Abstract
Cholesterol is essential for normal human health, but elevations in its serum levels have led to the development of various complications, including hypercholesterolemia (HC). Cholesterol accumulation in blood circulation formsplaques on artery walls and worsens the individuals’ health. To overcome this complication, different pharmacological and non-pharmacological approaches are employed to reduce elevated blood cholesterol levels. Atorvastatin and rosuvastatin are the most commonly used drugs, but their prolonged use leads to several acute side effects. In recent decades, the potential benefit of ingesting yogurt on lipid profile has attracted the interest of researchers and medical professionals worldwide. This review aims to give an overview of the current knowledge about HC and the different therapeutic approaches. It also discusses the health benefits of yogurt consumption and highlights the overlooked phyto-enrichment option to enhance the yogurt’s quality. Finally, clinical studies using different phyto-enriched yogurts for HC management are also reviewed. Yogurt has a rich nutritional value, but its processing degrades the content of minerals, vitamins, and other vital constituents with beneficial health effects. The option of enriching yogurt with phytoconstituents has drawn a lot of attention. Different pre-clinical and clinical studies have provided new insights on their benefits on gut microbiota and human health. Thus, the yogurtphyto-enrichment with stanol and β-glucan have opened new paths in functional food industries and found healthy andeffective alternatives for HC all along with conventional treatment approaches.
1. Introduction
Low-density lipoprotein (LDL) cholesterol and serum total cholesterol (TC) levels are both linked to a high risk of ischemic heart disease found in people at a young age and people at low risk of coronary heart disease [1,2,3,4]. With the increasing incidence of hypercholesterolemia and associated cardiovascular risk, safe, effective, and inexpensive therapeutic approaches were developed to manage such affections [5]. However, over time, it is necessary to understand the extent of blood lipid-induced complications and how they can be managed, which will allow a clear understanding of coronary risk factors among populations [4,5,6,7]. Such studies will also help to identify opportunities to reduce coronary heart risk [8]. According to the World Health Organization (WHO) guidelines, in Kazakhstan, the age-standardized prevalence of total cholesterol increase (≥6.2 mmol/L) was estimated at 12%, which is close to the Russian Federation (15%), but much higher than other Central Asian countries. For instance, Turkmenistan estimated the age-standardized prevalence of total cholesterol increase as the highest, i.e., 8%, and the minimum was 5% in Tajikistan. However, in Central Asian countries, it was estimated to be much lower than in other developed countries, such as Germany (25%) and England (22%) [9].
Regarding blood cholesterol management and distribution, national population-based studies have been conducted in some countries [10,11,12,13,14,15]. From 1999 to 2003, hypercholesterolemia (HC) in Western Europe contributed to heart attacks by about 45%, and in Central and Eastern Europe, it accounted for approximately 35% of heart attack cases [16,17]. However, the risk of heart attack is three times greater in people with high cholesterol levels than those with normal blood lipid profiles. WHO has also demarcated some unhealthy diets, leading to increased cardiovascular risk, e.g., free sugar, high-fat diets, salt, and sugars low in complex carbohydrates [18].
Nowadays, functional foods are referred to as “superfoods”, and, when consumed as part of the daily diets, are believed to have the potential to reduce the risk of several diseases [19]. There are a variety of food products amid the superfoods, including fruits, vegetables, nuts, seeds, and dairy products such as kefir and yogurt [20].
Milk and its products represent an essential part of a healthy balanced diet, rich in proteins and micronutrients [21,22]. Nonetheless, there was a misconception regarding dairy products consumption in the past, linked to the premise that they are high-risk factors for cardiovascular diseases and create adverse effects on human health due to the presence of a marked content of saturated fatty acids [23]. Though, this claim was proved wrong by the fact that dairy products have functional components (calcium, milk proteins, and phospholipids) of high nutritional value, which are efficient in lowering the risk of cardiovascular disease. Their health benefit is attributed to their probiotic effects and the ability to modulate the lipoproteins metabolism [24,25]. More recently, studies have even reported that the consumption of dairy products does not cause any cardiovascular disease [21,22,23,26]. For example, yogurt, a fermented milk product, has been reported to have nutrients with beneficial effects on glucose metabolism, lipid metabolism, and obesity [21,27,28,29,30,31,32]. Considering these aspects, the fortification of yogurt with phytoconstituents may be viewed as a key way to improve their beneficial health effects and organoleptic and nutritional quality. Indeed, this approach of enriching the yogurt with phytoconstituents has gained significant interest, and now future investigations are being carried outin this direction.
In this sense, the present review discusses hypercholesterolemia and the clinical interventions used for its management. Moreover, it also discusses the health benefits of yogurt consumption and the concept of food enrichment. Additionally, it highlights the phyto-enrichment of yogurt and clinical evidence supporting its potential use in managing hypercholesterolemia.
2. Hypercholesterolemia
2.1. Low-Density Lipoprotein-Cholesterol and the Concept of Hypercholesterolemia
Hypercholesterolemia (HC) is related to an elevated level of plasma low-density lipoprotein-cholesterol (LDL-C), as plasma LDL is the chief carrier of cholesterol [33]. The gut absorbs dietary cholesterol primarily packed in chylomicrons(triglyceride-rich); these chylomicrons first break down with the help of lipoprotein lipase (LPL), then the fatty acids and monoglycerides released are further supplied to the adipose tissue and muscles. In contrast, the remnant of chylomicron passes through the liver (Figure 1). Then liver produces very-low-density lipoproteins (VLDL), from which they are exuded into the bloodstream.VLDL becomes enlarged due to the presence of triglycerides in it. As these triglycerides are unable to accommodate themselves in VLDL, instead they start to aggregate themselves in the liver resulting in the development of fatty liver disease.LPL metabolizes VLDL and produces intermediate-density lipoproteins (IDL). Later, it becomesconverted to LDL. The liver also produces high-density lipoprotein (HDL) particles from cholesterol, incorporating cholesteryl esters released from peripheral tissues. In this way, HDL becomesinvolved in the reverse transport of cholesterol from peripheral tissues to the liver. Cholesteryl ester-laden HDL particles are moved to LDLs via cholesteryl ester transfer protein (CETP). Then, these cholesteryl esters are carted via LDL particles, which are absorbed by the liver and peripheral tissues (to a lesser extent). The LDL uptakes, as well as degradation in the liver, rely on LDL particles’ binding onto cell surface receptors (LDL-receptors) of hepatocytes. These receptors are particularly connected to apolipoprotein B (apoB) on the LDL particle. Then, the LDL: LDL-receptor complex is internalized via endocytosis. The whole internalization process is reconciled through the LDL receptor adaptor protein. These receptor molecules becomerecycled, and the LDL particles undergo lysosomal degradation. A protein expressed in hepatocytes, the proprotein convertase subtilisin/kexin type 9 (PCSK9), is believed to play a vital role in the catabolism of LDL-receptors [34].
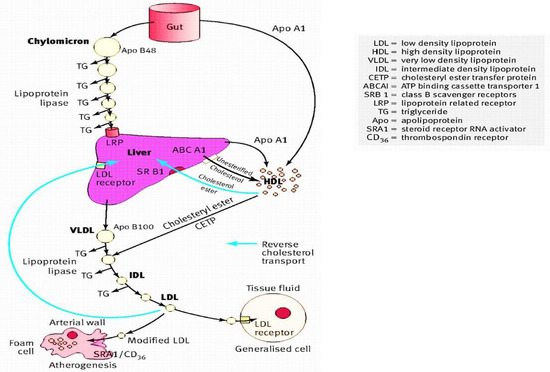
Figure 1.
Diagrammatic representation of the cholesterol role in the lipoprotein metabolismadapted from [35] with license number 5090021099627.
From the genetic point of view, the genetic mutations encoding proteins are functional during LDL uptake, and catabolism (i.e., apolipoprotein-B (ApoB) via the APOB gene, PCSK9 protein via the PCSK9 gene, LDL-receptor via the LDLR gene and LDL receptor adaptor protein via the LDLRAP1 gene) and have been distinguished in causing familial HC due to degradation and defective LDL uptake, which causes a rise in the plasma LDL-C level, form the HC phenotype [33]. Extreme HC perfectly characterizes these conditions, with excessive LDL-C level elevation resulting in atherosclerosis and cardiovascular diseases [33]. In adults, HC is a profound trait generated by the interplay involving harsh factorssuch asobesity, excessive amounts of saturated fat-rich diets, physical inactivity, and the susceptible genotype [33].
2.2. Epidemiology
Among the Indian population, the prevalence of HC differs between rural (10–15%) and urban (25–30%) populations [36]. To date, different data-based studies were performed on the Indian population, including the India Migration Study (n = 1983), India Heart Watch (n = 6123), Indian Industrial Population Surveillance Study (n = 10,442), Indian Women Health Study (n = 4624), Indian Council of Medical Research (ICMR) Integrated Disease Surveillance Project (urban n = 15,223, slum/periurbann = 15,751, rural n = 13,517), a nationwide industry-sponsored FitHeart Study (n = 46,919) and the INDIAB study (n = 2042) [37,38,39,40,41,42]. Among those, Al-Kharj of Saudi Arabia showed a positive association between the prevalence of HC and increasing age in the general population [43]. Another study reported that overweight participants have a higher risk of suffering from HC. In addition, a publicly funded cross-sectional survey carried out on the French population found that the HC prevalence in France is 23.3%, while in Spain, a cross-sectional study conducted from June 2008 to October 2010 with 11554 representative individuals of the population aged ≥18 years found that 50.5% of the population suffer from HC [44]. In the elderly population of Cyprus, a study conducted found a positive association between smoking habits and HC, whereas an inverse connection was observed among HC, adherence to the Mediterranean diet, and an alcohol drinking, after controlling for sex, age, and other factors [45]. The different studies performed in various countries to assess the prevalence of HC are shown in Table 1.

Table 1.
Epidemiological studies related to the prevalence of hypercholesterolemia.
2.3. Investigation and Laboratory Assessment
Currently, there are various therapeutic options to manage HC; however, before starting the treatment for HC, clinical examination, detailed history, and basic laboratory tests are needed to properly diagnose the causes of secondary HC, other complications related to atherosclerosis, and primary manifestations of lipoprotein changes [35]. In this sense, a family as well as occupational history, including the history of alcohol consumption, smoking, and dietary preferences, will help to determine the level to which these factors contribute to the risk of cardiovascular disease and/or HC and determine the patient’s ability to change lifestyle [35]. Regarding physical examination, it should include waist circumference, body weight, blood pressure, height, and a search for the presence of xanthoma [35]. Finally, family history is also an important factor in helping cascade testing at the primary stage of HC [55].
Moreover, during HC screening, it is advisable to obtain blood samples post-fasting for a minimum period of 10 h to avoid the postprandial contribution of plasma triglycerides [35]. If the plasma triglycerides range is in the limit of up to 4.5 mmol/L, the LDL cholesterol concentration can be calculated using the Friedewald formula:
Low density lipoprotein cholesterol = total serum cholesterol—(HDL cholesterol + (serum triglycerides/2.2)).
Non-HDL cholesterol = total cholesterol − HDL cholesterol.
Non-HDL cholesterol may act as a target for statin treatment if LDL-C cannot be measured owing to hypertriglyceridemia. The HDL cholesterol and total cholesterol: HDL ratio values help evaluate the risk of cardiovascular disease, but LDL cholesterol can be used as a therapeutic target whenever possible. Non-HDL cholesterol targets are 0.75 mmol/L more than the LDL cholesterol target. In addition, to assess the risk of cardiovascular disease, it is also important to determine fasting glucose concentration, and before starting lipid-lowering treatment, some parameters must be measured, such as creatine kinase activity, liver function tests, dipstick urine protein, and serum creatinine [35].
For routine assessment, many testing laboratories use handheld point-of-care testing (POCT) devices and automated analyzers depends on enzymatic assays a commercialised cholesterol quantitation assay kits [56,57]. Point-of-care testing (POCT) gives quick results, with simplefunction, making it more suitable for people screening tests. POCT clinical application has been found efficient in raising awareness regarding significance of lipid levels to prevent future stroke events and CVD [58]. The CardioChek PA analyzer (PTS Diagnostics) is a handy whole blood test system including a single test strip to determinetriglycerides (TG)HDL cholesterol (HDL-C) and total cholesterol (TC) [59]. In Brazil, the CardioChek PA analyzer used by health professional workers is well recommended for the proposed screening programs; the diagnostic performance is appropriate for use as part of national health services, providing quick and accurate results.
2.4. Treatment
2.4.1. Non-Pharmacological Therapy
There are various non-pharmacological options to manage HC, and dietary therapy is one of the most important ones. Among others, this approach’s primary goals are to progressively lessen the intake of total fat, saturated fats (saturated fatty acids), cholesterol and attain desirable body weight. For example, it is advisable to reduce the intake of saturated fat daily up to 7% of calories, the daily intake of total fat to 25 to 35% of calories, to limit the dietary cholesterol quantity to no more than 200 mg/day; incite the intake of soluble fiber to 20 to 30 g/day, widely abundant in oats, beans, peas, and in some specific fruits [60]. Dietary fibers containing insoluble and soluble fibers attained from plants involvinglignin and non-digestible carbohydrates. Soluble fibers consist of viscous fibers such asmucilage, gum, β-glucans, pectin, fructans (inulin, fructooligosaccharides), and hemicellulose (non-viscous fibers). The insoluble fibers consist of some lignin, cellulose, and hemicellulose [61]. While both insoluble and soluble fibers are not digestible and can be fermented by bacteria with the help of enzymes to hydrolyze the fiber, soluble fibers are more easily fermented by the gut bacteria and have prebiotic functions providing a short-chain fatty acids source. As such, short-chain fatty acids are quickly absorbed by the large intestine, can be oxidized, and used for the production of energy. Short-chain fatty acids suchas propionic acid absorption have been found to reducethe synthesis of cholesterol in the liver, leading to lessening the blood cholesterol and enhanced water and sodium absorption into the colonic mucosal cells [62,63]. Alternatively, functional fibers are nondigestible carbohydrates that are either synthesized or extracted (isolated) and manufactured, to confer valuable health effects. Functional fibers are chitosan, β-glucans, chitins, cellulose, gums, fructans, resistant dextrins, lignin, polydextrose, pectin, and resistant starches, polyols, and psylliums [64].
There are numerous studiescarried outonmetabolism diseases to check the effect of oat β-glucan [65]. A meta-analysis that included 17 randomized controlled trials (RCTs) (916 hypercholesterolemic patients) displayed that consumption of β-glucan significantly reduced LDL-C (−0.21 mmol/L (8.1 mg/dL)) [66]. In a randomized, single-blind, wheat bran–controlled study, it revealed that within 8 h if 11 g oat bran β-glucantaken it nearly doubled the plasma secretion of bile acids and reduces serum cholesterol by measuring the metabolite 7-hydroxy-4-cholesten-3-one in the plasma [67].
It is also expected the inclusion of plant stanols or sterols in the diet (2 to 3 g daily) plus vegetable oils. Other target food items used in reducing total cholesterol include cold-water fishes, such as salmon, sardines, and mackerel, which have rich omega-3 fatty acid contents, widely recognized for lowering triglyceride levels. Similarly, soybeans present in soy, nuts, tofu, and various meat items have a potent antioxidant effect that can help in lowering LDL-C [60].
2.4.2. Pharmacological Therapy
Among the various drugs available to manage HC, HMG-CoA reductase inhibitors, bile acid resins, fibric acids, niacin, and ezetimibe, are the most often used, as briefly described below.
HMG-CoA Reductase Inhibitors (Atorvastatin, Lovastatin, Simvastatin, Fluvastatin, Rosuvastatin, Pravastatin)
In de novo cholesterol biosynthesis, statins act by inhibiting the 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, disrupting the conversion of HMG-CoA into mevalonate, which is a rate-limiting step. From this activity, a reduction in LDL-C synthesis and enhancement in LDL-C catabolism mediated via LDL receptors emerge as the primary mechanisms for statins’ lipid-lowering effects [60,68].
Bile Acid Resins (Colesevelam, Colestipol, Cholestyramine)
The major action of bile acid resins (BARs) is to bind bile acids in the region of the intestinal lumen, with a concurrent interruption of enterohepatic circulation of bile acids, which then leads to a decrease in the pool size of bile acid and provokes the bile acids hepatic synthesis from cholesterol. Then, the hepatic pool of cholesterol depletion results in an enhancement in cholesterol biosynthesis and rising in LDL receptors number in the hepatocyte membrane, provoking and stimulating an increase in catabolism rate from plasma, which consequently reduces the LDL-C levels. High hepatic cholesterol biosynthesis may be paralleled by high hepatic VLDL production and, in such patients; BARs may exacerbate hypertriglyceridemia and hyperlipidemia [60,68].
Fibric Acids (Gemfibrozil, Fenofibrate, Clofibrate) and Niacin
Among the various fibric acids available, Gemfibrozil reduces the VLDL synthesis to a minimum level, with a simultaneous rise in the rate of apolipoprotein B elimination rich in triglycerides from plasma. Niacin (nicotinic acid) lowers the synthesis of hepatic VLDL, causing a reduction in LDL synthesis. In addition, by reducing its catabolism, niacin raises the HDL-C levels [56,57]. In general, Gemfibrozil or niacin is more effective than clofibrate in lowering VLDL-C production [60,68].
Ezetimibe
Ezetimibe restricts cholesterol absorption within the intestinal brush border; this is the unique mechanism that makes it superior for adjunctive therapy, supported as monotherapy, or used with statins. The daily dose given is 10 mg once, with or without food. It is worth mentioning that the use of Ezetimibe alone results in approx. 18% reduction in LDL cholesterol level, while when used in combination with statins, an LDL-C reduction of 12 to 20% is stated [60,68].
2.4.3. Herbal Treatment
It is widely recognized that Mother Nature has a plethora of potential. With a broad spectrum of activity, a systematic review has suggested that medicinal plants are also rich sources of compounds with anti-HC action rather than saturated fat; plant sterols containing drinks and margarine or stanols can reduce the plasma cholesterol up to 10% [68].
3. Yogurt
3.1. Concept, History, and Health Effects
Yogurt (also spelled “yoghourt” or “yoghurt”) is a fermented milk-based product believed by some regulatory agencies worldwide as lactose-free and defined explicitly by containing Streptococcus thermophilus and Lactobacillus bulgaricus viable bacterial strains [69]. In ancient times, the use of yogurt for food purposes was recognized by other names over the millennia: cuajada (Spain), mast (Iran), katyk (Armenia), matsoni (Georgia, Russia, and Japan),roba (Sudan), zabadi (Egypt), laban (Iraq and Lebanon), dahi (India), coalhada (Portugal), leben raib (Saudi Arabia), iogurte (Brazil) and dovga (Azerbaijan). Indeed, it has been reported that milk-based products were added to the human diet near around 10,000–5000 BC, with the help of domestic milk-producing animals (such asgoats, cows, yaks, sheep, and camels, as well as buffalo and horses) [70].
Indian Ayurveda dated back approx. 6000 BC, about the health-related benefits of having fermented milk-based items [69]. These days, around 700 different cheeses and yogurt items are consumed as part of Indian food. Yogurt was well known in the ROman and Greek empires, and the Greeks were the first to mention it in written references in 100 BC, noting the use of yogurt by barbarous nations [69]. In the book Bible, Abraham owed his long life and fecundity to consuming yogurt, as is referenced in the description of the “Land of Milk and Honey,” which several historians claim refers to yogurt [69]. Figure 2 summarizes some of the health benefits associated with yogurt consumption. Both yogurts’ bacterial and non-bacterial components are believed to play health-promoting effects in human health, specifically on the host’s immune system. Among other constituents, bioactive peptides, conjugated linoleic acid (CLA), group B vitamins, c-aminobutyric acid are a few metabolites are found in yogurt, and where the dairy products matrix, bioactive metabolites (i.e., exopolysaccharides and peptides) secreted throughout fermentation along with the active enzymes, fermentation process, are responsible for the health benefits of yogurt [71,72]. Based on fat content, the three most important types of yogurts currently available are low-fat, regular, and non-fat yogurts. Low-fat yogurts are made from partially skim or low-fat milk, whereas regular yogurt is formed from full-fat milk. Skim milk is also used for non-fat yogurt [73]. The nutritional composition of yogurt is shown in Table 2.
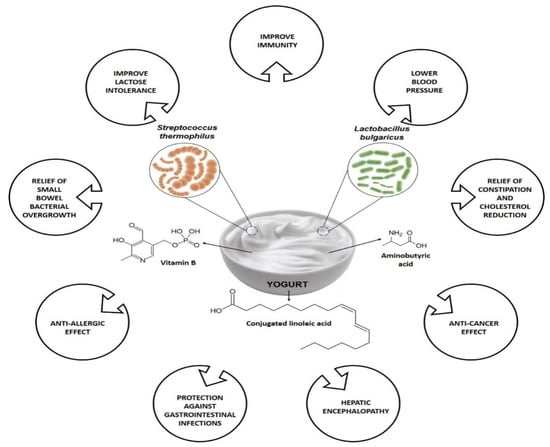
Figure 2.
Variety of health benefits of yogurt consumption.

Table 2.
Composition of nutrients in yogurt with different fat content [74].
3.2. Concept of Food Enrichment
An enriched food refers to the food where nutrients have been added to supplement the product with nutrients that are usually present in the original form, but were removed during processing. For example, white bread is a commonly consumed enriched food where some specific vitamins are added because the bleaching process, depletes them [75].
In a broad sense, despite both enrichment and fortification refer to the addition of nutrients in food, the accurate definition varies. The WHO and the Food and Agricultural Organization of the United Nations (FAO) identifies the term fortification as “the practicing deliberately increasing the essential micronutrient content, i.e., minerals (including trace elements) and vitamins in food irrespective of whether the nutritional components were primarily present before processing in food or not, so this is to enhance the quality of the nutrients food supply and to avail public health benefit with least health risk”, whereas the term enrichment is defined as “synonymous with fortification and refers to the adding micronutrients in food which are removed during the time of processing” [75].
3.3. Phyto-Enrichment of Yogurt
Plants produce a broad pool of secondary metabolites that, among other functions, help them to adapt to various types of harsh environments, and defend them from different pests and microbial attacks, and resist all kinds of abiotic and biotic stresses. In this broad group of secondary metabolites, phenolic compounds have gained significant attention these days because of their anti-mutagenic, antioxidant, anti-clotting, and anti-inflammatory potential, which has been directly linked to their ability to decrease the risk of cardiovascular diseases and cancer development [76,77,78].
Phenolic compounds are the primary dietary source found in fruits [79]. It has been increasingly underlined that fruit juices, extracts, and powders show different biological activities, owing to which they have been used as functional ingredients in the food industry, such as dairy food industries [80,81]. Nonetheless, it is also worthy to note that the seasonal variation in vegetables and fruit production and the high demand for fresh fruits in the market have led researchers to explore alternative sources and strategies for the bioproduction of naturally-occurring bioactive compounds similar to phenolic acids and anthocyanins [82]. For example, plant callus andin vitro cell cultures were found to be promising tools for producing anthocyanins and other phenolic compounds, namely cherries, grapes, and carrots [82,83,84]. For instance, thesein vitro cultures have displayed various advantages over fresh fruit extracts in the possibility of producing natural compounds continuously, at a large scale depending on general needs, with less cost and opportunity of alternating the direction of phenolic or other anthocyanin’s biosynthesis [85,86].
In this way, several foodstuffs have also been used, and specifically, yogurt is a well renowned fermented dairy-based product. Despite its nutritional features and significance in the human diet, it is not being used as a chief source of phenolic compounds [87]. In dairy food products, the amount of phenolics is minimal due to cattle feed, including a low quantity of phenolics given, contamination of food production equipment with other sanitizing agents, and bacterial decomposition in milk proteins. Hence, some plant-derived additives have been incorporated to raise the phenolic content of yogurt, including the addition of four types of grape callus and grape varieties as functional ingredients [87,88]. Table 3 shows several studies addressing the impact of phyto-enriched yogurt on human health and general nutritional quality.

Table 3.
Variety of phytoenriched yogurt and their effects on nutritional quality and general health.
Jovanović et al. reported that apple pomace flour (APF)-enriched yogurts presented an increased total phenolic content and antioxidant activity in a dose-dependent manner [107]. Similarly, Jaster et al. revealed that anthocyanins present in strawberries-enriched yogurts were directly correlated with a higher antioxidant activity (ABTS) on the 1st and 7th day of storage for control and fortified yogurt, respectively [90]. A similar trend was stated using the DPPH method, indicating a strong correlation between the antioxidant activity and the anthocyanins content for control and fortified yogurts on the 1st and 7th day, respectively. Marand et al. revealed that after 14 days of storage, the total phenolic content in flaxseed enriched yogurt was higher than that of control yogurt, attributed to the phenolic compounds: ρ-coumaric acid, lignans, ferulic acid, and hydroxycinnamic acid derivatives [98] (Figure 3). The authors also showed that flaxseed-derived proteins are rich in sulfur amino acids (Met and Cys) and that the lignan protein joined with γ-tocopherol acts as a valuable, healthy compound, presenting good antioxidant activity. Helal and Tagliazucchi demonstrated in their study that in the supernatant of fortified yogurt, the addition of cinnamon powder led to a significant increase in the content of total phenolics as compared to the supernatant of plain yogurt [94]. The most valuable monomeric phenolic compounds present in the supernatant of cinnamon-fortified yogurt were cinnamaldehyde, identified and quantified by HPLC. Finally, Georgakouli et al. revealed that the intake of olive fruit polyphenol-enriched yogurt (400 g) with encapsulated olive polyphenols (experimental condition, EC; 50 mg) significantly reduced body mass index, body weight, hip circumference, and systolic blood pressure in nonsmoking volunteers when compared to plain yogurt (control condition, CC) after two weeks [103].
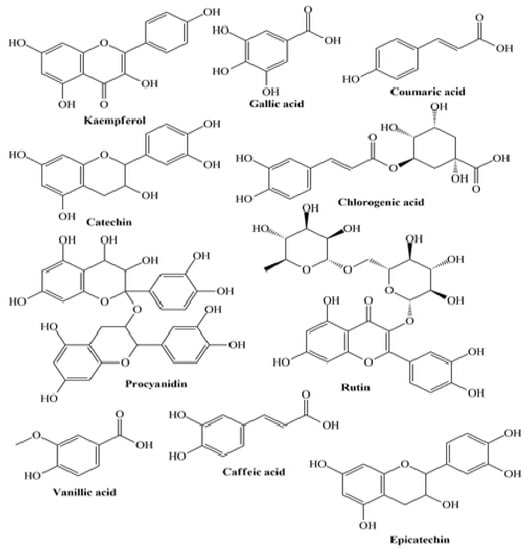
Figure 3.
Some plant-derived phytocompounds present in enriched yogurt.
4. Phyto-Enriched Yogurt and Hypercholesterolemia Management: Clinical Evidence
There has been an increasing interest in addressing the impact of phyto-enriched yogurt in hypercholesterolemia management in clinical studies (Table 4). For example, Buyuktuncer et al., in a double-blind, placebo-controlled randomized study for 4 weeks, given to the control group (n = 35) a placebo yogurt and the intervention (n = 35) group consumed low-fat yogurt (115 g) with 1.9 g/day plant stanols as esters [112]. The main findings were a marked decrease in LDL cholesterol (6.3%), serum total cholesterol (4.6%), and non-HDL cholesterol (6.2%) levels from baseline in the intervention group as compared to the control. Insignificant changes were observed at the anthropometric level during the intervention. Similarly, Párraga-Martínez et al. conducted a double-blind, placebo-controlled study involving 182 adults diagnosed with HC [113]. The authors defined two study groups: the intervention group orally received 2 g of plant stanols containing yogurt drink (n = 91), and the control group received an un-supplemented yogurt (n = 91). At 12 months, the lipid profile, defined as the primary endpoint, was changed. In addition, the authors found a >10% reduction in LDL-C in the intervention group (RR 1.7; 95% CI 1.1–2.7). Similarly, Vásquez-Trespalacios et al. revealed in their study that the consumption of a yogurt drink (regular) supplemented with 4 g stanols (plant origin) added as esters compared to yogurt drink (Benecol®, Colanta) promoted a significant reduction in LDL-C and total cholesterol [114]. Doornbos et al. revealed that as compared to a placebo, a single-dose yogurt drink (100 g) taken with a meal regardless of its fat content led to a marked decrease in LDL-C [115].

Table 4.
Clinical trial studies evaluating the effect of phyto-enriched yogurt on hypercholesterolemic subjects.
5. Conclusions
Yogurt is proclaimed as a healthy fermented milk-derived product containing rich contents of protein of high quality. Several studies have underlined that yogurt has a beneficial effect on individuals suffering from HC due to the presence of conjugated linolenic acid, calcium, casein, probiotics, and proteins. As per the available data, various factors, including the amount of yogurt consumed by the individual under evaluation, fat content, type of milk, and difference among targeted populations, act as direct contributors to the health beneficial effects of yogurt. Additionally, yogurt has been stated to significantly improve the quality of diet and overpower appetite, ultimately helping to regulate glucose metabolism and control obesity. Moreover, supplementation of dietary fiber has been reported to influence the quality parameters of yogurt as they act as bulking agent, colorant, fat replacer, functional ingredient, nutraceutical and probiotic agent. Furthermore, incorporation of dietary fibers has been proclaimed to enhance satiety more effectually in contrast to other beverages. Owing to which, the incorporation of dietary fiber in diet and control intake of food is effective way to regulate the cholesterol level.Despite the low cholesterol levels and saturated fatty acids, yogurt overcomes the negative aspects via its nutrient-rich compositions encompassing various minerals and vitamins that play a substantial role in preventing and treating HC-induced complications.
Nonetheless, yogurt processing degrades its content of minerals, vitamins, and other vital constituents, which have a beneficial effect on an individual’s health. Thus, the overlooked option of enriching yogurt with phytoconstituents has attracted considerable attention. Differentin vitroand clinical studies have provided new insights into the benefits of phytoconstituents for improving gut microbiota and human health. Specifically, studies related to the use of phyto-enriched yogurt have unveiled that it effectively prevents HC and other chronic diseases. Taken together, the data discussed here underline that the phyto-enrichment of yogurt has opened and will even boost new avenues for food sector industries that could serve as an effective and healthy alternative for treating HC, instead of conventional treatment approaches.
Author Contributions
Conceptualization, N.C.-M., N.S.D. and D.K.; writing-review, H.K., K.B. and R.S. (Ruchi Sharma); editing, S.A.S., D.S.D., R.S. (Reena Singh), C.C., A.D. and R.V. All authors have read and agreed to the published version of the manuscript.
Funding
This work received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not Applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Verschuren, W.M.; Jacobs, D.R.; Bloemberg, B.P.; Kromhout, D.; Menotti, A.; Aravanis, C.; Toshima, H. Serum total cholesterol and long-term coronary heart disease mortality in different cultures: Twenty-five-year follow-up of the seven countries study. JAMA 1995, 274, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Stamler, J.; Daviglus, M.L.; Garside, D.B.; Dyer, A.R.; Greenland, P.; Neaton, J.D. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA 2000, 284, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Baigent, C.; Keech, A.; Kearney, P.M.; Blackwell, L.; Buck, G.; Pollicino, C. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90056 participants in 14 randomised trials of statins. Lancet 2005, 366, 1267–1278. [Google Scholar] [PubMed]
- Guallar-Castillón, P.; Gil-Montero, M.; León-Muñoz, L.M.; Graciani, A.; Bayán-Bravo, A.; Taboada, J.M.; Rodríguez-Artalejo, F. Magnitude and management of hypercholesterolemia in the adult population of Spain, 2008–2010: The ENRICA Study. Rev. Esp. Cardiol. 2012, 65, 551–558. [Google Scholar] [CrossRef]
- Catapano, A.L.; Reiner, Ž.; De Backer, G.; Graham, I.; Taskinen, M.R.; Wiklund, O.; Wood, D. ESC/EAS Guidelines for the management of dyslipidaemias: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis 2011, 217, 1–44. [Google Scholar] [CrossRef]
- Kuulasmaa, K.; Tunstall-Pedoe, H.; Dobson, A.; Fortmann, S.; Sans, S.; Tolonen, H.; Ferrario, M. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet 2000, 355, 675–687. [Google Scholar] [CrossRef]
- Flores-Mateo, G.; Grau, M.; O’Flaherty, M.; Ramos, R.; Elosua, R.; Violan-Fors, C.; Capewell, S. Analyzing the coronary heart disease mortality decline in a Mediterranean population: Spain 1988-2005. Rev. Esp. Cardiol. 2011, 64, 988–996. [Google Scholar] [CrossRef]
- Rodŕiguez-Artalejo, F.; Guallar-Castillon, P.; Banegas, J.R. Critical review and proposals for improvement of the health information systems on cardiovascular diseases in Spain. Med. Clin. 2008, 131, 302–311. [Google Scholar]
- Supiyev, A.; Nurgozhin, T.; Zhumadilov, Z.; Peasey, A.; Hubacek, J.A.; Bobak, M. Prevalence, awareness, treatment and control of dyslipidemia in older persons in urban and rural population in the Astana region, Kazakhstan. BMC Public Health 2017, 17, 1–9. [Google Scholar] [CrossRef] [Green Version]
- He, J.; Gu, D.; Reynolds, K.; Wu, X.; Muntner, P.; Zhao, J.; Whelton, P.K. Serum total and lipoprotein cholesterol levels and awareness, treatment, and control of hypercholesterolemia in China. Circulation 2004, 110, 405–411. [Google Scholar] [CrossRef] [Green Version]
- Carroll, M.D.; Lacher, D.A.; Sorlie, P.D.; Cleeman, J.I.; Gordon, D.J.; Wolz, M.; Johnson, C.L. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA 2005, 294, 1773–1781. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Primatesta, P.; Poulter, N.R. Levels of dyslipidaemia and improvement in its management in England: Results from the Health Survey for England 2003. Clin. Endocrinol. 2006, 64, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.D.; Lacher, D.A.; Wolz, M.; Sorlie, P.D. 30-year trends in serum lipids among United States adults: Results from the national health and nutrition examination surveys II, III, and 1999–2006. Am. J. Cardiol. 2011, 107, 1868–1870. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Vital signs: Prevalence, treatment, and control of high levels of low-density lipoprotein cholesterol—United States, 1999–2002 and 2005–2008. MMWR Morb. Mortal. Wkly Rep. 2011, 60, 109–114. [Google Scholar]
- Roth, G.A.; Fihn, S.D.; Mokdad, A.H.; Aekplakorn, W.; Hasegawa, T.; Lim, S.S. High total serum cholesterol, medication coverage and therapeutic control: An analysis of national health examination survey data from eight countries. Bull. World Health Organ. 2011, 89, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Kumar, M.; Nagpal, R.; Kumar, R.; Hemalatha, R.; Verma, V.; Kumar, A.; Yadav, H. Cholesterol-lowering probiotics as potential biotherapeutics for metabolic diseases. Exp. Diabetes Res. 2012, 2012, 902717. [Google Scholar] [CrossRef] [Green Version]
- Anandharaj, M.; Sivasankari, B.; Parveen Rani, R. Effects of probiotics, prebiotics, and synbiotics on hypercholesterolemia: A review. Chin. J. Biol. 2014, 572754, 1–7. [Google Scholar] [CrossRef]
- Proestos, C. Superfoods: Recent data on their role in the prevention of diseases. Curr. Res. Nutr. Food Sci. J. 2018, 6, 576–593. [Google Scholar] [CrossRef]
- van den Driessche, J.J.; Plat, J.; Mensink, R.P. Effects of superfoods on risk factors of metabolic syndrome: A systematic review of human intervention trials. Food Funct. 2018, 9, 1944–1966. [Google Scholar] [CrossRef]
- Astrup, A. Yogurt and dairy product consumption to prevent cardiometabolic diseases: Epidemiologic and experimental studies. Am. J. Clin. Nutr. 2014, 99, 1235S–1242S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandez, M.A.; Panahi, S.; Daniel, N.; Tremblay, A.; Marette, A. Yogurt and cardiometabolic diseases: A critical review of potential mechanisms. Adv. Nutr. 2017, 8, 812–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lordan, R.; Tsoupras, A.; Mitra, B.; Zabetakis, I. Dairy fats and cardiovascular disease: Do we really need to be concerned? Foods 2018, 7, 29. [Google Scholar] [CrossRef] [Green Version]
- Şanlier, N.; Gökcen, B.B.; Sezgin, A.C. Health benefits of fermented foods. Crit. Rev. Food Sci. Nutr. 2019, 59, 506–527. [Google Scholar] [PubMed]
- Wang, H.; Livingston, K.A.; Fox, C.S.; Meigs, J.B.; Jacques, P.F. Yogurt consumption is associated with better diet quality and metabolic profile in American men and women. Nutr. Res. 2013, 33, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Hidayat, K.; Yu, L.G.; Yang, J.R.; Zhang, X.Y.; Zhou, H.; Shi, Y.J.; Qin, L.Q. The association between milk consumption and the metabolic syndrome: A cross-sectional study of the residents of Suzhou, China and a meta-analysis. Br. J. Nutr. 2020, 123, 1013–1023. [Google Scholar] [CrossRef]
- Cormier, H.; Thifault, É.; Garneau, V.; Tremblay, A.; Drapeau, V.; Pérusse, L.; Vohl, M.C. Association between yogurt consumption, dietary patterns, and cardio-metabolic risk factors. Eur. J. Nutr. 2016, 55, 577–587. [Google Scholar] [CrossRef]
- Gijsbers, L.; Ding, E.L.; Malik, V.S.; De Goede, J.; Geleijnse, J.M.; Soedamah-Muthu, S.S. Consumption of dairy foods and diabetes incidence: A dose-response meta-analysis of observational studies. Am. J. Clin. Nutr. 2016, 103, 1111–1124. [Google Scholar] [CrossRef] [Green Version]
- Buendia, J.R.; Li, Y.; Hu, F.B.; Cabral, H.J.; Bradlee, M.L.; Quatromoni, P.A.; Moore, L.L. Regular yogurt intake and risk of cardiovascular disease among hypertensive adults. Am. J. Hypertens 2018, 31, 557–565. [Google Scholar] [CrossRef]
- Watanabe, D.; Kuranuki, S.; Sunto, A.; Matsumoto, N.; Nakamura, T. Daily yogurt consumption improves glucose metabolism and insulin sensitivity in young nondiabetic Japanese subjects with type-2 diabetes risk alleles. Nutrients 2018, 10, 1834. [Google Scholar] [CrossRef] [Green Version]
- Bridge, A.; Brown, J.; Snider, H.; Nasato, M.; Ward, W.E.; Roy, B.D.; Josse, A.R. Greek yogurt and 12 weeks of exercise training on strength, muscle thickness and body composition in lean, untrained, university-aged males. Front. Nutr. 2019, 6, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panahi, S.; Gallant, A.; Tremblay, A.; Pérusse, L.; Després, J.P.; Drapeau, V. The relationship between yogurt consumption, body weight, and metabolic profiles in youth with a familial predisposition to obesity. Eur. J. Clin. Nutr. 2019, 73, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Paththinige, C.S.; Sirisena, N.D.; Dissanayake, V.H.W. Genetic determinants of inherited susceptibility to hypercholesterolemia–a comprehensive literature review. Lipids Health Dis. 2017, 16, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Soutar, A.K.; Naoumova, R.P. Mechanisms of disease: Genetic causes of familial hypercholesterolemia. Nat. Clin. Pract. Cardiovasc. Med. 2007, 4, 214–225. [Google Scholar] [CrossRef]
- Bhatnagar, D.; Soran, H.; Durrington, P.N. Hypercholesterolaemia and its management. BMJ 2008, 337, a993. [Google Scholar] [CrossRef] [Green Version]
- Gupta, R.; Rao, R.S.; Misra, A.; Sharma, S.K. Recent trends in epidemiology of dyslipidemias in India. Indian Heart J. 2017, 69, 382–392. [Google Scholar] [CrossRef]
- Reddy, K.S.; Prabhakaran, D.; Chaturvedi, V.; Jeemon, P.; Thankappan, K.R.; Ramakrishnan, L.; Jaison, T.M. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull. World Health Organ. 2006, 84, 461–469. [Google Scholar] [CrossRef]
- Kinra, S.; Bowen, L.J.; Lyngdoh, T.; Prabhakaran, D.; Reddy, K.S.; Ramakrishnan, L.; Ebrahim, S. Sociodemographic patterning of non-communicable disease risk factors in rural India: A cross sectional study. BMJ 2010, 341, c4974. [Google Scholar] [CrossRef] [Green Version]
- Shah, B.; Mathur, P. Surveillance of cardiovascular disease risk factors in India: The need & scope. Indian J. Med. Res. 2010, 132, 634–642. [Google Scholar]
- Pandey, R.M.; Gupta, R.; Misra, A.; Misra, P.; Singh, V.; Agrawal, A.; Sharma, V. Determinants of urban–rural differences in cardiovascular risk factors in middle-aged women in India: A cross-sectional study. Int. J. Cardio. 2013, 163, 157–162. [Google Scholar] [CrossRef]
- Guptha, S.; Gupta, R.; Deedwania, P.; Bhansali, A.; Maheshwari, A.; Gupta, A.; Sharma, K.K. Cholesterol lipoproteins and prevalence of dyslipidemias in urban Asian Indians: A cross sectional study. Indian Heart J. 2014, 66, 280–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joshi, S.R.; Anjana, R.M.; Deepa, M.; Pradeepa, R.; Bhansali, A.; Dhandania, V.K.; ICMR–INDIAB Collaborative Study Group. Prevalence of dyslipidemia in urban and rural India: The ICMR–INDIAB study. PLoS ONE 2014, 9, e96808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Zahrani, J.; Shubair, M.M.; Al-Ghamdi, S.; Alrasheed, A.A.; Alduraywish, A.A.; Alreshidi, F.S.; Aldossari, K.K. The prevalence of hypercholesterolemia and associated risk factors in Al-Kharj population, Saudi Arabia: A cross-sectional survey. BMC Cardiovas. Disord. 2021, 21, 1–8. [Google Scholar] [CrossRef]
- Blacher, J.; Gabet, A.; Vallée, A.; Ferrières, J.; Bruckert, E.; Farnier, M.; Olié, V. Prevalence and management of hypercholesterolemia in France, the Esteban observational study. Medicine 2020, 99, e23445. [Google Scholar] [CrossRef] [PubMed]
- Polychronopoulos, E.; Panagiotakos, D.B.; Polystipioti, A. Diet, lifestyle factors and hypercholesterolemia in elderly men and women from Cyprus. Lipids Health Dis. 2005, 4, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shawar, S.M.; Al-Bati, N.A.; Al-Mahameed, A.; Nagalla, D.S.; Obeidat, M. Hypercholesterolemia among apparently healthy university students. Oman Med. J. 2012, 27, 274. [Google Scholar] [CrossRef] [PubMed]
- Khonputsa, P.; Veerman, J.L.; Vos, T.; Aekplakorn, W.; Bertram, M.; Abbott-Klafter, J.; Lim, S.S. Joint prevalence and control of hypercholesterolemia and hypertension in Thailand: Third national health examination survey. Asia Pac. J. Public Health 2012, 24, 185–194. [Google Scholar] [CrossRef]
- Posadas-Romero, C.; Tapia-Conyer, R.; Lerman-Garber, I.; Zamora-González, J.; Cardoso-Saldaña, G.; Salvatierra-Izaba, B.; Sepúlveda-Amor, J.A. Cholesterol levels and prevalence of hypercholesterolemia in a Mexican adult population. Atherosclerosis 1995, 118, 275–284. [Google Scholar] [CrossRef]
- Aryan, Z.; Mahmoudi, N.; Sheidaei, A.; Rezaei, S.; Mahmoudi, Z.; Gohari, K.; Farzadfar, F. The prevalence, awareness, and treatment of lipid abnormalities in Iranian adults: Surveillance of risk factors of non-communicable diseases in Iran 2016. J. Clin. Lipidol. 2018, 12, 1471–1481. [Google Scholar] [CrossRef]
- Caroll, M.D.; Cheryl, D.F.; Duong, T.N. Total and High-density Lipoprotein Cholesterol in Adults: United States, 2015–2016. 2017. Available online: https://www.cdc.gov/nchs/data/databriefs/db290.pdf. (accessed on 12 December 2020).
- Fujiyoshi, N.; Arima, H.; Satoh, A.; Ojima, T.; Nishi, N.; Okuda, N.; NIPPON DATA 2010 Research Group. Associations between socioeconomic status and the prevalence and treatment of hypercholesterolemia in a general Japanese population: NIPPON DATA2010. J. Atheroscler. Thromb. 2018, 25, 606–620. [Google Scholar] [CrossRef] [Green Version]
- Zaman, M.M.; Choudhury, S.R.; Ahmed, J.; Talukder, M.H.; Rahman, A.S. Blood glucose and cholesterol levels in adult population of Bangladesh: Results from STEPS 2006 survey. Indian Heart J. 2016, 68, 52–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rifin, H.M.; Lourdes, T.G.R.; Ab Majid, N.L.; Abd Hamid, H.A.; Hasani, W.S.R.; Ling, M.Y.; Omar, M.A. Hypercholesterolemia prevalence, awareness, treatment and control among adults in Malaysia: The 2015 National Health and Morbidity Survey, Malaysia. Glob. J. Health Sci. 2018, 10, 1–11. [Google Scholar] [CrossRef]
- Olusi, S.O.; Prabha, K.; Sulaiman, A.; Sugathan, T.N. Prevalence of hypercholesterolemia in a Kuwaiti hospital outpatient population. Ann. Saudi. Med. 1997, 17, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, D.; Morgan, J.; Siddiq, S.; Mackness, M.I.; Miller, J.P.; Durrington, P.N. Outcome of case finding among relatives of patients with known heterozygous familial hypercholesterolemia. BMJ 2000, 321, 1497. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, C.E.D.S.; França, C.N.; Correr, C.J.; Zucker, M.L.; Andriolo, A.; Scartezini, M. Clinical correlation between a point-of-care testing system and laboratory automation for lipid profile. Clin. Chim. Acta 2015, 446, 263–266. [Google Scholar] [CrossRef]
- Owen, W.E.; Thatcher, M.L.; Crabtree, K.J.; Greer, R.W.; Strathmann, F.G.; Straseski, J.A.; Genzen, J.R. Body fluid matrix evaluation on a Roche cobas 8000 system. Clin. Biochem. 2015, 48, 911–914. [Google Scholar] [CrossRef]
- Singh, A.; Dubey, A.; Sonker, A.; Chaudhary, R. Evaluation of various methods of point-of care testing of haemoglobin concentration in blood donors. Blood Transfus. 2014, 29, 1–7. [Google Scholar]
- Matteucci, E.; Della Bartola, L.; Rossi, L.; Pellegrini, G.; Giampietro, O. Improving CardioCheck PA analytical performance: Three-year study. Clin. Chem. Lab. Med. 2014, 52, 1291–12966. [Google Scholar] [CrossRef]
- Gupta, M.; Vandana, S.; Sidharth, M. Hyperlipidemia: An Updated Review. Int. J. Biopharm. Toxicol. Res. 2011, 1, 81–89. [Google Scholar]
- Soliman, G.A. Dietary fiber, atherosclerosis, and cardiovascular disease. Nutrients 2019, 11, 1155. [Google Scholar] [CrossRef] [Green Version]
- Anderson, J.W. Dietary fiber, lipids and atherosclerosis. Am. J. Cardiol. 1987, 60, 17–22. [Google Scholar] [CrossRef]
- Anderson, J.W.; Baird, P.; Davis, R.H., Jr.; Ferreri, S.; Knudtson, M.; Koraym, A.; Waters, V.; Williams, C.L. Health benefits of dietary fiber. Nutr. Rev. 2009, 67, 188–205. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.S.; Smith, J. Advanced Nutrition and Human Metabolism, 6th ed.; Wadsworth Publishing: Belmont, CA, USA, 2013. [Google Scholar]
- Nie, Y.; Luo, F. Dietary fiber: An opportunity for a global control of hyperlipidemia. Oxid. Med. Cell Longev. 2021, 2021, 5542342. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Sun, X.; Wang, M.; Zhang, C.; Cao, Y.; Mo, G.; Liang, J.; Zhu, S. Quantitative assessment of the effects of beta-glucan consumption on serum lipid profile and glucose level in hypercholesterolemic subjects. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 714–723. [Google Scholar] [CrossRef]
- Andersson, M.; Ellegård, L.; Andersson, H. Oat bran stimulates bile acid synthesis within 8 h as measured by 7α-hydroxy-4-cholesten-3-one. Am. J. Clin. Nutr. 2002, 76, 1111–1116. [Google Scholar] [CrossRef] [Green Version]
- Dhaliya, S.A.; Surya, A.S.; Dawn, V.T.; Betty, C.; Arun, K.; Sunil, C. A review of hyperlipidemia and medicinal plants. Int. JA PS BMS 2013, 2, 219–237. [Google Scholar]
- Fisberg, M.; Machado, R. History of yogurt and current patterns of consumption. Nutr. Rev. 2015, 73, 4–7. [Google Scholar] [CrossRef] [Green Version]
- Aznar, L.A.M.; Ral, P.C.; Ortega Anta, R.M.; Díaz Martín, J.J.; Baladia, E.; Basulto, J.; Salas-Salvado, J. Scientific evidence about the role of yogurt and other fermented milks in the healthy diet for the spanish population. Nutr. Hosp. 2013, 28, 2039–2089. [Google Scholar]
- Pei, R.; Martin, D.A.; DiMarco, D.M.; Bolling, B.W. Evidence for the effects of yogurt on gut health and obesity. Crit. Rev. Food Sci. Nutr. 2017, 57, 1569–1583. [Google Scholar] [CrossRef]
- Fernandez, M.A.; Marette, A. Novel perspectives on fermented milks and cardiometabolic health with a focus on type 2 diabetes. Nutr. Rev. 2018, 76, 16–28. [Google Scholar] [CrossRef] [Green Version]
- Weerathilake, W.A.D.V.; Rasika, D.M.D.; Ruwanmali, J.K.U.; Munasinghe, M.A.D.D. The evolution, processing, varieties and health benefits of yogurt. Int. J. Sci. Res. Publ. 2014, 4, 1–10. [Google Scholar]
- United States Department of Agriculture (USDA). Yogurt. 2020. Available online: https://reedir.arsnet.usda.gov/codesearchwebapp/(S(v04bt44vdd5jhdz0lbv5s1he))/codesearch.aspx (accessed on 18 December 2020).
- Kumar, H.; Bhardwaj, K.; Kuča, K.; Sharifi-Rad, J.; Verma, R.; Machado, M.; Kumar, D.; Cruz-Martins, N. Edible mushrooms’ enrichment in food and feed: A mini review. Int. J. Food Sci. Tech. 2022, 57, 1386–1398. [Google Scholar] [CrossRef]
- Fresco, P.; Borges, F.; Marques, M.P.M.; Diniz, C. The anticancer properties of dietary polyphenols and its relation with apoptosis. Curr. Pharm. Des. 2010, 16, 114–134. [Google Scholar] [CrossRef] [Green Version]
- Loke, W.M.; Proudfoot, J.M.; Hodgson, J.M.; McKinley, A.J.; Hime, N.; Magat, M.; Croft, K.D. Specific dietary polyphenols attenuate atherosclerosis in apolipoprotein E–knockout mice by alleviating inflammation and endothelial dysfunction. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 749–757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ostertag, L.M.; O’Kennedy, N.; Kroon, P.A.; Duthie, G.G.; De Roos, B. Impact of dietary polyphenols on human platelet function–a critical review of controlled dietary intervention studies. Mol. Nutr. Food Res. 2010, 54, 60–81. [Google Scholar] [CrossRef] [PubMed]
- Record, I.R.; Dreosti, I.E.; McInerney, J.K. Changes in plasma antioxidant status following consumption of diets high or low in fruit and vegetables or following dietary supplementation with an antioxidant mixture. Br. J. Nutr. 2001, 85, 459–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coïsson, J.D.; Travaglia, F.; Piana, G.; Capasso, M.; Arlorio, M. Euterpe oleracea juice as a functional pigment for yogurt. Food Res. Int. 2005, 38, 893–897. [Google Scholar] [CrossRef]
- Wallace, T.C.; Giusti, M.M. Determination of color, pigment, and phenolic stability in yogurt systems colored with nonacylated anthocyanins from Berberis boliviana L. as compared to other natural/synthetic colorants. J. Food Sci. 2008, 73, C241–C248. [Google Scholar] [CrossRef]
- Blando, F.; Gerardi, C.; Nicoletti, I. Sour cherry (Prunus cerasus L.) anthocyanins as ingredients for functional foods. J. Biomed. Biotechnol. 2004, 2004, 253. [Google Scholar] [CrossRef] [Green Version]
- Gläßgen, W.E.; Wray, V.; Strack, D.; Metzger, J.W.; Seitz, H.U. Anthocyanins from cell suspension cultures of Daucus carota. Phytochemistry 1992, 31, 1593–1601. [Google Scholar] [CrossRef]
- Hiroyuki, H.; Kousuke, H.; Eiji, N.; Mariko, O.; Yoshihito, K.; Setsuro, H.; Takeshi, K. Enhanced anthocyanin production from grape callus in an air-lift type bioreactor using a viscous additive-supplemented medium. J. Biosci. Bioeng. 2002, 94, 135–139. [Google Scholar] [CrossRef]
- Curtin, C.; Zhang, W.; Franco, C. Manipulating anthocyanin composition in Vitis vinifera suspension cultures by elicitation with jasmonic acid and light irradiation. Biotechnol. Lett. 2003, 25, 1131–1135. [Google Scholar] [CrossRef] [PubMed]
- Plata, N.; Konczak-Islam, I.; Jayram, S.; McClelland, K.; Woolford, T.; Franks, P. Effect of methyl jasmonate and p-coumaric acid on anthocyanin composition in a sweet potato cell suspension culture. Biochem. Eng. J. 2003, 14, 171–177. [Google Scholar] [CrossRef]
- O’connell, J.E.; Fox, P.F. Significance and applications of phenolic compounds in the production and quality of milk and dairy products: A review. Int. Dairy J. 2001, 11, 103–120. [Google Scholar] [CrossRef]
- Karaaslan, M.; Ozden, M.; Vardin, H.; Turkoglu, H. Phenolic fortification of yogurt using grape and callus extracts. LWT 2011, 44, 1065–1072. [Google Scholar] [CrossRef]
- Sah, B.N.P.; Vasiljevic, T.; McKechnie, S.; Donkor, O.N. Effect of pineapple waste powder on probiotic growth, antioxidant and antimutagenic activities of yogurt. J. Food Sci. Technol. 2016, 53, 1698–1708. [Google Scholar] [CrossRef]
- Jaster, H.; Arend, G.D.; Rezzadori, K.; Chaves, V.C.; Reginatto, F.H.; Petrus, J.C.C. Enhancement of antioxidant activity and physicochemical properties of yogurt enriched with concentrated strawberry pulp obtained by block freeze concentration. Food Res. Int. 2018, 104, 119–125. [Google Scholar] [CrossRef]
- Shokery, E.S.; El-Ziney, M.G.; Yossef, A.H.; Mashaly, R.I. Effect of green tea and Moringa leave extracts fortification on the physicochemical, rheological, sensory and antioxidant properties of set-type yoghurt. Adv. Dairy Res. 2017, 5, 2. [Google Scholar] [CrossRef]
- Dhawi, F.; El-Beltagi, H.S.; Aly, E.; Hamed, A.M. Antioxidant, antibacterial activities and mineral content of buffalo yoghurt fortified with fenugreek and Moringa oleifera seed flours. Foods 2020, 9, 1157. [Google Scholar] [CrossRef]
- Bertolino, M.; Belviso, S.; Dal Bello, B.; Ghirardello, D.; Giordano, M.; Rolle, L.; Zeppa, G. Influence of the addition of different hazelnut skins on the physicochemical, antioxidant, polyphenol and sensory properties of yogurt. LWT 2015, 63, 1145–1154. [Google Scholar] [CrossRef] [Green Version]
- Helal, A.; Tagliazucchi, D. Impact of in-vitro gastro-pancreatic digestion on polyphenols and cinnamaldehyde bioaccessibility and antioxidant activity in stirred cinnamon-fortified yogurt. LWT 2018, 89, 164–170. [Google Scholar] [CrossRef]
- Bchir, B.; Bouaziz, M.A.; Blecker, C.; Attia, H. Physico-Chemical, antioxidant activities, textural, and sensory properties of yoghurt fortified with different states and rates of pomegranate seeds (Punica granatum L.). J.Texture Stud. 2020, 51, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Cho, W.Y.; Yeon, S.J.; Choi, S.H.; Lee, C.H. Effects of lotus (Nelumbo nucifera) leaf on quality and antioxidant activity of yogurt during refrigerated storage. Food Sci. Anim. Resour. 2019, 39, 792. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.A.M.; Alqah, H.A.; Saleh, A.; Al-Juhaimi, F.Y.; Babiker, E.E.; Ghafoor, K.; Fickak, A. Physicochemical quality attributes and antioxidant properties of set-type yogurt fortified with argel (Solenostemma argel Hayne) leaf extract. LWT 2021, 137, 110389. [Google Scholar] [CrossRef]
- Marand, M.A.; Amjadi, S.; Marand, M.A.; Roufegarinejad, L.; Jafari, S.M. Fortification of yogurt with flaxseed powder and evaluation of its fatty acid profile, physicochemical, antioxidant, and sensory properties. Powder Technol. 2020, 359, 76–84. [Google Scholar] [CrossRef]
- Nguyen, L.; Hwang, E.S. Quality characteristics and antioxidant activity of yogurt supplemented with aronia (Aronia melanocarpa) juice. Prev. Nutr. Food Sci. 2016, 21, 330. [Google Scholar] [CrossRef]
- Hernández-Carranza, P.; Jattar-Santiago, K.Y.; Avila-Sosa, R.; Pérez-Xochipa, I.; Guerrero-Beltrán, J.A.; Ochoa-Velasco, C.E.; Ruiz-López, I.I. Antioxidant fortification of yogurt with red cactus pear peel and its mucilage. CyTAJ. Food 2019, 17, 824–833. [Google Scholar] [CrossRef] [Green Version]
- Suharto, E.L.S.; Arief, I.I.; Taufik, E. Quality and antioxidant activity of yogurt supplemented with roselle during cold storage. J. Exot. Pet. Med. 2016, 39, 82–89. [Google Scholar] [CrossRef] [Green Version]
- Cho, W.Y.; Yeon, S.J.; Hong, G.E.; Kim, J.H.; Tsend-Ayush, C.; Lee, C.H. Antioxidant activity and quality characteristics of yogurt added green olive powder during storage. Korean J. Food Sci. Anim. Resour. 2017, 37, 865. [Google Scholar]
- Georgakouli, K.; Mpesios, A.; Kouretas, D.; Petrotos, K.; Mitsagga, C.; Giavasis, I.; Jamurtas, A.Z. The effects of an olive fruit polyphenol-enriched yogurt on body composition, blood redox status, physiological and metabolic parameters and yogurt microflora. Nutrients 2016, 8, 344. [Google Scholar] [CrossRef] [Green Version]
- Jeong, C.H.; Ryu, H.; Zhang, T.; Lee, C.H.; Seo, H.G.; Han, S.G. Green tea powder supplementation enhances fermentation and antioxidant activity of set-type yogurt. Food Sci. Biotechnol. 2018, 27, 1419–1427. [Google Scholar] [CrossRef]
- Shori, A.B.; Baba, A.S. Antioxidant activity and inhibition of key enzymes linked to type-2 diabetes and hypertension by Azadirachta indica-yogurt. J. Saudi Chem. Soc. 2013, 17, 295–301. [Google Scholar] [CrossRef]
- Marchiani, R.; Bertolino, M.; Belviso, S.; Giordano, M.; Ghirardello, D.; Torri, L.; Zeppa, G. Yogurt enrichment with grape pomace: Effect of grape cultivar on physicochemical, microbiological and sensory properties. J. Food Qual. 2016, 39, 77–89. [Google Scholar] [CrossRef]
- Jovanović, M.; Petrović, M.; Miočinović, J.; Zlatanović, S.; LaličićPetronijević, J.; Mitić-Ćulafić, D.; Gorjanović, S. Bioactivity and sensory properties of probiotic yogurt fortified with apple pomace flour. Foods 2020, 9, 763. [Google Scholar] [CrossRef] [PubMed]
- Sigdel, A.; Ojha, P.; Karki, T.B. Phytochemicals and syneresis of osmo-dried mulberry incorporated yoghurt. Food Sci. Nutr. 2018, 6, 1045–1052. [Google Scholar] [CrossRef] [Green Version]
- Shori, A.B. Storage quality and antioxidant properties of yogurt fortified with polyphenol extract from nutmeg, black pepper, and white pepper. Electron. J. Biotechnol. 2022, 57, 24–30. [Google Scholar] [CrossRef]
- Shahein, M.R.; Atwaa, E.S.H.; El-Zahar, K.M.; Elmaadawy, A.A.; Hijazy, H.H.A.; Sitohy, M.Z.; Albrakati, A.; Elmahallawy, E.K. Remedial action of yoghurt enriched withwatermelon seed milk on renal injured hyperuricemic rats. Fermentation 2022, 8, 41. [Google Scholar] [CrossRef]
- Atwaa, E.S.H.; Shahein, M.R.; El-Sattar, E.S.A.; Hijazy, H.H.A.; Albrakati, A.; Elmahallawy, E.K. Bioactivity, physciochemcial and sensory properties of probitoic yoghurt made from whole milk powder reconstituted in aqueous fennel extract. Fermentation 2022, 8, 52. [Google Scholar] [CrossRef]
- Buyuktuncer, Z.; Fisunoğlu, M.; Guven, G.S.; Unal, S.; Besler, H.T. The cholesterol lowering efficacy of plant stanol ester yoghurt in a Turkish population: A double-blind, placebo-controlled trial. Lipids Health Dis. 2013, 12, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Párraga-Martínez, I.; López-Torres-Hidalgo, J.D.; Del Campo, J.M.; Galdón-Blesa, M.P.; Precioso-Yáñez, J.C.; Rabanales-Sotos, J.; Lloret-Callejo, Á. Long-term effects of plant stanols on the lipid profile of patients with hypercholesterolemia. A randomized clinical trial. Rev. Esp. Cardiol. 2015, 68, 665–671. [Google Scholar] [CrossRef]
- Vásquez-Trespalacios, E.M.; Romero-Palacio, J. Efficacy of yogurt drink with added plant stanol esters (Benecol®, Colanta) in reducing total and LDL cholesterol in subjects with moderate hypercholesterolemia: A randomized placebo-controlled crossover trial NCT01461798. Lipids Health Dis. 2014, 13, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doornbos, A.M.E.; Meynen, E.M.; Duchateau, G.S.M.J.E.; Van der Knaap, H.C.M.; Trautwein, E.A. Intake occasion affects the serum cholesterol lowering of a plant sterol-enriched single-dose yoghurt drink in mildly hypercholesterolaemic subjects. Eur. J. Clin. Nutr. 2006, 60, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Ferro, Y.; Mazza, E.; Salvati, M.; Santariga, E.; Giampà, S.; Spagnuolo, R.; Montalcini, T. Effects of a Portfolio-Mediterranean Diet and a Mediterranean Diet with or without a Sterol-Enriched Yogurt in Individuals with Hypercholesterolemia. Endocrino. Metabol. 2020, 35, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Volpe, R.; Niittynen, L.; Korpela, R.; Sirtori, C.; Bucci, A.; Fraone, N.; Pazzucconi, F. Effects of yoghurt enriched with plant sterols on serum lipids in patients with moderate hypercholesterolaemia. Br. J. Nutr. 2001, 86, 233–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Penchalaraju, M.; Kuna, A.; Shailaja, P.S.S.; Kumar, K.V.; Devi, P.U.; Supraja, T.; Jones, P.J. Cholesterol-lowering efficacy of plant sterol-enriched flavored milk, yogurt, fruit bar, and soya milk in mild hypercholesterolemic Indian subjects. Clin. J. Nutr. Diet 2018, 1, 1–6. [Google Scholar]
- Hyun, Y.J.; Kim, O.Y.; Kang, J.B.; Lee, J.H.; Jang, Y.; Liponkoski, L.; Salo, P. Plant stanol esters in low-fat yogurt reduces total and low-density lipoprotein cholesterol and low-density lipoprotein oxidation in normocholesterolemic and mildly hypercholesterolemic subjects. Nutr. Res. 2005, 25, 743–753. [Google Scholar] [CrossRef]
- Noakes, M.; Clifton, P.M.; Doornbos, A.M.; Trautwein, E.A. Plant sterol ester–enriched milk and yoghurt effectively reduce serum cholesterol in modestly hypercholesterolemic subjects. Eur. J. Nutr. 2005, 44, 214–222. [Google Scholar] [CrossRef]
- Rudkowska, I.; AbuMweis, S.S.; Nicolle, C.; Jones, P.J. Cholesterol-lowering efficacy of plant sterols in low-fat yogurt consumed as a snack or with a meal. J. Am. Coll. Nutr. 2008, 27, 588–595. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).