IL-18 But Not IL-1 Signaling Is Pivotal for the Initiation of Liver Injury in Murine Non-Alcoholic Fatty Liver Disease
Abstract
1. Introduction
2. Results
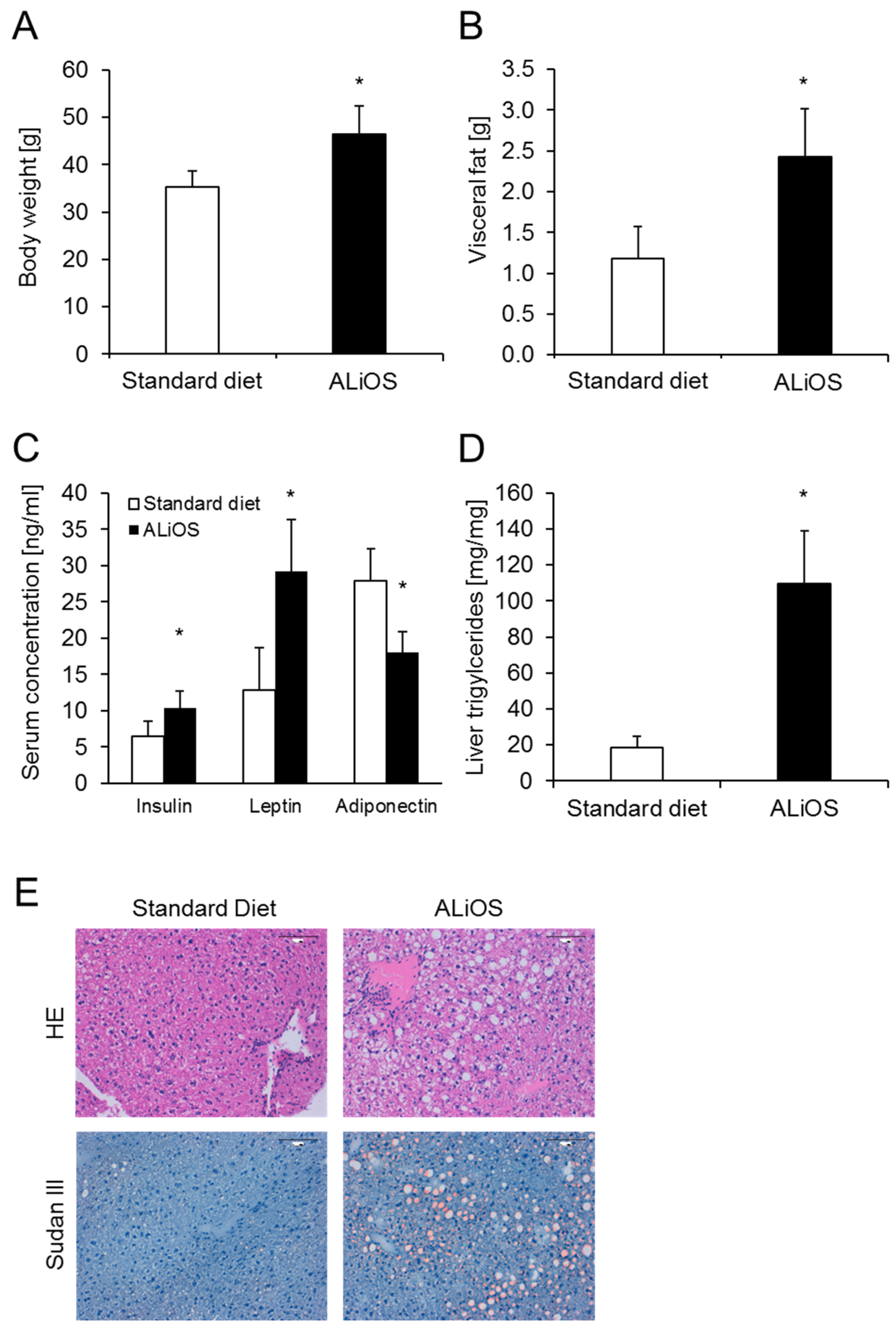
2.1. Mice Fed ALiOS Diet Develop Obesity, Metabolic Syndrome and Fatty Liver
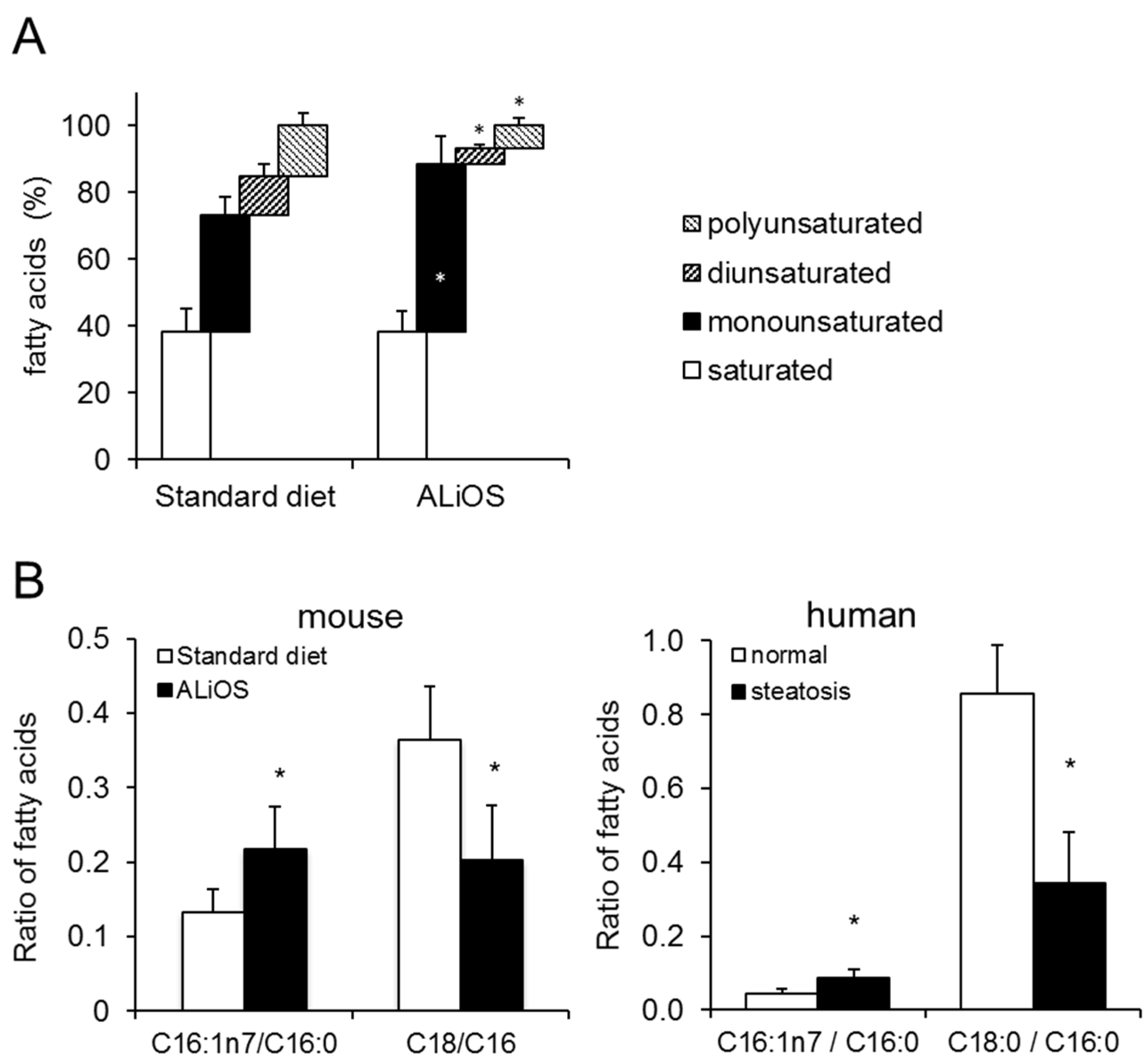
2.2. The Hepatic Lipidome in the ALiOS Model Closely Mimics Changes in the Human Hepatic Lipidome in NAFLD
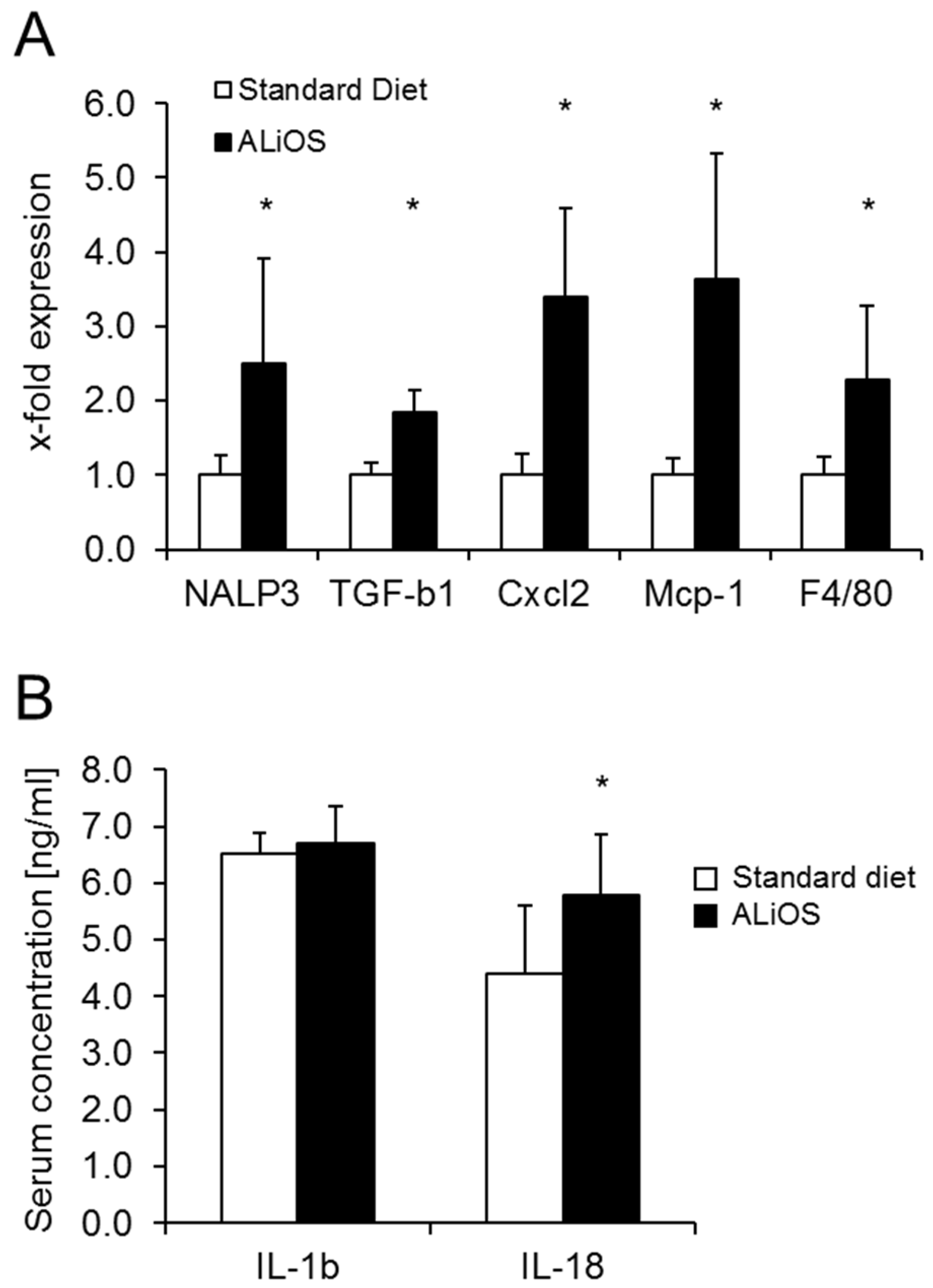
2.3. ALiOS Diet Leads to Activation of the Inflammasome
2.4. ALiOS Diet Leads to NAFLD but Not NASH
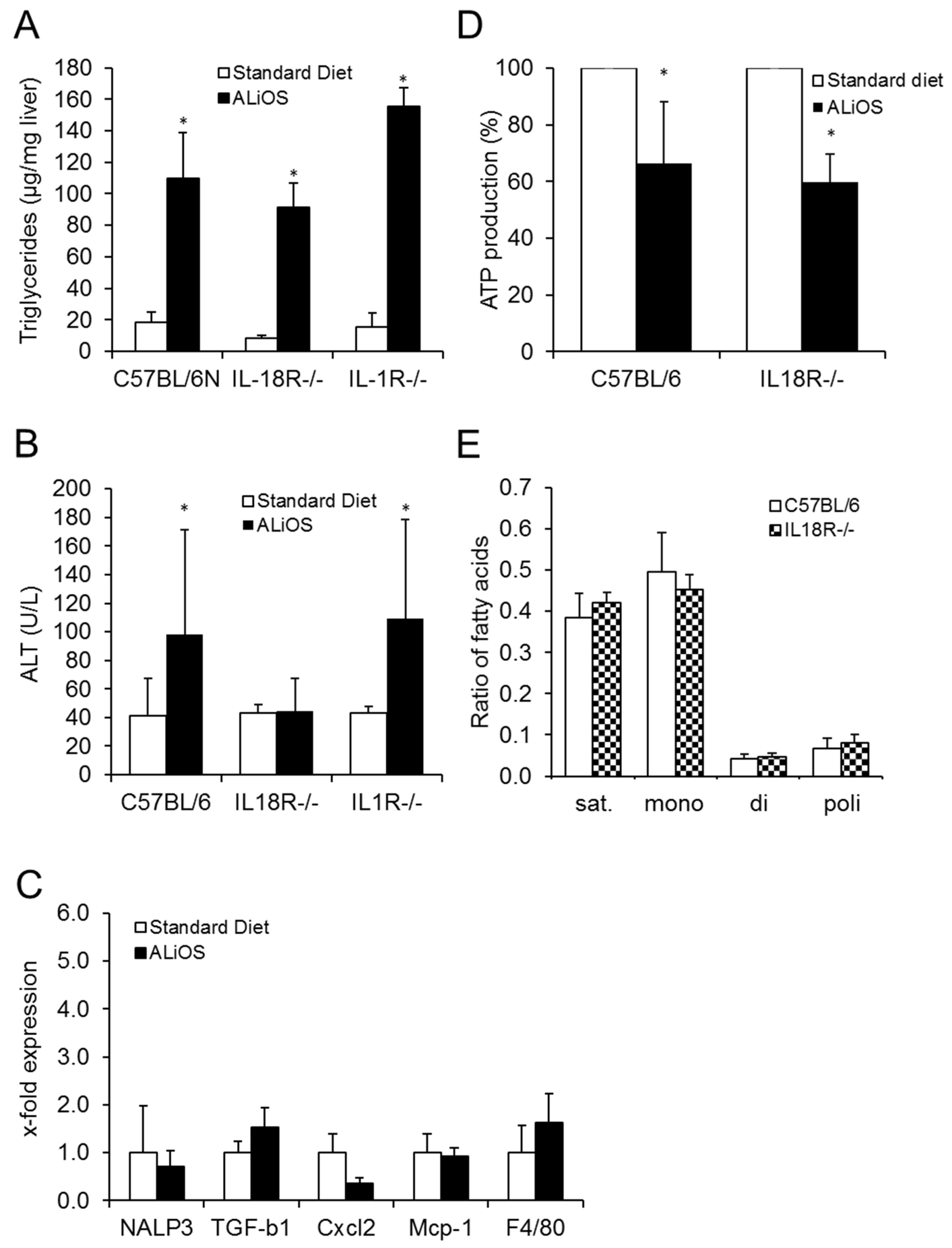
2.5. IL-18 but Not IL-1 Is a Downstream Mediator of the Activated Inflammasome in NAFLD
2.6. IL-18R Deficiency Leads to Silencing of the Pro-Inflammatory Environment in Steatotic Livers
3. Discussion
4. Materials and Methods
4.1. Animal Experiments
4.2. Human Tissue
4.3. Serum Biochemistry
4.4. Liver Histology and Determination of Triglycerides and Hydroxyproline in Liver Tissue
4.5. Analysis of Fatty Acids by Gas Chromatography
4.6. Isolation of Mitochondria
4.7. PCR
| Gapdh: | left | AGCGAGACCCCACTAACATC |
| right | GGCGGAGATGATGACCCTTT | |
| 36B4: | left | TCTAGGACCCGAGAAGACCT |
| right | CCCACCTTGTCTCCAGTCTT | |
| Nalp3: | left | AAAGCTAAGAAGGACCAGCC |
| right | TATCCCAGCAAACCCATCCA | |
| Tgf-b1: | left | CGCAACAACGCCATCTATGA |
| right | ACTGCTTCCCGAATGTCTGA | |
| CxCl2: | left | TCTTGAGCTTGGTGACAAAAAC |
| right | GGCTGGAGAGCTACAAGAGG | |
| Mcp-1: | left | GCTGCTACTCATTCACCAGC |
| right | CTTCTTGGGGTCAGCACAGA | |
| F4/80: | left | AACCAACTTTCAAGGCCCAG |
| right | TGCAGACTGAGTTAGGACCA |
4.8. Multiplex Assay
4.9. Statistical Testing
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Stepanova, M.; Younossi, Y.; Golabi, P.; Mishra, A.; Rafiq, N.; Henry, L. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut 2019, 69, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.J. Past, present and future perspectives in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 377–386. [Google Scholar] [CrossRef]
- Loomba, R.; Sanyal, A.J. The global NAFLD epidemic. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 686–690. [Google Scholar] [CrossRef] [PubMed]
- EASL; EASD; EASO. Clinical Practice Guidelines for the Management of Non-Alcoholic Fatty Liver Disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef]
- Hohenester, S.; Christiansen, S.; Nagel, J.M.; Wimmer, R.; Artmann, R.; Denk, G.; Bischoff, M.; Bischoff, G.; Rust, C. Lifestyle intervention for morbid obesity: Effects on liver steatosis, inflammation, and fibrosis. Am. J. Physiol. Liver Physiol. 2018, 315, G329–G338. [Google Scholar] [CrossRef]
- Mahli, A.; Saugspier, M.; Koch, A.; Sommer, J.; Dietrich, P.; Lee, S.; Thasler, R.; Schulze-Luehrmann, J.; Luehrmann, A.; Thasler, W.E.; et al. ERK activation and autophagy impairment are central mediators of irinotecan-induced steatohepatitis. Gut 2018, 67, 746–756. [Google Scholar] [CrossRef]
- Alwahsh, S.M.; Gebhardt, R. Dietary fructose as a risk factor for non-alcoholic fatty liver disease (NAFLD). Arch. Toxicol. 2017, 91, 1545–1563. [Google Scholar] [CrossRef]
- Austin, P.; Gerber, L.H.; Paik, J.M.; Price, J.K.; Escheik, C.; Younossi, Z.M. Aerobic capacity and exercise performance in nonalcoholic fatty liver disease. J. Sports Med. Phys. Fit. 2019, 59, 1376–1388. [Google Scholar] [CrossRef]
- Alwahsh, S.M.; Xu, M.; Schultze, F.C.; Wilting, J.; Mihm, S.; Raddatz, D.; Ramadori, G. Combination of Alcohol and Fructose Exacerbates Metabolic Imbalance in Terms of Hepatic Damage, Dyslipidemia, and Insulin Resistance in Rats. PLoS ONE 2014, 9, e104220. [Google Scholar] [CrossRef]
- Brandt, A.; Hernández-Arriaga, A.; Kehm, R.; Sánchez, V.; Jin, C.J.; Nier, A.; Baumann, A.; Camarinha-Silva, A.; Bergheim, I. Metformin attenuates the onset of non-alcoholic fatty liver disease and affects intestinal microbiota and barrier in small intestine. Sci. Rep. 2019, 9, 6668. [Google Scholar] [CrossRef] [PubMed]
- Einer, C.; Hohenester, S.; Wimmer, R.; Wottke, L.; Artmann, R.; Schulz, S.; Gosmann, C.; Simmons, A.; Leitzinger, C.; Eberhagen, C.; et al. Mitochondrial adaptation in steatotic mice. Mitochondrion 2018, 40, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Einer, C.; Hohenester, S.; Wimmer, R.; Wottke, L.; Artmann, R.; Schulz, S.; Gosmann, C.; Simmons, A.; Leitzinger, C.; Eberhagen, C.; et al. Data on chow, liver tissue and mitochondrial fatty acid compositions as well as mitochondrial proteome changes after feeding mice a western diet for 6–24 weeks. Data Brief 2017, 15, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Einer, C.; Leitzinger, C.; Lichtmannegger, J.; Eberhagen, C.; Rieder, T.; Borchard, S.; Wimmer, R.; Denk, G.; Popper, B.; Neff, F.; et al. A High-Calorie Diet Aggravates Mitochondrial Dysfunction and Triggers Severe Liver Damage in Wilson Disease Rats. Cell. Mol. Gastroenterol. Hepatol. 2019, 7, 571–596. [Google Scholar] [CrossRef]
- Yamada, K.; Mizukoshi, E.; Sunagozaka, H.; Arai, K.; Yamashita, T.; Takeshita, Y.; Misu, H.; Takamura, T.; Kitamura, S.; Zen, Y.; et al. Characteristics of hepatic fatty acid compositions in patients with nonalcoholic steatohepatitis. Liver Int. 2014, 35, 582–590. [Google Scholar] [CrossRef]
- Wen, H.; Gris, D.; Lei, Y.; Jha, S.; Zhang, L.; Huang, M.T.-H.; Brickey, W.J.; Ting, J.P.-Y. Fatty acid–induced NLRP3-ASC inflammasome activation interferes with insulin signaling. Nat. Immunol. 2011, 12, 408–415. [Google Scholar] [CrossRef]
- Lamkanfi, M.; Dixit, V.M. Inflammasomes and Their Roles in Health and Disease. Annu. Rev. Cell Dev. Biol. 2012, 28, 137–161. [Google Scholar] [CrossRef]
- Kubes, P.; Mehal, W.Z. Sterile Inflammation in the Liver. Gastroenterology 2012, 143, 1158–1172. [Google Scholar] [CrossRef]
- Martinon, F.; Tschopp, J. Inflammatory Caspases: Linking an intracellular innate immune system to autoinflammatory diseases. Cell 2004, 117, 561–574. [Google Scholar] [CrossRef]
- Csak, T.; Ganz, M.; Pespisa, J.; Kodys, K.; Dolganiuc, A.; Szabo, G. Fatty acid and endotoxin activate inflammasomes in mouse hepatocytes that release danger signals to stimulate immune cells. Hepatology 2011, 54, 133–144. [Google Scholar] [CrossRef]
- Simoes, I.C.M.; Janikiewicz, J.; Bauer, J.; Karkucińska-Więckowska, A.; Kalinowski, P.; Dobrzyń, A.; Wolski, A.; Pronicki, M.; Zieniewicz, K.; Dobrzyn, P.; et al. Fat and Sugar—A Dangerous Duet. A Comparative Review on Metabolic Remodeling in Rodent Models of Nonalcoholic Fatty Liver Disease. Nutrients 2019, 11, 2871. [Google Scholar] [CrossRef] [PubMed]
- Tetri, L.H.; Basaranoglu, M.; Brunt, E.M.; Yerian, L.M.; Neuschwander-Tetri, B.A. Severe NAFLD with hepatic necroinflammatory changes in mice fed trans fats and a high-fructose corn syrup equivalent. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 295, G987–G995. [Google Scholar] [CrossRef] [PubMed]
- Gadd, V.L.; Skoien, R.; Powell, E.E.; Fagan, K.J.; Winterford, C.; Horsfall, L.U.; Irvine, K.; Clouston, A.D. The portal inflammatory infiltrate and ductular reaction in human nonalcoholic fatty liver disease. Hepatology 2014, 59, 1393–1405. [Google Scholar] [CrossRef] [PubMed]
- Duval, C.; Thissen, U.; Keshtkar, S.; Accart, B.; Stienstra, R.; Boekschoten, M.V.; Roskams, T.; Kersten, S.; Müller, M. Adipose Tissue Dysfunction Signals Progression of Hepatic Steatosis Towards Nonalcoholic Steatohepatitis in C57Bl/6 Mice. Diabetes 2010, 59, 3181–3191. [Google Scholar] [CrossRef]
- Sigrist-Flores, S.; Ponciano-Gómez, A.; Pedroza-González, A.; Gallardo-Ortíz, I.A.; Villalobos-Molina, R.; Pardo-Vázquez, J.; Saucedo-Campos, A.; Jiménez-Flores, J.R.; Méndez-Cruz, A.R.; Suacedo-Campos, A. Chronic intake of moderate fat-enriched diet induces fatty liver and low-grade inflammation without obesity in rabbits. Chem. Biol. Interact. 2019, 300, 56–62. [Google Scholar] [CrossRef]
- Flisiak-Jackiewicz, M.; Bobrus-Chociej, A.; Tarasów, E.; Wojtkowska, M.; Białokoz-Kalinowska, I.; Lebensztejn, D.M. Predictive Role of Interleukin-18 in Liver Steatosis in Obese Children. Can. J. Gastroenterol. Hepatol. 2018, 2018, 3870454. [Google Scholar] [CrossRef]
- McKie, E.A.; Reid, J.L.; Mistry, P.C.; DeWall, S.L.; Abberley, L.; Ambery, P.D.; Gil-Extremera, B. A Study to Investigate the Efficacy and Safety of an Anti-Interleukin-18 Monoclonal Antibody in the Treatment of Type 2 Diabetes Mellitus. PLoS ONE 2016, 11, e0150018. [Google Scholar] [CrossRef]
- Henao-Mejia, J.; Elinav, E.; Jin, C.-C.; Hao, L.; Mehal, W.Z.; Strowig, T.; Thaiss, C.A.; Kau, A.L.; Eisenbarth, S.C.; Jurczak, M.J.; et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature 2012, 482, 179–185. [Google Scholar] [CrossRef]
- Reiter, F.P.; Wimmer, R.; Wottke, L.; Artmann, R.; Nagel, J.M.; Carranza, M.O.; Mayr, D.; Rust, C.; Fickert, P.; Trauner, M.; et al. Role of interleukin-1 and its antagonism of hepatic stellate cell proliferation and liver fibrosis in the Abcb4(-/-) mouse model. World J. Hepatol. 2016, 8, 401–410. [Google Scholar] [CrossRef]
- Miura, K.; Kodama, Y.; Inokuchi, S.; Schnabl, B.; Aoyama, T.; Ohnishi, H.; Olefsky, J.M.; Brenner, D.A.; Seki, E. Toll-like receptor 9 promotes steatohepatitis by induction of interleukin-1beta in mice. Gastroenterology 2010, 139, 323–334.e327. [Google Scholar] [CrossRef]
- Kamari, Y.; Shaish, A.; Vax, E.; Shemesh, S.; Kandel-Kfir, M.; Arbel, Y.; Olteanu, S.; Barshack, I.; Dotan, S.; Voronov, E.; et al. Lack of interleukin-1alpha or interleukin-1beta inhibits transformation of steatosis to steatohepatitis and liver fibrosis in hypercholesterolemic mice. J. Hepatol. 2011, 55, 1086–1094. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.-W.; Lee, M.-S. Mitochondria and the NLRP3 inflammasome: Physiological and pathological relevance. Arch. Pharmacal. Res. 2016, 39, 1503–1518. [Google Scholar] [CrossRef] [PubMed]
- Bedossa, P.; Poitou, C.; Veyrie, N.; Bouillot, J.-L.; Basdevant, A.; Paradis, V.; Tordjman, J.; Clement, K. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology 2012, 56, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Kleiner, D.E.; Brunt, E.M.; Van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.-C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Menke, A.L.; Driessen, A.; Koek, G.H.; Lindeman, J.H.; Stoop, R.; Havekes, L.M.; Kleemann, R.; Hoek, A.M.V.D. Establishment of a General NAFLD Scoring System for Rodent Models and Comparison to Human Liver Pathology. PLoS ONE 2014, 9, e115922. [Google Scholar] [CrossRef]
- Edwards, C.; O’Brien, W. Modified assay for determination of hydroxyproline in a tissue hydrolyzate. Clin. Chim. Acta 1980, 104, 161–167. [Google Scholar] [CrossRef]
- Folch, J.; Lees, M.; Stanley, G.S. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 1957, 226, 497–509. [Google Scholar]
- Thasler, W.E.; Weiss, T.S.; Schillhorn, K.; Stoll, P.-T.; Irrgang, B.; Jauch, K.-W. Charitable State-Controlled Foundation Human Tissue and Cell Research: Ethic and Legal Aspects in the Supply of Surgically Removed Human Tissue for Research in the Academic and Commercial Sector in Germany. Cell Tissue Bank. 2003, 4, 49–56. [Google Scholar] [CrossRef]
- Schulz, S.; Lichtmannegger, J.; Schmitt, S.; Leitzinger, C.; Eberhagen, C.; Einer, C.; Kerth, J.; Aichler, M.; Zischka, H. A Protocol for the Parallel Isolation of Intact Mitochondria from Rat Liver, Kidney, Heart, and Brain. Methods Mol. Biol. 2015, 1295, 75–86. [Google Scholar] [CrossRef]
| Rodent Score | No NAFLD | NAFL | NASH | p |
| Standard Diet | 4 | 2 | 0 | |
| ALiOS | 0 | 6 | 0 | 0.061 |
| NAS | No NAFLD | NAFL | NASH | |
| Standard Diet | 6 | 0 | 0 | |
| ALiOS | 0 | 6 | 0 | 0.002 |
| SAF | No NAFLD | mild disease | Moderate or severe | |
| Standard Diet | 6 | 0 | 0 | |
| ALiOS | 0 | 6 | 0 | 0.002 |
| C57BL/6 wt MW ± SD (-Fold Increase) | IL18R−/− MW ± SD (-Fold Increase) | IL1R−/− MW ± SD (-Fold Increase) | |
|---|---|---|---|
| Body weight (g) | |||
| Standard diet | 35.22 ± 3.37 | 32.72 ± 2.17 | 34.87 ± 2.84 |
| ALiOS | 46.44 ± 5.97 ** | 38.82 ± 3.28 ** | 45.28 ± 2.09 ** |
| (1.32) | (1.19) | (1.21) | |
| Visceral fat (g) | |||
| Standard diet | 1.18 ± 0.40 | 0.54 ± 0.10 | 1.21 ± 0.36 |
| ALiOS | 2.43 ± 0.59 ** | 1.85 ± 0.59 ** | 2.48 ± 0.22 ** |
| (2.06) | (3.43) | (2.05) | |
| NEFA (mmol/L) | |||
| Standard diet | 0.46 ± 0.11 | 0.53 ± 0.11 | 0.72 ± 0.20 |
| ALiOS | 0.93 ± 0.23 ** | 1.10 ± 0.21 ** | 0.98 ± 0.14 ** |
| (2.02) | (2.08) | (1.36) | |
| Hydroxyprolin (µg/g) | |||
| Standard diet | 84.91 ± 44.15 | 137.39 ± 50.37 | 117.08 ± 52.64 |
| ALiOS | 115.66 ± 77.12 | 122.78 ± 35.86 | 96.25 ± 34.55 |
| (1.36) | (0.89) | (0.82) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hohenester, S.; Kanitz, V.; Schiergens, T.; Einer, C.; Nagel, J.; Wimmer, R.; Reiter, F.P.; Gerbes, A.L.; De Toni, E.N.; Bauer, C.; et al. IL-18 But Not IL-1 Signaling Is Pivotal for the Initiation of Liver Injury in Murine Non-Alcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2020, 21, 8602. https://doi.org/10.3390/ijms21228602
Hohenester S, Kanitz V, Schiergens T, Einer C, Nagel J, Wimmer R, Reiter FP, Gerbes AL, De Toni EN, Bauer C, et al. IL-18 But Not IL-1 Signaling Is Pivotal for the Initiation of Liver Injury in Murine Non-Alcoholic Fatty Liver Disease. International Journal of Molecular Sciences. 2020; 21(22):8602. https://doi.org/10.3390/ijms21228602
Chicago/Turabian StyleHohenester, Simon, Veronika Kanitz, Tobias Schiergens, Claudia Einer, Jutta Nagel, Ralf Wimmer, Florian P. Reiter, Alexander L. Gerbes, Enrico N. De Toni, Christian Bauer, and et al. 2020. "IL-18 But Not IL-1 Signaling Is Pivotal for the Initiation of Liver Injury in Murine Non-Alcoholic Fatty Liver Disease" International Journal of Molecular Sciences 21, no. 22: 8602. https://doi.org/10.3390/ijms21228602
APA StyleHohenester, S., Kanitz, V., Schiergens, T., Einer, C., Nagel, J., Wimmer, R., Reiter, F. P., Gerbes, A. L., De Toni, E. N., Bauer, C., Holdt, L., Mayr, D., Rust, C., Schnurr, M., Zischka, H., Geier, A., & Denk, G. (2020). IL-18 But Not IL-1 Signaling Is Pivotal for the Initiation of Liver Injury in Murine Non-Alcoholic Fatty Liver Disease. International Journal of Molecular Sciences, 21(22), 8602. https://doi.org/10.3390/ijms21228602






