Phytochemical and Ethnopharmacological Perspectives of Ehretia laevis
Abstract
1. Introduction
2. Materials and Methods
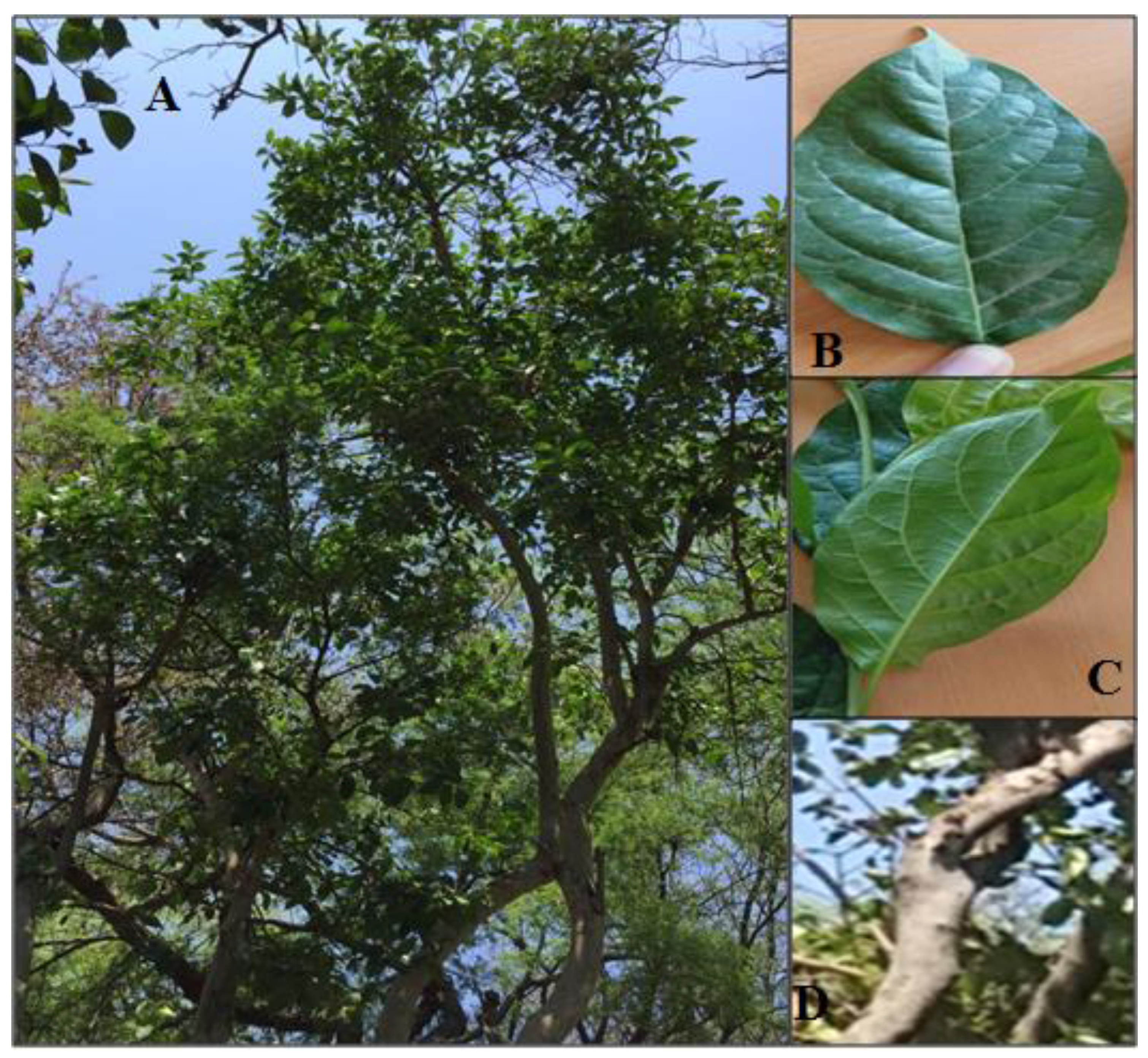
2.1. Botanical Description
2.2. Geographical Distribution
3. Local and Contemporary Uses of E. laevis
4. Phytochemistry
4.1. Pentacyclic Triterpenoids and Phytosterol
4.1.1. Betulinic Acid
4.1.2. Betulin
4.1.3. Lupeol
4.1.4. Ursolic Acid
4.1.5. α-Amyrin
4.1.6. β-Amyrin
4.1.7. β-Sitosterol
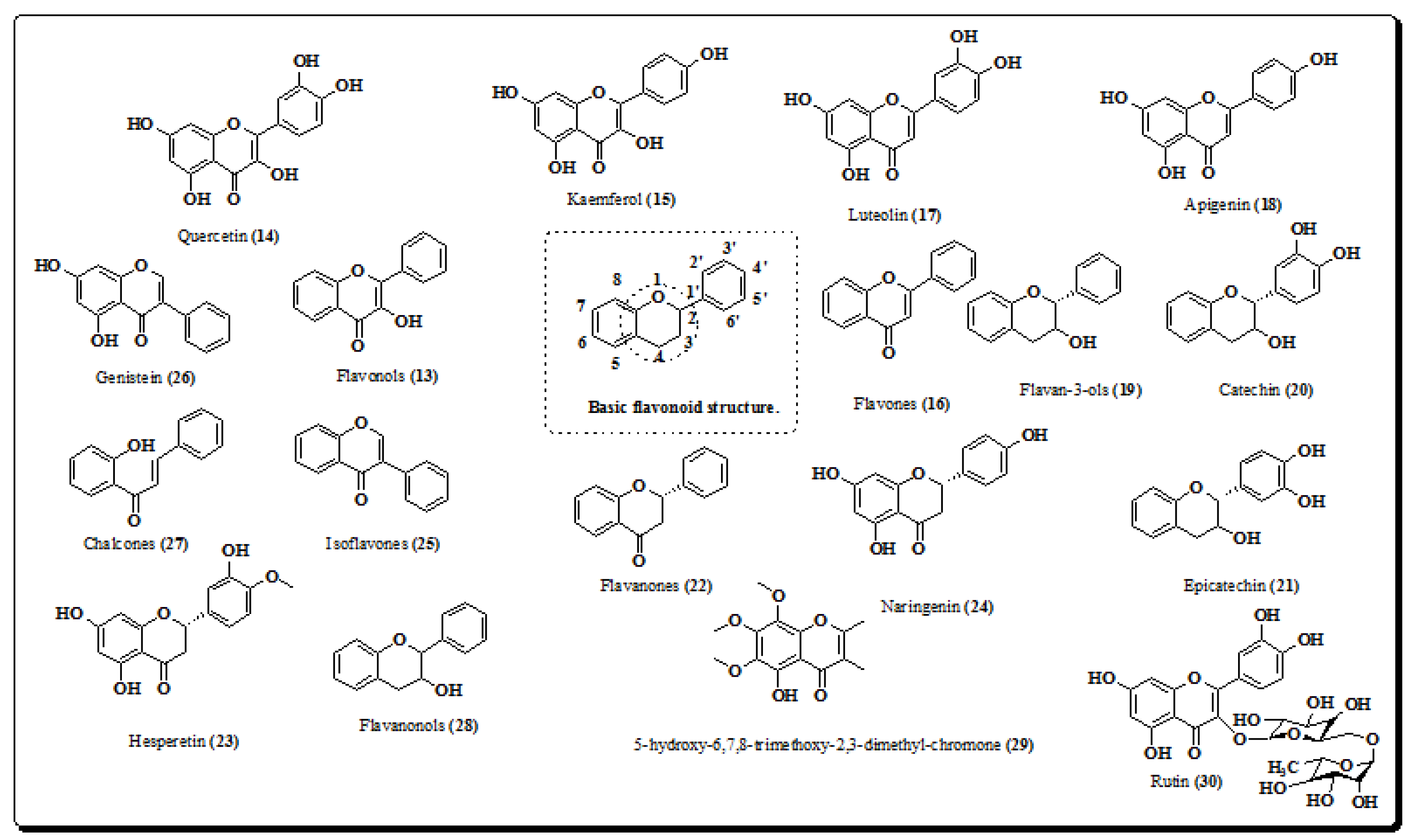
4.2. Flavonoids
4.2.1. Quercetin
4.2.2. Kaempferol
4.2.3. Luteolin
4.2.4. Apigenin
4.2.5. Naringenin
4.2.6. Rutin
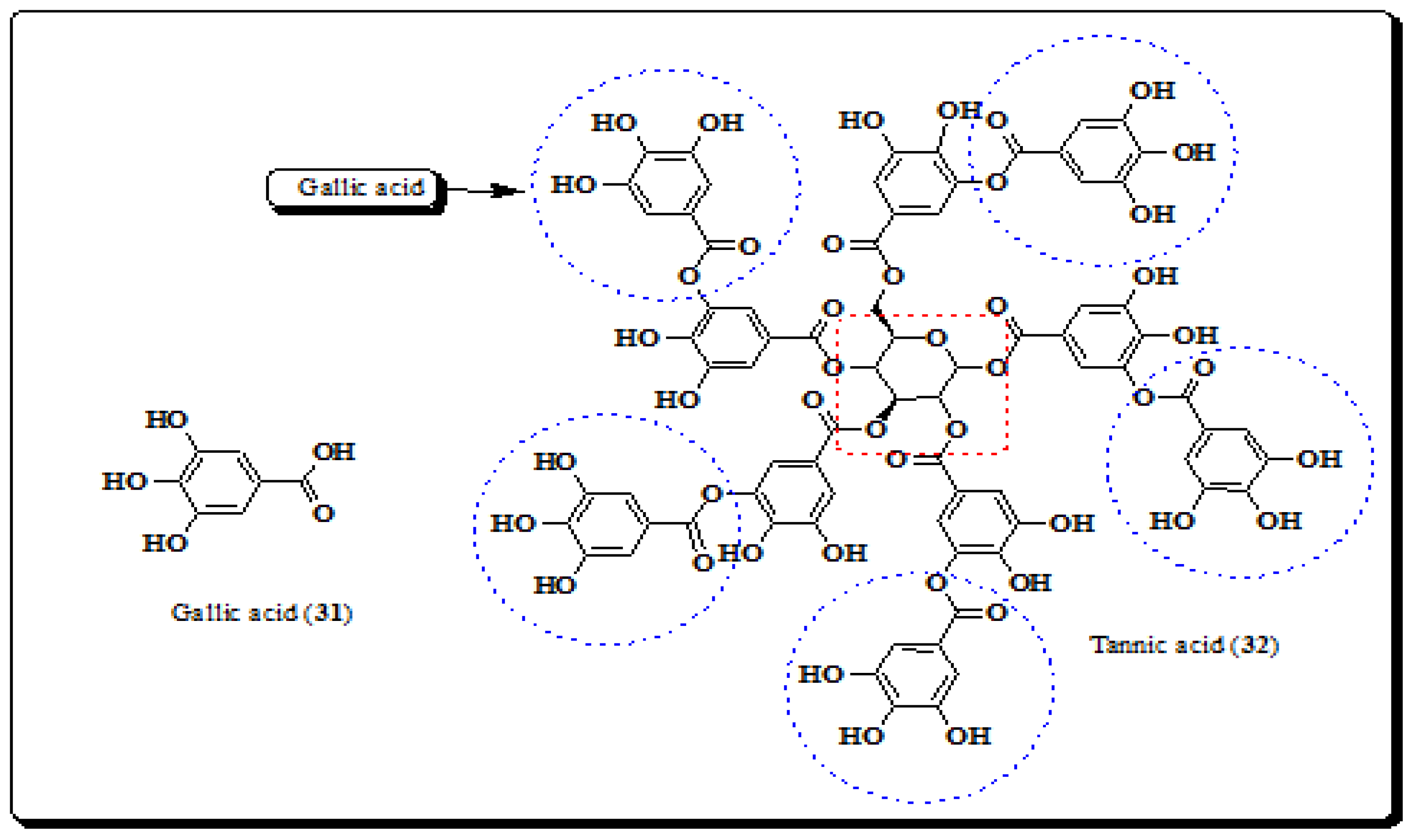
4.3. Phenolic Acids and Tannins
4.3.1. Gallic Acid
4.3.2. Tannic Acid
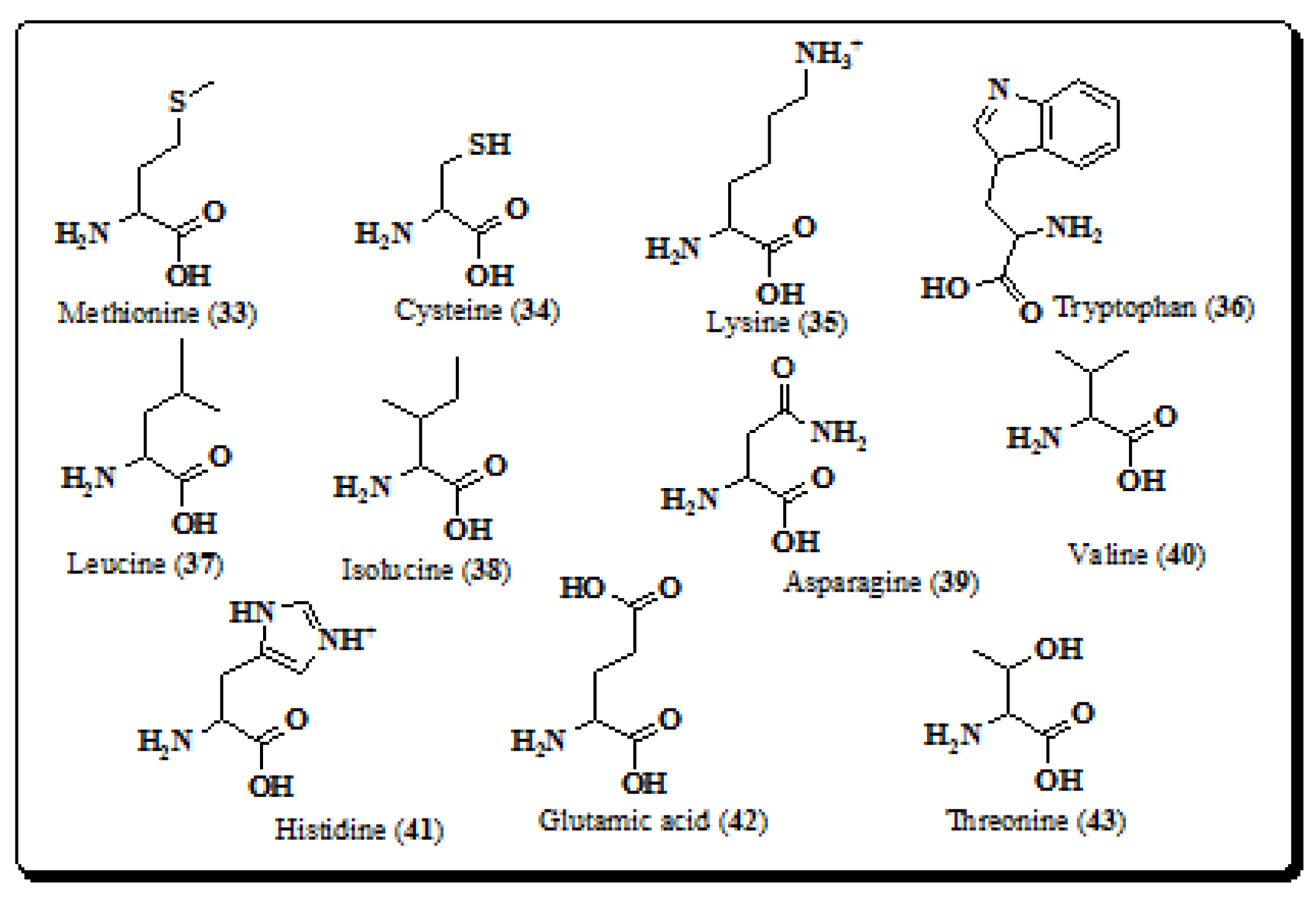
4.4. Amino Acids
4.5. Carbohydrates
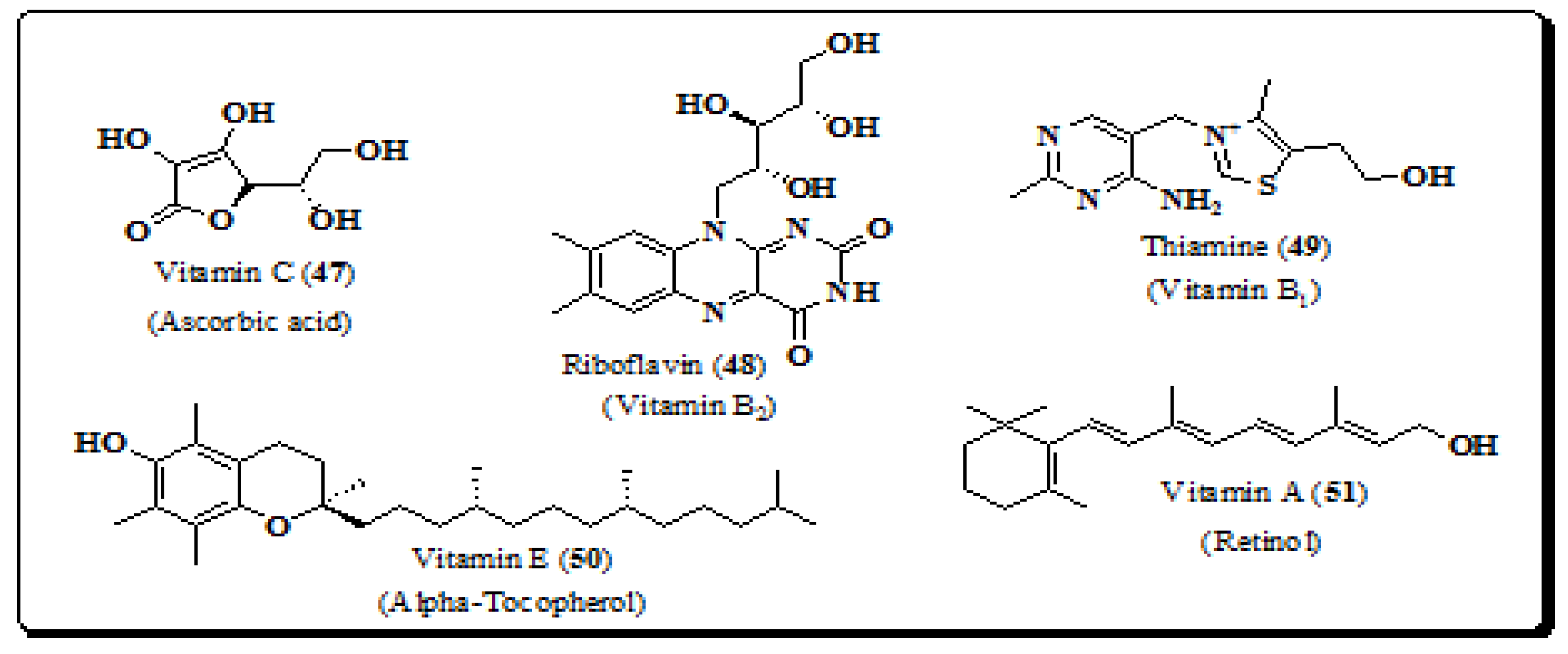
4.6. Vitamins
4.7. Minerals
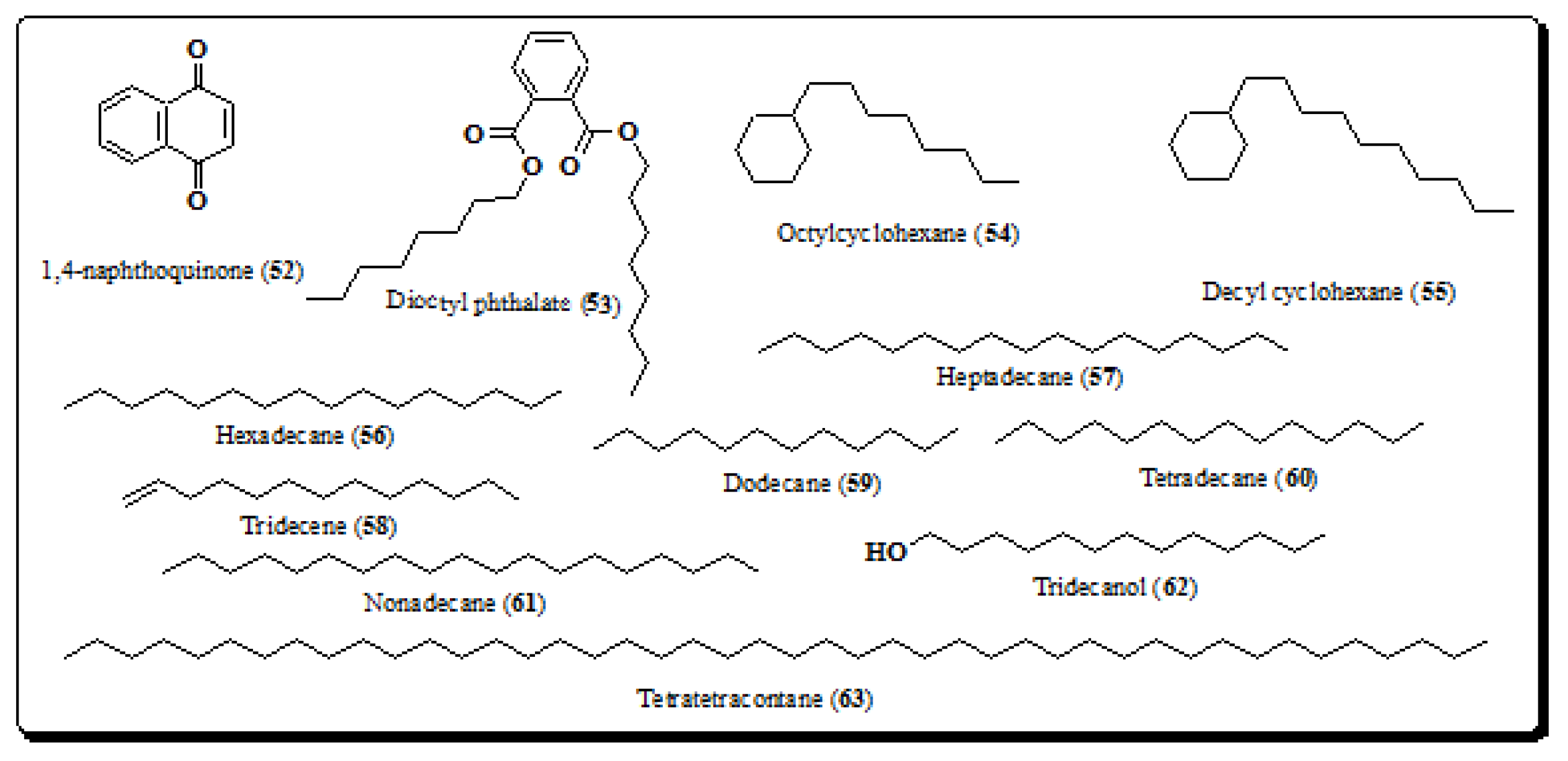
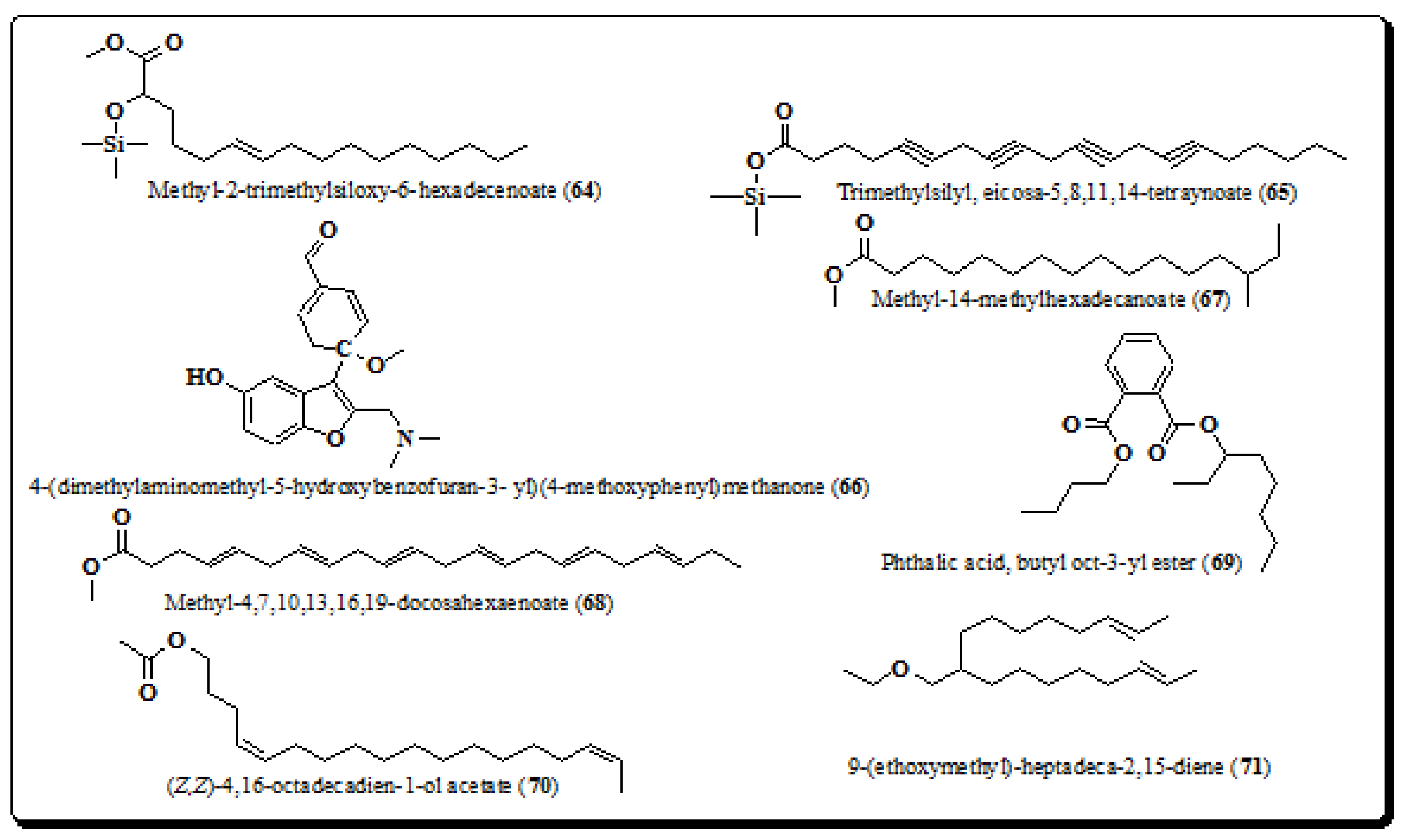
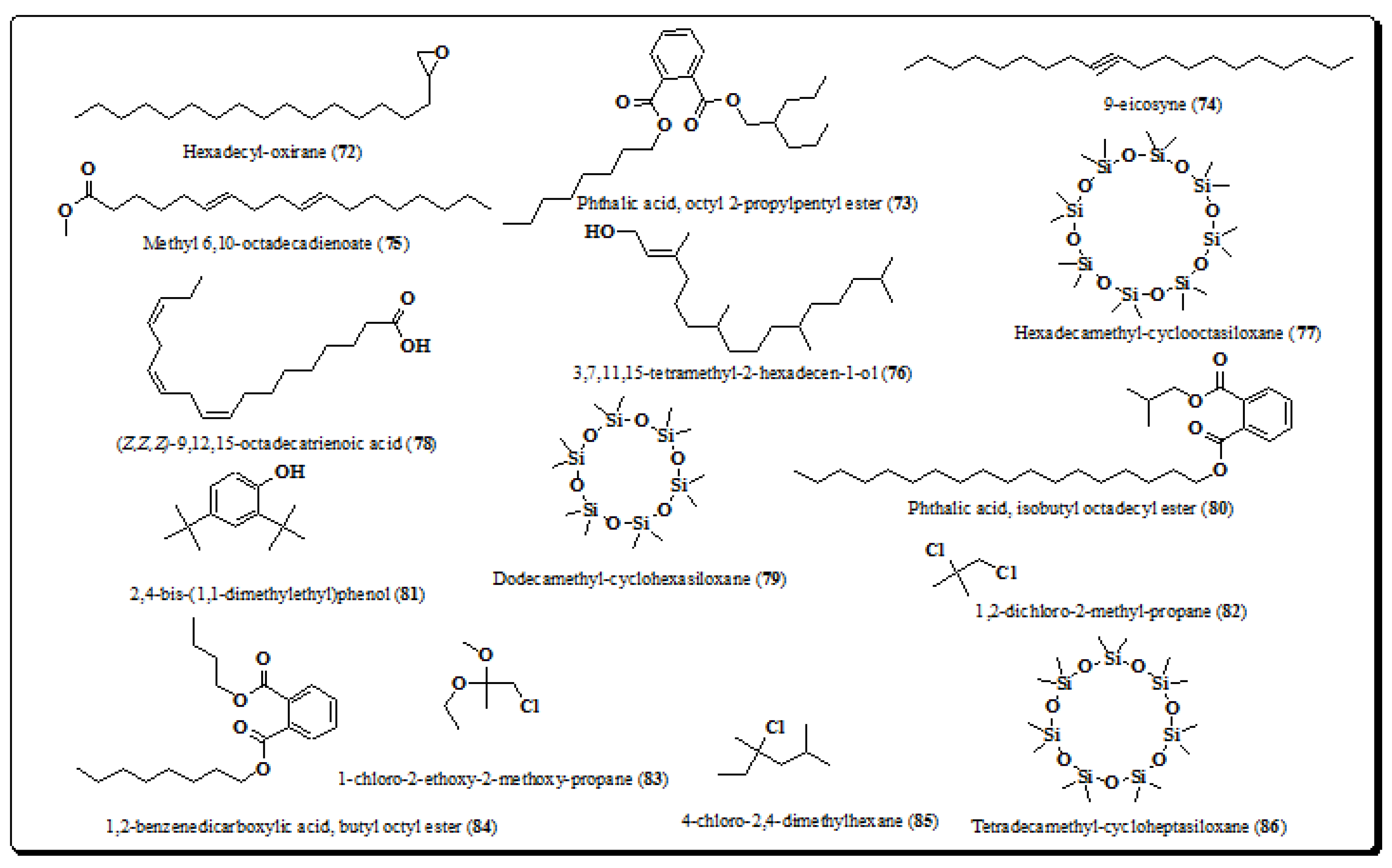
4.8. Miscellaneous
5. Pharmacological Reports
5.1. Anti-inflammatory, Antiarthritic and Analgesic Activities
5.2. Antioxidant Activity
5.3. Antimicrobial Activity
5.4. Wound Healing Activity
5.5. Dental Caries
5.6. Miscellaneous Activities
6. Toxicology
7. Discussion
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miller, J.S. A revision of the new world species of Ehretia (Boraginaceae). Ann. Mo. Bot. Gard. 1989, 76, 1050–1076. [Google Scholar] [CrossRef]
- Joshi, S.G. Medicinal Plants; Oxford and IBH Publishing Co. Private Ltd.: New Delhi, India, 2000; p. 102. [Google Scholar]
- Khare, C.P. Indian Medicinal Plants; An Illustrated Dictionary; Society for New Age Herbals: New Delhi, India, 2007; pp. 231–232. [Google Scholar]
- Kirtikar, K.R.; Basu, B.D. Indian Medicinal Plants; Lalit Mohan Publication: Allahabad, India, 1935; Volume 3, pp. 1680–1681. [Google Scholar]
- Sastri, B.N. The Wealth of India; A Dictionary of Indian Raw Materials and Industrial Products; Council of Scientific and Industrial Research: New Delhi, India, 1952; Volume 3, p. 129. [Google Scholar]
- Torane, R.C.; Ruikar, A.D.; Chandrachood, P.S.; Deshpande, N.R. Study of amino acids and carbohydrates from the leaves of Ehretia Laevis. Asian J. Chem. 2009, 21, 1636–1638. [Google Scholar]
- Li, L.; Yong, P.; Xia, Y.; Li-Jia, X.; Ta-Na, W.; Yong, L.; Ren-Bing, S.; Pei-Gen, X. Chemical constituents and biological activities of plants from the genus Ehretia Linn. Chin. Herb. Med. 2010, 2, 106–111. [Google Scholar]
- Velappan, S.; Thangaraj, P. Phytochemical constituents and antiarthritic activity of Ehretia laevis Roxb. J. Food Biochem. 2014, 38, 433–443. [Google Scholar] [CrossRef]
- Joshi, U.P.; Wagh, R.D. GC-MS analysis of phytochemical compounds present in the bark extracts of Ehretia laevis Roxb. Int. J. Res. Dev. Pharm. Life Sci. 2018, 7, 3150–3154. [Google Scholar] [CrossRef]
- Rangnathrao, T.S.; Shanmugasundar, P. Preliminary phytochemical screening and HPTLC method for qualitative determination of phytochemical compounds in extract of Ehretia laevis Roxb. J. Pharmacogn. Phytochem. 2018, 7, 867–874. [Google Scholar]
- Admuthe, N.B.; Nalwade, A.R. Micropropagation for Ehretia laevis Roxb.: A rare Indian medicinal plant. Int. J. Adv. Sci. Res. 2016, 3, 411–422. [Google Scholar]
- Khobragade, P.; Khobragade, M.; Nandgaonkar, P. Pharmacognostic and phytochemical studies on the leaves of Khanduchakka (Ehretia laevis Roxb.): A folklore plant. J. Indian Med. Sys. 2017, 5, 71–74. [Google Scholar]
- Thakre, R.; Bhutada, S.; Chouragade, B.; Khobragde, P.; Harne, K. Ethnobotanical properties of unexplored plant Khandu chakka (Ehretia laevis Roxb.). Int. J. Ayurveda Pharma. Res. 2016, 4, 68–73. [Google Scholar]
- Anonymous. The Ayurvedic Formulary of India; Ministry of Health and Family Welfare, Government of India: New Delhi, India, 1978; pp. 1–120.
- Padhye, M.D.; Deshmukh, V.K.; Tiwari, V.J. Ethnobotanical study of the Korku tribe of Amravati district, Maharashtra state, India. Int. J. Pharmacogn. 1992, 30, 17–20. [Google Scholar] [CrossRef]
- Patil, S.L.; Patil, D.A. Ethnomedicinal plants of Dhule district of Maharashtra. Nat. Prod. Radiance 2007, 6, 148–151. [Google Scholar]
- Dhenge, S.; Khandare, K. Efficacy of local application of Khandu chakka (Ehretia laevis roxb) Ghrita in Dushtavrana—A case report. Int. J. Ayurveda Integr. Med. 2016, 7, 3726–3731. [Google Scholar]
- Meena, K.L.; Yadav, B.L. Some ethnomedicinal plants used by the Garasia tribe of Siroh, Rajasthan. Indian J. Trad. Knowl. 2011, 10, 354–357. [Google Scholar]
- Bose, D.; Roy, J.G.; Mahapatra, S.D.; Datta, T.; Mahapatra, S.D.; Biswas, H. Medicinal plants used by tribals in Jalpaiguri district, West Bengal, India. J. Med. Plants Stud. 2015, 3, 15–21. [Google Scholar]
- Sharma, J.; Gairola, S.; Gaur, R.D.; Painuli, R.M. The treatment of jaundice with medicinal plants in indigenous communities of the Sub-Himalayan region of Uttarakhand, India. J. Ethnopharmacol. 2012, 143, 262–291. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.; Gairola, S.; Sharma, Y.P.; Gaur, R.D. Ethnomedicinal plants used to treat skin diseases by Tharu community of district Udham Singh Nagar, Uttarakhand, India. J. Ethnopharmacol. 2014, 158, 140–206. [Google Scholar] [CrossRef]
- Liu, R.H. Health benefits of fruits and vegetables are from additive and synergistic combinations of phytochemicals. Am. J. Clin. Nutr. 2003, 78, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Torane, R.C.; Kamble, G.S.; Gadkari, T.V.; Tambe, A.S.; Deshpande, N.R. GC-MS study of nutritious leaves of Ehretia laevis. Int. J. Chem. Res. 2011, 3, 1589–1591. [Google Scholar]
- Jain, A.; Katewa, S.S.; Galav, P.; Nag, A. Some therapeutic uses of biodiversity among the tribes of Rajasthan. Indian J. Tradit. Knowl. 2008, 7, 256–262. [Google Scholar]
- Mishra, N.; Pareek, A. Floristic diversity of angiosperms with special reference to their medicinal properties from Kota district of Rajasthan, India. Int. J. Adv. Res. 2015, 3, 994–1007. [Google Scholar]
- Deshpande, R.; Kamath, A.; Chaturvedi, S.; Mutha, M.M.; Shep, S.; Torane, R. Comparative evaluation of antimicrobial properties of different extracts of ‘Ehretia laevis’ against salivary microflora. Res. J. Pharm. Biol. Chem. Sci. 2014, 5, 489–491. [Google Scholar]
- Tripathi, S.; Ray, S.; Mondal, A.K.; Verma, N.K. Rare ethno medicinal plants of South West Bengal, India with their different medicinal uses: Needs conversation. Int. J. Life Sci. Biotechnol. Pharma Res. 2013, 2, 114–122. [Google Scholar]
- Soni, V.; Prakash, A.; Nema, M. Study on ethno medicinal botany of some plants of Dindori district of Madhya Pradesh, India. Int. J. Pharm. Pharm. Sci. 2012, 8, 1926–1929. [Google Scholar]
- Mohammad, S.; Ghiasi, J.; Chen, A. Bone fracture healing in mechanobiological modelling: A review of principles and methods. Bone Rep. 2017, 6, 87–100. [Google Scholar]
- Das, P.K.; Mondal, A.K. Report to the rare and endangered medicinal plant resources in the dry deciduous forest areas of Paschim Medinipur district, West Bengal. Int. J. Drug Dis. Herbal Res. 2012, 2, 418–429. [Google Scholar]
- Jyothirmai, N.; Nagaraju, B.; Deepika, M.Y.; Kumar, J.N.; Rani, G.S. Evaluation of anti-inflammatory and antibacterial activities of different solvent extracts of Ehretia laevis Roxb. Int. J. Pharm. Sci. Res. 2016, 8, 715–720. [Google Scholar]
- Ali, S.J.; Nasir, Y.J. Flora of Pakistan; National Herbarium, NARC, Department of Botany, University of Karachi: Islamabad, Karachi, Pakistan, 1989; pp. 191–193. [Google Scholar]
- Gaur, R.D.; Sharma, J. Indigenous knowledge on the utilization of medicinal plant diversity in Siwalik region of Garhwal Himalaya, Uttarakhand. J. For. Sci. 2011, 27, 23–31. [Google Scholar]
- Torane, R.C.; Kamble, G.S.; Chandrachood, P.S.; Deshpande, N.R. Preliminary phytochemical screening and nutritional analysis of leaves of Ehretia laevis. J. Pharm. Res. 2010, 3, 1384–1385. [Google Scholar]
- Jagtap, S.D.; Deokule, S.; Pawar, P.K.; Harsulkar, A.M. Traditional ethno medicinal knowledge confined to the Pawra tribe of Satpura Hills, Maharashtra, India. Ethnobot. Leaflets 2009, 13, 98–115. [Google Scholar]
- Chander, M.P.; Kartick, C.; Vijayachari, P. Herbal medicine and healthcare practices among Nicobarese of Nancowry group of Islands, an indigenous tribe of Andaman & Nicobar Islands. Indian J. Med. Res. 2015, 141, 720–744. [Google Scholar]
- Sivasankari, V.; Revathi, P.; Parimela, Z. Evaluation of in vitro antioxidant activity in edible fruits of Ehretia laevis Roxb. Int. J. Pharma Bio Sci. 2013, 4, 847–857. [Google Scholar]
- Dan, S.; Dan, S.S. Triterpenoids of the bark of Ehretia laevis. Fitoterapia 1982, 53, 51–52. [Google Scholar]
- Thapliyal, P.C.; Yadav, S.K. A new naphthoquinone from aerial parts of Ehretia laevis. J. Inst. Chem. 2003, 75, 13–15. [Google Scholar]
- Ali, M. Textbook of Pharmacognosy, 2nd ed.; CBS Publishers: Daryaganj, New Delhi, India, 2007; pp. 490–504. [Google Scholar]
- Torane, R.C.; Kamble, G.S.; Kale, A.A.; Gadkari, T.V.; Deshpande, N.R. Quantification of dioctyl phthalate from Ehretia laevis Roxb by HPTLC. J. Chem. Pharm. Res. 2011, 3, 48–51. [Google Scholar]
- Bringmann, G.; Saeb, W.; Assi, L.A.; Francois, G.; Narayanan, A.S.S.; Peters, K.; Peters, E.M. Betulinic acid: Isolation from Triphyophyllum peltatum and Ancistrocladus heyneanus, antimalarial activity, and crystal structure of the benzyl ester. Planta Med. 1997, 63, 255–257. [Google Scholar] [CrossRef]
- Huguet, A.I.; Recio, M.D.C.; Manez, S.; Giner, R.M.; Rios, J.L. Effect of triterpenoids on the inflammation induced by protein kinase C activators, neuronally acting irritants and other agents. Eur. J. Pharmacol. 2000, 410, 69–81. [Google Scholar] [CrossRef]
- Kinoshita, K.; Akiba, M.; Saitoh, M.; Ye, Y.; Koyama, K.; Takahashi, K.; Kondo, N.; Yuasa, H. Antinociceptive effect of triterpenes from Cacti. Pharm. Biol. 1998, 36, 50–57. [Google Scholar] [CrossRef]
- Chandramu, C.; Manohar, R.D.; Krupadanam, D.G.; Dashavantha, R.V. Isolation, characterization and biological activity of betulinic acid and ursolic acid from Vitex negundo L. Phytother. Res. 2003, 17, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Fulda, S.; Debatin, K.M. Betulinic acid induces apoptosis through a direct effect on mitochondria in neuroectodermal tumors. Med. Pediatr. Oncol. 2000, 35, 616–618. [Google Scholar] [CrossRef]
- Zuco, V.; Supino, R.; Righetti, S.C.; Cleris, L.; Marchesi, E.; Gambacorti-Passerini, C.; Formelli, F. Selective cytotoxicity of betulinic acid on tumor cell lines, but not on normal cells. Cancer Lett. 2002, 175, 17–25. [Google Scholar] [CrossRef]
- Zhao, J.; Li, R.; Pawlak, A.; Henklewska, M.; Sysak, A.; Wen, L.; Yi, J.; Obminska-Mrukowicz, B. Antitumor activity of betulinic acid and betulin in canine cancer cell lines. In Vivo 2018, 32, 1081–1088. [Google Scholar] [CrossRef]
- Krasutsky, P.A. Birch bark research and development. Nat. Prod. Rep. 2006, 23, 919–942. [Google Scholar] [CrossRef] [PubMed]
- Krol, S.K.; Kielbus, M.; Rivero-Müller, A.; Stepulak, A. Comprehensive review on betulin as a potent anticancer agent. Natural bioactive in cancer treatment and prevention. BioMed Res. Int. 2015, 2015, 584189. [Google Scholar] [CrossRef] [PubMed]
- Pavlova, N.I.; Savinova, O.V.; Nikolaeva, S.N.; Boreko, E.I.; Flekhter, O.B. Antiviral activity of betulin, betulinic and betulonic acids against some enveloped and non-enveloped viruses. Fitoterapia 2003, 74, 489–492. [Google Scholar] [CrossRef]
- Bernard, P.; Scior, T.; Didier, B.; Hibert, M.; Berthon, J. Ethnopharmacology and bioinformatic combination for lead discovery: Application to phospholipase A2 inhibitors. Phytochemistry 2001, 58, 865–874. [Google Scholar] [CrossRef]
- Simone, F. Betulinic acid for cancer treatment and prevention. Int. J. Mol. Sci. 2008, 9, 1096–1107. [Google Scholar]
- Dzubak, P.; Hajduch, M.; Vydra, D.; Hustova, A.; Kvasnica, M.; Biedermann, D.; Ova, L.M.; Urban, M.; Sarek, J. Pharmacological activities of natural triterpenoids and their therapeutic implications. Nat. Prod. Res. 2006, 23, 394–411. [Google Scholar]
- Geetha, T.; Varalakshmi, P. Anti-inflammatory activity of lupeol and lupeol linoleate in rats. J. Ethnopharmacol. 2001, 76, 77–80. [Google Scholar] [CrossRef]
- Tsai, F.S.; Lin, L.W.; Wu, C.R. Lupeol and its role in chronic diseases. Adv. Exp. Med. Biol. 2016, 929, 145–175. [Google Scholar]
- Fernandez, M.A.; de las Heras, B.; Garcia, M.D.; Saenz, M.T.; Villar, A. New insights into the mechanism of action of the anti-inflammatory triterpene lupeol. J. Pharm. Pharmacol. 2001, 53, 1533–1539. [Google Scholar] [CrossRef]
- Sudhahar, V.; Kumar, S.A.; Sudharsanm, P.T.; Varalakshmi, P. Protective effect of Lupeol and its ester on cardiac abnormalities in experimental hypercholesterolemia. Vascul. Pharmacol. 2007, 46, 412–418. [Google Scholar] [CrossRef]
- Alam, P.; Al-Yousef, H.M.; Siddiqui, N.A.; Alhowiriny, T.A.; Alqasoumi, S.I.; Amina, M.; Hassan, W.H.B.; Abdelaziz, S.; Abdalla, R.H. Anticancer activity and concurrent analysis of ursolic acid, β-sitosterol and lupeol in three different species of Hibiscus species by validated HPTLC method. Saudi Pharm. J. 2018, 26, 1060–1067. [Google Scholar] [CrossRef]
- Bag, P.; Chattopadhyay, D.; Mukherjee, H.; Ojha, D.; Mandal, N.; Sarkar, M.C.; Chatterjee, T.; Das, G.; Chakraborti, S. Anti-herpes virus activities of bioactive fraction and isolated pure constituents of Mallotus peltatus an ethnomedicine from Andaman Islands. Virol. J. 2012, 9, 98–109. [Google Scholar] [CrossRef]
- Gupta, M.B.; Nath, R.; Gupta, G.P.; Bhargava, K.P. Antiulcer activity of some plant triterpenoids. Indian J. Med. Res. 1981, 73, 649–652. [Google Scholar] [PubMed]
- Hirota, M.; Mori, T.; Yoshida, M.; Iriye, R. Antitumor-promoting and anti-inflammatory activities of triterpenoids and sterols from plants and fungi. Agric. Biol. Chem. 1990, 54, 1073–1075. [Google Scholar]
- Aragao, G.F.; Carneiro, L.M.V.; Junior, A.P.F.; Vieira, L.C.; Bandeira, P.N.; Lemos, T.L.G.; Viana, G.S. A possible mechanism for anxiolytic and antidepressant effects of alpha- and beta-amyrin from Protium heptaphyllum (Aubl.). Pharmacol. Biochem. Behav. 2006, 85, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Johann, S.; Soldi, C.; Lyon, J.P.; Pizzolath, M.G.; Resende, M.A. Antifungal activity of the amyrin derivatives and in vitro inhibition of Candida albicans adhesion to human epithelial cells. Lett. Appl. Microbiol. 2007, 45, 148–153. [Google Scholar] [CrossRef]
- Okoye, N.N.; Ajaghaku, D.L.; Okeke, H.N.; Ilodigwe, E.E.; Nworu, C.S.; Okoye, F.B.C. β-amyrin and α-amyrin acetate isolated from the stem bark of Alstonia boonei display profound anti-inflammatory activity. Pharm. Biol. 2014, 52, 1478–1486. [Google Scholar] [CrossRef] [PubMed]
- Santos, F.A.; Frota, J.T.; Arruda, B.R.; de Melo, T.S.; da Silva, A.A.; de Castro Brito, G.A.; Chaves, M.H.; Rao, V.S. Antihyperglycemic and hypolipidemic effects of α, β-amyrin, a triterpenoid mixture from Protium heptaphyllum in mice. Lipids Health Dis. 2012, 11, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Kathryn, A.B.; da Silva, S.; Paszcuk, A.F.; Passos, G.F.; Silva, S.E.; Bento, A.F.; Meotti, F.C.; Calixto, J.B. Activation of cannabinoid receptors by the pentacyclic triterpene α, β-amyrin inhibits inflammatory and neuropathic persistent pain in mice. Pain 2011, 152, 1872–1887. [Google Scholar]
- Melo, C.M.; Carvalho, K.M.M.B.; Neves, J.C.S.; Morais, T.C.; Rao, V.S.; Santos, F.A.; Brito, G.A.B.; Chaves, M.H. α, β-amyrin, a natural triterpenoid ameliorates L-arginine induced acute pancreatitis in rats. World J. Gastroenterol. 2010, 16, 4272–4280. [Google Scholar] [CrossRef] [PubMed]
- Batovska, D.I.; Todorova, I.T.; Nedelcheva, D.V.; Parushev, S.P.; Atanassov, A.J.; Hvarleva, T.D.; Djakova, G.J.; Bankova, V.S. Preliminary study on biomarkers for the fungal resistance in Vitis vinifera leaves. J. Plant. Physiol. 2008, 165, 791–795. [Google Scholar] [CrossRef] [PubMed]
- Jabeen, K.; Javaid, A.; Ahmad, E.; Athar, M. Antifungal compounds from Melia azederach leaves for management of Ascochyta rabiei, the cause of chickpea blight. Nat. Prod. Res. 2011, 25, 264–276. [Google Scholar] [CrossRef] [PubMed]
- Vitor, C.E.; Figueiredo, C.P.; Hara, D.B.; Bento, A.F.; Mazzuco, T.L.; Calixto, J.B. Therapeutic action and underlying mechanisms of a combination of two pentacyclic triterpenes alpha- and beta-amyrin, in a mouse model of colitis. Br. J. Pharmacol. 2009, 157, 1034–1044. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.B.; Roy, R.; Fink, C.S. β-sitosterol, a plant sterol, induces apoptosis and activates key caspases in MDA-MB-231 human breast cancer cells. Oncol. Rep. 2003, 10, 497–500. [Google Scholar] [CrossRef]
- Kumar, D.; Nepali, K.; Bedi, P.M.S.; Kumar, S.; Malik, F.; Jain, S. 4,6-diaryl Pyrimidones as Constrained Chalcone Analogues: Design, Synthesis and Evaluation as Antiproliferative Agents. Anticancer Agents Med. Chem. 2015, 15, 793–803. [Google Scholar] [CrossRef]
- Kumar, D.; Singh, O.; Nepali, K.; Bedi, P.M.S.; Qayum, A.; Singh, S.; Jain, S.K. Naphthoflavones as anti-proliferative agents: Design, synthesis and biological evaluation. Anticancer Agents Med. Chem. 2016, 16, 881–890. [Google Scholar] [CrossRef]
- Shukla, A.; Kaur, A. A systematic review of traditional uses bioactive phytoconstituents of genus Ehretia. Asian J. Pharm. Clin. Res. 2018, 11, 88–100. [Google Scholar] [CrossRef]
- Kumar, D.; Sharma, P.; Nepali, K.; Mahajan, G.; Mintoo, M.J.; Singh, A.; Singh, G.D.; Mondhe, D.M.; Singh, G.; Jain, S.K.; et al. Antitumour, acute toxicity and molecular modelling studies of 4-(pyridine-4-yl)-6-(thiophen-2- yl)pyrimidin-2(1H)–one against Ehrlich ascites Carcinoma and sarcoma-180. Heliyon 2018, 4, 61. [Google Scholar] [CrossRef]
- Kumar, D.; Malik, F.; Bedi, P.M.S.; Jain, S. 2,4-Diarylpyrano[3,2-c]chromen-5(4H)-ones as Antiproliferative Agents: Design, Synthesis and Biological Evaluation. Chem. Pharm. Bull. 2016, 64, 399–409. [Google Scholar] [CrossRef]
- Kumar, D.; Jain, S.K. A Comprehensive Review of N-Heterocycles as Cytotoxic Agents. Curr. Med. Chem. 2016, 23, 4338–4394. [Google Scholar] [CrossRef]
- Sharma, P.; Sharma, R.; Rao, H.S.; Kumar, D. Phytochemistry and Medicinal Attributes of A. Scholaris: A Review. Int. J. Pharm. Sci. Res. 2015, 6, 505–513. [Google Scholar]
- Kumar, D.; Sharma, P.; Singh, H.; Nepali, K.; Gupta, G.K.; Jain, S.K.; Ntie-Kang, F. The value of pyrans as anticancer scaffolds in medicinal chemistry. RSC Adv. 2017, 7, 36977–36999. [Google Scholar] [CrossRef]
- Kaur, T.; Sharma, P.; Gupta, G.; Ntie-Kang, F.; Kumar, D. Treatment of Tuberculosis by Natural Drugs: A Review. Plant. Arch. 2019, 19, 2168–2176. [Google Scholar]
- Kumar, D.; Singh, G.; Sharma, P.; Qayum, A.; Mahajan, G.; Mintoo, M.J.; Singh, S.K.; Mondhe, D.M.; Bedi, P.M.S.; Jain, S.K.; et al. 4-aryl/heteroaryl-4H-fused pyrans as Anti-proliferative Agents: Design, Synthesis and Biological Evaluation. Anticancer Agents Med. Chem. 2018, 18, 57–73. [Google Scholar] [CrossRef] [PubMed]
- Bekono, B.D.; Ntie-Kang, F.; Onguene, P.A.; Lifongo, L.L.; Sippl, W.; Fester, K.; Owono, L.C.O. The potential of antimalarial compounds derived from African medicinal plants: A review of pharmacological evaluations from 2013 to 2019. Malar. J. 2020, 9, 1–35. [Google Scholar]
- Zhishen, J.; Cheng, T.; Jianming, W. The determination of flavonoid contents on mulberry and their scavenging effects on superoxide radical. Food Chem. 1999, 64, 555–559. [Google Scholar] [CrossRef]
- Hakkinen, S.H.; Karenlampi, S.O.; Heinonen, I.M.; Mykkanen, H.M.; Torronen, A.R. Content of the flavonols quercetin, myricetin, and kaempferol in 25 edible berries. J. Agric. Food Chem. 1999, 47, 2274–2279. [Google Scholar] [CrossRef]
- Stewart, A.J.; Bozonnet, S.; Mullen, W.; Jenkins, G.I.; Lean, M.E.; Crozier, A. Occurrence of flavonols in tomatoes and tomato-based products. J. Agric. Food Chem. 2000, 48, 2663–2669. [Google Scholar] [CrossRef] [PubMed]
- Ferry, D.R.; Smith, A.; Malkhandi, J. Phase I clinical trial of the flavonoid quercetin: Pharmacokinetics and evidence for in vivo tyrosine kinase inhibition. Clin. Cancer Res. 1996, 2, 659–668. [Google Scholar]
- Davis, W.L.; Matthew, S.B. Antioxidants and cancer III: Quercetin. Altern. Med. Rev. 2000, 5, 196–208. [Google Scholar]
- Zerin, T.; Kim, Y.S.; Hong, S.Y.; Song, H.Y. Quercetin reduces oxidative damage induced by paraquat via modulating expression of antioxidant genes in A549 cells. J. Appl. Toxicol. 2013, 33, 1460–1467. [Google Scholar] [CrossRef]
- Lesjak, M.; Beara, I.; Simin, N.; Pintac, D.; Majkic, T.; Bekvalac, K.; Orcic, D.; Mimica-Dukic, N. Antioxidant and anti-inflammatory activities of quercetin and its derivatives. J. Funct. Foods 2018, 40, 68–75. [Google Scholar] [CrossRef]
- Boots, A.W.; Haenen, G.; Bast, A. A health effect of quercetin: From antioxidant to nutraceutical. Eur. J. Pharmacol. 2008, 585, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Hu, M.J.; Wang, Y.Q.; Cui, Y.L. Antioxidant activities of quercetin and its complexes for medicinal application. Molecules 2019, 24, 1123. [Google Scholar] [CrossRef]
- Jain, A.K.; Thanki, K.; Jain, S. Co-encapsulation of tamoxifen and quercetin in polymeric nanoparticles: Implications on oral bioavailability, antitumor efficacy, and drug induced toxicity. Mol. Pharm. 2013, 10, 3459–3474. [Google Scholar] [CrossRef]
- Miean, K.H.; Mohamed, S. Flavonoid (myricetin, quercetin, kaempferol, luteolin and apigenin) content of edible tropical plants. J. Agric. Food Chem. 2001, 49, 3106–3112. [Google Scholar] [CrossRef] [PubMed]
- Somerset, S.M.; Johannot, L. Dietary flavonoid source in Australian adults. Nutr. Cancer 2008, 60, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.Y.; Chen, Y.C. A review of dietary flavonoid, Kaempferol on human health and cancer prevention. Food Chem. 2013, 138, 2099–2107. [Google Scholar] [CrossRef]
- Suchal, K.; Malik, S.; Khan, S.I.; Malhotra, R.K.; Goyal, S.N.; Bhatia, J.; Ojha, S.; Arya, D.S. Molecular pathways involved in the amelioration of myocardial injury in diabetic rats by kaempferol. Int. J. Mol. Sci. 2017, 18, 1001. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Zhang, S.; You, S.; Liu, T.; Xu, F.; Ji, T.; Gu, Z. Hepatoprotective effects of nicotiflorin from nymphaea candida against concanavalin α-induced and D-galactosamine-induced liver injury in mice. Int. J. Mol. Sci. 2017, 18, 587. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, A.M.; Maria-Ferreira, D.; Lin, F.T.D.; Kimura, A.; de Santana-Filho, A.P.; de P. Werner, M.F.; Iacomini, M.; Sassaki, G.L.; Cipriani, T.R.; de Souza, L.M. Phytochemical analysis and anti-inflammatory evaluation of compounds from an aqueous extract of Croton cajucara benth. J. Pharm. Biomed. Anal. 2017, 145, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Arif, H.; Sohail, A.; Farhan, M.; Rehman, A.A.; Ahmad, A.; Hadi, S.M. Flavonoids induced redox cycling of copper ions leads to generation of reactive oxygen species: A potential role in cancer chemoprevention. Int. J. Biol. Macromol. 2018, 106, 569–578. [Google Scholar] [CrossRef]
- Wang, L.; Tu, Y.C.; Lian, T.W.; Hung, J.T.; Yen, J.H.; Wu, M.J. Distinctive antioxidant and anti-inflammatory effects of flavonols. J. Agric. Food Chem. 2006, 54, 9798–9804. [Google Scholar] [CrossRef]
- Wu, Y.; Sun, J.; George, J.; Ye, H.; Cui, Z.; Li, Z. Study of neuroprotective function of Ginkgo biloba extract derived-flavonoid monomers using a three-dimensional stem cell-derived neural model. Biotechnol. Prog. 2016, 32, 735–744. [Google Scholar] [CrossRef]
- Li, F.; Zhang, B.; Chen, G.; Fu, X. The novel contributors of antidiabetic potential in mulberry polyphenols revealed by UHPLC-HR-ESI-TOF-MS/MS. Food Res. Int. 2017, 100, 873–884. [Google Scholar] [CrossRef]
- Calderon-Montano, J.M.; Burgos-Moron, E.; Perez-Guerrero, C.; Lopez-Lazaro, M. A review on the dietary flavonoid kaempferol. Mini Rev. Med. Chem. 2011, 11, 298. [Google Scholar] [CrossRef] [PubMed]
- Pei, J.; Chen, A.; Zhao, L.; Cao, F.; Ding, G.; Xiao, W. One pot synthesis of hyperoside by a three-enzyme cascade using a UDP galactose regeneration system. J. Agric. Food Chem. 2017, 65, 6042–6048. [Google Scholar] [CrossRef]
- Tang, X.L.; Liu, J.X.; Dong, W.; Li, P.; Li, L.; Hou, J.C.; Zheng, Y.Q.; Lin, C.R.; Ren, J.G. Protective effect of kaempferol on LPS plus ATP induced inflammatory response in cardiac fibroblasts. Inflammation 2015, 38, 94–101. [Google Scholar] [CrossRef]
- Harborne, J.B.; Williams, C.A. Advances in flavonoid research since 1992. Phytochemistry 2000, 55, 481–504. [Google Scholar] [CrossRef]
- Batra, P.; Sharma, A.K. Anticancer potential of flavonoids: Recent trends and future perspectives. 3 Biotech 2013, 3, 439–459. [Google Scholar] [CrossRef]
- Knekt, P.; Jarvinen, R.; Seppanen, R.; Hellovaar, M.; Teppo, L.; Pukkala, E.; Aromaa, A. Dietary flavonoids and the risk of lung cancer and other malignant neoplasms. Am. J. Epidemiol. 1997, 146, 223–230. [Google Scholar] [CrossRef]
- Birt, D.F.; Hendrich, S.; Wang, W. Dietary agents in cancer prevention: Flavonoids and isoflavonoids. Pharmacol. Ther. 2001, 90, 157–177. [Google Scholar] [CrossRef]
- Neuhouser, M.L. Dietary flavonoids and cancer risk: Evidence from human population studies. Nutr. Cancer 2004, 50, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.F.; Yang, W.E.; Chang, H.R.; Chu, S.C.; Hsieh, Y.S. Luteolin induces apoptosis in oral squamous cancer cells. J. Dent. Res. 2008, 87, 401–406. [Google Scholar] [CrossRef]
- Ju, W.; Wang, X.; Shi, H.; Chen, W.; Belinsky, S.A.; Lin, Y. A critical role of luteolin induced reactive oxygen species in blockage of tumor necrosis factor activated nuclear factor kappa B pathway and sensitization of apoptosis in lung cancer cells. Mol. Pharmacol. 2007, 71, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhao, X.H.; Wang, Z.J. Flavones and flavonols exert cytotoxic effects on a human oesophageal adenocarcinoma cell line (OE33) by causing G2/M arrest and inducing apoptosis. Food Chem. Toxicol. 2008, 46, 2042–2053. [Google Scholar] [CrossRef]
- Chiu, F.L.; Lin, J.K. Down regulation of androgen receptor expression by luteolin causes inhibition of cell proliferation and induction of apoptosis in human prostate cancer cells and xenografts. Prostate 2008, 68, 61–71. [Google Scholar] [CrossRef]
- Lin, Y.; Shi, R.; Wang, X.; Shen, H.M. Luteolin, a flavonoid with potentials for cancer prevention and therapy. Curr. Cancer Drug Targets 2008, 8, 634–646. [Google Scholar] [CrossRef]
- Harborne, J.B.; Baxter, H. The Handbook of Natural Flavonoids; John Wiley and Sons: Chichester, UK, 1999; Volume 1, p. 12. [Google Scholar]
- Hostetler, G.L.; Ralston, R.A.; Schwartz, S.J. Flavones: Food sources, bioavailability, metabolism, and bioactivity. Adv. Nutr. 2017, 8, 423–435. [Google Scholar] [CrossRef]
- Falcone-Ferreyra, M.L.; Rius, S.P.; Casati, P. Flavonoids: Biosynthesis, biological functions, and biotechnological applications. Front. Plant. Sci. 2012, 3, 222. [Google Scholar] [CrossRef]
- Kabera, J.N.; Semana, E.; Mussa, A.R.; He, X. Plant secondary metabolites: Biosynthesis, classification, function and pharmacological properties. J. Pharm. Pharmacol. 2014, 2, 377–392. [Google Scholar]
- Seo, H.S.; Ku, J.M.; Choi, H.S.; Woo, J.K.; Jang, B.H.; Shin, Y.C.; Ko, S.G. Induction of caspase-dependent apoptosis by apigenin by inhibiting STAT3 signalling in HER2-overexpressing MDA-MB-453 breast cancer cells. Anticancer Res. 2014, 34, 2869–2882. [Google Scholar]
- Salehi, B.; Venditti, A.; Sharifi-Rad, M.; Kregiel, D.; Sharifi-Rad, J.; Durazzo, A.; Lucarini, M.; Santini, A.; Souto, E.B.; Novellino, E.; et al. The therapeutic potential of apigenin. Int. J. Mol. Sci. 2019, 20, 1305. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Zhao, D.; Qu, R.; Fu, Q.; Ma, S. The effects of apigenin on lipopolysaccharide induced depressive like behavior in mice. Neurosci. Lett. 2015, 594, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Pamunuwa, G.; Karunaratne, D.N.; Waisundara, V.Y. Antidiabetic properties, bioactive constituents, and other therapeutic effects of Scoparia dulcis. Evid. Based Complement. Alternat. Med. 2016, 16, 824–830. [Google Scholar]
- Tang, R.; Chen, K.; Cosentino, M.; Lee, K.H. Apigenin-7-O-β-D-glucopyranoside, an anti-HIV principle from Kummerowia Striata. Bioorg. Med. Chem. Lett. 1994, 4, 455–458. [Google Scholar] [CrossRef]
- Ali, F.; Naz, F.; Jyoti, S.; Siddique, Y.H. Health functionality of apigenin: A review. Int. J. Food Prop. 2017, 20, 1197–1238. [Google Scholar] [CrossRef]
- Kaur, R.; Sharma, P.; Gupta, G.K.; Ntie-Kang, F.; Kumar, D. Structure activity relationship and mechanistic insights for anti-HIV natural products. Molecules 2020, 25, 2070. [Google Scholar] [CrossRef] [PubMed]
- Erlund, I. Review of the flavonoids quercetin, hesperetin, and naringenin: Dietary sources, bioactivities, bioavailability, and epidemiology. Nutr. Res. 2004, 24, 851–874. [Google Scholar] [CrossRef]
- Rani, N.; Bharti, S.; Krishnamurthy, B.; Bhatia, J.; Sharma, C.; Kamal, M.A.; Ojha, S.; Arya, D.S. Pharmacological properties and therapeutic potential of naringenin: A citrus flavonoid of pharmaceutical promise. Curr. Pharm. Des. 2016, 22, 1–19. [Google Scholar] [CrossRef]
- Jadeja, R.N.; Devkar, R.V. Polyphenols and flavonoids in controlling non-alcoholic steatohepatitis. In Polyphenols in Human Health and Disease; Academic Press: San Diego, CA, USA, 2014; Volume 1, pp. 615–623. [Google Scholar]
- Mbaveng, A.T.; Zhao, Q.; Kuete, V. Harmful and protective effects of phenolic compounds from African medicinal plants. In Toxicological Survey of African Medicinal Plants, 1st ed.; Kuete, V., Ed.; Elsevier: New York, NY, USA, 2014; Volume 1, Chapter 20; pp. 577–609. [Google Scholar]
- Pinho-Ribeiro, F.A.; Zarpelon, A.C.; Fattori, V.; Manchope, M.F.; Mizokami, S.S.; Casagrande, R.; Verri, W.A. Naringenin reduces inflammatory pain in mice. Neuropharmacology 2016, 105, 508–519. [Google Scholar] [CrossRef] [PubMed]
- Zobeiri, M.; Belwal, T.; Parvizi, F.; Naseri, R.; Farzaei, M.H.; Nabavi, S.F.; Sureda, A.; Nabavi, S.M. Naringenin and its nano-formulations for fatty liver: Cellular modes of action and clinical perspective. Curr. Pharm. Biotechnol. 2018, 19, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Salehi, B.; Fokou, P.V.T.; Sharifi-Rad, M.; Zucca, P.; Pezzani, R.; Martins, N.; Sharifi-Rad, J. The therapeutic potential of naringenin: A review of clinical trials. Pharmaceuticals 2019, 12, 11. [Google Scholar] [CrossRef]
- Wang, N.; Li, D.; Lu, N.H.; Yi, L.; Huang, X.W.; Gao, Z.H. Peroxynitrite and haemoglobin mediated nitrative/oxidative modification of human plasma protein: Effects of some flavonoids. J. Asian Nat. Prod. Res. 2010, 12, 257–264. [Google Scholar] [CrossRef]
- Arul, D.; Subramanian, P. Naringenin (citrus flavanone) induces growth inhibition, cell cycle arrest and apoptosis in human hepatocellular carcinoma cells. Pathol. Oncol. Res. 2013, 19, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Chandrika, B.B.; Steephan, M.; Kumar, T.R.S.; Sabu, A.; Haridas, M. Hesperetin and naringenin sensitize HER2 positive cancer cells to death by serving as HER2 tyrosine kinase inhibitors. Life Sci. 2016, 160, 47–56. [Google Scholar] [CrossRef]
- Lim, W.; Park, S.; Bazer, F.W.; Song, G. Naringenin induced apoptotic cell death in prostate cancer cells is mediated via the PI3K/AKT and MAPK signalling pathways. J. Cell. Biochem. 2017, 118, 1118–1131. [Google Scholar] [CrossRef]
- Hernandez-Aquino, E.; Muriel, P. Beneficial effects of naringenin in liver diseases: Molecular mechanisms. World J. Gastroenterol. 2018, 24, 1679–1707. [Google Scholar] [CrossRef]
- Kapoor, R.; Rizvi, F.; Kakkar, P. Naringenin prevents high glucose induced mitochondria mediated apoptosis involving AIF, Endo-G and caspases. Apoptosis 2013, 18, 9–27. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, R.; Kakkar, P. Naringenin accords hepato protection from streptozotocin induced diabetes in vivo by modulating mitochondrial dysfunction and apoptotic signalling cascade. Toxicol. Rep. 2014, 1, 569–581. [Google Scholar] [CrossRef]
- Kreft, S.; Knapp, M.; Kreft, I. Extraction of rutin from buckwheat (Fagopyrum esculentum Moench) seeds and determination by capillary electrophoresis. J. Agric. Food Chem. 1999, 47, 4649–4652. [Google Scholar] [CrossRef] [PubMed]
- Javed, H.; Khan, M.M.; Ahmad, A.; Vaibhav, K.; Ahmad, M.E.; Khan, A.; Ashafaq, M.; Islam, F.; Siddiqui, M.S.; Safhi, M.M.; et al. Rutin prevents cognitive impairments by ameliorating oxidative stress and neuro inflammation in rat model of sporadic dementia of Alzheimer type. Neuroscience 2012, 17, 340–352. [Google Scholar] [CrossRef] [PubMed]
- Trumbeckaite, S.; Bernatoniene, J.; Majiene, D.; Jakstas, V.; Savickas, A.; Toleikis, A. The effect of flavonoids on rat heart mitochondrial function. Biomed. Pharmacother. 2006, 60, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Al-Dhabi, N.A.; Arasu, M.V.; Park, C.H.; Park, S.U. An up-to-date review of rutin and its biological and pharmacological activities. EXCLI J. 2015, 14, 59–63. [Google Scholar] [PubMed]
- Enogieru, A.B.; Haylett, W.; Hiss, D.C.; Bardien, S.; Ekpo, O. Rutin as potent antioxidants: Implications for neurodegenerative disorders. Oxid. Med. Cell. Longev. 2018, 4, 1–17. [Google Scholar] [CrossRef] [PubMed]
- La Casa, C.; Villegas, I.; De La Lastra, C.A.; Motilva, V.; Martin, C.M.J. Evidence for protective and antioxidant properties of rutin, a natural flavone, against ethanol induced gastric lesions. J. Ethnopharmacol. 2000, 71, 45–53. [Google Scholar] [CrossRef]
- Perk, A.A.; Mytsyk, I.S.; Gerçek, Y.C.; Boztas, K.; Yazgan, M.; Fayyaz, S.; Farooq, A.A. Rutin mediated targeting of signalling machinery in cancer cells. Cancer Cell Int. 2014, 14, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Mellou, F.; Loutrari, H.; Stamatis, H.; Roussos, C.; Kolisis, F.N. Enzymatic esterification of flavonoids with unsaturated fatty acids: Effect of the novel esters on vascular endothelial growth factor release from K562 cells. Process. Biochem. 2006, 41, 2029–3204. [Google Scholar] [CrossRef]
- Schwedhelm, E.; Maas, R.; Troost, R.; Boger, R.H. Clinical pharmacokinetics of antioxidants and their impact on systemic oxidative stress. Clin. Pharmacokinet. 2003, 42, 437–459. [Google Scholar] [CrossRef]
- Ganeshpurkar, A.; Saluja, A.K. The pharmacological potential of Rutin. Saudi Pharm. J. 2017, 25, 149–164. [Google Scholar] [CrossRef]
- Kerry, N.L.; Abbey, M. Red wine and fractionated phenolic compounds prepared from red wine inhibit low density lipoprotein oxidation in vitro. Atherosclerosis 1997, 135, 93–102. [Google Scholar] [CrossRef]
- Erlejman, A.G.; Verstraeten, S.V.; Fraga, C.G.; Oteiza, P.I. The interaction of flavonoids with membranes: Potential determinant of flavonoid antioxidant effects. Free Radic. Res. 2014, 38, 1311–1320. [Google Scholar] [CrossRef] [PubMed]
- Tapas, A.R.; Sakarkar, D.M.; Kakde, R.B. Flavonoids as nutraceuticals: A review. Trop. J. Pharm. Res. 2008, 7, 1089–1099. [Google Scholar] [CrossRef]
- Middleton, E.; Kandaswami, C.; Theoharides, T.C. The effects of plant flavonoids on mammalian cells: Implications for inflammation, heart disease and cancer. Pharmacol. Rev. 2000, 52, 673–751. [Google Scholar] [PubMed]
- Rocha, L.D.; Monterio, M.C.; Teodoro, A.J. Anticancer properties of hydroxycinnamic acids: A review. J. Cancer Res. Clin. Oncol. 2012, 1, 109–121. [Google Scholar] [CrossRef]
- Badhani, B.; Sharma, N.; Kakkar, R. Gallic acid: A versatile antioxidant with promising therapeutic and industrial applications. RSC Adv. 2015, 5, 27540–27557. [Google Scholar] [CrossRef]
- Heleno, S.A.; Martins, A.; Queiroz, M.J.; Ferreira, I.C. Bioactivity of phenolic acids: Metabolites versus parent compounds: A review. Food Chem. 2015, 173, 501–513. [Google Scholar] [CrossRef]
- Yokozawa, T.; Chen, C.P.; Dong, E.; Tanaka, T.; Nonaka, G.I.; Nishioka, I. Study on the inhibitory effect of tannins and flavonoids against DPPH radical. J. Agric. Food Chem. 1998, 56, 213–222. [Google Scholar]
- Akinmoladun, A.C.; Ibukun, E.O.; Afor, E.; Obuotor, E.M.; Farombi, E.O. Phytochemical constituent and antioxidant activity of extract from the leaves of Ocimum gratissimum. Sci. Res. Ess. 2007, 2, 163–166. [Google Scholar]
- Kumar, N.; Goel, N. Phenolic acids: Natural versatile molecules with promising therapeutic applications. Appl. Biotechnol. Rep. 2019, 24, e00370. [Google Scholar] [CrossRef]
- Del-Rio, D.; Costa, L.G.; Lean, M.E.J.; Crozier, A. Polyphenols and health. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Anand, K.K.; Singh, B.; Saxena, A.K.; Chandan, B.K.; Gupta, V.N.; Bhardwaj, V. 3,4,5-Trihydroxy benzoic acid (Gallic Acid) the hepatoprotective principle in the fruits of Terminalia belerica bioassay guided activity. Pharmacol. Res. 1997, 36, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, S.; Chaar, J.; Yano, T. Chemotherapeutic potential of two gallic acid derivative compounds from leaves of Casearia sylvestris (Flacourtiaceae). Eur. J. Pharmacol. 2009, 608, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Chanwitheesuk, A.; Teerawutgulrag, A.; Kilburn, J.D.; Rakariyatham, N. Antimicrobial gallic acid from Caesalpinia mimosoides Lamk. Food Chem. 2007, 100, 1044–1048. [Google Scholar] [CrossRef]
- Kahkeshani, N.; Farzaei, F.; Fotouhi, M.; Alavi, S.S.H.; Bahramsoltani, R.; Naseri, R.; Momtaz, S.; Abbasabadi, Z.; Rahimi, R.; Farzaei, M.H.; et al. Pharmacological effects of gallic acid in health and diseases: A mechanistic review. Iran. J. Basic Med. Sci. 2019, 22, 225–237. [Google Scholar]
- Park, J.; Han, W.; Park, J.; Choi, S.; Choi, J. Changes in hepatic drug metabolizing enzymes and lipid peroxidation by methanol extract and major compound of Orostachys japonicus. J. Ethnopharmacol. 2005, 102, 313–318. [Google Scholar] [CrossRef]
- Choubey, S.; Goyal, S.; Varughese, L.R.; Kumar, V.; Sharma, A.K.; Beniwal, V. Probing Gallic Acid for Its Broad-Spectrum Applications. Mini Rev. Med. Chem. 2018, 18, 1283–1293. [Google Scholar] [CrossRef]
- Chung, K.T.; Wong, T.Y.; Wei, C.; Huang, Y.W.; Lin, Y. Tannins and human health: A review. Crit. Rev. Food Sci. Nutr. 1998, 38, 421–464. [Google Scholar] [CrossRef]
- Hussein, I.A.S.; Mona-Mansour, M.S.M. Polyphenols: Properties, occurrence, content in food and potential effects. J. Environ. Sci. Eng. 2017, 6, 232–261. [Google Scholar]
- Tillman, P.B. Determination of nutrient values for commercial amino acids. J. Appl. Poult. Res. 2019, 28, 526–530. [Google Scholar] [CrossRef]
- WHO; FAO; UNO. Protein and amino acid requirements in human nutrition, report of a joint WHO/FAO/UNU expert consultation. In WHO Technical Report Series No; WHO: Geneva, Switzerland, 2007; p. 935. Available online: https://apps.who.int/iris/handle/10665/43411 (accessed on 1 May 2021).
- Arunachalam, K.; Parimelazhagan, T. Evaluation of nutritional composition and antioxidant properties of underutilized Ficus talboti King fruit for nutraceuticals and food supplements. J. Food Sci. Technol. 2014, 51, 1260–1268. [Google Scholar] [CrossRef]
- Block, R.J.; Drrum, E.L.; Zweig, G. A Manual of Paper Chromatography and Electrophoresis, 2nd ed.; Academic Press: New York, NY, USA, 1958; p. 494. [Google Scholar]
- Patridge, S.M. Aniline hydrogen phthalate as a spraying reagent for chromatography of sugars. Nature 1949, 164, 443. [Google Scholar] [CrossRef]
- The Indian Pharmacopoeia; Government of India, Ministry of Health and Family Welfare, Addendum 2000; The Controller of Publications: Delhi, India, 1996; Volume 4, pp. 495–499.
- United States Pharmacopoeia. The National Formulary; The United States Pharmacopoeial Convention, Inc.: Rockville, MD, USA, 2000; p. 20852. [Google Scholar]
- Yen, G.C.; Chen, H.Y. Relationship between antimutagenic activity and major components of various teas. Mutagenesis 1996, 11, 37–41. [Google Scholar] [CrossRef]
- Carr, A.C.; Frei, B. Toward a new recommended dietary allowance for vitamin C based on antioxidant and health effects in humans. Am. J. Clin. Nutr. 1999, 69, 1086–1107. [Google Scholar] [CrossRef] [PubMed]
- Padyatty, S.J.; Katz, A.; Wang, Y.; Eck, P.; Kwon, O.; Lee, J.H.; Chen, S.; Corpe, C.; Dutta, A.; Dutta, S.K.; et al. Vitamin C as an antioxidant: Evaluation of its role in disease prevention. J. Am. Coll. Nutr. 2003, 22, 18–35. [Google Scholar] [CrossRef] [PubMed]
- Tada, A.; Miura, H. The relationship between vitamin C and periodontal disease: A systematic review. Int. J. Environ. Res. 2019, 16, 2472. [Google Scholar] [CrossRef] [PubMed]
- FAO. Food and Agriculture; Statistic Series no. 94; Food and Agriculture Organisation: Rome, Italy, 1990. [Google Scholar]
- Malik, A.H.; Khuroo, A.A.; Dar, G.H.; Khan, Z.S. The woody flora of Jammu and Kashmir State, India, An updated checklist. J. Econ. Taxon. Bot. 2010, 32, 274–292. [Google Scholar]
- Mukherjee, P.K. Quality Control and Evaluation of Herbal Drug, 1st ed.; Business Horizon Publication: New Delhi, India, 2002; pp. 186–193. [Google Scholar]
- Al-Owaisi, M.; Al-Hadiwi, N.; Khan, S.A. GC-MS analysis, determination of total phenolics, flavonoid content and free radical scavenging activities of various crude extracts of Moringa peregrina (Forssk.) Fiori leaves. Asian Pac. J. Trop. Biomed. 2014, 4, 964–970. [Google Scholar] [CrossRef]
- Abdel-Aal, E.I.; Haroon, A.M.; Mofeed, J. Successive solvent extraction and GC-MS analysis for the evaluation of the phytochemical constituents of the filamentous green alga Spirogyra longata. Egypt. J. Aquat. Res. 2015, 41, 233–246. [Google Scholar] [CrossRef]
- Gupta, K.K.; Kumar, A. Leaf chemistry and food selection by common Langurs (Presbytis entellus) in Rajaji National Park, Uttar Pradesh, India. Int. J. Primatol. 1994, 15, 75–93. [Google Scholar] [CrossRef]
- Reddy, K.N.; Pattanaik, C.; Reddy, C.S.; Raju, V.S. Traditional knowledge of wild food plants in Andhra Pradesh. Indian J. Tradit. Knowl. 2007, 6, 223–229. [Google Scholar]
- Yadav, R.K.; Mishra, A. Aromatic wild-type plants at terai region of Uttar Pradesh with traditional knowledge. Ann. Phytomed. 2015, 4, 106–111. [Google Scholar]
- Dutta, B.K.; Dutta, P.K. Potential of ethnobotanical studies in North East India: An overview. Indian J. Tradit. Knowl. 2005, 4, 7–14. [Google Scholar]
- Abad, M.J.; Bermejo, P.; Carretero, E.; Martinez-Acitores, C.; Noguera, B.; Villar, A. Antiinflammatory activity of some medicinal plant extracts from Venezuela. J. Ethnopharmacol. 1996, 55, 63–68. [Google Scholar] [CrossRef]
- Szeto, Y.T.; Tomlinson, B.; Benzie, I.F. Total antioxidant and ascorbic acid content of fresh fruits and vegetables: Implications for dietary planning and food preservation. Br. J. Nutr. 2002, 87, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.C.; Lin, C.C. Anti-inflammatory effects of Taiwan folk medicine “Teng-Khaia-U” on carrageenan and adjuvant induced paw edema in rats. J. Ethnopharmacol. 1999, 64, 85–89. [Google Scholar] [CrossRef]
- Nielen, M.M.; Schaardenburg, D.V.; Reesink, H.W.; Twisk, J.W.R.; Van De Stadt, R.J.; Vander Horst, B.I.E.; De Koning, M.H.; Habibuw, M.R.; Dijkman, B.A. Simultaneous development of acute phase response and auto-antibodies in preclinical rheumatoid arthritis. Ann. Rheum. Dis. 2006, 65, 535–537. [Google Scholar] [CrossRef] [PubMed]
- Kamalutheen, M.; Gopalakrishnan, S.; Ismail, T.S. Anti-inflammatory and antiarthritic activities of Merremia tridentate (L.). J. Chem. 2009, 6, 943–948. [Google Scholar]
- Patil, K.S.; Suryavanshi, J. Effect of Celastrus paniculatus wild seed on adjuvant induced arthritis in rats. Pharmacogn. Mag. 2007, 3, 177–181. [Google Scholar]
- Hu, F.; Hepburn, H.R.; Li, Y.; Chen, M.; Radloff, S.E.; Daya, S. Effect of ethanol and water extracts of Propolis (bee glue) on acute inflammatory animal models. J. Ethnopharmacol. 2005, 10, 276–283. [Google Scholar] [CrossRef]
- Srinivasan, R.; Chandrasekar, M.J.N.; Nanjan, M.J.; Suresh, B. Antioxidant activity of Caesalpinia digyna root. J. Ethnopharmacol. 2007, 113, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Kumaraswamy, M.V.; Satish, S. Antioxidant and anti-lipoxygenase activity of Thespesia lampas Dalz and Gibs. Adv. Biol. Res. 2008, 2, 56–59. [Google Scholar]
- Badami, S.; Gupta, M.K.; Suresh, B. Antioxidant activity of ethanolic extract of Striga orobanchioides. J. Ethnopharmacol. 2003, 85, 227–230. [Google Scholar] [CrossRef]
- Pisoschi, A.M.; Negulescu, G.P. Methods for total antioxidant activity determination: A review. Anal. Biochem. 2011, 4, 1–10. [Google Scholar] [CrossRef]
- Sultana, B.; Anwar, F.; Ashraf, M. Effect of extraction solvent/technique on the antioxidant activity of selected medicinal plant extracts. Molecules 2009, 14, 2167–2180. [Google Scholar] [CrossRef]
- Saad, R.; Asmani, F.; Saad, M.; Hussain, M.; Khan, J.; Kaleemullah, M.; Othman, N.B.; Tofigh, A.; Yusuf, E. A new approach for predicting antioxidant property of herbal extracts. Int. J. Pharmacogn. Phytochem. Res. 2015, 7, 166–174. [Google Scholar]
- Torane, R.C.; Kamble, G.S.; Khatiwor, E.; Ghayal, N.A.; Deshpande, N.R. Antioxidant capacity of leaves and stem of Ehretia laevis. Int. J. Pharm. Pharm. Sci. 2011, 3, 149–151. [Google Scholar]
- Florence, T.M. The role of free radicals in disease. Aust. N. Z. J. Ophthalmol. 1995, 23, 3–7. [Google Scholar] [CrossRef]
- Cook, N.C.; Samman, S. Flavonoid chemistry, metabolism, cardio protective effects and dietary sources. J. Nutr. Biochem. 1996, 7, 66–76. [Google Scholar] [CrossRef]
- Kumpulainen, J.T.; Salonen, J.T. Natural Antioxidants and Anticarcinogens in Nutrition, Health and Disease. R. Soc. Chem. 1999, 5, 178–187. [Google Scholar]
- Adibhatla, R.M.; Hatcher, J.F. Altered lipid metabolism in brain injury and disorders. Subcell. Biochem. 2008, 49, 241–268. [Google Scholar]
- Valsaraj, R.; Pushpangadan, P.; Smitt, U.W.; Adsersen, A.; Nyman, U. Antimicrobial screening of selected medicinal plants from India. J. Ethnopharmacol. 1997, 58, 75–83. [Google Scholar] [CrossRef]
- Aqil, F.; Ahmad, I. Broad-spectrum antibacterial and antifungal properties of certain traditionally used Indian medicinal plants. World J. Microbiol. Biotechnol. 2003, 19, 653–657. [Google Scholar] [CrossRef]
- Jan, S.; Hamayun, M.; Ahmad, N.; Khan, A.L.; Iqbal, A.; Rehman, K.U.; Nawaz, Y.; Lee, I. Antibacterial potential of plants traditionally used for curing diarrhea in Khyber Pakhtunkhwa, Pakistan. J. Med. Plant. Res. 2012, 6, 4039–4047. [Google Scholar]
- Mutha, M.; Deshpande, R.R.; Patil, V.; Shep, S.; Deshpande, N.R.; Torne, R. Comparative evaluation of antibacterial properties of different extracts of Mimusops Elengi (Bakul) and Ehretia laevis (Ajaan) against salivary microflora. Asian J. Pharm. Clin. Res. 2015, 8, 217–219. [Google Scholar]
- Jadhav, M.V.; Deshpande, R.R.; Dadpe, M.; Mahajan, P.; Kakade, P.; Kamble, G.; Deshpande, N.R. Screening of antimicrobial activity of active compounds of Embelia basal, chlorhexidine and amoxicillin against salivary microflora of mixed dentition age group. Res. J. Pharm. Biol. Chem. 2012, 3, 1334–1339. [Google Scholar]
- Murarkar, K.; Bande, D.; Chandak, A. Antimicrobial activity and minimum inhibitory concentration of Ehretia laevis leaves extracts against different microorganisms. World J. Pharm. Res. 2018, 7, 691–697. [Google Scholar]
- Bibi, Y.; Naeem, J.; Zahara, K.; Arshad, M.; Qayyum, A. In vitro antimicrobial assessment of selected plant extracts from Pakistan. Iran. J. Sci. Technol. 2018, 42, 267–272. [Google Scholar] [CrossRef]
- Gupta, N.; Gupta, S.K.; Shukla, V.K.; Singh, S.P.J. An Indian community based epidemiological study of wounds. Wound Care 2004, 13, 323–325. [Google Scholar] [CrossRef]
- Thakre, R.; Bhutada, S.; Chouragade, B.; Khobragade, P.; Ketaki, H. Unexpected wound healing property of Ehretia laevis Roxb. (Khandu Chakka) plant. Int. J. Res. Ayurveda Pharm. 2016, 7, 54–57. [Google Scholar] [CrossRef]
- Rao, M.; Kumar, P.; Das, B. Comparative study of efficacy of Jatyadi Ghrita Pichu and Yasthimadhu Ghrita Pichu in the management of parikartika (fissure-in-ano). Int. J. Ayurveda Pharma Res. 2016, 4, 1–9. [Google Scholar]
- Samantaray, S.; Bishwal, R.; Singhai, S. Clinical efficacy of jatyadi taila in parikartika (fissure-in-ano). World J. Pharm. Med. Res. 2017, 3, 250–254. [Google Scholar]
- Tichkule, S.V.; Khandare, K.B.; Shrivastav, P.P. Proficiency of Khanduchakka Ghrit in the management of Parikartika: A case report. Indian J. Med. Res. 2019, 7, 47–50. [Google Scholar] [CrossRef]
- Tefere, Y.; Chanie, S.; Dessie, T.; Gedamu, H. Assessment of prevalence of dental caries and the associated factors among patients attending dental clinics in Debre Tabor general hospital: A hospital based cross sectional study. BMC Oral Health 2018, 18, 119–125. [Google Scholar] [CrossRef]
- Deshpande, R.; Walimbe, H.; Jadhav, M.; Deshpande, N.; Devare, S. Comparative evaluation of antimicrobial activity of various extracts of ‘Morinda pubescens’ in different concentration on human salivary microflora. Int. J. Pharm. Pharm. Sci. 2013, 5, 910–912. [Google Scholar]
- Hiremath, A.; Murugaboopathy, V.; Ankola, A.V.; Hebbal, M.; Mohandoss, S.; Pastay, P. Prevalence of dental caries among primary school children of India: A cross-sectional study. J. Clin. Diagn. Res. 2016, 10, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, R.; Khare, A.; Shah, A.; Mutha, M.; Deshpande, N. Going back to where it all started: An overview of five medicinal plants. Int. J. Contemp. Med. Res. 2015, 2, 1392–1396. [Google Scholar]
- Shah, A.; Marwat, S.K.; Gohar, F.; Khan, A.; Bhatti, K.H.; Amin, M.; Din, N.U.; Ahmad, M.; Zafar, M. Ethnobotanical study of medicinal plants of semi-tribal area of Makerwal & Gulla Khel (lying between Khyber Pakhtunkhwa and Punjab Provinces), Pakistan. Am. J. Plant. Sci. 2013, 4, 98–116. [Google Scholar]
- Kumar, P.R. Ethno medicinal plants used for oral health care in India. Int. J. Herb. Med. 2014, 2, 81–87. [Google Scholar]
- Deshpande, R.; Patil, V.; Shah, H.; Ruikar, A.; Gaikwad, S.; Kamble, G.; Mundhe, K.; Adsul, V. Back to mother nature: Novel herbal medicines in preventing dental caries. J. Dent. 2018, 113, 295–311. [Google Scholar]
- Bande, D.; Murarkar, K. Blood coagulation properties of Khandu Chakka (Ehretia laevis) plant leaves. Int. J. Curr. Res. Life Sci. 2018, 7, 2220–2222. [Google Scholar]
- Tichkule, S.V.; Khandare, K.B.; Shrivastav, P.P. Role of Khanduchakka (Ehretia laevis) Lepan (local application) in the management of delayed union of metatarsal fracture: A case report. J. Indian Sys. Med. 2019, 7, 127–130. [Google Scholar] [CrossRef]
- Shisha, T. Parameters for defining efficacy in fracture healing. Clin. Cases Miner. Bone Metab. 2010, 7, 15–16. [Google Scholar]
- Mohiuddin, M.; Arbain, D.; Islam, A.K.; Rahman, M.; Ahmad, M.S.; Ahmad, M.N. Electrochemical measurement of the antidiabetic potential of medicinal plants using multi-walled carbon nanotubes paste electrodes. Russ. J. Electrochem. 2015, 51, 368–375. [Google Scholar] [CrossRef]
- Ecobichon, D.J. The Basis of Toxicology Testing; CRC Press: New York, NY, USA, 1997; pp. 43–86. [Google Scholar]
- Goel, R.K.; Singh, D.; Lagunin, A.; Poroikov, V. PASS-assisted exploration of new therapeutic potential of natural products. Med. Chem. Res. 2011, 20, 1509–1514. [Google Scholar] [CrossRef]
- Gaikwad, K.N.; Mali, M.V. Tree flora of Nashik city, Maharashtra. Int. J. Life Sci. Pharm. Res. 2012, 2, 94–101. [Google Scholar]
- Rohini, I.; Jirouthu, B.; Kumar, N.S.; Bhavya, C.; Kumar, K.S. An ethno-medicinal survey of medicinal plants used by traditional healers of Araku valley, Andhra Pradesh, India. Int. J. Curr. Res. 2017, 9, 48633–48645. [Google Scholar]



| S. No. | Ailment/Use | Part of Plant | Locality/System of Medicine | Preparation Used | References |
|---|---|---|---|---|---|
| 1 | Abdominal pain | All parts of plants | Tribal of Wardha district of Maharashtra | Decoction and juice | [5,11] |
| 2 | Acute and chronic inflammations | Root | Korku tribe | Root extract | [15] |
| 3 | Analgesic | Bark | Jalpaiguri/West Bengal | The paste of bark has been used for the relief of pain especially for lower limbs. | [19] |
| 4 | Anthelmintic | Fruits and seeds | Asia and Australian tropics/Pune (Maharashtra) | Decoction | [2,23] |
| 5 | Antidote to vegetable poison | Stem bark, leaves and fruits | Tropical Asia and Australian tropics/Krishnagiri District, Tamil Nadu, India | Unknown | [5] |
| 6 | Antivenom (Vishaghna) | Leaves | Ayurveda | Unknown | [13] |
| 7 | Aphrodisiac | Powder of flowers | Tropical Asia and Australian tropics/Krishnagiri District, Tamil Nadu, India | Powder of flowers with milk has been employed as an aphrodisiac. | [5] |
| 8 | Asthma | Leaves and bark | Garasia tribes/Rajasthan | Decoction, juice of leaves and bark juice. | [18] |
| 9 | Astringent | Fruits | Asia and Australian tropics/Pune (Maharashtra) | Juice of fruits | [2,23] |
| 10 | Blisters of mouth | Leaves | Remote areas of Rajasthan | Powdered leaves were chewed with equal quantities of sugar. | [24,25] |
| 11 | Cachexia | Stem bark, leaves and fruits | Tropical Asia and Australian tropics/Krishnagiri District, Tamil Nadu, India | Unknown | [5] |
| 12 | Cough and cold | Leaves and bark | Garasia tribes/Rajasthan | Decoction of leaves and bark juice. | [18] |
| 13 | Cuts and wounds | Leaves | Garasia tribes/Rajasthan | The leaves were grounded and its paste is applied topically on wounds. | [18,21] |
| 14 | Delivery pain | Bark | Garasia tribes/Rajasthan | Bark juice | [18] |
| 15 | Demulcent | Fruits | Asia and Australian tropics/Pune (Maharashtra) | Unknown | [2,23] |
| 16 | Dental caries | Stems | Ayurveda | Bark is used as toothbrush | [26] |
| 17 | Diabetes (Prameha) | Leaves | Ayurveda | Decoction | [13] |
| 18 | Diarrhea | Bark and roots | Ayurveda | Decoction of bark and roots | [5] |
| 19 | Diphtheria | Stems and bark | Ayurveda | Decoction of stem and bark for the treatment of diphtheria. | [5] |
| 20 | Diuretic | Fruit | Asia and Australian tropics/Pune (Maharashtra) | Decoction | [2,23] |
| 21 | Dysentery | Stem bark | South West Bengal/district—Dindori, Madhyapradesh | Stem bark powder has been administered orally thrice in a day for the treatment of dysentery. | [27,28] |
| 22 | Dysuria | Leaves | Kota district of Rajasthan | Leaf powder was mixed with sugar and divided into 10 equal doses. Each dose has been administered daily orally along with goat milk or curd for cure of dysuria. | [25] |
| 23 | Eczema | Leaves | Tharu community/Uttarakhand | Paste of leaves was applied topically for the cure of eczema. | [21] |
| 24 | Expectorant | Fruit | Asia and Australian tropics/Pune (Maharashtra) | Decoction | [2,23] |
| 25 | Fever | Leaves | Garasia tribes/ Rajasthan | Decoction of leaves | [18] |
| 26 | Fissure | Leaves | Wardha Tribe/Maharashtra | Ghrit was prepared by using fresh leaves and applied locally on anal fissure twice a day for 21 days. Additionally, Triphala Churna (10 g) has also been recommended before bed time for one month with lukewarm water. | [17] |
| 27 | Food and fodder | Bark, leaves, stems and fruits | Tropical Asia and Australian tropics/Krishnagiri District, Tamil Nadu, India. | Inner bark of E. laevis has been used as food (dietary supplement for humans and cattle). Fruits are also edible by tribal children. | [5,23] |
| 28 | Fracture | Leaves | Ayurveda/ Garasia tribes/Rajasthan | Kalka (paste) was prepared and applied all over the foot. Cotton pad and cotton roll were applied firmly. The thickness of Kalka was 0.5–1 cm. This Kalka Lepana was kept for 24 h everyday with dressing for two weeks. | [14,18,29] |
| 29 | Fungal infections | Leaves | Dry deciduous forest areas of Paschim Medinipur district, West Bengal | Paste of leaves applied locally. | [30] |
| 30 | Gum’s problems | Stems | Dhule district/Maharashtra | Brush with stem piece can also be used. | [16] |
| 31 | Headache | Roots and leaves | Ayurveda | Paste of leaves were applied. | [23] |
| 32 | Joint pain | Leaves | Tribal of Wardha district of Maharashtra | Decoction and juice | [5] |
| 33 | Liver ailments | Leaves and seeds | Paste of seeds | [31] | |
| 34 | Liver diseases/jaundice | Seeds | Gujjar tribes/Sub-Himalayan region, Uttarakhand | Paste of soaked seeds was mixed with powder of Amomum subulatum and given with milk three times a day. | [20] |
| 35 | Manufacturing of cosmetics, wines and dyes | Stem bark, leaves and fruits | Tropical Asia and Australian tropics, Krishnagiri District, Tamil Nadu, India | Unknown | [2,8,32] |
| 36 | Ornamental pot herb | Whole plant | Tropical Asia and Australian tropics, Krishnagiri District, Tamil Nadu, India | Grown in earthen pots | [2,8,32] |
| 37 | Ringworm infections | Powdered kernel | Pune (Maharashtra) | Powdered kernel was mixed with oil and is applied topically to the affected area as a remedy for ringworm infections. | [2,23] |
| 38 | Scabies | Leaves | South West Bengal | Decoction and juice | [23] |
| 39 | Skin diseases | Leaves | Tharu community/Uttarakhand | The leaves were grounded and its paste is applied topically on affected areas. | [21,33] |
| 40 | Stomach diseases | Stem bark, leaves and fruits | Tropical Asia and Australian tropics/Krishnagiri District, Tamil Nadu, India | Decoction of leaves and barks. | [5] |
| 41 | Syphilis | Bark and roots | Ayurveda | Decoction of bark and roots. | [5,34] |
| 42 | Throat infections | Bark | Tropical Asia and Australian tropics | Bark is used internally and as a gargle in throat infections. | [23] |
| 43 | Toothache | Young branches | Pawra Tribe of Satpura Hills. | Young branches are used as toothbrushes. | [5,35] |
| 44 | Malaria and fever | Leaves | Tribe of Andaman & Nicobar Islands | Decoction of leaves | [36] |
| 45 | Ulcers | Stem | Dhule district/Maharashtra | Paste of leaves | [16] |
| 46 | Urinary tract infections | Bark and roots | Decoction of bark and roots | [5] | |
| 47 | Venereal diseases | Bark and roots | Ayurveda | Decoction of bark and roots have been recommended. | [5,11,34,37] |
| S. No. | Mineral (g/Kg) | Leaf | Bark | Fruit |
|---|---|---|---|---|
| 1 | Sodium | 2.12 | 1.59 | 1.09 |
| 2 | Phosphorous | 7.36 | 4.12 | 3.45 |
| 3 | Calcium | 38.31 | 38.03 | 36.12 |
| 4 | Zinc | 0.18 | 3.16 | 0.21 |
| 5 | Potassium | 26.23 | 22.33 | 28.12 |
| 6 | Iron | 1.11 | 0.30 | 1.28 |
| 7 | Magnesium | 12.21 | 6.46 | 13.45 |
| 8 | Copper | 0.02 | 0.05 | 0.01 |
| 9 | Manganese | 0.03 | 0.02 | 0.04 |
| 10 | Silica | 3.12 | 5.21 | 1.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, P.; Shri, R.; Ntie-Kang, F.; Kumar, S. Phytochemical and Ethnopharmacological Perspectives of Ehretia laevis. Molecules 2021, 26, 3489. https://doi.org/10.3390/molecules26123489
Sharma P, Shri R, Ntie-Kang F, Kumar S. Phytochemical and Ethnopharmacological Perspectives of Ehretia laevis. Molecules. 2021; 26(12):3489. https://doi.org/10.3390/molecules26123489
Chicago/Turabian StyleSharma, Pooja, Richa Shri, Fidele Ntie-Kang, and Suresh Kumar. 2021. "Phytochemical and Ethnopharmacological Perspectives of Ehretia laevis" Molecules 26, no. 12: 3489. https://doi.org/10.3390/molecules26123489
APA StyleSharma, P., Shri, R., Ntie-Kang, F., & Kumar, S. (2021). Phytochemical and Ethnopharmacological Perspectives of Ehretia laevis. Molecules, 26(12), 3489. https://doi.org/10.3390/molecules26123489







