Nano-Based Approaches in Surface Modifications of Dental Implants: A Literature Review
Abstract
1. Introduction
2. Methods
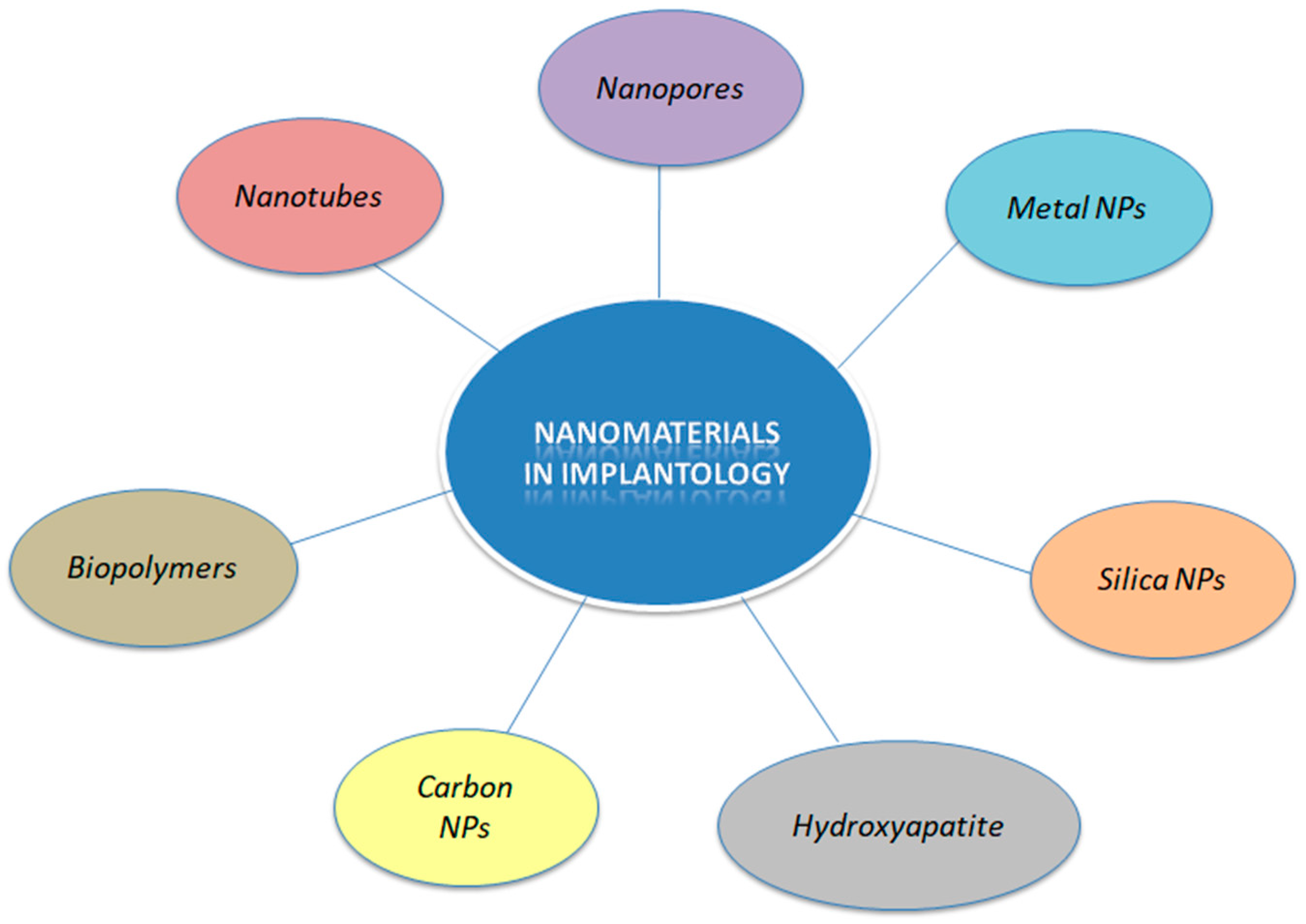
3. Nanomaterials in Implantology
3.1. Nanotubes
3.2. Nanopores
3.3. Metal Nanoparticles
3.4. Silica Nanoparticles
3.5. Hydroxyapatite
3.6. Carbon Nanoparticles
3.7. Biopolymers
4. Enhancement of Implant Integration
4.1. TNTs for Enhancement of Soft and Hard Tissue Integration
4.2. TNTs for Osteoporosis
4.3. TNTs for Alleviation of Diabetes
4.4. Other Nanomaterials
5. Immunomodulation Strategies
5.1. Non-Biofouling Strategies
5.2. Anti-Inflammatory Drug Loading
6. Prevention of Peri-Implantitis
6.1. NPs with Inherent Antibacterial Properties
6.2. NPs Loaded with Drugs
6.3. Chitosan Hybrid Coatings
6.4. Other Nanomaterials
7. Corrosion Resistance
8. Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Branemark, P.I.; Adell, R.; Breine, U.; Hansson, B.O.; Lindstrom, J.; Ohlsson, A. Intra-osseous anchorage of dental prostheses: I. Experimental studies. Scand. J. Plast. Reconstr. Surg. 1969, 3, 81–100. [Google Scholar] [CrossRef] [PubMed]
- Ogle, O.E. Implant surface material, design, and osseointegration. Dent. Clin. N. Am. 2015, 59, 505–520. [Google Scholar] [CrossRef] [PubMed]
- Coelho, P.G.; Granjeiro, J.M.; Romanos, G.E.; Suzuki, M.; Silva, N.R.; Cardaropoli, G.; Thompson, V.P.; Lemons, J.E. Basic research methods and current trends of dental implant surfaces. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 579–596. [Google Scholar] [CrossRef] [PubMed]
- Gaviria, L.; Salcido, J.P.; Guda, T.; Ong, J.L. Current trends in dental implants. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Variola, F.; Yi, J.H.; Richert, L.; Wuest, J.D.; Rosei, F.; Nanci, A. Tailoring the surface properties of Ti6Al4V by controlled chemical oxidation. Biomaterials 2008, 29, 1285–1298. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, G.; Mendonça, D.B.; Aragão, F.J.; Cooper, L.F. Advancing dental implant surface technology--from micron- to nanotopography. Biomaterials 2008, 29, 3822–3835. [Google Scholar] [CrossRef]
- Webster, T.J.; Ergun, C.; Doremus, R.H.; Siegel, R.W.; Bizios, R. Specific proteins mediate enhanced osteoblast adhesion on nanophase ceramics. J. Biomed. Mater. Res. 2000, 51, 475–483. [Google Scholar] [CrossRef]
- Colon, G.; Ward, B.C.; Webster, T.J. Increased osteoblast and decreased Staphylococcus epidermidis functions on nanophase ZnO and TiO2. J. Biomed. Mater. Res. A 2006, 78, 595–604. [Google Scholar] [CrossRef]
- Rasouli, R.; Barhoum, A.; Uludag, H. A review of nanostructured surfaces and materials for dental implants: Surface coating, patterning and functionalization for improved performance. Biomater. Sci. 2018, 6, 1312–1338. [Google Scholar] [CrossRef]
- Valamvanos, T.-F.; Dereka, X.; Katifelis, H.; Gazouli, M.; Lagopati, N. Recent Advances in Scaffolds for Guided Bone Regeneration. Biomimetics 2024, 9, 153. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, H.; Chan, S.M.; Li, R.; Wu, Y.; Cai, M.; Wang, A.; Wang, Y. TiO2 Nanotubes Alleviate Diabetes-Induced Osteogenetic Inhibition. Int. J. Nanomed. 2020, 15, 3523–3537. [Google Scholar] [CrossRef] [PubMed]
- De Avila, E.D.; Van Oirschot, B.A.; Van den Beucken, J.J.J.P. Biomaterial-based possibilities for managing peri-implantitis. J. Periodontal Res. 2020, 55, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Gulati, K.; Chopra, D.; Kocak-Oztug, N.A.; Verron, E. Fit and forget: The future of dental implant therapy via nanotechnology. Adv. Drug Deliv. Rev. 2023, 199, 114900. [Google Scholar] [CrossRef] [PubMed]
- Kunrath, M.F.; Shah, F.A.; Dahlin, C. Bench-to-bedside: Feasibility of nano-engineered and drug-delivery biomaterials for bone-anchored implants and periodontal applications. Mater. Today Bio 2022, 18, 100540. [Google Scholar] [CrossRef] [PubMed]
- Demetzos, C. Pharmaceutical Nanotechnology Fundamentals and Practical Applications; Adis: Singapore, 2018. [Google Scholar]
- Chopra, D.; Gulati, K.; Ivanovski, S. Understanding and optimizing the antibacterial functions of anodized nano-engineered titanium implants. Acta Biomater. 2021, 127, 80–101. [Google Scholar] [CrossRef]
- Lee, J.K.; Choi, D.S.; Jang, I.; Choi, W.Y. Improved osseointegration of dental titanium implants by TiO2 nanotube arrays with recombinant human bone morphogenetic protein-2: A pilot in vivo study. Int. J. Nanomed. 2015, 10, 1145–1154. [Google Scholar]
- Zhang, Y.; Gulati, K.; Li, Z.; Di, P.; Liu, Y. Dental Implant Nano-Engineering: Advances, Limitations and Future Directions. Nanomaterials 2021, 11, 2489. [Google Scholar] [CrossRef]
- Bapat, R.A.; Chaubal, T.V.; Joshi, C.P.; Bapat, P.R.; Choudhury, H.; Pandey, M.; Gorain, B.; Kesharwani, P. An overview of application of silver nanoparticles for biomaterials in dentistry. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 91, 881–898. [Google Scholar] [CrossRef]
- Roco, M.C. Nanoscale Science and Engineering: Unifying and Transforming Tools. AIChE J. 2004, 50, 890–897. [Google Scholar] [CrossRef]
- Abdulkareem, E.H.; Memarzadeh, K.; Allaker, R.P.; Huang, J.; Pratten, J.; Spratt, D. Anti-biofilm activity of zinc oxide and hydroxyapatite nanoparticles as dental implant coating materials. J. Dent. 2015, 43, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Vagena, I.-A.; Gatou, M.-A.; Theocharous, G.; Pantelis, P.; Gazouli, M.; Pippa, N.; Gorgoulis, V.G.; Pavlatou, E.A.; Lagopati, N. Functionalized ZnO-Based Nanocomposites for Diverse Biological Applications: Current Trends and Future Perspectives. Nanomaterials 2024, 14, 397. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, P.; Zhao, R.; Zhao, L.; Liu, J.; Peng, S.; Fu, X.; Wang, X.; Luo, R.; Wang, R.; et al. Silica nanoparticles: Biomedical applications and toxicity. Biomed. Pharmacother. 2022, 151, 113053. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhou, X.; He, C. Mesoporous silica nanoparticles for tissue-engineering applications. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1573. [Google Scholar] [CrossRef] [PubMed]
- Abraham, C.M. A brief historical perspective on dental implants, their surface coatings and treatments. Open Dent. J. 2014, 8, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Lagopati, N.; Agathopoulos, S. Hydroxyapatite Scaffolds Produced from Cuttlefish Bone via Hydrothermal Transformation for Application in Tissue Engineering and Drug Delivery Systems. In Marine-Derived Biomaterials for Tissue Engineering Applications; Choi, A., Ben-Nissan, B., Eds.; Springer Series in Biomaterials Science and Engineering; Springer: Singapore, 2019; Volume 14. [Google Scholar]
- Almeida, D.; Sartoretto, S.C.; Calasans-Maia, J.A.; Ghiraldini, B.; Bezerra, F.J.B.; Granjeiro, J.M.; Calasans-Maia, M.D. In vivo osseointegration evaluation of implants coated with nanostructured hydroxyapatite in low density bone. PLoS ONE 2023, 18, 0282067. [Google Scholar] [CrossRef]
- Zhou, W.; Liu, Z.; Xu, S.; Hao, P.; Xu, F.; Sun, A. Long-term survivability of hydroxyapatite-coated implants: A meta-analysis. Oral Surg. 2011, 4, 2–7. [Google Scholar] [CrossRef]
- Jang, W.; Kim, H.S.; Alam, K.; Ji, M.K.; Cho, H.S.; Lim, H.P. Direct-Deposited Graphene Oxide on Dental Implants for Antimicrobial Activities and Osteogenesis. Int. J. Nanomed. 2021, 16, 5745–5754. [Google Scholar] [CrossRef]
- Di Carlo, R.; Di Crescenzo, A.; Pilato, S.; Ventrella, A.; Piattelli, A.; Recinella, L.; Chiavaroli, A.; Giordani, S.; Baldrighi, M.; Camisasca, A.; et al. Osteoblastic Differentiation on Graphene Oxide-Functionalized Titanium Surfaces: An In Vitro Study. Nanomaterials 2020, 10, 654. [Google Scholar] [CrossRef]
- López-Valverde, N.; Aragoneses, J.; López-Valverde, A.; Rodríguez, C.; Macedo de Sousa, B.; Aragoneses, J.M. Role of chitosan in titanium coatings. trends and new generations of coatings. Front. Bioeng. Biotechnol. 2022, 10, 907589. [Google Scholar] [CrossRef]
- Gulati, K.; Ivanovski, S. Dental implants modified with drug releasing titania nanotubes: Therapeutic potential and developmental challenges. Expert Opin. Drug. Deliv. 2017, 14, 1009–1024. [Google Scholar] [CrossRef]
- Balasundaram, G.; Yao, C.; Webster, T.J. TiO2 nanotubes functionalized with regions of bone morphogenetic protein-2 increases osteoblast adhesion. J. Biomed. Mater. Res. A 2008, 84, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Kodama, A.; Bauer, S.; Komatsu, A.; Asoh, H.; Ono, S.; Schmuki, P. Bioactivation of titanium surfaces using coatings of TiO(2) nanotubes rapidly pre-loaded with synthetic hydroxyapatite. Acta Biomater. 2009, 5, 2322–2330. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhou, X.; Li, S.; Lai, R.; Zhou, Z.; Zhang, Y.; Zhou, L. Effects of titania nanotubes with or without bovine serum albumin loaded on human gingival fibroblasts. Int. J. Nanomed. 2014, 9, 1185–1198. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Oh, T.J.; Bae, T.S.; Lee, M.H.; Soh, Y.; Kim, B.I.; Kim, H.S. Effect of bisphosphonates on anodized and heat-treated titanium surfaces: An animal experimental study. J. Periodontol. 2011, 82, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Ma, P.; Hu, Y.; Gaoqiang, X.; Xu, K.; Chen, W.; Ran, Q.; Dai, L.; Yu, Y.; Mu, C.; et al. Alendronate-loaded hydroxyapatite-TiO2 nanotubes for improved bone formation in osteoporosis rabbits. J. Mater. Chem. B 2016, 4, 1423–1436. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Sándor, G.K.; Dore, E.; Morrison, A.D.; Alsahli, M.; Amin, F.; Peters, E.; Hanley, D.A.; Chaudry, S.R.; Lentle, B.; et al. Canadian Taskforce on Osteonecrosis of the Jaw. Bisphosphonate associated osteonecrosis of the jaw. J. Rheumatol. 2009, 36, 478–490. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Jin, Y.; Qian, S.; Li, J.; Chang, Q.; Ye, D.; Pan, H.; Zhang, M.; Cao, H.; Liu, X.; et al. Vacuum extraction enhances rhPDGF-BB immobilization on nanotubes to improve implant osseointegration in ovariectomized rats. Nanomedicine 2014, 10, 1809–1818. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Bhattarai, G.; Park, I.S.; Kim, G.R.; Kim, G.E.; Lee, M.H.; Yi, H.K. Bone regeneration around N-acetyl cysteine-loaded nanotube titanium dental implant in rat mandible. Biomaterials 2013, 34, 10199–10208. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, X.; Wang, B.; Lan, J.; Yang, H.; Wang, Z.; Chang, X.; Wang, S.; Ma, X.; Qiao, H.; et al. Synergistic effects of lanthanum and strontium to enhance the osteogenic activity of TiO2 nanotube biological interface. Ceram. Int. 2020, 46, 13969–13979. [Google Scholar] [CrossRef]
- de Araújo Nobre, M.; Maló, P.; Gonçalves, Y.; Sabas, A.; Salvado, F. Dental implants in diabetic patients: Retrospective cohort study reporting on implant survival and risk indicators for excessive marginal bone loss at 5 years. J. Oral Rehabil. 2016, 43, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Chambrone, L.; Palma, L.F. Current status of dental implants survival and peri-implant bone loss in patients with uncontrolled type-2 diabetes mellitus. Curr. Opin. Endocrinol. Diabetes Obes. 2019, 26, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Kim, J.S.; Kim, J.E.; Lee, M.H.; Jeon, J.G.; Park, I.S.; Yi, H.K. Nanoparticle mediated PPARγ gene delivery on dental implants improves osseointegration via mitochondrial biogenesis in diabetes mellitus rat model. Nanomedicine 2017, 13, 1821–1832. [Google Scholar] [CrossRef] [PubMed]
- Fang, K.; Song, W.; Wang, L.; Jia, S.; Wei, H.; Ren, S.; Xu, X.; Song, Y. Immobilization of chitosan film containing semaphorin 3A onto a microarc oxidized titanium implant surface via silane reaction to improve MG63 osteogenic differentiation. Int. J. Nanomed. 2014, 9, 4649–4657. [Google Scholar]
- Yamada, M.; Ueno, T.; Tsukimura, N.; Ikeda, T.; Nakagawa, K.; Hori, N.; Suzuki, T.; Ogawa, T. Bone integration capability of nanopolymorphic crystalline hydroxyapatite coated on titanium implants. Int. J. Nanomed. 2012, 7, 859–873. [Google Scholar]
- Zhao, S.F.; Jiang, Q.H.; Peel, S.; Wang, X.X.; He, F.M. Effects of magnesium-substituted nanohydroxyapatite coating on implant osseointegration. Clin. Oral Implants Res. 2013, 24 (Suppl. A100), 34–41. [Google Scholar] [CrossRef] [PubMed]
- Heo, D.N.; Ko, W.K.; Lee, H.R.; Lee, S.J.; Lee, D.; Um, S.H.; Lee, J.H.; Woo, Y.H.; Zhang, L.G.; Lee, D.W.; et al. Titanium dental implants surface-immobilized with gold nanoparticles as osteoinductive agents for rapid osseointegration. J. Colloid Interface Sci. 2016, 1, 129–137. [Google Scholar] [CrossRef]
- Qiao, S.; Cao, H.; Zhao, X.; Lo, H.; Zhuang, L.; Gu, Y.; Shi, J.; Liu, X.; Lai, H. Ag-plasma modification enhances bone apposition around titanium dental implants: An animal study in Labrador dogs. Int. J. Nanomed. 2015, 10, 653–664. [Google Scholar]
- Bartkowiak, A.; Suchanek, K.; Menaszek, E.; Szaraniec, B.; Lekki, J.; Perzanowski, M.; Marszałek, M. Biological effect of hydrothermally synthesized silica nanoparticles within crystalline hydroxyapatite coatings for titanium implants. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 92, 88–95. [Google Scholar] [CrossRef]
- Jo, Y.K.; Choi, B.H.; Kim, C.S.; Cha, H.J. Diatom-Inspired Silica Nanostructure Coatings with Controllable Microroughness Using an Engineered Mussel Protein Glue to Accelerate Bone Growth on Titanium-Based Implants. Adv. Mater. 2017, 29, 46. [Google Scholar] [CrossRef]
- Covarrubias, C.; Mattmann, M.; Von Marttens, A.; Caviedes, P.; Arriagadac, C.; Valenzuelaa, F.; Rodríguez, J.P.; Corral Núñez, C. Osseointegration properties of titanium dental implants modified with a nanostructured coating based on ordered porous silica and bioactive glass nanoparticles. Appl. Surf. Sci. 2016, 363, 286–295. [Google Scholar] [CrossRef]
- Vandamme, K.; Thevissen, K.; Mesquita, M.F.; Coropciuc, R.G.; Agbaje, J.; Thevissen, P.; da Silva, W.J.; Vleugels, J.; De Cremer, K.; Gerits, E.; et al. Implant functionalization with mesoporous silica: A promising antibacterial strategy, but does such an implant osseointegrate? Clin. Exp. Dent. Res. 2021, 7, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, T.; Graw, C.L.; Engel, N.; Gerber, T.; Frerich, B.; Dau, M. Sustainable Surface Modification of Polyetheretherketone (PEEK) Implants by Hydroxyapatite/Silica Coating-An In Vivo Animal Study. Materials 2021, 14, 4589. [Google Scholar] [CrossRef] [PubMed]
- Frandsen, C.J.; Brammer, K.S.; Noh, K.; Connelly, L.; Oh, S.; Chen, L.-H.; Jin, S. Zirconium oxide nanotube surface prompts increased osteoblast functionality and mineralization. Mater. Sci. Eng. 2011, 31, 1716–1722. [Google Scholar] [CrossRef]
- Wang, C.; Hu, H.; Li, Z.; Shen, Y.; Xu, Y.; Zhang, G.; Zeng, X.; Deng, J.; Zhao, S.; Ren, T.; et al. Enhanced Osseointegration of Titanium Alloy Implants with Laser Microgrooved Surfaces and Graphene Oxide Coating. ACS Appl. Mater. Interfaces 2019, 11, 39470–39483. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Baldini, N.; Gatti, F.; Martinolli, M.; Xhanari, E.; Meloni, S.M.; Gabriele, C.; Immacolata, L.A. Role of New Hydrphilic Surfaces on Early Success Rate and Implant Stability: 1-Year Post-loading Results of a Multicenter, Split-Mouth, Randomized Controlled Trial. Eur. J. Dent. 2021, 15, 1–7. [Google Scholar] [PubMed]
- Tallarico, M.; Gatti, F.; Xhanari, E.; Muzzi, L.; Gheorghita, M.; de Waal, A.; Deliverska, E.; Widmer, N.; Melodia, D.; Ceruso, F.M.; et al. A split-mouth, multicentre randomized controlled trial comparing single sandblasted acidetched implants with or without surface modified with ph buffering agent: Results one year after loading. Clin. Trials Dent. 2023, 5, 29. [Google Scholar] [CrossRef]
- Zhang, J.; Bai, H.; Bai, M.; Wang, X.; Li, Z.; Xue, H.; Wang, J.; Cui, Y.; Wang, H.; Wang, Y.; et al. Bisphosphonate-incorporated coatings for orthopedic implants functionalization. Mater. Today Bio 2023, 22, 100737. [Google Scholar] [CrossRef] [PubMed]
- Trindade, R.; Albrektsson, T.; Tengvall, P.; Wennerberg, A. Foreign Body Reaction to Biomaterials: On Mechanisms for Buildup and Breakdown of Osseointegration. Clin. Implant. Dent. Relat. Res. 2016, 18, 192–203. [Google Scholar] [CrossRef]
- Eren, T.; Baysal, G.; Doğan, F. Biocidal Activity of Bone Cements Containing Curcumin and Pegylated Quaternary Polyethylenimine. J. Polym. Environ. 2020, 28, 2469–2480. [Google Scholar] [CrossRef]
- Amengual-Peñafiel, L.; Córdova, L.A.; Constanza Jara-Sepúlveda, M.; Brañes-Aroca, M.; Marchesani-Carrasco, F.; Cartes-Velásquez, R. Osteoimmunology drives dental implant osseointegration: A new paradigm for implant dentistry. Jpn. Dent. Sci. Rev. 2021, 57, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.M.; Kong, B.; Oh, E.; Choi, J.S.; Choi, I.S. Osteoconductive conjugation of bone morphogenetic protein-2 onto titanium/titanium oxide surfaces coated with non-biofouling poly(poly(ethylene glycol) methacrylate). Colloids Surf. B Biointerfaces 2010, 75, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.S.; Capellato, P.; Kelley, S.; Gonzalez-Juarrero, M.; Popat, K.C. Reduced in vitro immune response on titania nanotube arrays compared to titanium surface. Biomater. Sci. 2013, 1, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Neacsu, P.; Mazare, A.; Schmuki, P.; Cimpean, A. Attenuation of the macrophage inflammatory activity by TiO2 nanotubes via inhibition of MAPK and NF-κB pathways. Int. J. Nanomed. 2015, 10, 6455–6467. [Google Scholar]
- Gulati, K.; Moon, H.J.; Li, T.; Sudheesh Kumar, P.T.; Ivanovski, S. Titania nanopores with dual micro-/nano-topography for selective cellular bioactivity. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 91, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Zhang, H.; Yao, X.; Tang, B.; Chu, P.; Zhang, X. Regulation of TiO2 nanoarrays on titanium implants for enhanced osteogenic activity and immunomodulation. J. Mater. Sci. Technol. 2023, 150, 233–244. [Google Scholar] [CrossRef]
- Su, J.; Du, Z.; Xiao, L.; Wei, F.; Yang, Y.; Li, M.; Qiu, Y.; Liu, J.; Chen, J.; Xiao, Y. Graphene oxide coated Titanium Surfaces with Osteoimmunomodulatory Role to Enhance Osteogenesis. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 113, 110983. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Zhang, L.; Wang, D.; Liu, X.; Li, H.; Liang, C.; Zhao, X. Thermo-sensitive hydrogel on anodized titanium surface to regulate immune response. Surf. Coat. Technol. 2020, 405, 126624. [Google Scholar] [CrossRef]
- Chen, D.; Yu, C.; Ying, Y.; Luo, Y.; Ren, L.; Zhu, C.; Yang, K.; Wu, B.; Liu, Q. Study of the Osteoimmunomodulatory Properties of Curcumin-Modified Copper-Bearing Titanium. Molecules 2022, 27, 3205. [Google Scholar] [CrossRef]
- Liu, J.; Shi, Y.; Zhao, Y.; Liu, Y.; Yang, X.; Li, K.; Zhao, W.; Han, J.; Li, J.; Ge, S. A Multifunctional Metal-Phenolic Nanocoating on Bone Implants for Enhanced Osseointegration via Early Immunomodulation. Adv. Sci. 2024, 11, e2307269. [Google Scholar] [CrossRef]
- Doadrio, A.L.; Conde, A.; Arenas, M.A.; Hernández-López, J.M.; de Damborenea, J.J.; Pérez-Jorge, C.; Esteban, J.; Vallet-Regí, M. Use of anodized titanium alloy as drug carrier: Ibuprofen as model of drug releasing. Int. J. Pharm. 2015, 492, 207–212. [Google Scholar] [CrossRef]
- Shen, K.; Tang, Q.; Fang, X.; Zhang, C.; Zhu, Z.; Hou, Y.; Lai, M. The sustained release of dexamethasone from TiO2 nanotubes reinforced by chitosan to enhance osteoblast function and anti-inflammation activity. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 116, 111241. [Google Scholar] [CrossRef]
- Luo, J.; Ding, X.; Song, W.; Bai, J.-Y.; Liu, J.; Li, Z.; Meng, F.-H.; Chen, F.-H.; Zhang, Y.-M. Inducing macrophages M2 polarization by dexamethasone laden mesoporous silica nanoparticles from titanium implant surface for enhanced osteogenesis. Acta Metall. Sin. 2019, 32, 1253–1260. [Google Scholar] [CrossRef]
- Wei, Y.; Liu, Z.; Zhu, X.; Jiang, L.; Shi, W.; Wang, Y.; Xu, N.; Gang, F.; Wang, X.; Zhao, L.; et al. Dual directions to address the problem of aseptic loosening via electrospun PLGA @ aspirin nanofiber coatings on titanium. Biomaterials 2020, 257, 120237. [Google Scholar] [CrossRef]
- You, Y.; Wang, W.; Li, Y.; Song, Y.; Jiao, J.; Wang, Y.; Chen, B.; Liu, J.; Qi, H.; Liang, Y. Aspirin/PLGA coated 3D-printed Ti-6Al-4V alloy modulate macrophage polarization to enhance osteoblast differentiation and osseointegration. J. Mater. Sci. Mater. Med. 2022, 33, 73. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhang, Y.; Xiao, L.; Lu, H.; Ma, Y.; Liu, Q.; Wang, X. Surface engineering of titania nanotubes incorporated with double-layered extracellular vesicles to modulate inflammation and osteogenesis. Regen. Biomater. 2021, 8, rbab010. [Google Scholar] [CrossRef]
- Jayasree, A.; Liu, C.; Salomon, C.; Ivanovski, S.; Gulati, K.; Han, P. Microvesicle-eluting nano-engineered implants influence inflammatory response of keratinocytes. Drug. Deliv. Transl. Res. 2023. online ahead of print. [Google Scholar]
- Silva, R.C.S.; Agrelli, A.; Andrade, A.N.; Mendes-Marques, C.L.; Arruda, I.R.S.; Santos, L.R.L.; Vasconcelos, N.F.; Machado, G. Titanium Dental Implants: An Overview of Applied Nanobiotechnology to Improve Biocompatibility and Prevent Infections. Materials 2022, 15, 3150. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Periodontol. 2018, 89, 267–290. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, 286–291. [Google Scholar] [CrossRef]
- Derks, J.; Schaller, D.; Håkansson, J.; Wennström, J.L.; Tomasi, C.; Berglundh, T. Peri-implantitis—Onset and pattern of progression. J. Clin. Periodontol. 2016, 43, 383–388. [Google Scholar] [CrossRef]
- Schwarz, F.; Ramanauskaite, A. It is all about peri-implant tissue health. Periodontol. 2000 2022, 88, 9–12. [Google Scholar] [CrossRef]
- Moraes, G.; Zambom, C.; Siqueira, W.L. Nanoparticles in Dentistry: A Comprehensive Review. Pharmaceuticals 2021, 14, 752. [Google Scholar] [CrossRef]
- Lagopati, N.; Efstathopoulos, E.P.; Veroutis, D.; Katifelis, H.; Theocharous, G.; Pantelis, P.; Evangelou, K.; Gorgoulis, V.G.; Gazouli, M. Hybrid Multifunctional Nanomaterials for Diagnostic and Therapeutic Applications. In Pharmaceutical Nanobiotechnology for Targeted Therapy, 1st ed.; Barabadi, H., Mostafavi, E., Saravanan, M., Eds.; Nanotechnology in the Life Sciences; Springer: Cham, Sawitzerland, 2022; pp. 489–519. [Google Scholar]
- Lagopati, N.; Pippa, N.; Gatou, M.-A.; Papadopoulou-Fermeli, N.; Gorgoulis, V.G.; Gazouli, M.; Pavlatou, E.A. Marine-Originated Materials and Their Potential Use in Biomedicine. Appl. Sci. 2023, 13, 9172. [Google Scholar] [CrossRef]
- Gatou, M.-A.; Skylla, E.; Dourou, P.; Pippa, N.; Gazouli, M.; Lagopati, N.; Pavlatou, E.A. Magnesium Oxide (MgO) Nanoparticles: Synthetic Strategies and Biomedical Applications. Crystals 2024, 14, 215. [Google Scholar] [CrossRef]
- Puckett, S.D.; Taylor, E.; Raimondo, T.; Webster, T.J. The relationship between the nanostructure of titanium surfaces and bacterial attachment. Biomaterials 2010, 31, 706–713. [Google Scholar] [CrossRef]
- Cao, H.; Liu, X.; Meng, F.; Chu, P.K. Biological actions of silver nanoparticles embedded in titanium controlled by micro-galvanic effects. Biomaterials 2011, 32, 693–705. [Google Scholar] [CrossRef]
- Zhu, Y.; Cao, H.; Qiao, S.; Wang, M.; Gu, Y.; Luo, H.; Meng, F.; Liu, X.; Lai, H. Hierarchical micro/nanostructured titanium with balanced actions to bacterial and mammalian cells for dental implants. Int. J. Nanomed. 2015, 10, 6659–6674. [Google Scholar] [CrossRef]
- Lampé, I.; Beke, D.; Biri, S.; Csarnovics, I.; Csik, A.; Dombrádi, Z.; Hajdu, P.; Hegedűs, V.; Rácz, R.; Varga, I.; et al. Investigation of silver nanoparticles on titanium surface created by ion implantation technology. Int. J. Nanomed. 2019, 14, 4709–4721. [Google Scholar] [CrossRef]
- Liu, X.; Man, H.C. Laser fabrication of Ag-HA nanocomposites on Ti6Al4V implant for enhancing bioactivity and antibacterial capability. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 70, 1–8. [Google Scholar] [CrossRef]
- Gosau, M.; Haupt, M.; Thude, S.; Strowitzki, M.; Schminke, B.; Buergers, R. Antimicrobial effect and biocompatibility of novel metallic nanocrystalline implant coatings. J. Biomed. Mater. Res. B Appl. Biomater. 2016, 104, 1571–1579. [Google Scholar] [CrossRef]
- Hameed, H.A.; Ariffin, A.; Luddin, N.; Husein, A. Evaluation of antibacterial properties of copper nanoparticles surface coating on titanium dental implant. J. Pharm. Sci. Res. 2018, 10, 1157–1160. [Google Scholar]
- Liu, M.; Zhou, J.; Yang, Y.; Zheng, M.; Yang, J.; Tan, J. Surface modification of zirconia with polydopamine to enhance fibroblast response and decrease bacterial activity in vitro: A potential technique for soft tissue engineering applications. Colloids Surf. B Biointerfaces 2015, 136, 74–83. [Google Scholar] [CrossRef]
- Zhao, L.; Wang, H.; Huo, K.; Cui, L.; Zhang, W.; Ni, H.; Zhang, Y.; Wu, Z.; Chu, P.K. Antibacterial nano-structured titania coating incorporated with silver nanoparticles. Biomaterials 2011, 32, 5706–5716. [Google Scholar] [CrossRef]
- Huo, K.; Zhang, X.; Wang, H.; Zhao, L.; Liu, X.; Chu, P.K. Osteogenic activity and antibacterial effects on titanium surfaces modified with Zn-incorporated nanotube arrays. Biomaterials 2013, 34, 3467–3478. [Google Scholar] [CrossRef]
- Wang, R.; Shi, M.; Xu, F.; Qiu, Y.; Zhang, P.; Shen, K.; Zhao, Q.; Yu, J.; Zhang, Y. Graphdiyne-modified TiO2 nanofibers with osteoinductive and enhanced photocatalytic antibacterial activities to prevent implant infection. Nat. Commun. 2020, 11, 4465. [Google Scholar] [CrossRef]
- Gulati, K.; Ramakrishnan, S.; Aw, M.S.; Atkins, G.J.; Findlay, D.M.; Losic, D. Biocompatible polymer coating of titania nanotube arrays for improved drug elution and osteoblast adhesion. Acta Biomater. 2012, 8, 449–456. [Google Scholar] [CrossRef]
- Kumeria, T.; Mon, H.; Aw, M.S.; Gulati, K.; Santos, A.; Griesser, H.J.; Losic, D. Advanced biopolymer-coated drug-releasing titania nanotubes (TNTs) implants with simultaneously enhanced osteoblast adhesion and antibacterial properties. Colloids Surf. B Biointerfaces 2015, 130, 255–263. [Google Scholar] [CrossRef]
- Baghdan, E.; Pinnapireddy, S.; Vögeling, H.; Schaefer, J.; Eckert, A.; Bakowsky, U. Nano spray drying: A novel technique to prepare well-defined surface coatings for medical implants. J. Drug Deliv. Sci. Technol. 2018, 48, 145–151. [Google Scholar] [CrossRef]
- Ma, M.; Kazemzadeh-Narbat, M.; Hui, Y.; Lu, S.; Ding, C.; Chen, D.D.; Hancock, R.E.; Wang, R. Local delivery of antimicrobial peptides using self-organized TiO2 nanotube arrays for peri-implant infections. J. Biomed. Mater. Res. A 2012, 100, 278–285. [Google Scholar] [CrossRef]
- Srivastava, M.G.; Kamarudin, N.H.N.; Aktan, M.K.; Zheng, K.; Zayed, N.; Yongabi, D.; Wagner, P.; Teughels, W.; Boccaccini, A.R.; Braem, A. pH-Triggered Controlled Release of Chlorhexidine Using Chitosan-Coated Titanium Silica Composite for Dental Infection Prevention. Pharmaceutics 2024, 16, 377. [Google Scholar] [CrossRef]
- Cheng, Y.F.; Zhang, J.Y.; Wang, Y.B.; Li, C.M.; Lu, Z.S.; Hu, X.F.; Xu, L.Q. Deposition of catechol-functionalized chitosan and silver nanoparticles on biomedical titanium surfaces for antibacterial application. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 98, 649–656. [Google Scholar] [CrossRef]
- Mishra, S.K.; Ferreira, J.M.; Kannan, S. Mechanically stable antimicrobial chitosan-PVA-silver nanocomposite coatings deposited on titanium implants. Carbohydr. Polym. 2015, 121, 37–48. [Google Scholar] [CrossRef]
- Song, J.; Chen, Q.; Zhang, Y.; Diba, M.; Kolwijck, E.; Shao, J.; Jansen, J.A.; Yang, F.; Boccaccini, A.R.; Leeuwenburgh, S.C. Electrophoretic deposition of chitosan coatings modified with gelatin nanospheres to tune the release of antibiotics. ACS Appl. Mater. Interfaces 2016, 8, 13785–13792. [Google Scholar] [CrossRef]
- Choi, S.H.; Jang, Y.S.; Jang, J.H.; Bae, T.S.; Lee, S.J.; Lee, M.H. Enhanced antibacterial activity of titanium by surface modification with polydopamine and silver for dental implant application. J. Appl. Biomater. Funct. Mater. 2019, 17, 2280800019847067. [Google Scholar] [CrossRef]
- Palla-Rubio, B.; Araújo-Gomes, N.; Fernández-Gutiérrez, M.; Rojo, L.; Suay, J.; Gurruchaga, M.; Goñi, I. Synthesis and characterization of silica-chitosan hybrid materials as antibacterial coatings for titanium implants. Carbohydr. Polym. 2019, 203, 331–341. [Google Scholar] [CrossRef]
- Xu, G.; Shen, X.; Dai, L.; Ran, Q.; Ma, P.; Cai, K. Reduced bacteria adhesion on octenidine loaded mesoporous silica nanoparticles coating on titanium substrates. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 70, 386–395. [Google Scholar] [CrossRef]
- Li, Y.; Liu, X.; Tan, L.; Cui, Z.; Yang, X.; Yeung, K.W.K.; Pan, H.; Wu, S. Construction of N-halamine labeled silica/zinc oxide hybrid nanoparticles for enhancing antibacterial ability of Ti implants. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 76, 50–58. [Google Scholar] [CrossRef]
- Kulshrestha, S.; Khan, S.; Meena, R.; Singh, B.R.; Khan, A.U. A graphene/zinc oxide nanocomposite film protects dental implant surfaces against cariogenic Streptococcus mutans. Biofouling 2014, 30, 1281–1294. [Google Scholar] [CrossRef]
- De Leo, V.; Mattioli-Belmonte, M.; Cimmarusti, M.T.; Panniello, A.; Dicarlo, M.; Milano, F.; Agostiano, A.; De Giglio, E.; Catucci, L. Liposome-modified titanium surface: A strategy to locally deliver bioactive molecules. Colloids Surf. B Biointerfaces 2017, 158, 387–396. [Google Scholar] [CrossRef]
- Nagay, B.E.; Cordeiro, J.M.; Barao, V.A.R. Insight Into Corrosion of Dental Implants: From Biochemical Mechanisms to Designing Corrosion-Resistant Materials. Curr. Oral Health Rep. 2022, 9, 7–21. [Google Scholar] [CrossRef]
- Guo, T.; Scimeca, J.C.; Ivanovski, S.; Verron, E.; Gulati, K. Enhanced Corrosion Resistance and Local Therapy from Nano-Engineered Titanium Dental Implants. Pharmaceutics 2023, 15, 315. [Google Scholar] [CrossRef]
- Indira, K.; Mudali, U.K.; Rajendran, N. In-vitro biocompatibility and corrosion resistance of strontium incorporated TiO2 nanotube arrays for orthopaedic applications. J. Biomater. Appl. 2014, 29, 113–129. [Google Scholar] [CrossRef]
- Al-Saady, F.; Rushdi, S.; Abbar, A. Improvement the corrosion Behavior of Titanium by Nanotubular Oxide in a simulated saliva solution. IOP Conf. Ser. Mater. Sci. Eng. 2020, 870, 012060. [Google Scholar] [CrossRef]
- Azari, R.; Rezaie, H.R.; Khavandi, A. Effect of titanium dioxide intermediate layer on scratch and corrosion resistance of sol-gel-derived HA coating applied on Ti-6Al-4V substrate. Prog. Biomater. 2021, 10, 259–269. [Google Scholar] [CrossRef]
- Shen, Y.; Fang, K.; Xiang, Y.; Xu, K.; Yu, L.; Chen, J.; Ma, P.; Cai, K.; Shen, X.; Liu, J. Improvement in osteogenesis, vascularization, and corrosion resistance of titanium with silicon-nitride doped micro-arc oxidation coatings. Front. Bioeng. Biotechnol. 2022, 10, 1023032. [Google Scholar] [CrossRef]
- Afrouzian, A.; Avila, J.D.; Bandyopadhyay, A. Biotribocorrosion of 3D-Printed silica-coated Ti6Al4V for load-bearing implants. J. Mater. Res. 2021, 36, 3974–3984. [Google Scholar] [CrossRef]
- Hsu, S.M.; Fares, C.; Xia, X.; Rasel, M.A.J.; Ketter, J.; Afonso Camargo, S.E.; Haque, M.A.; Ren, F.; Esquivel-Upshaw, J.F. In Vitro Corrosion of SiC-Coated Anodized Ti Nano-Tubular Surfaces. J. Funct. Biomater. 2021, 12, 52. [Google Scholar] [CrossRef]
- Harb, S.V.; Bassous, N.J.; de Souza, T.A.C.; Trentin, A.; Pulcinelli, S.H.; Santilli, C.V.; Webster, T.J.; Lobo, A.O.; Hammer, P. Hydroxyapatite and β-TCP modified PMMA-TiO2 and PMMA-ZrO2 coatings for bioactive corrosion protection of Ti6Al4V implants. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 116, 111149. [Google Scholar] [CrossRef]
- Kazemi, M.; Ahangarani, S.H.; Esmailian, M.; Shanaghi, A. Investigation on the corrosion behavior and biocompatibility of Ti-6Al-4V implant coated with HA/TiN dual layer for medical applications. Surf. Coat. Technol. 2020, 397, 126044. [Google Scholar] [CrossRef]
- Aydin, B.A.; Siğircik, G.; Takci, H. Antimicrobial properties and corrosion behavior of TiO2-NTs electrodes modified with Ag and ZnO nanorod in simulated body fluid solution. J. Mol. Struct. 2021, 1240, 130569. [Google Scholar] [CrossRef]
- Xia, C.; Ma, X.; Zhang, X.; Li, K.; Tan, J.; Qiao, Y.; Liu, X. Enhanced physicochemical and biological properties of C/Cu dual ions implanted medical titanium. Bioact. Mater. 2020, 5, 377–386. [Google Scholar] [CrossRef]
- Zheng, Y.F.; Liu, D.; Liu, X.L.; Li, L. Enhanced corrosion resistance of Zr coating on biomedical TiNi alloy prepared by plasma immersion ion implantation and deposition. Appl. Surf. Sci. 2008, 255, 512–514. [Google Scholar] [CrossRef]
- Yusuf, D.; Maryani, E.; Mardhian, D.F.; Noviyanti, A.R. Evaluation of Structural Stability, Mechanical Properties, and Corrosion Resistance of Magnesia Partially Stabilized Zirconia (Mg-PSZ). Molecules 2023, 28, 6054. [Google Scholar] [CrossRef]
- Zaher, H.; Hefnawy, M.A.; Medany, S.; Kamel, S.; Fadl-allah, S. Synergetic effect of essential oils and calcium phosphate nanoparticles for enhancement the corrosion resistance of titanium dental implant. Sci. Rep. 2024, 14, 1573. [Google Scholar] [CrossRef]
| Studies with Nanomaterials for Osseointegration Improvement | |||
|---|---|---|---|
| Study | Method | Nanomaterial | Result |
| Yang et al., 2020 [12] | In vitro and in vivo | TNTs | Reversed overproduction of ROS, antioxidant effect |
| Balasundaram et al., 2007 [34] | In vitro | TNTs loaded with BMP-2 | Increased osteoblast adhesion |
| Kodama et al., 2009 [35] | In vitro | TNTs loaded with synthetic HA | Enhanced BIC and apatite formation |
| Liu et al., 2014 [36] | In vitro | TNTs loaded with BSA | Preservation of crestal bone, conductivity for soft tissue attachment, antibacterial properties |
| 6Lee et al., 2011 [37] | In vitro and In vivo | TNTs loaded with ibandronate | Higher removal torque values, increased bone density and bone formation markers expression |
| Shen et al., 2016 [38] | In vitro and in vivo | TNTs and HA loaded with alendronate | In vitro inhibition of osteoclast differentiation and the improvement of osteoblast activity and in vivo early local osseointegration and mechanical fixation |
| Zhang et al., 2014 [40] | In vitro and In vivo | TNTs loaded with rhPDGF-BB | Enhanced MSC adhesion, proliferation and differentiation, rapid bone formation |
| Lee et al., 2013 [41] | In vivo | TNTs loaded with NAC peptide | New bone formation, excellent osseointegration |
| Zhang et al., 2020 [42] | In vitro | TNTs loaded with Sr-La | Superior osseointegration ability and increased cellular functions |
| Lee et al., 2017 [45] | In vitro and in vivo | Chitosan-Au NPs with PRAγ cDNA | Regional bone regeneration and improved osseointegration |
| Fang et al., 2014 [46] | In vitro | Chitosan loaded with Sema 3A | Higher osteogenic gene expression and Ca apposition |
| Yamada et al., 2012 [47] | In vivo | Nano-HA on microroughened implants | Increased strength at bone implant interface, higher BIC and bone volume |
| Zhao et al., 2011 [48] | In vitro and in vivo | Nano-HA Mg doped | In vitro promotion of osteogenesis and in vivo improvement of osseointegration |
| Heo et al., 2016 [49] | In vitro and in vivo | GNP coating | In vitro stimulated cellular responses and in vivo enhance new bone formation |
| Qiao et al., 2015 [50] | In vitro and in vivo | AgNPs | Increased implant stability and enhanced bone formation |
| Bartkowiak et al., 2018 [51] | In vitro | SiNPs on HA treated implants | Favorable mineralization of deposited bone matrix and accelerated bone healing |
| Jo et al., 2017 [52] | In vitro and in vivo | SiNPs | Increase microroughness, osteopromotive conditions |
| Covarrubias et al., 2016 [53] | In vitro and in vivo | Nanoporous silica coating loaded with bioactive glass nanoparticles (nBG/NSC) on Ti implants | Accelerate the formation of bone tissue in the periphery of the implant after 3 weeks of implantation. |
| Vandamme et al., 2020 [54] | In vivo | Mesoporous SiO2 customization on Ti implants | Does not seem to compromise the osseointegration process. |
| Frankenberger et al., 2021 [55] | In vivo | Nanocrystalline hydroxyapatite (ncHA) embedded in a silica matrix and interfacial composite layer (SPI) on PEEK implants | Higher bone to implant contact (BIC) and pull-out tests revealed higher pull-out forces. |
| Frandsen et al., 2011 [56] | In vitro | Zirconia nanotubes | Enhanced cell adhesion and spreading and improved osteoblast growth |
| Wang et al., 2019 [57] | In vitro | GO | Increased surface wettability and apatite formation |
| Studies with Nanomaterials for Immunomodulation | |||
|---|---|---|---|
| Study | Method | Nanomaterial | Result |
| Kang et al., 2010 [64] | In vitro | PEG and BMP-2 on Ti implants | Non-biofouling and simultaneous osteoconductive properties. |
| Smith et al., 2013 [65] | In vitro | TNTs | Decrease in monocyte, macrophage and neutrophil functionality and reduced stimulation of immune responses. |
| Neascu et al., 2015 [66] | In vitro | TNTs | Suppression of MAPK and NF-κB pathways, potential mechanism for anti-inflammatory activity. |
| Gulati et al., 2018 [67] | In vitro | nanopores | Reduced proliferation of macrophages, increased osteoblast and fibroblast activity. |
| Li et al., 2023 [68] | In vitro | TiO2 nanoarrays with different morphologies in titanium. | TiO2 nanorods with a larger diameter promotes osteogenic differentiation of BMSCs and stimulates macrophage polarization to M2 generating an immune microenvironment. |
| Su et al., 2020 [69] | In vitro | Graphene oxide (GO) coating in titanium surfaces | Manipulate the polarization of macrophages and the expression of inflammatory cytokines. lmmunomodulatory effects in osteogenesis. |
| Li et al., 2020 [70] | In vitro | Thermo-sensitive hydrogel on anodized Ti surfaces | Macrophages polarize toward the M2 phenotype, promotes tissue repair and osteoblast differentiation. |
| Chen et al., 2022 [71] | In vitro | Curcumin loaded through polydopamine (PDA) onto copper-bearing titanium alloy (Cu-Ti) | Immune regulation of macrophages through regulation of their polar differentiation. |
| Liu et al., 2024 [72] | In vitro and in vivo | Metal phenolic nanocoating consisting of tannic acid and strontium on Ti substrates | Antioxidant properties, accelerated osteogenic differentiation, inhibition of inflammatory responses. |
| Doadrio et al., 2015 [73] | In vitro | TNTs and ibuprofen | Confirmation of the ability of TNTs to act as an intelligent nanomaterial |
| Shen et al., 2020 [74] | In vitro | TNT-Cht and DEX | Enhanced proliferation and differentiation of osteoblasts, suppressed production of nitric oxide (NO) and pro-inflammatory cytokines from macrophages. |
| Luo et al., 2019 [75] | In vitro | MSNs + DEX | M2-polarization of macrophages, favorable osteogenesis but dose dependent toxicity. |
| Wei et al., 2020 [76] | In vitro and in vivo | PLGA nanofibers loaded with aspirin | In vitro inhibition of M1 polarization and increased proliferation and differentiation of MSCs to osteoblasts, in vivo enhanced osseointegration. |
| You et al., 2022 [77] | In vitro and in vivo | PLGA loaded with aspirin in 3D printed Ti alloy implants | In vitro enhanced M2 gene and protein expression and in vivo superior osseointegration. |
| Zhao et al., 2021 [78] | In vitro | Double layer customization on TNTs Internal layer: MSC-derived exosomes on polydopamine External layer: 3-day differentiated MSC-derived exosomes on hydrogel | Enhances the migration and osteogenic differentiation of hBMSCs. Modulation of macrophage polarization. |
| Jayasree et al., 2023 [79] | In vitro | TNTs loaded with microvessels (MVs) | Controlled local release pattern for up to 7 days. Reduction in the production of pro-inflammatory cytokines in keratinocytes. |
| Studies with Nanomaterials for the Prevention of Peri-Implantitis | |||
|---|---|---|---|
| Study | Method | Nanomaterial | Result |
| Puckett et al., 2010 [89] | In vitro | Nanorough Ti surfaces from electron beam evaporation | Decreased bacterial adhesion especially of S. aureus, S. epidermidis and P. aeruginosa. |
| Cao et al., 2011 [90] | In vitro | AgNPs | Inhibition of S. aureus and E. coli growth and enhanced antibacterial activity of the surface due to micro galvanic effects. The amounts of S. aureus and E. coli on 0.5h-Ag-PIII are reduced by approximately 93% and 95% after 24 h. |
| Zhu et al., 2015 [91] | In vitro | AgNPs | Anti-bacterial activity against gram-positive S. aureus and gram-negative F. nucleatum. The antibacterial activity of Ag NPs against F. nucleatum was superior to S. aureus. |
| Lampé et al., 2019 [92] | In vitro | AgNPs | 64.6% of antibacterial effect was noted for the nanoparticle-covered samples. |
| Liu et al., 2017 [93] | In vitro | AgNPs contained in HA | Bacterial inhibition for percentage of 2% silver. |
| Gosau et al., 2015 [94] | In vitro | Nanocrystalline Ag, Cu and Bis coating | Favorable anti-bacterial effects, but cytotoxicity for Cu. |
| Hameed et al., 2018 [95] | In vitro | CuNPs | Enhanced antibacterial effect against P. gingivalis. |
| Liu et al., 2015 [96] | In vitro | Polydopamine (PDA) coated zirconia | Increased cell adhesion and proliferation. The number of adherent bacteria decreased significantly on zirconia after PDA coating. The PDA coated zirconia showed both lower percentages of S. gordonii (0.91 ± 0.16%) and S. mutans (1.85 ± 0.48%) than the pristine zirconia (1.73 ± 0.32% and 3.06 ± 0.47%) (p < 0.01). |
| Zhao et al., 2011 [97] | In vitro | TNTs loaded with AgNPs | TNTs kill planktonic bacteria for the first days after surgery and inhibit bacterial adhesion for 30 days. |
| Huo et al., 2013 [98] | In vitro | TNTs loaded with Zn | Good intrinsic antibacterial properties with simultaneous favorable soft and hard tissue integration. |
| Wang et al., 2020 [99] | In vitro and in vivo | graphdiyne (GDY) composite TiO2 nanofiber coating | Increased photocatalysis and prolonged antibacterial ability, especially against methicillin-resistant staphylococcus aureus (MRSA). ROS release from this system prevented the formation of biofilm. In standard plate counting assay tests, the number of colonies of the TiO2/GDY + UV group reduced by 98% compared to that of the group not treated with UV |
| Gulati et al., 2012 [100] | In vitro | TNTs loaded with indomethacin and covered by chitosan/PLGA | Extended drug release properties, favorable bone cell adhesion and improved anti-bacterial properties. |
| Kumeria et al., 2015 [101] | In vitro | TNTs decorated with micelles loaded with gentamicin and covered by chitosan/PLGA | Long term and improved anti-bacterial properties, prevention of biofilm formation. |
| Baghdan et al., 2022 [102] | In vitro | PLGA loaded with norfloxacin on Ti discs | Up to 99.83% reduction in the number of viable bacterial colonies. |
| Ma et al., 2011 [103] | In vitro | TNTs loaded with AMPs | Reduction of gram-positive bacterium S. aureus levels and inhibition of bacterial adhesion on the implant surface. In survival assay tests, AMP loaded TNTs demonstrated bacterial killing with approximately 99.9% decrease. About 200-fold decrease of bacterial colonies was observed for the peptide-loaded groups compared with the groups without peptide. |
| Srivastava et al., 2024 [104] | In vitro | Macroporous Ti matrix is filled with mesoporous silica, coated with crosslinked chitosan releasing CHX | reduced numbers of bacterial growth compared to the uncoated Ti/SiO2 sample (S. sobrinus, F. nucleatum) |
| Cheng et al., 2019 [105] | In vitro | AgNPs on catechol-containing chitosan (CACS) coatings | Anti-bacterial properties of the system, both against gram-positive and gram-negative bacteria. |
| Mishra et al., 2017 [106] | In vitro | Cht-PVA-Silver nanocomposite coating | Better functional properties and enhanced bactericidal activity against S. aureus and E. coli. |
| Song et al., 2016 [107] | In vitro | Gelatin nanospheres loaded with antibiotics and encapsulated in chitosan matrix | Inhibition of bacterial growth. In inhibition zone tests the samples that contained moxifloxacin with or without gelatin nanospheres displayed an obvious inhibition zone whereas none of the groups with or without vancomycin induced the formation of an inhibition zone. |
| Choi et al., 2019 [108] | In vitro | AgNPs on PDA | Less bacteria colonization in Ag/PDA treated implants when compared with uncoated titanium surfaces, bacterial growth was found retarded in bacterial growth curves for S. mutans and P. gingivalis. |
| Palla-Rubio et al., 2019 [109] | In vitro | Silica—chitosan coating on Ti implants | Coatings with 5% and 10% of chitosan have particularly good bactericidal properties. |
| Xu et al., 2017 [110] | In vitro | MSNs loaded with OCT | Inhibition of bacterial adhesion was noted, especially for S. mutans and E. coli. The antibacterial ratios of S. aureus and E. coli were 21.5 ± 6.2% and 13.1 ± 4.8%, and 97.1 ± 0.8% and 86.3 ± 1.2%, in respect to MAO/Si substrates and MAO/Si/OCT substrates, respectively. |
| Li et al., 2017 [111] | In vitro | PSA nanoparticles, zinc oxide (ZnO) covered by a silica film on the outside and N-halamine polymer labeling | Excellent anti-bacterial activity against P. aeruginosa, E. coli and S. aureus with no obvious cytotoxicity. |
| Kulshrestha et al., 2014 [112] | In vitro | Graphene ZnO coating | Reduction in biofilm deposition. |
| De Leo et al., 2017 [113] | In vitro | Liposome coatings | The system can be utilized for the incorporation of various moieties with different polarities such as an antibiotics, anti-inflammatory drugs and protein like growth factors. |
| Studies with Nanomaterials for Corrosion Resistance | |||
|---|---|---|---|
| Study | Method | Nanomaterial | Result |
| Indira et al., 2004 [116] | In vitro | ZrNPs loaded in TNTs | Enhanced corrosion resistance. |
| Al-Saady et al., 2023 [117] | In vitro | Titanium oxide nanotubes | Enhanced corrosion resistance. |
| Azari et al., 2023 [118] | In vitro | HA coating with intermediateTiO2 layer on Ti6Al4V substrates | Intermediate layer reduces the corrosion current by 65 percent and improves the corrosion resistance of monolayer HA-coated Ti-6Al-4 V alloy. |
| Shen et al., 2022 [119] | In vitro | Silicon nitride (Si3N4) nanoparticles | Corrosion tendency and corrosion rate of Si3N4-doped specimens were significantly reduced, with Si3N4 concentration dependence. |
| Afrouzian et al., 2021 [120] | In vitro | Silica coating (SiO2) on the surface of Ti6Al4V alloy via 3D printing | Promising tribological performance. |
| Hsu et al., 2021 [121] | In vitro | Silicon carbide (SiC) on titanium dioxide nanotubes (ATO) | Improved corrosion resistance. |
| Harb et al., 2020 [122] | In vitro | PMMA-TiO2 and PMMA-ZrO2 nanocomposite coatings with calcium phosphates in Ti6Al4V implants | Excellent corrosion resistance in SBF solution. PMMA-TiO2-βTCP coating presented low frequency impedance modulus of 430 GΩ cm2 unchanged for 21 days. (>100 GΩ cm2 in coatings indicate very good anticorrosion protection). |
| Kazemi et al., 2020 [123] | In vitro | Titanium Nitride (TiN)-HA multilayer composite in Ti6Al4V implants | Lowest corrosion current density and highest corrosion potential. |
| Aydin et al., 2021 [124] | In vitro | TiO2 nanotubes modifies with ZnO nanorods and AgNPs | ZnO-TiO2 nanotubes exhibited high resistance value at immersion of 7 days. |
| Xia et al., 2020 [125] | In vitro | C/Cu NPs | Improved mechanical properties and reduction of free copper ions. The Cu ion release was regulated by the galvanic corrosion effect of the system, with no additional cytotoxicity induced. |
| Zheng et al., 2008 [126] | In vitro | Zr coating in TiNi alloy implant | Reduced Ni ion release and improved corrosion resistance was noted for Zr coated substrates. |
| Yusuf et al., 2023 [127] | In vitro | Nano Mg-PSZ partially stabilized zirconia | The greater the concentration of magnesia (MgO) in doping the ZrO2, the greater the degradation resistance of Mg-PSZ in simulated body fluid (SBF) solution. |
| Zaher et al., 2024 [128] | In vitro | Amorphous calcium phosphate nanoparticles (ACP-NPs) in Ti bare | Increased corrosion resistance. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marasli, C.; Katifelis, H.; Gazouli, M.; Lagopati, N. Nano-Based Approaches in Surface Modifications of Dental Implants: A Literature Review. Molecules 2024, 29, 3061. https://doi.org/10.3390/molecules29133061
Marasli C, Katifelis H, Gazouli M, Lagopati N. Nano-Based Approaches in Surface Modifications of Dental Implants: A Literature Review. Molecules. 2024; 29(13):3061. https://doi.org/10.3390/molecules29133061
Chicago/Turabian StyleMarasli, Chrysa, Hector Katifelis, Maria Gazouli, and Nefeli Lagopati. 2024. "Nano-Based Approaches in Surface Modifications of Dental Implants: A Literature Review" Molecules 29, no. 13: 3061. https://doi.org/10.3390/molecules29133061
APA StyleMarasli, C., Katifelis, H., Gazouli, M., & Lagopati, N. (2024). Nano-Based Approaches in Surface Modifications of Dental Implants: A Literature Review. Molecules, 29(13), 3061. https://doi.org/10.3390/molecules29133061







