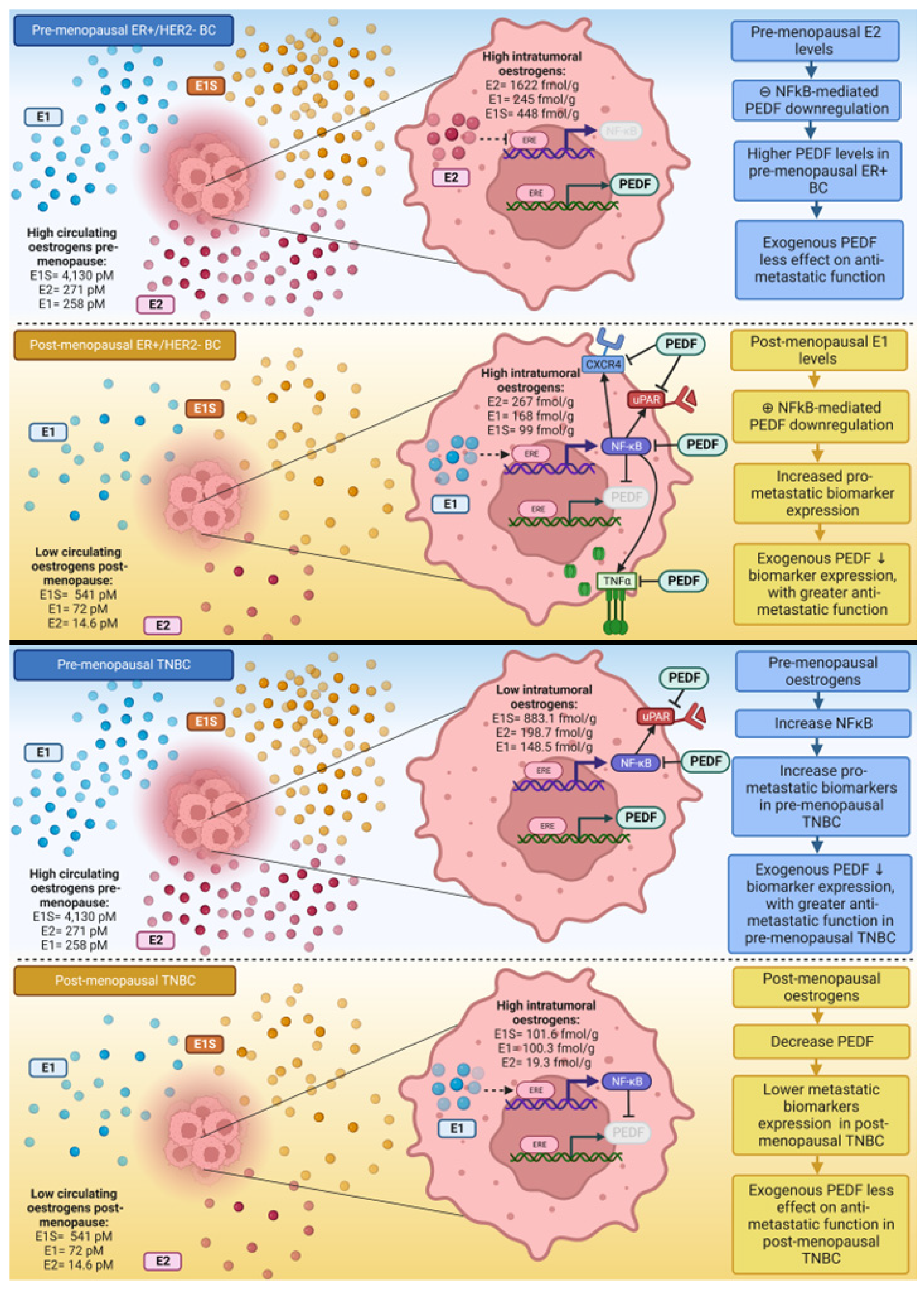
NFκB-Mediated Mechanisms Drive PEDF Expression and Function in Pre- and Post-Menopausal Oestrogen Levels in Breast Cancer
Abstract
1. Introduction
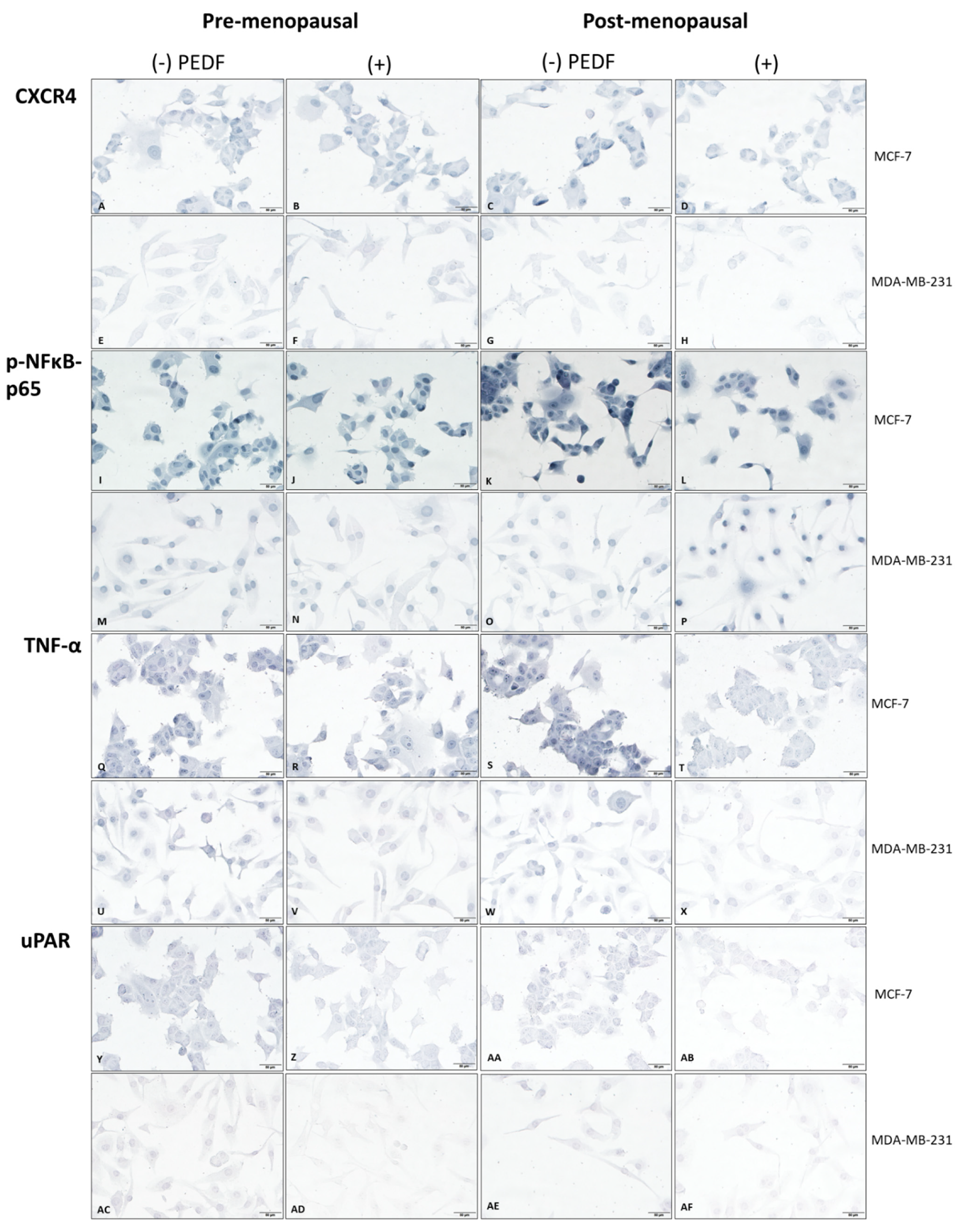
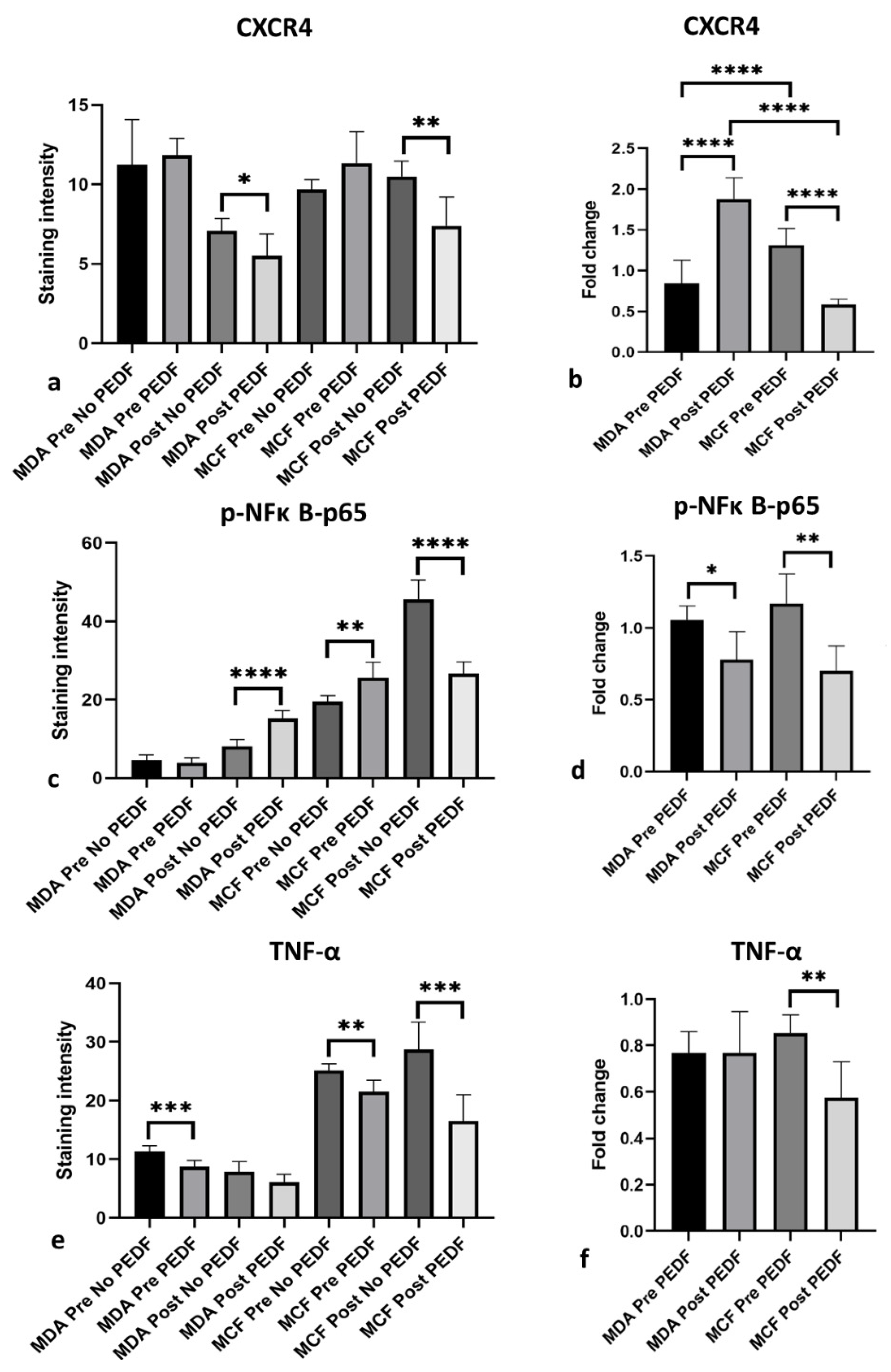
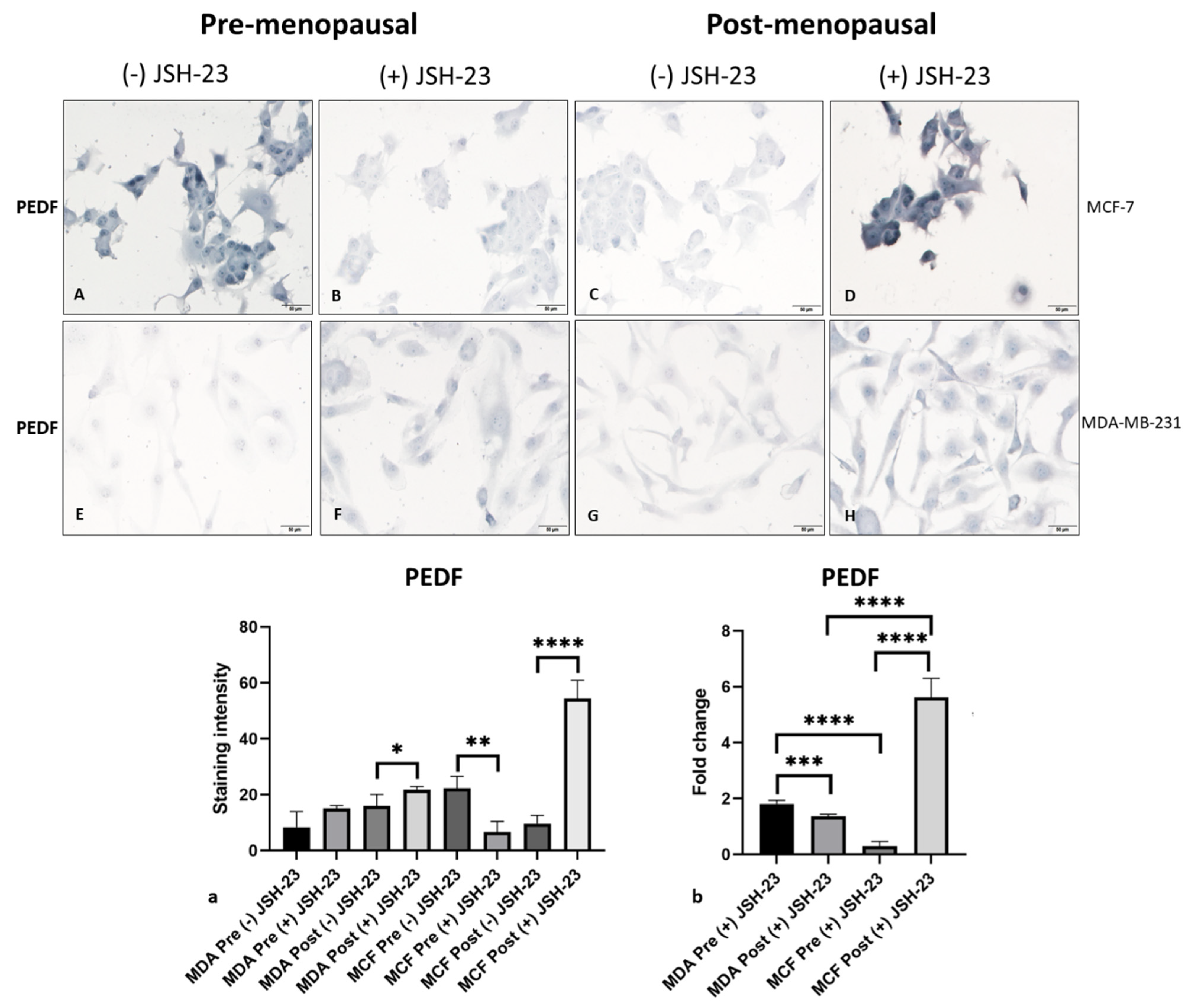
2. Results
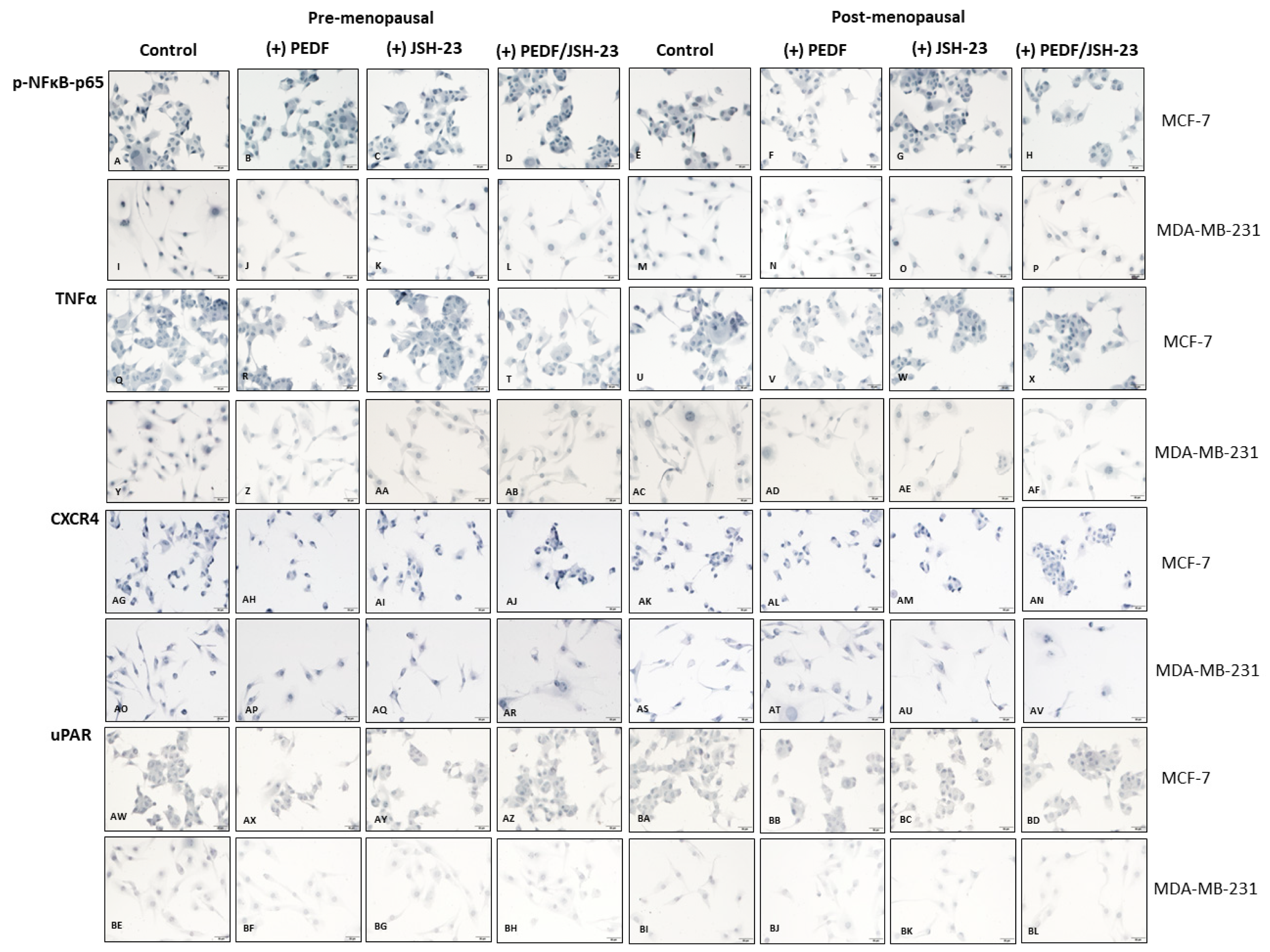
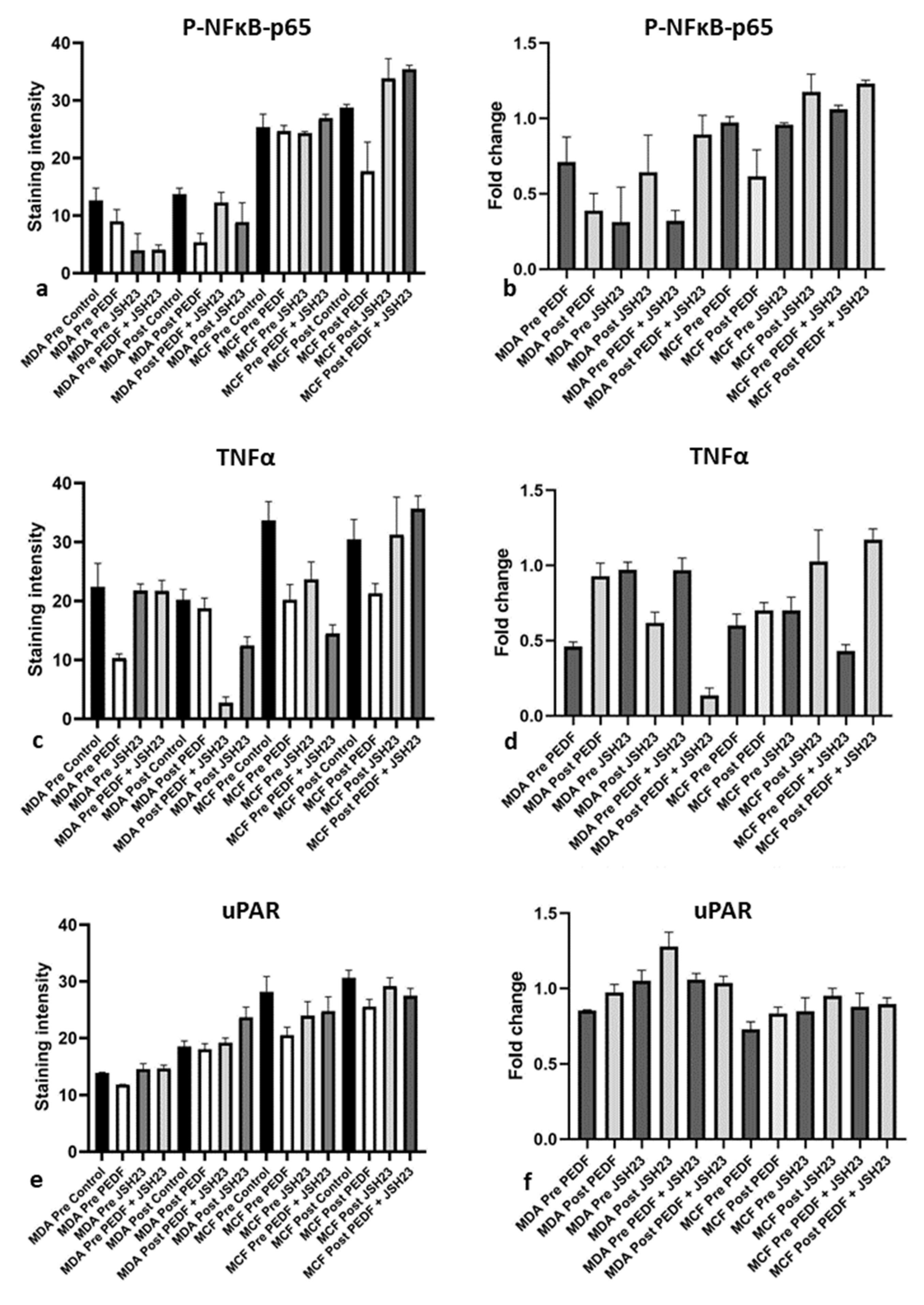
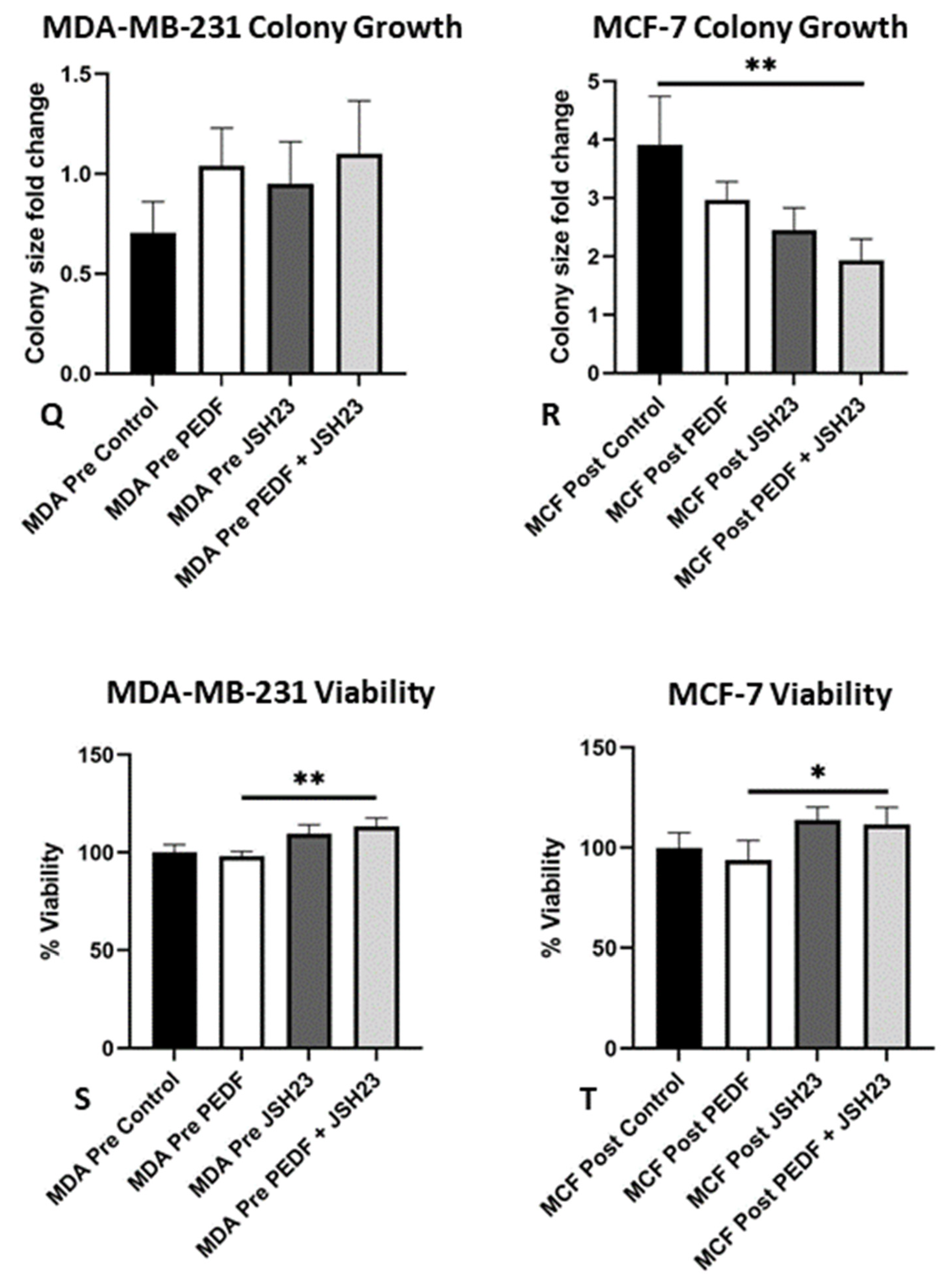
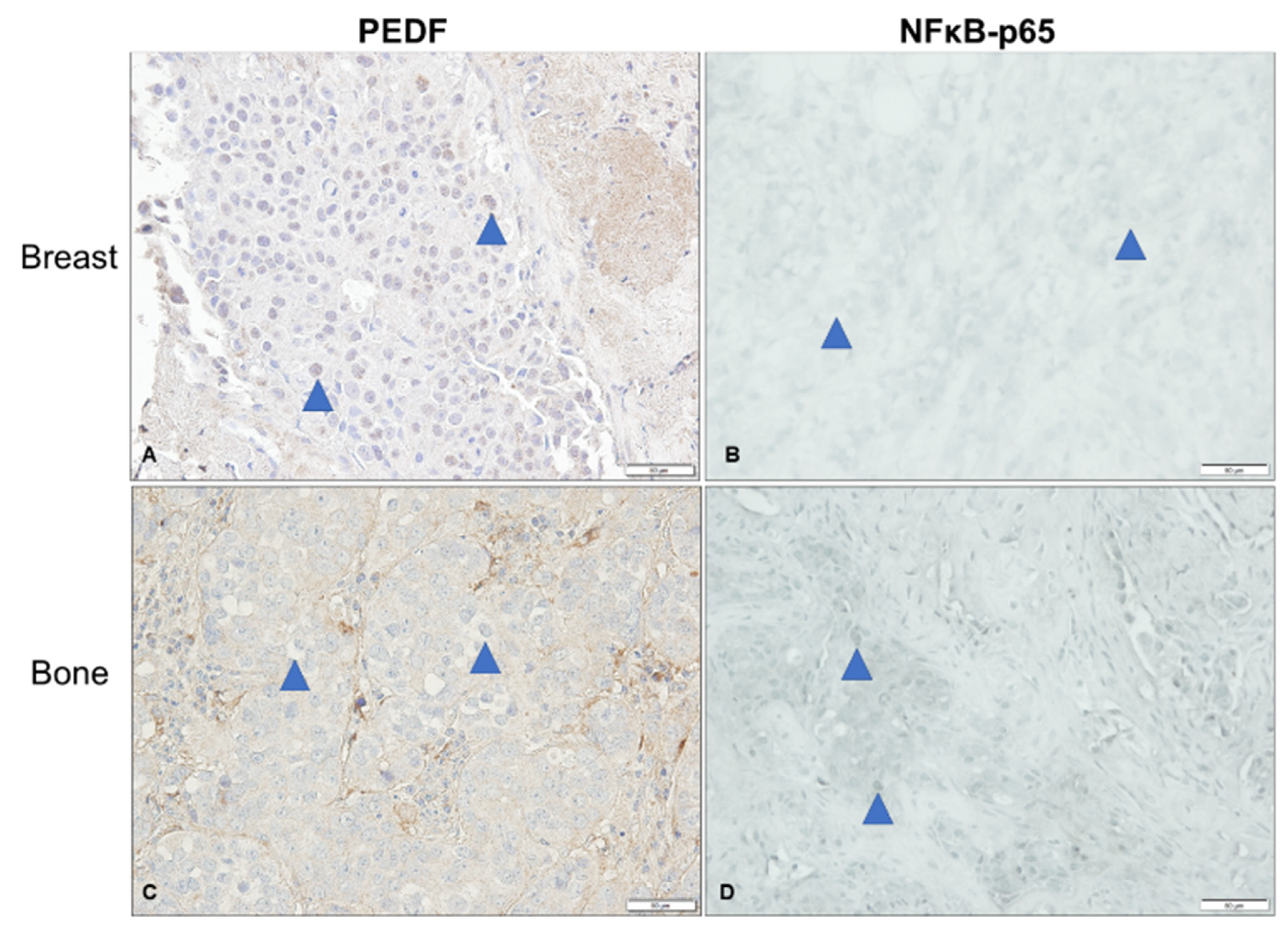
PEDF Differentially Regulates Biomarker Expression in Menopausal Conditions in ER + BC and TNBC Cells
3. Discussion
4. Materials and Methods
4.1. Reagents
4.2. Ethics
4.3. Patient Tissue Samples
4.4. Immunohistochemistry
4.5. Scoring of IHC
4.6. Cell Culture
4.7. Immunocytochemistry
4.8. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BC | breast cancer |
| CXCR4 | C-X-C chemokine receptor type 4 |
| DFS | disease-free survival |
| E1 | oestrone |
| E1S | oestrone sulphate |
| E2 | oestradiol |
| EPC-1 | early population doubling level cDNA-1 |
| ER | oestrogen receptor |
| FAK | focal adhesion kinase |
| HER2 | human epidermal growth factor receptor-2 |
| MT1-MMP | membrane-type 1 matrix metalloproteinase |
| NFκB | nuclear factor kappa B |
| OATP | organic anion transport protein |
| PEDF | pigment epithelium-derived factor |
| p-NFκB-p65 | phosphorylated-nuclear factor kappa B-p65 subunit |
| RANKL | receptor activator of nuclear factor kappa-Β ligand |
| RHOA | ras homolog family member A |
| RT | room temperature |
| SERPINF1 | serpin family F member 1 |
| STS | steroid sulfatase |
| TME | tumour microenvironment |
| TNBC | triple negative BC |
| TNF-α | tumour necrosis factor-alpha |
| uPA | urokinase-type plasminogen activator |
| uPAR | urokinase-type plasminogen activator receptor |
| VEGF | vascular endothelial growth factor |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: Individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012, 13, 1141–1151. [Google Scholar]
- Coleman, R. Metastatic bone disease: Clinical features, pathophysiology and treatment strategies. Cancer Treat. Rev. 2001, 27, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Brook, N.; Brook, E.; Dharmarajan, A.; Dass, C.R.; Chan, A. Breast cancer bone metastases: Pathogenesis and therapeutic targets. Int. J. Biochem. Cell Biol. 2018, 96, 63–78. [Google Scholar] [CrossRef]
- Hofbauer, L.C.; Rachner, T.D.; Coleman, R.E.; Jakob, F. Endocrine aspects of bone metastases. Lancet Diabetes Endocrinol. 2014, 2, 500–512. [Google Scholar] [CrossRef]
- Coleman, R.E.; Marshall, H.; Cameron, D.; Dodwell, D.; Burkinshaw, R.; Keane, M.; Gil, M.; Houston, S.J.; Grieve, R.J.; Barrett-Lee, P.J.; et al. Breast-Cancer Adjuvant Therapy with Zoledronic Acid. N. Engl. J. Med. 2011, 365, 1396–1405. [Google Scholar] [CrossRef]
- Tombran-Tink, J.; Pawar, H.; Swaroop, A.; Rodríguez, I.; Chader, G.J. Localization of the Gene for Pigment Epithelium-Derived Factor (PEDF) to Chromosome 17p13.1 and Expression in Cultured Human Retinoblastoma Cells. Genomics 1994, 19, 266–272. [Google Scholar] [CrossRef]
- Tombran-Tink, J.; Shivaram, S.M.; Chader, G.J.; Johnson, L.V.; Bok, D. Expression, Secretion, and Age-Related Downregulation of Pigment Epithelium-Derived Factor, a Serpin with Neurotrophic Activity. J. Neurosci. 1995, 15, 4992–5003. [Google Scholar] [CrossRef]
- Alberdi, E.; Hyde, C.C.; Becerra, S.P. Pigment Epithelium-Derived Factor (PEDF) Binds to Glycosaminoglycans: Analysis of the Binding Site. Biochemistry 1998, 37, 10643–10652. [Google Scholar] [CrossRef]
- Cauble, M.; Yang, P.; Baumann, U.; Gebauer, J.M.; Orr, B.G.; Duong, L.T.; Holl, M.M.B. Microstructure dependent binding of pigment epithelium derived factor (PEDF) to type I collagen fibrils. J. Struct. Biol. 2017, 199, 132–139. [Google Scholar] [CrossRef]
- Akiyama, T.; Dass, C.R.; Shinoda, Y.; Kawano, H.; Tanaka, S.; Choong, P.F. PEDF regulates osteoclasts via osteoprotegerin and RANKL. Biochem. Biophys. Res. Commun. 2010, 391, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Song, N.; Tombran-Tink, J.; Niyibizi, C. Pigment Epithelium-Derived Factor Enhances Differentiation and Mineral Deposition of Human Mesenchymal Stem Cells. Stem Cells 2013, 31, 2714–2723. [Google Scholar] [CrossRef] [PubMed]
- Alcantara, M.B.; Nemazannikova, N.; Elahy, M.; Dass, C.R. Pigment epithelium-derived factor upregulates collagen I and downregulates matrix metalloproteinase 2 in osteosarcoma cells, and colocalises to collagen I and heat shock protein 47 in fetal and adult bone. J. Pharm. Pharmacol. 2014, 66, 1586–1592. [Google Scholar] [PubMed]
- Chuderland, D.; Ben-Ami, I.; Kaplan-Kraicer, R.; Grossman, H.; Komsky, A.; Satchi-Fainaro, R.; Eldar-Boock, A.; Ron-El, R.; Shalgi, R. Hormonal regulation of pigment epithelium-derived factor (PEDF) in granulosa cells. Mol. Hum. Reprod. 2012, 19, 72–81. [Google Scholar] [CrossRef]
- Brook, N.; Brook, E.; Dass, C.; Chan, A.; Dharmarajan, A. Pigment Epithelium-Derived Factor and Sex Hormone-Responsive Cancers. Cancers 2020, 12, 3483. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Parr, C.; Watkins, G.; Jiang, W.G.; Boulton, M. Decreased Pigment Epithelium–Derived Factor Expression in Human Breast Cancer Progression. Clin. Cancer Res. 2006, 12, 3510–3517. [Google Scholar] [CrossRef]
- Palmieri, D.; Fitzgerald, D.; Shreeve, S.M.; Hua, E.; Bronder, J.L.; Weil, R.J.; Davis, S.; Stark, A.M.; Merino, M.J.; Kurek, R.; et al. Analyses of Resected Human Brain Metastases of Breast Cancer Reveal the Association between Up-Regulation of Hexokinase 2 and Poor Prognosis. Mol. Cancer Res. 2009, 7, 1438–1445. [Google Scholar] [CrossRef]
- Zhou, D.; Cheng, S.-Q.; Ji, H.-F.; Wang, J.-S.; Xu, H.-T.; Zhang, G.-Q.; Pang, D. Evaluation of protein pigment epithelium-derived factor (PEDF) and microvessel density (MVD) as prognostic indicators in breast cancer. J. Cancer Res. Clin. Oncol. 2010, 136, 1719–1727. [Google Scholar] [CrossRef]
- Brook, N.; Gill, J.; Chih, H.; Francis, K.; Dharmarajan, A.; Chan, A.; Dass, C.R. Pigment epithelium-derived factor downregulation in oestrogen receptor positive breast cancer bone metastases is associated with menopause. Mol. Cell. Endocrinol. 2023, 559, 111792. [Google Scholar] [CrossRef]
- Hung, C.-S.; Su, H.-Y.; Liang, H.-H.; Lai, C.-W.; Chang, Y.-C.; Ho, Y.-S.; Wu, C.-H.; Ho, J.-D.; Wei, P.-L.; Chang, Y.-J. High-level expression of CXCR4 in breast cancer is associated with early distant and bone metastases. Tumor Biol. 2013, 35, 1581–1588. [Google Scholar] [CrossRef]
- Boudot, A.; Kerdivel, G.; Habauzit, D.; Eeckhoute, J.; Le Dily, F.; Flouriot, G.; Samson, M.; Pakdel, F. Differential Estrogen-Regulation of CXCL12 Chemokine Receptors, CXCR4 and CXCR7, Contributes to the Growth Effect of Estrogens in Breast Cancer Cells. PLoS ONE 2011, 6, e20898. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Wei, Y.; Xia, J.; Wang, S.; Wu, J.; Chen, F.; Huang, G.; Chen, J. CXCL12–CXCR4 contributes to the implication of bone marrow in cancer metastasis. Futur. Oncol. 2014, 10, 749–759. [Google Scholar] [CrossRef]
- Winkler, J.; Abisoye-Ogunniyan, A.; Metcalf, K.J.; Werb, Z. Concepts of extracellular matrix remodelling in tumour progression and metastasis. Nat. Commun. 2020, 11, 5120. [Google Scholar] [CrossRef] [PubMed]
- Bennett, L.; Mallon, E.A.; Horgan, P.G.; Paul, A.; McMillan, D.C.; Edwards, J. The relationship between members of the canonical NF-κB pathway, components of tumour microenvironment and survival in patients with invasive ductal breast cancer. Oncotarget 2017, 8, 33002–33013. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Jiang, G.; Hu, X.; Yang, D.; Tan, T.; Gao, Z.; Chen, Z.; Xiang, C.; Li, S.; Ouyang, Z.; et al. Punicalin Attenuates Breast Cancer-Associated Osteolysis by Inhibiting the NF-κB Signaling Pathway of Osteoclasts. Front. Pharmacol. 2021, 12, 789552. [Google Scholar] [CrossRef]
- El-Shennawy, L.; Dubrovskyi, O.; Kastrati, I.; Danes, J.M.; Zhang, Y.; Whiteley, H.E.; Creighton, C.J.; Frasor, J. Coactivation of Estrogen Receptor and IKKβ Induces a Dormant Metastatic Phenotype in ER-Positive Breast CancerNovel Model of Dormant, Metastatic ER+ Breast Cancer. Cancer Res. 2018, 78, 974–984. [Google Scholar] [CrossRef]
- Olsen, S.N.; Wronski, A.; Castaño, Z.; Dake, B.; Malone, C.; De Raedt, T.; Enos, M.; DeRose, Y.S.; Zhou, W.; Guerra, S.; et al. Loss of RasGAP Tumor Suppressors Underlies the Aggressive Nature of Luminal B Breast CancersPathways That Drive Luminal B Tumor Progression. Cancer Discov. 2017, 7, 202–217. [Google Scholar] [CrossRef]
- Nicolin, V.; Bortul, R.; Bareggi, R.; Baldini, G.; Martinelli, B.; Narducci, P. Breast adenocarcinoma MCF-7 cell line induces spontaneous osteoclastogenesis via a RANK-ligand-dependent pathway. Acta Histochem. 2008, 110, 388–396. [Google Scholar] [CrossRef]
- Jones, D.H.; Nakashima, T.; Sanchez, O.H.; Kozieradzki, I.; Komarova, S.V.; Sarosi, I.; Morony, S.; Rubin, E.; Sarao, R.; Hojilla, C.V.; et al. Regulation of cancer cell migration and bone metastasis by RANKL. Nature 2006, 440, 692–696. [Google Scholar] [CrossRef]
- Plaks, V.; Kong, N.; Werb, Z. The Cancer Stem Cell Niche: How Essential Is the Niche in Regulating Stemness of Tumor Cells? Cell Stem Cell 2015, 16, 225–238. [Google Scholar] [CrossRef]
- Gentile, M.; Centonza, A.; Lovero, D.; Palmirotta, R.; Porta, C.; Silvestris, F.; D’Oronzo, S. Application of “omics” sciences to the prediction of bone metastases from breast cancer: State of the art. J. Bone Oncol. 2021, 26, 100337. [Google Scholar] [CrossRef] [PubMed]
- Duffy, M.J. The role of proteolytic enzymes in cancer invasion and metastasis. Clin. Exp. Metastasis 1992, 10, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-Y.; Nam, J.-S. The force awakens: Metastatic dormant cancer cells. Exp. Mol. Med. 2020, 52, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.; Gounari, F.; Prifti, S.; Hacker, H.J.; Schirrmacher, V.; Khazaie, K. EblacZ tumor dormancy in bone marrow and lymph nodes: Active control of proliferating tumor cells by CD8+ immune T cells. Cancer Res. 1998, 58, 5439–5446. [Google Scholar] [PubMed]
- Lønning, P.; Helle, H.; Duong, N.; Ekse, D.; Aas, T.; Geisler, J. Tissue estradiol is selectively elevated in receptor positive breast cancers while tumour estrone is reduced independent of receptor status. J. Steroid Biochem. Mol. Biol. 2009, 117, 31–41. [Google Scholar] [CrossRef]
- Zhou, D.; Zhang, M.; Xu, P.; Yu, Y.; Ye, G.; Zhang, L.; Wu, A. Expression of pigment epithelium-derived factor is associated with a good prognosis and is correlated with epithelial-mesenchymal transition-related genes in infiltrating ductal breast carcinoma. Oncol. Lett. 2015, 11, 116–124. [Google Scholar] [CrossRef]
- Hoesel, B.; Schmid, J.A. The complexity of NF-κB signaling in inflammation and cancer. Mol. Cancer 2013, 12, 1–15. [Google Scholar] [CrossRef]
- Qureshi, R.; Picon-Ruiz, M.; Aurrekoetxea-Rodriguez, I.; de Paiva, V.N.; D’Amico, M.; Yoon, H.; Radhakrishnan, R.; Morata-Tarifa, C.; Ince, T.; Lippman, M.E.; et al. The Major Pre- and Postmenopausal Estrogens Play Opposing Roles in Obesity-Driven Mammary Inflammation and Breast Cancer Development. Cell Metab. 2020, 31, 1154–1172. [Google Scholar] [CrossRef]
- Martínez-Reza, I.; Díaz, L.; García-Becerra, R. Preclinical and clinical aspects of TNF-α and its receptors TNFR1 and TNFR2 in breast cancer. J. Biomed. Sci. 2017, 24, 90. [Google Scholar] [CrossRef]
- Wolczyk, D.; Zaremba-Czogalla, M.; Hryniewicz-Jankowska, A.; Tabola, R.; Grabowski, K.; Sikorski, A.F.; Augoff, K. TNF-α promotes breast cancer cell migration and enhances the concentration of membrane-associated proteases in lipid rafts. Cell. Oncol. 2016, 39, 353–363. [Google Scholar] [CrossRef]
- To, S.Q.; Cheung, V.; Lazarus, K.A.; Knower, K.C.; Clyne, C.D. Estradiol regulates Tumor Necrosis Factor-α expression and secretion in Estrogen Receptor positive breast cancer cells. Mol. Cell. Endocrinol. 2014, 394, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Moll, N.M.; Ransohoff, R.M. CXCL12 and CXCR4 in bone marrow physiology. Expert Rev. Hematol. 2010, 3, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Everts, V.; Daci, E.; Tigchelaar-Gutter, W.; Hoeben, K.A.; Torrekens, S.; Carmeliet, G.; Beertsen, W. Plasminogen activators are involved in the degradation of bone by osteoclasts. Bone 2008, 43, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Furlan, F.; Galbiati, C.; Jorgensen, N.R.; Jensen, J.-E.B.; Mrak, E.; Rubinacci, A.; Talotta, F.; Verde, P.; Blasi, F. Urokinase Plasminogen Activator Receptor Affects Bone Homeostasis by Regulating Osteoblast and Osteoclast Function. J. Bone Miner. Res. 2007, 22, 1387–1396. [Google Scholar] [CrossRef] [PubMed]
- Daci, E.; Everts, V.; Torrekens, S.; Van Herck, E.; Tigchelaar-Gutterr, W.; Bouillon, R.; Carmeliet, G. Increased Bone Formation in Mice Lacking Plasminogen Activators. J. Bone Miner. Res. 2003, 18, 1167–1176. [Google Scholar] [CrossRef]
- Grøndahl-Hansen, J.; Peters, H.A.; Van Putten, W.L.; Look, M.P.; Pappot, H.; Rønne, E.; Dano, K.; Klijn, J.G.; Brünner, N.; Foekens, J.A. Prognostic significance of the receptor for urokinase plasminogen activator in breast cancer. Clin. Cancer Res. 1995, 1, 1079–1087. [Google Scholar]
- Grøndahl-Hansen, J.; Christensen, I.J.; Briand, P.; Pappot, H.; Mouridsen, H.T.; Blichert-Toft, M.; Danø, K.; Brünner, N. Plasminogen activator inhibitor type 1 in cytosolic tumor extracts predicts prognosis in low-risk breast cancer patients. Clin. Cancer Res. 1997, 3, 233–239. [Google Scholar]
- Henic, E.; Noskova, V.; Høyer-Hansen, G.; Hansson, S.; Casslén, B. Estradiol Attenuates EGF-Induced Rapid uPAR Mobilization and Cell Migration via the G-protein-Coupled Receptor 30 in Ovarian Cancer Cells. Int. J. Gynecol. Cancer 2009, 19, 214–222. [Google Scholar] [CrossRef]
- Zhang, S.X.; Wang, J.J.; Gao, G.; Shao, C.; Mott, R.; Ma, J. Pigment epithelium-derived factor (PEDF) is an endogenous antiinflammatory factor. FASEB J. 2005, 20, 323–325. [Google Scholar] [CrossRef]
- Wang, J.J.; Zhang, S.X.; Mott, R.; Chen, Y.; Knapp, R.R.; Cao, W.; Ma, J.-X. Anti-inflammatory effects of pigment epithelium-derived factor in diabetic nephropathy. Am. J. Physiol. Physiol. 2008, 294, F1166–F1173. [Google Scholar] [CrossRef]
- Zolochevska, O.; Yu, G.; Gimble, J.M.; Figueiredo, M.L. Pigment Epithelial-Derived Factor and Melanoma Differentiation Associated Gene-7 Cytokine Gene Therapies Delivered by Adipose-Derived Stromal/Mesenchymal Stem Cells are Effective in Reducing Prostate Cancer Cell Growth. Stem Cells Dev. 2012, 21, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Dass, C.R.; Choong, P.F.M. uPAR mediates anticancer activity of PEDF. Cancer Biol. Ther. 2008, 7, 1262–1270. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brook, N.; Brook, E.; Dharmarajan, A.; Chan, A.; Dass, C.R. The role of pigment epithelium-derived factor in protecting against cellular stress. Free. Radic. Res. 2019, 53, 1166–1180. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, F.; Deng, H.; Bi, Y.; Sun, W.; Zhao, Y.; Chen, Z.; Weng, J. PEDF Expression Is Inhibited by Insulin Treatment in Adipose Tissue via Suppressing 11β-HSD1. PLoS ONE 2013, 8, e84016. [Google Scholar] [CrossRef]
- Adak, M.; Das, D.; Niyogi, S.; Nagalakshmi, C.; Ray, D.; Chakrabarti, P. Inflammasome activation in Kupffer cells confers a protective response in nonalcoholic steatohepatitis through pigment epithelium-derived factor expression. FASEB J. 2018, 32, 6510–6524. [Google Scholar] [CrossRef] [PubMed]
- Helbig, G.; Christopherson, K.W.; Bhat-Nakshatri, P.; Kumar, S.; Kishimoto, H.; Miller, K.D.; Broxmeyer, H.E.; Nakshatri, H. NF-κ B Promotes Breast Cancer Cell Migration and Metastasis by Inducing the Expression of the Chemokine Receptor CXCR4. J. Biol. Chem. 2003, 278, 21631–21638. [Google Scholar] [CrossRef]
- Shanmugam, M.K.; Ahn, K.S.; Hsu, A.; Woo, C.C.; Yuan, Y.; Tan, K.H.B.; Chinnathambi, A.; Alahmadi, T.A.; Alharbi, S.A.; Koh, A.P.F.; et al. Thymoquinone Inhibits Bone Metastasis of Breast Cancer Cells Through Abrogation of the CXCR4 Signaling Axis. Front. Pharmacol. 2018, 9, 1294. [Google Scholar] [CrossRef]
- Moreau, M.; Mourah, S.; Dosquet, C. β-Catenin and NF-κB cooperate to regulate the uPA/uPAR system in cancer cells. Int. J. Cancer 2011, 128, 1280–1292. [Google Scholar] [CrossRef]
- Fan, P.; Tyagi, A.K.; Agboke, F.A.; Mathur, R.; Pokharel, N.; Jordan, V.C. Modulation of nuclear factor-kappa B activation by the endoplasmic reticulum stress sensor PERK to mediate estrogen-induced apoptosis in breast cancer cells. Cell Death Discov. 2018, 4, 15. [Google Scholar] [CrossRef]
- Pignolo, R.J. Putative role for EPC-1/PEDF in the G0 growth arrest of human diploid fibroblasts. J. Cell. Physiol. 2003, 195, 12–20. [Google Scholar]
- Haynes, B.P.; Straume, A.H.; Geisler, J.; A’Hern, R.; Helle, H.; Smith, I.E.; Lønning, P.E.; Dowsett, M. Intratumoral Estrogen Disposition in Breast Cancer. Clin. Cancer Res. 2010, 16, 1790–1801. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.W.T.; Au, S.C.L.; Cheung, A.N.Y.; Ngan, H.Y.S.; Tombran-Tink, J.; Auersperg, N.; Wong, A.S.T. Pigment Epithelium-Derived Factor Is Estrogen Sensitive and Inhibits the Growth of Human Ovarian Cancer and Ovarian Surface Epithelial Cells. Endocrinology 2006, 147, 4179–4191. [Google Scholar] [CrossRef] [PubMed]
- Chuderland, D.; Ben-Ami, I.; Friedler, S.; Hasky, N.; Ninio-Many, L.; Goldberg, K.; Bar-Joseph, H.; Grossman, H.; Shalgi, R. Hormonal regulation of pigment epithelium-derived factor (PEDF) expression in the endometrium. Mol. Cell. Endocrinol. 2014, 390, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Salamanna, F.; Borsari, V.; Brogini, S.; Torricelli, P.; Cepollaro, S.; Cadossi, M.; Fini, M. A Human 3D In Vitro Model to Assess the Relationship Between Osteoporosis and Dissemination to Bone of Breast Cancer Tumor Cells. J. Cell. Physiol. 2017, 232, 1826–1834. [Google Scholar] [CrossRef] [PubMed]
- Rothenberger, N.J.; Somasundaram, A.; Stabile, L.P. The Role of the Estrogen Pathway in the Tumor Microenvironment. Int. J. Mol. Sci. 2018, 19, 611. [Google Scholar] [CrossRef]
- Ottewell, P.D.; Wang, N.; Brown, H.K.; Fowles, C.A.; Croucher, P.I.; Eaton, C.L.; Holen, I. OPG-Fc inhibits ovariectomy-induced growth of disseminated breast cancer cells in bone. Int. J. Cancer 2015, 137, 968–977. [Google Scholar] [CrossRef]
- Lønning, P.E.; Haynes, B.P.; Straume, A.H.; Dunbier, A.; Helle, H.; Knappskog, S.; Dowsett, M. Exploring Breast Cancer Estrogen Disposition: The Basis for Endocrine Manipulation. Clin. Cancer Res. 2011, 17, 4948–4958. [Google Scholar] [CrossRef]
- Al Sarakbi, W.; Mokbel, R.; Salhab, M.; Jiang, W.; Reed, M.J.; Mokbel, K. The role of STS and OATP-B mRNA expression in predicting the clinical outcome in human breast cancer. Anticancer Res. 2007, 26, 4985–4990. [Google Scholar]
- Zhu, B.T.; Han, G.-Z.; Shim, J.-Y.; Wen, Y.; Jiang, X.-R. Quantitative Structure-Activity Relationship of Various Endogenous Estrogen Metabolites for Human Estrogen Receptor α and β Subtypes: Insights into the Structural Determinants Favoring a Differential Subtype Binding. Endocrinology 2006, 147, 4132–4150. [Google Scholar] [CrossRef]
- Williams, C.; Lin, C.-Y. Oestrogen receptors in breast cancer: Basic mechanisms and clinical implications. Ecancermedicalscience 2013, 7, 370. [Google Scholar]
- Secky, L.; Svoboda, M.; Klameth, L.; Bajna, E.; Hamilton, G.; Zeillinger, R.; Jäger, W.; Thalhammer, T. The Sulfatase Pathway for Estrogen Formation: Targets for the Treatment and Diagnosis of Hormone-Associated Tumors. J. Drug Deliv. 2013, 2013, 957605. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, N.; Miller, N.; Allen, C.; Bendayan, R. Expression of membrane transporters and metabolic enzymes involved in estrone-3-sulphate disposition in human breast tumour tissues. Breast Cancer Res. Treat. 2014, 145, 647–661. [Google Scholar] [CrossRef] [PubMed]
- Austin, D.; Hamilton, N.; Elshimali, Y.; Pietras, R.; Wu, Y.; Vadgama, J. Estrogen receptor-beta is a potential target for triple negative breast cancer treatment. Oncotarget 2018, 9, 33912–33930. [Google Scholar] [CrossRef]
- Al-Bader, M.; Ford, C.; Al-Ayadhy, B.; Francis, I. Analysis of estrogen receptor isoforms and variants in breast cancer cell lines. Exp. Ther. Med. 2011, 2, 537–544. [Google Scholar] [CrossRef]
- Song, P.; Li, Y.; Dong, Y.; Liang, Y.; Qu, H.; Qi, D.; Lu, Y.; Jin, X.; Guo, Y.; Jia, Y.; et al. Estrogen receptor β inhibits breast cancer cells migration and invasion through CLDN6-mediated autophagy. J. Exp. Clin. Cancer Res. 2019, 38, 354. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Notari, L.; Becerra, S.P. Mapping the type I collagen-binding site on pigment epithelium-derived factor: Implications for its antiangiogenic activity. J. Biol. Chem. 2002, 277, 45400–45407. [Google Scholar] [CrossRef] [PubMed]
- Yasui, N.; Mori, T.; Morito, D.; Matsushita, O.; Kourai, H.; Nagata, A.K.; Koide, T. Dual-Site Recognition of Different Extracellular Matrix Components by Anti-Angiogenic/Neurotrophic Serpin, PEDF. Biochemistry 2003, 42, 3160–3167. [Google Scholar] [CrossRef]
- Jan, R.; Huang, M.; Lewis-Wambi, J. Loss of pigment epithelium-derived factor: A novel mechanism for the development of endocrine resistance in breast cancer. Breast Cancer Res. 2012, 14, R146. [Google Scholar] [CrossRef]
- Wang, N.; Wang, B.; Wang, Y.; Hu, J. Estrogen receptor positive operable breast cancer: Does menopausal status impact on HER2 and progesterone receptor status? Breast 2011, 20, 519–524. [Google Scholar] [CrossRef]
- Sitterley, G. Collagen attachment protocols, solubility, and stability. BioFiles 2008, 3, 5. [Google Scholar]
- Petersen, S.V.; Valnickova, Z.; Enghild, J.J. Pigment-epithelium-derived factor (PEDF) occurs at a physiologically relevant concentration in human blood: Purification and characterization. Biochem. J. 2003, 374, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.M.; Zhang, H.; Park, C.C. NF-κB regulates radioresistance mediated by β1-integrin in three-dimensional culture of breast cancer cells. Cancer Res. 2013, 73, 3737–3748. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Ma, J.; Fu, Z.; Zhang, Z.; Cao, J.; Huang, L.; Li, W.; Xu, P.; Cao, X. Promotion of breast cancer cells MDA-MB-231 invasion by di (2-ethylhexyl) phthalate through matrix metalloproteinase-2/-9 overexpression. Environ. Sci. Pollut. Res. 2016, 23, 9742–9749. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, C.Y.; Barberi, T.J.; Ghosh, P.; Longo, D.L. Phosphorylation of RelA/p65 on serine 536 defines an IκBα-independent NF-κB pathway. J. Biol. Chem. 2005, 280, 34538–34547. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.-C.; Chen, S.-L.; Shih, S.-C.; Wu, J.-Y.; Han, W.-H.; Cheng, H.-C.; Yang, S.-L.; Tsao, Y.-P. Pigment Epithelium-Derived Factor Is an Intrinsic Antifibrosis Factor Targeting Hepatic Stellate Cells. Am. J. Pathol. 2010, 177, 1798–1811. [Google Scholar] [CrossRef]



| Biomarker | Function in Breast Cancer Bone Metastasis | References |
|---|---|---|
| CXCR4 | Promotes BC cell homing to bone; enhances BC cell proliferation and survival; increases neovascularisation; drives chemoresistance. | [20,21,22] |
| MT1-MMP | Promotes ECM proteolysis and BC cell invasion | [23] |
| NFκB | Promotes osteoclastogenesis; promotes BC cell survival; promotes DTC dormancy; promotes BC cell invasion; drives EMT. | [24,25,26,27] |
| RANKL | Promotes osteoclastogenesis; promotes osteolysis; Promotes BC cell homing to bone; | [28,29] |
| TNFα | Promotes DTC colonisation and survival in bone; promotes osteoclastogenesis and osteolysis. | [30,31] |
| uPA/uPAR | Promotes ECM proteolysis and BC cell invasion; promotes DTC dormancy | [32,33,34] |
| Tumour Site and Subcellular Localisation | Overall Scores (Mean ± Standard Deviation) | p-Value | |
|---|---|---|---|
| Breast (n = 4) | PEDF | p-NFκB-p65 | |
| − Cytoplasm | 3.25 ± 0.96 | 3 ± 2.45 | 0.8555 |
| − Nuclear | 2.75 ± 1.5 | 2.5 ± 1.91 | 0.8439 |
| Bone (n = 4) | |||
| − Cytoplasm | 3 ± 0.82 | 2.5 ± 3 | 0.7586 |
| − Nuclear | 1.5 ± 1 | 4.75 ± 2.22 | 0.0369 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brook, N.; Gill, J.; Dharmarajan, A.; Chan, A.; Dass, C.R. NFκB-Mediated Mechanisms Drive PEDF Expression and Function in Pre- and Post-Menopausal Oestrogen Levels in Breast Cancer. Int. J. Mol. Sci. 2022, 23, 15641. https://doi.org/10.3390/ijms232415641
Brook N, Gill J, Dharmarajan A, Chan A, Dass CR. NFκB-Mediated Mechanisms Drive PEDF Expression and Function in Pre- and Post-Menopausal Oestrogen Levels in Breast Cancer. International Journal of Molecular Sciences. 2022; 23(24):15641. https://doi.org/10.3390/ijms232415641
Chicago/Turabian StyleBrook, Naomi, Jespal Gill, Arun Dharmarajan, Arlene Chan, and Crispin R. Dass. 2022. "NFκB-Mediated Mechanisms Drive PEDF Expression and Function in Pre- and Post-Menopausal Oestrogen Levels in Breast Cancer" International Journal of Molecular Sciences 23, no. 24: 15641. https://doi.org/10.3390/ijms232415641
APA StyleBrook, N., Gill, J., Dharmarajan, A., Chan, A., & Dass, C. R. (2022). NFκB-Mediated Mechanisms Drive PEDF Expression and Function in Pre- and Post-Menopausal Oestrogen Levels in Breast Cancer. International Journal of Molecular Sciences, 23(24), 15641. https://doi.org/10.3390/ijms232415641








