Noninvasive Biological Samples to Detect and Diagnose Infections due to Trypanosomatidae Parasites: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Results and Discussion
2.1. Study Selection
2.2. Systematic Review of Non-Invasive Sampling Strategies for the Diagnosis and Detection of Trypanosomatid Pathogens and Infections
2.2.1. Urine
2.2.2. Feces
2.2.3. Saliva/Oral Swab/Sputum
2.2.4. Conjunctival Swab/Lacrimal Fluid/Occular
2.2.5. Genital Organs: Semen/Vulvular Secretion
2.2.6. Milk
2.2.7. Nasal Secretion
2.2.8. Ear Swab/Cerumen
2.2.9. Hair/Bristles
2.3. Meta-Analysis of Non-Invasive Sampling Methodologies for Trypanosomatid Infection Diagnosis: Overview and Limitations
2.3.1. Urine
2.3.2. Feces
2.3.3. Saliva/Oral Swab/Sputum
2.3.4. Conjunctival Swab/Lacrimal Fluid
2.3.5. Genital Organs: Semen/Vulvular Secretions
2.3.6. Milk
2.3.7. Nasal Secretion
2.3.8. Hair/bristles
3. Materials and Methods
3.1. Protocol and Registration
3.2. Information Source
3.3. Search
- “Leishmania”,
- “Leishmaniasis”,
- “Trypanosoma”,
- “Trypanosomiasis”, and
- “Chagas disease”,
- 6.
- “urine”,
- 7.
- “lacrimal”,
- 8.
- “conjunctival”,
- 9.
- “ocular”,
- 10.
- “eyes”,
- 11.
- “saliva”,
- 12.
- “sputum”,
- 13.
- “oral swab”,
- 14.
- “ear swab”,
- 15.
- “buccal swab”,
- 16.
- “cerumen”,
- 17.
- “semen”,
- 18.
- “vulvular”,
- 19.
- “feces”, “fecal”,
- 20.
- “hair”,
- 21.
- “skin”,
- 22.
- “nasal swab”,
- 23.
- “nostril”,
- 24.
- “pharyngeal”,
- 25.
- “mucosal”,
- 26.
- “milk”, and
- 27.
- “sweat”.
3.4. Study Selection
- 1-
- Leishmaniases, Chagas disease, or trypanosomiases
- 2-
- Identification and/or diagnosis with molecular, immunological, or parasitological methods
- 3-
- Experimentally or naturally acquired infection.
3.5. Data Collection Process and Items
3.6. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| HAT | Human African Trypanosomiasis |
| CD | Chagas disease |
| AT | Animal Trypanosomiasis |
| AAT | African Animal Trypanosomiasis |
| CVL | Canine visceral leihmaniasis |
References
- Simpson, A.G.B.; Stevens, J.R.; Lukeš, J. The evolution and diversity of kinetoplastid flagellates. Trends Parasitol. 2006, 22, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Brun, R.; Blum, J.; Chappuis, F.; Burri, C. Human African trypanosomiasis. Lancet 2010, 375, 148–159. [Google Scholar] [CrossRef]
- Wang, Y.; Utzinger, J.; Saric, J.; Li, J.V.; Burckhardt, J.; Dirnhofer, S.; Nicholson, J.K.; Singer, B.H.; Brun, R.; Holmes, E. Global metabolic responses of mice to Trypanosoma brucei brucei infection. Proc. Natl. Acad. Sci. USA 2008, 105, 6127–6132. [Google Scholar] [CrossRef] [PubMed]
- Akhoundi, M.; Kuhls, K.; Cannet, A.; Votýpka, J.; Marty, P.; Delaunay, P.; Sereno, D. A Historical Overview of the Classification, Evolution, and Dispersion of Leishmania Parasites and Sandflies. PLoS Negl. Trop. Dis. 2016, 10, e0004349. [Google Scholar] [CrossRef] [PubMed]
- Sereno, D. Leishmania (Mundinia) spp.: From description to emergence as new human and animal Leishmania pathogens. New Microbes New Infect. 2019, 30, 100540. [Google Scholar] [CrossRef] [PubMed]
- Truc, P.; Büscher, P.; Cuny, G.; Gonzatti, M.I.; Jannin, J.; Joshi, P.; Juyal, P.; Lun, Z.-R.; Mattioli, R.; Pays, E.; et al. Atypical human infections by animal trypanosomes. PLoS Negl. Trop. Dis. 2013, 7, e2256. [Google Scholar] [CrossRef]
- Ebhodaghe, F.; Ohiolei, J.A.; Isaac, C. A systematic review and meta-analysis of small ruminant and porcine trypanosomiasis prevalence in sub-Saharan Africa (1986 to 2018). Acta Trop. 2018, 188, 118–131. [Google Scholar] [CrossRef]
- Ebhodaghe, F.; Isaac, C.; Ohiolei, J.A. A meta-analysis of the prevalence of bovine trypanosomiasis in some African countries from 2000 to 2018. Prev. Vet. Med. 2018, 160, 35–46. [Google Scholar] [CrossRef]
- Stuart, K.; Brun, R.; Croft, S.; Fairlamb, A.; Gürtler, R.E.; McKerrow, J.; Reed, S.; Tarleton, R. Kinetoplastids: Related protozoan pathogens, different diseases. J. Clin. Investig. 2008, 118, 1301–1310. [Google Scholar] [CrossRef]
- Silva, F.L.; Oliveira, R.G.; Silva, T.M.A.; Xavier, M.N.; Nascimento, E.F.; Santos, R.L. Venereal transmission of canine visceral leishmaniasis. Vet. Parasitol. 2009, 160, 55–59. [Google Scholar] [CrossRef]
- de Oliveira, V.V.G.; Alves, L.C.; da Silva Junior, V.A. Transmission routes of visceral leishmaniasis in mammals. Ciênc. Rural 2015, 45, 1622–1628. [Google Scholar] [CrossRef]
- Turchetti, A.P.; Souza, T.D.; Paixão, T.A.; Santos, R.L. Sexual and vertical transmission of visceral leishmaniasis. J. Infect. Dev. Ctries. 2014, 8, 403–407. [Google Scholar] [CrossRef] [PubMed]
- SYMMERS, W.S. Leishmaniasis acquired by contagion: A case of marital infection in Britain. Lancet 1960, 1, 127–132. [Google Scholar] [CrossRef]
- Bosch, R.J.; Rodrigo, A.B.; Sánchez, P.; de Gálvez, M.V.; Herrera, E. Presence of Leishmania organisms in specific and non-specific skin lesions in HIV-infected individuals with visceral leishmaniasis. Int. J. Dermatol. 2002, 41, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Owens, S.D.; Oakley, D.A.; Marryott, K.; Hatchett, W.; Walton, R.; Nolan, T.J.; Newton, A.; Steurer, F.; Schantz, P.; Giger, U. Transmission of visceral leishmaniasis through blood transfusions from infected English foxhounds to anemic dogs. J. Am. Vet. Med. Assoc. 2001, 219, 1076–1083. [Google Scholar] [CrossRef]
- Boehme, C.C.; Hain, U.; Novosel, A.; Eichenlaub, S.; Fleischmann, E.; Löscher, T. Congenital visceral leishmaniasis. Emerg. Infect. Dis. 2006, 12, 359–360. [Google Scholar] [CrossRef]
- Low, G.; Edin, M.; Lond, F.; Cooke, W.; Irel, F. A congenital case of Kala-azar. Lancet 1926, 13, 1209–1211. [Google Scholar] [CrossRef]
- Alvar, J.; Vélez, I.D.; Bern, C.; Herrero, M.; Desjeux, P.; Cano, J.; Jannin, J.; den Boer, M. WHO Leishmaniasis Control Team Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 2012, 7, e35671. [Google Scholar] [CrossRef]
- Burza, S.; Croft, S.L.; Boelaert, M. Leishmaniasis. Lancet 2018, 392, 951–970. [Google Scholar] [CrossRef]
- Eddaikra, N.; Kherachi Djenad, I.; Benbetka, S.; Benikhlef, R.; Aït-Oudhia, K.; Moulti-Mati, F.; Oury, B.; Sereno, D.; Harrat, Z. Development of a Murine Infection Model with Leishmania killicki, Responsible for Cutaneous Leishmaniosis in Algeria: Application in Pharmacology. BioMed Res. Int. 2016, 2016. [Google Scholar] [CrossRef]
- Ostyn, B.; Gidwani, K.; Khanal, B.; Picado, A.; Chappuis, F.; Singh, S.P.; Rijal, S.; Sundar, S.; Boelaert, M. Incidence of symptomatic and asymptomatic Leishmania donovani infections in high-endemic foci in India and Nepal: A prospective study. PLoS Negl. Trop. Dis. 2011, 5, e1284. [Google Scholar] [CrossRef] [PubMed]
- Silveira, F.T.; Lainson, R.; Crescente, J.A.; de Souza, A.A.A.; Campos, M.B.; Gomes, C.M.C.; Laurenti, M.D.; Corbett, C.E.P. A prospective study on the dynamics of the clinical and immunological evolution of human Leishmania (L.) infantum chagasi infection in the Brazilian Amazon region. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Travi, B.L.; Cordeiro-da-Silva, A.; Dantas-Torres, F.; Miró, G. Canine visceral leishmaniasis: Diagnosis and management of the reservoir living among us. PLoS Negl. Trop. Dis. 2018, 12, e0006082. [Google Scholar] [CrossRef] [PubMed]
- Roura, X.; Fondati, A.; Lubas, G.; Gradoni, L.; Maroli, M.; Oliva, G.; Paltrinieri, S.; Zatelli, A.; Zini, E. Prognosis and monitoring of leishmaniasis in dogs: A working group report. Vet. J. 2013, 198, 43–47. [Google Scholar] [CrossRef]
- Peña, M.T.; Naranjo, C.; Klauss, G.; Fondevila, D.; Leiva, M.; Roura, X.; Davidson, M.G.; Dubielzig, R.R. Histopathological features of ocular leishmaniosis in the dog. J. Comp. Pathol. 2008, 138, 32–39. [Google Scholar] [CrossRef]
- Pérez-Molina, J.A.; Norman, F.; López-Vélez, R. Chagas disease in non-endemic countries: epidemiology, clinical presentation and treatment. Curr. Infect. Dis. Rep. 2012, 14, 263–274. [Google Scholar] [CrossRef]
- Pérez-Molina, J.A.; Molina, I. Chagas disease. Lancet (Lond. Engl.) 2018, 391, 82–94. [Google Scholar] [CrossRef]
- Arnal, A.; Waleckx, E.; Rico-Chávez, O.; Herrera, C.; Dumonteil, E. Estimating the current burden of Chagas disease in Mexico: A systematic review and meta-analysis of epidemiological surveys from 2006 to 2017. PLoS Negl. Trop. Dis. 2019, 13, e0006859. [Google Scholar] [CrossRef]
- Silva-Dos-Santos, D.; Barreto-de-Albuquerque, J.; Guerra, B.; Moreira, O.C.; Berbert, L.R.; Ramos, M.T.; Mascarenhas, B.A.S.; Britto, C.; Morrot, A.; Serra Villa-Verde, D.M.; et al. Unraveling Chagas disease transmission through the oral route: Gateways to Trypanosoma cruzi infection and target tissues. PLoS Negl. Trop. Dis. 2017, 11, e0005507. [Google Scholar] [CrossRef]
- Breniere, S.-F.; Waleckx, E.; Aznar, C. American Trypanosomiasis (Chagas Disease), One Hundred Years of Research, 2nd ed.; Telleria, J., Tibayrenc, M., Eds.; Elservier INC: Amsterdam, The Netherlands, 2017; pp. 561–578. [Google Scholar]
- Jardim, E.; Takayanagui, O.M. Chagasic meningoencephalitis with detection of Trypanosoma cruzi in the cerebrospinal fluid of an immunodepressed patient. J. Trop. Med. Hyg. 1994, 97, 367–370. [Google Scholar]
- Diazgranados, C.A.; Saavedra-Trujillo, C.H.; Mantilla, M.; Valderrama, S.L.; Alquichire, C.; Franco-Paredes, C. Chagasic encephalitis in HIV patients: Common presentation of an evolving epidemiological and clinical association. Lancet. Infect. Dis. 2009, 9, 324–330. [Google Scholar] [CrossRef]
- Junqueira, C.; Caetano, B.; Bartholomeu, D.C.; Melo, M.B.; Ropert, C.; Rodrigues, M.M.; Gazzinelli, R.T. The endless race between Trypanosoma cruzi and host immunity: Lessons for and beyond Chagas disease. Expert. Rev. Mol. Med. 2010, 12, e29. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, A.R.; Figueiredo, F.; Rezende Filho, J.; Macêdo, V. Chagas’ disease: A clinical, parasitological, immunological, and pathological study in rabbits. Am. J. Trop. Med. Hyg. 1983, 32, 258–272. [Google Scholar] [CrossRef]
- Bey, E.; Paucara Condori, M.B.; Gaget, O.; Solano, P.; Revollo, S.; Saussine, C.; Brenière, S.F. Lower urinary tract dysfunction in chronic Chagas disease: Clinical and urodynamic presentation. World J. Urol. 2018, 37, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- da Silva Junior, G.B.; Amélia Reis Jereissati, A.; Karoline Medina Neri, A.; da Costa Lino, D.O.; de Oliveira, J.G.R.; De Francesco Daher, E. Neglected Tropical Diseases with an Impact on Kidney Function. IntechOpen 2018. [Google Scholar] [CrossRef]
- da Silva Junior, G.B.; Antunes, V.V.H.; Motta, M.; Barros, E.J.G.; Daher, E.D.F. Chagas disease-associated kidney injury – A review. Nefrol. Latinoam. 2017, 14, 22–26. [Google Scholar] [CrossRef]
- Riganti, J.; Maqueda, M.G.; Piñero, M.C.B.; Volonteri, V.I.; Galimberti, R.L. Reactivation of Chagas’ disease: cutaneous manifestations in two immunosuppressed patients. Int. J. Dermatol. 2012, 51, 829–834. [Google Scholar] [CrossRef]
- Franco, J.R.; Simarro, P.P.; Diarra, A.; Jannin, J.G. Epidemiology of human African trypanosomiasis. Clin. Epidemiol. 2014, 6, 257–275. [Google Scholar]
- Dumas, M.; Bouteille, B. Human African trypanosomiasis: Present and future treatment. Bull. Soc. Pathol. Exot. 2002, 95, 341–344. [Google Scholar]
- Dumas, M.; Bouteille, B. Current status of trypanosomiasis. Med. Trop. 1997, 57, 65–69. [Google Scholar]
- Atouguia, J.L.M.; Kennedy, P. Neurological aspects of human African trypanosomiasis. In Infectious Diseases of the Nervous System; Le, D., Pge, K., Eds.; Butterwort: Oxford, UK, 2000. [Google Scholar]
- Duggan, A.J.; Hutchinson, M.P. Sleeping sickness in Europeans: A review of 109 cases. J. Trop. Med. Hyg. 1966, 69, 124–131. [Google Scholar]
- Collomb, H.; Bartoli, D. The heart in human African trypanosomiasis caused by Trypanosoma gambiense. Bull. Soc. Pathol. Exot. Filiales 1967, 60, 142–156. [Google Scholar] [PubMed]
- Collomb, H.; Bartoli, D.; Ayats, H.; Koate, P. Cardiac disorders in human African trypanosomiasis due to Trypanosoma gambiense. Bull. Soc. Med. Afr. Noire Lang. Fr. 1968, 13, 337–339. [Google Scholar] [PubMed]
- Poltera, A.A.; Cox, J.N.; Owor, R. Cardiac valvulitis in human African trypanosomiasis. East Afr. Med. J. 1977, 54, 497–499. [Google Scholar] [PubMed]
- Poltera, A.A.; Cox, J.N.; Owor, R. African human trypanosomal pancarditis involving the conduting system and all valves. Pathol. Microbiol. 1975, 43, 117–119. [Google Scholar]
- Poltera, A.A.; Cox, J.N. Pancarditis with valvulitis in endomyocardial fibrosis (=emf) and in human African trypanosomiasis (= hat). A comparative histological study of four Ugandan cases. Virchows Arch. A 1977, 375, 53–70. [Google Scholar] [CrossRef]
- Dwinger, R.H.; Rudin, W.; Moloo, S.K.; Murray, M. Development of Trypanosoma congolense, T vivax and T brucei in the skin reaction induced in goats by infected Glossina morsitans centralis: A light and electron microscopical study. Res. Vet. Sci. 1988, 44, 154–163. [Google Scholar] [CrossRef]
- McGovern, T.W.; Williams, W.; Fitzpatrick, J.E.; Cetron, M.S.; Hepburn, B.C.; Gentry, R.H. Cutaneous manifestations of African trypanosomiasis. Arch. Dermatol. 1995, 131, 1178–1182. [Google Scholar] [CrossRef]
- Tatibouet, M.H.; Gentilini, M.; Brucker, G. Cutaneous lesions in human African trypanosomiasis. Sem. Hop. 1982, 58, 2318–2324. [Google Scholar]
- Capewell, P.; Cren-Travaillé, C.; Marchesi, F.; Johnston, P.; Clucas, C.; Benson, R.A.; Gorman, T.-A.; Calvo-Alvarez, E.; Crouzols, A.; Jouvion, G.; et al. The skin is a significant but overlooked anatomical reservoir for vector-borne African trypanosomes. Elife 2016, 5, e17716. [Google Scholar] [CrossRef]
- Caljon, G.; Van Reet, N.; De Trez, C.; Vermeersch, M.; Pérez-Morga, D.; Van Den Abbeele, J. The Dermis as a Delivery Site of Trypanosoma brucei for Tsetse Flies. PLoS Pathog. 2016, 12, e1005744. [Google Scholar] [CrossRef] [PubMed]
- Büscher, P.; Gonzatti, M.I.; Hébert, L.; Inoue, N.; Pascucci, I.; Schnaufer, A.; Suganuma, K.; Touratier, L.; Van Reet, N. Equine trypanosomosis: Enigmas and diagnostic challenges. Parasit. Vectors 2019, 12, 234. [Google Scholar] [CrossRef] [PubMed]
- Raina, A.K.; Kumar, R.; Sridhar, V.R.; Singh, R.P. Oral transmission of Trypanosoma evansi infection in dogs and mice. Vet. Parasitol. 1985, 18, 67–69. [Google Scholar] [CrossRef]
- Sinha, P.K.; Mukherjee, G.S.; Das, M.S.; Lahiri, R.K. Outbreak of trypanosomiasis evansi amongst tigers and jaguars in the zoological garden, Calcutta. Indian Vet. J. 1971, 48, 306–310. [Google Scholar] [PubMed]
- Gibson, W. Molecular epidemiology of African trypanosomiasis: The contributions of David George Godfrey OBE to the biochemical characterization of trypanosomes. Parasite 2008, 15, 233–236. [Google Scholar] [CrossRef][Green Version]
- Auty, H.; Torr, S.J.; Michoel, T.; Jayaraman, S.; Morrison, L.J. Cattle trypanosomosis: The diversity of trypanosomes and implications for disease epidemiology and control. Rev. Sci. Tech. 2015, 34, 587–598. [Google Scholar] [CrossRef]
- Desquesnes, M.; Dia, M.L. Mechanical transmission of Trypanosoma congolense in cattle by the African tabanid Atylotus agrestis. Exp. Parasitol. 2003, 105, 226–231. [Google Scholar] [CrossRef]
- Morrison, L.J.; Vezza, L.; Rowan, T.; Hope, J.C. Animal African Trypanosomiasis: Time to Increase Focus on Clinically Relevant Parasite and Host Species. Trends Parasitol. 2016, 32, 599–607. [Google Scholar] [CrossRef]
- Cox, F.E.G. Pathogenesis of animal trypanosomiasis. Nature 1979, 277, 603–604. [Google Scholar] [CrossRef]
- Taylor, K.; Authié, E.M.L. Pathogenesis of animal trypanosomiasis. In The Trypanosomiases; Centre for Agriculture and Bioscience International: Wallingford, UK, 2004; pp. 331–353. [Google Scholar]
- Nasereddin, A.; Jaffe, C.L. Rapid diagnosis of Old World Leishmaniasis by high-resolution melting analysis of the 7SL RNA gene. J. Clin. Microbiol. 2010, 48, 2240–2242. [Google Scholar] [CrossRef]
- Higuera, S.L.; Guhl, F.; Ramírez, J.D. Identification of Trypanosoma cruzi discrete typing units (DTUs) through the implementation of a high-resolution melting (HRM) genotyping assay. Parasit. Vectors 2013, 6, 112. [Google Scholar] [CrossRef] [PubMed]
- Mugasa, C.M.; Laurent, T.; Schoone, G.J.; Basiye, F.L.; Saad, A.A.; El Safi, S.; Kager, P.A.; Schallig, H.D. Simplified molecular detection of Leishmania parasites in various clinical samples from patients with leishmaniasis. Parasit. Vectors 2010, 3, 13. [Google Scholar] [CrossRef] [PubMed]
- Deborggraeve, S.; Laurent, T.; Espinosa, D.; Van der Auwera, G.; Mbuchi, M.; Wasunna, M.; El-Safi, S.; Al-Basheer, A.A.; Arévalo, J.; Miranda-Verástegui, C.; et al. A simplified and standardized polymerase chain reaction format for the diagnosis of leishmaniasis. J. Infect. Dis. 2008, 198, 1565–1572. [Google Scholar] [CrossRef] [PubMed]
- Notomi, T.; Okayama, H.; Masubuchi, H.; Yonekawa, T.; Watanabe, K.; Amino, N.; Hase, T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000, 28, E63. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.G.M.; Bhaskar, K.R.H.; Salam, M.A.; Akther, T.; Pluschke, G.; Mondal, D. Diagnostic accuracy of loop-mediated isothermal amplification (LAMP) for detection of Leishmania DNA in buffy coat from visceral leishmaniasis patients. Parasit. Vectors 2012, 5, 280. [Google Scholar] [CrossRef] [PubMed]
- Kuboki, N.; Inoue, N.; Sakurai, T.; Di Cello, F.; Grab, D.J.; Suzuki, H.; Sugimoto, C.; Igarashi, I. Loop-mediated isothermal amplification for detection of African trypanosomes. J. Clin. Microbiol. 2003, 41, 5517–5524. [Google Scholar] [CrossRef]
- Fife, E.H.; Muschel, L.H. Fluorescent-antibody technic for serodiagnosis of Trypanosoma cruzi infection. Proc. Soc. Exp. Biol. Med. 1959, 101, 540–543. [Google Scholar] [CrossRef]
- Suter-Kopp, V.; Fricker, F. Indirect immunofluorescence method in sleeping sickness (T. rhodesiense) with Trypanosoma brucei as antigen. Acta Trop. 1972, 29, 200–204. [Google Scholar]
- Lanotte, G.; Rioux, J.A.; Croset, H.; Vollhardt, Y. Ecology of leishmaniasis in the south of France. 8. Complement to the epidemiological application of the immunofluorescence technic: Geometric and arithmetic mean titers in canine leighmaniasis. Ann. Parasitol. Hum. Comp. 1975, 50, 1–5. [Google Scholar] [CrossRef]
- Connor, R. The diagnosis, treatment and prevention of animal trypanosomiasis under field conditions. In Proceedings of the FAO Panel of Experts, Harare, Zimbabwe, 24–26 June 1991. [Google Scholar]
- Magnus, E.; Vervoort, T.; Van Meirvenne, N. A card-agglutination test with stained trypanosomes (C.A.T.T.) for the serological diagnosis of T. B. gambiense trypanosomiasis. Ann. Soc. Belg. Med. Trop. 1978, 58, 169–176. [Google Scholar]
- Da Silva, A.S.; da Krawczak, F.S.; Soares, J.F.; Klauck, V.; Pazinato, R.; Marcili, A.; Labruna, M.B. Seroprevalence of Trypanosoma evansi infection in capybaras (Hydrochoerus hydrochaeris) from a nonendemic area in Brazil. J. Vet. Diagn. Investig. 2016, 28, 171–174. [Google Scholar] [CrossRef]
- Attar, Z.J.; Chance, M.L.; El-Safi, S.; Carney, J.; Azazy, A.; El-Hadi, M.; Dourado, C.; Hommel, M. Latex agglutination test for the detection of urinary antigens in visceral leishmaniasis. Acta Trop. 2001, 78, 11–16. [Google Scholar] [CrossRef]
- Noyes, H.A.; Reyburn, H.; Bailey, J.W.; Smith, D. A nested-PCR-based schizodeme method for identifying Leishmania kinetoplast minicircle classes directly from clinical samples and its application to the study of the epidemiology of Leishmania tropica in Pakistan. J. Clin. Microbiol. 1998, 36, 2877–2881. [Google Scholar] [CrossRef] [PubMed]
- Desquesnes, M.; Dávila, A.M.R. Applications of PCR-based tools for detection and identification of animal trypanosomes: A review and perspectives. Vet. Parasitol. 2002, 109, 213–231. [Google Scholar] [CrossRef]
- Gibson, W. Species-specific probes for the identification of the African tsetse-transmitted trypanosomes. Parasitology 2009, 136, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Mugasa, C.M.; Laurent, T.; Schoone, G.J.; Kager, P.A.; Lubega, G.W.; Schallig, H.D.F.H. Nucleic acid sequence-based amplification with oligochromatography for detection of Trypanosoma brucei in clinical samples. J. Clin. Microbiol. 2009, 47, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Mugasa, C.M.; Deborggraeve, S.; Schoone, G.J.; Laurent, T.; Leeflang, M.M.; Ekangu, R.A.; El Safi, S.; Saad, A.A.; Basiye, F.L.; De Doncker, S.; et al. Accordance and concordance of PCR and NASBA followed by oligochromatography for the molecular diagnosis of Trypanosoma brucei and Leishmania. Trop. Med. Int. Health 2010, 15, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Masake, R.A.; Njuguna, J.T.; Brown, C.C.; Majiwa, P.A.O. The application of PCR-ELISA to the detection of Trypanosoma brucei and T. vivax infections in livestock. Vet. Parasitol. 2002, 105, 179–189. [Google Scholar] [CrossRef]
- De Doncker, S.; Hutse, V.; Abdellati, S.; Rijal, S.; Singh Karki, B.M.; Decuypere, S.; Jacquet, D.; Le Ray, D.; Boelaert, M.; Koirala, S.; et al. A new PCR-ELISA for diagnosis of visceral leishmaniasis in blood of HIV-negative subjects. Trans. R. Soc. Trop. Med. Hyg. 2005, 99, 25–31. [Google Scholar] [CrossRef]
- Cabrera, L.; De Witte, J.; Victor, B.; Vermeiren, L.; Zimic, M.; Brandt, J.; Geysen, D. Specific detection and identification of African trypanosomes in bovine peripheral blood by means of a PCR-ELISA assay. Vet. Parasitol. 2009, 164, 111–117. [Google Scholar] [CrossRef]
- Delespaux, V.; Ayral, F.; Geysen, D.; Geerts, S. PCR-RFLP using Ssu-rDNA amplification: Applicability for the diagnosis of mixed infections with different trypanosome species in cattle. Vet. Parasitol. 2003, 117, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Freitas, J.M.; Lages-Silva, E.; Crema, E.; Pena, S.D.J.; Macedo, A.M. Real time PCR strategy for the identification of major lineages of Trypanosoma cruzi directly in chronically infected human tissues. Int. J. Parasitol. 2005, 35, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Sá, A.R.N.; Kimoto, K.Y.; Steindel, M.; Grisard, E.C.; Gomes, M.L. Limit of detection of PCR/RFLP analysis of cytochrome oxidase II for the identification of genetic groups of Trypanosoma cruzi and Trypanosoma rangeli in biological material from vertebrate hosts. Parasitol. Res. 2018, 117, 2403–2410. [Google Scholar] [CrossRef] [PubMed]
- Akhoundi, M.; Downing, T.; Votýpka, J.; Kuhls, K.; Lukeš, J.; Cannet, A.; Ravel, C.; Marty, P.; Delaunay, P.; Kasbari, M.; et al. Leishmania infections: Molecular targets and diagnosis. Mol. Aspects Med. 2017, 57, 1–29. [Google Scholar] [CrossRef]
- Tilley, A.; Hide, G. Characterization of Trypanosoma brucei stocks using PCR-RFLP analysis of ribosomal internal transcribed spacers (IRT). Ann. Trop. Med. Parasitol. 2001, 95, 617–621. [Google Scholar] [CrossRef]
- Melville, S.E. Parasite genome analysis. Genome research in Trypanosoma brucei: Chromosome size polymorphism and its relevance to genome mapping and analysis. Trans. R. Soc. Trop. Med. Hyg. 1997, 91, 116–120. [Google Scholar] [CrossRef]
- Henriksson, J.; Aslund, L.; Macina, R.A.; de Cazzulo, B.M.F.; Cazzulo, J.J.; Frasch, A.C.; Pettersson, U. Chromosomal localization of seven cloned antigen genes provides evidence of diploidy and further demonstration of karyotype variability in Trypanosoma cruzi. Mol. Biochem. Parasitol. 1990, 42, 213–223. [Google Scholar] [CrossRef]
- Besuschio, S.A.; Llano Murcia, M.; Benatar, A.F.; Monnerat, S.; Cruz, I.; Picado, A.; Curto, M.d.L.Á.; Kubota, Y.; Wehrendt, D.P.; Pavia, P.; et al. Analytical sensitivity and specificity of a loop-mediated isothermal amplification (LAMP) kit prototype for detection of Trypanosoma cruzi DNA in human blood samples. PLoS Negl. Trop. Dis. 2017, 11, e0005779. [Google Scholar] [CrossRef]
- Frean, J.; Sieling, W.; Pahad, H.; Shoul, E.; Blumberg, L. Clinical management of East African trypanosomiasis in South Africa: Lessons learned. Int. J. Infect. Dis. 2018, 75, 101–108. [Google Scholar] [CrossRef]
- Brumpt, E. Le xénodiagnostic. Application au diagnostic de quelques infections parasitaires et en particulier à la Trypanosomose de Chagas. Bull. Soc. Pathol. Exot. 1914, 7, 706–710. [Google Scholar]
- Sadlova, J.; Seblova, V.; Votypka, J.; Warburg, A.; Volf, P. Xenodiagnosis of Leishmania donovani in BALB/c mice using Phlebotomus orientalis: A new laboratory model. Parasit. Vectors 2015, 8, 158. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, M.; Zulantay, I.; Apt, W.; Castillo, J.; Araya, E.; Martínez, G.; Rodríguez, J. Quantification by real-time PCR of Trypanosoma cruzi DNA in samples of Triatoma infestans used in xenodiagnosis of chronic Chagas disease patients. Parasit. Vectors 2016, 9, 382. [Google Scholar] [CrossRef] [PubMed]
- Frezil, J.L. Application of xenodiagnosis in the detection of T. gambiense trypanosomiasis in immunologically suspect patients. Bull. Soc. Pathol. Exot. Filiales 1971, 64, 871–878. [Google Scholar] [PubMed]
- Guedes, D.C.; Minozzo, J.C.; Pasquali, A.K.S.; Faulds, C.; Soccol, C.R.; Thomaz-Soccol, V. New strategy to improve quality control of Montenegro skin test at the production level. Rev. Soc. Bras. Med. Trop. 2017, 50, 788–794. [Google Scholar] [CrossRef]
- Sarkari, B.; Hatam, G.R.; Mikaeili, F.; Sadeghi, H.; Ebrahimi, S. A comparative study of antigen and antibody detection in visceral leishmaniasis using serum and urine-based ELISA. Trop. Biomed. 2008, 25, 96–99. [Google Scholar]
- Sguassero, Y.; Roberts, K.N.; Harvey, G.B.; Comandé, D.; Ciapponi, A.; Cuesta, C.B.; Aguiar, C.; de Castro, A.M.; Danesi, E.; de Andrade, A.L.; et al. Course of serological tests in treated subjects with chronic Trypanosoma cruzi infection: A systematic review and meta-analysis of individual participant data. Int. J. Infect. Dis. 2018, 73, 93–101. [Google Scholar] [CrossRef]
- Berrizbeitia, M.; Ndao, M.; Bubis, J.; Gottschalk, M.; Ache, A.; Lacouture, S.; Medina, M.; Ward, B.J. Purified Excreted-Secreted Antigens from Trypanosoma cruzi Trypomastigotes as Tools for Diagnosis of Chagas’ Disease. J. Clin. Microbiol. 2006, 44, 291–296. [Google Scholar] [CrossRef]
- Nantulya, V.M.; Lindqvist, K.J. Antigen-detection enzyme immunoassays for the diagnosis of Trypanosoma vivax, T. congolense and T. brucei infections in cattle. Trop. Med. Parasitol. 1989, 40, 267–272. [Google Scholar]
- Nozais, J.P.; Giordano, C.; Doucet, J.; Bertrand, E. Value of indirect immunofluorescence in the diagnosis of “Trypanosoma gambiense” trypanosomiasis. 46 cases (author’s translation). Bull. Soc. Pathol. Exot. Filiales 1975, 68, 390–398. [Google Scholar]
- Frezil, J.; Louembet, M.; Alary, J. L’antigène “Trypanosoma gambiense” dans la réaction d’immunofluorescence indirecte. Cah. ORSTOM 1978, 16, 231–237. [Google Scholar]
- Singh, D.P.; Goyal, R.K.; Singh, R.K.; Sundar, S.; Mohapatra, T.M. In search of an ideal test for diagnosis and prognosis of kala-azar. J. Health Popul. Nutr. 2010, 28, 281–285. [Google Scholar] [PubMed]
- Chappuis, F.; Rijal, S.; Soto, A.; Menten, J.; Boelaert, M. A meta-analysis of the diagnostic performance of the direct agglutination test and rK39 dipstick for visceral leishmaniasis. BMJ 2006, 333, 723. [Google Scholar] [CrossRef] [PubMed]
- Büscher, P.; Gilleman, Q.; Lejon, V. Rapid diagnostic test for sleeping sickness. N. Engl. J. Med. 2013, 368, 1069–1070. [Google Scholar] [CrossRef] [PubMed]
- Lejon, V.; Büscher, P.; Nzoumbou-Boko, R.; Bossard, G.; Jamonneau, V.; Bucheton, B.; Truc, P.; Lemesre, J.-L.; Solano, P.; Vincendeau, P. The separation of trypanosomes from blood by anion exchange chromatography: From Sheila Lanham’s discovery 50 years ago to a gold standard for sleeping sickness diagnosis. PLoS Negl. Trop. Dis. 2019, 13, e0007051. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei, A.; Ahmadipour, F.; Cannet, A.; Marty, P.; Delaunay, P.; Perrin, P.; Dorkeld, F.; Sereno, D.; Akhoundi, M. Immunodetection and molecular determination of visceral and cutaneous Leishmania infection using patients’ urine. Infect. Genet. Evol. 2018, 63, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Riera, C.; Verges, M.; Iniesta, L.; Fisa, R.; Gállego, M.; Tebar, S.; Portús, M. Identification of a Western blot pattern for the specific diagnosis of Trypanosoma cruzi infection in human sera. Am. J. Trop. Med. Hyg. 2012, 86, 412–416. [Google Scholar] [CrossRef]
- Lachaud, L.; Fernández-Arévalo, A.; Normand, A.-C.; Lami, P.; Nabet, C.; Donnadieu, J.L.; Piarroux, M.; Djenad, F.; Cassagne, C.; Ravel, C.; et al. Identification of Leishmania by Matrix-Assisted Laser Desorption Ionization-Time of Flight (MALDI-TOF) Mass Spectrometry Using a Free Web-Based Application and a Dedicated Mass-Spectral Library. J. Clin. Microbiol. 2017, 55, 2924–2933. [Google Scholar] [CrossRef]
- Avila, C.C.; Almeida, F.G.; Palmisano, G. Direct identification of trypanosomatids by matrix-assisted laser desorption ionization-time of flight mass spectrometry (DIT MALDI-TOF MS). J. Mass Spectrom. 2016, 51, 549–557. [Google Scholar] [CrossRef]
- Sakthianandeswaren, A.; Foote, S.J.; Handman, E. The role of host genetics in leishmaniasis. Trends Parasitol. 2009, 25, 383–391. [Google Scholar] [CrossRef]
- Geerts, S.; Osaer, S.; Goossens, B.; Faye, D. Trypanotolerance in small ruminants of sub-Saharan Africa. Trends Parasitol. 2009, 25, 132–138. [Google Scholar] [CrossRef]
- Sternberg, J.M.; Maclean, L. A spectrum of disease in human African trypanosomiasis: The host and parasite genetics of virulence. Parasitology 2010, 137, 2007–2015. [Google Scholar] [CrossRef] [PubMed]
- Mangano, V.D.; Modiano, D. Host genetics and parasitic infections. Clin. Microbiol. Infect. 2014, 20, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Marsden, P. Survival of trypanosoma cruzi in human saliva and urine. Trans. R. Soc. Trop. Med. Hyg. 1966, 60, 562. [Google Scholar] [CrossRef]
- Howard, M.K.; Pharoah, M.M.; Ashall, F.; Miles, M.A. Human urine stimulates growth of Leishmania in vitro. Trans. R. Soc. Trop. Med. Hyg. 1991, 85, 477–479. [Google Scholar] [CrossRef]
- Mebrahtu, Y.B.; Hendricks, L.D.; Oster, C.N.; Lawyer, P.G.; Perkins, P.V.; Pamba, H.; Koech, D.; Roberts, C.R. Leishmania donovani parasites in the nasal secretions, tonsillopharyngeal mucosa, and urine centrifugates of visceral leishmaniasis patients in Kenya. Am. J. Trop. Med. Hyg. 1993, 48, 530–535. [Google Scholar] [CrossRef]
- da Costa Lima, M.S.; Hartkopf, A.C.L.; de Souza Tsujisaki, R.A.; Oshiro, E.T.; Shapiro, J.T.; de Fatima Cepa Matos, M.; Cavalheiros Dorval, M.E. Isolation and molecular characterization of Leishmania infantum in urine from patients with visceral leishmaniasis in Brazil. Acta Trop. 2018, 178, 248–251. [Google Scholar] [CrossRef]
- Fisa, R.; Riera, C.; López-Chejade, P.; Molina, I.; Gállego, M.; Falcó, V.; Ribera, E.; Portús, M. Leishmania infantum DNA detection in urine from patients with visceral leishmaniasis and after treatment control. Am. J. Trop. Med. Hyg. 2008, 78, 741–744. [Google Scholar] [CrossRef]
- Riera, C.; Valladares, J.E. Viable Leishmania infantum in urine and semen in experimentally infected dogs. Parasitol. Today 1996, 12, 412. [Google Scholar] [CrossRef]
- Caravaca, F.; Muñoz, A.; Pizarro, J.L.; de Santamaría, J.S.; Fernandez-Alonso, J. Acute renal failure in visceral leishmaniasis. Am. J. Nephrol. 1991, 11, 350–352. [Google Scholar] [CrossRef]
- de Alcântara, C.C.S.; Santana, L.R.L.; Evangelista, P.D.; Teixeira, A.C.; da Silva Junior, G.B.; Daher, E.D.F. Renal dysfunction in Leishmaniasis and Chagas disease coinfection: A case report. Rev. Inst. Med. Trop. Sao Paulo 2018, 60, e73. [Google Scholar] [CrossRef]
- Koutinas, A.F.; Koutinas, C.K. Pathologic mechanisms underlying the clinical findings in canine leishmaniasis due to Leishmania infantum/chagasi. Vet. Pathol. 2014, 51, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Pennisi, M.-G.; Cardoso, L.; Baneth, G.; Bourdeau, P.; Koutinas, A.; Miró, G.; Oliva, G.; Solano-Gallego, L. LeishVet update and recommendations on feline leishmaniosis. Parasit. Vectors 2015, 8, 302. [Google Scholar] [CrossRef]
- Clementi, A.; Battaglia, G.; Floris, M.; Castellino, P.; Ronco, C.; Cruz, D.N. Renal involvement in leishmaniasis: A review of the literature. NDT Plus 2011, 4, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, G.S.N.; Barbosa, W.L.; da Silva, E.D.; Leal, N.C.; de Medeiros, Z.M. Urine as a promising sample for Leishmania DNA extraction in the diagnosis of visceral leishmaniasis—A review. Braz. J. Infect. Dis. 2019, 23, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Ben-Abid, M.; Galaï, Y.; Habboul, Z.; Ben-Abdelaziz, R.; Ben-Sghaier, I.; Aoun, K.; Bouratbine, A. Diagnosis of Mediterranean visceral leishmaniasis by detection of Leishmania -related antigen in urine and oral fluid samples. Acta Trop. 2017, 167, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Veland, N.; Espinosa, D.; Valencia, B.M.; Ramos, A.P.; Calderon, F.; Arevalo, J.; Low, D.E.; Llanos-Cuentas, A.; Boggild, A.K. Polymerase chain reaction detection of Leishmania kDNA from the urine of Peruvian patients with cutaneous and mucocutaneous leishmaniasis. Am. J. Trop. Med. Hyg. 2011, 84, 556–561. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Rodriguez-Cortes, A.; Trotta, M.; Zampieron, C.; Razia, L.; Furlanello, T.; Caldin, M.; Roura, X.; Alberola, J. Detection of Leishmania infantum DNA by fret-based real-time PCR in urine from dogs with natural clinical leishmaniosis. Vet. Parasitol. 2007, 147, 315–319. [Google Scholar] [CrossRef]
- Manna, L.; Reale, S.; Picillo, E.; Vitale, F.; Gravino, A.E. Urine sampling for real-time polymerase chain reaction based diagnosis of canine leishmaniasis. J. Vet. Diagn. Investig. 2008, 20, 64–67. [Google Scholar] [CrossRef]
- Pessoa-e-Silva, R.; Mendonça Trajano-Silva, L.A.; Lopes da Silva, M.A.; da Cunha Gonçalves-de-Albuquerque, S.; de Goes, T.C.; Silva de Morais, R.C.; Lopes de Melo, F.; de Paiva-Cavalcanti, M. Evaluation of urine for Leishmania infantum DNA detection by real-time quantitative PCR. J. Microbiol. Methods 2016, 131, 34–41. [Google Scholar] [CrossRef]
- Phumee, A.; Kraivichian, K.; Chusri, S.; Noppakun, N.; Vibhagool, A.; Sanprasert, V.; Tampanya, V.; Wilde, H.; Siriyasatien, P. Detection of Leishmania siamensis DNA in saliva by polymerase chain reaction. Am. J. Trop. Med. Hyg. 2013, 89, 899–905. [Google Scholar] [CrossRef]
- Franceschi, A.; Merildi, V.; Guidi, G.; Mancianti, F. Occurrence of Leishmania DNA in urines of dogs naturally infected with leishmaniasis. Vet. Res. Commun. 2007, 31, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Burrows, W.; Havens, I. 1. Studies on immunity to Asiatic cholera; the absorption of immuneglobulin from the bowel and its excretion in the urine and feces of experimental animals and human volunteers. J. Infect. Dis. 1948, 82, 231–251. [Google Scholar] [CrossRef] [PubMed]
- Hanson, L.; Tan, E. Characterization of antibodies in human urine. J. Clin. Investig. 1965, 44, 703–715. [Google Scholar] [CrossRef] [PubMed]
- Kohanteb, J.; Ardehali, S.M.; Rezai, H.R. Detection of Leishmania donovani soluble antigen and antibody in the urine of visceral leishmaniasis patients. Trans. R. Soc. Trop. Med. Hyg. 1987, 81, 578–580. [Google Scholar] [CrossRef]
- Islam, M.Z.; Itoh, M.; Shamsuzzaman, S.M.; Mirza, R.; Matin, F.; Ahmed, I.; Shamsuzzaman Choudhury, A.K.M.; Hossain, M.A.; Qiu, X.-G.; Begam, N.; et al. Diagnosis of visceral leishmaniasis by enzyme-linked immunosorbent assay using urine samples. Clin. Diagn. Lab. Immunol. 2002, 9, 789–794. [Google Scholar] [CrossRef][Green Version]
- Islam, M.Z.; Itoh, M.; Mirza, R.; Ahmed, I.; Ekram, A.R.M.S.; Sarder, A.H.; Shamsuzzaman, S.M.; Hashiguchi, Y.; Kimura, E. Direct agglutination test with urine samples for the diagnosis of visceral leishmaniasis. Am. J. Trop. Med. Hyg. 2004, 70, 78–82. [Google Scholar] [CrossRef][Green Version]
- Islam, M.Z.; Itoh, M.; Takagi, H.; Islam, A.U.; Ekram, A.R.M.S.; Rahman, A.; Takesue, A.; Hashiguchi, Y.; Kimura, E. Enzyme-linked immunosorbent assay to detect urinary antibody against recombinant rKRP42 antigen made from Leishmania donovani for the diagnosis of visceral leishmaniasis. Am. J. Trop. Med. Hyg. 2008, 79, 599–604. [Google Scholar] [CrossRef]
- Hatam, G.; Mikaeili, F.; Sadjjadi, S.; Sarkari, B. Direct Agglutination Test and Enzyme Linked Immunosorbent Assay with Urine Samples for the Diagnosis of Visceral Leishmaniasis. Iran. J. Parasitol. 2007, 2, 24–28. [Google Scholar]
- Khan, M.G.M.; Alam, M.S.; Podder, M.P.; Itoh, M.; Jamil, K.M.; Haque, R.; Wagatsuma, Y. Evaluation of rK-39 strip test using urine for diagnosis of visceral leishmaniasis in an endemic area in Bangladesh. Parasit. Vectors 2010, 3, 114. [Google Scholar] [CrossRef]
- Singh, D.; Pandey, K.; Das, V.N.R.; Das, S.; Verma, N.; Ranjan, A.; Lal, S.C.; Topno, K.R.; Singh, S.K.; Verma, R.B.; et al. Evaluation of rK-39 strip test using urine for diagnosis of visceral leishmaniasis in an endemic region of India. Am. J. Trop. Med. Hyg. 2013, 88, 222–226. [Google Scholar] [CrossRef]
- Chakravarty, J.; Kumar, S.; Kumar, R.; Gautam, S.; Rai, M.; Sundar, S. Evaluation of rk39 immunochromatographic test with urine for diagnosis of visceral leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 2011, 105, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Goswami, R.P.; Goswami, R.P.; Das, S.; Ray, Y.; Rahman, M. Testing urine samples with rK39 strip as the simplest non-invasive field diagnosis for visceral leishmaniasis: An early report from eastern India. J. Postgrad. Med. 2012, 58, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Ejazi, S.A.; Bhattacharya, P.; Bakhteyar, M.A.K.; Mumtaz, A.A.; Pandey, K.; Das, V.N.R.; Das, P.; Rahaman, M.; Goswami, R.P.; Ali, N. Noninvasive Diagnosis of Visceral Leishmaniasis: Development and Evaluation of Two Urine-Based Immunoassays for Detection of Leishmania donovani Infection in India. PLoS Negl. Trop. Dis. 2016, 10, e0005035. [Google Scholar] [CrossRef]
- Diro, E.; Techane, Y.; Tefera, T.; Assefa, Y.; Kebede, T.; Genetu, A.; Kebede, Y.; Tesfaye, A.; Ergicho, B.; Gebre-Yohannes, A.; et al. Field evaluation of FD-DAT, rK39 dipstick and KATEX (urine latex agglutination) for diagnosis of visceral leishmaniasis in northwest Ethiopia. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Pandey, K.; Das, V.N.R.; Das, S.; Kumar, S.; Topno, R.K.; Das, P. Novel noninvasive method for diagnosis of visceral leishmaniasis by rK39 testing of sputum samples. J. Clin. Microbiol. 2009, 47, 2684–2685. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mohapatra, S.; Samantaray, J.C.; Ghosh, A. A Comparative Study of Serum, Urine and Saliva Using rk39 Strip for the Diagnosis of Visceral Leishmaniasis. J. Arthropod Borne. Dis. 2016, 10, 87–91. [Google Scholar]
- Islam, M.Z.; Itoh, M.; Ul Islam, M.A.; Saifuddin Ekram, A.R.M.; Rahman, M.A.; Takagi, H.; Takesue, A.; Hashiguchi, Y.; Kimura, E. ELISA with recombinant rKRP42 antigen using urine samples: A tool for predicting clinical visceral leishmaniasis cases and its outbreak. Am. J. Trop. Med. Hyg. 2012, 87, 658–662. [Google Scholar] [CrossRef]
- De Colmenares, M.; Portus, M.; Riera, C.; Gallego, M.; Aisa, M.J.; Torras, S.; Munoz, C. Short report: Detection of 72-75-kD and 123-kD fractions of Leishmania antigen in urine of patients with visceral leishmaniasis. Am. J. Trop. Med. Hyg. 1995, 52, 427–428. [Google Scholar] [CrossRef][Green Version]
- Zaragoza, C.; Barrera, R.; Centeno, F.; Tapia, J.A.; Durán, E.; González, M.; Mañé, M.C. SDS-PAGE and Western blot of urinary proteins in dogs with leishmaniasis. Vet. Res. 2003, 34, 137–151. [Google Scholar] [CrossRef][Green Version]
- de Lira, N.M.S. Avaliação Física, Química, Microbiológica e Pesquisa de Anticorpos Anti-IgG em Urina de Cães (Canis familiaris) Linnaeus, 1785) Naturalmente Infectados por Leishmania (Leishmania) Chagasi (Cunha & Chagas, 1937). Master’s Thesis, Universidade Federal Rural de Pernambuco, Pernmbuco, Brazil, 2008. [Google Scholar]
- Solano-Gallego, L.; Rodríguez, A.; Iniesta, L.; Arboix, M.; Portús, M.; Alberola, J. Detection of anti-Leishmania immunoglobulin G antibodies in urine specimens of dogs with leishmaniasis. Clin. Diagn. Lab. Immunol. 2003, 10, 849–855. [Google Scholar] [CrossRef]
- Todolí, F.; Solano-Gallego, L.; Ojeda, A.; Quintana, J.; Lloret, A.; Roura, X.; Alberola, J.; Rodríguez-Cortés, A. Anti-Leishmania IgA in urine samples from dogs with clinical leishmaniasis. Vet. Parasitol. 2009, 159, 17–23. [Google Scholar] [CrossRef]
- Azazy, A.A.; Chance, M.L.; Devaney, E. A time-course study of circulating antigen and parasite-specific antibody in cotton rats infected with Leishmania donovani. Ann. Trop. Med. Parasitol. 1997, 91, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Kashino, S.S.; Abeijon, C.; Qin, L.; Kanunfre, K.A.; Kubrusly, F.S.; Silva, F.O.; Costa, D.L.; Campos, D.; Costa, C.H.N.; Raw, I.; et al. Identification of Leishmania infantum chagasi proteins in urine of patients with visceral leishmaniasis: A promising antigen discovery approach of vaccine candidates. Parasite Immunol. 2012, 34, 360–371. [Google Scholar] [CrossRef] [PubMed]
- Abeijon, C.; Kashino, S.S.; Silva, F.O.; Costa, D.L.; Fujiwara, R.T.; Costa, C.H.N.; Campos-Neto, A. Identification and Diagnostic Utility of Leishmania infantum Proteins Found in Urine Samples from Patients with Visceral Leishmaniasis. Clin. Vaccine Immunol. 2012, 19, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Ferlizza, E. Urine Proteome in Animals of Veterinary Interest: Species Comparison and New Biomarkers of Nephropathy. Master’s Thesis, Università di Bologna, Bologna, Italy, 2015. [Google Scholar]
- Abeijon, C.; Alves, F.; Monnerat, S.; Wasunna, M.; Mbui, J.; Viana, A.G.; Bueno, L.L.; Siqueira, W.F.; Carvalho, S.G.; Agrawal, N.; et al. Development of a multiplexed assay for the detection of Leishmania donovani/Leishmania infantum protein biomarkers in the urine of patients with visceral leishmaniasis. J. Clin. Microbiol. 2019, 57. [Google Scholar] [CrossRef] [PubMed]
- Sarkari, B.; Chance, M.; Hommel, M. Antigenuria in visceral leishmaniasis: Detection and partial characterisation of a carbohydrate antigen. Acta Trop. 2002, 82, 339–348. [Google Scholar] [CrossRef]
- Vallur, A.C.; Tutterrow, Y.L.; Mohamath, R.; Pattabhi, S.; Hailu, A.; Abdoun, A.O.; Ahmed, A.E.; Mukhtar, M.; Salam, M.A.; Almeida, M.L.; et al. Development and comparative evaluation of two antigen detection tests for Visceral Leishmaniasis. BMC Infect. Dis. 2015, 15, 384. [Google Scholar] [CrossRef][Green Version]
- El-Safi, S.H.; Abdel-Haleem, A.; Hammad, A.; El-Basha, I.; Omer, A.; Kareem, H.G.; Boelaert, M.; Chance, M.; Hommel, M. Field evaluation of latex agglutination test for detecting urinary antigens in visceral leishmaniasis in Sudan. East. Mediterr. Health J. 2003, 9, 844–855. [Google Scholar]
- Rijal, S.; Boelaert, M.; Regmi, S.; Karki, B.M.S.; Jacquet, D.; Singh, R.; Chance, M.L.; Chappuis, F.; Hommel, M.; Desjeux, P.; et al. Evaluation of a urinary antigen-based latex agglutination test in the diagnosis of kala-azar in eastern Nepal. Trop. Med. Int. Health 2004, 9, 724–729. [Google Scholar] [CrossRef]
- Vilaplana, C.; Blanco, S.; Domínguez, J.; Giménez, M.; Ausina, V.; TUral, C.; Muñoz, C. Noninvasive method for diagnosis of visceral leishmaniasis by a latex agglutination test for detection of antigens in urine samples. J. Clin. Microbiol. 2004, 42, 1853–1854. [Google Scholar] [CrossRef][Green Version]
- Sundar, S.; Agrawal, S.; Pai, K.; Chance, M.; Hommel, M. Detection of leishmanial antigen in the urine of patients with visceral leishmaniasis by a latex agglutination test. Am. J. Trop. Med. Hyg. 2005, 73, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Motazedian, M.H.M.; Fakhar, M.; Motazedian, M.H.M.; Hatam, G.; Mikaeili, F. A urine-based polymerase chain reaction method for the diagnosis of visceral leishmaniasis in immunocompetent patients. Diagn. Microbiol. Infect. Dis. 2008, 60, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Riera, C.; Fisa, R.; Lopez, P.; Ribera, E.; Carrió, J.; Falcó, V.; Molina, I.; Gállego, M.; Portús, M. Evaluation of a latex agglutination test (KAtex) for detection of Leishmania antigen in urine of patients with HIV-Leishmania coinfection: Value in diagnosis and post-treatment follow-up. Eur. J. Clin. Microbiol. Infect. Dis. 2004, 23, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Boelaert, M.; Verdonck, K.; Menten, J.; Sunyoto, T.; van Griensven, J.; Chappuis, F.; Rijal, S. Rapid tests for the diagnosis of visceral leishmaniasis in patients with suspected disease. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef]
- van Griensven, J.; Mengesha, B.; Mekonnen, T.; Fikre, H.; Takele, Y.; Adem, E.; Mohammed, R.; Ritmeijer, K.; Vogt, F.; Adriaensen, W.; et al. Leishmania Antigenuria to Predict Initial Treatment Failure and Relapse in Visceral Leishmaniasis/HIV Coinfected Patients: An Exploratory Study Nested Within a Clinical Trial in Ethiopia. Front. Cell. Infect. Microbiol. 2018, 8, 94. [Google Scholar] [CrossRef]
- Asfaram, S.; Hosseini Teshnizi, S.; Fakhar, M.; Banimostafavi, E.S.; Soosaraei, M. Is urine a reliable clinical sample for the diagnosis of human visceral leishmaniasis? A systematic review and meta-analysis. Parasitol. Int. 2018, 67, 575–583. [Google Scholar] [CrossRef]
- Ngotho, M.; Kagira, J.M.; Gachie, B.M.; Karanja, S.M.; Waema, M.W.; Maranga, D.N.; Maina, N.W. Loop Mediated Isothermal Amplification for Detection of Trypanosoma brucei gambiense in Urine and Saliva Samples in Nonhuman Primate Model. BioMed Res. Int. 2015, 2015, 867846. [Google Scholar] [CrossRef]
- Itazi, O.K.; Enyaru, J.C. The nature of proteins excreted in the urine of rabbits infected with T. brucei subgroup organisms. Trans. R. Soc. Trop. Med. Hyg. 1973, 67, 263. [Google Scholar] [CrossRef]
- Boreham, P.F.L.; Facer, C.A. Fibrinogen and fibrinogen/fibrin degradation products in the urine of rabbits infected with Trypanosoma (Trypanozoon) brucei. Z. Parasitenkd. 1977, 52, 257–265. [Google Scholar] [CrossRef]
- Hall, J.; Seed, J. Quantification of aromatic amino acid catabolites in urine of mice acutely infected with Trypanosoma brucei gambiense. Comp. Biochem. Physiol. 1981, 69, 791–796. [Google Scholar]
- Seed, J.R.; Hall, J.E.; Sechelski, J. Phenylalanine metabolism in Microtus montanus chronically infected with Trypanosoma brucei gambiense. Comp. Biochem. Physiol. 1982, 71, 209–215. [Google Scholar] [CrossRef]
- Hall, J.E.; Seed, J.R.; Sechelski, J.B. Multiple alpha-keto aciduria in Microtus montanus chronically infected with Trypanosoma brucei gambiense. Comp. Biochem. Physiol. 1985, 82, 73–78. [Google Scholar] [CrossRef]
- Hall, J.E.; Seed, J.R. Increased urinary excretion of aromatic amino acid catabolites by Microtus montanus chronically infected with Trypanosoma brucei gambiense. Comp. Biochem. Physiol. 1984, 77, 755–760. [Google Scholar] [CrossRef]
- El Sawalhy, A.; Seed, J.R.; Hall, J.E.; El Attar, H. Increased excretion of aromatic amino acid catabolites in animals infected with Trypanosoma brucei evansi. J. Parasitol. 1998, 84, 469–473. [Google Scholar] [CrossRef]
- Nowicki, C.; Cazzulo, J.J. Aromatic amino acid catabolism in trypanosomatids. Comp. Biochem. Physiol. Part A Mol. Integr. Physiol. 2008, 151, 381–390. [Google Scholar] [CrossRef]
- Bonnet, J.; Garcia, C.; Leger, T.; Couquet, M.-P.; Vignoles, P.; Vatunga, G.; Ndung’u, J.; Boudot, C.; Bisser, S.; Courtioux, B. Proteome characterization in various biological fluids of Trypanosoma brucei gambiense-infected subjects. J. Proteom. 2019, 196, 150–161. [Google Scholar] [CrossRef]
- Simaren, J.; Ogunnaike, M. Urinary biochemical changes, histopathologic effect of kidney damage observed in rats infected with Trypanosoma b. brucei. Trop. Med. Parasitol. 1989, 11, 35–46. [Google Scholar]
- Seed, J.R. Trypanosoma gambiense and T. lewisi: Increased vascular permeability and skin lesions in rabbits. Exp. Parasitol. 1969, 26, 214–223. [Google Scholar] [CrossRef]
- Monroy, F.P.; Dusanic, D.G. The kidney form of Trypanosoma musculi: A distinct stage in the life cycle? Parasitol. Today 2000, 16, 107–110. [Google Scholar] [CrossRef]
- Arias, L.F.; Duque, E.; Ocampo, C.; Henao, J.; Zuluaga, G.; Varela, G.; Carvajal, J.; Duque, J.; Robledo-Villegas, M.; Arbeláez, M. Detection of amastigotes of Trypanosoma cruzi in a kidney graft with acute dysfunction. Transplant. Proc. 2006, 38, 885–887. [Google Scholar] [CrossRef]
- González, G.; Sunnemark, D.; Orn, A.; Grönvik, K.O. Detection of cruzipain, the major cysteine proteinase from Trypanosoma cruzi and its C-terminal extension in biological fluids during experimental infection in mice. Scand. J. Immunol. 1996, 44, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Yauri, V.; Castro-Sesquen, Y.E.; Verastegui, M.; Angulo, N.; Recuenco, F.; Cabello, I.; Malaga, E.; Bern, C.; Gavidia, C.M.; Gilman, R.H. Domestic Pig (Sus scrofa) as an Animal Model for Experimental Trypanosoma cruzi Infection. Am. J. Trop. Med. Hyg. 2016, 94, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sesquen, Y.E.; Gilman, R.H.; Yauri, V.; Cok, J.; Angulo, N.; Escalante, H.; Bern, C. Detection of soluble antigen and DNA of Trypanosoma cruzi in urine is independent of renal injury in the guinea pig model. PLoS ONE 2013, 8, e58480. [Google Scholar] [CrossRef] [PubMed]
- Freilij, H.L.; Corral, R.S.; Katzin, A.M.; Grinstein, S. Antigenuria in infants with acute and congenital Chagas’ disease. J. Clin. Microbiol. 1987, 25, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Corral, R.; Freilij, H.; Montemayor, A.; Grinstein, S. Trypanosoma-cruzi antigens in urine from patients with chagas-disease. IRCS Med. Sci. 1984, 12, 1034–1035. [Google Scholar]
- Corral, R.S.; Altcheh, J.; Alexandre, S.R.; Grinstein, S.; Freilij, H.; Katzin, A.M. Detection and characterization of antigens in urine of patients with acute, congenital, and chronic Chagas’ disease. J. Clin. Microbiol. 1996, 34, 1957–1962. [Google Scholar] [CrossRef]
- Katzin, A.M.; Marcipar, A.; Freilij, H.; Corral, R.; Yanovsky, J.F. Rapid determination of Trypanosoma cruzi urinary antigens in human chronic Chagas disease by agglutination test. Exp. Parasitol. 1989, 68, 208–215. [Google Scholar] [CrossRef]
- Umezawa, E.S.; Shikanai-Yasuda, M.A.; da Silveira, J.F.; Cotrim, P.C.; Paranhos, G.; Katzin, A.M. Trypanosoma cruzi: Detection of a circulating antigen in urine of chagasic patients sharing common epitopes with an immunodominant repetitive antigen. Exp. Parasitol. 1993, 76, 352–357. [Google Scholar] [CrossRef]
- Corral, R.S.; Orn, A.; Freilij, H.L.; Bergman, T.; Grinstein, S. Purification and characterization of an 80-kilodalton Trypanosoma cruzi urinary antigen. J. Clin. Microbiol. 1989, 27, 145–151. [Google Scholar] [CrossRef]
- Corral, R.S.; Bertot, G.M.; Petray, P.B.; Altcheh, J.M.; Singh, M.; Orn, A.; Rapoport, M.F.; Grinstein, S. An iron-binding Trypanosoma cruzi urinary antigen. Parasite 1995, 2, 339–344. [Google Scholar]
- Málaga-Machaca, E.S.; Romero-Ramirez, A.; Gilman, R.H.; Astupiña-Figueroa, S.; Angulo, N.; Florentini, A.; Lovon-Luque, C.J.; Gonza, R.A.; Del Carpio-Sanz, A.; Cabello, I.; et al. Polyclonal antibodies for the detection of Trypanosoma cruzi circulating antigens. PLoS Negl. Trop. Dis. 2017, 11, e0006069. [Google Scholar] [CrossRef] [PubMed]
- Luchini, A.; Geho, D.H.; Bishop, B.; Tran, D.; Xia, C.; Dufour, R.L.; Jones, C.D.; Espina, V.; Patanarut, A.; Zhou, W.; et al. Smart hydrogel particles: Biomarker harvesting: One-step affinity purification, size exclusion, and protection against degradation. Nano Lett. 2008, 8, 350–361. [Google Scholar] [CrossRef] [PubMed]
- Douglas, T.A.; Tamburro, D.; Fredolini, C.; Espina, B.H.; Lepene, B.S.; Ilag, L.; Espina, V.; Petricoin, E.F.; Liotta, L.A.; Luchini, A. The use of hydrogel microparticles to sequester and concentrate bacterial antigens in a urine test for Lyme disease. Biomaterials 2011, 32, 1157–1166. [Google Scholar] [CrossRef]
- Castro-Sesquen, Y.E.; Gilman, R.H.; Galdos-Cardenas, G.; Ferrufino, L.; Sánchez, G.; Valencia Ayala, E.; Liotta, L.; Bern, C.; Luchini, A. Working Group on Chagas Disease in Bolivia and Peru Use of a novel chagas urine nanoparticle test (chunap) for diagnosis of congenital chagas disease. PLoS Negl. Trop. Dis. 2014, 8, e3211. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sesquen, Y.E.; Gilman, R.H.; Mejia, C.; Clark, D.E.; Choi, J.; Reimer-McAtee, M.J.; Castro, R.; Valencia-Ayala, E.; Flores, J.; Bowman, N.; et al. Use of a Chagas Urine Nanoparticle Test (Chunap) to Correlate with Parasitemia Levels in T. cruzi/HIV Co-infected Patients. PLoS Negl. Trop. Dis. 2016, 10, e0004407. [Google Scholar] [CrossRef]
- Mackie, F. Note on some bodies of unknown nature found in faeces of kala-azar patients. Indian J. Med. Res. 1914, 2, 510–515. [Google Scholar]
- Shortt, H.; Smith, R.; D’Silva, M.; Swaminath, C. Leishmania donovani in human faeces in indian kala-azar. Indian J. Med. Res. 1929, 17, 644–646. [Google Scholar]
- Dollahon, N.R.; Janovy, J. Insect flagellates from feces and gut contents of four genera of lizards. J. Parasitol. 1971, 57, 1130–1132. [Google Scholar] [CrossRef] [PubMed]
- Nery, G.; Meneses, I.D.S.; Trueb, I.; Larangeira, D.F.; Barrouin-Melo, S.M. Ocorrência de Leishmania infantum em fezes de cão. Arq. Bras. Med. Vet. Zootec. 2015, 67, 1249–1253. [Google Scholar] [CrossRef][Green Version]
- Hamad, I.; Forestier, C.-L.; Peeters, M.; Delaporte, E.; Raoult, D.; Bittar, F. Wild gorillas as a potential reservoir of Leishmania major. J. Infect. Dis. 2015, 211, 267–273. [Google Scholar] [CrossRef]
- Hamad, I.; Forestier, C.-L.; Greub, G.; Jaton, K.; Raoult, D.; Bittar, F. Reply to Bastien et al. J. Infect. Dis. 2015, 212, 506–508. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bastien, P.; Volf, P.; Depaquit, J.; Dondji, B.; Gallego, M.; Gangneux, J.-P.; Izri, A.; Marty, P.; Piarroux, R.; Pratlong, F.; et al. Comments on Leishmania major in Gorilla Feces. J. Infect. Dis. 2015, 212, 505–506. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Votýpka, J.; Pafčo, B.; Modrý, D.; Mbohli, D.; Tagg, N.; Petrželková, K.J. An unexpected diversity of trypanosomatids in fecal samples of great apes. Int. J. Parasitol. Parasites Wildl. 2018, 7, 322–325. [Google Scholar] [CrossRef] [PubMed]
- Santiago-Rodriguez, T.M.; Fornaciari, G.; Luciani, S.; Dowd, S.E.; Toranzos, G.A.; Marota, I.; Cano, R.J. Taxonomic and predicted metabolic profiles of the human gut microbiome in pre-Columbian mummies. FEMS Microbiol. Ecol. 2016. [Google Scholar] [CrossRef]
- Sereno, D.; Dorkeld, F.; Akhoundi, M.; Perrin, P. Pathogen Species Identification from Metagenomes in Ancient Remains: The Challenge of Identifying Human Pathogenic Species of Trypanosomatidae via Bioinformatic Tools. Genes 2018, 9, 418. [Google Scholar] [CrossRef]
- Sereno, D.; Akhoundi, M.; Dorkeld, F.; Oury, B.; Momen, H.; Perrin, P. What pre-Columbian mummies could teach us about South American leishmaniases? Pathog. Dis. 2017. [Google Scholar] [CrossRef]
- Jirků, M.; Votýpka, J.; Petrželková, K.J.; Jirků-Pomajbíková, K.; Kriegová, E.; Vodička, R.; Lankester, F.; Leendertz, S.A.J.; Wittig, R.M.; Boesch, C.; et al. Wild chimpanzees are infected by Trypanosoma brucei. Int. J. Parasitol. Parasites Wildl. 2015, 4, 277–282. [Google Scholar] [CrossRef][Green Version]
- Fernandes, A.; Iñiguez, A.M.; Lima, V.S.; de Souza, S.M.F.M.; Ferreira, L.F.; Vicente, A.C.P.; Jansen, A.M. Pre-Columbian Chagas disease in Brazil: Trypanosoma cruzi I in the archaeological remains of a human in Peruaçu Valley, Minas Gerais, Brazil. Mem. Inst. Oswaldo Cruz 2008, 103, 514–516. [Google Scholar] [CrossRef]
- Araújo, A.; Jansen, A.M.; Reinhard, K.; Ferreira, L.F. Paleoparasitology of Chagas disease—A review. Mem. Inst. Oswaldo Cruz 2009, 104, 9–16. [Google Scholar] [CrossRef]
- Franco, D.J.; Vago, A.R.; Chiari, E.; Meira, F.C.A.; Galvão, L.M.C.; Machado, C.R.S. Trypanosoma cruzi: Mixture of two populations can modify virulence and tissue tropism in rat. Exp. Parasitol. 2003, 104, 54–61. [Google Scholar] [CrossRef]
- Andrade, L.O.; Machado, C.R.; Chiari, E.; Pena, S.D.; Macedo, A.M. Differential tissue distribution of diverse clones of Trypanosoma cruzi in infected mice. Mol. Biochem. Parasitol. 1999, 100, 163–172. [Google Scholar] [CrossRef]
- Lewis, M.D.; Fortes Francisco, A.; Taylor, M.C.; Burrell-Saward, H.; McLatchie, A.P.; Miles, M.A.; Kelly, J.M. Bioluminescence imaging of chronic Trypanosoma cruzi infections reveals tissue-specific parasite dynamics and heart disease in the absence of locally persistent infection. Cell. Microbiol. 2014, 16, 1285–1300. [Google Scholar] [CrossRef] [PubMed]
- McCall, L.-I.; Tripathi, A.; Vargas, F.; Knight, R.; Dorrestein, P.C.; Siqueira-Neto, J.L. Experimental Chagas disease-induced perturbations of the fecal microbiome and metabolome. PLoS Negl. Trop. Dis. 2018, 12, e0006344. [Google Scholar] [CrossRef] [PubMed]
- Urdaneta-Morales, S.; Nironi, I. Trypanosoma cruzi in the anal glands of urban opossums. I—Isolation and experimental infections. Mem. Inst. Oswaldo Cruz 1996, 91, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Forkner, C.E.; Zia, L.S. Viable leishmania donovani in nasal and oral secretions of patients with kala-azar and the bearing of this finding on the transmission of the disease. J. Exp. Med. 1934, 59, 491–499. [Google Scholar] [CrossRef] [PubMed]
- de Brito, M.E.F.; Almeida, E.L.; Medeiros, A.C.R.; Werkhäuser, R.P.; de Alexandre, J.L.A.; Sá, B.S.L.F.; Rodrigues, E.H.G.; Brandão-Filho, S.P. Leishmania (Viannia) braziliensis isolated from the saliva of patients in a cutaneous leishmaniasis-endemic area of northeastern Brazil. Mem. Inst. Oswaldo Cruz 2018, 113, e170250. [Google Scholar] [CrossRef]
- Siriyasatien, P.; Chusri, S.; Kraivichian, K.; Jariyapan, N.; Hortiwakul, T.; Silpapojakul, K.; Pym, A.M.; Phumee, A. Early detection of novel Leishmania species DNA in the saliva of two HIV-infected patients. BMC Infect. Dis. 2016, 16, 89. [Google Scholar] [CrossRef]
- Chusri, S.; Hortiwakul, T.; Silpapojakul, K.; Siriyasatien, P. Consecutive cutaneous and visceral leishmaniasis manifestations involving a novel Leishmania species in two HIV patients in Thailand. Am. J. Trop. Med. Hyg. 2012, 87, 76–80. [Google Scholar] [CrossRef]
- Pandey, N.; Siripattanapipong, S.; Leelayoova, S.; Manomat, J.; Mungthin, M.; Tan-ariya, P.; Bualert, L.; Naaglor, T.; Siriyasatien, P.; Phumee, A.; et al. Detection of Leishmania DNA in saliva among patients with HIV/AIDS in Trang Province, southern Thailand. Acta Trop. 2018, 185, 294–300. [Google Scholar] [CrossRef]
- Sriworarat, C.; Phumee, A.; Mungthin, M.; Leelayoova, S.; Siriyasatien, P. Development of loop-mediated isothermal amplification (LAMP) for simple detection of Leishmania infection. Parasit. Vectors 2015, 8, 591. [Google Scholar] [CrossRef]
- Vaish, M.; Mehrotra, S.; Chakravarty, J.; Sundar, S. Noninvasive molecular diagnosis of human visceral leishmaniasis. J. Clin. Microbiol. 2011, 49, 2003–2005. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Halder, A.; Rabidas, V.N.; Mandal, A.; Das, P. Specific noninvasive detection of Leishmania donovani in desquamated buccal cell swab samples from human visceral Leishmaniasis-HIV coinfected patients. J. Clin. Microbiol. 2014, 52, 1238–1241. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Pennisi, M.G.; Lupo, T.; Migliazzo, A.; Caprì, A.; Solano-Gallego, L. Detection of Leishmania infantum DNA by real-time PCR in canine oral and conjunctival swabs and comparison with other diagnostic techniques. Vet. Parasitol. 2012, 184, 10–17. [Google Scholar] [CrossRef] [PubMed]
- de Ferreira, S.A.; Almeida, G.G.; de Silva, S.O.; Vogas, G.P.; Fujiwara, R.T.; de Andrade, A.S.R.; Melo, M.N. Nasal, oral and ear swabs for canine visceral leishmaniasis diagnosis: New practical approaches for detection of Leishmania infantum DNA. PLoS Negl. Trop. Dis. 2013, 7, e2150. [Google Scholar] [CrossRef]
- Masum, M.A.; Evans, D.A. Agglutinating anti-leishmanial antibodies in the saliva of kala-azar patients. Trans. R. Soc. Trop. Med. Hyg. 1994, 88, 660. [Google Scholar] [CrossRef]
- Cantos-Barreda, A.; Escribano, D.; Bernal, L.J.; Cerón, J.J.; Martínez-Subiela, S. Quantification of anti-Leishmania antibodies in saliva of dogs. Vet. Parasitol. 2017, 242, 54–58. [Google Scholar] [CrossRef]
- Rosenthal, E. Leishmania in Bronchoalveolar Lavage. Ann. Intern. Med. 1991, 114, 1064. [Google Scholar] [CrossRef]
- Jokipii, L.; Salmela, K.; Saha, H.; Kyrönseppä, H.; Eklund, B.; Evans, D.; Von Willebrand, E.; Jokipii, A.M.M. Leishmaniasis Diagnosed from Bronchoalveolar Lavage. Scand. J. Infect. Dis. 1992, 24, 677–681. [Google Scholar] [CrossRef]
- Lejon, V.; Kwete, J.; Büscher, P. Towards saliva-based screening for sleeping sickness? Trop. Med. Int. Health 2003, 8, 585–588. [Google Scholar] [CrossRef]
- Lejon, V.; Jamonneau, V.; Solano, P.; Atchade, P.; Mumba, D.; Nkoy, N.; Bébronne, N.; Kibonja, T.; Balharbi, F.; Wierckx, A.; et al. Detection of trypanosome-specific antibodies in saliva, towards non-invasive serological diagnosis of sleeping sickness. Trop. Med. Int. Health 2006, 11, 620–627. [Google Scholar] [CrossRef]
- Marsden, P.D.; Hagstrom, J.W. Experimental Trypanosoma cruzi infection in beagle puppies. The effect of variations in the dose and source of infecting trypanosomes and the route of inoculation on the course of the infection. Trans. R. Soc. Trop. Med. Hyg. 1968, 62, 816–824. [Google Scholar] [CrossRef]
- Pinho, R.T.; Pedrosa, R.C.; Costa-Martins, P.; Castello-Branco, L.R. Saliva ELISA: A method for the diagnosis of chronic Chagas disease in endemic areas. Acta Trop. 1999, 72, 31–38. [Google Scholar] [CrossRef]
- Cortes-Serra, N.; Pinazo, M.-J.; de la Torre, L.; Galizzi, M.; Gascon, J.; Bustamante, J.M. Diagnosis of Trypanosoma cruzi Infection Status using Saliva of Infected Subjects. Am. J. Trop. Med. Hyg. 2018, 98, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, J.L.M.; Minuzzi-Souza, T.T.C.; Silva, L.R.; Oliveira, A.C.; Mendonça, V.J.; Nitz, N.; Aguiar, L.M.S.; Gurgel-Gonçalves, R. High frequency of trypanosomatids in gallery forest bats of a Neotropical savanna. Acta Trop. 2018, 177, 200–206. [Google Scholar] [CrossRef] [PubMed]
- el Hassan, A.M.; Khalil, E.A.; el Sheikh, E.A.; Zijlstra, E.E.; Osman, A.; Ibrahim, M.E. Post kala-azar ocular leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 1998, 92, 177–179. [Google Scholar] [CrossRef]
- Ferrari, T.C.; Guedes, A.C.; Oréfice, F.; Genaro, O.; Pinheiro, S.R.; Marra, M.A.; Silveira, I.L.; Miranda, M.O. Isolation of Leishmania sp. from aqueous humor of a patient with cutaneous disseminated leishmaniasis and bilateral iridocyclitis (preliminary report). Rev. Inst. Med. Trop. Sao Paulo 1990, 32, 296–298. [Google Scholar] [CrossRef]
- Reinecke, P.; Gabbart, H.E.; Strunk, W.; Lösche, C.C. Ocular scleromalacia caused by leishmaniasis: A rare cause of scleral perforation. Br. J. Ophthalmol. 2001, 85, 240–241. [Google Scholar] [CrossRef]
- Doroodgar, M.; Doroodgar, M.; Doroodgar, A. Unusual Presentation of Cutaneous Leishmaniasis: Ocular Leishmaniasis. Case Rep. Infect. Dis. 2017, 2017, 3198547. [Google Scholar] [CrossRef]
- Abrishami, M.; Soheilian, M.; Farahi, A.; Dowlati, Y. Successful treatment of ocular leishmaniasis. Eur. J. Dermatol. 2002, 12, 88–89. [Google Scholar]
- Nikandish, M.; Goyonlo, V.M.; Taheri, A.R.; Kiafar, B. Ocular Leishmaniasis Treated by Intralesional Amphotericin B. Middle East Afr. J. Ophthalmol. 2016, 23, 153–155. [Google Scholar]
- Mencía-Gutiérrez, E.; Gutiérrez-Díaz, E.; Rodríguez-Peralto, J.L.; Monsalve-Córdova, J. Old World eyelid cutaneous leishmaniasis: A case report. Dermatol. Online J. 2005, 11, 29. [Google Scholar] [PubMed]
- Mohammadpour, I.; Motazedian, M.H.; Handjani, F.; Hatam, G.R. Cutaneous Leishmaniasis of the Eyelids: A Case Series with Molecular Identification and Literature Review. Korean J. Parasitol. 2016, 54, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Doroodgar, M.; Doroodgar, M.; Doroodgar, A. Eyelid Cutaneous Leishmaniasis: A Case Report. Iran. J. Public Health 2017, 46, 261–264. [Google Scholar] [PubMed]
- Razeghinejad, M.R.; Monabati, A.; Kadivar, M.R.; Alborzi, A. Conjunctival leishmaniasis in a case of disseminated cutaneous leishmaniasis. Trop. Dr. 2017, 47, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Perrin-Terrin, A.; Auriol, S.; Mahieu, L.; Debard, A.; Eden, A.; Cassagne, M.; Pagot-Mathis, V.; Malecaze, F.; Soler, V. Recurrent bilateral anterior uveitis due to Leishmania infantum in a patient with immune deficiency related to HIV infection: A case report and literature review. J. Fr. Ophtalmol. 2014, 37, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Nandy, A.; Addy, M.; Chowdhury, A.B. Leishmanial blepharo-conjunctivitis. Trop. Geogr. Med. 1991, 43, 303–306. [Google Scholar]
- Di Pietro, S.; Bosco, V.R.F.; Crinò, C.; Francaviglia, F.; Giudice, E. Prevalence, type, and prognosis of ocular lesions in shelter and owned-client dogs naturally infected by Leishmania infantum. Vet. World 2016, 9, 633–637. [Google Scholar] [CrossRef]
- McConnell, E.E.; Chaffee, E.F.; Cashell, I.G.; Garner, F.M. Visceral leishmaniasis with ocular involvement in a dog. J. Am. Vet. Med. Assoc. 1970, 156, 197–203. [Google Scholar]
- Richter, M.; Schaarschmidt-Kiener, D.; Krudewig, C. Ocular signs, diagnosis and long-term treatment with allopurinol in a cat with leishmaniasis. Schweiz. Arch. Tierheilkd. 2014, 156, 289–294. [Google Scholar] [CrossRef]
- Veraldi, S.; Bottini, S.; Currò, N.; Gianotti, R. Leishmaniasis of the eyelid mimicking an infundibular cyst and review of the literature on ocular leishmaniasis. Int. J. Infect. Dis. 2010, 14, e230–e232. [Google Scholar] [CrossRef]
- Garcia-Alonso, M.; Nieto, C.G.; Blanco, A.; Requena, J.M.; Alonso, C.; Navarrete, I. Presence of antibodies in the aqueous humour and cerebrospinal fluid during Leishmania infections in dogs. Pathological features at the central nervous system. Parasite Immunol. 1996, 18, 539–546. [Google Scholar] [CrossRef] [PubMed]
- García-Alonso, M.; Blanco, A.; Reina, D.; Serrano, F.J.; Alonso, C.; Nieto, C.G. Immunopathology of the uveitis in canine leishmaniasis. Parasite Immunol. 1996, 18, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, C.; Fondevila, D.; Leiva, M.; Roura, X.; Peña, T. Detection of Leishmania spp. and associated inflammation in ocular-associated smooth and striated muscles in dogs with patent leishmaniosis. Vet. Ophthalmol. 2010, 13, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, C.; Fondevila, D.; Leiva, M.; Roura, X.; Peña, T. Characterization of lacrimal gland lesions and possible pathogenic mechanisms of keratoconjunctivitis sicca in dogs with leishmaniosis. Vet. Parasitol. 2005, 133, 37–47. [Google Scholar] [CrossRef]
- Barbosa, V.T.; Silva, M.A.G.; Sousa, M.G.; Gering, A.P.; Santos, H.D.; Laus, J.L. Detecção de formas amastigotas em exame parasitológico de esfregaço obtido a partir de suabe conjuntival de cães com leishmaniose visceral. Arq. Bras. Med. Vet. Zootec. 2012, 64, 1465–1470. [Google Scholar] [CrossRef][Green Version]
- Bielory, B.P.; Lari, H.B.; Mirani, N.; Kapila, R.; Fitzhugh, V.A.; Turbin, R.E. Conjunctival squamous cell carcinoma harboring Leishmania amastigotes in a human immunodeficiency virus-positive patient. Arch. Ophthalmol. 2011, 129, 1230–1231. [Google Scholar] [CrossRef][Green Version]
- Naranjo, C.; Fondevila, D.; Altet, L.; Francino, O.; Ríos, J.; Roura, X.; Peña, T. Evaluation of the presence of Leishmania spp. by real-time PCR in the lacrimal glands of dogs with leishmaniosis. Vet. J. 2012, 193, 168–173. [Google Scholar] [CrossRef]
- Strauss-Ayali, D.; Jaffe, C.L.; Burshtain, O.; Gonen, L.; Baneth, G.; Strauss-Ayali, D.; Jaffe, C.L.; Burshtain, O.; Gonen, L.; Baneth, G. Polymerase chain reaction using noninvasively obtained samples, for the detection of Leishmania infantum DNA in dogs. J. Infect. Dis. 2004, 189, 1729–1733. [Google Scholar] [CrossRef]
- de Almeida Ferreira, S.; Ituassu, L.T.; de Melo, M.N.; de Andrade, A.S.R. Evaluation of the conjunctival swab for canine visceral leishmaniasis diagnosis by PCR-hybridization in Minas Gerais State, Brazil. Vet. Parasitol. 2008, 152, 257–263. [Google Scholar] [CrossRef]
- Pereira, V.F.; Benassi, J.C.; Starke-Buzetti, W.A.; Silva, D.T.; Ferreira, H.L.; Keid, L.B.; Soares, R.M.; de Azevedo Ruiz, V.L.; de Sousa Oliveira, T.M.F. Detection of canine visceral leishmaniasis by conjunctival swab PCR. Rev. Soc. Bras. Med. Trop. 2016, 49, 104–106. [Google Scholar] [CrossRef]
- Otranto, D.; Napoli, E.; Latrofa, M.S.; Annoscia, G.; Tarallo, V.D.; Greco, G.; Lorusso, E.; Gulotta, L.; Falsone, L.; Basano, F.S.; et al. Feline and canine leishmaniosis and other vector-borne diseases in the Aeolian Islands: Pathogen and vector circulation in a confined environment. Vet. Parasitol. 2017, 236, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Leite, R.S.; de Almeida Ferreira, S.; Ituassu, L.T.; de Melo, M.N.; de Andrade, A.S.R. PCR diagnosis of visceral leishmaniasis in asymptomatic dogs using conjunctival swab samples. Vet. Parasitol. 2010, 170, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Benassi, J.C.; Benvenga, G.U.; Ferreira, H.L.; Pereira, V.F.; Keid, L.B.; Soares, R.; de Sousa Oliveira, T.M.F. Detection of Leishmania infantum DNA in conjunctival swabs of cats by quantitative real-time PCR. Exp. Parasitol. 2017, 177, 93–97. [Google Scholar] [CrossRef] [PubMed]
- de Sousa Oliveira, T.M.F.; Pereira, V.F.; Benvenga, G.U.; Martin, M.F.A.; Benassi, J.C.; da Silva, D.T.; Starke-Buzetti, W.A. Conjunctival swab PCR to detect Leishmania spp. in cats. Rev. Bras. Parasitol. Vet. 2015, 24, 220–222. [Google Scholar] [CrossRef]
- Karakuş, M.; Arserim, S.K.; Erişöz Kasap, Ö.; Pekağırbaş, M.; Aküzüm, D.; Alten, B.; Töz, S.; Özbel, Y. Vector and reservoir surveillance study in a canine and human leishmaniasis endemic area in most western part of Turkey, Karaburun. Acta Trop. 2019, 190, 177–182. [Google Scholar] [CrossRef]
- Ionică, A.M.; Deak, G.; Kalmár, Z.; Gherman, C.M.; Mihalca, A.D.; Dumitrache, M.O. Molecular Survey on Leishmania Infantum Infection in Red Foxes (Vulpes Vulpes) From Romania. Bull. Univ. Agric. Sci. Vet. Med. ClujNapoca. Vet. Med. 2017, 74, 230. [Google Scholar] [CrossRef][Green Version]
- Nsiangani, L.N.; Kaimbo Wa Kaimbo, D.; Kazumba, M.L. Anterior uveitis as the first sign of human African trypanosomiasis: A case report. Med. Sante Trop. 2016, 26, 334–336. [Google Scholar] [CrossRef]
- Morrison, W.I.; Murray, M.; Sayer, P.D.; Preston, J.M. The pathogenesis of experimentally induced Trypanosoma brucei infection in the dog. I. Tissue and organ damage. Am. J. Pathol. 1981, 102, 168–181. [Google Scholar]
- Panigrahi, P.N.; Mahendran, K.; Jena, S.C.; Behera, P.; Mahajan, S.; Arjun, K.; Dey, S. Trypanosoma evansi infection in a German shepherd dog—Apparent successful treatment using serial low dose of diminazene aceturate. Vet. Parasitol. Reg. Stud. Rep. 2015, 1–2, 70–74. [Google Scholar] [CrossRef]
- Mortelmans, J.; Neetens, A. Ocular lesions in experimental Trypanosoma brucei infection in cats. Acta Zool. Pathol. Antverp. 1975, 62, 149–172. [Google Scholar]
- Da Silva, A.S.; Pierezan, F.; Wolkmer, P.; Costa, M.M.; Oliveiro, C.B.; Tonin, A.A.; Santurio, J.M.; Lopes, S.T.A.; Monteiro, S.G. Pathological Findings Associated with Experimental Infection by Trypanosoma evansi in Cats. J. Comp. Pathol. 2010, 142, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Morales, I.; de León, M.; Morales, M.; Dalla, F.; Gutierrez, C. Ocular lesions associated with Trypanosoma evansi in experimentally infected goats. Vet. Parasitol. 2006, 141, 325–329. [Google Scholar] [CrossRef]
- Prata, A. Evolution of the clinical and epidemiological knowledge about Chagas disease 90 years after its discovery. Mem. Inst. Oswaldo Cruz 1999, 94, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Marsden, P.D. Trypanosoma cruzi infections in CFI mice. II. Infections induced by different routes. Ann. Trop. Med. Parasitol. 1967, 61, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Giddings, O.K.; Eickhoff, C.S.; Smith, T.J.; Bryant, L.A.; Hoft, D.F. Anatomical route of invasion and protective mucosal immunity in Trypanosoma cruzi conjunctival infection. Infect. Immun. 2006, 74, 5549–5560. [Google Scholar] [CrossRef]
- Bahia, M.T.; Tafuri, W.L.; Caliari, M.V.; Veloso, V.M.; Carneiro, C.M.; Coelho, G.L.L.M.; Lana, M. Comparison of Trypanosoma cruzi infection in dogs inoculated with blood or metacyclic trypomastigotes of Berenice-62 and Berenice-78 strains via intraperitoneal and conjunctival routes. Rev. Soc. Bras. Med. Trop. 2002, 35, 339–345. [Google Scholar] [CrossRef]
- Conrady, C.D.; Hanson, K.E.; Mehra, S.; Carey, A.; Larochelle, M.; Shakoor, A. The First Case of Trypanosoma cruzi-Associated Retinitis in an Immunocompromised Host Diagnosed With Pan-Organism Polymerase Chain Reaction. Clin. Infect. Dis. 2018, 67, 141–143. [Google Scholar] [CrossRef]
- Herrera, L.; Martínez, C.; Carrasco, H.; Jansen, A.M.; Urdaneta-Morales, S. Cornea as a tissue reservoir of Trypanosoma cruzi. Parasitol. Res. 2007, 100, 1395–1399. [Google Scholar] [CrossRef]
- Shiadeh, M.N.; Niyyati, M.; Fallahi, S.; Rostami, A. Human parasitic protozoan infection to infertility: A systematic review. Parasitol. Res. 2016, 115, 469–477. [Google Scholar] [CrossRef]
- Teichmann, C.; Da Silva, A.; Monteiro, S.; Barbosa, C.; Barcelos, R. Evidence of Venereal and Transplacental Transmission of Canine Visceral Leishmaniasis in Southern Brazil. ACTA Sci. Vet. 2011, 39, 1–4. [Google Scholar]
- Naucke, T.; Lorentz, S. Non-sandfly transmission of canine leishmaniasis. Tieraerztl. Umsch. 2013, 68, 121–125. [Google Scholar]
- Karkamo, V.; Kaistinen, A.; Näreaho, A.; Dillard, K.; Vainio-Siukola, K.; Vidgrén, G.; Tuoresmäki, N.; Anttila, M. The first report of autochthonous non-vector-borne transmission of canine leishmaniosis in the Nordic countries. Acta Vet. Scand. 2014, 56, 84. [Google Scholar] [CrossRef] [PubMed]
- Schubach, A.; Cuzzi-Maya, T.; Gonçalves-Costa, S.C.; Pirmez, C.; Oliveira-Neto, M.P. Leishmaniasis of glans penis. J. Eur. Acad. Dermatol. Venereol. 1998, 10, 226–228. [Google Scholar] [CrossRef] [PubMed]
- Cabello, I.; Caraballo, A.; Millan, Y. Leishmaniasis in the genital area. Rev. Inst. Med. Trop. Sao Paulo 2002, 44, 105–107. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cain, C.; Stone, M.S.; Thieberg, M.; Wilson, M.E. Nonhealing genital ulcers. Cutaneous leishmaniasis. Arch. Dermatol. 1994, 130, 1313–1315. [Google Scholar] [CrossRef]
- Andrade, Z.A.; Andrade, S.G. Some new aspects of the kala-azar pathology. (Morphologic study of 13 autopsy cases). Rev. Inst. Med. Trop. Sao Paulo 1966, 8, 259–266. [Google Scholar]
- Martínez-García, F.; Regadera, J.; Mayer, R.; Sanchez, S.; Nistal, M. Protozoan infections in the male genital tract. J. Urol. 1996, 156, 340–349. [Google Scholar] [CrossRef]
- Diniz, S.A.; Melo, M.S.; Borges, A.M.; Bueno, R.; Reis, B.P.; Tafuri, W.L.; Nascimento, E.F.; Santos, R.L. Genital lesions associated with visceral leishmaniasis and shedding of Leishmania sp. in the semen of naturally infected dogs. Vet. Pathol. 2005, 42, 650–658. [Google Scholar] [CrossRef]
- Mir, F.; Fontaine, E.; Reyes-Gomez, E.; Carlus, M.; Fontbonne, A. Subclinical leishmaniasis associated with infertility and chronic prostatitis in a dog. J. Small Anim. Pract. 2012, 53, 419–422. [Google Scholar] [CrossRef]
- Boechat, V.C.; Mendes Junior, A.A.V.; de Madeira, M.F.; Ferreira, L.C.; Figueiredo, F.B.; Rodrigues, F.; Oliveira, V.; de Oliveira, R.V.C.; Menezes, R.C. Occurrence of Leishmania infantum and associated histological alterations in the genital tract and mammary glands of naturally infected dogs. Parasitol. Res. 2016, 115, 2371–2379. [Google Scholar] [CrossRef]
- Silva, L.C.; Assis, V.P.; Ribeiro, V.M.; Tafuri, W.L.; Toledo Júnior, J.C.; Silva, S.O.; Melo, M.N.; Rachid, M.A.; Valle, G.R. Detection of Leishmania infantum in the smegma of infected dogs. Arq. Bras. Med. Vet. Zootec. 2014, 66, 731–736. [Google Scholar] [CrossRef][Green Version]
- Hernández, L.; Montoya, A.; Checa, R.; Dado, D.; Gálvez, R.; Otranto, D.; Latrofa, M.S.; Baneth, G.; Miró, G. Course of experimental infection of canine leishmaniosis: Follow-up and utility of noninvasive diagnostic techniques. Vet. Parasitol. 2015, 207, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.L.; Rodrigues, A.A.M.; Rego, I.O.P.; Santos, R.L.R.L.H.; Oliveira, R.G.; Silva, T.M.A.; Xavier, M.N.; Nascimento, E.F.; Santos, R.L.R.L.H. Genital lesions and distribution of amastigotes in bitches naturally infected with Leishmania chagasi. Vet. Parasitol. 2008, 151, 86–90. [Google Scholar] [CrossRef]
- Bouteille, B.; Buguet, A. The detection and treatment of human African trypanosomiasis. Res. Rep. Trop. Med. 2012, 3, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Apted, F. Clinical manifestations and diagnosis of sleep-ing sickness. In The African Trypanosomiases; Mulligan, H., Pott, W., Eds.; Allen & Unwin Ltd.: Crow Nest, Australia, 1970; pp. 661–683. [Google Scholar]
- Rocha, G.; Martins, A.; Gama, G.; Brandão, F.; Atouguia, J. Possible cases of sexual and congenital transmission of sleeping sickness. Lancet 2004, 363, 247. [Google Scholar] [CrossRef]
- Suganuma, K.; Narantsatsral, S.; Battur, B.; Yamasaki, S.; Otgonsuren, D.; Musinguzi, S.P.; Davaasuren, B.; Battsetseg, B.; Inoue, N. Isolation, cultivation and molecular characterization of a new Trypanosoma equiperdum strain in Mongolia. Parasit. Vectors 2016, 9, 481. [Google Scholar] [CrossRef]
- Danek, J. Microorganisms in stallion semen. Med. Weter. Vet. Med. Sci. Pract. 2005, 61, 387–390. [Google Scholar]
- Ahmed, Y.; Hagos, A.; Merga, B.; Van Soom, A.; Duchateau, L.; Goddeeris, B.; Govaere, J. Trypanosoma equiperdum in the horse - a neglected threat? Vlaams Diergeneeskd. Tijdschr. 2018, 87, 66–75. [Google Scholar]
- Al-Busadah, K.A.; El-Bahr, S.M.; Khalafalla, A.I. Serum biochemical profile and molecular detection of pathogens in semen of infertile male dromedary camels (Camelus dromedarius). Anim. Reprod. Sci. 2017, 180, 58–65. [Google Scholar] [CrossRef]
- Ogundele, F.A.; Okubanjo, O.O.; Ajanusi, O.J.; Fadason, S.T. Semen characteristics and reaction time of Yankasa rams experimentally infected with Trypanosoma evansi infection. Theriogenology 2016, 86, 667–673. [Google Scholar] [CrossRef]
- Bezerra, N.M.; Moura, G.H.F.; de Araújo, H.N.; Bezerra, F.S.B.; de Paiva, K.A.R.; de Freitas Mendonça Costa, K.M.; Costa, W.P.; Medeiros, D.A.S.; Batista, J.S. Detection of Trypanosoma vivax DNA in semen from experimentally infected goats. Vet. Res. Commun. 2018, 42, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Ikede, B.O. Genital lesions in experimental chronic Trypanosoma brucei infection in rams. Res. Vet. Sci. 1979, 26, 145–151. [Google Scholar] [CrossRef]
- Anosa, V.O.; Isoun, T.T. Further observations on the testicular pathology in Trypanosoma vivax infection of sheep and goats. Res. Vet. Sci. 1980, 28, 151–160. [Google Scholar] [CrossRef]
- Kaaya, G.P.; Oduor-Okelo, D. The effects of Trypanosoma congolense infection on the testis and epididymis of the goat. Bull. Anim. Health Prod. Afr. 1980, 28, 1–5. [Google Scholar]
- Isoun, T.T.; Anosa, V.O. Lesions in the reproductive organs of sheep and goats experimentally infected with Trypanosoma vivax. Tropenmed. Parasitol. 1974, 25, 469–476. [Google Scholar] [PubMed]
- Adamu, S.; Fatihu, M.Y.; Useh, N.M.; Mamman, M.; Sekoni, V.O.; Esievo, K.A.N. Sequential testicular and epididymal damage in Zebu bulls experimentally infected with Trypanosoma vivax. Vet. Parasitol. 2007, 143, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Anosa, V.O.; Isoun, T.T. Pathology of experimental Trypanosoma vivax infection in sheep and goats. Zentralbl. Veterinarmed. B 1983, 30, 685–700. [Google Scholar] [CrossRef]
- Claes, F.; Vodnala, S.K.; van Reet, N.; Boucher, N.; Lunden-Miguel, H.; Baltz, T.; Goddeeris, B.M.; Büscher, P.; Rottenberg, M.E. Bioluminescent imaging of Trypanosoma brucei shows preferential testis dissemination which may hamper drug efficacy in sleeping sickness. PLoS Negl. Trop. Dis. 2009, 3, e486. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, T.; Trindade, S.; Pimenta, S.; Santos, A.B.; Rijo-Ferreira, F.; Figueiredo, L.M. Trypanosoma brucei triggers a marked immune response in male reproductive organs. PLoS Negl. Trop. Dis. 2018, 12, e0006690. [Google Scholar] [CrossRef]
- Araujo, P.F.; Almeida, A.B.; Pimentel, C.F.; Silva, A.R.; Sousa, A.; Valente, S.A.; Valente, V.C.; Britto, M.M.; Rosa, A.C.; Alves, R.M.; et al. Sexual transmission of American trypanosomiasis in humans: A new potential pandemic route for Chagas parasites. Mem. Inst. Oswaldo Cruz 2017, 112, 437–446. [Google Scholar] [CrossRef]
- Bittencourt, A.L. Chagasic placentitis and congenital transmission of Chagas’ disease. Rev. Inst. Med. Trop. Sao Paulo 1963, 5, 62–67. [Google Scholar] [PubMed]
- Vianna, G. Contribuicao para o estudo da anatomia patolojica da “molestia de Carlos Chagas”. (Esquizotripanoze humana ou tireoidite parazitaria). Mem. Inst. Oswaldo Cruz 1911, 3, 276. [Google Scholar] [CrossRef][Green Version]
- Chagas, C. Tripanosomiase americana. Forma aguda da mo- 16stia. Mem. Inst. Oswaldo Cruz 1916, 8, 77. [Google Scholar] [CrossRef]
- Lamano Carvalho, T.; Ferreira, A.; Sahao, M. Alteracoes do testIculo humano na molestia de Chagas. II—Estudo morfometrico do tecido intersticial. Rev. Inst. Med. Trop. Sao Paulo 1982, 24, 214–221. [Google Scholar] [PubMed]
- Lenzi, H.L.; Castelo-Branco, M.T.; Pelajo-Machado, M.; Oliveira, D.N.; Gattass, C.R. Trypanosoma cruzi: Compromise of reproductive system in acute murine infection. Acta Trop. 1998, 71, 117–129. [Google Scholar] [CrossRef]
- Carvalho, L.O.P.; Abreu-Silva, A.L.; de Hardoim, D.J.; Tedesco, R.C.; Mendes, V.G.; da Costa, S.C.G.; da Calabrese, K.S. Trypanosoma cruzi and myoid cells from seminiferous tubules: Interaction and relation with fibrous components of extracellular matrix in experimental Chagas’ disease. Int. J. Exp. Pathol. 2009, 90, 52–57. [Google Scholar] [CrossRef]
- Ribeiro, M.; Nitz, N.; Santana, C.; Moraes, A.; Hagström, L.; Andrade, R.; Rios, A.; Sousa, A.; Dallago, B.; Gurgel-Gonçalves, R.; et al. Sexual transmission of Trypanosoma cruzi in murine model. Exp. Parasitol. 2016, 162, 1–6. [Google Scholar] [CrossRef]
- Crespillo-Andujar, C.; Díaz-Menéndez, M.; Mora-Rillo, M. Evidence for Previously Unidentified Sexual Transmission of Protozoan Parasites. Emerg. Infect. Dis. 2018, 24, 602–603. [Google Scholar] [CrossRef]
- Anderson, C. Nouveaux essais de culture de Leishmania donovani. Arch. Inst. Pasteur Tunis. 1935, 24, 131. [Google Scholar]
- Henry, A.; Guilhon, J. LE ROLE DU LAIT DANS LA TRANSMISSION DE QUELQUES PROTOZOOSES. In Le Lait; INRA Editions: Paris, France, 1944; pp. 23–35. [Google Scholar]
- Nathan-Larrier, L. Sur le passage des trypanosomes dans le lait. Rev. Pathol. Comp. 1913, 13, 282–285. [Google Scholar]
- Calvo-Méndez, M.L.; Nogueda-Torres, B.; Alejandre-Aguilar, R.; Cortés-Jiménez, M. Experimental Trypanosoma cruzi infection via contaminated water and food. Rev. Latinoam. Microbiol. 1994, 36, 67–69. [Google Scholar]
- Disko, R.; Krampitz, H.E. Occurrence of Trypanosoma cruzi in the milk of infected mice. Z. Tropenmed. Parasitol. 1971, 22, 56–66. [Google Scholar]
- Miles, M.A. Trypanosoma cruzi—Milk transmission of infection and immunity from mother to young. Parasitology 1972, 65, 1. [Google Scholar] [CrossRef]
- das Medina-Lopes, M.D.; Macêdo, V. Trypanosoma cruzi no colostro humano. Rev. Soc. Bras. Med. Trop. 1983, 16, 170. [Google Scholar] [CrossRef][Green Version]
- Jörg, M.E. The transmission of Trypanosoma cruzi via human milk. Rev. Soc. Bras. Med. Trop. 1992, 25, 83. [Google Scholar] [CrossRef]
- Amato Neto, V.; Matsubara, L.; Campos, R.; Moreira, A.A.; Pinto, P.L.; Faccioli, R.; Zugaib, M. Trypanosoma cruzi in the milk of women with chronic Chagas disease. Rev. Hosp. Clin. 1992, 47, 10–11. [Google Scholar]
- Campos, R.; Pinto, P.L.; Moreira, A.A.; Amato Neto, V.; Duarte, M.I.; de Sant’Ana, E.J.; Tiago, G.G. Experimental study on the transmission of Chagas’ disease by milk. Rev. Hosp. Clin. 1988, 43, 146–147. [Google Scholar]
- Norman, F.F.; López-Vélez, R. Chagas disease and breast-feeding. Emerg. Infect. Dis. 2013, 19, 1561–1566. [Google Scholar] [CrossRef]
- Ribeiro, R.D.; Lopes, R.A.; Garcia, T.A.; Campos, A. Histopathological study of the mammary gland in Trypanosoma cruzi-infected mice. Parasitol. Res. 1988, 74, 290–292. [Google Scholar] [CrossRef]
- Ferreira, C.S.; Martinho, P.C.; Amato Neto, V.; Cruz, R.R. Pasteurization of human milk to prevent transmission of Chagas disease. Rev. Inst. Med. Trop. Sao Paulo 2001, 43, 161–162. [Google Scholar] [CrossRef]
- Santos Ferreira, C.; Amato Neto, V.; Gakiya, E.; Bezerra, R.C.; Alarcón, R.S.R. Microwave treatment of human milk to prevent transmission of Chagas disease. Rev. Inst. Med. Trop. Sao Paulo 2003, 45, 41–42. [Google Scholar] [CrossRef]
- Canário, A.; Queiroz, M.; Cunha, G.; Cavalcante, T.; Riesz, V.; Sharma, R.; de Noronha, A.; Correia, T.; Barral-Netto, M.; Barral, A.; et al. Presence of parasite DNA in clinically unaffected nasal mucosa during cutaneous leishmaniasis caused by Leishmania (Viannia) braziliensis. Clin. Microbiol. Infect. 2019, 25, 515. [Google Scholar] [CrossRef]
- Harrison, N.; Walochnik, J.; Ramsebner, R.; Veletzky, L.; Lagler, H.; Ramharter, M. Progressive Perforation of the Nasal Septum Due to Leishmania major: A Case of Mucosal Leishmaniasis in a Traveler. Am. J. Trop. Med. Hyg. 2017, 96, 653–655. [Google Scholar] [CrossRef]
- Muñoz-Madrid, R.; Belinchón-Lorenzo, S.; Iniesta, V.; Fernández-Cotrina, J.; Parejo, J.C.; Serrano, F.J.; Monroy, I.; Baz, V.; Gómez-Luque, A.; Gómez-Nieto, L.C. First detection of Leishmania infantum kinetoplast DNA in hair of wild mammals: Application of qPCR method to determine potential parasite reservoirs. Acta Trop. 2013, 128, 706–709. [Google Scholar] [CrossRef]
- Belinchón-Lorenzo, S.; Muñoz-Madrid, R.; Grano, F.G.; Iniesta, V.; Fernández-Cotrina, J.; Parejo, J.C.; Monroy, I.; Baz, V.; Gómez-Luque, A.; Barneto, J.L.; et al. Application of qPCR method to hair and cerumen samples for the diagnosis of canine leishmaniosis in Araçatuba, Brazil. Vet. Parasitol. Reg. Stud. Rep. 2019, 15, 100267. [Google Scholar] [CrossRef]
- Ferro, C.; Cadena, H.; Travi, B.L.; Tabares, C.J.; Osorio, Y. Canine visceral leishmaniasis in Colombia: Relationship between clinical and parasitologic status and infectivity for sand flies. Am. J. Trop. Med. Hyg. 2001, 64, 119–124. [Google Scholar]
- Goodrich, E.S.; Sears, S.C.; Sorrells, T.; Radike, J.K.; Miladi, A.; Glass, J.S. A Case of Cutaneous Leishmaniasis guyanensis Mimicking Otitis Externa. Mil. Med. 2017, 182, e1969–e1972. [Google Scholar] [CrossRef]
- Penn, D.; Potts, W.K. Chemical signals and parasite-mediated sexual selection. Trends Ecol. Evol. 1998, 13, 391–396. [Google Scholar] [CrossRef]
- de Oliveira, L.S.; de Rodrigues, F.M.; de Oliveira, F.S.; Mesquita, P.R.R.; Leal, D.C.; Alcântara, A.C.; Souza, B.M.; Franke, C.R.; de Pereira, P.A.P.; de Andrade, J.B. Headspace solid phase microextraction/gas chromatography-mass spectrometry combined to chemometric analysis for volatile organic compounds determination in canine hair: A new tool to detect dog contamination by visceral leishmaniasis. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2008, 875, 392–398. [Google Scholar] [CrossRef]
- Magalhães-Junior, J.T.; Mesquita, P.R.R.; Oliveira, W.F.; Oliveira, F.S.; Franke, C.R.; de Rodrigues, F.M.; de Andrade, J.B.; Barrouin-Melo, S.M. Identification of biomarkers in the hair of dogs: New diagnostic possibilities in the study and control of visceral leishmaniasis. Anal. Bioanal. Chem. 2014, 406, 6691–6700. [Google Scholar] [CrossRef]
- Iniesta, V.; Belinchón-Lorenzo, S.; Soto, M.; Fernández-Cotrina, J.; Muñoz-Madrid, R.; Monroy, I.; Baz, V.; Gómez-Luque, A.; Parejo, J.C.; Alonso, C.; et al. Detection and chronology of parasitic kinetoplast DNA presence in hair of experimental Leishmania major infected BALB/c mice by Real Time PCR. Acta Trop. 2013, 128, 468–472. [Google Scholar] [CrossRef][Green Version]
- Ortega, M.V.; Moreno, I.; Domínguez, M.; de la Cruz, M.L.; Martín, A.B.; Rodríguez-Bertos, A.; López, R.; Navarro, A.; González, S.; Mazariegos, M.; et al. Application of a specific quantitative real-time PCR (qPCR) to identify Leishmania infantum DNA in spleen, skin and hair samples of wild Leporidae. Vet. Parasitol. 2017, 243, 92–99. [Google Scholar] [CrossRef]
- de Sousa Gonçalves, R.; Franke, C.R.; Magalhães-Junior, J.T.; Souza, B.M.P.S.; Solcà, M.S.; Larangeira, D.F.; Barrouin-Melo, S.M. Association between Leishmania infantum DNA in the hair of dogs and their infectiousness to Lutzomyia longipalpis. Vet. Parasitol. 2016, 232, 43–47. [Google Scholar] [CrossRef]
- Karram, S.; Loya, A.; Hamam, H.; Habib, R.H.; Khalifeh, I. Transepidermal elimination in cutaneous leishmaniasis: A multiregional study. J. Cutan. Pathol. 2012, 39, 406–412. [Google Scholar] [CrossRef]
- Vasconcellos, C.; Sotto, M.N. Experimental cutaneous leishmaniasis: Transmission electron microscopy of the inoculation site. Int. J. Exp. Pathol. 1997, 78, 81–89. [Google Scholar] [CrossRef]
- de Mendonça, I.L.; Batista, J.F.; Alves, L.C. Leishmania (infantum) chagasi in canine urinary sediment. Rev. Bras. Parasitol. Vet. 2015, 24, 92–94. [Google Scholar] [CrossRef][Green Version]
- Ghosh, P.; Bhaskar, K.R.H.; Hossain, F.; Khan, M.A.A.; Vallur, A.C.; Duthie, M.S.; Hamano, S.; Salam, M.A.; Huda, M.M.; Khan, M.G.M.; et al. Evaluation of diagnostic performance of rK28 ELISA using urine for diagnosis of visceral leishmaniasis. Parasit. Vectors 2016, 9, 383. [Google Scholar] [CrossRef]
- Vogt, F.; Mengesha, B.; Asmamaw, H.; Mekonnen, T.; Fikre, H.; Takele, Y.; Adem, E.; Mohammed, R.; Ritmeijer, K.; Adriaensen, W.; et al. Antigen Detection in Urine for Noninvasive Diagnosis and Treatment Monitoring of Visceral Leishmaniasis in Human Immunodeficiency Virus Coinfected Patients: An Exploratory Analysis from Ethiopia. Am. J. Trop. Med. Hyg. 2018, 99, 957–966. [Google Scholar] [CrossRef]
- Fernández-Roldán, C.; Rodríguez-Grangér, J.; Javier Martínez, R.; López-Ruz, M.A.; Navarro-Marí, J.M.; Gutiérrez-Fernández, J. Performance of the KAtex test in screening and diagnosis for visceral leishmaniasis in a reference hospital. Rev. Esp. Quimioter. 2017, 30, 464–467. [Google Scholar]
- Salam, M.A.; Khan, M.G.M.; Mondal, D. Urine antigen detection by latex agglutination test for diagnosis and assessment of initial cure of visceral leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 2011, 105, 269–272. [Google Scholar] [CrossRef]
- Corral, R.S.; Altcheh, J.M.; Freilij, H.L. Presence of IgM antibodies to Trypanosoma cruzi urinary antigen in sera from patients with acute Chagas’ disease. Int. J. Parasitol. 1998, 28, 589–594. [Google Scholar] [CrossRef]
- García-García, J.A.; Martín-Sánchez, J.; Gállego, M.; Rivero-Román, A.; Camacho, A.; Riera, C.; Morillas-Márquez, F.; Vergara, S.; Macías, J.; Pineda, J.A. Use of noninvasive markers to detect Leishmania infection in asymptomatic human immunodeficiency virus-infected patients. J. Clin. Microbiol. 2006, 44, 4455–4458. [Google Scholar] [CrossRef]
- Abeijon, C.; Dilo, J.; Tremblay, J.M.; Viana, A.G.; Bueno, L.L.; Carvalho, S.F.G.; Fujiwara, R.T.; Shoemaker, C.B.; Campos-Neto, A. Use of VHH antibodies for the development of antigen detection test for visceral leishmaniasis. Parasite Immunol. 2018, 40, e12584. [Google Scholar] [CrossRef]
- Cruz, I.; Chicharro, C.; Nieto, J.; Bailo, B.; Cañavate, C.; Figueras, M.-C.; Alvar, J. Comparison of new diagnostic tools for management of pediatric Mediterranean visceral leishmaniasis. J. Clin. Microbiol. 2006, 44, 2343–2347. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Abeijon, C.; Campos-Neto, A. Potential non-invasive urine-based antigen (protein) detection assay to diagnose active visceral leishmaniasis. PLoS Negl. Trop. Dis. 2013, 7, e2161. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Abeijon, C.; Singh, O.P.; Chakravarty, J.; Sundar, S.; Campos-Neto, A. Novel Antigen Detection Assay to Monitor Therapeutic Efficacy of Visceral Leishmaniasis. Am. J. Trop. Med. Hyg. 2016, 95, 800–802. [Google Scholar] [CrossRef] [PubMed]
- Boni, S.M.; Oyafuso, L.K.; de Soler, R.C.; Lindoso, J.A.L. Efficiency of noninvasive sampling methods (swab) together with Polymerase Chain Reaction (PCR) for diagnosing American Tegumentary Leishmaniasis. Rev. Inst. Med. Trop. Sao Paulo 2017, 59, e38. [Google Scholar] [CrossRef]
- Aschar, M.; de Oliveira, E.T.B.; Laurenti, M.D.; Marcondes, M.; Tolezano, J.E.; Hiramoto, R.M.; Corbett, C.E.P.; da Matta, V.L.R. Value of the oral swab for the molecular diagnosis of dogs in different stages of infection with Leishmania infantum. Vet. Parasitol. 2016, 225, 108–113. [Google Scholar] [CrossRef]
- de Almeida Ferreira, S.; Leite, R.S.; Ituassu, L.T.; Almeida, G.G.; Souza, D.M.; Fujiwara, R.T.; de Andrade, A.S.R.; Melo, M.N. Canine skin and conjunctival swab samples for the detection and quantification of Leishmania infantum DNA in an endemic urban area in Brazil. PLoS Negl. Trop. Dis. 2012, 6, e1596. [Google Scholar] [CrossRef][Green Version]
- Di Muccio, T.; Veronesi, F.; Antognoni, M.T.; Onofri, A.; Piergili Fioretti, D.; Gramiccia, M. Diagnostic value of conjunctival swab sampling associated with nested PCR for different categories of dogs naturally exposed to Leishmania infantum infection. J. Clin. Microbiol. 2012, 50, 2651–2659. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Morell, P.; Arboix, M.; Alberola, J.; Ferrer, L. Prevalence of Leishmania infantum infection in dogs living in an area of canine leishmaniasis endemicity using PCR on several tissues and serology. J. Clin. Microbiol. 2001, 39, 560–563. [Google Scholar] [CrossRef] [PubMed]
- Ceccarelli, M.; Galluzzi, L.; Sisti, D.; Bianchi, B.; Magnani, M. Application of qPCR in conjunctival swab samples for the evaluation of canine leishmaniasis in borderline cases or disease relapse and correlation with clinical parameters. Parasit. Vectors 2014, 7, 460. [Google Scholar] [CrossRef] [PubMed]
- Carvalho Ferreira, A.L.; Carregal, V.M.; de Almeida Ferreira, S.; Leite, R.S.; de Andrade, A.S.R. Detection of Leishmania infantum in 4 different dog samples by real-time PCR and ITS-1 nested PCR. Diagn. Microbiol. Infect. Dis. 2014, 78, 418–421. [Google Scholar] [CrossRef] [PubMed]
- Geisweid, K.; Weber, K.; Sauter-Louis, C.; Hartmann, K. Evaluation of a conjunctival swab polymerase chain reaction for the detection of Leishmania infantum in dogs in a non-endemic area. Vet. J. 2013, 198, 187–192. [Google Scholar] [CrossRef]
- Pilatti, M.M.; de Ferreira, S.A.; de Melo, M.N.; de Andrade, A.S.R. Comparison of PCR methods for diagnosis of canine visceral leishmaniasis in conjunctival swab samples. Res. Vet. Sci. 2009, 87, 255–257. [Google Scholar] [CrossRef]
- Gao, C.; Ding, D.; Wang, J.; Steverding, D.; Wang, X.; Yang, Y.; Shi, F. Development of a LAMP assay for detection of Leishmania infantum infection in dogs using conjunctival swab samples. Parasit. Vectors 2015, 8, 370. [Google Scholar] [CrossRef]
- Belinchón-Lorenzo, S.; Parejo, J.C.; Iniesta, V.; Fernández-Cotrina, J.; Muñoz-Madrid, R.; Monroy, I.; Baz, V.; Gómez-Luque, A.; Serrano-Aguilera, F.J.; Barneto, J.L.; et al. First detection of Leishmania kDNA in canine cerumen samples by qPCR. Vet. Parasitol. 2016, 228, 65–68. [Google Scholar] [CrossRef]
- Belinchón-Lorenzo, S.; Iniesta, V.; Parejo, J.C.; Fernández-Cotrina, J.; Muñoz-Madrid, R.; Soto, M.; Alonso, C.; Gómez Nieto, L.C. Detection of Leishmania infantum kinetoplast minicircle DNA by Real Time PCR in hair of dogs with leishmaniosis. Vet. Parasitol. 2013, 192, 43–50. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Nakagawa, S.; Noble, D.W.A.; Senior, A.M.; Lagisz, M. Meta-evaluation of meta-analysis: Ten appraisal questions for biologists. BMC Biol. 2017, 15, 18. [Google Scholar] [CrossRef]
- Freeman, M.; Tukey, J. Transformations related to the angular and the square root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- Barendregt, J.J.; Doi, S.A.; Lee, Y.Y.; Norman, R.E.; Vos, T. Meta-analysis of prevalence. J. Epidemiol. Community Health 2013, 67, 974–978. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
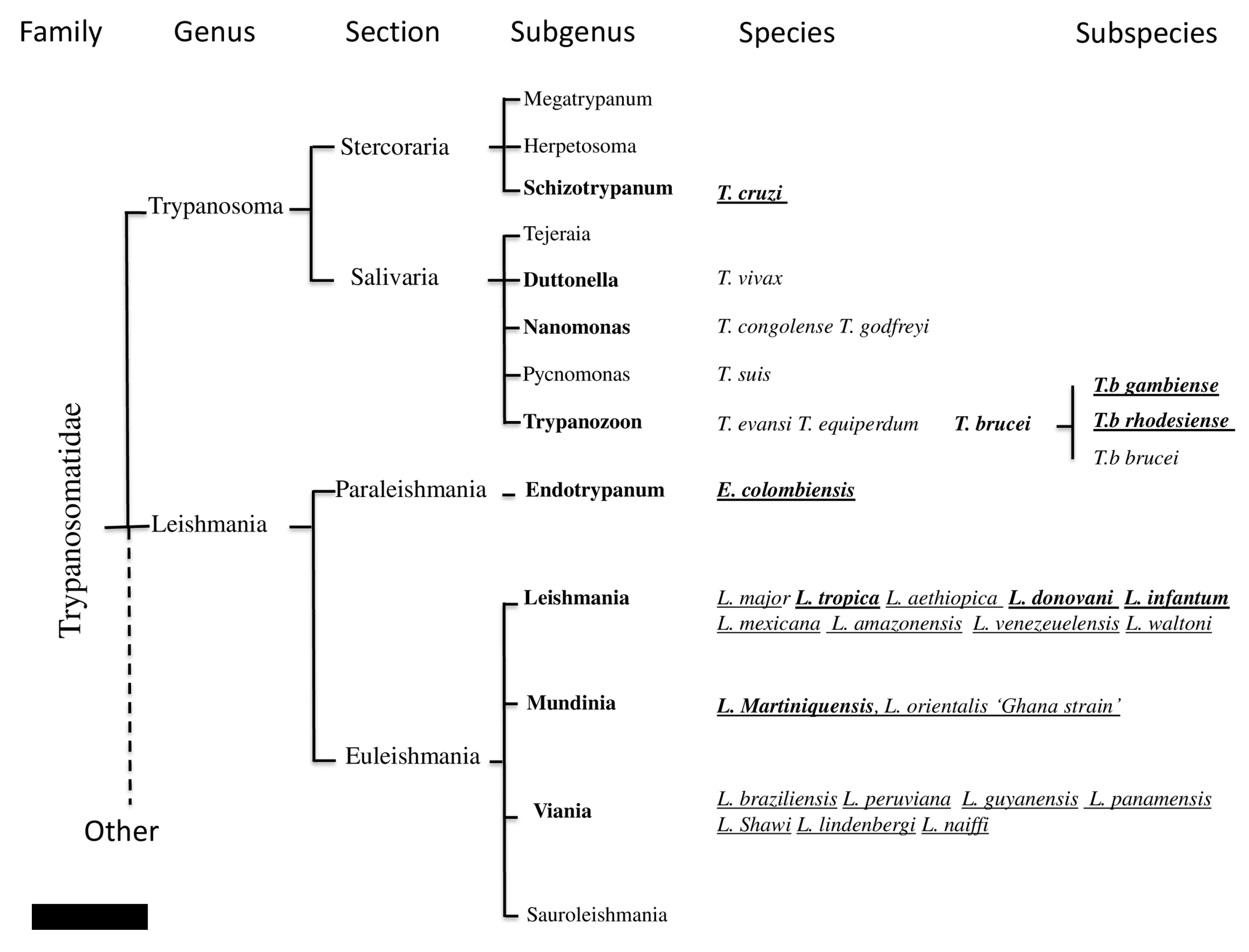
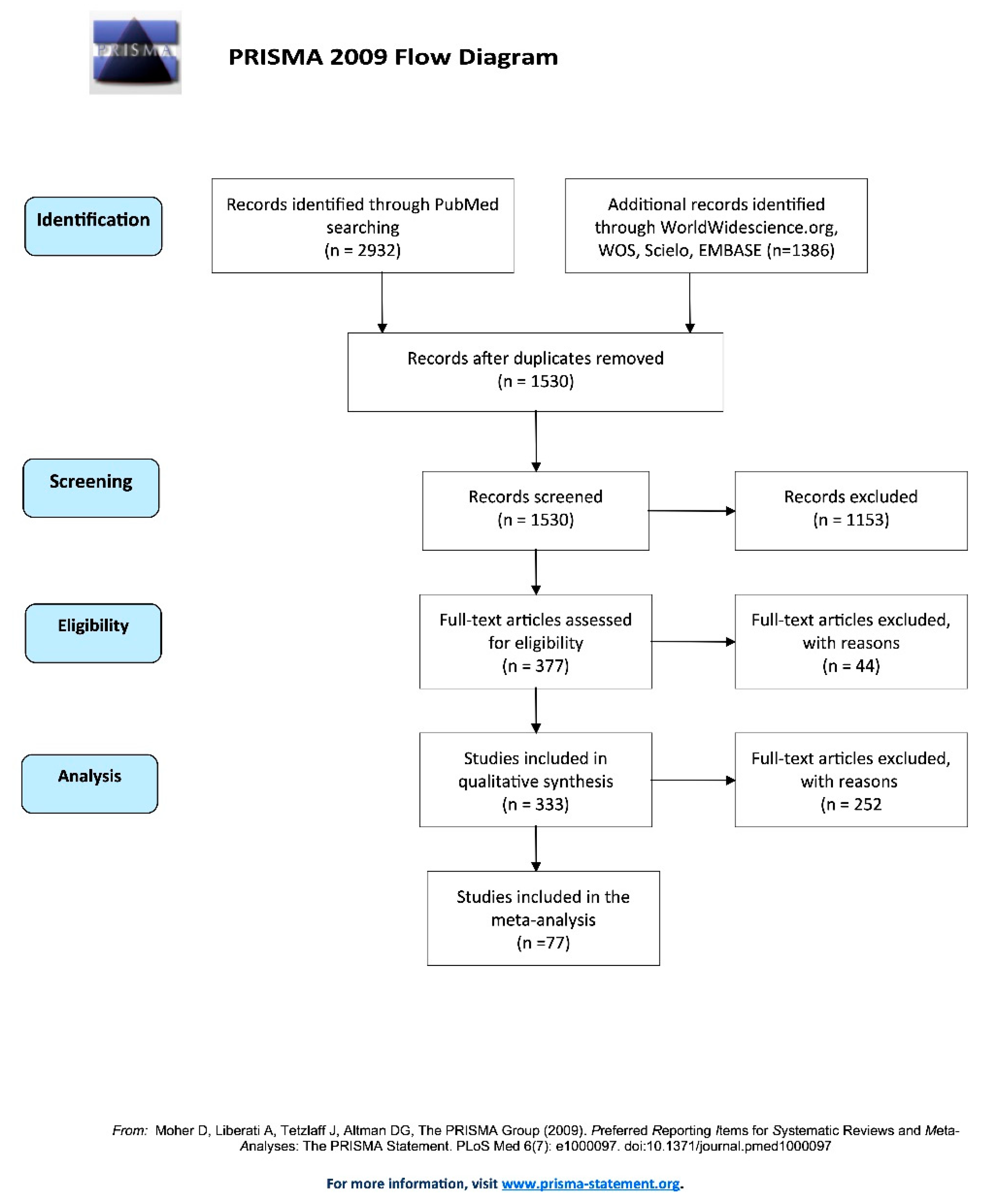
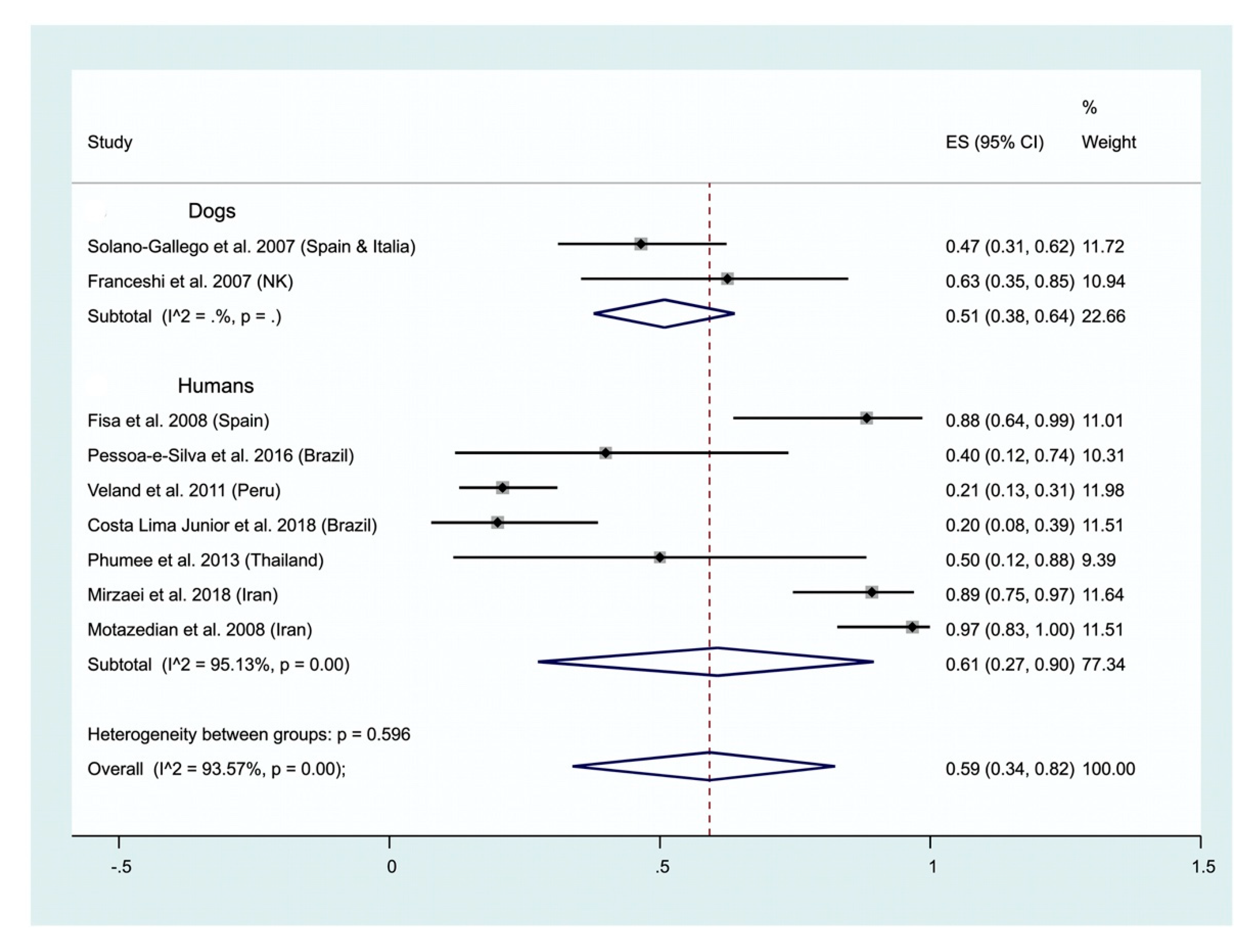
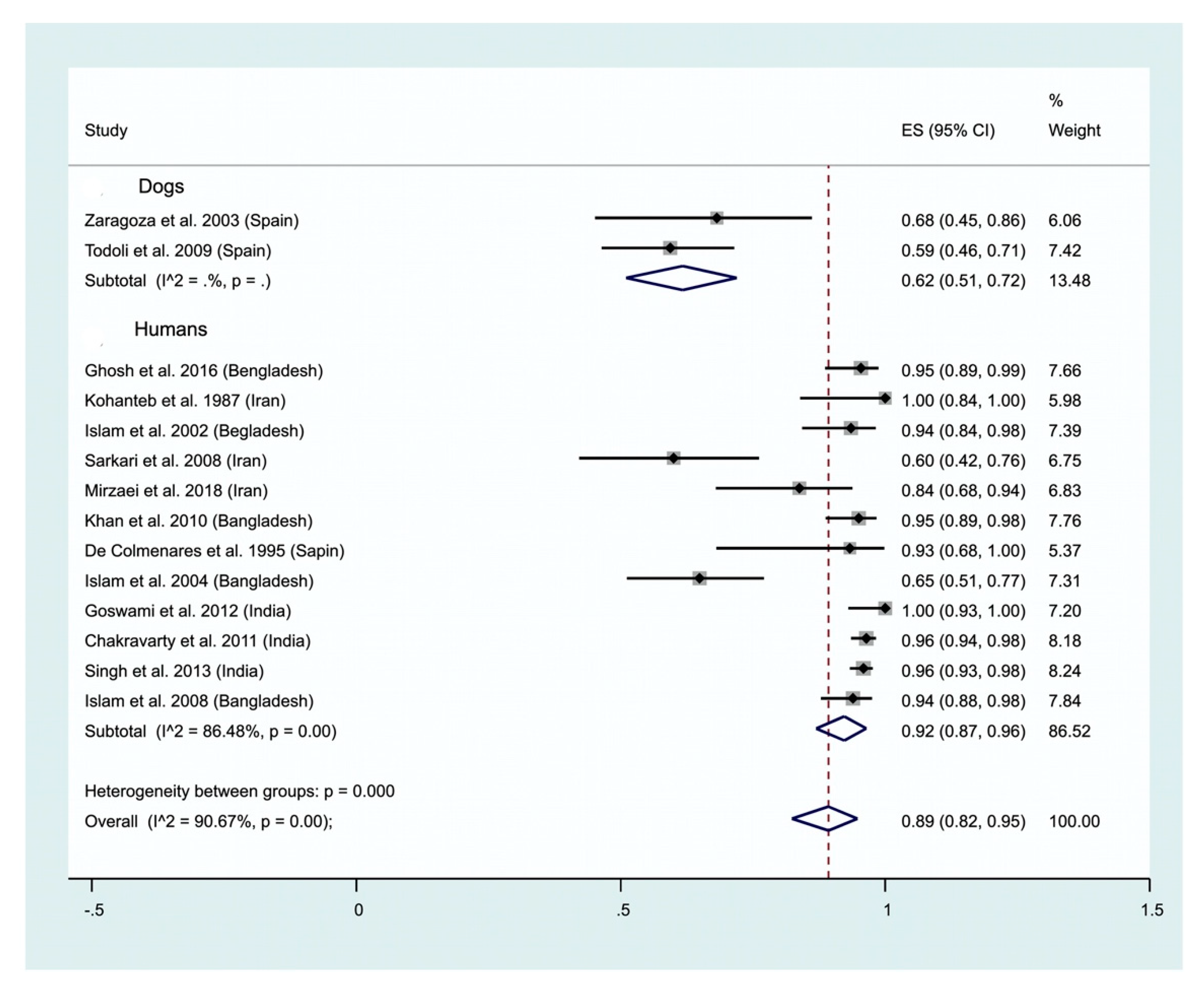
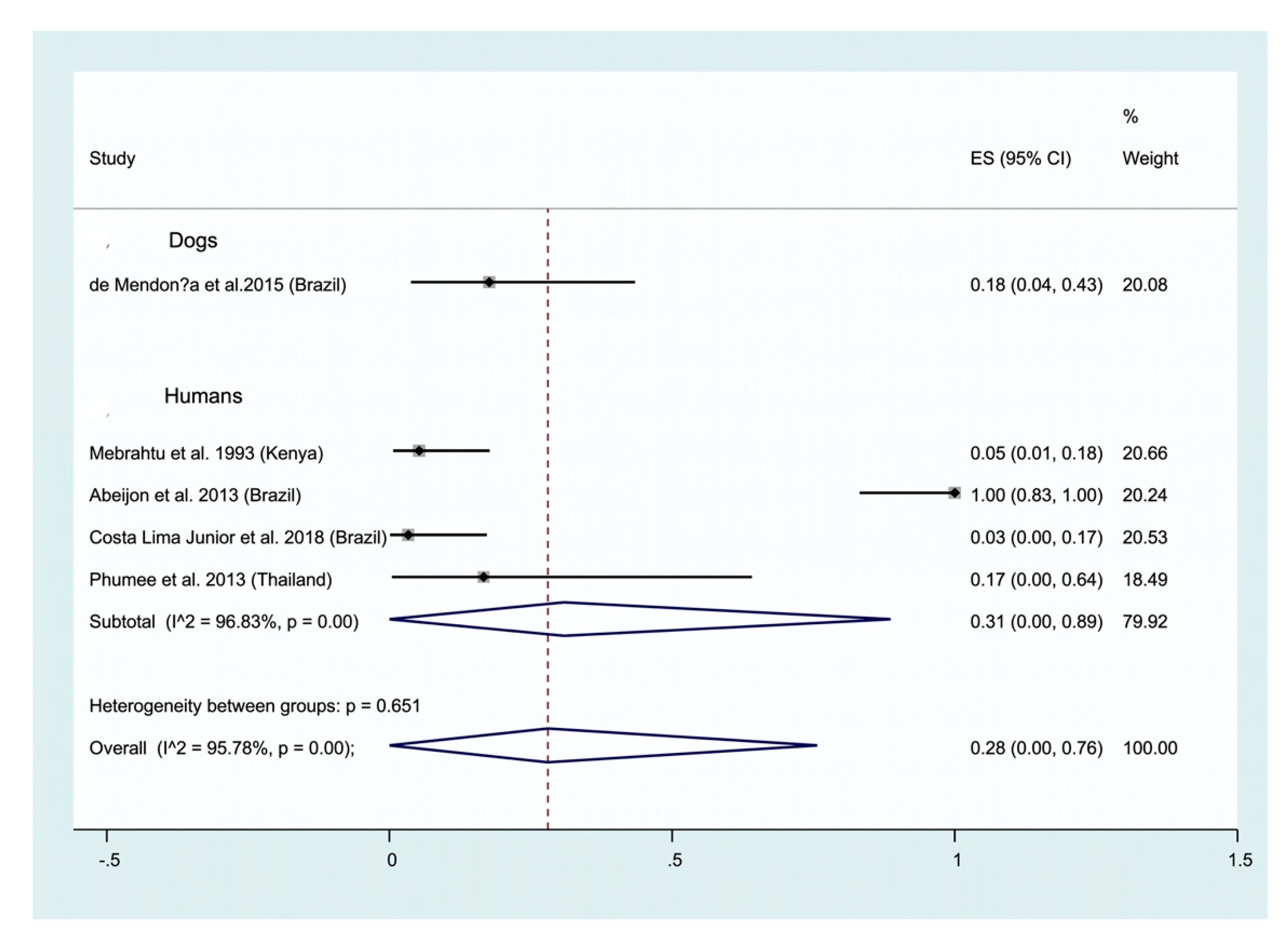
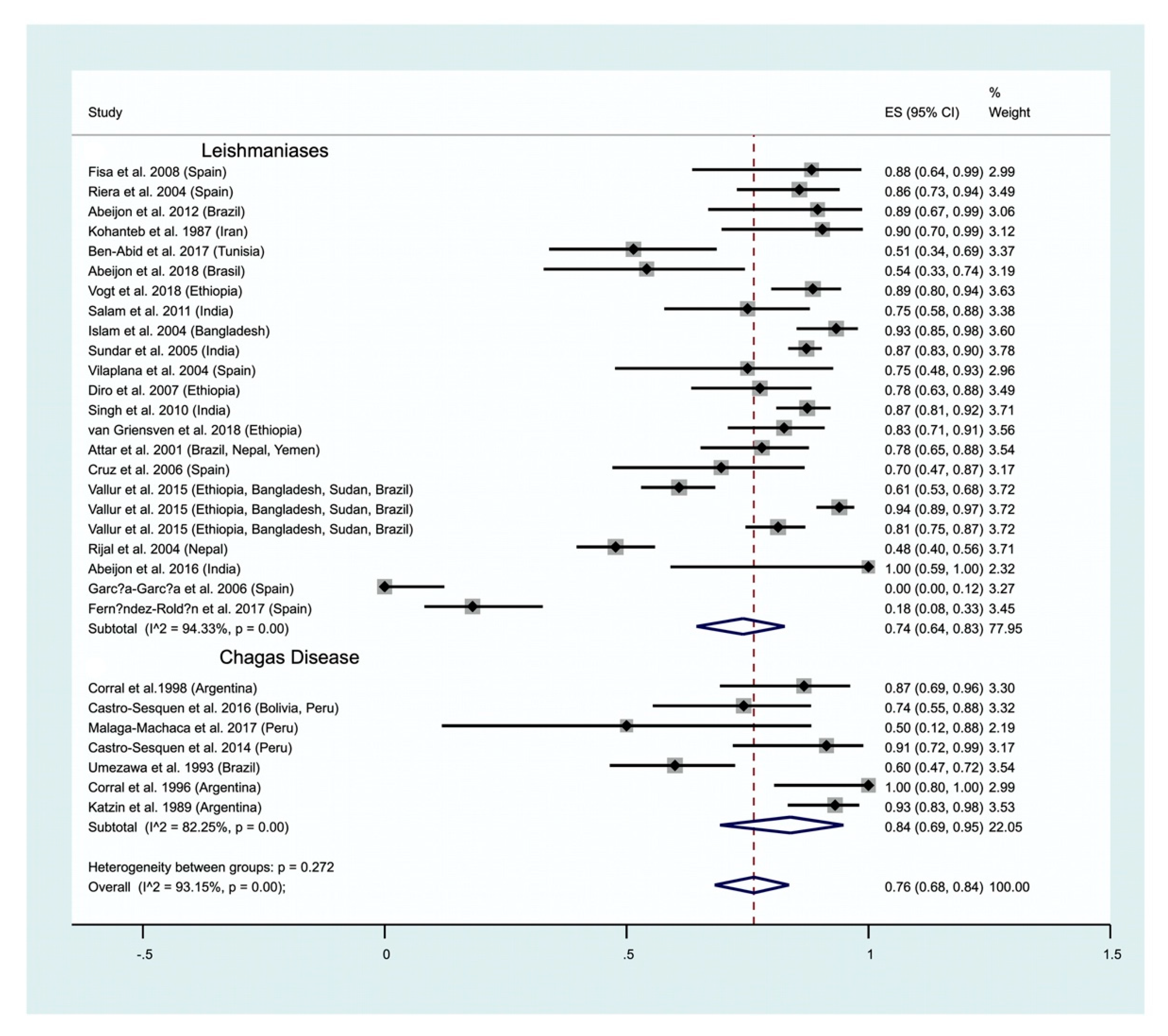
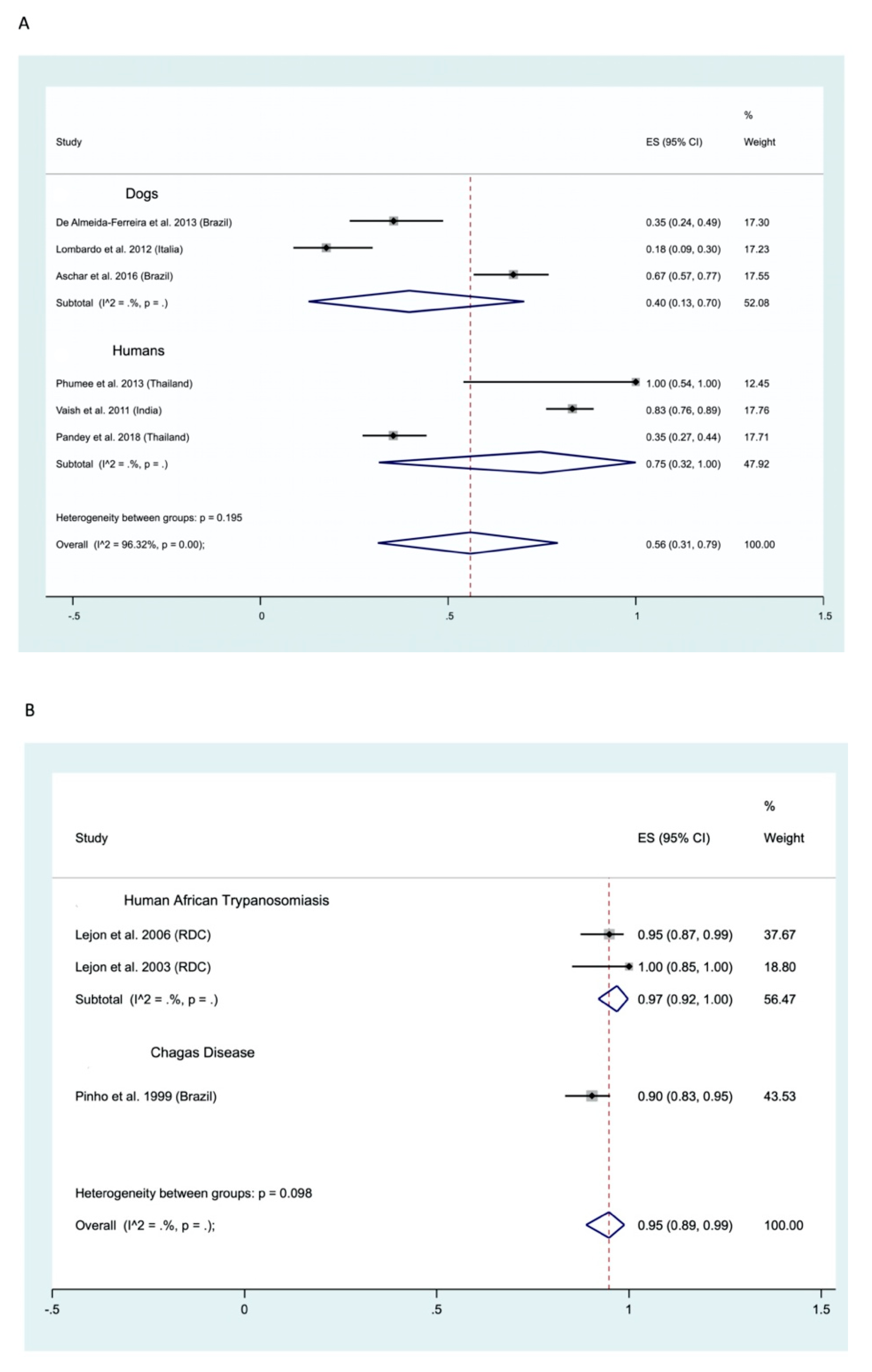
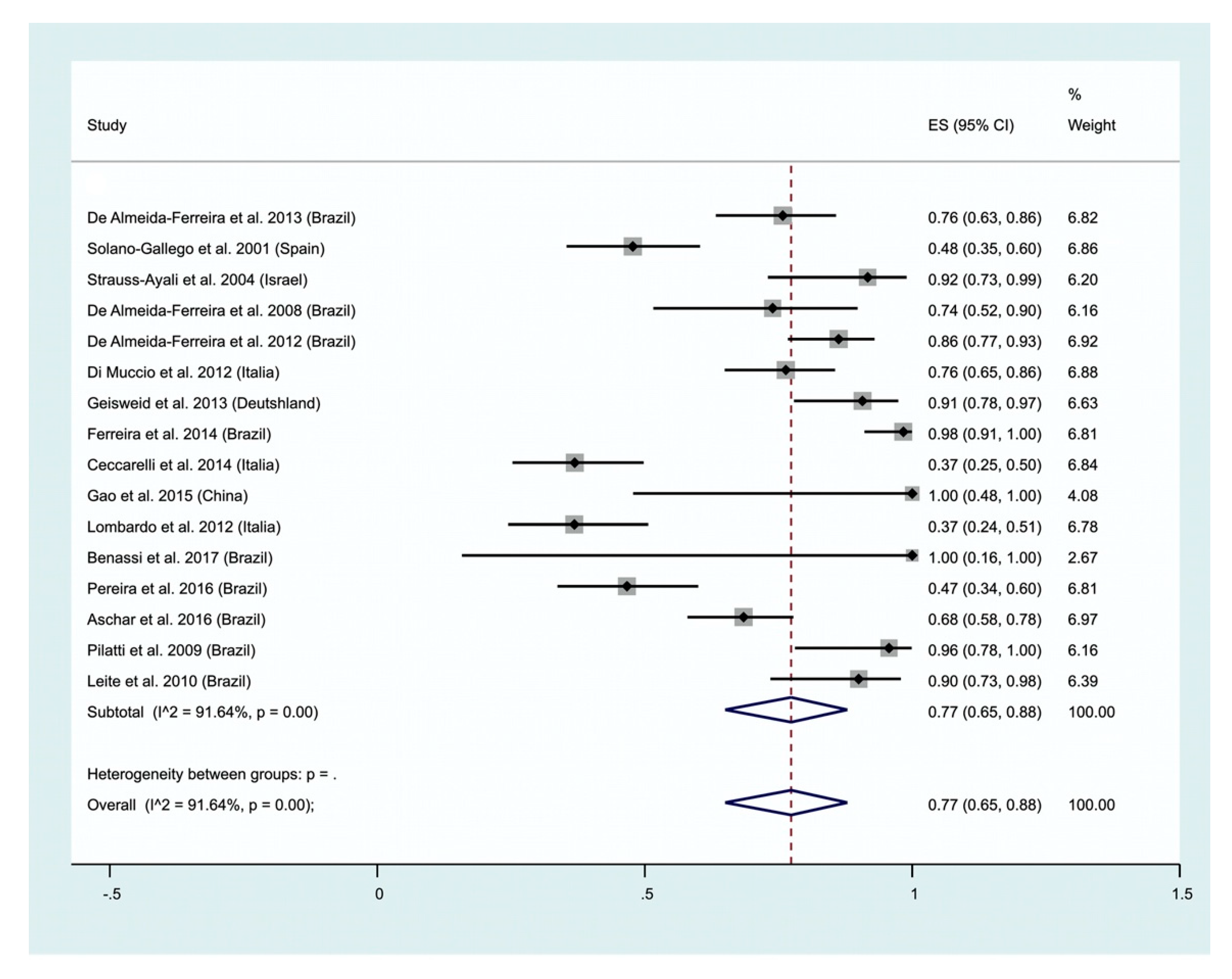
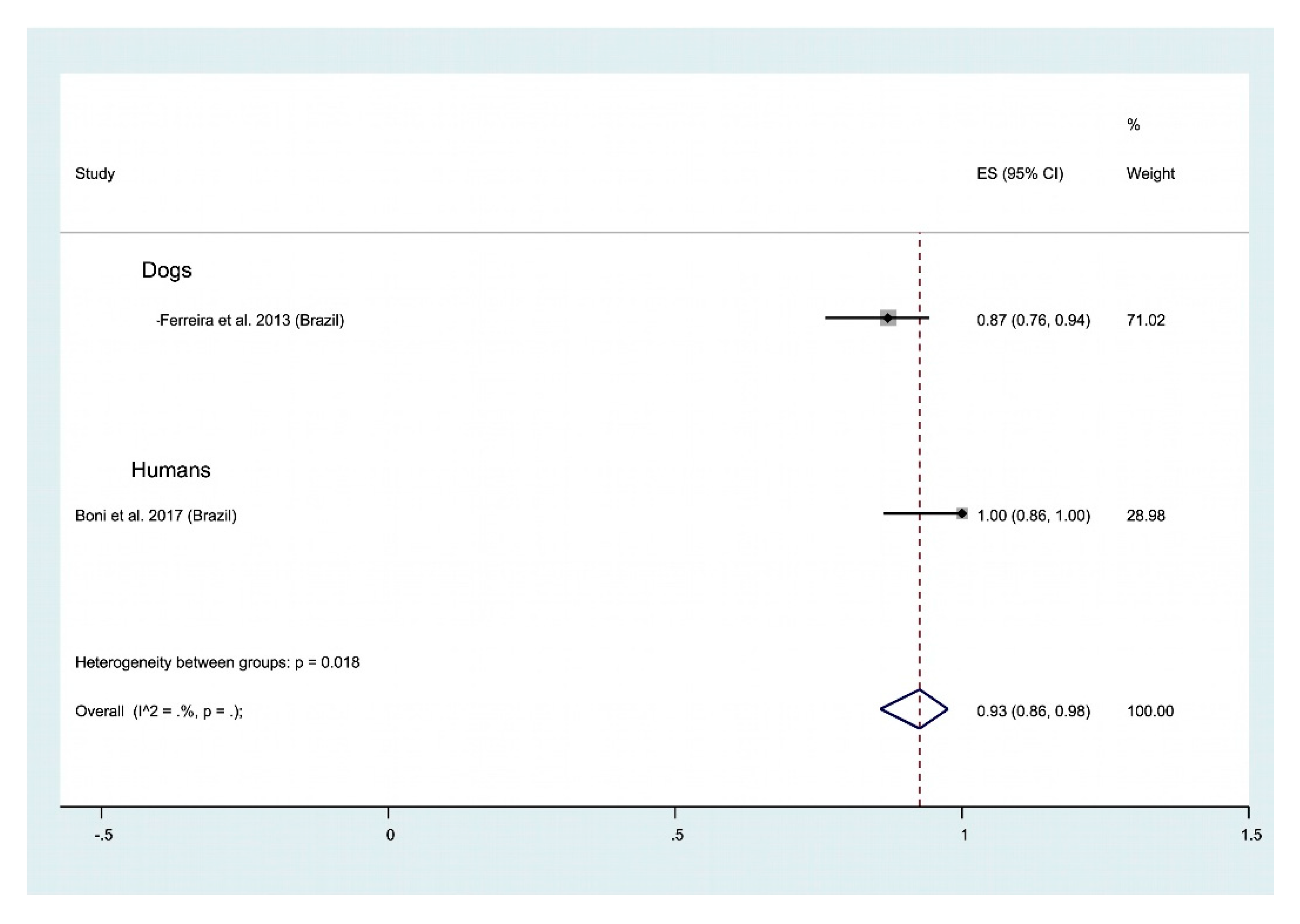
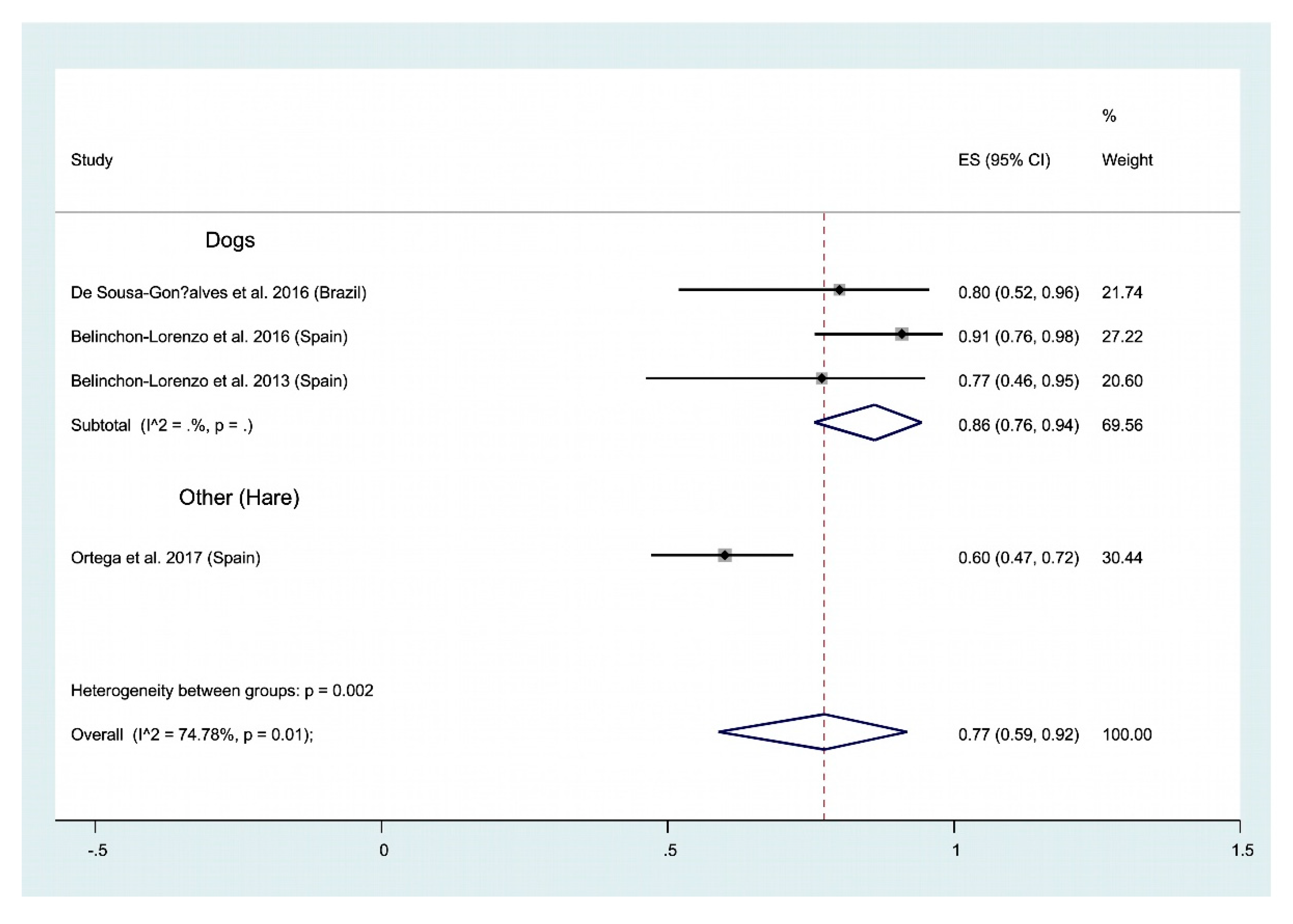
| Methodologies | Quantification | Culture | CD Detection and Identification | AT Detection and Identification | HAT Detection and Identification | Leishmania Detection and Identification | Ref | ||
|---|---|---|---|---|---|---|---|---|---|
| DNA/RNA-based Methods | PCR | PCR/qPCR/Multiplex | yes | no | yes/DTU | yes/sp | yes/sp | yes/sp | [77,78,79] |
| PCR–OC | no | no | NA/NA | yes/sp | yes/sp | yes/sp | [80,81] | ||
| PCR–ELISA | yes | no | NA/NA | yes/sp | yes/sp | yes/sp | [82,83,84,85] | ||
| PCR–HRM | no | no | yes/DTU | NA/NA | NA/NA | yes/sp | [63,86] | ||
| PCR–RFLP | no | no | yes/DTU | yes/sp | yes/sp | yes/sp | [87,88,89] | ||
| PCR-sequencing | no | no | yes/DTU | yes/sp | yes/sp | yes/sp | [78,88] | ||
| Other | PFGE | no | yes | yes/NA | yes/sp | yes/sp | no/sp | [88,90,91] | |
| NASBA | no | no | NA/NA | NA/NA | yes/sp | yes/sp | [81] | ||
| LAMP | poss | no | yes/no | yes/sp | yes/sp | yes/sp | [69,92] | ||
| Non DNA-based Methods | Parasitology | Microscopic examination | yes | no | yes/no | yes/no | yes/no | yes/no | [2,19,27,93] |
| In vitro parasite culture | no | yes | yes/no | yes/no | yes/no | yes/no | / | ||
| Isolation in experimental animals | no | no | yes/no | NA/NA | yes/no | yes/no | / | ||
| Xenodiagnosis | no | no | yes/no | NA/NA | yes/no | yes/no | [94,95,96,97] | ||
| Dermal diagnostic tests | no | no | NA/NA | NA/NA | NA/NA | yes/no | [98] | ||
| Immunology/Serology | ELISA Ab | no | no | yes/no | yes/no | yes/no | yes/no | [99,100,101] | |
| ELISA Ag | no | no | yes/no | yes/no | NA/NA | yes/no | [102] | ||
| IFAT | no | no | yes/no | yes/no | yes/no | yes/gen | [71,72,73,103,104] | ||
| ICT Ag | no | no | NA/NA | NA/NA | NA/NA | yes/gen | [105] | ||
| ICT Ab | no | no | NA/NA | NA/NA | yes/no | yes/no | [106,107] | ||
| DAT/CATT | no | no | yes/yes | yes/yes | yes/yes | yes/yes | [74,99,100,108] | ||
| Western blot | no | no | yes/no | NA/NA | NA/NA | yes/sp | [109,110] | ||
| Protein-based methods | MLEE | no | yes | no/DTU | no/sp | no/sp | no/sp | / | |
| MALDI-TOF | no | yes | no/DTU | NA/NA | no/sp | no/sp | [111,112] | ||
| Ref | Author/year | Country | Pathogen | Host | Clinic | HIV | Methodology | Sample | Sa Size |
|---|---|---|---|---|---|---|---|---|---|
| [119] | Mebrahtu 1993 | Kenya | L. donovani | Human | VL | No | Parasitology | U | 64 |
| [120] | da Costa Lima 2018 | Brazil | L. infantum | Human | VL | No | Parasitology and genetic material | U | 30 |
| [133] | Pessoa-E-Silva 2016 | Brazil | L. infantum | Human | VL | Yes | Parasitology | U | 18 |
| [354] | de Mendonça 2015 | Brazil | L. infantum | Dog | CVL | NA | Parasitology | U | 17 |
| [130] | Veland 2011 | Peru | Leishmania spp. | Human | CL-MCL | No | Genetic material | U | 86 |
| [131] | Solano-Gallego 2007 | Spain and Italy | L. infantum | Dog | CVL | NA | Genetic material | U | 43 |
| [109] | Mirzaei 2018 | Iran | Leishmania spp. | Human | VL-CL | No | Genetic material-Immunology/Ab | U | 37 |
| [168] | Motazedian 2008 | Iran | L. infantum | Human | VL | No | Genetic material | U | 30 |
| [121] | Fisa 2008 | Spain | L. infantum | Human | VL | Yes | Genetic material | U | 17 |
| [135] | Franceschi 2007 | NK | Leishmania spp. | Dog | CVL | NA | Genetic material | U | 16 |
| [167] | Sundar 2005 | India | L. donovani | Human | VL | No | Immunology/Ag | U | 382 |
| [144] | Singh 2013 | India | L. donovani | Human | VL | No | Immunology/Ab-Ag | U | 365 |
| [145] | Chakravarty 2011 | India | L. donovani | Human | VL | No | Immunology/Ab | U | 280 |
| [163] | Vallur 2015 | Ethiopia, Bangladesh, Sudan, Brazil | Leishmania spp. | Human | VL | No | Immunology/Ag | U | 166 |
| [165] | Rijal 2004 | Nepal | L. donovani | Human | VL | No | Immunology/Ab | U | 155 |
| [105] | Singh 2010 | India | L. donovani | Human | VL | No | Immunology/Ag-Ab | U | 150 |
| [141] | Islam 2008 | Bangladesh | L. donovani | Human | VL | No | Immunology/Ab | U | 115 |
| [143] | Khan 2010 | Bangladesh | L. donovani | Human | VL | No | Immunology/Ab | U | 100 |
| [355] | Ghosh 2016 | Bangladesh | L. donovani | Human | VL | No | Immunology/Ab | U | 87 |
| [148] | Diro 2007 | Ethiopia | L. donovani | Human | VL | No | Immunology/Ag-Ab | U | 87 |
| [356] | Vogt 2018 | Ethiopia | L. donovani | Human | VL | No | Immunology/Ag | U | 87 |
| [140] | Islam 2004 | Bangladesh | L. donovani | Human | VL | No | Immunology/Ab | U | 75 |
| [156] | Todolí 2009 | Spain | L. infantum | Dog | CVL | NA | Immunology/Ab | U | 64 |
| [171] | van Griensven 2018 | Ethiopia | L. donovani | Human | VL | No | Immunology/Ag | U | 63 |
| [139] | Islam 2002 | Bangladesh | L. donovani | Human | VL | No | Immunology/Ab | U | 62 |
| [194] | Umezawa 1993 | Brazil | T. cruzi | Human | CD | No | Immunology/Ag | U | 60 |
| [76] | Attar 2001 | Brazil, Nepal, Yemen | Leishmania spp. | Human | VL | No | Immunology/Ag | U | 59 |
| [193] | Katzin 1989 | Argentina | T. cruzi | Human | CD | No | Immunology/Ag | U | 58 |
| [169] | Riera 2004 | Spain | L. infantum | Human | VL | Yes | Immunology/Ag | U | 49 |
| [357] | Fernández-Roldán 2017 | Spain | L. infantum | Human | VL | No | Immunology/Ag | U | 44 |
| [146] | Goswami 2012 | India | L. donovani | Human | VL-PKDL | yes | Immunology/Ab | U | 42 |
| [358] | Salam 2011 | India | L. donovani | Human | VL | No | Immunology/Ag | U | 36 |
| [99] | Sarkari 2008 | Iran? | Leishmania spp. | Human | VL | No | Immunology/Ag-Ab | U | 35 |
| [129] | Ben-Abid 2017 | Tunisia | L. infantum | Human | VL | No | Immunology/Ag | U-S | 35 |
| [201] | Castro-Sesquen 2016 | Bolivia, Peru | T. cruzi | Human | CD | No | Immunology/Ag | U | 31 |
| [359] | Corral 1998 | Argentina, Paraguay | T. cruzi | Human | CD | No | Immunology/Ab | U | 30 |
| [360] | García-García 2006 | Spain | L. infantum | Human | VL | Yes | Immunology/Ab | U | 28 |
| [361] | Abeijon 2018 | Brazil | L. infantum | Human | VL | No | Immunology/Ag | U | 24 |
| [362] | Cruz 2006 | Spain | L. infantum | Human | VL | No | Immunology/Ag | U | 23 |
| [200] | Castro-Sesquen 2014 | Bolivia, Peru | T. cruzi | Human | CD | No | Immunology/Ag | U | 23 |
| [153] | Zaragoza 2003 | Spain | L. infantum | Dog | CVL | NA | Immunology/Ag | U | 22 |
| [363] | Abeijon 2013 | Brazil | L. infantum | Human | VL | No | Immunology/Ag | U | 20 |
| [138] | Kohanteb 1987 | Iran | L. infantum? | Human | VL | No | Immunology/Ag-Ab | U | 21 |
| [159] | Abeijon 2012 | Brazil | L. infantum | Human | VL | No | Immunology/Ag | U | 19 |
| [192] | Corral 1996 | Argentina | T. cruzi | Human | CD | No | Immunology/Ag | U | 17 |
| [166] | Vilaplana 2004 | Spain | L. infantum | Human | VL | yes | Immunology/Ag | U | 16 |
| [152] | De Colmenares 1995 | Spain | L. infantum | Human | VL | No | Immunology/Ag | U | 15 |
| [364] | Abeijon 2016 | India | L. donovani | Human | VL | No | Immunology/Ag | U | 7 |
| [197] | Málaga-Machaca 2017 | Peru | T. cruzi | Human | CD | No | Immunology/Ag | U | 6 |
| [227] | Vaish 2011 | India | L. donovani | Human | VL | No | Genetic material | S | 148 |
| [225] | Pandey 2018 | Thailand | L. martiniquensis? | Human | VL | Yes | Genetic material | S | 130 |
| [365] | Boni 2017 | Brazil | Leishmania spp. | Human | CL-MCL | No | Genetic material | S-N | 15 |
| [134] | Phumee 2013 | Thailand | L. martiniquensis | Human | VL-CL | No | Genetic material and Parasitology | S-U | 6 |
| [238] | Pinho 1999 | Brazil | T. cruzi | Human | CD | No | Immunology/Ab | S | 114 |
| [235] | Lejon 2003 | DRC | T. b. brucei | Human | SleepS | No | Immunology/Ab | S | 78 |
| [236] | Lejon 2006 | DRC, Benin | T. b. brucei | Human | SleepS | No | Immunology/Ab | S | 23 |
| [25] | Peña 2008 | Spain | L. infantum | Dog | CVL | NA | Parasitology | O | 60 |
| [366] | Aschar 2016 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O-S | 92 |
| [367] | de Almeida Ferreira 2012 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O | 80 |
| [368] | Di Muccio 2012 | Italy | L. infantum | Dog | CVL | NA | Genetic material | O | 72 |
| [369] | Solano-Gallego 2001 | Spain | L. infantum | Dog | CVL | NA | Genetic material | O | 67 |
| [370] | Ceccarelli 2014 | Italy | L. infantum | Dog | CVL | NA | Genetic material | O | 65 |
| [230] | Ferreira 2013 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O-S-N | 62 |
| [266] | Pereira 2016 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O | 60 |
| [371] | Carvalho Ferreira 2014 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O | 60 |
| [229] | Lombardo 2012 | Italy | L. infantum | Dog | CVL | NA | Genetic material | O-S | 57 |
| [265] | Ferreira 2008 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O | 46 |
| [372] | Geisweid 2013 | Germany | L. infantum | Dog | CVL | NA | Genetic material | O | 43 |
| [268] | Leite 2010 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O | 30 |
| [264] | Strauss-Ayali 2004 | Israel | L. infantum | Dog | CVL | NA | Genetic material | O | 24 |
| [373] | Pilatti 2009 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | O | 23 |
| [374] | Gao 2015 | China | L. infantum | Dog | CVL | NA | Genetic material | O | 5 |
| [269] | Benassi 2017 | Brazil | Leishmania | Cat | ? | NA | Genetic material | O | 2 |
| [350] | Ortega 2017 | Spain | Leishmania | Leporidae | ? | NA | Genetic material | H | 65 |
| [375] | Belinchón-Lorenzo 2016 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | H | 30 |
| [376] | Belinchón-Lorenzo 2013 | Spain | L. infantum | Dog | CVL | NA | Genetic material | H | 28 |
| [351] | de Sousa Gonçalves 2016 | Brazil | L. infantum | Dog | CVL | NA | Genetic material | H | 15 |
| Positivity (95% CI) | Heterogeneity | ||||
|---|---|---|---|---|---|
| df | p | I2 (%) | Tau2 | ||
| Positive PCR in Urine | 0.73(0.63–0.84) | 8 | <0.0001 | 100 | 0.250 |
| Positive Ab in Urine | 0.57(0.37–0.76) | 13 | <0.0001 | 100 | 0.139 |
| Positive Ag in Urine | 0.59(0.47–0.72) | 28 | <0.0001 | 100 | 0.117 |
| Positive Parasite in Urine | 0.85(0.80–0.91) | 5 | <0.0001 | 100 | 0.004 |
| Positive PCR in Conjunctival Swab | 0.56(0.30–0.81) | 17 | <0.0001 | 100 | 0.306 |
| Positive PCR in Oral Saliva | 0.57(0.28–0.85) | 6 | <0.0001 | 100 | 0.148 |
| Positive PCR in Nasal | 0.73(0.48–0.98) | 1 | <0.0001 | 100 | 0.033 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sereno, D.; Akhoundi, M.; Sayehmri, K.; Mirzaei, A.; Holzmuller, P.; Lejon, V.; Waleckx, E. Noninvasive Biological Samples to Detect and Diagnose Infections due to Trypanosomatidae Parasites: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2020, 21, 1684. https://doi.org/10.3390/ijms21051684
Sereno D, Akhoundi M, Sayehmri K, Mirzaei A, Holzmuller P, Lejon V, Waleckx E. Noninvasive Biological Samples to Detect and Diagnose Infections due to Trypanosomatidae Parasites: A Systematic Review and Meta-Analysis. International Journal of Molecular Sciences. 2020; 21(5):1684. https://doi.org/10.3390/ijms21051684
Chicago/Turabian StyleSereno, Denis, Mohammad Akhoundi, Kourosh Sayehmri, Asad Mirzaei, Philippe Holzmuller, Veerle Lejon, and Etienne Waleckx. 2020. "Noninvasive Biological Samples to Detect and Diagnose Infections due to Trypanosomatidae Parasites: A Systematic Review and Meta-Analysis" International Journal of Molecular Sciences 21, no. 5: 1684. https://doi.org/10.3390/ijms21051684
APA StyleSereno, D., Akhoundi, M., Sayehmri, K., Mirzaei, A., Holzmuller, P., Lejon, V., & Waleckx, E. (2020). Noninvasive Biological Samples to Detect and Diagnose Infections due to Trypanosomatidae Parasites: A Systematic Review and Meta-Analysis. International Journal of Molecular Sciences, 21(5), 1684. https://doi.org/10.3390/ijms21051684






