Noscapine Acts as a Protease Inhibitor of In Vitro Elastase-Induced Collagen Deposition in Equine Endometrium
Abstract
1. Introduction
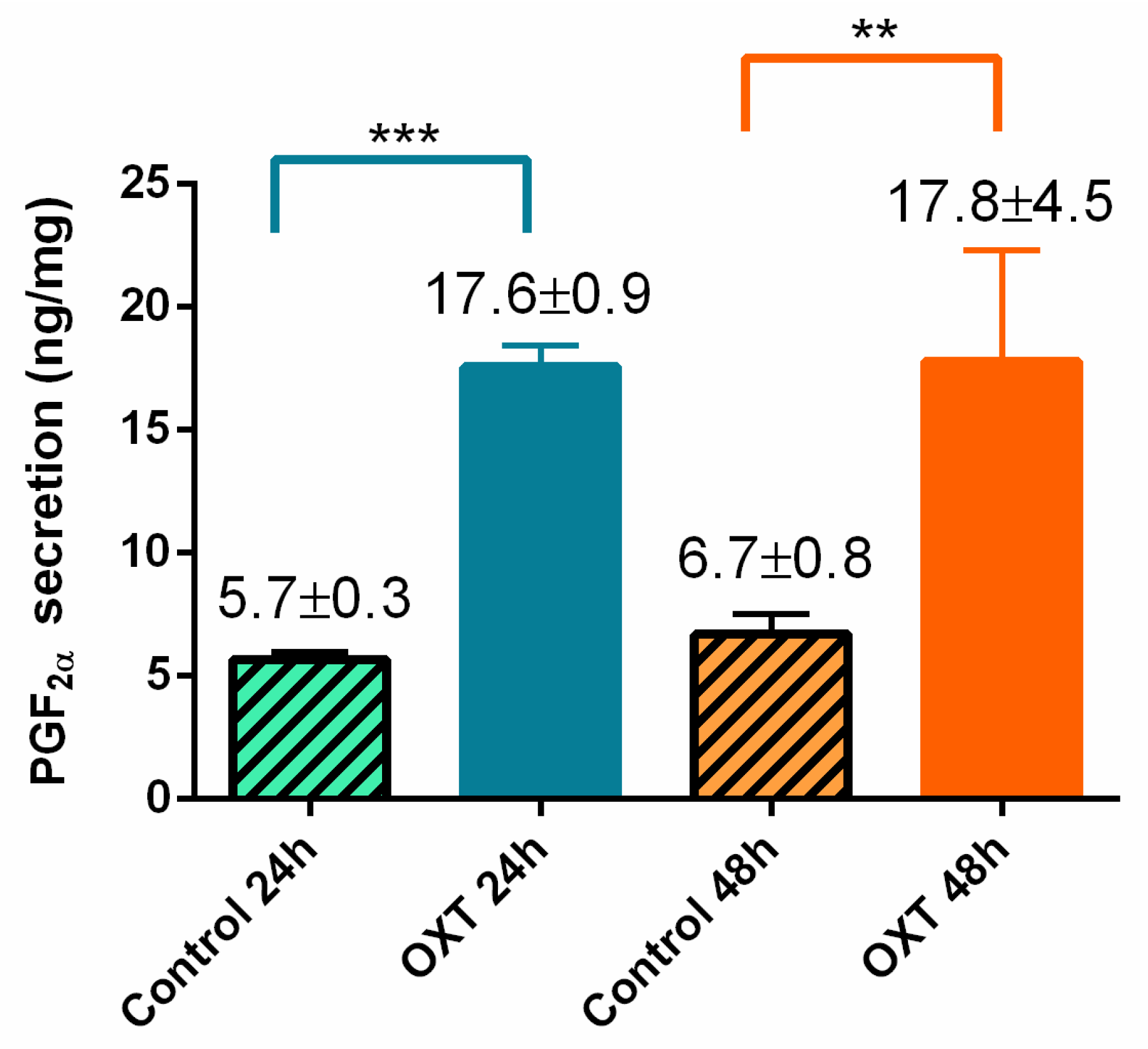
2. Results
2.1. Viability Data of Cultured Equine Endometrial Explants
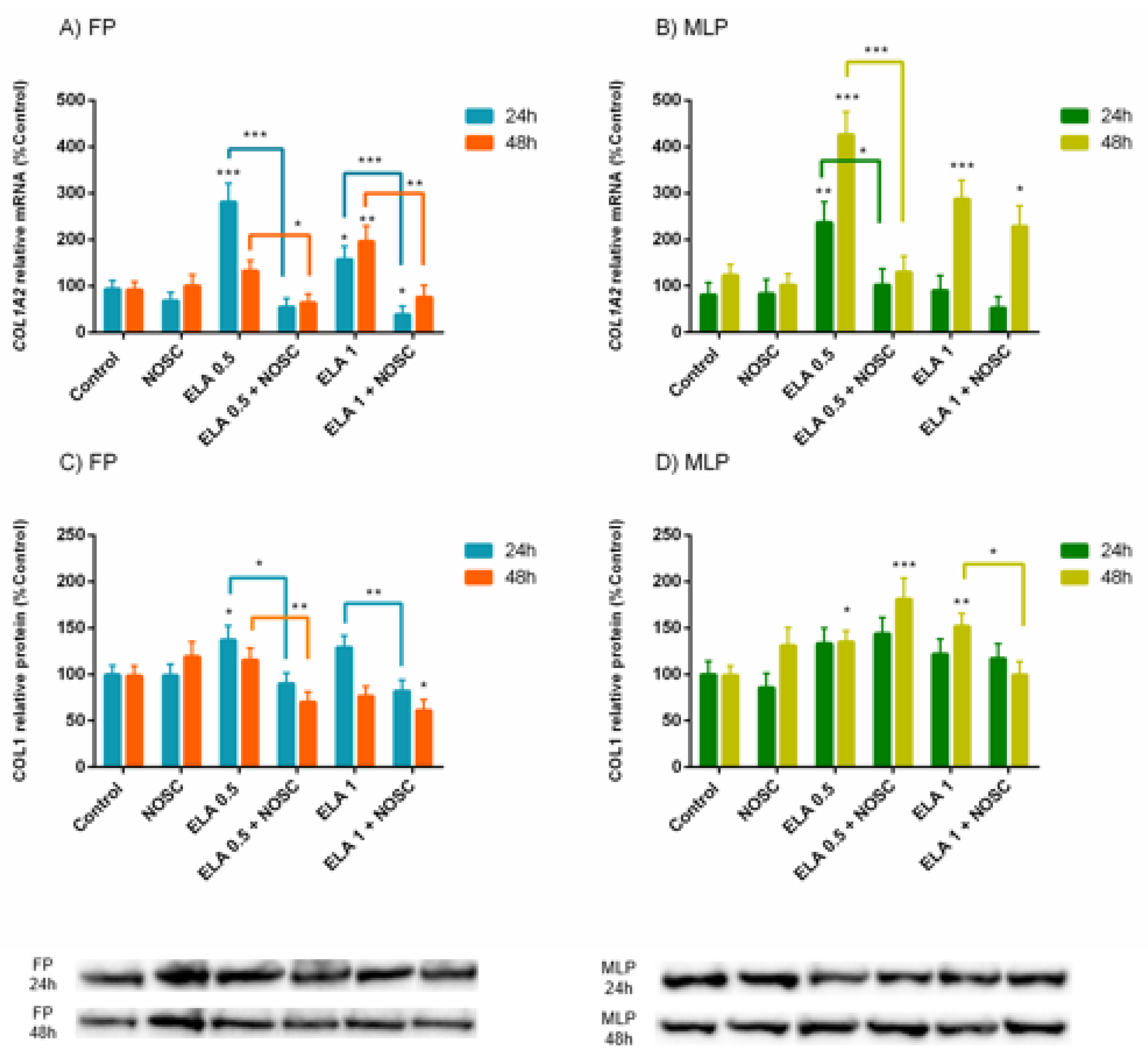
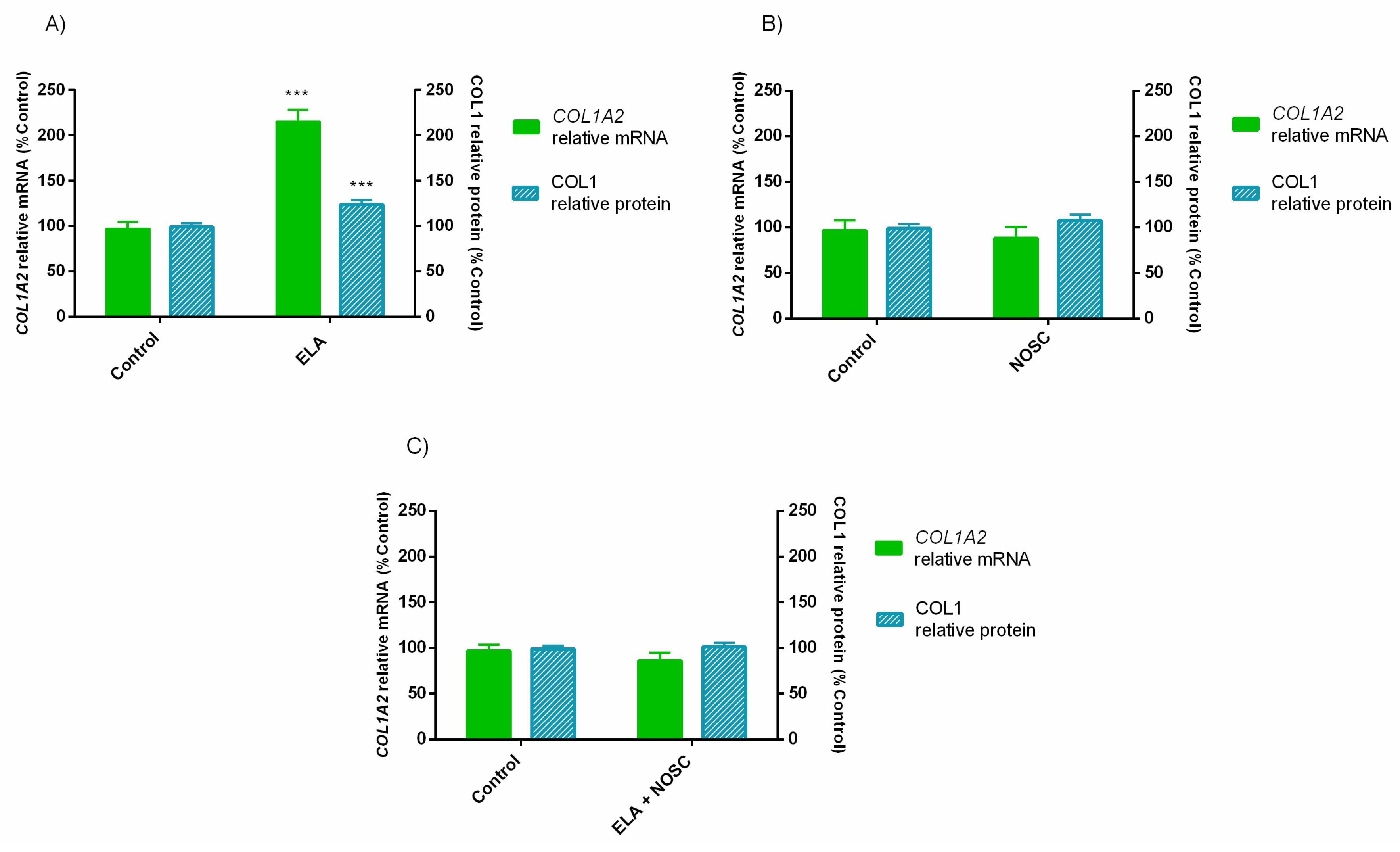
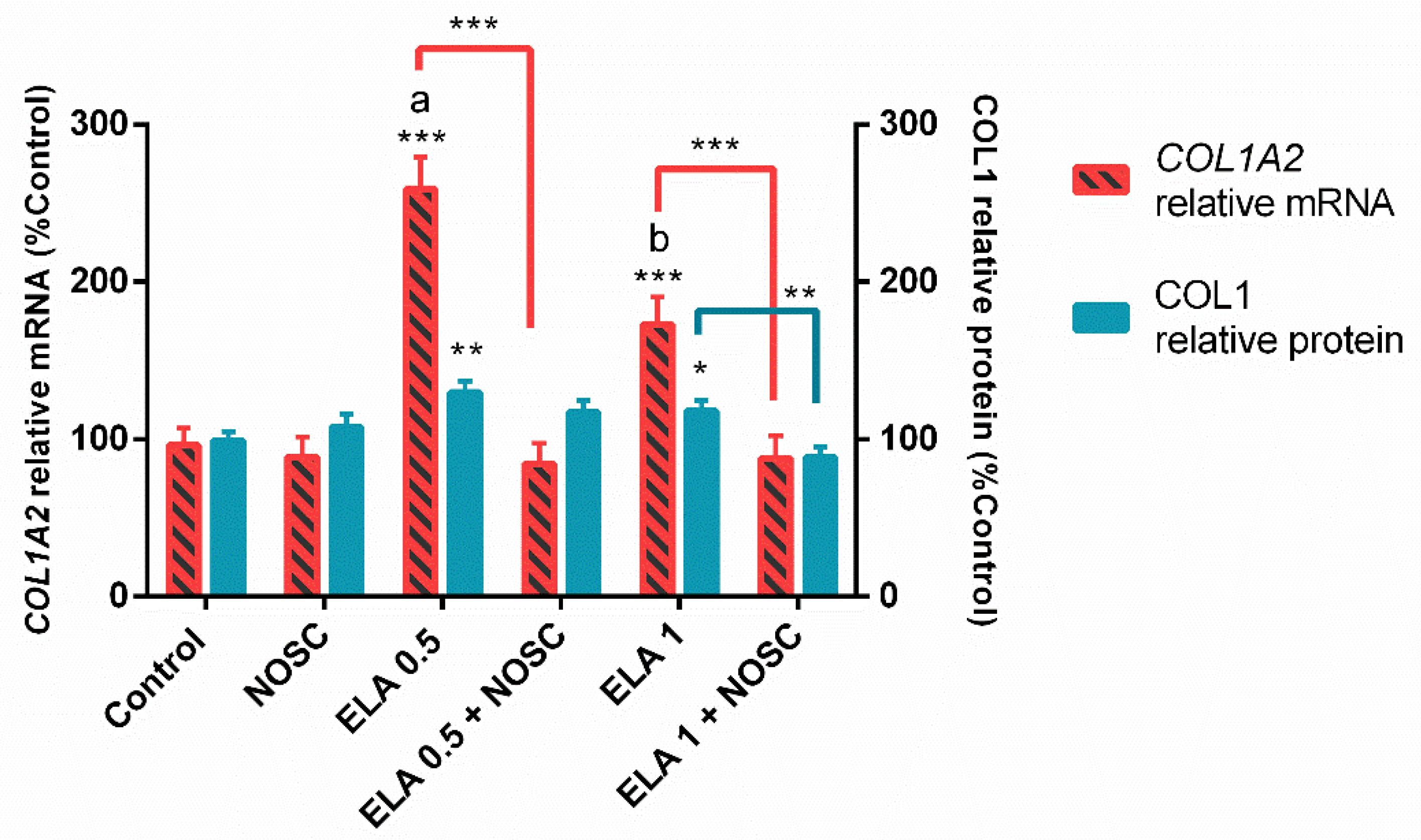
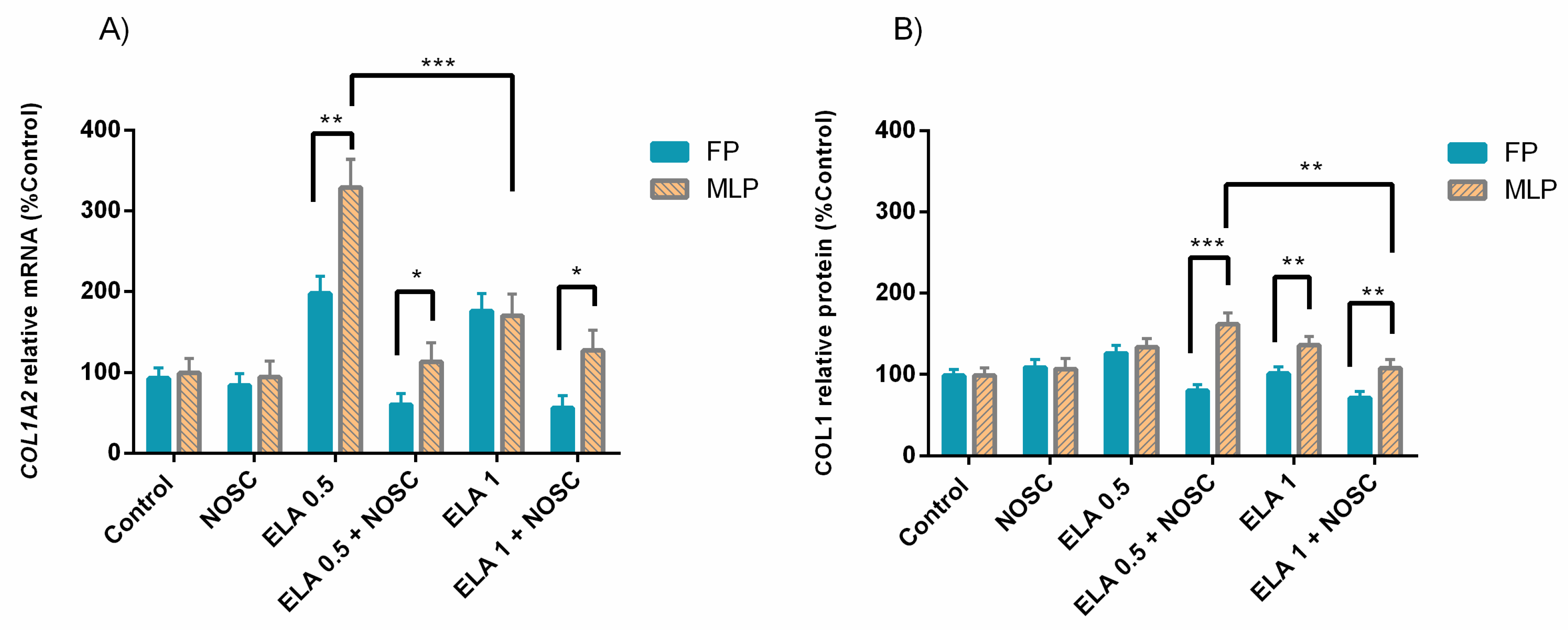
2.2. Noscapine Reduced the ELA-Induced COL1 Expression in Both Estrous Cycle Phases and Treatment Times
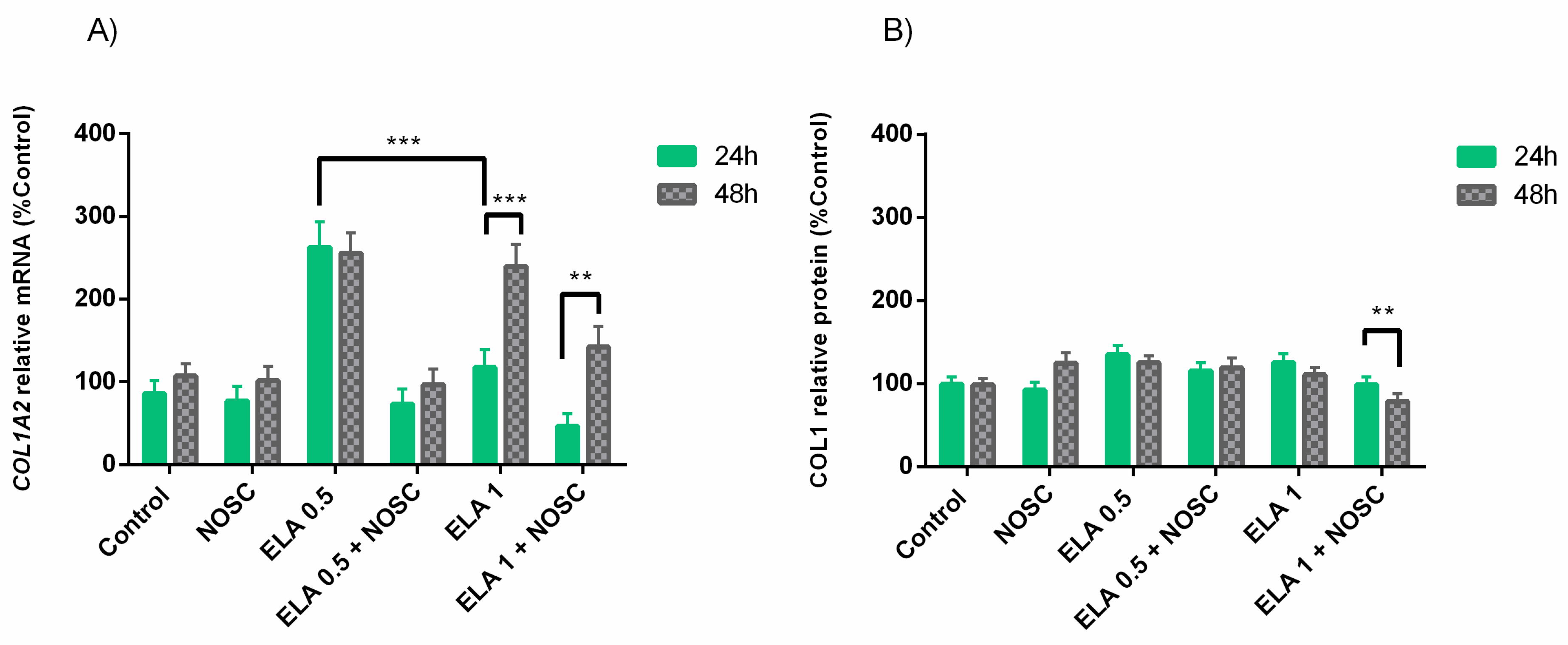
2.3. The Overall Effect of ELA and NOSC Treatments on COL1 in Equine Endometrial Explants
2.4. Noscapine Inhibition of the Profibrotic Effects of ELA Regardless of Estrous Cycle Phase and Treatment Time
2.5. The Effect of ELA and NOSC Treatments on Mare Endometrial Explants Is Dependent on Estrous Cycle Phase
2.6. The Effect of ELA and NOSC Treatments on Mare Endometrial Explants Is Dependent on Treatment Time
3. Discussion
4. Materials and Methods
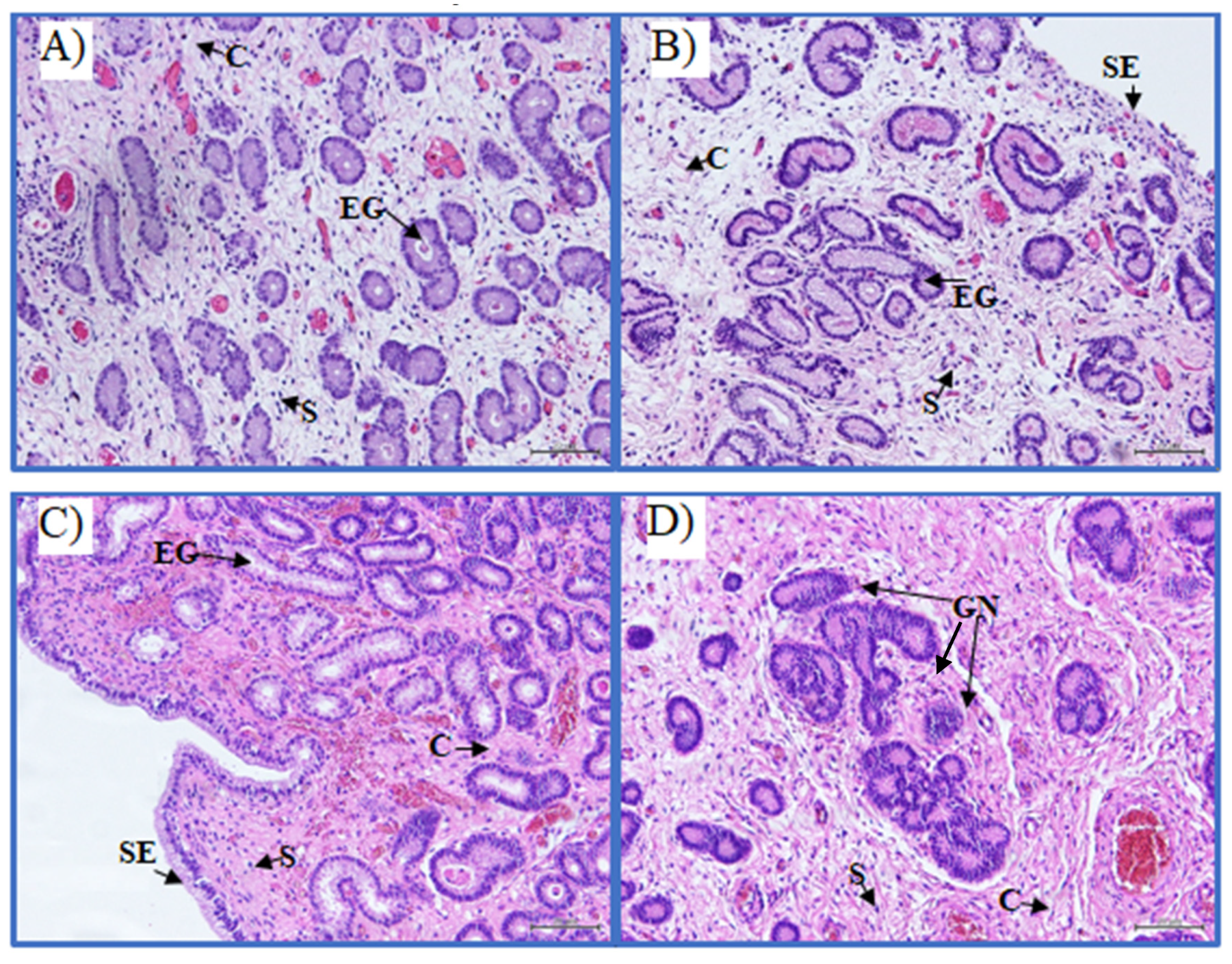
4.1. Mare Sample Collection
4.2. Equine Endometrial Explants In Vitro Culture
4.3. Determination of Mare Endometrial Explants Viability
4.4. Molecular Biology: Extraction of Total RNA, cDNA Synthesis and Quantitative Real-Time Polymerase Chain Reaction (qPCR) for COL1A2 mRNA Determination
4.5. Western Blot: COL1 Protein Relative Abundance Determination
4.6. Statistical Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kenney, R.M.; Doig, P.A. Equine endometrial biopsy. In Current Therapy in Theriogenology 2: Diagnosis, Treatment, and Prevention of Reproductive Diseases in Small and Large Animals, 2nd ed.; Morrow, D.A., Ed.; W.B. Saunders: Philadelphia, PA, USA, 1986; pp. 723–729. [Google Scholar]
- Hoffmann, C.; Ellenberger, C.; Mattos, R.C.; Aupperle, H.; Dhein, S.; Stief, B.; Schoon, H.-A. The Equine Endometrosis: New Insights into the Pathogenesis. Anim. Reprod. Sci. 2009, 111, 261–278. [Google Scholar] [CrossRef]
- Kenney, R.M. The aetiology, diagnosis, and classification of chronic degenerative endometritis. In Workshop on Equine Endometritis; Hughes, J.P., Ed.; Newmarket Press: New York, NY, USA, 1992; Volume 125, p. 186. [Google Scholar]
- Katkiewicz, M.; Witkowski, M.; Zajac, S. Endometrial biopsy of mares: Visualization of healthy and diseased structure. Med. Weter. 2007, 63, 463–466. [Google Scholar]
- Szóstek-Mioduchowska, A.Z.; Lukasik, K.; Skarzynski, D.J.; Okuda, K. Effect of Transforming Growth Factor -Β1 on α-Smooth Muscle Actin and Collagen Expression in Equine Endometrial Fibroblasts. Theriogenology 2019, 124, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Szóstek-Mioduchowska, A.Z.; Baclawska, A.; Okuda, K.; Skarzynski, D.J. Effect of Proinflammatory Cytokines on Endometrial Collagen and Metallopeptidase Expression during the Course of Equine Endometrosis. Cytokine 2019, 123, 154767. [Google Scholar] [CrossRef] [PubMed]
- Szóstek-Mioduchowska, A.; Słowińska, M.; Pacewicz, J.; Skarzynski, D.J.; Okuda, K. Matrix Metallopeptidase Expression and Modulation by Transforming Growth Factor-Β1 in Equine Endometrosis. Sci. Rep. 2020, 10, 1119. [Google Scholar] [CrossRef] [PubMed]
- Szóstek-Mioduchowska, A.Z.; Baclawska, A.; Rebordão, M.R.; Ferreira-Dias, G.; Skarzynski, D.J. Prostaglandins Effect on Matrix Metallopeptidases and Collagen in Mare Endometrial Fibroblasts. Theriogenology 2020, 153, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Rebordão, M.R.; Amaral, A.; Lukasik, K.; Szóstek-Mioduchowska, A.; Pinto-Bravo, P.; Galvão, A.; Skarzynski, D.J.; Ferreira-Dias, G. Constituents of Neutrophil Extracellular Traps Induce in Vitro Collagen Formation in Mare Endometrium. Theriogenology 2018, 113, 8–18. [Google Scholar] [CrossRef]
- Rebordão, M.R.; Amaral, A.; Lukasik, K.; Szóstek-Mioduchowska, A.; Pinto-Bravo, P.; Galvão, A.; Skarzynski, D.J.; Ferreira-Dias, G. Impairment of the Antifibrotic Prostaglandin E2 Pathway May Influence Neutrophil Extracellular Traps–Induced Fibrosis in the Mare Endometrium. Domest. Anim. Endocrinol. 2019, 67, 1–10. [Google Scholar] [CrossRef]
- Amaral, A.; Fernandes, C.; Lukasik, K.; Szóstek-Mioduchowska, A.; Baclawska, A.; Rebordão, M.R.; Aguiar-Silva, J.; Pinto-Bravo, P.; Skarzynski, D.J.; Ferreira-Dias, G. Elastase Inhibition Affects Collagen Transcription and Prostaglandin Secretion in Mare Endometrium during the Estrous Cycle. Reprod. Dom. Anim. 2018, 53, 66–69. [Google Scholar] [CrossRef]
- Amaral, A.; Fernandes, C.; Rebordão, M.R.; Szóstek-Mioduchowska, A.; Lukasik, K.; Gawronska-Kozak, B.; Telo da Gama, L.; Skarzynski, D.J.; Ferreira-Dias, G. The In Vitro Inhibitory Effect of Sivelestat on Elastase Induced Collagen and Metallopeptidase Expression in Equine Endometrium. Animals 2020, 10, 863. [Google Scholar] [CrossRef]
- Amaral, A.; Fernandes, C.; Morazzo, S.; Rebordão, M.R.; Szóstek-Mioduchowska, A.; Lukasik, K.; Gawronska-Kozak, B.; Telo da Gama, L.; Skarzynski, D.J.; Ferreira-Dias, G. The Inhibition of Cathepsin G on Endometrial Explants With Endometrosis in the Mare. Front. Vet. Sci. 2020, 7, 582211. [Google Scholar] [CrossRef]
- Amaral, A.; Fernandes, C.; Rebordão, M.R.; Szóstek-Mioduchowska, A.; Lukasik, K.; Pinto-Bravo, P.; Telo da Gama, L.; Jan Skarzynski, D.; Ferreira-Dias, G. Myeloperoxidase Inhibition Decreases the Expression of Collagen and Metallopeptidase in Mare Endometria under In Vitro Conditions. Animals 2021, 11, 208. [Google Scholar] [CrossRef] [PubMed]
- Kotilainen, T.; Huhtinen, M.; Katila, T. Sperm-Induced Leukocytosis in the Equine Uterus. Theriogenology 1994, 41, 629–636. [Google Scholar] [CrossRef]
- Katila, T. Onset and Duration of Uterine Inflammatory Response of Mares after Insemination with Fresh Semen. Biol. Reprod. 1995, 52, 515–517. [Google Scholar] [CrossRef]
- Troedsson, M.H.T.; Liu, I.K.M.; Thurmond, M. Function of Uterine and Blood-Derived Polymorphonuclear Neutrophils in Mares Susceptible and Resistant to Chronic Uterine Infection: Phagocytosis and Chemotaxis1. Biol. Reprod. 1993, 49, 507–514. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Troedsson, M.H.T. Breeding-Induced Endometritis in Mares. Vet. Clin. N. Am. Equine Pract. 2006, 22, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Brinkmann, V. Neutrophil Extracellular Traps Kill Bacteria. Science 2004, 303, 1532–1535. [Google Scholar] [CrossRef] [PubMed]
- Jorch, S.K.; Kubes, P. An Emerging Role for Neutrophil Extracellular Traps in Noninfectious Disease. Nat. Med. 2017, 23, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, S.W.; Alonso, S. The Effect of Age and Parity on the Development of Equine Chronic Endometrial Disease. Equine Vet. J. 1991, 23, 189–192. [Google Scholar] [CrossRef]
- Woodward, E.M.; Christoffersen, M.; Campos, J.; Squires, E.L.; Troedsson, M.H.T. Susceptibility to Persistent Breeding-Induced Endometritis in the Mare: Relationship to Endometrial Biopsy Score and Age, and Variations between Seasons. Theriogenology 2012, 78, 495–501. [Google Scholar] [CrossRef]
- Ricketts, S.W. The treatment of equine endometritis in studfarm practice. PHK 1999, 15, 588–593. [Google Scholar] [CrossRef]
- LeBlanc, M.; Causey, R. Clinical and Subclinical Endometritis in the Mare: Both Threats to Fertility. Reprod. Domest. Anim. 2009, 44, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Pycock, J.F. Equine Breeding Management and Artificial Insemination, 2nd ed.; Samper, J.C., Ed.; Saunders Elsevier: St. Louis, MO, USA, 2009. [Google Scholar]
- Scoggin, C.F. Not Just a Number: Effect of Age on Fertility, Pregnancy and Offspring Vigour in Thoroughbred Brood-Mares. Reprod. Fertil. Dev. 2015, 27, 872–879. [Google Scholar] [CrossRef] [PubMed]
- Oddsdóttir, C. Development of Endometrial Fibrosis in the Mare: Factors Involved in Tissue Remodeling and Collagen Deposition. Ph.D Thesis, University of Edinburgh, Edinburgh, UK, 2007. [Google Scholar]
- Korkmaz, B.; Moreau, T.; Gauthier, F. Neutrophil Elastase, Proteinase 3 and Cathepsin G: Physicochemical Properties, Activity and Physiopathological Functions. Biochimie 2008, 90, 227–242. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, A.J.; Jin, Y.; Knudsen, G.M.; Perera, N.C.; Jenne, D.E.; Murphy, J.E.; Craik, C.S.; Hermiston, T.W. Global Substrate Profiling of Proteases in Human Neutrophil Extracellular Traps Reveals Consensus Motif Predominantly Contributed by Elastase. PLoS ONE 2013, 8, e75141. [Google Scholar]
- Gregory, A.D.; Kliment, C.R.; Metz, H.E.; Kim, K.-H.; Kargl, J.; Agostini, B.A.; Crum, L.T.; Oczypok, E.A.; Oury, T.A.; Houghton, A.M. Neutrophil Elastase Promotes Myofibroblast Differentiation in Lung Fibrosis. J. Leukoc. Biol. 2015, 98, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Dittrich, A.S.; Kühbandner, I.; Gehrig, S.; Rickert-Zacharias, V.; Twigg, M.; Wege, S.; Taggart, C.C.; Herth, F.; Schultz, C.; Mall, M.A. Elastase Activity on Sputum Neutrophils Correlates with Severity of Lung Disease in Cystic Fibrosis. Eur. Respir. J. 2018, 51, 1701910. [Google Scholar] [CrossRef]
- Ley, W.B.; Bowen, J.M.; Sponenberg, D.P.; Lessard, P.N. Dimethyl Sulfoxide Intrauterine Therapy in the Mare: Effects upon Endometrial Histological Features and Biopsy Classification. Theriogenology 1989, 32, 263–276. [Google Scholar] [CrossRef]
- Podico, G.; Canisso, I.F.; Roady, P.J.; Austin, S.M.; Carossino, M.; Balasuriya, U.; Ellerbrock, R.E.; Lima, F.S.; Ferreira-Dias, G.; Douglas, R.H. Uterine Responses and Equine Chorionic Gonadotropin Concentrations after Two Intrauterine Infusions with Kerosene Post Early Fetal Loss in Mares. Theriogenology 2020, 147, 202–210. [Google Scholar] [CrossRef]
- Navarrete, F.; Saravia, F.; Cisterna, G.; Rojas, F.; Silva, P.P.; Rodríguez-Alvarez, L.; Rojas, D.; Cabezas, J.; Mançanares, A.C.F.; Castro, F.O. Assessment of the Anti-Inflammatory and Engraftment Potential of Horse Endometrial and Adipose Mesenchymal Stem Cells in an in Vivo Model of Post Breeding Induced Endometritis. Theriogenology 2020, 155, 33–42. [Google Scholar] [CrossRef]
- Cabezas, J.; Rojas, D.; Wong, Y.; Telleria, F.; Manriquez, J.; Mançanares, A.C.F.; Rodriguez-Alvarez, L.; Castro, F.O. In Vitro Preconditioning of Equine Adipose Mesenchymal Stem Cells with Prostaglandin E2, Substance P and Their Combination Changes the Cellular Protein Secretomics and Improves Their Immunomodulatory Competence without Compromising Stemness. Vet. Immunol. Immunopathol. 2020, 228, 110100. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, M.O.; Dahlström, B.; Eckernäs, S.-Å.; Johansson, M.; Tufvesson Alm, A. Pharmacokinetics of Oral Noscapine. Eur. J. Clin. Pharmacol. 1990, 39, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Rida, P.C.G.; LiVecche, D.; Ogden, A.; Zhou, J.; Aneja, R. The Noscapine Chronicle: A Pharmaco-Historic Biography of the Opiate Alkaloid Family and Its Clinical Applications: THE NOSCAPINE CHRONICLE. Med. Res. Rev. 2015, 35, 1072–1096. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudian, M.; Mehrpour, M.; Benaissa, F.; Siadatpour, Z. A Preliminary Report on the Application of Noscapine in the Treatment of Stroke. Eur. J. Clin. Pharmacol. 2003, 59, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Khanmoradi, M.; Ali Mard, S.; Aboutaleb, N.; Nobakht, M.; Mahmoudian, M. The Protective Activity of Noscapine on Renal Ischemia—Reperfusion Injury in Male Wistar Rat. Iran J. Basic Med. Sci. 2014, 17, 244–249. [Google Scholar] [PubMed]
- Zughaier, S.; Karna, P.; Stephens, D.; Aneja, R. Potent Anti-Inflammatory Activity of Novel Microtubule-Modulating Brominated Noscapine Analogs. PLoS ONE 2010, 5, e9165. [Google Scholar] [CrossRef]
- Ye, K.; Ke, Y.; Keshava, N.; Shanks, J.; Kapp, J.A.; Tekmal, R.R.; Petros, J.; Joshi, H.C. Opium Alkaloid Noscapine Is an Antitumor Agent That Arrests Metaphase and Induces Apoptosis in Dividing Cells. Proc. Natl. Acad. Sci. USA 1998, 95, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Winter, C.A.; Flataker, L. Toxicity Studies on Noscapine. Toxicol. Appl. Pharmacol. 1961, 3, 96–106. [Google Scholar] [CrossRef]
- Quisbert-Valenzuela, E.O.; Calaf, G.M. Apoptotic Effect of Noscapine in Breast Cancer Cell Lines. Int. J. Oncol. 2016, 48, 2666–2674. [Google Scholar] [CrossRef]
- Esnaashari, S.S.; Amani, A. A Combinational Approach Towards Treatment of Breast Cancer: An Analysis of Noscapine-Loaded Polymeric Nanoparticles and Doxorubicin. AAPS PharmSciTech 2020, 21, 166. [Google Scholar] [CrossRef]
- Kach, J.; Sandbo, N.; La, J.; Denner, D.; Reed, E.B.; Akimova, O.; Koltsova, S.; Orlov, S.N.; Dulin, N.O. Antifibrotic Effects of Noscapine through Activation of Prostaglandin E2 Receptors and Protein Kinase, A.J. Biol. Chem. 2014, 289, 7505–7513. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Sood, D.; van der Spek, P.J.; Sharma, H.S.; Chandra, R. Molecular Binding Mechanism and Pharmacology Comparative Analysis of Noscapine for Repurposing against SARS-CoV-2 Protease. J. Proteome Res. 2020, 19, 4678–4689. [Google Scholar] [CrossRef] [PubMed]
- Mirea, A.-M.; Toonen, E.J.M.; van den Munckhof, I.; Munsterman, I.D.; Tjwa, E.T.T.L.; Jaeger, M.; Oosting, M.; Schraa, K.; Rutten, J.H.W.; van der Graaf, M.; et al. Increased Proteinase 3 and Neutrophil Elastase Plasma Concentrations Are Associated with Non-Alcoholic Fatty Liver Disease (NAFLD) and Type 2 Diabetes. Mol. Med. 2019, 25, 16. [Google Scholar] [CrossRef] [PubMed]
- Martinod, K.; Witsch, T.; Erpenbeck, L.; Savchenko, A.; Hayashi, H.; Cherpokova, D.; Gallant, M.; Mauler, M.; Cifuni, S.M.; Wagner, D.D. Peptidylarginine Deiminase 4 Promotes Age-Related Organ Fibrosis. J. Exp. Med. 2017, 214, 439–458. [Google Scholar] [CrossRef] [PubMed]
- Salazar-Gonzalez, H.; Zepeda-Hernandez, A.; Melo, Z.; Saavedra-Mayorga, D.E.; Echavarria, R. Neutrophil Extracellular Traps in the Establishment and Progression of Renal Diseases. Medicina 2019, 55, 431. [Google Scholar] [CrossRef] [PubMed]
- Tucker, S.L.; Sarr, D.; Rada, B. Neutrophil Extracellular Traps Are Present in the Airways of ENaC-Overexpressing Mice with Cystic Fibrosis-like Lung Disease. BMC Immunol. 2021, 22, 7. [Google Scholar] [CrossRef]
- Vandenberg, L.N.; Maffini, M.V.; Sonnenschein, C.; Rubin, B.S.; Soto, A.M. Bisphenol-A and the Great Divide: A Review of Controversies in the Field of Endocrine Disruption. Endocr. Rev. 2009, 30, 75–95. [Google Scholar] [CrossRef]
- Schug, T.T.; Janesick, A.; Blumberg, B.; Heindel, J.J. Endocrine Disrupting Chemicals and Disease Susceptibility. J. Steroid. Biochem. Mol. Biol. 2011, 127, 204–215. [Google Scholar] [CrossRef]
- Myers, J.P.; Zoeller, R.T.; vom Saal, F.S. A Clash of Old and New Scientific Concepts in Toxicity, with Important Implications for Public Health. Environ. Health Perspect. 2009, 117, 1652–1655. [Google Scholar] [CrossRef] [PubMed]
- Ganjam, V.K.; McLeod, C.; Klesius, P.H.; Washburn, S.M.; Kwapien, R.; Brown, B.; Fazeli, M.H. Effect of Ovarian Hormones on the Phagocytic Response of Ovariectomized Mares. J. Reprod. Fertil. Suppl. 1982, 32, 169–174. [Google Scholar]
- Evans, M.J.; Hamer, J.M.; Gason, L.M.; Irvine, C.H. Factors Affecting Uterine Clearance of Inoculated Materials in Mares. J. Reprod. Fertil. Suppl. 1987, 35, 327–334. [Google Scholar] [PubMed]
- Vogel, C.; Marcotte, E.M. Insights into the Regulation of Protein Abundance from Proteomic and Transcriptomic Analyses. Nat. Rev. Genet. 2012, 13, 227–232. [Google Scholar] [CrossRef]
- Schwarz, R.I. Collagen I and the Fibroblast: High Protein Expression Requires a New Paradigm of Post-Transcriptional, Feedback Regulation. Biochem. Biophys. Rep. 2015, 3, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Altinoz, M.A.; Topcu, G.; Hacimuftuoglu, A.; Ozpinar, A.; Ozpinar, A.; Hacker, E.; Elmaci, İ. Noscapine, a Non-Addictive Opioid and Microtubule-Inhibitor in Potential Treatment of Glioblastoma. Neurochem. Res. 2019, 44, 1796–1806. [Google Scholar] [CrossRef] [PubMed]
- Aneja, R.; Zhou, J.; Zhou, B.; Chandra, R.; Joshi, H.C. Treatment of Hormone-Refractory Breast Cancer: Apoptosis and Regression of Human Tumors Implanted in Mice. Mol. Cancer Ther. 2006, 5, 2366–2377. [Google Scholar] [CrossRef]
- Newcomb, E.W.; Lukyanov, Y.; Smirnova, I.; Schnee, T.; Zagzag, D. Noscapine Induces Apoptosis in Human Glioma Cells by an Apoptosis-Inducing Factor-Dependent Pathway. Anti-Cancer Drugs 2008, 19, 553–563. [Google Scholar] [CrossRef] [PubMed]
- Landen, J.W.; Hau, V.; Wang, M.; Davis, T.; Ciliax, B.; Wainer, B.H.; Van Meir, E.G.; Glass, J.D.; Joshi, H.C.; Archer, D.R. Noscapine Crosses the Blood-Brain Barrier and Inhibits Glioblastoma Growth. Clin. Cancer Res. 2004, 10, 5187–5201. [Google Scholar] [CrossRef]
- Newcomb, E.; Lukyanov, Y.; Schnee, T.; Ali, M.; Lan, L.; Zagzag, D. Noscapine Inhibits Hypoxia-Mediated HIF-1α Expression Andangiogenesis in Vitro: A Novel Function for an Old Drug. Int. J. Oncol. 2006, 5, 1121–1130. [Google Scholar] [CrossRef]
- Sung, B.; Ahn, K.S.; Aggarwal, B.B. Noscapine, a Benzylisoquinoline Alkaloid, Sensitizes Leukemic Cells to Chemotherapeutic Agents and Cytokines by Modulating the NF-ΚB Signaling Pathway. Cancer Res. 2010, 70, 3259–3268. [Google Scholar] [CrossRef]
- Chougule, M.B.; Patel, A.R.; Jackson, T.; Singh, M. Antitumor Activity of Noscapine in Combination with Doxorubicin in Triple Negative Breast Cancer. PLoS ONE 2011, 6, e17733. [Google Scholar] [CrossRef]
- Acuff, C.; Kalman, D. Noscapine and Noscapine Analogs and Their Use in treating Infectious Diseases by Tubulin Binding Inhibition. U.S. Patent Application 20110274651-A1, 10 November 2011. Available online: http://www.freepatentsonline.com/20110274651.pdf (accessed on 6 May 2021).
- Singh, P.; Kumar, D.; Vishvakarma, V.K.; Yadav, P.; Jayaraj, A.; Kumari, K. Computational Approach to Study the Synthesis of Noscapine and Potential of Stereoisomers against NsP3 Protease of CHIKV. Heliyon 2019, 5, e02795. [Google Scholar] [CrossRef] [PubMed]
- Sandbo, N.; Ngam, C.; Torr, E.; Kregel, S.; Kach, J.; Dulin, N. Control of Myofibroblast Differentiation by Microtubule Dynamics through a Regulated Localization of MDia2. J. Biol. Chem. 2013, 288, 15466–15473. [Google Scholar] [CrossRef]
- Xiong, A.; Liu, Y. Targeting Hypoxia Inducible Factors-1α as a Novel Therapy in Fibrosis. Front. Pharmacol. 2017, 8, 326. [Google Scholar] [CrossRef] [PubMed]
- Benko, S.; Magalhaes, J.G.; Philpott, D.J.; Girardin, S.E. NLRC5 Limits the Activation of Inflammatory Pathways. J. Immunol. 2010, 185, 1681–1691. [Google Scholar] [CrossRef]
- Canisso, I.F.; Segabinazzi, L.G.T.M.; Fedorka, C.E. Persistent Breeding-Induced Endometritis in Mares—A Multifaceted Challenge: From Clinical Aspects to Immunopathogenesis and Pathobiology. Int. J. Mol. Sci. 2020, 21, 1432. [Google Scholar] [CrossRef] [PubMed]
- Woodward, E.M.; Christoffersen, M.; Campos, J.; Betancourt, A.; Horohov, D.; Scoggin, K.E.; Squires, E.L.; Troedsson, M.H.T. Endometrial Inflammatory Markers of the Early Immune Response in Mares Susceptible or Resistant to Persistent Breeding-Induced Endometritis. Reproduction 2013, 145, 289–296. [Google Scholar] [CrossRef]
- Roberto da Costa, R.P.; Ferreira-Dias, G.; Mateus, L.; Korzekwa, A.; Andronowska, A.; Platek, R.; Skarzynski, D.J. Endometrial Nitric Oxide Production and Nitric Oxide Synthases in the Equine Endometrium: Relationship with Microvascular Density during the Estrous Cycle. Domest. Anim. Endocrinol. 2007, 32, 287–302. [Google Scholar] [CrossRef]
- Riddle, W.T.; LeBlanc, M.M.; Stromberg, A.J. Relationships between Uterine Culture, Cytology and Pregnancy Rates in a Thoroughbred Practice. Theriogenology 2007, 68, 395–402. [Google Scholar] [CrossRef]
- Nash, D.; Lane, E.; Herath, S.; Sheldon, I.M. Endometrial Explant Culture for Characterizing Equine Endometritis. Am. J. Reprod. Immunol. 2008, 59, 105–117. [Google Scholar] [CrossRef]
- Szóstek, A.Z.; Lukasik, K.; Galvão, A.M.; Ferreira-Dias, G.M.; Skarzynski, D.J. Impairment of the Interleukin System in Equine Endometrium during the Course of Endometrosis. Biol. Reprod. 2013, 89, 79. [Google Scholar] [CrossRef]
- Yang, Z.-R.; Liu, M.; Peng, X.-L.; Lei, X.-F.; Zhang, J.-X.; Dong, W.-G. Noscapine Induces Mitochondria-Mediated Apoptosis in Human Colon Cancer Cells in Vivo and in Vitro. Biochem. Biophys. Res. Commun. 2012, 421, 627–633. [Google Scholar] [CrossRef]
- Schafer, W.R.; Fischer, L.; Roth, K.; Jullig, A.K.; Stuckenschneider, J.E.; Schwartz, P.; Weimer, M.; Orlowska-Volk, M.; Hanjalic-Beck, A.; Kranz, I.; et al. Critical Evaluation of Human Endometrial Explants as an Ex Vivo Model System: A Molecular Approach. Mol. Hum. Reprod. 2011, 17, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Dheda, K.; Huggett, J.F.; Bustin, S.A.; Johnson, M.A.; Rook, G.; Zumla, A. Validation of Housekeeping Genes for Normalizing RNA Expression in Real-Time PCR. BioTechniques 2004, 37, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Fernald, R.D. Comprehensive Algorithm for Quantitative Real-Time Polymerase Chain Reaction. J. Comput. Biol. 2005, 12, 1047–1064. [Google Scholar] [CrossRef] [PubMed]
- UniProtKB—F6RTI8 (F6RTI8_HORSE). Available online: https://www.uniprot.org/uniprot/F6RTI8 (accessed on 6 May 2021).
- Posch, A.; Kohn, J.; Oh, K.; Hammond, M.; Liu, N. V3 Stain-Free Workflow for a Practical, Convenient, and Reliable Total Protein Loading Control in Western Blotting. JoVE 2013, 82, 50948. [Google Scholar] [CrossRef] [PubMed]
| Incubation Period | Activity of LDH (%) |
|---|---|
| 1 h | 95.1 ± 0.7 a |
| 24 h | 90.7 ± 0.7 b |
| 48 h | 87.6 ± 1.0 c |
| Gene (Accession Number) | Sequence 5′-3′ | Amplicon |
|---|---|---|
| RPL32 (XM_001492042.6) | Forward: AGCCATCTACTCGGCGTCA | 144 |
| Reverse: GTCAATGCCTCTGGGTTTCC | ||
| COL1A2 (XM_001492939.3) | Forward: CAAGGGCATTAGGGGACACA | 196 |
| Reverse: ACCCACACTTCCATCGCTTC |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amaral, A.; Fernandes, C.; Szóstek-Mioduchowska, A.; Rebordão, M.R.; Skarzynski, D.J.; Ferreira-Dias, G. Noscapine Acts as a Protease Inhibitor of In Vitro Elastase-Induced Collagen Deposition in Equine Endometrium. Int. J. Mol. Sci. 2021, 22, 5333. https://doi.org/10.3390/ijms22105333
Amaral A, Fernandes C, Szóstek-Mioduchowska A, Rebordão MR, Skarzynski DJ, Ferreira-Dias G. Noscapine Acts as a Protease Inhibitor of In Vitro Elastase-Induced Collagen Deposition in Equine Endometrium. International Journal of Molecular Sciences. 2021; 22(10):5333. https://doi.org/10.3390/ijms22105333
Chicago/Turabian StyleAmaral, Ana, Carina Fernandes, Anna Szóstek-Mioduchowska, Maria Rosa Rebordão, Dariusz Jan Skarzynski, and Graça Ferreira-Dias. 2021. "Noscapine Acts as a Protease Inhibitor of In Vitro Elastase-Induced Collagen Deposition in Equine Endometrium" International Journal of Molecular Sciences 22, no. 10: 5333. https://doi.org/10.3390/ijms22105333
APA StyleAmaral, A., Fernandes, C., Szóstek-Mioduchowska, A., Rebordão, M. R., Skarzynski, D. J., & Ferreira-Dias, G. (2021). Noscapine Acts as a Protease Inhibitor of In Vitro Elastase-Induced Collagen Deposition in Equine Endometrium. International Journal of Molecular Sciences, 22(10), 5333. https://doi.org/10.3390/ijms22105333









