Application of Asymmetrical Flow Field-Flow Fractionation for Characterizing the Size and Drug Release Kinetics of Theranostic Lipid Nanovesicles
Abstract
1. Introduction
2. Results
2.1. Liposome Size Characterization
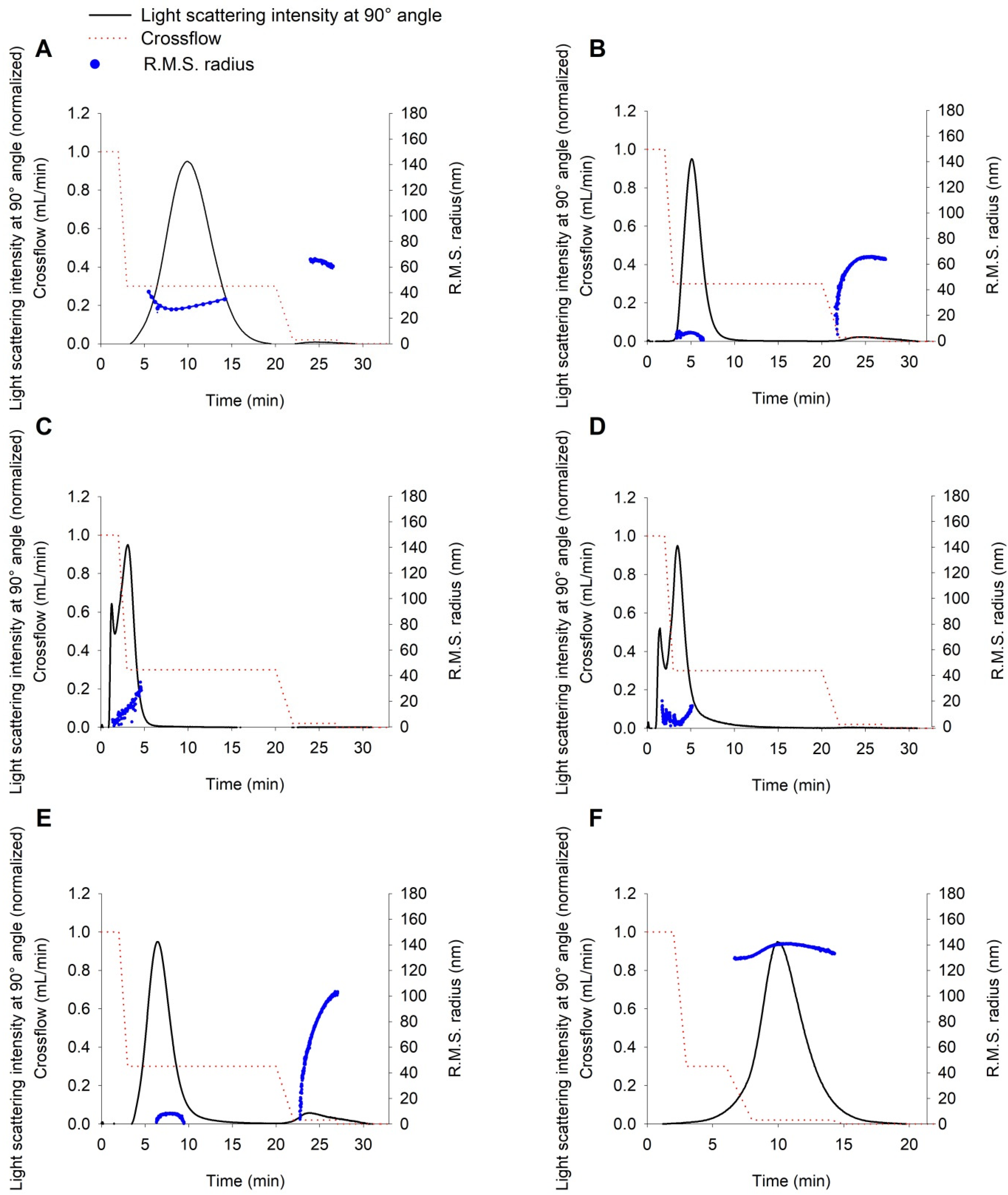
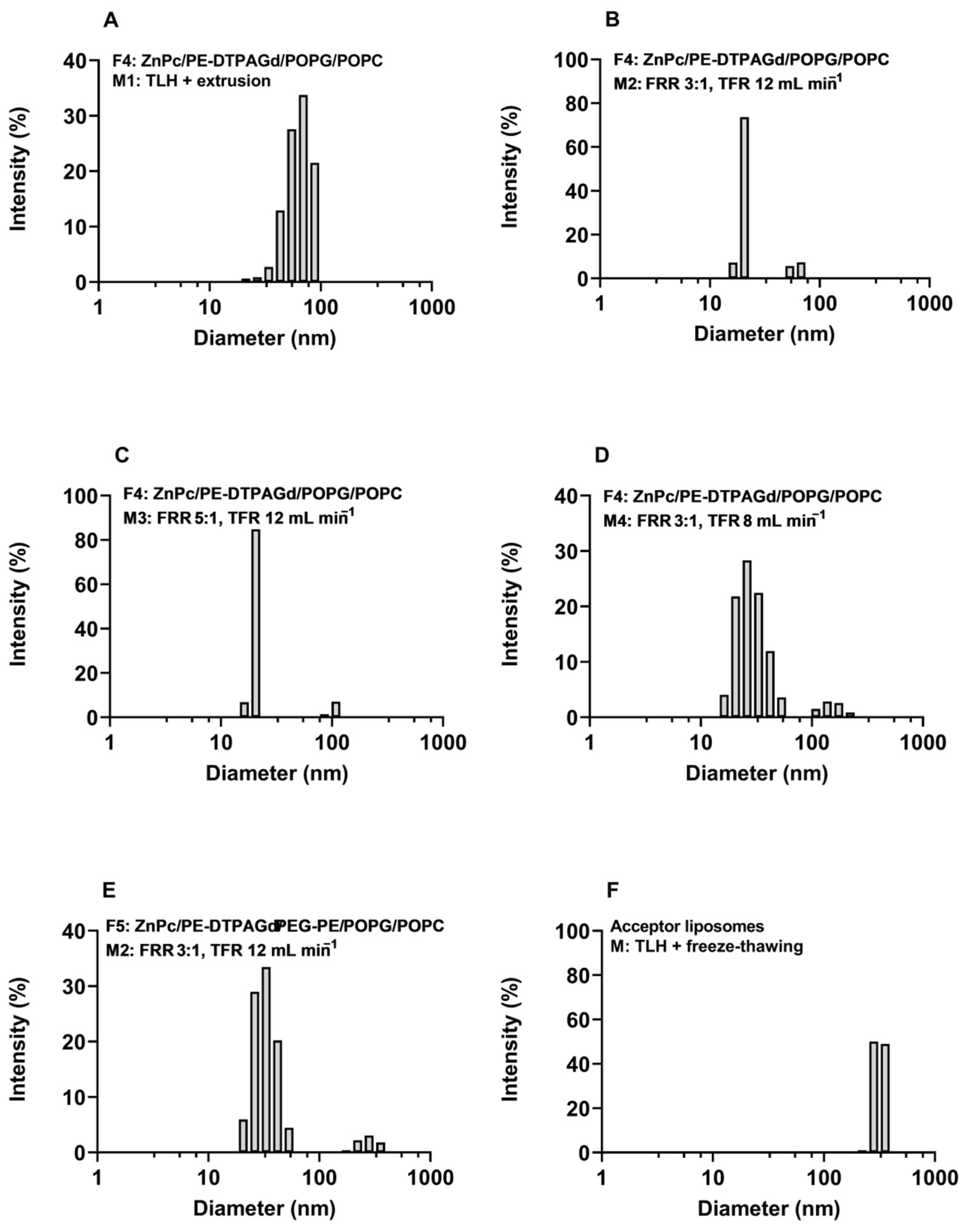
2.2. Characterization of Liposome Size by DLS and AF4-MALLS
2.3. Transfer Study
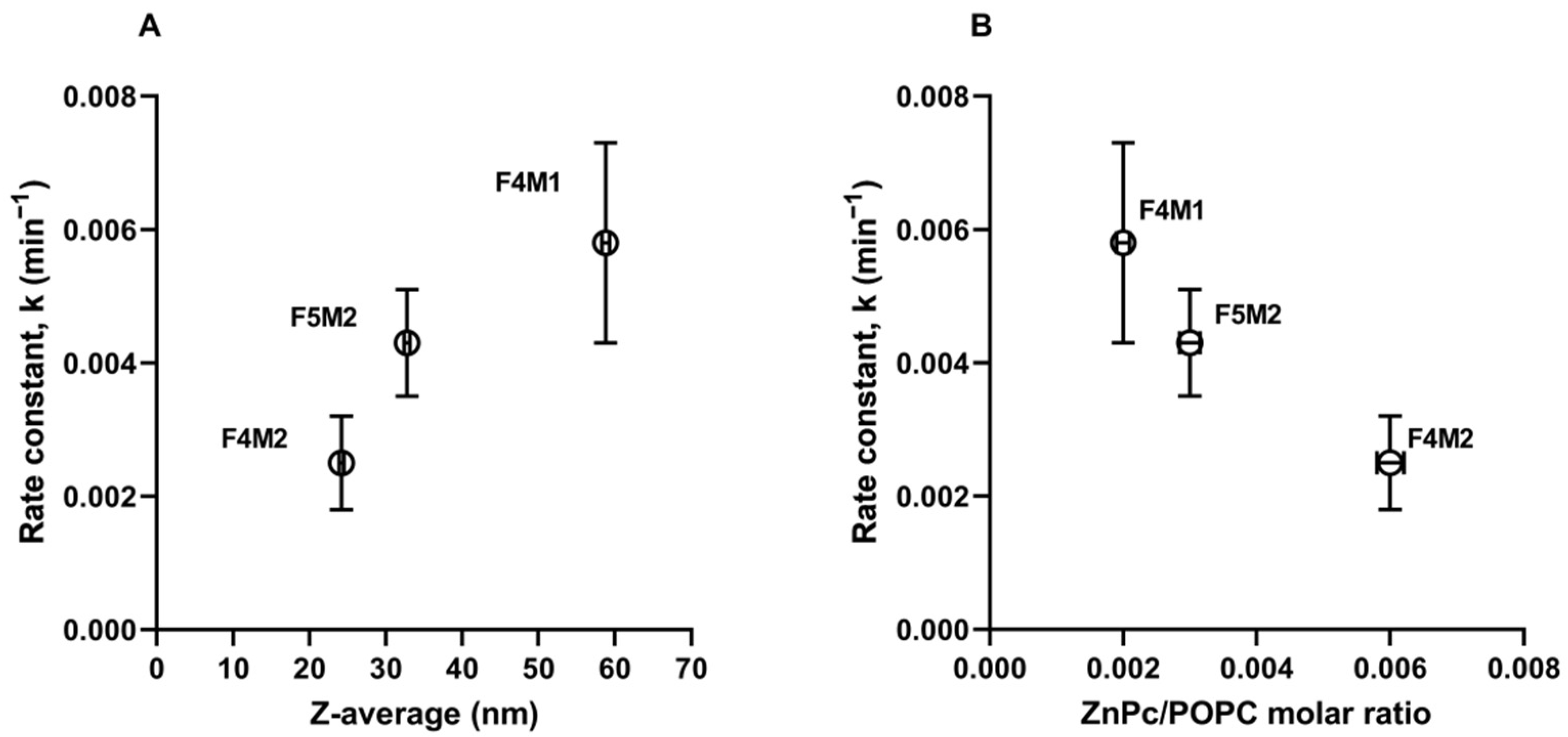
2.4. Mathematical Modeling of ZnPc Release from DL
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Thin Lipid Film Hydration Followed by Extrusion (TLH+Extrusion)
4.3. Micromixer and Microfluidic Preparation of Liposomes
4.4. Acceptor Liposome Preparation
4.5. Quantification of ZnPc, Phosphatidylcholine and Gd Chelate Content in Liposome Formulations
4.6. Dynamic Light Scattering (DLS) Measurements
4.7. Asymmetrical Flow Field-Flow Fractionation System with MALLS Detection
4.8. Size Analysis by AF4 with MALLS Detection
4.9. Transfer Study and Offline Quantification of ZnPc
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Center for Drug Evaluation and Research. Liposome Drug Products: Chemistry, Manufacturing, and Controls; Human Pharmacokinetics and Bioavailability; and Labeling Documentation. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/liposome-drug-products-chemistry-manufacturing-and-controls-human-pharmacokinetics-and (accessed on 28 February 2021).
- European Medicines Agency Data Requirements for Intravenous Liposomal Products Developed with Reference to an Innovator Product. Available online: https://www.ema.europa.eu/en/data-requirements-intravenous-liposomal-products-developed-reference-innovator-liposomal-product-0 (accessed on 28 February 2021).
- Cheng, X.; Gao, J.; Ding, Y.; Lu, Y.; Wei, Q.; Cui, D.; Fan, J.; Li, X.; Zhu, E.; Lu, Y.; et al. Multi-Functional Liposome: A Powerful Theranostic Nano-Platform Enhancing Photodynamic Therapy. Adv. Sci. 2021, 76, 2100876. [Google Scholar] [CrossRef]
- Lee, W.; Im, H.-J. Theranostics Based on Liposome: Looking Back and Forward. Nucl. Med. Mol. Imaging 2019, 53, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Porfire, A.; Achim, M.; Barbalata, C.; Rus, I.; Tomuta, I.; Cristea, C. Pharmaceutical Development of Liposomes Using the QbD Approach. In Liposomes—Advances and Perspectives; Catala, A., Ed.; IntechOpen: London, UK, 2019; ISBN 978-1-78984-494-8. [Google Scholar]
- Gómez-Hens, A.; Fernández-Romero, J.M. Analytical Methods for the Control of Liposomal Delivery Systems. TrAC Trends Anal. Chem. 2006, 25, 167–178. [Google Scholar] [CrossRef]
- Filippov, A.V.; Khakimov, A.M.; Munavirov, B.V. Chapter Two—31P NMR Studies of Phospholipids. In Annual Reports on NMR Spectroscopy; Webb, G.A., Ed.; Academic Press: Cambridge, MA, USA, 2015; Volume 85, pp. 27–92. [Google Scholar]
- Kothalawala, N.; Mudalige, T.K.; Sisco, P.; Linder, S.W. Novel Analytical Methods to Assess the Chemical and Physical Properties of Liposomes. J. Chromatogr. B 2018, 1091, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Fehér, B.; Kitka, D.; Wacha, A.; Bóta, A.; Berényi, S.; Pipich, V.; Fraikin, J.-L. Size Measurement of Extracellular Vesicles and Synthetic Liposomes: The Impact of the Hydration Shell and the Protein Corona. Colloids Surf. B Biointerfaces 2020, 192, 111053. [Google Scholar] [CrossRef] [PubMed]
- Hinna, A.; Steiniger, F.; Hupfeld, S.; Stein, P.; Kuntsche, J.; Brandl, M. Filter-Extruded Liposomes Revisited: A Study into Size Distributions and Morphologies in Relation to Lipid-Composition and Process Parameters. J. Liposome Res. 2016, 26, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Quattrini, F.; Berrecoso, G.; Crecente-Campo, J.; Alonso, M.J. Asymmetric Flow Field-Flow Fractionation as a Multifunctional Technique for the Characterization of Polymeric Nanocarriers. Drug Deliv. Transl. Res. 2021, 11, 373–395. [Google Scholar] [CrossRef] [PubMed]
- Mildner, R.; Hak, S.; Parot, J.; Hyldbakk, A.; Borgos, S.E.; Some, D.; Johann, C.; Caputo, F. Improved Multidetector Asymmetrical-Flow Field-Flow Fractionation Method for Particle Sizing and Concentration Measurements of Lipid-Based Nanocarriers for RNA Delivery. Eur. J. Pharm. Biopharm. 2021, 163, 252–265. [Google Scholar] [CrossRef] [PubMed]
- Fraunhofer, W.; Winter, G. The Use of Asymmetrical Flow Field-Flow Fractionation in Pharmaceutics and Biopharmaceutics. Eur. J. Pharm. Biopharm. 2004, 58, 369–383. [Google Scholar] [CrossRef]
- Hinna, A.; Steiniger, F.; Hupfeld, S.; Brandl, M.; Kuntsche, J. Asymmetrical Flow Field-Flow Fractionation with on-Line Detection for Drug Transfer Studies: A Feasibility Study. Anal. Bioanal. Chem. 2014, 406, 7827–7839. [Google Scholar] [CrossRef]
- Petersen, S.; Fahr, A.; Bunjes, H. Flow Cytometry as a New Approach To Investigate Drug Transfer between Lipid Particles. Mol. Pharm. 2010, 7, 350–363. [Google Scholar] [CrossRef]
- Hinna, A.H.; Hupfeld, S.; Kuntsche, J.; Brandl, M. The Use of Asymmetrical Flow Field-Flow Fractionation with on-Line Detection in the Study of Drug Retention within Liposomal Nanocarriers and Drug Transfer Kinetics. J. Pharm. Biomed. Anal. 2016, 124, 157–163. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, S. A Review of In Vitro Drug Release Test Methods for Nano-Sized Dosage Forms. Available online: https://www.hindawi.com/journals/ap/2014/304757/ (accessed on 14 June 2020).
- Solomon, D.; Gupta, N.; Mulla, N.S.; Shukla, S.; Guerrero, Y.A.; Gupta, V. Role of In Vitro Release Methods in Liposomal Formulation Development: Challenges and Regulatory Perspective. AAPS J. 2017, 19, 1669–1681. [Google Scholar] [CrossRef]
- de Souza, T.D.; Ziembowicz, F.I.; Müller, D.F.; Lauermann, S.C.; Kloster, C.L.; Santos, R.C.V.; Lopes, L.Q.S.; Ourique, A.F.; Machado, G.; Villetti, M.A. Evaluation of Photodynamic Activity, Photostability and in Vitro Drug Release of Zinc Phthalocyanine-Loaded Nanocapsules. Eur. J. Pharm. Sci. 2016, 83, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Gil, D.; Frank-Kamenetskii, A.; Barry, J.; Reukov, V.; Xiang, Y.; Das, A.; Varma, A.K.; Kindy, M.S.; Banik, N.L.; Vertegel, A. Albumin-Assisted Method Allows Assessment of Release of Hydrophobic Drugs From Nanocarriers. Biotechnol. J. 2018, 13, 1700337. [Google Scholar] [CrossRef]
- de Paula, C.S.; Tedesco, A.C.; Primo, F.L.; Vilela, J.M.C.; Andrade, M.S.; Mosqueira, V.C.F. Chloroaluminium Phthalocyanine Polymeric Nanoparticles as Photosensitisers: Photophysical and Physicochemical Characterisation, Release and Phototoxicity in Vitro. Eur. J. Pharm. Sci. 2013, 49, 371–381. [Google Scholar] [CrossRef]
- Strasdat, B.; Bunjes, H. Development of a New Approach to Investigating the Drug Transfer from Colloidal Carrier Systems Applying Lipid Nanosuspension-Containing Alginate Microbeads as Acceptor. Int. J. Pharm. 2015, 489, 203–209. [Google Scholar] [CrossRef]
- Knoke, S.; Bunjes, H. Transfer of Lipophilic Drugs from Nanoemulsions into Lipid-Containing Alginate Microspheres. Pharmaceutics 2021, 13, 173. [Google Scholar] [CrossRef] [PubMed]
- Hinna, A.H.; Hupfeld, S.; Kuntsche, J.; Bauer-Brandl, A.; Brandl, M. Mechanism and Kinetics of the Loss of Poorly Soluble Drugs from Liposomal Carriers Studied by a Novel Flow Field-Flow Fractionation-Based Drug Release−/Transfer-Assay. J. Control. Release 2016, 232, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Skupin-Mrugalska, P.; Sobotta, L.; Warowicka, A.; Wereszczynska, B.; Zalewski, T.; Gierlich, P.; Jarek, M.; Nowaczyk, G.; Kempka, M.; Gapinski, J.; et al. Theranostic Liposomes as a Bimodal Carrier for Magnetic Resonance Imaging Contrast Agent and Photosensitizer. J. Inorg. Biochem. 2018, 180, 1–14. [Google Scholar] [CrossRef]
- Skupin-Mrugalska, P.; Zalewski, T.; Elvang, P.A.; Nowaczyk, G.; Czajkowski, M.; Piotrowska-Kempisty, H. Insight into Theranostic Nanovesicles Prepared by Thin Lipid Hydration and Microfluidic Method. Colloids Surf. B Biointerfaces 2021, 205, 111871. [Google Scholar] [CrossRef]
- Isele, U.; van Hoogevest, P.; Leuenberger, H.; Capraro, H.-G.; Schieweck, K. Pharmaceutical Development of CGP 55847: A Liposomal Zn-Phthalocyanine Formulation Using a Controlled Organic Solvent Dilution Method; SPIE: Bellingham, WA USA, 1994; Volume 2078, pp. 397–403. [Google Scholar]
- Schieweck, K.; Capraro, H.-G.; Isele, U.; van Hoogevest, P.; Ochsner, M.; Maurer, T.; Batt, E. CGP 55 847, Liposome-Delivered Zinc(II)-Phthalocyanine as a Phototherapeutic Agent for Tumors; SPIE: Bellingham, WA USA, 1994; Volume 2078, pp. 107–118. [Google Scholar]
- Sekkat, N.; van den Bergh, H.; Nyokong, T.; Lange, N. Like a Bolt from the Blue: Phthalocyanines in Biomedical Optics. Molecules 2011, 17, 98–144. [Google Scholar] [CrossRef]
- Skupin-Mrugalska, P.; Piskorz, J.; Goslinski, T.; Mielcarek, J.; Konopka, K.; Düzgüneş, N. Current Status of Liposomal Porphyrinoid Photosensitizers. Drug Discov. Today 2013, 18, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Castano, A.P.; Demidova, T.N.; Hamblin, M.R. Mechanisms in Photodynamic Therapy: Part Two—Cellular Signaling, Cell Metabolism and Modes of Cell Death. Photodiagn. Photodyn. Ther. 2005, 2, 1–23. [Google Scholar] [CrossRef]
- Biel, M.A. Photodynamic Therapy of Head and Neck Cancers. Methods Mol. Biol. 2010, 635, 281–293. [Google Scholar] [CrossRef] [PubMed]
- de Lima, J.M.; Bonan, P.R.; da Cruz Perez, D.E.; Hier, M.; Alaoui-Jamali, M.A.; da Silva, S.D. Nanoparticle-Based Chemotherapy Formulations for Head and Neck Cancer: A Systematic Review and Perspectives. Nanomaterials 2020, 10, 1938. [Google Scholar] [CrossRef]
- Strieth, S.; Dunau, C.; Michaelis, U.; Jäger, L.; Gellrich, D.; Wollenberg, B.; Dellian, M. Phase I/II Clinical Study on Safety and Antivascular Effects of Paclitaxel Encapsulated in Cationic Liposomes for Targeted Therapy in Advanced Head and Neck Cancer. Head Neck 2014, 36, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Harrington, K.J.; Lewanski, C.; Northcote, A.D.; Whittaker, J.; Peters, A.M.; Vile, R.G.; Stewart, J.S.W. Phase II Study of Pegylated Liposomal Doxorubicin (CaelyxTM) as Induction Chemotherapy for Patients with Squamous Cell Cancer of the Head and Neck. Eur. J. Cancer 2001, 37, 2015–2022. [Google Scholar] [CrossRef]
- Litzinger, D.C.; Buiting, A.M.J.; van Rooijen, N.; Huang, L. Effect of Liposome Size on the Circulation Time and Intraorgan Distribution of Amphipathic Poly(Ethylene Glycol)-Containing Liposomes. Biochim. Biophys. Acta (BBA)-Biomembr. 1994, 1190, 99–107. [Google Scholar] [CrossRef]
- Zhang, Y.; Huo, M.; Zhou, J.; Zou, A.; Li, W.; Yao, C.; Xie, S. DDSolver: An Add-In Program for Modeling and Comparison of Drug Dissolution Profiles. AAPS J. 2010, 12, 263–271. [Google Scholar] [CrossRef]
- Mathematical models of drug release. In Strategies to Modify the Drug Release from Pharmaceutical Systems; Bruschi, M.L., Ed.; Woodhead Publishing: Cambridge, UK, 2015; pp. 63–86. ISBN 978-0-08-100092-2. [Google Scholar]
- Ernsting, M.J.; Murakami, M.; Roy, A.; Li, S.-D. Factors Controlling the Pharmacokinetics, Biodistribution and Intratumoral Penetration of Nanoparticles. J. Control. Release 2013, 172, 782–794. [Google Scholar] [CrossRef]
- Matsumura, Y.; Maeda, H. A New Concept for Macromolecular Therapeutics in Cancer Chemotherapy: Mechanism of Tumoritropic Accumulation of Proteins and the Antitumor Agent Smancs. Cancer Res. 1986, 46, 6387–6392. [Google Scholar]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor Vascular Permeability and the EPR Effect in Macromolecular Therapeutics: A Review. J. Control. Release 2000, 65, 271–284. [Google Scholar] [CrossRef]
- Choi, H.S.; Liu, W.; Misra, P.; Tanaka, E.; Zimmer, J.P.; Ipe, B.I.; Bawendi, M.G.; Frangioni, J.V. Renal Clearance of Nanoparticles. Nat. Biotechnol. 2007, 25, 1165–1170. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Mori, A.; Huang, L. Role of Liposome Size and RES Blockade in Controlling Biodistribution and Tumor Uptake of GM1-Containing Liposomes. Biochim. Biophys. Acta (BBA)-Biomembr. 1992, 1104, 95–101. [Google Scholar] [CrossRef]
- Yuan, F.; Dellian, M.; Fukumura, D.; Leunig, M.; Berk, D.A.; Torchilin, V.P.; Jain, R.K. Vascular Permeability in a Human Tumor Xenograft: Molecular Size Dependence and Cutoff Size. Cancer Res. 1995, 55, 3752–3756. [Google Scholar]
- Harrington, K.J.; Mohammadtaghi, S.; Uster, P.S.; Glass, D.; Peters, A.M.; Vile, R.G.; Stewart, J.S.W. Effective Targeting of Solid Tumors in Patients With Locally Advanced Cancers by Radiolabeled Pegylated Liposomes. Clin. Cancer Res. 2001, 7, 243–254. [Google Scholar]
- Cabral, H.; Matsumoto, Y.; Mizuno, K.; Chen, Q.; Murakami, M.; Kimura, M.; Terada, Y.; Kano, M.R.; Miyazono, K.; Uesaka, M.; et al. Accumulation of Sub-100 Nm Polymeric Micelles in Poorly Permeable Tumours Depends on Size. Nat. Nanotech. 2011, 6, 815–823. [Google Scholar] [CrossRef]
- Huo, S.; Ma, H.; Huang, K.; Liu, J.; Wei, T.; Jin, S.; Zhang, J.; He, S.; Liang, X.-J. Superior Penetration and Retention Behavior of 50 Nm Gold Nanoparticles in Tumors. Cancer Res. 2013, 73, 319–330. [Google Scholar] [CrossRef]
- Lee, H.; Fonge, H.; Hoang, B.; Reilly, R.M.; Allen, C. The Effects of Particle Size and Molecular Targeting on the Intratumoral and Subcellular Distribution of Polymeric Nanoparticles. Mol. Pharm. 2010, 7, 1195–1208. [Google Scholar] [CrossRef]
- Reddi, E.; Castro, G.L.; Biolo, R.; Jori, G. Pharmacokinetic Studies with Zinc(II)-Phthalocyanine in Tumour-Bearing Mice. Br. J. Cancer 1987, 56, 597. [Google Scholar] [CrossRef] [PubMed]
- Ginevra, F.; Biffanti, S.; Pagnan, A.; Biolo, R.; Reddi, E.; Jori, G. Delivery of the Tumour Photosensitizer Zinc(II)-Phthalocyanine to Serum Proteins by Different Liposomes: Studies in Vitro and in Vivo. Cancer Lett. 1990, 49, 59–65. [Google Scholar] [CrossRef]
- Isele, U.; Schieweck, K.; Kessler, R.; Hoogevest, P.; van Capraro, H.-G. Pharmacokinetics and Body Distribution of Liposomal Zinc Phthalocyanine in Tumor-Bearing Mice: Influence of Aggregation State, Particle Size, and Composition. J. Pharm. Sci. 1995, 84, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Taha, M.S.; Padmakumar, S.; Singh, A.; Amiji, M.M. Critical Quality Attributes in the Development of Therapeutic Nanomedicines toward Clinical Translation. Drug Deliv. Transl. Res. 2020, 10, 766–790. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Lillard, J.W. Nanoparticle-Based Targeted Drug Delivery. Exp. Mol. Pathol. 2009, 86, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y. Drug Release and Pharmacokinetic Properties of Liposomal DB-67. Master’s Theses, University of Kentucky, Lexington, KY, USA, 2010. Available online: https://uknowledge.uky.edu/gradschool_theses/17 (accessed on 28 February 2021).
- Johnston, M.J.W.; Semple, S.C.; Klimuk, S.K.; Edwards, K.; Eisenhardt, M.L.; Leng, E.C.; Karlsson, G.; Yanko, D.; Cullis, P.R. Therapeutically Optimized Rates of Drug Release Can Be Achieved by Varying the Drug-to-Lipid Ratio in Liposomal Vincristine Formulations. Biochim. Biophys. Acta 2006, 1758, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Johnston, M.J.W.; Edwards, K.; Karlsson, G.; Cullis, P.R. Influence of Drug-to-Lipid Ratio on Drug Release Properties and Liposome Integrity in Liposomal Doxorubicin Formulations. J. Liposome Res. 2008, 18, 145–157. [Google Scholar] [CrossRef] [PubMed]
- Chountoulesi, M.; Naziris, N.; Pippa, N.; Demetzos, C. The Significance of Drug-to-Lipid Ratio to the Development of Optimized Liposomal Formulation. J. Liposome Res. 2017, 6, 1–10. [Google Scholar] [CrossRef]
- Reshetov, V.; Kachatkou, D.; Shmigol, T.; Zorin, V.; D’Hallewin, M.-A.; Guillemin, F.; Bezdetnaya, L. Redistribution of Meta-Tetra(Hydroxyphenyl)Chlorin (m-THPC) from Conventional and PEGylated Liposomes to Biological Substrates. Photochem. Photobiol. Sci. 2011, 10, 911. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Tristram-Nagle, S.; Nagle, J.F. Effect of Cholesterol on Structural and Mechanical Properties of Membranes Depends on Lipid Chain Saturation. Phys. Rev. E Stat. Nonlin. Soft Matter Phys. 2009, 80, 021931. [Google Scholar] [CrossRef]
- Chakraborty, S.; Doktorova, M.; Molugu, T.R.; Heberle, F.A.; Scott, H.L.; Dzikovski, B.; Nagao, M.; Stingaciu, L.-R.; Standaert, R.F.; Barrera, F.N.; et al. How Cholesterol Stiffens Unsaturated Lipid Membranes. Proc. Natl. Acad. Sci. USA 2020, 117, 21896–21905. [Google Scholar] [CrossRef]
- Jain, A.; Jain, S.K. In Vitro Release Kinetics Model Fitting of Liposomes: An Insight. Chem. Phys. Lipids 2016, 201, 28–40. [Google Scholar] [CrossRef]
- Feuser, P.E.; Possato, J.C.; Scussel, R.; Cercena, R.; de Araújo, P.H.H.; Machado-de-Ávila, R.A.; Dal Bó, A.G. In Vitro Phototoxicity of Zinc Phthalocyanine (ZnPc) Loaded in Liposomes against Human Breast Cancer Cells. J. Porphyr. Phthalocyanines 2021, 25, 153–161. [Google Scholar] [CrossRef]
- Grohganz, H.; Ziroli, V.; Massing, U.; Brandl, M. Quantification of Various Phosphatidylcholines in Liposomes by Enzymatic Assay. AAPS PharmSciTech 2003, 4, 500–505. [Google Scholar] [CrossRef][Green Version]




| Sample Name | Components | Molar Ratio | ZnPc Load (µg/mL) | Phosphatidylcholine Concentration from Enzymatic Assay (mg/mL) |
|---|---|---|---|---|
| Method 1: Thin lipid film hydration + extrusion | ||||
| F4M1 | ZnPc/PE-DTPAGd/POPG/POPC | 0.05/0.75/2/8 | 8.03 ± 0.06 | 5.1 ± 0.3 |
| Method 2: microfluidic FRR 3:1, TFR 12 mL min−1 | ||||
| F4M2 | ZnPc/PE-DTPAGd/POPG/POPC | 0.05/0.75/2/8 | 19.86 ± 0.93 | 4.6 ± 0.4 |
| F5M2 | ZnPc/PE-DTPAGd/PEG-PE/POPG/POPC | 0.05/0.75/0.2/2/8 | 11.00 ± 0.12 | 5.8 ± 0.3 |
| Method 3: microfluidic FRR 5:1, TFR 12 mL min−1 | ||||
| F4M3 | ZnPc/PE-DTPAGd/POPG/POPC | 0.05/0.75/2/8 | 22.02 ± 0.99 | 3.2 ± 0.2 |
| Method 4: microfluidic FRR 3:1, TFR 8 mL min−1 | ||||
| F4M4 | ZnPc/PE-DTPAGd/POPG/POPC | 0.05/0.75/2/8 | 12.29 ± 0.26 | 2.8 ± 0.2 |
| Method: TLH + freeze–thawing | ||||
| Acceptor liposomes | egg phosphatidylcholine (PC) | - | - | 9.8 ± 0.2 |
| Sample Name | AF4-MALLS | DLS | ||||||
|---|---|---|---|---|---|---|---|---|
| Peak 1 Dz (nm) | Peak 2 Dz (nm) | Regularization Analysis | Cumulants | |||||
| Peak 1 (nm) | Intensity (%) | Peak 2 (nm) | Intensity (%) | Zav (nm) | PDI | |||
| Method 1: TLH+extrusion | ||||||||
| F4M1 | 67.1 ± 5.1 | 123.2 ± 7.4 | 64.5 | 100.0% | no peak identified | 58.8 ± 0.5 | 0.084 ± 0.020 | |
| Method 2: microfluidic FRR 3:1, TFR 12 mL min−1 | ||||||||
| F4M2 | 25.3 ± 1.8 | 196.9 ± 5.6 | 20.2 | 80.9% | 61.4 | 19.1% | 24.2 ± 0.3 | 0.235 ± 0.002 |
| F5M2 | 24.5 ± 2.4 | 185.9 ± 0.7 | 28.9 | 93.0% | 297.3 | 7.0% | 32.8 ± 0.4 | 0.164 ± 0.016 |
| Method 3: microfluidic FRR 5:1, TFR 12 mL min−1 | ||||||||
| F4M3 | 23.7 ± 0.4 | no peak identified | 20.3 | 91.6% | 104.9 | 8.4% | 22.1 ± 0.4 | 0.175 ± 0.018 |
| Method 4: microfluidic FRR 3:1, TFR 8 mL min−1 | ||||||||
| F4M4 | 31.0 ± 3.1 | no peak identified | 29.2 | 92.2% | 153.7 | 7.8% | 28.1 ± 0.3 | 0.163 ± 0.016 |
| Method: TLH + freeze–thawing | ||||||||
| Acceptor liposomes | 276.2 ± 0.8 | no peak identified | 49.4 | 0.6% | 319.2 | 99.4% | 302.9 ± 16.7 | 0.111 ± 0.023 |
| AF4-MALLS Method | Method 1: Donor Liposomes Size Measurement | Method 2: Acceptor Liposomes Size Measurement | Method 3: Separation of Donor and Acceptor Liposomes | Method 4: Separation of Donor and Acceptor Liposomes | ||||
|---|---|---|---|---|---|---|---|---|
| Focus flow (VF) | 1 mL/min | 1 mL/min | 1 mL/min | 1 mL/min | ||||
| Injection volume | 10–20 µL | 5 µL | 200 µL | 200 µL | ||||
| Crossflow parameters | Crossflow gradient (mL/min) | Duration | Crossflow gradient (mL/min) | Duration | Crossflow gradient (mL/min) | Duration | Crossflow gradient (mL/min) | Duration |
| Laser power | 100% | 100% | 20% | 20% | ||||
| Mode: Elution + Injection | 1 | for 2 min | 1 | for 2 min | 1 | for 1 min | 2 | for 1 min |
| 1–0.3 | over 1 min | 1–0.3 | over 1 min | 1–0.2 | over 3 min | 2–0.5 | over 1 min | |
| 0.3 | for 17 min | 0.3 | for 3 min | 0.2 | for 12 min | 0.5 | for 10 min | |
| 0.3–0.02 | over 2 min | 0.3–0.02 | over 2 min | 0.2–0.02 | over 5 min | 0.5–0.02 | over 4 min | |
| 0.02 | for 5 min | 0.02 | for 8 min | 0.02 | for 5 min | 0.02 | for 5 min | |
| 0.02–0 | over 1 min | 0.02–0 | over 1 min | 0.02–0 | over 1 min | 0.02–0 | over 1 min | |
| 0 | for 5 min | 0 | for 5 min | 0 | for 13 min | 0 | for 9 min | |
| Method duration | 33 min | 22 min | 40 min | 31 min | ||||
| Sample | F4M1 | F4M2 | F5M2 | |
|---|---|---|---|---|
| Parameter | ||||
| Plateau Yeq (%) | 48.7 ± 2.6 | 46.6 ± 3.9 | 53.1 ± 2.0 | |
| Rate constant, k (min−1) | 0.0058 ± 0.0015 | 0.0025 ± 0.0007 | 0.0043 ± 0.0008 | |
| Half-life, t1/2 (min) | 119.5 ± 0.3 | 277.3 ± 0.3 | 161.2 ± 0.2 | |
| R2 | 0.9231 | 0.9366 | 0.9612 | |
| Model | Parameter | Formulation | ||
|---|---|---|---|---|
| F4M1 | F4M2 | F5M2 | ||
| Higuchi; | ||||
| kH | 0.985 | 0.959 | 0.870 | |
| R2 | 0.912 | 0.955 | 0.984 | |
| AIC | 54.323 | 48.645 | 37.902 | |
| T25 (min) | 644.759 | 679.713 | 826.294 | |
| T50 (min) | 2579.036 | 2718.85 | 3305.175 | |
| Korsmeyer-Peppas; | ||||
| kKP | 2.658 | 1.627 | 0.741 | |
| n | 0.363 | 0.428 | 0.522 | |
| R2 | 0.969 | 0.968 | 0.985 | |
| AIC | 45.859 | 47.298 | 39.351 | |
| T25 (min) | 477.134 | 596.683 | 847.264 | |
| T50 (min) | 3213.824 | 3019.090 | 2197.589 | |
| Peppas-Sahlin; | ||||
| k1 | 1.122 | 0.672 | 0.336 | |
| k2 | −0.007 | −0.002 | −0.001 | |
| m | 0.542 | 0.615 | 0.671 | |
| R2 | 0.985 | 0.983 | 0.991 | |
| AIC | 40.813 | 42.920 | 36.382 | |
| T25 (min) | 429.097 | 532.850 | 779.341 | |
| T50 (min) | None Calc | None Calc | None Calc | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skupin-Mrugalska, P.; Elvang, P.A.; Brandl, M. Application of Asymmetrical Flow Field-Flow Fractionation for Characterizing the Size and Drug Release Kinetics of Theranostic Lipid Nanovesicles. Int. J. Mol. Sci. 2021, 22, 10456. https://doi.org/10.3390/ijms221910456
Skupin-Mrugalska P, Elvang PA, Brandl M. Application of Asymmetrical Flow Field-Flow Fractionation for Characterizing the Size and Drug Release Kinetics of Theranostic Lipid Nanovesicles. International Journal of Molecular Sciences. 2021; 22(19):10456. https://doi.org/10.3390/ijms221910456
Chicago/Turabian StyleSkupin-Mrugalska, Paulina, Philipp A. Elvang, and Martin Brandl. 2021. "Application of Asymmetrical Flow Field-Flow Fractionation for Characterizing the Size and Drug Release Kinetics of Theranostic Lipid Nanovesicles" International Journal of Molecular Sciences 22, no. 19: 10456. https://doi.org/10.3390/ijms221910456
APA StyleSkupin-Mrugalska, P., Elvang, P. A., & Brandl, M. (2021). Application of Asymmetrical Flow Field-Flow Fractionation for Characterizing the Size and Drug Release Kinetics of Theranostic Lipid Nanovesicles. International Journal of Molecular Sciences, 22(19), 10456. https://doi.org/10.3390/ijms221910456






