Evaluation of Prognostic Factors of Severity in Acute Biliary Pancreatitis
Abstract
1. Introduction
2. Results
2.1. Demographic, Clinical and Biochemical Characteristics of Patients
2.2. Laboratory Parameters and Score Systems on Admission
2.3. Laboratory Parameters and Score Systems at 48 h after Symptom Onset
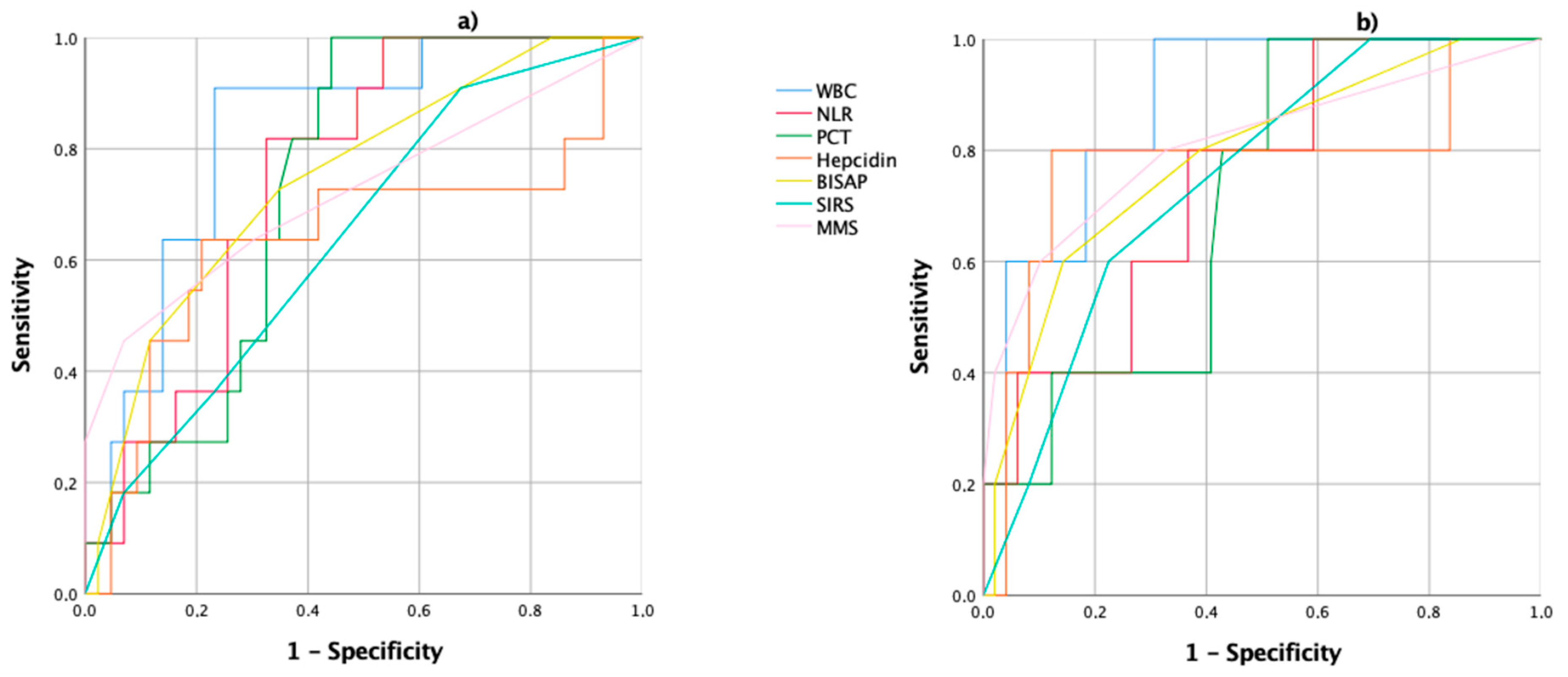
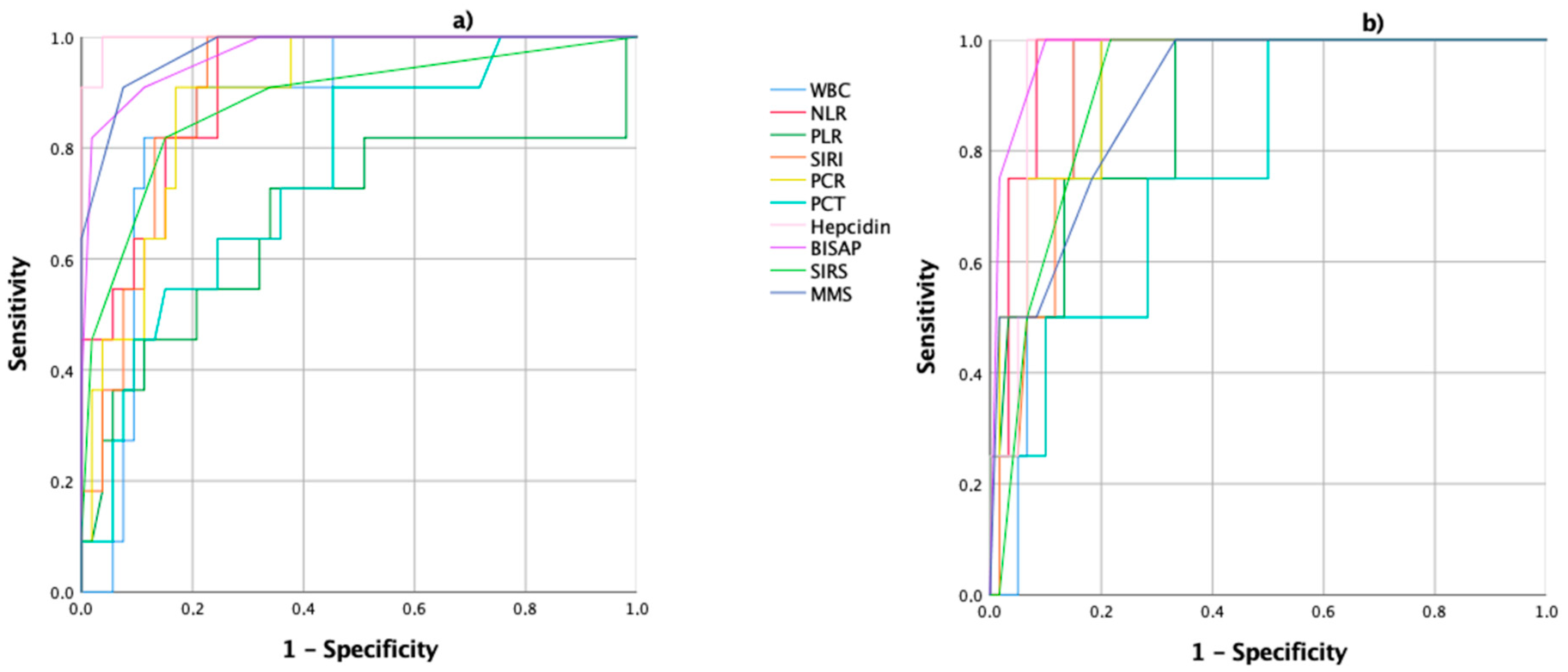
2.4. Prognostic Accuracy of Laboratory and Score Systems
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. Inclusion and Exclusion Criteria
4.3. Analysis of Biomarkers
4.4. Score Systems Determination
4.5. Statistical Methods
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AP | Acute pancreatitis |
| APACHE | Acute physiology and chronic health evaluation |
| AUC | Area under the curve |
| BISAP | Bedside index of severity in acute pancreatitis |
| BMI | Body mass index |
| CECT | Contrast-enhanced computed tomography |
| CI | Confidence interval |
| CRP | C-reactive protein |
| HAMP | Hepcidin antimicrobial peptide |
| IL | Interleukin |
| L | Lymphocyte |
| LEAP | Liver-expressed antimicrobial peptide |
| M | Monocyte |
| MMS | Modified Marshall score |
| MRI | Magnetic resonance imaging |
| N | Neutrophil |
| NLR | Neutrophil–lymphocyte ratio |
| NPV | Negative predictive value |
| NS | Not significant |
| PCT | Procalcitonin |
| PEP | Post-endoscopic retrograde cholangiopancreatography pancreatitis |
| PLR | Platelet–lymphocyte ratio |
| PPV | Positive predictive value |
| QT | Chemotherapy |
| RAC | Revised Atlanta classification |
| ROC | Received operating characteristics |
| SD | Standard deviation |
| Se | Sensibility |
| SIRI | Systemic inflammatory response index |
| SIRS | Systemic inflammatory response syndrome |
| Sp | Specificity |
| STAT | Signal transducer and activator of transcription |
| US | Ultrasound |
| WBC | White blood count |
References
- Ruiz-Rebollo, M.L.; Muñoz-Moreno, M.F.; Mayo-Iscar, A.; Udaondo-Cascante, M.A.; Nistal, R.B. Statin intake can decrease acute pancreatitis severit. Pancreatology 2019, 19, 807–812. [Google Scholar] [CrossRef]
- Roberts, S.E.; Morrison-Rees, S.; John, A.; Williams, J.G.; Brown, T.H.; Samuel, D.G. The incidence and aetiology of acute pancreatitis across Europe. Pancreatology 2017, 17, 155–165. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, S.M.; Hallensleben, N.D.; van Santvoort, H.C.; Fockens, P.; van Goor, H.; Bruno, M.J.; Besselink, M.G. Acute pancreatitis: Recent advances through randomised trials. Gut 2017, 66, 2024–2032. [Google Scholar] [CrossRef]
- García-Rayado, G.; Varela-Moreiras, G.; Lanas, Á.; Ferrández, Á.; Balza-Lareu, N.; Cervera, J.I.; Bodenlle-Bello, M.P.; Argüelles-Arias, A.M.; Latorre, P.; Udaondo-Cascante, M.A.; et al. Dietary fat patterns and outcomes in acute pancreatitis in Spain. Front. Med. 2020, 7, 126. [Google Scholar] [CrossRef] [PubMed]
- Párniczky, A.; Kui, B.; Szentesi, A.; Balázs, A.; Szűcs, Á.; Mosztbacher, D.; Czimmer, J.; Sarlós, P.; Bajor, J.; Gódi, S.; et al. Prospective, multicentre, nationwide clinical data from 600 cases of acute pancreatitis. PLoS ONE 2016, 11, e0165309. [Google Scholar] [CrossRef] [PubMed]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S. Classification of acute pancreatitis–2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Silva-Vaz, P.; Abrantes, A.M.; Castelo-Branco, M.; Gouveia, A.; Botelho, M.F.; Tralhao, J.G. Multifactorial scores and biomarkers of prognosis of acute pancreatitis: Applications to research and practice. Int. J. Mol. Sci. 2020, 21, 338. [Google Scholar] [CrossRef] [PubMed]
- Farkas, N.; Hanák, L.; Mikó, A.; Bajor, J.; Sarlós, P.; Czimmer, J.; Vincze, Á.; Gódi, S.; Pécsi, D.; Varjú, P.; et al. A multicenter, international cohort analysis of 1435 cases to support clinical trial design in acute pancreatitis. Front. Physiol. 2019, 10, 1092. [Google Scholar] [CrossRef]
- Zhang, X.-X.; Deng, L.-H.; Chen, W.-W.; Shi, N.; Jin, T.; Lin, Z.-Q.; Ma, Y.; Jiang, K.; Yang, X.-N.; Xia, Q. Circulating microRNA 216 as a marker for the early identification of severe acute pancreatitis. Am. J. Med. Sci. 2017, 353, 178–186. [Google Scholar] [CrossRef]
- Khanna, A.K.; Meher, S.; Prakash, S.; Tiwary, S.K.; Singh, U.; Srivastava, A.; Dixit, V. Comparison of Ranson, Glasgow, MOSS, SIRS, BISAP, APACHE-II, CTSI Scores, IL-6, CRP, and procalcitonin in predicting severity, organ failure, pancreatic necrosis, and mortality in acute pancreatitis. HPB Surg. 2013, 2013, 367581. [Google Scholar] [CrossRef]
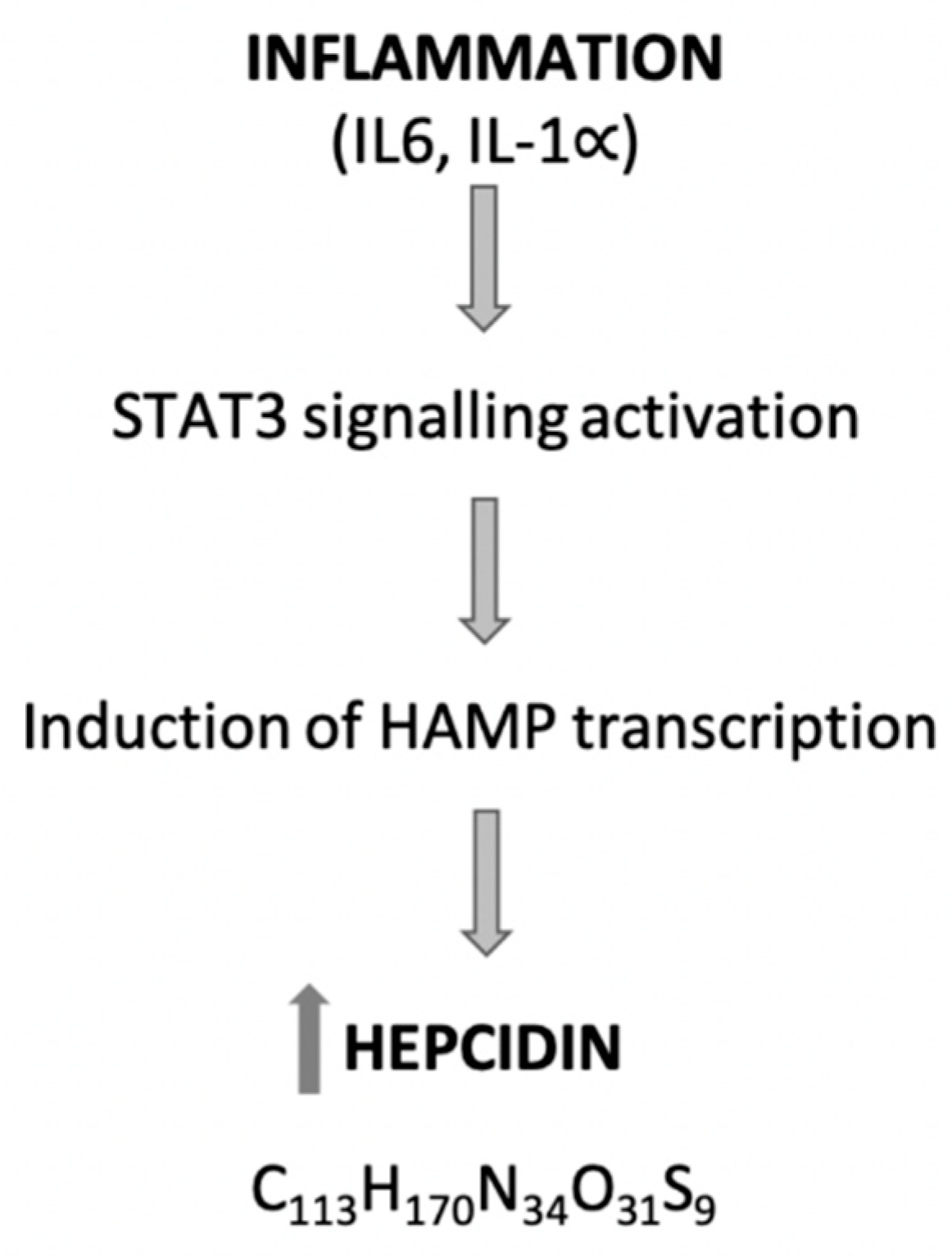
- Wrighting, D.M.; Andrews, N.C. Interleukin-6 induces hepcidin expression through STAT3. Blood 2006, 108, 3204–3209. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, G.; Chauvet, C.; Viatte, L.; Danan, J.L.; Bigard, X.; Devaux, I.; Beaumont, C.; Kahn, A.; Vaulont, S. The gene encoding the iron regulatory peptide hepcidin is regulated by anemia, hypoxia, and inflammation. J. Clin. Investig. 2002, 110, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Wang, B.M.; Cai, S.; Liu, P.L. The role of serum high mobility group box 1 and interleukin-6 levels in acute pancreatitis: A meta-analysis. J. Cell. Biochem. 2018, 119, 616–624. [Google Scholar] [CrossRef]
- Dudkowiak, R.; Neubauer, K.; Poniewierka, E. Hepcidin and its role in inflammatory bowel disease. Adv. Clin. Exp. Med. 2013, 22, 585–591. [Google Scholar]
- Kulaksiz, H.; Fein, E.; Redecker, P.; Stremmel, W.; Adler, G.; Cetin, Y. Pancreatic b-cells express hepcidin, an iron-uptake regulatory peptide. J. Endocrinol. 2008, 197, 241–250. [Google Scholar] [CrossRef]
- Arabul, M.; Celik, M.; Aslan, O.; Torun, S.; Beyazit, Y.; Alper, E.; Kandemir, A.; Unsal, B. Hepcidin as a predictor of disease severity in acute pancreatitis: A single center prospective study. Hepatogastroenterology 2013, 60, 595–600. [Google Scholar] [CrossRef]
- Azab, B.; Jaglall, N.; Atallah, J.P.; Lamet, A.; Raja-Surya, V.; Farah, B.; Lesser, M.; Widmann, W.D. Neutrophil-lymphocyte ratio as a predictor of adverse outcomes of acute pancreatitis. Pancreatology 2011, 11, 445–452. [Google Scholar] [CrossRef]
- Djordjevic, D.; Rondovic, G.; Surbatovic, M.; Stanojevic, I.; Udovicic, I.; Andjelic, T.; Zeba, S.; Milosavljevic, S.; Stankovic, N.; Abazovic, D.; et al. Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically ill and injured patients: Which ratio to choose to predict outcome and nature of bacteremia? Mediators Inflamm. 2018, 2018, 3758068. [Google Scholar] [CrossRef]
- Qi, Q.; Zhuang, L.; Shen, Y.; Geng, Y.; Yu, S.; Chen, H.; Liu, L.; Meng, Z.; Wang, P.; Chen, Z. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer 2016, 122, 2158–2167. [Google Scholar] [CrossRef] [PubMed]
- Kamposioras, K.; Razzaq, M.; Ahmad, U.; Damyanova, I.; Papaxoinis, G. Systemic inflammatory response index (SIRI) predicts poor survival in pancreatic cancer patients treated with FOLFIRINOX. Ann. Oncol. 2019, 30 (Suppl. 4), iv45. [Google Scholar] [CrossRef]
- Silva-Vaz, P.; Abrantes, A.M.; Castelo-Branco, M.; Gouveia, A.; Botelho, M.F.; Tralhão, J.G. Murine Models of Acute Pancreatitis: A Critical Appraisal of Clinical Relevance. Int. J. Mol. Sci. 2019, 20, 2794. [Google Scholar] [CrossRef] [PubMed]
- Windsor, J.A. Search for prognostic markers for acute pancreatitis. Lancet 2000, 355, 1924–1925. [Google Scholar] [CrossRef]
- Kamal, A.; Akshintala, V.S.; Kamal, M.M.; El Zein, M.; Besharati, S.; Kumbhari, V.; Ngamruengphong, S.; Shin, E.J.; Singh, V.K.; Kalloo, A.N.; et al. Does etiology of pancreatitis matter? Differences in outcomes among patients with post-endoscopic retrograde cholangiopancreatography, acute biliary, and alcoholic pancreatitis. Pancreas 2019, 48, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Mosztbacher, D.; Hanák, L.; Farkas, N.; Szentesi, A.; Mikó, A.; Bajor, J.; Sarlós, P.; Czimmer, J.; Vincze, R.; Hegyi, P.J.; et al. Hypertriglyceridemia-induced acute pancreatitis: A prospective, multicenter, international cohort analysis of 716 acute pancreatitis cases. Pancreatology 2020, 20, 608–616. [Google Scholar] [CrossRef]
- Zhao, X.; Chen, D.Z.; Lang, R.; Jin, Z.K.; Fan, H.; Wu, T.M.; Li, X.L.; He, Q. Enhanced recovery in the management of mild gallstone pancreatitis: A prospective cohort study. Surg. Today 2013, 43, 643–647. [Google Scholar] [CrossRef]
- Gungor, B.; Caglayan, K.; Polat, C.; Seren, D.; Erzurumlu, K.; Malazgirt, Z. The predictivity of serum biochemical markers in acute biliary pancreatitis. ISRN Gastroenterol. 2011, 2011, 279607. [Google Scholar] [CrossRef]
- Kolber, W.; Kuśnierz-Cabala, B.; Dumnicka, P.; Maraj, M.; Mazur-Laskowska, M.; Pędziwiatr, M.; Ceranowicz, P. Serum Urokinase-type plasminogen activator receptor does not outperform c-reactive protein and procalcitonin as an early marker of severity of acute pancreatitis. J. Clin. Med. 2018, 7, 305. [Google Scholar] [CrossRef]
- Wu, B.U.; Batech, M.; Quezada, M.; Lew, D.; Fujikawa, K.; Kung, J.; Jamil, L.H.; Chen, W.; Afghani, E.; Reicher, S.; et al. Dynamic measurement of disease activity in acute pancreatitis: The pancreatitis activity scoring system. Am. J. Gastroenterol. 2017, 112, 1144–1152. [Google Scholar] [CrossRef]
- Mikó, A.; Vigh, É.; Mátrai, P.; Soós, A.; Garami, A.; Balaskó, M.; Czakó, L.; Mosdósi, B.; Sarlós, P.; Erőss, B.; et al. Computed tomography severity index vs. other indices in the prediction of severity and mortality in acute pancreatitis: A predictive accuracy meta-analysis. Front. Physiol. 2019, 10, 1002. [Google Scholar] [CrossRef]
- Garrey, W.; Bryan, W.R. Variations in white blood cell counts. Physiol. Rev. 1935, 15, 597–638. [Google Scholar] [CrossRef]
- Unal, Y.; Barlas, A.M. Role of increased immature granulocyte percentage in the early prediction of acute necrotizing pancreatitis. Ulus. Travma Acil. Cerrahi. Derg. 2019, 25, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Mayer, A.; McMahon, M.; Bowen, M.; Cooper, E. C reactive protein: An aid to assessment and monitoring of acute pancreatitis. J. Clin. Pathol. 1984, 37, 207–211. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhou, H.; Mei, X.; He, X.; Lan, T.; Guo, S. Severity stratification and prognostic prediction of patients with acute pancreatitis at early phase: A retrospective study. Medicine 2019, 98, e15275. [Google Scholar] [CrossRef] [PubMed]
- Suppiah, A.; Malde, D.; Arab, T.; Hamed, M.; Allgar, V.; Smith, A.M.; Morris-Stiff, G. The prognostic value of the neutrophil-lymphocyte ratio (NLR) in acute pancreatitis: Identification of an optimal NLR. J. Gastrointest. Surg. 2013, 17, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Gulen, B.; Sonmez, E.; Yaylaci, S.; Serinken, M.; Eken, C.; Dur, A.; Turkdogan, F.T.; Sogut, O. Effect of harmless acute pancreatitis score, red cell distribution width and neutrophil/lymphocyte ratio on the mortality of patients with nontraumatic acute pancreatitis at the emergency department. World J. Emerg. Med. 2015, 6, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, M.; Ates, I.; Oztas, E.; Yuksel, M.; Akpinar, M.Y.; Coskun, O.; Kayacetin, E. A new marker to determine prognosis of acute pancreatitis: PLR and NLR combination. J. Med. Biochem. 2018, 37, 21–30. [Google Scholar] [CrossRef]
- Tanoglu, A.; Duzenli, T. Neutrophil-to-lymphocyte ratio alone may not be a true indicator of the severity of acute pancreatitis. Turk. J. Gastroenterol. 2019, 30, 937. [Google Scholar] [CrossRef]
- Petrescu, G.S.; Georgescu, I.; Petrescu, A.M.; Radulescu, D.; Petrescu, M.O.; Patrascu, S. Balthazar score and neutrophil-lymphocytes ratio in acute pancreatitis. Curr. Health Sci. J. 2019, 45, 316–320. [Google Scholar] [CrossRef]
- Park, H.S.; In, S.G.; Yoon, H.J.; Lee, W.J.; Woo, S.H.; Kim, D. Predictive values of neutrophil-lymphocyte ratio as an early indicator for severe acute pancreatitis in the emergency department patients. J. Lab. Physicians 2019, 11, 259–264. [Google Scholar] [CrossRef]
- Gu, L.; Ma, X.; Wang, L.; Li, H.; Chen, L.; Li, X.; Zhang, Y.; Xie, Y.; Zhang, X. Prognostic value of a systemic inflammatory response index in metastatic renal cell carcinoma and construction of a predictive model. Oncotarget 2017, 8, 52094–52103. [Google Scholar] [CrossRef]
- Pacheco-Barcia, V.; Mondejar Solis, R.; France, T.; Asselah, J.; Donnay, O.; Zogopoulos, G.; Bouganim, N.; Guo, K.; Rogado, J.; Martin, E.; et al. A systemic inflammation response index (SIRI) correlates with survival and predicts oncological outcome for mFOLFIRINOX therapy in metastatic pancreatic cancer. Pancreatology 2019, 20, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Kong, X.; Wang, Z.; Wang, X.; Fang, Y.; Wang, J. Pretreatment systemic inflammation response index in patients with breast cancer treated with neoadjuvant chemotherapy as a useful prognostic indicator. Cancer Manag. Res. 2020, 12, 1543–1567. [Google Scholar] [CrossRef] [PubMed]
- Miglani, R.K.; Bhateja, N.; Bhat, R.S.; Kumar, K.V. Diagnostic role of platelet lymphocyte ratio(PLR) in pancreatic head masses. Indian J. Surg. 2013, 75, 4–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cho, S.K.; Jung, S.; Lee, K.J.; Kim, J.W. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio can predict the severity of gallstone pancreatitis. BMC Gastroenterol. 2018, 18, 18. [Google Scholar] [CrossRef]
- Ilhan, M.; Ilhan, G.; Gok, A.F.; Bademler, S.; Verit Atmaca, F.; Ertekin, C. Evaluation of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and red blood cell distribution width-platelet ratio as early predictor of acute pancreatitis in pregnancy. J. Matern. Fetal Neonatal Med. 2016, 29, 1476–1480. [Google Scholar] [CrossRef]
- Rau, B.; Steinbach, G.; Gansauge, F.; Mayer, J.M.; Grunert, A.; Beger, H.G. The potential role of procalcitonin and interleukin 8 in the prediction of infected necrosis in acute pancreatitis. Gut 1997, 41, 832–840. [Google Scholar] [CrossRef]
- Kylanpaa-Back, M.L.; Takala, A.; Kemppainen, E.; Puolakkainen, P.; Haapiainen, R.; Repo, H. Procalcitonin strip test in the early detection of severe acute pancreatitis. Br. J. Surg. 2001, 88, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Brunkhorst, F.M.; Eberhard, O.K.; Brunkhorst, R. Early identification of biliary pancreatitis with procalcitonin. Am. J. Gastroenterol. 1998, 93, 1191–1192. [Google Scholar] [CrossRef]
- Mofidi, R.; Suttie, S.A.; Patil, P.V.; Ogston, S.; Parks, R.W. The value of procalcitonin at predicting the severity of acute pancreatitis and development of infected pancreatic necrosis: Systematic review. Surgery 2009, 146, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.S.; Ricardo, L.B.; Oliveira, A.M.; Canena, J.M.; Horta, D.V.; Papoila, A.L.; Deus, J.R. C-reactive protein prognostic accuracy in acute pancreatitis: Timing of measurement and cutoff points. Eur. J. Gastroenterol. Hepatol. 2013, 25, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Stirling, A.D.; Moran, N.R.; Kelly, M.E.; Ridgway, P.F.; Conlon, K.C. The predictive value of C-reactive protein (CRP) in acute pancreatitis–is interval change in CRP an additional indicator of severity? HPB 2017, 19, 874–880. [Google Scholar] [CrossRef]
- Rau, B.; Steinbach, G.; Baumgart, K.; Gansauge, F.; Grunert, A.; Beger, H.G. Serum amyloid A versus C-reactive protein in acute pancreatitis: Clinical value of an alternative acute-phase reactant. Crit. Care Med. 2000, 28, 736–742. [Google Scholar] [CrossRef]
- Krause, A.; Neitz, S.; Mägert, H.-J.; Schulz, A.; Forssmann, W.-G.; Schulz-Knappe, P.; Adermann, K. LEAP-1, a novel highly disulfide-bonded human peptide, exhibits antimicrobial activity. FEBS Lett. 2000, 480, 147–150. [Google Scholar] [CrossRef]
- Park, C.H.; Valore, E.V.; Waring, A.J.; Ganz, T. Hepcidin, a urinary antimicrobial peptide synthesized in the liver. J. Biol. Chem. 2001, 276, 7806–7810. [Google Scholar] [CrossRef] [PubMed]
- Kali, A.; Charles, M.V.P.; Seetharam, R.S.K. Hepcidin-A novel biomarker with changing trends. Pharmacogn. Rev. 2015, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.; Sangwaiya, A.; Manglam, V.; Geoghegan, F.; Thursz, M.; Busbridge, M. Presence of hepcidin-25 in biological fluids: Bile, ascitic and pleural fluids. World J. Gastroenterol. 2010, 16, 2129. [Google Scholar] [CrossRef]
- Babitt, J.L.; Huang, F.W.; Wrighting, D.M.; Xia, Y.; Sidis, Y.; Samad, T.A.; Campagna, J.A.; Chung, R.T.; Schneyer, A.L.; Woolf, C.J. Bone morphogenetic protein signaling by hemojuvelin regulates hepcidin expression. Nat. Genet. 2006, 38, 531. [Google Scholar] [CrossRef]
- Wang, R.-H.; Li, C.; Xu, X.; Zheng, Y.; Xiao, C.; Zerfas, P.; Cooperman, S.; Eckhaus, M.; Rouault, T.; Mishra, L. A role of SMAD4 in iron metabolism through the positive regulation of hepcidin expression. Cell Metab. 2005, 2, 399–409. [Google Scholar] [CrossRef]
- Wu, B.U.; Johannes, R.S.; Sun, X.; Tabak, Y.; Conwell, D.L.; Banks, P.A. The early prediction of mortality in acute pancreatitis: A large population-based study. Gut 2008, 57, 1698–1703. [Google Scholar] [CrossRef]
- Yang, Y.X.; Li, L. Evaluating the Ability of the Bedside Index for Severity of Acute Pancreatitis Score to Predict Severe Acute Pancreatitis: A Meta-Analysis. Med. Princ. Pract. 2016, 25, 137–142. [Google Scholar] [CrossRef]
- Hagjer, S.; Kumar, N. Evaluation of the BISAP scoring system in prognostication of acute pancreatitis—A prospective observational study. Int. J. Surg. 2018, 54, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.K.; Wu, B.U.; Bollen, T.L.; Repas, K.; Maurer, R.; Johannes, R.S.; Mortele, K.J.; Conwell, D.L.; Banks, P.A. A prospective evaluation of the bedside index for severity in acute pancreatitis score in assessing mortality and intermediate markers of severity in acute pancreatitis. Am. J. Gastroenterol. 2009, 104, 966. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Midha, S.; Mahapatra, S.J.; Gupta, S.; Sharma, M.K.; Nayak, B.; Jacob, T.G.; Shalimar; Garg, P.K. Interleukin-6 significantly improves predictive value of systemic inflammatory response syndrome for predicting severe acute pancreatitis. Pancreatology 2018. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total (n = 75) | Mild AP (n = 47) | Moderately Severe AP (n = 15) | Severe AP (n = 13) | p |
|---|---|---|---|---|---|
| Age (years) | 72 ± 17.4 | 70 ± 18.7 | 73 ± 14.1 | 74 ± 17.1 | NS |
| Female sex | 57.3% | 55.3% | 66.7% | 53.8% | NS |
| BMI ≥ 30 kg/m2 | 18.6% | 19.1% | 20.0% | 15.4% | NS |
| Charlson Index | 3 (2–4) | 3 (1–4) | 3 (2–4) | 3 (2–4) | NS |
| Hospital stay (days) | 8 (6–12) | 7 (6–9) | 11 (7–15) | 18 (11–24) | <0.001 |
| Mortality | 5 (6.7%) | 0 | 0 | 5 (38.4%) | NA |
| Admission | |||||
| WBC (103/µL) | 13.99 ± 4.89 | 13.03 ± 4.46 | 12.53 ± 4.76 | 18.29 ± 4.08 | 0.001 |
| Neutrophil (103/µL) | 11.88 ± 4.74 | 10.71 ± 4.38 | 10.79 ± 4.39 | 16.37 ± 3.55 | <0.001 |
| Lymphocyte (103/µL) | 1.31 ± 0.91 | 1.49 ± 1.07 | 1.04 ± 0.51 | 1.01 ± 0.52 | NS |
| NLR | 13.15 ± 8.50 | 11.42 ± 8.72 | 12.36 ± 6.19 | 18.94 ± 7.86 | 0.003 |
| PLR | 229.11 ± 141.3 | 215.60 ± 142.5 | 232.90 ± 122.9 | 313.73 ± 140.9 | NS |
| SIRI | 8.75 ± 8.78 | 8.84 ± 10.42 | 6.98 ± 6.30 | 10.24 ± 5.08 | NS |
| CRP (mg/mL) | 59.99 ± 97.66 | 45.12 ± 77.37 | 44.50 ± 63.43 | 118.76 ± 152.31 | NS |
| PCT (ng/mL) | 3.41 ± 6.69 | 2.33 ± 5.58 | 4.18 ± 5.46 | 5.77 ± 10.00 | 0.013 |
| Hepcidin (ng/mL)* | 71.21 ± 78.21 | 52.93 ± 74.43 | 85.83 ± 57.90 | 109.76 ± 94.64 | 0.026 |
| BISAP | 1 (1–2) | 1 (1–2) | 1 (1–3) | 2 (1–3) | <0.01 |
| SIRS | 1 (0–2) | 1 (0–1) | 1 (0–2) | 1 (1–2) | <0.05 |
| MMS | 0 (0–1) | 0 (0–0) | 0 (0–1) | 1 (0–3) | <0.01 |
| 48 h | |||||
| WBC (103/µL) | 10.08 ± 4.84 | 8.60 ± 3.52 | 11.38 ± 6.69 | 15.07 ± 2.71 | 0.001 |
| Neutrophil (103/µL) | 8.02 ± 4.89 | 6.10 ± 3.61 | 9.37 ± 6.08 | 13.41 ± 2.63 | <0.001 |
| Lymphocyte (103/µL) | 1.37 ± 0.58 | 1.39 ± 0.52 | 1.25 ± 0.77 | 0.85 ± 0.36 | 0.002 |
| NLR | 8.26 ± 6.80 | 5.37 ± 4.27 | 8.87 ± 4.87 | 18.06 ± 7.55 | <0.001 |
| PLR | 174.65 ± 98.19 | 158.13 ± 83.9 | 176.43 ± 75.9 | 232.62 ± 146.7 | 0.029 |
| SIRI | 4.69 ± 4.69 | 2.94 ± 2.74 | 5.21 ± 5.39 | 10.44 ± 5.08 | <0.001 |
| CRP (mg/mL) | 161.68 ± 134.48 | 103.9 ± 102.66 | 200.73 ± 117.49 | 325.61 ± 106.58 | <0.001 |
| PCT (ng/mL) | 3.39 ± 5.85 | 2.01 ± 3.99 | 4.27 ± 7.03 | 7.36 ± 8.27 | 0.001 |
| Hepcidin (ng/mL) * | 92.44 ± 102.91 | 44.96 ± 39.62 | 74.42 ± 50.78 | 286.42 ± 81.74 | <0.001 |
| BISAP | 1 (1–3) | 1 (1–2) | 2 (1–3) | 4 (4–5) | <0.001 |
| SIRS | 0 (0–2) | 0 (0–1) | 0 (0–1) | 3 (2–3) | <0.001 |
| MMS | 0 (0–1) | 0 (0–0) | 0 (0–2) | 3 (2–4) | <0.001 |
| Outcome to Predict | Predictor | AUC (95% CI) |
|---|---|---|
| Severe disease | WBC | 0.829 (0.707–0.951) |
| NLR | 0.751 (0.615–0.886) | |
| PCT | 0.735 (0.601–0.869) | |
| Hepcidin | 0.641 (0.423–0.859) | |
| BISAP | 0.747 (0.588–0.907) | |
| SIRS | 0.643 (0.469–0.817) | |
| MMS | 0.723 (0.528–0.918) | |
| Mortality | WBC | 0.886 (0.767–1) |
| NLR | 0.743 (0.538–0.948) | |
| PCT | 0.708 (0.512–0.904) | |
| Hepcidin | 0.776 (0.499–1) | |
| BISAP | 0.786 (0.571–1) | |
| SIRS | 0.747 (0.555–0.939) | |
| MMS | 0.810 (0.572–1) |
| Variable | Se | Sp | PPV | NPV |
|---|---|---|---|---|
| WBC ≥ 14.88 × 103/µL | 91 | 75 | 44 | 98 |
| NLR ≥ 14.64 | 82 | 67 | 36 | 96 |
| PCT ≥ 0.58 ng/mL | 73 | 65 | 29 | 93 |
| Hepcidin ≥ 72.8 ng/mL | 64 | 79 | 47 | 90 |
| BISAP ≥ 3 | 45 | 89 | 46 | 89 |
| SIRS ≥ 2 | 36 | 75 | 24 | 85 |
| MMS ≥ 2 | 45 | 94 | 56 | 88 |
| Outcome to Predict | Predictor | AUC (95% CI) |
|---|---|---|
| Severe disease | WBC | 0.868 (0.771–0.965) |
| NLR | 0.914 (0.841–0.988) | |
| PLR | 0.675 (0.464–0.886) | |
| SIRI | 0.906 (0.833–0.979) | |
| CRP | 0.892 (0.807–0.977) | |
| PCT | 0.757 (0.609–0.906) | |
| Hepcidin | 0.997 (0.987–1) | |
| BISAP | 0.970 (0.826–1) | |
| SIRS | 0.883 (0.758–1) | |
| MMS | 0.975 (0.939–1) | |
| Mortality | WBC | 0.917 (0.843–0.990) |
| NLR | 0.963 (0.914–1) | |
| PLR | 0.877 (0.736–1) | |
| SIRI | 0.915 (0.836–0.993) | |
| CRP | 0.929 (0.839–1) | |
| PCT | 0.779 (0.579–1) | |
| Hepcidin | 0.954 (0.901–1) | |
| BISAP | 0.979 (0.943–1) | |
| SIRS | 0.908 (0.824–0.992) | |
| MMS | 0.898 (0.780–1) |
| Variable | Se | Sp | PPV | NPV |
|---|---|---|---|---|
| WBC ≥ 12.09 × 103/µL | 91 | 80 | 43 | 82 |
| NLR ≥ 10.89 | 82 | 85 | 45 | 93 |
| SIRI ≥ 7.14 | 82 | 87 | 53 | 96 |
| PLR ≥ 187.80 | 73 | 66 | 34 | 93 |
| CRP ≥ 150 mg/mL | 100 | 60 | 34 | 100 |
| PCT ≥ 2.83 ng/mL | 64 | 76 | 38 | 91 |
| Hepcidin ≥ 154.7 ng/mL | 100 | 96 | 86 | 100 |
| BISAP ≥ 3 | 91 | 89 | 55 | 96 |
| SIRS ≥ 2 | 82 | 85 | 48 | 94 |
| MMS ≥ 2 | 91 | 93 | 65 | 97 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva-Vaz, P.; Abrantes, A.M.; Morgado-Nunes, S.; Castelo-Branco, M.; Gouveia, A.; Botelho, M.F.; Tralhão, J.G. Evaluation of Prognostic Factors of Severity in Acute Biliary Pancreatitis. Int. J. Mol. Sci. 2020, 21, 4300. https://doi.org/10.3390/ijms21124300
Silva-Vaz P, Abrantes AM, Morgado-Nunes S, Castelo-Branco M, Gouveia A, Botelho MF, Tralhão JG. Evaluation of Prognostic Factors of Severity in Acute Biliary Pancreatitis. International Journal of Molecular Sciences. 2020; 21(12):4300. https://doi.org/10.3390/ijms21124300
Chicago/Turabian StyleSilva-Vaz, Pedro, Ana Margarida Abrantes, Sara Morgado-Nunes, Miguel Castelo-Branco, António Gouveia, Maria Filomena Botelho, and José Guilherme Tralhão. 2020. "Evaluation of Prognostic Factors of Severity in Acute Biliary Pancreatitis" International Journal of Molecular Sciences 21, no. 12: 4300. https://doi.org/10.3390/ijms21124300
APA StyleSilva-Vaz, P., Abrantes, A. M., Morgado-Nunes, S., Castelo-Branco, M., Gouveia, A., Botelho, M. F., & Tralhão, J. G. (2020). Evaluation of Prognostic Factors of Severity in Acute Biliary Pancreatitis. International Journal of Molecular Sciences, 21(12), 4300. https://doi.org/10.3390/ijms21124300









