Gypsogenin Battling for a Front Position in the Pentacyclic Triterpenes Game of Thrones on Anti-Cancer Therapy: A Critical Review—Dedicated to the Memory of Professor Hanaa M. Rady
Abstract
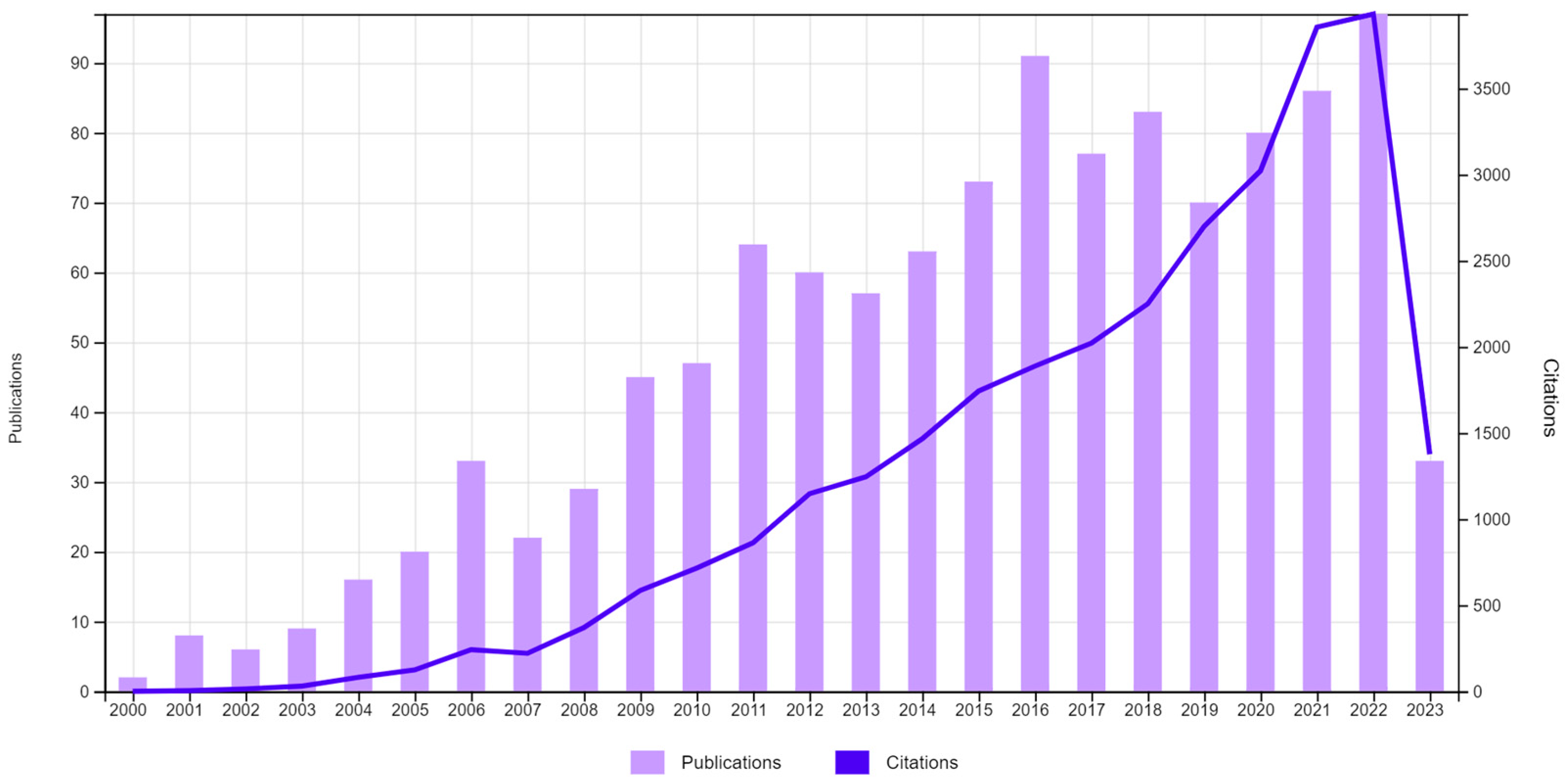
1. Introduction
2. Methodology
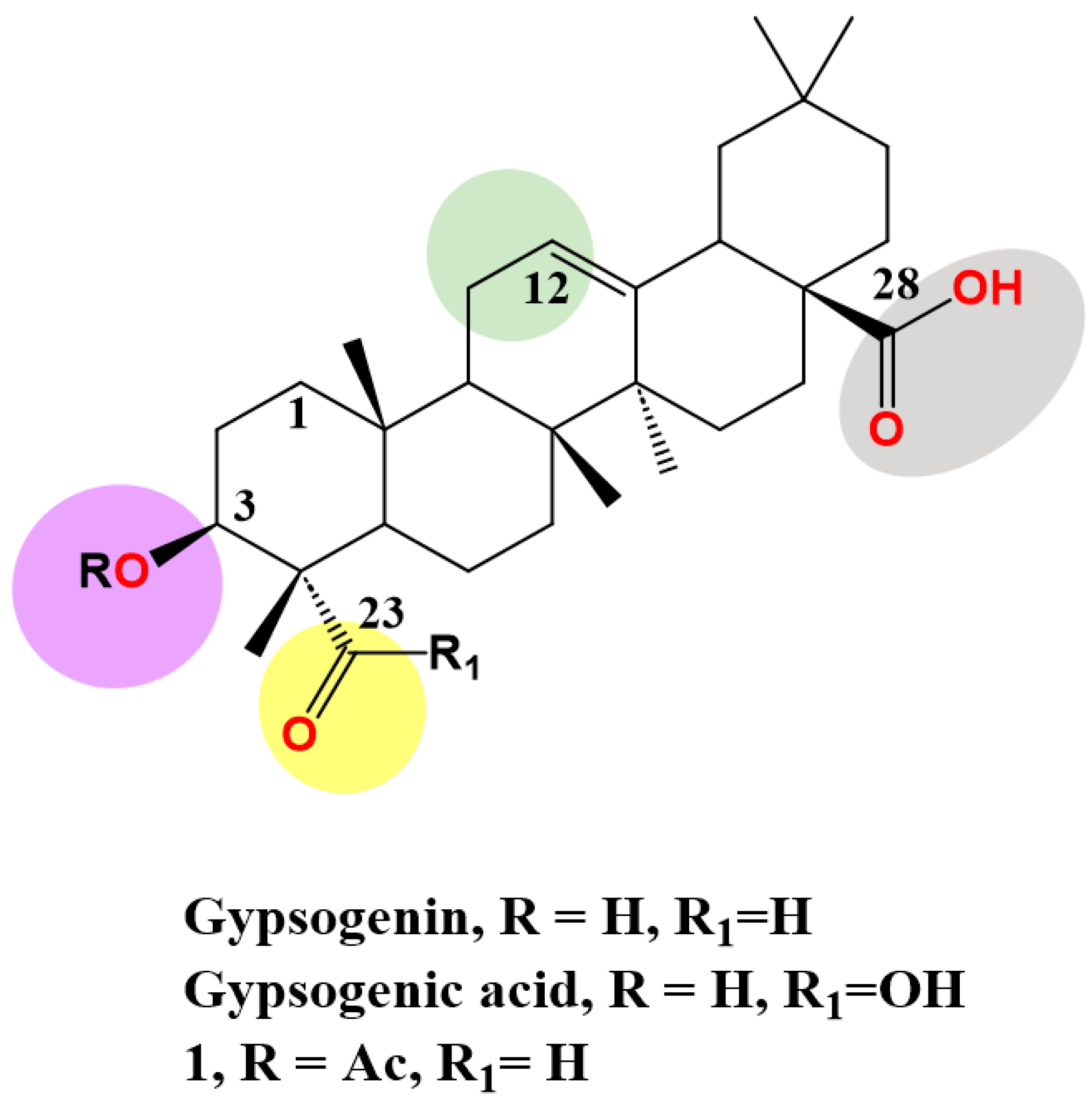
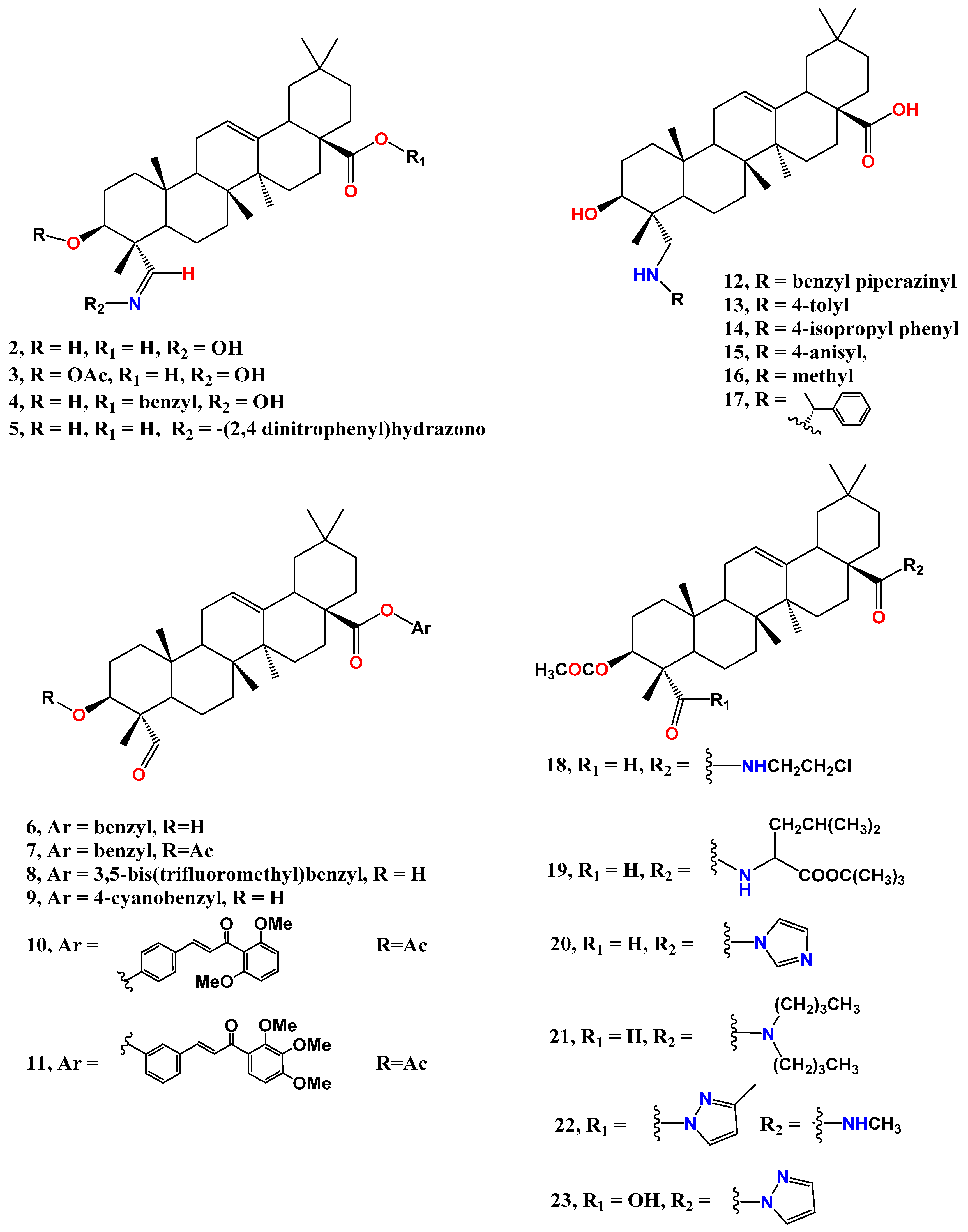
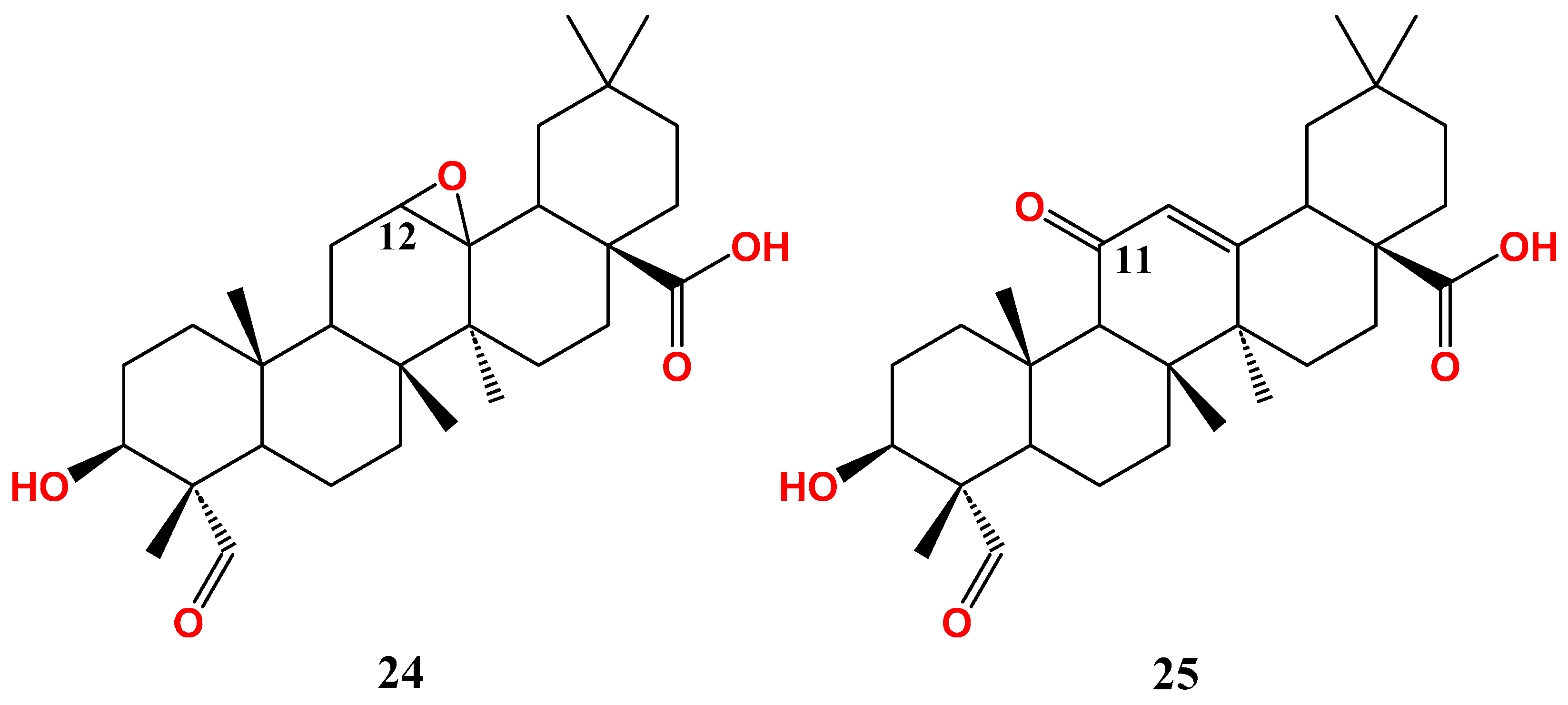
3. Gypsogenin Extraction and Chemical Transformation
4. Anti-Cancer Effect of Gypsogenin, Gypsogenic Acid, and Their Semisynthetic Derivatives
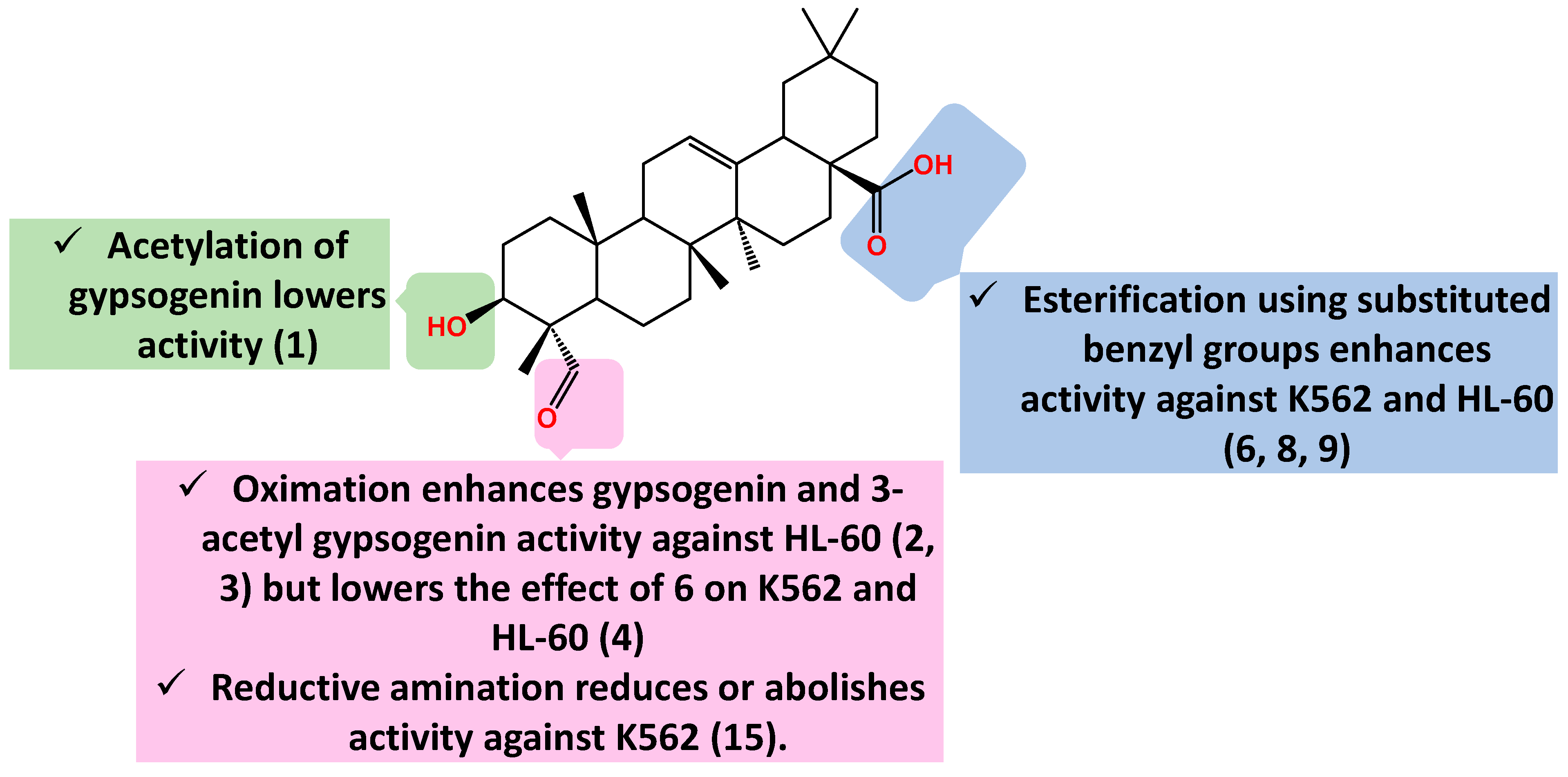
4.1. Anti-Leukemic Activity
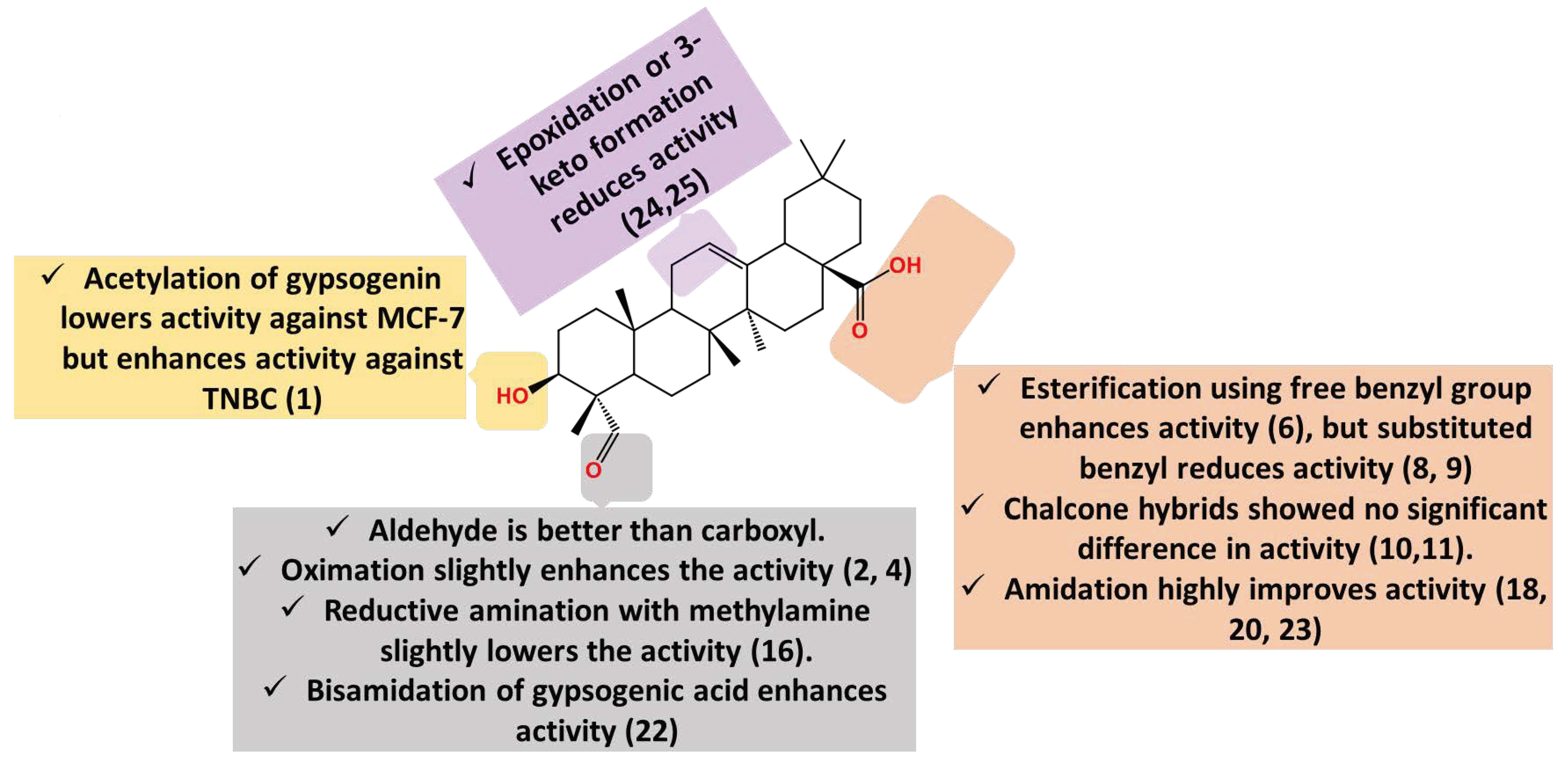
4.2. Anti-Breast Cancer Activity
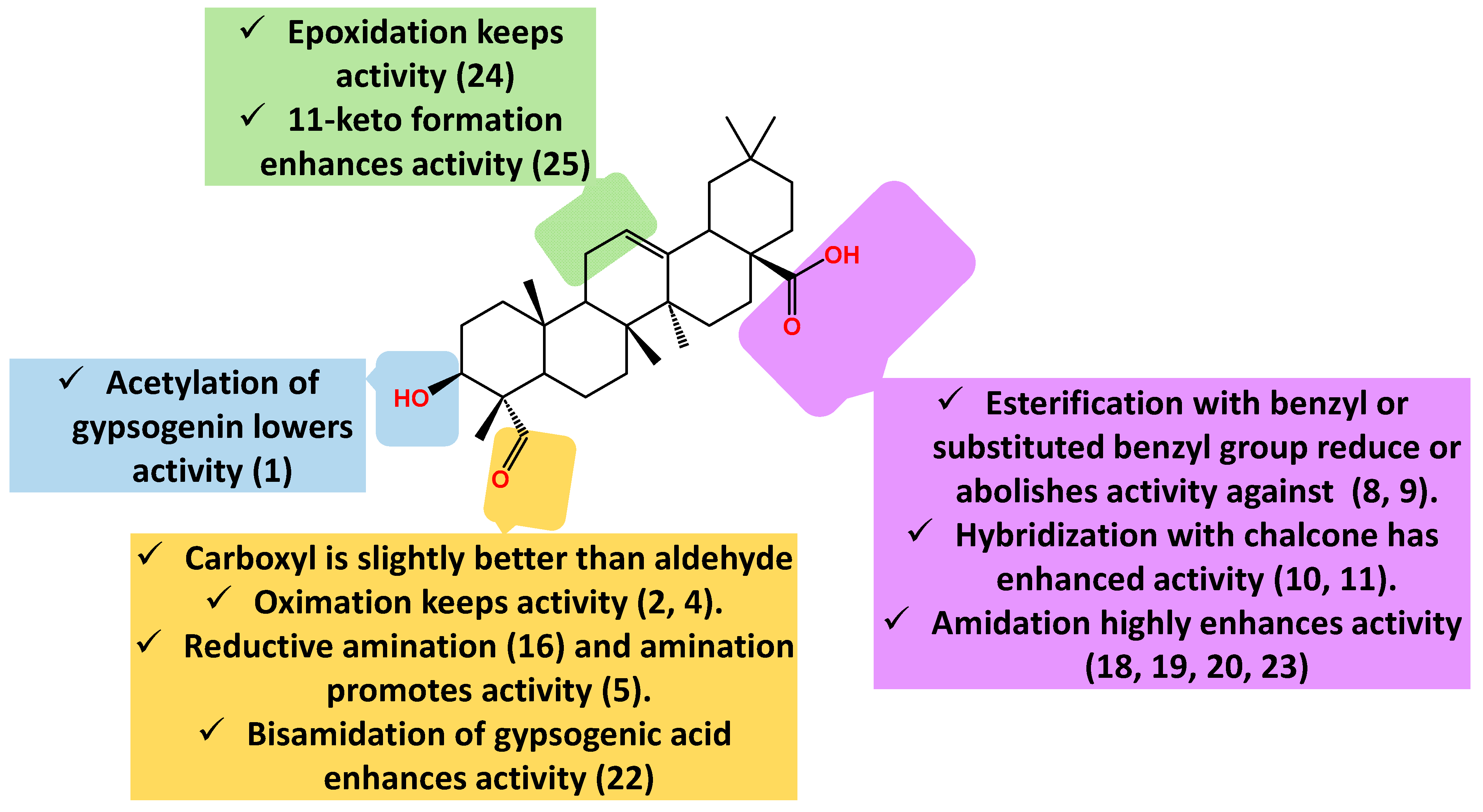
4.3. Anti-Lung Cancer Activity
4.4. Other Anti-Cancer Activities
5. Conclusions and Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer Incidence and Mortality Worldwide: Sources, Methods and Major Patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Santucci, C.; Carioli, G.; Bertuccio, P.; Malvezzi, M.; Pastorino, U.; Boffetta, P.; Negri, E.; Bosetti, C.; La Vecchia, C. Progress in Cancer Mortality, Incidence, and Survival: A Global Overview. Eur. J. Cancer Prev. Off. J. Eur. Cancer Prev. Organ. ECP 2020, 29, 367–381. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Dyba, T.; Randi, G.; Bettio, M.; Gavin, A.; Visser, O.; Bray, F. Cancer Incidence and Mortality Patterns in Europe: Estimates for 40 Countries and 25 Major Cancers in 2018. Eur. J. Cancer Oxf. Engl. 1990 2018, 103, 356–387. [Google Scholar] [CrossRef]
- Ciftci, H.I.; Can, M.; Ellakwa, D.E.; Suner, S.C.; Ibrahim, M.A.; Oral, A.; Sekeroglu, N.; Özalp, B.; Otsuka, M.; Fujita, M.; et al. Anticancer Activity of Turkish Marine Extracts: A Purple Sponge Extract Induces Apoptosis with Multitarget Kinase Inhibition Activity. Investig. New Drugs 2020, 38, 1326–1333. [Google Scholar] [CrossRef]
- Dagenais, G.R.; Leong, D.P.; Rangarajan, S.; Lanas, F.; Lopez-Jaramillo, P.; Gupta, R.; Diaz, R.; Avezum, A.; Oliveira, G.B.F.; Wielgosz, A.; et al. Variations in Common Diseases, Hospital Admissions, and Deaths in Middle-Aged Adults in 21 Countries from Five Continents (PURE): A Prospective Cohort Study. Lancet 2019, 395, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Li, D.; Zhu, X. Cancer Immunotherapy: Pros, Cons and Beyond. Biomed. Pharmacother. Biomed. Pharmacother. 2020, 124, 109821. [Google Scholar] [CrossRef]
- Liu, Z.; Ren, Y.; Weng, S.; Xu, H.; Li, L.; Han, X. A New Trend in Cancer Treatment: The Combination of Epigenetics and Immunotherapy. Front. Immunol. 2022, 13, 809761. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.; Billaud, M.; Almeida, R. RNA-Binding Proteins in Cancer: Old Players and New Actors. Trends Cancer 2017, 3, 506–528. [Google Scholar] [CrossRef]
- Bhinder, B.; Gilvary, C.; Madhukar, N.S.; Elemento, O. Artificial Intelligence in Cancer Research and Precision Medicine. Cancer Discov. 2021, 11, 900–915. [Google Scholar] [CrossRef]
- Radwan, M.O.; Toma, T.; Arakaki, Y.; Kamo, M.; Inoue, N.; Koga, R.; Otsuka, M.; Tateishi, H.; Fujita, M. New Insight into the Bioactivity of Substituted Benzimidazole Derivatives: Repurposing from Anti-HIV Activity to Cell Migration Inhibition Targeting HnRNP M. Bioorg. Med. Chem. 2023, 86, 117294. [Google Scholar] [CrossRef] [PubMed]
- Rupaimoole, R.; Slack, F.J. MicroRNA Therapeutics: Towards a New Era for the Management of Cancer and Other Diseases. Nat. Rev. Drug Discov. 2017, 16, 203–222. [Google Scholar] [CrossRef] [PubMed]
- Alqathama, A.; Yonbawi, A.R.; Shao, L.; Bader, A.; Abdalla, A.N.; Gibbons, S.; Prieto, J.M. The in Vitro Cytotoxicity against Human Melanoma Cells, Tyrosinase Inhibition and Antioxidant Activity of Grewia Tenax Leaves Extracts. Boletin Latinoam. Caribe Plantas Med. Aromat. 2022, 22, 268–276. [Google Scholar] [CrossRef]
- Bader, A.; Abdalla, A.N.; Obaid, N.A.; Youssef, L.; Naffadi, H.M.; Elzubier, M.E.; Almaimani, R.A.; Flamini, G.; Pieracci, Y.; El-Readi, M.Z. In Vitro Anticancer and Antibacterial Activities of the Essential Oil of Forsskal’s Basil Growing in Extreme Environmental Conditions. Life 2023, 13, 651. [Google Scholar] [CrossRef]
- Abo-Elghiet, F.; Ibrahim, M.H.; El Hassab, M.A.; Bader, A.; Abdallah, Q.M.A.; Temraz, A. LC/MS Analysis of Viscum Cruciatum Sieber Ex Boiss. Extract with Anti-Proliferative Activity against MCF-7 Cell Line via G0/G1 Cell Cycle Arrest: An in-Silico and in-Vitro Study. J. Ethnopharmacol. 2022, 295, 115439. [Google Scholar] [CrossRef]
- Bader, A.; Bkhaitan, M.M.; Abdalla, A.N.; Abdallah, Q.M.A.; Ali, H.I.; Sabbah, D.A.; Albadawi, G.; Abushaikha, G.M. Design and Synthesis of 4-O-Podophyllotoxin Sulfamate Derivatives as Potential Cytotoxic Agents. Evid. Based Complement. Alternat. Med. 2021, 2021, e6672807. [Google Scholar] [CrossRef]
- Gutiérrez-Rebolledo, G.A.; Siordia-Reyes, A.G.; Meckes-Fischer, M.; Jiménez-Arellanes, A. Hepatoprotective Properties of Oleanolic and Ursolic Acids in Antitubercular Drug-Induced Liver Damage. Asian Pac. J. Trop. Med. 2016, 9, 644–651. [Google Scholar] [CrossRef]
- Xu, G.B.; Xiao, Y.H.; Zhang, Q.Y.; Zhou, M.; Liao, S.G. Hepatoprotective Natural Triterpenoids. Eur. J. Med. Chem. 2018, 145, 691–716. [Google Scholar] [CrossRef]
- Ayeleso, T.B.; Matumba, M.G.; Mukwevho, E. Oleanolic Acid and Its Derivatives: Biological Activities and Therapeutic Potential in Chronic Diseases. Molecules 2017, 22, 1915. [Google Scholar] [CrossRef]
- Aly, A.M.; Al-Alousi, L.; Salem, H.A. Licorice: A Possible Anti-Inflammatory and Anti-Ulcer Drug. AAPS PharmSciTech 2005, 6, E74–E82. [Google Scholar] [CrossRef]
- Tsai, S.J.; Yin, M.C. Antioxidative and Anti-Inflammatory Protection of Oleanolic Acid and Ursolic Acid in PC12 Cells. J. Food Sci. 2008, 73, H174–H178. [Google Scholar] [CrossRef]
- Radwan, M.O.; Ismail, M.A.H.; El-Mekkawy, S.; Ismail, N.S.M.; Hanna, A.G. Synthesis and Biological Activity of New 18β-Glycyrrhetinic Acid Derivatives. Arab. J. Chem. 2016, 9, 390–399. [Google Scholar] [CrossRef]
- Somova, L.I.; Shode, F.O.; Ramnanan, P.; Nadar, A. Antihypertensive, Antiatherosclerotic and Antioxidant Activity of Triterpenoids Isolated from Olea Europaea, Subspecies Africana Leaves. J. Ethnopharmacol. 2003, 84, 299–305. [Google Scholar] [CrossRef]
- Somova, L.O.; Nadar, A.; Rammanan, P.; Shode, F.O. Cardiovascular, Antihyperlipidemic and Antioxidant Effects of Oleanolic and Ursolic Acids in Experimental Hypertension. Phytomedicine 2003, 10, 115–121. [Google Scholar] [CrossRef]
- Zhang, S.; Liu, Y.; Wang, X.; Tian, Z.; Qi, D.; Li, Y.; Jiang, H. Antihypertensive Activity of Oleanolic Acid Is Mediated via Downregulation of Secretory Phospholipase A2 and Fatty Acid Synthase in Spontaneously Hypertensive Rats. Int. J. Mol. Med. 2020, 46, 2019–2034. [Google Scholar] [CrossRef] [PubMed]
- Pompei, R.; Laconi, S.; Ingianni, A. Antiviral Properties of Glycyrrhizic Acid and Its Semisynthetic Derivatives. Mini-Rev. Med. Chem. 2012, 9, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.-G.; Zhao, T.-T.; Lu, N.; Yang, Y.-A.; Zhu, H.-L. Research Progress of Glycyrrhizic Acid on Antiviral Activity. Mini-Rev. Med. Chem. 2019, 19, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Tohmé, M.J.; Giménez, M.C.; Peralta, A.; Colombo, M.I.; Delgui, L.R. Ursolic Acid: A Novel Antiviral Compound Inhibiting Rotavirus Infection in Vitro. Int. J. Antimicrob. Agents 2019, 54, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Huang, Y.; Huang, C.; Lv, X.; Liu, L.; Wang, Y.; Li, J. Antifibrosis Effects of Triterpene Acids of Eriobotrya Japonica (Thunb.) Lindl. Leaf in a Rat Model of Bleomycin-Induced Pulmonary Fibrosis. J. Pharm. Pharmacol. 2012, 64, 1751–1760. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.K.; Lee, K.Y.; Jeon, H.Y.; Sung, S.H.; Kim, Y.C. Antifibrotic Activity of Triterpenoids from the Aerial Parts of Euscaphis Japonica on Hepatic Stellate Cells. J. Enzyme Inhib. Med. Chem. 2009, 24, 1276–1279. [Google Scholar] [CrossRef] [PubMed]
- Xiang, H.; Han, Y.; Zhang, Y.; Yan, W.; Xu, B.; Chu, F.; Xie, T.; Jia, M.; Yan, M.; Zhao, R.; et al. A New Oleanolic Acid Derivative against CCl4-Induced Hepatic Fibrosis in Rats. Int. J. Mol. Sci. 2017, 18, 553. [Google Scholar] [CrossRef]
- Farina, C.; Pinza, M.; Pifferi, G. Synthesis and Anti-Ulcer Activity of New Derivatives of Glycyrrhetic, Oleanolic and Ursolic Acids. Il Farm. 1998, 53, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Somensi, L.B.; Costa, P.; Boeing, T.; Mariano, L.N.B.; Longo, B.; Magalhães, C.G.; Duarte, L.P.; Maciel e Silva, A.T.; de Souza, P.; de Andrade, S.F.; et al. Gastroprotective Properties of Lupeol-Derived Ester: Pre-Clinical Evidences of Lupeol-Stearate as a Potent Antiulcer Agent. Chem. Biol. Interact. 2020, 321, 108964. [Google Scholar] [CrossRef] [PubMed]
- Chudzik, M.; Korzonek-Szlacheta, I.; Król, W. Triterpenes as Potentially Cytotoxic Compounds. Molecules 2015, 20, 1610–1625. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.-Y.; Li, Y.; Tang, Y.-T.; Ma, X.-D.; Tang, Z.-Y. Anticancer Activity of Oleanolic Acid and Its Derivatives: Recent Advances in Evidence, Target Profiling and Mechanisms of Action. Biomed. Pharmacother. 2022, 145, 112397. [Google Scholar] [CrossRef]
- Salvador, J.A.R.; Leal, A.S.; Valdeira, A.S.; Gonçalves, B.M.F.; Alho, D.P.S.; Figueiredo, S.A.C.; Silvestre, S.M.; Mendes, V.I.S. Oleanane-, Ursane-, and Quinone Methide Friedelane-Type Triterpenoid Derivatives: Recent Advances in Cancer Treatment. Eur. J. Med. Chem. 2017, 142, 95–130. [Google Scholar] [CrossRef]
- Laszczyk, M.N. Pentacyclic Triterpenes of the Lupane, Oleanane and Ursane Group as Tools in Cancer Therapy. Planta Med. 2009, 75, 1549–1560. [Google Scholar] [CrossRef]
- Ghante, M.H.; Jamkhande, P.G. Role of Pentacyclic Triterpenoids in Chemoprevention and Anticancer Treatment: An Overview on Targets and Underling Mechanisms. J. Pharmacopunct. 2019, 22, 55–67. [Google Scholar] [CrossRef]
- Shaheen, U.; Ragab, E.A.; Abdalla, A.N.; Bader, A. Triterpenoidal Saponins from the Fruits of Gleditsia Caspica with Proapoptotic Properties. Phytochemistry 2018, 145, 168–178. [Google Scholar] [CrossRef]
- Kumar, A.; Gupta, K.B.; Dhiman, M.; Arora, S.; Jaitak, V. New Pentacyclic Triterpene from Potentilla Atrosanguinea Lodd. as Anticancer Agent for Breast Cancer Targeting Estrogen Receptor-α. Nat. Prod. Res. 2022, 36, 4352–4357. [Google Scholar] [CrossRef]
- Ghosh, A.; Panda, C.K. Role of Pentacyclic Triterpenoid Acids in the Treatment of Bladder Cancer. Mini Rev. Med. Chem. 2022, 22, 1331–1340. [Google Scholar] [CrossRef] [PubMed]
- Liese, J.; Abhari, B.A.; Fulda, S. Smac Mimetic and Oleanolic Acid Synergize to Induce Cell Death in Human Hepatocellular Carcinoma Cells. Cancer Lett. 2015, 365, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Bai, H.; Zhang, X.; Liu, J.; Cao, P.; Liao, N.; Zhang, W.; Wang, Z.; Hai, C. Inhibitory Effect of Oleanolic Acid on Hepatocellular Carcinoma via ERK-P53-Mediated Cell Cycle Arrest and Mitochondrial-Dependent Apoptosis. Carcinogenesis 2013, 34, 1323–1330. [Google Scholar] [CrossRef]
- Mu, D.-W.; Guo, H.-Q.; Zhou, G.-B.; Li, J.-Y.; Su, B. Oleanolic Acid Suppresses the Proliferation of Human Bladder Cancer by Akt/MTOR/S6K and ERK1/2 Signaling. Int. J. Clin. Exp. Pathol. 2015, 8, 13864–13870. [Google Scholar]
- Amara, S.; Zheng, M.; Tiriveedhi, V. Oleanolic Acid Inhibits High Salt-Induced Exaggeration of Warburg-like Metabolism in Breast Cancer Cells. Cell Biochem. Biophys. 2016, 74, 427–434. [Google Scholar] [CrossRef]
- Chakravarti, B.; Maurya, R.; Siddiqui, J.A.; Bid, H.K.; Rajendran, S.M.; Yadav, P.P.; Konwar, R. In Vitro Anti-Breast Cancer Activity of Ethanolic Extract of Wrightia Tomentosa: Role of pro-Apoptotic Effects of Oleanolic Acid and Urosolic Acid. J. Ethnopharmacol. 2012, 142, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Liu, M.; Li, D. Oleanolic Acid Suppresses the Proliferation of Lung Carcinoma Cells by MiR-122/Cyclin G1/MEF2D Axis. Mol. Cell. Biochem. 2015, 400, 1–7. [Google Scholar] [CrossRef]
- Furtado, R.A.; Rodrigues, E.P.; Araújo, F.R.R.; Oliveira, W.L.; Furtado, M.A.; Castro, M.B.; Cunha, W.R.; Tavares, D.C. Ursolic Acid and Oleanolic Acid Suppress Preneoplastic Lesions Induced by 1,2-Dimethylhydrazine in Rat Colon. Toxicol. Pathol. 2008, 36, 576–580. [Google Scholar] [CrossRef]
- Janakiram, N.B.; Indranie, C.; Malisetty, S.V.; Jagan, P.; Steele, V.E.; Rao, C.V. Chemoprevention of Colon Carcinogenesis by Oleanolic Acid and Its Analog in Male F344 Rats and Modulation of COX-2 and Apoptosis in Human Colon HT-29 Cancer Cells. Pharm. Res. 2008, 25, 2151–2157. [Google Scholar] [CrossRef]
- Žiberna, L.; Šamec, D.; Mocan, A.; Nabavi, S.F.; Bishayee, A.; Farooqi, A.A.; Sureda, A.; Nabavi, S.M. Oleanolic Acid Alters Multiple Cell Signaling Pathways: Implication in Cancer Prevention and Therapy. Int. J. Mol. Sci. 2017, 18, 643. [Google Scholar] [CrossRef]
- Yadav, V.R.; Prasad, S.; Sung, B.; Kannappan, R.; Aggarwal, B.B. Targeting Inflammatory Pathways by Triterpenoids for Prevention and Treatment of Cancer. Toxins 2010, 2, 2428–2466. [Google Scholar] [CrossRef]
- Borella, R.; Forti, L.; Gibellini, L.; De Gaetano, A.; De Biasi, S.; Nasi, M.; Cossarizza, A.; Pinti, M. Synthesis and Anticancer Activity of CDDO and CDDO-Me, Two Derivatives of Natural Triterpenoids. Molecules 2019, 24, 4097. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.-C.; Hsieh, W.-C.; Chen, S.-H.; Li, Y.-Z.; Liao, H.-F.; Lin, M.-Y.; Sheu, S.-M. 18β-Glycyrrhetinic Acid Modulated Autophagy Is Cytotoxic to Breast Cancer Cells. Int. J. Med. Sci. 2023, 20, 444–454. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, Z.-Q.; Song, J.; Liu, Q.-M.; Wang, C.; Huang, Z.; Chu, L.; Liang, H.-F.; Zhang, B.-X.; Chen, X.-P. 18β-Glycyrrhetinic-Acid-Mediated Unfolded Protein Response Induces Autophagy and Apoptosis in Hepatocellular Carcinoma. Sci. Rep. 2018, 8, 9365. [Google Scholar] [CrossRef]
- Sun, Y.; Dai, C.; Yin, M.; Lu, J.; Hu, H.; Chen, D. Hepatocellular Carcinoma-Targeted Effect of Configurations and Groups of Glycyrrhetinic Acid by Evaluation of Its Derivative-Modified Liposomes. Int. J. Nanomed. 2018, 13, 1621–1632. [Google Scholar] [CrossRef]
- Lee, C.S.; Kim, Y.J.; Lee, M.S.; Han, E.S.; Lee, S.J. 18beta-Glycyrrhetinic Acid Induces Apoptotic Cell Death in SiHa Cells and Exhibits a Synergistic Effect against Antibiotic Anti-Cancer Drug Toxicity. Life Sci. 2008, 83, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, H.; Noshita, T.; Yu, T.; Kidachi, Y.; Kamiie, K.; Umetsu, H.; Ryoyama, K. Novel Effects of Glycyrrhetinic Acid on the Central Nervous System Tumorigenic Progenitor Cells: Induction of Actin Disruption and Tumor Cell-Selective Toxicity. Eur. J. Med. Chem. 2010, 45, 2943–2948. [Google Scholar] [CrossRef] [PubMed]
- Roohbakhsh, A.; Iranshahy, M.; Iranshahi, M. Glycyrrhetinic Acid and Its Derivatives: Anti-Cancer and Cancer Chemopreventive Properties, Mechanisms of Action and Structure- Cytotoxic Activity Relationship. Curr. Med. Chem. 2016, 23, 498–517. [Google Scholar] [CrossRef] [PubMed]
- Zafar, S.; Khan, K.; Hafeez, A.; Irfan, M.; Armaghan, M.; ur Rahman, A.; Gürer, E.S.; Sharifi-Rad, J.; Butnariu, M.; Bagiu, I.-C.; et al. Ursolic Acid: A Natural Modulator of Signaling Networks in Different Cancers. Cancer Cell Int. 2022, 22, 399. [Google Scholar] [CrossRef]
- Raphael, T.J.; Kuttan, G. Effect of Naturally Occurring Triterpenoids Ursolic Acid and Glycyrrhizic Acid on the Cell-Mediated Immune Responses of Metastatic Tumor-Bearing Animals. Immunopharmacol. Immunotoxicol. 2008, 30, 243–255. [Google Scholar] [CrossRef]
- Kim, D.-K.; Baek, J.H.; Kang, C.-M.; Yoo, M.-A.; Sung, J.-W.; Kim, D.-K.; Chung, H.-Y.; Kim, N.D.; Choi, Y.H.; Lee, S.-H.; et al. Apoptotic Activity of Ursolic Acid May Correlate with the Inhibition of Initiation of DNA Replication. Int. J. Cancer 2000, 87, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-S.; Jiang, J. Induction of Apoptosis and Regulation of the MAPK Pathway by Ursolic Acid in Human Leukemia K562 Cells. Planta Med. 2007, 73, 1192–1194. [Google Scholar] [CrossRef] [PubMed]
- Pisha, E.; Chai, H.; Lee, I.S.; Chagwedera, T.E.; Farnsworth, N.R.; Cordell, G.A.; Beecher, C.W.; Fong, H.H.; Kinghorn, A.D.; Brown, D.M. Discovery of Betulinic Acid as a Selective Inhibitor of Human Melanoma That Functions by Induction of Apoptosis. Nat. Med. 1995, 1, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Hordyjewska, A.; Ostapiuk, A.; Horecka, A.; Kurzepa, J. Betulin and Betulinic Acid: Triterpenoids Derivatives with a Powerful Biological Potential. Phytochem. Rev. 2019, 18, 929–951. [Google Scholar] [CrossRef]
- Fulda, S. Betulinic Acid: A Natural Product with Anticancer Activity. Mol. Nutr. Food Res. 2009, 53, 140–146. [Google Scholar] [CrossRef]
- Selzer, E.; Pimentel, E.; Wacheck, V.; Schlegel, W.; Pehamberger, H.; Jansen, B.; Kodym, R. Effects of Betulinic Acid Alone and in Combination with Irradiation in Human Melanoma Cells. J. Investig. Dermatol. 2000, 114, 935–940. [Google Scholar] [CrossRef]
- Fulda, S.; Debatin, K.-M. Sensitization for Anticancer Drug-Induced Apoptosis by Betulinic Acid. Neoplasia 2005, 7, 162–170. [Google Scholar] [CrossRef]
- Li, X.; Jiang, W.; Li, W.; Dong, S.; Du, Y.; Zhang, H.; Zhou, W. Betulinic Acid-Mediating MiRNA-365 Inhibited the Progression of Pancreatic Cancer. Oncol. Res. 2023, 31, 505–514. [Google Scholar] [CrossRef]
- Lim, H.Y.; Ong, P.S.; Wang, L.; Goel, A.; Ding, L.; Li-Ann Wong, A.; Ho, P.C.; Sethi, G.; Xiang, X.; Goh, B.C. Celastrol in Cancer Therapy: Recent Developments, Challenges and Prospects. Cancer Lett. 2021, 521, 252–267. [Google Scholar] [CrossRef]
- Yang, H.; Chen, D.; Cui, Q.C.; Yuan, X.; Dou, Q.P. Celastrol, a Triterpene Extracted from the Chinese “Thunder of God Vine,” Is a Potent Proteasome Inhibitor and Suppresses Human Prostate Cancer Growth in Nude Mice. Cancer Res. 2006, 66, 4758–4765. [Google Scholar] [CrossRef]
- Nagase, M.; Oto, J.; Sugiyama, S.; Yube, K.; Takaishi, Y.; Sakato, N. Apoptosis Induction in HL-60 Cells and Inhibition of Topoisomerase II by Triterpene Celastrol. Biosci. Biotechnol. Biochem. 2003, 67, 1883–1887. [Google Scholar] [CrossRef] [PubMed]
- Kannaiyan, R.; Manu, K.A.; Chen, L.; Li, F.; Rajendran, P.; Subramaniam, A.; Lam, P.; Kumar, A.P.; Sethi, G. Celastrol Inhibits Tumor Cell Proliferation and Promotes Apoptosis through the Activation of C-Jun N-Terminal Kinase and Suppression of PI3 K/Akt Signaling Pathways. Apoptosis Int. J. Program. Cell Death 2011, 16, 1028–1041. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Mu, Y.; Wang, F.; Song, L.; Sun, J.; Liu, Y.; Sun, J. Synthesis of Gypsogenin Derivatives with Capabilities to Arrest Cell Cycle and Induce Apoptosis in Human Cancer Cells. R. Soc. Open Sci. 2018, 5, 171510. [Google Scholar] [CrossRef] [PubMed]
- Gampe, C.; Verma, V.A. Curse or Cure? A Perspective on the Developability of Aldehydes as Active Pharmaceutical Ingredients. J. Med. Chem. 2020, 63, 14357–14381. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.; Adler, F.; Buhles, A.; Stamm, C.; Fairhurst, R.A.; Kiffe, M.; Sterker, D.; Centeleghe, M.; Wartmann, M.; Kinyamu-Akunda, J.; et al. FGF401, A First-In-Class Highly Selective and Potent FGFR4 Inhibitor for the Treatment of FGF19-Driven Hepatocellular Cancer. Mol. Cancer Ther. 2019, 18, 2194–2206. [Google Scholar] [CrossRef]
- Covalent Docking of Large Libraries for the Discovery of Chemical Probes|Nature Chemical Biology. Available online: https://www.nature.com/articles/nchembio.1666 (accessed on 29 June 2023).
- Heller, L.; Schwarz, S.; Weber, B.A.; Csuk, R. Gypsogenin Derivatives: An Unexpected Class of Inhibitors of Cholinesterases. Arch. Pharm. 2014, 347, 707–716. [Google Scholar] [CrossRef]
- Furtado, N.A.J.C.; Pirson, L.; Edelberg, H.; Miranda, L.M.; Loira-Pastoriza, C.; Preat, V.; Larondelle, Y.; André, C.M. Pentacyclic Triterpene Bioavailability: An Overview of In Vitro and In Vivo Studies. Molecules 2017, 22, 400. [Google Scholar] [CrossRef]
- Gypsogenin Türevi Ile Kalkon Bileşiklerinin Yeni Yari Sentezi ve bu Türevlerinin Insan Kanser Hücre Hatlari Üzerindeki Çalişmalari—TR201922043A2|PatentGuru. Available online: https://www.patentguru.com/TR201922043A2 (accessed on 11 July 2023).
- Sun, J.; Zhang, H.; Mou, Y.; Sun, J.; Wang, F.; Wu, Z.; Wang, Y.; Song, L. Gypsogenin Derivatives. CN107236017A. 10 October 2017. Available online: https://patents.google.com/patent/CN107236017A/en?oq=CN+107236017A (accessed on 11 July 2023).
- Acebes, B.; Díaz-Lanza, A.M.; Bernabé, M. A Saponin from the Roots of Gypsophila bermejoi. Phytochemistry 1998, 49, 2077–2079. [Google Scholar] [CrossRef]
- Emirdağ-Öztürk, S.; Babahan, İ.; Özmen, A. Synthesis, Characterization and In Vitro Anti-Neoplastic Activity of Gypsogenin Derivatives. Bioorganic Chem. 2014, 53, 15–23. [Google Scholar] [CrossRef]
- Sikriwal, D.; Ghosh, P.; Batra, J.K. Ribosome Inactivating Protein Saporin Induces Apoptosis through Mitochondrial Cascade, Independent of Translation Inhibition. Int. J. Biochem. Cell Biol. 2008, 40, 2880–2888. [Google Scholar] [CrossRef]
- Kucukkurt, I.; Ince, S.; Enginar, H.; Eryavuz, A.; Fidan, A.F.; Kargioglu, M. Protective effects of Agrostemma githago L. and Saponaria officinalis L. extracts against ionizing radiation-induced oxidative damage in rats. Rev. Med. Vet. 2011, 162, 289–296. [Google Scholar]
- Chandra, S.; Rawat, D.S. Medicinal Plants of the Family Caryophyllaceae: A Review of Ethno-Medicinal Uses and Pharmacological Properties. Integr. Med. Res. 2015, 4, 123–131. [Google Scholar] [CrossRef]
- Oladeji, O.S.; Oyebamiji, A.K. Stellaria media (L.) Vill.—A Plant with Immense Therapeutic Potentials: Phytochemistry and Pharmacology. Heliyon 2020, 6, e04150. [Google Scholar] [CrossRef]
- Li, Y.; Wang, J.; Li, L.; Song, W.; Li, M.; Hua, X.; Wang, Y.; Yuan, J.; Xue, Z. Natural Products of Pentacyclic Triterpenoids: From Discovery to Heterologous Biosynthesis. Nat. Prod. Rep. 2022. [Google Scholar] [CrossRef]
- Mikołajczyk-Bator, K.; Błaszczyk, A.; Czyżniejewski, M.; Kachlicki, P. Characterisation and Identification of Triterpene Saponins in the Roots of Red Beets (Beta vulgaris L.) Using Two HPLC-MS Systems. Food Chem. 2016, 192, 979–990. [Google Scholar] [CrossRef] [PubMed]
- Burnouf-Radosevich, M.; Delfel, N.E.; England, R. Gas Chromatography-Mass Spectrometry of Oleanane- and Ursane-Type Triterpenes—Application to Chenopodium Quinoa Triterpenes. Phytochemistry 1985, 24, 2063–2066. [Google Scholar] [CrossRef]
- Anderson, O.; Beckett, J.; Briggs, C.C.; Natrass, L.A.; Cranston, C.F.; Wilkinson, E.J.; Owen, J.H.; Williams, R.M.; Loukaidis, A.; Bouillon, M.E.; et al. An Investigation of the Antileishmanial Properties of Semi-Synthetic Saponins. RSC Med. Chem. 2020, 11, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Emirdağ-Öztürk, S.; Karayıldırım, T.; Çapcı-Karagöz, A.; Alankuş-Çalışkan, Ö.; Özmen, A.; Poyrazoğlu-Çoban, E. Synthesis, Antimicrobial and Cytotoxic Activities, and Structure-Activity Relationships of Gypsogenin Derivatives against Human Cancer Cells. Eur. J. Med. Chem. 2014, 82, 565–573. [Google Scholar] [CrossRef]
- Sun, K.-P.; Zhao, T.-T.; Liu, L.; Mu, X.-D.; Sun, J.-Y. Anticancer Structure-Activity Relationships and Potential Target Exploration of the Natural Product Gypsogenin. ChemistrySelect 2023, 8, e202300072. [Google Scholar] [CrossRef]
- Wu, G.; Chu, H.; Wang, J.; Mu, Y.; Sun, J. Synthesis of Gypsogenin and Gypsogenic Acid Derivatives with Antitumor Activity by Damaging Cell Membranes. New J. Chem. 2019, 43, 18898–18914. [Google Scholar] [CrossRef]
- Ciftci, H.I.; Radwan, M.O.; Sever, B.; Hamdy, A.K.; Emirdağ, S.; Ulusoy, N.G.; Sozer, E.; Can, M.; Yayli, N.; Araki, N.; et al. EGFR-Targeted Pentacyclic Triterpene Analogues for Glioma Therapy. Int. J. Mol. Sci. 2021, 22, 10945. [Google Scholar] [CrossRef]
- Ulusoy, N.G.; Emirdağ, S.; Sözer, E.; Radwan, M.O.; Çiftçi, H.; Aksel, M.; Bölükbaşı, S.Ş.; Özmen, A.; Yaylı, N.; Karayıldırım, T.; et al. Design, Semi-Synthesis and Examination of New Gypsogenin Derivatives against Leukemia via Abl Tyrosine Kinase Inhibition and Apoptosis Induction. Int. J. Biol. Macromol. 2022, 222, 1487–1499. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, H.I.; Radwan, M.O.; Ozturk, S.E.; Ulusoy, N.G.; Sozer, E.; Ellakwa, D.E.; Ocak, Z.; Can, M.; Ali, T.F.S.; Abd-Alla, H.I.; et al. Design, Synthesis and Biological Evaluation of Pentacyclic Triterpene Derivatives: Optimization of Anti-ABL Kinase Activity. Molecules 2019, 24, 3535. [Google Scholar] [CrossRef]
- Lee, I.; Yoo, J.K.; Na, M.; Min, B.S.; Lee, J.; Yun, B.S.; Jin, W.; Kim, H.; Youn, U.; Chen, Q.C.; et al. Cytotoxicity of Triterpenes Isolated from Aceriphyllum Rossii. Chem. Pharm. Bull. 2007, 55, 1376–1378. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Krasteva, I.; Yotova, M.; Yosifov, D.; Benbassat, N.; Jenett-Siems, K.; Konstantinov, S. Cytotoxicity of Gypsogenic Acid Isolated from Gypsophila trichotoma. Pharmacogn. Mag. 2014, 10 (Suppl. S2), S430–S433. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, H.I.; Ozturk, S.E.; Ali, T.F.S.; Radwan, M.O.; Tateishi, H.; Koga, R.; Ocak, Z.; Can, M.; Otsuka, M.; Fujita, M. The First Pentacyclic Triterpenoid Gypsogenin Derivative Exhibiting Anti-ABL1 Kinase and Anti-Chronic Myelogenous Leukemia Activities. Biol. Pharm. Bull. 2018, 41, 570–574. [Google Scholar] [CrossRef]
- Almansour, N.M. Triple-Negative Breast Cancer: A Brief Review About Epidemiology, Risk Factors, Signaling Pathways, Treatment and Role of Artificial Intelligence. Front. Mol. Biosci. 2022, 9, 836417. [Google Scholar]
- Tian, G.; Zhou, L.; Zhong, Y.; Xu, W.; Bai, H.; Liu, L.; Cui, S. Experimental Studies of the Therapeutic Effect of Gypsophila oldhamiana Gypsogenin on Lewis Lung Cancer in Mice. Chin. J. Clin. Oncol. 2008, 5, 206–210. [Google Scholar] [CrossRef]
- Liu, Y.; Li, X.; Jiang, S.; Ge, Q. Inhibitory effect of Gypsophila oldhamiana gypsogenin on NCI-N87 gastric cancer cell line. Eur. J. Inflamm. 2018, 16. [Google Scholar] [CrossRef]
| Compound | Cell Line and IC50 Value (µM) | ||
|---|---|---|---|
| HT-29 [92] | Saos-2 [82] | HeLa [91] | |
| Gypsogenin | 10.4 | 7.8 | 22.4 |
| 1 | 11.1 | 8.2 | 35.0 |
| 2 | 10.8 | 7.9 | 8.7 |
| 3 | 6.7 | 8.9 | >100 |
| LOVO [93] | |||
| 16 | 5.8 | ||
| 18 | 7.2 | ||
| 19 | 0.8 | ||
| 24 | >30 | ||
| 25 | 17.8 | ||
| LOVO [74] | HePG2 [73] | SKOV3 [73] | |
| 5 | 2.9 | 10.0 | 9.7 |
| 21 | 3.5 | 12.5 | 13.1 |
| HepG2 [94] | TE-1 [93] | MC3-8 [93] | |
| 20 | 4.0 | 4.7 | 2.9 |
| 22 | 3.6 | 5.4 | 4.8 |
| 23 | 2.2 | 4.2 | 2.6 |
| HeLa [80,97] | PANC-1 [80] | ||
| Gypsogenin | 9.4 | 13.5 | |
| 1 | 3.3 | 5.0 | |
| 8 | 35.2 | - | |
| 9 | 5.6 | - | |
| 10 | 9.5 | 8.7 | |
| 11 | 10.2 | 7.9 | |
| U251 | T98G | U87 | |
| 17 [95] | 5.8 | 8.1 | 17.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radwan, M.O.; Abd-Alla, H.I.; Alsaggaf, A.T.; El-Mezayen, H.; Abourehab, M.A.S.; El-Beeh, M.E.; Tateishi, H.; Otsuka, M.; Fujita, M. Gypsogenin Battling for a Front Position in the Pentacyclic Triterpenes Game of Thrones on Anti-Cancer Therapy: A Critical Review—Dedicated to the Memory of Professor Hanaa M. Rady. Molecules 2023, 28, 5677. https://doi.org/10.3390/molecules28155677
Radwan MO, Abd-Alla HI, Alsaggaf AT, El-Mezayen H, Abourehab MAS, El-Beeh ME, Tateishi H, Otsuka M, Fujita M. Gypsogenin Battling for a Front Position in the Pentacyclic Triterpenes Game of Thrones on Anti-Cancer Therapy: A Critical Review—Dedicated to the Memory of Professor Hanaa M. Rady. Molecules. 2023; 28(15):5677. https://doi.org/10.3390/molecules28155677
Chicago/Turabian StyleRadwan, Mohamed O., Howaida I. Abd-Alla, Azhaar T. Alsaggaf, Hatem El-Mezayen, Mohammed A. S. Abourehab, Mohamed E. El-Beeh, Hiroshi Tateishi, Masami Otsuka, and Mikako Fujita. 2023. "Gypsogenin Battling for a Front Position in the Pentacyclic Triterpenes Game of Thrones on Anti-Cancer Therapy: A Critical Review—Dedicated to the Memory of Professor Hanaa M. Rady" Molecules 28, no. 15: 5677. https://doi.org/10.3390/molecules28155677
APA StyleRadwan, M. O., Abd-Alla, H. I., Alsaggaf, A. T., El-Mezayen, H., Abourehab, M. A. S., El-Beeh, M. E., Tateishi, H., Otsuka, M., & Fujita, M. (2023). Gypsogenin Battling for a Front Position in the Pentacyclic Triterpenes Game of Thrones on Anti-Cancer Therapy: A Critical Review—Dedicated to the Memory of Professor Hanaa M. Rady. Molecules, 28(15), 5677. https://doi.org/10.3390/molecules28155677










