Detection of Salivary Small Extracellular Vesicles Associated Inflammatory Cytokines Gene Methylation in Gingivitis
Abstract
1. Introduction
2. Results
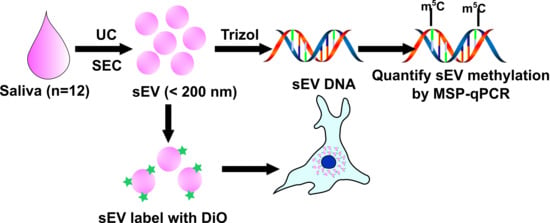
2.1. Periodontal Status of Participants
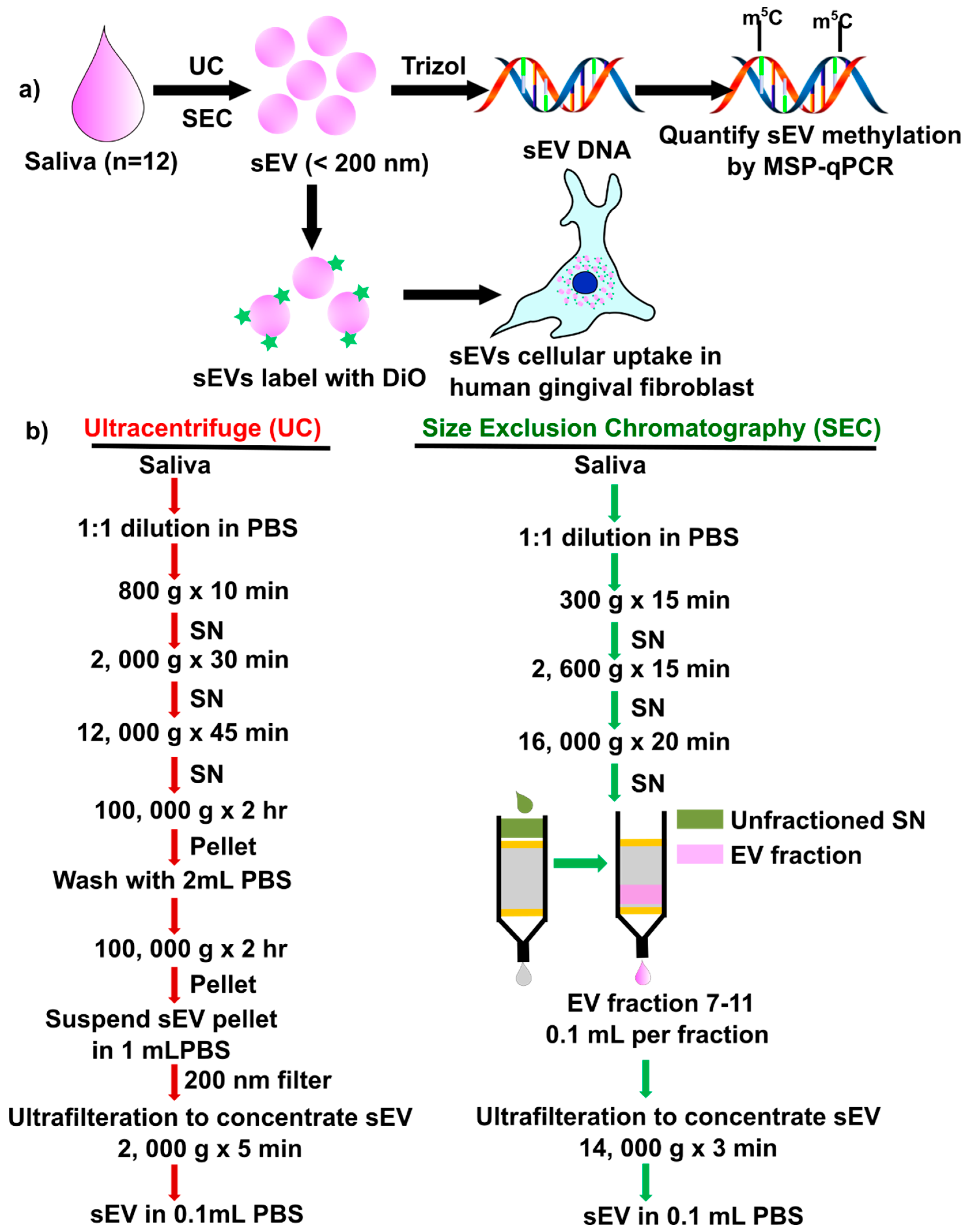
2.2. Particle and Characteristics of Salivary sEV by UC or SEC
2.3. Effect of UC and SEC Isolation Methods on Healthy and Gingivitis-Derived sEV Characteristics
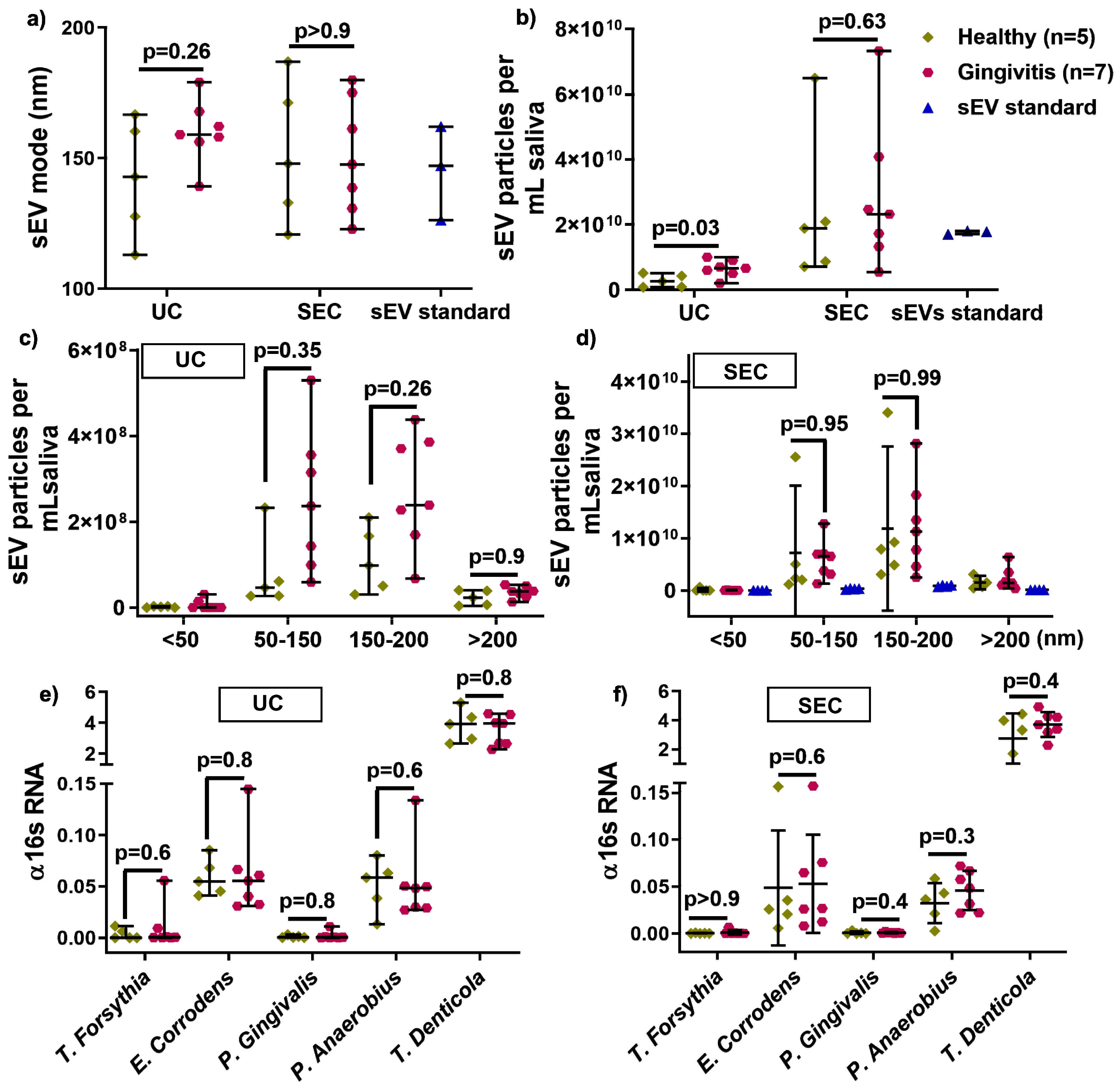
2.4. UC and SEC on sEV Inflammatory Cytokines Genes DNA Methylation
2.5. Comparison of Pooled UC- and SEC-sEV on hGFs DNA Methylation
3. Discussion
3.1. Effect of UC and SEC Isolation Method on Salivary sEV Yield and Bacteria Detection
3.2. Utilizing a Commercial sEV Standard as a Control
3.3. Healthy and Gingivitis-Derived sEV Characteristics—A Pilot Study
3.4. UC and SEC on Five Inflammation Genes DNA Methylation in Salivary sEV
4. Materials and Methods
4.1. Participant Recruitment and Saliva Sample Collection
4.2. Salivary sEV Isolation
4.2.1. Salivary sEV Isolation Using the Differential Ultracentrifugation Method
4.2.2. Salivary sEV Isolation Using SEC Method
4.3. Salivary sEV Characterization
4.3.1. Transmission Electron Microscopy (TEM)
4.3.2. Nanoparticle Tracking Analysis (NTA)
4.3.3. Protein Content and Western Blot
4.4. sEV DNA and RNA Isolation by Trizol Method
4.5. DNA Bisulfite Conversion and Quantitative Methylation-Specific Polymerase Chain Reaction (qMSP)
4.6. Salivary sEV Labelling and Uptake by Human Primary Gingival Fibroblasts
4.6.1. Human Primary Gingival Fibroblasts Cell Culture
4.6.2. sEV Labelling, hGFs Uptake, and Cellular qMSP
4.7. Statistical Analysis
4.8. EV-TRACK
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Edgar, J.R. Q&a: What are exosomes, exactly? BMC. Biol. 2016, 14, 46. [Google Scholar]
- Alharbi, M.Z.F.; Elfeky, O.; Guanzon, D.; Lai, A.; Rice, G.E.; Perrin, L.; Hooper, J.; Salomon, C. The potential role of mirnas and exosomes in chemotherapy in ovarian cancer. Endocrine-Related. Cancer 2018. [Google Scholar] [CrossRef] [PubMed]
- Salomon, C.; Nuzhat, Z.; Dixon, C.L.; Menon, R. Placental exosomes during gestation: Liquid biopsies carrying signals for the regulation of human parturition. Curr. Pharm. Des. 2018, 24, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Zuniga, F.; Rice, G.E.; Perrin, L.C.; Hooper, J.D.; Salomon, C. Tumor-derived exosomes in ovarian cancer - liquid biopsies for early detection and real-time monitoring of cancer progression. Oncotarget 2017, 8, 104687–104703. [Google Scholar] [CrossRef] [PubMed]
- Sarker, S.; Scholz-Romero, K.; Perez, A.; Illanes, S.E.; Mitchell, M.D.; Rice, G.E.; Salomon, C. Placenta-derived exosomes continuously increase in maternal circulation over the first trimester of pregnancy. J. Transl. Med. 2014, 12, 204. [Google Scholar] [CrossRef]
- Zlotogorski-Hurvitz, A.; Dayan, D.; Chaushu, G.; Salo, T.; Vered, M. Morphological and molecular features of oral fluid-derived exosomes: Oral cancer patients versus healthy individuals. J. Cancer. Res. Clin. Oncol. 2016, 142, 101–110. [Google Scholar] [CrossRef]
- Zheng, X.; Chen, F.; Zhang, Q.; Liu, Y.; You, P.; Sun, S.; Lin, J.; Chen, N. Salivary exosomal psma7: A promising biomarker of inflammatory bowel disease. Protein. Cell. 2017, 8, 686–695. [Google Scholar] [CrossRef]
- Sun, Y.; Xia, Z.; Shang, Z.; Sun, K.; Niu, X.; Qian, L.; Fan, L.Y.; Cao, C.X.; Xiao, H. Facile preparation of salivary extracellular vesicles for cancer proteomics. Sci. Rep. 2016, 6, 24669. [Google Scholar] [CrossRef]
- Amado, F.M.; Vitorino, R.M.; Domingues, P.M.; Lobo, M.J.; Duarte, J.A. Analysis of the human saliva proteome. Expert. Rev. Proteomics 2005, 2, 521–539. [Google Scholar] [CrossRef]
- Tobon-Arroyave, S.I.; Celis-Mejia, N.; Cordoba-Hidalgo, M.P.; Isaza-Guzman, D.M. Decreased salivary concentration of cd9 and cd81 exosome-related tetraspanins may be associated with the periodontal clinical status. J. Clin. Periodontol. 2019, 46, 470–480. [Google Scholar] [CrossRef]
- Boing, A.N.; van der Pol, E.; Grootemaat, A.E.; Coumans, F.A.; Sturk, A.; Nieuwland, R. Single-step isolation of extracellular vesicles by size-exclusion chromatography. J. Extracell. Vesicles 2014, 3. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Bartold, P.M.; Salomon, C.; Ivanovski, S. Salivary small extracellular vesicles associated mirnas in periodontal status-a pilot study. Int. J. Mol. Sci. 2020, 21. [Google Scholar] [CrossRef] [PubMed]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Syndergaard, B.; Al-Sabbagh, M.; Kryscio, R.J.; Xi, J.; Ding, X.; Ebersole, J.L.; Miller, C.S. Salivary biomarkers associated with gingivitis and response to therapy. J. Periodontol. 2014, 85, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.G. Epigenetic regulation of gene expression in the inflammatory response and relevance to common diseases. J. Periodontol. 2008, 79, 1514–1519. [Google Scholar] [CrossRef]
- Meng, H.X.; Hackett, J.A.; Nestor, C.; Dunican, D.S.; Madej, M.; Reddington, J.P.; Pennings, S.; Harrison, D.J.; Meehan, R.R. Apoptosis and DNA methylation. Cancers 2011, 3, 1798–1820. [Google Scholar] [CrossRef]
- Han, P.; Ivanovski, S. Effect of saliva collection methods on the detection of periodontium-related genetic and epigenetic biomarkers-a pilot study. Int. J. Mol. Sci. 2019, 20. [Google Scholar] [CrossRef]
- Kurushima, Y.; Tsai, P.C.; Castillo-Fernandez, J.; Couto Alves, A.; El-Sayed Moustafa, J.S.; Le Roy, C.; Spector, T.D.; Ide, M.; Hughes, F.J.; Small, K.S.; et al. Epigenetic findings in periodontitis in uk twins: A cross-sectional study. Clin. Epigenetics 2019, 11, 27. [Google Scholar] [CrossRef]
- Ivanovski, S.; Li, H.; Haase, H.R.; Bartold, P.M. Expression of bone associated macromolecules by gingival and periodontal ligament fibroblasts. J. Periodontal. Res. 2001, 36, 131–141. [Google Scholar] [CrossRef]
- Zlotogorski-Hurvitz, A.; Dayan, D.; Chaushu, G.; Korvala, J.; Salo, T.; Sormunen, R.; Vered, M. Human saliva-derived exosomes: Comparing methods of isolation. J. Histochem. Cytochem. 2015, 63, 181–189. [Google Scholar] [CrossRef]
- Chapple, I.L.C.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J. Clin. Periodontol. 2018, 89, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Thery, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (misev2018): A position statement of the international society for extracellular vesicles and update of the misev2014 guidelines. J. Extracell. Vesicles 2018, 7, 1535750. [Google Scholar] [CrossRef] [PubMed]
- Takov, K.; Yellon, D.M.; Davidson, S.M. Comparison of small extracellular vesicles isolated from plasma by ultracentrifugation or size-exclusion chromatography: Yield, purity and functional potential. J. Extracell. Vesicles 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Oeyen, E.; Van Mol, K.; Baggerman, G.; Willems, H.; Boonen, K.; Rolfo, C.; Pauwels, P.; Jacobs, A.; Schildermans, K.; Cho, W.C.; et al. Ultrafiltration and size exclusion chromatography combined with asymmetrical-flow field-flow fractionation for the isolation and characterisation of extracellular vesicles from urine. J. Extracell. Vesicles 2018, 7. [Google Scholar] [CrossRef]
- Lobb, R.J.; Becker, M.; Wen, S.W.; Wong, C.S.; Wiegmans, A.P.; Leimgruber, A.; Möller, A. Optimized exosome isolation protocol for cell culture supernatant and human plasma. J. Extracell. Vesicles 2015, 4, 27031. [Google Scholar] [CrossRef]
- Webber, J.; Clayton, A. How pure are your vesicles? J. Extracell. Vesicles 2013, 2, 19861. [Google Scholar] [CrossRef]
- Han, P.; Ivanovski, S. Saliva-friend and foe in the covid-19 outbreak. Diagnostics 2020, 10. [Google Scholar] [CrossRef]
- Cecil, J.D.; Sirisaengtaksin, N.; O’Brien-Simpson, N.M.; Krachler, A.M. Outer membrane vesicle-host cell interactions. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef]
- Scannapieco, F.A. Periodontal inflammation: From gingivitis to systemic disease? Compend. Contin. Educ. Dent. 2004, 25, 16–25. [Google Scholar]
- Kim, J.; Amar, S. Periodontal disease and systemic conditions: A bidirectional relationship. Odontology 2006, 94, 10–21. [Google Scholar] [CrossRef]
- Moore, L.D.; Le, T.; Fan, G. DNA methylation and its basic function. Neuropsychopharmacology 2013, 38, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Gardiner-Garden, M.; Frommer, M. Cpg islands in vertebrate genomes. J. Mol. Biol. 1987, 196, 261–282. [Google Scholar] [CrossRef]
- Grover, V.; Kapoor, A.; Malhotra, R.; Gupta, M.; Kaur, G. Epigenetics and inflammation: Exploring the link for chronic human diseases including periodontal disease. J. Adv. Oral. Res. 2015, 6, 16–23. [Google Scholar] [CrossRef]
- Benakanakere, M.R.; Finoti, L.; Palioto, D.B.; Teixeira, H.S.; Kinane, D.F. Epigenetics, inflammation, and periodontal disease. Current. Oral. Health. Rep. 2019, 6, 37–46. [Google Scholar] [CrossRef]
- Lim, Y.; Totsika, M.; Morrison, M.; Punyadeera, C. The saliva microbiome profiles are minimally affected by collection method or DNA extraction protocols. Sci. Rep. 2017, 7, 8523. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Scholz-Romero, K.; Rice, G.E.; Salomon, C. Methods to Enrich Exosomes from Conditioned Media and Biological Fluids; Humana Press: New York, NY, USA, 2018; pp. 103–115. [Google Scholar]
- Thery, C.; Amigorena, S.; Raposo, G.; Clayton, A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr. Protoc. Cell. Biol. 2006, 30, 3–22. [Google Scholar] [CrossRef] [PubMed]
- Truong, G.; Guanzon, D.; Kinhal, V.; Elfeky, O.; Lai, A.; Longo, S.; Nuzhat, Z.; Palma, C.; Scholz-Romero, K.; Menon, R.; et al. Oxygen tension regulates the mirna profile and bioactivity of exosomes released from extravillous trophoblast cells - liquid biopsies for monitoring complications of pregnancy. PLoS ONE 2017, 12, 0174514. [Google Scholar] [CrossRef]
- Han, P.P.; Wu, C.T.; Xiao, Y. The effect of silicate ions on proliferation, osteogenic differentiation and cell signalling pathways (wnt and shh) of bone marrow stromal cells. Biomater. Sci. UK 2013, 1, 379–392. [Google Scholar] [CrossRef]
- Han, P.; Ivanovski, S.; Crawford, R.; Xiao, Y. Activation of the canonical wnt signaling pathway induces cementum regeneration. J. Bone. Miner. Res. 2015, 30, 1160–1174. [Google Scholar] [CrossRef]
- Han, P.P.; Wu, C.T.; Chang, J.; Xiao, Y. The cementogenic differentiation of periodontal ligament cells via the activation of wnt/beta-catenin signalling pathway by li+ ions released from bioactive scaffolds. Biomaterials 2012, 33, 6370–6379. [Google Scholar] [CrossRef]
- Zhang, X.; Han, P.; Jaiprakash, A.; Wu, C.; Xiao, Y. A stimulatory effect of ca(3)zrsi(2)o(9) bioceramics on cementogenic/osteogenic differentiation of periodontal ligament cells. J. Mater. Chem. B 2014, 2, 1415–1423. [Google Scholar] [CrossRef]
- Han, S.; Chen, Z.; Han, P.; Hu, Q.; Xiao, Y. Activation of macrophages by lipopolysaccharide for assessing the immunomodulatory property of biomaterials. Tissue. Eng. Part A 2017, 23, 1100–1109. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Lloyd, T.; Chen, Z.; Xiao, Y. Proinflammatory cytokines regulate cementogenic differentiation of periodontal ligament cells by wnt/ca(2+) signaling pathway. J. Interferon. Cytokine. Res. 2016, 36, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Li, L.C.; Dahiya, R. Methprimer: Designing primers for methylation pcrs. Bioinformatics 2002, 18, 1427–1431. [Google Scholar] [CrossRef] [PubMed]
- Horibe, S.; Tanahashi, T.; Kawauchi, S.; Murakami, Y.; Rikitake, Y. Mechanism of recipient cell-dependent differences in exosome uptake. BMC Cancer 2018, 18, 47. [Google Scholar] [CrossRef] [PubMed]
- Banizs, A.B.; Huang, T.; Dryden, K.; Berr, S.S.; Stone, J.R.; Nakamoto, R.K.; Shi, W.B.; He, J. In vitro evaluation of endothelial exosomes as carriers for small interfering ribonucleic acid delivery. Int. J. Nanomed. 2014, 9, 4223–4230. [Google Scholar]
- Consortium, E.-T.; Van Deun, J.; Mestdagh, P.; Agostinis, P.; Akay, O.; Anand, S.; Anckaert, J.; Martinez, Z.A.; Baetens, T.; Beghein, E.; et al. Ev-track: Transparent reporting and centralizing knowledge in extracellular vesicle research. Nat. Methods 2017, 14, 228–232. [Google Scholar]


| Gender | Age | PPD | BOP | Race |
|---|---|---|---|---|
| F | 33 | <4 mm | 27% | Asian |
| M | 28 | <4 mm | 41% | Asian |
| M | 39 | <4 mm | 14% | Other |
| F | 24 | <4 mm | 39% | Caucasian |
| M | 40 | <4 mm | 39% | Asian |
| F | 26 | <4 mm | 26% | Caucasian |
| F | 38 | <4 mm | 10% | Asian |
| M | 24 | <4 mm | 6% | Caucasian |
| M | 34 | <4 mm | 49% | Caucasian |
| M | 36 | <4 mm | 14% | Asian |
| M | 34 | <4 mm | 70% | Caucasian |
| M | 48 | <4 mm | 14% | Caucasian |
| UC-sEV | SEC-sEV | |
|---|---|---|
| sEV particles/mL saliva | 5.07 × 109 ± 2.9 × 109 | 2.7 × 1010 ± 2.2 × 1010 |
| sEV particles/mL saliva: <50 nm | 2.8 × 105 ± 5.7 × 105 | 1.1 × 105 ± 2.8 × 105 |
| sEV particles/mL saliva: 50–150 nm | 1.1 × 107 ± 9.9 × 106 | 6.6 × 108 ± 6.9 × 108 |
| sEV particles/mL saliva: 150–200 nm | 1.2 × 107± 8.3 × 106 | 1.3 × 109 ± 9.9 × 108 |
| sEV particles/mL saliva: >200 nm | 1.9 × 106 ± 1.1 × 106 | 1.9 × 108 ± 1.6 × 108 |
| sEV particles per μg protein | 1.6 × 107 ± 9.4 × 107 | 2.6 × 108 ± 1.5 × 108 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, P.; Lai, A.; Salomon, C.; Ivanovski, S. Detection of Salivary Small Extracellular Vesicles Associated Inflammatory Cytokines Gene Methylation in Gingivitis. Int. J. Mol. Sci. 2020, 21, 5273. https://doi.org/10.3390/ijms21155273
Han P, Lai A, Salomon C, Ivanovski S. Detection of Salivary Small Extracellular Vesicles Associated Inflammatory Cytokines Gene Methylation in Gingivitis. International Journal of Molecular Sciences. 2020; 21(15):5273. https://doi.org/10.3390/ijms21155273
Chicago/Turabian StyleHan, Pingping, Andrew Lai, Carlos Salomon, and Sašo Ivanovski. 2020. "Detection of Salivary Small Extracellular Vesicles Associated Inflammatory Cytokines Gene Methylation in Gingivitis" International Journal of Molecular Sciences 21, no. 15: 5273. https://doi.org/10.3390/ijms21155273
APA StyleHan, P., Lai, A., Salomon, C., & Ivanovski, S. (2020). Detection of Salivary Small Extracellular Vesicles Associated Inflammatory Cytokines Gene Methylation in Gingivitis. International Journal of Molecular Sciences, 21(15), 5273. https://doi.org/10.3390/ijms21155273