Ezetimibe-Loaded Nanostructured Lipid Carrier Based Formulation Ameliorates Hyperlipidaemia in an Experimental Model of High Fat Diet
Abstract
1. Introduction
2. Results and Discussion
2.1. Phase Solubility Study of EZE between the Lipids
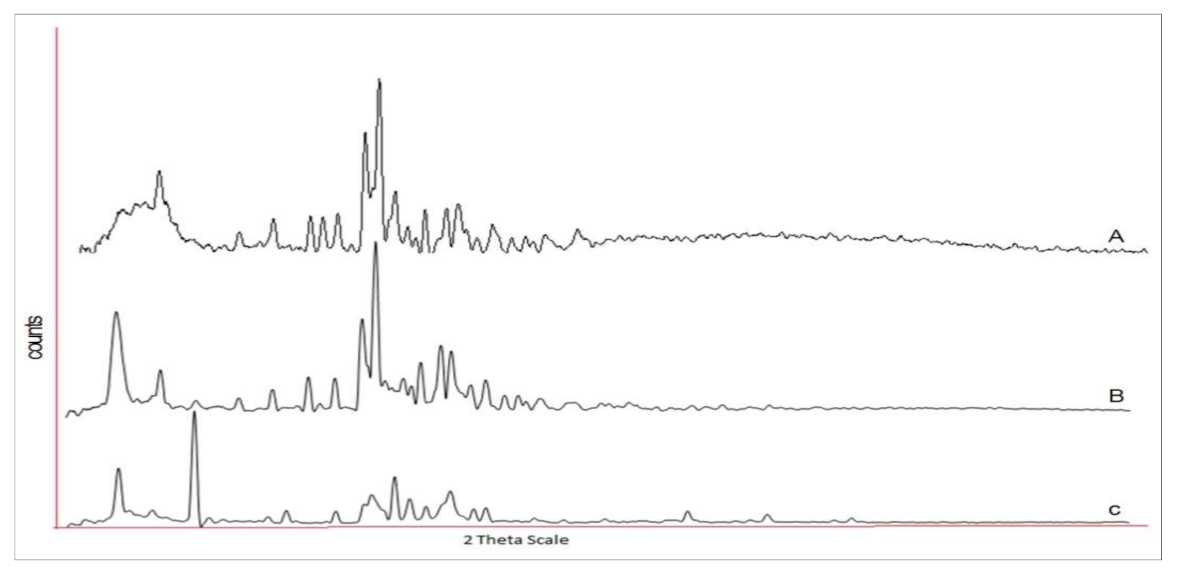
2.2. Development and Optimization of EZE Loaded NLCs by Factorial Design
2.3. Optimization Data Analysis and Model Validation
2.3.1. Fitting of the Data to the Model
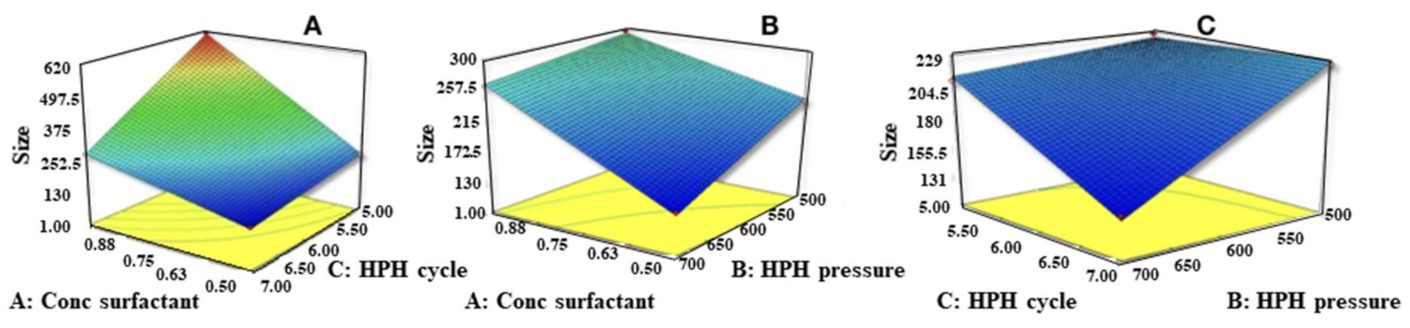
2.3.2. Effects of Independent Variables on Particle Size (Y1)
2.3.3. Effect of Independent Variables on Drug Entrapment Efficiency (Y2)
2.4. Particle Size and Zeta Potential of Optimized EZE Loaded NLC
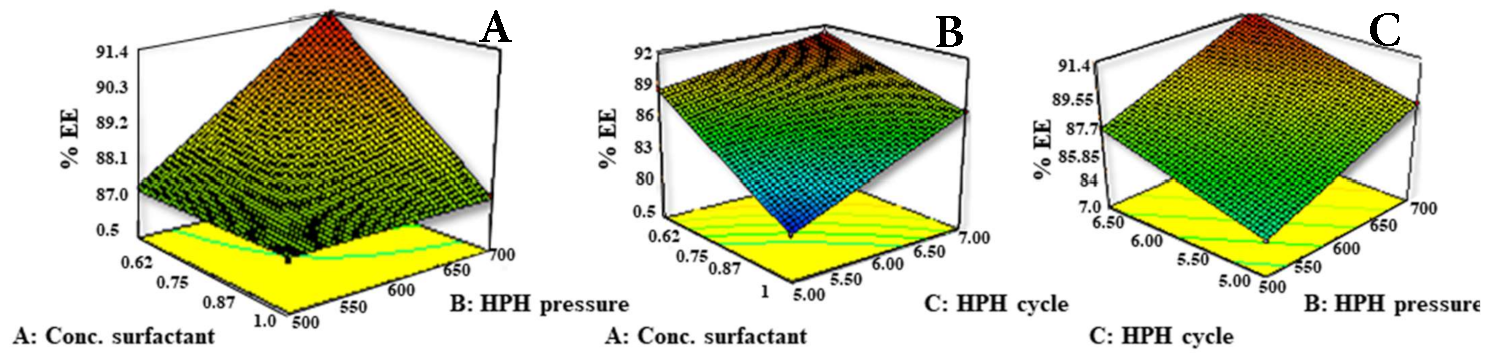
2.5. Thermal Analysis by Differential Scanning Calorimetry (DSC)
2.6. Morphological Analysis by Transmission Electron Microscopy
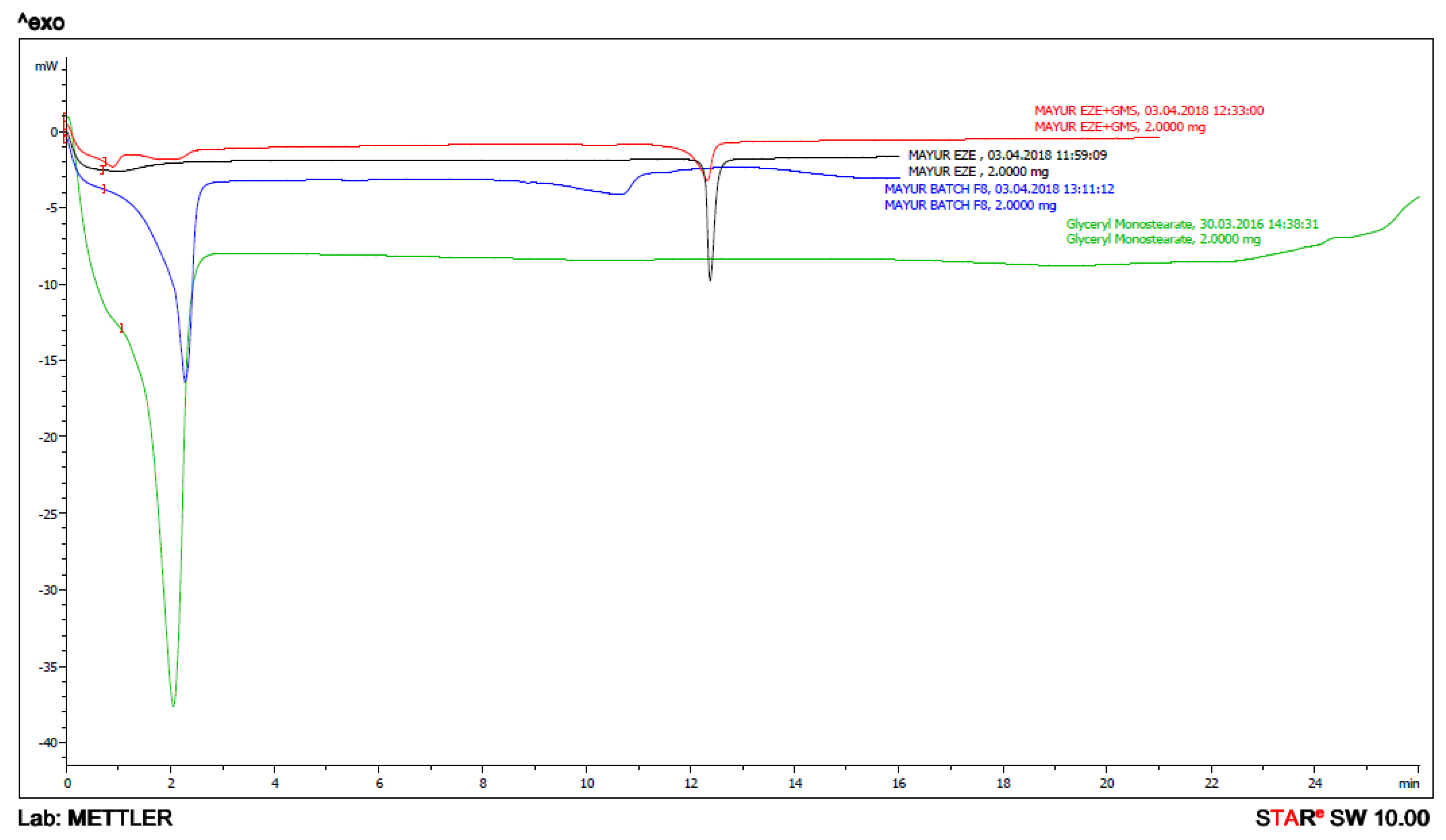
2.7. X-ray Diffraction Studies
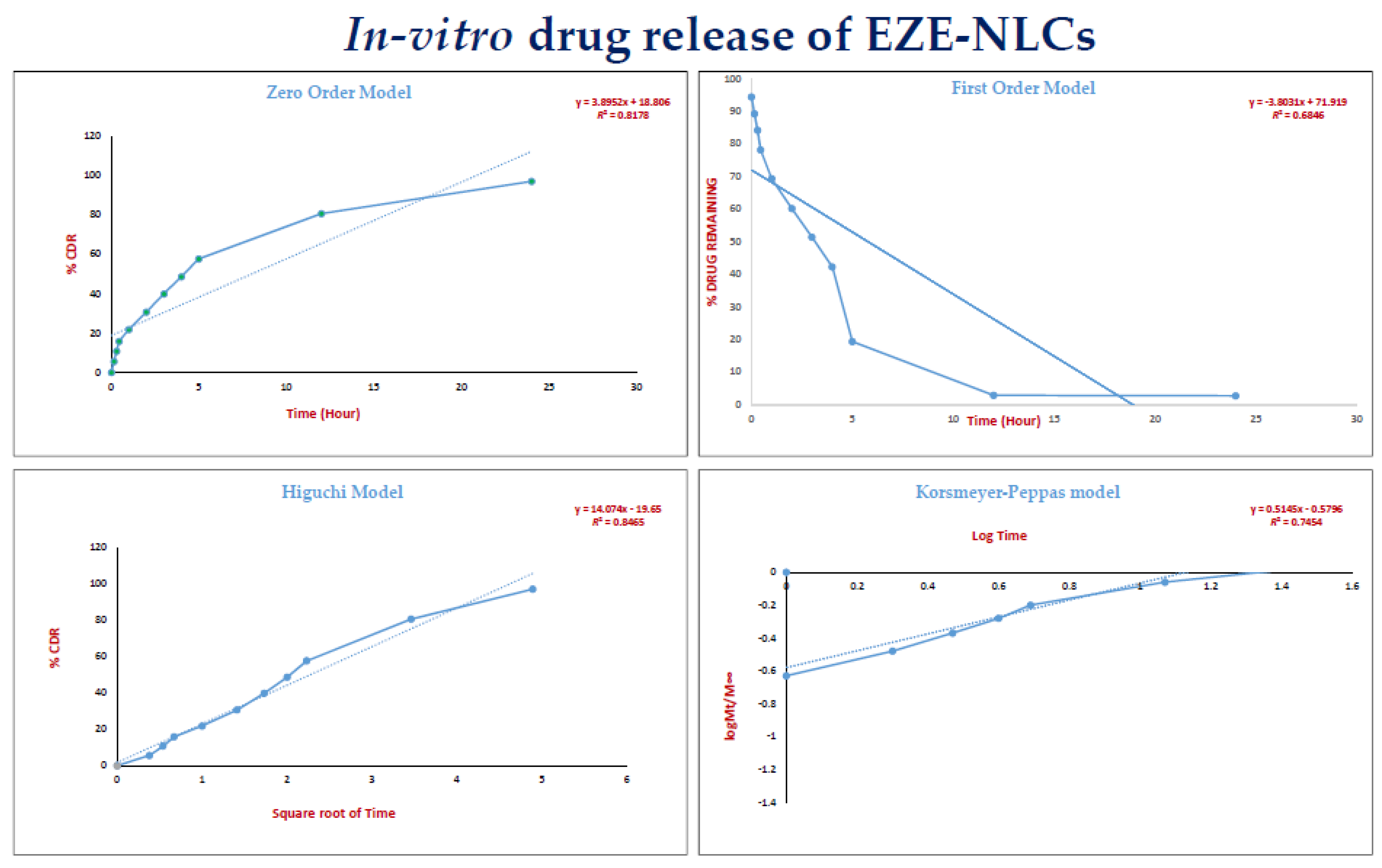
2.8. In-Vitro Drug Release of EZE-NLCs
2.9. Accelerated Stability Studies of EZE-NLCs
2.10. In-Vivo Animal Study
2.10.1. Effect of EZE-NLCs on Lipid Profile in High Fructose Diet (HFD)-Induced Hyperlipidemia
Serum Lipid Analysis
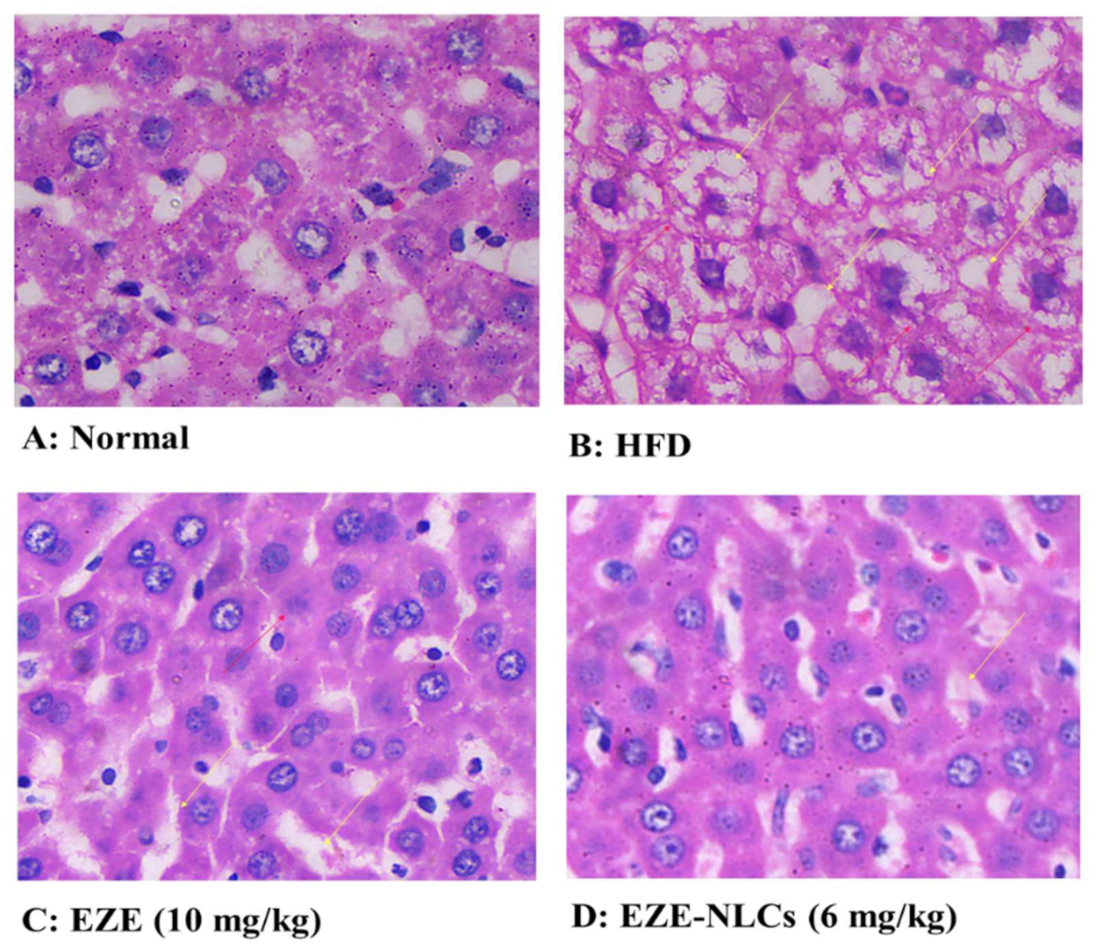
2.10.2. Histopathological Analysis
3. Materials and Methods
3.1. Initial Solubility Studies for screening of Lipids
3.1.1. Solubility of EZE in Liquid Lipids
3.1.2. Solubility of EZE in Solid Lipid
3.2. Preparation of Ezetimibe NLCs
3.3. Design of Experiment (DOE)
3.4. Determination of Particle Size, PDI and Zeta Potential of the EZE-NLCS
3.5. Percentage Entrapment Efficiency (%EE)
3.6. Differential Scanning Calorimetry (DSC)
3.7. Transmission Electron mMicroscopy (TEM) analysis
3.8. X-ray Diffraction Measurements
3.9. Determination of In-Vitro Drug Release from EZE-NLCs
3.10. Accelerated Stability Studies of EZE-NLCs
3.11. In-Vivo Anti-Hyperlipidemic Activity of EZE-NLCs
3.11.1. Animals
3.11.2. Induction of Hyperlipidemia
3.11.3. Experimental Design
3.11.4. Evaluation of Serum Lipid Profiles
3.11.5. Histopathology
3.11.6. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Gupta, R. Burden of coronary heart disease in India. Indian Heart J. 2005, 57, 632–638. [Google Scholar] [PubMed]
- Glass, C.K.; Witztum, J.L. Atherosclerosis: The road ahead. Cell 2001, 104, 503–516. [Google Scholar] [CrossRef]
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American college of cardiology/American heart association task force on practice guidelines. Circulation 2014, 129, S49–S73. [Google Scholar] [CrossRef]
- Patel, J.; Sheehan, V.; Gurk-Turner, G. Ezetimibe (Zetia): A New Type of Lipid-Lowering Agent. Proc. Bayl. Univ. Med. Cent. 2003, 16, 354–358. [Google Scholar] [CrossRef]
- Suchy, D.; Łabuzek, K.; Stadnicki, A.; Okopień, B. Ezetimibe—A new approach in hypercholesterolemia management. Pharm. Rep. 2011, 63, 1335–1348. [Google Scholar] [CrossRef]
- Din, U.F.; Zeb, A.; Shah, K.U.; Zia-ur-Rehman. Development, in-vitro and in-vivo evaluation of ezetimibe-loaded solid lipid nanoparticles and their comparison with marketed product. J. Drug Deliv. Sci. Technol. 2019, 51, 583–590. [Google Scholar] [CrossRef]
- O’Driscoll, C.M.; Griffin, B.T. Biopharmaceutical challenges associated with drugs with low aqueous solubility-The potential impact of lipid-based formulations. Adv. Drug Deliv. Rev. 2008, 60, 617–624. [Google Scholar] [CrossRef]
- Elmowafy, M.; Ibrahim, H.M.; Ahmed, M.A.; Shalaby, K.; Salama, A.; Hefesha, H. Atorvastatin-loaded nanostructured lipid carriers (Nlcs): Strategy to overcome oral delivery drawbacks. Drug Deliv. 2017, 24, 932–941. [Google Scholar] [CrossRef]
- Jawahar, N.; Hingarh, P.K.; Arun, R.; Selvaraj, J.; Anbarasan, A.; Sathianarayanan, S.; Nagaraju, G. Enhanced oral bioavailability of an antipsychotic drug through nanostructured lipid carriers. Int. J. Biol. Macromol. 2018, 110, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Cai, T.; Huang, Y.; Xia, X.; Cole, S.P.C.; Cai, Y. A review of the structure, preparation, and application of NLCs, PNPs, and PLNs. Nanomaterials 2017, 7, 122. [Google Scholar] [CrossRef]
- Agrawal, Y.; Petkar, K.C.; Sawant, K.K. Development, evaluation and clinical studies of Acitretin loaded nanostructured lipid carriers for topical treatment of psoriasis. Int. J. Pharm. 2010, 401, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Xia, Q. Alpha-lipoic acid-loaded nanostructured lipid carrier: Sustained release and biocompatibility to HaCaT cells in vitro. Drug Delivery 2014, 21, 328–341. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Hu, X.; Ma, Y.; Xie, Y.; Lu, Y.; Qi, J.; Xiang, L.; Li, F.; Wu, W. Lipids-based nanostructured lipid carriers (NLCs) for improved oral bioavailability of sirolimus. Drug Deliv. 2016, 23, 1469–1475. [Google Scholar] [CrossRef]
- Charman, W.N. Lipids, lipophilic drugs, and oral drug delivery—Some emerging concepts. J. Pharm. Sci. 2000, 89, 967–978. [Google Scholar] [CrossRef]
- Porter, C.J.H.; Charman, W.N. Intestinal lymphatic drug transport: An update. Adv. Drug Deliv. Rev. 2001, 50, 61–80. [Google Scholar] [CrossRef]
- Mahamuni, S.P.; Khose, R.D.; Menaa, F.; Badole, S.L. Therapeutic approaches to drug targets in hyperlipidemia. BioMedicine 2012, 2, 137–146. [Google Scholar] [CrossRef]
- Gaba, B.; Fazil, M.; Ali, A.; Baboota, S.; Sahni, J.K.; Ali, J. Nanostructured lipid (NLCs) carriers as a bioavailability enhancement tool for oral administration. Drug Deliv. 2015, 22, 691–700. [Google Scholar] [CrossRef]
- Zhou, J.; Zhou, D. Improvement of oral bioavailability of lovastatin by using nanostructured lipid carriers. Drug Des. Devel. Ther. 2015, 9, 5269–5275. [Google Scholar] [CrossRef] [PubMed]
- Prajapati, J.B.; Verma, S.D.; Patel, A.A. Oral bioavailability enhancement of agomelatine by loading into nanostructured lipid carriers: Peyer’s patch targeting approach. Int. J. Nanomed. 2018, 13, 35–38. [Google Scholar] [CrossRef]
- Khan, S.A.; Rehman, S.; Nabi, B.; Iqubal, A.; Nehal, N.; Fahmi, U.A.; Kotta, S.; Baboota, S.; Md, S.; Ali, J. Boosting the brain delivery of Atazanavir through nanostructured lipid carrier-based approach for mitigating neuroaids. Pharmaceutics 2020, 12, 59. [Google Scholar] [CrossRef]
- Agrawal, Y.O.; Mahajan, U.B.; Mahajan, H.S.; Ojha, S. Methotrexate-loaded nanostructured lipid carrier gel alleviates imiquimod-induced psoriasis by moderating inflammation: Formulation, optimization, characterization, in-vitro and in-vivo studies. Int. J. Nanomed. 2020, 15, 4763–4778. [Google Scholar] [CrossRef] [PubMed]
- Bali, V.; Ali, M.; Ali, J. Study of surfactant combinations and development of a novel nanoemulsion for minimising variations in bioavailability of ezetimibe. Colloids Surf. B Biointerfaces 2010, 76, 410–420. [Google Scholar] [CrossRef]
- Ha, E.S.; Kim, J.S.; Baek, I.H.; Hwang, S.J.; Kim, M.S. Enhancement of dissolution and bioavailability of ezetimibe by amorphous solid dispersion nanoparticles fabricated using supercritical antisolvent process. J. Pharm. Investig. 2015, 45, 641–649. [Google Scholar] [CrossRef]
- Thadkala, K.; Nanam, P.K.; Rambabu, B.; Sailu, C.; Aukunuru, J. Preparation and characterization of amorphous ezetimibe nanosuspensions intended for enhancement of oral bioavailability. Int. J. Pharma. Investig. 2014, 4, 131–137. [Google Scholar]
- Das, S.; Ng, W.K.; Tan, R.B.H. Are nanostructured lipid carriers (NLCs) better than solid lipid nanoparticles (SLNs): Development, characterizations and comparative evaluations of clotrimazole-loaded SLNs and NLCs? Eur. J. Pharm. Sci. 2012, 47, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Haider, M.; Abdin, S.M.; Kamal, L.; Orive, G. Nanostructured lipid carriers for delivery of chemotherapeutics: A review. Pharmaceutics 2020, 12, 288. [Google Scholar] [CrossRef]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: Applications, advantages and disadvantages. Res. Pharm. Sci. 2018, 13, 288–303. [Google Scholar]
- Zhang, Q.; Yang, H.; Sahito, B.; Li, X.; Peng, L.; Gao, X.; Ji, H.; Wang, L.; Jiang, S.; Guo, D. Nanostructured lipid carriers with exceptional gastrointestinal stability and inhibition of P-gp efflux for improved oral delivery of tilmicosin. Colloids Surf. B: Biointerfaces 2020, 187, 110649. [Google Scholar] [CrossRef]
- Tofani, R.P.; Sumirtapura, Y.C.; Darijanto, S.T. Formulation, characterisation, and in vitro skin diffusion of nanostructured lipid carriers for deoxyarbutin compared to a nanoemulsion and conventional cream. Sci. Pharm. 2016, 84, 634–645. [Google Scholar] [CrossRef]
- Gardouh, A.; Khafagy, E.S.; Elkady, M. Preparation of self-flocculated solid lipid nanoparticles. J. Res. Pharm. 2019, 23, 652–661. [Google Scholar]
- Managuli, R.S.; Wang, J.T.; Faruqu, F.N.; Kushwah, V.; Raut, S.Y.; Shreya, A.B.; Al-Jamal, K.T.; Jain, S.; Mutalik, S. Asenapine maleate-loaded nanostructured lipid carriers: Optimization and in vitro, ex vivo and in vivo evaluations. Nanomedicine 2019, 14, 889–910. [Google Scholar] [CrossRef]
- Proetto, M.T.; Rush, A.M.; Chien, M.-P.; Baeza, P.A.; Patterson, J.P.; Thompson, M.P.; Olson, N.H.; Moore, C.E.; Rheingold, A.L.; Andolina, C.; et al. Dynamics of soft nanomaterials captured by transmission electron microscopy in liquid water. J. Am. Chem. Soc. 2014, 136, 1162–1165. [Google Scholar] [CrossRef] [PubMed]
- Torras, M.; Roig, A. From Silver Plates to Spherical Nanoparticles: Snapshots of Microwave-Assisted Polyol Synthesis. ACS Omega 2020, 5, 5731–5738. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Mehnert, W.; Müller, R.H. Polymorphic behaviour of Compritol® 888 ATO as bulk lipid and as SLN and NLC. J. Microencapsul. 2006, 23, 417–433. [Google Scholar] [CrossRef] [PubMed]
- Ritger, P.L.; Peppas, N.A. Simple equation for description of solute swellable devices. J. Control. Rel. 1987, 5, 37–42. [Google Scholar] [CrossRef]
- Hixson, A.W.; Crowell, J.H. Dependence of Reaction Velocity upon surface and Agitation. Ind. Eng. Chem. 1931, 23, 923–931. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, G.; Peng, Y.; Wang, M.; Li, X. Anti-hyperglycemic and anti-hyperlipidemic effects of a special fraction of Luohanguo extract on obese T2DM rats. J. Ethnopharmacol. 2020, 247, 112273. [Google Scholar] [CrossRef] [PubMed]
- Tamjidi, F.; Shahedi, M.; Varshosaz, J.; Nasirpour, A. Stability of astaxanthin-loaded nanostructured lipid carriers as affected by pH, ionic strength, heat treatment, simulated gastric juice and freeze–thawing. J. Food Sci. Technol. 2017, 54, 3132–3141. [Google Scholar] [CrossRef]
- Saoji, S.D.; Belgamwar, V.S.; Dharashivkar, S.S.; Rode, A.A.; Mack, C.; Dave, V.S. The Study of the Influence of Formulation and Process Variables on the Functional Attributes of Simvastatin–Phospholipid Complex. J. Pharm. Innov. 2016, 11, 264–278. [Google Scholar] [CrossRef]
- Teng, Z.; Yu, M.; Ding, Y.; Zhang, H.; Shen, Y.; Jiang, M.; Liu, P.; Opoku-Damoah, Y.; Webster, T.J.; Zhou, J. Preparation and characterization of nimodipine-loaded nanostructured lipid systems for enhanced solubility and bioavailability. Int. J. Nanomed. 2019, 14, 119–133. [Google Scholar] [CrossRef]
- Chalikwar, S.S.; Belgamwar, V.S.; Talele, V.R.; Surana, S.J.; Patil, M.U. Formulation and evaluation of Nimodipine-loaded solid lipid nanoparticles delivered via lymphatic transport system. Colloids Surf. B: Biointerfaces 2012, 97, 109–116. [Google Scholar] [CrossRef]
- ZurMühlen, A.; Schwarz, C.; Mehnert, W. Solid lipid nanoparticles (SLN) for controlled drug delivery - Drug release and release mechanism. Eur. J. Pharm. Biopharm. 1998, 45, 149–155. [Google Scholar] [CrossRef]
- Severino, P.; Santana, M.H.A.; Souto, E.B. Optimizing SLN and NLC by 2 2 full factorial design: Effect of homogenization technique. Mater. Sci. Eng. C 2012, 32, 1375–1379. [Google Scholar] [CrossRef] [PubMed]
- Naseri, N.; Valizadeh, H.; Zakeri-Milani, P. Solid lipid nanoparticles and nanostructured lipid carriers: Structure preparation and application. Adv. Pharm. Bull. 2015, 5, 305–313. [Google Scholar] [CrossRef]
- Jenning, V.; Schäfer-Korting, M.; Gohla, S. Vitamin A-loaded solid lipid nanoparticles for topical use: Drug release properties. J. Control. Release 2000, 66, 115–126. [Google Scholar] [CrossRef]
- Wang, X.R.; Gao, S.Q.; Niu, X.Q.; Li, L.J.; Ying, X.Y.; Hu, Z.J.; Gao, J.Q. Capsaicin-loaded nanolipoidal carriers for topical application: Design, characterization, and in vitro/in vivo evaluation. Int. J. Nanomed. 2017, 12, 3881–3898. [Google Scholar] [CrossRef]
- Yang, G.; Wu, F.; Chen, M.; Jin, J.; Wang, R.; Yuan, Y. Formulation design, characterization, and in vitro and in vivo evaluation of nanostructured lipid carriers containing a bile salt for oral delivery of gypenosides. Int. J. Nanomed. 2019, 14, 2267–2280. [Google Scholar] [CrossRef] [PubMed]
- Nordin, N.; Yeap, S.K.; Zamberi, N.R.; Abu, N.; Mohamad, N.E.; Rahman, H.S.; How, C.W.; Masarudin, M.J.; Abdullah, R.; Alitheen, N.B. Characterization and toxicity of citral incorporated with nanostructured lipid carrier. PeerJ 2018, 6, e3916. [Google Scholar] [CrossRef] [PubMed]
- United States Pharmacopeia–National Formulary; United States Pharmacopeial Convention: Rockville, MD, USA, 1980.
- Ajayi, T.; Moody, J.; Odumuwagun, O.; Olugbuyiro, J. Lipid Altering Potential of Moringaoleifera Lam Seed Extract and Isolated Constituents InWistar Rats. J. Biomed. Res. 2020, 23, 77–85. [Google Scholar]
- Karam, I.; Ma, N.; Liu, X.; Li, J.; Yang, Y. Effect of Aspirin on Hyperlipidemia in Rats. JSM Pharmacol. Clin. Toxicol. 2019, 1, 6. [Google Scholar]


| Batch | Particle Size (nm) | PDI | Ζ Potential (mV) | Factor 1 | Factor 2 | Factor 3 | Response 1 | Response2 |
|---|---|---|---|---|---|---|---|---|
| A Conc. Surfactant % | B HPHP Ressure Bar | C No. of HPH Cycle | Particle Size (nm) | Entrapment Efficiency % | ||||
| F1 | 614.4 ± 3.3 | 0.798 ± 0.02 | −22.3 ± 0.5 | 1.00 | 700.00 | 5.00 | 614.4 ± 3.3 | 80.09 ± 1.9 |
| F2 | 550.1 ± 6.0 | 0.715 ± 0.04 | −19.1±0.6 | 1.00 | 500.00 | 5.00 | 550.1 ± 6.0 | 80.40 ± 0.5 |
| F3 | 208.0 ± 2.9 | 0.273 ± 0.03 | −23.6 ± 0.4 | 0.50 | 700.00 | 5.00 | 208.0 ± 2.9 | 88.51 ± 2.4 |
| F4 | 262.0 ± 4.9 | 0.524 ± 0.02 | −27.8 ± 0.6 | 1.00 | 700.00 | 7.00 | 262.0 ± 4.9 | 87.22 ± 0.7 |
| F5 | 227.2 ± 0.9 | 0.358 ± 0.02 | −20.1 ± 0.9 | 0.50 | 500.00 | 5.00 | 227.2 ± 0.9 | 84.07 ± 3.0 |
| F6 | 225.5 ± 4.8 | 0.282 ± 0.02 | −21.9 ± 0.5 | 0.50 | 500.00 | 7.00 | 225.5 ± 4.8 | 87.12 ± 2.0 |
| F7 | 296.7 ± 2.7 | 0.619 ± 0.07 | −26.3 ± 0.5 | 1.00 | 500.00 | 7.00 | 296.7 ± 2.7 | 87.04 ± 1.9 |
| F8 | 134.5 ± 2.5 | 0.244 ± 0.03 | −28.1 ± 0.3 | 0.50 | 700.00 | 7.00 | 134.5 ± 2.5 | 91.32 ± 1.8 |
| Response | Model | R2 | Adjusted R2 | Predicted R2 | F value | P Value | SD (±) | % CV | Mean |
|---|---|---|---|---|---|---|---|---|---|
| Particle Size | 2F1 | 0.9996 | 0.9969 | 0.9717 | 53.506 | 0.0394 | 9.59 | 3.05 | 314.81 |
| Entrapment Efficiency% | 2F1 | 0.9996 | 0.9975 | 0.9772 | 60.906 | 0.0354 | 0.20 | 0.23 | 85.68 |
| Model | (R2) Coefficient of Determination |
|---|---|
| Zero order | 0.8178 |
| First order | 0.6846 |
| Highuchi’s | 0.8465 |
| Korsmeyer-Peppas | 0.7454 |
| PS (nm) | PDI | EE % | |
|---|---|---|---|
| At the time of preparation | 134.5 ± 2.5 | 0.244 ± 0.03 | 91.32 ± 1.8 |
| Storage at Room Temperature (28–30 °C) | |||
| After 1 Month | 197.1 ± 4.9 | 0.333 ± 0.02 | 88.4 ± 1.5 |
| After 2 Month | 282.3 ± 2.0 | 0.417 ± 0.04 | 89.7 ± 1.5 |
| Storage Condition in Refrigerator (2–8 °C) | |||
| After 1 Month | 182.3 ± 3.0 | 0.329 ± 0.02 | 90.1 ± 2.9 |
| After 2 Month | 214.6 ± 3.6 | 0.382 ± 0.01 | 90.6 ± 1.4 |
| Group | Triglyceride (mg/dL) | Total Cholesterol (mg/dL) | LDL-c (mg/dL) | HDL-c (mg/dL) |
|---|---|---|---|---|
| Normal | 76.26 ± 1.96 | 112.2 ± 4.02 | 36.40 ± 4.60 | 84.84 ± 4.37 |
| HFD | 193.00 ± 7.23 ### | 220.7 ± 12.51 ### | 75.95 ± 4.58 ### | 41.19 ± 2.72 ### |
| HFD + EZE (10 mg/kg) | 110.3 ± 15.47 | 144.4 ± 4.61 | 51.58 ± 6.65 | 62.70 ± 6.10 |
| HFD + EZE-NLCs (6 mg/kg) | 90.87 ± 4.92 *** | 119.0 ± 8.28 *** | 35.99 ± 3.63 *** | 82.99 ± 3.19 *** |
| Vacuolization of Hepatocytes | Enlargement Sinusoids | Kupffer-Cell Infiltration | Vascular Congestion | |
|---|---|---|---|---|
| Normal | − | − | + | − |
| HFD | +++ | ++ | +++ | +++ |
| HFD + EZE (10 mg/kg) | ++ | + | + | + |
| HFD + EZE-NLCs (6 mg/kg) | − | + | − | − |
| Independent Variables | Level | ||
|---|---|---|---|
| Low (−1) | Medium (0) | High (+1) | |
| A: Amount of Poloxamer | 0.5 | 0.75 | 1 |
| B: Pressure of HPH | 500 | 600 | 700 |
| C: Number of cycles | 5 | 6 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agrawal, Y.O.; Mahajan, U.B.; Agnihotri, V.V.; Nilange, M.S.; Mahajan, H.S.; Sharma, C.; Ojha, S.; Patil, C.R.; Goyal, S.N. Ezetimibe-Loaded Nanostructured Lipid Carrier Based Formulation Ameliorates Hyperlipidaemia in an Experimental Model of High Fat Diet. Molecules 2021, 26, 1485. https://doi.org/10.3390/molecules26051485
Agrawal YO, Mahajan UB, Agnihotri VV, Nilange MS, Mahajan HS, Sharma C, Ojha S, Patil CR, Goyal SN. Ezetimibe-Loaded Nanostructured Lipid Carrier Based Formulation Ameliorates Hyperlipidaemia in an Experimental Model of High Fat Diet. Molecules. 2021; 26(5):1485. https://doi.org/10.3390/molecules26051485
Chicago/Turabian StyleAgrawal, Yogeeta O., Umesh B. Mahajan, Vinit V. Agnihotri, Mayur S. Nilange, Hitendra S. Mahajan, Charu Sharma, Shreesh Ojha, Chandragouda R. Patil, and Sameer N. Goyal. 2021. "Ezetimibe-Loaded Nanostructured Lipid Carrier Based Formulation Ameliorates Hyperlipidaemia in an Experimental Model of High Fat Diet" Molecules 26, no. 5: 1485. https://doi.org/10.3390/molecules26051485
APA StyleAgrawal, Y. O., Mahajan, U. B., Agnihotri, V. V., Nilange, M. S., Mahajan, H. S., Sharma, C., Ojha, S., Patil, C. R., & Goyal, S. N. (2021). Ezetimibe-Loaded Nanostructured Lipid Carrier Based Formulation Ameliorates Hyperlipidaemia in an Experimental Model of High Fat Diet. Molecules, 26(5), 1485. https://doi.org/10.3390/molecules26051485







