Clinical Application of Oncolytic Viruses: A Systematic Review
Abstract
1. Introduction
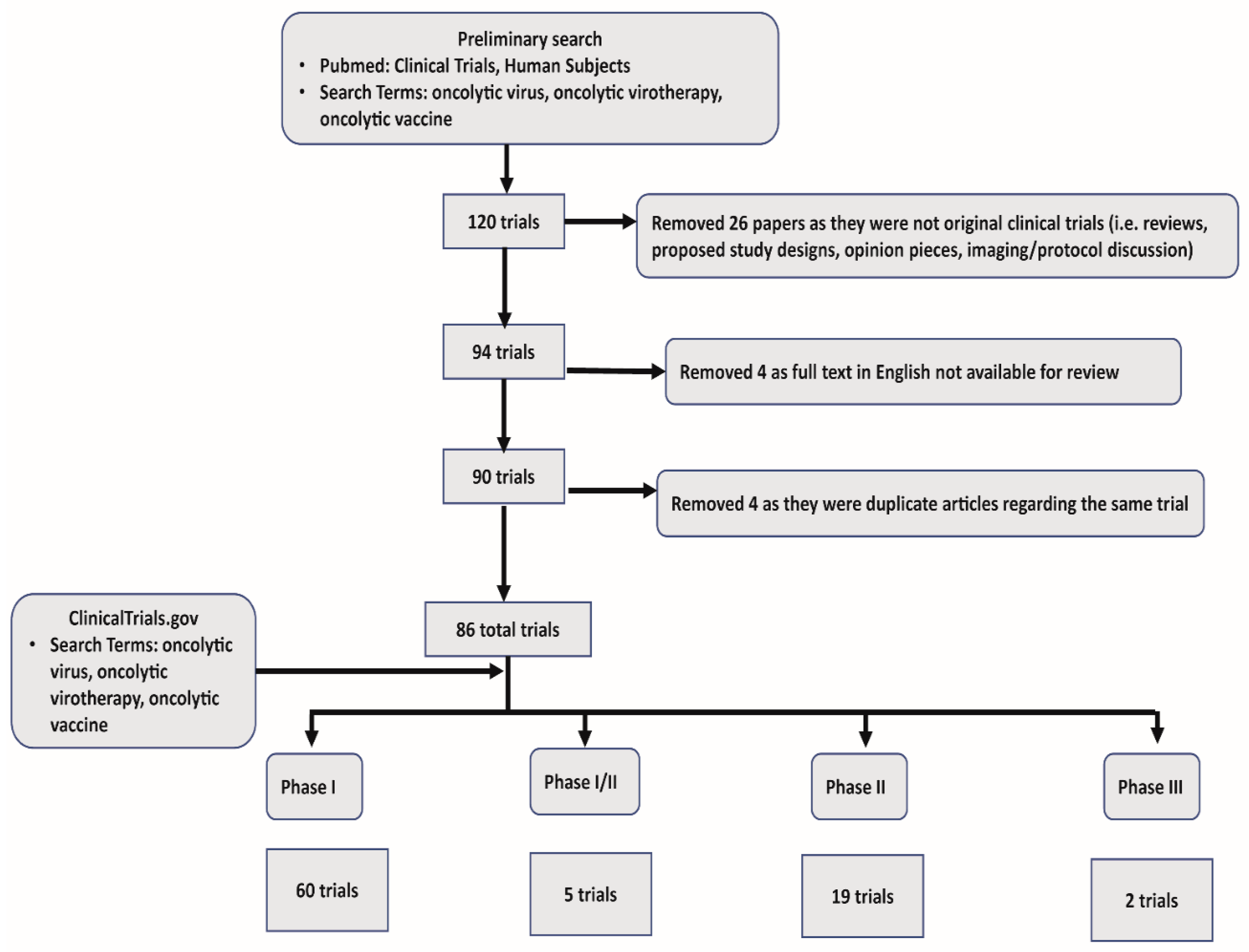
2. Methods
3. Mechanism of Action
4. Targeting Cancer Cells
5. Direct Tumor Cell Lysis
6. Antitumor Activity
7. Novel Trends in OV Advancements
8. Augmentation of Immune Checkpoint Inhibition. “Making Cold Tumors Hot: Immune Checkpoint Inhibitor–OV Combination Therapy Trials”
9. Modes of OV Delivery
9.1. Intralesional Route
9.2. Intravenous Route
10. Phase I Trials
11. Pexa-Vec
12. Ad5/3 delta 24 (CRAd)
13. Seneca Valley Virus
14. Polio Virus
15. MV-NIS
16. Phase II Trials
17. Reolysin
18. ProstAtak
19. ONYX-015
20. Cavatak
21. Phase 3 Trials
22. Talimogene Herparepvec
23. Limitations of OVs
24. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lichty, B.D.; Breitbach, C.J.; Stojdl, D.F.; Bell, J.C. Going viral with cancer immunotherapy. Nat. Rev. Cancer 2014, 14, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Amgen. FDA Approves IMLYGICTM (Talimogene Laherparepvic) as First Oncolytic Viral Therapy in the US. 2018. Available online: https://www.prnewswire.com/news-releases/fda-approves-imlygic-talimogene-laherparepvec-as-first-oncolytic-viral-therapy-in-the-us-300167270.html (accessed on 5 January 2020).
- Clemens, M.J. Targets and mechanisms for the regulation of translation in malignant transformation. Oncogene 2004, 23, 3180–3188. [Google Scholar] [CrossRef] [PubMed]
- Aghi, M.; Visted, T.; Depinho, R.A.; Chiocca, E.A. Oncolytic herpes virus with defective ICP6 specifically replicates in quiescent cells with homozygous genetic mutations in p16. Oncogene 2008, 27, 4249–4254. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Chan, M.K.; Pornchai, O.; Eisenberg, D.P.; Shah, J.P.; Singh, B.; Fong, Y.; Wong, R.J. Enhanced nectin-1 expression and herpes oncolytic sensitivity in highly migratory and invasive carcinoma. Clin. Cancer Res. 2005, 11, 4889–4897. [Google Scholar] [CrossRef]
- Anderson, B.D.; Nakamura, T.; Russell, S.J.; Peng, K.W. High CD46 receptor density determines preferential killing of tumor cells by oncolytic measles virus. Cancer Res. 2004, 64, 4919–4926. [Google Scholar] [CrossRef]
- Martuza, R.L.; Malick, A.; Markert, J.M.; Ruffner, K.L.; Coen, D.M. Experimental therapy of human glioma by means of a genetically engineered virus mutant. Science 1991, 252, 854–856. [Google Scholar] [CrossRef]
- Errington, F.; Steele, L.; Prestwich, R.; Harrington, K.J.; Pandha, H.S.; Vidal, L.; de Bono, J.; Selby, P.; Coffey, M.; Vile, R.; et al. Reovirus activates human dendritic cells to promote innate antitumor immunity. J. Immunol. 2008, 180, 6018–6026. [Google Scholar] [CrossRef]
- Sobol, P.T.; Boudreau, J.E.; Stephenson, K.; Wan, Y.; Lichty, B.D.; Mossman, K.L. Adaptive antiviral immunity is a determinant of the therapeutic success of oncolytic virotherapy. Mol. Ther. 2011, 19, 335–344. [Google Scholar] [CrossRef]
- Zamarin, D.; Holmgaard, R.B.; Subudhi, S.K.; Park, J.S.; Mansour, M.; Palese, P.; Merghoub, T.; Wolchok, J.D.; Allison, J.P. Localized oncolytic virotherapy overcomes systemic tumor resistance to immune checkpoint blockade immunotherapy. Sci. Transl. Med. 2014, 6, 226ra32. [Google Scholar] [CrossRef]
- Prestwich, R.J.; Errington, F.; Ilett, E.J.; Morgan, R.S.; Scott, K.J.; Kottke, T.; Thompson, J.; Morrison, E.E.; Harrington, K.J.; Pandha, H.S.; et al. Tumor infection by oncolytic reovirus primes adaptive antitumor immunity. Clin. Cancer Res. 2008, 14, 7358–7366. [Google Scholar] [CrossRef]
- Toda, M.; Rabkin, S.D.; Kojima, H.; Martuza, R.L. Herpes simplex virus as an in situ cancer vaccine for the induction of specific anti-tumor immunity. Hum. Gene Ther. 1999, 10, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Conry, R.M.; Westbrook, B.; McKee, S.; Norwood, T.G. Talimogene laherparepvec: First in class oncolytic virotherapy. Hum. Vaccin. Immunother. 2018, 14, 839–846. [Google Scholar] [CrossRef] [PubMed]
- Breitbach, C.J.; Arulanandam, R.; De Silva, N.; Thorne, S.H.; Patt, R.; Daneshmand, M.; Moon, A.; Ilkow, C.; Burke, J.; Hwang, T.H.; et al. Oncolytic vaccinia virus disrupts tumor-associated vasculature in humans. Cancer Res. 2013, 73, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Benencia, F.; Courreges, M.C.; Conejo-Garcia, J.R.; Buckanovich, R.J.; Zhang, L.; Carroll, R.H.; Morgan, M.A.; Coukos, G. Oncolytic HSV exerts direct antiangiogenic activity in ovarian carcinoma. Hum. Gene Ther. 2005, 16, 765–778. [Google Scholar] [CrossRef] [PubMed]
- Breitbach, C.J.; De Silva, N.S.; Falls, T.J.; Aladl, U.; Evgin, L.; Paterson, J.; Sun, Y.Y.; Roy, D.G.; Rintoul, J.L.; Daneshmand, M.; et al. Targeting tumor vasculature with an oncolytic virus. Mol. Ther. 2011, 19, 886–894. [Google Scholar] [CrossRef] [PubMed]
- A Phase 1 Study of M032 (NSC 733972), a Genetically Engineered HSV-1 Expressing IL-12, in Patients with Recurrent/Progressive Glioblastoma Multiforme, Anaplastic Astrocytoma, or Gliosarcoma. Available online: https://clinicaltrials.gov/ct2/show/NCT02062827 (accessed on 5 January 2020).
- A Phase 1, Open-Label, Dose-Escalation Clinical Trial of Tumor Necrosis Factor Alpha and Interleukin 2 Coding Oncolytic Adenovirus TILT-123 in Melanoma Patients Receiving Adoptive Cell Therapy with Tumor Infiltrating Lymphocytes. Available online: https://clinicaltrials.gov/ct2/show/NCT04217473 (accessed on 5 January 2020).
- Havunen, R.; Siurala, M.; Sorsa, S.; Gronberg-Vaha-Koskela, S.; Behr, M.; Tahtinen, S.; Santos, J.M.; Karell, P.; Rusanen, J.; Nettelbeck, D.M.; et al. Oncolytic Adenoviruses Armed with Tumor Necrosis Factor Alpha and Interleukin-2 Enable Successful Adoptive Cell Therapy. Mol. Ther. Oncolytics 2017, 4, 77–86. [Google Scholar] [CrossRef]
- Passaro, C.; Alayo, Q.; De Laura, I.; McNulty, J.; Grauwet, K.; Ito, H.; Bhaskaran, V.; Mineo, M.; Lawler, S.E.; Shah, K.; et al. Arming an Oncolytic Herpes Simplex Virus Type 1 with a Single-chain Fragment Variable Antibody against PD-1 for Experimental Glioblastoma Therapy. Clin. Cancer Res. 2019, 25, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Kyi, C.; Postow, M.A. Immune checkpoint inhibitor combinations in solid tumors: Opportunities and challenges. Immunotherapy 2016, 8, 821–837. [Google Scholar] [CrossRef]
- Rajani, K.R.; Vile, R.G. Harnessing the Power of Onco-Immunotherapy with Checkpoint Inhibitors. Viruses 2015, 7, 5889–5901. [Google Scholar] [CrossRef]
- Liu, Z.; Ravindranathan, R.; Kalinski, P.; Guo, Z.S.; Bartlett, D.L. Rational combination of oncolytic vaccinia virus and PD-L1 blockade works synergistically to enhance therapeutic efficacy. Nat. Commun. 2017, 8, 14754. [Google Scholar] [CrossRef]
- Intlekofer, A.M.; Thompson, C.B. At the bench: Preclinical rationale for CTLA-4 and PD-1 blockade as cancer immunotherapy. J. Leukoc. Biol. 2013, 94, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Bourgeois-Daigneault, M.C.; Roy, D.G.; Aitken, A.S.; El Sayes, N.; Martin, N.T.; Varette, O.; Falls, T.; St-Germain, L.E.; Pelin, A.; Lichty, B.D.; et al. Neoadjuvant oncolytic virotherapy before surgery sensitizes triple-negative breast cancer to immune checkpoint therapy. Sci. Transl. Med. 2018, 10, eaao1641. [Google Scholar] [CrossRef] [PubMed]
- Kleinpeter, P.; Fend, L.; Thioudellet, C.; Geist, M.; Sfrontato, N.; Koerper, V.; Fahrner, C.; Schmitt, D.; Gantzer, M.; Remy-Ziller, C.; et al. Vectorization in an oncolytic vaccinia virus of an antibody, a Fab and a scFv against programmed cell death -1 (PD-1) allows their intratumoral delivery and an improved tumor-growth inhibition. Oncoimmunology 2016, 5, e1220467. [Google Scholar] [CrossRef] [PubMed]
- Ilett, E.; Kottke, T.; Thompson, J.; Rajani, K.; Zaidi, S.; Evgin, L.; Coffey, M.; Ralph, C.; Diaz, R.; Pandha, H.; et al. Prime-boost using separate oncolytic viruses in combination with checkpoint blockade improves anti-tumour therapy. Gene Ther. 2017, 24, 21–30. [Google Scholar] [CrossRef]
- Ribas, A.; Dummer, R.; Puzanov, I.; VanderWalde, A.; Andtbacka, R.H.I.; Michielin, O.; Olszanski, A.J.; Malvehy, J.; Cebon, J.; Fernandez, E.; et al. Oncolytic Virotherapy Promotes Intratumoral T Cell Infiltration and Improves Anti-PD-1 Immunotherapy. Cell 2017, 170, 1109–1119.e10. [Google Scholar] [CrossRef]
- Chesney, J.; Puzanov, I.; Collichio, F.; Singh, P.; Milhem, M.M.; Glaspy, J.; Hamid, O.; Ross, M.; Friedlander, P.; Garbe, C.; et al. Randomized, Open-Label Phase II Study Evaluating the Efficacy and Safety of Talimogene Laherparepvec in Combination with Ipilimumab Versus Ipilimumab Alone in Patients with Advanced, Unresectable Melanoma. J. Clin. Oncol. 2018, 36, 1658–1667. [Google Scholar] [CrossRef]
- Coxsackievirus A21 Synergizes with Checkpoint Inhibitors. Cancer Discov. 2017, 7, OF9. [CrossRef][Green Version]
- Pandha, H.; Harrington, K.; Ralph, C.; Melcher, A.; Gupta, S.; Akerley, W.; Sandborn, R.E.; Rudin, C.; Rosenberg, J.; Kaufman, D.; et al. Abstract CT115: Phase 1b KEYNOTE 200 (STORM study): A study of an intravenously delivered oncolytic virus, Coxsackievirus A21 in combination with pembrolizumab in advanced cancer patients. Cancer Res. 2017, 77 (Suppl. 13), CT115. [Google Scholar]
- Rudin, C.M.; Pandha, H.S.; Gupta, S.; Zibelman, M.R.; Akerley, W.; Day, D.; Hill, A.G.; Sanborn, R.E.; O’Day, S.J.; Clay, T.D.; et al. LBA40—Phase Ib KEYNOTE-200: A study of an intravenously delivered oncolytic virus, coxsackievirus A21 in combination with pembrolizumab in advanced NSCLC and bladder cancer patients. Ann. Oncol. 2018, 29, viii732. [Google Scholar] [CrossRef]
- A Phase 1, Dose-finding and Signal-seeking Study of the Safety & Efficacy of Intravenous CAVATAK® Alone and in Combination with Pembrolizumab in Patients with Late Stage Solid Tumours (VLA-009 STORM/KEYNOTE-200). Available online: https://clinicaltrials.gov/ct2/show/NCT02043665 (accessed on 5 January 2020).
- Kelly, C.M.; Antonescu, C.R.; Bowler, T.; Munhoz, R.; Chi, P.; Dickson, M.A.; Gounder, M.M.; Keohan, M.L.; Movva, S.; Dholakia, R.; et al. Objective Response Rate Among Patients with Locally Advanced or Metastatic Sarcoma Treated with Talimogene Laherparepvec in Combination with Pembrolizumab: A Phase 2 Clinical Trial. JAMA Oncol. 2020, 6, 402–408. [Google Scholar] [CrossRef]
- Senzer, N.N.; Kaufman, H.L.; Amatruda, T.; Nemunaitis, M.; Reid, T.; Daniels, G.; Gonzalez, R.; Glaspy, J.; Whitman, E.; Harrington, K.; et al. Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor-encoding, second-generation oncolytic herpesvirus in patients with unresectable metastatic melanoma. J. Clin. Oncol. 2009, 27, 5763–5771. [Google Scholar] [CrossRef] [PubMed]
- Andtbacka, R.H.; Agarwala, S.S.; Ollila, D.W.; Hallmeyer, S.; Milhem, M.; Amatruda, T.; Nemunaitis, J.J.; Harrington, K.J.; Chen, L.; Shilkrut, M.; et al. Cutaneous head and neck melanoma in OPTiM, a randomized phase 3 trial of talimogene laherparepvec versus granulocyte-macrophage colony-stimulating factor for the treatment of unresected stage IIIB/IIIC/IV melanoma. Head Neck 2016, 38, 1752–1758. [Google Scholar] [CrossRef] [PubMed]
- Reid, T.; Galanis, E.; Abbruzzese, J.; Sze, D.; Wein, L.M.; Andrews, J.; Randlev, B.; Heise, C.; Uprichard, M.; Hatfield, M.; et al. Hepatic arterial infusion of a replication-selective oncolytic adenovirus (dl1520): Phase II viral, immunologic, and clinical endpoints. Cancer Res. 2002, 62, 6070–6079. [Google Scholar] [PubMed]
- Netti, P.A.; Berk, D.A.; Swartz, M.A.; Grodzinsky, A.J.; Jain, R.K. Role of extracellular matrix assembly in interstitial transport in solid tumors. Cancer Res. 2000, 60, 2497–2503. [Google Scholar]
- McKee, T.D.; Grandi, P.; Mok, W.; Alexandrakis, G.; Insin, N.; Zimmer, J.P.; Bawendi, M.G.; Boucher, Y.; Breakefield, X.O.; Jain, R.K. Degradation of fibrillar collagen in a human melanoma xenograft improves the efficacy of an oncolytic herpes simplex virus vector. Cancer Res. 2006, 66, 2509–2513. [Google Scholar] [CrossRef]
- Kumar, V.; Boucher, Y.; Liu, H.; Ferreira, D.; Hooker, J.; Catana, C.; Hoover, A.J.; Ritter, T.; Jain, R.K.; Guimaraes, A.R. Noninvasive Assessment of Losartan-Induced Increase in Functional Microvasculature and Drug Delivery in Pancreatic Ductal Adenocarcinoma. Transl. Oncol. 2016, 9, 431–437. [Google Scholar] [CrossRef][Green Version]
- Yokoda, R.; Nagalo, B.M.; Vernon, B.; Oklu, R.; Albadawi, H.; DeLeon, T.T.; Zhou, Y.; Egan, J.B.; Duda, D.G.; Borad, M.J. Oncolytic virus delivery: From nano-pharmacodynamics to enhanced oncolytic effect. Oncolytic Virother. 2017, 6, 39–49. [Google Scholar] [CrossRef]
- Fukumura, D.; Kashiwagi, S.; Jain, R.K. The role of nitric oxide in tumour progression. Nat. Rev. Cancer 2006, 6, 521–534. [Google Scholar] [CrossRef]
- Huang, Y.; Goel, S.; Duda, D.G.; Fukumura, D.; Jain, R.K. Vascular normalization as an emerging strategy to enhance cancer immunotherapy. Cancer Res. 2013, 73, 2943–2948. [Google Scholar] [CrossRef]
- Russell, S.J.; Peng, K.W. Oncolytic Virotherapy: A Contest between Apples and Oranges. Mol. Ther. 2017, 25, 1107–1116. [Google Scholar] [CrossRef]
- Miller, A.; Suksanpaisan, L.; Naik, S.; Nace, R.; Federspiel, M.; Peng, K.W.; Russell, S.J. Reporter gene imaging identifies intratumoral infection voids as a critical barrier to systemic oncolytic virus efficacy. Mol. Ther. Oncolytics 2014, 1, 14005. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.; Carlisle, R. Achieving systemic delivery of oncolytic viruses. Expert Opin. Drug Deliv. 2019, 16, 607–620. [Google Scholar] [CrossRef] [PubMed]
- Breitbach, C.J.; Burke, J.; Jonker, D.; Stephenson, J.; Haas, A.R.; Chow, L.Q.; Nieva, J.; Hwang, T.H.; Moon, A.; Patt, R.; et al. Intravenous delivery of a multi-mechanistic cancer-targeted oncolytic poxvirus in humans. Nature 2011, 477, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Evgin, L.; Acuna, S.A.; Tanese de Souza, C.; Marguerie, M.; Lemay, C.G.; Ilkow, C.S.; Findlay, C.S.; Falls, T.; Parato, K.A.; Hanwell, D.; et al. Complement inhibition prevents oncolytic vaccinia virus neutralization in immune humans and cynomolgus macaques. Mol. Ther. 2015, 23, 1066–1076. [Google Scholar] [CrossRef] [PubMed]
- Fisher, K.D.; Stallwood, Y.; Green, N.K.; Ulbrich, K.; Mautner, V.; Seymour, L.W. Polymer-coated adenovirus permits efficient retargeting and evades neutralising antibodies. Gene Ther. 2001, 8, 341–348. [Google Scholar] [CrossRef]
- Mace, A.T.; Ganly, I.; Soutar, D.S.; Brown, S.M. Potential for efficacy of the oncolytic Herpes simplex virus 1716 in patients with oral squamous cell carcinoma. Head Neck 2008, 30, 1045–1051. [Google Scholar] [CrossRef]
- Streby, K.A.; Geller, J.I.; Currier, M.A.; Warren, P.S.; Racadio, J.M.; Towbin, A.J.; Vaughan, M.R.; Triplet, M.; Ott-Napier, K.; Dishman, D.J.; et al. Intratumoral Injection of HSV1716, an Oncolytic Herpes Virus, Is Safe and Shows Evidence of Immune Response and Viral Replication in Young Cancer Patients. Clin. Cancer Res. 2017, 23, 3566–3574. [Google Scholar] [CrossRef]
- Hu, J.C.; Coffin, R.S.; Davis, C.J.; Graham, N.J.; Groves, N.; Guest, P.J.; Harrington, K.J.; James, N.D.; Love, C.A.; McNeish, I.; et al. A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor. Clin. Cancer Res. 2006, 12, 6737–6747. [Google Scholar] [CrossRef]
- Markert, J.M.; Razdan, S.N.; Kuo, H.C.; Cantor, A.; Knoll, A.; Karrasch, M.; Nabors, L.B.; Markiewicz, M.; Agee, B.S.; Coleman, J.M.; et al. A phase 1 trial of oncolytic HSV-1, G207, given in combination with radiation for recurrent GBM demonstrates safety and radiographic responses. Mol. Ther. 2014, 22, 1048–1055. [Google Scholar] [CrossRef]
- Fong, Y.; Kim, T.; Bhargava, A.; Schwartz, L.; Brown, K.; Brody, L.; Covey, A.; Karrasch, M.; Getrajdman, G.; Mescheder, A.; et al. A herpes oncolytic virus can be delivered via the vasculature to produce biologic changes in human colorectal cancer. Mol. Ther. 2009, 17, 389–394. [Google Scholar] [CrossRef]
- Voit, C.; Kron, M.; Schwurzer-Voit, M.; Sterry, W. Intradermal injection of Newcastle disease virus-modified autologous melanoma cell lysate and interleukin-2 for adjuvant treatment of melanoma patients with resectable stage III disease. J. Dtsch. Dermatol. Ges. 2003, 1, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Pecora, A.L.; Rizvi, N.; Cohen, G.I.; Meropol, N.J.; Sterman, D.; Marshall, J.L.; Goldberg, S.; Gross, P.; O’Neil, J.D.; Groene, W.S.; et al. Phase I trial of intravenous administration of PV701, an oncolytic virus, in patients with advanced solid cancers. J. Clin. Oncol. 2002, 20, 2251–2266. [Google Scholar] [CrossRef] [PubMed]
- Laurie, S.A.; Bell, J.C.; Atkins, H.L.; Roach, J.; Bamat, M.K.; O’Neil, J.D.; Roberts, M.S.; Groene, W.S.; Lorence, R.M. A phase 1 clinical study of intravenous administration of PV701, an oncolytic virus, using two-step desensitization. Clin. Cancer Res. 2006, 12, 2555–2562. [Google Scholar] [CrossRef] [PubMed]
- Hotte, S.J.; Lorence, R.M.; Hirte, H.W.; Polawski, S.R.; Bamat, M.K.; O’Neil, J.D.; Roberts, M.S.; Groene, W.S.; Major, P.P. An optimized clinical regimen for the oncolytic virus PV701. Clin. Cancer Res. 2007, 13, 977–985. [Google Scholar] [CrossRef]
- Roulstone, V.; Khan, K.; Pandha, H.S.; Rudman, S.; Coffey, M.; Gill, G.M.; Melcher, A.A.; Vile, R.; Harrington, K.J.; de Bono, J.; et al. Phase I trial of cyclophosphamide as an immune modulator for optimizing oncolytic reovirus delivery to solid tumors. Clin. Cancer Res. 2015, 21, 1305–1312. [Google Scholar] [CrossRef]
- Lolkema, M.P.; Arkenau, H.T.; Harrington, K.; Roxburgh, P.; Morrison, R.; Roulstone, V.; Twigger, K.; Coffey, M.; Mettinger, K.; Gill, G.; et al. A phase I study of the combination of intravenous reovirus type 3 Dearing and gemcitabine in patients with advanced cancer. Clin. Cancer Res. 2011, 17, 581–588. [Google Scholar] [CrossRef]
- Vidal, L.; Pandha, H.S.; Yap, T.A.; White, C.L.; Twigger, K.; Vile, R.G.; Melcher, A.; Coffey, M.; Harrington, K.J.; DeBono, J.S. A phase I study of intravenous oncolytic reovirus type 3 Dearing in patients with advanced cancer. Clin. Cancer Res. 2008, 14, 7127–7137. [Google Scholar] [CrossRef]
- Forsyth, P.; Roldan, G.; George, D.; Wallace, C.; Palmer, C.A.; Morris, D.; Cairncross, G.; Matthews, M.V.; Markert, J.; Gillespie, Y.; et al. A phase I trial of intratumoral administration of reovirus in patients with histologically confirmed recurrent malignant gliomas. Mol. Ther. 2008, 16, 627–632. [Google Scholar] [CrossRef]
- Harrington, K.J.; Karapanagiotou, E.M.; Roulstone, V.; Twigger, K.R.; White, C.L.; Vidal, L.; Beirne, D.; Prestwich, R.; Newbold, K.; Ahmed, M.; et al. Two-stage phase I dose-escalation study of intratumoral reovirus type 3 dearing and palliative radiotherapy in patients with advanced cancers. Clin. Cancer Res. 2010, 16, 3067–3077. [Google Scholar] [CrossRef]
- Comins, C.; Spicer, J.; Protheroe, A.; Roulstone, V.; Twigger, K.; White, C.M.; Vile, R.; Melcher, A.; Coffey, M.C.; Mettinger, K.L.; et al. REO-10: A phase I study of intravenous reovirus and docetaxel in patients with advanced cancer. Clin. Cancer Res. 2010, 16, 5564–5572. [Google Scholar] [CrossRef]
- Morris, D.G.; Feng, X.; DiFrancesco, L.M.; Fonseca, K.; Forsyth, P.A.; Paterson, A.H.; Coffey, M.C.; Thompson, B. REO-001: A phase I trial of percutaneous intralesional administration of reovirus type 3 dearing (Reolysin(R)) in patients with advanced solid tumors. Investig. New Drugs 2013, 31, 696–706. [Google Scholar] [CrossRef] [PubMed]
- Sborov, D.W.; Nuovo, G.J.; Stiff, A.; Mace, T.; Lesinski, G.B.; Benson, D.M., Jr.; Efebera, Y.A.; Rosko, A.E.; Pichiorri, F.; Grever, M.R.; et al. A phase I trial of single-agent reolysin in patients with relapsed multiple myeloma. Clin. Cancer Res. 2014, 20, 5946–5955. [Google Scholar] [CrossRef] [PubMed]
- Kicielinski, K.P.; Chiocca, E.A.; Yu, J.S.; Gill, G.M.; Coffey, M.; Markert, J.M. Phase 1 clinical trial of intratumoral reovirus infusion for the treatment of recurrent malignant gliomas in adults. Mol. Ther. 2014, 22, 1056–1062. [Google Scholar] [CrossRef] [PubMed]
- Kolb, E.A.; Sampson, V.; Stabley, D.; Walter, A.; Sol-Church, K.; Cripe, T.; Hingorani, P.; Ahern, C.H.; Weigel, B.J.; Zwiebel, J.; et al. A phase I trial and viral clearance study of reovirus (Reolysin) in children with relapsed or refractory extra-cranial solid tumors: A Children’s Oncology Group Phase I Consortium report. Pediatr. Blood Cancer 2015, 62, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Desjardins, A.; Gromeier, M.; Herndon, J.E., 2nd; Beaubier, N.; Bolognesi, D.P.; Friedman, A.H.; Friedman, H.S.; McSherry, F.; Muscat, A.M.; Nair, S.; et al. Recurrent Glioblastoma Treated with Recombinant Poliovirus. N. Engl. J. Med. 2018, 379, 150–161. [Google Scholar] [CrossRef]
- Cerullo, V.; Diaconu, I.; Kangasniemi, L.; Rajecki, M.; Escutenaire, S.; Koski, A.; Romano, V.; Rouvinen, N.; Tuuminen, T.; Laasonen, L.; et al. Immunological effects of low-dose cyclophosphamide in cancer patients treated with oncolytic adenovirus. Mol. Ther. 2011, 19, 1737–1746. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Dmitriev, I.P.; Saddekni, S.; Kashentseva, E.A.; Harris, R.D.; Aurigemma, R.; Bae, S.; Singh, K.P.; Siegal, G.P.; Curiel, D.T.; et al. A phase I clinical trial of Ad5/3-Delta24, a novel serotype-chimeric, infectivity-enhanced, conditionally-replicative adenovirus (CRAd), in patients with recurrent ovarian cancer. Gynecol. Oncol. 2013, 130, 518–524. [Google Scholar] [CrossRef]
- Kimball, K.J.; Preuss, M.A.; Barnes, M.N.; Wang, M.; Siegal, G.P.; Wan, W.; Kuo, H.; Saddekni, S.; Stockard, C.R.; Grizzle, W.E.; et al. A phase I study of a tropism-modified conditionally replicative adenovirus for recurrent malignant gynecologic diseases. Clin. Cancer Res. 2010, 16, 5277–5287. [Google Scholar] [CrossRef]
- Pesonen, S.; Diaconu, I.; Cerullo, V.; Escutenaire, S.; Raki, M.; Kangasniemi, L.; Nokisalmi, P.; Dotti, G.; Guse, K.; Laasonen, L.; et al. Integrin targeted oncolytic adenoviruses Ad5-D24-RGD and Ad5-RGD-D24-GMCSF for treatment of patients with advanced chemotherapy refractory solid tumors. Int. J. Cancer 2012, 130, 1937–1947. [Google Scholar] [CrossRef]
- Kanerva, A.; Nokisalmi, P.; Diaconu, I.; Koski, A.; Cerullo, V.; Liikanen, I.; Tahtinen, S.; Oksanen, M.; Heiskanen, R.; Pesonen, S.; et al. Antiviral and antitumor T-cell immunity in patients treated with GM-CSF-coding oncolytic adenovirus. Clin. Cancer Res. 2013, 19, 2734–2744. [Google Scholar] [CrossRef]
- Hemminki, O.; Parviainen, S.; Juhila, J.; Turkki, R.; Linder, N.; Lundin, J.; Kankainen, M.; Ristimaki, A.; Koski, A.; Liikanen, I.; et al. Immunological data from cancer patients treated with Ad5/3-E2F-Delta24-GMCSF suggests utility for tumor immunotherapy. Oncotarget 2015, 6, 4467–4481. [Google Scholar] [CrossRef] [PubMed]
- DeWeese, T.L.; van der Poel, H.; Li, S.; Mikhak, B.; Drew, R.; Goemann, M.; Hamper, U.; DeJong, R.; Detorie, N.; Rodriguez, R.; et al. A phase I trial of CV706, a replication-competent, PSA selective oncolytic adenovirus, for the treatment of locally recurrent prostate cancer following radiation therapy. Cancer Res. 2001, 61, 7464–7472. [Google Scholar] [PubMed]
- Small, E.J.; Carducci, M.A.; Burke, J.M.; Rodriguez, R.; Fong, L.; van Ummersen, L.; Yu, D.C.; Aimi, J.; Ando, D.; Working, P.; et al. A phase I trial of intravenous CG7870, a replication-selective, prostate-specific antigen-targeted oncolytic adenovirus, for the treatment of hormone-refractory, metastatic prostate cancer. Mol. Ther. 2006, 14, 107–117. [Google Scholar] [CrossRef]
- Burke, J.M.; Lamm, D.L.; Meng, M.V.; Nemunaitis, J.J.; Stephenson, J.J.; Arseneau, J.C.; Aimi, J.; Lerner, S.; Yeung, A.W.; Kazarian, T.; et al. A first in human phase 1 study of CG0070, a GM-CSF expressing oncolytic adenovirus, for the treatment of nonmuscle invasive bladder cancer. J. Urol. 2012, 188, 2391–2397. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Zhao, X.; Wu, X.; Guo, Y.; Guo, H.; Cao, J.; Guo, Y.; Lou, D.; Yu, D.; Li, J. A Phase I study of KH901, a conditionally replicating granulocyte-macrophage colony-stimulating factor: Armed oncolytic adenovirus for the treatment of head and neck cancers. Cancer Biol. Ther. 2009, 8, 676–682. [Google Scholar] [CrossRef]
- Nokisalmi, P.; Pesonen, S.; Escutenaire, S.; Sarkioja, M.; Raki, M.; Cerullo, V.; Laasonen, L.; Alemany, R.; Rojas, J.; Cascallo, M.; et al. Oncolytic adenovirus ICOVIR-7 in patients with advanced and refractory solid tumors. Clin. Cancer Res. 2010, 16, 3035–3043. [Google Scholar] [CrossRef]
- Li, J.L.; Liu, H.L.; Zhang, X.R.; Xu, J.P.; Hu, W.K.; Liang, M.; Chen, S.Y.; Hu, F.; Chu, D.T. A phase I trial of intratumoral administration of recombinant oncolytic adenovirus overexpressing HSP70 in advanced solid tumor patients. Gene Ther 2009, 16, 376–382. [Google Scholar] [CrossRef]
- Chiocca, E.A.; Abbed, K.M.; Tatter, S.; Louis, D.N.; Hochberg, F.H.; Barker, F.; Kracher, J.; Grossman, S.A.; Fisher, J.D.; Carson, K.; et al. A phase I open-label, dose-escalation, multi-institutional trial of injection with an E1B-Attenuated adenovirus, ONYX-015, into the peritumoral region of recurrent malignant gliomas, in the adjuvant setting. Mol. Ther. 2004, 10, 958–966. [Google Scholar] [CrossRef]
- Nemunaitis, J.; Senzer, N.; Sarmiento, S.; Zhang, Y.A.; Arzaga, R.; Sands, B.; Maples, P.; Tong, A.W. A phase I trial of intravenous infusion of ONYX-015 and enbrel in solid tumor patients. Cancer Gene Ther. 2007, 14, 885–893. [Google Scholar] [CrossRef]
- Ganly, I.; Kirn, D.; Eckhardt, G.; Rodriguez, G.I.; Soutar, D.S.; Otto, R.; Robertson, A.G.; Park, O.; Gulley, M.L.; Heise, C.; et al. A phase I study of Onyx-015, an E1B attenuated adenovirus, administered intratumorally to patients with recurrent head and neck cancer. Clin. Cancer Res. 2000, 6, 798–806. [Google Scholar]
- Nemunaitis, J.; Tong, A.W.; Nemunaitis, M.; Senzer, N.; Phadke, A.P.; Bedell, C.; Adams, N.; Zhang, Y.A.; Maples, P.B.; Chen, S.; et al. A phase I study of telomerase-specific replication competent oncolytic adenovirus (telomelysin) for various solid tumors. Mol. Ther. 2010, 18, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Carbonero, R.; Salazar, R.; Duran, I.; Osman-Garcia, I.; Paz-Ares, L.; Bozada, J.M.; Boni, V.; Blanc, C.; Seymour, L.; Beadle, J.; et al. Phase 1 study of intravenous administration of the chimeric adenovirus enadenotucirev in patients undergoing primary tumor resection. J. Immunother. Cancer 2017, 5, 71. [Google Scholar] [CrossRef] [PubMed]
- Freytag, S.O.; Khil, M.; Stricker, H.; Peabody, J.; Menon, M.; DePeralta-Venturina, M.; Nafziger, D.; Pegg, J.; Paielli, D.; Brown, S.; et al. Phase I study of replication-competent adenovirus-mediated double suicide gene therapy for the treatment of locally recurrent prostate cancer. Cancer Res. 2002, 62, 4968–4976. [Google Scholar] [PubMed]
- Freytag, S.O.; Stricker, H.; Peabody, J.; Pegg, J.; Paielli, D.; Movsas, B.; Barton, K.N.; Brown, S.L.; Lu, M.; Kim, J.H. Five-year follow-up of trial of replication-competent adenovirus-mediated suicide gene therapy for treatment of prostate cancer. Mol. Ther. 2007, 15, 636–642. [Google Scholar] [CrossRef]
- Freytag, S.O.; Stricker, H.; Pegg, J.; Paielli, D.; Pradhan, D.G.; Peabody, J.; DePeralta-Venturina, M.; Xia, X.; Brown, S.; Lu, M.; et al. Phase I study of replication-competent adenovirus-mediated double-suicide gene therapy in combination with conventional-dose three-dimensional conformal radiation therapy for the treatment of newly diagnosed, intermediate- to high-risk prostate cancer. Cancer Res. 2003, 63, 7497–7506. [Google Scholar]
- Freytag, S.O.; Movsas, B.; Aref, I.; Stricker, H.; Peabody, J.; Pegg, J.; Zhang, Y.; Barton, K.N.; Brown, S.L.; Lu, M.; et al. Phase I trial of replication-competent adenovirus-mediated suicide gene therapy combined with IMRT for prostate cancer. Mol. Ther. 2007, 15, 1016–1023. [Google Scholar] [CrossRef]
- Park, B.H.; Hwang, T.; Liu, T.C.; Sze, D.Y.; Kim, J.S.; Kwon, H.C.; Oh, S.Y.; Han, S.Y.; Yoon, J.H.; Hong, S.H.; et al. Use of a targeted oncolytic poxvirus, JX-594, in patients with refractory primary or metastatic liver cancer: A phase I trial. Lancet Oncol. 2008, 9, 533–542. [Google Scholar] [CrossRef]
- Hwang, T.H.; Moon, A.; Burke, J.; Ribas, A.; Stephenson, J.; Breitbach, C.J.; Daneshmand, M.; De Silva, N.; Parato, K.; Diallo, J.S.; et al. A mechanistic proof-of-concept clinical trial with JX-594, a targeted multi-mechanistic oncolytic poxvirus, in patients with metastatic melanoma. Mol. Ther. 2011, 19, 1913–1922. [Google Scholar] [CrossRef]
- Cripe, T.P.; Ngo, M.C.; Geller, J.I.; Louis, C.U.; Currier, M.A.; Racadio, J.M.; Towbin, A.J.; Rooney, C.M.; Pelusio, A.; Moon, A.; et al. Phase 1 study of intratumoral Pexa-Vec (JX-594), an oncolytic and immunotherapeutic vaccinia virus, in pediatric cancer patients. Mol. Ther. 2015, 23, 602–608. [Google Scholar] [CrossRef]
- Park, S.H.; Breitbach, C.J.; Lee, J.; Park, J.O.; Lim, H.Y.; Kang, W.K.; Moon, A.; Mun, J.H.; Sommermann, E.M.; Maruri Avidal, L.; et al. Phase 1b Trial of Biweekly Intravenous Pexa-Vec (JX-594), an Oncolytic and Immunotherapeutic Vaccinia Virus in Colorectal Cancer. Mol. Ther. 2015, 23, 1532–1540. [Google Scholar] [CrossRef]
- Husseini, F.; Delord, J.P.; Fournel-Federico, C.; Guitton, J.; Erbs, P.; Homerin, M.; Halluard, C.; Jemming, C.; Orange, C.; Limacher, J.M.; et al. Vectorized gene therapy of liver tumors: Proof-of-concept of TG4023 (MVA-FCU1) in combination with flucytosine. Ann. Oncol. 2017, 28, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Mell, L.K.; Brumund, K.T.; Daniels, G.A.; Advani, S.J.; Zakeri, K.; Wright, M.E.; Onyeama, S.J.; Weisman, R.A.; Sanghvi, P.R.; Martin, P.J.; et al. Phase I Trial of Intravenous Oncolytic Vaccinia Virus (GL-ONC1) with Cisplatin and Radiotherapy in Patients with Locoregionally Advanced Head and Neck Carcinoma. Clin. Cancer Res. 2017, 23, 5696–5702. [Google Scholar] [CrossRef] [PubMed]
- Zeh, H.J.; Downs-Canner, S.; McCart, J.A.; Guo, Z.S.; Rao, U.N.; Ramalingam, L.; Thorne, S.H.; Jones, H.L.; Kalinski, P.; Wieckowski, E.; et al. First-in-man study of western reserve strain oncolytic vaccinia virus: Safety, systemic spread, and antitumor activity. Mol. Ther. 2015, 23, 202–214. [Google Scholar] [CrossRef] [PubMed]
- Downs-Canner, S.; Guo, Z.S.; Ravindranathan, R.; Breitbach, C.J.; O’Malley, M.E.; Jones, H.L.; Moon, A.; McCart, J.A.; Shuai, Y.; Zeh, H.J.; et al. Phase 1 Study of Intravenous Oncolytic Poxvirus (vvDD) in Patients with Advanced Solid Cancers. Mol. Ther. 2016, 24, 1492–1501. [Google Scholar] [CrossRef] [PubMed]
- Heinzerling, L.; Kunzi, V.; Oberholzer, P.A.; Kundig, T.; Naim, H.; Dummer, R. Oncolytic measles virus in cutaneous T-cell lymphomas mounts antitumor immune responses in vivo and targets interferon-resistant tumor cells. Blood 2005, 106, 2287–2294. [Google Scholar] [CrossRef] [PubMed]
- Dispenzieri, A.; Tong, C.; LaPlant, B.; Lacy, M.Q.; Laumann, K.; Dingli, D.; Zhou, Y.; Federspiel, M.J.; Gertz, M.A.; Hayman, S.; et al. Phase I trial of systemic administration of Edmonston strain of measles virus genetically engineered to express the sodium iodide symporter in patients with recurrent or refractory multiple myeloma. Leukemia 2017, 31, 2791–2798. [Google Scholar] [CrossRef]
- Galanis, E.; Hartmann, L.C.; Cliby, W.A.; Long, H.J.; Peethambaram, P.P.; Barrette, B.A.; Kaur, J.S.; Haluska, P.J., Jr.; Aderca, I.; Zollman, P.J.; et al. Phase I trial of intraperitoneal administration of an oncolytic measles virus strain engineered to express carcinoembryonic antigen for recurrent ovarian cancer. Cancer Res. 2010, 70, 875–882. [Google Scholar] [CrossRef]
- Burke, M.J.; Ahern, C.; Weigel, B.J.; Poirier, J.T.; Rudin, C.M.; Chen, Y.; Cripe, T.P.; Bernhardt, M.B.; Blaney, S.M. Phase I trial of Seneca Valley Virus (NTX-010) in children with relapsed/refractory solid tumors: A report of the Children’s Oncology Group. Pediatr. Blood Cancer 2015, 62, 743–750. [Google Scholar] [CrossRef]
- Rudin, C.M.; Poirier, J.T.; Senzer, N.N.; Stephenson, J., Jr.; Loesch, D.; Burroughs, K.D.; Reddy, P.S.; Hann, C.L.; Hallenbeck, P.L. Phase I clinical study of Seneca Valley Virus (SVV-001), a replication-competent picornavirus, in advanced solid tumors with neuroendocrine features. Clin. Cancer Res. 2011, 17, 888–895. [Google Scholar] [CrossRef]
- Nakao, A.; Kasuya, H.; Sahin, T.T.; Nomura, N.; Kanzaki, A.; Misawa, M.; Shirota, T.; Yamada, S.; Fujii, T.; Sugimoto, H.; et al. A phase I dose-escalation clinical trial of intraoperative direct intratumoral injection of HF10 oncolytic virus in non-resectable patients with advanced pancreatic cancer. Cancer Gene Ther. 2011, 18, 167–175. [Google Scholar] [CrossRef]
- Hirooka, Y.; Kasuya, H.; Ishikawa, T.; Kawashima, H.; Ohno, E.; Villalobos, I.B.; Naoe, Y.; Ichinose, T.; Koyama, N.; Tanaka, M.; et al. A Phase I clinical trial of EUS-guided intratumoral injection of the oncolytic virus, HF10 for unresectable locally advanced pancreatic cancer. BMC Cancer 2018, 18, 596. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, H.L.; Kim, D.W.; Kim-Schulze, S.; DeRaffele, G.; Jagoda, M.C.; Broucek, J.R.; Zloza, A. Results of a randomized phase I gene therapy clinical trial of nononcolytic fowlpox viruses encoding T cell costimulatory molecules. Hum. Gene Ther. 2014, 25, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Grossardt, C.; Engeland, C.E.; Bossow, S.; Halama, N.; Zaoui, K.; Leber, M.F.; Springfeld, C.; Jaeger, D.; von Kalle, C.; Ungerechts, G. Granulocyte-macrophage colony-stimulating factor-armed oncolytic measles virus is an effective therapeutic cancer vaccine. Hum. Gene Ther. 2013, 24, 644–654. [Google Scholar] [CrossRef]
- Heo, J.; Reid, T.; Ruo, L.; Breitbach, C.J.; Rose, S.; Bloomston, M.; Cho, M.; Lim, H.Y.; Chung, H.C.; Kim, C.W.; et al. Randomized dose-finding clinical trial of oncolytic immunotherapeutic vaccinia JX-594 in liver cancer. Nat. Med. 2013, 19, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Cohn, D.E.; Sill, M.W.; Walker, J.L.; O’Malley, D.; Nagel, C.I.; Rutledge, T.L.; Bradley, W.; Richardson, D.L.; Moxley, K.M.; Aghajanian, C. Randomized phase IIB evaluation of weekly paclitaxel versus weekly paclitaxel with oncolytic reovirus (Reolysin(R)) in recurrent ovarian, tubal, or peritoneal cancer: An NRG Oncology/Gynecologic Oncology Group study. Gynecol. Oncol. 2017, 146, 477–483. [Google Scholar] [CrossRef]
- Galanis, E.; Markovic, S.N.; Suman, V.J.; Nuovo, G.J.; Vile, R.G.; Kottke, T.J.; Nevala, W.K.; Thompson, M.A.; Lewis, J.E.; Rumilla, K.M.; et al. Phase II trial of intravenous administration of Reolysin((R)) (Reovirus Serotype-3-dearing Strain) in patients with metastatic melanoma. Mol. Ther. 2012, 20, 1998–2003. [Google Scholar] [CrossRef]
- Mahalingam, D.; Fountzilas, C.; Moseley, J.; Noronha, N.; Tran, H.; Chakrabarty, R.; Selvaggi, G.; Coffey, M.; Thompson, B.; Sarantopoulos, J. A phase II study of REOLYSIN((R)) (pelareorep) in combination with carboplatin and paclitaxel for patients with advanced malignant melanoma. Cancer Chemother. Pharmacol. 2017, 79, 697–703. [Google Scholar] [CrossRef]
- Noonan, A.M.; Farren, M.R.; Geyer, S.M.; Huang, Y.; Tahiri, S.; Ahn, D.; Mikhail, S.; Ciombor, K.K.; Pant, S.; Aparo, S.; et al. Randomized Phase 2 Trial of the Oncolytic Virus Pelareorep (Reolysin) in Upfront Treatment of Metastatic Pancreatic Adenocarcinoma. Mol. Ther. 2016, 24, 1150–1158. [Google Scholar] [CrossRef]
- Mahalingam, D.; Goel, S.; Aparo, S.; Patel Arora, S.; Noronha, N.; Tran, H.; Chakrabarty, R.; Selvaggi, G.; Gutierrez, A.; Coffey, M.; et al. A Phase II Study of Pelareorep (REOLYSIN((R))) in Combination with Gemcitabine for Patients with Advanced Pancreatic Adenocarcinoma. Cancers 2018, 10, 160. [Google Scholar] [CrossRef]
- Bernstein, V.; Ellard, S.L.; Dent, S.F.; Tu, D.; Mates, M.; Dhesy-Thind, S.K.; Panasci, L.; Gelmon, K.A.; Salim, M.; Song, X.; et al. A randomized phase II study of weekly paclitaxel with or without pelareorep in patients with metastatic breast cancer: Final analysis of Canadian Cancer Trials Group IND.213. Breast Cancer Res. Treat. 2018, 167, 485–493. [Google Scholar] [CrossRef]
- Freytag, S.O.; Stricker, H.; Lu, M.; Elshaikh, M.; Aref, I.; Pradhan, D.; Levin, K.; Kim, J.H.; Peabody, J.; Siddiqui, F.; et al. Prospective randomized phase 2 trial of intensity modulated radiation therapy with or without oncolytic adenovirus-mediated cytotoxic gene therapy in intermediate-risk prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Martinez, A.; Manzanera, A.G.; Sukin, S.W.; Esteban-Maria, J.; Gonzalez-Guerrero, J.F.; Gomez-Guerra, L.; Garza-Guajardo, R.; Flores-Gutierrez, J.P.; Elizondo Riojas, G.; Delgado-Enciso, I.; et al. Intraprostatic distribution and long-term follow-up after AdV-tk immunotherapy as neoadjuvant to surgery in patients with prostate cancer. Cancer Gene Ther. 2013, 20, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Pound, C.R.; Partin, A.W.; Eisenberger, M.A.; Chan, D.W.; Pearson, J.D.; Walsh, P.C. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999, 281, 1591–1597. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, L.A.; Manzanera, A.G.; Bell, S.D.; Cavaliere, R.; McGregor, J.M.; Grecula, J.C.; Newton, H.B.; Lo, S.S.; Badie, B.; Portnow, J.; et al. Phase II multicenter study of gene-mediated cytotoxic immunotherapy as adjuvant to surgical resection for newly diagnosed malignant glioma. Neuro Oncol. 2016, 18, 1137–1145. [Google Scholar] [CrossRef]
- Khuri, F.R.; Nemunaitis, J.; Ganly, I.; Arseneau, J.; Tannock, I.F.; Romel, L.; Gore, M.; Ironside, J.; MacDougall, R.H.; Heise, C.; et al. A controlled trial of intratumoral ONYX-015, a selectively-replicating adenovirus, in combination with cisplatin and 5-fluorouracil in patients with recurrent head and neck cancer. Nat. Med. 2000, 6, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Nemunaitis, J.; Ganly, I.; Khuri, F.; Arseneau, J.; Kuhn, J.; McCarty, T.; Landers, S.; Maples, P.; Romel, L.; Randlev, B.; et al. Selective replication and oncolysis in p53 mutant tumors with ONYX-015, an E1B-55kD gene-deleted adenovirus, in patients with advanced head and neck cancer: A phase II trial. Cancer Res. 2000, 60, 6359–6366. [Google Scholar]
- Reid, T.R.; Freeman, S.; Post, L.; McCormick, F.; Sze, D.Y. Effects of Onyx-015 among metastatic colorectal cancer patients that have failed prior treatment with 5-FU/leucovorin. Cancer Gene Ther. 2005, 12, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Packiam, V.T.; Lamm, D.L.; Barocas, D.A.; Trainer, A.; Fand, B.; Davis, R.L., 3rd; Clark, W.; Kroeger, M.; Dumbadze, I.; Chamie, K.; et al. An open label, single-arm, phase II multicenter study of the safety and efficacy of CG0070 oncolytic vector regimen in patients with BCG-unresponsive non-muscle-invasive bladder cancer: Interim results. Urol. Oncol. 2018, 36, 440–447. [Google Scholar] [CrossRef]
- Heo, J.; Breitbach, C.; Cho, M.; Hwang, T.-H.; Kim, C.W.; Jeon, U.B.; Woo, H.Y.; Yoon, K.T.; Lee, J.W.; Burke, J.; et al. Phase II trial of Pexa-Vec (pexastimogene devacirepvec; JX-594), an oncolytic and immunotherapeutic vaccinia virus, followed by sorafenib in patients with advanced hepatocellular carcinoma (HCC). J. Clin. Oncol. 2013, 31 (Suppl. 15), 4122. [Google Scholar] [CrossRef]
- Xu, R.H.; Yuan, Z.Y.; Guan, Z.Z.; Cao, Y.; Wang, H.Q.; Hu, X.H.; Feng, J.F.; Zhang, Y.; Li, F.; Chen, Z.T.; et al. Phase II clinical study of intratumoral H101, an E1B deleted adenovirus, in combination with chemotherapy in patients with cancer. Ai Zheng 2003, 22, 1307–1310. [Google Scholar]
- Annels, N.E.; Mansfield, D.; Arif, M.; Ballesteros-Merino, C.; Simpson, G.R.; Denyer, M.; Sandhu, S.S.; Melcher, A.A.; Harrington, K.J.; Davies, B.; et al. Phase I Trial of an ICAM-1-Targeted Immunotherapeutic-Coxsackievirus A21 (CVA21) as an Oncolytic Agent against Non Muscle-Invasive Bladder Cancer. Clin. Cancer Res. 2019, 25, 5818–5831. [Google Scholar] [CrossRef] [PubMed]
- A Study of Intratumoral CAVATAK™ in Patients with Stage IIIc and Stage IV Malignant Melanoma (VLA-007 CALM) (CALM). Available online: https://clinicaltrials.gov/ct2/show/results/NCT01227551 (accessed on 5 January 2020).
- Schenk, E.L.; Mandrekar, S.J.; Dy, G.K.; Aubry, M.C.; Tan, A.D.; Dakhil, S.R.; Sachs, B.A.; Nieva, J.J.; Bertino, E.; Lee Hann, C.; et al. A Randomized Double-Blind Phase II Study of the Seneca Valley Virus (NTX-010) versus Placebo for Patients with Extensive-Stage SCLC (ES SCLC) Who Were Stable or Responding after at Least Four Cycles of Platinum-Based Chemotherapy: North Central Cancer Treatment Group (Alliance) N0923 Study. J. Thorac. Oncol. 2020, 15, 110–119. [Google Scholar] [PubMed]
- Evans, D.J.; Wasinger, A.M.; Brey, R.N.; Dunleavey, J.M.; St. Croix, B.; Bann, J.G. Seneca Valley Virus Exploits TEM8, a Collagen Receptor Implicated in Tumor Growth. Front. Oncol. 2018, 8, 506. [Google Scholar] [CrossRef] [PubMed]
- Karapanagiotou, E.M.; Roulstone, V.; Twigger, K.; Ball, M.; Tanay, M.; Nutting, C.; Newbold, K.; Gore, M.E.; Larkin, J.; Syrigos, K.N.; et al. Phase I/II trial of carboplatin and paclitaxel chemotherapy in combination with intravenous oncolytic reovirus in patients with advanced malignancies. Clin. Cancer Res. 2012, 18, 2080–2089. [Google Scholar] [CrossRef] [PubMed]
- Geletneky, K.; Hajda, J.; Angelova, A.L.; Leuchs, B.; Capper, D.; Bartsch, A.J.; Neumann, J.O.; Schoning, T.; Husing, J.; Beelte, B.; et al. Oncolytic H-1 Parvovirus Shows Safety and Signs of Immunogenic Activity in a First Phase I/IIa Glioblastoma Trial. Mol. Ther. 2017, 25, 2620–2634. [Google Scholar] [CrossRef]
- Harrington, K.J.; Hingorani, M.; Tanay, M.A.; Hickey, J.; Bhide, S.A.; Clarke, P.M.; Renouf, L.C.; Thway, K.; Sibtain, A.; McNeish, I.A.; et al. Phase I/II study of oncolytic HSV GM-CSF in combination with radiotherapy and cisplatin in untreated stage III/IV squamous cell cancer of the head and neck. Clin. Cancer Res. 2010, 16, 4005–4015. [Google Scholar] [CrossRef]
- Geevarghese, S.K.; Geller, D.A.; de Haan, H.A.; Horer, M.; Knoll, A.E.; Mescheder, A.; Nemunaitis, J.; Reid, T.R.; Sze, D.Y.; Tanabe, K.K.; et al. Phase I/II study of oncolytic herpes simplex virus NV1020 in patients with extensively pretreated refractory colorectal cancer metastatic to the liver. Hum. Gene Ther. 2010, 21, 1119–1128. [Google Scholar] [CrossRef]
- Galanis, E.; Okuno, S.H.; Nascimento, A.G.; Lewis, B.D.; Lee, R.A.; Oliveira, A.M.; Sloan, J.A.; Atherton, P.; Edmonson, J.H.; Erlichman, C.; et al. Phase I-II trial of ONYX-015 in combination with MAP chemotherapy in patients with advanced sarcomas. Gene Ther. 2005, 12, 437–445. [Google Scholar] [CrossRef]
- Freeman, A.I.; Zakay-Rones, Z.; Gomori, J.M.; Linetsky, E.; Rasooly, L.; Greenbaum, E.; Rozenman-Yair, S.; Panet, A.; Libson, E.; Irving, C.S.; et al. Phase I/II trial of intravenous NDV-HUJ oncolytic virus in recurrent glioblastoma multiforme. Mol. Ther. 2006, 13, 221–228. [Google Scholar] [CrossRef]
- Nemunaitis, J.; Khuri, F.; Ganly, I.; Arseneau, J.; Posner, M.; Vokes, E.; Kuhn, J.; McCarty, T.; Landers, S.; Blackburn, A.; et al. Phase II trial of intratumoral administration of ONYX-015, a replication-selective adenovirus, in patients with refractory head and neck cancer. J. Clin. Oncol. 2001, 19, 289–298. [Google Scholar] [CrossRef]
- Andtbacka, R.H.; Kaufman, H.L.; Collichio, F.; Amatruda, T.; Senzer, N.; Chesney, J.; Delman, K.A.; Spitler, L.E.; Puzanov, I.; Agarwala, S.S.; et al. Talimogene Laherparepvec Improves Durable Response Rate in Patients with Advanced Melanoma. J. Clin. Oncol. 2015, 33, 2780–2788. [Google Scholar] [CrossRef] [PubMed]
- Chesney, J.; Awasthi, S.; Curti, B.; Hutchins, L.; Linette, G.; Triozzi, P.; Tan, M.C.B.; Brown, R.E.; Nemunaitis, J.; Whitman, E.; et al. Phase IIIb safety results from an expanded-access protocol of talimogene laherparepvec for patients with unresected, stage IIIB-IVM1c melanoma. Melanoma Res. 2018, 28, 44–51. [Google Scholar] [CrossRef]
- Kohlhapp, F.J.; Kaufman, H.L. Molecular Pathways: Mechanism of Action for Talimogene Laherparepvec, a New Oncolytic Virus Immunotherapy. Clin. Cancer Res. 2016, 22, 1048–1054. [Google Scholar] [CrossRef] [PubMed]
- Puzanov, I.; Milhem, M.M.; Minor, D.; Hamid, O.; Li, A.; Chen, L.; Chastain, M.; Gorski, K.S.; Anderson, A.; Chou, J.; et al. Talimogene Laherparepvec in Combination with Ipilimumab in Previously Untreated, Unresectable Stage IIIB-IV Melanoma. J. Clin. Oncol. 2016, 34, 2619–2626. [Google Scholar] [CrossRef] [PubMed]
- Alemany, R.; Suzuki, K.; Curiel, D.T. Blood clearance rates of adenovirus type 5 in mice. J. Gen. Virol. 2000, 81 Pt 11, 2605–2609. [Google Scholar] [CrossRef]
- Tyler, K.L.; Fields, B.N. Reoviruses. In Virology, 2nd ed.; Fields, B.N., Knipe, D.M., Chanock, R.M., Hirsch, M.S., Melnick, J.L., Monath, T.P., Roizman, B., Eds.; Raven Press, Ltd.: New York, NY, USA, 1999; pp. 1307–1328. [Google Scholar]
- Russell, S.J.; Federspiel, M.J.; Peng, K.W.; Tong, C.; Dingli, D.; Morice, W.G.; Lowe, V.; O’Connor, M.K.; Kyle, R.A.; Leung, N.; et al. Remission of disseminated cancer after systemic oncolytic virotherapy. Mayo Clin. Proc. 2014, 89, 926–933. [Google Scholar] [CrossRef]

| Trial Name | Virus/ICI | Cancer | n | Central Questions and/or Outcomes |
|---|---|---|---|---|
| Oncolytic Virotherapy Promotes Intratumoral T Cell Infiltration and Improves Anti-PD-1 Immunotherapy [28] (Ribas 2017) | Talimogene Laherparepvec (T-VEC) ICI: Pembrolizumab | Melanoma | 21 | Safety and efficacy evaluation of combination T-VEC+Pembrolizumab in melanoma. No dose limiting toxicities noted. 62% confirmed objective responses. |
| Randomized, Open-Label Phase II Study Evaluating the Efficacy and Safety of Talimogene Laherparepvec in Combination with Ipilimumab Versus Ipilimumab Alone in Patients with Advanced, Unresectable Melanoma [29] (Chesney 2018) | Talimogene Laherparepvec (T-VEC) ICI: Ipilimumab | Melanoma | 198 | Efficacy evaluation of combination Ipilimumab+T-VEC vs. Ipilimumab alone in advance melanoma. 39% Objective response rate (ORR) in combination T-VEC/Ipilimumab arm vs. 18% ORR in single agent Ipilimumab arm. 52% pts showed reduction in visceral lesions in combination arm as compared to only 23% pts in single agent ipilimumab arm. |
| Objective Response Rate Among Patients with Locally Advanced or Metastatic Sarcoma Treated with Talimogene Laherparepvec in Combination with Pembrolizumab [34] (Kelly 2020) | Talimogene Laherparepvec (T-VEC) ICI: Pembrolizumab | Sarcoma | 20 | Phase II study evaluating efficaciy of combination T-VEC and pembrolizumab in metastatic sarcoma. 35% best objective response rate. 20% grade 3 AE and no grade 4 AE noted. |
| LBA40-Phase Ib KEYNOTE-200: A study of an intravenously delivered oncolytic virus, coxsackievirus A21 in combination with pembrolizumab in advanced NSCLC and bladder cancer patients [32] (Rudin 2018) | Cavatak (Coxsackievirus A21) ICI: Pembrolizumab | NSCLC; Bladder Cancer | 78 | No DLT noted. 12% pts reported to have grade 3 treatment related adverse events. No grade 4 or 5 toxicities reported. |
| Trial Name | Virus | Cancer | n | Administration, Adverse Events, Study Conclusions |
|---|---|---|---|---|
| Potential for efficacy of the oncolytic Herpes simplex virus 1716 in patients with oral squamous cell carcinoma [50] (Mace 2008). | HSV1716 | Oral squamous cell carcinoma | 20 | Study used intratumoral injection of HSV 1716; no reportable AE, but no detectable viral replication or effective oncolysis. Study of higher doses required. |
| Intratumoral injection of HSV1716, an oncolytic herpes virus, is safe and shows evidence of immune response and viral replication in young cancer patients [51] (Streby 2017). | HSV1716 | Pediatric extracranial cancers | 9 | Study used intratumoral injection of HSV1716; no major AE: mild constitutional symptoms (fever, chills, cyotopenia) reported. No clinical responses seen by RECIST criteria but viral replication was detected, and signs of inflammatory response was seen on PET/CT. |
| A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor [52] (Hu 2006). | OncoVEXGM–CSF (Herpes Virus JS1/34·5-/47-/GM-CSF) | Breast, head and neck, GI, melanoma | 30 | Study used intratumoral injection at different dose levels in 30 patients. AEs: fever, and injection site reaction. Three patients with SD. Some evidence of tumor necrosis was seen on biopsy which was strongly positive for HSV. |
| A phase 1 trial of oncolytic HSV-1, G207, given in combination with radiation for recurrent GBM demonstrates safety and radiographic responses [53] (Markert 2014). | G207 (HSV-1) | GBM | 9 | Intratumoral injection of G207 given 24 h prior to radiation. 67% with SD or PR. 3 patients with measurable response to radiation. No HSV encephalitis occurred. |
| A herpes oncolytic virus can be delivered via the vasculature to produce biologic changes in human colorectal cancer [54] (Fong 2009). | NV1020 | Metastatic colon cancer in liver previously refractory to chemotherapy (5 FU and leucovorin) | 12 | Study used IV injection of NV1020 into the hepatic artery. CEA levels dropped in patients, and one patient saw 75% reduction of tumor volume. Study reports 7 with SD, 3 with PD, 2 patients with reduction in tumor size at 28 days. Subsequent chemotherapy was hepatic artery injection of floxuridine with dexamethasone. All patients had PR. Results confounded by varying systemic chemotherapy regimens (7 had irinotecan, 2 with oxaliplatin and 3 got both). |
| Intradermal injection of Newcastle disease virus-modified autologous melanoma cell lysate and interleukin-2 for adjuvant treatment of melanoma patients with resectable stage III disease [55] (Voit 2003). | Newcastle disease virus (modified with autologous melanoma cell lysate and IL-2) | Melanoma | 29 | Double blind study with placebo or viral injection after resection of melanoma. No clinical efficacy demonstrated. |
| Phase I trial of intravenous administration of PV701, an oncolytic virus, in patients with advanced solid cancers [56] (Pecora 2002). | PV701 (Newcastle virus) | Advanced solid cancers | 79 | Patients with advanced solid cancers refractory to traditional therapies were divided into 4 groups of differing dosing schedules (single and multiple dosing schedules). Virus was administered via IV. 62 patients were available for assessment with 1 PR and 1 CR. AE included fever, chills, nausea, hypotension. |
| A phase 1 clinical study of intravenous administration of PV701, an oncolytic virus, using two-step desensitization [57] (Laurie 2006). | PV701 (Newcastle virus) | Advanced solid tumors | 16 | Previous studies (citation) demonstrated that patients could tolerate a much higher dose of the virus if they were desensitized first, so this study executed a two-step desensitization. Minimal constitutional symptoms reported, that decreased with subsequent doses. Symptoms were also less severe than in previous studies. Study reports, 1 tumor regression, and 4 SD. |
| An optimized clinical regimen for the oncolytic virus PV701 [58] (Hotte 2007). | PV701 (Newcastle virus) | Advanced cancers | 18 | Study used IV infusions of PV701 at a slow rate. Decreasing the infusion rate allowed patients to receive higher doses of the virus, with fewer AE (particularly decreased constitutional symptoms) and minimized infusion site reaction. Study reports 1 CR, 3 PR, 2 with minor response, and 5 with SD. |
| Phase I trial of cyclophosphamide as an immune modulator for optimizing oncolytic reovirus delivery to solid tumors [59] (Roulstone 2015). | RT3D (Reovirus Type 3 Dearing) | Advanced solid tumors | 36 | Study used combination cyclophosphamide and RT3D (intravenously) to decrease neutralizing antibodies to the virus. While it was well tolerated, it did not reduce NARA (neutralizing antireovirus antibody) titer. |
| A phase I study of the combination of intravenous reovirus type 3 Dearing and gemcitabine in patients with advanced cancer [60] (Lolkema 2011). | RT3D (Reovirus Type 3 Dearing) | advanced solid cancers | 16 | First study to combine IV Reovirus with chemotherapy. AE were similar to previous studies with fever, nausea/vomiting, and chills. Protocol revised because there were grade 3 rises in LFTs (but these patients were also taking acetaminophen.) Reovirus may exacerbate gemcitabine-related liver toxicity. Clinical response was best in a patient with nasopharyngeal cancer, but OR minimal. |
| A phase I study of intravenous oncolytic reovirus type 3 Dearing in patients with advanced cancer [61] (Vidal 2008). | RT3D (Reovirus Type 3 Dearing) | Advanced cancers | 36 | Patients received escalating doses of IV Reovirus. There were no dose limiting toxicities, but some grade 1–2 flu-like symptoms were reported and were dose dependent. Some antitumor activity was observed by monitoring serum tumor marker levels, but not by RECIST criteria. Neutralizing Ab were detected in all patients |
| A phase I trial of intratumoral administration of reovirus in patients with histologically confirmed recurrent malignant gliomas [62] (Forsyth 2008). | Reolysin | Recurrent malignant gliomas | 12 | Study used intratumoral injection of reovirus with escalating doses. No grade 3–4 adverse events. Study reported 1 SD, 10 with PD. (1 was unable to be evaluated) |
| Two-stage phase I dose-escalation study of intratumoral reovirus type 3 dearing and palliative radiotherapy in patients with advanced cancers [63] (Harrington 2010) | Reolysin | Advanced solid cancers open to palliative radiation | 23 | Protocol used escalating doses of radiotherapy followed by intratumoral injections of RT3D. AE included flu-like symptoms (grade 2 or less) as well as neutropenia and lymphopenia. Low dose group had 2 with PR and 5 with SD, and in the high dose group 5/7 had PR and 2/7 with SD. No viral shedding seen in bodily fluids. |
| REO-10: a phase I study of intravenous reovirus and docetaxel in patients with advanced cancer [64] (Comins 2010). | Reolysin | Advanced solid cancers | 16 | Study used IV Reolysin in combination with docetaxel chemotherapy. There was 1 CR, 3 PR, and 10 with SD. Overall 88% of patients had some degree of disease control. One grade 4 neutropenia was reported. |
| REO-001: A phase I trial of percutaneous intralesional administration of reovirus type 3 dearing (Reolysin®) in patients with advanced solid tumors [65] (Morris 2013). | Reolysin | Advanced solid tumors | 19 | Study used intra-lesional injection of virus and was well tolerated. Most reactions were grade 1–2, including malaise, and some erythema around injection site. Study reported 37% with local tumor response, including 1 CR, 3 PR, and 4 with SD. |
| A phase I trial of single-agent reolysin in patients with relapsed multiple myeloma [66] (Sborov 2014) | Reolysin | Multiple myeloma | 12 | Virus administered intravenously. No dose limiting AE reported but grade 3 AE included hypophosphatemia, thrombocytopenia, and neutropenia. While the virus did replicate in MM cells, there was little viral protein recovered from cells. Researchers concluded it could work as part of a combination therapy, but not as monotherapy. |
| Phase 1 clinical trial of intratumoral reovirus infusion for the treatment of recurrent malignant gliomas in adults [67] (Kicielinski 2014) | Reolysin | Malignant glioma | 15 | Study used intratumoral injection. This was a dose finding study (previous study established safety). No MTD or dose limiting toxicity identified. Adverse effects related to underlying cancer, such as seizure, convulsions rather than virus. Study reported 1 PR, and a few with SD |
| A phase I trial and viral clearance study of reovirus (Reolysin) in children with relapsed or refractory extra-cranial solid tumors: a Children’s Oncology Group Phase I Consortium report [68] (Kolb 2015). | Reolysin | Extracranial solid tumors | 24 | Study used IV injection of Reolysin alone or with cyclophosphamide. No objective response to therapy, and only 1/3 of patients had a detectable viral load after 5 days; none did after 17 days. Study reports 1 grade 5 respiratory failure and 1 grade 5 thromboembolic event. |
| Recurrent glioblastoma treated with recombinant poliovirus [69] (Desjardins 2018) | PVSRIPO (Polio Virus) | Glioblastoma | 61 | Virus was injected intratumorally. Grade 4 ICH at the highest injection dose was the only dose-limiting toxicity. Survival rate was higher in those who received therapy as compared to historical controls, at both 24 and 36 months. |
| Immunological effects of low-dose cyclophosphamide in cancer patients treated with oncolytic adenovirus [70] (Cerullo 2011). | Ad5/3-(delta)24 | Advanced solid tumors resistant to chemotherapy | 21 | Study used intratumoral injection with adenovirus followed by cyclophosphamide treatment in different dosing groups. AE were mostly grade 1–2 constitutional symptoms. The one year PFS and OS was increased compared to traditional chemotherapy resistant cancers. Study reports 8/12 patients with RECIST response: 2 with MR, 6 with SD, and 4 with PD. |
| A phase I clinical trial of Ad5/3-Δ24, a novel serotype-chimeric, infectivity-enhanced, conditionally-replicative adenovirus (CRAd), in patients with recurrent ovarian cancer [71] (Kim 2013). | Ad5/3-(delta)24 | Ovarian Cancer | 9 | Study used intraperitoneal injection of the virus. AE were flu-like grade 1–2: fever/chills, myalgias, fatigue, and nausea. Study reported 3 patients with a decrease in CA-125 levels at 1 month. |
| A phase I study of a tropism-modified conditionally replicative adenovirus for recurrent malignant gynecologic diseases [72] (Kimball 2010). | Ad5/3-(delta)24 | Gynecologic malignancy | 21 | Study used intraperitoneal injection of virus. Reported grade 1-2 adverse events included fatigue, fever an abdominal pain. Study reported 71% of patients had SD, and the remainder had PD at 1 month. No CR or PR were achieved. |
| Integrin targeted oncolytic adenoviruses Ad5-D24-RGD and Ad5-RGD-D24-GMCSF for treatment of patients with advanced chemotherapy refractory solid tumors [73] (Pesonen 2012). | Ad5-D24-RGD and Ad5-RGD-D24-GMCSF | advanced solid tumors resistant to chemotherapy | 16 | 16 patients were injected with adenovirus, 9 treated with Ad5-D24-RGD, and 7 treated with Ad5-RGD-D24-GMCSF. Virus for one group contained GM-CSF; as large tumors have immunosuppressive characteristics, GM-CSF might stimulate the immune system. Some patients in the GMCSF group showed SD, while all patients in the other group progressed. AE were low grade (1–2); constitutional symptoms or injection site pain. |
| Antiviral and antitumor T cell immunity in patients treated with GM-CSF-coding oncolytic adenovirus [74] (Kanerva 2013). | CGTG-102 (Ad5/3-delta24-GMCSF) | Advanced solid tumors | 60 | 60 patients received intratumoral injections. The study compared single injection (39 patients) to multiple injections (21 patients) to establish safety of multiple. Stable disease or better was achieved in 50% with serial injection vs. 41% with single injection. Mostly grade 1–2 AE occurred (constitutional symptoms). |
| Immunological data from cancer patients treated with Ad5/3-E2F-Δ24-GMCSF suggests utility for tumor immunotherapy [75] (Hemminki 2015). | CGTG-602 (Ad5/3-E2F-delta24-GMCSF) | Advanced solid tumors | 13 | 13 patients enrolled with varying doses and treatment rounds of virus via IV. 50% of patients noted a response to treatment. AE were predominately grade 1–2 constitutional symptoms, but some grade 3 AE were seen. |
| A phase I trial of CV706, a replication-competent, PSA selective oncolytic adenovirus, for the treatment of locally recurrent prostate cancer following radiation therapy [76] (DeWeese 2001). | CV706 (PSA selective adenovirus) | Prostate cancer | 20 | Study used intraprostatic injection of virus into patients with locally recurrent prostate cancer. There were no grade 3 or greater toxicities. There was evidence of replication in biopsy tissues. Those treated with higher doses of the virus had at least 50% drop in PSA levels. |
| A phase I trial of intravenous CG7870, a replication-selective, prostate-specific antigen-targeted oncolytic adenovirus, for the treatment of hormone-refractory, metastatic prostate cancer [77] (Small 2006). | CG7870 | Hormone refractory metastatic prostate cancer | 23 | Patients received intravenous dosing of the virus. Most AE were constitutional symptoms such as fatigue, fevers, nausea. Three grade 3 reactions occurred, including severe fatigue. MTD was reached due to transaminitis and elevated d-dimer levels. Using PSA as the endpoint, study reported 5 patients with PSA reduction of 25–49% after 1 treatment, but no PR or CR were reported. |
| A first in human phase 1 study of CG0070, a GM-CSF expressing oncolytic adenovirus, for the treatment of nonmuscle invasive bladder cancer [78] (Burke 2012). | CG0070 (GM-CSF expressing adenovirus) | Bladder cancer (non-muscle) | 35 | Patients received intravesical infusions of virus. Grade 1–2 bladder toxicities were the most frequent AE but 3 patients had grade 3 reactions for nocturia, dysuria and lymphopenia. Study reported CR of 48.6% across all groups, and higher (58.3%) in those with high Rb phosphorylation. |
| A Phase I study of KH901, a conditionally replicating granulocyte-macrophage colony-stimulating factor: armed oncolytic adenovirus for the treatment of head and neck cancers [79] (Chang 2009). | KH901 (GM-GSF Expressing Adenovirus) | recurrent head and neck cancers | 23 | KH901, selective for cells expressing telomerase, was injected intratumorally in patients with recurrent head and neck cancer. Groups included single, and multi-dose injections at escalating dosages. There were was no dose-limiting AE; majority were grade 1-2 constitutional symptoms. Study reports 7/19 patients with PD, 12 with SD. |
| Oncolytic adenovirus ICOVIR-7 in patients with advanced and refractory solid tumors [80] (Nokisalmi 2010). | ICOVIR-7 (adenovirus) | Advanced solid tumors | 21 | Study used intratumoral injection at varying doses. One grade 3 anemia was observed, while remaining side effects were grade 1–2 and included flu-like symptoms, increased liver transaminases, and hyponatremia. Study reported 5 objective responses including 1 PR, 2 minor, and 2 SD. All patients had PD prior to trial initiation. |
| A phase I trial of intratumoral administration of recombinant oncolytic adenovirus overexpressing HSP70 in advanced solid tumor patients [81] (Li 2009). | Telomelysin/OBP-301 (adenovirus with human telomerase reverse transcriptase, hTERT) | Advanced solid tumors | 27 | Study used intratumoral injection of virus in a dose escalation phase I study. Rare grade III fever and grave IV thrombocytopenia at high doses were observed. Most AE were fever, reaction at the injection site, as well as thrombocytopenia, and depressed leukocyte and lymphocyte counts. Study reported a minimum of 48% with SD, and 11% had CR or PR. |
| A phase I open-label, dose-escalation, multi-institutional trial of injection with an E1B-Attenuated adenovirus, ONYX-015, into the peritumoral region of recurrent malignant gliomas, in the adjuvant setting [82] (Chiocca 2004). | ONYX-015 | Malignant glioma | 24 | 24 patients received varying doses of ONYX-015 injected into 10 areas of the resected glioma cavity. No severe AE were reported that were likely related to treatment (10 patient did have AE, including 1 grade 3–4 neuropathy) Only 1 patient did not have PD and No real treatment effect could be correlated with the viral treatment. |
| A phase I trial of intravenous infusion of ONYX-015 and Enbrel in solid tumor patients [83] (Nemunaitis 2007). | ONYX-015 | Advanced cancers | 9 | Nine patients divided in 3 groups received IV infusion of onyx-015 of varying doses, with a dose of Enbrel. Study reported 4/9 with SD, but no regression was seen. AE were mild. Circulating viral DNA was higher when virus infusion is given in combination with Enbrel |
| A phase I study of Onyx-015, an E1B attenuated adenovirus, administered intratumorally to patients with recurrent head and neck cancer [84] (Ganly 2000). | ONYX-15 | Recurrent head and neck cancer | 22 | Study used single intratumoral injection that was well tolerated. Grade 1–2 constitutional symptoms were most common. Study reported no OR by RECIST criteria, but evidence of tumor necrosis seen on MRI in 5 patients with questionable PR was noted. |
| A phase I study of telomerase-specific replication competent oncolytic adenovirus (telomelysin) for various solid tumors [85] (Nemunaitis 2010). | H103 (Adenovirus expressing HSP70) | Advanced solid tumors | 27 | Study used intratumoral injection of virus in a dose escalation phase I study. Rare grade III fever and grave IV thrombocytopenia at high doses was observed. Most AE were fever, and a local reaction at the injection site, as well as thrombocytopenia, and depressed leukocyte and lymphocyte counts. Study reported 48% of patients had at least SD or better, and 11% had CR or PR. |
| Phase 1 study of intravenous administration of the chimeric adenovirus enadenotucirev in patients undergoing primary tumor resection [86] (Garcia-Carbonero 2017). | Enadenotucirev (adenovirus aka ColoAd1) | Colorectal, NSCLC, Urothelial, RCC | 17 | Study used IV infusion for NSCLC, RCC and urothelial cancers, and intrathehecal injection in colorectal cancer. Both demonstrated high local CD8+ cell infiltration, with no significant treatment-related AE. |
| Phase I study of replication-competent adenovirus-mediated double suicide gene therapy for the treatment of locally recurrent prostate cancer [87] (Freytag 2002). Five-year follow-up of trial of replication-competent adenovirus-mediated suicide gene therapy for treatment of prostate cancer [88] (Freytag 2007). | Ad5-CD/TKrep | Prostate (recurrent) | 16 | Patients were injected with virus, and two days later received ganciclovir and 5-fluorocytosine prodrug. Study reported >25% decreased PSA levels in 44% of patients. A 5-year follow up showed PSA doubling time was extended in patients who received the virus treatment indicating that patients had longer until salvage treatment was needed. |
| Phase I study of replication-competent adenovirus-mediated double-suicide gene therapy in combination with conventional-dose three-dimensional conformal radiation therapy for the treatment of newly diagnosed, intermediate- to high-risk prostate cancer [89] (Freytag 2003). | Ad5-CD/TKrep | Prostate | 15 | Patients had intraprostatic injection of adenovirus with cytosine deaminase and HSV thymidine kinase genes. 2 days later the patients received 5-fluorocytosine and valganciclovir prodrug for up to 4 weeks along with radiation. PSA ½ life was decreased in those with more than 1 week of prodrug therapy. 94% of AE were mild to moderate; severe reactions were similar to reactions obtained with standard radiation therapy. |
| Phase I trial of replication-competent adenovirus-mediated suicide gene therapy combined with IMRT for prostate cancer [90] (Freytag 2007). | Ad5-yCD/mutTKSR39rep-ADP | Prostate | 9 | This study used a second generation virus with improved enzyme activity administered via intraprostatic injection. Reported AE include 13% with grade 3 lymphopenia; other AE were grade 1–2. Prostate biopsies at the end of the trial had fewer positives for residual adenocarcinoma than expected (22% rather than >40%) |
| Use of a targeted oncolytic poxvirus, JX-594, in patients with refractory primary or metastatic liver cancer: a phase I trial [91] (Park 2008). | Pexa-Vec/JX-594 (pexastimogene devacirepvec) | Primary or metastatic liver cancer | 14 | This was a dose-escalation study of intratumoral injection of JX-594. Grade 3 hyperbilirubinemia occurred in patients with the highest dose. All experienced flu-like symptoms, ranging grade I–III and 4 had short-lived grade I–III dose dependent thrombocytopenia. Study reported response in the injected as well as non-injected tumors; 3 PR, 6 with SD and 1 with PD (and 4 could not be evaluated via imaging for different reasons). |
| A mechanistic proof-of-concept clinical trial with JX-594, a targeted multi-mechanistic oncolytic poxvirus, in patients with metastatic melanoma [92] (Hwang 2011). | Pexa-Vec/JX-594 (pexastimogene devacirepvec) | Metastatic melanoma | 10 | Patients were injected intratumorally with 1/10th the dose of normal JX-594. Biopsies demonstrated evidence of tumor necrosis, as well as gene expression from JX-594. Clinical outcomes were not reported (not focus of study). Mild constitutional symptoms as previously reported were the only AE. |
| Phase 1 study of intratumoral Pexa-Vec (JX-594), an oncolytic and immunotherapeutic vaccinia virus, in pediatric cancer patients [93] (Cripe 2015). | Pexa-Vec/JX-594 (pexastimogene devacirepvec) | neuroblastoma, Ewing sarcoma, HCC | 3 | Intratumoral injection of Pexa-Vec in 3 patients. All 3 developed skin pustules (grade 1) that lasted 3–4 weeks. Study reported no OR by RECIST criteria; one patient had evidence of tumor necrosis on imaging. |
| Phase 1b trial of biweekly intravenous Pexa-Vec (JX-594), an oncolytic and immunotherapeutic vaccinia virus in colorectal cancer [94] (Park 2015). | Pexa-Vec/JX-594 (pexastimogene devacirepvec) | Colorectal | 15 | Study used IV infusion of Pexa-Vec in 15 patients. AE were grade 1–2, and mostly constitutional symptoms such as fever, malaise, chills, myalgias. Study reported 67% patients with SD as seen on imaging. |
| Vectorized gene therapy of liver tumors: proof-of-concept of TG4023 (MVA-FCU1) in combination with flucytosine [95] (Husseini 2017). | TG4023 (MVA-FCU1 modified vaccinia virus) | Primary or metastatic liver tumors resistant to other forms of treatment | 16 | TG4023 contains the gene for an enzyme to convert flucytosine into cytotoxic 5-fluorouracil. 16 patients had intratumoral injection at escalating doses, and then the prodrug (flucytosine) on day 2. Tumor biopsy demonstrated therapeutic levels of the active drug were reached. 7 patients had dose limiting toxicity with non-sustained rise in AST and ALT. Most frequent AE were constitutional symptoms including anorexia, fever, and fatigue. Study reported 50% of patients with SD, the other half with PD. |
| Phase I trial of intravenous oncolytic vaccinia virus (GL-ONC1) with cisplatin and radiotherapy in patients with locoregionally advanced head and neck carcinoma [96] (Mell 2017). | GL-ONC1 (Vaccinia Virus) | Head and Neck Cancer (locoregionally advances without metastasis) | 19 | Study used IV injection of virus along with cisplatin and radiotherapy. Most AE were grade 1–2 constitutional symptoms and rash, but 2 patients had grade 3 hypotension, nausea/vomiting and mucositis. Study reported 5/19 patients had virus present in the biopsy. At 1 year/2 years: 74.4%/64.1% with PFS and 84.6%/69.2% OS |
| First-in-man study of western reserve strain oncolytic vaccinia virus: safety, systemic spread, and antitumor activity [97] (Zeh 2015). | vvDD (Poxvirus – western reserve strain oncolytic vaccinia virus) | Advanced solid tumors | 16 | Study used intratumoral injection of virus. Selective viral replication reported in both injected and non-injected rumors. Study reported 1 grade 3 events occurred, which was pain in a breast cancer patient around the time of highest inflammation. |
| Phase 1 Study of intravenous oncolytic Poxvirus (vvDD) in patients with advanced solid cancers [98] (Downs-Canner 2016). | vvDD (Poxvirus – western reserve strain oncolytic vaccinia virus) | Advanced colorectal or other solid cancers | 11 | Study used IV administration. No dose limiting toxicities reported, and most AE were grade 1 or 2 constitutional symptoms. Study reported Th1 cytokines and inflammatory reaction occurred. A mixed response on some liver metastasis with improvement of cutaneous melanoma. |
| Oncolytic measles virus in cutaneous T cell lymphomas mounts antitumor immune responses in vivo and targets interferon-resistant tumor cells [99] (Heinzerling 2005). | MV (Measles Virus, Edmonston-Zagreb strain) | Cutaneous T cell Lymphoma | 5 | Study used intratumoral injections of live virus with dose escalation. Endpoint was TBI (Tumor Burden Index: 1 lesion resolved (CR); 2 showed evidence of regression in local but non-injected lesions; remaining tumors unchanged. AE included grade 1 injection site erythema, arthralgias, itching only |
| Phase I trial of systemic administration of Edmonston strain of measles virus genetically engineered to express the sodium iodide symporter in patients with recurrent or refractory multiple myeloma [100] (Dispenzieri 2017). | MV-NIS (measles virus with sodium iodide symporter) | Relapsed and refractory multiple myeloma | 29 | Study used IV injection; one group with MV-NIS alone, another with cyclophosphamide prior to MV-NIS treatment. Study reported grade 3–4 hematologic AEs including decreased blood counts neutropenia, thrombocytopenia, anemia, and lymphopenia for both groups. 1 CR reported with some cases of short lived decreased circulating free light chains (increased once the body cleared the virus). Iodine was used to identify infection in myeloma cells. |
| Phase I trial of intraperitoneal administration of an oncolytic measles virus strain engineered to express carcinoembryonic antigen for recurrent ovarian cancer [101] (Galanis 2010). | MV-CEA (Measles virus, Edmonston strain) | Taxol and platinum-refractory recurrent ovarian with normal CEA levels | 21 | Study used intraperitoneal injection of the virus with CEA as measure of viral replication. Study reports best response (per RECIST) was SD in 14/21 and was dose dependent; 5 patients had marked decrease of CA-125 levels. Median survival was 12·15 compared to 6 months for historical controls. |
| Phase I trial of Seneca Valley Virus (NTX-010) in children with relapsed/refractory solid tumors: a report of the Children’s Oncology Group [102] (Burke 2015). | NTX-010 (Seneca Valley Virus) | Pediatric patients wih neuroblastoma, rhabdomyosarcoma, rare tumors with NET features | 22 | Study designed in 2 parts: part A was dose finding, virus only, using 3 doses; part B added cyclophosphamide. Study reported AEs were leukopenia, neutropenia; tumor pain in 1 patient was the only grade 3 toxicity observed. Nearly all patients (17/18) had neutralizing antibodies which prohibited virus efficacy. |
| Phase I clinical study of Seneca Valley Virus (SVV-001), a replication-competent picornavirus, in advanced solid tumors with neuroendocrine features [103] (Rudin 2011). | SVV-001 (Seneca Valley Virus, a picornavirus) | Advanced solid tumors with neuroendocrine features | 30 | Study used IV injection of virus. 1 patient with SCLC was progression free at 10 months. AEs included flu like symptoms (fever, fatigue headache) and one grade 3 lymphopenia |
| A phase I dose-escalation clinical trial of intraoperative direct intratumoral injection of HF10 oncolytic virus in non-resectable patients with advanced pancreatic cancer [104] (Nakao 2011). | HF-10 | Pancreatic cancer | 6 | Study used 3 intratumoral injections of HF-10. Study reported PD in 2 patients, SD in 3 patients, and 1 had a PR. No AE reported. |
| A Phase I clinical trial of EUS-guided intratumoral injection of the oncolytic virus, HF10 for unresectable locally advanced pancreatic cancer [105] (Hirooka 2018). | HF-10 | Pancreatic cancer | 10 | Study used EUS injection of HF10 for unresectable pancreatic cancer up to 4 times, every 2 weeks. Co-treatment was erlotinib and gemcitabine. Study reported AEs: 5 patients with severe myelosuppression; 2 patients had severe events not due to HF10. Study outcomes: 2 PD, 4 SD, and 3 PR. PFS 6·3 months, OS 15·5 months. 2 patients achieved CR after downstaging and surgery. |
| Results of a randomized phase I gene therapy clinical trial of nononcolytic fowlpox viruses encoding T cell costimulatory molecules [106] (Kaufman 2014). | rF-B7.1 and rF-TRICOM (recombinant fowlpox virus with either B7.1 or three genes: B7.1, ICAM-1, and LFA-3) | Melanoma and colon cancer | 12 | Study used intratumoral injection of one of the two viruses and at varying doses, every 4 weeks. AE were minimal, including injection site pain and pyrexia (in only 4 patients). Study reported no objective clinical responses but safety was established, and some T cell activity specific to the tumors was seen Stable disease noted for 3 patients which included both colon cancer cases. |
| Trial Name | Virus | Cancer | n | Outcomes |
|---|---|---|---|---|
| Randomized phase IIB evaluation of weekly paclitaxel versus weekly paclitaxel with oncolytic reovirus (Reolysin®) in recurrent ovarian, tubal, or peritoneal cancer [109] (Cohn 2017). | Reolysin | Ovarian, tubal or peritoneal cancer | 108 | Study reported Reolysin did not improve outcomes enough to induce further study. |
| Phase II trial of intravenous administration of Reolysin(®) (Reovirus Serotype-3-dearing Strain) in patients with metastatic melanoma [110] (Galanis 2012). | Reolysin | Melanoma | 21 | Viral replication confirmed in biopsies; 1 patient had 75–90% tumor necrosis, which provided evidence for treatment effect. |
| A phase II study of REOLYSIN® (pelareorep) in combination with carboplatin and paclitaxel for patients with advanced malignant melanoma [111] (Mahalingam 2017). | Reolysin | Melanoma | 14 | Study reported 3 partial responses: 1% ORR; PFS 5·2 months; OS 10·9 months. 1 year OS was 43%. Disease control rate 85%. |
| Randomized phase 2 trial of the oncolytic virus Pelareorep (Reolysin) in upfront treatment of metastatic pancreatic adenocarcinoma [112] (Noonan 2016). | Reolysin | Metastatic pancreatic adenocarcinoma | 73 | Study reported that addition of Reolysin to paclitaxel+carboplatin, did not improve PFS, but was well-tolerated. Presence of KRAS mutation also did not affect outcome. |
| A Phase II study of Pelareorep (REOLYSIN®) in combination with gemcitabine for patients with advanced pancreatic adenocarcinoma [113] (Mahalingam 2018). | Reolysin | Pancreatic adenocarcinoma | 34 | Study reported OS (10·2 vs. 6·8 months) as well as 1- and 2-year survival (45% and 22%, respectively) was increased compared to historical controls that used single agent gemcitabine (20–22%, 2·5%). |
| A randomized phase II study of weekly paclitaxel with or without pelareorep in patients with metastatic breast cancer: final analysis of Canadian Cancer Trials Group IND.213 [114] (Bernstein 2018). | Reolysin | Metastatic breast cancer | 74 | There was no statistical difference in RR or PFS but there was increased OS: 17·4 months vs. 10·4 months with paclitaxel alone. |
| Prospective randomized phase 2 trial of intensity modulated radiation therapy with or without oncolytic adenovirus-mediated cytotoxic gene therapy in intermediate-risk prostate cancer [115] (Freytag 2014). | Ad5-yCD/mutTKSR39rep-ADP adenovirus | Prostate | 44 | Combined intensity modulated radiation therapy (IMRT) with adenovirus. Significant decrease in the number of positive biopsies at 2 years: IMRT 58%; IMRT+virotherapy 33% (P = 0.13). |
| Intraprostatic distribution and long-term follow-up after AdV-tk immunotherapy as neoadjuvant to surgery in patients with prostate cancer [116] (Rojas-Martinez, 2013). | AdV-tk (aka aglatimagene besadenovec or ProstAtak | Prostate | 10 | Injected AdV-tk with valcyclovir or ganciclovir in 9 patients scheduled for prostatectomy. 6 of these patients had high risk features. At 10 years did not have signs of recurrence/metastasis. Historic controls with high risk features typically have 15% PSA failure with 34% of those have metastasis [117] (Pound 1999) |
| Phase II multicenter study of gene-mediated cytotoxic immunotherapy as adjuvant to surgical resection for newly diagnosed malignant glioma [118] (Wheeler 2016). | AdV-tk (aka aglatimagene besadenovec or ProstAtak | Glioma | 48 | Patients with malignant gliomas were injected AdV-tk during surgery. They then received valcyclovir along with standard therapy of radiation and temozolomide. Overall survival was extended for those who received viral therapy (especially in the group in which total gross resection was achieved at the initial surgery). |
| A controlled trial of intratumoral ONYX-015, a selectively-replicating adenovirus, in combination with cisplatin and 5-fluorouracil in patients with recurrent head and neck cancer [119] (Khuri 2000). | ONYX-15 | Recurrent squamous cell head and neck cancer | 37 | Patients were given cisplatin/5 FU along with intratumoral injection of ONYX-015. Study reported 27% CR and 36% PR. There were flu-like symptoms and injection site pain most commonly, and rare grade 3–4 mucositis. |
| Selective replication and oncolysis in p53 mutant tumors with ONYX-015, an E1B-55kD gene-deleted adenovirus, in patients with advanced head and neck cancer: a phase II trial [120] (Nemunaitis 2000). | ONYX-15 | Recurrent head and neck cancer | 37 | Intratumoral injection of virus led to marked tumor regression (as defined as >50% of lesion) in 21% of patients. Biopsy of surrounding normal tissues were negative for viral infection. |
| Hepatic arterial infusion of a replication-selective oncolytic adenovirus (dl1520): phase II viral, immunologic, and clinical endpoints [37] (Reid 2002). | Onyx-015 (Adenovirus dl1520) | Gastrointestinal cancer with liver metastasis | 27 | Study used hepatic artery infusion of the virus in combination with traditional chemotherapy (5-FU and leucovorin). Study reported biochemical response with virotherapy (increase TNF, IFN-gamma, IL-6 and IL-10) in some tumors resistant to chemotherapy alone. Some grade 3–4 adverse events were seen with hyperbilirubinemia. |
| Effects of Onyx-015 among metastatic colorectal cancer patients that have failed prior treatment with 5-FU/leucovorin [121] (Reid 2005). | Onyx-015 (Adenovirus dl1520) | Colorectal cancer with metastasis to liver | 24 | Study used hepatic artery infusion of virus in subjects that failed 5-FU/leucovorin. Study reported mixed results: some evidence of tumor necrosis and regression; many patients removed early due to CT-demonstrated enlargement of tumors. However, CT information may reflect inflammation in response to tumor infection with virus prior to regression; PET rather than CT use suggested in the future. |
| An open label, single-arm, phase II multicenter study of the safety and efficacy of CG0070 oncolytic vector regimen in patients with BCG-unresponsive non-muscle-invasive bladder cancer: Interim results [122] (Packiam 2017). | CG0070 (GM-CSF expressing adenovirus) | Non-muscle invasive bladder cancer (NMIBC), | 45 | Study used intravesical CG0070 for those resistant to bacillus Calmette–Guerin (BCG). Study reported a 47% CR at 6 months. |
| Randomized dose-finding clinical trial of oncolytic immunotherapeutic vaccinia JX-594 in liver cancer [108] (Heo 2013), | Pexa-Vec (JX-594 vaccinia virus) | HCC | 22 | mRECIST and Choi tumor response rates were equivalent for the low and high dose treatment groups. Median survival was greater in the high dose group (14·1 months vs. 6·7 months). |
| Phase II trial of Pexa-Vec (pexastimogene devacirepvec; JX-594), an oncolytic and immunotherapeutic vaccinia virus, followed by sorafenib in patients with advanced hepatocellular carcinoma (HCC) [123] (Heo 2013). | Pexa-Vec (JX-594 vaccinia virus) | HCC | 25 | Study used Pexa-Vec IV for Day 1 followed by intratumoral injections on Days 8 and 22; sorafenib was administered on Day 25. Per mRECIST criteria, 62% had disease control after Pexa-vec treatment, and 59% after use of sorafenib. |
| Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor-encoding, second-generation oncolytic herpesvirus in patients with unresectable metastatic melanoma [35] (Senzer 2009). | OncoVEXGM–CSF (Herpes Virus JS1/34·5-/47-/GM-CSF) | Melanoma | 50 | Study used intratumoral injection of the virus. Study reported a 26% response rate using the RECIST criteria which included uninjected tumors (and even visceral tumors). |
| Phase II clinical study of intratumoral H101, an E1B deleted adenovirus, in combination with chemotherapy in patients with cancer [124] (Xu 2003). | H101 (E1B deleted adenovirus) | Malignant tumors | 50 | Study used intratumoral injection 5 days/week for 3 weeks along with standard chemotherapy. Response rate was 28% vs 13% in control group. Grade 4 hematologic AE in 4 patients. |
| Phase I Trial of an ICAM-1-Targeted Immunotherapeutic-Coxsackievirus A21 (CVA21) as an Oncolytic Agent Against Non Muscle-Invasive Bladder Cancer [125] (Annels 2019) | Coxsackievirus A21 (CVA21) | Non-muscle invasive bladder cancer | 15 | Nine patients received intravesicular injection of virus; 6 patients received viral injection and subtherapeutic mitotycin C before resection. 1 CR (by histology) No serious AE reported. |
| A Study of Intratumoral CAVATAK™ in Patients with Stage IIIc and Stage IV Malignant Melanoma (VLA-007 CALM) (CALM) [126] (NCT01227551) | Coxsackievirus A21 (CVA21) | Stage IIIc and Stage IV Malignant Melanoma | 57 | Intratumoral injection of virus. Reported 38·6% immune-related Progression-Free Survival at 6 months, 21% durable response rate (CR+PR). 19% experience severe AE. |
| Trial Name | Virus | Cancer | n | Administration, Adverse Events, Study Conclusions |
|---|---|---|---|---|
| Phase I/II trial of carboplatin and paclitaxel chemotherapy in combination with intravenous oncolytic reovirus in patients with advanced malignancies [129] (Karapanagiotou 2012). | RT3D (Reovirus Type 3 Dearing) | Advanced head and neck cancer | 31 | Study used IV infusion of RT3D with carboplatin/paclitaxel. Study reported treatment was well tolerated, no MTD, and toxicities were largely grade I/II. Outcomes reported by RECIST were 1 CR (3·8%) and 6 PR (23·1%). |
| Oncolytic H-1 parvovirus shows safety and signs of immunogenic activity in a first phase I/IIa glioblastoma trial [130] (Geletneky 2017). | Parvovirus | Glioblastoma | 18 | Study used IV and intratumoral injection into cavity created from resection. Study reported: no MTD was reached; T cell infiltration and activation of macrophages and microglia were detected in the infected tumors (Evidence that it is stimulating the immune system) Median survival increased compared to recent meta-analyses. |
| Phase I/II study of oncolytic HSV GM-CSF in combination with radiotherapy and cisplatin in untreated stage III/IV squamous cell cancer of the head and neck [131] (Harrington 2010). | HSV GM-CSF | Stage III/IV squamous cell cancer of head and neck | 17 | Study used intratumoral injection every 21 days with radiation and cisplatin; neck dissection 6–10 weeks later. Study reported a median follow up of 29 months with 76·5% relapse free rate, 100% locoregional control (60–70% in historical controls). |
| Phase I/II study of oncolytic herpes simplex virus NV1020 in patients with extensively pretreated refractory colorectal cancer metastatic to the liver [132] (Geevarghese 2010). | NV1020 (Herpes Virus) | Colorectal liver metastases | I 13 II 19 | Study used hepatic arterial injections with virus then standard chemotherapy in patients with relapse. Study documents 50% SD with a median survival longer than historical controls. |
| Phase I–II trial of ONYX-015 in combination with MAP chemotherapy in patients with advanced sarcomas [133] (Galanis 2005). | Onyx-015 (Adenovirus dl1520) | Advanced sarcomas | 6 | Study used intratumoral injection of the virus in combination with MAP applied to metastases in the liver and chest wall. No significant toxicities identified. Study outcomes include:1 patient with PR that lasted 11 months; tumor had p53 mutation and MDM-2 amplification |
| Phase I/II trial of intravenous NDV-HUJ oncolytic virus in recurrent glioblastoma multiforme [134] (Freeman 2006). | NDV-HUJ (HUJ strain of Newcastle disease virus) | glioblastoma multiforem | 14 | Study used IV injection of virus. Study reported AEs grade I/II constitutional symptoms. 1 person with CR. |
| Trial Name | Virus | Cancer | n | Central Questions and/or Outcomes |
|---|---|---|---|---|
| A Study of Talimogene Laherparepvec in stage IIIc and stage IV malignant melanoma [136] (Andtbacka 2015). | Talimogene Laherparepvec | Stage IIB-IV melanoma | 295 | T-VEC was compared to subcutaneous GM-CSF. Higher DRR at 6 months and greater median OS with T-VEC particularly in untreated advanced melanoma. Lesions that were not directly injected showed response. OS was not improved. |
| Phase IIIb safety results from an expanded-access protocol of talimogene laherparepvec for patients with unresected, stage IIIB-IVM1c melanoma [137] (Chesney 2018). | Talimogene Laherparepvec | Melanoma | 41 | Safety profile was consistent with previous trials. As compared to OPTIM trial above, this trial also included ECOG of 2 (OPTIM was 0, 1 only). Efficacy was not assessed, as the primary outcome was to provide expand access to T-VEC until FDA approval. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cook, M.; Chauhan, A. Clinical Application of Oncolytic Viruses: A Systematic Review. Int. J. Mol. Sci. 2020, 21, 7505. https://doi.org/10.3390/ijms21207505
Cook M, Chauhan A. Clinical Application of Oncolytic Viruses: A Systematic Review. International Journal of Molecular Sciences. 2020; 21(20):7505. https://doi.org/10.3390/ijms21207505
Chicago/Turabian StyleCook, Mary, and Aman Chauhan. 2020. "Clinical Application of Oncolytic Viruses: A Systematic Review" International Journal of Molecular Sciences 21, no. 20: 7505. https://doi.org/10.3390/ijms21207505
APA StyleCook, M., & Chauhan, A. (2020). Clinical Application of Oncolytic Viruses: A Systematic Review. International Journal of Molecular Sciences, 21(20), 7505. https://doi.org/10.3390/ijms21207505




