has been suggested that the activation of multiple pathways due to the altered function of quality control systems monitoring the performance of the genomic and proteomic repertoire of the cells plays a major role [17]. In 2013, a total of nine biological hallmarks of aging have been identified: genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, mitochondrial dysfunction, cellular senescence, deregulated nutrient sensing, stem cell exhaustion, and altered intercellular communication [18,19,20].
Actually, most chronic neurodegenerative human diseases (Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, etc.) are inherently associated with increasing age, as cells with senescence features have been detected in both brains of elders and patients with neurodegenerative disease, where they promote dysfunction [21,22]. In fact, senescent cells are characterized by sustained cell cycle arrest and production of a distinct senescence-associated secretory phenotype, and they accumulate with age and age-related diseases throughout the body, where they actively promote tissue decay. Human aging and neurodegenerative diseases comprise a series of changes at the molecular, cellular, physiological, and functional levels [23].
Interestingly, among the functional alterations, the cognitive, emotional, and social deficiencies are very common and are mostly linked to brain alterations. Furthermore, among the cellular changes, a major role is played by oxidative stress alterations. Since these alterations are mostly inevitable, it has been suggested that the main objectives of medical interventions for elders and by extension to neurodegenerative disease patients should focus on maximizing the ability of an individual to function in his environment, maintaining autonomy and maximizing quality of life [23].
2.2. Brain Aging
Aging affects the brain and cognition because of multiple heterogeneous etiologies including alterations at various levels: molecular and cellular, vasculature, gross morphology, and cognition [24]. Numerous are the molecular and cellular changes brought by the aging process in the brain; these are characterized by a gradual reduction of neurophysiological functions, impaired adaptive neuroplasticity, dysregulated neuronal Ca2+ homeostasis, neuroinflammation, and oxidative alteration of molecules and organelles [25].
Brain aging-associated cellular and molecular changes are often related to neurodegenerative diseases due to increased oxidative stress, inflammation, energy metabolism disorders such as deregulated autophagy, mitochondrial dysfunction, and modifications of IGF-1, mTOR, ROS, AMPK, SIRTs, and p53 as central modulators of the metabolic control [26]. Interestingly, calorie restriction, physical exercise, and mental activities seem to be able to extend lifespan and increase nervous system resistance to age-associated neurodegenerative diseases, increasing protection against ROS generation, maintaining cellular Ca2+ homeostasis, and inhibiting apoptosis.
Our vascular changes and our blood pressure tend to rise, increasing the risk of stroke and ischemia and causing white matter lesions of various sizes. Aging blood vessels are characterized by shrunk blood flow, potentially leading to organ atrophy and loss of function, that in the case of cerebral vascular aging can cause loss of the blood–brain barrier integrity, eventually resulting in cognitive and sensorimotor decline as well as diseases such as vascular cognitive impairment and dementia (VCID) due to chronic cerebral hypoperfusion [27] (see Figure 1).
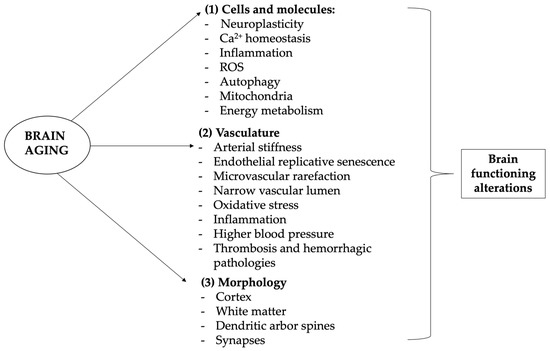
Figure 1.
Brain-related aging mechanisms. Aging and neurodegenerative diseases are associated with cognitive, emotional, and social deficiencies mostly linked to brain alterations. Aging of the brain differs from other organs aging, as neurons are highly differentiated postmitotic cells, so that their lifespan is mostly equal to the lifespan of the entire organism. Brain aging is complex and heterogeneous but it substantially involves four levels of involvement: molecular and cellular, vasculature, gross morphology, and cognition. (1) Cellular and molecular changes involve especially (but not only) calcium-altered homeostasis, leading to hormone and neurotransmission changes, as well as ROS production, energy metabolism alteration, and neuroinflammation, which lead to progressive DNA and macromolecules damage, mitochondrial dysfunction, inflammation reaction, apoptosis, and epigenetic modifications; (2) vascular alterations and related disorders are very common and one of the leading causes of neurological disorders, morbidity, and mortality in older patients, manifesting its influence both systemically and on the more specific brain context; (3) with age come modifications of brain structure, with the frontal and pre-frontal lobes more influenced and occipital ones less affected; (4) cellular and molecular changes, but also vascular alterations and brain morphology modifications, are associated to functional impairment, which manifests mainly with memory loss and slight cognitive impairment but can lead to major pathological diseases such as dementia. In this context, antioxidants may play a major role in preventing cognitive aging problems. ROS—reactive oxygen species. Images have been created by using the functionalities of Microsoft PowerPoint 365 Version 2112. https://www.microsoft.com/microsoft-365 (accessed on 30 November 2022). Used with permission from Microsoft.
Actually, multiple pathophysiological processes participate in accelerated aging and aging-related cerebrovascular disorders, including arterial stiffness, endothelial replicative senescence, microvascular rarefaction, narrowing of the vascular lumen, and oxidative stress in inflammation [28,29,30,31,32]. As we age, our brains shrink in size, particularly at the level of the prefrontal and frontal cortex and the late myelinating regions of the prefrontal and frontal lobes. All the brain is actually implicated in these alterations and, because of the individual differences observed in brain development and the aging brain, the evaluation is a complex task. Interestingly, the occipital cortex seems to be the least affected by brain aging. Brain deterioration mainly is due to the loss of neuronal cells but there are also changes in dendritic arbor, spines, and synapses.
The brain volume and weight start declining from age 20 with age, and the rate of deterioration reaches 5% per decade after age 40 with an increased decline rate after the age of 70 [33,34]. Indeed, there is a significantly larger loss of myelin lipids than of gangliosides. The loss of myelin lipids is particularly large in the female brain after 70 years of age, while the loss in male brain seems to be linear as early as 20 years of age.
Aging is associated with memory decline, and brain activation becomes more bilateral for memory tasks as an attempt to compensate and recruit additional networks or because specific areas are no longer easily accessible. Dementia is often associated with aging. Genetics, epigenetics, neurotransmitters, hormones, and experience all have a part to play in brain aging. Curiously, higher levels of education or occupational attainment may act as a protective factor. Healthy diet, low to moderate alcohol intake, and regular exercise are also protective. These results suggest that biological aging is not absolutely bound to chronological aging, and it may be possible to slow biological aging and even reduce the possibility of suffering from age-related diseases such as neurodegenerative pathologies.
3. Oxidative Stress
3.1. Oxidative Stress and Epigenetics
Oxidative stress or free radicals refer to an imbalance between reactive oxygen species (ROS) generation and antioxidant defense systems, which are implicated in different pathways of injury in the development of various disorders (including neurodegenerative disorders and aging) [16,35,36,37]. Interestingly, oxidative stress plays a major role in the aging process, both by direct damage and by causing epigenetic changes. Epigenetics is defined as a heritable regulation of gene expression through DNA and histone protein modifications without DNA sequence alteration [38]. Epigenetic modification is technically a reversible process, switching on/off genes in order to dynamically respond to the cellular milieu [39].
Dysregulation of epigenetics is frequently found in physiological conditions such as in aging but also in almost all diseases (especially cancers) [40]. Oxidative stress and epigenetic alterations usually coincide in diseases, suggesting a close relationship between these two events (Figure 2). It has been demonstrated that ROS cause global DNA hypomethylation, promoter hypermethylation, and altered histone modification, while epigenetic regulation of ROS-mediated processes suggests the possibility of promising tools to deepen in our comprehension of the process of senescence, and to develop novel therapeutic strategies [41,42,43]. Among the highlighted tools to counter the harmful epigenetic effects of oxidative stress, dietary nutrients seem to be placed in a high spot [44,45,46].
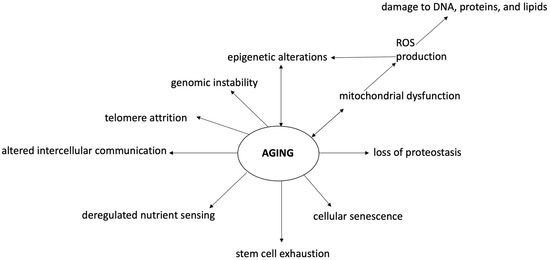
Figure 2.
Oxidative stress and epigenetic changes in the cognitive aging process. Aging and neurodegenerative diseases are associated with cognitive, emotional, and social deficiencies mostly linked to brain alterations. Aging is characterized by a state of genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, mitochondrial dysfunction, cellular senescence, deregulated nutrient sensing, stem cell exhaustion, and altered intercellular communication. In this context, oxidative stress and epigenetic modifications play a major role, both as perpetrators and consequences of aging processes. Oxidative stress and ROS increase cause DNA and macromolecule damage associated with mitochondrial dysfunction, inflammation reaction, apoptosis, and epigenetic modifications. Epigenetic changes are associated with DNA hypomethylation, promoter hypermethylation, and altered histone modification due to various mechanisms (including oxidative stress). In this context, antioxidants may play a major role in preventing cognitive aging problems. ROS—reactive oxygen species.
3.2. Role of Mitochondria
Mitochondria are intracellular organelles, manned with their own circular genome (mtDNA), which play a major role in maintaining cellular homeostasis—by producing adenosine triphosphate (ATP) and intermediate metabolites—and regulating energy metabolism, cell survival and proliferation, and Ca2+ signaling [47,48]. Mitochondria are critical regulators of cell death, a key feature of neurodegeneration. As mutations in mitochondrial DNA and oxidative stress both contribute to aging, which is the greatest risk factor for neurodegenerative disease, the evidence suggests that mitochondria also have a central role in aging-related neurodegenerative diseases [49].
Despite being well-known hallmarks of aging, recent findings have revealed a novel crosstalk between histone epigenetic modifications and oxidative stress during stem cell aging, which once more highlights the importance of these issues for aging and age-related diseases [50]. Evidence supports the major role of mitochondrial dysfunction in promoting aging and in supporting neurodegenerative progression [51]. Mutations accumulate at a higher rate in mtDNA than in nuclear DNA, resulting in mitochondrial dysfunction and diseases, and this is even more true in older people, where there coexists a reduced mitochondrial efficiency and a deterioration of the antioxidant system [52,53,54].
Studies in various species highlighted several alterations in mitochondria and mitochondrial DNA (mtDNA) associated with aging: increased disorganization of mitochondrial structure; decline in mitochondrial oxidative phosphorylation function; accumulation of mtDNA mutation; increased mitochondrial production of ROS (superoxide, hydrogen peroxide, hydroxyl radicals and singlet oxygen); increased extent of oxidative damage to DNA, proteins, and lipids [55].
Thus, the decline in mitochondrial energy metabolism that alters quality control pathways, the enhanced mitochondrial oxidative stress, and the accumulation of mtDNA mutations are important contributors to human aging. Since the efficacy of the respiratory chain diminishes, aging is associated with electron leakage, increased ROS production and reduced cellular ATP generation [56,57]. Mitochondria have been related also to multiple diseases, often aging-related, such as neurodegeneration and cancer [58,59,60]. Interestingly, it has been suggested that novel pathways that protect the cell through mitochondrial quality control may offer unique opportunities for disease therapy in situations where ongoing mitochondrial damage occurs [61].
Some interesting studies demonstrated the major role of oxidative stress in regulating the lifespan, so reducing oxidative stress resulted in the expanded life in murine models [62,63]. In a major study, to determine the role of the reactive oxygen species in mammalian longevity and pathology, the authors generated transgenic mice that overexpress human catalase localized in the peroxisome, nucleus, or mitochondria [62]. In the mice overexpressing the human mitochondria catalase, the median and maximum lifespans were maximally increased (averages of 5 months and 5.5 months, respectively), while cardiac diseases and cataract development were delayed, oxidative damage was reduced, H2O2 production and H2O2− induced aconitase inactivation were attenuated, and the development of mitochondrial deletions was reduced.
These results support the free radical theory of aging and reinforce the importance of mitochondria as a source of these radicals [62,63]. These results have been confirmed by another study that demonstrated how the overexpression of the antioxidant enzyme catalase in mitochondria can extend mouse lifespan, highlighting the importance of mitochondrial damage in aging and suggesting that, when targeted appropriately, boosting antioxidant defenses can increase mammalian life span [63,64]. Despite the need of further studies, therapies targeting basic mitochondrial processes, such as energy metabolism or free-radical generation, or specific interactions of disease-related proteins with mitochondria, hold great promise [49].
3.3. Mediterranean Diet
The Mediterranean diet refers to a traditional diet consumed in Mediterranean countries and characterized by a high consumption of vegetables and olive oil and moderate consumption of food rich in proteins. It has been demonstrated that the Mediterranean diet, abundant in minimally processed plant foods, reduces the risk of developing various chronic diseases and seems to increase life expectancy [65]. In fact, this diet has beneficial effects in the primary and secondary prevention of cardiovascular disease, type 2 diabetes, atrial fibrillation, and breast cancer [66,67].
The exact mechanism by which an increased adherence to the Mediterranean diet exerts its favorable effects is mostly unknown; however, evidence suggests that the major role is played by: lipid-lowering effect, protection against oxidative stress, inflammation and platelet aggregation, modification of hormones and growth factors involved in the pathogenesis of cancer (reduction of DNA damages, cell proliferation, and their survival, angiogenesis, inflammations, and metastasis), inhibition of nutrient sensing pathways by specific amino acid restriction, and gut microbiota-mediated production of metabolites influencing metabolic health [66,68,69,70].
Interestingly, it has been demonstrated that the Mediterranean diet, and nutrients in general, can modulate gene expression directly by binding to nuclear receptors or acting indirectly modulating epigenetic effects (DNA methylation, histone modifications, microRNAs) [69,71]. Among the nutrients contained in the Mediterranean diet, olive oil and red wine are probably the most widely consumed and, when assumed at the correct dosage, they have been demonstrated to have beneficial effects on health [72,73]. In bringing these positive results, a major role is played by the presence of antioxidants in these aliments and, being among the most studied antioxidants, in the following chapters we will report the experiences on hydroxytyrosol and resveratrol [74,75,76].
3.4. Antioxidants
As antioxidants are substances that are efficient to trap ROS and decrease oxidative damage, these products have been studied for therapeutic approaches to many different diseases. On the other hand, a deficiency of antioxidants such as vitamins C and E has been associated with cognitive disorders [77]. In literature, many natural products and pharmacological compounds have antioxidant properties [73,78]. Interestingly, resveratrol and other polyphenols extracted from olive and wine but also other natural goods are among the most studied and possess great antioxidant and anti-inflammatory properties [79,80,81,82].
3.5. Polyphenols
Polyphenols are natural, synthetic, or semi-synthetic organic molecules constituted by numerous hydroxyl groups on aromatic rings (phenolic groups), presenting neuroprotective and anti-inflammatory effects and capacity of control of oxidative stress, apoptosis and mitochondrial dysfunction [81,83,84]. These products are divided into four main groups: phenolic acids, flavonoids, stilbenes, and lignans.
The Mediterranean diet is a mainstay of nutritional therapeutic and preventive programs in many diseases because of a rich presence of foods and beverages abundant in polyphenols, such as olives, olive oil, wine, fresh and processed fruits and vegetables, leguminous plants, cereals, herbs, spices, tea, coffee, and beer [85,86]. A proper diet is one of major factors contributing to good health and is directly related to the general condition of the organism [87,88]. Polyphenols are converted and absorbed mainly in the oral cavity and stomach; in the large intestine, the remaining polyphenols are further modified by bacterial enzymes (e.g., glycosides, esters, etc.) to obtain metabolites of lower-weight easier to absorb; these metabolites then circulate within blood, bound to proteins (mainly albumin), and are conjugated in the liver and kidneys; finally, elimination happens in the urine and feces [89].
Polyphenols are present in liquid natural products such as olive oil and green tea; however, it is also true that they can be found in alcohols such as red wine (whose main polyphenol is resveratrol) and beer [79,81,87,90,91,92,93,94,95,96]. Interestingly, the evidence suggests that moderate wine consumption may decrease the risk of several cancers (including colon, basal cell carcinoma, ovarian, and prostate cancer) and cognitive diseases; on the other hand, it should be pinpointed to an adequate balance in order to avoid the negative effects due to the presence of substances such as ethanol [97,98,99].
3.6. Antioxidants and Cognition in the Aging Brain
Oxidative stress and the inflammation due to increased oxidative stress are associated to many chronic diseases, but the lack of anti-inflammatory drugs without side-effects has stimulated the search for new active substances. It has been demonstrated that the Central Nervous System (CNS) can benefit from nutritional strategies and dietary interventions that prevent the signs of senescence, such as cognitive decline or neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s Disease [100]. Both aging and associated neurodegenerative diseases are accompanied by the decline of several brain functions, including cognitive abilities, which are related to progressive deleterious changes at biochemical and physiological levels, leading to the generation of oxidative stress, disturbed protein metabolism with accumulation of protein aggregates, mitochondrial dysfunctions, loss of synaptic connections, and ultimately neurodegeneration and cognitive decline [101]. Because of its high energy demand, the brain is more susceptible to ROS-mediated damages, as it oxidizes lipids, proteins, and nucleic acids, thereby causing an imbalance in the homeostasis, and this especially occurs in the aging brain. It has been suggested that oxidative stress is a key factor for age-associated neurodegeneration and cognitive decline due to the imbalance between the rates of production and elimination of ROS.
Interestingly, the involvement of the heme oxygenase (HO) pathway in anti-degenerative mechanisms related to the induction of other heat shock proteins (HSPs, molecular chaperones involved in cell protection from various forms of stress) has been demonstrated during various physio-pathological conditions [102]. In fact, the vasoactive molecule carbon monoxide and the potent antioxidant bilirubin, products of the HO-catalyzed reaction, represent a protective system that is potentially active against the brain oxidative injury associated to the cognitive dysfunction in the aging-associated neurodegenerative diseases [103,104].
Studies on both animal and human subject demonstrated that dietary interventions and plant-derived bioactive compounds with antioxidant properties could be beneficial for recovering the memory or delaying the onset of memory impairment, especially in case of stress-mediated changes [105]. Recently, the supplementation of spice and herbs containing phenolic substances with potent antioxidant and chemo-preventive properties, such as curcumin (a powerful antioxidant derived from the curry spice turmeric), has been considered as an alternative, nutritional approach to reduce oxidant damage and neurodegenerative pathology associated with aging.
Recently, human studies have been conducted to determine the effective nutritional and lifestyle protocols for the prevention of neurodegenerative diseases [106]. The Mediterranean diet and antioxidant and anti-inflammatory products seem to play a significant role in most of the proposed protocols [107]. Furthermore, higher adherence to the Mediterranean dietary pattern has been associated with decreased cognitive decline and incidence of neurodegenerative diseases [108]. Here, we report the example of two among the most studied antioxidant products and their role in preventing cognitive dysfunction due to brain aging: hydroxytyrosol and resveratrol (see Table 1 for the evidence on neuroprotective and cognitive role of resveratrol and hydroxytyrosol and Figure 3 for a graphic description of the resveratrol and hydroxytyrosol molecular mechanisms of action).

Table 1.
Evidence on neuroprotective and cognitive role of resveratrol and hydroxytyrosol. AMPK, AMP-activated protein kinase; βA, beta amyloid, COX, cyclooxygenase; CSF, cerebrospinal fluid; ERβ, estrogen receptor β; ERK, extracellular signal-regulated kinase; LPS, lipopolysaccharide; MMP9, matrix metalloproteinase 9; NF-κB, nuclear factor κB; NO, nitric oxide, PGES-1, prostaglandin E synthase-1; TNF, tumor necrosis factor.
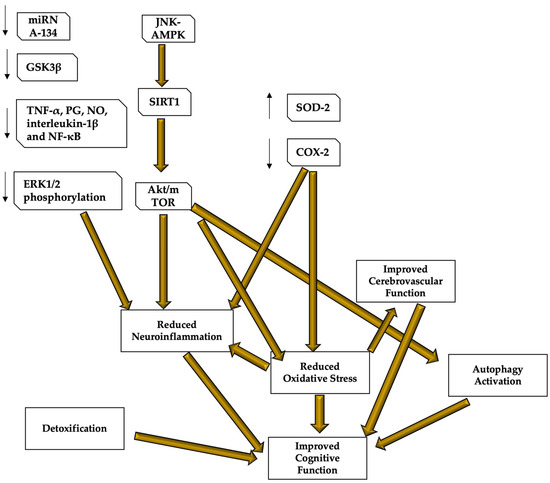
Figure 3.
Resveratrol and hydroxytyrosol molecular mechanisms of action. Resveratrol and hydroxytyrosol demonstrated to be able to improve cognitive performance and protect the brain from neurodegenerative and age-related diseases, mostly thanks to their role in regulating oxidative stress, neuroinflammation, cerebral blood flow, and autophagy, as well as because of their capacity of detoxifying the blood from those neuro-damaging compounds. Most of the mechanisms are still under study, but it seems that both resveratrol and hydroxytyrosol target the AMPK and the subsequent pathway leading to SIRT1 and Akt/mTOR to reduce neuroinflammation and oxidative stress, and stimulating autophagy. Oxidative stress reduction also inhibits inflammatory responses and stimulates cerebrovascular function, leading to better cerebral blood flow and brain functioning. These compounds are also important detoxicants. Resveratrol mechanisms are clearer and its role in reducing neuroinflammation has been also related to the capacity of lowering mRNA134, GSK3β, ERK1/2 phosphorylation and cerebral levels of TNF-α, PG, NO, interleukin-1β and NF-κB. Resveratrol also increases SOD-2 protecting functions and inhibits COX-2 to reduce ROS production. AMPK—AMP-activated protein kinase; COX—cyclooxygenase; ERK—extracellular signal-regulated kinase; LPS—lipopolysaccharide; MMP9—matrix metalloproteinase 9; NF-κB—nuclear factor κB; NO—nitric oxide, PGES-1—prostaglandin E synthase-1; ROS—reactive oxygen species; TNF—tumor necrosis factor; SOD—superoxide dismutase. Images have been created by using the functionalities of Microsoft PowerPoint 365 Version 2112. https://www.microsoft.com/microsoft-365 (accessed on 30 November 2022). Used with permission from Microsoft.
3.7. Hydroxytyrosol
As the Mediterranean diet entered the spotlight for its many beneficial properties, over the years, researchers have made an attempt to find which foods and food components are responsible for the beneficial effects on health. One of these components and currently the most actively investigated natural phenol is hydroxytyrosol, a phenolic phytochemical with antioxidant properties that can be found in olive leaves and oil [150].
This molecule gained particular interest for its role in various diseases due to its anti-inflammatory, antimicrobial, antiviral, antifungal, cardioprotective, neuroprotective, antitumoral, and chemo-modulating effects. The interest in this molecule has led to wide research on its biological activities, its beneficial effects on humans and in how to synthesize new molecules from hydroxytyrosol. In particular, due to its bioavailability, chemical properties and easy formulation along with its lack of toxicity, hydroxytyrosol is considered an excellent food supplement by the nutraceutical and food industries [151].
Furthermore, hydroxytyrosol has great pharmaceutical potential in cognitive and aging disorders because it improves endothelial dysfunction, decreases oxidative stress and has neuroprotective properties [152,153]. Unfortunately, most of the evidence comes from animal model-based experiments, but hydroxytyrosol seems to be able to stimulate neurogenesis by enhancing stem and progenitor cell proliferation and neuron survival [147].
It has been demonstrated that a diet rich in purified olive polyphenols has positive long-term effects on cognition and energy metabolism in the brains of aged mice [154,155]. Furthermore, recent studies demonstrated that hydroxytyrosol protects from the aging process by modulating the AMP-activated protein kinase (AMPK) signaling and autophagy, while the AMPK dysregulation has been associated with accelerated aging and promotion of inflammation, cancer, and metabolic pathologies such as diabetes and obesity [156].
Interestingly, in TgCRND8 mouse models, it has been demonstrated that hydroxytyrosol diet supplementation results in substantial neuroprotection improving cognitive functions and leading to significant changes in the brain cortex and hippocampal areas with also a marked reduction of the TNF-α expression and astrocyte reaction [144,157]. Furthermore, hydroxytyrosol is able to ameliorate neuronal impairment via modulating mitochondrial oxidative stress, neuronal inflammation, and apoptosis [121,158]. In Caenorhabditis elegans models, it has been demonstrated that an olive-derived extract 20% rich in hydroxytyrosol is able to prevent the β-amyloid aggregation and oxidative stress associated to Alzheimer’s disease [124,159]. These effects have been associated with the increased gene expression of the SKN-1/NRF2 transcription factor and the overexpression of HSP-16.2. In swine models, hydroxytyrosol prevented DNA hypomethylation associated with oxidative stress [160]. Interestingly, hydroxytyrosol can reduce hypoxia-mediated cell damage through activating the PI3K/AKT/mTOR-HIF-1 α signal pathway [161]. As ischemic events are more common in older people and are an important cause of neurological impairment, it is of interest noting that the hydroxytyrosol-enriched diet could serve as a beneficial therapeutic approach to attenuate ischemic stroke-associated damage [162,163].
3.8. Resveratrol
Resveratrol (3,5,4′-trihydroxy-trans-stilbene) is a natural non-flavonoid phenol and a phytoalexin with antioxidant and cytoprotective effects led by pleiotropic actions [80]. It is produced by several plants in response to injury or when these are under attack by pathogens (bacteria, fungi, etc.) and as such, it interacts with gut microbiota, inducing modifications in bacterial composition associated with beneficial effects.
The major food sources of resveratrol are grapes, blueberries, raspberries, mulberries, and peanuts. Resveratrol has neuroprotective and antiaging properties preventing the effects related to oxidative stress, reducing DNA damage and regulating molecular changes such as mitochondrial dysfunction, inflammation reaction, apoptosis, and epigenetic modifications, among others [164,165,166,167].
Recent evidence demonstrated that resveratrol mediates epigenetic changes (methylation and acetylation) that persist across generations and that are involved in aging and the function of the nervous system [168,169,170,171]. The study of key markers involved in senescence and rejuvenation (mitochondrial biogenesis and Sirt1-AMPK-PGC1-α) demonstrated that resveratrol is also able to modulate the changes in these cellular metabolic pathways. Interestingly, resveratrol may exert neuroprotective effects also by regulating autophagy and apoptosis mediated by the Akt/mTOR pathway [134,135]. Unfortunately, most of the evidence on resveratrol is based on animal experiments and the effects on human cognition are likely to be smaller [94,172].
On the other hand, recent clinical evidence, derived from randomized clinical trials, suggests that in humans, resveratrol is able to improve cerebral blood flow, cerebral vasodilator responsiveness to hypercapnia, some cognitive tests, perceived performances, and the Aβ40 plasma and cerebrospinal fluid level, modulates neuroinflammation, and induces adaptive immunity [109,128,173,174,175]. In particular, resveratrol causes a dose-dependent increase in cerebral blood flow and enhanced oxygen extraction, but its role in ameliorating cognitive performance is still under study [127,129]. Despite the lack of definite evidence, the role of resveratrol on the cerebral blood flow is important especially considering the vascular alterations found in most of the age-related diseases [176]. Interestingly, recent findings demonstrated that cis- and trans-resveratrol have the opposite effects on histone serine-ADP-ribosylation and tyrosine-induced neurodegeneration, so that the age-associated increase in serum tyrosine levels may affect neurocognitive and metabolic disorders, offering a plausible explanation for divergent results obtained in clinical trials using resveratrol [177].
3.9. The Limitation of the Blood–Brain-Barrier
In recent years, many compounds and drugs that affect the brain have been regarded for their potential role in the therapeutic management of various age-related diseases [178,179,180]. Regrettably, the administration of therapy that is able to reach the brain has inherent problems because of the blood–brain-barrier (BBB), which prevents the brain uptake of most pharmaceuticals, so that not every product that demonstrated to be able to reduce aging progression is capable of influencing the more specific brain aging.
This BBB property comes from the epithelial-like tight junctions within the brain capillary endothelium. Providing the drug has a molecular weight under 400 Da and forms less than eight hydrogen bonds, small molecules acting as agonists, modulators or enhancers targeting the associated receptors may cross the BBB via lipid-mediated free diffusion, but these chemical properties are lacking in the majority of small molecule drugs, as well as all large molecule drugs [181]. In fact, many solutions have been suggested, for example, the protein could be infused directly, produced by viral constructs, secreted from implanted protein-secreting cells or actively transported across the brain.
Drugs can be reengineered for BBB transport: small molecule drugs can be synthesized to be able to access carrier-mediated transport (CMT) systems within the BBB; large molecule drugs can be modified using molecular Trojan horse delivery systems to access receptor-mediated transport (RMT) systems within the BBB. Peptide and antisense radiopharmaceuticals can also guarantee made brain-penetrating properties by combining the use of RMT-based delivery systems and avidin–biotin technology.
Many studies suggested that the early disruption of the BBB to large molecules is mediated by ROS [182,183]. As the brain is exposed throughout life to damages due to ROS, various endogenous antioxidant defense mechanisms physiologically exist, including the removal of O2, scavenging of reactive oxygen/nitrogen species or their precursors, inhibition of ROS formation, binding of metal ions needed for the catalysis of ROS generation, and up-regulation of endogenous antioxidant defenses.
However, since our endogenous antioxidant defenses are not always completely effective, and since exposure to damaging environmental factors is increasing, it has been suggested that exogenous antioxidants could be very effective in diminishing the cumulative effects of oxidative damage. Unfortunately, the therapeutic use of most of the studied antioxidant compounds is limited, since they do not cross the blood–brain barrier.
Novel antioxidant molecules designed as potential neuroprotective treatments in neurodegenerative and age-related disorders are focusing on this limitation to be able to cross the BBB after systemic administration; furthermore, gender differences have been identified [184,185]. A recent study suggested that resveratrol is well tolerated and seems to be able to penetrate the blood–brain barrier to produce its neuroprotective effects [141]. Unfortunately, most of the evidence comes from pre-clinical and animal-based studies; so, further research is required before most of these therapies can be safely applied clinically.
4. Discussion
This report aims to provide a summary and a subsequent review of literature evidence on the role of antioxidants in preventing and improving cognition in the aging brain. As endogenous antioxidants are linked to antidegenerative mechanisms, exogenous antioxidant supplementation could play a major role in inhibiting oxidative damage and compensating for the decreased level of endogenous antioxidants. Conceivably, dietary supplementation with antioxidant polyphenolic agents such as hydroxytyrosol, resveratrol and curcumin reduces the development of aging-related cognitive diseases, their signs, and symptoms. Among others, dietary antioxidants play a major role in preventing and reducing DNA damage, mitochondrial dysfunction, inflammation, apoptosis, and transgenerational epigenetic modifications.
These products have numerous properties with antimicrobial, antiviral, antifungal, cardioprotective, neuroprotective, antitumor, and chemo-modulating effects. These results demonstrate that numerous pathways, mostly still unknown, are concerned, with pleiotropic actions involved [186]. Recently, an association of epigenetic, DNA methylation-based, clocks in brain tissue with brain pathologies and common aging phenotypes has been demonstrated [187]. It has also been suggested that these clocks may play an important role in age prediction to age reversion [188]. Since antioxidants seem to cause adaptive epigenetic changes (in part by reducing oxidative stress), their role in age prediction to age reversion is even more plausible [189].
In conclusion, the manipulation of endogenous cellular defense mechanisms through nutritional antioxidants or pharmacological compounds represents an innovative approach to therapeutic intervention in diseases causing tissue damage, such as neurodegeneration. Consistent with this notion, antioxidants may delay and/or modulate the cognitive brain aging processes and decrease the occurrence of their devastating effects on the brain. All compounds aiming to influence brain aging must be able to surpass the limitation represented by the BBB after systemic administration.
The potential preventive activity of antioxidants should be further evaluated in long-term exposure clinical trials, using preparations with high bioavailability and that are well standardized.
Author Contributions
Conceptualization, G.F.; investigation, M.F.; writing—original draft preparation, S.T., G.F. and M.F.; writing—review and editing, G.F., M.F., C.P., S.F. and M.L.; visualization, A.M. and A.G.; supervision, L.T. and M.R.; project administration, C.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Authors thank IBBC-CNR, and Sapienza University of Rome, Rome, Italy.
Conflicts of Interest
The authors declare no conflict of interest, financial or otherwise.
References
- Reuter-Lorenz, P.A.; Park, D.C. How Does it STAC Up? Revisiting the Scaffolding Theory of Aging and Cognition. Neuropsychol. Rev. 2014, 24, 355–370. [Google Scholar] [CrossRef]
- Goh, J.O.; Park, D.C. Neuroplasticity and cognitive aging: The scaffolding theory of aging and cognition. Restor. Neurol. Neurosci. 2009, 27, 391–403. [Google Scholar] [CrossRef] [PubMed]
- Harada, C.N.; Natelson Love, M.C.; Triebel, K.L. Normal cognitive aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Joubert, C.; Chainay, H. Aging brain: The effect of combined cognitive and physical training on cognition as compared to cognitive and physical training alone—A systematic review. Clin. Interv. Aging 2018, 13, 1267–1301. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Garagnani, P.; Morsiani, C.; Conte, M.; Santoro, A.; Grignolio, A.; Monti, D.; Capri, M.; Salvioli, S. The continuum of aging and age-related diseases: Common mechanisms but different rates. Front. Med. 2018, 5, 61. [Google Scholar] [CrossRef]
- Cheng, X.; Yang, Y.; Schwebel, D.C.; Liu, Z.; Li, L.; Cheng, P.; Ning, P.; Hu, G. Population ageing and mortality during 1990-2017: A global decomposition analysis. PLoS Med. 2020, 17, e1003138. [Google Scholar] [CrossRef] [PubMed]
- Wisdom, N.M.; Mignogna, J.; Collins, R.L. Variability in wechsler adult intelligence scale-IV subtest performance across age. Arch. Clin. Neuropsychol. 2012, 27, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Gunning-Dixon, F.M.; Gur, R.C.; Perkins, A.C.; Schroeder, L.; Turner, T.; Turetsky, B.I.; Chan, R.M.; Loughead, J.W.; Alsop, D.C.; Maldjian, J.; et al. Age-related differences in brain activation during emotional face processing. Neurobiol. Aging 2003, 24, 285–295. [Google Scholar] [CrossRef]
- Straka, K.; Tran, M.L.; Millwood, S.; Swanson, J.; Kuhlman, K.R. Aging as a Context for the Role of Inflammation in Depressive Symptoms. Front. Psychiatry 2021, 11, 605347. [Google Scholar] [CrossRef]
- Ruffman, T.; Henry, J.D.; Livingstone, V.; Phillips, L.H. A meta-analytic review of emotion recognition and aging: Implications for neuropsychological models of aging. Neurosci. Biobehav. Rev. 2008, 32, 863–881. [Google Scholar] [CrossRef]
- Bischof, G.N.; Park, D.C. Obesity and Aging: Consequences for Cognition, Brain Structure, and Brain Function. Psychosom. Med. 2015, 77, 697–709. [Google Scholar] [CrossRef] [PubMed]
- Cabeza, R.; Anderson, N.D.; Locantore, J.K.; McIntosh, A.R. Aging gracefully: Compensatory brain activity in high-performing older adults. Neuroimage 2002, 17, 1394–1402. [Google Scholar] [CrossRef] [PubMed]
- Cabeza, R. Hemispheric asymmetry reduction in older adults: The HAROLD model. Psychol. Aging 2002, 17, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Sadowska-Bartosz, I.; Bartosz, G. Effect of antioxidants supplementation on aging and longevity. Biomed Res. Int. 2014, 2014, 404680. [Google Scholar] [CrossRef] [PubMed]
- Herrera, E.; Jiménez, R.; Aruoma, O.I.; Hercberg, S.; Sánchez-García, I.; Fraga, C. Aspects of antioxidant foods and supplements in health and disease. Nutr. Rev. 2009, 67, S140–S144. [Google Scholar] [CrossRef]
- Terracina, S.; Ferraguti, G.; Petrella, C.; Bruno, S.M.; Blaconà, G.; Di Certo, M.G.; Minni, A.; Greco, A.; Musacchio, A.; Ralli, M.; et al. Characteristic Hallmarks of Aging and the Impact on Carcinogenesis. Curr. Cancer Drug Targets 2022, 22, 87–102. [Google Scholar] [CrossRef]
- Morimoto, R.I.; Cuervo, A.M. Proteostasis and the aging proteome in health and disease. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2014, 69, S33–S38. [Google Scholar] [CrossRef]
- Hou, Y.; Dan, X.; Babbar, M.; Wei, Y.; Hasselbalch, S.G.; Croteau, D.L.; Bohr, V.A. Ageing as a risk factor for neurodegenerative disease. Nat. Rev. Neurol. 2019, 15, 565–581. [Google Scholar] [CrossRef]
- Farr, J.N.; Almeida, M. The Spectrum of Fundamental Basic Science Discoveries Contributing to Organismal Aging. J. Bone Miner. Res. 2018, 33, 1568–1584. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The hallmarks of aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef]
- Lautrup, S.; Sinclair, D.A.; Mattson, M.P.; Fang, E.F. NAD+ in Brain Aging and Neurodegenerative Disorders. Cell Metab. 2019, 30, 630–655. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.J.; Petersen, R.C. Cellular senescence in brain aging and neurodegenerative diseases: Evidence and perspectives. J. Clin. Invest. 2018, 128, 1208–1216. [Google Scholar] [CrossRef] [PubMed]
- Guida, J.L.; Ahles, T.A.; Belsky, D.; Campisi, J.; Cohen, H.J.; DeGregori, J.; Fuldner, R.; Ferrucci, L.; Gallicchio, L.; Gavrilov, L.; et al. Measuring Aging and Identifying Aging Phenotypes in Cancer Survivors. J. Natl. Cancer Inst. 2019, 111, 1245–1254. [Google Scholar] [CrossRef] [PubMed]
- Peters, R. Ageing and the brain. Postgrad. Med. J. 2006, 82, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Trollor, J.N.; Valenzuela, M.J. Brain ageing in the new millennium. Aust. N. Z. J. Psychiatry 2001, 35, 788–805. [Google Scholar] [CrossRef]
- Zia, A.; Pourbagher-Shahri, A.M.; Farkhondeh, T.; Samarghandian, S. Molecular and cellular pathways contributing to brain aging. Behav. Brain Funct. 2021, 17, 6. [Google Scholar] [CrossRef]
- Yang, T.; Sun, Y.; Lu, Z.; Leak, R.K.; Zhang, F. The impact of cerebrovascular aging on vascular cognitive impairment and dementia. Ageing Res. Rev. 2017, 34, 15–29. [Google Scholar] [CrossRef]
- Semba, R.D.; Sun, K.; Schwartz, A.V.; Varadhan, R.; Harris, T.B.; Satterfield, S.; Garcia, M.; Ferrucci, L.; Newman, A.B.; Health ABC Study. Serum carboxymethyl-lysine, an advanced glycation end product, is associated with arterial stiffness in older adults. J. Hypertens. 2015, 33, 797–803, discussion 803. [Google Scholar] [CrossRef]
- Chinta, S.J.; Woods, G.; Rane, A.; Demaria, M.; Campisi, J.; Andersen, J.K. Cellular senescence and the aging brain. Exp. Gerontol. 2015, 68, 3–7. [Google Scholar] [CrossRef]
- Hajjar, I.; Goldstein, F.C.; Waller, E.K.; Moss, L.D.; Quyyumi, A. Circulating Progenitor Cells is Linked to Cognitive Decline in Healthy Adults. Am. J. Med. Sci. 2016, 351, 147–152. [Google Scholar] [CrossRef]
- Yurdagul, A.; Finney, A.C.; Woolard, M.D.; Orr, A.W. The arterial microenvironment: The where and why of atherosclerosis. Biochem. J. 2016, 473, 1281–1295. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Kaley, G.; de Cabo, R.; Sonntag, W.E.; Csiszar, A. Mechanisms of vascular aging: New perspectives. J. Gerontol. A. Biol. Sci. Med. Sci. 2010, 65, 1028–1041. [Google Scholar] [CrossRef] [PubMed]
- Svennerholm, L.; Boström, K.; Jungbjer, B. Changes in weight and compositions of major membrane components of human brain during the span of adult human life of Swedes. Acta Neuropathol. 1997, 94, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Svennerholm, L.; Boström, K.; Helander, C.G.; Jungbjer, B. Membrane lipids in the aging human brain. J. Neurochem. 1991, 56, 2051–2059. [Google Scholar] [CrossRef] [PubMed]
- Ferraguti, G.; Terracina, S.; Petrella, C.; Greco, A.; Minni, A.; Lucarelli, M.; Agostinelli, E.; Ralli, M.; de Vincentiis, M.; Raponi, G.; et al. Alcohol and Head and Neck Cancer: Updates on the Role of Oxidative Stress, Genetic, Epigenetics, Oral Microbiota, Antioxidants, and Alkylating Agents. Antioxidants 2022, 11, 145. [Google Scholar] [CrossRef]
- Micangeli, G.; Menghi, M.; Profeta, G.; Tarani, F.; Mariani, A.; Petrella, C.; Barbato, C.; Ferraguti, G.; Ceccanti, M.; Tarani, L.; et al. The Impact of Oxidative Stress on Pediatrics Syndromes. Antioxidants 2022, 11, 1983. [Google Scholar] [CrossRef]
- Ahmad, K.A.; Yuan Yuan, D.; Nawaz, W.; Ze, H.; Zhuo, C.X.; Talal, B.; Taleb, A.; Mais, E.; Qilong, D. Antioxidant therapy for management of oxidative stress induced hypertension. Free Radic. Res. 2017, 51, 428–438. [Google Scholar] [CrossRef]
- Sharma, P.; Ghanghas, P.; Kaushal, N.; Kaur, J.; Kaur, P. Epigenetics and oxidative stress: A twin-edged sword in spermatogenesis. Andrologia 2019, 51, e13432. [Google Scholar] [CrossRef]
- Boonla, C. Oxidative stress, epigenetics, and bladder cancer. Cancer Oxidative Stress Diet. Antioxid. 2021, 67–75. [Google Scholar] [CrossRef]
- Guillaumet-Adkins, A.; Yañez, Y.; Peris-Diaz, M.D.; Calabria, I.; Palanca-Ballester, C.; Sandoval, J. Epigenetics and Oxidative Stress in Aging. Oxid. Med. Cell. Longev. 2017, 2017, 9175806. [Google Scholar] [CrossRef]
- Romá-Mateo, C.; Seco-Cervera, M.; Ibáñez-Cabellos, J.S.; Pérez, G.; Berenguer-Pascual, E.; Rodríguez, L.R.; García-Giménez, J.L. Oxidative Stress and the Epigenetics of Cell Senescence: Insights from Progeroid Syndromes. Curr. Pharm. Des. 2019, 24, 4755–4770. [Google Scholar] [CrossRef] [PubMed]
- Crouch, J.; Shvedova, M.; Thanapaul, R.J.R.S.; Botchkarev, V.; Roh, D. Epigenetic Regulation of Cellular Senescence. Cells 2022, 11, 672. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Ni, X. ROS-Mediated DNA Methylation Pattern Alterations in Carcinogenesis. Curr. Drug Targets 2015, 16, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Ciafrè, S.; Carito, V.; Ferraguti, G.; Greco, A.; Chaldakov, G.N.; Fiore, M.; Ceccanti, M. How alcohol drinking affects our genes: An epigenetic point of view. Biochem. Cell Biol. 2019, 97, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Barrera, L.N.; Cassidy, A.; Johnson, I.T.; Bao, Y.; Belshaw, N.J. Postgraduate symposium: Epigenetic and antioxidant effects of dietary isothiocyanates and selenium: Potential implications for cancer chemoprevention. Proc. Nutr. Soc. 2012, 71, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Gerhauser, C. Epigenetic impact of dietary isothiocyanates in cancer chemoprevention. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Genovese, I.; Carinci, M.; Modesti, L.; Aguiari, G.; Pinton, P.; Giorgi, C. Mitochondria: Insights into crucial features to overcome cancer chemoresistance. Int. J. Mol. Sci. 2021, 22, 4770. [Google Scholar] [CrossRef]
- Nunnari, J.; Suomalainen, A. Mitochondria: In sickness and in health. Cell 2012, 148, 1145–1159. [Google Scholar] [CrossRef]
- Lin, M.T.; Beal, M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 2006, 443, 787–795. [Google Scholar] [CrossRef]
- Su, X.; Zhang, H.; Lei, F.; Wang, R.; Lin, T.; Liao, L. Epigenetic therapy attenuates oxidative stress in BMSCs during ageing. J. Cell. Mol. Med. 2022, 26, 375–384. [Google Scholar] [CrossRef]
- Moro, L. Mitochondrial dysfunction in aging and cancer. J. Clin. Med. 2019, 8, 1983. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.J.; Muniec, D.S.; Sullivan, K.; Woodyatt, N.; Alliston-Greiner, R.; Wilson, M.R.; Berry, D.L.; Holland, K.A.; Weedn, V.W.; Gill, P.; et al. A high observed substitution rate in the human mitochondrial DNA control region. Nat. Genet. 1997, 15, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Malyarchuk, B.A.; Rogozin, I.B.; Berikov, V.B.; Derenko, M.V. Analysis of phylogenetically reconstructed mutational spectra in human mitochondrial DNA control region. Hum. Genet. 2002, 111, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Vatner, S.F.; Zhang, J.; Oydanich, M.; Berkman, T.; Naftalovich, R.; Vatner, D.E. Healthful aging mediated by inhibition of oxidative stress. Ageing Res. Rev. 2020, 64, 101194. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Wei, Y.H. Mitochondria and aging. Adv. Exp. Med. Biol. 2012, 942, 311–327. [Google Scholar] [CrossRef] [PubMed]
- Ungvari, Z.; Tarantini, S.; Donato, A.J.; Galvan, V.; Csiszar, A. Mechanisms of vascular aging. Circ. Res. 2018, 123, 849–867. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.A. The anti-aging sweepstakes: Catalase runs for the ROSes. Science 2005, 308, 1875–1876. [Google Scholar] [CrossRef]
- Ralli, M.; Botticelli, A.; Visconti, I.C.; Angeletti, D.; Fiore, M.; Marchetti, P.; Lambiase, A.; De Vincentiis, M.; Greco, A. Immunotherapy in the Treatment of Metastatic Melanoma: Current Knowledge and Future Directions. J. Immunol. Res. 2020, 2020, 9235638. [Google Scholar] [CrossRef]
- Giorgi, C.; Marchi, S.; Simoes, I.C.M.; Ren, Z.; Morciano, G.; Perrone, M.; Patalas-Krawczyk, P.; Borchard, S.; Jędrak, P.; Pierzynowska, K.; et al. Mitochondria and Reactive Oxygen Species in Aging and Age-Related Diseases. Int. Rev. Cell Mol. Biol. 2018, 340, 209–344. [Google Scholar] [CrossRef]
- Connolly, N.M.C.; Theurey, P.; Adam-Vizi, V.; Bazan, N.G.; Bernardi, P.; Bolaños, J.P.; Culmsee, C.; Dawson, V.L.; Deshmukh, M.; Duchen, M.R.; et al. Guidelines on experimental methods to assess mitochondrial dysfunction in cellular models of neurodegenerative diseases. Cell Death Differ. 2018, 25, 542–572. [Google Scholar] [CrossRef]
- Franco-Iborra, S.; Vila, M.; Perier, C. Mitochondrial quality control in neurodegenerative diseases: Focus on Parkinson’s disease and Huntington’s disease. Front. Neurosci. 2018, 12, 342. [Google Scholar] [CrossRef] [PubMed]
- Schriner, S.E.; Linford, N.J.; Martin, G.M.; Treuting, P.; Ogburn, C.E.; Emond, M.; Coskun, P.E.; Ladiges, W.; Wolf, N.; Van Remmen, H.; et al. Medecine: Extension of murine life span by overexpression of catalase targeted to mitochondria. Science 2005, 308, 1909–1911. [Google Scholar] [CrossRef] [PubMed]
- Linford, N.J.; Schriner, S.E.; Rabinovitch, P.S. Oxidative damage and aging: Spotlight on mitochondria. Cancer Res. 2006, 66, 2497–2499. [Google Scholar] [CrossRef] [PubMed]
- Harman, D. Aging: A theory based on free radical and radiation chemistry. J. Gerontol. 1956, 11, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Bloomfield, H.E.; Koeller, E.; Greer, N.; MacDonald, R.; Kane, R.; Wilt, T.J. Effects on health outcomes of a mediterranean diet with no restriction on fat intake: A systematic review and meta-analysis. Ann. Intern. Med. 2016, 165, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and mediterranean diet: A review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef]
- Petrella, C.; Farioli-Vecchioli, S.; Cisale, G.Y.; Strimpakos, G.; Borg, J.J.; Ceccanti, M.; Fiore, M.; Monteleone, G.; Nisticò, R. A Healthy Gut for a Healthy Brain: Preclinical, Clinical and Regulatory Aspects. Curr. Neuropharmacol. 2020, 19, 610–628. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Simonetta, I.; Daidone, M.; Mogavero, A.; Ortello, A.; Pinto, A. Metabolic and vascular effect of the mediterranean diet. Int. J. Mol. Sci. 2019, 20, 4716. [Google Scholar] [CrossRef]
- Finicelli, M.; Di Salle, A.; Galderisi, U.; Peluso, G. The Mediterranean Diet: An Update of the Clinical Trials. Nutrients 2022, 14, 2956. [Google Scholar] [CrossRef]
- Scoditti, E.; Calabriso, N.; Massaro, M.; Pellegrino, M.; Storelli, C.; Martines, G.; De Caterina, R.; Carluccio, M.A. Mediterranean diet polyphenols reduce inflammatory angiogenesis through MMP-9 and COX-2 inhibition in human vascular endothelial cells: A potentially protective mechanism in atherosclerotic vascular disease and cancer. Arch. Biochem. Biophys. 2012, 527, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Carluccio, M.A.; Siculella, L.; Ancora, M.A.; Massaro, M.; Scoditti, E.; Storelli, C.; Visioli, F.; Distante, A.; De Caterina, R. Olive oil and red wine antioxidant polyphenols inhibit endothelial activation: Antiatherogenic properties of Mediterranean diet phytochemicals. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Ceccanti, M.; Mancinelli, R.; Tirassa, P.; Laviola, G.; Rossi, S.; Romeo, M.; Fiore, M. Early exposure to ethanol or red wine and long-lasting effects in aged mice. A study on nerve growth factor, brain-derived neurotrophic factor, hepatocyte growth factor, and vascular endothelial growth factor. Neurobiol. Aging 2012, 33, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Hornedo-Ortega, R.; Cerezo, A.B.; de Pablos, R.M.; Krisa, S.; Richard, T.; García-Parrilla, M.C.; Troncoso, A.M. Phenolic compounds characteristic of the mediterranean diet in mitigating microglia-mediated neuroinflammation. Front. Cell. Neurosci. 2018, 12, 373. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Tortose, M.d.C.; Pulido-Moran, M.; Granados, S.; Gaforio, J.J.; Quiles, J.L. Hydroxytyrosol as a Component of the Mediterranean Diet and Its Role in Disease Prevention. In The Mediterranean Diet: An Evidence-Based Approach; Elsevier: Amsterdam, The Netherlands, 2015; pp. 205–215. [Google Scholar] [CrossRef]
- Nani, A.; Murtaza, B.; Khan, A.S.; Khan, N.A.; Hichami, A. Antioxidant and anti-inflammatory potential of polyphenols contained in Mediterranean diet in obesity: Molecular mechanisms. Molecules 2021, 26, 985. [Google Scholar] [CrossRef]
- Shu, Y.; Zou, C.; Cai, Y.; He, Q.; Wu, X.; Zhu, H.; Qv, M.; Chao, Y.; Xu, C.; Tang, L.; et al. Vitamin C deficiency induces hypoglycemia and cognitive disorder through S-nitrosylation-mediated activation of glycogen synthase kinase 3β. Redox Biol. 2022, 56, 102420. [Google Scholar] [CrossRef]
- Fiore, M.; Mancinelli, R.; Aloe, L.; Laviola, G.; Sornelli, F.; Vitali, M.; Ceccanti, M. Hepatocyte growth factor, vascular endothelial growth factor, glial cell-derived neurotrophic factor and nerve growth factor are differentially affected by early chronic ethanol or red wine intake. Toxicol. Lett. 2009, 188, 208–213. [Google Scholar] [CrossRef]
- Fiore, M.; Messina, M.P.; Petrella, C.; D’Angelo, A.; Greco, A.; Ralli, M.; Ferraguti, G.; Tarani, L.; Vitali, M.; Ceccanti, M. Antioxidant properties of plant polyphenols in the counteraction of alcohol-abuse induced damage: Impact on the Mediterranean diet. J. Funct. Foods 2020, 71, 104012. [Google Scholar] [CrossRef]
- Petrella, C.; Di Certo, M.G.; Gabanella, F.; Barbato, C.; Ceci, F.M.; Greco, A.; Ralli, M.; Polimeni, A.; Angeloni, A.; Severini1, C.; et al. Mediterranean Diet, Brain and Muscle: Olive Polyphenols and Resveratrol Protection in Neurodegenerative and Neuromuscular Disorders. Curr. Med. Chem. 2021, 28, 7595–7613. [Google Scholar] [CrossRef]
- Carito, V.; Ceccanti, M.; Tarani, L.; Ferraguti, G.; Chaldakov, G.N.; Fiore, M. Neurotrophins’ Modulation by Olive Polyphenols. Curr. Med. Chem. 2016, 23, 3189–3197. [Google Scholar] [CrossRef]
- Carito, V.; Ciafrè, S.; Tarani, L.; Ceccanti, M.; Natella, F.; Iannitelli, A.; Tirassa, P.; Chaldakov, G.N.; Ceccanti, M.; Boccardo, C.; et al. TNF-α and IL-10 modulation induced by polyphenols extracted by olive pomace in a mouse model of paw inflammation. Ann. Ist. Super. Sanita 2015, 51, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Manach, C.; Scalbert, A.; Morand, C.; Rémésy, C.; Jime, L. Polyphenols: Food sources and bioavailability. Am. J. Clin. Nutr. 2004, 79, 727–747. [Google Scholar] [CrossRef] [PubMed]
- Manach, C.; Williamson, G.; Morand, C.; Scalbert, A.; Rémésy, C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am. J. Clin. Nutr. 2005, 81, 230S–242S. [Google Scholar] [CrossRef] [PubMed]
- Vogel, P.; Machado, I.K.; Garavaglia, J.; Zani, V.T.; de Souza, D.; Dal Bosco, S.M. Beneficios polifenoles hoja de olivo (Olea europaea L) para la salud humana. Nutr. Hosp. 2015, 31, 1427–1433. [Google Scholar] [CrossRef]
- Román, G.C.; Jackson, R.E.; Gadhia, R.; Román, A.N.; Reis, J. Mediterranean diet: The role of long-chain ω-3 fatty acids in fish; polyphenols in fruits, vegetables, cereals, coffee, tea, cacao and wine; probiotics and vitamins in prevention of stroke, age-related cognitive decline, and Alzheimer disease. Rev. Neurol. 2019, 175, 724–741. [Google Scholar] [CrossRef]
- Carito, V.; Venditti, A.; Bianco, A.; Ceccanti, M.; Serrilli, A.M.; Chaldakov, G.; Tarani, L.; De Nicolò, S.; Fiore, M. Effects of olive leaf polyphenols on male mouse brain NGF, BDNF and their receptors TrkA, TrkB and p75. Nat. Prod. Res. 2014, 28, 1970–1984. [Google Scholar] [CrossRef] [PubMed]
- Lewandowska, U.; Szewczyk, K.; Hrabec, E.; Janecka, A.; Gorlach, S. Overview of metabolism and bioavailability enhancement of polyphenols. J. Agric. Food Chem. 2013, 61, 12183–12199. [Google Scholar] [CrossRef]
- D’souza, S.; Addepalli, V. Preventive measures in oral cancer: An overview. Biomed. Pharmacother. 2018, 107, 72–80. [Google Scholar] [CrossRef]
- Petrella, C.; Ferraguti, G.; Tarani, L.; Chaldakov, G.N.; Ceccanti, M.; Greco, A.; Ralli, M.; Fiore, M. Chapter 39—Olive polyphenols and chronic alcohol protection. In Olives and Olive Oil in Health and Disease Prevention, 2nd ed.; Preedy, V.R., Ross Watson, R., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 471–478. [Google Scholar] [CrossRef]
- Chianese, R.; Coccurello, R.; Viggiano, A.; Scafuro, M.; Fiore, M.; Coppola, G.; Operto, F.F.; Fasano, S.; Laye, S.; Pierantoni, R.; et al. Impact of Dietary Fats on Brain Functions. Curr. Neuropharmacol. 2017, 16, 1059–1085. [Google Scholar] [CrossRef]
- Ceccanti, M.; De Nicolò, S.; Mancinelli, R.; Chaldakov, G.; Carito, V.; Ceccanti, M.; Laviola, G.; Tirassa, P.; Fiore, M. NGF and BDNF long-term variations in the thyroid, testis and adrenal glands of a mouse model of fetal alcohol spectrum disorders. Ann. Ist. Super. Sanita 2013, 49, 383–390. [Google Scholar] [CrossRef]
- Solfrizzi, V.; Capurso, C.; D’Introno, A.; Colacicco, A.M.; Santamato, A.; Ranieri, M.; Fiore, P.; Capurso, A.; Panza, F. Lifestyle-related factors in predementia and dementia syndromes. Expert Rev. Neurother. 2008, 8, 133–158. [Google Scholar] [CrossRef] [PubMed]
- Petrella, C.; Carito, V.; Carere, C.; Ferraguti, G.; Ciafrè, S.; Natella, F.; Bello, C.; Greco, A.; Ralli, M.; Mancinelli, R.; et al. Oxidative stress inhibition by resveratrol in alcohol-dependent mice. Nutrition 2020, 79–80, 110783. [Google Scholar] [CrossRef] [PubMed]
- Carito, V.; Ceccanti, M.; Cestari, V.; Natella, F.; Bello, C.; Coccurello, R.; Mancinelli, R.; Fiore, M. Olive polyphenol effects in a mouse model of chronic ethanol addiction. Nutrition 2017, 33, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Ceccanti, M.; Valentina, C.; Vitali, M.; Iannuzzi, S.; Tarani, L.; De Nicolo, S.; Ceccanti, M.M.; Ciafre, S.; Tirassa, P.; Capriglione, I.; et al. Serum BDNF and NGF Modulation by Olive Polyphenols in Alcoholics during Withdrawal. J. Alcohol. Drug Depend. 2015, 3, 1000214. [Google Scholar] [CrossRef]
- Kraft, T.E.; Parisotto, D.; Schempp, C.; Efferth, T. Fighting cancer with red wine? Molecular mechanisms of resveratrol. Crit. Rev. Food Sci. Nutr. 2009, 49, 782–799. [Google Scholar] [CrossRef] [PubMed]
- Bianchini, F.; Vainio, H. Wine and resveratrol: Mechanisms of cancer prevention? Eur. J. Cancer Prev. 2003, 12, 417–425. [Google Scholar] [CrossRef]
- Mongioì, L.M.; Vignera, S.L.; Cannarella, R.; Cimino, L.; Compagnone, M.; Condorelli, R.A.; Calogero, A.E. The role of resveratrol administration in human obesity. Int. J. Mol. Sci. 2021, 22, 4362. [Google Scholar] [CrossRef]
- Meng, X.; Zhou, J.; Zhao, C.N.; Gan, R.Y.; Li, H. Bin Health benefits and molecular mechanisms of resveratrol: A narrative review. Foods 2020, 9, 340. [Google Scholar] [CrossRef]
- Singh, P.; Barman, B.; Thakur, M.K. Oxidative stress-mediated memory impairment during aging and its therapeutic intervention by natural bioactive compounds. Front. Aging Neurosci. 2022, 14, 944697. [Google Scholar] [CrossRef]
- Calabrese, V.; Scapagnini, G.; Colombrita, C.; Ravagna, A.; Pennisi, G.; Giuffrida Stella, A.M.; Galli, F.; Butterfield, D.A. Redox regulation of heat shock protein expression in aging and neurodegenerative disorders associated with oxidative stress: A nutritional approach. Amino Acids 2003, 25, 437–444. [Google Scholar] [CrossRef]
- Calabrese, V.; Butterfield, D.A.; Stella, A.M.G. Nutritional antioxidants and the heme oxygenase pathway of stress tolerance: Novel targets for neuroprotection in Alzheimer’s disease. Ital. J. Biochem. 2003, 52, 177–181. [Google Scholar] [PubMed]
- Pentón-Rol, G.; Marín-Prida, J.; McCarty, M.F. C-Phycocyanin-derived Phycocyanobilin as a Potential Nutraceutical Approach for Major Neurodegenerative Disorders and COVID-19- induced Damage to the Nervous System. Curr. Neuropharmacol. 2021, 19, 2250–2275. [Google Scholar] [CrossRef] [PubMed]
- Farr, S.A.; Price, T.O.; Dominguez, L.J.; Motisi, A.; Saiano, F.; Niehoff, M.L.; Morley, J.E.; Banks, W.A.; Ercal, N.; Barbagallo, M. Extra Virgin Olive Oil Improves Learning and Memory in SAMP8 Mice. J. Alzheimers Dis. 2012, 28, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Norwitz, N.G.; Saif, N.; Ariza, I.E.; Isaacson, R.S. Precision nutrition for alzheimer’s prevention in apoe4 carriers. Nutrients 2021, 13, 1362. [Google Scholar] [CrossRef] [PubMed]
- Bucciantini, M.; Leri, M.; Nardiello, P.; Casamenti, F.; Stefani, M. Olive polyphenols: Antioxidant and anti-inflammatory properties. Antioxidants 2021, 10, 1044. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Barbagallo, M. Nutritional prevention of cognitive decline and dementia. Acta Biomed. 2018, 89, 276–290. [Google Scholar] [CrossRef]
- Moussa, C.; Hebron, M.; Huang, X.; Ahn, J.; Rissman, R.A.; Aisen, P.S.; Turner, R.S. Resveratrol regulates neuro-inflammation and induces adaptive immunity in Alzheimer’s disease. J. Neuroinflamm. 2017, 14, 1. [Google Scholar] [CrossRef]
- Abozaid, O.A.R.; Sallam, M.W.; El-Sonbaty, S.; Aziza, S.; Emad, B.; Ahmed, E.S.A. Resveratrol-Selenium Nanoparticles Alleviate Neuroinflammation and Neurotoxicity in a Rat Model of Alzheimer’s Disease by Regulating Sirt1/miRNA-134/GSK3β Expression. Biol. Trace Elem. Res. 2022, 200, 5104–5114. [Google Scholar] [CrossRef]
- Jin, F.; Wu, Q.; Lu, Y.-F.; Gong, Q.-H.; Shi, J.-S. Neuroprotective effect of resveratrol on 6-OHDA-induced Parkinson’s disease in rats. Eur. J. Pharmacol. 2008, 600, 78–82. [Google Scholar] [CrossRef]
- Candelario-Jalil, E.; de Oliveira, A.C.P.; Gräf, S.; Bhatia, H.S.; Hüll, M.; Muñoz, E.; Fiebich, B.L. Resveratrol potently reduces prostaglandin E2 production and free radical formation in lipopolysaccharide-activated primary rat microglia. J. Neuroinflamm. 2007, 4, 25. [Google Scholar] [CrossRef]
- Kim, Y.A.; Kim, G.-Y.; Park, K.-Y.; Choi, Y.H. Resveratrol inhibits nitric oxide and prostaglandin E2 production by lipopolysaccharide-activated C6 microglia. J. Med. Food 2007, 10, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.A.; Lim, S.-Y.; Rhee, S.-H.; Park, K.Y.; Kim, C.-H.; Choi, B.T.; Lee, S.J.; Park, Y.-M.; Choi, Y.H. Resveratrol inhibits inducible nitric oxide synthase and cyclooxygenase-2 expression in beta-amyloid-treated C6 glioma cells. Int. J. Mol. Med. 2006, 17, 1069–1075. [Google Scholar] [PubMed]
- Meng, X.-L.; Yang, J.-Y.; Chen, G.-L.; Wang, L.-H.; Zhang, L.-J.; Wang, S.; Li, J.; Wu, C.-F. Effects of resveratrol and its derivatives on lipopolysaccharide-induced microglial activation and their structure-activity relationships. Chem. Biol. Interact. 2008, 174, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wang, H.; Wu, Q.; Lu, Y.; Nie, J.; Xie, X.; Shi, J. Resveratrol protects cortical neurons against microglia-mediated neuroinflammation. Phytother. Res. 2013, 27, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Yuan, L.; Zhang, Q.; Gao, Y.; Liu, G.; Xiu, M.; Wei, X.; Wang, Z.; Liu, D. Resveratrol attenuates hypoxia-induced neurotoxicity through inhibiting microglial activation. Int. Immunopharmacol. 2015, 28, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Jing, T.; Yang, X.; He, Y.; Wang, B.; Xiao, Y.; Shang, C.; Zhang, J.; Lin, R. Hydroxytyrosol regulates the autophagy of vascular adventitial fibroblasts through the SIRT1-mediated signaling pathway. Can. J. Physiol. Pharmacol. 2018, 96, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Cabrerizo, S.; De La Cruz, J.P.; López-Villodres, J.A.; Muñoz-Marín, J.; Guerrero, A.; Reyes, J.J.; Labajos, M.T.; González-Correa, J.A. Role of the inhibition of oxidative stress and inflammatory mediators in the neuroprotective effects of hydroxytyrosol in rat brain slices subjected to hypoxia reoxygenation. J. Nutr. Biochem. 2013, 24, 2152–2157. [Google Scholar] [CrossRef]
- Muñoz-Marín, J.; De La Cruz, J.P.; Guerrero, A.; López-Leiva, I.; López-Villodres, J.A.; Reyes, J.J.; Espartero, J.L.; Madrona, A.; Labajos, M.T.; González-Correa, J.A. Cytoprotective effect of hydroxytyrosyl alkyl ether derivatives after oral administration to rats in a model of glucose-oxygen deprivation in brain slices. J. Agric. Food Chem. 2012, 60, 7659–7664. [Google Scholar] [CrossRef]
- Peng, Y.; Hou, C.; Yang, Z.; Li, C.; Jia, L.; Liu, J.; Tang, Y.; Shi, L.; Li, Y.; Long, J.; et al. Hydroxytyrosol mildly improve cognitive function independent of APP processing in APP/PS1 mice. Mol. Nutr. Food Res. 2016, 60, 2331–2342. [Google Scholar] [CrossRef]
- Shin, S.M.; Cho, I.J.; Kim, S.G. Resveratrol protects mitochondria against oxidative stress through AMP-activated protein kinase-mediated glycogen synthase kinase-3beta inhibition downstream of poly(ADP-ribose)polymerase-LKB1 pathway. Mol. Pharmacol. 2009, 76, 884–895. [Google Scholar] [CrossRef]
- Bastianetto, S.; Zheng, W.H.; Quirion, R. Neuroprotective abilities of resveratrol and other red wine constituents against nitric oxide-related toxicity in cultured hippocampal neurons. Br. J. Pharmacol. 2000, 131, 711–720. [Google Scholar] [CrossRef] [PubMed]
- Romero-Márquez, J.M.; Navarro-Hortal, M.D.; Jiménez-Trigo, V.; Muñoz-Ollero, P.; Forbes-Hernández, T.Y.; Esteban-Muñoz, A.; Giampieri, F.; Noya, I.D.; Bullón, P.; Vera-Ramírez, L.; et al. An Olive-Derived Extract 20% Rich in Hydroxytyrosol Prevents β-Amyloid Aggregation and Oxidative Stress, Two Features of Alzheimer Disease, via SKN-1/NRF2 and HSP-16.2 in Caenorhabditis elegans. Antioxidants 2022, 11, 629. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pérez, M.D.; Pérez de Algaba, I.; Martín-Aurioles, E.; Arrebola, M.M.; Ortega-Hombrados, L.; Verdugo, C.; Fernández-Prior, M.Á.; Bermúdez-Oria, A.; De La Cruz, J.P.; González-Correa, J.A. Neuroprotective Effect of 3′,4′-Dihydroxyphenylglycol in Type-1-like Diabetic Rats-Influence of the Hydroxytyrosol/3’,4’-dihydroxyphenylglycol Ratio. Nutrients 2022, 14, 1146. [Google Scholar] [CrossRef] [PubMed]
- Tasset, I.; Pontes, A.J.; Hinojosa, A.J.; de la Torre, R.; Túnez, I. Olive oil reduces oxidative damage in a 3-nitropropionic acid-induced Huntington’s disease-like rat model. Nutr. Neurosci. 2011, 14, 106–111. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Wightman, E.L.; Reay, J.L.; Lietz, G.; Okello, E.J.; Wilde, A.; Haskell, C.F. Effects of resveratrol on cerebral blood flow variables and cognitive performance in humans: A double-blind, placebo-controlled, crossover investigation. Am. J. Clin. Nutr. 2010, 91, 1590–1597. [Google Scholar] [CrossRef]
- Wightman, E.L.; Haskell-Ramsay, C.F.; Reay, J.L.; Williamson, G.; Dew, T.; Zhang, W.; Kennedy, D.O. The effects of chronic trans-resveratrol supplementation on aspects of cognitive function, mood, sleep, health and cerebral blood flow in healthy, young humans. Br. J. Nutr. 2015, 114, 1427–1437. [Google Scholar] [CrossRef]
- Evans, H.M.; Howe, P.R.C.; Wong, R.H.X. Effects of Resveratrol on Cognitive Performance, Mood and Cerebrovascular Function in Post-Menopausal Women; A 14-Week Randomised Placebo-Controlled Intervention Trial. Nutrients 2017, 9, 27. [Google Scholar] [CrossRef]
- Thaung Zaw, J.J.; Howe, P.R.; Wong, R.H. Long-term effects of resveratrol on cognition, cerebrovascular function and cardio-metabolic markers in postmenopausal women: A 24-month randomised, double-blind, placebo-controlled, crossover study. Clin. Nutr. 2021, 40, 820–829. [Google Scholar] [CrossRef]
- Thaung Zaw, J.J.; Howe, P.R.C.; Wong, R.H.X. Sustained Cerebrovascular and Cognitive Benefits of Resveratrol in Postmenopausal Women. Nutrients 2020, 12, 828. [Google Scholar] [CrossRef]
- Wong, R.H.X.; Nealon, R.S.; Scholey, A.; Howe, P.R.C. Low dose resveratrol improves cerebrovascular function in type 2 diabetes mellitus. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 393–399. [Google Scholar] [CrossRef]
- Wang, N.; He, J.; Pan, C.; Wang, J.; Ma, M.; Shi, X.; Xu, Z. Resveratrol Activates Autophagy via the AKT/mTOR Signaling Pathway to Improve Cognitive Dysfunction in Rats With Chronic Cerebral Hypoperfusion. Front. Neurosci. 2019, 13, 859. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; Xie, J.; Zhao, J.; Huang, T.; Guo, X.; Song, J. Resveratrol protects early brain injury after subarachnoid hemorrhage by activating autophagy and inhibiting apoptosis mediated by the Akt/mTOR pathway. Neuroreport 2018, 29, 368–379. [Google Scholar] [CrossRef] [PubMed]
- Pineda-Ramírez, N.; Alquisiras-Burgos, I.; Ortiz-Plata, A.; Ruiz-Tachiquín, M.-E.; Espinoza-Rojo, M.; Aguilera, P. Resveratrol Activates Neuronal Autophagy Through AMPK in the Ischemic Brain. Mol. Neurobiol. 2020, 57, 1055–1069. [Google Scholar] [CrossRef] [PubMed]
- Wightman, E.L.; Reay, J.L.; Haskell, C.F.; Williamson, G.; Dew, T.P.; Kennedy, D.O. Effects of resveratrol alone or in combination with piperine on cerebral blood flow parameters and cognitive performance in human subjects: A randomised, double-blind, placebo-controlled, cross-over investigation. Br. J. Nutr. 2014, 112, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Kwon, K.J.; Kim, H.-J.; Shin, C.Y.; Han, S.-H. Melatonin Potentiates the Neuroprotective Properties of Resveratrol Against Beta-Amyloid-Induced Neurodegeneration by Modulating AMP-Activated Protein Kinase Pathways. J. Clin. Neurol. 2010, 6, 127–137. [Google Scholar] [CrossRef]
- Han, Y.-S.; Zheng, W.-H.; Bastianetto, S.; Chabot, J.-G.; Quirion, R. Neuroprotective effects of resveratrol against beta-amyloid-induced neurotoxicity in rat hippocampal neurons: Involvement of protein kinase C. Br. J. Pharmacol. 2004, 141, 997–1005. [Google Scholar] [CrossRef]
- Schaffer, S.; Müller, W.E.; Eckert, G.P. Cytoprotective effects of olive mill wastewater extract and its main constituent hydroxytyrosol in PC12 cells. Pharmacol. Res. 2010, 62, 322–327. [Google Scholar] [CrossRef]
- Yeste, N.; Pérez-Valle, J.; Vázquez-Gómez, M.; García-Contreras, C.; González-Bulnes, A.; Bassols, A. Polyphenols and IUGR Pregnancies: Effects of the Antioxidant Hydroxytyrosol on the Hippocampus Proteome in a Porcine Model. Antioxidants 2022, 11, 1135. [Google Scholar] [CrossRef]
- Turner, R.S.; Thomas, R.G.; Craft, S.; Van Dyck, C.H.; Mintzer, J.; Reynolds, B.A.; Brewer, J.B.; Rissman, R.A.; Raman, R.; Aisen, P.S. A randomized, double-blind, placebo-controlled trial of resveratrol for Alzheimer disease. Neurology 2015, 85, 1383–1391. [Google Scholar] [CrossRef]
- Kumar, P.; Padi, S.S.V.; Naidu, P.S.; Kumar, A. Effect of resveratrol on 3-nitropropionic acid-induced biochemical and behavioural changes: Possible neuroprotective mechanisms. Behav. Pharmacol. 2006, 17, 485–492. [Google Scholar] [CrossRef]
- Raval, A.P.; Dave, K.R.; Perez-Pinzon, M.A. Resveratrol Mimics Ischemic Preconditioning in the Brain. J. Cereb. Blood Flow Metab. 2006, 26, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Hu, S.; Zhang, S.; Zhao, D.; Wang, Y.; Li, H.; Peng, Y.; Shi, L.; Xu, X.; Wang, C.; et al. Hydroxytyrosol Acetate Improves the Cognitive Function of APP/PS1 Transgenic Mice in ERβ-dependent Manner. Mol. Nutr. Food Res. 2021, 65, e2000797. [Google Scholar] [CrossRef] [PubMed]
- Arunsundar, M.; Shanmugarajan, T.S.; Ravichandran, V. 3,4-dihydroxyphenylethanol attenuates spatio-cognitive deficits in an Alzheimer’s disease mouse model: Modulation of the molecular signals in neuronal survival-apoptotic programs. Neurotox. Res. 2015, 27, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Zheng, A.; Li, H.; Cao, K.; Xu, J.; Zou, X.; Li, Y.; Chen, C.; Liu, J.; Feng, Z. Maternal hydroxytyrosol administration improves neurogenesis and cognitive function in prenatally stressed offspring. J. Nutr. Biochem. 2015, 26, 190–199. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, G.; Ceccarelli, M.; Bernini, R.; Clemente, M.; Santi, L.; Caruso, C.; Micheli, L.; Tirone, F. Hydroxytyrosol stimulates neurogenesis in aged dentate gyrus by enhancing stem and progenitor cell proliferation and neuron survival. FASEB J. 2020, 34, 4512–4526. [Google Scholar] [CrossRef] [PubMed]
- González-Correa, J.A.; Navas, M.D.; Lopez-Villodres, J.A.; Trujillo, M.; Espartero, J.L.; De La Cruz, J.P. Neuroprotective effect of hydroxytyrosol and hydroxytyrosol acetate in rat brain slices subjected to hypoxia-reoxygenation. Neurosci. Lett. 2008, 446, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Yeste, N.; Valent, D.; Arroyo, L.; Vázquez-Gómez, M.; García-Contreras, C.; Pumarola, M.; González-Bulnes, A.; Bassols, A. Polyphenols and IUGR Pregnancies: Effects of the Antioxidant Hydroxytyrosol on Brain Neurochemistry and Development in a Porcine Model. Antioxidants 2021, 10, 884. [Google Scholar] [CrossRef]
- Robles-Almazan, M.; Pulido-Moran, M.; Moreno-Fernandez, J.; Ramirez-Tortosa, C.; Rodriguez-Garcia, C.; Quiles, J.L.; Ramirez-Tortosa, M. Hydroxytyrosol: Bioavailability, toxicity, and clinical applications. Food Res. Int. 2018, 105, 654–667. [Google Scholar] [CrossRef]
- Bertelli, M.; Kiani, A.K.; Paolacci, S.; Manara, E.; Kurti, D.; Dhuli, K.; Bushati, V.; Miertus, J.; Pangallo, D.; Baglivo, M.; et al. Hydroxytyrosol: A natural compound with promising pharmacological activities. J. Biotechnol. 2020, 309, 29–33. [Google Scholar] [CrossRef]
- Warleta, F.; Quesada, C.S.; Campos, M.; Allouche, Y.; Beltrán, G.; Gaforio, J.J. Hydroxytyrosol protects against oxidative DNA damage in human breast cells. Nutrients 2011, 3, 839–857. [Google Scholar] [CrossRef]
- Fabiani, R.; Rosignoli, P.; De Bartolomeo, A.; Fuccelli, R.; Servili, M.; Montedoro, G.F.; Morozzi, G. Oxidative DNA damage is prevented by extracts of olive oil, hydroxytyrosol, and other olive phenolic compounds in human blood mononuclear cells and HL60 cells. J. Nutr. 2008, 138, 1411–1416. [Google Scholar] [CrossRef] [PubMed]
- Reutzel, M.; Grewal, R.; Silaidos, C.; Zotzel, J.; Marx, S.; Tretzel, J.; Eckert, G.P. Effects of long-term treatment with a blend of highly purified olive secoiridoids on cognition and brain ATP levels in aged NMRI mice. Oxid. Med. Cell. Longev. 2018, 2018, 4070935. [Google Scholar] [CrossRef] [PubMed]
- Leri, M.; Bertolini, A.; Stefani, M.; Bucciantini, M. Evoo polyphenols relieve synergistically autophagy dysregulation in a cellular model of alzheimer’s disease. Int. J. Mol. Sci. 2021, 22, 7225. [Google Scholar] [CrossRef] [PubMed]
- de Pablos, R.M.; Espinosa-Oliva, A.M.; Hornedo-Ortega, R.; Cano, M.; Arguelles, S. Hydroxytyrosol protects from aging process via AMPK and autophagy; a review of its effects on cancer, metabolic syndrome, osteoporosis, immune-mediated and neurodegenerative diseases. Pharmacol. Res. 2019, 143, 58–72. [Google Scholar] [CrossRef]
- Nardiello, P.; Pantano, D.; Lapucci, A.; Stefani, M.; Casamenti, F. Diet Supplementation with Hydroxytyrosol Ameliorates Brain Pathology and Restores Cognitive Functions in a Mouse Model of Amyloid-β Deposition. J. Alzheimer’s Dis. 2018, 63, 1161–1172. [Google Scholar] [CrossRef]
- Li, H.; Xu, X.; Cai, M.; Qu, Y.; Ren, Z.; Ye, C.; Shen, H. The combination of HT-ac and HBET improves the cognitive and learning abilities of heat-stressed mice by maintaining mitochondrial function through the PKA-CREB-BDNF pathway. Food Funct. 2022, 13, 6166–6179. [Google Scholar] [CrossRef]
- Romero-Márquez, J.M.; Navarro-Hortal, M.D.; Jiménez-Trigo, V.; Vera-Ramírez, L.; Forbes-Hernández, T.J.; Esteban-Muñoz, A.; Giampieri, F.; Bullón, P.; Battino, M.; Sánchez-González, C.; et al. An oleuropein rich-olive (Olea europaea L.) leaf extract reduces β-amyloid and tau proteotoxicity through regulation of oxidative- and heat shock-stress responses in Caenorhabditis elegans. Food Chem. Toxicol. 2022, 162, 112914. [Google Scholar] [CrossRef]
- Garcia-Contreras, C.; Vazquez-Gomez, M.; Barbero, A.; Pesantez, J.L.; Zinellu, A.; Berlinguer, F.; Gonzalez-Añover, P.; Gonzalez, J.; Encinas, T.; Torres-Rovira, L.; et al. Polyphenols and IUGR Pregnancies: Effects of Maternal Hydroxytyrosol Supplementation on Placental Gene Expression and Fetal Antioxidant Status, DNA-Methylation and Phenotype. Int. J. Mol. Sci. 2019, 20, 1187. [Google Scholar] [CrossRef]
- Li, X.; Tian, X.; Liu, T.; Li, M.; Wang, W.; Wang, P.; Guo, Z. Hydroxytyrosol Alleviated Hypoxia-Mediated PC12 Cell Damage through Activating PI3K/AKT/mTOR-HIF-1α Signaling. Oxid. Med. Cell. Longev. 2022, 2022, 8673728. [Google Scholar] [CrossRef]
- Calahorra, J.; Shenk, J.; Wielenga, V.H.; Verweij, V.; Geenen, B.; Dederen, P.J.; Peinado, M.Á.; Siles, E.; Wiesmann, M.; Kiliaan, A.J. Hydroxytyrosol, the Major Phenolic Compound of Olive Oil, as an Acute Therapeutic Strategy after Ischemic Stroke. Nutrients 2019, 11, 2430. [Google Scholar] [CrossRef]
- Barca, C.; Wiesmann, M.; Calahorra, J.; Wachsmuth, L.; Döring, C.; Foray, C.; Heiradi, A.; Hermann, S.; Peinado, M.Á.; Siles, E.; et al. Impact of hydroxytyrosol on stroke: Tracking therapy response on neuroinflammation and cerebrovascular parameters using PET-MR imaging and on functional outcomes. Theranostics 2021, 11, 4030–4049. [Google Scholar] [CrossRef] [PubMed]
- De Nicolò, S.; Carito, V.; Fiore, M.; Laviola, G. Aberrant Behavioral and Neurobiologic Profiles in Rodents Exposed to Ethanol or Red Wine Early in Development. Curr. Dev. Disord. Rep. 2014, 1, 173–180. [Google Scholar] [CrossRef]
- Griñán-Ferré, C.; Bellver-Sanchis, A.; Izquierdo, V.; Corpas, R.; Roig-Soriano, J.; Chillón, M.; Andres-Lacueva, C.; Somogyvári, M.; Sőti, C.; Sanfeliu, C.; et al. The pleiotropic neuroprotective effects of resveratrol in cognitive decline and Alzheimer’s disease pathology: From antioxidant to epigenetic therapy. Ageing Res. Rev. 2021, 67, 101271. [Google Scholar] [CrossRef] [PubMed]
- Lopez, M.S.; Dempsey, R.J.; Vemuganti, R. Resveratrol neuroprotection in stroke and traumatic CNS injury. Neurochem. Int. 2015, 89, 75–82. [Google Scholar] [CrossRef]
- Zhou, D.D.; Luo, M.; Huang, S.Y.; Saimaiti, A.; Shang, A.; Gan, R.Y.; Li, H. Bin Effects and Mechanisms of Resveratrol on Aging and Age-Related Diseases. Oxid. Med. Cell. Longev. 2021, 2021, 9932218. [Google Scholar] [CrossRef] [PubMed]
- Ceccanti, M.; Coccurello, R.; Carito, V.; Ciafrè, S.; Ferraguti, G.; Giacovazzo, G.; Mancinelli, R.; Tirassa, P.; Chaldakov, G.N.; Pascale, E.; et al. Paternal alcohol exposure in mice alters brain NGF and BDNF and increases ethanol-elicited preference in male offspring. Addict. Biol. 2016, 21, 776–787. [Google Scholar] [CrossRef] [PubMed]
- Miguel, C.A.; Noya-Riobó, M.V.; Mazzone, G.L.; Villar, M.J.; Coronel, M.F. Antioxidant, anti-inflammatory and neuroprotective actions of resveratrol after experimental nervous system insults. Special focus on the molecular mechanisms involved. Neurochem. Int. 2021, 150, 105188. [Google Scholar] [CrossRef] [PubMed]
- Palomera-Ávalos, V.; Griñán-Ferré, C.; Izquierdo, V.; Camins, A.; Sanfeliu, C.; Pallàs, M. Metabolic Stress Induces Cognitive Disturbances and Inflammation in Aged Mice: Protective Role of Resveratrol. Rejuvenation Res. 2017, 20, 202–217. [Google Scholar] [CrossRef]
- Terracina, S.; Ferraguti, G.; Tarani, L.; Messina, M.P.; Lucarelli, M.; Vitali, M.; De Persis, S.; Greco, A.; Minni, A.; Polimeni, A.; et al. Transgenerational Abnormalities Induced by Paternal Preconceptual Alcohol Drinking. Findings from Humans and Animal Models. Curr. Neuropharmacol. 2021, 19, 1158–1173. [Google Scholar] [CrossRef]
- Khorshidi, F.; Poljak, A.; Liu, Y.; Lo, J.W.; Crawford, J.D.; Sachdev, P.S. Resveratrol: A “miracle” drug in neuropsychiatry or a cognitive enhancer for mice only? A systematic review and meta-analysis. Ageing Res. Rev. 2021, 65, 101199. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Ruscica, M.; Banach, M. Resveratrol and cognitive decline: A clinician perspective. Arch. Med. Sci. 2019, 15, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Traversi, G.; Fiore, M.; Leone, S.; Basso, E.; Di Muzio, E.; Polticelli, F.; Degrassi, F.; Cozzi, R. Resveratrol and its methoxy-derivatives as modulators of DNA damage induced by ionising radiation. Mutagenesis 2016, 31, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Bastianetto, S.; Ménard, C.; Quirion, R. Neuroprotective action of resveratrol. Biochim. Biophys. Acta Mol. Basis Dis. 2015, 1852, 1195–1201. [Google Scholar] [CrossRef] [PubMed]
- Sakata, Y.; Zhuang, H.; Kwansa, H.; Koehler, R.C.; Doré, S. Resveratrol protects against experimental stroke: Putative neuroprotective role of heme oxygenase 1. Exp. Neurol. 2010, 224, 325–329. [Google Scholar] [CrossRef]
- Jhanji, M.; Rao, C.N.; Massey, J.C.; Hope, M.C.; Zhou, X.; Keene, C.D.; Ma, T.; Wyatt, M.D.; Stewart, J.A.; Sajish, M. Cis- and trans-resveratrol have opposite effects on histone serine-ADP-ribosylation and tyrosine induced neurodegeneration. Nat. Commun. 2022, 13, 3244. [Google Scholar] [CrossRef] [PubMed]
- Pardridge, W.M. Drug transport across the blood-brain barrier. J. Cereb. Blood Flow Metab. 2012, 32, 1959–1972. [Google Scholar] [CrossRef]
- Müller, W.E.; Eckert, A.; Kurz, C.; Eckert, G.P.; Leuner, K. Mitochondrial dysfunction: Common final pathway in brain aging and alzheimer’s disease-therapeutic aspects. Mol. Neurobiol. 2010, 41, 159–171. [Google Scholar] [CrossRef]
- Mattson, M.P.; Chan, S.L.; Duan, W. Modification of brain aging and neurodegenerative disorders by genes, diet, and behavior. Physiol. Rev. 2002, 82, 637–672. [Google Scholar] [CrossRef]
- Angelova, A.; Angelov, B.; Drechsler, M.; Lesieur, S. Neurotrophin delivery using nanotechnology. Drug Discov. Today 2013, 18, 1263–1271. [Google Scholar] [CrossRef]
- Oztaş, B.; Kiliç, S.; Dural, E.; Ispir, T. Influence of antioxidants on the blood-brain barrier permeability during epileptic seizures. J. Neurosci. Res. 2001, 66, 674–678. [Google Scholar] [CrossRef]
- Tasdemiroglu, E.; Christenberry, P.D.; Ardell, J.L.; Chronister, R.B.; Taylor, A.E. Effects of antioxidants on the blood-brain barrier and postischemic hyperemia. Acta Neurochir. 1994, 131, 302–309. [Google Scholar] [CrossRef]
- Oztas, B.; Akgul, S.; Seker, F.B. Gender difference in the influence of antioxidants on the blood-brain barrier permeability during pentylenetetrazol-induced seizures in hyperthermic rat pups. Biol. Trace Elem. Res. 2007, 118, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Pun, P.B.L.; Lu, J.; Moochhala, S. Involvement of ROS in BBB dysfunction. Free Radic. Res. 2009, 43, 348–364. [Google Scholar] [CrossRef] [PubMed]
- Mazzanti, G.; Di Giacomo, S. Curcumin and resveratrol in the management of cognitive disorders: What is the clinical evidence? Molecules 2016, 21, 1243. [Google Scholar] [CrossRef] [PubMed]
- Grodstein, F.; Lemos, B.; Yu, L.; Klein, H.U.; Iatrou, A.; Buchman, A.S.; Shireby, G.L.; Mill, J.; Schneider, J.A.; De Jager, P.L.; et al. The association of epigenetic clocks in brain tissue with brain pathologies and common aging phenotypes. Neurobiol. Dis. 2021, 157, 105428. [Google Scholar] [CrossRef]
- Noroozi, R.; Ghafouri-Fard, S.; Pisarek, A.; Rudnicka, J.; Spólnicka, M.; Branicki, W.; Taheri, M.; Pośpiech, E. DNA methylation-based age clocks: From age prediction to age reversion. Ageing Res. Rev. 2021, 68, 101314. [Google Scholar] [CrossRef]
- Bernal, A.J.; Dolinoy, D.C.; Huang, D.; Skaar, D.A.; Weinhouse, C.; Jirtle, R.L. Adaptive radiation-induced epigenetic alterations mitigated by antioxidants. FASEB J. 2013, 27, 665–671. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).