Ephedrae Herba: A Review of Its Phytochemistry, Pharmacology, Clinical Application, and Alkaloid Toxicity
Abstract
1. Introduction
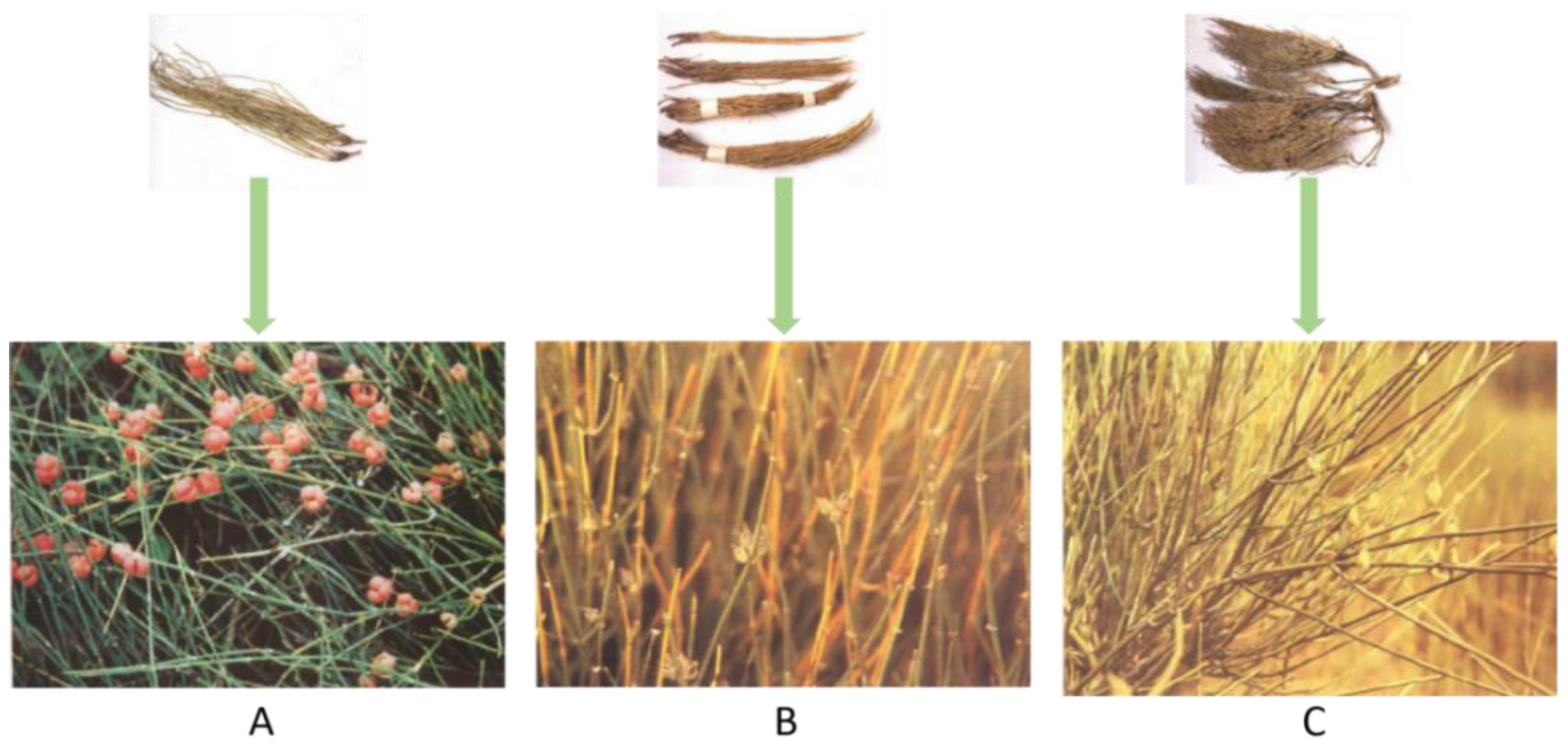
2. Phytochemistry
2.1. Alkaloids
2.2. Flavonoids
2.3. Tannins
2.4. Polysaccharides
2.5. Organic Acids
2.6. Organic Volatile Essential Oil
2.7. Other Ingredients
3. Pharmacological Effects
3.1. Antipyretic and Diaphoretic Effects
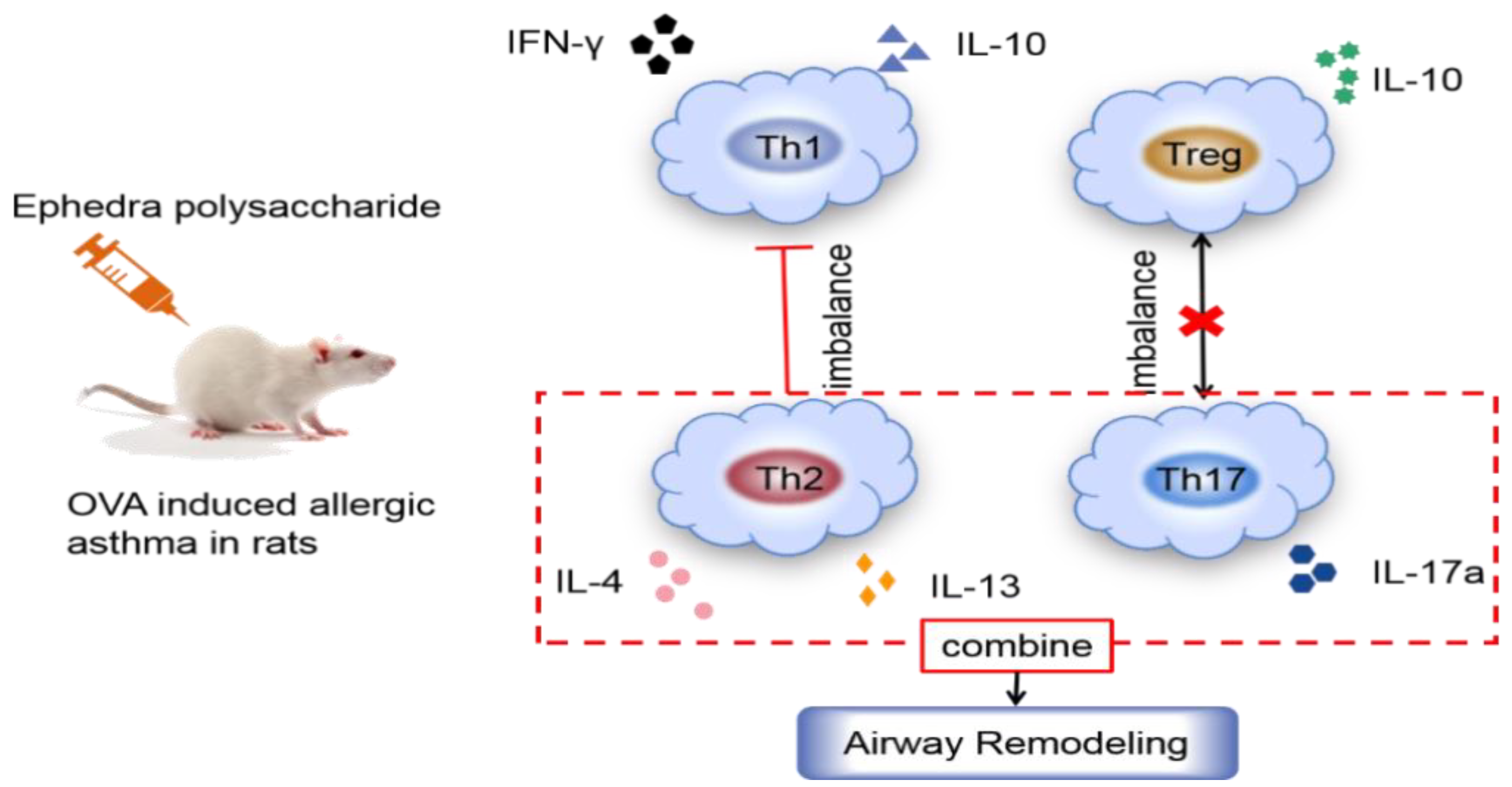
3.2. Inhibiting Asthma
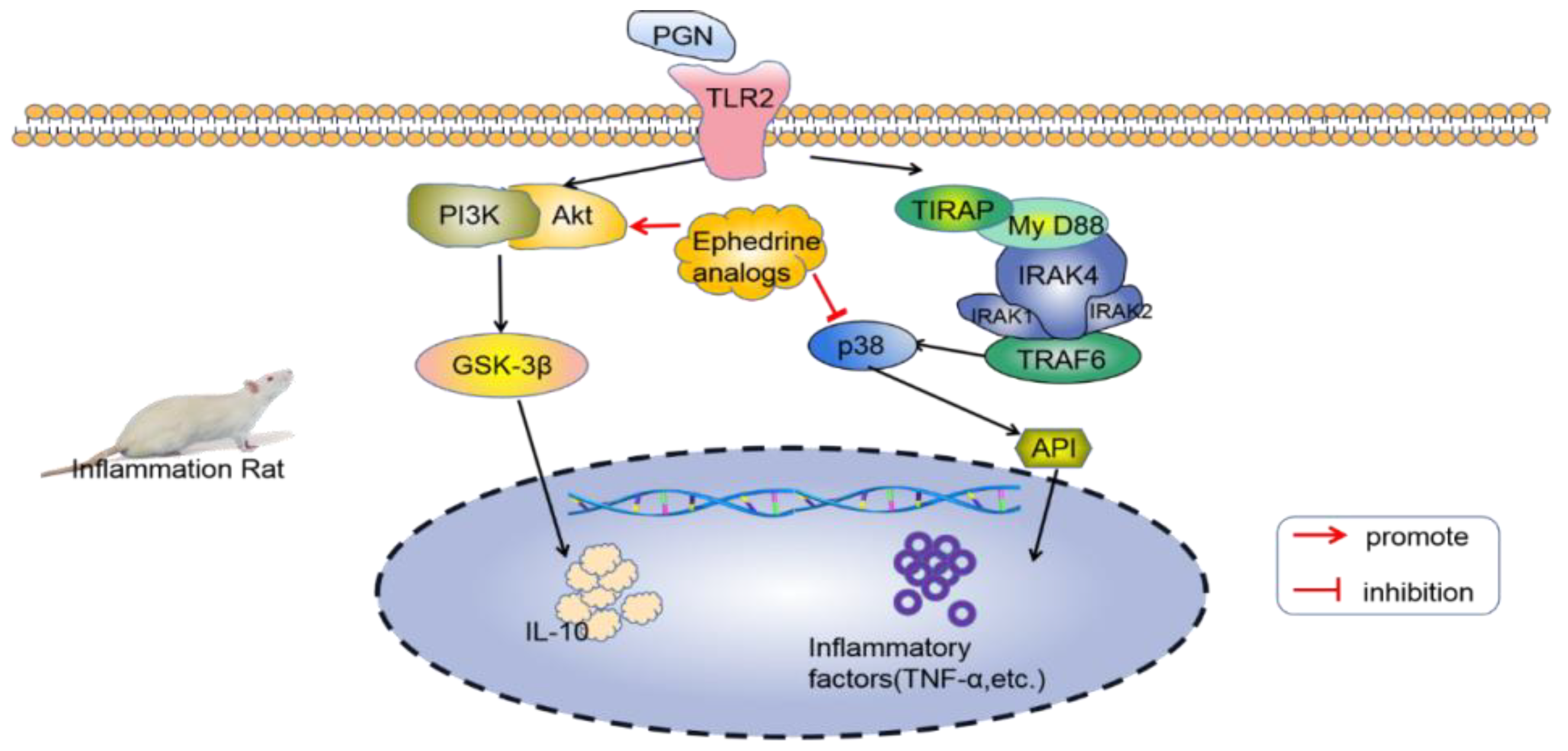
3.3. Anti-Inflammatory Effect
3.4. Hepatoprotection Effect
3.5. Antibacterial and Antifungal Effect
3.6. Anticancer and Analgesia
3.7. Antivirus Effect
4. Clinical Application
4.1. Treatment of Coronavirus Disease 2019 (COVID-19)
4.2. Treatment of Asthma
4.3. Raising Blood Pressure and Treating Muscle Weakness
4.4. Analgesic Effect
4.5. Treatment of Skin Diseases
4.6. Treatment of Gynecological Diseases
5. Alkaloid Toxicity
6. Conclusions and Future Perspective
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Xie, M.; Yang, Y.; Wang, B.; Wang, C. Interdisciplinary investigation on ancient Ephedra twigs from Gumugou Cemetery (3800 B.P.) in Xinjiang region, northwest China. Microsc. Res. Tech. 2013, 76, 663–672. [Google Scholar] [CrossRef]
- Nelson, R. FDA issues alert on ephedra supplements in the USA. Lancet 2004, 363, 135. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.Y.; Cao, L.H.; Kim, J.Y. Common responses in gene expression by Ephedra herba in brain and heart of mouse. Phytother. Res. 2011, 25, 1440–1446. [Google Scholar] [CrossRef] [PubMed]
- Andraws, R.; Chawla, P.; Brown, D.L. Cardiovascular effects of ephedra alkaloids: A comprehensive review. Prog. Cardiovasc. Dis. 2005, 47, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Dillon, P.F.; Root-Bernstein, R.S.; Lieder, C.M. Antioxidant-independent ascorbate enhancement of catecholamine inducedcontractions of vascular smooth muscle. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, 2353–2360. [Google Scholar] [CrossRef]
- Wan, J.Y.; Tian, Y.F.; Wan, H.T.; Yu, L.; Zhou, F.H.; Li, C.; He, Y. Pharmacokinetics of compatible effective components of Mahuang Decoction in febrile rats. Zhongguo Zhong Yao Za Zhi 2019, 44, 2149–2155. [Google Scholar] [PubMed]
- Takemoto, H.; Hyuga, S.; Takahashi, J.; Hyuga, S.; Odaguchi, H.; Uchiyama, N.; Maruyama, T.; Yamashita, T.; Hyuga, M.; Oshima, N.; et al. Ephedrine Alkaloids-Free Ephedra Herb Extract, EFE, Has No Adverse Effects Such as Excitation, Insomnia, and Arrhythmias. Biol. Pharm. Bull. 2018, 41, 247–253. [Google Scholar] [CrossRef]
- Pellati, F.; Benvenuti, S. Determination of ephedrine alkaloids in Ephedra natural products using HPLC on a pentafluorophenylpropyl stationary phase. J. Pharm. Biomed. Anal. 2008, 48, 254–263. [Google Scholar] [CrossRef]
- Roman, M.C. Determination of ephedrine alkaloids in botanicals and dietary supplements by HPLC-UV: Collaborative study. J. AOAC Int. 2004, 87, 1–14. [Google Scholar] [CrossRef]
- Gul, R.; Jan, S.U.; Faridullah, S.; Sherani, S.; Jahan, N. Preliminary Phytochemical Screening, Quantitative Analysis of Alkaloids, and Antioxidant Activity of Crude Plant Extracts from Ephedra intermedia Indigenous to Balochistan. Sci. World J. 2017, 2017, 5873648. [Google Scholar] [CrossRef]
- Ibragic, S.; Sofić, E. Chemical composition of various Ephedra species. Bosn. J. Basic Med. Sci. 2015, 15, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Kurosawa, W.; Kan, T.; Fukuyama, T. Stereocontrolled total synthesis of (-)-ephedradine A (orantine). J. Am. Chem. Soc. 2003, 125, 8112–8113. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Hesse, M. The spermine alkaloids of Chaenorhinum minus. Planta Med. 1988, 54, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Nezbedová, L.; Hesse, M.; Drandarov, K.; Werner, C. Dihydroxyverbacine is the terminal precursor in the biosynthesis of aphelandrine and orantine. Tetrahedron. Lett. 2000, 41, 7859–7862. [Google Scholar] [CrossRef]
- Hikino, H.; Kiso, Y.; Ogata, M.; Konno, C.; Aisaka, K.; Kubota, H.; Hirose, N.; Ishihara, T. Pharmacological actions of analogues of feruloylhistamine, an imidazole alkaloid of Ephedra roots. Planta Med. 1984, 50, 478–480. [Google Scholar] [CrossRef] [PubMed]
- Aghdasi, M.; Bojnoordi, M.M.; Mianabadi, M.; Nadaf, M. Chemical components of the Ephedra major from Iran. Nat. Prod. Res. 2016, 30, 369–371. [Google Scholar] [CrossRef]
- Ballero, M.; Foddis, C.; Sanna, C.; Scartezzini, P.; Poli, F.; Petitto, V.; Serafini, M.; Stanzione, A.; Bianco, A.; Serilli, A.M.; et al. Pharmacological activities on Ephedra nebrodensis Tineo. Nat. Prod. Res. 2010, 24, 1115–1124. [Google Scholar] [CrossRef]
- Groves, R.A.; Hagel, J.M.; Zhang, Y.; Kilpatrick, K.; Levy, A.; Marsolais, F.; Lewinsohn, E.; Sensen, C.W.; Facchini, P.J. Transcriptome profiling of khat (Catha edulis) and Ephedra sinica reveals gene candidates potentially involved in amphetamine-type alkaloid biosynthesis. PLoS ONE 2015, 10, e0119701. [Google Scholar] [CrossRef] [PubMed]
- Hikino, H.; Konno, C.; Takata, H.; Tamada, M. Antiinflammatory principle of Ephedra Herbs. Chem. Pharm. Bull. 1980, 28, 2900–2904. [Google Scholar] [CrossRef]
- Krizevski, R.; Bar, E.; Shalit, O.R.; Levy, A.; Hagel, J.M.; Kilpatrick, K.; Marsolais, F.; Facchini, P.J.; Ben-Shabat, S.; Sitrit, Y.; et al. Benzaldehyde is a precursor of phenylpropylamino alkaloids as revealed by targeted metabolic profiling and comparative biochemical analyses in Ephedra spp. Phytochemistry 2012, 81, 71–79. [Google Scholar] [CrossRef]
- Abdel-Kader, M.S.; Kassem, F.F.; Abdallah, R.M. Two alkaloids from Ephedra aphylla growing in Egypt. Nat. Prod. Sci. 2003, 9, 52–55. [Google Scholar]
- Zhang, D.; Deng, A.J.; Ma, L.; Li, Z.H.; Zhang, Z.H.; Jiang, J.D.; Qin, H.L. Phenylpropanoids from the stems of Ephedra sinica. J. Asian Nat. Prod. Res. 2016, 18, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Al-Khalil, S.; Alkofahi, A.; el-Eisawi, D.; al-Shibib, A. Transtorine, a new quinoline alkaloid from Ephedra transitoria. J. Nat. Prod. 1998, 61, 262–263. [Google Scholar] [CrossRef] [PubMed]
- Starratt, A.N.; Caveney, S. Quinoline-2-carboxylic acids from Ephedra species. Phytochemistry 1996, 42, 1477–1478. [Google Scholar] [CrossRef]
- Nawwar, M.A.M.; Barakat, H.H.; Buddrust, J.; Linscheidt, M. Alkaloidal, lignan and phenolic constituents of Ephedra alata. Phytochemistry 1985, 24, 878–879. [Google Scholar] [CrossRef]
- Hussein, S.A.M.; Barakat, H.H.; Nawar, M.A.M.; Willuhn, G. Flavonoids from Ephedra aphylla. Phytochemistry 1997, 45, 1529–1532. [Google Scholar] [CrossRef]
- Starratt, A.N.; Caveney, S. Four cyclopropane amino acids from Ephedra. Phytochemistry 1995, 40, 479–481. [Google Scholar] [CrossRef]
- Tamada, M.; Endo, K.; Hikino, H. Maokonine, hypertensive principle of Ephedra roots. Planta Med. 1978, 34, 291–293. [Google Scholar] [CrossRef]
- Zhao, W.; Deng, A.J.; Du, G.H.; Zhang, J.L.; Li, Z.H.; Qin, H.L. Chemical constituents of the stems of Ephedra sinica. J. Asian Nat. Prod. Res. 2009, 11, 168–171. [Google Scholar] [CrossRef]
- Khan, I.A.; Abourashed, E.A. Leung’s Encyclopedia of Common Natural Ingredients: Used in Food, Drugs and Cosmetics; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Fan, Y.B. The Research on Activity of Non-Alkaloid in Ephedra; Hubei University of Chinese Medicine: Wuhan, China, 2010. [Google Scholar]
- Chen, A.L.; Stuart, E.H.; Chen, K.K. The occurrence of methylbenzylamine in the extract of Ma Huang. J. Pharm. Sci. 1931, 20, 339–345. [Google Scholar] [CrossRef]
- Al-Rimawi, F.; Abu-Lafi, S.; Abbadi, J.; Alamarneh, A.A.A.; Sawahreh, R.A.; Odeh, I. Analysis Of Phenolic And Flavonoids Of Wild Ephedra Alata Plant Extracts By Lc/Pda And Lc/Ms And Their Antioxidant Activity. Afr. J. Tradit. Complement. Altern. Med. AJTCAM 2017, 14, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fu, W.; Wang, Z.B.; Kuang, H.X.; Wang, Q.H. Research progress of Ephedra polysaccharides. China J. Tradit. Chin. Med. Pharm. 2019, 34, 3138–3139. [Google Scholar]
- Okawa, M.; Kinjo, J.; Nohara, T.; Ono, M. DPPH (1,1-diphenyl-2-picrylhydrazyl) radical scavenging activity of flavonoids obtained from some medicinal plants. Biol. Pharm. Bull. 2001, 24, 1202–1205. [Google Scholar] [CrossRef] [PubMed]
- Purev, O.; Pospíšil, F.; Motl, O. Flavonoids from Ephedra sinica stapf. Collect. Czech Chem. C. 1988, 53, 3193–3196. [Google Scholar] [CrossRef]
- Tao, H.M. Flavonoids from roots of Ephedra sinica. Chin Tradit Herb Drugs 2011, 42, 1678–1682. [Google Scholar]
- Kasahara, Y.; Shimoyama, N.; Konno, C.; Hikino, H. Structure of mahuannin C, a hypotensive principle of Ephedra roots. Heterocycles 1983, 20, 1741–1744. [Google Scholar]
- Nawwar, M.A.; El-Sissi, H.I.; Barakat, H.H. Flavonoid constituents of Ephedra alata. Phytochemistry 1984, 23, 2937–2939. [Google Scholar] [CrossRef]
- Amakura, Y.; Yoshimura, M.; Yamakami, S.; Yoshida, T.; Wakana, D.; Hyuga, M.; Hyuga, S.; Hanawa, T.; Goda, Y. Characterization of phenolic constituents from ephedra herb extract. Molecules 2013, 18, 5326–5334. [Google Scholar] [CrossRef]
- Villalobos, A. Compositions and Methods for Enhancing Weight-Loss by Cyclical Administration of Compounds. U.S. Patent 7,977,378, 12 July 2011. [Google Scholar]
- Bouchard, N.C.; Howland, M.A.; Greller, H.A.; Hoffman, R.S.; Nelson, L.S. Ischemic stroke associated with use of an ephedra-free dietary supplement containing synephrine. Mayo. Clin. Proc. 2005, 80, 541–545. [Google Scholar] [CrossRef]
- Cottiglia, F.; Bonsignore, L.; Casu, L.; Deidda, D.; Pompei, R.; Casu, M.; Floris, C. Phenolic constituents from Ephedra nebrodensis. Nat. Prod. Res. 2005, 19, 117–123. [Google Scholar] [CrossRef]
- Zang, X.; Shang, M.; Xu, F.; Liang, J.; Wang, X.; Mikage, M.; Cai, S. A-type proanthocyanidins from the stems of Ephedra sinica (Ephedraceae) and their antimicrobial activities. Molecules 2013, 18, 5172–5189. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.M.; Wang, Z.B.; Xin, P.; Wang, Q.H.; Bu, H.; Kuang, H.X. Phytochemistry and pharmacology of genus Ephedra. Chin. J. Nat. Med. 2018, 16, 811–828. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, H.; Wiedemeyer, H. Die gerbstoffbildner in Ephedra helvetica. Planta Med. 1976, 30, 163–173. [Google Scholar] [CrossRef]
- Porter, P.L.; Wallace, J.W. C-glycosylflavones from species of Ephedra. Biochem. Syst. Ecol. 1988, 16, 261–262. [Google Scholar] [CrossRef]
- Wallace, J.W. C-Glycosylflavones In The Gnetopsida: A Preliminary Report. Am. J. Bot. 1979, 66, 343–346. [Google Scholar] [CrossRef]
- Ohba, S.; Yoshida, K.; Kondo, T. Swertisin dihydrate. Acta Cryst. C 2004, 60, 893–896. [Google Scholar] [CrossRef]
- Lv, M.; Chen, J.; Gao, Y.; Sun, J.; Zhang, Q.; Zhang, M.; Xu, F.; Zhang, Z. Metabolomics based on liquid chromatography with mass spectrometry reveals the chemical difference in the stems and roots derived from Ephedra sinica. J. Sep. Sci. 2015, 38, 3331–3336. [Google Scholar] [CrossRef]
- Oshima, N.; Maruyama, T.; Yamashita, T.; Uchiyama, N.; Amakura, Y.; Hyuga, S.; Hyuga, M.; Nakamori, S.; Takemoto, H.; Kobayashi, Y.; et al. Two flavone C-glycosides as quality control markers for the manufacturing process of ephedrine alkaloids-free Ephedra Herb extract (EFE) as a crude drug preparation. J. Nat. Med. 2018, 72, 73–79. [Google Scholar] [CrossRef]
- Morio, Y.; Yoshiaki, A.; Sumiko, H.; Masashi, H.; Shunsuke, N.; Takuro, M.; Naohiro, O.; Nahoko, U.; Jinwei, Y.; Hideki, O.; et al. Quality Evaluation and Characterization of Fractions with Biological Activity from Ephedra Herb Extract and Ephedrine Alkaloids-Free Ephedra Herb Extract. Chem. Pharm. Bull. 2020, 68, 140–149. [Google Scholar] [CrossRef]
- Tao, H.; Wang, L.; Cui, Z.; Zhao, D.; Liu, Y. Dimeric proanthocyanidins from the roots of Ephedra sinica. Planta Med. 2008, 74, 1823–1825. [Google Scholar] [CrossRef]
- Hikino, H. Structures of mahuannin A and B, hypotensive principles of Ephedra roots. Heterocycles 1982, 19, 97–105. [Google Scholar] [CrossRef]
- Tao, H.; Wang, L.; Cui, Z. Study on chemical constituents of root of Ephedra sinica. Chin. Tradit. Herb. Drugs 2010, 41, 533–536. [Google Scholar]
- Chumbalov, T.; Chekmeneva, L.; Polyakov, V. Phenolic acids of Ephedra equisetina. Chem. Nat. Compd. 1977, 13, 238–239. [Google Scholar] [CrossRef]
- Soua, L.; Koubaa, M.; Barba, F.J.; Fakhfakh, J.; Ghamgui, H.K.; Chaabouni, S.E. Water-Soluble Polysaccharides from Ephedra alata Stems: Structural Characterization, Functional Properties, and Antioxidant Activity. Molecules 2020, 25, 2210. [Google Scholar] [CrossRef]
- Zhao, W. Study on the Chemical Constituents of Ephedra Sinica; Chinese Academy of Medical Science & Peking Union Medical College: Beijing, China, 2009. [Google Scholar]
- Lee, C.-H.; Lee, H.-S. Growth inhibiting activity of quinaldic acid isolated from Ephedra pachyclada against intestinal bacteria. J. Korean Soc. Appl. Biol. Chem. 2009, 52, 331–335. [Google Scholar] [CrossRef]
- Zhang, L.R.; Zou, G.L.; Yang, T.M. Review of development in ephedta’s chemical researching and using. J. South-Cent. Univ Natl. (Nat. Sci.) 2000, 19, 87–90. [Google Scholar]
- Wang, Y.Y. Study on chemical constitutents of Ephedrae herba. Anti Infect. Pharm. 2014, 11, 416–418. [Google Scholar]
- Ma, Q.Y.; Li, C.S.; Zhou, J.; Huang, S.Z.; Zhao, Y.X. Study on chemical constituents of the ancient Ephedra species found in Yanghai, Xinjiang. J. Anhui Agric. Sci. 2012, 40, 7089–7090. [Google Scholar]
- Wang, L.; Zhao, D.; Liu, Y. GC-MS analysis of the supercritical CO2 fluid extraction of Ephedra sinica roots and its antisudorific activity. Chem. Nat. Compd. 2009, 45, 434–436. [Google Scholar] [CrossRef]
- Tellez, M.R.; Khan, I.A.; Schaneberg, B.T.; Crockett, S.L.; Rimando, A.M.; Kobaisy, M. Steam distillation–solid-phase microextraction for the detection of Ephedra sinica in herbal preparations. J. Chromatogr. A 2004, 1025, 51–56. [Google Scholar] [CrossRef]
- Zhou, L.; Wu, D.; Tang, Y. Research progress of chemical constituents in Ephedra. J. Nanjing Univ. TCM 2008, 24, 71–72. [Google Scholar]
- Yi, L.Z.; Gao, J.M.; Liu, X.Q.; Liang, Y.Z. Comparative on the components from different parts between wild growing and cultivated planting of Ephedra sinica. Chin. Tradit. Herb. Drugs 2007, 9, 1298–1301. [Google Scholar]
- Lao, Y.X.; Chen, K.; Lin, W.J.; Lin, L. GC-MS comparative analysis of the volatile oil of Ephedra sinica with different extraction methods. Res. Pract. Chin. Med. 2005, 53–56. [Google Scholar]
- Xue, J.; Wang, L.H.; Liu, L.J.; Chai, H.F. Analysis of Volatile Components of Ephedra from Different Places Based on GC-MS. J. Chin. Med. Mater. 2020, 43, 359–362. [Google Scholar]
- Ji, L.; Xu, Z.L.; Pan, G.G.; Yang, J. GC-MS analysis of constituent of essential oils from stems of Ephedra sinica Stapf, E.intermedia Schrenk et C. A. Mey. and E. equisetina Bge. Chin. J. Chin. Mat. Med. 1997, 22, 489–492. [Google Scholar]
- Wang, Y.H.; Wang, Q.H.; Xia, Y.G.; Kuang, H.X. GC-MS analysis of volatile oils from Ephedra sinica Stapf from Datong county, Shanxi province. Acta Chin. Med. Pharm. 2011, 39, 58–60. [Google Scholar]
- Sun, J.Y. Study on the new effective components of Ephedra. Chin. Herb. Med. 1983, 14, 9–10. [Google Scholar]
- Kallassy, H.; Fayyad-Kazan, M.; Makki, R.; El-Makhour, Y.; Rammal, H.; Leger, D.Y.; Sol, V.; Fayyad-Kazan, H.; Liagre, B.; Badran, B. Chemical Composition and Antioxidant, Anti-Inflammatory, and Antiproliferative Activities of Lebanese Ephedra Campylopoda Plant. Med. Sci. Monit. Basic Res. 2017, 23, 313–325. [Google Scholar] [CrossRef]
- Yang, Y.F.; Lu, Y.; Wu, G.F.; Xiao, M.Y.; Wu, H.Z. Chemical constituents of Ephedra root. Chin Tradit Pat. Med. 2010, 32, 1758–1760. [Google Scholar]
- Wang, Z.; Cui, Y.; Ding, G.; Zhou, M.; Ma, X.; Hou, Y.; Jiang, M.; Liu, D.; Bai, G. Mahuannin B an adenylate cyclase inhibitor attenuates hyperhidrosis via suppressing β(2)-adrenoceptor/cAMP signaling pathway. Phytomedicine Int. J. Phytother. Phytopharm. 2017, 30, 18–27. [Google Scholar] [CrossRef]
- Jo, Y.Y.; Kim, J.Y.; Kim, J.S.; Kwon, Y.; Shin, C.S. The effect of ephedrine on intraoperative hypothermia. Korean J. Anesthesiol. 2011, 60, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Carlisle, H.J.; Stock, M.J. Temperature-dependent effects of ephedrine in the cold. Physiol. Behav. 1996, 60, 1147–1150. [Google Scholar] [CrossRef]
- Stohs, S.J.; Badmaev, V. A Review of Natural Stimulant and Non-stimulant Thermogenic Agents. Phytother. Res. 2016, 30, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Lee, W.; Huh, E.; Choi, E.; Jang, Y.P.; Kim, Y.K.; Lee, T.H.; Oh, M.S. Ephedra sinica Stapf and Gypsum Attenuates Heat-Induced Hypothalamic Inflammation in Mice. Toxins 2019, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Mei, F.; Xing, X.-f.; Tang, Q.-f.; Chen, F.-l.; Guo, Y.; Song, S.; Tan, X.-m.; Luo, J.-B. Antipyretic and anti-asthmatic activities of traditional Chinese herb-pairs, Ephedra and Gypsum. Chin. J. Integr. Med. 2016, 22, 445–450. [Google Scholar] [CrossRef]
- Ma, C.H.; Ma, Z.Q.; Fu, Q.; Ma, S.P. Ma Huang Tang ameliorates asthma though modulation of Th1/Th2 cytokines and inhibition of Th17 cells in ovalbumin-sensitized mice. Chin. J. Nat. Med. 2014, 12, 361–366. [Google Scholar] [CrossRef]
- Zhang, B.B.; Zeng, M.N.; Zhang, Q.Q.; Wang, R.; Jia, J.F.; Cao, B.; Liu, M.; Guo, P.L.; Zhang, Y.H.; Zheng, X.K.; et al. Ephedrae Herba polysaccharides inhibit the inflammation of ovalbumin induced asthma by regulating Th1/Th2 and Th17/Treg cell immune imbalance. Mol. Immunol. 2022, 152, 14–26. [Google Scholar] [CrossRef]
- Huang, P.; Tang, Y.; Li, C.; Zhou, H.; Yu, L.; Wan, H.; He, Y. Correlation study between the pharmacokinetics of seven main active ingredients of Mahuang decoction and its pharmacodynamics in asthmatic rats. J. Pharm. Biomed. Anal. 2020, 183, 113144. [Google Scholar] [CrossRef]
- Tang, J.; Ji, H.; Shi, J.; Wu, L. Ephedra water decoction and cough tablets containing ephedra and liquorice induce CYP1A2 but not CYP2E1 hepatic enzymes in rats. Xenobiotica 2016, 46, 141–146. [Google Scholar] [CrossRef]
- Wang, J.; Xiong, Y.; Xiong, B.; Wang, S.P. Effects of aerosolized aqueous extract of Ephedra on airway inflammation in asth matic mice. Chongqing Med. J. 2013, 42, 304–307. [Google Scholar]
- Kasahara, Y.; Hikino, H.; Tsurufuji, S.; Watanabe, M.; Ohuchi, K. Antiinflammatory actions of ephedrines in acute inflammations1. Planta Med. 1985, 51, 325–331. [Google Scholar] [CrossRef]
- Zheng, Y.; Yang, Y.; Li, Y.; Xu, L.; Wang, Y.; Guo, Z.; Song, H.; Yang, M.; Luo, B.; Zheng, A.; et al. Ephedrine hydrochloride inhibits PGN-induced inflammatory responses by promoting IL-10 production and decreasing proinflammatory cytokine secretion via the PI3K/Akt/GSK3β pathway. Cell. Mol. Immunol. 2013, 10, 330–337. [Google Scholar] [CrossRef]
- He, W.; Ma, J.; Chen, Y.; Jiang, X.; Wang, Y.; Shi, T.; Zhang, Q.; Yang, Y.; Jiang, X.; Yin, S.; et al. Ephedrine hydrochloride protects mice from staphylococcus aureus-induced peritonitis. Am. J. Transl. Res. 2018, 10, 670–683. [Google Scholar]
- He, Y.; Lou, X.; Jin, Z.; Yu, L.; Deng, L.; Wan, H. Mahuang decoction mitigates airway inflammation and regulates IL-21/STAT3 signaling pathway in rat asthma model. J. Ethnopharmacol. 2018, 224, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Liu, Q.; Chen, D.; Qin, W.; Lu, B.; Bi, Q.; Wang, Z.; Jia, Y.; Tan, N. Identification of quality control markers in Suhuang antitussive capsule based on HPLC-PDA fingerprint and anti-inflammatory screening. J. Pharm. Biomed. Anal. 2020, 180, 113053. [Google Scholar] [CrossRef]
- Zhai, H.Q.; Hhang, J.R.; Gao, M.C.; Liu, Y.; Zhang, S.F.; Wang, X.H.; Meng, F.Y.; Wang, Y.P. Comparative study between Ephedra sinica Stapf and Fructus Schisandrae Chinensis on ET-1 and 6-keto-prostaglandin F1α in rats with idiopathic pulmonary fibrosis. Genet. Mol. Res. GMR 2014, 13, 3761–3771. [Google Scholar] [CrossRef] [PubMed]
- Zhai, H.Q.; Zhang, S.F.; Gao, M.C.; Liu, Y.; Ou, M.; Meng, F.Y.; Wang, Y.Y. Effects of Herba Ephedra Sinicae and Fructus Schisandrae Chinensis on pathology of rats with bleomycin A(5)-induced idiopathic pulmonary fibrosis. Zhong Xi Yi Jie He Xue Bao J. Chin. Integr. Med. 2011, 9, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Zhu, J.; Wu, Z. Ephedra protects rats against acute liver failure induced by D-galactosamine and lipopolysaccharide. Zhonghua Gan Zang Bing Za Zhi = Zhonghua Ganzangbing Zazhi = Chin. J. Hepatol. 2016, 24, 127–129. [Google Scholar] [CrossRef]
- Ghasemi, M.; Azarnia, M.; Jamali, M.; Mirabolghasemi, G.; Nazarian, S.; Naghizadeh, M.M.; Rajabi, M.; Tahamtani, Y. Protective effects of Ephedra pachyclada extract on mouse models of carbon tetrachloride- induced chronic and acute liver failure. Tissue Cell 2014, 46, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Yamada, I.; Goto, T.; Takeuchi, S.; Ohshima, S.; Yoneyama, K.; Shibuya, T.; Kataoka, E.; Segawa, D.; Sato, W.; Dohmen, T.; et al. Mao (Ephedra sinica Stapf) protects against D-galactosamine and lipopolysaccharide-induced hepatic failure. Cytokine 2008, 41, 293–301. [Google Scholar] [CrossRef]
- Song, M.K.; Um, J.Y.; Jang, H.J.; Lee, B.C. Beneficial effect of dietary Ephedra sinica on obesity and glucose intolerance in high-fat diet-fed mice. Exp. Ther. Med. 2012, 3, 707–712. [Google Scholar] [CrossRef] [PubMed]
- LiverTox. Chinese and other Asian Herbal Medicines. In LiverTox: Clinical and Research Information on Drug-Induced Liver Injury; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2012. [Google Scholar]
- Lee, A.Y.; Jang, Y.; Hong, S.H.; Chang, S.H.; Park, S.; Kim, S.; Kang, K.S.; Kim, J.E.; Cho, M.H. Ephedrine-induced mitophagy via oxidative stress in human hepatic stellate cells. J. Toxicol. Sci. 2017, 42, 461–473. [Google Scholar] [CrossRef] [PubMed]
- Caveney, S.; Charlet, D.A.; Freitag, H.; Maier-Stolte, M.; Starratt, A.N. New observations on the secondary chemistry of worldEphedra(Ephedraceae). Am. J. Bot. 2001, 88, 1199–1208. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Jan, G.; Khan, A.; Gul Jan, F.; Bahadur, A.; Danish, M. In Vitro Antioxidant and Antimicrobial Activities of Ephedra gerardiana (Root and Stem) Crude Extract and Fractions. Evid. Based Complement. Altern. Med. Ecam 2017, 2017, 4040254. [Google Scholar] [CrossRef]
- Parsaeimehr, A.; Sargsyan, E.; Javidnia, K. A comparative study of the antibacterial, antifungal and antioxidant activity and total content of phenolic compounds of cell cultures and wild plants of three endemic species of Ephedra. Molecules 2010, 15, 1668–1678. [Google Scholar] [CrossRef]
- Bagheri-Gavkosh, S.; Bigdeli, M.; Shams-Ghahfarokhi, M.; Razzaghi-Abyaneh, M. Inhibitory effects of Ephedra major Host on Aspergillus parasiticus growth and aflatoxin production. Mycopathologia 2009, 168, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Oshima, N. Efficient Preparation of Ephedrine Alkaloids-free Ephedra Herb Extract and Its Antitumor Effect and Putative Marker Compound. Yakugaku Zasshi J. Pharm. Soc. Jpn. 2017, 137, 173–177. [Google Scholar] [CrossRef]
- Hyuga, S.; Hyuga, M.; Oshima, N.; Maruyama, T.; Kamakura, H.; Yamashita, T.; Yoshimura, M.; Amakura, Y.; Hakamatsuka, T.; Odaguchi, H.; et al. Ephedrine alkaloids-free Ephedra Herb extract: A safer alternative to ephedra with comparable analgesic, anticancer, and anti-influenza activities. J. Nat. Med. 2016, 70, 571–583. [Google Scholar] [CrossRef]
- Hyuga, S.; Hyuga, M.; Yoshimura, M.; Amakura, Y.; Goda, Y.; Hanawa, T. Herbacetin, a constituent of ephedrae herba, suppresses the HGF-induced motility of human breast cancer MDA-MB-231 cells by inhibiting c-Met and Akt phosphorylation. Planta Med. 2013, 79, 1525–1530. [Google Scholar] [CrossRef]
- Kim, I.S.; Yoon, S.J.; Park, Y.J.; Lee, H.B. Inhibitory effect of ephedrannins A and B from roots of Ephedra sinica STAPF on melanogenesis. Biochim. Et Biophys. Acta 2015, 1850, 1389–1396. [Google Scholar] [CrossRef]
- Nam, N.H.; Lee, C.W.; Hong, D.H.; Kim, H.M.; Bae, K.H.; Ahn, B.Z. Antiinvasive, antiangiogenic and antitumour activity of Ephedra sinica extract. Phytothe Res 2003, 17, 70–76. [Google Scholar] [CrossRef]
- Murakami, T.; Harada, H.; Suico, M.A.; Shuto, T.; Suzu, S.; Kai, H.; Okada, S. Ephedrae herba, a component of Japanese herbal medicine Mao-to, efficiently activates the replication of latent human immunodeficiency virus type 1 (HIV-1) in a monocytic cell line. Biol. Pharm. Bull. 2008, 31, 2334–2337. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.Q.; Zhou, H.F.; Zhang, Y.Y.; Yang, J.H.; Wan, H.T.; He, Y. Antiviral effects of Yinhuapinggan granule against influenza virus infection in the ICR mice model. J. Nat. Med. 2016, 70, 75–88. [Google Scholar] [CrossRef] [PubMed]
- Bajgain, K.T.; Badal, S.; Bajgain, B.B.; Santana, M.J. Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. Am. J. Infect. Control. 2021, 49, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.L.D.; Lam, W.C.; Yang, W.; Chan, K.W.; Sze, S.C.W.; Miao, J.; Yung, K.K.L.; Bian, Z.; Wong, V.T. Potential Targets for Treatment of Coronavirus Disease 2019 (COVID-19): A Review of Qing-Fei-Pai-Du-Tang and Its Major Herbs. Am. J. Chin. Med. 2020, 48, 1051–1071. [Google Scholar] [CrossRef]
- Yao, K.T.; Liu, M.Y.; Li, X.; Hang, J.H.; Cai, H.B. Retrospective clinical analysis on treatment of coronavirus disease 2019 with traditional Chinese medicine Lianhua Qingwen. Chin J Exp Trad Med 2020, 26, 8–12. [Google Scholar]
- Li, X.; Qiu, Q.; Li, M.; Lin, H.; Cao, S.; Wang, Q.; Chen, Z.; Jiang, W.; Zhang, W.; Huang, Y.; et al. Chemical composition and pharmacological mechanism of ephedra-glycyrrhiza drug pair against coronavirus disease 2019 (COVID-19). Aging 2021, 13, 4811–4830. [Google Scholar] [CrossRef]
- Gao, K.; Song, Y.P.; Song, A. Exploring active ingredients and function mechanisms of Ephedra-bitter almond for prevention and treatment of Corona virus disease 2019 (COVID-19) based on network pharmacology. BioData Min. 2020, 13, 19. [Google Scholar] [CrossRef]
- Ang, L.; Lee, H.W.; Kim, A.; Lee, J.A.; Zhang, J.; Lee, M.S. Herbal medicine for treatment of children diagnosed with COVID-19: A review of guidelines. Complement. Ther. Clin. Pract. 2020, 39, 101174. [Google Scholar] [CrossRef]
- Mei, J.; Zhou, Y.; Yang, X.; Zhang, F.; Liu, X.; Yu, B. Active components in Ephedra sinica stapf disrupt the interaction between ACE2 and SARS-CoV-2 RBD: Potent COVID-19 therapeutic agents. J. Ethnopharmacol. 2021, 278, 284–296. [Google Scholar] [CrossRef]
- Wang, C.; Ming, H.; Jia, W.; Su, W.; Zhan, L.R.; Luo, D.; Yang, J.Y. Analysis of medication regularity and pharmacodynamic characteristics of traditional Chinese medicine treatment in 444 severe cases of COVID-19. Zhongguo Zhong Yao Za Zhi 2020, 45, 3007–3012. [Google Scholar] [CrossRef]
- Fan, T.; Chen, Y.; Bai, Y.; Ma, F.; Wang, H.; Yang, Y.; Chen, J.; Lin, Y. Analysis of medication characteristics of traditional Chinese medicine in treating COVID-19 based on data mining. Zhejiang Da Xue Xue Bao. Yi Xue Ban = J. Zhejiang University. Med. Sci. 2020, 49, 260–269. [Google Scholar] [CrossRef]
- Shergis, J.L.; Wu, L.; May, B.H.; Zhang, A.L.; Guo, X.; Lu, C.; Xue, C.C. Natural products for chronic cough: Text mining the East Asian historical literature for future therapeutics. Chronic Respir. Dis. 2015, 12, 204–211. [Google Scholar] [CrossRef]
- Hou, Y.; Cheng, B.; Zhou, M.; Fang, R.; Jiang, M.; Hou, W.; Bai, G. Searching for synergistic bronchodilators and novel therapeutic regimens for chronic lung diseases from a traditional Chinese medicine, Qingfei Xiaoyan Wan. PLoS ONE 2014, 9, e113104. [Google Scholar] [CrossRef]
- Brun, G.C. Mechanism of the Vasoconstrictor Action of Ephedrine: II. Interaction between Ephedrine and Adrenaline. Acta Pharmacol. Et Toxicol. 1947, 3, 239–251. [Google Scholar] [CrossRef] [PubMed]
- Santana, L.; Kiebzak, G.M.; Toomey, N.; Maul, T.M. Blood pressure measurements during intraoperative pediatric scoliosis surgery. Saudi J. Anaesth. 2020, 14, 152–156. [Google Scholar] [CrossRef]
- Kitaura, A.; Houri, K.; Nakao, S. Ephedrine-Induced Increases in Blood Pressure and Heart Rate Due to Suspected Cardiac Sympathetic Denervation Supersensitivity in a Patient with Parkinson’s Disease Under Spinal Anesthesia. Am. J. Case Rep. 2019, 20, 1104–1107. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Mao, M.; Liu, S.; Xu, S.; Yang, J. A Comparative Study of Bolus Norepinephrine, Phenylephrine, and Ephedrine for the Treatment of Maternal Hypotension in Parturients with Preeclampsia During Cesarean Delivery Under Spinal Anesthesia. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Liles, J.T.; Dabisch, P.A.; Hude, K.E.; Pradhan, L.; Varner, K.J.; Porter, J.R.; Hicks, A.R.; Corll, C.; Baber, S.R.; Kadowitz, P.J. Pressor responses to ephedrine are mediated by a direct mechanism in the rat. J. Pharm.. Exp. 2006, 316, 95–105. [Google Scholar] [CrossRef]
- Xiong, X.J. Experience of treating facial neuritis, unexplained limb weakness, cervical spondylosis, acute myelitis, acute radiculitis, Guillain Barre syndrome, multiple sclerosis, myasthenia gravis, motor neuron disease, dermatomyositis with Xiaoxuming Decoction. Zhongguo Zhong Yao Za Zhi 2020, 45, 2735–2751. [Google Scholar] [CrossRef] [PubMed]
- Nakamori, S.; Takahashi, J.; Hyuga, S.; Tanaka-Kagawa, T.; Jinno, H.; Hyuga, M.; Hakamatsuka, T.; Odaguchi, H.; Goda, Y.; Hanawa, T. Ephedra Herb extract activates/desensitizes transient receptor potential vanilloid 1 and reduces capsaicin-induced pain. J. Nat. Med. 2017, 71, 105–113, Correction in J. Nat. Med. 2018, 72, 594. [Google Scholar] [CrossRef] [PubMed]
- Schachtel, B.P.; Voelker, M.; Sanner, K.M.; Gagney, D.; Bey, M.; Schachtel, E.J.; Becka, M. Demonstration of the analgesic efficacy and dose-response of acetylsalicylic acid with pseudoephedrine. J. Clin. Pharmacol. 2010, 50, 1429–1437. [Google Scholar] [CrossRef] [PubMed]
- Basu, A. Middle-ear pain and trauma during air travel. Clin. Evidince 2007, 2007, 0501. [Google Scholar]
- Fan, Y.P.; Xiong, X.J. Chinese classical formulas Ephedra associated prescriptions for treatment of skin diseases. Zhongguo Zhong Yao Za Zhi 2018, 43, 2431–2434. [Google Scholar] [CrossRef]
- Adams, J.D., Jr.; Garcia, C. Women’s health among the Chumash. Evid. -Based Complement. Altern. Med. Ecam 2006, 3, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Jaradat, N.A.; Shawahna, R.; Eid, A.M.; Al-Ramahi, R.; Asma, M.K.; Zaid, A.N. Herbal remedies use by breast cancer patients in the West Bank of Palestine. J. Ethnopharmacol. 2016, 178, 1–8. [Google Scholar] [CrossRef]
- Ben-Arye, E.; Lavie, O.; Samuels, N.; Khamaisie, H.; Schiff, E.; Raz, O.G.; Mahajna, J. Safety of herbal medicine use during chemotherapy in patients with ovarian cancer: A "bedside-to-bench" approach. Med. Oncol. 2017, 34, 54. [Google Scholar] [CrossRef]
- Palamar, J. How ephedrine escaped regulation in the United States: A historical review of misuse and associated policy. Health Policy 2011, 99, 1–9. [Google Scholar] [CrossRef]
- Wang, Z.C.; Li, F.J.; Yang, J. Talking about the adverse reactions of Ephedra. Sci. Technol. Inf. 2010, 13, 407–408. [Google Scholar]
- Pittler, M.H.; Schmidt, K.; Ernst, E. Adverse events of herbal food supplements for body weight reduction: Systematic review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2005, 6, 93–111. [Google Scholar] [CrossRef]
- Powell, T.; Hsu, F.F.; Turk, J.; Hruska, K. Ma-huang strikes again: Ephedrine nephrolithiasis. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 1998, 32, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Han, H.Y.; Huh, J.I.; Han, S.R.; Kang, M.G.; Yoon, S.; Han, J.S.; Lee, B.S.; Kim, J.A.; Min, B.S. Assessing the safety of an Ephedrae Herba aqueous extract in rats: A repeat dose toxicity study. Regul. Toxicol. Pharmacol. RTP 2018, 94, 144–151. [Google Scholar] [CrossRef]
- Nyska, A.; Murphy, E.; Foley, J.F.; Collins, B.J.; Petranka, J.; Howden, R.; Hanlon, P.; Dunnick, J.K. Acute hemorrhagic myocardial necrosis and sudden death of rats exposed to a combination of ephedrine and caffeine. Toxicol. Sci. Off. J. Soc. Toxicol. 2005, 83, 388–396. [Google Scholar] [CrossRef]
- Dunnick, J.K.; Kissling, G.; Gerken, D.K.; Vallant, M.A.; Nyska, A. Cardiotoxicity of Ma Huang/caffeine or ephedrine/caffeine in a rodent model system. Toxicol. Pathol. 2007, 35, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, Y. Analgesic Effects and Side Effects of Ephedra Herb Extract and Ephedrine Alkaloids-free Ephedra Herb Extract. Yakugaku Zasshi J. Pharm. Soc. Jpn. 2017, 137, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Odaguchi, H.; Hyuga, S.; Sekine, M.; Nakamori, S.; Takemoto, H.; Huang, X.; Oshima, N.; Shimada, N.; Yang, J.; Amakura, Y.; et al. The Adverse Effects of Ephedra Herb and the Safety of Ephedrine Alkaloids-free Ephedra Herb Extract (EFE). Yakugaku Zasshi J. Pharm. Soc. Jpn. 2019, 139, 1417–1425. [Google Scholar] [CrossRef]
- Oshima, N.; Yamashita, T.; Hyuga, S.; Hyuga, M.; Kamakura, H.; Yoshimura, M.; Maruyama, T.; Hakamatsuka, T.; Amakura, Y.; Hanawa, T.; et al. Efficiently prepared ephedrine alkaloids-free Ephedra Herb extract: A putative marker and antiproliferative effects. J. Nat. Med. 2016, 70, 554–562. [Google Scholar] [CrossRef]
- Li, C.; Zheng, M.Y.; Xu, Y.J. Acute Toxicity of Mahuang Dingchuan Decoction and Lurong Dabu Decoction. Acta Chin. Med. Pharmacol. 2018, 46, 31–35. [Google Scholar]
- Liu, Y.G.; Luo, J.B.; Jiang, Y.P. Study on the acute toxicity, anti-inflammatory and anti-allergic effects of Mahuang Decoction. Chin. Tradit. Pat. Med. 2005, 2005, 101–102. [Google Scholar]
| No. | Classification | Compound Name | Ref. |
|---|---|---|---|
| 1 | Macrocyclic spermine alkaloids | Ephedradine A | [12] |
| 2 | Ephedradine B | [13] | |
| 3 | Ephedradine C | [13] | |
| 4 | Ephedradine D | [14] | |
| 5 | Imidazole alkaloids | Feruloylhistamine | [15] |
| 6 | Amphetamine-type alkaloids | D(–)-Ephedrine | [16] |
| 7 | L(+)-Pseudoephedrine | [17] [18] | |
| 8 | D(–)Norephedrine | [17] [18] | |
| 9 | L(+)-Noreseudoephedrine | [17] [18] | |
| 10 | D(–)Methylephedrine | [17] [18] | |
| 11 | L(+)-Methylpseudoephedrine | [17] [18] | |
| 12 | Ephedroxane | [19] [20] | |
| 13 | 3, 4-Dimethyl-5-pheyloxazolidine | [20] | |
| 14 | 2, 3, 4-Trimethyl-5-phenyloxazolidine | [20] | |
| 15 | O-benzoyl-L(+)-pseudoephedrine | [20] | |
| 16 | O-benzoyl-D(–)-ephedrine | [20] | |
| 17 | Hordenine | [21] | |
| 18 | (S)-N-((1R, 2S)-1-hydroxy-1-phenylpropan-2-yl)-5-oxopyrrolidine-2-carboxamide | [22] | |
| 19 | Quinoline alkaloids | Transtorine | [23] |
| 20 | 6-Methoxykynurenic acid | [24] | |
| 21 | Kynurenic acid | [24] | |
| 22 | 6-Hydroxykynurenic acids | [24] | |
| 23 | Ephedralone | [25] [26] | |
| 24 | Pyrrolidine alkaloids Other alkaloids | cis-3, 4-Methanoproline | [27] |
| 25 | Maokonine | [28] | |
| 26 | (±)-1-Phenyl-2-imido-1-propanol | [29] | |
| 27 | Tetramethylpyrazine | [30] | |
| 28 | Benzylamine | [31] | |
| 29 | N-methybenzlamine | [32] |
| No. | Classification | Compound Name | Ref. |
|---|---|---|---|
| 31 | Flavonols | Herbacetin | [36] |
| 32 | Kaempferol | [37] | |
| 33 | Quercetin | [37] | |
| 34 | Herbacetin 7-methylether | [36] | |
| 35 | Rutin | [38] | |
| 36 | Herbacetin 8-methyl ether3-O-glucoside-7-O-rutinoside | [39] | |
| 37 | Herbacetin 7-O-(6″-quinylglucoside) | [39] | |
| 38 | Herbacetin 3-O-rhamnoside 8-O-glucoside | [26] | |
| 39 | Pollenitin B | [40] | |
| 40 | Herbacetin-8-methyl ether 3-O-glucoside | [36] | |
| 41 | Herbacetin 7-O-glucoside | [40] | |
| 42 | Kaempferol 3-O-rhamnoside 7-O-glucoside | [40] | |
| 43 | Herbacetin 7-O-neohesperidoside | [40] | |
| 44 | Kaempferol-3-O-glucoside-7-O-rhamnoside | [40] | |
| 45 | Kaempferol 3-O-rhamnoside | [39] | |
| 46 | Quercetin 3-O-rhamnoside | [39] | |
| 47 | Quercetin-3-O-glucoside | [38] | |
| 48 | Dihydroflavonol | Dihydroquercetin | [37] |
| 49 | 3-Hydroxynaringenin | [41] | |
| 50 | Flavonone | 3′, 4′, 5, 7-Tetrahydroxy flavanone | [37] |
| 51 | Naringenin | [41] | |
| 52 | Hesperidin | [42] | |
| 53 | Flavanols | (–)-epicatechin | [43] |
| 54 | (–)-epiafzelechin | [37] | |
| 55 | Gallocatechin | [44] | |
| 56 | Epigallocatechin | [37] | |
| 57 | Leucoanthpcyanin | [45] | |
| 58 | Catechin | [40] | |
| 59 | Afzelechin | [37] | |
| 60 | Leucocyanidin | [46] | |
| 61 | Symplocoside | [40] | |
| 62 | Flavones | Tricin | [36] |
| 63 | Luteolin | [47] | |
| 64 | Luteolin-7-glucoside | [33] | |
| 65 | Apigeni | [37] | |
| 66 | 3-Methoxyherbacetin | [36] | |
| 67 | Apigenin-5-rhamnoside | [36] | |
| 68 | 6-C-glycosyl-chrysoeriol | [48] | |
| 69 | Swertisin | [49] | |
| 70 | Isovitexin | [50] | |
| 71 | Isovitexin-2″-O-rhamnoside | [40] | |
| 72 | Apigenin-7-O-glucoside | [38] | |
| 73 | Vitexin | [40] | |
| 74 | Lucenin III | [39] | |
| 75 | 2″, 2′″-Di-O-β-glucopyranosyl-vicenin II | [51] | |
| 76 | 6, 8-di-C-hexosyl apigenin | [44] | |
| 77 | 6/8-C-hexosyl-8/6-C-pentasyl apigenin | [44] | |
| 78 | Anthocyan | Leucodelphinidin | [46] |
| 79 | Leucopelargonin | [46] |
| No. | Classification | Compound Name | Ref. |
|---|---|---|---|
| 80 | Dimer proanthocyanidins | Ephedrannin A | [53] |
| 81 | Ephedrannin B | [53] | |
| 82 | Muhuannin A | [54] | |
| 83 | Muhuannin D | [53] | |
| 84 | Muhuannin B | [53] | |
| 85 | Muhuannin E | [53] | |
| 86 | Muhuannin C | [38] | |
| 87 | Muhuannin F | [55] | |
| 88 | Muhuannin G | [55] | |
| 89 | Muhuannin H | [56] | |
| 90 | Muhuannin I | [55] | |
| 91 | Muhuannin J | [56] | |
| 92 | Muhuannin K | [55] | |
| 93 | Ephedrannin D1 | [44] | |
| 94 | Ephedrannin D2 | [44] | |
| 95 | Ephedrannin D3 | [40] | |
| 96 | Ephedrannin D4 | [44] | |
| 97 | Ephedrannin D5 | [44] | |
| 98 | Ephedrannin D6 | [44] | |
| 99 | Ephedrannin D7 | [44] | |
| 100 | Ephedrannin D8 | [44] | |
| 101 | Ephedrannin D9 | [44] | |
| 102 | Ephedrannin D10 | [44] | |
| 103 | Ephedrannin D11 | [44] | |
| 104 | Ephedrannin D12 | [44] | |
| 105 | Ephedrannin D13 | [44] | |
| 106 | Ephedrannin D14 | [44] | |
| 107 | Trimer proanthocyanidins | Ephedrannin Tr1 | [44] |
| 108 | Ephedrannin Tr2 | [44] | |
| 109 | Ephedrannin Tr3 | [44] | |
| 110 | Ephedrannin Tr4 | [44] | |
| 111 | Ephedrannin Tr5 | [44] | |
| 112 | Ephedrannin Tr6 | [44] | |
| 113 | Ephedrannin Tr7 | [44] | |
| 114 | Ephedrannin Tr8 | [44] | |
| 115 | Ephedrannin Tr9 | [44] | |
| 116 | Ephedrannin Tr10 | [44] | |
| 117 | Ephedrannin Tr11 | [44] | |
| 118 | Ephedrannin Tr12 | [44] | |
| 119 | Ephedrannin Tr13 | [44] | |
| 120 | Ephedrannin Tr14 | [40] | |
| 121 | Ephedrannin Tr15 | [40] | |
| 122 | Tetramer proanthocyanidins | Ephedrannin Te1 | [40] |
| 123 | Ephedrannin Te2 | [40] | |
| 124 | Ephedrannin Te3 | [40] | |
| 125 | Ephedrannin Te4 | [40] | |
| 126 | Ephedrannin Te5 | [40] | |
| 127 | Hydrolytic tannins | Nilocitin | [39] |
| No. | Classification | Compound Name | Ref. |
|---|---|---|---|
| 128 | Organic acids | Nebrodenside A | [22] [43] |
| 129 | Nebrodenside B | [22] [43] | |
| 130 | O-coumaric acid glucoside | [22] [58] | |
| 131 | Trans-cinnamic acid | [58] | |
| 132 | Syringin | [45] | |
| 133 | O-Coumaric acid | [25] | |
| 134 | ρ-Hydroxybenzoic acid | [56] | |
| 135 | Protocatechuic acid | [58] | |
| 136 | Quinaldic acid | [59] | |
| 137 | 2-Hydroxyl-5-methoxybenzoic acid | [55] | |
| 138 | Iso-ferulic acid | [55] | |
| 139 | Vanillic acid | [56] | |
| 140 | Caffeic acid | [58] | |
| 141 | Chlorogenic acid | [58] | |
| 142 | (3R)-3-O-β-D-glucopyranosyl-3-phenylpropanoic acid | [22] | |
| 143 | Malic acid | [60] | |
| 144 | Citric acid | [60] | |
| 145 | Oxalic acid | [60] | |
| 146 | Fumaric acid | [60] | |
| 147 | 4-O-β-D-glucoside benzoic acid | [61] | |
| 148 | 5-(hydroxy-isopropyl)-cyclohexenecarboxylic acid | [58] | |
| 149 | Pseudolaroside B | [61] | |
| 150 | n-hexacosane acid | [62] | |
| 151 | Trans-aconitic acid | [50] |
| No. | Classification | Compound Name | Ref. |
|---|---|---|---|
| 152 | Organic volatile essential oil | β-Sitosterol | [63] |
| 153 | 9Z, 12Z-Octadecadienoic acid | [63] | |
| 154 | 9-E-Octadecenoic acid | [63] | |
| 155 | Ergost-5-en-3β-ol | [63] | |
| 156 | Nonacosanol | [63] | |
| 157 | L-α-terpineol | [69] | |
| 158 | Linolenic acid | [63] | |
| 159 | Terpineol acetate | [70] | |
| 160 | 3, 7, 11, 15-Tetramethyl-2-hexadecen-1-ol | [63] | |
| 161 | Stearic acid | [63] | |
| 162 | Globulol | [70] | |
| 163 | γ-eudesmol | [69] | |
| 164 | Linalool | [69] | |
| 165 | Eicosanoic acid | [63] | |
| 166 | Cis-2-ρ-menthen-7-ol | [69] | |
| 167 | Terpinen-4-ol | [69] | |
| 168 | β-terpineol | [71] | |
| 169 | Myrcene | [71] | |
| 170 | Dihydrocarveol | [71] | |
| 171 | 1, 3, 4-Trimethyl-3-cyclohexene-1-carboxaldehyde | [71] | |
| 172 | Trans-phytol | [72] | |
| 173 | Linolenic acid methyl ester | [72] | |
| 174 | γ-Sitosterol | [72] | |
| 175 | 1, 4-Cineole | [69] | |
| 176 | 1, 8-Cineole | [69] | |
| 177 | ρ-Cymene | [69] | |
| 178 | Limonene | [69] | |
| 179 | γ-Terpinene | [69] | |
| 180 | Hexadecanoic acid | [69] | |
| 181 | Dibutyl phthalate | [69] |
| No. | Classification | Compound Name | Ref. |
|---|---|---|---|
| 182 | Lignans | DL-Syringaresinol | [25] |
| 183 | Sesquipinsapol B | [55] | |
| 184 | Naphthalenes | Methyl-2,3-methylenedioxy-6-naphthalenecarboxylic acid methyl ester | [58] |
| 185 | Esters | Ethyl caprylate | [73] |
| 186 | Terpenoids | (–)-α-Terpineol-8-O-β-D-glucopyranoside | [55] |
| 187 | (+)-α-Terpineol-8-O-β-D-glucopyranoside | [55] | |
| 188 | Geranyl-β-D-glucopyranoside | [55] | |
| 189 | Daucosterol | [55] | |
| 190 | Sitosterol | [55] | |
| 191 | Stigmasterol-3-O-β-D-glucopyranoside | [73] | |
| 192 | Quinones | Physcion | [58] |
| 193 | Rhein | [58] | |
| 194 | Phenols | ρ-Aminophenol | [58] |
| 195 | Rhododendrol-4′-O-β-D-glucopyranoside | [61] | |
| 196 | Vinylguaiacol | [72] | |
| 197 | Di-tert-butylphenol | [72] | |
| 198 | Antiarol | [72] | |
| 199 | Ureas | Allantoin | [44] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, S.; Ren, J.; Kong, L.; Yan, G.; Liu, C.; Han, Y.; Sun, H.; Wang, X.-J. Ephedrae Herba: A Review of Its Phytochemistry, Pharmacology, Clinical Application, and Alkaloid Toxicity. Molecules 2023, 28, 663. https://doi.org/10.3390/molecules28020663
Tang S, Ren J, Kong L, Yan G, Liu C, Han Y, Sun H, Wang X-J. Ephedrae Herba: A Review of Its Phytochemistry, Pharmacology, Clinical Application, and Alkaloid Toxicity. Molecules. 2023; 28(2):663. https://doi.org/10.3390/molecules28020663
Chicago/Turabian StyleTang, Songyuan, Junling Ren, Ling Kong, Guangli Yan, Chang Liu, Ying Han, Hui Sun, and Xi-Jun Wang. 2023. "Ephedrae Herba: A Review of Its Phytochemistry, Pharmacology, Clinical Application, and Alkaloid Toxicity" Molecules 28, no. 2: 663. https://doi.org/10.3390/molecules28020663
APA StyleTang, S., Ren, J., Kong, L., Yan, G., Liu, C., Han, Y., Sun, H., & Wang, X.-J. (2023). Ephedrae Herba: A Review of Its Phytochemistry, Pharmacology, Clinical Application, and Alkaloid Toxicity. Molecules, 28(2), 663. https://doi.org/10.3390/molecules28020663




