The Role of Bcl-xL Protein Research in Veterinary Oncology
Abstract
1. Introduction
1.1. Comparative Oncology—Canine Models in Cancer Biology and Therapy
1.2. Role of Bcl-xL Protein in Apoptosis
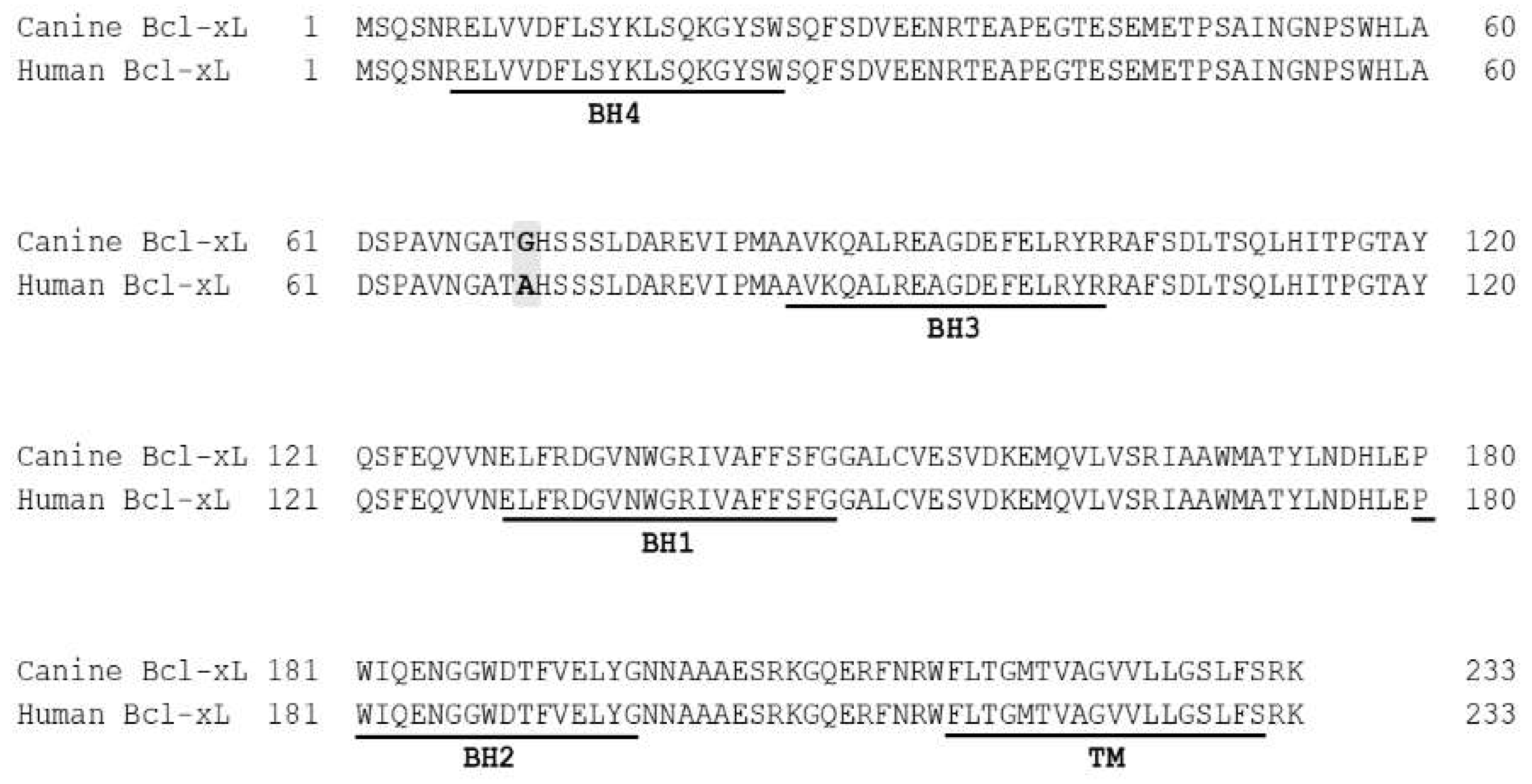
2. Bcl-xL Protein and Its Canine Version
Structure and Function of Bcl-xL Protein in Apoptosis
3. Bcl-xL in Canine Cancer Studies
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| APAF-1 | apoptotic protease activating factor 1 |
| ASM | aggressive systemic mastocytosis |
| BAD | Bcl-2-antagonist of cell death |
| BAK | Bcl-2 antagonist/killer |
| BAX | Bcl-2 associated X |
| Bcl-2 | B-cell lymphoma 2 |
| Bcl-xL | B-cell lymphoma-extra large |
| BH | Bcl-2 homology |
| BID | BH-3 interacting domain death agonist |
| BIK | Bcl-2 interacting killer |
| BIM | Bcl-2 interacting mediator of cell death |
| BMF | Bcl-2 modifying factor |
| BOK | Bcl-2 related ovarian killer |
| cFLIP | Cellular FLICE (FADD-like IL-1β-converting enzyme)-inhibitory protein |
| ER | endoplasmic reticulum |
| FIV | Feline immunodeficiency virus |
| HRK | harakiri, Bcl-2 interacting protein |
| HtrA2 | high temperature requirement protein A2 |
| IAPs | inhibitor of apoptosis proteins |
| JAK/STAT | Janus kinase/Signal transducer and activator of transcription |
| LPS | Lipopolysaccharide |
| MC | mast cells |
| MCL | mast cell leukemia |
| Mcl-1 | myeloid cell leukemia 1 |
| MOMP | mitochondrial outer membrane permeability |
| MPT | mitochondrial permeability transition |
| NF-kB | nuclear factor kappaB |
| PBMC | peripheral blood mononuclear cells |
| PI 3-kinase | phosphatidylinositol 3-kinase |
| PNETs | primitive neuroectodermal tumors |
| Pt-TCEP | complex of platinum with tris(2-carboxyethyl)phosphine |
| PUMA | p53 upregulated modulator of apoptosis |
| RT-PCR | reverse-transcription polymerase chain reaction |
| SAPK/JNK | stress-activated protein kinase/c-Jun NH2-terminal kinase |
| siRNA | small interfering RNA |
| Smac/DIABLO | second mitochondria derived activator of caspases/direct inhibitor of apoptosis binding protein with a low isoelectric point |
| TRAIL | TNF-related apoptosis inducing ligand |
| TUNEL | Tdt-mediated dUTP nick-end labeling |
| XIAP | X-linked inhibitor of apoptosis |
References
- Paoloni, M.C.; Khanna, C. Comparative oncology today. Vet. Clin. N. Am. Small Anim. Pract. 2007, 37, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Withrow, S.J.; Vail, D.M.; Page, R. Withrow and MacEwen’s Small Animal Clinical Oncology; Elsevier Health Sciences: St. Louis, MO, USA, 2013. [Google Scholar]
- Zappulli, V.; De Zan, G.; Cardazzo, B.; Bargelloni, L.; Castagnaro, M. Feline mammary tumours in comparative oncology. J. Dairy Res. 2005, 72, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Schoemaker, N.J. Ferret Oncology: Diseases, Diagnostics, and Therapeutics. Vet. Clin. N. Am. Exot. Anim. Pract. 2017, 20, 183–208. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.L.; Andrews, P.A.; Smith, D.D.; DeGeorge, J.J.; Justice, R.L.; Beitz, J.G. Predictive value of preclinical toxicology studies for platinum anticancer drugs. Clin. Cancer Res. 1999, 5, 1161–1167. [Google Scholar]
- Paoloni, M.; Khanna, C. Translation of new cancer treatments from pet dogs to humans. Nat. Rev. Cancer 2008, 8, 147–156. [Google Scholar] [CrossRef]
- LeBlanc, A.K.; Mazcko, C.N.; Khanna, C. Defining the Value of a Comparative Approach to Cancer Drug Development. Clin. Cancer Res. 2016, 22, 2133–2138. [Google Scholar] [CrossRef]
- Lindblad-Toh, K.; Wade, C.M.; Mikkelsen, T.S.; Karlsson, E.K.; Jaffe, D.B.; Kamal, M.; Clamp, M.; Chang, J.L.; Kulbokas, E.J.; Zody, M.C.; et al. Genome sequence, comparative analysis and haplotype structure of the domestic dog. Nature 2005, 438, 803–819. [Google Scholar] [CrossRef]
- Hansen, K.; Khanna, C. Spontaneous and genetically engineered animal models; use in preclinical cancer drug development. Eur. J. Cancer 2004, 40, 858–880. [Google Scholar] [CrossRef]
- Olson, P.N. Using the canine genome to cure cancer and other diseases. Theriogenology 2007, 68, 378–381. [Google Scholar] [CrossRef]
- Lee, C.H.; Kim, W.H.; Lim, J.H.; Kang, M.S.; Kim, D.Y.; Kweon, O.K. Mutation and overexpression of p53 as a prognostic factor in canine mammary tumors. J. Vet. Sci. 2004, 5, 63–69. [Google Scholar] [CrossRef]
- Thomas, R.; Smith, K.C.; Ostrander, E.A.; Galibert, F.; Breen, M. Chromosome aberrations in canine multicentric lymphomas detected with comparative genomic hybridisation and a panel of single locus probes. Br. J. Cancer 2003, 89, 1530–1537. [Google Scholar] [CrossRef] [PubMed]
- Lingaas, F.; Comstock, K.E.; Kirkness, E.F.; Sorensen, A.; Aarskaug, T.; Hitte, C.; Nickerson, M.L.; Moe, L.; Schmidt, L.S.; Thomas, R.; et al. A mutation in the canine BHD gene is associated with hereditary multifocal renal cystadenocarcinoma and nodular dermatofibrosis in the German Shepherd dog. Hum. Mol. Genet. 2003, 12, 3043–3053. [Google Scholar] [CrossRef] [PubMed]
- Setoguchi, A.; Sakai, T.; Okuda, M.; Minehata, K.; Yazawa, M.; Ishizaka, T.; Watari, T.; Nishimura, R.; Sasaki, N.; Hasegawa, A.; et al. Aberrations of the p53 tumor suppressor gene in various tumors in dogs. Am. J. Vet. Res. 2001, 62, 433–439. [Google Scholar] [CrossRef] [PubMed]
- London, C.A.; Galli, S.J.; Yuuki, T.; Hu, Z.Q.; Helfand, S.C.; Geissler, E.N. Spontaneous canine mast cell tumors express tandem duplications in the proto-oncogene c-kit. Exp. Hematol. 1999, 27, 689–697. [Google Scholar] [CrossRef]
- Modiano, J.F.; Breen, M.; Burnett, R.C.; Parker, H.G.; Inusah, S.; Thomas, R.; Avery, P.R.; Lindblad-Toh, K.; Ostrander, E.A.; Cutter, G.C.; et al. Distinct B-cell and T-cell lymphoproliferative disease prevalence among dog breeds indicates heritable risk. Cancer Res. 2005, 65, 5654–5661. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.L.; Yu, V.C. Proteins of the bcl-2 family in apoptosis signalling: From mechanistic insights to therapeutic opportunities. Clin. Exp. Pharmacol. Physiol. 2004, 31, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Czabotar, P.E.; Lessene, G.; Strasser, A.; Adams, J.M. Control of apoptosis by the BCL-2 protein family: Implications for physiology and therapy. Nat. Rev. Mol. Cell Biol. 2014, 15, 49–63. [Google Scholar] [CrossRef]
- Shamas-Din, A.; Kale, J.; Leber, B.; Andrews, D.W. Mechanisms of action of Bcl-2 family proteins. Cold Spring Harb. Perspect. Biol. 2013, 5, a008714. [Google Scholar] [CrossRef]
- Kale, J.; Osterlund, E.J.; Andrews, D.W. BCL-2 family proteins: Changing partners in the dance towards death. Cell Death Differ. 2018, 25, 65–80. [Google Scholar] [CrossRef]
- Wu, X.; Zhang, L.S.; Toombs, J.; Kuo, Y.C.; Piazza, J.T.; Tuladhar, R.; Barrett, Q.; Fan, C.W.; Zhang, X.; Walensky, L.D.; et al. Extra-mitochondrial prosurvival BCL-2 proteins regulate gene transcription by inhibiting the SUFU tumour suppressor. Nat. Cell Biol. 2017, 19, 1226–1236. [Google Scholar] [CrossRef]
- Kim, H.; Rafiuddin-Shah, M.; Tu, H.C.; Jeffers, J.R.; Zambetti, G.P.; Hsieh, J.J.; Cheng, E.H. Hierarchical regulation of mitochondrion-dependent apoptosis by BCL-2 subfamilies. Nat. Cell Biol. 2006, 8, 1348–1358. [Google Scholar] [CrossRef] [PubMed]
- Cheng, E.H.; Wei, M.C.; Weiler, S.; Flavell, R.A.; Mak, T.W.; Lindsten, T.; Korsmeyer, S.J. BCL-2, BCL-X(L) sequester BH3 domain-only molecules preventing BAX- and BAK-mediated mitochondrial apoptosis. Mol. Cell 2001, 8, 705–711. [Google Scholar] [CrossRef]
- Miyashita, T.; Reed, J.C. Tumor suppressor p53 is a direct transcriptional activator of the human bax gene. Cell 1995, 80, 293–299. [Google Scholar] [PubMed]
- Garrido, C.; Galluzzi, L.; Brunet, M.; Puig, P.E.; Didelot, C.; Kroemer, G. Mechanisms of cytochrome c release from mitochondria. Cell Death Differ. 2006, 13, 1423–1433. [Google Scholar] [CrossRef] [PubMed]
- Elmore, S. Apoptosis: A review of programmed cell death. Toxicol. Pathol. 2007, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Boise, L.H.; Gonzalez-Garcia, M.; Postema, C.E.; Ding, L.; Lindsten, T.; Turka, L.A.; Mao, X.; Nunez, G.; Thompson, C.B. bcl-x, a bcl-2-related gene that functions as a dominant regulator of apoptotic cell death. Cell 1993, 74, 597–608. [Google Scholar] [CrossRef]
- Lee, E.F.; Fairlie, W.D. The Structural Biology of Bcl-xL. Int. J. Mol. Sci. 2019, 20, 2234. [Google Scholar] [CrossRef]
- Sano, J.; Oguma, K.; Kano, R.; Hsegawa, A. Canine Bcl-xL gene and its expression in tumor cell lines. J. Vet. Med. Sci. 2003, 65, 149–151. [Google Scholar] [CrossRef][Green Version]
- de Brot, S.; Schade, B.; Croci, M.; Dettwiler, M.; Guscetti, F. Sequence and partial functional analysis of canine Bcl-2 family proteins. Res. Vet. Sci. 2016, 104, 126–135. [Google Scholar] [CrossRef]
- Sano, J.; Nagafuchi, S.; Yamazaki, J.; Oguma, K.; Kano, R.; Hasegawa, A. Effect of antineoplastic drugs on the expression of Bcl-2 and Bcl-xL genes in the feline T-cell leukemia cell line. Res. Vet. Sci. 2005, 79, 197–201. [Google Scholar] [CrossRef]
- Kirito, K.; Watanabe, T.; Sawada, K.; Endo, H.; Ozawa, K.; Komatsu, N. Thrombopoietin regulates Bcl-xL gene expression through Stat5 and phosphatidylinositol 3-kinase activation pathways. J. Biol. Chem. 2002, 277, 8329–8337. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Benito, A.; Sanz, C.; Prosper, F.; Ekhterae, D.; Nunez, G.; Fernandez-Luna, J.L. Erythropoietin can induce the expression of bcl-x(L) through Stat5 in erythropoietin-dependent progenitor cell lines. J. Biol. Chem. 1999, 274, 22165–22169. [Google Scholar] [CrossRef] [PubMed]
- Masuda, A.; Matsuguchi, T.; Yamaki, K.; Hayakawa, T.; Yoshikai, Y. Interleukin-15 prevents mouse mast cell apoptosis through STAT6-mediated Bcl-xL expression. J. Biol. Chem. 2001, 276, 26107–26113. [Google Scholar] [CrossRef]
- Calo, V.; Migliavacca, M.; Bazan, V.; Macaluso, M.; Buscemi, M.; Gebbia, N.; Russo, A. STAT proteins: From normal control of cellular events to tumorigenesis. J. Cell. Physiol. 2003, 197, 157–168. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.; Baltimore, D. Circuitry of nuclear factor kappaB signaling. Immunol. Rev. 2006, 210, 171–186. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Dadgostar, H.; Cheng, Q.; Shu, J.; Cheng, G. NF-kappaB-mediated up-regulation of Bcl-x and Bfl-1/A1 is required for CD40 survival signaling in B lymphocytes. Proc. Natl. Acad. Sci. USA 1999, 96, 9136–9141. [Google Scholar] [CrossRef] [PubMed]
- Tamatani, M.; Che, Y.H.; Matsuzaki, H.; Ogawa, S.; Okado, H.; Miyake, S.; Mizuno, T.; Tohyama, M. Tumor necrosis factor induces Bcl-2 and Bcl-x expression through NFkappaB activation in primary hippocampal neurons. J. Biol. Chem. 1999, 274, 8531–8538. [Google Scholar] [CrossRef]
- Chen, C.; Edelstein, L.C.; Gelinas, C. The Rel/NF-kappaB family directly activates expression of the apoptosis inhibitor Bcl-x(L). Mol. Cell Biol. 2000, 20, 2687–2695. [Google Scholar] [CrossRef]
- Kharbanda, S.; Saxena, S.; Yoshida, K.; Pandey, P.; Kaneki, M.; Wang, Q.; Cheng, K.; Chen, Y.N.; Campbell, A.; Sudha, T.; et al. Translocation of SAPK/JNK to mitochondria and interaction with Bcl-x(L) in response to DNA damage. J. Biol. Chem. 2000, 275, 322–327. [Google Scholar] [CrossRef]
- Sedlak, T.W.; Oltvai, Z.N.; Yang, E.; Wang, K.; Boise, L.H.; Thompson, C.B.; Korsmeyer, S.J. Multiple Bcl-2 family members demonstrate selective dimerizations with Bax. Proc. Natl. Acad. Sci. USA 1995, 92, 7834–7838. [Google Scholar] [CrossRef]
- Sattler, M.; Liang, H.; Nettesheim, D.; Meadows, R.P.; Harlan, J.E.; Eberstadt, M.; Yoon, H.S.; Shuker, S.B.; Chang, B.S.; Minn, A.J.; et al. Structure of Bcl-xL-Bak peptide complex: Recognition between regulators of apoptosis. Science 1997, 275, 983–986. [Google Scholar] [CrossRef] [PubMed]
- Pecot, J.; Maillet, L.; Le Pen, J.; Vuillier, C.; Trecesson, S.C.; Fetiveau, A.; Sarosiek, K.A.; Bock, F.J.; Braun, F.; Letai, A.; et al. Tight Sequestration of BH3 Proteins by BCL-xL at Subcellular Membranes Contributes to Apoptotic Resistance. Cell Rep. 2016, 17, 3347–3358. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Dai, S.; Zhu, Y.; Marrack, P.; Kappler, J.W. The structure of a Bcl-xL/Bim fragment complex: Implications for Bim function. Immunity 2003, 19, 341–352. [Google Scholar] [CrossRef]
- Rajan, S.; Choi, M.; Baek, K.; Yoon, H.S. Bh3 induced conformational changes in Bcl-Xl revealed by crystal structure and comparative analysis. Proteins 2015, 83, 1262–1272. [Google Scholar] [CrossRef]
- Chen, H.C.; Kanai, M.; Inoue-Yamauchi, A.; Tu, H.C.; Huang, Y.; Ren, D.; Kim, H.; Takeda, S.; Reyna, D.E.; Chan, P.M.; et al. An interconnected hierarchical model of cell death regulation by the BCL-2 family. Nat. Cell Biol. 2015, 17, 1270–1281. [Google Scholar] [CrossRef]
- Chipuk, J.E.; Kuwana, T.; Bouchier-Hayes, L.; Droin, N.M.; Newmeyer, D.D.; Schuler, M.; Green, D.R. Direct activation of Bax by p53 mediates mitochondrial membrane permeabilization and apoptosis. Science 2004, 303, 1010–1014. [Google Scholar] [CrossRef]
- Bharatham, N.; Chi, S.W.; Yoon, H.S. Molecular basis of Bcl-X(L)-p53 interaction: Insights from molecular dynamics simulations. PLoS ONE 2011, 6, e26014. [Google Scholar] [CrossRef]
- Chipuk, J.E.; Bouchier-Hayes, L.; Kuwana, T.; Newmeyer, D.D.; Green, D.R. PUMA couples the nuclear and cytoplasmic proapoptotic function of p53. Science 2005, 309, 1732–1735. [Google Scholar] [CrossRef]
- Clem, R.J.; Cheng, E.H.; Karp, C.L.; Kirsch, D.G.; Ueno, K.; Takahashi, A.; Kastan, M.B.; Griffin, D.E.; Earnshaw, W.C.; Veliuona, M.A.; et al. Modulation of cell death by Bcl-XL through caspase interaction. Proc. Natl. Acad. Sci. USA 1998, 95, 554–559. [Google Scholar] [CrossRef]
- White, C.; Li, C.; Yang, J.; Petrenko, N.B.; Madesh, M.; Thompson, C.B.; Foskett, J.K. The endoplasmic reticulum gateway to apoptosis by Bcl-X(L) modulation of the InsP3R. Nat. Cell Biol. 2005, 7, 1021–1028. [Google Scholar] [CrossRef]
- Vervliet, T.; Lemmens, I.; Vandermarliere, E.; Decrock, E.; Ivanova, H.; Monaco, G.; Sorrentino, V.; Nadif Kasri, N.; Missiaen, L.; Martens, L.; et al. Ryanodine receptors are targeted by anti-apoptotic Bcl-XL involving its BH4 domain and Lys87 from its BH3 domain. Sci. Rep. 2015, 5, 9641. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Vais, H.; Gu, W.; Foskett, J.K. Biphasic regulation of InsP3 receptor gating by dual Ca2+ release channel BH3-like domains mediates Bcl-xL control of cell viability. Proc. Natl. Acad. Sci. USA 2016, 113, 14. [Google Scholar] [CrossRef] [PubMed]
- Monaco, G.; Decrock, E.; Arbel, N.; van Vliet, A.R.; La Rovere, R.M.; De Smedt, H.; Parys, J.B.; Agostinis, P.; Leybaert, L.; Shoshan-Barmatz, V.; et al. The BH4 domain of anti-apoptotic Bcl-XL, but not that of the related Bcl-2, limits the voltage-dependent anion channel 1 (VDAC1)-mediated transfer of pro-apoptotic Ca2+ signals to mitochondria. J. Biol. Chem. 2015, 290, 9150–9161. [Google Scholar] [CrossRef] [PubMed]
- Stoica, G.; Kim, H.T.; Hall, D.G.; Coates, J.R. Morphology, immunohistochemistry, and genetic alterations in dog astrocytomas. Vet. Pathol. 2004, 41, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Ide, T.; Uchida, K.; Kikuta, F.; Suzuki, K.; Nakayama, H. Immunohistochemical characterization of canine neuroepithelial tumors. Vet. Pathol. 2010, 47, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, F.; Kano, R.; Sano, J.; Oguma, K.; Hasegawa, A. Apoptosis of canine mammary tumor cells induced by small interfering RNA (siRNA) against Bcl-xL gene. J. Vet. Med. Sci. 2006, 68, 1199–1201. [Google Scholar] [CrossRef]
- Nagamatsu, K.; Tsuchiya, F.; Oguma, K.; Maruyama, H.; Kano, R.; Hasegawa, A. The effect of small interfering RNA (siRNA) against the Bcl-2 gene on apoptosis and chemosensitivity in a canine mammary gland tumor cell line. Res. Vet. Sci. 2008, 84, 49–55. [Google Scholar] [CrossRef]
- Misdorp, W. Mast cells and canine mast cell tumours. A review. Vet. Q. 2004, 26, 156–169. [Google Scholar] [CrossRef]
- Peter, B.; Cerny-Reiterer, S.; Hadzijusufovic, E.; Schuch, K.; Stefanzl, G.; Eisenwort, G.; Gleixner, K.V.; Hoermann, G.; Mayerhofer, M.; Kundi, M.; et al. The pan-Bcl-2 blocker obatoclax promotes the expression of Puma, Noxa, and Bim mRNA and induces apoptosis in neoplastic mast cells. J. Leukoc. Biol. 2014, 95, 95–104. [Google Scholar] [CrossRef]
- Alizadeh, B.H.; Foroumadi, A.; Emami, S.; Khoobi, M.; Panah, F.; Ardestani, S.K.; Shafiee, A. Isochaihulactone analogues: Synthesis and anti-proliferative activity of novel dibenzylbutyrolactones. Eur J. Med. Chem. 2010, 45, 5979–5984. [Google Scholar] [CrossRef]
- Makela, T.H.; Kaltia, S.A.; Wahala, K.T.; Hase, T.A. alpha,beta-Dibenzyl-gamma-butyrolactone lignan alcohols: Total synthesis of (+/-)-7′-hydroxyenterolactone, (+/-)-7′-hydroxymatairesinol and (+/-)-8-hydroxyenterolactone. Steroids 2001, 66, 777–784. [Google Scholar] [CrossRef]
- Fatima, A.; Kohn, L.K.; Carvalho, J.E.; Pilli, R.A. Cytotoxic activity of (S)-goniothalamin and analogues against human cancer cells. Bioorg. Med. Chem. 2006, 14, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Benedekovic, G.; Popsavin, M.; Francuz, J.; Kovacevic, I.; Kojic, V.; Bogdanovic, G.; Divjakovic, V.; Popsavin, V. Design, synthesis and SAR analysis of antitumour styryl lactones related to (+)-crassalactones B and C. Eur. J. Med. Chem. 2014, 87, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, A.; Koszuk, J.F.; Modranka, J.; Rozalski, M.; Krajewska, U.; Janecka, A.; Studzian, K.; Janecki, T. Synthesis and cytotoxic activity of gamma-aryl substituted alpha-alkylidene-gamma-lactones and alpha-alkylidene-gamma-lactams. Bioorg. Med. Chem. 2008, 16, 4872–4882. [Google Scholar] [CrossRef]
- Albrecht, L.; Wojciechowski, J.; Albrecht, A.; Wolf, W.; Janecka, A.; Studzian, K.; Krajewska, U.; Rozalski, M.; Janecki, T.; Krawczyk, H. Synthesis and cytotoxic evaluation of b-alkyl or b-aryl-d-methyl-a-methylene-d-lactones. Comparison with the corresponding g-lactones. Eur. J. Med. Chem. 2010, 45, 710–718. [Google Scholar] [CrossRef]
- Wzorek, A.; Gawdzik, B.; Gładkowski, W.; Urbaniak, M.; Barańska, A.; Malińska, M.; Woźniak, K.; Kempińska, K.; Wietrzyk, J. Synthesis, characterization and antiproliferative activity of β-aryl-δ-iodo-γ-lactones. J. Mol. Struct. 2013, 1047, 160–168. [Google Scholar] [CrossRef]
- Pawlak, A.; Gładkowski, W.; Kutkowska, J.; Mazur, M.; Obmińska-Mrukowicz, B.; Rapak, A. Enantiomeric trans β-aryl-δ-iodo-γ-lactones derived from 2,5-dimethylbenzaldehyde induce apoptosis in canine lymphoma cell lines by downregulation of anti-apoptotic Bcl-2 family members Bcl-xL and Bcl-2. Bioorg. Med. Chem. Lett. 2018, 28, 1171–1177. [Google Scholar] [CrossRef]
- Henklewska, M.; Pawlak, A.; Kutkowska, J.; Pruchnik, H.; Rapak, A.; Obminska-Mrukowicz, B. In vitro effects of the activity of novel platinum (II) complex in canine and human cell lines. Vet. Comp. Oncol. 2019, 17, 497–506. [Google Scholar] [CrossRef]
- Villedieu, M.; Louis, M.H.; Dutoit, S.; Brotin, E.; Lincet, H.; Duigou, F.; Staedel, C.; Gauduchon, P.; Poulain, L. Absence of Bcl-xL down-regulation in response to cisplatin is associated with chemoresistance in ovarian carcinoma cells. Gynecol. Oncol. 2007, 105, 31–44. [Google Scholar] [CrossRef]
- Galluzzi, L.; Senovilla, L.; Vitale, I.; Michels, J.; Martins, I.; Kepp, O.; Castedo, M.; Kroemer, G. Molecular mechanisms of cisplatin resistance. Oncogene 2012, 31, 1869–1883. [Google Scholar] [CrossRef]
- Pawlak, A.; De Miguel, D.; Kutkowska, J.; Obmińska-Mrukowicz, B.O.; Rapak, A.; Lostao, L.M. Flavopiridol Strongly Sensitizes Canine Lymphoma Cells to TRAIL-induced Apoptosis. Anticancer Res. 2017, 37, 6655–6665. [Google Scholar] [PubMed]
- Rosato, R.R.; Almenara, J.A.; Coe, S.; Grant, S. The multikinase inhibitor sorafenib potentiates TRAIL lethality in human leukemia cells in association with Mcl-1 and cFLIPL down-regulation. Cancer Res. 2007, 67, 9490–9500. [Google Scholar] [CrossRef] [PubMed]
- Fandy, T.E.; Ross, D.D.; Gore, S.D.; Srivastava, R.K. Flavopiridol synergizes TRAIL cytotoxicity by downregulation of FLIPL. Cancer Chemother. Pharmacol. 2007, 60, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Miyashita, K.; Shiraki, K.; Fuke, H.; Inoue, T.; Yamanaka, Y.; Yamaguchi, Y.; Yamamoto, N.; Ito, K.; Sugimoto, K.; Nakano, T. The cyclin-dependent kinase inhibitor flavopiridol sensitizes human hepatocellular carcinoma cells to TRAIL-induced apoptosis. Int. J. Mol. Med. 2006, 18, 249–256. [Google Scholar] [CrossRef][Green Version]
- Palacios, C.; Yerbes, R.; Lopez-Rivas, A. Flavopiridol induces cellular FLICE-inhibitory protein degradation by the proteasome and promotes TRAIL-induced early signaling and apoptosis in breast tumor cells. Cancer Res. 2006, 66, 8858–8869. [Google Scholar] [CrossRef]
- Dolka, I.; Krol, M.; Sapierzynski, R. Evaluation of apoptosis-associated protein (Bcl-2, Bax, cleaved caspase-3 and p53) expression in canine mammary tumors: An immunohistochemical and prognostic study. Res. Vet. Sci. 2016, 105, 124–133. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pawlak, A.; Henklewska, M. The Role of Bcl-xL Protein Research in Veterinary Oncology. Int. J. Mol. Sci. 2020, 21, 2511. https://doi.org/10.3390/ijms21072511
Pawlak A, Henklewska M. The Role of Bcl-xL Protein Research in Veterinary Oncology. International Journal of Molecular Sciences. 2020; 21(7):2511. https://doi.org/10.3390/ijms21072511
Chicago/Turabian StylePawlak, Aleksandra, and Marta Henklewska. 2020. "The Role of Bcl-xL Protein Research in Veterinary Oncology" International Journal of Molecular Sciences 21, no. 7: 2511. https://doi.org/10.3390/ijms21072511
APA StylePawlak, A., & Henklewska, M. (2020). The Role of Bcl-xL Protein Research in Veterinary Oncology. International Journal of Molecular Sciences, 21(7), 2511. https://doi.org/10.3390/ijms21072511




