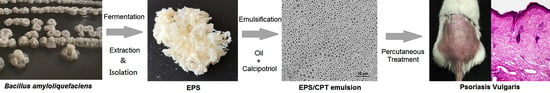
Preparation of Calcipotriol Emulsion Using Bacterial Exopolysaccharides as Emulsifier for Percutaneous Treatment of Psoriasis Vulgaris
Abstract
1. Introduction
2. Results
2.1. Strain Identification and Growth Curve
2.2. EPS Preparation, Mw Determination and Monosaccharide Analysis
2.3. Emulsifying Behavior of the EPS
2.4. Preparation and Physicochemical Characteristics of the EPS/CPT Emulsion
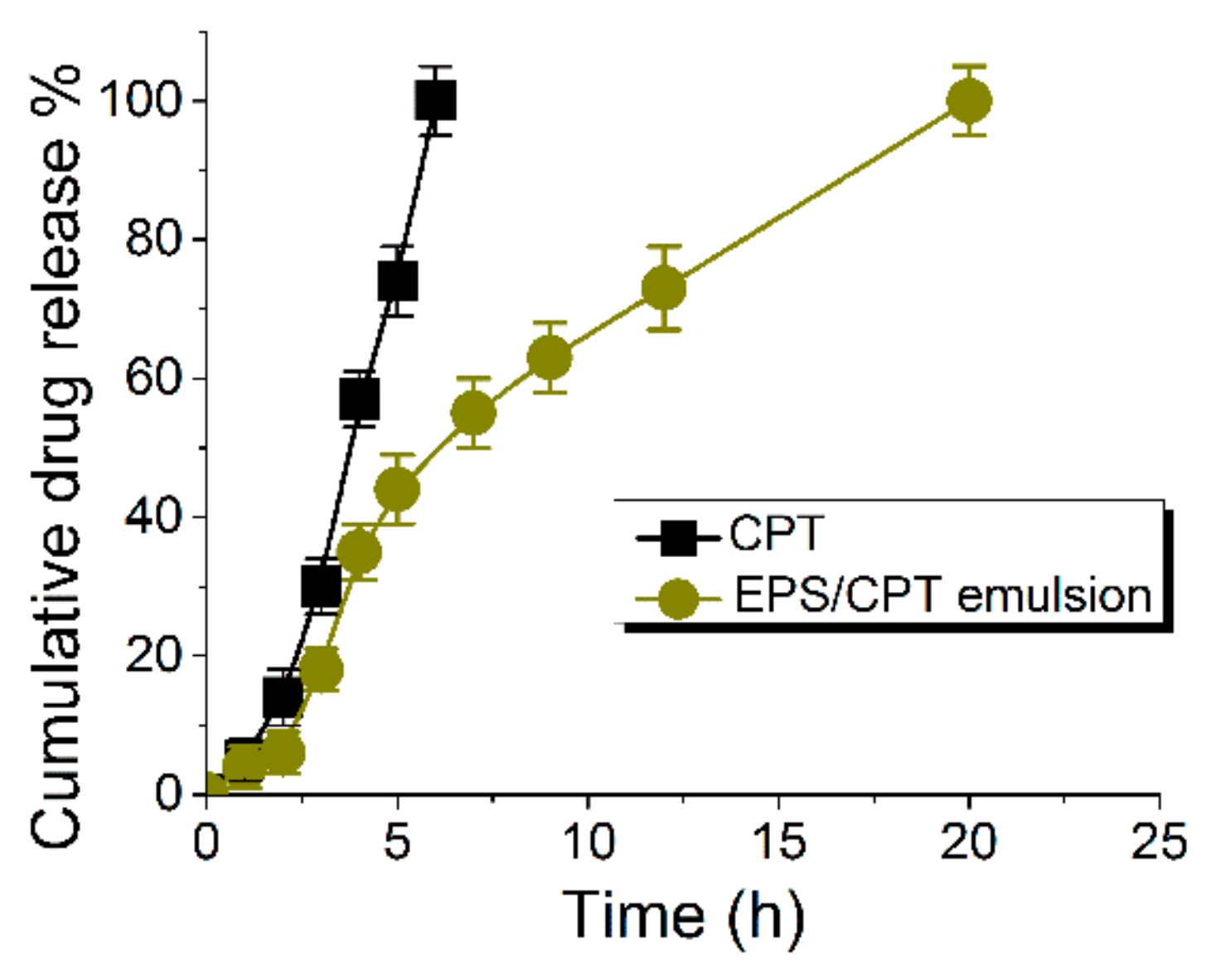
2.5. Drug Release from the EPS/CPT Emulsion In Vitro
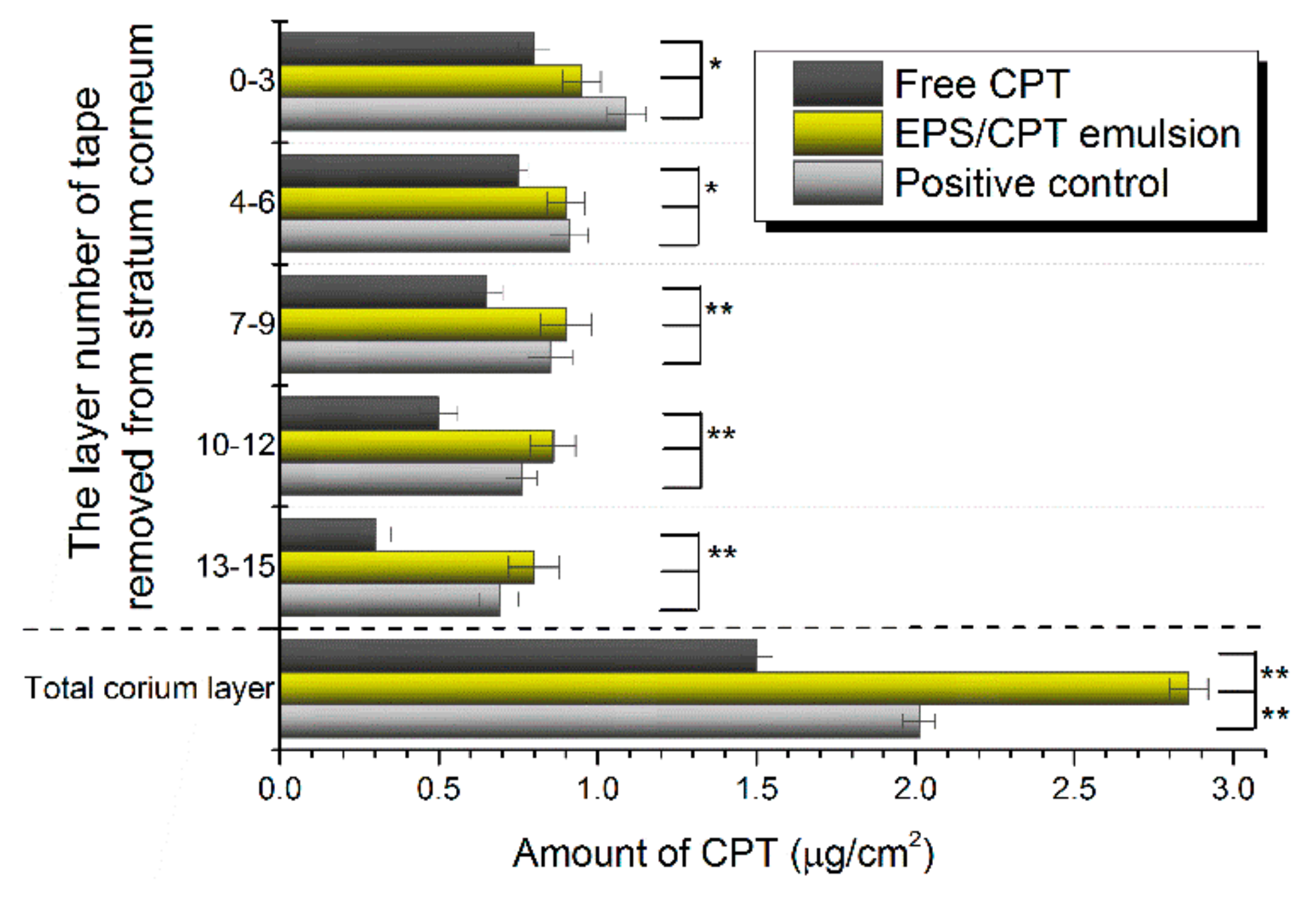
2.6. Skin Permeation and Dermal Pharmacokinetics
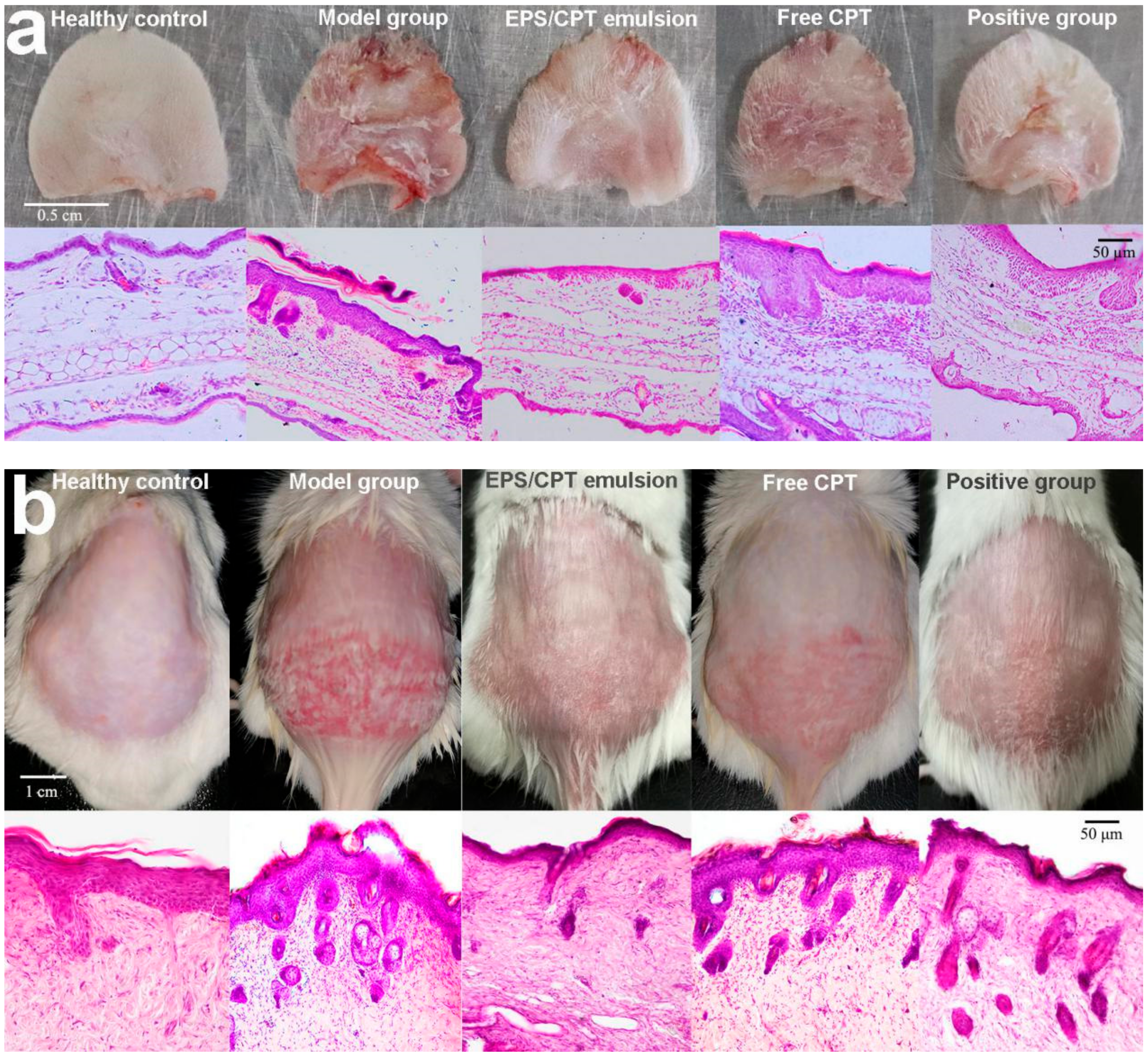
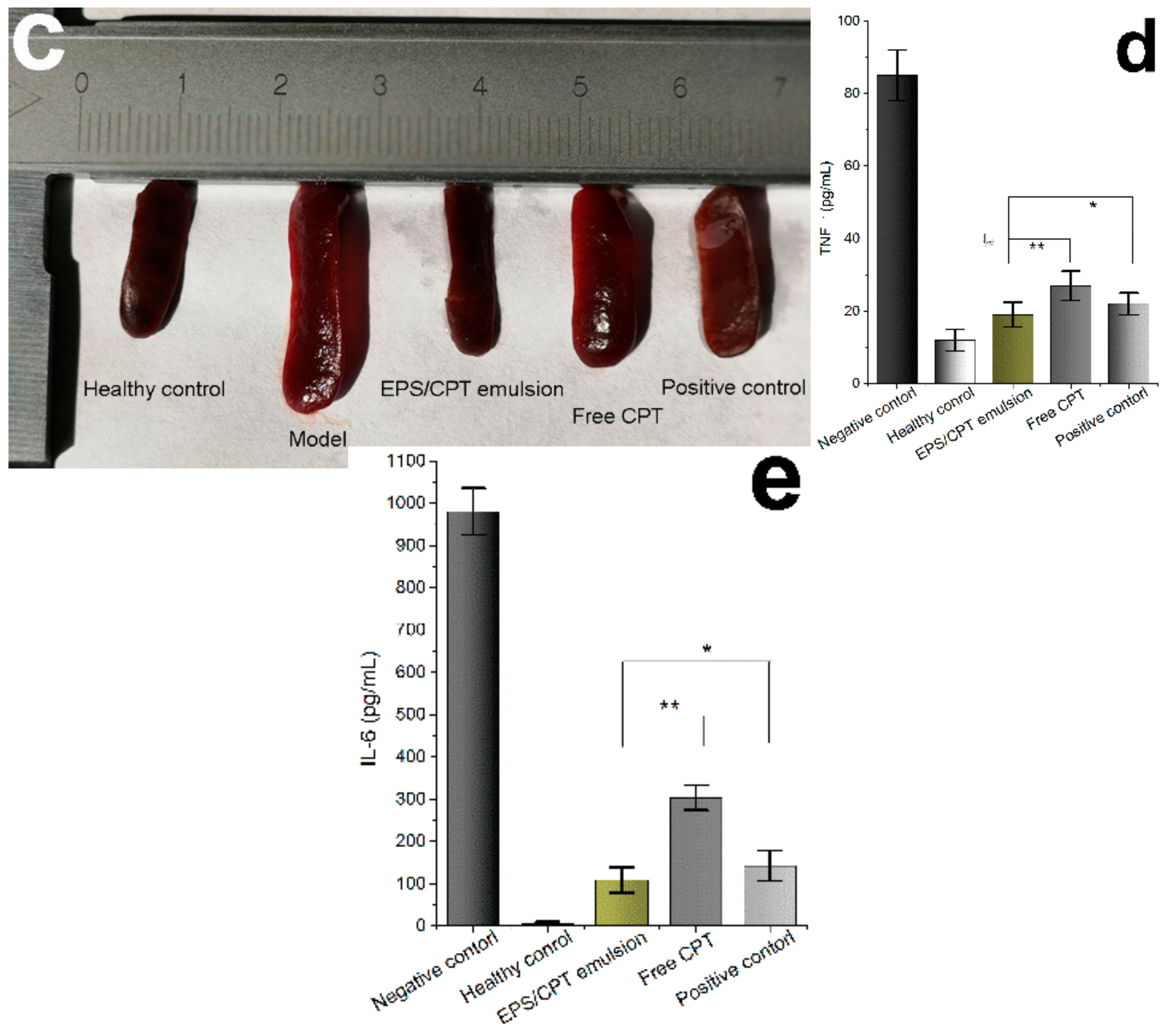
2.7. Psoriasis Animal Experiments
2.7.1. Histomorphology and Inflammatory Factors
2.7.2. Evaluation of Skin Irritation
3. Discussion
4. Materials and Methods
4.1. Strain and Reagents
4.2. Strain Identification
4.3. Growth Curve of ZWJ Strain
4.3.1. Fermentation
4.3.2. Emulsification Index (E) of the Supernatant
4.3.3. Total Sugar Content of the Supernatant
4.4. Preparation and Physicochemical Properties of EPS
4.5. The Emulsion Behavior of EPS
4.6. Preparation and Properties of the EPS/CPT Emulsion
4.7. Drug Release In Vitro
4.8. Ex Vivo Skin Permeability Test
4.8.1. Skin Permeation
4.8.2. Dermal Pharmacokinetic Study
4.9. In Vivo Animal Experiments
4.9.1. Imiquimod Cream Induces Psoriasis Mouse Model
4.9.2. Evaluation of Indicators
4.9.3. Histological Examination of the Skin and Spleen
4.9.4. Analysis of the Serum Levels of the Cytokines TNF and IL6
4.10. Skin Irritation Test
4.11. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Margaret, P.H. Under their skin. Natrue 2012, 492, 64–65. [Google Scholar]
- Kaushik, S.B.; Lebwohl, M.G. Psoriasis: Which therapy for which patient focus on special populations and chronic infections. J. Am. Acad. Dermatol. 2019, 80, 43–53. [Google Scholar] [CrossRef]
- Frieder, J.; Kivelevitch, D.; Menter, A. Calcipotriene betamethasone dipropionate aerosol foam in the treatment of plaque psoriasis: A review of the literature. Ther. Deliv. 2017, 8, 737–746. [Google Scholar] [CrossRef]
- Kaur, A.; Katiyar, S.S.; Kushwah, V.; Jain, S. Nanoemulsion loaded gel for topical co-delivery of clobitasol propionate and calcipotriol in psoriasis. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 1473–1482. [Google Scholar] [CrossRef]
- Rai, V.K.; Mishra, N.; Yadav, K.S.; Prasad, N. Nanoemulsion as pharmaceutical carrier for dermal and transdermal drug delivery: Formulation development, stability issues, basic considerations and applications. J. Control. Release Off. J. Control. Release Soc. 2018, 270, 203–225. [Google Scholar] [CrossRef]
- Pinto, M.F.; Moura, C.C.; Cláudia, N.; Marcela, A.S.; Sofia, A.C.L.; Salette, R.A. New topical formulation for psoriasis: Development of methotrexate-loaded nanostructured lipid carriers. Int. J. Pharm. 2014, 477, 519–526. [Google Scholar] [CrossRef]
- Najafi-Taher, R.; Ghaemi, B.; Amani, A. Delivery of adapalene using a novel topical gel based on tea tree oil nano-emulsion: Permeation, antibacterial and safety assessments. Eur. J. Pharm. Sci. 2018, 120, 142. [Google Scholar] [CrossRef]
- Carrión, O.; Delgado, L.; Mercade, E. New emulsifying and cryoprotective exopolysaccharide from Antarctic pseudomonas, sp. id1. Carbohydr. Polym. 2015, 117, 1028–1034. [Google Scholar] [CrossRef]
- Satpute, S.K.; Banat, I.M.; Dhakephalkar, P.K.; Banpurkar, A.G.; Chopade, B.A. Biosurfactants, bioemulsifiers and exopolysaccharides from marine microorganisms. Biotechnol. Adv. 2010, 28, 436–450. [Google Scholar] [CrossRef]
- Gudmundsdottir, A.B.; Omarsdottir, S.; Brynjolfsdottir, A.; Berit, S.; Paulsen, B.S. Exopolysaccharides from Cyanobacterium aponinum from the Blue Lagoon in Iceland increase IL-10 secretion by human dendritic cells and their ability to reduce the IL-17+RORγt+/IL-10+FoxP3+ ratio in CD4+ T cells. Immunol. Lett. 2015, 163, 157–162. [Google Scholar] [CrossRef]
- Song, B.; Rong, Y.J.; Zhao, M.X.; Chi, Z.M. Antifungal activity of the lipopeptides produced by Bacillus amyloliquefaciens anti-CA against Candida albicans isolated from clinic. Appl. Microbiol. Biotechnol. 2013, 97, 7141–7150. [Google Scholar] [CrossRef]
- Yang, H.; Deng, J.; Yuan, Y.; Daidi Fan, D.D.; Zhang, Y.; Zhang, R.J.; Han, B. Two Novel Exopolysaccharides from Bacillus amyloliquefaciens C-1: Antioxidation and Effect on Oxidative Stress. Curr. Microbiol. 2015, 70, 298–306. [Google Scholar] [CrossRef]
- Han, Y.; Liu, E.; Liu, L.; Zhang, B.; Wang, Y.; Gui, M.; Wu, R.Y.; Li, P.L. Rheological, emulsifying and thermostability properties of two exopolysaccharides produced by Bacillus amyloliquefaciens lpl061. Carbohydr. Polym. 2015, 115, 230–237. [Google Scholar] [CrossRef]
- Horozov, T.S.; Binks, B.P.; Gottschalk-Gaudig, T. Effect of electrolyte in silicone oil-in-water emulsions stabilised by fumed silica particles. Phys. Chem. Chem. Phys. 2007, 9, 6398–6404. [Google Scholar] [CrossRef]
- Prasanna, P.H.P.; Bell, A.; Grandison, A.S. Emulsifying, rheological and physicochemical properties of exopolysaccharide produced by Bifidobacterium longum subsp. infantis CCUG 52486 and Bifidobacterium infantis NCIMB 702205. Carbohyd. Polym. 2012, 90, 533–540. [Google Scholar] [CrossRef]
- Kodali, V.P.; Das, S.; Sen, R. An exopolysaccharide from a probiotic: Biosynthesis dynamics, composition and emulsifying activity. Food Res. Int. 2009, 42, 695–699. [Google Scholar] [CrossRef]
- Iyer, A.; Mody, K.; Jha, B. Emulsifying properties of a marine bacterial exopolysaccharide. Enzyme Microb. Technol. 2006, 38, 220–222. [Google Scholar] [CrossRef]
- Daudt, R.M.; Back, P.I.; Cardozo, N.S.M.; Marczak, L.D.F.; Külkamp-Guerreiro, I.C. Pinhão starch and coat extract as new natural cosmetic ingredients: Topical formulation stability and sensory analysis. Carbohydr. Polym. 2015, 13, 573–580. [Google Scholar] [CrossRef]
- Douguet, M.; Picard, C.; Savary, G.; Merlaud, F.; Loubat-Bouleuc, N.; Grisel, M. Spreading properties of cosmetic emollients: Use of synthetic skin surface to elucidate structural effect. Colloids Surf. B Biointerfaces 2017, 154, 307–314. [Google Scholar] [CrossRef]
- Khamanga, S.M.M.; Walker, R. In vitro dissolution kinetics of captopril from microspheres manufactured by solvent evaporation. Dissolut. Technol. 2012, 19, 42–51. [Google Scholar] [CrossRef]
- Sonawane, R.; Harde, H.; Katariya, M.; Agrawal, S.; Jain, S. Solid lipid nanoparticles-loaded topical gel containing combination drugs: An approach to offset psoriasis. Expert Opin. Drug Deliv. 2014, 11, 1833–1847. [Google Scholar] [CrossRef]
- Bonifati, C.; Ameglio, F. Cytokines in psoriasis. Int. J. Derm. 2010, 38, 241–251. [Google Scholar] [CrossRef]
- Balato, N.; Napolitano, M.; Ayala, F.; Patruno, C.; Megna, M.; Tarantino, G. Nonalcoholic fatty liver disease, spleen and psoriasis: New aspects of low-grade chronic inflammation. World J. Gastroenterol. 2015, 21, 6892–6897. [Google Scholar] [CrossRef]
- Zhong, S.Y.; Dong, Y.Y.; Liu, D.X.; Xu, D.H.; Xiao, S.X.; Chen, H.L.; Kong, M.G. Surface air plasma-induced cell death and cytokine release of human keratinocytes in the context of psoriasis. Br. J. Derm. 2016, 174, 542–552. [Google Scholar] [CrossRef]
- Zheng, Y.; Danilenko, D.M.; Valdez, P.; Kasman, I.; Eastham-Anderson, J.; Wu, J.; Ouyang, W.J. Interleukin-22, a th17 cytokine, mediates il-23-induced dermal inflammation and acanthosis. Nature 2007, 445, 648–651. [Google Scholar] [CrossRef]
- Pradhan, M.; Singh, D.; Singh, M.R. Novel colloidal carriers for psoriasis: Current issues, mechanistic insight and novel delivery approaches. J. Control. Release Off. J. Control. Release Soc. 2013, 170, 380–395. [Google Scholar] [CrossRef]
- Zhu, W.J.; Wang, Y.Z.; Yan, F.; Song, R.T.; Li, Z.J.; Li, Y.Q.; Song, B. Physical and chemical properties, percutaneous absorption-promoting effects of exopolysaccharide produced by Bacillus atrophaeus WYZ strain. Carbohydr. Polym. 2018, 192, 52–60. [Google Scholar] [CrossRef]
- Sambrook, J.; Fritsch, E.F.; Maniatis, T. Preparation and analysis of eukaryotic genomic DNA. In Molecular Cloning: A Laboratory Manual, 2nd ed.; Cold Spring Harbor Laboratory Press: Beijing, China, 1989; pp. 367–370. [Google Scholar]
- Zhao, K.; Xue, P.J.; Guang-Ye, G.U. Study on Determination of Reducing Sugar Content Using 3,5-Dinitrosalicylic Acid Method. Food Sci. 2008, 29, 534–536. [Google Scholar]
- Kaci, M.; Arab-Tehrany, E.; Desjardins, I.; Banon-Desobry, S.; Desobry, S. Emulsifier free emulsion: Comparative study between a new high frequency ultrasound process and standard emulsification processes. J. Food Eng. 2016, 194, 109–118. [Google Scholar] [CrossRef]


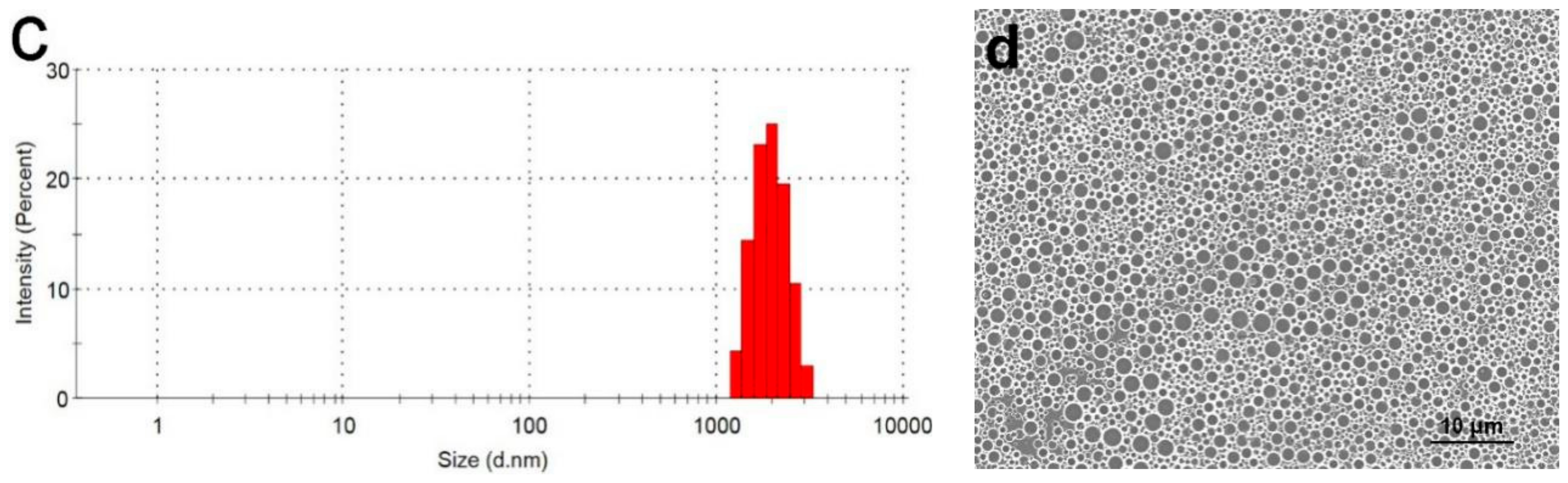
| Emulsion Type | Viscosity (Torque Value Is 50%) | Spreading Value (20 μL Sample) | Average Droplet Size | Calcipotriol (CPT) Content % |
|---|---|---|---|---|
| Oil in Water (O/W) | 105.3 ± 6.8 mPa·s | 542 ± 30 mm2 | 2433 nm | 0.00492 |
| Groups | Days | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| Healthy control | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 |
| Model Group | 4.00 ± 0.00 | 4.00 ± 0.00 | 4.00 ± 0.00 | 3.33 ± 0.47 | 3.17 ± 0.37 | 3.00 ± 0.00 | 3.00 ± 0.00 |
| EPS/CPT emulsion | 3.33 ± 0.47 | 3.00 ± 0.00 | 2.83 ± 0.37 | * 2.00 ± 0.00 | * 1.67 ± 0.47 | * 1.50 ± 0.50 | ** 1.00 ± 0.00 |
| Free CPT | 4.00 ± 0.00 | 3.33 ± 0.47 | 3.17 ± 0.37 | 3.00 ±0.00 | 2.83 ± 0.37 | * 2.50 ± 0.50 | * 2.00 ± 0.00 |
| Positive control group | 3.33 ± 0.47 | 3.00 ± 0.00 | 2.67 ± 0.37 | * 2.00 ± 0.00 | * 2.00 ± 0.00 | * 1.67 ± 0.47 | * 1.67 ± 0.37 |
| Groups | Days | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Saline | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 |
| EPS/CPT emulsion | 0 ± 0.00 | 0 ± 0.00 | 0 ± 0.00 | * 0.7 ± 0.47 |
| Daivonex | 0 ± 0.00 | 0.33 ± 0.47 | 0.67 ± 0.47 | 1.0 ± 0.00 |
| Capsaicin | 3.0 ± 0.00 | 3.0 ± 0.00 | 3.33 ± 0.47 | 3.33 ± 0.47 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, B.; Song, R.; Cheng, M.; Chu, H.; Yan, F.; Wang, Y. Preparation of Calcipotriol Emulsion Using Bacterial Exopolysaccharides as Emulsifier for Percutaneous Treatment of Psoriasis Vulgaris. Int. J. Mol. Sci. 2020, 21, 77. https://doi.org/10.3390/ijms21010077
Song B, Song R, Cheng M, Chu H, Yan F, Wang Y. Preparation of Calcipotriol Emulsion Using Bacterial Exopolysaccharides as Emulsifier for Percutaneous Treatment of Psoriasis Vulgaris. International Journal of Molecular Sciences. 2020; 21(1):77. https://doi.org/10.3390/ijms21010077
Chicago/Turabian StyleSong, Bo, Ruiteng Song, Min Cheng, Hairong Chu, Fang Yan, and Yuzhen Wang. 2020. "Preparation of Calcipotriol Emulsion Using Bacterial Exopolysaccharides as Emulsifier for Percutaneous Treatment of Psoriasis Vulgaris" International Journal of Molecular Sciences 21, no. 1: 77. https://doi.org/10.3390/ijms21010077
APA StyleSong, B., Song, R., Cheng, M., Chu, H., Yan, F., & Wang, Y. (2020). Preparation of Calcipotriol Emulsion Using Bacterial Exopolysaccharides as Emulsifier for Percutaneous Treatment of Psoriasis Vulgaris. International Journal of Molecular Sciences, 21(1), 77. https://doi.org/10.3390/ijms21010077