Flavonoids with Anti-Angiogenesis Function in Cancer
Abstract
1. Introduction
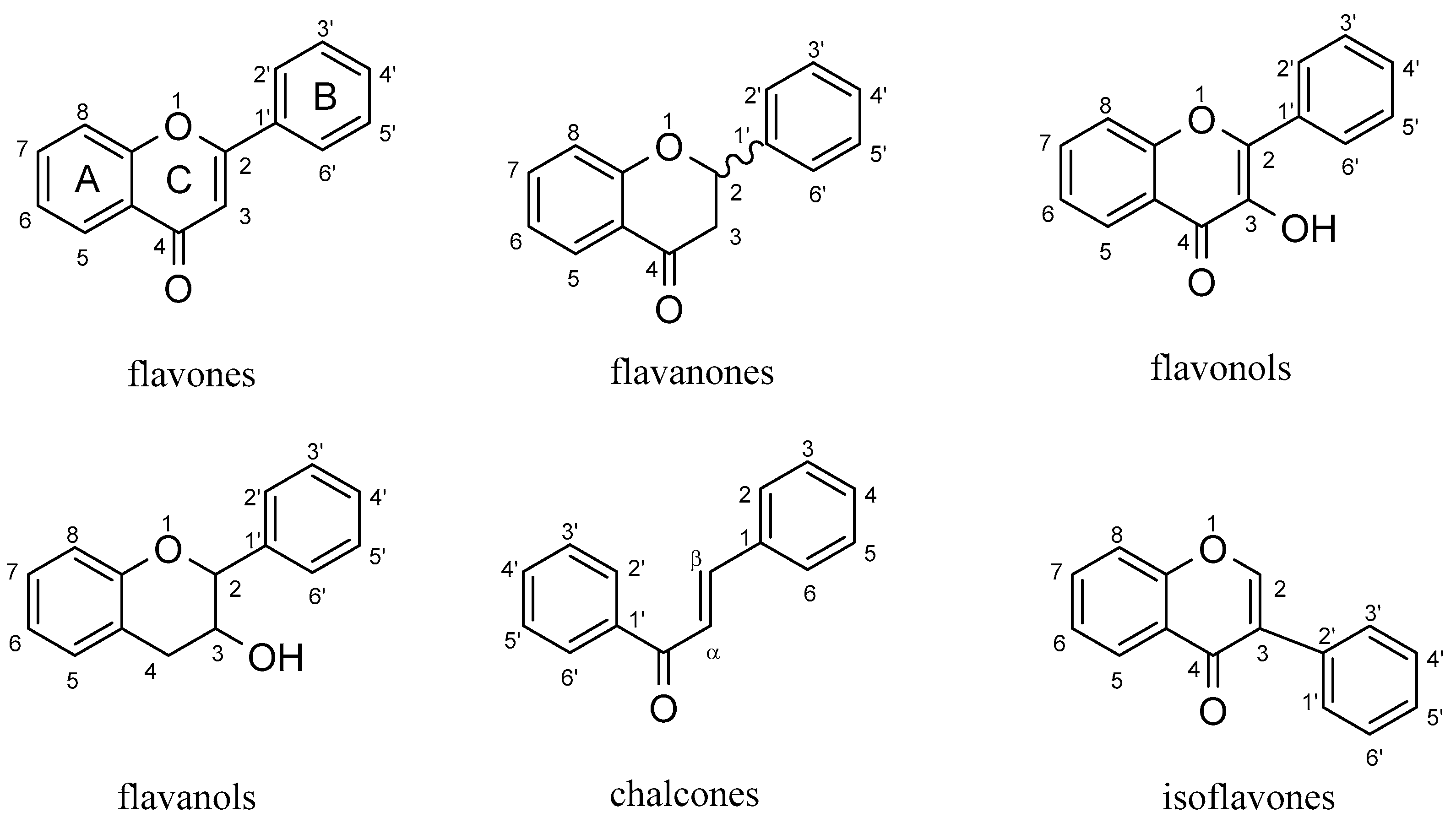
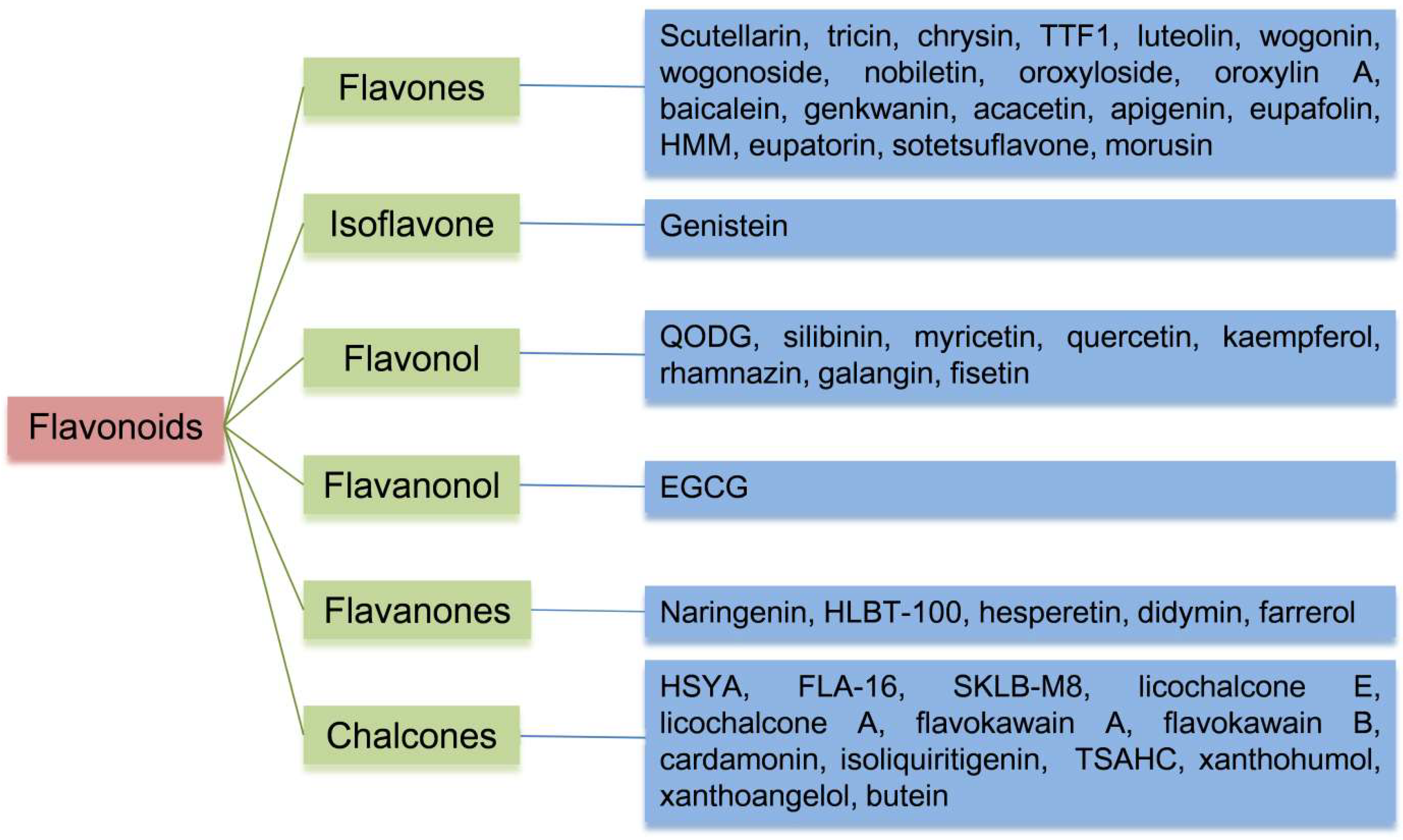
2. Flavonoids
3. Results
3.1. Chemical Components
3.2. Anti-Angiogenic Flavonoids in Cancer
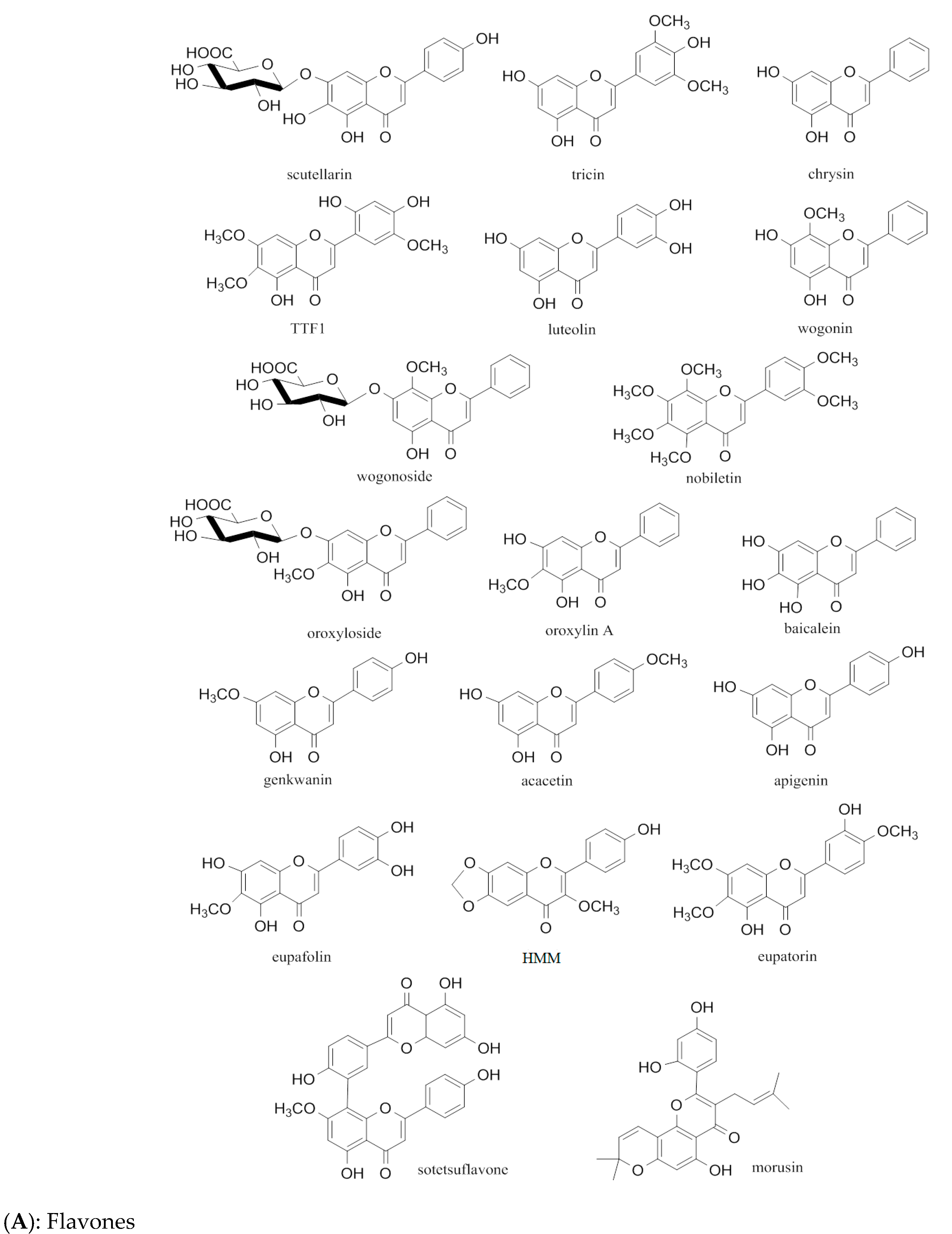
3.2.1. Flavones
| Type | Compounds (No.) | Mechanism | References |
|---|---|---|---|
| Flavone | Scutellarin (1) | Targeting ephrinb2 signaling; possibly regulating transcription factor AP-1; inhibiting PI3K/Akt/mTOR pathway | [20,21,22] |
| Tricin (2) | Reducing ROS; inhibiting HIF-1αaccumulation | [23] | |
| Chrysin (3) | Regulating PI3K/Akt signaling; downregulating JAK1/STAT3 pathway and VEGF/VEGFR2 expression | [24,25,26] | |
| TTF1 (4) | Downregulating VEGF, KDR, bFGF, HIF-1α, and COX-2 | [27] | |
| Luteonin (5) | Downregulating AEG-1, MMP-2, MMP-9, HIF-1α, and STAT3; stimulating immune response; inhibiting AKT/ERK/mTOR/P70S6K/MMPs pathway or PI3K/Akt/mTOR pathway; elevating JNK phosphorylation; inhibiting NF-κB-DNA binding activity; modulating IL-6/STAT3 pathway | [28,29,30,31,32,33,34,35,36] | |
| Wogonin (6) | Degrading HIF-1α protein; modulating c-Myc/HIF-1α/VEGF signaling axis; inhibiting VEGFR2phosphorylation or PI3K/Akt/NF-κB signaling | [37,38,39,40] | |
| Wogonoside (7) | Suppressing Wnt/β-catenin pathway | [41] | |
| Nobiletin (8) | Inhibiting VEGF- and bFGF-induced signaling; activating caspase pathway; inhibiting Akt phosphorylation; mediating Src/FAK/STAT3 signaling | [42,43,44] | |
| Oroxylin A (9) | Blocking KDR/Flk-1 phosphorylation | [45] | |
| Oroxyloside (10) | Inhibiting Akt/MAPK/NF-κB pathway | [46] | |
| Baicalein (11) | Partly mediating VEGF and FGFR-2 signalling; regulating p53/Rb signaling and TRAF6-mediated TLR4 pathway;inhibiting VEGF, HIF-1α, cMyc, NFκB, MMP-2, ROS, and PI 3K/Akt pathway, as well as ERK1/2 and p38 MAPK phospho-activation | [47,48,49,50,51,52] | |
| Genkwanin (12) | Inhibiting invasion and tube formation | [53] | |
| Acacetin (13) | Inhibiting AKT/HIF-1α pathway or STAT-VEGF axis | [54,55] | |
| Apigenin (14) | Blocking the ERK and ERK 1/2 survival signaling or IGF-I/IGFBP-3 signaling; regulating PI3K/AKT/p70S6K1 and HDM2/p53 pathways; downregulating HIF-1α, GLUT-1, and VEGF | [56,57,58,59] | |
| Eupafolin (15) | Blocking VEGFR2activation, ERK1/2, and Akt phosphorylation | [60] | |
| HMM (16) | Inhibiting cathepsins B and L | [61] | |
| Eupatorin (17) | Blocking the phospho-Akt pathway and cell cycle | [62] | |
| Sotetsuflavone (18) | Modulating PI3K/AKT and TNF-α/NF-κB pathways; inhibiting TGF-β, STAT3,and β-catenin; increasing endostatin and ZO-1 | [63,64] | |
| Morusin (19) | Attenuating IL-6/STAT3 signaling; inhibiting VEGF and COX-2genes | [65,66] | |
| Isoflavone | Genistein (20) | Suppressing autocrine and paracrine signalings, hypoxic activation of HIF-1, MMP-1, VEGF, PDGF-A, TF, uPA, MMP-2, and MMP-9; upregulating PAI-1, endostatin, angiostatin, TSP-1, CTGF, and CTAP; downregulating type IV collagenase, uPAR, protease M, PAR-2, VEGF, VEGFR, TGF-b, BPGF, LPA, TSP, JNK, and p38 activation; modulating TIMP-1 and -2 and PAI-1 | [67,68,69,70,71,72] |
| Flavonol | Quercetin (21) | Regulating AKT/mTOR/P70S6K signaling; inhibiting NF-κB and MMP-2/MMP-9 signalings, the H-ras protein synthesis, VEGF and bFGF, STAT3 tyrosine phosphorylation, and Akt phosphorylation, NF-κB activity, eNOS, and early M-phase cell cyclearrest, p300 signaling and the binding of multiple transactivators to COX-2 promoter; upregulating TSP-1 | [73,74,75,76,77,78,79,80] |
| QODG (22) | Suppressing VEGFR2-mediated signaling | [81] | |
| Silibinin (23) | Downregulating survivin, VEGF, VEGFR-2, bFGF, NOS, COX, HIF-1α; increasing p53; inhibiting Akt and NF-kB signaling, MMP-2 secretion, PI3K/Akt signaling or Raf/MEK/ERK pathway, VEGF and endothelial cell growth, or NF-κB signaling; inducingapoptosis; upregulating VEGFR-1 | [82,83,84,85,86,87,88,89,90] | |
| Myricetin (24) | Suppressing PI-3 kinase activity or PI3K/Akt/mTOR signaling; attenuating Akt/p70S6K phosphorylation; modulating Akt/p70S6K/HIF-1α/VEGF and p21/HIF-1α/VEGF pathways | [91,92,93] | |
| Kaempferol (25) | Regulating ERK-NF-κB-cMyc-p21-VEGF and VEGFR2 pathways, ERK/p38 MAPK and PI3K/Akt/mTOR pathways, Akt/HIF and ESRRA pathways; inhibiting VEGFR2 expression, VEGF and FGF pathways or PI3K/AKT, MEK, and ERK pathways | [94,95,96,97,98] | |
| Rhamnazin (26) | Regulating VEGF and PEDF; downregulating the VEGFR2/STAT3/MAPK/Akt pathway | [99,100] | |
| Galangin (27) | Downregulating CD44 and VEGF; modulating Akt/p70S6K/HIF-1α/VEGF pathway | [92,101] | |
| Fisetin (28) | Inhibiting MMPs, MMP-8, and MMP-13, p38 MAPK-dependent NF-κB pathway, NF-κB, MAPK, Wnt, Akt, and mTOR; G1 phrase-G2/M arrest; downregulating cyclin D1, survivin, VEGF, eNOS, iNOS, Bcl-2; inducing p53 and p21, Bax expression and cleavage of caspases-3 and -7, and PARP; regulated by HO-1 viatranscription factor Nrf2; inactivating PI3K/Akt and JNK pathways; diminishing NF-κB and AP-1 DNA-binding activities | [102,103,104,105,106,107,108,109,110,111,112] | |
| Flavanonol | EGCG (29) | Inhibiting VEGF-induced VEGFR2 signaling or NF-κB and ERK1/2 signalings, endoglin/pSmad1 signaling, DNA synthesis, cell proliferation, and signal transduction pathway, and PI3K/AKT/mTOR/HIF1α pathway; downregulating VEGF, uPA, angiopoietin 1 and 2, VEGFR-1 and -2, ERK-1 and -2, MMP-2 and -9, HIF-1α, and CXCL12; suppressing HIF-1 and VEGF/VEGFR axis activation, VEGF, IL-8, and CD31 and Akt activation, NF-κB, and MT1-MMP; increasing endostatin and TIMP1; modulating the genes transcription | [113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133] |
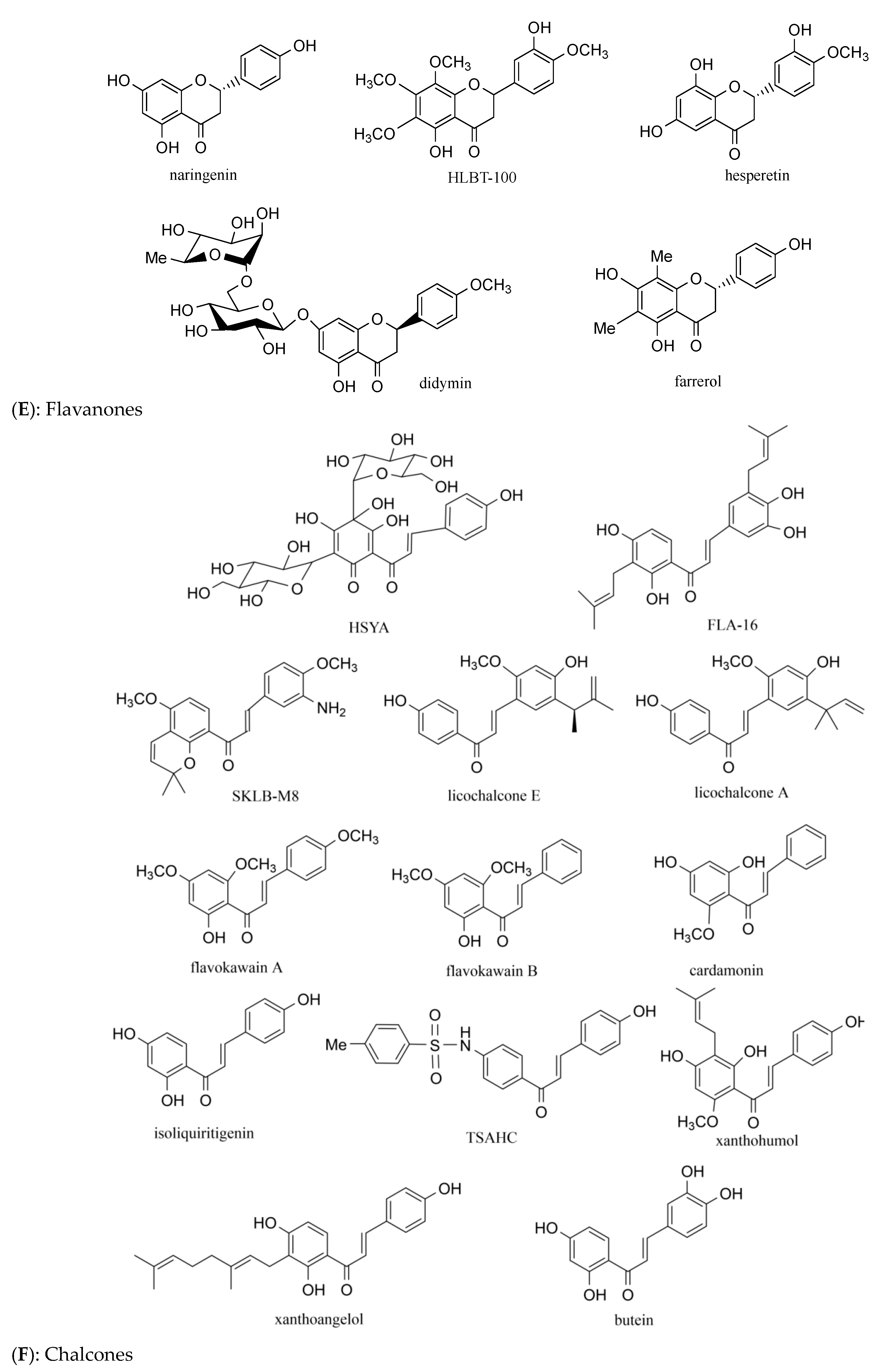
| Flavanones | Naringenin (30) | Mediating ERRα/VEGF/KDR signaling | [134] |
| HLBT-001 (31) | Not mentioned | [135] | |
| Hesperetin (32) | Modulating PI3K/AKT, ERK and p38 MAPK signalings | [136] | |
| Inhibiting angiogenic growth factors and COX-2 mRNA expression | [137] | ||
| Didymin (33) | Preventing NF-κB and expression of adhesion molecules | [138] | |
| Farrerol (34) | Downregulating Akt/mTOR, Erk and Jak2/Stat3 signalings | [139] | |
| Chalcone | HSYA (35) | Inhibiting tumor vascularization; blocking ERK/MAPK and NF-κB signaling or p38 MAPK phosphorylation; downregulating VEGF, bFGF and MMP-9 | [140,141,142,143,144] |
| FLA-16 (36) | Modulating PI3K/Akt signaling through the inhibition of CYP4A | [145] | |
| SKLB-M8 (37) | Decreasing ERK1/2 phosphorylation | [146] | |
| LicA (38) | Blocking VEGF/VEGFR-2 signaling | [147] | |
| LicE (39) | Decreasing VEGFR2, VEGF-A, HIF-1α, COX-2 and iNOS | [148] | |
| FKB (40) | Reducing angiogenin, F3, SDF-1, serpin F1, and TSP-2; suppressing the formation of vessels | [149,150] | |
| FKA (41) | Inhibiting new blood vessels; downregulating the androgen receptor | [151,152] | |
| Cardamonin (42) | Inhibiting HIF-α and VEGF; regulating ERK1/2 and AKT signaling; downregulating miR-21 | [153,154,155] | |
| Isoliquiritigenin (43) | Hampering MAPK signaling of JNK and p38, VEGF/VEGFR2 pathway, ERK1/2 and VEGF; promoting PEDF expression or JNK | [156,157,158,159,160] | |
| TSAHC (44) | Disturbing protein–protein interaction between TM4SF5 and other membrane receptors | [161] | |
| Xanthohumol (45) | Mitigating NF-κB activity, AMPK and AKT/mTOR pathways, and Akt/NF-kB signaling; modulating NF-κB signalling; inhibiting ICAM-1, MMP-9, VEGF, and NF-κB activity | [113,114,115,116,162,163,164] | |
| Xanthoangelol (46) | Inhibiting tube formationand the binding of VEGF to vascular endothelial cells | [117] | |
| Butein (47) | Targeting the AKT/mTOR translation-dependent signaling; inhibiting NF-κB signaling | [118,119] |

3.2.2. Isoflavone
3.2.3. Flavonol
3.2.4. Flavanonol
3.2.5. Flavanones
3.2.6. Chalcones
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Arora, V.; Sharma, N.; Tarique, M.; Vyas, G.; Sharma, R.B. An overview of flavonoids: A diverse group of bioactive phytoconstituents. Curr. Tradit. Med. 2023, 9, 1–12. [Google Scholar] [CrossRef]
- Hazafa, A.; Rehman, K.U.; Jahan, N.; Jabeen, Z. The role of polyphenol (flavonoids) compounds in the treatment of cancer cells. Nutr. Cancer 2020, 72, 386–397. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.U.; Dagur, H.S.; Khan, M.; Malik, N.; Alam, M.; Mushtaque, M. Therapeutic role of flavonoids and flavones in cancer prevention: Current trends and future perspectives. Eur. J. Med. Chem. Rep. 2021, 3, 100010. [Google Scholar] [CrossRef]
- Slika, H.; Mansour, H.; Wehbe, N.; Nasser, S.A.; Iratni, R.; Nasrallah, G.; Shaito, A.; Ghaddar, T.; Kobeissy, F.; Eid, A.H. Therapeutic potential of flavonoids in cancer: ROS-mediated mechanisms. Biomed. Pharmacother. 2022, 146, 112442. [Google Scholar] [CrossRef] [PubMed]
- Scagliarini, A.; Mathey, A.; Aires, V.; Delmas, D. Xanthohumol, a prenylated flavonoid from hops, induces DNA damages in colorectal cancer cells and sensitizes SW480 cells to the SN38 chemotherapeutic agent. Cells 2020, 9, 932. [Google Scholar] [CrossRef]
- Pang, X.; Zhang, X.; Jiang, Y.; Su, Q.; Li, Q.; Li, Z. Autophagy: Mechanisms and therapeutic potential of flavonoids in cancer. Biomolecules 2021, 11, 135. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, M.; Xing, S.; Zhang, C. Flavonoids of Rosa rugosa Thunb. inhibit tumor proliferation and metastasis in human hepatocellular carcinoma HepG2 cells. Food Sci. Hum. Wellness 2022, 11, 374–382. [Google Scholar] [CrossRef]
- Subbaraj, G.K.; Kumar, Y.S.; Kulanthaivel, L. Antiangiogenic role of natural flavonoids and their molecular mechanism: An update. Egypt. J. Intern. Med. 2021, 33, 29. [Google Scholar] [CrossRef]
- Vaiyapuri, M.; Natesan, K.; Vasamsetti, B.M.; Mekapogu, M.; Swamy, M.K.; Thangaraj, K. Orientin: A C-glycosyl flavonoid that mitigates colorectal cancer. In Plant-Derived Bioactives: Chemistry and Mode of Action; Springer: Singapore, 2020; pp. 1–9. [Google Scholar] [CrossRef]
- Fares, J.; Fares, M.Y.; Khachfe, H.H.; Salhab, H.A.; Fares, Y. Molecular principles of metastasis: A hallmark of cancer revisited. Signal Transduct. Target. Ther. 2020, 5, 28. [Google Scholar] [CrossRef]
- Hyytiäinen, A.; Wahbi, W.; Väyrynen, O.; Saarilahti, K.; Karihtala, P.; Salo, T.; Al-Samadi, A. Angiogenesis inhibitors for head and neck squamous cell carcinoma treatment: Is there still hope? Front. Oncol. 2021, 2123, 683570. [Google Scholar] [CrossRef]
- Qin, S.; Li, A.; Yi, M.; Yu, S.; Zhang, M.; Wu, K. Recent advances on anti-angiogenesis receptor tyrosine kinase inhibitors in cancer therapy. J. Hematol. Oncol. 2019, 12, 27. [Google Scholar] [CrossRef] [PubMed]
- Abdulkadir, S.; Li, C.; Jiang, W.; Zhao, X.; Sang, P.; Wei, L.; Hu, Y.; Li, Q.; Cai, J. Modulating angiogenesis by proteomimetics of vascular endothelial growth factor. J. Am. Chem. Soc. 2021, 144, 270–281. [Google Scholar] [CrossRef]
- Fallahi, P.; Ferrari, S.M.; Galdiero, M.R.; Varricchi, G.; Elia, G.; Ragusa, F.; Paparo, S.R.; Benvenga, S.; Antonelli, A. Molecular targets of tyrosine kinase inhibitors in thyroid cancer. Semin. Cancer Biol. 2022, 79, 180–196. [Google Scholar] [CrossRef] [PubMed]
- Breznik, B.; Mitrović, A.; Lah, T.T.; Kos, J. Cystatins in cancer progression: More than just cathepsin inhibitors. Biochimie 2019, 166, 233–250. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Li, Q.Z.; Wang, R.L. Flavonoid components, distribution, and biological activities in Taxus: A review. Molecules 2023, 28, 1713. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cao, Y.; Chen, S.; Lin, J.; Bian, J.; Huang, D. Anti-inflammation activity of flavones and their structure–activity relationship. J. Agric. Food Chem. 2021, 69, 7285–7302. [Google Scholar] [CrossRef] [PubMed]
- Kota, S.; Senthil, R.R. Flavonoids-apoptotic inducers in cancer therapy. NeuroQuantology 2022, 20, 733–741. [Google Scholar]
- Du, E.; Li, X.; He, S.; Li, X.; He, S. The critical role of the interplays of EphrinB2/EphB4 and VEGF in the induction of angiogenesis. Mol. Biol. Rep. 2020, 47, 4681–4690. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.T.; Mao, M.; Liu, Z.G.; Tao, L.; Yan, B.C. Scutellarin suppresses human colorectal cancer metastasis and angiogenesis by targeting ephrinb2. Am. J. Transl. Res. 2017, 9, 5094. [Google Scholar]
- Li, H.X.; Huang, D.Y.; Gao, Z.X.; Chen, Y.; Zhang, L.; Zheng, J.-H. Scutellarin inhibits the growth and invasion of human tongue squamous carcinoma through the inhibition of matrix metalloproteinase-2 and-9 and αvβ6 integrin. Int. J. Oncol. 2013, 42, 1674–1681. [Google Scholar] [CrossRef]
- Li, C.Y.; Wang, Q.; Wang, X.M.; Li, G.X.; Wei, X.L. Scutellarin inhibits the invasive potential of malignant melanoma cells through the suppression epithelial-mesenchymal transition and angiogenesis via the PI3K/Akt/mTOR signaling pathway. Eur. J. Pharmacol. 2019, 858, 172463. [Google Scholar] [CrossRef] [PubMed]
- Han, J.M.; Kwon, H.J.; Jung, H.J. Tricin, 4′,5,7-trihydroxy-3′,5′-dimethoxyflavone, exhibits potent antiangiogenic activity in vitro. Int. J. Oncol. 2016, 49, 1497–1504. [Google Scholar] [CrossRef] [PubMed]
- Fu, B.; Xue, J.; Li, Z.; Shi, X.; Jiang, B.-H.; Fang, J. Chrysin inhibits expression of hypoxia-inducible factor-1alpha through reducing hypoxia-inducible factor-1alpha stability and inhibiting its protein synthesis. Mol. Cancer Ther. 2007, 6, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.M.; Shyu, K.G.; Wang, B.W.; Chang, H.; Chen, Y.H.; Chiu, J.H. Chrysin suppresses IL-6-induced angiogenesis via down-regulation of JAK1/STAT3 and VEGF: An in vitro and in ovo approach. J. Agric. Food Chem. 2010, 58, 7082–7087. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.M.; Chang, H.; Li, S.Y.; Wu, I.H.; Chiu, J.H. Chrysin inhibits lipopolysaccharide-induced angiogenesis via down-regulation of VEGF/VEGFR-2 (KDR) and IL-6/IL-6R pathways. Planta Med. 2006, 72, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, X.W.; Cui, L.M.; Li, L.C.; Chen, L.Y.; Zhang, X.-W. Inhibition of tumor angiogenesis by TTF1 from extract of herbal medicine. World J. Gastroenterol. 2011, 17, 4875. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xie, K.P.; Huo, H.N.; Wang, L.M.; Zou, W.; Xie, M.J. Inhibitory effect of luteolin on the angiogenesis of chick chorioallantoic membrane and invasion of breast cancer cells via downregulation of AEG-1 and MMP-2. Acta Physiol. Sin. 2013, 65, 513–518. [Google Scholar]
- Lu, X.Y.; Li, Y.H.; Xiao, X.W.; Li, X.B. Inhibitory effects of luteolin on human gastric carcinoma xenografts in nude mice and its mechanism. Nat. Med. J. China 2013, 93, 142–146. [Google Scholar]
- Pratheeshkumar, P.; Son, Y.O.; Budhraja, A.; Wang, X.; Ding, S.-Z.; Wang, L.; Hitron, A.; Lee, J.C.; Kim, D.; Divya, S.P.; et al. Luteolin inhibits human prostate tumor growth by suppressing vascular endothelial growth factor receptor 2-mediated angiogenesis. PLoS ONE 2012, 7, e52279. [Google Scholar] [CrossRef]
- Cai, X.; Lu, W.; Ye, T.; Lu, M.; Wang, J.; Huo, J.; Qian, S.-H.; Wang, X.-N.; Cao, P. The molecular mechanism of luteolin-induced apoptosis is potentially related to inhibition of angiogenesis in human pancreatic carcinoma cells. Oncol. Rep. 2012, 28, 1353–1361. [Google Scholar] [CrossRef]
- Gui, S.; Zhou, S.; Liu, M.; Zhang, Y.; Gao, L.; Wang, T.; Zhou, R. Elevated levels of soluble Axl (sAxl) regulates key angiogenic molecules to induce placental endothelial dysfunction and a preeclampsia-like phenotype. Front. Physiol. 2021, 12, 619137. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, M.; Lei, X.; Huang, M.; Ye, W.; Zhang, R.; Zhang, D. Luteolin inhibits angiogenesis by blocking Gas6/Axl signaling pathway. Int. J. Oncol. 2017, 51, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Astone, M.; Alam, S.K.; Zhu, Z.; Pei, W.; Frank, D.A.; Burgess, S.M.; Hoeppner, L.H. Suppressing STAT3 activity protects the endothelial barrier from VEGF-mediated vascular permeability. Dis. Models Mech. 2021, 14, dmm049029. [Google Scholar] [CrossRef] [PubMed]
- Fang, B.; Chen, X.; Wu, M.; Kong, H.; Chu, G.; Zhou, Z.; Zhang, C.; Chen, B. Luteolin inhibits angiogenesis of the M2-like TAMs via the downregulation of hypoxia inducible factor-1α and the STAT3 signalling pathway under hypoxia. Mol. Med. Rep. 2018, 18, 2914–2922. [Google Scholar] [CrossRef] [PubMed]
- Lamy, S.; Akla, N.; Ouanouki, A.; Lord-Dufour, S.; Beliveau, R. Diet-derived polyphenols inhibit angiogenesis by modulating the interleukin-6/STAT3 pathway. Exp. Cell Res. 2012, 318, 1586–1596. [Google Scholar] [CrossRef] [PubMed]
- Song, X.M.; Yao, J.Y.; Wang, F.; Zhou, M.; Zhou, Y.X.; Wang, H.; Wei, L.B.; Zhao, L.; Li, Z.Y.; Lu, N.; et al. Wogonin inhibits tumor angiogenesis via degradation of HIF-1α protein. Toxicol. Appl. Pharmacol. 2013, 271, 144–155. [Google Scholar] [CrossRef] [PubMed]
- Fu, R.; Chen, Y.; Wang, X.P.; An, T.; Tao, L.; Zhou, Y.X.; Huang, Y.-J.; Chen, B.-A.; Li, Z.Y.; You, Q.D.; et al. Wogonin inhibits multiple myeloma-stimulated angiogenesis via the c-Myc/VHL/HIF-1α signaling axis. Oncotarget 2016, 7, 5715–5727. [Google Scholar] [CrossRef]
- Lu, N.; Gao, Y.; Ling, Y.; Chen, Y.; Gu, H.Y.; Qi, Q.; Liu, W.; Wang, X.T.; You, Q.D.; Guo, Q.L. Wogonin suppresses tumor growth in vivo and VEGF-induced angiogenesis through inhibiting tyrosine phosphorylation of VEGFR2. Life Sci. 2008, 82, 956–963. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Song, X.; Huang, Y.; Wei, L.; Li, Z.; You, Q.; Guo, Q.; Lu, N. Wogonin inhibits H2O2-induced angiogenesis via suppressing the PI3K/Akt/NF-κB signaling pathway. Vasc. Pharmacol. 2014, 60, 110–119. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, K.; Hu, Y.; Zhou, Y.; Luo, X.; Li, X.; Wei, L.; Li, Z.; You, Q.; Guo, Q.; et al. Wogonoside inhibits angiogenesis in breast cancer via suppressing the Wnt/β-catenin pathway. Mol. Carcinog. 2016, 55, 1598–1612. [Google Scholar] [CrossRef]
- Kunimasa, K.; Ikekita, M.; Sato, M.; Ohta, T.; Yamori, Y.; Ikeda, M.; Kuranuki, S.; Oikawa, T. Nobiletin, a citrus polymethoxyflavonoid, suppresses multiple angiogenesis-related endothelial cell functions and angiogenesis in vivo. Cancer Sci. 2010, 101, 2462–2469. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, A.Y.; Huang, H.; Ye, X.; Rollyson, W.D.; Perry, H.E.; Brown, K.C.; Rojanasakul, Y.; Rankin, G.O.; Dasgupta, P.; et al. The flavonoid nobiletin inhibits tumor growth and angiogenesis of ovarian cancers via the Akt pathway. Int. J. Oncol. 2015, 46, 2629–2638. [Google Scholar] [CrossRef] [PubMed]
- Sp, N.; Kang, D.Y.; Joung, Y.H.; Park, J.H.; Kim, W.S.; Lee, H.K.; Song, K.D.; Park, Y.M.; Yang, Y.M. Nobiletin inhibits angiogenesis by regulating Src/FAK/STAT3-mediated signaling through PXN in ER(+) breast cancer cells. Int. J. Mol. Sci. 2017, 18, 935. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Lu, N.; Ling, Y.; Chen, Y.; Wang, L.; Zhao, Q.; Qi, Q.; Liu, W.; Zhang, H.; You, Q.; et al. Oroxylin A inhibits angiogenesis through blocking vascular endothelial growth factor-induced KDR/Flk-1 phosphorylation. J. Cancer Res. Clin. 2010, 136, 667–675. [Google Scholar] [CrossRef]
- Zhao, K.; Li, X.; Lin, B.; Yang, D.; Zhou, Y.; Li, Z.; Guo, Q.; Lu, N. Oroxyloside inhibits angiogenesis through suppressing internalization of VEGFR2/Flk-1 in endothelial cells. J. Cell Physiol. 2018, 233, 3454–3464. [Google Scholar] [CrossRef] [PubMed]
- Cathcart, M.C.; Useckaite, Z.; Drakeford, C.; Semik, V.; Lysaght, J.; Gately, K.; O’Byrne, K.J.; Pidgeon, G.P. Anti-cancer effects of baicalein in non-small cell lung cancer in vitro and in vivo. BMC Cancer 2016, 16, 707. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.J.; Huang, T.S.; Cheng, W.F.; Lu, F.J. Baicalein and baicalin are potent inhibitors of angiogenesis: Inhibition of endothelial cell proliferation, migration and differentiation. Int. J. Cancer 2003, 106, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Li, Z.; Chen, A.Y.; Ye, X.; Luo, H.; Rankin, G.O.; Chen, Y.C. Inhibitory effect of baicalin and baicalein on ovarian cancer cells. Int. J. Mol. Sci. 2013, 14, 6012–6025. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.Y.; Oh, Y.T.; Yoon, H.; Lee, J.; Kim, H.; Choe, W.; Kang, I. Baicalein suppresses hypoxia-induced HIF-1alpha protein accumulation and activation through inhibition of reactive oxygen species and PI3-kinase/Akt pathway in BV2 murine microglial cells. Neurosci. Lett. 2008, 444, 264–269. [Google Scholar] [CrossRef]
- Ling, Y.; Chen, Y.; Chen, P.; Hui, H.; Song, X.; Lu, Z.; Li, C.; Lu, N.; Guo, Q. Baicalein potently suppresses angiogenesis induced by vascular endothelial growth factor through the p53/Rb signaling pathway leading to G1/S cell cycle arrest. Exp. Biol. Med. 2011, 236, 851–858. [Google Scholar] [CrossRef]
- Ling, Y.; Wang, L.; Chen, Y.; Feng, F.; You, Q.; Lu, N.; Guo, Q. Baicalein inhibits angiogenesis induced by lipopolysaccharide through TRAF6 mediated toll-like receptor 4 pathway. Biomed. Prev. Nutr. 2011, 1, 172–179. [Google Scholar] [CrossRef]
- Koirala, N. Metabolic Engineering of Eescherichia coli BL21 (DE3) for the Production of Methylated/Glycosylated Flavonoids and Their Biological Activities. Ph.D. Thesis, Sun Moon University, Asan-si, Republic of Korea, 2017. Available online: http://archive.nnl.gov.np:8080/handle/123456789/245 (accessed on 9 March 2024).
- Liu, L.Z.; Jing, Y.; Jiang, L.L.; Jiang, X.E.; Jiang, Y.; Rojanasakul, Y.; Jiang, B.H. Acacetin inhibits VEGF expression, tumor angiogenesis and growth through AKT/HIF-1α pathway. Biochem. Biophys. Res. Commun. 2011, 413, 299–305. [Google Scholar] [CrossRef]
- Bhat, T.A.; Nambiar, D.; Tailor, D.; Pal, A.; Agarwal, R.; Singh, R.P. Acacetin inhibits in vitro and in vivo angiogenesis and downregulates STAT signaling and VEGF expression. Cancer Prev. Res. 2013, 6, 1128–1139. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Ahn, M.-R. Apigenin suppresses angiogenesis by inhibiting tube formation and inducing apoptosis. Nat. Prod. Commun. 2016, 11, 1433–1436. [Google Scholar] [CrossRef]
- Fang, J.; Xia, C.; Cao, Z.; Zheng, J.Z.; Reed, E.; Jiang, B.H. Apigenin inhibits VEGF and HIF-1 expression via PI3K/AKT/p70S6K1 and HDM2/p53 pathways. FASEB J. 2005, 19, 342–353. [Google Scholar] [CrossRef]
- Melstrom, L.G.; Salabat, M.R.; Ding, X.Z.; Strouch, M.J.; Grippo, P.J.; Mirzoeva, S.; Pelling, J.C.; Bentrem, D.J. Apigenin down-regulates the hypoxia response genes: HIF-1α, GLUT-1, and VEGF in human pancreatic cancer cells. J. Surg. Res. 2011, 167, 173–181. [Google Scholar] [CrossRef]
- Shukla, S.; MacLennan, G.T.; Fu, P.; Gupta, S. Apigenin attenuates insulin-like growth Factor-I signaling in an autochthonous mouse prostate cancer model. Pharm. Res. 2012, 29, 1506–1517. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Wu, D.; Xu, D.; Yu, H.; Zhao, Z.; Ma, D.; Jin, J. Eupafolin exhibits potent anti-angiogenic and antitumor activity in hepatocellular carcinoma. Int. J. Biol. Sci. 2017, 13, 701–711. [Google Scholar] [CrossRef] [PubMed]
- de Novais, L.M.; de Arueira, C.C.; Ferreira, L.F.; Ribeiro, T.A.; Sousa, P.T., Jr.; Jacinto, M.J.; de Carvalho, M.G.; Judice, W.A.; Jesus, L.O.; de Souza, A.A.; et al. 4′-Hydroxy-6,7-methylenedioxy-3-methoxyflavone: A novel flavonoid from Dulacia egleri with potential inhibitory activity against cathepsins B and L. Fitoterapia 2019, 132, 26–29. [Google Scholar] [CrossRef]
- Razak, N.A.; Abu, N.; Ho, W.Y.; Zamberi, N.R.; Tan, S.W.; Alitheen, N.B.; Long, K.; Yeap, S.K. Cytotoxicity of eupatorin in MCF-7 and MDA-MB-231 human breast cancer cells via cell cycle arrest, anti-angiogenesis and induction of apoptosis. Sci. Rep. 2019, 9, 1514. [Google Scholar] [CrossRef]
- Wang, S.; Yan, Y.; Cheng, Z.; Hu, Y.; Liu, T. Sotetsuflavone suppresses invasion and metastasis in non-small-cell lung cancer A549 cells by reversing EMT via the TNF-α/NF-κB and PI3K/AKT signaling pathway. Cell Death Discov. 2018, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.K.; Wang, S.H.; Hu, Y.L.; Yan, Y.; Liu, T.X. Effects of sotetsuflavone on expression of endostatin, TGF-β, STAT3, β-catenin and ZO-1 in non-small cell lung cancer A549 cells. TMR Cancer 2018, 1, 58–65. [Google Scholar] [CrossRef]
- Gao, L.; Wang, L.; Sun, Z.; Li, H.; Wang, Q.; Yi, C.; Wang, X. Morusin shows potent antitumor activity for human hepatocellular carcinoma in vitro and in vivo through apoptosis induction and angiogenesis inhibition. Drug Des. Dev. Ther. 2017, 11, 1789–1802. [Google Scholar] [CrossRef]
- Yin, X.L.; Lv, Y.; Wang, S.; Zhang, Y.Q. Morusin suppresses A549 cell migration and induces cell apoptosis by downregulating the expression of COX 2 and VEGF genes. Oncol. Rep. 2018, 40, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Wang, S.; Hoot, D.R.; Clinton, S.K. Suppression of VEGF-mediated autocrine and paracrine interactions between prostate cancer cells and vascular endothelial cells by soy isoflavones. J. Nutr. Biochem. 2007, 18, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Büchler, P.; Reber, H.A.; Büchler, M.W.; Friess, H.; Lavey, R.S.; Hines, O.J. Antiangiogenic activity of genistein in pancreatic carcinoma cells is mediated by the inhibition of hypoxia-inducible factor-1 and the down-regulation of VEGF gene expression. Cancer 2004, 100, 201–210. [Google Scholar] [CrossRef]
- Kim, M.H. Flavonoids inhibit VEGF/bFGF-induced angiogenesis in vitro by inhibiting the matrix-degrading proteases. J. Cell Biochem. 2003, 89, 529–538. [Google Scholar] [CrossRef]
- Su, S.J.; Yeh, T.M.; Chuang, W.J.; Ho, C.L.; Chang, K.L.; Cheng, H.L.; Liu, H.S.; Cheng, H.L.; Hsu, P.Y.; Chow, N.H. The novel targets for anti-angiogenesis of genistein on human cancer cells. Biochem. Pharmacol. 2005, 69, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Sarkar, F.H. Down-regulation of invasion and angiogenesis-related genes identified by cDNA microarray analysis of PC3 prostate cancer cells treated with genistein. Cancer Lett. 2002, 186, 157–164. [Google Scholar] [CrossRef]
- Yu, X.; Zhu, J.; Mi, M.; Chen, W.; Pan, Q.; Wei, M. Anti-angiogenic genistein inhibits VEGF induced endothelial cell activation by decreasing PTK activity and MAPK activation. Med. Oncol. 2012, 29, 349–357. [Google Scholar] [CrossRef]
- Pratheeshkumar, P.; Budhraja, A.; Son, Y.O.; Wang, X.; Zhang, Z.; Ding, S.-Z.; Wang, L.; Hitron, A.; Lee, J.C.; Xu, M.; et al. Quercetin inhibits angiogenesis mediated human prostate tumor growth by targeting VEGFR 2 regulated AKT/mTOR/P70S6K signaling pathways. PLoS ONE 2012, 7, e47516. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.W.; Hsu, S.C.; Chueh, F.S.; Chen, Y.Y.; Yang, J.S.; Lin, J.P.; Lien, J.C.; Tsai, C.H.; Chung, J.G. Quercetin inhibits migration and invasion of SAS human oral cancer cells through inhibition of NF-κB and matrix metalloproteinase-2/-9 signaling pathways. Anticancer Res. 2013, 33, 1941–1950. [Google Scholar] [PubMed]
- Kong, L.; Wu, K.; Lin, H. Inhibitory effects of quercetin on angiogenesis of experimental mammary carcinoma. Chin. J. Clin. Oncol. 2005, 2, 631–636. [Google Scholar] [CrossRef]
- Yang, F.; Jiang, X.; Song, L.; Wang, H.; Mei, Z.; Xu, Z.; Xing, N. Quercetin inhibits angiogenesis through thrombospondin-1 upregulation to antagonize human prostate cancer PC-3 cell growth in vitro and in vivo. Oncol. Rep. 2016, 35, 1602–1610. [Google Scholar] [CrossRef] [PubMed]
- Ansó, E.; Zuazo, A.; Irigoyen, M.; Urdaci, M.C.; Rouzaut, A.; Martínez-Irujo, J.J. Flavonoids inhibit hypoxia-induced vascular endothelial growth factor expression by a HIF-1 independent mechanism. Biochem. Pharmacol. 2010, 79, 1600–1609. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.Y.; Dai, Z.R.; Li, W.-M.; Wang, R.G.; Yang, S.M. Inhibition of EGF expression and NF-κB activity by treatment with quercetin leads to suppression of angiogenesis in nasopharyngeal carcinoma. Saudi. J. Biol. Sci. 2018, 25, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.J.; Venema, R.C. Quercetin inhibits eNOS, microtubule polymerization, and mitotic progression in bovine aortic endothelial cells. J. Nutr. 2006, 136, 1178–1184. [Google Scholar] [CrossRef]
- Xiao, X.; Shi, D.; Liu, L.; Wang, J.; Xie, X.; Kang, T.; Deng, W. Quercetin suppresses cyclooxygenase-2 expression and angiogenesis through inactivation of P300 signaling. PLoS ONE 2011, 6, e22934. [Google Scholar] [CrossRef]
- Lin, C.; Wu, M.; Dong, J. Quercetin-4′-O-β-D-glucopyranoside (QODG) inhibits angiogenesis by suppressing VEGFR2-mediated signaling in zebrafish and endothelial cells. PLoS ONE 2012, 7, e31708. [Google Scholar] [CrossRef]
- Singh, R.P.; Tyagi, A.; Sharma, G.; Mohan, S.; Agarwal, R. Oral silibinin inhibits in vivo human bladder tumor xenograft growth involving down-regulation of survivin. Clin. Cancer Res. 2008, 14, 300–308. [Google Scholar] [CrossRef]
- Yang, S.-H.; Lin, J.K.; Huang, C.J.; Chen, W.S.; Li, S.Y.; Chiu, J.H. Silibinin inhibits angiogenesis via Flt-1, but not KDR, receptor up-regulation. J. Surg. Res. 2005, 128, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Sharma, G.; Dhanalakshmi, S.; Agarwal, C.; Agarwal, R. Suppression of advanced human prostate tumor growth in athymic mice by silibinin feeding is associated with reduced cell proliferation, increased apoptosis, and inhibition of angiogenesis. Cancer Epidemiol. Biomark. Prev. 2003, 12, 933–939. [Google Scholar]
- Gu, M.; Singh, R.P.; Dhanalakshmi, S.; Agarwal, C.; Agarwal, R. Silibinin inhibits inflammatory and angiogenic attributes in photocarcinogenesis in SKH-1 hairless mice. Cancer Res. 2007, 67, 3483–3491. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Raina, K.; Sharma, G.; Agarwal, R. Silibinin inhibits established prostate tumor growth, progression, invasion, and metastasis and suppresses tumor angiogenesis and epithelial-mesenchymal transition in transgenic adenocarcinoma of the mouse prostate model mice. Clin. Cancer Res. 2008, 14, 7773–7780. [Google Scholar] [CrossRef]
- Singh, R.P.; Gu, M.; Agarwal, R. Silibinin inhibits colorectal cancer growth by inhibiting tumor cell proliferation and angiogenesis. Cancer Res. 2008, 68, 2043–2050. [Google Scholar] [CrossRef]
- Singh, R.P.; Dhanalakshmi, S.; Agarwal, C.; Agarwal, R. Silibinin strongly inhibits growth and survival of human endothelial cells via cell cycle arrest and downregulation of survivin, Akt and NF-κB: Implications for angioprevention and antiangiogenic therapy. Oncogene 2005, 24, 1188–1202. [Google Scholar] [CrossRef] [PubMed]
- García-Maceira, P.; Mateo, J. Silibinin inhibits hypoxia-inducible factor-1alpha and mTOR/p70S6K/4E-BP1 signaling pathway in human cervical and hepatoma cancer cells: Implications for anticancer therapy. Oncogene 2009, 28, 313. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Choi, J.H.; Lim, H.I.; Lee, S.K.; Kim, W.W.; Kim, J.S.; Kim, J.H.; Choe, J.H.; Yang, J.H.; Nam, S.J.; et al. Silibinin prevents TPA-induced MMP-9 expression and VEGF secretion by inactivation of the Raf/MEK/ERK pathway in MCF-7 human breast cancer cells. Phytomedicine 2009, 16, 573–580. [Google Scholar] [CrossRef]
- Jung, S.K.; Lee, K.W.; Byun, S.; Lee, E.J.; Kim, J.E.; Bode, A.M.; Dong, Z.; Lee, H.J. Myricetin inhibits UVB-induced angiogenesis by regulating PI-3 kinase in vivo. Carcinogenesis 2010, 31, 911–917. [Google Scholar] [CrossRef]
- Huang, H.; Chen, A.Y.; Rojanasakul, Y.; Ye, X.; Rankin, G.O.; Chen, Y.C. Dietary compounds galangin and myricetin suppress ovarian cancer cell angiogenesis. J. Funct. Foods 2015, 15, 464–475. [Google Scholar] [CrossRef]
- Kim, G.D. Myricetin inhibits angiogenesis by inducing apoptosis and suppressing PI3K/Akt/mTOR signaling in endothelial cells. J. Cancer Prev. 2017, 22, 219–227. [Google Scholar] [CrossRef]
- Luo, H.; Rankin, G.O.; Juliano, N.; Jiang, B.H.; Chen, Y.C. Kaempferol inhibits VEGF expression and in vitro angiogenesis through a novel ERK-NFkappaB-cMyc-p21 pathway. Food Chem. 2012, 130, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Rankin, G.O.; Liu, L.; Daddysman, M.K.; Jiang, B.H.; Chen, Y.C. Kaempferol inhibits angiogenesis and VEGF expression through both HIF dependent and independent pathways in human ovarian cancer cells. Nutr. Cancer 2009, 61, 554–563. [Google Scholar] [CrossRef]
- Liang, F.; Han, Y.; Gao, H.; Xin, S.; Chen, S.; Wang, N.; Qin, W.; Zhong, H.; Lin, S.; Yao, X.; et al. Kaempferol identified by zebrafish assay and fine fractionations strategy from Dysosma versipellis inhibits angiogenesis through VEGF and FGF pathways. Sci. Rep. 2015, 5, 14468. [Google Scholar] [CrossRef]
- Chin, H.K.; Horng, C.T.; Liu, Y.S.; Lu, C.C.; Su, C.Y.; Chen, P.S.; Chiu, H.Y.; Tsai, F.J.; Shieh, P.C.; Yang, J.S. Kaempferol inhibits angiogenic ability by targeting VEGF receptor-2 and downregulating the PI3K/AKT, MEK and ERK pathways in VEGF-stimulated human umbilical vein endothelial cells. Oncol. Rep. 2018, 39, 2351–2357. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.D. Kaempferol Inhibits Angiogenesis by Suppressing HIF-1α and VEGFR2 Activation via ERK/p38 MAPK and PI3K/Akt/mTOR Signaling Pathways in Endothelial Cells. Prev. Nutr. Food Sci. 2017, 22, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Zhou, X.Z.; Ye, L.; Yuan, Q.; Freeberg, S.; Shi, C.; Zhu, P.W.; Bao, J.; Jiang, N.; Shao, Y. Rhamnazin attenuates inflammation and inhibits alkali burn-induced corneal neovascularization in rats. RSC Adv. 2018, 8, 26696–26706. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Cai, W.; Pei, C.G.; Shao, Y. Rhamnazin, a novel inhibitor of VEGFR2 signaling with potent antiangiogenic activity and antitumor efficacy. Biochem. Biophys. Res. Commun. 2015, 458, 913–919. [Google Scholar] [CrossRef]
- Chen, D.; Li, D.; Xu, X.B.; Qiu, S.; Luo, S.; Qiu, E.; Rong, Z.; Zhang, J.; Zheng, D. Galangin inhibits epithelial-mesenchymal transition and angiogenesis by downregulating CD44 in glioma. J. Cancer 2019, 10, 4499. [Google Scholar] [CrossRef]
- Khodadadi, N.; Abbasi, B. The effect of Fisetin on the colorectal cancer: A review. Food Health 2020, 3, 35–44. [Google Scholar]
- Arowosegbe, M.A.; Ogunleye, A.J.; Eniafe, G.O.; Omotuyi, O.I.; Ehima, V.O.; Metibemu, D.S.; Ogungbe, B.; Kanmodi, R.I.; Ogunmola, O.J. Applications of in silico methodologies in exploring the inhibitory potentials of fisetin on MMP-8 and MMP-13 in colorectal cancer progression. Int. J. Drug Dev. Res. 2017, 9, 9–15. [Google Scholar]
- Bhat, T.A.; Nambiar, D.; Pal, A.; Agarwal, R.; Singh, R.P. Fisetin inhibits various attributes of angiogenesis in vitro and in vivo—Implications for angioprevention. Carcinogenesis 2012, 33, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Jang, Y.J.; Choi, Y.J.; Jang, J.W.; Kim, J.H.; Rho, Y.K.; Kim, I.J.; Kim, H.J.; Leem, M.J.; Lee, S.T. Fisetin inhibits matrix metalloproteinases and reduces tumor cell invasiveness and endothelial cell tube formation. Nutr. Cancer 2013, 65, 1192–1199. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.F.; Chen, J.H.; Chang, C.N.; Lu, D.Y.; Chang, P.C.; Wang, S.L.; Yeh, W.L. Fisetin inhibits cell migration via inducing HO-1 and reducing MMPs expression in breast cancer cell lines. Food Chem. Toxicol. 2018, 120, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Chien, C.-S.; Shen, K.-H.; Huang, J.-S.; Ko, S.-C.; Shih, Y.-W. Antimetastatic potential of fisetin involves inactivation of the PI3K/Akt and JNK signaling pathways with downregulation of MMP-2/9 expressions in prostate cancer PC-3 cells. Mol. Cell. Biochem. 2009, 333, 169–180. [Google Scholar] [CrossRef]
- Chou, R.H.; Hsieh, S.C.; Yu, Y.L.; Huang, M.H.; Huang, Y.C.; Hsieh, Y.H. Fisetin inhibits migration and invasion of human cervical cancer cells by down-regulating urokinase plasminogen activator expression through suppressing the p38 MAPK-dependent NF-κB signaling pathway. PLoS ONE 2013, 8, e71983. [Google Scholar] [CrossRef] [PubMed]
- Murtaza, I.; Adhami, V.M.; Hafeez, B.B.; Saleem, M.; Mukhtar, H. Fisetin, a natural flavonoid, targets chemoresistant human pancreatic cancer AsPC-1 cells through DR3-mediated inhibition of NF-κB. Int. J. Cancer 2009, 125, 2465–2473. [Google Scholar] [CrossRef] [PubMed]
- Bassères, D.S.; Baldwin, A.S. Nuclear factor-κB and inhibitor of κB kinase pathways in oncogenic initiation and progression. Oncogene 2006, 25, 6817–6830. [Google Scholar] [CrossRef]
- Syed, D.N.; Adhami, V.M.; Khan, M.I.; Mukhtar, H. Inhibition of Akt/mTOR signaling by the dietary flavonoid fisetin. Anti-Cancer Agents Med. Chem. 2013, 13, 995–1001. [Google Scholar] [CrossRef]
- Aksamitiene, E.; Kiyatkin, A.; Kholodenko, B.N. Cross-talk between mitogenic Ras/MAPK and survival PI3K/Akt pathways: A fine balance. Biochem. Soc. Trans. 2012, 40, 139–146. [Google Scholar] [CrossRef]
- Dell’Eva, R.; Ambrosini, C.; Vannini, N.; Piaggio, G.; Albini, A.; Ferrari, N. AKT/NF-κB inhibitor xanthohumol targets cell growth and angiogenesis in hematologic malignancies. Cancer 2007, 110, 2007–2011. [Google Scholar] [CrossRef] [PubMed]
- Albini, A.; Dell’Eva, R.; Vené, R.; Ferrari, N.; Buhler, D.R.; Noonan, D.M.; Fassina, G. Mechanisms of the antiangiogenic activity by the hop flavonoid xanthohumol: NF-κB and Akt as targets. FASEB J. 2006, 20, 527–529. [Google Scholar] [CrossRef] [PubMed]
- Harikumar, K.B.; Kunnumakkara, A.B.; Ahn, K.S.; Anand, P.; Krishnan, S.; Guha, S.; Aggarwal, B.B. Modification of the cysteine residues in IκBα kinase and NF-κB (p65) by xanthohumol leads to suppression of NF-κB–regulated gene products and potentiation of apoptosis in leukemia cells. Blood. J. Am. Soc. Hematol. 2009, 113, 2003–2013. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Matsuo, Y.; Imafuji, H.; Okubo, T.; Maeda, Y.; Sato, T.; Shamoto, T.; Tsuboi, K.; Morimoto, M.; Takahashi, H.; et al. Xanthohumol inhibits angiogenesis by suppressing nuclear factor-κB activation in pancreatic cancer. Cancer Sci. 2018, 109, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Baba, K. Antitumor and antimetastatic activities of Angelica keiskei roots, part 1: Isolation of an active substance, xanthoangelol. Int. J. Cancer 2003, 106, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.H.; Chang, C.H.; Chen, S.S.; Wang, H.H.; Yen, J.Y.; Hsiao, C.J.; Wu, N.L.; Chen, Y.L.; Huang, T.F.; Wang, P.C. Butein inhibits angiogenesis of human endothelial progenitor cells via the translation dependent signaling pathway. Evid. Based Complement. Altern. Med. 2013, 2013, 943187. [Google Scholar] [CrossRef] [PubMed]
- Moon, D.O.; Choi, Y.H.; Moon, S.K.; Kim, W.J.; Kim, G.Y. Butein suppresses the expression of nuclear factor-kappa B-mediated matrix metalloproteinase-9 and vascular endothelial growth factor in prostate cancer cells. Toxicol. In Vitro 2010, 24, 1927–1934. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Song, J.; Jin, Y. A flavonoid monomer tricin in Gramineous plants: Metabolism, bio/chemosynthesis, biological properties, and toxicology. Food Chem. 2020, 320, 126617. [Google Scholar] [CrossRef]
- Saleem, H.; Anwar, S.; Alafnan, A.; Ahemad, N. Luteolin in a centum of valuable plant bioactives. In A Centum of Valuable Plant Bioactives; Academic Press: Cambridge, MA, USA, 2021; pp. 509–523. [Google Scholar] [CrossRef]
- Yin, Y.; Qu, L.; Zhu, D.; Wu, Y.; Zhou, X. Effect of SOCS3 on apoptosis of human trophoblasts via adjustment of the JAK2/STAT3 signaling pathway in preterm birth. Transl. Pediatr. 2021, 10, 1637. [Google Scholar] [CrossRef]
- Murata, T.; Ishiwa, S.; Lin, X.; Nakazawa, Y.; Tago, K.; Funakoshi-Tago, M. The citrus flavonoid, nobiletin inhibits neuronal inflammation by preventing the activation of NF-κB. Neurochem. Int. 2023, 171, 105613. [Google Scholar] [CrossRef]
- Wang, C.; Gao, M.Q. Research progress on the antidepressant effects of baicalin and its aglycone baicalein: A systematic review of the biological mechanisms. Neurochem. Res. 2023, 49, 14–28. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Lee, Y.C. Plant-derived nanoscale-encapsulated antioxidants for oral and topical uses: A brief review. Int. J. Mol. Sci. 2022, 23, 3638. [Google Scholar] [CrossRef]
- Bozorova, M.I.; Maulyanov, S.A.; Abdumalikov, I.I.; Amanova, Z.K.; Sharipova, F.S.; Kungirotova, A.I.; Toshmatov, Z.O. Flavonoids from Leonurus turkestanicus. Chem. Nat. Compd. 2021, 57, 152–153. [Google Scholar] [CrossRef]
- Adzet, T.; Martinez, F. Flavonoids in the leaves of Thymus: A chemotaxonomic survey. Biochem. Syst. Ecol. 1981, 9, 293–295. [Google Scholar] [CrossRef]
- Daneshvar, S.; Zamanian, M.Y.; Ivraghi, M.S.; Golmohammadi, M.; Modanloo, M.; Kamiab, Z.; Pourhosseini, S.M.E.; Heidari, M.; Bazmandegan, G. A comprehensive view on the apigenin impact on colorectal cancer: Focusing on cellular and molecular mechanisms. Food Sci. Nutr. 2023, 11, 6789–6801. [Google Scholar] [CrossRef] [PubMed]
- Thakur, M.; Kumar, I.; Dhiman, S. A review on artemisia princeps: Pharmacology and anti-Inflammatory potential of phytoconstituents. Asian J. Pharm. Technol. 2023, 13, 285–292. [Google Scholar] [CrossRef]
- Patel, D.K. Protective role of eupafolin against tumor, inflammation, melanogenesis, viral disease and renal injury: Pharmacological and analytical aspects through scientific data analysis. Curr. Chin. Sci. 2022, 2, 143–151. [Google Scholar] [CrossRef]
- Alafnan, A.; Nadeem, M.F.; Ahmad, S.F.; Sarfraz, M.; Aalamri, A.; Khalifa, N.E.; Ahemad, N.; Saleem, H. A comprehensive assessment of phytochemicals from Phyla nodiflora (L.) Greene as a potential enzyme inhibitor, and their biological potential: An in-silico, in-vivo, and in-vitro approach. Arab. J. Chem. 2023, 16, 105233. [Google Scholar] [CrossRef]
- Mustafa, A.; Elkhamisy, F.; Arghiani, N.; Pranjol, M.Z.I. Potential crosstalk between pericytes and cathepsins in the tumour microenvironment. Biomed. Pharmacother. 2023, 164, 114932. [Google Scholar] [CrossRef] [PubMed]
- Zakiyanov, O.; Kalousová, M.; Zima, T.; Tesař, V. Matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases in kidney disease. Adv. Clin. Chem. 2021, 105, 141–212. [Google Scholar] [CrossRef]
- Li, Q.; Wang, Y.; Zhang, L.; Chen, L.; Du, Y.; Ye, T.; Shi, X. Naringenin exerts anti-angiogenic effects in human endothelial cells: Involvement of ERRα/VEGF/KDR signaling pathway. Fitoterapia 2016, 111, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Lowe, H.I.; Toyang, N.J.; Watson, C.T.; Ayeah, K.N.; Bryant, J. HLBT-100: A highly potent anti-cancer flavanone from Tillandsia recurvata (L.) L. Cancer Cell Int. 2017, 17, 38. [Google Scholar] [CrossRef]
- Kim, G.D. Hesperetin inhibits vascular formation by suppressing of the PI3K/AKT, ERK, and p38 MAPK signaling pathways. Prev. Nutr. Food Sci. 2014, 19, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Nalini, N.; Aranganathan, S.; Kabalimurthy, J. Chemopreventive efficacy of hesperetin (citrus flavonone) against 1,2-dimethylhydrazine-induced rat colon carcinogenesis. Toxicol. Mech. Methods 2012, 22, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Shukla, K.; Sonowal, H.; Saxena, A.; Ramana, K.V. Didymin by suppressing NF-κB activation prevents VEGF-induced angiogenesis in vitro and in vivo. Vascul. Pharmacol. 2019, 115, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Dai, F.; Gao, L.; Zhao, Y.; Wang, C.; Xie, S. Farrerol inhibited angiogenesis through Akt/mTOR, Erk and Jak2/Stat3 signal pathway. Phytomedicine 2016, 23, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Xi, S.Y.; Zhang, Q.; Liu, C.Y.; Xie, H.; Yue, L.F.; Gao, X.M. Effects of hydroxy safflower yellow-A on tumor capillary angiogenesis in transplanted human gastric adenocarcinoma BGC-823 tumors in nude mice. J. Tradit. Chin. Med. 2012, 32, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Xi, S.Y.; Zhang, Q.; Xie, H.; Liu, L.; Liu, C.; Gao, X.; Zhang, J.; Wu, L.; Qian, L.; Deng, X. Effects of hydroxy safflor yellow A on blood vessel and mRNA expression with VEGF and bFGF of transplantation tumor with gastric adenocarcinoma cell line BGC-823 in nude mice. China J. Chin. Mater. Med. 2009, 34, 605–610. [Google Scholar]
- Xi, S.; Zhang, Q.; Liu, C.; Xie, H.; Yue, L.; Zhao, Y.; Zang, B.; Gao, X. Effects of HSYA on expression of bFGF protein and MMP-9 in BGC-823 transplantation tumor of nude mice. China J. Chin. Mater. Med. 2010, 35, 2877–2881. [Google Scholar] [CrossRef]
- Yang, F.; Li, J.; Zhu, J.; Wang, D.; Chen, S.; Bai, X. Hydroxysafflor yellow A inhibits angiogenesis of hepatocellular carcinoma via blocking ERK/MAPK and NF-κB signaling pathway in H22 tumor-bearing mice. Eur. J. Pharmacol. 2015, 754, 105–114. [Google Scholar] [CrossRef]
- Zhang, J.; Li, J.; Song, H.; Xiong, Y.; Liu, D.; Bai, X. Hydroxysafflor yellow A suppresses angiogenesis of hepatocellular carcinoma through inhibition of p38 MAPK phosphorylation. Biomed. Pharmacother. 2019, 109, 806–814. [Google Scholar] [CrossRef]
- Wang, C.; Li, Y.; Chen, H.; Zhang, J.; Zhang, J.; Qin, T.; Duan, C.; Chen, X.; Liu, Y.; Zhou, X.; et al. Inhibition of CYP4A by a novel flavonoid FLA-16 prolongs survival and normalizes tumor vasculature in glioma. Cancer Lett. 2017, 402, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yang, Z.; Wen, J.; Ma, F.; Wang, F.; Yu, K.; Tang, M.; Wu, W.; Dong, Y.; Cheng, X.; et al. SKLB-M8 induces apoptosis through the AKT/mTOR signaling pathway in melanoma models and inhibits angiogenesis with a decrease of ERK1/2 phosphorylation. J. Pharmacol. Sci. 2014, 126, 198–207. [Google Scholar] [CrossRef]
- Kim, Y.H.; Shin, E.K.; Kim, D.H.; Lee, H.H.; Park, J.H.Y.; Kim, J.K. Antiangiogenic effect of licochalcone A. Biochem. Pharmacol. 2010, 80, 1152–1159. [Google Scholar] [CrossRef]
- Kwon, S.J.; Park, S.Y.; Kwon, G.T.; Lee, K.W.; Kang, Y.H.; Choi, M.S.; Yun, J.W.; Jeon, J.H.; Jun, J.G.; Park, J.H.Y. Licochalcone E present in licorice suppresses lung metastasis in the 4T1 mammary orthotopic cancer model. Cancer Prev. Res. 2013, 6, 603–613. [Google Scholar] [CrossRef]
- Abu, N.; Mohamed, N.E.; Yeap, S.K.; Lim, K.L.; Akhtar, M.N.; Zulfadli, A.J.; Kee, B.B.; Abdullah, M.P.; Omar, A.R.; Alitheen, N.B. In vivo antitumor and antimetastatic effects of flavokawain B in 4T1 breast cancer cell-challenged mice. Drug Des. Devel. Ther. 2015, 9, 1401–1417. [Google Scholar] [CrossRef] [PubMed]
- Abu, N.; Akhtar, M.N.; Yeap, S.K.; Lim, K.L.; Ho, W.Y.; Abdullah, M.P.; Ho, C.L.; Omar, A.R.; Ismail, J.; Alitheen, N.B. Flavokawain B induced cytotoxicity in two breast cancer cell lines, MCF-7 and MDA-MB231 and inhibited the metastatic potential of MDA-MB231 via the regulation of several tyrosine kinases in vitro. BMC Complement. Altern. Med. 2016, 16, 86. [Google Scholar] [CrossRef]
- Abu, N.; Akhtar, M.N.; Yeap, S.K.; Lim, K.L.; Ho, W.Y.; Zulfadli, A.J.; Omar, A.R.; Sulaiman, M.R.; Abdullah, M.P.; Alitheen, N.B. Flavokawain A induces apoptosis in MCF-7 and MDA-MB231 and inhibits the metastatic process in vitro. PLoS ONE 2014, 9, e105244. [Google Scholar] [CrossRef]
- Liu, Z.; Xu, X.; Li, X.; Liu, S.; Simoneau, A.R.; He, F.; Wu, X.R.; Zi, X. Kava chalcone, flavokawain A, inhibits urothelial tumorigenesis in the UPII-SV40T transgenic mouse model. Cancer Prev. Res. 2013, 6, 1365–1375. [Google Scholar] [CrossRef]
- Xue, Z.G.; Niu, P.G.; Shi, D.H.; Liu, Y.; Deng, J.; Chen, Y.Y. Cardamonin inhibits angiogenesis by mTOR downregulation in SKOV3 cells. Planta Med. 2016, 82, 70–75. [Google Scholar] [CrossRef]
- Tian, S.S.; Jiang, F.S.; Zhang, K.; Zhu, X.X.; Jin, B.; Lu, J.J.; Ding, Z.S. Flavonoids from the leaves of Carya cathayensis Sarg. inhibit vascular endothelial growth factor-induced angiogenesis. Fitoterapia 2014, 92, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.S.; Tian, S.S.; Lu, J.J.; Ding, X.H.; Qian, C.D.; Ding, B.; Ding, Z.S.; Jin, B. Cardamonin regulates miR-21 expression and suppresses angiogenesis induced by vascular endothelial growth factor. BioMed Res. Int. 2015, 2015, 501581. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.W.; Choi, J.S.; Choi, Y.J.; Bae, J.Y.; Li, J.; Kim, D.S.; Kim, J.L.; Shin, S.Y.; Lee, Y.J.; Kwun, I.S.; et al. Licorice isoliquiritigenin dampens angiogenic activity via inhibition of MAPK-responsive signaling pathways leading to induction of matrix metalloproteinases. J. Nutr. Biochem. 2010, 21, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, N.; Han, S.; Wang, D.; Mo, S.; Yu, L. Dietary compound isoliquiritigenin inhibits breast cancer neoangiogenesis via VEGF/VEGFR-2 signaling pathway. PLoS ONE 2013, 8, e68566. [Google Scholar] [CrossRef]
- Sun, Z.J.; Chen, G.; Zhang, W.; Hu, X.; Huang, C.F.; Wang, Y.F.; Jia, J.; Zhao, Y.F. Mammalian target of rapamycin pathway promotes tumor-induced angiogenesis in adenoid cystic carcinoma: Its suppression by isoliquiritigenin through dual activation of c-Jun NH2-terminal kinase and inhibition of extracellular signal-regulated kinase. J. Pharmacol. Exp. Ther. 2010, 334, 500–512. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Li, Y. Phytochemical isoliquiritigenin inhibits angiogenesis ex vivo and corneal neovascularization in mice. Altern. Integr. Med. 2014, 3, 176. [Google Scholar] [CrossRef]
- Jhanji, V.; Liu, H.; Law, K.; Lee, V.Y.-W.; Huang, S.-F.; Pang, C.-P.; Yam, G.H.-F. Isoliquiritigenin from licorice root suppressed neovascularization in experimental ocular angiogenesis models. Brit. J. Ophthalmol. 2011, 95, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.A.; Lee, M.; Ryu, H.; Kwak, T.; Kim, H.; Kang, M.; Jung, O.; Kim, H.; Park, K.; Lee, J. Differential inhibition of transmembrane 4 L six family member 5 (TM4SF5)-mediated tumorigenesis by TSAHC and sorafenib. Cancer Biol. Ther. 2011, 11, 330–336. [Google Scholar] [CrossRef]
- Negrão, R.; Incio, J.; Lopes, R.; Azevedo, I.; Soares, R. Evidence for the effects of xanthohumol in disrupting angiogenic, but not stable vessels. Int. J. Biomed. Sci. 2007, 3, 279. [Google Scholar] [CrossRef]
- Monteiro, R.; Calhau, C.; Silva, A.O.E.; Pinheiro-Silva, S.; Guerreiro, S.; Gärtner, F.; Azevedo, I.; Soares, R. Xanthohumol inhibits inflammatory factor production and angiogenesis in breast cancer xenografts. J. Cell. Biochem. 2008, 104, 1699–1707. [Google Scholar] [CrossRef]
- Gallo, C.; Dallaglio, K.; Bassani, B.; Rossi, T.; Rossello, A.; Noonan, D.M.; D’Uva, G.; Bruno, A.; Albini, A. Hop derived flavonoid xanthohumol inhibits endothelial cell functions via AMPK activation. Oncotarget 2016, 7, 59917. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Siddiqui, N.; Etim, I.; Du, T.; Zhang, Y.; Liang, D. Developing nutritional component chrysin as a therapeutic agent: Bioavailability and pharmacokinetics consideration, and ADME mechanisms. Biomed. Pharmacother. 2021, 142, 112080. [Google Scholar] [CrossRef] [PubMed]
- Karamanos, N.K.; Theocharis, A.D.; Piperigkou, Z.; Manou, D.; Passi, A.; Skandalis, S.S.; Vynios, D.H.; Orian-Rousseau, V.; Ricard-Blum, S.; Schemlzer, C.E.H.; et al. A guide to the composition and functions of the extracellular matrix. FEBS J. 2021, 288, 6850–6912. [Google Scholar] [CrossRef] [PubMed]
- Chriscensia, E.; Aqila Arham, A.; Chrestella Wibowo, E.; Gracius, L.; Nathanael, J.; Hartrianti, P. Eupatorin from Orthosiphon aristatus: A review of the botanical origin, pharmacological effects and isolation methods. Curr. Bioact. Compd. 2023, 19, 45–60. [Google Scholar] [CrossRef]
- López-Sáez, J.A.; Pérez-Alonso, M.J.; Negueruela, A.V. Biflavonoids of Selaginella denticulata growing in Spain. Z. Naturforschung C 1994, 49, 267–270. [Google Scholar] [CrossRef]
- Li, S.H.; Zhang, H.J.; Niu, X.M.; Yao, P.; Sun, H.D.; Fong, H.H. Chemical constituents from Amentotaxus yunnanensis and Torreya yunnanensis. J. Nat. Prod. 2003, 66, 1002–1005. [Google Scholar] [CrossRef] [PubMed]
- Chan, E.W.C.; Wong, S.K.; Tangah, J.; Inoue, T.; Chan, H.T. Phenolic constituents and anticancer properties of Morus alba (white mulberry) leaves. J. Integr. Med. 2020, 18, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Mansour, F.R.; Abdallah, I.A.; Bedair, A.; Hamed, M. Analytical methods for the determination of quercetin and quercetin glycosides in pharmaceuticals and biological Samples. Crit. Rev. Anal. Chem. 2023, 1–26. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Z.; Wu, S.C. Health benefits of Silybum marianum: Phytochemistry, pharmacology, and applications. J. Agric. Food. Chem. 2020, 68, 11644–11664. [Google Scholar] [CrossRef]
- González-Sarrías, A.; Tomás-Barberán, F.A.; García-Villalba, R. Structural diversity of polyphenols and distribution in foods. In Dietary Polyphenols: Their Metabolism and Health Effects; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2020; pp. 1–29. [Google Scholar] [CrossRef]
- Simón, J.; Casado-Andrés, M.; Goikoetxea-Usandizaga, N.; Serrano-Maciá, M.; Martínez-Chantar, M.L. Nutraceutical properties of polyphenols against liver diseases. Nutrients 2020, 12, 3517. [Google Scholar] [CrossRef]
- Prabhu, S.; Molath, A.; Choksi, H.; Kumar, S.; Mehra, R. Classifications of polyphenols and their potential application in human health and diseases. Int. J. Physiol. Nutr. Phys. Educ. 2021, 6, 293–301. [Google Scholar] [CrossRef]
- Kumar, N.; Jain, V. Kaempferol: A key emphasis on its counter-wired potential. Int. J. Innov. Sci. Res. Technol. 2023, 8, 2534–2540. [Google Scholar]
- Abbaszadeh, H.; Keikhaei, B.; Mottaghi, S. A review of molecular mechanisms involved in anticancer and antiangiogenic effects of natural polyphenolic compounds. Phytother. Res. 2019, 33, 2002–2014. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Syed, D.N.; Ahmad, N.; Mukhtar, H. Fisetin: A dietary antioxidant for health promotion. Antioxid. Redox Signal. 2013, 19, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Nitti, M.; Ivaldo, C.; Traverso, N.; Furfaro, A.L. Clinical significance of heme oxygenase 1 in tumor progression. Antioxidants 2021, 10, 789. [Google Scholar] [CrossRef] [PubMed]
- Masucci, M.T.; Minopoli, M.; Di Carluccio, G.; Motti, M.L.; Carriero, M.V. Therapeutic strategies targeting urokinase and its receptor in cancer. Cancers 2022, 14, 498. [Google Scholar] [CrossRef]
- Kretschmer, M.; Rüdiger, D.; Zahler, S. Mechanical aspects of angiogenesis. Cancers 2021, 13, 4987. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Abedini, A.; Plesner, A.; Verchere, C.B.; Raleigh, D.P. The flavanol (−)-epigallocatechin 3-gallate inhibits amyloid formation by islet amyloid polypeptide, disaggregates amyloid fibrils, and protects cultured cells against IAPP-induced toxicity. Biochemistry. 2010, 49, 8127–8133. [Google Scholar] [CrossRef]
- Moyle, C.W.; Cerezo, A.B.; Winterbone, M.S.; Hollands, W.J.; Alexeev, Y.; Needs, P.W.; Kroon, P.A. Potent inhibition of VEGFR-2 activation by tight binding of green tea epigallocatechin gallate and apple procyanidins to VEGF: Relevance to angiogenesis. Mol. Nutr. Food Res. 2015, 59, 401–412. [Google Scholar] [CrossRef]
- Munir, S.; Shah, A.A.; Shahid, M.; Ahmed, M.S.; Shahid, A.; Rajoka, M.S.; Akash, M.S.; Akram, M.; Khurshid, M. Anti-angiogenesis potential of phytochemicals for the therapeutic management of tumors. Curr. Pharm. Des. 2020, 26, 265–278. [Google Scholar] [CrossRef]
- Fassina, G.; Vene, R.; Morini, M.; Minghelli, S.; Benelli, R.; Noonan, D.M.; Albini, A. Mechanisms of inhibition of tumor angiogenesis and vascular tumor growth by epigallocatechin-3-gallate. Clin. Cancer Res. 2004, 10, 4865–4873. [Google Scholar] [CrossRef]
- Zhou, F.; Zhou, H.; Wang, T.; Mu, Y.; Wu, B.; Guo, D.L.; Zhang, X.M.; Wu, Y. Epigallocatechin-3-gallate inhibits proliferation and migration of human colon cancer SW620 cells in vitro. Acta Pharmacol. Sin. 2012, 33, 120–126. [Google Scholar] [CrossRef]
- Sakamoto, Y.; Terashita, N.; Muraguchi, T.; Fukusato, T.; Kubota, S. Effects of epigallocatechin-3-gallate (EGCG) on A549 lung cancer tumor growth and angiogenesis. Biosci. Biotechnol. Biochem. 2013, 77, 1799–1803. [Google Scholar] [CrossRef]
- Shimizu, M.; Shirakami, Y.; Sakai, H.; Yasuda, Y.; Kubota, M.; Adachi, S.; Tsurumi, H.; Hara, Y.; Moriwaki, H. (−)-Epigallocatechin gallate inhibits growth and activation of the VEGF/VEGFR axis in human colorectal cancer cells. Chem. Biol. Interact. 2010, 185, 247–252. [Google Scholar] [CrossRef]
- He, L.; Zhang, E.; Shi, J.; Li, X.; Zhou, K.; Zhang, Q.; Le, A.D.; Tang, X. (−)-Epigallocatechin-3-gallate inhibits human papillomavirus (HPV)-16 oncoprotein-induced angiogenesis in non-small cell lung cancer cells by targeting HIF-1α. Cancer Chemother. Pharmacol. 2013, 71, 713–725. [Google Scholar] [CrossRef]
- Rashidi, B.; Malekzadeh, M.; Goodarzi, M.; Masoudifar, A.; Mirzaei, H. Green tea and its anti-angiogenesis effects. Biomed. Pharmacother. 2017, 89, 949–956. [Google Scholar] [CrossRef]
- Zhu, B.H.; Chen, H.Y.; Zhan, W.H.; Wang, C.Y.; Cai, S.R.; Wang, Z.; Zhang, C.H.; He, Y.L. (−)-Epigallocatechin-3-gallate inhibits VEGF expression induced by IL-6 via Stat3 in gastric cancer. World J. Gastroenterl. 2011, 17, 2315–2325. [Google Scholar] [CrossRef]
- (154) Zhu, B.H.; Zhan, W.H.; Li, Z.R.; Wang, Z.; He, Y.L.; Peng, J.S.; Cai, S.R.; Ma, J.P.; Zhang, C.H. (−)-Epigallocatechin-3-gallate inhibits growth of gastric cancer by reducing VEGF production and angiogenesis. World J. Gastroenterol. 2007, 13, 1162. [Google Scholar] [CrossRef]
- Shi, J.L.; Liu, F.; Zhang, W.Z.; Liu, X.; Lin, B.H.; Tang, X.D. Epigallocatechin-3-gallate inhibits nicotine-induced migration and invasion by the suppression of angiogenesis and epithelial-mesenchymal transition in non-small cell lung cancer cells. Oncol. Rep. 2015, 33, 2972–2980. [Google Scholar] [CrossRef]
- Siddiqui, I.A.; Malik, A.; Adhami, V.M.; Asim, M.; Hafeez, B.B.; Sarfaraz, S.; Mukhtar, H. Green tea polyphenol EGCG sensitizes human prostate carcinoma LNCaP cells to TRAIL-mediated apoptosis and synergistically inhibits biomarkers associated with angiogenesis and metastasis. Oncogene 2008, 27, 2055–2063. [Google Scholar] [CrossRef]
- Chen, C.Y.; Lin, Y.J.; Wang, C.C.N.; Lan, Y.H.; Lan, S.J.; Sheu, M.J. Epigallocatechin-3-gallate inhibits tumor angiogenesis: Involvement of endoglin/Smad1 signaling in human umbilical vein endothelium cells. Biomed. Pharmacother. 2019, 120, 109491. [Google Scholar] [CrossRef]
- Tudoran, O.; Soritau, O.; Balacescu, O.; Balacescu, L.; Braicu, C.; Rus, M.; Gherman, C.; Virag, P.; Irimie, F.; Berindan-Neagoe, I. Early transcriptional pattern of angiogenesis induced by EGCG treatment in cervical tumour cells. J. Cell. Mol. Med. 2012, 16, 520–530. [Google Scholar] [CrossRef]
- Ohga, N.; Hida, K.; Hida, Y.; Muraki, C.; Tsuchiya, K.; Matsuda, K.; Ohiro, Y.; Totsuka, Y.; Shindoh, M. Inhibitory effects of epigallocatechin-3 gallate, a polyphenol in green tea, on tumor-associated endothelial cells and endothelial progenitor cells. Cancer Sci. 2009, 100, 1963–1970. [Google Scholar] [CrossRef]
- Neuhaus, T.; Pabst, S.; Stier, S.; Weber, A.A.; Schrör, K.; Sachinidis, A.; Vetter, H.; Ko, Y.D. Inhibition of the vascular-endothelial growth factor-induced intracellular signaling and mitogenesis of human endothelial cells by epigallocatechin-3 gallate. Eur. J. Pharmacol. 2004, 483, 223–227. [Google Scholar] [CrossRef]
- Gu, J.W.; Makey, K.L.; Tucker, K.B.; Chinchar, E.; Mao, X.; Pei, I.; Thomas, E.Y.; Miele, L. EGCG, a major green tea catechin suppresses breast tumor angiogenesis and growth via inhibiting the activation of HIF-1α and NFκB, and VEGF expression. Vasc. Cell. 2013, 5, 9. [Google Scholar] [CrossRef]
- Li, X.; Feng, Y.; Liu, J.; Feng, X.; Zhou, K.; Tang, X. Epigallocatechin-3-gallate inhibits IGF-I-stimulated lung cancer angiogenesis through downregulation of HIF-1α and VEGF expression. J. Nutr. Nutr. 2013, 6, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Yamakawa, S.; Asai, T.; Uchida, T.; Matsukawa, M.; Akizawa, T.; Oku, N. (−)-Epigallocatechin gallate inhibits membrane-type 1 matrix metalloproteinase, MT1-MMP, and tumor angiogenesis. Cancer Lett. 2004, 210, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Garbisa, S.; Sartor, L.; Biggin, S.; Salvato, B.; Benelli, R.; Albini, A. Tumor gelatinases and invasion inhibited by the green tea flavanol epigallocatechin-3-gallate. Cancer 2001, 91, 822–832. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Man, G.C.W.; Chan, T.H.; Kwong, J.; Wang, C.C. A prodrug of green tea polyphenol (–)-epigallocatechin-3-gallate (Pro-EGCG) serves as a novel angiogenesis inhibitor in endometrial cancer. Cancer Lett. 2018, 412, 10–20. [Google Scholar] [CrossRef]
- Khan, A.; Ikram, M.; Hahm, J.R.; Kim, M.O. Antioxidant and anti-inflammatory effects of citrus flavonoid hesperetin: Special focus on neurological disorders. Antioxidants 2020, 9, 609. [Google Scholar] [CrossRef] [PubMed]
- Abu El-Asrar, A.M.; Nawaz, M.I.; Ahmad, A.; Dillemans, L.; Siddiquei, M.; Allegaert, E.; Gikandi, P.W.; Hertogh, G.D.; Opdenakker, G.; Struyf, S. CD40 Ligand–CD40 Interaction is an intermediary between inflammation and angiogenesis in proliferative diabetic retinopathy. Int. J. Mol. Sci. 2023, 24, 15582. [Google Scholar] [CrossRef]
- Shukla, K.; Sonowal, H.; Saxena, A.; Ramana, K.V. Didymin prevents hyperglycemia-induced human umbilical endothelial cells dysfunction and death. Biochem. Pharmacol. 2018, 152, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Lai, Z.; Pang, Y.; Sun, Q.; Yang, W.; Wang, W. PD-1 blocking strategy for enhancing the anti-tumor effect of CAR T cells targeted CD105. Heliyon 2023, 9, e12688. [Google Scholar] [CrossRef] [PubMed]
- Ao, H.; Feng, W.; Peng, C. Hydroxysafflor yellow A: A promising therapeutic agent for a broad spectrum of diseases. Evid.-Based Complement. Altern. Med. 2018, 2018, 8259280. [Google Scholar] [CrossRef] [PubMed]
- Cheng, B.F.; Gao, Y.X.; Lian, J.J.; Guo, D.D.; Wang, L.; Wang, M.; Yang, H.J.; Feng, Z.W. Hydroxysafflor yellow A inhibits IL-1β-induced release of IL-6, IL-8, and MMP-1 via suppression of ERK, NF-κB and AP-1 signaling in SW982 human synovial cells. Food Funct. 2016, 7, 4516–4522. [Google Scholar] [CrossRef] [PubMed]
- Kalyanakrishnan, K. Effect of ATF2 Transcription Factor on DLL4 Gene Expression in Angiogenesis. Master’s Thesis, University of Wolverhampton, Wolverhampton, UK, 2021. Available online: https://wlv.openrepository.com/handle/2436/624703 (accessed on 1 November 2021).
- Haibe, Y.; Kreidieh, M.; El Hajj, H.; Khalifeh, I.; Mukherji, D.; Temraz, S.; Shamseddine, A. Resistance mechanisms to anti-angiogenic therapies in cancer. Front. Oncol. 2020, 10, 221. [Google Scholar] [CrossRef] [PubMed]
- Colombero, C.; Cárdenas, S.; Venara, M.; Martin, A.; Pennisi, P.; Barontini, M.; Nowicki, S. Cytochrome 450 metabolites of arachidonic acid (20-HETE, 11, 12-EET and 14, 15-EET) promote pheochromocytoma cell growth and tumor-associated angiogenesis. Biochimie 2020, 171, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Lafta, H.A.; AbdulHussein, A.H.; Al-Shalah, S.A.; Alnassar, Y.S.; Mohammed, N.M.; Akram, S.M.; Maytham, T.; Najafi, M. Tumor-associated macrophages (TAMs) in cancer resistance; modulation by natural products. Curr. Top. Med. Chem. 2023, 23, 1104–1122. [Google Scholar] [CrossRef] [PubMed]
- Celentano, A.; Yiannis, C.; Paolini, R.; Zhang, P.; Farah, C.S.; Cirillo, N.; Yap, T.; McCullough, M. Kava constituents exert selective anticancer effects in oral squamous cell carcinoma cells in vitro. Sci. Rep. 2020, 10, 15904. [Google Scholar] [CrossRef] [PubMed]
- Angeline, P.; Thomas, A.; Sankaranarayanan, S.A.; Rengan, A.K. Effect of pH on Isoliquiritigenin (ISL) fluorescence in lipo-polymeric system and metallic nanosystem. Spectrochim. Acta A 2021, 252, 119545. [Google Scholar] [CrossRef] [PubMed]
- Plyusnin, S.N.; Babak, T.V.; Orlovskaya, N.V.; Ulyasheva, N.S.; Golubev, D.A.; Alekseev, A.; Shaposhnikov, M.V.; Moskalev, A. Sources of potential geroprotectors in the flora of the European Northeast. J. Herb. Med. 2023, 41, 100717. [Google Scholar] [CrossRef]
- Rahim, N.S.; Wu, Y.S.; Sim, M.S.; Velaga, A.; Bonam, S.R.; Gopinath, S.; Subramaniyan, V.; Choy, K.W.; Teow, S.-Y.; Fareez, I.M.; et al. Three members of transmembrane-4-superfamily, TM4SF1, TM4SF4, and TM4SF5, as emerging anticancer molecular targets against cancer phenotypes and chemoresistance. Pharmaceuticals 2023, 16, 110. [Google Scholar] [CrossRef] [PubMed]
- Yao-Lei, S.; Tian-Shuang, X.; Yi, J.; Na-Ni, W.; Ling-Chuan, X.; Ting, H.; Hai-Liang, X. Humulus lupulus L. extract and its active constituent xanthohumol attenuate oxidative stress and nerve injury induced by iron overload via activating AKT/GSK3 β and Nrf2/NQO1 pathways. J. Nat. Med. 2023, 77, 12–27. [Google Scholar] [CrossRef]
- Javid, H.; Afshari, A.R.; Zahedi Avval, F.; Asadi, J.; Hashemy, S.I. Aprepitant promotes caspase-dependent apoptotic cell death and G2/M arrest through PI3K/Akt/NF-κB axis in cancer stem-like esophageal squamous cell carcinoma spheres. BioMed Res. Int. 2021, 2021, 8808214. [Google Scholar] [CrossRef] [PubMed]
- Mottin, M.; Caesar, L.K.; Brodsky, D.; Mesquita, N.C.; de Oliveira, K.Z.; Noske, G.D.; Sousa, B.; Ramos, P.; Jarmer, H.; Loh, B.; et al. Chalcones from Angelica keiskei (ashitaba) inhibit key Zika virus replication proteins. Bioorgan. Chem. 2022, 120, 105649. [Google Scholar] [CrossRef] [PubMed]
- Yetkin-Arik, B.; Kastelein, A.W.; Klaassen, I.; Jansen, C.H.; Latul, Y.P.; Vittori, M.; Biri, A.; Kahraman, K.; Griggioen, A.W.; Amant, F.; et al. Angiogenesis in gynecological cancers and the options for anti-angiogenesis therapy. Biochim. Biophys. Acta (BBA)-Rev. Cancer 2021, 1875, 188446. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Dai, L.; Ma, Y.; Wang, J.; Liu, Z. Implications of HIF-1α in the tumorigenesis and progression of pancreatic cancer. Cancer Cell Int. 2020, 20, 273. [Google Scholar] [CrossRef]
- Vimalraj, S. A concise review of VEGF, PDGF, FGF, Notch, angiopoietin, and HGF signalling in tumor angiogenesis with a focus on alternative approaches and future directions. Int. J. Biol. Macromol. 2022, 221, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Guan, C.; Liu, C.; Li, H.; Wu, J.; Sun, C. Targeting hypoxia-inducible factor-1alpha: A new strategy for triple-negative breast cancer therapy. Biomed. Pharmacother. 2022, 156, 113861. [Google Scholar] [CrossRef] [PubMed]
- Han, J.M.; Choi, Y.S.; Dhakal, D.; Sohng, J.K.; Jung, H.J. Novel nargenicin A1 analog inhibits angiogenesis by downregulating the endothelial VEGF/VEGFR2 signaling and tumoral HIF-1α/VEGF pathway. Biomedicines 2020, 8, 252. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, R.; Kawabe, J.I.; Wakabayashi, I. VEGF-independent angiogenic factors: Beyond VEGF/VEGFR2 signaling. J. Vasc. Res. 2022, 59, 78–89. [Google Scholar] [CrossRef] [PubMed]
- You, L.; Wu, W.; Wang, X.; Fang, L.; Adam, V.; Nepovimova, E.; Wu, Q.; Kuca, K. The role of hypoxia-inducible factor 1 in tumor immune evasion. Med. Res. Rev. 2021, 41, 1622–1643. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Chen, Y.; Liu, G.; Li, C.; Song, Y.; Cao, Z.; Li, W.; Hu, J.; Lu, C.; Liu, Y. PI3K/AKT pathway as a key link modulates the multidrug resistance of cancers. Cell Death Dis. 2020, 11, 797. [Google Scholar] [CrossRef] [PubMed]
- Miricescu, D.; Balan, D.G.; Tulin, A.; Stiru, O.; Vacaroiu, I.A.; Mihai, D.A.; Popa, C.C.; Papacocea, R.I.; Enyedi, M.; Sorin, N.A.; et al. PI3K/AKT/mTOR signalling pathway involvement in renal cell carcinoma pathogenesis. Exp. Ther. Med. 2021, 21, 540. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Zhang, X.; Liu, X.; Zhang, C.; Shang, W.; Xue, J.; Chen, R.; Xing, Y.; Song, D.; Xu, R. Ginsenoside Rg1 promotes cerebral angiogenesis via the PI3K/Akt/mTOR signaling pathway in ischemic mice. Eur. J. Pharmacol. 2019, 856, 172418. [Google Scholar] [CrossRef] [PubMed]
- Ji, X.K.; Madhurapantula, S.V.; He, G.; Wang, K.Y.; Song, C.H.; Zhang, J.Y.; Wang, K.J. Genetic variant of cyclooxygenase-2 in gastric cancer: More inflammation and susceptibility. World J. Gastroenterol. 2021, 27, 4653. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Wang, J.; He, Z.; Rao, Z.; Zhang, Z.; Zhou, J.; Zhou, T.; Wang, H. A review on the effect of COX-2-mediated mechanisms on development and progression of gastric cancer induced by nicotine. Biochem. Pharmacol. 2024, 220, 115980. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Liu, M.; Zhou, H.; He, X.; Shi, W.; Yuan, Q.; Zuo, Y.; Li, B.; Hu, Q.; Xie, Y. COX-2/PGE2/VEGF signaling promotes ERK-mediated BMSCs osteogenic differentiation under hypoxia by the paracrine action of ECs. Cytokine 2023, 161, 156058. [Google Scholar] [CrossRef] [PubMed]
- Szweda, M.; Rychlik, A.; Babińska, I.; Pomianowski, A. Significance of cyclooxygenase-2 in oncogenesis. J. Vet. Res. 2019, 63, 215. [Google Scholar] [CrossRef] [PubMed]
- Suryanti, S.; Agustina, H.; Aziz, A.; Yulianti, H.; Suryawathy, B.; Putri, L. High immunoexpression of COX-2 as a metastatic risk factor in ccRCC without PD-L1 involvement. Res. Rep. Urol. 2021, 13, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Pond, K.W.; Doubrovinski, K.; Thorne, C.A. Wnt/β-catenin signaling in tissue self-organization. Genes 2020, 11, 939. [Google Scholar] [CrossRef] [PubMed]
- Mankuzhy, P.; Dharmarajan, A.; Perumalsamy, L.R.; Sharun, K.; Samji, P.; Dilley, R.J. The role of Wnt signaling in mesenchymal stromal cell-driven angiogenesis. Tissue Cell 2023, 85, 102240. [Google Scholar] [CrossRef] [PubMed]
- Bats, M.L.; Peghaire, C.; Delobel, V.; Dufourcq, P.; Couffinhal, T.; Duplàa, C. Wnt/frizzled signaling in endothelium: A major player in blood-retinal- and blood-brain-barrier integrity. CSH Perspect. Med. 2022, 12, a041219. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yang, J.; Qi, J.; Jin, Y.; Tong, L. Activation of NADPH/ROS pathway contributes to angiogenesis through JNK signaling in brain endothelial cells. Microvasc. Res. 2020, 131, 104012. [Google Scholar] [CrossRef]
- Zhou, W.; Yang, L.; Nie, L.; Lin, H. Unraveling the molecular mechanisms between inflammation and tumor angiogenesis. Am. J. Cancer Res. 2021, 11, 301. [Google Scholar] [PubMed]
- Wan, M.L.; Wang, Y.; Zeng, Z.; Deng, B.; Zhu, B.S.; Cao, T.; Li, Y.K.; Xiao, J.; Han, Q.; Wu, Q. Colorectal cancer (CRC) as a multifactorial disease and its causal correlations with multiple signaling pathways. Biosci. Rep. 2020, 40, BSR20200265. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.G.; Lee, K.S.; Nam, K.S. Anti-metastatic effects of arctigenin are regulated by MAPK/AP-1 signaling in 4T-1 mouse breast cancer cells. Mol. Med. Rep. 2020, 21, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, J.G.; Kim, K.Y. Trichosanthes kirilowii extract promotes wound healing through the phosphorylation of ERK1/2 in Keratinocytes. Biomimetics 2022, 7, 154. [Google Scholar] [CrossRef] [PubMed]
- Ricard, N.; Zhang, J.; Zhuang, Z.W.; Simons, M. Isoform-specific roles of ERK1 and ERK2 in arteriogenesis. Cells 2019, 9, 38. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wei, Q.; Zhang, Y.-h. Flavonoids with Anti-Angiogenesis Function in Cancer. Molecules 2024, 29, 1570. https://doi.org/10.3390/molecules29071570
Wei Q, Zhang Y-h. Flavonoids with Anti-Angiogenesis Function in Cancer. Molecules. 2024; 29(7):1570. https://doi.org/10.3390/molecules29071570
Chicago/Turabian StyleWei, Qiang, and Yi-han Zhang. 2024. "Flavonoids with Anti-Angiogenesis Function in Cancer" Molecules 29, no. 7: 1570. https://doi.org/10.3390/molecules29071570
APA StyleWei, Q., & Zhang, Y.-h. (2024). Flavonoids with Anti-Angiogenesis Function in Cancer. Molecules, 29(7), 1570. https://doi.org/10.3390/molecules29071570








