A New Oleanane Type Saponin from the Aerial Parts of Nigella sativa with Anti-Oxidant and Anti-Diabetic Potential
Abstract
1. Introduction
2. Results
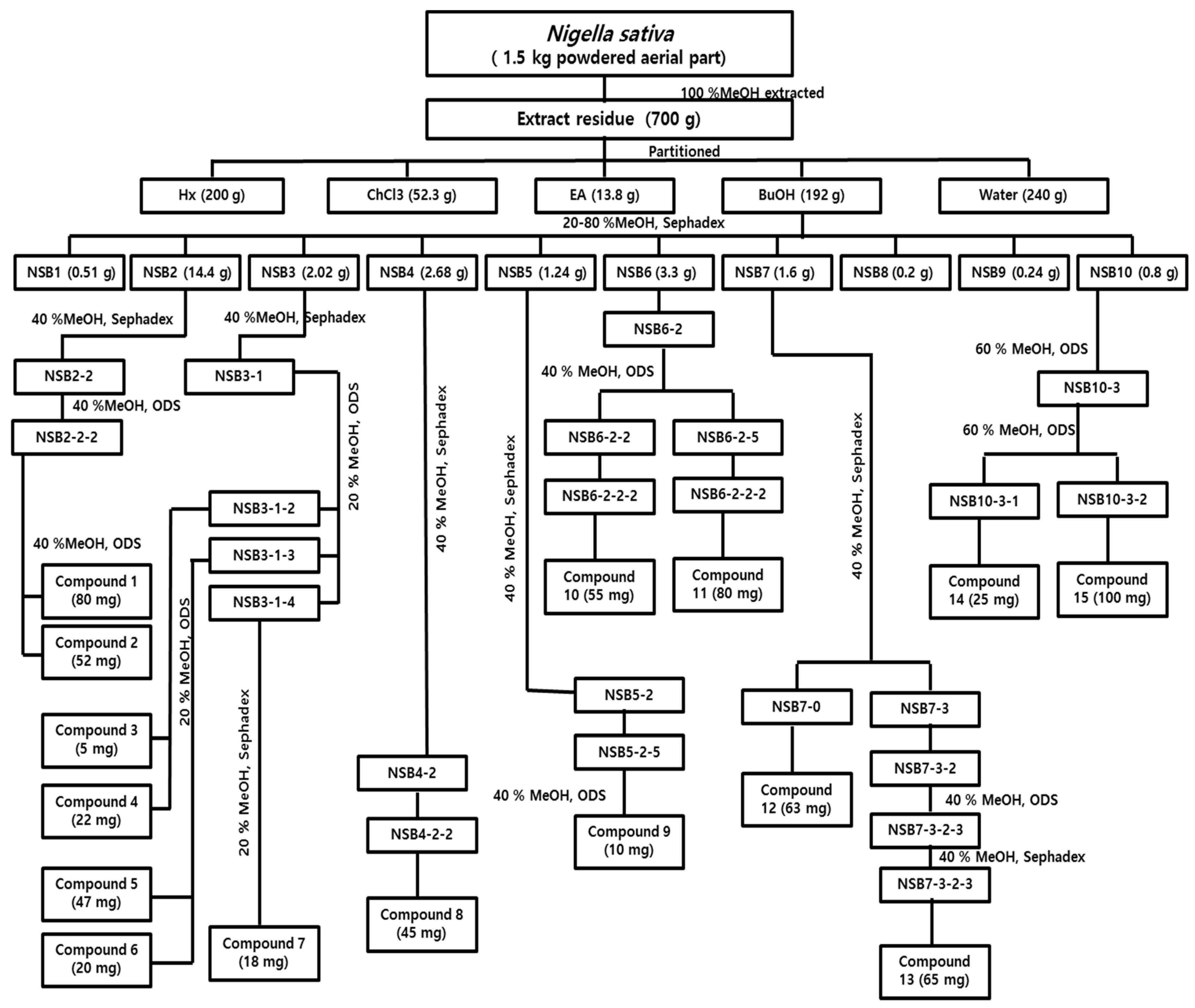
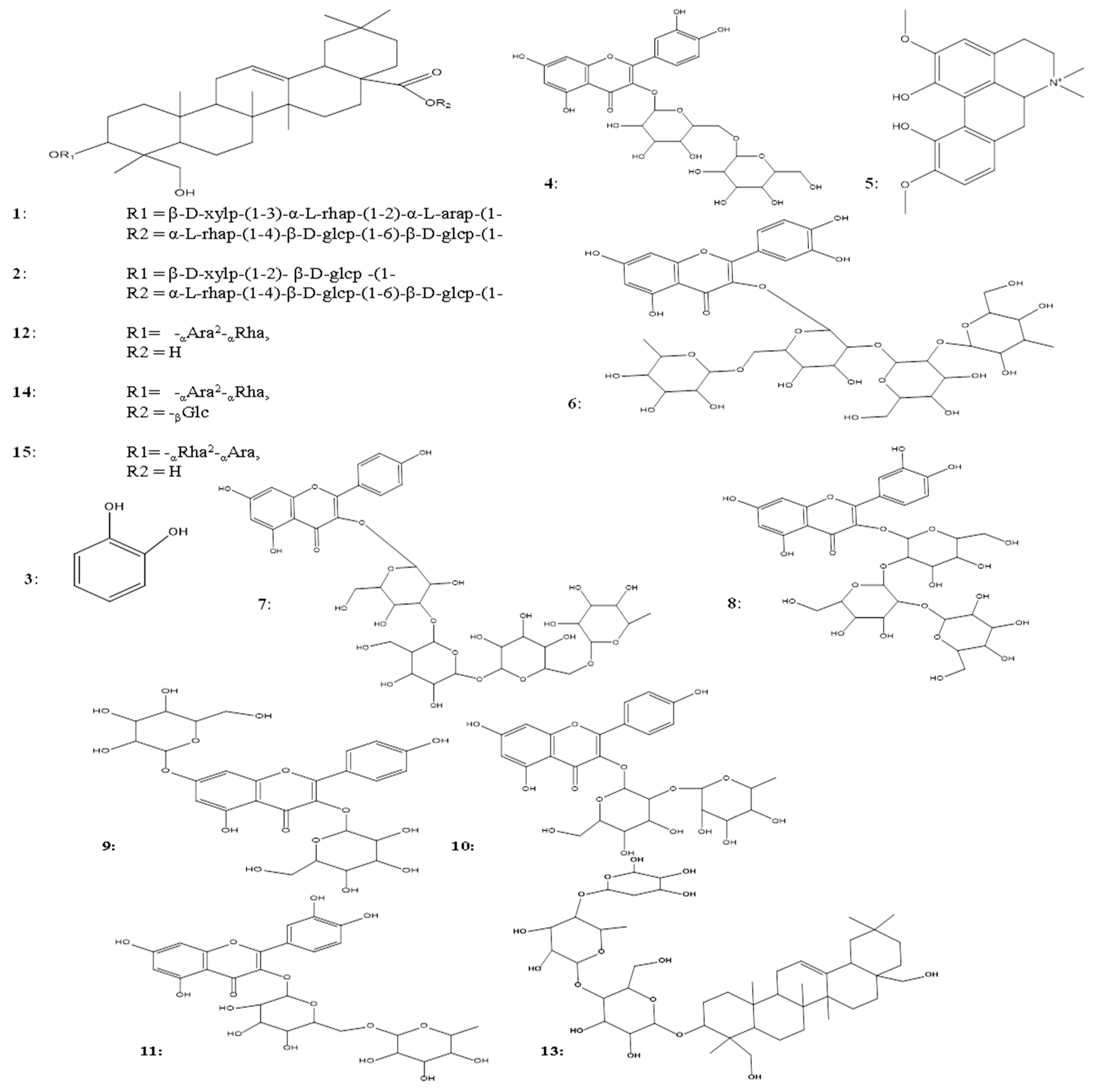
2.1. Extraction, Isolation, and Identification of Phytochemicals
2.2. Structure Elucidation of 3β,23,28-trihydroxyolean-12-ene 3-O-α-l-arabinopyranoside (1→4)-α-l-rhamnopyranosyl (1→4)-β-d-glucopyranoside Compound (13)
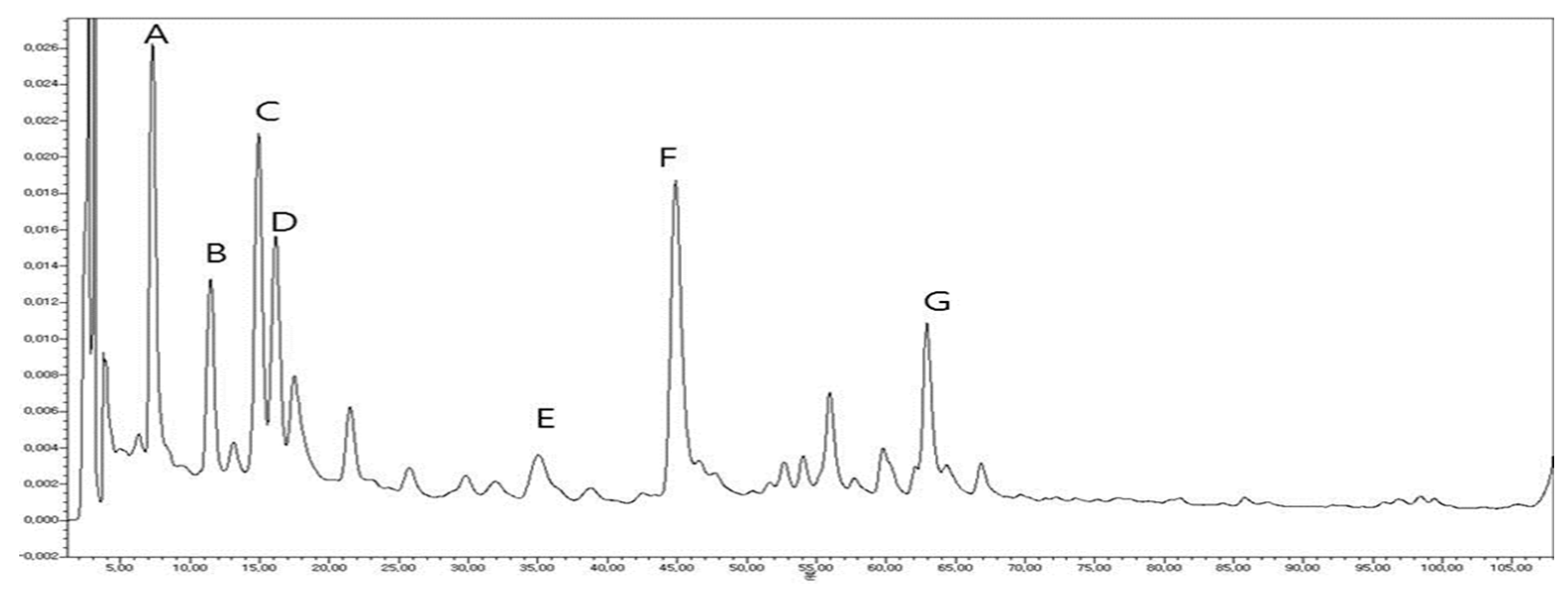
2.3. Fingerprint Analysis by HPLC–UV
2.4. Bioassays
2.4.1. Antioxidant Assays
DPPH Assay
ABTS Assay
2.4.2. Anti-Diabetic Assays
α-Glucosidase Assay
PTP1B Assay
3. Discussion
4. Materials and Methods
4.1. Chemicals and Equipment
4.2. Collection and Identification of Plant Materials
4.3. Extraction, Isolation and Identification of Phytochemicals
4.4. Development of a Fingerprint Pattern of Nigella sativa by HPLC-UV along with Quantitative and Qualitative Analysis
4.5. Bioassays
4.5.1. Antioxidant assays
1-Diphenyl-2-picryl-hydrazyl (DPPH) Assay
2′-Azino-bis (3-ethylbenzothiazoline-6-sulphonic acid (ABTS) Assay
4.5.2. Anti-diabetic Assays
α-Glucosidase Assay
Protein Tyrosine Phosphatase 1B (PTP1B) Inhibitory Assay
Supplementary Materials
Supplementary File 1Author Contributions
Funding
Conflicts of Interest
References
- Adhami, S.; Siraj, S.; Farooqi, H. Unexplored Medicinal Plants of Potential Therapeutic Importance: A Review. Trop. J. Nat. Prod. Res. 2018, 2, 3–11. [Google Scholar]
- Parveen, A.; Kim, J.H.; Oh, B.G.; Subedi, L.; Khan, Z.; Kim, S.Y. Phytochemicals: Target-based therapeutic strategies for diabetic retinopathy. Molecules 2018, 23, 1519. [Google Scholar] [CrossRef] [PubMed]
- Parveen, A.; Jin, M.; Kim, S.Y. Bioactive phytochemicals that regulate the cellular processes involved in diabetic nephropathy. Phytomedicine 2018, 39, 146–159. [Google Scholar] [CrossRef]
- Parveen, A.; Subedi, L.; Kim, H.W.; Khan, Z.; Zahra, Z.; Farooqi, M.Q.; Kim, S.Y. Phytochemicals targeting VEGF and VEGF-related multifactors as anticancer therapy. J. Clin. Med. 2019, 8, 350. [Google Scholar] [CrossRef] [PubMed]
- Abel-Salam, B.K. Immunomodulatory effects of black seeds and garlic on alloxan-induced diabetes in albino rat. Allergol. Immunopathol. 2012, 40, 336–340. [Google Scholar] [CrossRef]
- Abdel-Sater, K.A. Gastroprotective effects of Nigella Sativa oil on the formation of stress gastritis in hypothyroidal rats. Int. J. Physiol. Pathophysiol. Pharm. 2009, 1, 143–149. [Google Scholar]
- Assayed, M.E. Radioprotective effects of black seed (Nigella sativa) oil against hemopoietic damage and immunosuppression in gamma-irradiated rats. Immunopharmacol. Immunotoxicol. 2010, 32, 284–296. [Google Scholar] [CrossRef]
- Ahmad, A.; Husain, A.; Mujeeb, M.; Khan, S.A.; Najmi, A.K.; Siddique, N.A.; Damanhouri, Z.A.; Anwar, F. A review on therapeutic potential of Nigella sativa: A miracle herb. Asian Pac. J. Trop. Biomed. 2013, 3, 337–352. [Google Scholar] [CrossRef]
- Al-Ali, A.; Alkhawajah, A.A.; Randhawa, M.A.; Shaikh, N.A. Oral and intraperitoneal LD50 of thymoquinone, an active principle of Nigella sativa, in mice and rats. J. Ayub Med. Coll. Abbottabad 2008, 20, 25–27. [Google Scholar]
- Danaei, G.; Finucane, M.M.; Lu, Y.; Singh, G.M.; Cowan, M.J.; Paciorek, C.J.; Lin, J.K.; Farzadfar, F.; Khang, Y.-H.; Stevens, G.A. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2· 7 million participants. Lancet 2011, 378, 31–40. [Google Scholar] [CrossRef]
- Bamosa, A.O.; Kaatabi, H.; Lebdaa, F.M.; Elq, A.; Al-Sultanb, A. Effect of Nigella sativa seeds on the glycemic control of patients with type 2 diabetes mellitus. Indian J. Physiol. Pharm. 2010, 54, 344–354. [Google Scholar]
- Wang, M.; Hu, R.-Y.; Wu, H.-B.; Pan, J.; Gong, W.-W.; Guo, L.-H.; Zhong, J.-M.; Fei, F.-R.; Yu, M. Cancer risk among patients with type 2 diabetes mellitus: A population-based prospective study in China. Sci. Rep. 2015, 5, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ryan, G.J.; Jobe, L.J.; Martin, R. Pramlintide in the treatment of type 1 and type 2 diabetes mellitus. Clin. Ther. 2005, 27, 1500–1512. [Google Scholar] [CrossRef] [PubMed]
- Association, A.D. Economic costs of diabetes in the US in 2012. Diabetes Care 2013, 36, 1033–1046. [Google Scholar] [CrossRef]
- Parthiban, A.; Vijayalingam, S.; Shanmugasundaram, K.R.; Mohan, R. Oxidative stress and the development of diabetic complications-antioxidants and lipid peroxidation in erythrocytes and cell membrane. Cell Biol. Int. 1995, 19, 987–994. [Google Scholar]
- Herren, D.; Norman, J.B.; Anderson, R.; Tremblay, M.L.; Huby, A.-C.; de Chantemèle Belin, E. Deletion of protein tyrosine phosphatase 1B (PTP1B) enhances endothelial cyclooxygenase 2 expression and protects mice from type 1 diabetes-induced endothelial dysfunction. PLoS ONE 2015, 10, e0126866. [Google Scholar]
- Abdelsalam, S.S.; Korashy, H.M.; Zeidan, A.; Agouni, A. The Role of Protein Tyrosine Phosphatase (PTP)-1B in Cardiovascular Disease and Its Interplay with Insulin Resistance. Biomolecules 2019, 9, 286. [Google Scholar] [CrossRef]
- Kumar, S.; Narwal, S.; Kumar, V.; Prakash, O. α-glucosidase inhibitors from plants: A natural approach to treat diabetes. Pharmacogn. Rev. 2011, 5, 19. [Google Scholar] [CrossRef]
- Ye, W.-C.; Zhang, Q.-W.; Zhao, S.-X.; CHE, C.-T. Four new oleanane saponins from Anemone anhuiensis. Chem. Pharm. Bull. 2001, 49, 632–634. [Google Scholar] [CrossRef]
- Nair, P.R.; Melnick, S.J.; Wnuk, S.F.; Rapp, M.; Escalon, E.; Ramachandran, C. Isolation and characterization of an anticancer catechol compound from Semecarpus anacardium. J. Ethnopharmacol. 2009, 122, 450–456. [Google Scholar] [CrossRef]
- Lee, Y.K.; Hong, E.Y.; Whang, W.K. Inhibitory effect of chemical constituents isolated from Artemisia iwayomogi on polyol pathway and simultaneous quantification of major bioactive compounds. Biomed Res. Int. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Yan, R.; Wang, W.; Guo, J.; Liu, H.; Zhang, J.; Yang, B. Studies on the Alkaloids of the Bark of Magnolia officinalis: Isolation and On-line Analysis by HPLC-ESI-MSn. Molecules 2013, 18, 7739–7750. [Google Scholar] [CrossRef] [PubMed]
- Yoshimitsu, H.; Nishida, M.; Okawa, M.; Nohara, T. Four new triterpene glycosides from Nigella damascena. Chem. Pharm. Bull. 2007, 55, 488–491. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Manivannan, R.; Shopna, R. Isolation of Quercetin and Isorhamnetin Derivatives and Evaluation of Anti-microbial and Anti-inflammatory Activities of Persicaria glabra. Nat. Prod. Sci. 2015, 21, 170–175. [Google Scholar]
- Iwashina, T.; Kitajima, J.; Mizuno, T.; Smirnov, S.V.; Damdinsuren, O.; Kondo, K. New Kaempferol 3, 7-Diglycosides from Asplenium ruta-muraria and Asplenium altajense. Nat. Prod. Commun. 2015, 10, 1934578X1501000310. [Google Scholar] [CrossRef]
- Erosa Rejón, G.; Peña Rodríguez, L.M.; Sterner, O. Isolation of kaempferol-3-rutinoside from the leaf extract of Sideroxylon foetidissimum subsp. Gaumeri. Rev. Latinoam. Química 2010, 38, 7–11. [Google Scholar]
- Georgeta, S.; Pana, P.; Tunde, H.; Sanda, B. The isolation and identification of rutin from pharmaceutical products. An. Univ. Oradea Fasc. Ecotoxicol. Zooteh. Tehnol. Ind. Aliment. 2016, 109–113. [Google Scholar]
- Kumara, S.S.M.; Huat, B.T.K. Extraction, isolation and characterisation of antitumor principle, α-hederin, from the seeds of Nigella sativa. Planta Med. 2001, 67, 29–32. [Google Scholar] [CrossRef]
- Thu, V.K.; Van Thang, N.; Nhiem, N.X.; Tai, B.H.; Nam, N.H.; Van Kiem, P.; Van Minh, C.; Anh, H.L.T.; Kim, N.; Park, S. Oleanane-type saponins from Glochidion glomerulatum and their cytotoxic activities. Phytochemistry 2015, 116, 213–220. [Google Scholar] [CrossRef]
- Goldstein, B.J.; Bittner-Kowalczyk, A.; White, M.F.; Harbeck, M. Tyrosine dephosphorylation and deactivation of insulin receptor substrate-1 by protein-tyrosine phosphatase 1B Possible facilitation by the formation of a ternary complex with the Grb2 adaptor protein. J. Biol. Chem. 2000, 275, 4283–4289. [Google Scholar] [CrossRef]
- Aronson, D. Hyperglycemia and the pathobiology of diabetic complications. In Cardiovascular Diabetology: Clinical, Metabolic and Inflammatory Facets; Karger Publishers: Basel, Switzerland, 2008; Volume 45, pp. 1–16. [Google Scholar]
- Kim, D.H.; Lee, S.; Chung, Y.W.; Kim, B.M.; Kim, H.; Kim, K.; Yang, K.M. Antiobesity and antidiabetes effects of a Cudrania tricuspidata hydrophilic extract presenting PTP1B inhibitory potential. Biomed Res. Int. 2016, 2016. [Google Scholar]
- Elya, B.; Basah, K.; Mun’im, A.; Yuliastuti, W.; Bangun, A.; Septiana, E.K. Screening of α-glucosidase inhibitory activity from some plants of Apocynaceae, Clusiaceae, Euphorbiaceae, and Rubiaceae. Biomed Res. Int. 2011, 6. [Google Scholar]
- Zhang, X.D.; Liu, X.Q.; Kim, Y.H.; Whang, W.K. Chemical constituents and their acetyl cholinesterase inhibitory and antioxidant activities from leaves of Acanthopanax henryi: Potential complementary source against Alzheimer’s disease. Arch. Pharmacal. Res. 2014, 37, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.; Islam, M.; Jung, H.; Choi, J. In vitro antidiabetic potential of the fruits of Crataegus pinnatifida. Res. Pharm. Sci. 2014, 9, 11. [Google Scholar] [PubMed]
| Compound Number | DPPH Assay | ABTS Assay | α-Glucosidase Assay | PTP1B Assay |
|---|---|---|---|---|
| 1 | Nd | Nd | 217.5 ± 2.6 | Nd |
| 2 | Nd | Nd | 256.7 ± 3.7 | Nd |
| 3 | Nd | Nd | Nd | Nd |
| 4 | Nd | Nd | 254.2 ± 4.5 | Nd |
| 5 | 71.0 ± 0.5 | 139.2 ± 0.5 | 335.3 ± 0.2 | Nd |
| 6 | 32.7 ± 0.1 | 95.18 ± 0.9 | 257.8 ± 0.8 | Nd |
| 7 | Nd | Nd | 276.2 ± 2.1 | Nd |
| 8 | 35.5 ± 0.5 | 98.8 ± 0.5 | 274.1 ± 0.3 | Nd |
| 9 | 197.8 ± 2.7 | 247 ± 2.7 | 360.0 ± 0.3 | Nd |
| 10 | Nd | Nd | 214.5 ± 0.0 | Nd |
| 11 | 39.6 ± 0.5 | 129.0 ± 0.5 | 331.9 ± 1.6 | Nd |
| 12 | Nd | Nd | Nt | 91.3 ± 2.5 |
| 13 | Nd | Nd | Nt | Nd |
| 14 | Nd | Nd | Nt | Nd |
| 15 | Nd | Nd | Nt | Nd |
| Ascorbic acid | 51.7 ± 0.1 | 82.9 ± 2 | Nt | Nt |
| Trolox | 59.4 ± 0.9 | 96.2 ± 1.5 | Nt | Nt |
| Acarbose | Nt | Nt | 127.9 ± 2.0 | Nt |
| Ursolic acid | Nt | Nt | Nt | 0.8 ± 1.4 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parveen, A.; Farooq, M.A.; Kyunn, W.W. A New Oleanane Type Saponin from the Aerial Parts of Nigella sativa with Anti-Oxidant and Anti-Diabetic Potential. Molecules 2020, 25, 2171. https://doi.org/10.3390/molecules25092171
Parveen A, Farooq MA, Kyunn WW. A New Oleanane Type Saponin from the Aerial Parts of Nigella sativa with Anti-Oxidant and Anti-Diabetic Potential. Molecules. 2020; 25(9):2171. https://doi.org/10.3390/molecules25092171
Chicago/Turabian StyleParveen, Amna, Muhammad Asim Farooq, and Whang Wan Kyunn. 2020. "A New Oleanane Type Saponin from the Aerial Parts of Nigella sativa with Anti-Oxidant and Anti-Diabetic Potential" Molecules 25, no. 9: 2171. https://doi.org/10.3390/molecules25092171
APA StyleParveen, A., Farooq, M. A., & Kyunn, W. W. (2020). A New Oleanane Type Saponin from the Aerial Parts of Nigella sativa with Anti-Oxidant and Anti-Diabetic Potential. Molecules, 25(9), 2171. https://doi.org/10.3390/molecules25092171