Current Status of Herbal Medicines in Chronic Liver Disease Therapy: The Biological Effects, Molecular Targets and Future Prospects
Abstract
:1. Introduction
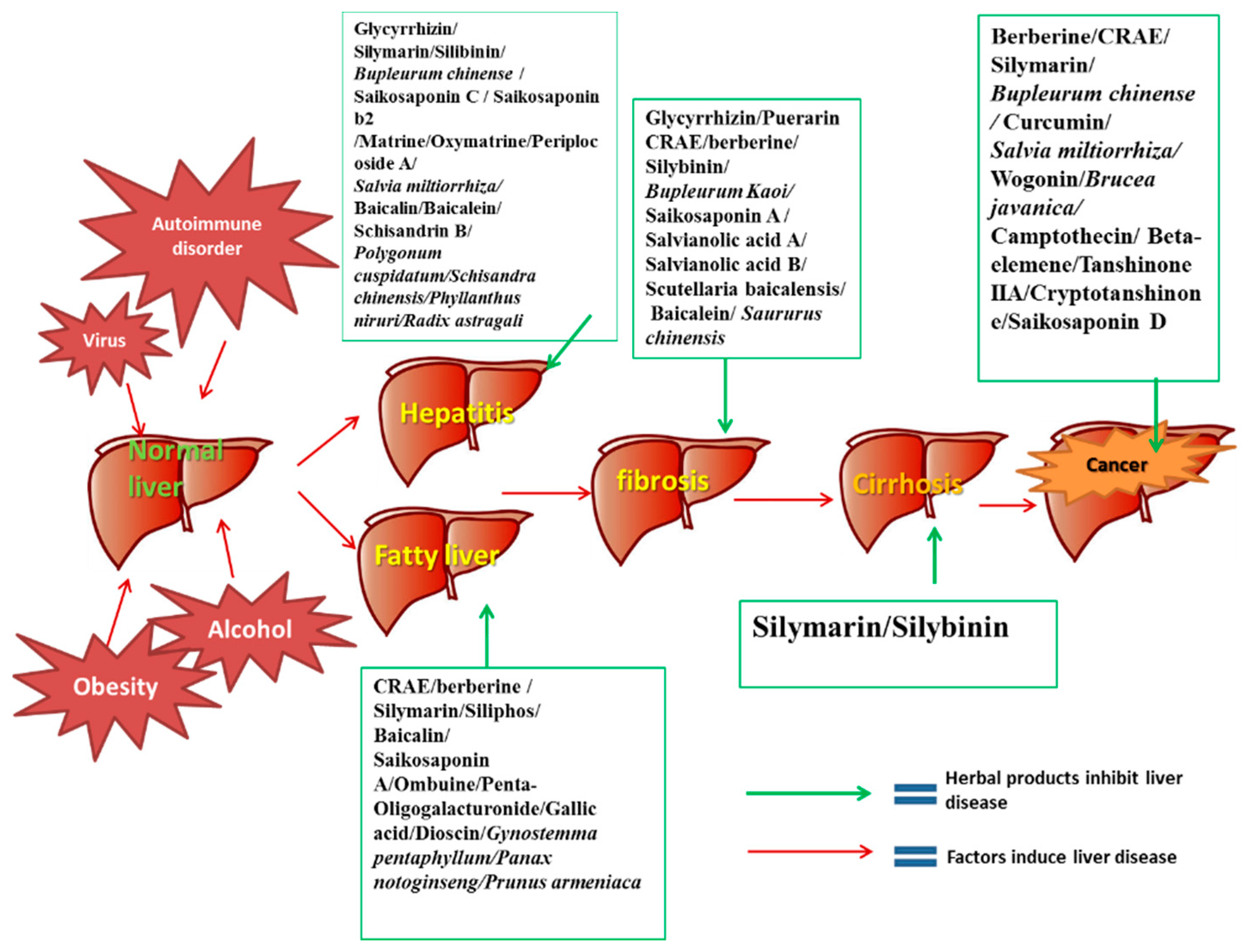
2. Recent Research on the Roles of Herbs and Phytochemicals in Chronic Liver Disease Treatment
2.1. Herbs and Phytochemicals in the Treatment of Chronic Hepatitis
2.1.1. The Epidemiological and Pathological Characteristics of Chronic Hepatitis and Current Therapeutic Strategy
2.1.2. Herbs and Phytochemicals in the Treatment of Chronic Hepatitis
| Herbal Medicines (Herbs or Phytochemicals) | The Sources of Herbal Medicines | Type of Study | Biological Effects and Molecular Mechanism | Reference |
|---|---|---|---|---|
| Glycyrrhizin | Root of Glycyrrhiza uralensis Fisch | In vitro | Suppression of Hepatitis C by decreasing the activity of phospholipase A2. | [24] |
| In vivo | Suppressing the cytolytic activity of complement. | [25] | ||
| Clinical study | Enhancing the secretion of IL-10 by dendritic cells. | [26] | ||
| Controlling HBV replication. | [27] | |||
| Decreasing serum ALT. | [28] | |||
| Silibinin | Fruits of Silybum marianum (L.) Gaertn | In vitro | Inhibiting HCV by blocking the clathrin-dependent trafficking. | [36] |
| Clinical study | Decreasing the secretions of ALT, AST and alkaline phosphatase in patients with chronic active hepatitis. | [37] | ||
| Saikosaponin C, Saikosaponin b2 | Root of Bupleurum marginatum Wall. ex DC | In vitro | Decreasing HBV antigen in culture medium. | [50] |
| Suppressing early HCV entry. | [51] | |||
| Matrine, Oxymatrine | Root of Sophora flavescens Aiton | In vitro | Improving the effect of lamivudine on suppressing the secretion of HBeAg in combination with oxymatrine or matrine, | [54] |
| In vivo | Improving the vasomotion in liver tissue by increasing the concentration of NO in culture supernatant of rat intestinal microvascular endothelial cells and up-regulating the eNOS concentration. | [55] | ||
| In vivo | Activating the peripheral lymphocytes and inducing antiviral cytokine secretion by regulating TLR9 signal pathway. | [56] | ||
| Periplocoside A | Bark of Periploca sepium Bunge | In vitro and in vivo | Ameliorating autoimmune hepatitis induced by ConeA by decreasing the secretions of (IL)-4, IFN-gamma and ALT. | [57] |
| Baicalin, Baicalein | Root of Scutellaria baicalensis Georgi | In vitro | Protecting hepatocytes from oxidative stress by up-regulating both liver fatty acid binding protein expression and activity of intracellular SOD and GSH. | [59] |
| Anti-inflammatory, anti-oxidant, and anti-apoptotic in hepatic cells. | [60] | |||
| In vivo | Iron chelation and antioxidant effects in iron overload liver. | [61] | ||
| Accelerating liver cells regeneration by modulating IL-6 and TNF-alpha mediated signal pathways. | [62] | |||
| In vitro | Inhibiting apoptosis in liver cells by the protective effect on mitochondria, inhibiting the release of cytochrome c, decreasing the Bax/Bcl-2 ratio, and inhibiting the phosphorylation of NF-kappaB, JNK and ERK. | [63] | ||
| Schisandrin B | Fruit of Schisandra chinensis (Turcz.) Baill | In vitro | Anti-inflammation in liver by inducing nuclear translocation of Nrf2 and increasing the transcription of HO-1. | [66] |
| Silymarin | Flavonolignans mixture from the fruits of Silybum marianum (L.) Gaertn. | In vitro | Down-regulating the HCV core mRNA and protein expression. | [30] |
| Blocking of HCV entry and transmission by inhibiting microsomal triglyceride transfer protein activity, apolipoprotein B secretion, and infectious virion production into culture supernatants. | [31] | |||
| Clinical study | Decreasing serum transaminases in patients with chronic viral hepatitis, but not affecting viral content in vivo. | [32,33] | ||
| Inhibiting inflammatory by suppressing the pro-inflammatory cytokine and up-regulating the IL-10. | [34] | |||
| Salvia miltiorrhiza Bunge | Aqueous extract of root and rhizome of Salvia miltiorrhiza Bunge | In vivo | Reducing inflammation in the liver by inhibition of NFkappaB and p38 signaling. | [52] |
| Improving the hepatic morphology, decreasing iron deposition as well as inhibiting the expression of type I and type III collagen, TGF-beta mRNA, and increasing the expression of MMP-9 mRNA in the liver. | [53] | |||
| Bupleurum chinense DC | Aqueous extract of root or leaf of Bupleurum chinense DC | In vitro | Scavenging free radical activity and suppressing the superoxide anion formation. | [49] |
| In vivo | Reducing inflammatory cytokine expression. | [48] | ||
| Polygonum cuspidatum Willd. ex Spreng. | Ethanol extract of rhizome of Polygonum cuspidatum Willd. ex Spreng. | In vitro | Suppressing the expression of HBeAg and the production of HBV DNA. | [47] |
| Schisandra chinensis (Turcz.) Baill | Aqueous extract of fruit of Schisandra chinensis (Turcz.) Baill | In vitro | Anti-Hepatitis B virus activity by suppressing HBV DNA replication. | [65] |
| Phyllanthus niruri L | Aqueous extract of whole plant of Phyllanthus niruri L | In vitro | Inhibiting HBsAg secretion and HBsAg mRNA expression by up-regulation of annexin A7. | [42] |
| Clinical study | Clearance of serum HBsAg, HBeAg and HBV DNA. | [43] | ||
| Astragalus membranaceus (Fisch.) Bunge | Aqueous extract of root of Astragalus membranaceus (Fisch.) Bunge | In vivo | Suppressing duck HBV DNA replication. | [72] |
| Clinical study | Clearance of serum HBeAg and HBV DNA in chronic viral hepatitis patients. |
2.2. Herbs and Phytochemicals in the Treatment of Fatty Liver Disease
2.2.1. The Epidemiological and Pathological Characteristics of Fatty Liver Disease and Current Therapeutic Strategy
2.2.2. Herbs and Phytochemicals in the Treatment of Fatty Liver Disease
| Herbal Medicines (Herbs or Phytochemicals) | The Sources of Herbal Medicines | Type of Study | Biological Effects and Molecular Mechanism | Reference |
|---|---|---|---|---|
| Berberine | Rhizoma of Coptis chinensis Franch | In vitro | Reducing TG accumulation in the FFA-induced hepatic steatosis. | [81] |
| In vivo | Enhancing insulin resistance of nonalcoholic fatty liver disease by increasing the expression of IRS-2. | [82] | ||
| Suppressing lipogenesis and promoting lipolysis by inhibiting the expression of SCD1, FAS, SREBP1c and increasing the expression of CPT1. | [83] | |||
| Ombuine | Whole plant of Gynostemma pentaphyllum (Thunb.) Makino | In vitro | Reducing intracellular concentrations of triglyceride and cholesterol in HepG2 cells and decreased the expression of several lipogenic genes by activating of PPARalpha and delta/beta. | [87] |
| Penta-oligogalacturonide | Fruit of Crataegus pinnatifida Bunge | In vitro | Scavenging hydroxyl, superoxide anion and DPPH radicals in liver cells. | [92] |
| In vivo | Enhance the antioxidant enzyme activities of superoxide dismutase, catalase, glutathione peroxidase, increase the levels of glutathione and the total antioxidant capacity, but lowered the production of malondialdehyde in the liver of high-fat fed mice. | |||
| Glycyrrhizin | Root of Glycyrrhiza uralensis Fisch | In vivo | Inhibiting the process of fibrosis on nonalcoholic steatohepatitis in rats. | [97] |
| Suppressing the development of hepatic steatosis, attenuating ultrastructural alterations of mitochondria of the hepatocyte, down-regulating the ROS in mice liver. | [98] | |||
| Siliphos | Fruits of Silybum marianum (L.) Gaertn. | In vitro | Alleviating the damage of lipid membranes by protecting of mitochondrial function. | [100] |
| Clinical study | Decreasing ultrasonographic scores for liver steatosis in patients with nonalcoholic fatty liver disease. | [101] | ||
| Baicalin | Root of Scutellaria baicalensis Georgi | In vivo | Decreasing the level of serum total cholesterol, triglycerides, LDL, ALT and AST, and increase the level of serum HDL by mediation of CaMKKbeta/AMPK/ACC pathway. | [107] |
| Clinical study | Attenuating the ischemia/reperfusion injury in alcoholic fatty liver by suppressing of myeloid differentiation factor 88 and TLR4 protein expressions and the nuclear translocation of NF-kB after reperfusion. | [108] | ||
| Gallic acid | Picarp of Punica granatum L | In vivo | Recovering impaired glucose and lipid homeostasis in high fat diet-induced NAFLD mice. | [95] |
| In vivo | Reducing GSSG content and oxidative stress and increasing the levels of GSH peroxidase, glutathione, GSH S-transferase and GSH reductase in liver tissue. | [96] | ||
| Dioscin | Rhizoma of Dioscorea opposita Thunb | In vitro and in vivo | Relieving oxidative damage, inhibiting inflammation, cholesterol and triglyceride synthesis, decreasing MAPK phosphorylation levels, promoting fatty acid beta-oxidation, and inducing autophagy to improve fatty liver conditions. | [93] |
| In vivo | Protective effect against alcoholic fatty liver by relieving alcohol-induced oxidative stress, inflammatory cytokine production, mitochondrial function, apoptosis and liver steatosis. | [94] | ||
| Total saponins of Panax notoginseng (Burkill) F.H.Chen | Flower, root, leaf of Panax notoginseng (Burkill) F.H.Chen | In vitro | Attenuating the ethanol induced hepatic lipid accumulation by inhibiting the production of MDA, GSH l and reactive ROS, reducing TNF-alpha and IL-6 levels, as well as enhancing the SOD)activity in liver, and abrogated CYP2E1 induction. | [88] |
| In vivo | Relieve oxidative stress and insulin resistance in NAFLD rats. | |||
| Gynostemma pentaphyllum (Thunb.) Makino | Aqueous extract of whole plant of Gynostemma pentaphyllum (Thunb.) Makino | In vitro | Promoting lipid metabolism, and decreasing serum lipids level by down-regulating the production of TMAO and up-regulating phosphatidylcholine. | [84] |
| Inhibiting the accumulation of cholesterol and triglycerides as well as preventing oxidative stress by enhancing the production of NO and affects the molecular composition of the mitochondrial phospholipid CL. | [85] | |||
| Clinical study | Reducing the level of serum AST, ALP, insulin, decrease BMI and insulin resistance index. | [86] | ||
| Prunus armeniaca L | Aqueous extract of kernels of Prunus armeniaca L | In vivo | Relieving CCl4-induced liver steatosis by antioxidant and radical-scavenging. | [103] |
| Clinical study | Protective effects on fatty liver disease patient by decreasing the serum AST and ALT levels. | [104] |
2.3. Herbs and Phytochemicals in the Treatment of Cirrhosis
2.3.1. The Epidemiological and Pathological Characteristics of Cirrhosis and Current Therapeutic Strategy
2.3.2. Herbs and Phytochemicals in the Treatment of Cirrhosis
| Herbal Medicines (Herbs or Phytochemicals) | The Sources of Herbal Medicines | Type of Study | Biological Effects and Molecular Mechanism | Reference |
|---|---|---|---|---|
| Berberine | Rhizoma of Coptis chinensis Franch | In vivo | Remedying CCl(4)-induced chronic oxide stress by anti-oxidant mechanisms, reducing myofibroblast proliferation and the expression of TGF- b1 and a-SMA. | [122] |
| Puerarin | Rhizoma of Pueraria lobata | In vivo | Attenuating the CCl4-induced toxicity in the hepatic cells of hepatic fibrosis rats, mediating anti-fibrosis effects through modulating the PPAR-gamma expression and inhibiting the PI3K/Akt signal pathway. | [125] |
| Mediating anti-fibrosis effects in hepatic fibrosis rats through down-regulating the TNF-alpha and NF-kB expression. | [126] | |||
| Inducing apoptosis of hepatic stellate cells by down-regulating bcl-2 mRNA. | [127] | |||
| Glycyrrhizin | Root of Glycyrrhiza uralensis Fisch | In vivo | Reducing serum ALT and improving histological changes by decreasing NF-kappa B binding activity. | [131] |
| Improving histological changes and inhibited collagen deposition by decreasing the expressions of Smad2, Smad3, SP-1 and TGF-beta1. | [132] | |||
| Clinical study | Reducing serum ALT level after 12 weeks of treatment and suppression of necro-inflammation and fibrosis. | [133] | ||
| Silybinin | Fruits of Silybum marianum (L.) Gaertn. | In vivo | Preventing the production of mitochondrial ROS and inhibiting the cardiolipin oxidation or citrate carrier failure in the liver of cirrhosis rat. | [134] |
| Exhibiting significant anti-inflammatory effects in cirrhotic rat liver by decreasing the expression of LPCAT and increasing platelet-activating factor level. | [135] | |||
| Saikosaponin A | Root of Bupleurum kaoi Liu, C.Y.Chao & Chuang | In vitro | Increasing the expression of BMP-4 and inhibiting the activation of hepatic stellate cells. | [139] |
| In vivo | Combination therapy with IFN-alpha can increase peripheral blood CD4+ T cells and CD8+ T cell ratios, down-regulating plasma AST and ALT activities, decreasing the plasma and hepatic cholesterol and triglyceride levels. | [140,141] | ||
| Salvianolic acid B | Root and rhizome of Salvia miltiorrhiza Bunge | In vitro | Inhibiting intracellular signal transduction of TGF-β1 in hepatic stellate cells and suppressing the expression of its receptor protein. | [142] |
| In vivo | Decreasing fibrous tissue deposition in the portal areas, and obviously decreasing collagen deposition. In addition, decreasing oTIMP1 and collagen 1(alpha) protein. | |||
| Inhibiting the process of liver fibrosis and improve liver function by reducing the nonfunctioning fibers in the liver. | [143] | |||
| Baicalein | Root of Scutellaria baicalensis Georgi | In vivo | Inhibiting hypertrophic scar formation by suppressing TGF-beta/Smad2/3 signaling pathway in mice with mechanical load-induced scars. | [146] |
| Suppressing stellate cell activation by decreasing the expression of PDGF-beta receptor. | [147] | |||
| Silymarin | Flavonolignans mixture from the fruits of Silybum marianum (L.) Gaertn. | Clinical study | Long-term use may reduce symptoms and quality-of-life in cirrhosis patients. | [137] |
| Coptis chinensis Franch | Aqueous extract of rhizoma of Coptis chinensis Franch | In vivo | Increasing serum SOD activity and the histological results in CCl(4)-induced liver fibrosis by anti-oxidant mechanisms. | [120,121] |
| Saururus chinensis (Lour.) Baill | Ethanol extract of rhizoma of Saururus chinensis (Lour.) Baill | In vivo | Reducing the elevated levels of liver index such as serum ALT, AST, HA, and hepatic MDA contents in hepatic fibrosis rats. | [130] |
| Bupleurum kaoi Liu, C.Y.Chao & Chuang | Ethanol extract of root of Bupleurum kaoi Liu, C.Y.Chao & Chuang | In vitro | Exhibiting the anti-fibrotic and anti-inflammatory activities in liver cells by anti-oxidant activity of increasing glutathione expression. | [138] |
| Scutellaria baicalensis Georgi | Ethanol extract of root of Scutellaria baicalensis Georgi | In vitro | Reducing the levels of liver malondialdehyde and hydroxyproline significantly, with ameliorative histological results which indicated the anti-fibrosis effect. | [144] |
| Suppressing the proliferation and activation of hepatic stellate cells by inducing cell cycle arrest in G2/M phase and inducing stellate cell apoptosis via caspase and Bax pathway. | [145] |
2.4. Herbs and Phytochemicals in the Treatment of Primary Liver Cancer
2.4.1. The Epidemiological and Pathological Characteristics of Primary Liver Cancer and Current Therapeutic Strategy
2.4.2. Herbs and Phytochemicals in the Treatment of Primary Liver Cancer
| Herbal Medicines (Herbs or Phytochemicals) | The Sources of Herbal Medicines | Type of Study | Biological Effects and Molecular Mechanism | Reference |
|---|---|---|---|---|
| Berberine | Rhizoma of Coptis chinensis Franch | In vitro and in vivo | Increasing miR-23a expression in human HCC cells and may activate the transcription of p53-related tumor suppressive GADD45alpha and p21 genes. | [158] |
| In vitro | Inducing mitochondrial apoptosis in liver cancer cells and activating autophagic cell death in liver cancer cells by activation of Beclin-1 and suppressing the mTOR-signaling pathway. | [160] | ||
| Saikosaponin D | Root or leaf of Bupleurum chinense DC | In vitro | Increasing cell apoptosis by activation of caspases 3 and 7 and finally causing the DNA fragmentation. | [165] |
| In vitro | Inhibiting HCC development and metastasis by decreasing the expression of syndecan-2, MMP-2, MMP-13 in rat liver cell. | [166] | ||
| Cryptotanshinone, Tanshinone IIA | Root and rhizome of Salvia miltiorrhiza Bunge | In vitro | Suppressing doxorubicin efflux by regulating P-glycoprotein expression. | [168] |
| In vitro | Inducing apoptotic effects without influencing oxidative stress and synergism with doxorubicin in HCC cells. | [168] | ||
| Wogonin | Root of Scutellaria baicalensis Georgi | In vitro | Suppressing the VEGF-C-induced lymphangiogenesis by a decrease in VEGF-C-induced VEGFR-3 phosphorylation through suppressing of IL-1beta and COX-2 production. | [170] |
| In vivo | Exhibiting protective effects against genotoxicities by down-regulating hepatic DNA adducts’ formation in mice. | [171] | ||
| Beta-elemene | Rhizome of Curcuma aromatica Salisb | In vitro | Inducing cell apoptosis and suppressing the proliferation of HepG2 cells by suppressing microtubular polymerization and decreasing alpha-tubulin. | [173] |
| In vitro | Suppressing the growth of H22 cells by increasing the expression of histone H1 at the protein level. | [174] | ||
| Camptothecin | Bark or stem of Camptotheca acuminata Decne | In vitro | Suppressing SMMC-7721 cell growth by arresting cell cycle at the S and G2/M phases, and inducing mitochondrial pathway mediated apoptosis. | [177] |
| In vitro | Inducing TRAIL-mediated apoptosis in HCC cells by increasing ROS and ERK/p38-dependent DR5. | [178] | ||
| Curcumin | Rhizome of Curcuma longa L | In vitro | Inhibiting cell proliferation and inducing apoptosis on human liver carcinoma cells. | [180] |
| Silymarin | Flavonolignans mixture from the fruits of Silybum marianum (L.) Gaertn. | In vivo | Inhibiting cell proliferation, inducing cell apoptosis, and sensitizing the detoxification system in hepatocellular carcinoma cells. | [161] |
| In vitro and in vivo | Inhibiting inflammatory activity and metastases of HCC cells by down-regulating the mitochondrial transmembrane potential of liver cells. | [163] | ||
| Coptidis rhizoma | Aqueous extract of rhizoma of Coptis chinensis Franch | In vitro and in vivo | Inhibiting VEGF by suppressing the activity of eEF2 in liver cancer | [156] |
| In vitro | Suppressing HCC cells migration through Rho/ROCK signaling pathway inhibition. | [159] | ||
| Bupleurum chinense DC | Aqueous extract of root or leaf of Bupleurum chinense DC | In vitro | Increasing the micronuclei frequency and DNA damage in liver cancer cells in combination with chemotherapy. | [164] |
| Salvia miltiorrhiza Bunge | Aqueous extract of root and rhizome of Salvia miltiorrhiza Bunge | In vivo | Preventing human HCC on DEN-induced hepatocarcinogenesis by suppressing fibrosis and plasminogen activator inhibitor-1 mRNA transcription. | [167] |
| Brucea javanica (L.) Merr | Aqueous extract of seeds of Brucea javanica (L.) Merr | In vitro | Inducing liver cancer cell apoptosis by regulating the mitochondrial dependent pathway and activating caspase 3. | [175] |
| In vitro and in vivo | Suppressing the proliferation of HepG2 cells in a dose-dependent manner and inhibiting metastasis. | [176] |
3. Traditional Chinese Medicine Herbal Formulae for Chronic Liver Disease Treatment
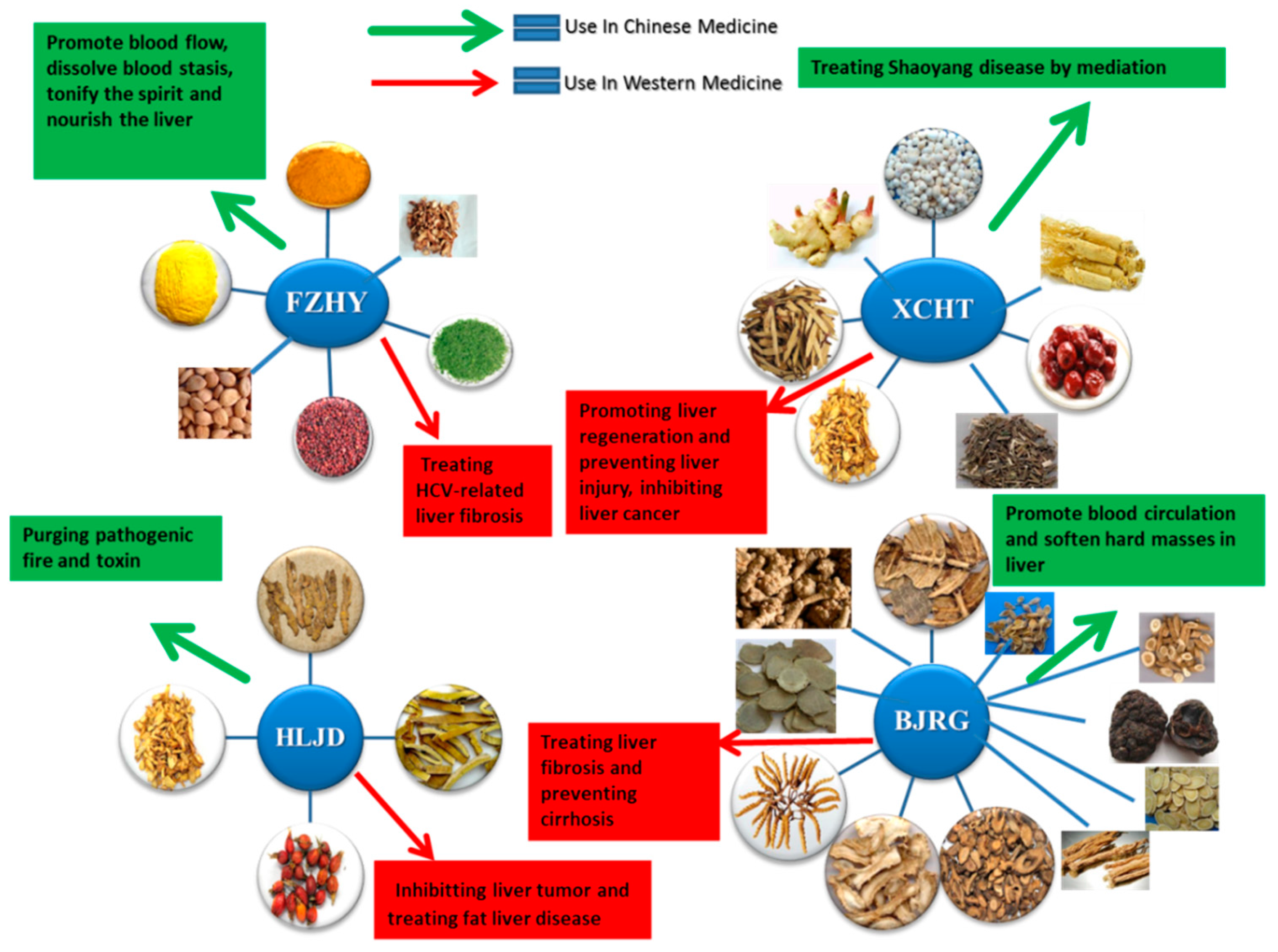
3.1. Fuzheng Huayu Tablet for Chronic Liver Disease Treatment
3.2. Xiao Chai Hu Tang for Chronic Liver Disease Treatment
3.3. Huanglian Jiedu Decoction in Liver Disease Treatment
3.4. Biejia Ruangan Tablets in Liver Disease Treatment
4. The Potential Side-Effects or Toxicity of Herbal Products in Chronic Liver Disease Treatment
4.1. The Potential Side-Effects or Toxicity of Coptis Chinensis Franch and Berberine in Chronic Liver Disease Treatment
4.2. The Potential Side-Effects or Toxicity of Glycyrrhizin in Chronic Liver Disease Treatment
4.3. The Potential Side-Effects or Toxicity of Silymarine and Silybinin in Liver Disease Treatment
4.4. The Potential Side-Effects or Toxicity of Bupleurum Chinensis DC and Saikosaponins in Chronic Liver Disease Treatment
4.5. The Potential Side-Effects or Toxicity of Salvia Miltiorrhiza Bunge in Chronic Liver Disease Treatment
4.6. The Potential Side-Effects or Toxicity of Scutellaria Baicalensis Georgi in Chronic Liver Disease Treatment
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wood, N.J. Liver: Nonobese individuals in the developing world are at risk of nonalcoholic fatty liver and liver disease. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 357. [Google Scholar] [CrossRef] [PubMed]
- Vong, S.; Bell, B.P. Chronic liver disease mortality in the united states, 1990–1998. Hepatology 2004, 39, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Lazerow, S.K.; Abdi, M.S.; Lewis, J.H. Drug-induced liver disease 2004. Curr. Opin. Gastroenterol. 2005, 21, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Baig, N.A.; Herrine, S.K.; Rubin, R. Liver disease and diabetes mellitus. Clin. Lab. Med. 2001, 21, 193–207. [Google Scholar] [PubMed]
- Orman, E.S.; Odena, G.; Bataller, R. Alcoholic liver disease: Pathogenesis, management, and novel targets for therapy. J. Gastroenterol. Hepatol. 2013, 28, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.E. Treatment of chronic liver diseases with traditional chinese medicine. J. Gastroenterol. Hepatol. 2000, 15, E67–E70. [Google Scholar] [CrossRef] [PubMed]
- Dhiman, A.; Nanda, A.; Ahmad, S. A recent update in research on the antihepatotoxic potential of medicinal plants. J. Chin. Integr. Med. 2012, 10, 117–127. [Google Scholar] [CrossRef]
- Del Prete, A.; Scalera, A.; Iadevaia, M.D.; Miranda, A.; Zulli, C.; Gaeta, L.; Tuccillo, C.; Federico, A.; Loguercio, C. Herbal products: Benefits, limits, and applications in chronic liver disease. Evid. Based Complement. Altern. Med. eCAM 2012, 2012, 837939. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Wang, J.; He, X.; Zhao, Y.; Wang, J.; Zhang, P.; Zhu, Y.; Zhong, L.; Zheng, Q.; Xiao, X. Large dosage of chishao in formulae for cholestatic hepatitis: A systematic review and meta-analysis. Evid. Based Complement. Altern. Med. eCAM 2014, 2014, 328152. [Google Scholar] [CrossRef] [PubMed]
- Dunkelberg, J.C.; Berkley, E.M.; Thiel, K.W.; Leslie, K.K. Hepatitis b and c in pregnancy: A review and recommendations for care. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2014, 34, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Damgaard Sandahl, T. Alcoholic hepatitis. Dan. Med. J. 2014, 61, B4755. [Google Scholar] [PubMed]
- Ghabril, M.; Chalasani, N.; Bjornsson, E. Drug-induced liver injury: A clinical update. Curr. Opin. Gastroenterol. 2010, 26, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Krawitt, E.L. Clinical features and management of autoimmune hepatitis. World J. Gastroenterol. WJG 2008, 14, 3301–3305. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Pobre, P.; Gonzalez, C.; Paz, E.; Colina, F.; Castellano, G.; Munoz-Yague, T.; Rodriguez, S.; Yela, C.; Alvarez, V.; Solis-Herruzo, J. Chronic hepatitis c and autoimmune cholangitis: A case study and literature review. Dig. Dis. Sci. 2002, 47, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Bodenheimer, H.C., Jr.; Clain, D.J.; Min, A.D.; Theise, N.D. Hepatic lipogranulomas in patients with chronic liver disease: Association with hepatitis c and fatty liver disease. World J. Gastroenterol. WJG 2010, 16, 5065–5069. [Google Scholar] [CrossRef] [PubMed]
- Bartneck, M.; Warzecha, K.T.; Tacke, F. Therapeutic targeting of liver inflammation and fibrosis by nanomedicine. Hepatobil. Surg. Nutr. 2014, 3, 364–376. [Google Scholar]
- Lee, U.E.; Friedman, S.L. Mechanisms of hepatic fibrogenesis. Best Pract. Res. Clin. Gastroenterol. 2011, 25, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Tariq, Z.; Green, C.J.; Hodson, L. Are oxidative stress mechanisms the common denominator in the progression from hepatic steatosis towards non-alcoholic steatohepatitis (nash)? Liv. Int. Off. J. Int. Assoc. Study Liv. 2014, 34, e180–e190. [Google Scholar] [CrossRef] [PubMed]
- Lotersztajn, S.; Julien, B.; Teixeira-Clerc, F.; Grenard, P.; Mallat, A. Hepatic fibrosis: Molecular mechanisms and drug targets. Annu. Rev. Pharmacol. Toxicol. 2005, 45, 605–628. [Google Scholar] [CrossRef] [PubMed]
- Arenas, V.J.J.; Nieto, G.M.; Romero, D.R.; Tortajada, G.B.; Faus, F.V. Review of enteral drugs administration for viral diseases: Hiv, hbv and hcv. Farm. Hosp. Org. Off. Exp. Cient. Soc. Esp. Farm. Hosp. 2013, 37, 412–418. [Google Scholar]
- Babineaux, M.J.; Anand, B.S. General aspects of the treatment of alcoholic hepatitis. World J. Hepatol. 2011, 3, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Najera, O.; Velasco-Zamora, J.A.; Torre, A. Overlap syndromes of autoimmune hepatitis: Diagnosis and treatment. Rev. Gastroenterol. Mex. 2015, 80, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Kumada, H. Long-term treatment of chronic hepatitis c with glycyrrhizin [stronger neo-minophagen c (snmc)] for preventing liver cirrhosis and hepatocellular carcinoma. Oncology 2002, 62, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, Y.; Matsuura, T.; Aoyagi, H.; Matsuda, M.; Hmwe, S.S.; Date, T.; Watanabe, N.; Watashi, K.; Suzuki, R.; Ichinose, S.; et al. Antiviral activity of glycyrrhizin against hepatitis c virus in vitro. PLoS ONE 2013, 8, e68992. [Google Scholar] [CrossRef] [PubMed]
- Fujisawa, Y.; Sakamoto, M.; Matsushita, M.; Fujita, T.; Nishioka, K. Glycyrrhizin inhibits the lytic pathway of complement-possible mechanism of its anti-inflammatory effect on liver cells in viral hepatitis. Microbiol. Immunol. 2000, 44, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Akbar, F.; Hasebe, A.; Horiike, N.; Onji, M. Glycyrrhizin enhances interleukin-10 production by liver dendritic cells in mice with hepatitis. J. Gastroenterol. 2003, 38, 962–967. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Takenaka, K.; Shimomura, H.; Fujii, N.; Shinagawa, K.; Kiura, K.; Harada, M. Lamivudine and glycyrrhizin for treatment of chemotherapy-induced hepatitis b virus (hbv) hepatitis in a chronic hbv carrier with non-hodgkin lymphoma. Leuk. Lymphoma 2001, 41, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Van Rossum, T.G.; Vulto, A.G.; Hop, W.C.; Schalm, S.W. Glycyrrhizin-induced reduction of alt in european patients with chronic hepatitis c. Am. J. Gastroenterol. 2001, 96, 2432–2437. [Google Scholar] [CrossRef]
- Kidd, P.; Head, K. A review of the bioavailability and clinical efficacy of milk thistle phytosome: A silybin-phosphatidylcholine complex (siliphos). Altern. Med. Rev. J. Clin. Ther. 2005, 10, 193–203. [Google Scholar]
- Bonifaz, V.; Shan, Y.; Lambrecht, R.W.; Donohue, S.E.; Moschenross, D.; Bonkovsky, H.L. Effects of silymarin on hepatitis c virus and haem oxygenase-1 gene expression in human hepatoma cells. Liv. Int. Off. J. Int. Assoc. Study Liv. 2009, 29, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Wagoner, J.; Negash, A.; Kane, O.J.; Martinez, L.E.; Nahmias, Y.; Bourne, N.; Owen, D.M.; Grove, J.; Brimacombe, C.; McKeating, J.A.; et al. Multiple effects of silymarin on the hepatitis c virus lifecycle. Hepatology 2010, 51, 1912–1921. [Google Scholar] [CrossRef] [PubMed]
- Mayer, K.E.; Myers, R.P.; Lee, S.S. Silymarin treatment of viral hepatitis: A systematic review. J. Viral Hepat. 2005, 12, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Strickland, G.T.; Tanamly, M.D.; Tadros, F.; Labeeb, S.; Makld, H.; Nessim, D.; Mikhail, N.; Magder, L.S.; Afdhal, N.H.; Medhat, A.; et al. Two-year results of a randomised double-blinded trial evaluating silymarin for chronic hepatitis c. Dig. Liv. Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liv. 2005, 37, 542–543. [Google Scholar] [CrossRef] [PubMed]
- Adeyemo, O.; Doi, H.; Rajender Reddy, K.; Kaplan, D.E. Impact of oral silymarin on virus- and non-virus-specific t-cell responses in chronic hepatitis c infection. J. Viral Hepat. 2013, 20, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.; Liu, S.K.; Liu, X.Y.; Li, Z.J.; Li, B.; Zhou, Y.L.; Zhang, H.Y.; Li, Y.W. Meta-analysis: Silymarin and its combination therapy for the treatment of chronic hepatitis b. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2013, 32, 657–669. [Google Scholar] [CrossRef] [PubMed]
- Blaising, J.; Levy, P.L.; Gondeau, C.; Phelip, C.; Varbanov, M.; Teissier, E.; Ruggiero, F.; Polyak, S.J.; Oberlies, N.H.; Ivanovic, T.; et al. Silibinin inhibits hepatitis c virus entry into hepatocytes by hindering clathrin-dependent trafficking. Cell. Microbiol. 2013, 15, 1866–1882. [Google Scholar] [CrossRef] [PubMed]
- Buzzelli, G.; Moscarella, S.; Giusti, A.; Duchini, A.; Marena, C.; Lampertico, M. A pilot study on the liver protective effect of silybin-phosphatidylcholine complex (idb1016) in chronic active hepatitis. Int. J. Clin. Pharmacol. Ther. Toxicol. 1993, 31, 456–460. [Google Scholar] [PubMed]
- Liu, S.; Wei, W.; Li, Y.; Lin, X.; Shi, K.; Cao, X.; Zhou, M. In vitro and in vivo anti-hepatitis b virus activities of the lignan nirtetralin b isolated from phyllanthus niruri l. J. Ethnopharmacol. 2014, 157, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, D.; Hong, L.S.; Kuppan, N. Antimicrobial activity of crude methanolic extract from phyllanthus niruri. Nat. Prod. Commun. 2013, 8, 493–496. [Google Scholar] [PubMed]
- Manjrekar, A.P.; Jisha, V.; Bag, P.P.; Adhikary, B.; Pai, M.M.; Hegde, A.; Nandini, M. Effect of phyllanthus niruri linn. Treatment on liver, kidney and testes in ccl4 induced hepatotoxic rats. Indian J. Exp. Biol. 2008, 46, 514–520. [Google Scholar] [PubMed]
- Amin, Z.A.; Abdulla, M.A.; Ali, H.M.; Alshawsh, M.A.; Qadir, S.W. Assessment of in vitro antioxidant, antibacterial and immune activation potentials of aqueous and ethanol extracts of phyllanthus niruri. J. Sci. Food Agric. 2012, 92, 1874–1877. [Google Scholar] [CrossRef] [PubMed]
- Lam, W.Y.; Leung, K.T.; Law, P.T.; Lee, S.M.; Chan, H.L.; Fung, K.P.; Ooi, V.E.; Waye, M.M. Antiviral effect of phyllanthus nanus ethanolic extract against hepatitis b virus (hbv) by expression microarray analysis. J. Cell. Biochem. 2006, 97, 795–812. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Lin, H.; McIntosh, H. Genus phyllanthus for chronic hepatitis b virus infection: A systematic review. J. Viral Hepat. 2001, 8, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Li, C.; Kwok, S.T.; Zhang, Q.W.; Chan, S.W. A review of the pharmacological effects of the dried root of polygonum cuspidatum (hu zhang) and its constituents. Evid. Based Complement. Altern. Med. eCAM 2013, 2013, 208349. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Qin, R.; Li, X.; Zhou, H. Botany, phytochemistry, pharmacology, and potential application of polygonum cuspidatum sieb.Et zucc.: A review. J. Ethnopharmacol. 2013, 148, 729–745. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, G.; Hou, W.; Li, P.; Dulin, A.; Bonkovsky, H.L. Contemporary clinical research of traditional chinese medicines for chronic hepatitis b in china: An analytical review. Hepatology 2010, 51, 690–698. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.S.; Liu, H.W.; Wang, K.C.; Chen, M.C.; Chiang, L.C.; Hua, Y.C.; Lin, C.C. Ethanol extract of polygonum cuspidatum inhibits hepatitis b virus in a stable hbv-producing cell line. Antivir. Res. 2005, 66, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Cai, W.M.; Qin, C.J.; Miao, L.C.; Yun, L.T.; Hua, Y.; Weilin, L. Intervention of tlr4 signal pathway cytokines in severe liver injury with obstructive jaundice in rats. Int. J. Sports Med. 2012, 33, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.T.; Chuang, P.T.; Wu, C.Y.; Weng, Y.M.; Chen, W.; Tseng, C.Y. Antioxidative and in vitro hepatoprotective activity of bupleurum kaoi leaf infusion. Phytother. Res. PTR 2006, 20, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.C.; Ng, L.T.; Liu, L.T.; Shieh, D.E.; Lin, C.C. Cytotoxicity and anti-hepatitis b virus activities of saikosaponins from bupleurum species. Planta Med. 2003, 69, 705–709. [Google Scholar] [PubMed]
- Lin, L.T.; Chung, C.Y.; Hsu, W.C.; Chang, S.P.; Hung, T.C.; Shields, J.; Russell, R.S.; Lin, C.C.; Li, C.F.; Yen, M.H.; et al. Saikosaponin b2 is a naturally occurring terpenoid that efficiently inhibits hepatitis c virus entry. J. Hepatol. 2015, 62, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Yue, S.; Hu, B.; Wang, Z.; Yue, Z.; Wang, F.; Zhao, Y.; Yang, Z.; Shen, M. Salvia miltiorrhiza compounds protect the liver from acute injury by regulation of p38 and nfkappab signaling in kupffer cells. Pharm. Biol. 2014, 52, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, Y.; Xie, Y.; Gao, Y.; Ma, J.; Yuan, J.; Li, J.; Wang, J.; Li, L.; Zhang, J.; et al. Multitargeted inhibition of hepatic fibrosis in chronic iron-overloaded mice by salvia miltiorrhiza. J. Ethnopharmacol. 2013, 148, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.J.; Li, Q.; Wang, J.B.; Zhao, Y.L.; Zhong, Y.W.; Bai, Y.F.; Wang, R.L.; Li, J.Y.; Yang, H.Y.; Zeng, L.N.; et al. Combining oxymatrine or matrine with lamivudine increased its antireplication effect against the hepatitis b virus in vitro. Evid. Based Complement. Altern. Med. eCAM 2013, 2013, 186573. [Google Scholar]
- Suo, Z.; Liu, Y.; Ferreri, M.; Zhang, T.; Liu, Z.; Mu, X.; Han, B. Impact of matrine on inflammation related factors in rat intestinal microvascular endothelial cells. J. Ethnopharmacol. 2009, 125, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Yao, N.; Wang, X. In vitro immunomodulatory activity of oxymatrine on toll-like receptor 9 signal pathway in chronic hepatitis b. Am. J. Chin. Med. 2014, 42, 1399–1410. [Google Scholar] [CrossRef] [PubMed]
- Wan, J.; Zhu, Y.N.; Feng, J.Q.; Chen, H.J.; Zhang, R.J.; Ni, J.; Chen, Z.H.; Hou, L.F.; Liu, Q.F.; Zhang, J.; et al. Periplocoside a, a pregnane glycoside from periploca sepium bge, prevents concanavalin a-induced mice hepatitis through inhibiting nkt-derived inflammatory cytokine productions. Int. Immunopharmacol. 2008, 8, 1248–1256. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ni, J.; Chen, Z.H.; Li, X.; Zhang, R.J.; Tang, W.; Zhao, W.M.; Yang, Y.F.; Zuo, J.P. Periplocoside a prevents experimental autoimmune encephalomyelitis by suppressing il-17 production and inhibits differentiation of th17 cells. Acta Pharmacol. Sin. 2009, 30, 1144–1152. [Google Scholar] [CrossRef] [PubMed]
- Ai, Z.L.; Zhang, W.S.; Yao, S.K.; Xie, B.S.; Gao, C. [effect of baicalin on liver fatty acid binding protein in oxidative stress model in vitro]. Chin. J. Hepatol. 2011, 19, 927–931. [Google Scholar]
- Kim, S.J.; Moon, Y.J.; Lee, S.M. Protective effects of baicalin against ischemia/reperfusion injury in rat liver. J. Nat. Prod. 2010, 73, 2003–2008. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, H.; Gao, Z.; Xu, H. Effects of dietary baicalin supplementation on iron overload-induced mouse liver oxidative injury. Eur. J. Pharmacol. 2005, 509, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.L.; Wang, Y.J.; Zhang, Q.Y.; Liu, B.; Wang, F.Y.; Li, J.J.; Zhu, R.Z. Hepatoprotective effects of baicalein against ccl(4)-induced acute liver injury in mice. World J. Gastroenterol. WJG 2012, 18, 6605–6613. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.L.; Lian, L.H.; Wan, Y.; Nan, J.X. Baicalein inhibits nuclear factor-kappab and apoptosis via c-flip and mapk in d-galn/lps induced acute liver failure in murine models. Chem. Biol. Interact. 2010, 188, 526–534. [Google Scholar] [CrossRef] [PubMed]
- Yim, S.Y.; Lee, Y.J.; Lee, Y.K.; Jung, S.E.; Kim, J.H.; Kim, H.J.; Son, B.G.; Park, Y.H.; Lee, Y.G.; Choi, Y.W.; et al. Gomisin n isolated from schisandra chinensis significantly induces anti-proliferative and pro-apoptotic effects in hepatic carcinoma. Mol. Med. Rep. 2009, 2, 725–732. [Google Scholar] [PubMed]
- Xue, Y.; Li, X.; Du, X.; Li, X.; Wang, W.; Yang, J.; Chen, J.; Pu, J.; Sun, H. Isolation and anti-hepatitis b virus activity of dibenzocyclooctadiene lignans from the fruits of schisandra chinensis. Phytochemistry 2015, 116, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Checker, R.; Patwardhan, R.S.; Sharma, D.; Menon, J.; Thoh, M.; Bhilwade, H.N.; Konishi, T.; Sandur, S.K. Schisandrin b exhibits anti-inflammatory activity through modulation of the redox-sensitive transcription factors nrf2 and nf-kappab. Free Radic. Biol. Med. 2012, 53, 1421–1430. [Google Scholar] [CrossRef] [PubMed]
- Cai, L.; Cao, B.; Lin, D. Effects of traditional chinese medicine huangqi injection (radix astragali) on random skin flap survival in rats. J. Reconstr. Microsurg. 2015, 31, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.Z.; Liu, J.; Guo, B.L.; Zhao, Z.Z.; Hong, H.; Chen, H.B.; Cai, S.Q. Microscopic research on a multi-source traditional chinese medicine, astragali radix. J. Nat. Med. 2014, 68, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Liu, Z.J.; Chen, T.; Zhao, D. Pharmaceutical properties of calycosin, the major bioactive isoflavonoid in the dry root extract of radix astragali. Pharm. Biol. 2014, 52, 1217–1222. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.Y. [progress in pharmacological research on radix astragali]. Chin. J. Mod. Dev. Tradit. Med. 1991, 11, 312–314. [Google Scholar]
- Tang, L.L.; Sheng, J.F.; Xu, C.H.; Liu, K.Z. Clinical and experimental effectiveness of astragali compound in the treatment of chronic viral hepatitis b. J. Int. Med. Res. 2009, 37, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Li, J.; Huang, H.; Gao, W.; Zhuang, C.; Li, B.; Zhou, P.; Kong, D. Anti-hepatitis b virus activities of astragaloside iv isolated from radix astragali. Biol. Pharm. Bull. 2009, 32, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Bobe, G.; Young, J.W.; Beitz, D.C. Invited review: Pathology, etiology, prevention, and treatment of fatty liver in dairy cows. J. Dairy Sci. 2004, 87, 3105–3124. [Google Scholar] [CrossRef]
- Bellentani, S.; Bedogni, G.; Miglioli, L.; Tiribelli, C. The epidemiology of fatty liver. Eur. J. Gastroenterol. Hepatol. 2004, 16, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Miglioli, L.; Masutti, F.; Tiribelli, C.; Marchesini, G.; Bellentani, S. Prevalence of and risk factors for nonalcoholic fatty liver disease: The dionysos nutrition and liver study. Hepatology 2005, 42, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Levene, A.P.; Goldin, R.D. The epidemiology, pathogenesis and histopathology of fatty liver disease. Histopathology 2012, 61, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Yeh, M.M.; Brunt, E.M. Pathological features of fatty liver disease. Gastroenterology 2014, 147, 754–764. [Google Scholar] [CrossRef] [PubMed]
- Park, K.S.; Lee, Y.S.; Park, H.W.; Seo, S.H.; Jang, B.G.; Hwang, J.Y.; Cho, K.B.; Hwang, J.S.; Ahn, S.H.; Kang, Y.N.; et al. Factors associated or related to with pathological severity of nonalcoholic fatty liver disease. Korean J. Intern. Med. 2004, 19, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Corrado, R.L.; Torres, D.M.; Harrison, S.A. Review of treatment options for nonalcoholic fatty liver disease. Med. Clin. N. Am. 2014, 98, 55–72. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M. Review article: Current management of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2008, 28, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.; Chen, Y.Y.; Bei, W.J.; Wang, L.Y.; Chen, B.T.; Guo, J. In vitro screening for antihepatic steatosis active components within coptidis rhizoma alkaloids extract using liver cell extraction with hplc analysis and a free fatty acid-induced hepatic steatosis hepg2 cell assay. Evid. Based Complement. Altern. Med. eCAM 2013, 2013, 459390. [Google Scholar]
- Xing, L.J.; Zhang, L.; Liu, T.; Hua, Y.Q.; Zheng, P.Y.; Ji, G. Berberine reducing insulin resistance by up-regulating irs-2 mrna expression in nonalcoholic fatty liver disease (nafld) rat liver. Eur. J. Pharmacol. 2011, 668, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Xue, M.; Zhang, L.; Yang, M.X.; Zhang, W.; Li, X.M.; Ou, Z.M.; Li, Z.P.; Liu, S.H.; Li, X.J.; Yang, S.Y. Berberine-loaded solid lipid nanoparticles are concentrated in the liver and ameliorate hepatosteatosis in db/db mice. Int. J. Nanomed. 2015, 10, 5049–5057. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, F.; Wang, Y.; Ma, X.; Zhao, M.; Zhao, C. Metabonomics study of the therapeutic mechanism of gynostemma pentaphyllum and atorvastatin for hyperlipidemia in rats. PLoS ONE 2013, 8, e78731. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.; Gardemann, A.; Keilhoff, G.; Peter, D.; Wiswedel, I.; Schild, L. Prevention of free fatty acid-induced lipid accumulation, oxidative stress, and cell death in primary hepatocyte cultures by a gynostemma pentaphyllum extract. Phytomed. Int. J. Phytother. Phytopharmacol. 2012, 19, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Chou, S.C.; Chen, K.W.; Hwang, J.S.; Lu, W.T.; Chu, Y.Y.; Lin, J.D.; Chang, H.J.; See, L.C. The add-on effects of gynostemma pentaphyllum on nonalcoholic fatty liver disease. Altern. Ther. Health Med. 2006, 12, 34–39. [Google Scholar] [PubMed]
- Malek, M.A.; Hoang, M.H.; Jia, Y.; Lee, J.H.; Jun, H.J.; Lee, D.H.; Lee, H.J.; Lee, C.; Lee, M.K.; Hwang, B.Y.; et al. Ombuin-3-o-beta-d-glucopyranoside from gynostemma pentaphyllum is a dual agonistic ligand of peroxisome proliferator-activated receptors α and δ/β. Biochem. Biophys. Res. Commun. 2013, 430, 1322–1328. [Google Scholar] [CrossRef] [PubMed]
- Ding, R.B.; Tian, K.; Cao, Y.W.; Bao, J.L.; Wang, M.; He, C.; Hu, Y.; Su, H.; Wan, J.B. Protective effect of panax notoginseng saponins on acute ethanol-induced liver injury is associated with ameliorating hepatic lipid accumulation and reducing ethanol-mediated oxidative stress. J. Agric. Food Chem. 2015, 63, 2413–2422. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Liao, M.; Yang, Z.; Guo, J.; Gao, Q. [effect of panax notoginseng on genes expression of cyp and gst in liver tissues of rats]. China J. Chin. Mater. Med. 2009, 34, 2390–2393. [Google Scholar]
- Shi, K.Q.; Fan, Y.C.; Liu, W.Y.; Li, L.F.; Chen, Y.P.; Zheng, M.H. Traditional chinese medicines benefit to nonalcoholic fatty liver disease: A systematic review and meta-analysis. Mol. Biol. Rep. 2012, 39, 9715–9722. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Li, S.; Dong, Y.; Zhu, R.; Liu, Y. Antioxidant activity of penta-oligogalacturonide, isolated from haw pectin, suppresses triglyceride synthesis in mice fed with a high-fat diet. Food Chem. 2014, 145, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Li, T.P.; Zhu, R.G.; Dong, Y.P.; Liu, Y.H.; Li, S.H.; Chen, G. Effects of pectin pentaoligosaccharide from hawthorn ( crataegus pinnatifida bunge. Var. Major) on the activity and mrna levels of enzymes involved in fatty acid oxidation in the liver of mice fed a high-fat diet. J. Agric. Food Chem. 2013, 61, 7599–7605. [Google Scholar] [PubMed]
- Liu, M.; Xu, L.; Yin, L.; Qi, Y.; Xu, Y.; Han, X.; Zhao, Y.; Sun, H.; Yao, J.; Lin, Y.; et al. Potent effects of dioscin against obesity in mice. Sci. Rep. 2015, 5, 7973. [Google Scholar] [PubMed]
- Xu, T.; Zheng, L.; Xu, L.; Yin, L.; Qi, Y.; Xu, Y.; Han, X.; Peng, J. Protective effects of dioscin against alcohol-induced liver injury. Arch. Toxicol. 2014, 88, 739–753. [Google Scholar] [PubMed]
- Chao, J.; Huo, T.I.; Cheng, H.Y.; Tsai, J.C.; Liao, J.W.; Lee, M.S.; Qin, X.M.; Hsieh, M.T.; Pao, L.H.; Peng, W.H. Gallic acid ameliorated impaired glucose and lipid homeostasis in high fat diet-induced nafld mice. PLoS ONE 2014, 9, e96969. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.L.; Yen, G.C. Effect of gallic acid on high fat diet-induced dyslipidaemia, hepatosteatosis and oxidative stress in rats. Br. J. Nutr. 2007, 98, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.J.; Wei, S.L.; Wang, H.C.; Liu, X.Y.; Wan, H.J.; Yi, X.R.; Yuan, Y.C.; Kong, X.P. [therapeutic effects of compound glycyrrhizin liposome on fibrosis of the rats with nonalcoholic steatohepatitis]. Chin. J. Hepatol. 2009, 17, 877–878. [Google Scholar]
- Korenaga, M.; Hidaka, I.; Nishina, S.; Sakai, A.; Shinozaki, A.; Gondo, T.; Furutani, T.; Kawano, H.; Sakaida, I.; Hino, K. A glycyrrhizin-containing preparation reduces hepatic steatosis induced by hepatitis c virus protein and iron in mice. Liv. Int. Off. J. Int. Assoc. Study Liv. 2011, 31, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Feher, J.; Lengyel, G. Silymarin in the treatment of chronic liver diseases: Past and future. Orv. Hetil. 2008, 149, 2413–2418. [Google Scholar] [CrossRef] [PubMed]
- Serviddio, G.; Bellanti, F.; Giudetti, A.M.; Gnoni, G.V.; Petrella, A.; Tamborra, R.; Romano, A.D.; Rollo, T.; Vendemiale, G.; Altomare, E. A silybin-phospholipid complex prevents mitochondrial dysfunction in a rodent model of nonalcoholic steatohepatitis. J. Pharmacol. Exp.Ther. 2010, 332, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Loguercio, C.; Federico, A.; Trappoliere, M.; Tuccillo, C.; de Sio, I.; di Leva, A.; Niosi, M.; D'Auria, M.V.; Capasso, R.; Del Vecchio Blanco, C.; et al. The effect of a silybin-vitamin e-phospholipid complex on nonalcoholic fatty liver disease: A pilot study. Dig. Dis. Sci. 2007, 52, 2387–2395. [Google Scholar] [CrossRef] [PubMed]
- Shtroblia, A.L.; Fira, L.S.; Likhatskii, P.G.; Pyla, V.P.; Vashkeba, E.M.; Medvid, II. Studying of hepatoprotective properties of dry extract from apricot leaves on the model of liver lesion by tetrachloromethane. V. Ross. Akad. Med. Nauk Ross. 2013, 3, 68–72. [Google Scholar]
- Ozturk, F.; Gul, M.; Ates, B.; Ozturk, I.C.; Cetin, A.; Vardi, N.; Otlu, A.; Yilmaz, I. Protective effect of apricot (prunus armeniaca l.) on hepatic steatosis and damage induced by carbon tetrachloride in wistar rats. Br. J. Nutr. 2009, 102, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Hokari, A.; Ishikawa, T.; Tajiri, H.; Matsuda, T.; Ishii, O.; Matsumoto, N.; Okuse, C.; Takahashi, H.; Kurihara, T.; Kawahara, K.; et al. Efficacy of mk615 for the treatment of patients with liver disorders. World J. Gastroenterol. WJG 2012, 18, 4118–4126. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.H.; Luo, Y.H.; Liang, J.C.; Huang, Y.K. Baicalin regulates lipid metabolism in high-fat feeding sd rat liver and the mechanism involves modulation of ampk-alpha pathway. Chin. J. Hepatol. 2010, 18, 711–712. [Google Scholar]
- Guo, H.X.; Liu, D.H.; Ma, Y.; Liu, J.F.; Wang, Y.; Du, Z.Y.; Wang, X.; Shen, J.K.; Peng, H.L. Long-term baicalin administration ameliorates metabolic disorders and hepatic steatosis in rats given a high-fat diet. Acta Pharmacol. Sin. 2009, 30, 1505–1512. [Google Scholar] [PubMed]
- Xi, Y.; Wu, M.; Li, H.; Dong, S.; Luo, E.; Gu, M.; Shen, X.; Jiang, Y.; Liu, Y.; Liu, H. Baicalin attenuates high fat diet-induced obesity and liver dysfunction: Dose-response and potential role of camkkbeta/ampk/acc pathway. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2015, 35, 2349–2359. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Lee, S.M. Effect of baicalin on toll-like receptor 4-mediated ischemia/reperfusion inflammatory responses in alcoholic fatty liver condition. Toxicol. Appl. Pharmacol. 2012, 258, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Sivanathan, V.; Kittner, J.M.; Sprinzl, M.F.; Weinmann, A.; Koch, S.; Wiltink, J.; Nguyen-Tat, M.; Marquardt, J.U.; Worns, M.A.; Zimmermann, T.; et al. Etiology and complications of liver cirrhosis: Data from a german centre. Dtsch. Med. Wochenschr. 2014, 139, 1758–1762. [Google Scholar] [PubMed]
- Wang, X.; Lin, S.X.; Tao, J.; Wei, X.Q.; Liu, Y.T.; Chen, Y.M.; Wu, B. Study of liver cirrhosis over ten consecutive years in southern china. World J. Gastroenterol. WJG 2014, 20, 13546–13555. [Google Scholar] [CrossRef] [PubMed]
- Mokdad, A.A.; Lopez, A.D.; Shahraz, S.; Lozano, R.; Mokdad, A.H.; Stanaway, J.; Murray, C.J.; Naghavi, M. Liver cirrhosis mortality in 187 countries between 1980 and 2010: A systematic analysis. BMC Med. 2014, 12, 145. [Google Scholar] [CrossRef] [PubMed]
- Pruszczynski, A. Histogenesis and pathological anatomy of liver cirrhosis. Pol. Arch. Med. Wewn. 1962, 32, 1379–1388. [Google Scholar] [PubMed]
- Bataller, R.; Schwabe, R.F.; Choi, Y.H.; Yang, L.; Paik, Y.H.; Lindquist, J.; Qian, T.; Schoonhoven, R.; Hagedorn, C.H.; Lemasters, J.J.; et al. Nadph oxidase signal transduces angiotensin ii in hepatic stellate cells and is critical in hepatic fibrosis. J. Clin. Investig. 2003, 112, 1383–1394. [Google Scholar] [CrossRef] [PubMed]
- Marra, F.; Arrighi, M.C.; Fazi, M.; Caligiuri, A.; Pinzani, M.; Romanelli, R.G.; Efsen, E.; Laffi, G.; Gentilini, P. Extracellular signal-regulated kinase activation differentially regulates platelet-derived growth factor's actions in hepatic stellate cells, and is induced by in vivo liver injury in the rat. Hepatology 1999, 30, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Schnabl, B.; Kweon, Y.O.; Frederick, J.P.; Wang, X.F.; Rippe, R.A.; Brenner, D.A. The role of smad3 in mediating mouse hepatic stellate cell activation. Hepatology 2001, 34, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Marra, F.; Efsen, E.; Romanelli, R.G.; Caligiuri, A.; Pastacaldi, S.; Batignani, G.; Bonacchi, A.; Caporale, R.; Laffi, G.; Pinzani, M.; et al. Ligands of peroxisome proliferator-activated receptor gamma modulate profibrogenic and proinflammatory actions in hepatic stellate cells. Gastroenterology 2000, 119, 466–478. [Google Scholar] [CrossRef] [PubMed]
- Paik, Y.H.; Schwabe, R.F.; Bataller, R.; Russo, M.P.; Jobin, C.; Brenner, D.A. Toll-like receptor 4 mediates inflammatory signaling by bacterial lipopolysaccharide in human hepatic stellate cells. Hepatology 2003, 37, 1043–1055. [Google Scholar] [CrossRef] [PubMed]
- Boya, P.; Larrea, E.; Sola, I.; Majano, P.L.; Jimenez, C.; Civeira, M.P.; Prieto, J. Nuclear factor- κb in the liver of patients with chronic hepatitis c: Decreased rela expression is associated with enhanced fibrosis progression. Hepatology 2001, 34, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Fialla, A.D.; Israelsen, M.; Hamberg, O.; Krag, A.; Gluud, L.L. Nutritional therapy in cirrhosis or alcoholic hepatitis: A systematic review and meta-analysis. Liv. Int. Off. J. Int. Assoc. Study Liv. 2015, 35, 2072–2078. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Wang, N.; Ye, X.; Li, H.; Feng, Y.; Cheung, F.; Nagamatsu, T. Hepatoprotective effect and its possible mechanism of coptidis rhizoma aqueous extract on carbon tetrachloride-induced chronic liver hepatotoxicity in rats. J. Ethnopharmacol. 2011, 138, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Feng, Y.; Tong, Y.; Ng, K.M.; Tsao, S.; Lau, G.K.; Sze, C.; Zhang, Y.; Tang, J.; Shen, J.; et al. Hepatoprotective effects of coptidis rhizoma aqueous extract on carbon tetrachloride-induced acute liver hepatotoxicity in rats. J. Ethnopharmacol. 2009, 124, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.J.; Xu, D.; Guo, Y.; Ping, J.; Chen, L.B.; Wang, H. Protection by and anti-oxidant mechanism of berberine against rat liver fibrosis induced by multiple hepatotoxic factors. Clin. Exp. Pharmacol. Physiol. 2008, 35, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Pan, Y.; Kan, M.; Xiao, X.; Wang, Y.; Guan, F.; Zhang, X.; Chen, L. Hepatoprotective effects of berberine on liver fibrosis via activation of amp-activated protein kinase. Life Sci. 2014, 98, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Feng, Y.; Cheung, F.; Chow, O.Y.; Wang, X.; Su, W.; Tong, Y. A comparative study on the hepatoprotective action of bear bile and coptidis rhizoma aqueous extract on experimental liver fibrosis in rats. BMC Complement. Altern. Med. 2012, 12, 239. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Xu, L.; He, Q.; Liang, T.; Duan, X.; Li, R. Anti-fibrotic effects of puerarin on ccl4-induced hepatic fibrosis in rats possibly through the regulation of ppar-gamma expression and inhibition of pi3k/akt pathway. Food Chem. Toxicol. An Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2013, 56, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Xu, L.; Liang, T.; Li, Y.; Zhang, S.; Duan, X. Puerarin mediates hepatoprotection against ccl4-induced hepatic fibrosis rats through attenuation of inflammation response and amelioration of metabolic function. Food Chem. Toxicol. An Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2013, 52, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Ji, G.; Liu, J. Reversal of chemical-induced liver fibrosis in wistar rats by puerarin. J. Nutr. Biochem. 2006, 17, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Kwon, R.H.; Ha, B.J. Protection of saururus chinensis extract against liver oxidative stress in rats of triton wr-1339-induced hyperlipidemia. Toxicol. Res. 2014, 30, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Hong, T.G.; Jin, M.; Yang, J.H.; Suh, S.J.; Piao, D.G.; Ko, H.K.; Seo, C.S.; Chang, Y.C.; Kim, C.H.; et al. Saucerneol g, a new lignan, from saururus chinensis inhibits matrix metalloproteinase-9 induction via a nuclear factor kappab and mitogen activated protein kinases in lipopolysaccharide-stimulated raw264.7 cells. Biol. Pharm. Bull. 2010, 33, 1944–1948. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Cheng, D.; Wang, H.; di, L.; Zhou, X.; Xu, T.; Yang, X.; Liu, Y. The hepatoprotective and antifibrotic effects of saururus chinensis against carbon tetrachloride induced hepatic fibrosis in rats. J. Ethnopharmacol. 2009, 126, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Guo, J.; Liu, S. [inhibitory effect of glycyrrhizin on nf-kappa b binding activity in ccl4 plus ethanol induced liver cirrhosis in rats]. Chin. J. Hepatol. 1999, 7, 42–43. [Google Scholar]
- Qu, Y.; Zong, L.; Xu, M.; Dong, Y.; Lu, L. Effects of 18alpha-glycyrrhizin on tgf-beta1/smad signaling pathway in rats with carbon tetrachloride-induced liver fibrosis. Int. J. Clin. Exp. Pathol. 2015, 8, 1292–1301. [Google Scholar] [PubMed]
- Manns, M.P.; Wedemeyer, H.; Singer, A.; Khomutjanskaja, N.; Dienes, H.P.; Roskams, T.; Goldin, R.; Hehnke, U.; Inoue, H.; European, S.S.G. Glycyrrhizin in patients who failed previous interferon alpha-based therapies: Biochemical and histological effects after 52 weeks. J. Viral Hepat. 2012, 19, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Serviddio, G.; Bellanti, F.; Stanca, E.; Lunetti, P.; Blonda, M.; Tamborra, R.; Siculella, L.; Vendemiale, G.; Capobianco, L.; Giudetti, A.M. Silybin exerts antioxidant effects and induces mitochondrial biogenesis in liver of rat with secondary biliary cirrhosis. Free Radic.Biol. Med. 2014, 73, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Stanca, E.; Serviddio, G.; Bellanti, F.; Vendemiale, G.; Siculella, L.; Giudetti, A.M. Down-regulation of lpcat expression increases platelet-activating factor level in cirrhotic rat liver: Potential antiinflammatory effect of silybin. Biochim. Biophys. Acta 2013, 1832, 2019–2026. [Google Scholar] [CrossRef] [PubMed]
- Seeff, L.B.; Curto, T.M.; Szabo, G.; Everson, G.T.; Bonkovsky, H.L.; Dienstag, J.L.; Shiffman, M.L.; Lindsay, K.L.; Lok, A.S.; Di Bisceglie, A.M.; et al. Herbal product use by persons enrolled in the hepatitis c antiviral long-term treatment against cirrhosis (halt-c) trial. Hepatology 2008, 47, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Pares, A.; Planas, R.; Torres, M.; Caballeria, J.; Viver, J.M.; Acero, D.; Panes, J.; Rigau, J.; Santos, J.; Rodes, J. Effects of silymarin in alcoholic patients with cirrhosis of the liver: Results of a controlled, double-blind, randomized and multicenter trial. J. Hepatol. 1998, 28, 615–621. [Google Scholar] [CrossRef]
- Yen, M.H.; Weng, T.C.; Liu, S.Y.; Chai, C.Y.; Lin, C.C. The hepatoprotective effect of bupleurum kaoi, an endemic plant to taiwan, against dimethylnitrosamine-induced hepatic fibrosis in rats. Biol. Pharm. Bull. 2005, 28, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, Q.; Burczynski, F.J.; Kong, W.; Gong, Y. Saikosaponin a of bupleurum chinense (chaihu) elevates bone morphogenetic protein 4 (bmp-4) during hepatic stellate cell activation. Phytomed. Int. J. Phytother. Phytopharm. 2013, 20, 1330–1335. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.Q.; Han, D.W.; Ma, X.H.; Zhao, Y.C.; Yin, L.; Li, C.M. Preventive and therapeutic actions of glycyrrhizin, glycyrrhetic acid and crude saikosides on experimental liver cirrhosis in rats. Acta Pharm. Sin. 1983, 18, 325–331. [Google Scholar]
- Wu, S.J.; Lin, Y.H.; Chu, C.C.; Tsai, Y.H.; Chao, J.C. Curcumin or saikosaponin a improves hepatic antioxidant capacity and protects against ccl4-induced liver injury in rats. J. Med. Food 2008, 11, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Parajuli, D.R.; Zhao, Y.Z.; Jin, H.; Chi, J.H.; Li, S.Y.; Kim, Y.C.; Sohn, D.H.; Lee, S.H. Anti-fibrotic effect of pf2401-sf, a standardized fraction of salvia miltiorrhiza, in thioacetamide-induced experimental rats liver fibrosis. Arch. Pharm. Res. 2015, 38, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Xiping, Z.; Jie, Z.; Shuyun, Y.; Qili, W.; Guanghua, F.; Yan, P. Influence of salvia miltiorrhizae on the mesenteric lymph node of rats with severe acute pancreatitis or obstructive jaundice. Med. Inflamm. 2009, 2009, 675195. [Google Scholar]
- Nan, J.X.; Park, E.J.; Kim, Y.C.; Ko, G.; Sohn, D.H. Scutellaria baicalensis inhibits liver fibrosis induced by bile duct ligation or carbon tetrachloride in rats. J. Pharm. Pharmacol. 2002, 54, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Pan, T.L.; Wang, P.W.; Leu, Y.L.; Wu, T.H.; Wu, T.S. Inhibitory effects of scutellaria baicalensis extract on hepatic stellate cells through inducing g2/m cell cycle arrest and activating erk-dependent apoptosis via bax and caspase pathway. J. Ethnopharmacol. 2012, 139, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.F.; Zhou, S.Z.; Cheng, X.Y.; Yi, B.; Shan, S.Z.; Wang, J.; Li, Q.F. Baicalein attenuates hypertrophic scar formation via inhibiting tgf-beta/smad2/3 signaling pathway. Br. J. Dermatol. 2015. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Che, Q.M.; Zhao, X.; Pu, X.P. Antifibrotic effects of chronic baicalein administration in a ccl4 liver fibrosis model in rats. Eur. J. Pharmacol. 2010, 631, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Prasad, V.; Goldstein, J.A. Us news and world report cancer hospital rankings: Do they reflect measures of research productivity? PLoS ONE 2014, 9, e107803. [Google Scholar] [CrossRef] [PubMed]
- Ni, Y.Q.; Zhao, H.R.; Mao, R.; Zhang, H.; Wen, H.; Xiao, L.; Tursun, A.; Bao, Y.X. Clinical epidemiological analysis of 3602 cases of primary liver cancer in xinjiang. Chin. J. Oncol. 2012, 34, 374–377. [Google Scholar]
- La Vecchia, C.; Negri, E. A review of epidemiological data on epilepsy, phenobarbital, and risk of liver cancer. Eur. J. Cancer Prev. Off. J. Eur. Cancer Prev. Organ. 2014, 23, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.Y.; Huang, T.R.; Yu, J.H.; Zhang, Z.Q.; Li, J.L.; Deng, W.; Ye, S.Y.; Zhou, D.N.; He, Z.F. Epidemiological analysis of primary liver cancer in the early 21st century in guangxi province of china. Chin. J. Cancer 2010, 29, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Deugnier, Y.M.; Guyader, D.; Crantock, L.; Lopez, J.M.; Turlin, B.; Yaouanq, J.; Jouanolle, H.; Campion, J.P.; Launois, B.; Halliday, J.W.; et al. Primary liver cancer in genetic hemochromatosis: A clinical, pathological, and pathogenetic study of 54 cases. Gastroenterology 1993, 104, 228–234. [Google Scholar] [PubMed]
- Safrany, L.; Balazs, M.; Marton, I. Primary liver cancer. Clinical and pathological study of 74 cases. Orv. Hetil. 1969, 110, 457–463. [Google Scholar] [PubMed]
- Zuo, C.; Xia, M.; Wu, Q.; Zhu, H.; Liu, J.; Liu, C. Role of antiviral therapy in reducing recurrence and improving survival in hepatitis b virus-associated hepatocellular carcinoma following curative resection (review). Oncol. Lett. 2015, 9, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Ricci, S.; Mazzaferro, V.; Hilgard, P.; Gane, E.; Blanc, J.F.; de Oliveira, A.C.; Santoro, A.; Raoul, J.L.; Forner, A.; et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008, 359, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.Y.; Wang, N.; Tsao, S.W.; Zhang, Z.; Feng, Y. Suppression of vascular endothelial growth factor via inactivation of eukaryotic elongation factor 2 by alkaloids in coptidis rhizoma in hepatocellular carcinoma. Integr. Cancer Ther. 2014, 13, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Zhu, M.; Wang, X.; Tan, H.Y.; Tsao, S.W.; Feng, Y. Berberine-induced tumor suppressor p53 up-regulation gets involved in the regulatory network of mir-23a in hepatocellular carcinoma. Biochim. Biophys. Acta 2014, 1839, 849–857. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Wang, N.; Tsao, S.W.; Yuen, M.F.; Feng, Y.; Wan, T.S.; Man, K.; Feng, Y. Up-regulation of micrornas, mir21 and mir23a in human liver cancer cells treated with coptidis rhizoma aqueous extract. Exp. Ther. Med. 2011, 2, 27–32. [Google Scholar] [PubMed]
- Wang, N.; Feng, Y.; Lau, E.P.; Tsang, C.; Ching, Y.; Man, K.; Tong, Y.; Nagamatsu, T.; Su, W.; Tsao, S. F-actin reorganization and inactivation of rho signaling pathway involved in the inhibitory effect of coptidis rhizoma on hepatoma cell migration. Integr. Cancer Ther. 2010, 9, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Feng, Y.; Zhu, M.; Tsang, C.M.; Man, K.; Tong, Y.; Tsao, S.W. Berberine induces autophagic cell death and mitochondrial apoptosis in liver cancer cells: The cellular mechanism. J. Cell. Biochem. 2010, 111, 1426–1436. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, R.; Sundaram, J.; Sattu, K.; Pandi, A.; Thiruvengadam, D. Dietary supplementation of silymarin is associated with decreased cell proliferation, increased apoptosis, and activation of detoxification system in hepatocellular carcinoma. Mol. Cell. Biochem. 2013, 377, 163–176. [Google Scholar] [CrossRef] [PubMed]
- Feher, J.; Lengyel, G. Silymarin in the prevention and treatment of liver diseases and primary liver cancer. Curr. Pharm. Biotechnol. 2012, 13, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, G.; Lo Muzio, L.; Elinos-Baez, C.M.; Jagan, S.; Augustine, T.A.; Kamaraj, S.; Anandakumar, P.; Devaki, T. Silymarin inhibited proliferation and induced apoptosis in hepatic cancer cells. Cell Prolif. 2009, 42, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.J.; Lee, Y.J.; Kim, B.M.; Kim, Y.J.; Woo, H.D.; Jeon, H.K.; Chung, H.W. Effect of bupleuri radix extracts on the toxicity of 5-fluorouracil in hepg2 hepatoma cells and normal human lymphocytes. Basic Clin. Pharmacol. Toxicol. 2008, 103, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.F.; Wang, X.J.; Kang, H.F.; Bai, M.H.; Guan, H.T.; Wang, Z.W.; Zan, Y.; Song, L.Q.; Min, W.L.; Lin, S.; et al. Saikosaponin-d enhances radiosensitivity of hepatoma cells under hypoxic conditions by inhibiting hypoxia-inducible factor-1alpha. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2014, 33, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Jia, X.; Dang, S.; Cheng, Y.; Zhang, X.; Li, M.; Li, Y.; Li, S. Effects of saikosaponin-d on syndecan-2, matrix metalloproteinases and tissue inhibitor of metalloproteinases-2 in rats with hepatocellular carcinoma. J. Tradit. Chin. Med. 2012, 32, 415–422. [Google Scholar] [CrossRef]
- Rui, W.; Xie, L.; Liu, X.; He, S.; Wu, C.; Zhang, X.; Zhang, L.; Yang, Y. Compound astragalus and salvia miltiorrhiza extract suppresses hepatocellular carcinoma progression by inhibiting fibrosis and pai-1 mrna transcription. J. Ethnopharmacol. 2014, 151, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.Y.; Cheung, C.C.; Liu, K.W.; Fung, K.P.; Wong, J.; Lai, P.B.; Yeung, J.H. Cytotoxic effects of tanshinones from salvia miltiorrhiza on doxorubicin-resistant human liver cancer cells. J. Nat. Prod. 2010, 73, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.Y.; Chiu, L.C.; Yeung, J.H. Cytotoxicity of major tanshinones isolated from danshen (salvia miltiorrhiza) on hepg2 cells in relation to glutathione perturbation. Food Chem. Toxicol. An Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2008, 46, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Sumiyoshi, M. Anti-tumor and anti-metastatic actions of wogonin isolated from scutellaria baicalensis roots through anti-lymphangiogenesis. Phytomed. Int. J. Phytother. Phytopharmacol. 2013, 20, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Ueng, Y.F.; Shyu, C.C.; Liu, T.Y.; Oda, Y.; Lin, Y.L.; Liao, J.F.; Chen, C.F. Protective effects of baicalein and wogonin against benzo[a]pyrene- and aflatoxin b(1)-induced genotoxicities. Biochem. Pharmacol. 2001, 62, 1653–1660. [Google Scholar] [CrossRef]
- Tian, J.; Wang, L.; Wang, L.; Ke, X. A wogonin-loaded glycyrrhetinic acid-modified liposome for hepatic targeting with anti-tumor effects. Drug Deliv. 2014, 21, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Zhang, J.; Hou, L.; Cui, X. The effect of beta-elemene on alpha-tubulin polymerization in human hepatoma hepg2 cells. Chin. J. Cancer Res. 2013, 25, 770–776. [Google Scholar] [PubMed]
- Bao, F.; Qiu, J.; Zhang, H. Potential role of beta-elemene on histone h1 in the h22 ascites hepatoma cell line. Mol. Med. Rep. 2012, 6, 185–190. [Google Scholar] [PubMed]
- Lau, F.Y.; Chui, C.H.; Gambari, R.; Kok, S.H.; Kan, K.L.; Cheng, G.Y.; Wong, R.S.; Teo, I.T.; Cheng, C.H.; Wan, T.S.; et al. Antiproliferative and apoptosis-inducing activity of brucea javanica extract on human carcinoma cells. Int. J. Mol. Med. 2005, 16, 1157–1162. [Google Scholar] [CrossRef] [PubMed]
- Yue, Y.; Yang, Y.; Shi, L.; Wang, Z. Suppression of human hepatocellular cancer cell proliferation by brucea javanica oil-loaded liposomes via induction of apoptosis. Arch. Med. Sci. 2015, 11, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Qiu, W.; Zhu, Q.; Zu, Y.; Deng, X.; Zhao, T.; Jiang, C.; Zhang, L. Camptothecin-20(s)-o-[n-(3'alpha,12'alpha-dihydroxy-24'-carbonyl-5'beta-cholan)]-lysine, a novel camptothecin analogue, induces apoptosis towards hepatocellular carcinoma smmc-7721 cells. Molecules 2011, 16, 7803–7814. [Google Scholar] [CrossRef] [PubMed]
- Jayasooriya, R.G.; Choi, Y.H.; Hyun, J.W.; Kim, G.Y. Camptothecin sensitizes human hepatoma hep3b cells to trail-mediated apoptosis via ros-dependent death receptor 5 upregulation with the involvement of mapks. Environ. Toxicol. Pharmacol. 2014, 38, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Li, X.; Chen, X.; Li, Z.; Liu, X.; Zhou, S.; Zhong, Q.; Yi, T.; Wei, Y.; Zhao, X.; et al. In vivo antitumor and antimetastatic activities of camptothecin encapsulated with n-trimethyl chitosan in a preclinical mouse model of liver cancer. Cancer Lett. 2010, 297, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Notarbartolo, M.; Poma, P.; Perri, D.; Dusonchet, L.; Cervello, M.; D'Alessandro, N. Antitumor effects of curcumin, alone or in combination with cisplatin or doxorubicin, on human hepatic cancer cells. Analysis of their possible relationship to changes in nf-kb activation levels and in iap gene expression. Cancer Lett. 2005, 224, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.Z.; Cheng, J.; Luo, J.; Zhuang, S.M. Abrogation of g2/m arrest sensitizes curcumin-resistant hepatoma cells to apoptosis. FEBS Lett. 2008, 582, 2689–2695. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.N.; Zhang, G.B.; Zhang, Y.Y.; Su, S.B. Clinical applications of omics technologies on zheng differentiation research in traditional chinese medicine. Evid. Based Complement. Altern. Med. eCAM 2013, 2013, 989618. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Shang, H.C. Correlation between traditional chinese medicine syndromes and omics: A literature review. J. Chin. Integr. Med. 2011, 9, 1286–1291. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, S.; Lee, M.Y.; Shin, H.K. Therapeutic effect of soshiho-tang, a traditional herbal formula, on liver fibrosis or cirrhosis in animal models: A systematic review and meta-analysis. J. Ethnopharmacol. 2014, 154, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Zhong, G.; Luo, Y.; Xiang, L.; Xie, Y.; Xie, Q.; Li, Y.; Zhang, C. Clinical efficacy study on calming liver and restraining yang formula in treating patients with mild or moderate degree of essential hypertension. China J. Chin. Mater. Med. 2010, 35, 776–781. [Google Scholar]
- Liu, W.; Zheng, J.; Xing, R. Clinical significance of a scoring formula of liver injury for the preoperative evaluation of patients with liver cirrhosis. Eur. J. Gastroenterol. Hepatol. 2014, 26, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Ma, X.; Zhou, C.; Zhao, J.; Guo, J.; Xu, W. Effect of fuzhenghuayu compound on hepatocyte expression of nrf2 in a mouse model of hepatic fibrosis. Chin. J. Hepatol. 2014, 22, 609–615. [Google Scholar]
- Song, Y.N.; Sun, J.J.; Lu, Y.Y.; Xu, L.M.; Gao, Y.Q.; Zhang, W.; Wang, X.S.; Xue, D.Y.; Zheng, Q.S.; Su, S.B. Therapeutic efficacy of fuzheng-huayu tablet based traditional chinese medicine syndrome differentiation on hepatitis-b-caused cirrhosis: A multicenter double-blind randomized controlled trail. Evid. Based Complement. Altern. Med. eCAM 2013, 2013, 709305. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.Q.; Mi, H.M.; Li, H.; Zhao, S.X.; Jia, Y.H.; Nan, Y.M. Modulation of ikkbeta/nf-kappab and tgf-beta1/smad via fuzheng huayu recipe involves in prevention of nutritional steatohepatitis and fibrosis in mice. Iran. J. Basic Med. Sci. 2015, 18, 404–411. [Google Scholar] [PubMed]
- Tang, C.L.; Zhou, Z.; Shi, W.Q. Effects of fuzheng huayu capsule on the ratio of tgf-beta1/bmp-7 of chronic viral hepatitis b fibrosis patients of gan-shen insufficiency blood-stasis obstruction syndrome. Chin. J. Integr. Tradit. West. Med. 2012, 32, 20–24. [Google Scholar]
- Liu, P.; Hu, Y.Y.; Liu, C.; Xu, L.M.; Liu, C.H.; Sun, K.W.; Hu, D.C.; Yin, Y.K.; Zhou, X.Q.; Wan, M.B.; et al. Multicenter clinical study on fuzhenghuayu capsule against liver fibrosis due to chronic hepatitis b. World J. Gastroenterol. WJG 2005, 11, 2892–2899. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Jiang, C.M.; Liu, C.H.; Liu, P.; Hu, Y.Y. Effect of fuzhenghuayu decoction on vascular endothelial growth factor secretion in hepatic stellate cells. Hepatobiliary Pancreat. Dis. Int. Hbpd Int 2002, 1, 207–210. [Google Scholar] [PubMed]
- Sato, A.; Toyoshima, M.; Kondo, A.; Ohta, K.; Sato, H.; Ohsumi, A. [pneumonitis induced by the herbal medicine sho-saiko-to in japan]. Nih. Kyobu Shikkan Gakkai Zasshi 1997, 35, 391–395. [Google Scholar]
- Chang, J.S.; Wang, K.C.; Liu, H.W.; Chen, M.C.; Chiang, L.C.; Lin, C.C. Sho-saiko-to (xiao-chai-hu-tang) and crude saikosaponins inhibit hepatitis b virus in a stable hbv-producing cell line. Am. J. Chin. Med. 2007, 35, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Tajiri, H.; Kozaiwa, K.; Ozaki, Y.; Miki, K.; Shimuzu, K.; Okada, S. Effect of sho-saiko-to(xiao-chai-hu-tang) on hbeag clearance in children with chronic hepatitis b virus infection and with sustained liver disease. Am. J. Chin. Med. 1991, 19, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Deng, G.; Kurtz, R.C.; Vickers, A.; Lau, N.; Yeung, K.S.; Shia, J.; Cassileth, B. A single arm phase ii study of a far-eastern traditional herbal formulation (sho-sai-ko-to or xiao-chai-hu-tang) in chronic hepatitis c patients. J. Ethnopharmacol. 2011, 136, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.H.; Chen, J.C.; Tsai, C.C.; Wang, W.C.; Chang, D.C.; Lin, C.C.; Hsieh, H.Y. Sho-saiko-to prevents liver fibrosis induced by bile duct ligation in rats. Am. J. Chin. Med. 2004, 32, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.H.; Chen, J.C.; Tsai, C.C.; Wang, W.C.; Chang, D.C.; Tu, D.G.; Hsieh, H.Y. The role of tgf-beta 1 and cytokines in the modulation of liver fibrosis by sho-saiko-to in rat's bile duct ligated model. J. Ethnopharmacol. 2005, 97, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Oka, H.; Yamamoto, S.; Kuroki, T.; Harihara, S.; Marumo, T.; Kim, S.R.; Monna, T.; Kobayashi, K.; Tango, T. Prospective study of chemoprevention of hepatocellular carcinoma with sho-saiko-to (tj-9). Cancer 1995, 76, 743–749. [Google Scholar] [CrossRef]
- Watanabe, S.; Kitade, Y.; Masaki, T.; Nishioka, M.; Satoh, K.; Nishino, H. Effects of lycopene and sho-saiko-to on hepatocarcinogenesis in a rat model of spontaneous liver cancer. Nutr. Cancer 2001, 39, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Feng, Y.; Tan, H.Y.; Cheung, F.; Hong, M.; Lao, L.; Nagamatsu, T. Inhibition of eukaryotic elongation factor-2 confers to tumor suppression by a herbal formulation huanglian-jiedu decoction in human hepatocellular carcinoma. J. Ethnopharmacol. 2015, 164, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Wen, Q.H.; Song, Y.; Li, X.; Jin, J.; Ma, J.S.; Zhou, Q.L. Study on antitumor activities of huanglian jiedu decoction. China J. Chin. Mater. Med. 2006, 31, 1461–1463. [Google Scholar]
- Ma, Y.L.; Li, T.; Wang, B.B.; Jia, B.; Chen, B.; Su, J.; Wang, X.B.; Zeng, H. Protection of huanglian jiedu decoction on livers of hyperlipidemia mice. Chin. J. Integr. Tradit. West. Med. 2013, 33, 1107–1111. [Google Scholar]
- Jin, J.; Zhang, Y.; Hu, W.X.; Zhang, Z.Y.; Xu, N.N.; Zhou, Q.L. Effects of huanglian jiedu decoction on blood lipid metabolism and its related gene expressions in rats with hyperlipidemia. J. Chin. Integr. Med. 2010, 8, 275–279. [Google Scholar] [CrossRef]
- Zhao, Z.J.; Qiu, Q.; Zhang, X.X.; Yang, M.J. Effect of compound biejia ruangan tablet on expressions of connective tissue growth factor mrna and protein in kidney tissue of rats with adriamycin-induced nephropathy. J. Chin. Integr. Med. 2007, 5, 651–655. [Google Scholar] [CrossRef]
- Zhou, J.; Chen, X.M.; Liu, S.W.; Fu, B.; Hong, Q.; Wang, S.J. Effects of biejia ruangan tablet-containing serum on matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 expression in cultured renal interstitial fibroblasts. Chin. J. Integr. Med. 2015, 21, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.R.; Fang, B.W.; Lou, J.S. Effects of fufang biejia ruangan pills on hepatic fibrosis in vivo and in vitro. World J. Gastroenterol. WJG 2013, 19, 5326–5333. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.M.; Yang, Y.P.; Chen, D.Y.; Han, J.; Jin, X.Y.; Huang, Z.X.; Xu, C.B.; Shen, Y.M. Efficacy and safety of fufang biejia ruangan tablet in patients with chronic hepatitis b complicated with hepatic fibrosis. Chin. J. Exp. Clin. Virol. 2007, 21, 358–360. [Google Scholar]
- Bai, J.X.; Dai, L.; Chen, H.G.; Xu, H.; Yin, R.L.; Han, J.; Yuan, H.L. Study on rational daily administration frequency of fufang biejia ruangan tablet based on integrated serum pharmacologic and pharmacokinetic model. China J. Chin. Mater. Med. 2013, 38, 2394–2398. [Google Scholar]
- Allard, T.; Wenner, T.; Greten, H.J.; Efferth, T. Mechanisms of herb-induced nephrotoxicity. Curr. Med. Chem. 2013, 20, 2812–2819. [Google Scholar] [CrossRef] [PubMed]
- Vartholomaios, S.; Pitsios, C.; Mikos, N.; Kompoti, E.; Kouridakis, I.S. Allergy to basil, a lamiaceae herb. J. Investig. Allergol. Clin. Immunol. 2007, 17, 348–349. [Google Scholar] [PubMed]
- Kheir, M.M.; Wang, Y.; Hua, L.; Hu, J.; Li, L.; Lei, F.; Du, L. Acute toxicity of berberine and its correlation with the blood concentration in mice. Food Chem. Toxicol. An Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2010, 48, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Kowalewski, Z.; Mrozikiewicz, A.; Bobkiewicz, T.; Drost, K.; Hladon, B. [toxicity of berberine sulfate]. Acta Polon. Pharm. 1975, 32, 113–120. [Google Scholar]
- Shin, K.S.; Choi, H.S.; Zhao, T.T.; Suh, K.H.; Kwon, I.H.; Choi, S.O.; Lee, M.K. Neurotoxic effects of berberine on long-term l-dopa administration in 6-hydroxydopamine-lesioned rat model of parkinson's disease. Arch. Pharm. Res. 2013, 36, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.B. Singapore kernicterus. Singap. Med. J. 1980, 21, 556–567. [Google Scholar]
- Yeung, C.Y.; Lee, F.T.; Wong, H.N. Effect of a popular chinese herb on neonatal bilirubin protein binding. Biol. Neonat. 1990, 58, 98–103. [Google Scholar] [CrossRef]
- Chan, E. Displacement of bilirubin from albumin by berberine. Biol. Neonat. 1993, 63, 201–208. [Google Scholar] [CrossRef]
- Imanshahidi, M.; Hosseinzadeh, H. Pharmacological and therapeutic effects of berberis vulgaris and its active constituent, berberine. Phytother. Res. PTR 2008, 22, 999–1012. [Google Scholar] [CrossRef] [PubMed]
- Conn, J.W.; Rovner, D.R.; Cohen, E.L. Licorice-induced pseudoaldosteronism: Hypertension, hypokalemia, aldosteronopenia, and suppressed plasma renin activity. JAMA J. Am. Med. Assoc. 1968, 205, 492–496. [Google Scholar] [CrossRef]
- Somjen, D.; Knoll, E.; Vaya, J.; Stern, N.; Tamir, S. Estrogen-like activity of licorice root constituents: Glabridin and glabrene, in vascular tissues in vitro and in vivo. J. Steroid Biochem. Mol. Biol. 2004, 91, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Strandberg, T.E.; Jarvenpaa, A.L.; Vanhanen, H.; McKeigue, P.M. Birth outcome in relation to licorice consumption during pregnancy. Am. J. Epidemiol. 2001, 153, 1085–1088. [Google Scholar] [CrossRef] [PubMed]
- Armanini, D.; Bonanni, G.; Palermo, M. Reduction of serum testosterone in men by licorice. N. Engl. J. Med. 1999, 341, 1158. [Google Scholar] [CrossRef] [PubMed]
- Isbrucker, R.A.; Burdock, G.A. Risk and safety assessment on the consumption of licorice root (glycyrrhiza sp.), its extract and powder as a food ingredient, with emphasis on the pharmacology and toxicology of glycyrrhizin. Regul. Toxicol. Pharmacol. RTP 2006, 46, 167–192. [Google Scholar] [CrossRef] [PubMed]
- Flaig, T.W.; Gustafson, D.L.; Su, L.J.; Zirrolli, J.A.; Crighton, F.; Harrison, G.S.; Pierson, A.S.; Agarwal, R.; Glode, L.M. A phase i and pharmacokinetic study of silybin-phytosome in prostate cancer patients. Investig. New Drugs 2007, 25, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Pliskova, M.; Vondracek, J.; Kren, V.; Gazak, R.; Sedmera, P.; Walterova, D.; Psotova, J.; Simanek, V.; Machala, M. Effects of silymarin flavonolignans and synthetic silybin derivatives on estrogen and aryl hydrocarbon receptor activation. Toxicology 2005, 215, 80–89. [Google Scholar] [CrossRef] [PubMed]
- El-Shitany, N.A.; Hegazy, S.; El-Desoky, K. Evidences for antiosteoporotic and selective estrogen receptor modulator activity of silymarin compared with ethinylestradiol in ovariectomized rats. Phytomed. Int. J. Phytother. Phytopharmacol. 2010, 17, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Loguercio, C.; Festi, D. Silybin and the liver: From basic research to clinical practice. World J. Gastroenterol. WJG 2011, 17, 2288–2301. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Okajima, K.; Sakata, K.; Takatsuki, K. A possible mechanism of interstitial pneumonia during interferon therapy with sho-saiko-to. Nih. Kyobu Shikkan Gakkai Zasshi 1995, 33, 389–394. [Google Scholar]
- Kim, K.H.; Gam, C.O.; Choi, S.H.; Ku, S.K. Mouse single oral dose toxicity test of bupleuri radix aqueous extracts. Toxicol. Res. 2012, 28, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Li, H.; Xu, H.; Yue, X.L.; Cheng, X.Q.; Hou, W.J.; Zhang, Y.Y.; Chen, D.F. Beneficial effect of bupleurum polysaccharides on autoimmune disease induced by campylobacter jejuni in balb/c mice. J. Ethnopharmacol. 2009, 124, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Lv, L.; Huang, W.; Huang, Y.; Sun, R. Research on mechanism of energy metabolism disorders of rat's hepatoxicity induced by saikosaponins. China J. Chin. Mater. Med. 2011, 36, 2557–2561. [Google Scholar]
- Huang, W.; Sun, R. Study on hepatotoxicity on rats caused by crude extracts of total saikosaponins and correlation with oxidative damage mechanism. China J. Chin. Mater. Med. 2010, 35, 1745–1749. [Google Scholar]
- Kong, X.Y.; Hao, Y.; Wu, T.X.; Xie, Y.M. Adverse drug reactions or adverse events of chaihu injection: A systematic review. J. Chin. Integr. Med. 2010, 8, 1124–1132. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, F.; Kong, D.; Zhu, X.; Chen, W.; Wang, A.; Zheng, S. Saikosaponin d disrupts platelet-derived growth factor-beta receptor/p38 pathway leading to mitochondrial apoptosis in human lo2 hepatocyte cells: A potential mechanism of hepatotoxicity. Chem. Biol. Interact. 2013, 206, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Yang, X.; Ho, P.C.; Chan, S.Y.; Heng, P.W.; Chan, E.; Duan, W.; Koh, H.L.; Zhou, S. Herb-drug interactions: A literature review. Drugs 2005, 65, 1239–1282. [Google Scholar] [CrossRef] [PubMed]
- Chan, T.Y. Interaction between warfarin and danshen (salvia miltiorrhiza). Ann. Pharmacother. 2001, 35, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Fugh-Berman, A. Herb-drug interactions. Lancet 2000, 355, 134–138. [Google Scholar] [CrossRef]
- Yang, W.; Yu, X.; He, P.; Hao, W.; Li, Y. Experimental study on anaphylactoid reactions of guinea pig induced by danshen injection and its components. China J. Chin. Mater. Med. 2012, 37, 1894–1897. [Google Scholar]
- Wang, J.Y.; Lee, C.Y.; Pan, P.J.; Chang, W.C.; Chiu, J.H.; Chen, W.S.; Shyr, Y.M. Herb-induced autoimmune-like hepatitis in c57bl/6j mice. Liv. Int. Off. J. Int. Assoc. Study Liv. 2014, 34, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Itoh, S.; Marutani, K.; Nishijima, T.; Matsuo, S.; Itabashi, M. Liver injuries induced by herbal medicine, syo-saiko-to (xiao-chai-hu-tang). Dig. Dis. Sci. 1995, 40, 1845–1848. [Google Scholar] [CrossRef] [PubMed]
- Hsu, L.M.; Huang, Y.S.; Tsay, S.H.; Chang, F.Y.; Lee, S.D. Acute hepatitis induced by chinese hepatoprotective herb, xiao-chai-hu-tang. J. Chin. Med. Assoc. JCMA 2006, 69, 86–88. [Google Scholar] [CrossRef]
- Qi, Q.; Peng, J.; Liu, W.; You, Q.; Yang, Y.; Lu, N.; Wang, G.; Guo, Q. Toxicological studies of wogonin in experimental animals. Phytother. Res. PTR 2009, 23, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Song, D.; Guo, J.; Wang, Y. Study on ingredients of scutellaria radix extract penetrable through placental barrier of pregnant rat. China J. Chin. Mater. Med. 2012, 37, 327–330. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, M.; Li, S.; Tan, H.Y.; Wang, N.; Tsao, S.-W.; Feng, Y. Current Status of Herbal Medicines in Chronic Liver Disease Therapy: The Biological Effects, Molecular Targets and Future Prospects. Int. J. Mol. Sci. 2015, 16, 28705-28745. https://doi.org/10.3390/ijms161226126
Hong M, Li S, Tan HY, Wang N, Tsao S-W, Feng Y. Current Status of Herbal Medicines in Chronic Liver Disease Therapy: The Biological Effects, Molecular Targets and Future Prospects. International Journal of Molecular Sciences. 2015; 16(12):28705-28745. https://doi.org/10.3390/ijms161226126
Chicago/Turabian StyleHong, Ming, Sha Li, Hor Yue Tan, Ning Wang, Sai-Wah Tsao, and Yibin Feng. 2015. "Current Status of Herbal Medicines in Chronic Liver Disease Therapy: The Biological Effects, Molecular Targets and Future Prospects" International Journal of Molecular Sciences 16, no. 12: 28705-28745. https://doi.org/10.3390/ijms161226126
APA StyleHong, M., Li, S., Tan, H. Y., Wang, N., Tsao, S.-W., & Feng, Y. (2015). Current Status of Herbal Medicines in Chronic Liver Disease Therapy: The Biological Effects, Molecular Targets and Future Prospects. International Journal of Molecular Sciences, 16(12), 28705-28745. https://doi.org/10.3390/ijms161226126







