The Ability of the Nitric Oxide Synthases Inhibitor T1023 to Selectively Protect the Non-Malignant Tissues
Abstract
:1. Introduction
2. Results
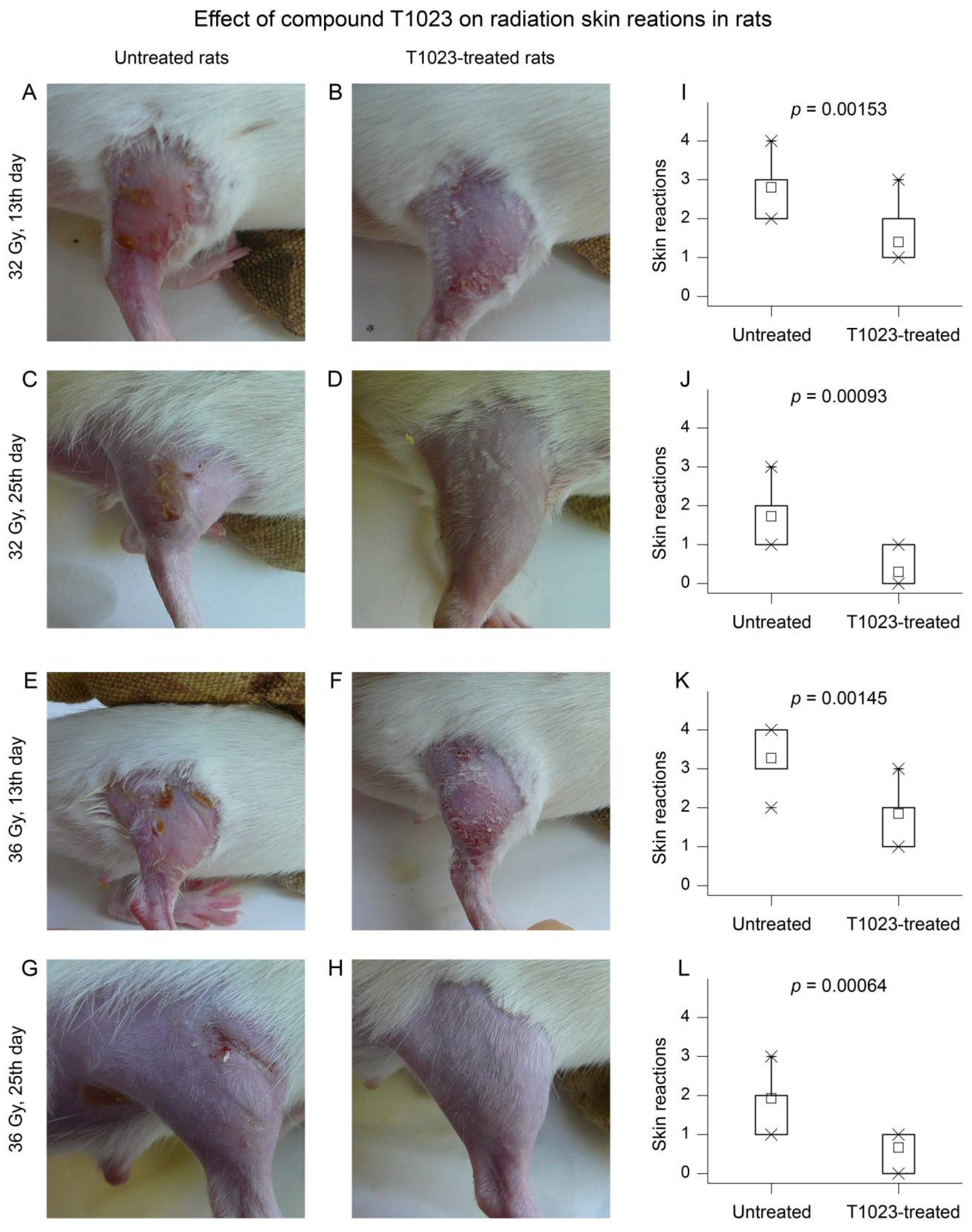
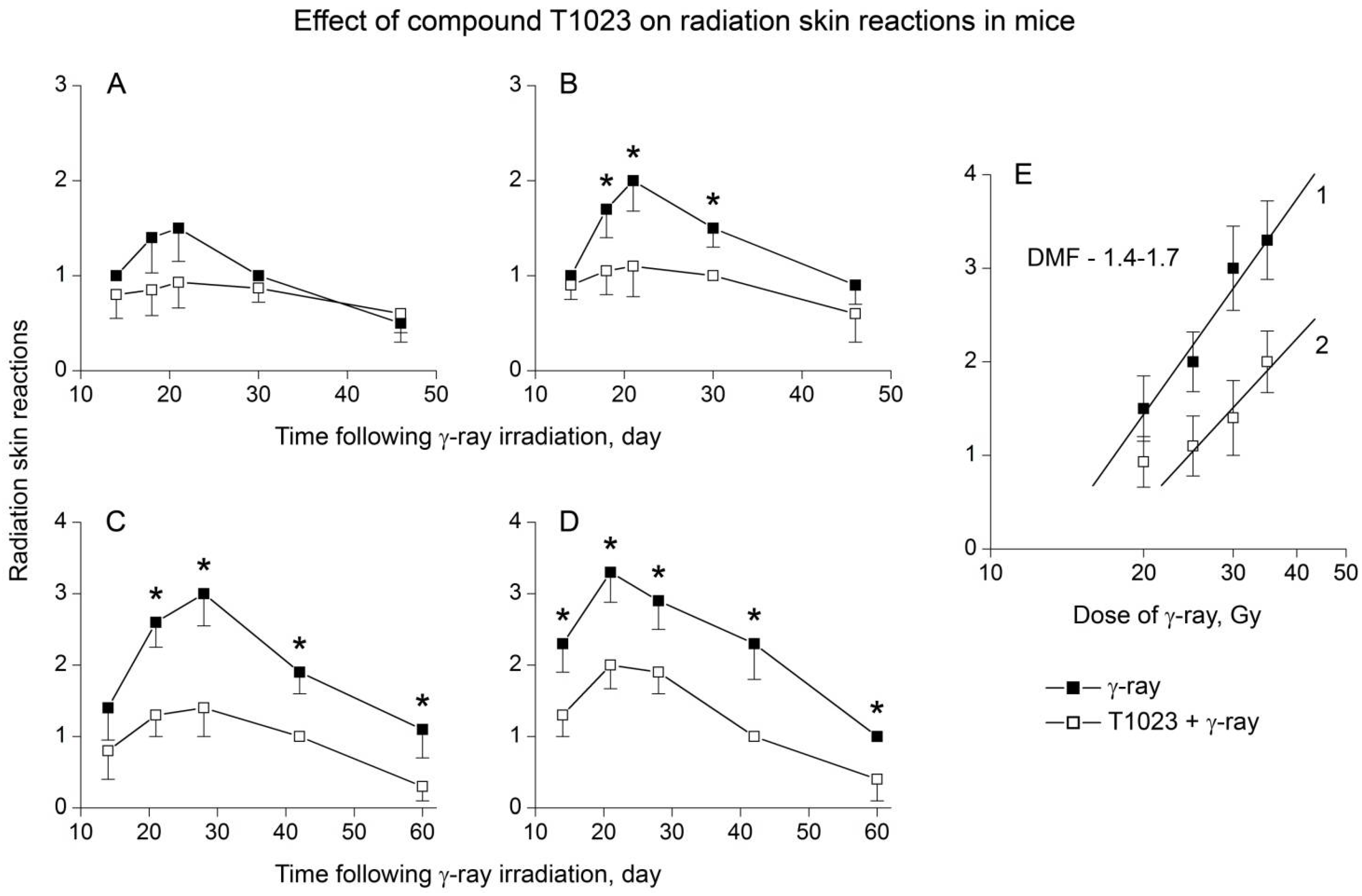
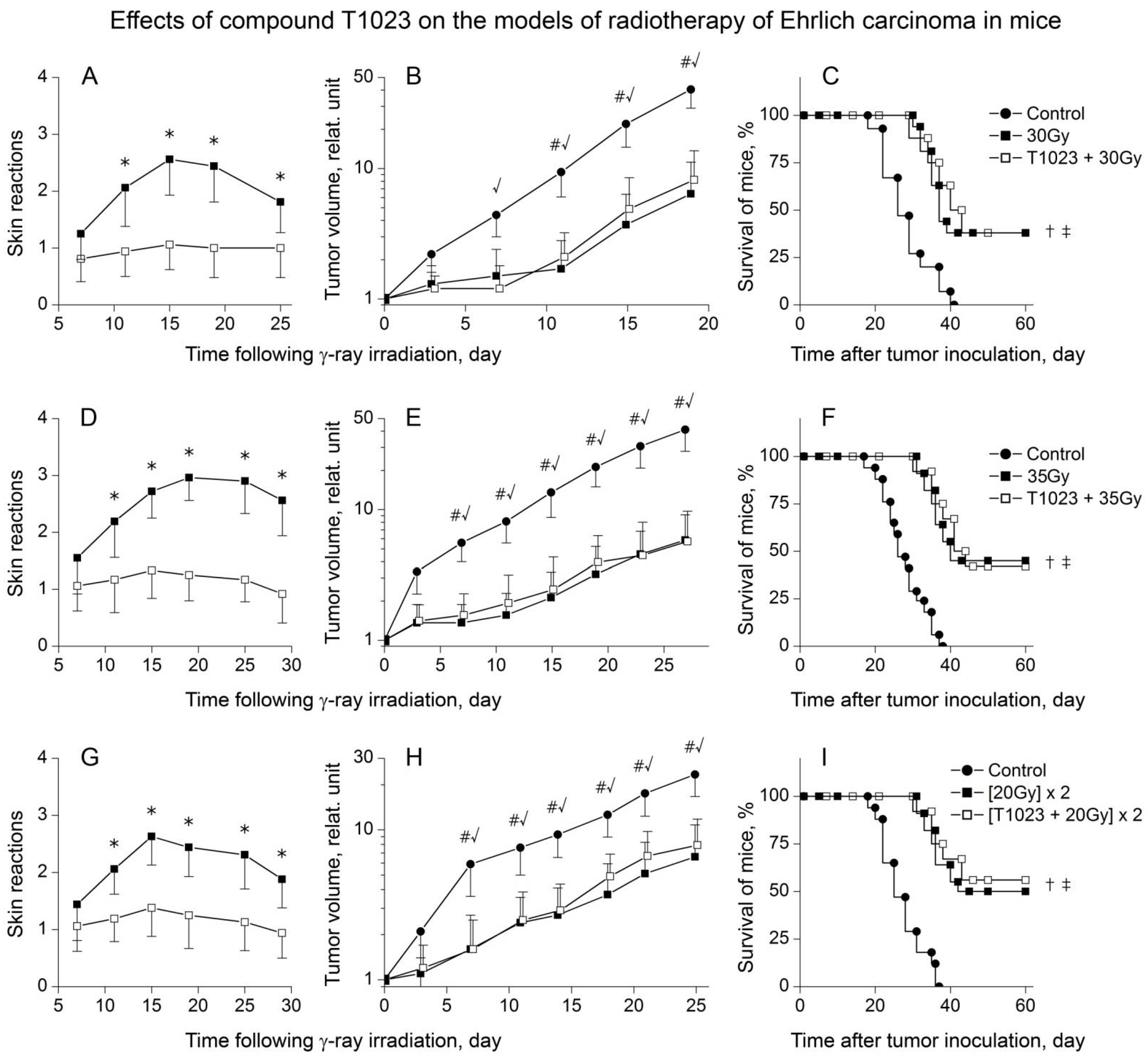
2.1. T1023 Limits the Severity of Acute Radiation Damage to Normal Tissues
2.1.1. Clinical and Morphological Study in Rats
2.1.2. Histological Study in Rats
2.1.3. Clinical and Morphological Study in Mice
2.2. The Radioprotective Effect of T1023 Does Not Develop in the Malignant Tissues of Solid Tumors
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Drugs
4.3. Radiation Exposure
4.4. Tumor Models
4.5. Radiation-Induced Skin Reactions
4.6. Antitumor Effects
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Zaridze, D.G.; Kaprin, A.D.; Stilidi, I.S. Dynamics of morbidity and mortality from malignant tumors in Russia. Vopr. Onkol. 2018, 64, 578–591. (In Russian) [Google Scholar]
- Baskar, R.; Lee, K.A.; Yeo, R.; Yeoh, K.W. Cancer and Radiation therapy: Current advances and future directions. Int. J. Med. Sci. 2012, 9, 193–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lushnikov, E.F.; Abrosimov, A.Y. Modern Radiation Pathology of Human: Problems of Methodology, Etiology, Pathogenesis and Classification; Medical Radiological Research Center of the Ministry of Health of the Russian Federation: Obninsk, Russia, 2012; 235p. (In Russian) [Google Scholar]
- Joye, I.; Haustermans, K. Early and late toxicity of radiotherapy of rectal cancer. Recent Results Cancer Res. 2014, 203, 189–201. [Google Scholar] [PubMed]
- Meattini, I.; Guenzi, M.; Fozza, A.; Vidali, C.; Rovea, P.; Meacci, F.; Livi, L. Overview on cardiac, pulmonary and cutaneous toxicity in patients treated with adjuvant radiotherapy for breast cancer. Breast Cancer 2017, 24, 52–62. [Google Scholar] [CrossRef]
- Stubblefield, M.D. Clinical evaluation and management of radiation fibrosis syndrome. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 89–100. [Google Scholar] [CrossRef]
- Strojan, P.; Hutcheson, K.A.; Eisbruch, A.; Beitler, J.J.; Langendijk, J.A.; Lee, A.W.M.; Corry, J.; Mendenhall, W.M.; Smee, R.; Rinaldo, A.; et al. Treatment of late sequelae after radiotherapy for head and neck cancer. Cancer Treat. Rev. 2017, 59, 79–92. [Google Scholar] [CrossRef] [Green Version]
- Fliedner, T.M.; Dorr, D.H.; Meineke, V. Multi-organ involvement as a pathogenetic principle of the radiation syndromes: A study involving 110 case histories documented in SEARCH and classified as the bases of haematopoietic indicators of effect. BJR 2005, 78 (Suppl. 27), 1–8. [Google Scholar] [CrossRef]
- Satyamitra, M.M.; DiCarlo, A.L.; Taliaferro, L. Understanding the pathophysiology and challenges of development of medical countermeasures for radiation -induced vascular/endothelial cell injuries: Report of a NIAID workshop, August 20, 2015. Radiat. Res. 2016, 186, 99–111. [Google Scholar] [CrossRef]
- Moding, E.J.; Kastan, M.B.; Kirsch, D.G. Strategies for optimizing the response of cancer and normal tissues to radiation. Nat. Rev. Drug Discov. 2013, 12, 526–542. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Jenrow, K.A.; Brown, S.L. Mechanisms of radiation -induced normal tissue toxicity and implications for future clinical trials. Radiat. Oncol. J. 2014, 32, 103–115. [Google Scholar] [CrossRef] [Green Version]
- Montay-Gruel, P.; Meziani, L.; Yakkada, C.; Vozenin, M. Expanding the therapeutic index of radiation therapy by normal tissue protection. Br. J. Radiol. 2019, 92, 20180008. [Google Scholar] [CrossRef]
- Proskuryakov, S.Y.; Kucherenko, N.G.; Trishkina, A.I.; Filimonova, M.V.; Shevchuk, A.S.; Shtein, L.V.; Verkhovsky, Y.G.; Konoplyannikov, A.G.; Mandrugin, A.A.; Fedoseev, V.M.; et al. NO-inhibiting and vasotropic activity of some compounds with thioamidine group. Bull. Exp. Biol. Med. 2002, 134, 338–341. [Google Scholar] [CrossRef]
- Proskurjakov, S.Y.; Filimonova, M.V.; Borovaya, O.N.; Kucherenko, N.G.; Trishkina, A.I.; Shteyn, L.V.; Skvortsov, V.G.; Ulyanova, L.P.; Shevchenko, L.I.; Verkhovsky, Y.G. Effect of NO inhibitors on hypovolemic shock-induced hypotension. Bull. Exp. Biol. Med. 2010, 150, 18–22. [Google Scholar] [CrossRef]
- Filimonova, M.V.; Proskuryakov, S.Y.; Shevchenko, L.I.; Shevchuk, A.S.; Lushnikova, G.A.; Makarchuk, V.M.; Arzamastsev, E.V.; Laba, V.I.; Malinovskaya, K.I.; Levitskaya, E.L. Radioprotective properties of isothiourea derivatives with NO-inhibitory mechanism of action. Radiat. Biol. Radioecol. 2012, 52, 593–601. (In Russian) [Google Scholar]
- Filimonova, M.V.; Shevchenko, L.I.; Trofimova, T.P.; Makarchuk, V.M.; Shevchuk, A.S.; Lushnikova, G.A. On the mechanism of radioprotective effect of NO-synthase inhibitors. Radiat. Biol. Radioecol. 2014, 54, 500–506. (In Russian) [Google Scholar]
- Makarchuk, V.M.; Filimonova, M.V.; Filimonov, A.S.; Shevchenko, L.I.; Izmestieva, O.S.; Saburova, A.S. Lactatemia as a possible pharmacological marker of NOS-inhibitor T1023 induced radioresistance. Radiat. Risk 2020, 29, 45–56. (In Russian) [Google Scholar] [CrossRef]
- Filimonova, M.V.; Makarchuk, V.M.; Shevchenko, L.I.; Saburova, A.S.; Surinova, V.I.; Izmestieva, O.S.; Lychagin, A.A.; Saburov, V.O.; Shegay, P.V.; Kaprin, A.D.; et al. Radioprotective activity of nitric oxide synthase inhibitor T1023. Toxicological and biochemical properties, cardiovascular and radioprotective effects. Radiat. Res. 2020, 194, 532–543. [Google Scholar] [CrossRef]
- Wells, M.; MacBride, S. Radiation Skin Reactions. In Supportive Care in Radiotherapy; Churchill Livingstone: Edinburgh, UK, 2003; pp. 135–159. [Google Scholar]
- DiCarlo, A.L.; Bandremer, A.C.; Hollingsworth, B.A.; Kasim, S.; Laniyonu, A.; Todd, N.F.; Wang, S.-J.; Wertheimer, E.R.; Rios, C. Cutaneous radiation injuries: Models, assessment and treatments. Radiat. Res. 2020, 194, 315–344. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.K.; Garcia, M.; Seed, T.M. A review of radiation countermeasures focusing on injury-specific medicinals and regulatory approval status: Part II. Countermeasures for limited indications, internalized radionuclides, emesis, late effects, and agents demonstrating efficacy in large animals with or without FDA IND status. Int. J. Radiat. Biol. 2017, 93, 870–884. [Google Scholar]
- Singh, V.K.; Hanlon, B.K.; Santiago, P.T.; Seed, T.M. A review of radiation countermeasures focusing on injury-specific medicinals and regulatory approval status: Part III. Countermeasures under early stages of development along with ‘standard of care’ medicinal and procedures not requiring regulatory approval for use. Int. J. Radiat. Biol. 2017, 93, 885–906. [Google Scholar] [PubMed]
- Grebenyuk, A.N.; Gladkikh, V.D. Modern condition and prospects for the development of medicines towards prevention and early treatment of radiation damage. Biol. Bull. 2019, 46, 1540–1555. [Google Scholar] [CrossRef]
- Kouvaris, J.R.; Kouloulias, V.E.; Vlahos, L.J. Amifostine: The first selective-target and broad-spectrum radioprotector. Oncologist 2007, 12, 738–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, M.; Joseph, S.; Albert, A.; Thomas, T.V.; Nittala, M.R.; Woods, W.C.; Vijayakumar, S.; Packianathan, S. Use of amifostine for cytoprotection during radiation therapy: A review. Oncology 2020, 98, 61–80. [Google Scholar] [CrossRef] [PubMed]
- Khussar, I.P. Protective action of cystamine on thyroid tissue in acute radiation injury. Tsitologiia 1963, 5, 91–93. (In Russian) [Google Scholar]
- Vasin, M.V.; Ushakov, I.B.; Suvorov, N.N. Radioprotective effectiveness of indralin in local gamma irradiation of skin. Radiat. Biol. Radioecol. 1998, 38, 42–54. (In Russian) [Google Scholar]
- Vasin, M.V.; Ushakov, I.B.; Korovkina, E.P.; Kovtun, V.Y. Radioprotective capacity of indralin in reducing radiation injury to salivary glands. Radiat. Biol. Radioecol. 2004, 44, 333–335. (In Russian) [Google Scholar]
- Turgunov, M.B.; Sorokina, I.D.; Turusov, V.S. Effect of 5-methoxytryptamine on cutaneous changes caused by ionizing radiation in mice and rats. Med. Radiol. 1964, 9, 70–74. (In Russian) [Google Scholar]
- Cho, Y.J.; Yi, C.O.; Jeon, B.T.; Jeong, Y.Y.; Kang, G.M.; Lee, J.E.; Roh, G.S.; Lee, J.D. Curcumin attenuates radiation-induced inflammation and fibrosis in rat lungs. Korean J. Physiol. Pharmacol. 2013, 17, 267–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guven, B.; Can, M.; Piskin, O.; Aydin, B.G.; Karakaya, K.; Elmas, O.; Acikgoz, B. Flavonoids protect colon against radiation induced colitis. Regul. Toxicol. Pharmacol. 2019, 104, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.M.; Sonis, S.T.; Lee, C.M.; Adkins, D.; Allen, B.G.; Sun, W.; Agarwala, S.S.; Venigalla, M.L.; Chen, Y.; Zhen, W.; et al. Phase 1b/2a trial of the superoxide dismutase mimetic GC4419 to reduce chemoradiotherapy-induced oral mucositis in patients with oral cavity or oropharyngeal carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2018, 100, 427–435. [Google Scholar] [CrossRef] [Green Version]
- Shrishrimal, S.; Kosmacek, E.A.; Chaterjee, A.; Tyson, M.J.; Oberly-Deegan, R.E. The SOD mimic, MnTE-2-PyP, protects from chronic fibrosis and inflammation in irradiated pelvic tissues. Antioxidants 2017, 6, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dvorak, H.F. Rous-Whipple Award Lecture. How tumors make bad blood vessels and stroma. Am. J. Pathol. 2003, 162, 1747–1757. [Google Scholar] [CrossRef] [Green Version]
- Goel, S.; Duda, D.G.; Xu, L.; Munn, L.L.; Boucher, Y.; Fukumura, D.; Jain, R.K. Normalization of the vasculature for treatment of cancer and other diseases. Physiol. Rev. 2011, 93, 1071–1121. [Google Scholar] [CrossRef] [PubMed]
- Molls, M.; Vaupel, P. Blood Perfusion and Microenvironment of Human Tumors; Springer: Berlin/Heidelberg, Germany, 2000; 240p. [Google Scholar]
- Multhoff, G.; Radons, J.; Vaupel, P. Critical role of aberrant angiogenesis in the development of tumor hypoxia and associated radioresistance. Cancers 2014, 6, 813–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abrams, H.L. Altered drug response of tumour vessels in man. Nature 1964, 201, 167–170. [Google Scholar] [CrossRef]
- Tveit, E.; Weiss, L.; Lundstam, S.; Hultborn, R. Perfusion characteristics and norepinephrine reactivity of human renal carcinoma. Cancer Res. 1987, 47, 4709–4713. [Google Scholar]
- Thews, O.; Kelleher, D.K.; Vaupel, P. Disparate responses of tumour vessels to angiotensin II: Tumour volume-dependent effects on perfusion and oxygenation. Br. J. Cancer 2000, 83, 225–231. [Google Scholar] [CrossRef]
- Saburova, A.S.; Filimonova, M.V.; Yuzhakov, V.V.; Shevchenko, L.I.; Yakovleva, N.D.; Bandurko, L.N.; Koretskaya, A.E.; Fomina, N.K.; Saburov, V.O.; Filimonov, A.S. The influence of nitric oxide synthases inhibitor T1023 on the development of radiation pneumofibrosis in rats. Radiatsionnaya Gig. 2020, 13, 60–67. (In Russian) [Google Scholar] [CrossRef]
- Cox, J.D.; Stetz, J.; Pajak, T.F. Toxicity criteria of the Radiat.ion Therapy Oncology Group (RTOG) and the European Organization of Research and Treatment of Cancer (EORTC). Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1341–1346. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filimonova, M.; Saburova, A.; Makarchuk, V.; Shevchenko, L.; Surinova, V.; Yuzhakov, V.; Yakovleva, N.; Sevankaeva, L.; Saburov, V.; Koryakin, S.; et al. The Ability of the Nitric Oxide Synthases Inhibitor T1023 to Selectively Protect the Non-Malignant Tissues. Int. J. Mol. Sci. 2021, 22, 9340. https://doi.org/10.3390/ijms22179340
Filimonova M, Saburova A, Makarchuk V, Shevchenko L, Surinova V, Yuzhakov V, Yakovleva N, Sevankaeva L, Saburov V, Koryakin S, et al. The Ability of the Nitric Oxide Synthases Inhibitor T1023 to Selectively Protect the Non-Malignant Tissues. International Journal of Molecular Sciences. 2021; 22(17):9340. https://doi.org/10.3390/ijms22179340
Chicago/Turabian StyleFilimonova, Marina, Alina Saburova, Victoria Makarchuk, Ljudmila Shevchenko, Valentina Surinova, Vadim Yuzhakov, Nina Yakovleva, Larisa Sevankaeva, Vyacheslav Saburov, Sergey Koryakin, and et al. 2021. "The Ability of the Nitric Oxide Synthases Inhibitor T1023 to Selectively Protect the Non-Malignant Tissues" International Journal of Molecular Sciences 22, no. 17: 9340. https://doi.org/10.3390/ijms22179340
APA StyleFilimonova, M., Saburova, A., Makarchuk, V., Shevchenko, L., Surinova, V., Yuzhakov, V., Yakovleva, N., Sevankaeva, L., Saburov, V., Koryakin, S., Shegay, P., Kaprin, A., Ivanov, S., & Filimonov, A. (2021). The Ability of the Nitric Oxide Synthases Inhibitor T1023 to Selectively Protect the Non-Malignant Tissues. International Journal of Molecular Sciences, 22(17), 9340. https://doi.org/10.3390/ijms22179340




