Donor CYP3A5 Gene Polymorphism Alone Cannot Predict Tacrolimus Intrarenal Concentration in Renal Transplant Recipients
Abstract
1. Introduction
2. Results
2.1. Patient Characteristics and CYP3A5 Polymorphism
2.2. Influence of CYP3A5 Polymorphism on Tacrolimus Pharmacokinetics
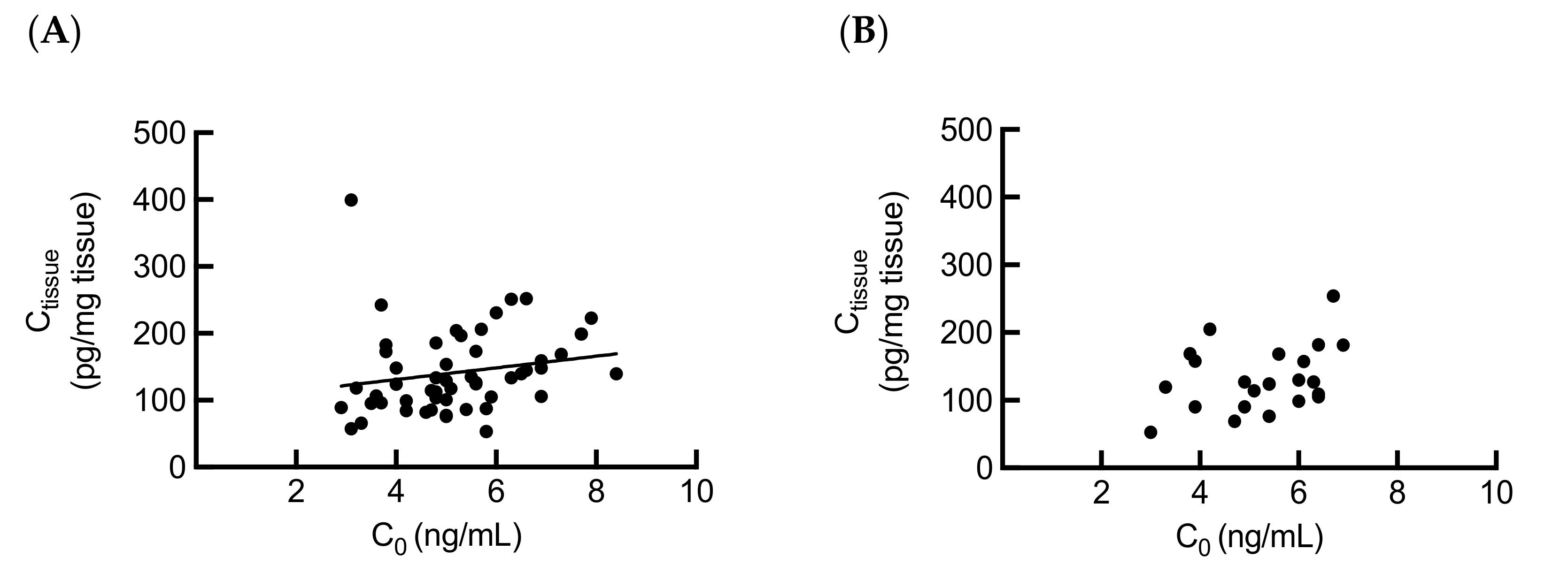
2.3. Association between Intrarenal and Whole Blood Tacrolimus Levels
2.4. Influence of Donor CYP3A5 Gene Polymorphism on Tacrolimus Metabolism in Kidney
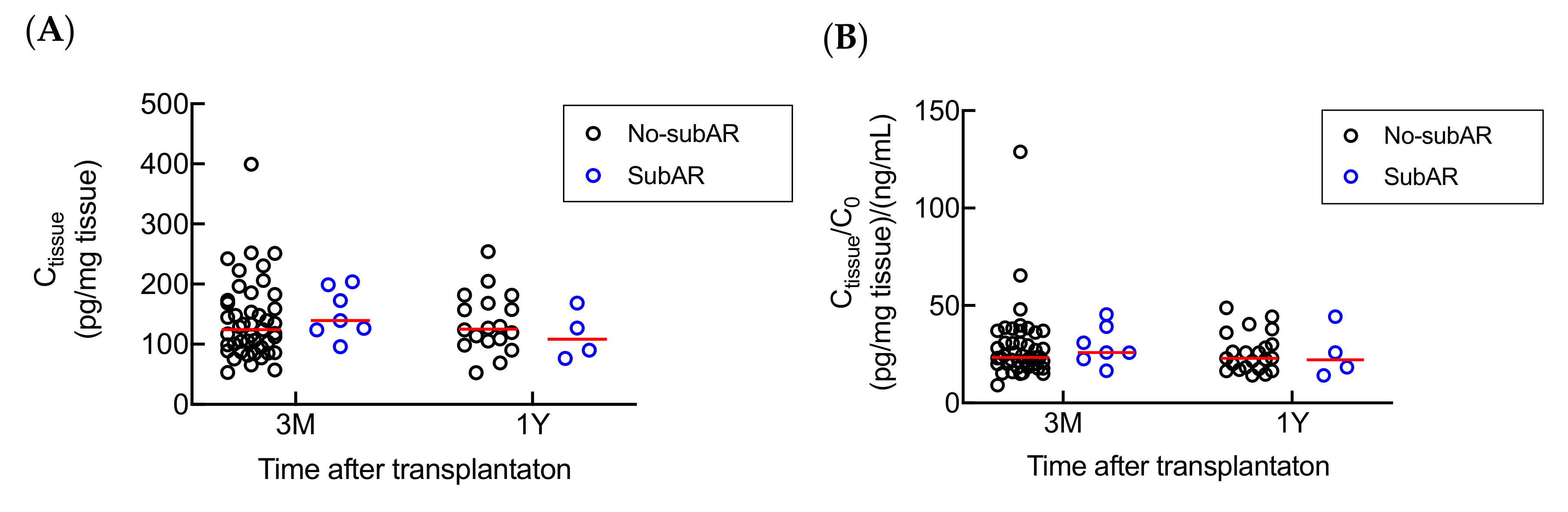
2.5. Associations between Subclinical Acute Rejection (subAR) and Tacrolimus Ctissue or Ctissue/C0.
3. Discussion
4. Materials and Methods
4.1. Subjects
4.2. Diagnostic Criteria for Subclinical Acute Rejection (SubAR)
4.3. Measurement of Tacrolimus Trough Concentration
4.4. Measurement of Tacrolimus Renal Concentration
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| C0 | Tacrolimus trough concentration |
| Ctissue | Tacrolimus intrarenal concentration |
| CNI | Calcineurin inhibitor |
| AR | Acute rejection |
| SubAR | Subclinical acute rejection |
| C0/D | Dose-adjusted C0 |
| CM1 | Intrarenal concentration of 13-O-desmethyl tacrolimus |
References
- De Jonge, H.; Naesens, M.; Kuypers, D.R. New insights into the pharmacokinetics and pharmacodynamics of the calcineurin inhibitors and mycophenolic acid: Possible consequences for therapeutic drug monitoring in solid organ transplantation. Ther. Drug Monit. 2009, 31, 416–435. [Google Scholar] [CrossRef]
- Schiff, J.; Cole, E.; Cantarovich, M. Therapeutic monitoring of calcineurin inhibitors for the nephrologist. Clin. J. Am. Soc. Nephrol. 2007, 2, 374–384. [Google Scholar] [CrossRef]
- Bouamar, R.; Shuker, N.; Hesselink, D.A.; Weimar, W.; Ekberg, H.; Kaplan, B.; Bernasconi, C.; Van Gelder, T. Tacrolimus predose concentrations do not predict the risk of acute rejection after renal transplantation: A pooled analysis from three randomized-controlled clinical trials(†). Am. J. Transplant. 2013, 13, 1253–1261. [Google Scholar] [CrossRef]
- Iwasaki, K.; Shiraga, T.; Nagase, K.; Tozuka, Z.; Noda, K.; Sakuma, S.; Fujitsu, T.; Shimatani, K.; Sato, A.; Fujioka, M. Isolation, identification, and biological activities of oxidative metabolites of FK506, a potent immunosuppressive macrolide lactone. Drug Metab. Dispos. 1993, 21, 971–977. [Google Scholar]
- Kuypers, D.R.; De Jonge, H.; Naesens, M.; Lerut, E.; Verbeke, K.; Vanrenterghem, Y. CYP3A5 and CYP3A4 but not MDR1 single-nucleotide polymorphisms determine long-term tacrolimus disposition and drug-related nephrotoxicity in renal recipients. Clin. Pharm. 2007, 82, 711–725. [Google Scholar] [CrossRef]
- Zegarska, J.; Hryniewiecka, E.; Zochowska, D.; Samborowska, E.; Jazwiec, R.; Borowiec, A.; Tszyrsznic, W.; Chmura, A.; Nazarewski, S.; Dadlez, M.; et al. Tacrolimus Metabolite M-III May Have Nephrotoxic and Myelotoxic Effects and Increase the Incidence of Infections in Kidney Transplant Recipients. Transplant. Proc. 2016, 48, 1539–1542. [Google Scholar] [CrossRef]
- Zegarska, J.; Hryniewiecka, E.; Zochowska, D.; Samborowska, E.; Jazwiec, R.; Maciej, K.; Nazarewski, S.; Dadlez, M.; Paczek, L. Evaluation of the Relationship Between Concentrations of Tacrolimus Metabolites, 13-O-Demethyl Tacrolimus and 15-O-Demethyl Tacrolimus, and Clinical and Biochemical Parameters in Kidney Transplant Recipients. Transplant. Proc. 2018, 50, 2235–2239. [Google Scholar] [CrossRef]
- Hesselink, D.A.; Van Schaik, R.H.; Van der Heiden, I.P.; Van der Werf, M.; Gregoor, P.J.; Lindemans, J.; Weimar, W.; Van Gelder, T. Genetic polymorphisms of the CYP3A4, CYP3A5, and MDR-1 genes and pharmacokinetics of the calcineurin inhibitors cyclosporine and tacrolimus. Clin. Pharm. 2003, 74, 245–254. [Google Scholar] [CrossRef]
- Chen, L.; Prasad, G.V.R. CYP3A5 polymorphisms in renal transplant recipients: Influence on tacrolimus treatment. Pharmgenomics Pers. Med. 2018, 11, 23–33. [Google Scholar] [CrossRef]
- Glowacki, F.; Lionet, A.; Buob, D.; Labalette, M.; Allorge, D.; Provôt, F.; Hazzan, M.; Noël, C.; Broly, F.; Cauffiez, C. CYP3A5 and ABCB1 polymorphisms in donor and recipient: Impact on Tacrolimus dose requirements and clinical outcome after renal transplantation. Nephrol. Dial. Transplant. 2011, 26, 3046–3050. [Google Scholar] [CrossRef]
- Wang, L.; Liu, L.H.; Tong, W.H.; Wang, M.X.; Lu, S.C. Effect of CYP3A5 gene polymorphisms on tacrolimus concentration/dosage ratio in adult liver transplant patients. Genet. Mol. Res. 2015, 14, 15148–15157. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Z.H.; Zheng, J.M.; Chen, Z.H.; Tang, Z.; Chen, J.S.; Li, L.S. Influence of CYP3A5 and MDR1 polymorphisms on tacrolimus concentration in the early stage after renal transplantation. Clin. Transplant. 2005, 19, 638–643. [Google Scholar] [CrossRef]
- Haehner, B.D.; Gorski, J.C.; Vandenbranden, M.; Wrighton, S.A.; Janardan, S.K.; Watkins, P.B.; Hall, S.D. Bimodal distribution of renal cytochrome P450 3A activity in humans. Mol. Pharm. 1996, 50, 52–59. [Google Scholar]
- Dai, Y.; Hebert, M.F.; Isoherranen, N.; Davis, C.L.; Marsh, C.; Shen, D.D.; Thummel, K.E. Effect of CYP3A5 polymorphism on tacrolimus metabolic clearance in vitro. Drug Metab. Dispos. 2006, 34, 836–847. [Google Scholar] [CrossRef]
- Zheng, S.; Tasnif, Y.; Hebert, M.F.; Davis, C.L.; Shitara, Y.; Calamia, J.C.; Lin, Y.S.; Shen, D.D.; Thummel, K.E. Measurement and compartmental modeling of the effect of CYP3A5 gene variation on systemic and intrarenal tacrolimus disposition. Clin. Pharm. 2012, 92, 737–745. [Google Scholar] [CrossRef]
- Krogstad, V.; Vethe, N.T.; Robertsen, I.; Hasvold, G.; Ose, A.D.; Hermann, M.; Andersen, A.M.; Chan, J.; Skauby, M.; Svensson, M.H.S.; et al. Determination of Tacrolimus Concentration and Protein Expression of P-Glycoprotein in Single Human Renal Core Biopsies. Drug Monit. 2018, 40, 292–300. [Google Scholar] [CrossRef]
- Noll, B.D.; Coller, J.K.; Somogyi, A.A.; Morris, R.G.; Russ, G.R.; Hesselink, D.A.; Van Gelder, T.; Sallustio, B.C. Validation of an LC-MS/MS method to measure tacrolimus in rat kidney and liver tissue and its application to human kidney biopsies. Drug Monit. 2013, 35, 617–623. [Google Scholar] [CrossRef]
- Brunet, M.; Van Gelder, T.; Åsberg, A.; Haufroid, V.; Hesselink, D.A.; Langman, L.; Lemaitre, F.; Marquet, P.; Seger, C.; Shipkova, M.; et al. Therapeutic Drug Monitoring of Tacrolimus-Personalized Therapy: Second Consensus Report. Drug Monit. 2019, 41, 261–307. [Google Scholar] [CrossRef]
- Chen, J.S.; Li, L.S.; Cheng, D.R.; Ji, S.M.; Sun, Q.Q.; Cheng, Z.; Wen, J.Q.; Sha, G.Z.; Liu, Z.H. Effect of CYP3A5 genotype on renal allograft recipients treated with tacrolimus. Transplant. Proc. 2009, 41, 1557–1561. [Google Scholar] [CrossRef]
- Goto, M.; Masuda, S.; Kiuchi, T.; Ogura, Y.; Oike, F.; Okuda, M.; Tanaka, K.; Inui, K. CYP3A5*1-carrying graft liver reduces the concentration/oral dose ratio of tacrolimus in recipients of living-donor liver transplantation. Pharmacogenetics 2004, 14, 471–478. [Google Scholar] [CrossRef]
- Kato, H.; Usui, M.; Muraki, Y.; Tanemura, A.; Murata, Y.; Kuriyama, N.; Azumi, Y.; Kishiwada, M.; Mizuno, S.; Sakurai, H.; et al. Long-Term Influence of CYP3A5 Gene Polymorphism on Pharmacokinetics of Tacrolimus and Patient Outcome After Living Donor Liver Transplantation. Transplant. Proc. 2016, 48, 1087–1094. [Google Scholar] [CrossRef]
- Vanhove, T.; De Jonge, H.; De Loor, H.; Oorts, M.; De Hoon, J.; Pohanka, A.; Annaert, P.; Kuypers, D.R.J. Relationship between In Vivo CYP3A4 Activity, CYP3A5 Genotype, and Systemic Tacrolimus Metabolite/Parent Drug Ratio in Renal Transplant Recipients and Healthy Volunteers. Drug Metab. Dispos. 2018, 46, 1507–1513. [Google Scholar] [CrossRef]
- Fukudo, M.; Yano, I.; Yoshimura, A.; Masuda, S.; Uesugi, M.; Hosohata, K.; Katsura, T.; Ogura, Y.; Oike, F.; Takada, Y.; et al. Impact of MDR1 and CYP3A5 on the oral clearance of tacrolimus and tacrolimus-related renal dysfunction in adult living-donor liver transplant patients. Pharm. Genom. 2008, 18, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Bolbrinker, J.; Seeberg, S.; Schostak, M.; Kempkensteffen, C.; Baelde, H.; De Heer, E.; Kreutz, R. CYP3A5 genotype-phenotype analysis in the human kidney reveals a strong site-specific expression of CYP3A5 in the proximal tubule in carriers of the CYP3A5*1 allele. Drug Metab. Dispos. 2012, 40, 639–641. [Google Scholar] [CrossRef]
- Knops, N.; Levtchenko, E.; Van den Heuvel, B.; Kuypers, D. From gut to kidney: Transporting and metabolizing calcineurin-inhibitors in solid organ transplantation. Int. J. Pharm. 2013, 452, 14–35. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.Y.; Li, Q.X.; Li, J.; Xie, X.F.; Ao, Y.; Ai, Y.X. Hepatotoxicity and gene expression down-regulation of CYP isozymes caused by renal ischemia/reperfusion in the rat. Exp. Toxicol. Pathol. 2009, 61, 169–176. [Google Scholar] [CrossRef]
- Fu, R.; Tajima, S.; Suetsugu, K.; Watanabe, H.; Egashira, N.; Masuda, S. Biomarkers for individualized dosage adjustments in immunosuppressive therapy using calcineurin inhibitors after organ transplantation. Acta Pharm. Sin. 2019, 40, 151–159. [Google Scholar] [CrossRef]
- Kravljaca, M.; Perovic, V.; Pravica, V.; Brkovic, V.; Milinkovic, M.; Lausevic, M.; Naumovic, R. The importance of MDR1 gene polymorphisms for tacrolimus dosage. Eur. J. Pharm. Sci. 2016, 83, 109–113. [Google Scholar] [CrossRef]
- Staatz, C.E.; Goodman, L.K.; Tett, S.E. Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: Part II. Clin. Pharmacokinet. 2010, 49, 207–221. [Google Scholar] [CrossRef]
- Tsuchiya, N.; Satoh, S.; Tada, H.; Li, Z.; Ohyama, C.; Sato, K.; Suzuki, T.; Habuchi, T.; Kato, T. Influence of CYP3A5 and MDR1 (ABCB1) polymorphisms on the pharmacokinetics of tacrolimus in renal transplant recipients. Transplantation 2004, 78, 1182–1187. [Google Scholar] [CrossRef]
- Stefanović, N.Z.; Cvetković, T.P.; Jevtović-Stoimenov, T.M.; Ignjatović, A.M.; Paunović, G.J.; Veličković, R.M. Investigation of CYP 3A5 and ABCB1 gene polymorphisms in the long-term following renal transplantation: Effects on tacrolimus exposure and kidney function. Exp. Med. 2015, 10, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Capron, A.; Mourad, M.; De Meyer, M.; De Pauw, L.; Eddour, D.C.; Latinne, D.; Elens, L.; Haufroid, V.; Wallemacq, P. CYP3A5 and ABCB1 polymorphisms influence tacrolimus concentrations in peripheral blood mononuclear cells after renal transplantation. Pharmacogenomics 2010, 11, 703–714. [Google Scholar] [CrossRef] [PubMed]
- Dessilly, G.; Elens, L.; Panin, N.; Capron, A.; Decottignies, A.; Demoulin, J.B.; Haufroid, V. ABCB1 1199G>A genetic polymorphism (Rs2229109) influences the intracellular accumulation of tacrolimus in HEK293 and K562 recombinant cell lines. PLoS ONE 2014, 9, e91555. [Google Scholar] [CrossRef] [PubMed]
- Bandur, S.; Petrasek, J.; Hribova, P.; Novotna, E.; Brabcova, I.; Viklicky, O. Haplotypic structure of ABCB1/MDR1 gene modifies the risk of the acute allograft rejection in renal transplant recipients. Transplantation 2008, 86, 1206–1213. [Google Scholar] [CrossRef]
- Naesens, M.; Lerut, E.; De Jonge, H.; Van Damme, B.; Vanrenterghem, Y.; Kuypers, D.R. Donor age and renal P-glycoprotein expression associate with chronic histological damage in renal allografts. J. Am. Soc. Nephrol. 2009, 20, 2468–2480. [Google Scholar] [CrossRef]
- Yigitaslan, S.; Erol, K.; Cengelli, C. The Effect of P-Glycoprotein Inhibition and Activation on the Absorption and Serum Levels of Cyclosporine and Tacrolimus in Rats. Adv. Clin. Exp. Med. 2016, 25, 237–242. [Google Scholar] [CrossRef]
- Knops, N.; Van den Heuvel, L.P.; Masereeuw, R.; Bongaers, I.; De Loor, H.; Levtchenko, E.; Kuypers, D. The functional implications of common genetic variation in CYP3A5 and ABCB1 in human proximal tubule cells. Mol. Pharm. 2015, 12, 758–768. [Google Scholar] [CrossRef]
- Elens, L.; Capron, A.; Kerckhove, V.V.; Lerut, J.; Mourad, M.; Lison, D.; Wallemacq, P.; Haufroid, V. 1199G>A and 2677G>T/A polymorphisms of ABCB1 independently affect tacrolimus concentration in hepatic tissue after liver transplantation. Pharm. Genom. 2007, 17, 873–883. [Google Scholar] [CrossRef]
- Iwasaki, K. Metabolism of tacrolimus (FK506) and recent topics in clinical pharmacokinetics. Drug Metab. Pharm. 2007, 22, 328–335. [Google Scholar] [CrossRef]
- Vincent, S.H.; Karanam, B.V.; Painter, S.K.; Chiu, S.H. In vitro metabolism of FK-506 in rat, rabbit, and human liver microsomes: Identification of a major metabolite and of cytochrome P450 3A as the major enzymes responsible for its metabolism. Arch. Biochem. Biophys. 1992, 294, 454–460. [Google Scholar] [CrossRef]
- Chen, Y.L.; Hirabayashi, H.; Akhtar, S.; Pelzer, M.; Kobayashi, M. Simultaneous determination of three isomeric metabolites of tacrolimus (FK506) in human whole blood and plasma using high performance liquid chromatography-tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2006, 830, 330–341. [Google Scholar] [CrossRef]
- Dubbelboer, I.R.; Pohanka, A.; Said, R.; Rosenborg, S.; Beck, O. Quantification of tacrolimus and three demethylated metabolites in human whole blood using LC-ESI-MS/MS. Drug Monit. 2012, 34, 134–142. [Google Scholar] [CrossRef]
- Andrews, L.M.; Li, Y.; De Winter, B.C.M.; Shi, Y.Y.; Baan, C.C.; Van Gelder, T.; Hesselink, D.A. Pharmacokinetic considerations related to therapeutic drug monitoring of tacrolimus in kidney transplant patients. Expert Opin. Drug Metab. Toxicol. 2017, 13, 1225–1236. [Google Scholar] [CrossRef]
- Tajima, S.; Fu, R.; Shigematsu, T.; Noguchi, H.; Kaku, K.; Tsuchimoto, A.; Okabe, Y.; Masuda, S. Urinary Human Epididymis Secretory Protein 4 as a Useful Biomarker for Subclinical Acute Rejection Three Months after Kidney Transplantation. Int. J. Mol. Sci. 2019, 20, 4699. [Google Scholar] [CrossRef]



| Characteristics | n = 52 |
|---|---|
| Recipient age (years) | 43.9 ± 13.3 |
| Recipient sex (male/female) | 31/21 |
| Body weight (kg) | 58.15 ± 14.48 |
| Reasons for renal transplantation (n) | |
| IgA nephropathy | 8 |
| Diabetic gastropathy | 8 |
| Chronic glomerulonephritis | 10 |
| Polycystic kidney | 3 |
| Type 1 diabetes | 2 |
| Type 2 diabetes | 3 |
| Hypertensive nephrosclerosis | 3 |
| Others | 15 |
| Serum creatinine (mg/dL) | |
| Pre-transplant | 7.85 ± 3.38 |
| 3-month | 1.14 ± 0.28 |
| Donor CYP3A5 genotype | |
| *1/*1 or *1/*3 | 25 (48.1%) |
| *3/*3 | 27 (51.9%) |
| Recipient CYP3A5 genotype | |
| *1/*1 or *1/*3 | 23 (44.2%) |
| *3/*3 | 29 (55.8%) |
| PK-Parameter | CYP3A5 Genotype | 3 Months after Renal Transplantation (n = 52) | 1 Year after Renal Transplantation (n = 22) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean ± SD | p | n | Mean ± SD | p | ||
| C0 (ng/mL) | Recipient CYP3A5*1 | 23 | 5.30 ± 1.32 | 0.5368 | 8 | 5.01 ± 1.45 | 0.7002 |
| Recipient CYP3A5*3/*3 | 29 | 5.08 ± 1.35 | 14 | 5.37 ± 1.00 | |||
| C0/D (ng/mL/mg) | Recipient CYP3A5*1 | 23 | 0.95 ± 0.37 | <0.0001 | 8 | 0.97 ± 0.37 | 0.0167 |
| Recipient CYP3A5*3/*3 | 29 | 1.56 ± 0.66 | 14 | 1.58 ± 0.68 | |||
| C0 (ng/mL) | Donor CYP3A5*1 | 25 | 5.03 ± 1.11 | 0.5760 | 10 | 5.32 ± 1.24 | 0.7339 |
| Donor CYP3A5*3/*3 | 27 | 5.31 ± 1.51 | 12 | 5.18 ± 1.14 | |||
| C0/D (ng/mL/mg) | Donor CYP3A5*1 | 25 | 1.31 ± 0.69 | 0.9964 | 10 | 1.43 ± 0.60 | 0.4078 |
| Donor CYP3A5*3/*3 | 27 | 1.27 ± 0.57 | 12 | 1.30 ± 0.71 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Tajima, S.; Shigematsu, T.; Fu, R.; Noguchi, H.; Kaku, K.; Tsuchimoto, A.; Okabe, Y.; Egashira, N.; Masuda, S. Donor CYP3A5 Gene Polymorphism Alone Cannot Predict Tacrolimus Intrarenal Concentration in Renal Transplant Recipients. Int. J. Mol. Sci. 2020, 21, 2976. https://doi.org/10.3390/ijms21082976
Zhang M, Tajima S, Shigematsu T, Fu R, Noguchi H, Kaku K, Tsuchimoto A, Okabe Y, Egashira N, Masuda S. Donor CYP3A5 Gene Polymorphism Alone Cannot Predict Tacrolimus Intrarenal Concentration in Renal Transplant Recipients. International Journal of Molecular Sciences. 2020; 21(8):2976. https://doi.org/10.3390/ijms21082976
Chicago/Turabian StyleZhang, Mengyu, Soichiro Tajima, Tomohiro Shigematsu, Rao Fu, Hiroshi Noguchi, Keizo Kaku, Akihiro Tsuchimoto, Yasuhiro Okabe, Nobuaki Egashira, and Satohiro Masuda. 2020. "Donor CYP3A5 Gene Polymorphism Alone Cannot Predict Tacrolimus Intrarenal Concentration in Renal Transplant Recipients" International Journal of Molecular Sciences 21, no. 8: 2976. https://doi.org/10.3390/ijms21082976
APA StyleZhang, M., Tajima, S., Shigematsu, T., Fu, R., Noguchi, H., Kaku, K., Tsuchimoto, A., Okabe, Y., Egashira, N., & Masuda, S. (2020). Donor CYP3A5 Gene Polymorphism Alone Cannot Predict Tacrolimus Intrarenal Concentration in Renal Transplant Recipients. International Journal of Molecular Sciences, 21(8), 2976. https://doi.org/10.3390/ijms21082976






