Chitosan-Based Biomimetically Mineralized Composite Materials in Human Hard Tissue Repair
Abstract
1. Introduction
2. Structure, Properties and Applications of Chitosan
3. Chitosan-Based Biomimetically Mineralized Composite Materials
3.1. Properties of Composite Materials
3.2. Techniques for the Preparations of Chitosan Organic Templates with Composite Materials
3.2.1. Electrospinning
3.2.2. Freeze Drying
3.2.3. Gelation by Physical or Chemical Crosslinking
3.2.4. Layer-by-Layer (LBL) Self-Assembly
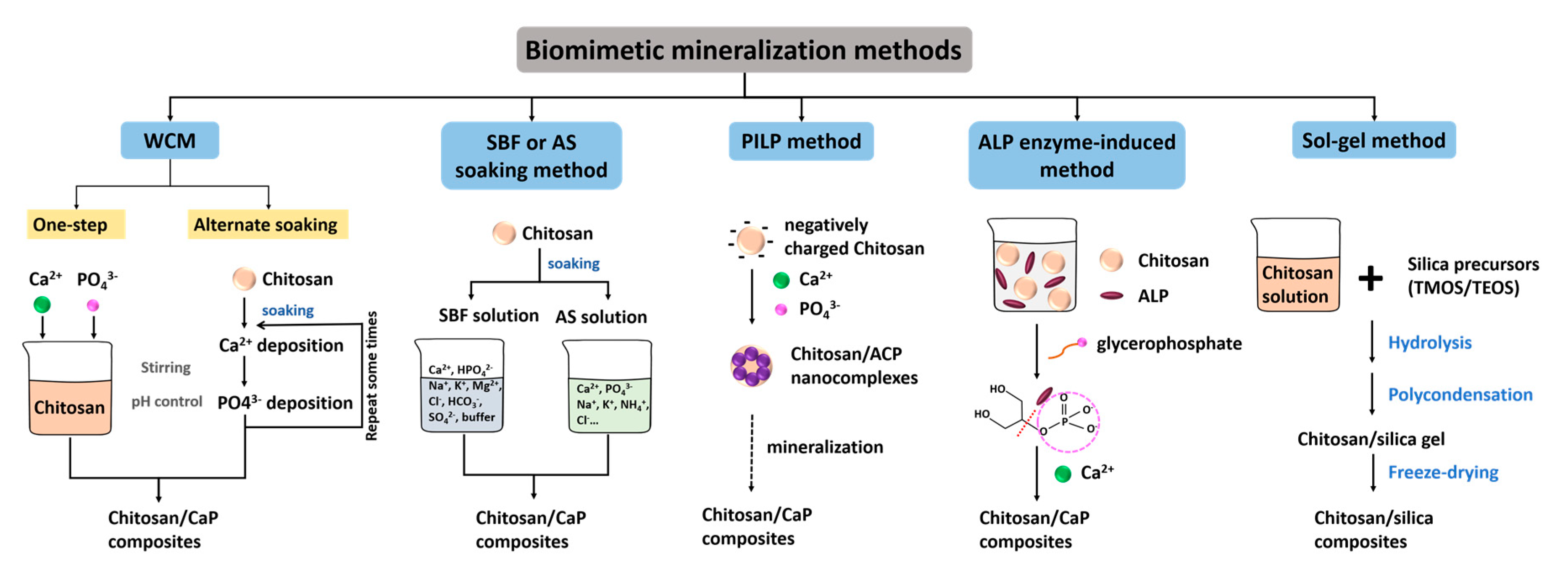
3.3. Biomimetic Mineralization Materials and Techniques for the Fabrication of Chitosan-Based Composites
3.3.1. Wet Chemical Method (WCM)
3.3.2. Simulated Body Fluid (SBF) or Artificial Saliva (AS) Soaking Method
3.3.3. Polymer-Induced Liquid Precursor (PILP) Method
3.3.4. Alkaline Phosphatase (ALP) Enzyme-Induced Method
3.3.5. Solution-Gelatin (sol-gel) Method
4. Applications of Chitosan-Based Biomimetically Mineralized Composite Materials in Human Hard Tissue Repair
4.1. Applications in Bone Tissue Engineering
4.2. Applications in Dental Hard Tissue Repair
5. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- Liu, Y.; Luo, D.; Wang, T. Hierarchical Structures of Bone and Bioinspired Bone Tissue Engineering. Small 2016, 12, 4611–4632. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, P.F.; Sallum, E.A.; Sallum, A.W.; Casati, M.Z.; Nociti, F.H. Dental cementum reviewed:development, structure, composition, regeneration and potential functions. Braz. J. Oral Sci. 2005, 4, 12. [Google Scholar]
- Goldberg, M.; Kulkarni, A.B.; Young, M.; Boskey, A. Dentin: Structure, composition and mineralization. Front. Biosci. 2011, 3, 711. [Google Scholar] [CrossRef]
- Ruan, Q.; Moradian-Oldak, J. Amelogenin and enamel biomimetics. J. Mater. Chem. B 2015, 3, 3112–3129. [Google Scholar] [CrossRef]
- Uskokovic, V. When 1 + 1 > 2: Nanostructured composites for hard tissue engineering applications. Mat. Sci. Eng. C-Mater. 2015, 57, 434–451. [Google Scholar] [CrossRef] [PubMed]
- Elsharkawy, S.; Mata, A. Hierarchical Biomineralization: From Nature’s Designs to Synthetic Materials for Regenerative Medicine and Dentistry. Adv. Healthc. Mater. 2018, 7, e1800178. [Google Scholar] [CrossRef]
- Wubneh, A.; Tsekoura, E.K.; Ayranci, C.; Uludağ, H. Current state of fabrication technologies and materials for bone tissue engineering. Acta Biomater. 2018, 80, 1–30. [Google Scholar] [CrossRef]
- Holzwarth, J.M.; Ma, P.X. Biomimetic nanofibrous scaffolds for bone tissue engineering. Biomaterials 2011, 32, 9622–9629. [Google Scholar] [CrossRef]
- Park, J.Y.; Park, S.H.; Kim, M.G.; Park, S.H.; Yoo, T.H.; Kim, M.S. Biomimetic Scaffolds for Bone Tissue Engineering. Adv. Exp. Med. Biol. 2018, 1064, 109–121. [Google Scholar]
- Tania, L.; Luca, T.; Francesca, P.; Andrea, G.; Marco, A.; Gerardo, P.; Patrizio, C.; Enzo, D.F. Fabrication and Applications of Micro/Nanostructured Devices for Tissue Engineering. Nano-Micro Lett. 2017, 9, 3–15. [Google Scholar]
- Ding, C.M.; Chen, Z.X.; Li, J.S. From molecules to macrostructures: Recent development of bioinspired hard tissue repair. Biomater. Sci. 2017, 5, 1435–1449. [Google Scholar] [CrossRef] [PubMed]
- Pandya, M.; Diekwisch, T.G.H. Enamel biomimetics-fiction or future of dentistry. Int. J. Oral Sci. 2019, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.M.; Abouauf, E.A.; AbuBakr, N.; Dörfer, C.E.; El-Sayed, K.F. Tissue Engineering Approaches for Enamel, Dentin, and Pulp Regeneration: An Update. Stem Cells Int. 2020, 2020, 5734539. [Google Scholar] [CrossRef] [PubMed]
- Younes, I.; Rinaudo, M. Chitin and chitosan preparation from marine sources. Structure, properties and applications. Mar. Drugs 2015, 13, 1133–1174. [Google Scholar] [CrossRef]
- Aguilar, A.; Zein, N.; Harmouch, E.; Hafdi, B.; Bornert, F.; Offner, D.; Clauss, F.; Fioretti, F.; Huck, O.; Benkirane-Jessel, N.; et al. Application of Chitosan in Bone and Dental Engineering. Molecules 2019, 24, 3009. [Google Scholar] [CrossRef]
- Vukajlovic, D.; Parker, J.; Bretcanu, O.; Novakovic, K. Chitosan based polymer/bioglass composites for tissue engineering applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 96, 955–967. [Google Scholar] [CrossRef]
- Singh, R.; Shitiz, K.; Singh, A. Chitin and chitosan: Biopolymers for wound management. Int. Wound J. 2017, 14, 1276–1289. [Google Scholar] [CrossRef]
- Husain, S.; Al-Samadani, K.H.; Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Zohaib, S.; Qasim, S.B. Chitosan Biomaterials for Current and Potential Dental Applications. Materials 2017, 10, 602. [Google Scholar] [CrossRef]
- Varlamov, V.P.; Il’ina, A.V.; Shagdarova, B.T.; Lunkov, A.P.; Mysyakina, I.S. Chitin/Chitosan and Its Derivatives: Fundamental Problems and Practical Approaches. Biochemistry 2020, 85, S154–S176. [Google Scholar] [CrossRef]
- Kim, C.H.; Park, S.J.; Yang, D.H.; Chun, H.J. Chitosan for Tissue Engineering. Adv. Exp. Med. Biol. 2018, 1077, 475–485. [Google Scholar]
- Detsi, A.; Kavetsou, E.; Kostopoulou, I.; Pitterou, I.; Pontillo, A.R.N.; Tzani, A.; Christodoulou, P.; Siliachli, A.; Zoumpoulakis, P. Nanosystems for the Encapsulation of Natural Products: The Case of Chitosan Biopolymer as a Matrix. Pharmaceutics 2020, 12, 669. [Google Scholar] [CrossRef]
- Philibert, T.; Lee, B.H.; Fabien, N. Current Status and New Perspectives on Chitin and Chitosan as Functional Biopolymers. Appl. Biochem. Biotechnol. 2017, 181, 1314–1337. [Google Scholar] [CrossRef]
- Foster, L.J.; Ho, S.; Hook, J.; Basuki, M.; Marçal, H. Chitosan as a Biomaterial: Influence of Degree of Deacetylation on Its Physiochemical, Material and Biological Properties. PLoS ONE 2015, 10, e0135153. [Google Scholar] [CrossRef] [PubMed]
- Chatelet, C.; Damour, O.; Domard, A. Influence of the degree of acetylation on some biological properties of chitosan films. Biomaterials 2001, 22, 261–268. [Google Scholar] [CrossRef]
- Tangsadthakun, C.; Kanokpanont, S.; Sanchavanakit, N.; Pichyangkura, R.; Banaprasert, T.; Tabata, Y.; Damrongsakkul, S. The influence of molecular weight of chitosan on the physical and biological properties of collagen/chitosan scaffolds. J. Biomater. Sci. Polym. Ed. 2007, 18, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R.; Rehman, S.R.U.; Ahmed, R.; Zahid, A.A.; Sharifi, M.; Falahati, M.; Hasan, A. Electrospun chitosan membranes containing bioactive and therapeutic agents for enhanced wound healing. Int. J. Biol. Macromol. 2020, 156, 153–170. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Bhuiyan, M.A.R.; Islam, M.N. Chitin and Chitosan: Structure, Properties and Applications in Biomedical Engineering. J. Polym. Environ. 2016, 25, 854–866. [Google Scholar] [CrossRef]
- Shariatinia, Z. Carboxymethyl chitosan: Properties and biomedical applications. Int. J. Biol. Macromol. 2018, 120 (Pt B), 1406–1419. [Google Scholar] [CrossRef]
- Fakhri, E.; Eslami, H.; Maroufi, P.; Pakdel, F.; Taghizadeh, S.; Ganbarov, K.; Yousefi, M.; Tanomand, A.; Yousefi, B.; Mahmoudi, S.; et al. Chitosan biomaterials application in dentistry. Int. J. Biol. Macromol. 2020, 162, 956–974. [Google Scholar] [CrossRef]
- Wang, W.; Meng, Q.; Li, Q.; Liu, J.; Zhou, M.; Jin, Z.; Zhao, K. Chitosan Derivatives and Their Application in Biomedicine. Int. J. Mol. Sci. 2020, 21, 487. [Google Scholar] [CrossRef]
- Ali, A.; Ahmed, S. A review on chitosan and its nanocomposites in drug delivery. Int. J. Biol. Macromol. 2018, 109, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, S.M.; Thomas, M.; Reddy, K.K.; Sooraparaju, S.G.; Asthana, A.; Bhatnagar, I. Chitosan as biomaterial in drug delivery and tissue engineering. Int. J. Biol. Macromol. 2018, 110, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Preethi Soundarya, S.; Haritha Menon, A.; Viji Chandran, S.; Selvamurugan, N. Bone tissue engineering: Scaffold preparation using chitosan and other biomaterials with different design and fabrication techniques. Int. J. Biol. Macromol. 2018, 119, 1228–1239. [Google Scholar] [CrossRef]
- Bano, I.; Arshad, M.; Yasin, T.; Ghauri, M.A.; Younus, M. Chitosan: A potential biopolymer for wound management. Int. J. Biol. Macromol. 2017, 102, 380–383. [Google Scholar] [CrossRef] [PubMed]
- Park, J.U.; Song, E.H.; Jeong, S.H.; Song, J.; Kim, H.E.; Kim, S. Chitosan-Based Dressing Materials for Problematic Wound Management. Adv. Exp. Med. Biol. 2018, 1077, 527–537. [Google Scholar]
- Fathi, M.; Majidi, S.; Zangabad, P.S.; Barar, J.; Erfan-Niya, H.; Omidi, Y. Chitosan-based multifunctional nanomedicines and theranostics for targeted therapy of cancer. Med. Res. Rev. 2018, 38, 2110–2136. [Google Scholar] [CrossRef] [PubMed]
- Santos-Carballal, B.; Fernández Fernández, E.; Goycoolea, F.M. Chitosan in Non-Viral Gene Delivery: Role of Structure, Characterization Methods, and Insights in Cancer and Rare Diseases Therapies. Polymers 2018, 10, 444. [Google Scholar] [CrossRef] [PubMed]
- Chuan, D.; Jin, T.; Fan, R.; Zhou, L.; Guo, G. Chitosan for gene delivery: Methods for improvement and applications. Adv. Colloid Interface Sci. 2019, 268, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Pham, D.T.N.; Oloketuyi, S.F.; Manivasagan, P.; Oh, J.; Kim, Y.M. Chitosan and their derivatives: Antibiofilm drugs against pathogenic bacteria. Colloids Surf. B Biointerfaces 2020, 185, 110627. [Google Scholar] [CrossRef]
- Tsiourvas, D.; Sapalidis, A.; Papadopoulos, T. Hydroxyapatite/chitosan-based porous three-dimensional scaffolds with complex geometries. Mater. Today. Commun. 2016, 7, 59–66. [Google Scholar] [CrossRef]
- Zhang, L.; Dong, Y.S.; Xue, Y.M.; Shi, J.; Zhang, X.Y.; Liu, Y.F.; Midgley, A.C.; Wang, S.F. Multifunctional Triple-Layered Composite Scaffolds Combining Platelet-Rich Fibrin Promote Bone Regeneration. ACS Biomater. Sci. Eng. 2019, 5, 6691–6702. [Google Scholar] [CrossRef]
- Kumar, P.; Saini, M.; Dehiya, B.S.; Umar, A.; Sindhu, A.; Mohammed, H.; Al-Hadeethi, Y.; Guo, Z.H. Fabrication and in-vitro biocompatibility of freeze-dried CTS-nHA and CTS-nBG scaffolds for bone regeneration applications. Int. J. Biol. Macromol. 2020, 149, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Ding, H.; Song, F.; Wang, J. Effects of preparation methods on the bone formation potential of apatite-coated chitosan microspheres. J. Biomater. Sci. Polym. Ed. 2014, 25, 2080–2093. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.-P.; Guan, J.-J.; Yang, J.; Wang, Y.; Zhang, C.-Q.; Ke, Q.-F. Hybrid nanostructured hydroxyapatite-chitosan composite scaffold: Bioinspired fabrication, mechanical properties and biological properties. J. Mater. Chem. B 2015, 3, 4679–4689. [Google Scholar] [CrossRef]
- Li, J.; Zhu, D.; Yin, J.; Liu, Y.; Yao, F.; Yao, K. Formation of nano-hydroxyapatite crystal in situ in chitosan-pectin polyelectrolyte complex network. Mat. Sci. Eng. C-Mater. 2010, 30, 795–803. [Google Scholar] [CrossRef]
- Hu, Y.; Chen, J.; Fan, T.; Zhang, Y.; Zhao, Y.; Shi, X.; Zhang, Q. Biomimetic mineralized hierarchical hybrid scaffolds based on in situ synthesis of nano-hydroxyapatite/chitosan/chondroitin sulfate/hyaluronic acid for bone tissue engineering. Colloids Surf. B Biointerfaces 2017, 157, 93–100. [Google Scholar] [CrossRef]
- Park, K.H.; Kim, S.J.; Hwang, M.J.; Song, H.J.; Park, Y.J. Biomimetic fabrication of calcium phosphate/chitosan nanohybrid composite in modified simulated body fluids. Express Polym. Lett. 2017, 11, 14–20. [Google Scholar] [CrossRef]
- Li, Y.; Chen, X.; Fok, A.; Rodriguez-Cabello, J.C.; Aparicio, C. Biomimetic Mineralization of Recombinamer-Based Hydrogels toward Controlled Morphologies and High Mineral Density. ACS Appl. Mater. Interfaces 2015, 7, 25784–25792. [Google Scholar] [CrossRef]
- Cochrane, N.J.; Cai, F.; Huq, N.L.; Burrow, M.F.; Reynolds, E.C. New approaches to enhanced remineralization of tooth enamel. J. Dent. Res. 2010, 89, 1187–1197. [Google Scholar] [CrossRef]
- Xu, A.-W.; Ma, Y.; Cölfen, H. Biomimetic mineralization. J. Mater. Chem. 2007, 17, 415–449. [Google Scholar] [CrossRef]
- Porter, J.R.; Ruckh, T.T.; Popat, K.C. Bone tissue engineering: A review in bone biomimetics and drug delivery strategies. Biotechnol. Prog. 2009, 25, 1539–1560. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Annu; Ali, A.; Sheikh, J. A review on chitosan centred scaffolds and their applications in tissue engineering. Int. J. Biol. Macromol. 2018, 116, 849–862. [Google Scholar] [CrossRef] [PubMed]
- Reneker, D.H.; Chun, I. Nanometre diameter fibres of polymer, produced by electrospinning. Nanotechnology 1999, 7, 216–223. [Google Scholar] [CrossRef]
- Schiffman, J.D.; Schauer, C.L. One-step electrospinning of cross-linked chitosan fibers. Biomacromolecules 2007, 8, 2665–2667. [Google Scholar] [CrossRef]
- Kalantari, K.; Afifi, A.M.; Jahangirian, H.; Webster, T.J. Biomedical applications of chitosan electrospun nanofibers as a green polymer - Review. Carbohydr. Polym. 2019, 207, 588–600. [Google Scholar] [CrossRef] [PubMed]
- Doan Van Hong, T.; Ho, M.H.; Hsiao, S.W.; Li, C.H. Wet chemical process to enhance osteoconductivity of electrospun chitosan nanofibers. J. Mater. Sci. 2015, 50, 1575–1585. [Google Scholar] [CrossRef]
- Yu, Y.; Hua, S.; Yang, M.; Fu, Z.; Teng, S.; Niu, K.; Zhao, Q.; Yi, C. Fabrication and characterization of electrospinning/3D printing bone tissue engineering scaffold. RSC Adv. 2016, 6, 112. [Google Scholar] [CrossRef]
- Araujo, J.V.; Carvalho, P.P.; Best, S.M. Electrospinning of Bioinspired Polymer Scaffolds. In Engineering Mineralized and Load Bearing Tissues; Bertassoni, L.E., Coelho, P.G., Eds.; Springer Nature: New York, NY, USA, 2015; pp. 33–53. [Google Scholar]
- Zhao, X.; Zhou, L.; Li, Q.; Zou, Q.; Du, C. Biomimetic mineralization of carboxymethyl chitosan nanofibers with improved osteogenic activity in vitro and in vivo. Carbohydr. Polym. 2018, 195, 225–234. [Google Scholar] [CrossRef]
- Lv, Q.; Feng, Q. Preparation of 3-D regenerated fibroin scaffolds with freeze drying method and freeze drying/foaming technique. J. Mater. Sci. Mater. Med. 2006, 17, 1349–1356. [Google Scholar] [CrossRef]
- Valencia, C.; Valencia, C.H.; Zuluaga, F.; Valencia, M.E.; Mina, J.H.; Grande-Tovar, C.D. Synthesis and Application of Scaffolds of Chitosan-Graphene Oxide by the Freeze-Drying Method for Tissue Regeneration. Molecules 2018, 23, 2651. [Google Scholar] [CrossRef]
- Lu, T.; Li, Y.; Chen, T. Techniques for fabrication and construction of three-dimensional scaffolds for tissue engineering. Int. J. Nanomed. 2013, 8, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Matinfar, M.; Mesgar, A.S.; Mohammadi, Z. Evaluation of physicochemical, mechanical and biological properties of chitosan/carboxymethyl cellulose reinforced with multiphasic calcium phosphate whisker-like fibers for bone tissue engineering. Mat. Sci. Eng. C-Mater. 2019, 100, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Zhou, L.; Xie, W.L.; Zeng, D.Y.; Cai, D.Q.; Wang, H.Y.; Zhou, C.R.; Wang, J.; Li, L.H. Alkaline phosphatase enzyme-induced biomineralization of chitosan scaffolds with enhanced osteogenesis for bone tissue engineering. Chem. Eng. J. 2019, 371, 618–630. [Google Scholar] [CrossRef]
- Chen, Z.; Cao, S.; Wang, H.; Li, Y.; Kishen, A.; Deng, X.; Yang, X.; Wang, Y.; Cong, C.; Wang, H.; et al. Biomimetic Remineralization of Demineralized Dentine Using Scaffold of CMC/ACP Nanocomplexes in an In Vitro Tooth Model of Deep Caries. PLoS ONE 2015, 10, e0016553. [Google Scholar] [CrossRef]
- Hamedi, H.; Moradi, S.; Hudson, S.M.; Tonelli, A.E. Chitosan based hydrogels and their applications for drug delivery in wound dressings: A review. Carbohydr. Polym. 2018, 199, 445–460. [Google Scholar] [CrossRef] [PubMed]
- Pella, M.C.G.; Lima-Tenorio, M.K.; Tenorio-Neto, E.T.; Guilherme, M.R.; Muniz, E.C.; Rubira, A.F. Chitosan-based hydrogels: From preparation to biomedical applications. Carbohydr. Polym. 2018, 196, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Desai, K.G. Chitosan Nanoparticles Prepared by Ionotropic Gelation: An Overview of Recent Advances. Crit. Rev. Ther. Drug Carrier Syst. 2016, 33, 107–158. [Google Scholar] [CrossRef] [PubMed]
- Koukaras, E.N.; Papadimitriou, S.A.; Bikiaris, D.N.; Froudakis, G.E. Insight on the formation of chitosan nanoparticles through ionotropic gelation with tripolyphosphate. Mol. Pharm. 2012, 9, 2856–2862. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, H.; Zorzi, G.K.; Fecker, T.; El Gueddari, N.E.; Moerschbacher, B.M.; Goycoolea, F.M. A rational approach towards the design of chitosan-based nanoparticles obtained by ionotropic gelation. Colloids Surf. B 2015, 135, 99–108. [Google Scholar] [CrossRef]
- Divya, K.; Jisha, M.S. Chitosan nanoparticles preparation and applications. Environ. Chem. Lett. 2017, 16, 101–112. [Google Scholar] [CrossRef]
- Zou, L.; Zhang, Y.; Liu, X.; Chen, J.; Zhang, Q. Biomimetic mineralization on natural and synthetic polymers to prepare hybrid scaffolds for bone tissue engineering. Colloids Surf. B 2019, 178, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Nitta, S.; Komatsu, A.; Ishii, T.; Ohnishi, M.; Inoue, A.; Iwamoto, H. Fabrication and characterization of water-dispersed chitosan nanofiber/poly(ethylene glycol) diacrylate/calcium phosphate-based porous composites. Carbohydr. Polym. 2017, 174, 1034–1040. [Google Scholar] [CrossRef]
- Zaharia, A.; Plescan, V.G.; Anghel, E.M.; Musat, V. Human Dentine Remineralization under Non-colagen Materials Action. Rev. Chim. 2017, 68, 928–932. [Google Scholar] [CrossRef]
- Zaharia, A.; Musat, V.; Anghel, E.M.; Atkinson, I.; Mocioiu, O.-C.; Busila, M.; Plescan, V.G. Biomimetic chitosan-hydroxyapatite hybrid biocoatings for enamel remineralization. Ceram. Int. 2017, 43, 11390–11402. [Google Scholar] [CrossRef]
- Richardson, J.J.; Björnmalm, M.; Caruso, F. Multilayer assembly. Technology-driven layer-by-layer assembly of nanofilms. Science 2015, 348, aaa2491. [Google Scholar] [CrossRef]
- Tang, Z.; Wang, Y.; Podsiadlo, P.; Kotov, N.A. Biomedical applications of layer-by-layer assembly: From biomimetics to tissue engineering. Adv. Mater. 2007, 19, 3203–3224. [Google Scholar] [CrossRef]
- Zhang, S.; Xing, M.; Li, B. Biomimetic Layer-by-Layer Self-Assembly of Nanofilms, Nanocoatings, and 3D Scaffolds for Tissue Engineering. Int. J. Mol. Sci. 2018, 19, 1641. [Google Scholar] [CrossRef]
- Yoshida, M.; Langer, R.; Lahann, J.; Lendlein, A. From Advanced Biomedical Coatings to Multi-Functionalized Biomaterials. J. Macromol. Sci. C 2006, 46, 347–375. [Google Scholar] [CrossRef]
- Liang, H.; Sheng, F.; Zhou, B.; Pei, Y.; Li, B.; Li, J. Phosphoprotein/chitosan electrospun nanofibrous scaffold for biomineralization. Int. J. Biol. Macromol. 2017, 102, 218–224. [Google Scholar] [CrossRef]
- Shakir, M.; Jolly, R.; Khan, M.S.; Iram, N.; Khan, H.M. Nano-hydroxyapatite/chitosan-starch nanocomposite as a novel bone construct: Synthesis and in vitro studies. Int. J. Biol. Macromol. 2015, 80, 282–292. [Google Scholar] [CrossRef]
- Ding, C.C.; Teng, S.H.; Pan, H. In-situ generation of chitosan/hydroxyapatite composite microspheres for biomedical application. Mater. Lett. 2012, 79, 72–74. [Google Scholar] [CrossRef]
- Wang, Y.; Ngo Van, M.; Wang, H.; Zhong, X.; Zhang, X.; Li, C. Synergistic intrafibrillar/extrafibrillar mineralization of collagen scaffolds based on a biomimetic strategy to promote the regeneration of bone defects. Int. J. Nanomed. 2016, 11, 2053–2067. [Google Scholar]
- Ruan, Q.; Liberman, D.; Zhang, Y.; Ren, D.; Zhang, Y.; Nutt, S.; Moradian-Oldak, J. Assembly of Layered Monetite-Chitosan Nanocomposite and Its Transition to Organized Hydroxyapatite. ACS Biomater. Sci. Eng. 2016, 2, 1049–1058. [Google Scholar] [CrossRef]
- Pipattanawarothai, A.; Suksai, C.; Srisook, K.; Trakulsujaritchok, T. Non-cytotoxic hybrid bioscaffolds of chitosan-silica: Sol-gel synthesis, characterization and proposed application. Carbohydr. Polym. 2017, 178, 190–199. [Google Scholar] [CrossRef]
- Salama, A.; Hesemann, P. Synthesis and characterization of N-guanidinium chitosan/silica ionic hybrids as templates for calcium phosphate mineralization. Int. J. Biol. Macromol. 2020, 147, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Olszta, M.J.; Cheng, X.; Jee, S.S.; Kumar, R.; Kim, Y.Y.; Kaufman, M.J.; Douglas, E.P.; Gower, L.B. Bone structure and formation: A new perspective. Mat. Sci. Eng. R. 2007, 58, 77–116. [Google Scholar] [CrossRef]
- Akao, M.; Aoki, H.; Kato, K. Mechanical properties of sintered hydroxyapatite for prosthetic applications. J. Mater. Sci. 1981, 16, 809–812. [Google Scholar] [CrossRef]
- Kong, L.B.; Ma, J.; Boey, F. Nanosized hydroxyapatite powders derived from coprecipitation process. J. Mater. Sci. 2002, 37, 1131–1134. [Google Scholar] [CrossRef]
- Ivan, F.D.; Marian, A.; Tanase, C.E.; Butnaru, M.; Verestiuc, L. Biomimetic composites based on calcium phosphates and chitosan-hyaluronic acid with potential application in bone tissue engineering. Key Eng. Mater. 2014, 587, 191–196. [Google Scholar] [CrossRef]
- Chen, P.; Liu, L.; Pan, J.; Mei, J.; Li, C.; Zheng, Y. Biomimetic composite scaffold of hydroxyapatite/gelatin-chitosan core-shell nanofibers for bone tissue engineering. Mat. Sci. Eng. C-Mater. 2019, 97, 325–335. [Google Scholar] [CrossRef]
- Liu, Z.; Xu, D.; Tong, S.; Tian, Y.; Li, G.; Sun, X.; Wang, X. Comparison studies of mineralized and non-mineralized SF/CS hybrid bone scaffolds co-cultured with the osteoblast cell line MC3T3-E1 in vitro. Int. J. Clin. Exp. Med. 2017, 10, 8969–8978. [Google Scholar]
- Lu, X.; Leng, Y. Theoretical analysis of calcium phosphate precipitation in simulated body fluid. Biomaterials 2005, 26, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Hong Thien, D.; Hsiao, S.W.; Ho, M.H.; Li, C.H.; Shih, J.L. Electrospun chitosan/hydroxyapatite nanofibers for bone tissue engineering. J. Mater. Sci. 2013, 48, 1640–1645. [Google Scholar] [CrossRef]
- Depan, D.; Pesacreta, T.C.; Misra, R.D.K. The synergistic effect of a hybrid graphene oxide-chitosan system and biomimetic mineralization on osteoblast functions. Biomater. Sci. 2014, 2, 264–274. [Google Scholar] [CrossRef]
- Leung, V.W.; Darvell, B.W. Artificial salivas for in vitro studies of dental materials. J. Dent. 1997, 25, 475–484. [Google Scholar] [CrossRef]
- Vimalraj, S. Alkaline phosphatase: Structure, expression and its function in bone mineralization. Gene 2020, 754, 144855. [Google Scholar] [CrossRef]
- Douglas, T.E.L.; Skwarczynska, A.; Modrzejewska, Z.; Balcaen, L.; Schaubroeck, D.; Lycke, S.; Vanhaecke, F.; Vandenabeele, P.; Dubruel, P.; Jansen, J.A.; et al. Acceleration of gelation and promotion of mineralization of chitosan hydrogels by alkaline phosphatase. Int. J. Biol. Macromol. 2013, 56, 122–132. [Google Scholar] [CrossRef]
- Liu, B.; Cao, Y.; Huang, Z.; Duan, Y.; Che, S. Silica biomineralization via the self-assembly of helical biomolecules. Adv. Mater. 2015, 27, 479–497. [Google Scholar] [CrossRef] [PubMed]
- Ivanenko, M.V.; Nikitina, E.Y.; Khonina, T.G.; Shadrina, E.V.; Novoselova, M.E.; Kuznetsov, D.K.; Karabanalov, M.S. Features of formation and structure of silicon-polysaccharide-containing polyolate hydrogels obtained by the method of biomimetic mineralization. J. Sol.-Gel. Sci. Technol. 2019, 92, 376–385. [Google Scholar] [CrossRef]
- Singh, V.; Srivastava, P.; Singh, A.; Singh, D.; Malviya, T. Polysaccharide-Silica Hybrids: Design and Applications. Polym. Rev. 2016, 56, 113–136. [Google Scholar] [CrossRef]
- Owens, G.J.; Singh, R.K.; Foroutan, F.; Alqaysi, M.; Han, C.-M.; Mahapatra, C.; Kim, H.-W.; Knowles, J.C. Sol–gel based materials for biomedical applications. Prog. Mater. Sci. 2016, 77, 1–79. [Google Scholar] [CrossRef]
- Reznikov, N.; Shahar, R.; Weiner, S. Bone hierarchical structure in three dimensions. Acta Biomater. 2014, 10, 3815–3826. [Google Scholar] [CrossRef]
- Chahal, S.; Kumar, A.; Hussian, F.S.J. Development of biomimetic electrospun polymeric biomaterials for bone tissue engineering. A review. J. Biomater. Sci. Polym. Ed. 2019, 30, 1308–1355. [Google Scholar] [CrossRef] [PubMed]
- Przekora, A. The summary of the most important cell-biomaterial interactions that need to be considered during in vitro biocompatibility testing of bone scaffolds for tissue engineering applications. Mat. Sci. Eng. C-Mater. 2019, 97, 1036–1051. [Google Scholar] [CrossRef] [PubMed]
- Venkatesan, J.; Kim, S.K. Nano-hydroxyapatite composite biomaterials for bone tissue engineering--a review. J. Biomed. Nanotechnol. 2014, 10, 3124–3140. [Google Scholar] [CrossRef]
- Farokhi, M.; Mottaghitalab, F.; Samani, S.; Shokrgozar, M.A.; Kundu, S.C.; Reis, R.L.; Fatahi, Y.; Kaplan, D.L. Silk fibroin/hydroxyapatite composites for bone tissue engineering. Biotechnol. Adv. 2018, 36, 68–91. [Google Scholar] [CrossRef]
- Tao, F.; Cheng, Y.; Shi, X.; Zheng, H.; Du, Y.; Xiang, W.; Deng, H. Applications of chitin and chitosan nanofibers in bone regenerative engineering. Carbohydr. Polym. 2020, 230, 115658. [Google Scholar] [CrossRef] [PubMed]
- Budiraharjo, R.; Neoh, K.G.; Kang, E.T. Hydroxyapatite-coated carboxymethyl chitosan scaffolds for promoting osteoblast and stem cell differentiation. J. Colloid Interface Sci. 2012, 366, 224–232. [Google Scholar] [CrossRef]
- Upadhyaya, L.; Singh, J.; Agarwal, V.; Tewari, R.P. The implications of recent advances in carboxymethyl chitosan based targeted drug delivery and tissue engineering applications. J. Control. Release 2014, 186, 54–87. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Xi, P.; Xie, G.; Shi, Y.; Wang, J. Simultaneous Reduction and Surface Functionalization of Graphene Oxide for Hydroxyapatite Mineralization. J. Phys. Chem. C. 2012, 116, 3334–3341. [Google Scholar] [CrossRef]
- Liu, H.; Cheng, J.; Chen, F.; Bai, D.; Shao, C.; Wang, J.; Xi, P.; Zeng, Z. Gelatin functionalized graphene oxide for mineralization of hydroxyapatite: Biomimetic and in vitro evaluation. Nanoscale 2014, 6, 5315–5322. [Google Scholar] [CrossRef]
- Asha, S.; Ananth, A.N.; Jose, S.P.; Rajan, M.A.J. Reduced graphene oxide aerogel networks with soft interfacial template for applications in bone tissue regeneration. Appl. Nanosci. 2018, 8, 395–405. [Google Scholar] [CrossRef]
- Lin, M.L.; Liu, H.H.; Deng, J.J.; An, R.; Shen, M.J.; Li, Y.Q.; Zhang, X. Carboxymethyl chitosan as a polyampholyte mediating intrafibrillar mineralization of collagen via collagen/ACP self-assembly. J. Mater. Sci. Technol. 2019, 35, 1894–1905. [Google Scholar] [CrossRef]
- Kuttappan, S.; Mathew, D.; Nair, M.B. Biomimetic composite scaffolds containing bioceramics and collagen/gelatin for bone tissue engineering—A mini review. Int. J. Biol. Macromol. 2016, 93, 1390–1401. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, C.; Bruenler, R.; Kreschel, C.; Kruppke, B.; Bernhardt, R.; Aibibu, D.; Cherif, C.; Wiesmann, H.P.; Hanke, T. Bioinspired calcium phosphate mineralization on Net-Shape-Nonwoven chitosan scaffolds stimulates human bone marrow stromal cell differentiation. Biomed. Mater. 2019, 14, 045017. [Google Scholar] [CrossRef] [PubMed]
- Cojocaru, F.D.; Balan, V.; Popa, M.I.; Lobiuc, A.; Antoniac, A.; Antoniac, I.V.; Verestiuc, L. Biopolymers-Calcium phosphates composites with inclusions of magnetic nanoparticles for bone tissue engineering. Int. J. Biol. Macromol. 2019, 125, 612–620. [Google Scholar] [CrossRef]
- Lin, C.C.; Fu, S.J.; Lin, Y.C.; Yang, I.K.; Gu, Y. Chitosan-coated electrospun PLA fibers for rapid mineralization of calcium phosphate. Int. J. Biol. Macromol. 2014, 68, 39–47. [Google Scholar] [CrossRef]
- Cao, C.Y.; Mei, M.L.; Li, Q.L.; Lo, E.C.; Chu, C.H. Methods for biomimetic remineralization of human dentine: A systematic review. Int. J. Mol. Sci. 2015, 16, 4615–4627. [Google Scholar] [CrossRef]
- Xiao, Z.; Que, K.; Wang, H.; An, R.; Chen, Z.; Qiu, Z.; Lin, M.; Song, J.; Yang, J.; Lu, D.; et al. Rapid biomimetic remineralization of the demineralized enamel surface using nano-particles of amorphous calcium phosphate guided by chimaeric peptides. Dent. Mater. 2017, 33, 1217–1228. [Google Scholar] [CrossRef]
- Simeonov, M.; Gussiyska, A.; Mironova, J.; Nikolova, D.; Apostolov, A.; Sezanova, K.; Dyulgerova, E.; Vassileva, E. Novel hybrid chitosan/calcium phosphates microgels for remineralization of demineralized enamel - A model study. Eur. Polym. J. 2019, 119, 14–21. [Google Scholar] [CrossRef]
- Li, J.; Yang, J.; Li, J.; Chen, L.; Liang, K.; Wu, W.; Chen, X.; Li, J. Bioinspired intrafibrillar mineralization of human dentine by PAMAM dendrimer. Biomaterials 2013, 34, 6738–6747. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.; Mao, C.; Gu, T.; Pan, H.; Shao, C.; Sun, J.; Chen, C.; Tang, R.; Gu, X. Phosphorylated chitosan to promote biomimetic mineralization of type I collagen as a strategy for dentin repair and bone tissue engineering. New J. Chem. 2019, 43, 2002–2010. [Google Scholar] [CrossRef]
- Gilpin, A.; Yang, Y. Decellularization Strategies for Regenerative Medicine: From Processing Techniques to Applications. BioMed Res. Int. 2017, 2017, 9831534. [Google Scholar] [CrossRef]
- Deepthi, S.; Venkatesan, J.; Kim, S.K.; Bumgardner, J.D.; Jayakumar, R. An overview of chitin or chitosan/nano ceramic composite scaffolds for bone tissue engineering. Int. J. Biol. Macromol. 2016, 93, 1338–1353. [Google Scholar] [CrossRef] [PubMed]
| Chitosan or Its Derivatives | Composite Forms | Minerals | Other Organic/Inorganic Components | Preparation Techniques of Chitosan Template | Methods of Biomimetic Mineralization | Important Properties | Reference |
|---|---|---|---|---|---|---|---|
| Chitosan | Nanofibers | HAP | - | Electrospinning | Alternate soaking of WCM | Promoted osteogenic differentiation by inducing ossification | [56] |
| Carboxymethyl chitosan | Nanofibers | HAP | - | Electrospinning | Soaking in 5 times SBF solution | Increased the ALP activity, promoted the gene expression level of Runx2 and ALP, promoted new bone formation and maturation | [59] |
| Chitosan | Porous scaffolds | DCPD, HAP | - | Needle-punching process | dip-coating method and in situ precipitation by WCM | Excellent biocompatibility, osteoinductivity and mechanical properties | [44] |
| Chitosan | Membranes | HAP | GO | Chemical conjugation with GO | Soaking in 5 times SBF solution | Influenced osteoblastic cell differentiation, mineralization, and cell growth | [95] |
| Chitosan | Aerogel networks | HAP | RGO | Functionalize RGO | Soaking in 1.5 times SBF solution | Exhibited relatively higher rate of cell proliferation, osteogenic differentiation and osteoid matrix formation | [113] |
| Carboxymethyl chitosan | Nanocomplexes | ACP | Collagen | Dissolved in water | PILP method | Promoted the proliferation and differentiation of mouse preosteoblasts, accelerated the regeneration of bone in the defects of rat calvaria bone | [83] |
| Chitosan | Porous scaffolds | nHAP | Collagen, PLA | Emulsion-crosslinking | WCM | Improved the mechanical properties and the formation of crystals in SBF, had good biocompatibility, maintained the cell growth | [72] |
| Chitosan | Core-shell structured nanofibers | HAP | Gelatin | Coaxial electrospinning technique | WCM | Enhanced osteoblast cell proliferation | [91] |
| Chitosan | Fibers | HAP | Gelatin | Net-Shape-Nonwoven (NSN) technique | Double migration technique | Improved attachment, proliferation, and differentiation of hBMSC | [116] |
| Chitosan | Nanofibers | HAP | Cellulose, phosvitin | LBL self-assembly technique | Soaking in 1.5 times SBF solution | excellent cytocompatibility, as well as good performance of cell adhesion and spreading | [80] |
| Chitosan | Fibers | HAP | PLA | Modification on electrospun PLA nanofiber | Soaking in 10 times SBF solution | Mimicked structural, compositional, and biological functions of native bone | [118] |
| Chitosan | Hydrogel | HAP, DCPD | PEG | Chemical crosslinking with PEG | Alternate soaking of WCM | Induced excellent cell adhesion ability | [73] |
| Chitosan | Porous scaffolds | HAP | Silk fibroin | Freeze drying | Alternate soaking of WCM | Good mechanical property, promoted early cell attachment and enhanced osteogenic differentiation | [92] |
| Chitosan | Porous scaffolds | nHAP | ALP | Freeze drying | ALP enzyme-induced mineralization method | promoted the osteogenic differentiation of pre-osteoblasts in vitro and demonstrated excellent tissue integration in vivo | [64] |
| Chitosan | Thermosensitive hydrogels | CaP | ALP | Gelation | ALP enzyme-induced mineralization method | Promoted mineralization, may be suitable materials for bone replacement. | [98] |
| Chitosan | Hybrid scaffolds | Silica | - | Freeze drying | Sol-gel process | No cytotoxicity, excellent in vitro bone bioactivity | [85] |
| N-guanidinium-chitosan acetate | Hybrid scaffolds | Silica | - | Freeze drying | Sol-gel process | Acted as versatile templates for biomineralization, inducing the formation of HAP | [86] |
| Chitosan or Its Derivatives | Composite Forms | Minerals | Other Organic/Inorganic Components | Preparation Techniques of Chitosan Template | Methods of Biomimetic Mineralization | Important Properties | Reference |
|---|---|---|---|---|---|---|---|
| Carboxymethyl chitosan | Nano-complexes | ACP | Chimaeric peptides | Dissolved in water | PILP method, immersing in AS solution | Promoted rapid biomimetic remineralization of the demineralized enamel, formed well-organized enamel-like crystals | [120] |
| Chitosan | Coating | Carbonate-substituted B-type HAP | Emdogain | Gelation | Immersing in AS solution | Provided highly organized enamel-like structure for teeth remineralization | [75] |
| Chitosan | Hybrid microgels | Amorphous CaP and poorly crystalline carbonated B- type HAP | - | Ionotropic gelation | in situ precipitation by WCM | Owned several advantages as remineralizing agent, including bio-adhesiveness, antimicrobial properties as well as continuous supply of calcium and phosphate ions to ensure the successful remineralization of the model initial caries lesions | [121] |
| Chitosan | Coating | B-type Ca-deficient HAP | Agarose | Gelation | Immersing in AS solution | Showed a benefic effect on remineralization of etched dentine | [74] |
| Carboxymethyl chitosan | Nanocomplexes | ACP | Collagen | Dissolved in water | PILP method, immersing in SBF solution | Partially remineralized the completely demineralized dentine in an in vitro tooth model of deep caries, a potential indirect pulp capping material | [65] |
| Phosphorylated chitosan | Fibers | ACP | Collagen | Chemical modification on collagen fibers | PILP method | Promoted intrafibrillar mineralization of collagen, achieved remineralization of calcium-depleted dentin within 96 h | [123] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, D.; Ren, Q.; Li, Z.; Zhang, L. Chitosan-Based Biomimetically Mineralized Composite Materials in Human Hard Tissue Repair. Molecules 2020, 25, 4785. https://doi.org/10.3390/molecules25204785
Hu D, Ren Q, Li Z, Zhang L. Chitosan-Based Biomimetically Mineralized Composite Materials in Human Hard Tissue Repair. Molecules. 2020; 25(20):4785. https://doi.org/10.3390/molecules25204785
Chicago/Turabian StyleHu, Die, Qian Ren, Zhongcheng Li, and Linglin Zhang. 2020. "Chitosan-Based Biomimetically Mineralized Composite Materials in Human Hard Tissue Repair" Molecules 25, no. 20: 4785. https://doi.org/10.3390/molecules25204785
APA StyleHu, D., Ren, Q., Li, Z., & Zhang, L. (2020). Chitosan-Based Biomimetically Mineralized Composite Materials in Human Hard Tissue Repair. Molecules, 25(20), 4785. https://doi.org/10.3390/molecules25204785







