Ankyrin Repeat and Kinase Domain Containing 1 Gene, and Addiction Vulnerability
Abstract
1. Introduction
2. The Gene That Codes ANKK1, the TaqIA SNV, and Addictions
3. The Functional Relationship of ANKK1 and DRD2
4. The Locus of the Gene ANKK1 and Addictions
5. ANKK1 Protein, Brain Structure, and Addiction
6. Conclusion and Future Considerations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Koob, G.F.; Volkow, N.D. Neurocircuitry of addiction. Neuropsychopharmacology 2010, 35, 217–238. [Google Scholar] [CrossRef] [PubMed]
- Egervari, G.; Ciccocioppo, R.; Jentsch, J.D.; Hurd, Y.L. Shaping vulnerability to addiction—The contribution of behavior, neural circuits and molecular mechanisms. Neurosci. Biobehav. Rev. 2018, 85, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Boyle, M. Neuroscience of Addiction: Relevance to Prevention and Treatment. Am. J. Psychiatry 2018, 175, 729–740. [Google Scholar] [CrossRef] [PubMed]
- Bevilacqua, L.; Goldman, D. Genes and Addictions. Clin. Pharmacol. Ther. 2009, 85, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Kendler, K.S.; Davis, C.; Kessler, R.C. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: A family history study. Br. J. Psychiatry 1997, 170, 541–548. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Stolar, M.; Stevens, D.E.; Goulet, J.; Preisig, M.A.; Fenton, B.; Zhang, H.; O’Malley, S.S.; Rounsaville, B.J. Familial transmission of substance use disorders. Arch. Gen. Psychiatry 1998, 55, 973–979. [Google Scholar] [CrossRef]
- Goldman, D.; Oroszi, G.; Ducci, F. The genetics of addictions: Uncovering the genes. Nat. Rev. Genet. 2005, 6, 521–532. [Google Scholar] [CrossRef]
- Deroche-Gamonet, V.; Belin, D.; Piazza, P.V. Evidence for Addiction-like Behavior in the Rat. Science 2004, 305, 1014–1017. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Avenevoli, S. Implications of genetic epidemiology for the prevention of substance use disorders. Addict. Behav. 2000, 25, 807–820. [Google Scholar] [CrossRef]
- Nestler, E.J.; Lüscher, C. The Molecular Basis of Drug Addiction: Linking Epigenetic to Synaptic and Circuit Mechanisms. Neuron 2019, 102, 48–59. [Google Scholar] [CrossRef]
- Baarendse, P.J.J.; Limpens, J.H.W.; Vanderschuren, L.J.M.J. Disrupted social development enhances the motivation for cocaine in rats. Psychopharmacology (Berl) 2014, 231, 1695–1704. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.C.; Ford, K.A.; Pagels, N.E.; McCutcheon, J.E.; Marinelli, M. Adolescents are more vulnerable to cocaine addiction: Behavioral and electrophysiological evidence. J. Neurosci. 2013, 33, 4913–4922. [Google Scholar] [CrossRef]
- Blum, K.; Noble, E.P.; Sheridan, P.J.; Montgomery, A.; Ritchie, T.; Jagadeeswaran, P.; Nogami, H.; Briggs, A.H.; Cohn, J.B. Allelic association of human dopamine D2 receptor gene in alcoholism. JAMA 1990, 263, 2055–2060. [Google Scholar] [CrossRef]
- Noble, E.P. D2 dopamine receptor gene in psychiatric and neurologic disorders and its phenotypes. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2003, 116, 103–125. [Google Scholar] [CrossRef] [PubMed]
- Ponce, G.; Perez-Gonzalez, R.; Aragüés, M.; Palomo, T.; Rodríguez-Jiménez, R.; Jimenez-Arriero, M.A.; Hoenicka, J. The ANKK1 Kinase Gene and Psychiatric Disorders. Neurotox. Res. 2009, 16, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Simen, A.; Arias, A.; Lu, Q.-W.; Zhang, H. A large-scale meta-analysis of the association between the ANKK1/DRD2 Taq1A polymorphism and alcohol dependence. Hum. Genet. 2012, 132, 347–358. [Google Scholar] [CrossRef] [PubMed][Green Version]
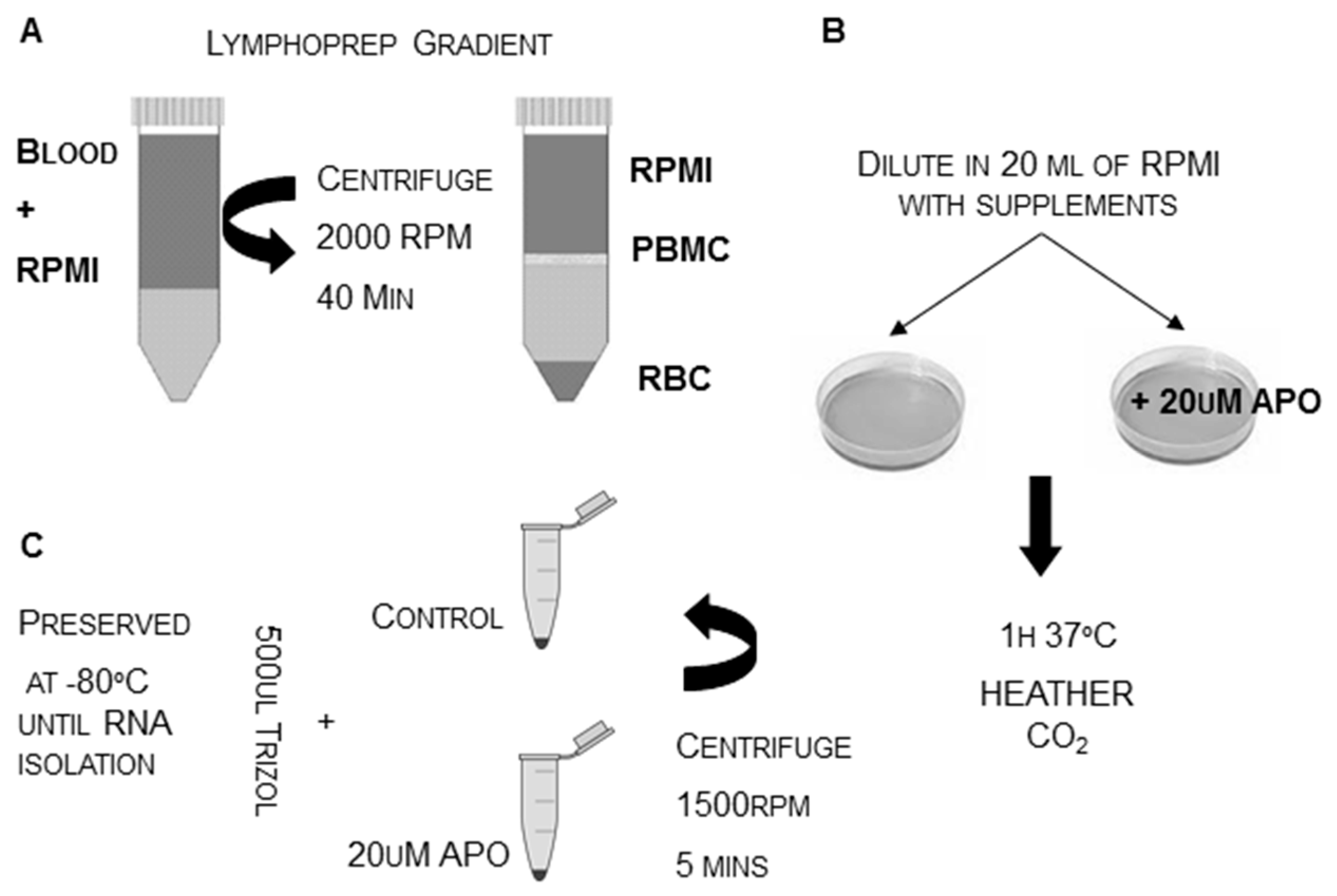
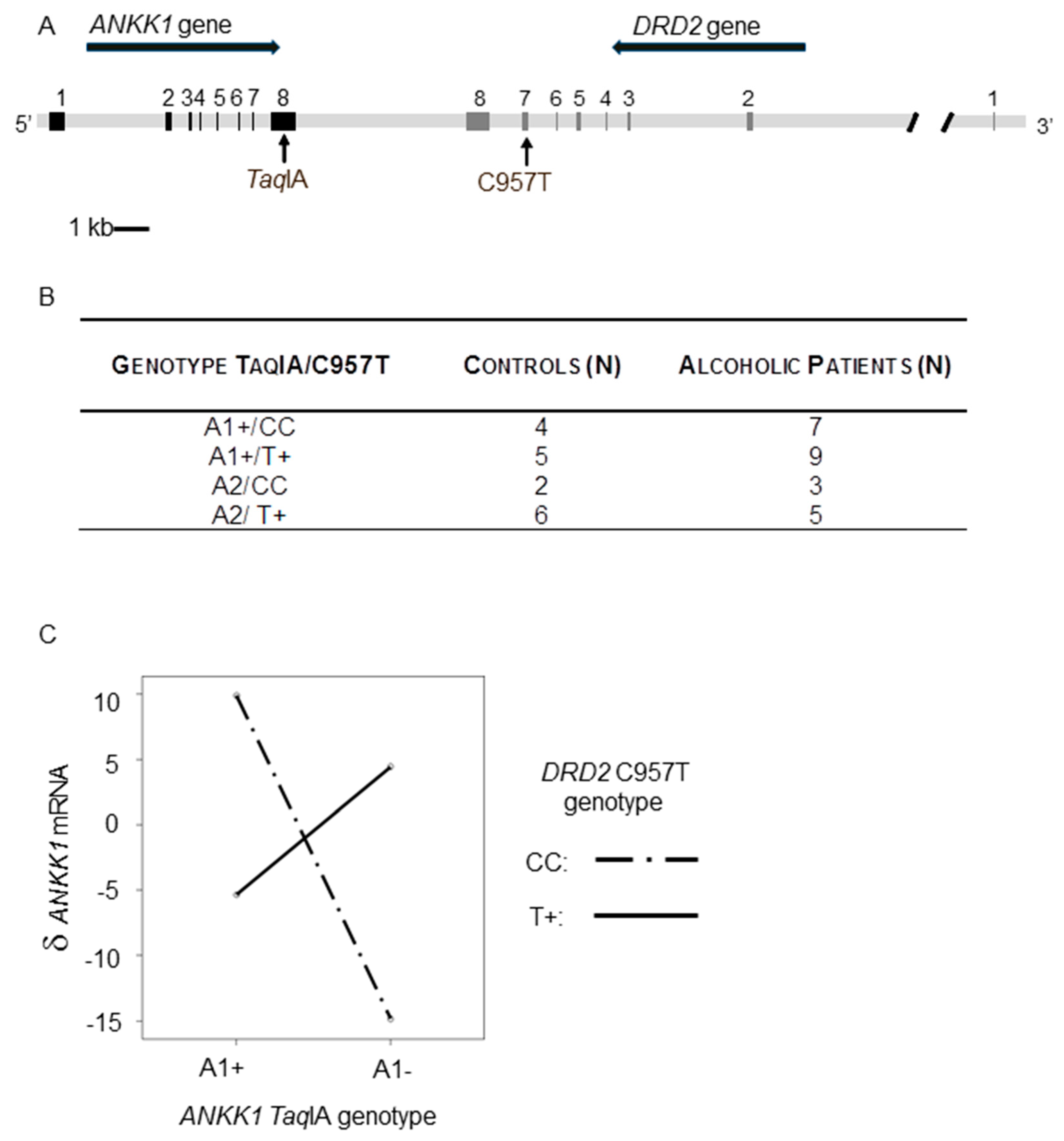
- Hoenicka, J.; Lombraña, A.Q.; España-Serrano, L.; Alvira, X.; Kremer, L.; Perez-Gonzalez, R.; Rodríguez-Jiménez, R.; Jimenez-Arriero, M.A.; Ponce, G.; Palomo, T. The ANKK1 Gene Associated with Addictions Is Expressed in Astroglial Cells and Upregulated by Apomorphine. Boil. Psychiatry 2010, 67, 3–11. [Google Scholar] [CrossRef] [PubMed]
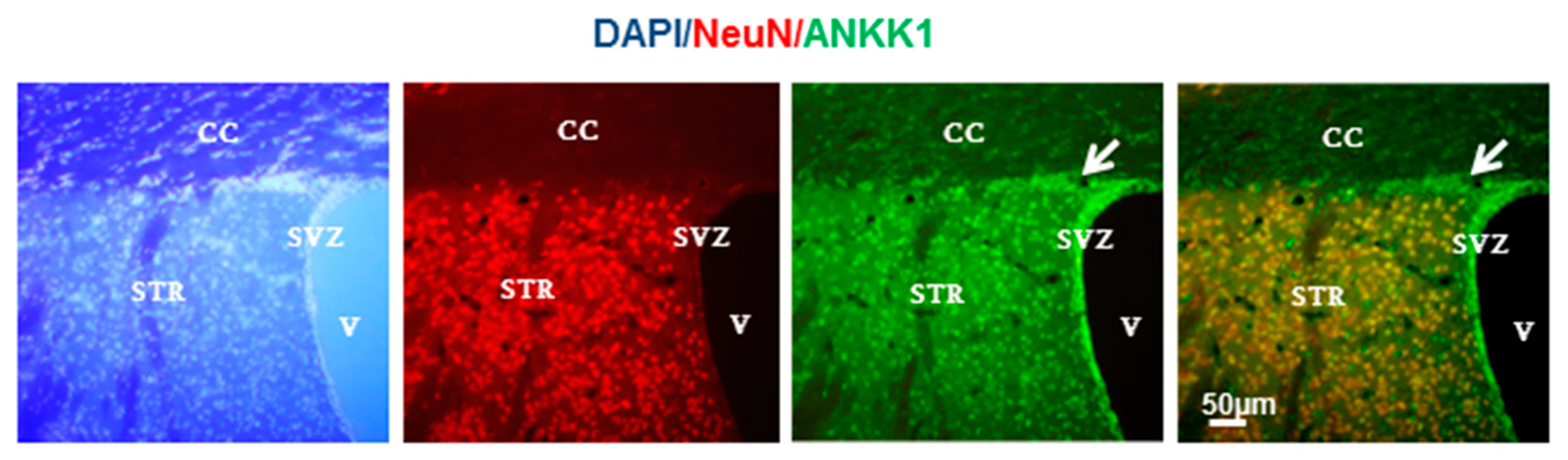
- España-Serrano, L.; Martín-Palanco, N.G.; Montero-Pedrazuela, A.; Perez-Santamarina, E.; Vidal, R.; García-Consuegra, I.; Valdizan, E.; Pazos, A.; Palomo, T.; Jiménez-Arriero, M.; et al. The Addiction-Related Protein ANKK1 is Differentially Expressed During the Cell Cycle in Neural Precursors. Cereb. Cortex 2017, 27, 2809–2819. [Google Scholar] [CrossRef]
- Garrido, E.; Palomo, T.; Ponce, G.; Garcia-Consuegra, I.; Jiménez-Arriero, M.A.; Hoenicka, J. The ANKK1 protein associated with addictions has nuclear and cytoplasmic localization and shows a differential response of Ala239Thr to apomorphine. Neurotox. Res. 2011, 20, 32–39. [Google Scholar] [CrossRef]
- Ponce, G.; Lombraña, A.Q.; Martín-Palanco, N.G.; Rubio-Solsona, E.; Jimenez-Arriero, M.A.; Palomo, T.; Hoenicka, J. The Addiction-Related Gene Ankk1 is Oppositely Regulated by D1R- and D2R-Like Dopamine Receptors. Neurotox. Res. 2016, 29, 345–350. [Google Scholar] [CrossRef]
- Neville, M.J.; Johnstone, E.C.; Walton, R.T. Identification and characterization of ANKK1: A novel kinase gene closely linked to DRD2 on chromosome band 11q23.1. Hum. Mutat. 2004, 23, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Blum, K.; Noble, E.P.; Sheridan, P.J.; Finley, O.; Montgomery, A.; Ritchie, T.; Ozkaragoz, T.; Fitch, R.J.; Sadlack, F.; Sheffield, D.; et al. Association of the A1 allele of the D2 dopamine receptor gene with severe alcoholism. Alcohol 1991, 8, 409–416. [Google Scholar] [CrossRef]
- Comings, D.E.; Muhleman, D.; Dietz, G.; Shahbahrami, B.; Tast, D.; Knell, E.; Kocsis, P.; Baumgarten, R.; Kovacs, B.W.; Levy, D.L.; et al. The Dopamine D2 Receptor Locus as a Modifying Gene in Neuropsychiatric Disorders. JAMA 1991, 266, 1793–1800. [Google Scholar] [CrossRef] [PubMed]
- Parsian, A.; Todd, R.D.; Devor, E.J.; O’Malley, K.L.; Suarez, B.K.; Reich, T.; Cloninger, C.R. Alcoholism and alleles of the human D2 dopamine receptor locus. Studies of association and linkage. Arch. Gen. Psychiatry 1991, 48, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Blum, K.; Noble, E.P. Alcoholism and the D2 Dopamine Receptor Gene. JAMA 1993, 270, 1547–1548. [Google Scholar] [CrossRef]
- Neiswanger, K.; Hill, S.Y.; Kaplan, B.B. Association and linkage studies of the TAQI A1 allele at the dopamine D2 receptor gene in samples of female and male alcoholics. Am. J. Med. Genet. 1995, 60, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Hietala, J.; Pohjalainen, T.; Heikkilä-Kallio, U.; West, C.; Salaspuro, M.; Syvälahti, E. Allelic association between D2 but not D1 dopamine receptor gene and alcoholism in Finland. Psychiatr. Genet. 1997, 7, 19–25. [Google Scholar] [CrossRef]
- Kono, Y.; Yoneda, H.; Sakai, T.; Nonomura, Y.; Inayama, Y.; Koh, J.; Sakai, J.; Inada, Y.; Imamichi, H.; Asaba, H. Association between early-onset alcoholism and the dopamine D2 receptor gene. Am. J. Med. Genet. 1997, 74, 179–182. [Google Scholar] [CrossRef]
- Ishiguro, H.; Arinami, T.; Saito, T.; Akazawa, S.; Enomoto, M.; Mitushio, H.; Fujishiro, H.; Tada, K.; Akimoto, Y.; Mifune, H.; et al. Association study between the -141C Ins/Del and TaqI A polymorphisms of the dopamine D2 receptor gene and alcoholism. Alcohol. Clin. Exp. Res. 1998, 22, 845–848. [Google Scholar] [CrossRef]
- Foley, P.F.; Loh, E.W.; Innes, D.J.; Williams, S.M.; Tannenberg, A.E.G.; Harper, C.G.; Dodd, P.R. Association Studies of Neurotransmitter Gene Polymorphisms in Alcoholic Caucasians. Ann. N. Y. Acad. Sci. 2004, 1025, 39–46. [Google Scholar] [CrossRef]
- Bolos, A.M.; Dean, M.; Lucas-Derse, S.; Ramsburg, M.; Brown, G.L.; Goldman, D. Population and Pedigree Studies Reveal a Lack of Association Between the Dopamine D2 Receptor Gene and Alcoholism. JAMA 1991, 264, 3156–3160. [Google Scholar] [CrossRef]
- Gelernter, J.; O’Malley, S.; Risch, N.; Kranzler, H.R.; Krystal, J.; Merikangas, K.; Kennedy, J.L.; Kidd, K.K. No association between an allele at the D2 dopamine receptor gene (DRD2) and alcoholism. JAMA 1991, 266, 1801–1807. [Google Scholar] [CrossRef] [PubMed]
- Turner, E.; Ewing, J.; Shilling, P.; Smith, T.L.; Irwin, M.R.; Schuckit, M.; Kelsoe, J.R. Lack of association between an RFLP near the D2 dopamine receptor gene and severe alcoholism. Boil. Psychiatry 1992, 31, 285–290. [Google Scholar] [CrossRef]
- Goldman, D.; Dean, M.; Brown, G.L.; Bolos, A.M.; Tokola, R.; Virkkunen, M.; Linnoila, M. D2dopamine receptor genotype and cerebrospinal fluid homovanillic acid, 5-hydroxyindoleacetic acid and 3-methoxy-4-hydroxyphenylglycol in alcoholics in Finland and the United States. Acta Psychiatr. Scand. 1992, 86, 351–357. [Google Scholar] [CrossRef]
- Arinami, T.; Itokawa, M.; Komiyama, T.; Mitsushio, H.; Mori, H.; Mifune, H.; Hamaguchi, H.; Toru, M. Association between severity of alcoholism and the A1 allele of the dopamine D2 receptor gene TaqI A RFLP in Japanese. Boil. Psychiatry 1993, 33, 108–114. [Google Scholar] [CrossRef]
- Goldman, D.; Urbanek, M.; Guenther, D.; Robin, R.; Long, J.C. Linkage and association of a functional DRD2 variant [Ser311Cys] and DRD2 markers to alcoholism, substance abuse and schizophrenia in Southwestern American Indians. Am. J. Med. Genet. 1997, 74, 386–394. [Google Scholar] [CrossRef]
- Suarez, B.; Parsian, A.; Hampe, C.; Todd, R.; Reich, T.; Cloninger, C. Linkage Disequilibria at the D2 Dopamine Receptor Locus (DRD2) in Alcoholics and Controls. Genomics 1994, 19, 12–20. [Google Scholar] [CrossRef]
- Cruz, C.; Camarena, B.; Mejía, J.M.; Páez, F.; Eroza, V.; De La Fuente, J.R.; Kershenobich, D.; Nicolini, H. The dopamine D2 receptor gene TaqI A1 polymorphism and alcoholism in a Mexican population. Arch. Med. Res. 1995, 26, 421–426. [Google Scholar]
- Sander, T.; Harms, H.; Podschus, J.; Finckh, U.; Nickel, B.; Rolfs, A.; Rommelspacher, H.; Schmidt, L.G. Dopamine D1, D2 and D3 receptor genes in alcohol dependence. Psychiatr. Genet. 1995, 5, 171–176. [Google Scholar] [CrossRef]
- Sander, T.; Ladehoff, M.; Samochowiec, J.; Finckh, U.; Rommelspacher, H.; Schmidt, L.G. Lack of an allelic association between polymorphisms of the dopamine D2 receptor gene and alcohol dependence in the German population. Alcohol. Clin. Exp. Res. 1999, 23, 578–581. [Google Scholar] [CrossRef]
- Lu, R.-B.; Ko, H.-C.; Chang, F.-M.; Castiglione, C.M.; Schoolfield, G.; Pakstis, A.J.; Kidd, J.R.; Kidd, K.K. No association between alcoholism and multiple polymorphisms at the dopamine D2 receptor gene (DRD2) in three distinct taiwanese populations. Boil. Psychiatry 1996, 39, 419–429. [Google Scholar] [CrossRef]
- Chen, C.; Chien, S.; Hwu, H.-G. Lack of association between TaqI A1 allele of dopamine D2 receptor gene and alcohol-use disorders in Atayal natives of Taiwan. Am. J. Med. Genet. 1996, 67, 488–490. [Google Scholar] [CrossRef]
- Chen, W.; Lu, M.L.; Hsu, Y.P.; Chen, C.C.; Yu, J.M.; Cheng, A.T. Dopamine D2 receptor gene and alcoholism among four aboriginal groups and Han in Taiwan. Am. J. Med. Genet. 1997, 74, 129–136. [Google Scholar] [CrossRef]
- Edenberg, H.J.; Foroud, T.; Koller, D.L.; Goate, A.; Rice, J.; Van Eerdewegh, P.; Reich, T.; Cloninger, C.R.; Nurnberger, J.I.; Kowalczuk, M.; et al. A family-based analysis of the association of the dopamine D2 receptor (DRD2) with alcoholism. Alcohol. Clin. Exp. Res. 1998, 22, 505–512. [Google Scholar] [CrossRef]
- Lobos, E.A.; Todd, R.D. Association analysis in an evolutionary context: Cladistic analysis of the DRD2 locus to test for association with alcoholism. Am. J. Med. Genet. 1998, 81, 411–419. [Google Scholar] [CrossRef]
- Gelernter, J. D2 Dopamine Receptor Gene (DRD2) Allele and Haplotype Frequencies in Alcohol Dependent and Control Subjects No Association with Phenotype or Severity of Phenotype. Neuropsychopharmacology 1999, 20, 640–649. [Google Scholar] [CrossRef]
- Lee, J.-F.; Lu, R.-B.; Ko, H.-C.; Chang, F.-M.; Yin, S.-J.; Pakstis, A.J.; Kidd, K. No Association Between DRD2 Locus and Alcoholism After Controlling the ADH and ALDH Genotypes in Chinese Han Population. Alcohol. Clin. Exp. Res. 1999, 23, 592–599. [Google Scholar] [CrossRef]
- Waldman, I.D.; Robinson, B.F.; Rhee, S.H. A logistic regression extension of the transmission disequilibrium test for continuous traits: Application to linkage disequilibrium between alcoholism and the candidate genes DRD2 and ADH3. Genet. Epidemiol. 1999, 17, S379–S384. [Google Scholar] [CrossRef]
- Parsian, A.; Cloninger, C.R.; Zhang, Z.H. Functional variant in the DRD2 receptor promoter region and subtypes of alcoholism. Am. J. Med. Genet. 2000, 96, 407–411. [Google Scholar] [CrossRef]
- Munafò, M.R.; Matheson, I.J.; Flint, J.; Munaf, I.J.M.M.R. Association of the DRD2 gene Taq1A polymorphism and alcoholism: A meta-analysis of case–control studies and evidence of publication bias. Mol. Psychiatry 2007, 12, 454–461. [Google Scholar] [CrossRef]
- Smith, L.; Watson, M.; Gates, S.; Ball, D.; Foxcroft, D. Meta-Analysis of the Association of the Taq1A Polymorphism with the Risk of Alcohol Dependency: A HuGE Gene-Disease Association Review. Am. J. Epidemiol. 2008, 167, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Bühler, K.-M.; Giné, E.; Echeverry-Alzate, V.; Calleja-Conde, J.; De Fonseca, F.R.; Moreno, J.A.L. Common single nucleotide variants underlying drug addiction: More than a decade of research. Addict. Boil. 2015, 20, 845–871. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.; Montel, R.A.; Shen, P.-H.; Mash, D.C.; Goldman, D. Assessment of the Association of D2 Dopamine Receptor Gene and Reported Allele Frequencies with Alcohol Use Disorders: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e1914940. [Google Scholar] [CrossRef] [PubMed]
- Ponce, G.; Jimenez-Arriero, M.A.; Rubio, G.; Hoenicka, J.; Ampuero, I.; Ramos, J.A.; Palomo, T. The A1 allele of the DRD2 gene (TaqI A polymorphisms) is associated with antisocial personality in a sample of alcohol-dependent patients. Eur. Psychiatry 2003, 18, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Jiménez, R.; Hoenicka, J.; Jiménez-Arriero, M.; Ponce, G.; Bagney, A.; Aragues, M.; Palomo, T. Performance in the Wisconsin Card Sorting Test and the C957T Polymorphism of the DRD2 Gene in Healthy Volunteers. Neuropsychobiology 2006, 54, 166–170. [Google Scholar] [CrossRef]
- Uhl, G.; Blum, K.; Noble, E.; Smith, S. Substance abuse vulnerability and D2 receptor genes. Trends Neurosci. 1993, 16, 83–88. [Google Scholar] [CrossRef]
- Li, M.D.; Ma, J.; Beuten, J. Progress in searching for susceptibility loci and genes for smoking-related behaviour. Clin. Genet. 2004, 66, 382–392. [Google Scholar] [CrossRef]
- Munafò, M.R.; Clark, T.G.; Johnstone, E.C.; Murphy, M.F.G.; Walton, R.T. The genetic basis for smoking behavior: A systematic review and meta-analysis. Nicotine Tob. Res. 2004, 6, 583–597. [Google Scholar] [CrossRef]
- Lawford, B.R.; Young, R.M.; Noble, E.P.; Sargent, J.; Rowell, J.; Shadforth, S.; Zhang, X.; Ritchie, T. The D(2) dopamine receptor A(1) allele and opioid dependence: Association with heroin use and response to methadone treatment. Am. J. Med. Genet. 2000, 96, 592–598. [Google Scholar] [CrossRef]
- Cobos, J.P.D.L.; Baiget, M.; Trujols, J.; Sinol, N.; Volpini, V.; Banuls, E.; Calafell, F.; Luquero, E.; Del Rio, E.; Álvarez, E. Allelic and genotypic associations of DRD2 TaqI A polymorphism with heroin dependence in Spanish subjects: A case control study. Behav. Brain Funct. 2007, 3, 25. [Google Scholar] [CrossRef]
- Hou, Q.-F.; Li, S.-B. Potential association of DRD2 and DAT1 genetic variation with heroin dependence. Neurosci. Lett. 2009, 464, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Vereczkei, A.; Demetrovics, Z.; Szekely, A.; Sárközy, P.; Antal, P.; Szilágyi, Á.; Sasvári-Székely, M.; Barta, C. Multivariate Analysis of Dopaminergic Gene Variants as Risk Factors of Heroin Dependence. PLoS ONE 2013, 8, e66592. [Google Scholar] [CrossRef] [PubMed]
- Barratt, D.; Coller, J.K.; Somogyi, A.A. Association between theDRD2 A1 allele and response to methadone and buprenorphine maintenance treatments. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2006, 141, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Crettol, S.; Besson, J.; Croquette-Krokar, M.; Hämmig, R.; Gothuey, I.; Monnat, M.; Deglon, J.-J.; Preisig, M.; Eap, C.B. Association of dopamine and opioid receptor genetic polymorphisms with response to methadone maintenance treatment. Prog. Neuro-Psychopharmacol. Boil. Psychiatry 2008, 32, 1722–1727. [Google Scholar] [CrossRef]
- Doehring, A.; Von Hentig, N.; Graff, J.; Salamat, S.; Schmidt, M.; Geisslinger, G.; Harder, S.; Lötsch, J. Genetic variants altering dopamine D2 receptor expression or function modulate the risk of opiate addiction and the dosage requirements of methadone substitution. Pharmacogenetics Genom. 2009, 19, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.D.; Jiang, H.; Ma, Y.; Gao, Q.; Zhang, B.; Mu, B.; Zhang, L.-X.; Zhang, W.; Er, Z.-E.M.; Xie, Y.; et al. Association between DRD2/ANKK1 TaqIA polymorphism and common illicit drug dependence: Evidence from a meta-analysis. Hum. Immunol. 2015, 76, 42–51. [Google Scholar] [CrossRef]
- Chiara, G.; Imperato, A. Preferential Stimulation of Dopamine Release in the Nucleus Accumbens by Opiates, Alcohol, and Barbiturates: Studies with Transcerebral Dialysis in Freely Moving Rats. Ann. N. Y. Acad. Sci. 1986, 473, 367–381. [Google Scholar] [CrossRef]
- Volkow, N.D.; Fowler, J.S.; Wang, G.-J.; Telang, F.; Baler, R. Imaging Dopamine’s Role in Drug Abuse and Addiction. Neuropharmacology 2009, 56, 3–8. [Google Scholar] [CrossRef]
- Sahu, A.; Tyeryar, K.R.; Vongtau, H.O.; Sibley, D.R.; Undieh, A. D5 dopamine receptors are required for dopaminergic activation of phospholipase C. Mol. Pharmacol. 2009, 75, 447–453. [Google Scholar] [CrossRef]
- Everett, P.B.; Senogles, S.E. D3dopamine receptor signals to activation of phospholipase D through a complex with Rho. J. Neurochem. 2010, 112, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Koshibu, K.; Gräff, J.; Beullens, M.; Heitz, F.D.; Berchtold, D.; Russig, H.; Farinelli, M.; Bollen, M.; Mansuy, I.M. Protein Phosphatase 1 Regulates the Histone Code for Long-Term Memory. J. Neurosci. 2009, 29, 13079–13089. [Google Scholar] [CrossRef] [PubMed]
- Gräff, J.; Koshibu, K.; Jouvenceau, A.; Dutar, P.; Mansuy, I.M. Protein phosphatase 1-dependent transcriptional programs for long-term memory and plasticity. Learn. Mem. 2010, 17, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Koeneke, A.; Ponce, G.; Hoenicka, J.; Huertas, E. The ANKK1/DRD2 locus is a genomic substrate for affective priming and recognition of angry faces. Brain Behav. 2015, 5, e00405. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Bertolino, A.; Fazio, L.; Blasi, G.; Rampino, A.; Romano, R.; Lee, M.-L.T.; Xiao, T.; Papp, A.; Wang, D.; et al. Polymorphisms in human dopamine D2 receptor gene affect gene expression, splicing, and neuronal activity during working memory. Proc. Natl. Acad. Sci. USA 2007, 104, 20552–20557. [Google Scholar] [CrossRef] [PubMed]
- Valli, M.; Cho, S.S.; Masellis, M.; Chen, R.; Rusjan, P.; Kim, J.; Koshimori, Y.; Mihaescu, A.; Strafella, A.P. DRD2 Genotype-Based Variants Modulates D2 Receptor Distribution in Ventral Striatum. Mol. Neurobiol. 2019, 56, 6512–6520. [Google Scholar] [CrossRef] [PubMed]
- Laakso, A.; Pohjalainen, T.; Bergman, J.; Kajander, J.; Haaparanta, M.; Solin, O.; Syvälahti, E.; Hietala, J. The A1 allele of the human D2 dopamine receptor gene is associated with increased activity of striatal L-amino acid decarboxylase in healthy subjects. Pharmacogenetics Genom. 2005, 15, 387–391. [Google Scholar] [CrossRef]
- Duan, J.; Wainwright, M.S.; Comeron, J.M.; Saitou, N.; Sanders, A.R.; Gelernter, J.; Gejman, P.V. Synonymous mutations in the human dopamine receptor D2 (DRD2) affect mRNA stability and synthesis of the receptor. Hum. Mol. Genet. 2003, 12, 205–216. [Google Scholar] [CrossRef]
- Hirvonen, M.; Laakso, A.; Någren, K.; Rinne, J.; Pohjalainen, T.; Hietala, J. C957T polymorphism of the dopamine D2 receptor (DRD2) gene affects striatal DRD2 availability in vivo. Mol. Psychiatry 2004, 9, 1060–1061. [Google Scholar] [CrossRef]
- Ponce, G.; Hoenicka, J.; Jiménez-Arriero, M.A.; Rodríguez-Jiménez, R.; Aragües, M.; Martin-Sune, N.; Huertas, E.; Palomo, T. DRD2 and ANKK1 genotype in alcohol-dependent patients with psychopathic traits: Association and interaction study. Br. J. Psychiatry 2008, 193, 121–125. [Google Scholar] [CrossRef]
- Huertas, E.; Ponce, G.; Koeneke, M.A.; Poch, C.; Palomo, T.; Hoenicka, J.; España-Serrano, L.; Jiménez-Arriero, M.Á. The D2 dopamine receptor gene variant C957T affects human fear conditioning and aversive priming. Genes Brain Behav. 2010, 9, 103–109. [Google Scholar] [CrossRef]
- Klaus, K.; Butler, K.; Curtis, F.; Bridle, C.; Pennington, K. The effect of ANKK1 Taq1A and DRD2 C957T polymorphisms on executive function: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2019, 100, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Ariza, M.; Garolera, M.; Jurado, M.A.; Garcia-Garcia, I.; Hernan, I.; Sánchez-Garre, C.; Vernet-Vernet, M.; Sender-Palacios, M.J.; Marques-Iturria, I.; Pueyo, R.; et al. Dopamine genes (DRD2/ANKK1-TaqA1 and DRD4-7R) and executive function: Their interaction with obesity. PLoS ONE 2012, 7, e41482. [Google Scholar] [CrossRef] [PubMed]
- Butcher, P.A. Cortical-Subcortical Interactions in Cognitive Control, Associative Learning and Motor Control. Ph.D. Thesis, University of California, Berkeley, CA, USA, 2014. [Google Scholar]
- Berryhill, M.E.; Wiener, M.; Stephens, J.A.; Lohoff, F.W.; Coslett, H.B. COMT and ANKK1-Taq-Ia Genetic Polymorphisms Influence Visual Working Memory. PLoS ONE 2013, 8, e55862. [Google Scholar] [CrossRef] [PubMed]
- Stelzel, C.; Basten, U.; Montag, C.; Reuter, M.; Fiebach, C. Frontostriatal Involvement in Task Switching Depends on Genetic Differences in D2 Receptor Density. J. Neurosci. 2010, 30, 14205–14212. [Google Scholar] [CrossRef]
- Nkam, I.; Ramoz, N.; Breton, F.; Mallet, J.; Gorwood, P.; Dubertret, C. Impact of DRD2/ANKK1 and COMT Polymorphisms on Attention and Cognitive Functions in Schizophrenia. PLoS ONE 2017, 12, e0170147. [Google Scholar] [CrossRef]
- Bellander, M.; Bäckman, L.; Liu, T.; Schjeide, B.-M.M.; Bertram, L.; Schmiedek, F.; Lindenberger, U.; Lövdén, M. Lower baseline performance but greater plasticity of working memory for carriers of the val allele of the COMT Val(1)(5)(8)Met polymorphism. Neuropsychology 2015, 29, 247–254. [Google Scholar] [CrossRef][Green Version]
- Colzato, L.S.; Steenbergen, L.; Sellaro, R.; Stock, A.-K.; Arning, L.; Beste, C. Effects of l-Tyrosine on working memory and inhibitory control are determined by DRD2 genotypes: A randomized controlled trial. Cortex 2016, 82, 217–224. [Google Scholar] [CrossRef]
- Klaus, K.; Butler, K.; Durrant, S.J.; Ali, M.; Inglehearn, C.F.; Hodgson, T.L.; Gutierrez, H.; Pennington, K. The effect of COMT Val158Met and DRD2 C957T polymorphisms on executive function and the impact of early life stress. Brain Behav. 2017, 7, e00695. [Google Scholar] [CrossRef]
- Gurvich, C.; Rossell, S.L. Genetic variations in dopamine and inhibitory control: Lack of influence on action restraint. Behav. Brain Res. 2014, 267, 12–16. [Google Scholar] [CrossRef]
- Ferrari, M.; Cosentino, M.; Marino, F.; Bombelli, R.; Rasini, E.; Lecchini, S.; Frigo, G. Dopaminergic D1-like receptor-dependent inhibition of tyrosine hydroxylase mRNA expression and catecholamine production in human lymphocytes. Biochem. Pharmacol. 2004, 67, 865–873. [Google Scholar] [CrossRef]
- Ahangari, G.; Shariati, G.H.; Asadi, M.R.; Ostadali, M.R.; Ahmadkhaniha, H.R. Novel Mutation Detection of Regulatory Molecule Dopamine Gene Receptors (D1-D5) Encoding Analysis on Human Peripheral Blood Lymphocytes in Schizophrenia Patients. Eur. J. Inflamm. 2009, 7, 145–152. [Google Scholar] [CrossRef]
- Mota, N.R.; Araujo-Jnr, E.V.; Paixão-Côrtes, V.R.; Bortolini, M.C.; Bau, C.H.D. Linking dopamine neurotransmission and neurogenesis: The evolutionary history of the NTAD (NCAM1-TTC12-ANKK1-DRD2) gene cluster. Genet. Mol. Boil. 2012, 35 (Suppl. 4), 912–918. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.-Z.; Kranzler, H.R.; Zhao, H.; Gruen, J.; Luo, X.; Gelernter, J. Association of haplotypic variants in DRD2, ANKK1, TTC12 and NCAM1 to alcohol dependence in independent case–control and family samples. Hum. Mol. Genet. 2007, 16, 2844–2853. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.-Z.; Kranzler, H.R.; Zhao, H.; Gruen, J.R.; Luo, X.; Gelernter, J. Haplotypic variants in DRD2, ANKK1, TTC12, and NCAM1 are associated with comorbid alcohol and drug dependence. Alcohol. Clin. Exp. Res. 2008, 32, 2117–2127. [Google Scholar] [CrossRef] [PubMed]
- Dick, D.; Wang, J.C.; Plunkett, J.; Aliev, F.; Hinrichs, A.; Bertelsen, S.; Budde, J.; Goldstein, E.L.; Kaplan, D.; Edenberg, H.J.; et al. Family-Based Association Analyses of Alcohol Dependence Phenotypes Across DRD2 and Neighboring Gene ANKK1. Alcohol. Clin. Exp. Res. 2007, 31, 1645–1653. [Google Scholar] [CrossRef] [PubMed]
- Gelernter, J.; Yu, Y.; Weiss, R.; Brady, K.; Panhuysen, C.; Yang, B.-Z.; Kranzler, H.R.; Farrer, L.A. Haplotype spanning TTC12 and ANKK1, flanked by the DRD2 and NCAM1 loci, is strongly associated to nicotine dependence in two distinct American populations. Hum. Mol. Genet. 2006, 15, 3498–3507. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Payne, T.; Ma, J.Z.; Beuten, J.; Dupont, R.T.; Inohara, N.; Li, M.D. Significant Association of ANKK1 and Detection of a Functional Polymorphism with Nicotine Dependence in an African-American Sample. Neuropsychopharmacology 2009, 34, 319–330. [Google Scholar] [CrossRef]
- Bidwell, L.C.; McGeary, J.E.; Gray, J.C.; Palmer, R.; Knopik, V.S.; MacKillop, J. NCAM1-TTC12-ANKK1-DRD2 variants and smoking motives as intermediate phenotypes for nicotine dependence. Psychopharmacology (Berl) 2015, 232, 1177–1186. [Google Scholar] [CrossRef]
- Bidwell, L.C.; McGeary, J.E.; Gray, J.C.; Palmer, R.; Knopik, V.; MacKillop, J. An initial investigation of associations between dopamine-linked genetic variation and smoking motives in African Americans. Pharmacol. Biochem. Behav. 2015, 138, 104–110. [Google Scholar] [CrossRef][Green Version]
- Liu, Q.; Xu, Y.; Mao, Y.; Ma, Y.; Wang, M.; Han, H.; Cui, W.; Yuan, W.; Payne, T.J.; Xu, Y.; et al. Genetic and Epigenetic Analysis Revealing Variants in the NCAM1–TTC12–ANKK1–DRD2 Cluster Associated Significantly with Nicotine Dependence in Chinese Han Smokers. Nicotine Tob. Res. 2019. [Google Scholar] [CrossRef]
- Nelson, E.C.; Lynskey, M.T.; Heath, A.C.; Wray, N.R.; Agrawal, A.; Shand, F.L.; Henders, A.; Wallace, L.; Todorov, A.A.; Schrage, A.J.; et al. ANKK1, TTC12, and NCAM1 polymorphisms and heroin dependence: Importance of considering drug exposure. JAMA Psychiatry 2013, 70, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Bonfanti, L. PSA-NCAM in mammalian structural plasticity and neurogenesis. Prog. Neurobiol. 2006, 80, 129–164. [Google Scholar] [CrossRef] [PubMed]
- Cerasa, A.; Gioia, M.C.; Tarantino, P.; Labate, A.; Arabia, G.; Annesi, G.; Lanza, P.; Di Palma, G.; Blasi, V.; Quattrone, A. The DRD2 TaqIA polymorphism associated with changed midbrain volumes in healthy individuals. Genes Brain Behav. 2009, 8, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Montag, C.; Weber, B.; Jentgens, E.; Elger, C.; Reuter, M. An epistasis effect of functional variants on the BDNF and DRD2 genes modulates gray matter volume of the anterior cingulate cortex in healthy humans. Neuropsychologia 2010, 48, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Papenberg, G.; Bäckman, L.; Persson, J. Influence of the DRD2/ANKK1 Taq1A polymorphism on caudate volume in older adults without dementia. Brain Struct. Funct. 2018, 223, 2653–2662. [Google Scholar] [CrossRef]
- Klein, T.A.; Neumann, J.; Reuter, M.; Hennig, J.; Von Cramon, D.Y.; Ullsperger, M. Genetically Determined Differences in Learning from Errors. Science 2007, 318, 1642–1645. [Google Scholar] [CrossRef] [PubMed]
- Lucht, M.; Rosskopf, D. Comment on “Genetically Determined Differences in Learning from Errors”. Science 2008, 321, 200. [Google Scholar] [CrossRef]
- Rubio-Solsona, E.; Martí, S.; Vílchez, J.J.; Palau, F.; Hoenicka, J. ANKK1 is found in myogenic precursors and muscle fibers subtypes with glycolytic metabolism. PLoS ONE 2018, 13, e0197254. [Google Scholar]
- Cashman, N.R.; Covault, J.; Wollman, R.L.; Sanes, J.R. Neural cell adhesion molecule in normal, denervated, and myopathic human muscle. Ann. Neurol. 1987, 21, 481–489. [Google Scholar] [CrossRef]
- Capkovic, K.L.; Stevenson, S.; Johnson, M.C.; Thelen, J.J.; Cornelison, D. Neural cell adhesion molecule (NCAM) marks adult myogenic cells committed to differentiation. Exp. Cell Res. 2008, 314, 1553–1565. [Google Scholar] [CrossRef]
- Witt, A.; Vucic, D. Diverse ubiquitin linkages regulate RIP kinases-mediated inflammatory and cell death signaling. Cell Death Differ. 2017, 24, 1160–1171. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Lin, J.; Han, J. Receptor-interacting protein (RIP) kinase family. Cell. Mol. Immunol. 2010, 7, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Meylan, E.; Tschopp, J. The RIP kinases: Crucial integrators of cellular stress. Trends Biochem. Sci. 2005, 30, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Munz, B.; Hildt, E.; Springer, M.L.; Blau, H.M. RIP2, a Checkpoint in Myogenic Differentiation. Mol. Cell. Biol. 2002, 22, 5879–5886. [Google Scholar] [CrossRef][Green Version]
- Adams, S.; Munz, B. RIP4 is a target of multiple signal transduction pathways in keratinocytes: Implications for epidermal differentiation and cutaneous wound repair. Exp. Cell Res. 2010, 316, 126–137. [Google Scholar] [CrossRef]
- Bahnassawy, L.; Nicklas, S.; Palm, T.; Menzl, I.; Birzele, F.; Gillardon, F.; Schwamborn, J.C. The Parkinson’s Disease-Associated LRRK2 Mutation R1441G Inhibits Neuronal Differentiation of Neural Stem Cells. Stem Cells Dev. 2013, 22, 2487–2496. [Google Scholar] [CrossRef]
- Leyton, M.; Vezina, P. Dopamine ups and downs in vulnerability to addictions: A neurodevelopmental model. Trends Pharmacol. Sci. 2014, 35, 268–276. [Google Scholar] [CrossRef]
- Nishi, A.; Bibb, J.A.; Matsuyama, S.; Hamada, M.; Higashi, H.; Nairn, A.C.; Greengard, P. Regulation of DARPP-32 dephosphorylation at PKA- and Cdk5-sites by NMDA and AMPA receptors: Distinct roles of calcineurin and protein phosphatase-2A. J. Neurochem. 2002, 81, 832–841. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koeneke, A.; Ponce, G.; Troya-Balseca, J.; Palomo, T.; Hoenicka, J. Ankyrin Repeat and Kinase Domain Containing 1 Gene, and Addiction Vulnerability. Int. J. Mol. Sci. 2020, 21, 2516. https://doi.org/10.3390/ijms21072516
Koeneke A, Ponce G, Troya-Balseca J, Palomo T, Hoenicka J. Ankyrin Repeat and Kinase Domain Containing 1 Gene, and Addiction Vulnerability. International Journal of Molecular Sciences. 2020; 21(7):2516. https://doi.org/10.3390/ijms21072516
Chicago/Turabian StyleKoeneke, Alejandra, Guillermo Ponce, Johanna Troya-Balseca, Tomás Palomo, and Janet Hoenicka. 2020. "Ankyrin Repeat and Kinase Domain Containing 1 Gene, and Addiction Vulnerability" International Journal of Molecular Sciences 21, no. 7: 2516. https://doi.org/10.3390/ijms21072516
APA StyleKoeneke, A., Ponce, G., Troya-Balseca, J., Palomo, T., & Hoenicka, J. (2020). Ankyrin Repeat and Kinase Domain Containing 1 Gene, and Addiction Vulnerability. International Journal of Molecular Sciences, 21(7), 2516. https://doi.org/10.3390/ijms21072516




