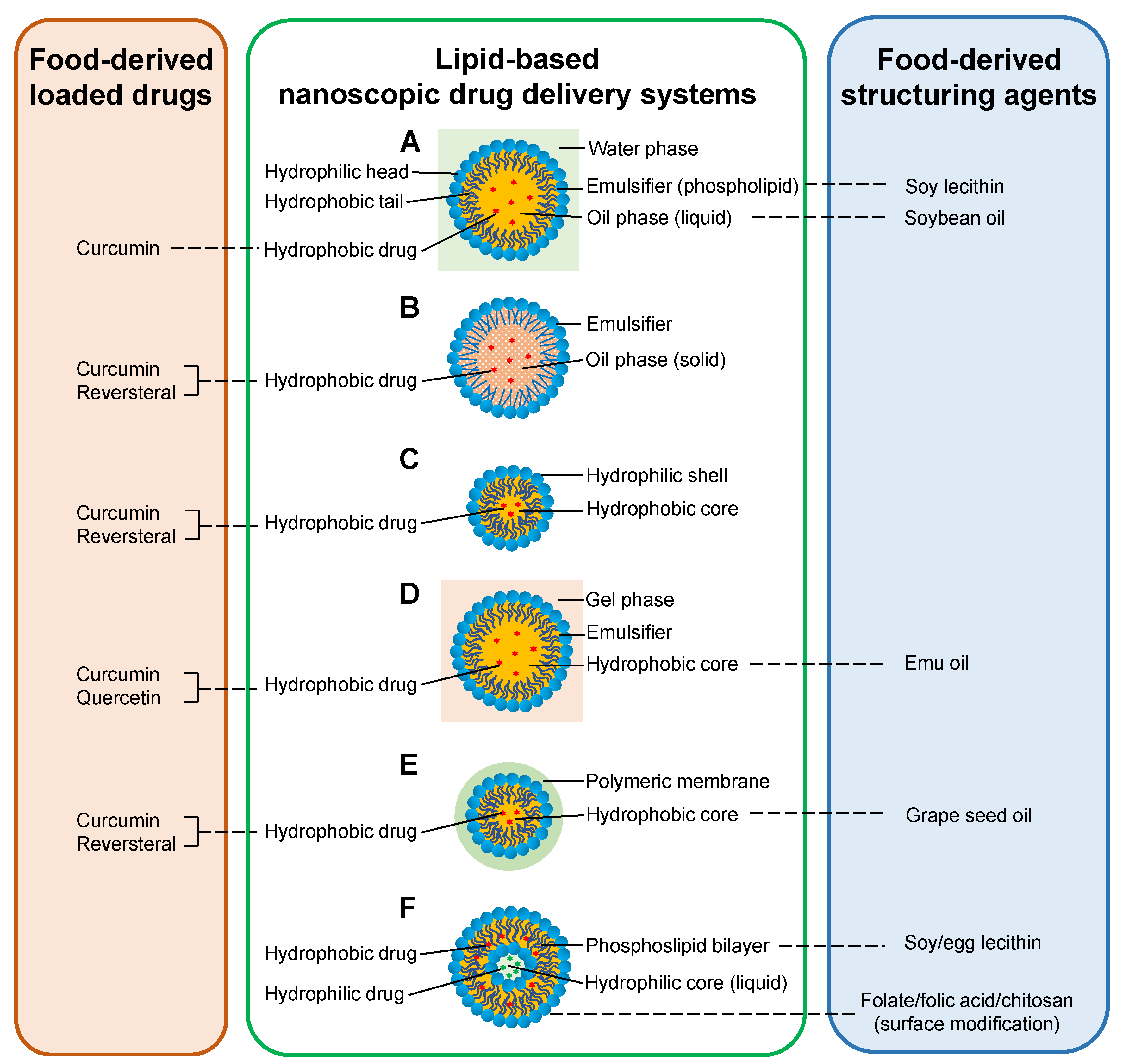
Food-Derived Nanoscopic Drug Delivery Systems for Treatment of Rheumatoid Arthritis
Abstract
1. Introduction
2. Food Components as Delivered Drugs to Treat RA
2.1. Polyphenols
2.1.1. Curcumin
2.1.2. Resveratrol
2.2. Flavonoids
2.2.1. Quercetin
2.2.2. Hesperidin
3. Food Components as Structuring Agents of Anti-RA Nanocarriers
3.1. Soybean Oil
3.2. Grape Seed Oil
3.3. Emu Oil
3.4. Lecithin
3.4.1. Soy Lecithin
3.4.2. Egg Lecithin
3.5. Chitosan
3.6. Folate and Folic Acid
3.7. Black Pepper
4. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- McInnes, I.; Schett, G. The Pathogenesis of Rheumatoid Arthritis. New Engl. J. Med. 2011, 365, 2205–2219. [Google Scholar] [CrossRef]
- McInnes, I.; Schett, G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet 2017, 389, 2328–2337. [Google Scholar] [CrossRef]
- Dougados, M. Comorbidities in rheumatoid arthritis. Curr. Opin. Rheumatol. 2016, 28, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Strehl, C.; Van Der Goes, M.C.; Bijlsma, J.W.J.; Jacobs, J.W.G.; Buttgereit, F. Glucocorticoid-targeted therapies for the treatment of rheumatoid arthritis. Expert Opin. Investig. Drugs 2017, 26, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Möller, B.; Pruijm, M.; Adler, S.; Scherer, A.; Villiger, P.M.; Finckh, A. Chronic NSAID use and long-term decline of renal function in a prospective rheumatoid arthritis cohort study. Ann. Rheum. Dis. 2013, 74, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Schett, G.; Emery, P.; Tanaka, Y.; Burmester, G.; Pisetsky, D.S.; Naredo, E.; Fautrel, B.; Van Vollenhoven, R. Tapering biologic and conventional DMARD therapy in rheumatoid arthritis: Current evidence and future directions. Ann. Rheum. Dis. 2016, 75, 1428–1437. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Gao, Y.; Chen, H.; Zeng, D.; Li, Y.; Zheng, Y.; Li, F.; Ji, X.; Wang, X.; Chen, F.; et al. Engineering Inorganic Nanoemulsions/Nanoliposomes by Fluoride-Silica Chemistry for Efficient Delivery/Co-Delivery of Hydrophobic Agents. Adv. Funct. Mater. 2012, 22, 1586–1597. [Google Scholar] [CrossRef]
- He, W.; Lu, Y.; Qi, J.; Chen, L.; Hu, F.; Wu, W. Nanoemulsion-templated shell-crosslinked nanocapsules as drug delivery systems. Int. J. Pharm. 2013, 445, 69–78. [Google Scholar] [CrossRef]
- Pham, C.T.N. Nanotherapeutic approaches for the treatment of rheumatoid arthritis. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2011, 3, 607–619. [Google Scholar] [CrossRef]
- Shang, W.; Zhao, L.-J.; Dong, X.-L.; Zhao, Z.-M.; Li, J.; Zhang, B.-B.; Cai, H. Curcumin inhibits osteoclastogenic potential in PBMCs from rheumatoid arthritis patients via the suppression of MAPK/RANK/c-Fos/NFATc1 signaling pathways. Mol. Med. Rep. 2016, 14, 3620–3626. [Google Scholar] [CrossRef]
- Shaikh, J.; Ankola, D.; Beniwal, V.; Singh, D.; Kumar, M.N.V.R. Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur. J. Pharm. Sci. 2009, 37, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Sonneville-Aubrun, O.; Simonnet, J.-T.; L’Alloret, F. Nanoemulsions: A new vehicle for skincare products. Adv. Colloid Interface Sci. 2004, 108, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Zheng, Z.; Sun, Y.; Liu, Z.; Zhang, M.; Li, C. The effect of curcumin and its nanoformulation on adjuvant-induced arthritis in rats. Drug Des. Dev. Ther. 2015, 9, 4931–4942. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, W.; Mäder, K. Solid lipid nanoparticles: Production, characterization and applications. Adv. Drug Deliv. Rev. 2012, 64, 83–101. [Google Scholar] [CrossRef]
- Thakkar, H.; Sharma, R.K.; Murthy, R.S.R. Enhanced retention of celecoxib-loaded solid lipid nanoparticles after intra-articular administration. Drugs R&D 2007, 8, 275–285. [Google Scholar] [CrossRef]
- Mei, L.; Zhang, Z.; Zhao, L.; Huang, L.; Yang, X.-L.; Tang, J.; Feng, S.-S. Pharmaceutical nanotechnology for oral delivery of anticancer drugs. Adv. Drug Deliv. Rev. 2013, 65, 880–890. [Google Scholar] [CrossRef]
- Luo, Y.; Chen, D.; Ren, L.; Zhao, X.; Qin, J. Solid lipid nanoparticles for enhancing vinpocetine’s oral bioavailability. J. Control. Release 2006, 114, 53–59. [Google Scholar] [CrossRef]
- Kakkar, V.; Singh, S.; Singla, D.; Kaur, I.P. Exploring solid lipid nanoparticles to enhance the oral bioavailability of curcumin. Mol. Nutr. Food Res. 2010, 55, 495–503. [Google Scholar] [CrossRef]
- Kaur, I.P.; Bhandari, R.; Bhandari, S.; Kakkar, V. Potential of solid lipid nanoparticles in brain targeting. J. Control. Release 2008, 127, 97–109. [Google Scholar] [CrossRef]
- Arora, R.; Kuhad, A.; Kaur, I.; Chopra, K. Curcumin loaded solid lipid nanoparticles ameliorate adjuvant-induced arthritis in rats. Eur. J. Pain 2014, 19, 940–952. [Google Scholar] [CrossRef]
- Torchilin, V.P. Micellar Nanocarriers: Pharmaceutical Perspectives. Pharm. Res. 2006, 24, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Li, S.-D.; Huang, L. Pharmacokinetics and Biodistribution of Nanoparticles. Mol. Pharm. 2008, 5, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Cagel, M.; Tesan, F.C.; Bernabeu, E.; Salgueiro, M.J.; Zubillaga, M.B.; Moretton, M.A.; Chiapetta, D.A. Polymeric mixed micelles as nanomedicines: Achievements and perspectives. Eur. J. Pharm. Biopharm. 2017, 113, 211–228. [Google Scholar] [CrossRef] [PubMed]
- Javadi, M.; Haghighian, H.K.; Goodarzy, S.; Abbasi, M.; Nassiri-Asl, M. Effect of curcumin nanomicelle on the clinical symptoms of patients with rheumatoid arthritis: A randomized, double-blind, controlled trial. Int. J. Rheum. Dis. 2019, 22, 1857–1862. [Google Scholar] [CrossRef] [PubMed]
- Gannu, R.; Palem, C.R.; Yamsani, V.V.; Yamsani, S.K.; Yamsani, M.R. Enhanced bioavailability of lacidipine via microemulsion based transdermal gels: Formulation optimization, ex vivo and in vivo characterization. Int. J. Pharm. 2010, 388, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Naz, Z.; Ahmad, F.J. Curcumin-loaded colloidal carrier system: Formulation optimization, mechanistic insight, ex vivo and in vivo evaluation. Int. J. Nanomedicine 2015, 10, 4293–4307. [Google Scholar] [CrossRef] [PubMed]
- Al-Rohaimi, A.H. Comparative anti-infammatory potential of crystalline and amorphous nano curcumin in topical drug delivery. J. Oleo Sci. 2015, 64, 27–40. [Google Scholar] [CrossRef]
- Jeengar, M.K.; Rompicharla, S.V.K.; Shrivastava, S.; Chella, N.; Shastri, N.R.; Naidu, V.G.M.; Sistla, R. Emu oil based nano-emulgel for topical delivery of curcumin. Int. J. Pharm. 2016, 506, 222–236. [Google Scholar] [CrossRef]
- Mora-Huertas, C.E.; Fessi, H.; Elaissari, A. Polymer-based nanocapsules for drug delivery. Int. J. Pharm. 2010, 385, 113–142. [Google Scholar] [CrossRef]
- Coradini, K.; Lima, F.O.; Oliveira, C.; Chaves, P.; Athayde, M.; Carvalho, L.; Beck, R. Co-encapsulation of resveratrol and curcumin in lipid-core nanocapsules improves their in vitro antioxidant effects. Eur. J. Pharm. Biopharm. 2014, 88, 178–185. [Google Scholar] [CrossRef]
- Coradini, K.; Friedrich, R.B.; Fonseca, F.N.; Vencato, M.S.; De Andrade, D.F.; Oliveira, C.M.; Battistel, A.P.; Guterres, S.S.; Da Rocha, M.I.U.; Pohlmann, A.R.; et al. A novel approach to arthritis treatment based on resveratrol and curcumin co-encapsulated in lipid-core nanocapsules: In vivo studies. Eur. J. Pharm. Sci. 2015, 78, 163–170. [Google Scholar] [CrossRef] [PubMed]
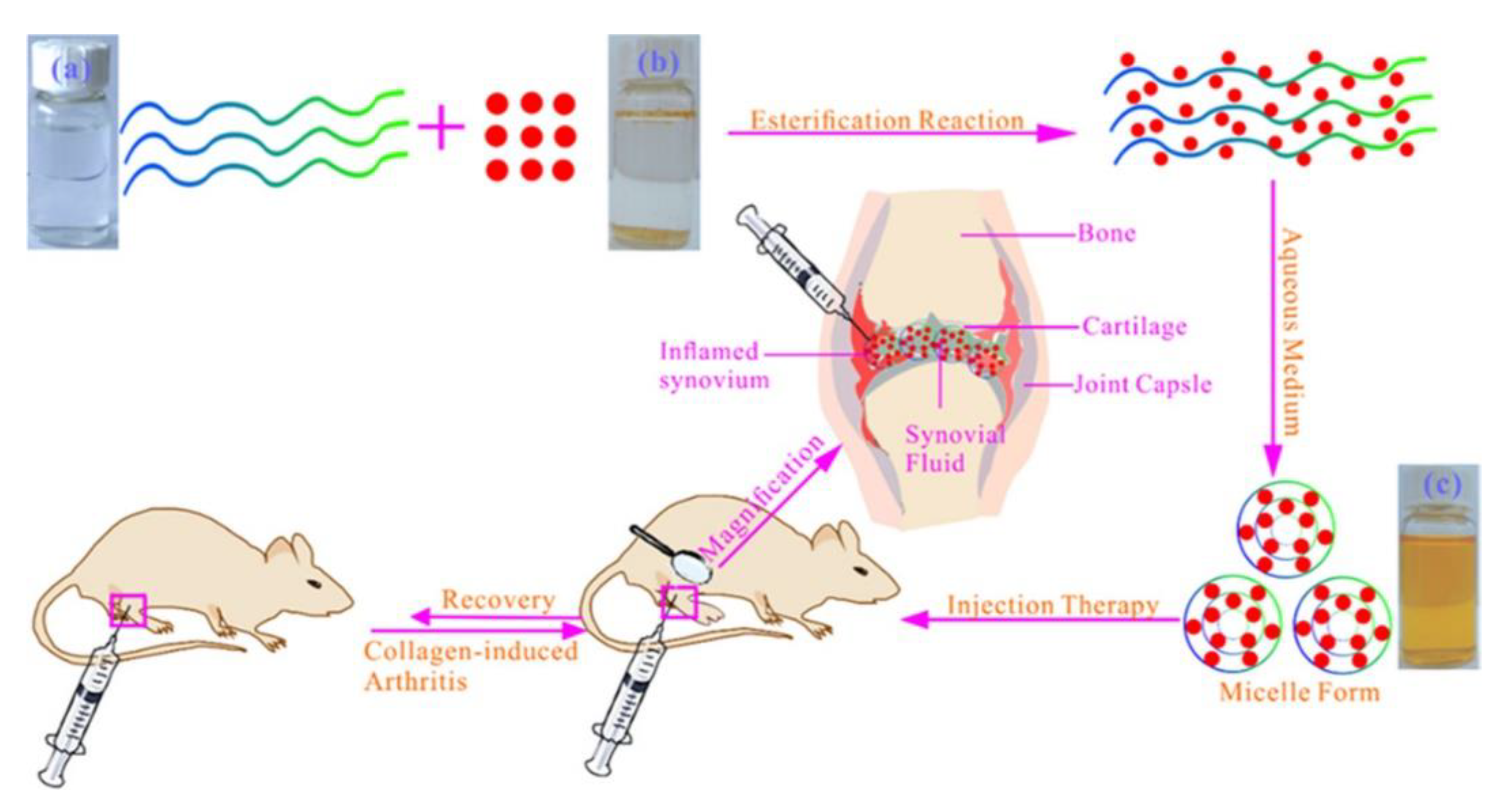
- Fan, Z.; Li, J.; Liu, J.; Jiao, H.; Liu, B. Anti-Inflammation and Joint Lubrication Dual Effects of a Novel Hyaluronic Acid/Curcumin Nanomicelle Improve the Efficacy of Rheumatoid Arthritis Therapy. ACS Appl. Mater. Interfaces 2018, 10, 23595–23604. [Google Scholar] [CrossRef]
- Cheon, Y.-H.; Kim, H.-O.; Suh, Y.-S.; Hur, J.H.; Jo, W.; Lim, H.-S.; Hah, Y.-S.; Sung, M.J.; Kwon, D.Y.; Lee, S.-I. Inhibitory Effects for Rheumatoid Arthritis of Dietary Supplementation with Resveratrol in Collagen-induced Arthritis. J. Rheum. Dis. 2015, 22, 93. [Google Scholar] [CrossRef]
- Ogando, J.; Tardáguila, M.; Díaz-Alderete, A.; Usategui, A.; Miranda-Ramos, V.; Martínez-Herrera, D.J.; De La Fuente, L.; García-León, M.J.; Moreno, M.C.; Escudero, S.; et al. Notch-regulated miR-223 targets the aryl hydrocarbon receptor pathway and increases cytokine production in macrophages from rheumatoid arthritis patients. Sci. Rep. 2016, 6, 20223. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, T.; Nguyen, N.T.; Nakahama, T.; Nguyen, C.H.; Tran, T.T.; Le, V.S.; Chu, H.H. Aryl hydrocarbon receptor antagonism and its role in rheumatoid arthritis. J. Exp. Pharmacol. 2015, 7, 29–35. [Google Scholar] [CrossRef]
- Almonte-Becerril, M.; Fernandez-Rodriguez, J.A.; Ramil-Gomez, O.; Riveiro-Naveira, R.R.; Hermida-Carballo, L.; Concha, A.; Vela-Anero, A.; Viñas, S.; Blanco, F.J.; Lopez-Armada, M.J. Resveratrol attenuates synovial hyperplasia in an acute antigen-induced arthritis model by augmenting autophagy and decreasing angiogenesis. Osteoarthr. Cartil. 2017, 25, S90–S91. [Google Scholar] [CrossRef]
- Kamel, R.; Abbas, H.; Shaffie, N.M. Development and evaluation of PLA-coated co-micellar nanosystem of Resveratrol for the intra-articular treatment of arthritis. Int. J. Pharm. 2019, 569, 118560. [Google Scholar] [CrossRef]
- Chen, X.; Zhu, X.; Ma, L.; Lin, A.; Gong, Y.; Yuan, G.; Liu, J. A core-shell structure QRu-PLGA-RES-DS NP nanocomposite with photothermal response-induced M2 macrophage polarization for rheumatoid arthritis therapy. Nanoscale 2019, 11, 18209–18223. [Google Scholar] [CrossRef]
- Harnly, J.M.; Doherty, R.F.; Beecher, G.R.; Holden, J.M.; Haytowitz, D.B.; Bhagwat, S.; Gebhardt, S. Flavonoid content of U.S. fruits, vegetables, and nuts. J. Agric. Food Chem. 2006, 54, 9966–9977. [Google Scholar] [CrossRef]
- Vicentini, F.T.M.C.; He, T.; Shao, Y.; Fonseca, M.J.V.; Verri, W.A.J.; Fisher, G.J.; Xu, Y. Quercetin inhibits UV irradiation-induced inflammatory cytokine production in primary human keratinocytes by suppressing NF-κB pathway. J. Dermatol. Sci. 2011, 61, 162–168. [Google Scholar] [CrossRef]
- Jackson, J.K.; Higo, T.; Hunter, W.L.; Burt, H.M. The antioxidants curcumin and quercetin inhibit inflammatory processes associated with arthritis. Inflamm. Res. 2006, 55, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Almeida, A.F.; Borge, G.I.A.; Piskula, M.; Tudose, A.; Tudoreanu, L.; Valentová, K.; Williamson, G.; Santos, C.N. Bioavailability of quercetin in humans with a focus on interindividual variation. Compr. Rev. Food Sci. Food Saf. 2018, 17, 714–731. [Google Scholar] [CrossRef]
- Jeyadevi, R.; Sivasudha, T.; Rameshkumar, A.; Ananth, D.A.; Aseervatham, G.S.B.; Kumaresan, K.; Kumar, L.D.; Jagadeeswari, S.; Renganathan, R. Enhancement of anti arthritic effect of quercetin using thioglycolic acid-capped cadmium telluride quantum dots as nanocarrier in adjuvant induced arthritic Wistar rats. Colloids Surf. B. Biointerfaces 2013, 112, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, J.P.; Mahajan, H.S.; Surana, S.J. Quercetin loaded nanoemulsion-based gel for rheumatoid arthritis: In vivo and in vitro studies. Biomed. Pharmacother. 2019, 112, 108622. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, V.; Krithica, N.; Madhan, B.; Sehgal, P.; Venkatachalam, N. Formulation and Evaluation of Quercetin Polycaprolactone Microspheres for the Treatment of Rheumatoid Arthritis. J. Pharm. Sci. 2011, 100, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Li, J.; Cai, L.; Hu, C.-M.; Zhang, L. Suppression of adjuvant arthritis by hesperidin in rats and its mechanisms. J. Pharm. Pharmacol. 2008, 60, 221–228. [Google Scholar] [CrossRef]
- Umar, S.; Kumar, A.; Sajad, M.; Zargan, J.; Ansari, M.; Ahmad, S.; Katiyar, C.K.; Khan, H.A. Hesperidin inhibits collagen-induced arthritis possibly through suppression of free radical load and reduction in neutrophil activation and infiltration. Rheumatol. Int. 2012, 33, 657–663. [Google Scholar] [CrossRef]
- Rao, K.; Aziz, S.; Roome, T.; Razzak, A.; Sikandar, B.; Jamali, K.S.; Imran, M.; Jabri, T.; Shah, M.R. Gum acacia stabilized silver nanoparticles based nano-cargo for enhanced anti-arthritic potentials of hesperidin in adjuvant induced arthritic rats. Artif. Cells Nanomed. Biotechnol. 2018, 46, 597–607. [Google Scholar] [CrossRef]
- US Department of Agriculture USDA National Nutrient Database for Standard Reference, Release 28 (Slightly revised). Available online: http://www.ars.usda.gov/ba/bhnrc/ndl (accessed on 1 June 2020).
- Fasina, O.O.; Hallman, H.; Craig-Schmidt, M.; Clements, C. Predicting temperature-dependence viscosity of vegetable oils from fatty acid composition. J. Am. Oil Chem. Soc. 2006, 83, 899–903. [Google Scholar] [CrossRef]
- Anuchapreeda, S.; Fukumori, Y.; Okonogi, S.; Ichikawa, H. Preparation of Lipid Nanoemulsions Incorporating Curcumin for Cancer Therapy. J. Nanotechnol. 2011, 2012, 1–11. [Google Scholar] [CrossRef]
- Moghaddasi, F.; Housaindokht, M.R.; Darroudi, M.; Bozorgmehr, M.R.; Sadeghi, A. Soybean oil-based nanoemulsion systems in absence and presence of curcumin: Molecular dynamics simulation approach. J. Mol. Liq. 2018, 264, 242–252. [Google Scholar] [CrossRef]
- Fang, J.-Y.; Zhang, L.-W.; Al-Suwayeh, S.A.; Hung, C.-F.; Chen, C.-C. Oil components modulate the skin delivery of 5-aminolevulinic acid and its ester prodrug from oil-in-water and water-in-oil nanoemulsions. Int. J. Nanomed. 2011, 6, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Mou, D.; Chen, H.; Du, D.; Mao, C.; Wan, J.; Xu, H.; Yang, X. Hydrogel-thickened nanoemulsion system for topical delivery of lipophilic drugs. Int. J. Pharm. 2008, 353, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Gref, R.; Couvreur, P.; Torchilin, V.P. Nanocapsules: Preparation, Characterization and Therapeutic Applications. Nanoparticulates Drug Carr. 2006, 255, 255–276. [Google Scholar] [CrossRef]
- Ferreira, C.D.; Nunes, I.L. Oil nanoencapsulation: Development, application, and incorporation into the food market. Nanoscale Res. Lett. 2019, 14, 9. [Google Scholar] [CrossRef]
- Kaki, S.S.; Ravinder, T.; Rao, B.V.S.K.; Chakrabarti, P.P.; Prasad, R.B.N. Isolation and characterization of oil from fatty tissues of emu birds farmed in India. J. Lipid Sci. Technol. 2013, 45, 13–19. [Google Scholar]
- Simard, M.; Julien, P.; Fradette, J.; Pouliot, R. Modulation of the lipid profile of reconstructed skin substitutes after essential fatty acid supplementation affects testosterone permeability. Cells 2019, 8, 1142. [Google Scholar] [CrossRef]
- Jeengar, M.K.; Shrivastava, S.; Nair, K.; Singareddy, S.R.; Putcha, U.K.; Talluri, M.V.N.K.; Naidu, V.G.M.; Sistla, R. Improvement of bioavailability and anti-inflammatory potential of curcumin in combination with emu oil. Inflammation 2014, 37, 2139–2155. [Google Scholar] [CrossRef]
- Asomaning, J.; Curtis, J.M. Enzymatic modification of egg lecithin to improve properties. Food Chem. 2017, 220, 385–392. [Google Scholar] [CrossRef]
- Inoue, M.; Senoo, N.; Sato, T.; Nishimura, Y.; Nakagawa, T.; Miyoshi, N.; Goda, T.; Morita, A.; Miura, S. Effects of the dietary carbohydrate–fat ratio on plasma phosphatidylcholine profiles in human and mouse. J. Nutr. Biochem. 2017, 50, 83–94. [Google Scholar] [CrossRef]
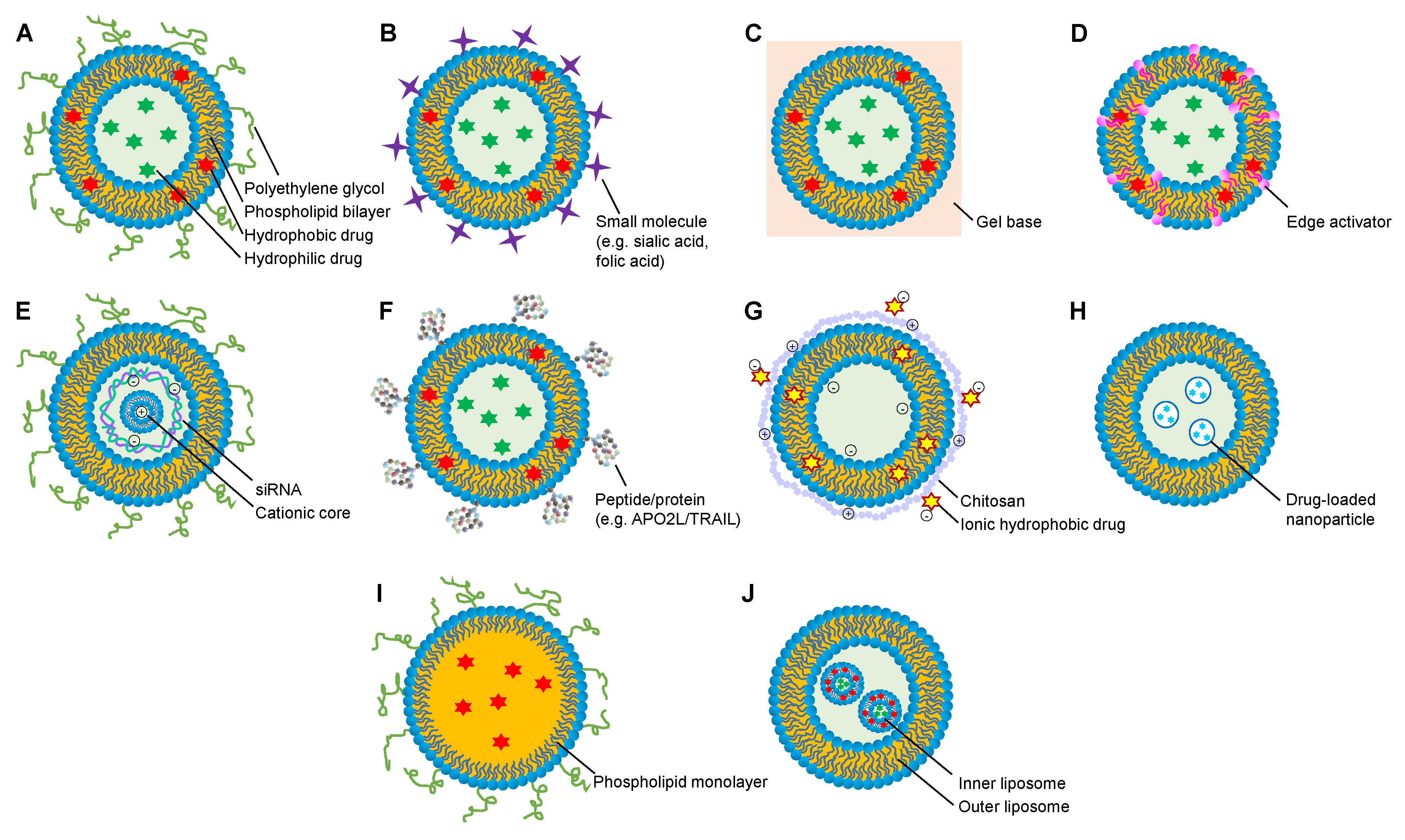
- Daraee, H.; Eatemadi, A.; Kouhi, M.; Alimirzalu, S.; Akbarzadeh, A. Application of liposomes in medicine and drug delivery. Artif. Cells Nanomed. Biotechnol. 2014, 44, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Moghimipour, E.; Handali, S. Utilization of thin film method for preparation of celecoxib loaded liposomes. Adv. Pharm. Bull. 2012, 2, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Li, H.M.; Lan, S.B.; Chang, M.X. Effects of transdermal liposome preparation of triptolide on arthritis induced by collagen II. Chin. Tradit. Herb. Drugs 2013, 44, 199–202. [Google Scholar] [CrossRef]
- Albiero, L.R.; De Andrade, M.F.; Marchi, L.F.; Landi-Librandi, A.P.; De Figueiredo-Rinhel, A.S.G.; Carvalho, C.A.; Kabeya, L.M.; De Oliveira, R.D.R.; Azzolini, A.E.C.S.; Pupo, M.T.; et al. Immunomodulating action of the 3-phenylcoumarin derivative 6,7-dihydroxy-3-[3′,4′-methylenedioxyphenyl]-coumarin in neutrophils from patients with rheumatoid arthritis and in rats with acute joint inflammation. Inflamm. Res. 2019, 69, 115–130. [Google Scholar] [CrossRef] [PubMed]
- Avnir, Y.; Ulmansky, R.; Wasserman, V.; Broyer, M.; Barenholz, Y.; Naparstek, Y.; Even-Chen, S. Amphipathic weak acid glucocorticoid prodrugs remote-loaded into sterically stabilized nanoliposomes evaluated in arthritic rats and in a Beagle dog: A novel approach to treating autoimmune arthritis. Arthritis Rheum. 2007, 58, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Ulmansky, R.; Turjeman, K.; Baru, M.; Katzavian, G.; Harel, M.; Sigal, A.; Naparstek, Y.; Barenholz, Y. Glucocorticoids in nano-liposomes administered intravenously and subcutaneously to adjuvant arthritis rats are superior to the free drugs in suppressing arthritis and inflammatory cytokines. J. Control. Release 2012, 160, 299–305. [Google Scholar] [CrossRef]
- Björkman, L.; Christenson, K.; Davidsson, L.; Mårtensson, J.; Amirbeagi, F.; Welin, A.; Forsman, H.; Karlsson, A.; Dahlgren, C.; Bylund, J. Neutrophil recruitment to inflamed joints can occur without cellular priming. J. Leukoc. Boil. 2018, 105, 1123–1130. [Google Scholar] [CrossRef]
- Zhang, T.; She, Z.; Huang, Z.; Li, J.; Luo, X.; Deng, Y. Application of sialic acid/polysialic acid in the drug delivery systems. Asian J. Pharm. Sci. 2014, 9, 75–81. [Google Scholar] [CrossRef]
- Hu, L.; Luo, X.; Zhou, S.; Zhu, J.; Xiao, M.; Li, C.; Zheng, H.; Qiu, Q.; Lai, C.; Liu, X.; et al. Neutrophil-Mediated Delivery of Dexamethasone Palmitate-Loaded Liposomes Decorated with a Sialic Acid Conjugate for Rheumatoid Arthritis Treatment. Pharm. Res. 2019, 36, 97. [Google Scholar] [CrossRef]
- Srinath, P.; Vyas, S.P.; Diwan, P.V. Preparation and Pharmacodynamic Evaluation of Liposomes of Indomethacin. Drug Dev. Ind. Pharm. 2000, 26, 313–321. [Google Scholar] [CrossRef]
- Chen, G.; Hao, B.; Ju, D.; Liu, M.; Zhao, H.; Du, Z.; Xia, J. Pharmacokinetic and pharmacodynamic study of triptolide-loaded liposome hydrogel patch under microneedles on rats with collagen-induced arthritis. Acta Pharm. Sin. B 2015, 5, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-K.; Zeb, A.; Qureshi, O.S.; Kim, H.-S.; Cha, J.-H.; Kim, H.-S. Improved skin permeation of methotrexate via nanosized ultradeformable liposomes. Int. J. Nanomed. 2016, 11, 3813–3824. [Google Scholar] [CrossRef] [PubMed]
- Zeb, A.; Qureshi, O.S.; Yu, C.-H.; Akram, M.; Kim, H.-S.; Kim, M.-S.; Kang, J.-H.; Majid, A.; Chang, S.-Y.; Bae, O.-N.; et al. Enhanced anti-rheumatic activity of methotrexate-entrapped ultradeformable liposomal gel in adjuvant-induced arthritis rat model. Int. J. Pharm. 2017, 525, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Yagi, N.; Manabe, I.; Tottori, T.; Ishihara, A.; Ogata, F.; Kim, J.H.; Nishimura, S.; Fujiu, K.; Oishi, Y.; Itaka, K.; et al. A Nanoparticle System Specifically Designed to Deliver Short Interfering RNA Inhibits Tumor Growth In vivo. Cancer Res. 2009, 69, 6531–6538. [Google Scholar] [CrossRef] [PubMed]
- Komano, Y.; Yagi, N.; Onoue, I.; Kaneko, K.; Miyasaka, N.; Nanki, T. Arthritic Joint-Targeting Small Interfering RNA-Encapsulated Liposome: Implication for Treatment Strategy for Rheumatoid Arthritis. J. Pharmacol. Exp. Ther. 2011, 340, 109–113. [Google Scholar] [CrossRef]
- Lorenzo, M.J.M.; Anel, A.; Sáez, B.; Royo-Cañas, M.; Bosque, A.; Alava, M.A.; Piñeiro, A.; Lasierra, P.; Asín-Ungría, J.; Larrad, L. Rheumatoid synovial fluid T cells are sensitive to APO2L/TRAIL. Clin. Immunol. 2007, 122, 28–40. [Google Scholar] [CrossRef]
- Martinez-Lostao, L.; García-Álvarez, F.; Basañez, G.; Alegre-Aguarón, E.; Desportes, P.; Larrad, L.; Naval, J.; Martinez-Lostao, L.; Anel, A. Liposome-bound APO2L/TRAIL is an effective treatment in a rabbit model of rheumatoid arthritis. Arthritis Rheum. 2010, 62, 2272–2282. [Google Scholar] [CrossRef]
- Sogias, I.A.; Williams, A.; Khutoryanskiy, V.V. Why is Chitosan Mucoadhesive? Biomacromolecules 2008, 9, 1837–1842. [Google Scholar] [CrossRef]
- Dalmoro, A.; Bochicchio, S.; Nasibullin, S.F.; Bertoncin, P.; Lamberti, G.; Barba, A.A.; Moustafine, R.I. Polymer-lipid hybrid nanoparticles as enhanced indomethacin delivery systems. Eur. J. Pharm. Sci. 2018, 121, 16–28. [Google Scholar] [CrossRef]
- Kumar, V.; Leekha, A.; Tyagi, A.; Kaul, A.; Mishra, A.K.; Verma, A.K. Preparation and evaluation of biopolymeric nanoparticles as drug delivery system in effective treatment of rheumatoid arthritis. Pharm. Res. 2017, 34, 654–667. [Google Scholar] [CrossRef]
- Kumar, C.S.; Ashok, R.; Prabu, S.L.; Ruckmani, K. Evaluation of betamethasone sodium phosphate loaded chitosan nanoparticles for anti-rheumatoid activity. IET Nanobiotechnology 2018, 12, 6–11. [Google Scholar] [CrossRef]
- Cui, P.; Qu, F.; Sreeharsha, N.; Sharma, S.; Mishra, A.; Gubbiyappa, S.K. Antiarthritic effect of chitosan nanoparticle loaded with embelin against adjuvant-induced arthritis in Wistar rats. IUBMB Life 2020, 72, 1054–1064. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.; Ahmad, A.; Mishra, R.K.; Raza, S.S.; Khan, R. Zinc Gluconate-Loaded Chitosan Nanoparticles Reduce Severity of Collagen-Induced Arthritis in Wistar Rats. ACS Biomater. Sci. Eng. 2019, 5, 3380–3397. [Google Scholar] [CrossRef]
- Zhang, N.; Wardwell, P.R.; Bader, R.A. In Vitro Efficacy of Polysaccharide-Based Nanoparticles Containing Disease-Modifying Antirheumatic Drugs. Pharm. Res. 2014, 31, 2326–2334. [Google Scholar] [CrossRef]
- Li, X.; Qu, J.; Zhang, T.; He, X.; Jiang, Y.; Chen, J. Nuclear Factor kappa B (NF-κB) Targeted Self-Assembled Nanoparticles Loaded with Methotrexate for Treatment of Rheumatoid Arthritis. Med. Sci. Monit. 2019, 25, 8204–8212. [Google Scholar] [CrossRef]
- Gul, R.; Ahmed, N.; Ullah, N.; Khan, M.I.; Elaissari, A.; Rehman, A.U. Biodegradable Ingredient-Based Emulgel Loaded with Ketoprofen Nanoparticles. AAPS PharmSciTech 2018, 19, 1869–1881. [Google Scholar] [CrossRef]
- Onishi, H.; Isoda, Y.; Matsuyama, M. In vivo evaluation of chondroitin sulfate-glycyl-prednisolone for anti-arthritic effectiveness and pharmacokinetic characteristics. Int. J. Pharm. 2013, 456, 113–120. [Google Scholar] [CrossRef]
- Radivojša, M.; Grabnar, I.; Grabnar, P.A. Thermoreversible in situ gelling poloxamer-based systems with chitosan nanocomplexes for prolonged subcutaneous delivery of heparin: Design and in vitro evaluation. Eur. J. Pharm. Sci. 2013, 50, 93–101. [Google Scholar] [CrossRef]
- Russo, E.; Gaglianone, N.; Baldassari, S.; Parodi, B.; Croce, I.; Bassi, A.; Vernazza, S.; Caviglioli, G. Chitosan-clodronate nanoparticles loaded in poloxamer gel for intra-articular administration. Colloids Surf. B Biointerfaces 2016, 143, 88–96. [Google Scholar] [CrossRef]
- Roman-Blas, J.A.; Jimenez, S.A. NF-κB as a potential therapeutic target in osteoarthritis and rheumatoid arthritis. Osteoarthr. Cartil. 2006, 14, 839–848. [Google Scholar] [CrossRef]
- Wardwell, P.R.; Forstner, M.B.; Bader, R.A. Investigation of the cytokine response to NF-ΚB decoy oligonucleotide coated polysaccharide based nanoparticles in rheumatoid arthritis in vitro models. Arthritis Res. Ther. 2015, 17. [Google Scholar] [CrossRef] [PubMed]
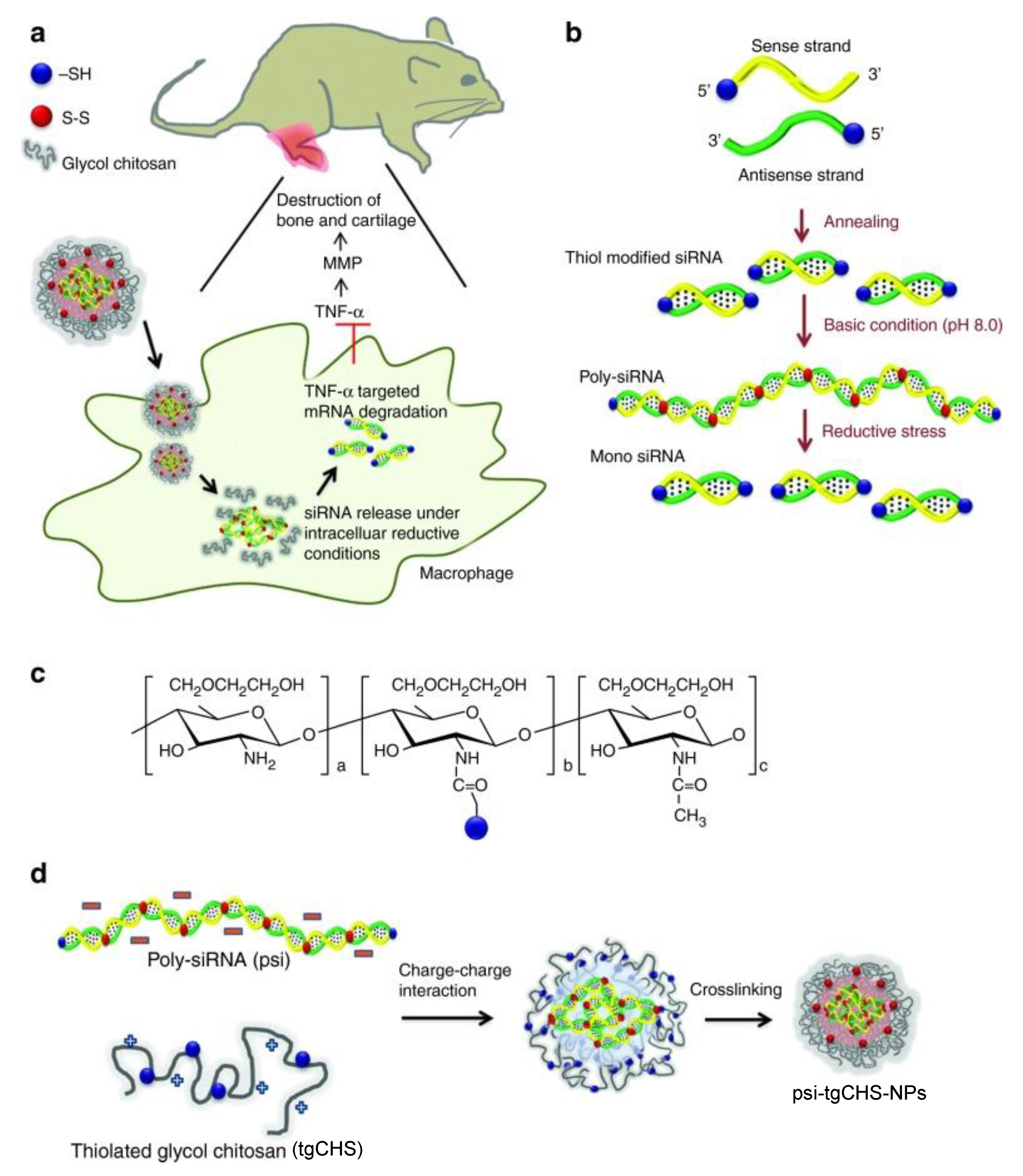
- Lee, S.J.; Lee, A.; Hwang, S.R.; Park, J.-S.; Jang, J.; Huh, M.S.; Joo-Yong, L.; Yoon, S.-Y.; Byun, Y.; Kim, S.H.; et al. TNF-α Gene Silencing Using Polymerized siRNA/Thiolated Glycol Chitosan Nanoparticles for Rheumatoid Arthritis. Mol. Ther. 2014, 22, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Park, J.-S.; Lee, S.J.; Jang, J.; Park, J.S.; Back, S.H.; Bahn, G.; Park, J.H.; Kang, Y.M.; Kim, S.H.; et al. Notch1 targeting siRNA delivery nanoparticles for rheumatoid arthritis therapy. J. Control. Release 2015, 216, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Looman, M.; Berg, C.V.D.; Geelen, A.; Samlal, R.A.K.; Heijligenberg, R.; Gunnewiek, J.M.T.K.; Balvers, M.G.J.; Leendertz-Eggen, C.L.; Wijnberger, L.D.E.; Feskens, E.; et al. Supplement Use and Dietary Sources of Folate, Vitamin D, and n-3 Fatty Acids during Preconception: The GLIMP2 Study. Nutrients 2018, 10, 962. [Google Scholar] [CrossRef]
- Low, P.S.; Henne, W.A.; Doorneweerd, D.D. Discovery and Development of Folic-Acid-Based Receptor Targeting for Imaging and Therapy of Cancer and Inflammatory Diseases. Accounts Chem. Res. 2008, 41, 120–129. [Google Scholar] [CrossRef]
- Kesharwani, P.; Gothwal, A.; Iyer, A.K.; Jain, K.; Chourasia, M.K.; Gupta, U. Dendrimer nanohybrid carrier systems: An expanding horizon for targeted drug and gene delivery. Drug Discov. Today 2018, 23, 300–314. [Google Scholar] [CrossRef]
- Thomas, T.P.; Goonewardena, S.N.; Majoros, I.J.; Kotlyar, A.; Cao, Z.; Leroueil, P.R.; Baker, J.R. Folate-targeted nanoparticles show efficacy in the treatment of inflammatory arthritis. Arthritis Rheum. 2011, 63, 2671–2680. [Google Scholar] [CrossRef]
- Bilthariya, U.; Jain, N.; Rajoriya, V.; Jain, A.K. Folate-conjugated albumin nanoparticles for rheumatoid arthritis-targeted delivery of etoricoxib. Drug Dev. Ind. Pharm. 2013, 41, 95–104. [Google Scholar] [CrossRef]
- Duan, W.; Li, H. Combination of NF-kB targeted siRNA and methotrexate in a hybrid nanocarrier towards the effective treatment in rheumatoid arthritis. J. Nanobiotechnology 2018, 16, 58. [Google Scholar] [CrossRef]
- Mandal, B.; Bhattacharjee, H.; Mittal, N.K.; Sah, H.; Balabathula, P.; Thoma, L.A.; Wood, G.C. Core–shell-type lipid–polymer hybrid nanoparticles as a drug delivery platform. Nanomed. Nanotechnol. Boil. Med. 2013, 9, 474–491. [Google Scholar] [CrossRef]
- Mura, S.; Nicolas, J.; Couvreur, P.; Patrick, C. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013, 12, 991–1003. [Google Scholar] [CrossRef] [PubMed]
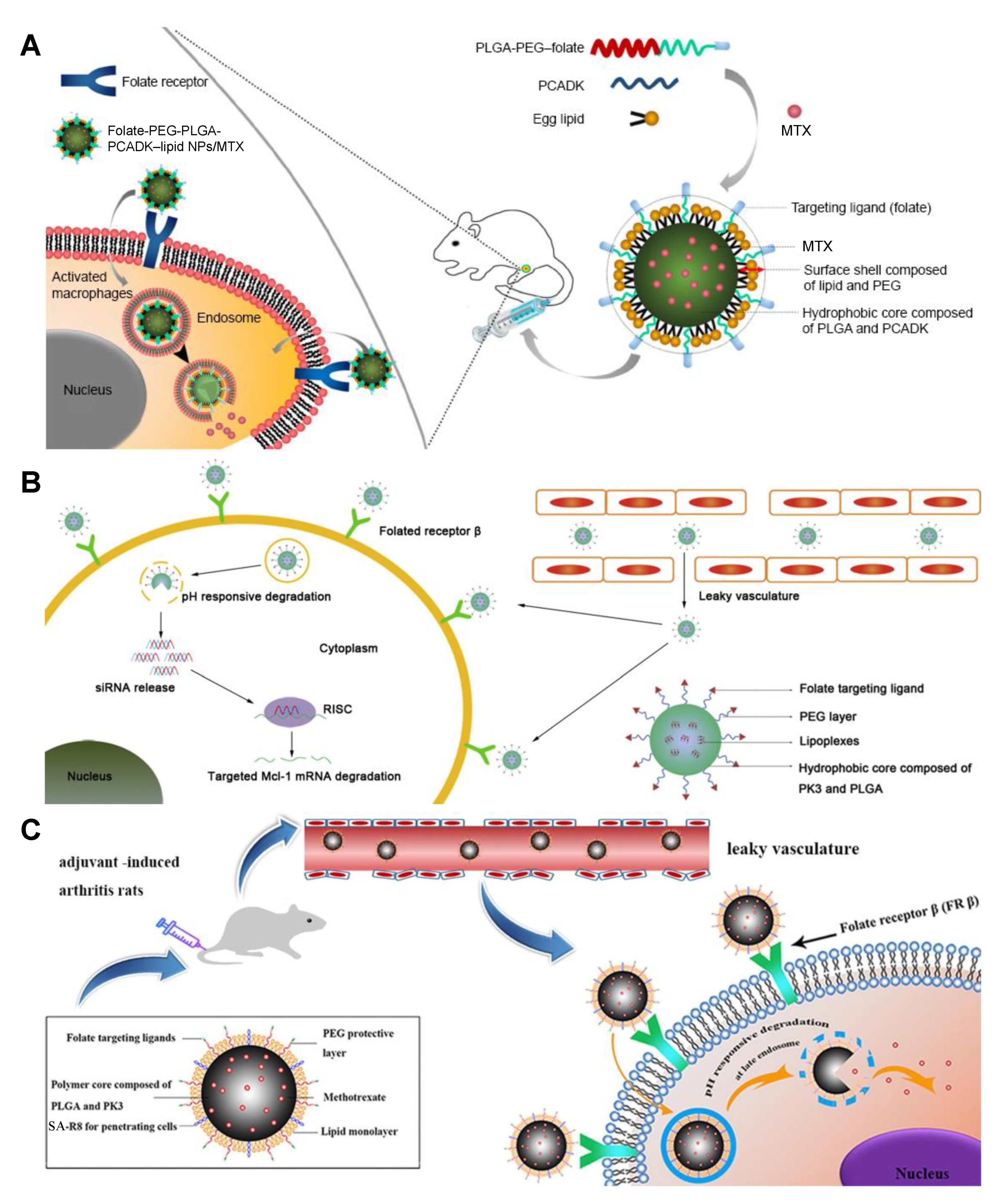
- Zhao, J.; Zhao, M.; Yu, C.; Zhang, X.; Liu, J.; Cheng, X.; Lee, R.J.; Sun, F.; Teng, L.; Li, Y. Multifunctional folate receptor-targeting and pH-responsive nanocarriers loaded with methotrexate for treatment of rheumatoid arthritis. Int. J. Nanomed. 2017, 12, 6735–6746. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Dong, S.; Li, X.; Yu, K.; Sun, F.; Lee, R.J.; Li, Y.; Teng, L. Delivery of siRNA using folate receptor-targeted pH-sensitive polymeric nanoparticles for rheumatoid arthritis therapy. Nanomed. Nanotechnol. Boil. Med. 2019, 20, 102017. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Zhang, X.; Sun, X.; Zhao, M.; Yu, C.; Lee, R.J.; Sun, F.; Zhou, Y.; Li, Y.; Teng, L. Dual-functional lipid polymeric hybrid pH-responsive nanoparticles decorated with cell penetrating peptide and folate for therapy against rheumatoid arthritis. Eur. J. Pharm. Biopharm. 2018, 130, 39–47. [Google Scholar] [CrossRef]
- Khojah, H.M.; Ahmed, S.; Abdel-Rahman, M.S.; Hamza, A.-B. Reactive oxygen and nitrogen species in patients with rheumatoid arthritis as potential biomarkers for disease activity and the role of antioxidants. Free. Radic. Boil. Med. 2016, 97, 285–291. [Google Scholar] [CrossRef]
- Ni, R.; Song, G.; Fu, X.; Song, R.; Li, L.; Pu, W.; Gao, J.; Hu, J.; Liu, Q.; He, F.; et al. Reactive oxygen species-responsive dexamethasone-loaded nanoparticles for targeted treatment of rheumatoid arthritis via suppressing the iRhom2/TNF-α/BAFF signaling pathway. Biomaterials 2019, 232, 119730. [Google Scholar] [CrossRef]
- Chen, M.; Kambere Amerigos Daddy, J.C.; Su, Z.; ElIslem Guissi, N.; Xiao, Y.; Zong, L.; Ping, Q. Folate receptor-targeting and reactive oxygen species-responsive liposomal formulation of methotrexate for treatment of rheumatoid arthritis. Pharmaceutics 2019, 11, 582. [Google Scholar] [CrossRef]
- Verma, A.; Jain, A.; Tiwari, A.; Saraf, S.; Panda, P.K.; Agrawal, G.P.; Jain, S.K. Folate Conjugated Double Liposomes Bearing Prednisolone and Methotrexate for Targeting Rheumatoid Arthritis. Pharm. Res. 2019, 36, 123. [Google Scholar] [CrossRef]
- Zhang, N.; Xu, C.; Li, N.; Zhang, S.; Fu, L.; Chu, X.; Hua, H.; Zeng, X.; Zhao, Y. Folate receptor-targeted mixed polysialic acid micelles for combating rheumatoid arthritis: In vitro and in vivo evaluation. Drug Deliv. 2018, 25, 1182–1191. [Google Scholar] [CrossRef]
- Kingma, P.S.; Whitsett, J.A. In defense of the lung: Surfactant protein A and surfactant protein D. Curr. Opin. Pharmacol. 2006, 6, 277–283. [Google Scholar] [CrossRef]
- Nogueira, E.; Mangialavori, I.C.; Loureiro, A.; Azoia, N.; Passos, M.; Nogueira, P.; Freitas, J.; Härmark, J.; Shimanovich, U.; Rollett, A.; et al. Peptide Anchor for Folate-Targeted Liposomal Delivery. Biomacromolecules 2015, 16, 2904–2910. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.; Dai, F.; Deng, H.; Du, M.; Zhang, X.; Liu, Q.; Zhang, X. A rheumatoid arthritis magnetic resonance imaging contrast agent based on folic acid conjugated PEG-b-PAA@SPION. J. Mater. Chem. B 2014, 2, 2938–2946. [Google Scholar] [CrossRef] [PubMed]
- Dai, F.; Du, M.; Liu, Y.; Liu, G.; Liu, Q.; Zhang, X. Folic acid-conjugated glucose and dextran coated iron oxide nanoparticles as MRI contrast agents for diagnosis and treatment response of rheumatoid arthritis. J. Mater. Chem. B 2014, 2, 2240–2247. [Google Scholar] [CrossRef] [PubMed]
- Hebeish, A.; El-Rafie, M.; El-Sheikh, M.; Seleem, A.A.; El-Naggar, M.E.; El-Rafie, M.; El-Sheikh, M.A. Antimicrobial wound dressing and anti-inflammatory efficacy of silver nanoparticles. Int. J. Boil. Macromol. 2014, 65, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Roy, N.; Gaur, A.; Jain, A.; Bhattacharya, S.; Rani, V. Green synthesis of silver nanoparticles: An approach to overcome toxicity. Environ. Toxicol. Pharmacol. 2013, 36, 807–812. [Google Scholar] [CrossRef]
- Shukla, V.K.; Singh, R.P.; Pandey, A.C. Black pepper assisted biomimetic synthesis of silver nanoparticles. J. Alloy. Compd. 2010, 507, L13–L16. [Google Scholar] [CrossRef]
- Mani, A.; Vasanthi, C.; Gopal, V.; Chellathai, D. Role of phyto-stabilised silver nanoparticles in suppressing adjuvant induced arthritis in rats. Int. Immunopharmacol. 2016, 41, 17–23. [Google Scholar] [CrossRef]

| Food ingredient | Nano system | Model | Dose | Pharmacological Effects | Ref. |
|---|---|---|---|---|---|
| Curcumin | NEs | AIA rats | 50 mg/kg/d; p.o.; 14 days | Paw swelling↓↓ a; TNF-α and IL-1β decreased | [13] |
| Curcumin | Solid lipid nanoparticles | AIA rats | 10 and 30 mg/kg/d; p.o.; 14 days | Joint hyperalgesia↓↓↓ a; mobility score↑↑↑↑ a; joint stiffness↓↓↓↓ a; paw volume↓↓↓↓ a; radiological score decreased | [20] |
| Curcumin | Nanomicelles | RA patients | 40 mg/tid.; p.o.; 12 weeks | Disease activity score of joints↓↓↓↓ b; tender joint count↓↓↓ b; swollen joint count↓↓ b | [24] |
| Curcumin | NEG | AIA rats | 25.71 mg/kg/bid.; top.; 28 days | Body weight ↑↑ a; tibiotarsal joint thickness↓ a; IL-1β, TNF-α↓↓ a; paw volume decreased; histopathological changes alleviated | [26] |
| Curcumin | NEG | Carrageenan-induced paw edema; rat skin | 30 mg/kg; top. | Anti-inflammatory effects↑↑↑ d; skin permeation increased | [27] |
| Curcumin | NEG | Carrageenan-induced paw edema; AIA rats | Paw edema↓↓↓ a; body weight↑↑↑ a; paw volume↓↓↓ a; motor incoordination↓↓↓ a; arthritic clinical score↓↓↓ a; synovium TNF-α, IL-6, IL-1β ↓↓↓ a; serum TNF-α, IL-6 ↓↓↓ a; radiological score↓↓↓ a; histopathological changes alleviated | [28] | |
| Curcumin and Resveratrol | Lipid core nanocapsules | AIA rats | 1.75 mg/kg/bid; i.p.; 8 days | Paw edema↓ d; synovial fibrosis ↓ a; cartilage loss↓ a; bone loss↓ a; histopathological changes alleviated | [31] |
| Curcumin | Nanomicelles | CIA rats | 33.6 μg; IA inj. | Paw edema↓ b; TNF-α, IL-1, VEGF↓ a; histopathological changes alleviated | [32] |
| Resveratrol | Nanomicelles | AIA rats | 1 mg/mL/week; IA inj.; 14 days | Knee swelling↓ a; TNF-α↓ a; histopathological changes alleviated | [37] |
| sveratrol | QRu-PLGA-DS NPs | RAW 264.7 cells; CIA mice | TNF-α, IL-1β, IL-6↓↓ a; IL-4, IL-10, TGF-β↑↑ a; histopathological changes alleviated | [38] | |
| Quercetin | TGA-CdTe QDs | AIA rats | 0.2 and 0.4 mg/kg/d; p.o.; 21 days | Inflammation reduced; cartilage regeneration improved; histopathological changes alleviated | [43] |
| Quercetin | NEG | AIA rats | 10 mg/bid; top.; 28 days | TNF-α↓ c; arthritic index↓ a; stiffness score↓ a; paw circumference↓ a; rheumatoid factor↓ a | [44] |
| Quercetin | PCL microspheres | HIG-82 cells, rats | 0.1 mL; IA inj. | Synovial macrophage proliferation reduced; controlled release of quercetin in the joint cavity for more than 30 days | [45] |
| Hesperidin | AgNPs | AIA rats | 1mg/kg; p.o.; 14 days | Arthritic score↓↓↓ a; paw swelling↓↓↓ a; TLR-2, TLR-4↓↓↓ a | [48] |
| Food Material | Nano System | Loaded Drug | Model | Dose | Pharmacological Effects | Ref. |
|---|---|---|---|---|---|---|
| Soybean oil | NEs | Curcumin | AIA rats | 50 mg/kg/d; p.o.; 14 days | Paw swelling↓↓ a; TNF-α and IL-1β decreased | [13] |
| Soybean oil | NEs | Oily mixture of camphor, menthol and methyl salicylate | Rat skin | 5% camphor, 5% menthol, and 5% methyl salicylate | Permeation rates increased | [54] |
| Grape seed oil | Lipid core nanocapsules | Curcumin, resveratrol | AIA rats | 1.75 mg/kg/bid; i.p.; 8 days | Paw edema↓ d; synovial fibrosis↓ a; cartilage loss↓ a; bone loss↓ a; radiological score decreased | [31] |
| Emu oil | NEG | Curcumin | Carrageenan induced paw edema, AIA rats | Top. | Paw edema↓↓↓ a; body weight↑↑↑ a; motor incoordination↓↓↓ a; arthritic clinical score↓↓↓ a; synovial TNF-α, IL-6, IL-1β↓↓↓ a; serum TNF-α, IL-6 ↓↓↓ a; radiological score↓↓↓ a; histopathological changes alleviated | [28] |
| Soy lecithin | Liposomes | Triptolide | CIA mice | 200 mg/kg/d; top.; 25 days | Pannus number↓↓ a; histopathological changes alleviated | [64] |
| Soy lecithin | NSSLs | MPS; BMS | AIA rats | ①At early stage: 10 mg/kg; i.v.; 2 times (NSSLs-MPS) or 3 times (NSSLs-BMS). ②At late stage: 10 mg/kg (NSSLs-MPS) or 5 mg/kg (NSSLs-BMS), i.v., 2 times | ①At early stage: arthritis score↓↓↓ a ②At late stage: arthritis score↓ a | [66] |
| Soy lecithin | NSSLs | MPS; BMS | AIA rats | NSSLs-MPS: ①10 mg/kg/week; i.v.; 3 times; ②10 mg/kg/week; s.c.; 2 times; ③2 mg/kg/week; s.c.; 3 times; ④1 or 10 mg/kg; i.v.; 1 time; ⑤10 mg/kg; i.v. NSSLs-BMS: 1 mg/kg/week; s.c.; 3 times | NSSLs-MPS: ①arthritis score↓ a; ②arthritis score↓↓ a; ③arthritis score↓↓ a;④arthritis score↓ a; ⑤splenocyte IL-6↓↓ a, IL-10↓ a, INF-γ↓ a; serum IL-6↓ a NSSLs-BMS: arthritis score↓↓ a | [67] |
| Soy lecithin | Sialic acid-modified liposomes | Dexamethasane palmitate | AIA rats | 0.9 mg/kg/3 days; i.v.; 5 times | Paw thickness↓↓ a; joint score↓↓↓ a; IL-1β↓ a, TNF-α↓↓↓ a; histological scores↓↓ a | [70] |
| Egg lecithin | Liposomes | Indomethacin | AIA rats | 3 mg/kg/d; i.p.; 15 days | Edema volume↓↓ c; Ulcerogenicity↓↓ c | [71] |
| Egg lecithin | Liposome hydrogel patch | Triptolide | CIA rats | 20 mg/kg; top.; 4 weeks; 40 mg/kg; top.; 4 weeks | 20 mg/kg: joint swelling↓↓ a; IL-1β↓ a, IL-6↓↓↓ a; Flk-1↓↓↓ a; Flt-4↓↓↓ a; HIF-1α↓ a 40 mg/kg: joint swelling↓↓↓ a; IL-1β, IL-6↓↓↓ a; Flk-1↓↓↓ a; Flt-4↓↓↓ a; HIF-1↓↓ a | [72] |
| Egg lecithin | Ultradeformable liposomal gel | MTX | AIA rats | 0.5 mg/kg/3 days; top.; 8 times | Paw edema volume↓↓↓ a; body weight↑↑↑ a; paw histological score↓↓ a; leukocyte infiltration↓ a; neutrophils in paw tissues↓ a; TNF-a↓ a; IL-1β↓ a | [74] |
| Egg lecithin | WSs | TNF-α siRNA | CIA mice | 10 μg/body; three times a week; i.v.;11 days | Arthritis incidance↓; arthritis score↓; paw thickness↓; TNF-α↓ | [76] |
| Egg lecithin | Large unilamellar vesicles | APO2L/TRAIL | Antigen-induced arthritic rabbits | 5 μg; 10 μg | 5 μg: Knee lateral diameter ↓ a; inflammation↓ a; synovial hyperplasia↓ a 10 μg: Knee lateral diameter↓↓ a | [78] |
| Food material | Nano system | Loaded drug | Model | Dose | Pharmacological effects | Ref. |
|---|---|---|---|---|---|---|
| CHS | CHS NPs | Betamethasone sodium phosphate | Rats | 1 and 2 mg/kg | Without any toxic effect on vital organs | [82] |
| CHS | CHS NPs | Embelin | AIA rats | 25 and 50 mg/kg/d; p.o.; 14days | 25 and 50 mg/kg: arthritic score and paw swelling decreased 25 mg/kg: TNF-α↓↓ a; IL-1β↓ a; IL-6↓ a50 mg/kg: TNF-α; IL-1β; IL-6↓↓↓ a | [83] |
| CHS | CHS NPs | Zinc gluconate | CIA rats | 112.93 mg/kg; i.p. | Serum TNF-α↓↓ a, IL-1β↓↓↓ a; joint synovial IL-6↓↓↓ a, TNF-α↓↓↓ a, iNOS↓↓↓ a; histopathological changes alleviated | [84] |
| CHS | Polysialic acid-trimethyl CHS NPs | DEX; MTX | SW-982 cells | 1.0 mg/mL | DEX: IL-6↓ a,d; IL-8↓ a MTX: IL-8↓ a | [85] |
| CHS | Glycol CHS-steric acid NPs | MTX | AIA mice | 0.5 mg/kg/3d; i.v. | Arthritis score↓↓ a; paw thickness↓↓ a; IL-1β, TNF-a↓ c | [86] |
| CHS | CHS-chondroitin sulfate NP-loaded argan oil emulsion gel | Ketoprofen | Mice skin | Compared with marketed gel, skin permeability↑↑↑↑; compared with NP-loaded gel, skin permeability↑↑ | [87] | |
| CHS | CHS-NP-loaded poloxamer gel | Clodronate | THP1 cells | 1, 2, and 4 μg/mL | IL-8 and IL-1β decreased | [90] |
| CHS | Thiolated glycol CHS NPs | Polymerized siRNA | RAW 264.7 cells; CIA mice | 50 μg; i.v. | TNF-α in RAW 264.7 cells decreased; TNF-α in serum and arthritic joints↓ b; arthritic score, paw thickness decreased; bone erosions in paws and ankle joints decreased | [93] |
| CHS | Thiolated glycol CHS NPs | Polymerized siRNA | RAW 264.7 cells; CIA mice | Notch1 in RAW 264.7 cells ↓↓↓ a; synovial inflammation↓↓↓ a; cartilage erosion↓↓ a; neutrophil infiltration↓↓↓ a; clinical score, bone damage decreased | [94] |
| Food material | Nano system | Loaded drug | Model | Dose | Pharmacological effects | Ref. |
|---|---|---|---|---|---|---|
| Folate | Folate-conjugated albumin nanoparticles | Etoricoxib | Carrageenan induced arthritis | 5 mg/kg; i.v. | Inhibition of edema increased | [99] |
| Folate | Folate-conjugated liposomes | NF-kB-targeted siRNA; MTX | RAW 264.7 cells; arthritic mice | i.v. | Cellular uptake increased; paw thickness, arthritic scores, TNF-α and IL-1β decreased | [100] |
| Folate | Folate-liposomes | MTX; catalase | RAW 264.7 cells; CIA mice | 1 mg/kg/2d; i.v.; 5 times | Cellular uptake increased; arthritis score↓↓ a; paw thickness↓↓ a; body weight↑↑ a; TNF-α↓↓↓ a, IL-1β↓↓↓ a | [108] |
| Folate | Folate conjugated double liposomes | PRD; MTX | CIA rats | 1 mg/kg; i.v. | Inhibition of edema increased | [109] |
| Folate | FA-PEG-PLGA-PCADK-lipid NPs | MTX | RAW 264.7 cells; AIA rats | 257 μg/kg/2d; i.v. | Cellular uptake increased; clinical score↓↓ c; paw thickness↓↓ c; TNF-α↓↓↓ c, IL-6↓↓ c; histopathological changes alleviated | [103] |
| Folate | FA-PEG-PLGA-PK3 NPs | Mcl-1 siRNA | RAW 264.7 cells; AIA rats | 4 nmol/kg/2d; i.v.; three times | Cellular uptake increased; clinical score↓↓↓ a; paw thickness↓↓↓ a; TNF-α↓↓↓ a, IL-6↓↓a, IL-1β↓↓ a; histopathological changes alleviated | [104] |
| Folate | SA-R8-FA-PEG-PLGA-lipid polymeric hybrid NPs | MTX | RAW 264.7 cells; AIA rats | Cellular uptake increased; clinical score↓↓↓ c; paw thickness↓↓↓ c; TNF-α↓↓ c, IL-6↓↓↓c, IL-1β↓↓↓ c; histopathological changes alleviated | [105] | |
| FA | FA-Oxi-αCD NPs | DEX | RAW 264.7 cells; CIA mice | 1.25mg/kg/4d; i.v. | TNF-a↓ a; arthritis index↓ a; paw thickness↓ a; synovial inflammation↓ a; cartilage erosion a; histopathological changes alleviated | [107] |
| FA | FA-polysialic acid- cholesteryl chloroformate micelles | DEX | RAW 264.7 cells; AIA mice | RAW 264.7 cells: 0.1mg/mL AIA mice: 0.02mg/ 2d; 10 days | RAW 264.7 cells: TNF-a, IL-6 decreased AIA mice: Paw thickness, clinical index, TNF-a, IL-6 decreased | [110] |
| FA | FA-SP-D-liposomes | Celecoxib | Caco-2 cells | Compared with celecoxib-loaded liposomes, COX-2↓ | [112] | |
| FA | FA-PEG-PAA@SPIONPs | RAW 264.7 cells; Antigen induced arthritic rats | 5 mg/kg; i.v. | Cellular uptake increased; MRI enhanced in diagnosis | [113] | |
| FA | FA-glucose-dextran-SPIONPs | RAW 264.7 cells; Antigen induced arthritic rats | 25 mg/kg; i.v. | Cellular uptake increased; MRI enhanced in diagnosis and therapy response | [114] | |
| Black pepper extract | Phyto-stabilised AgNPs | AIA rats | 25 and 50 mg/kg/2d; i.p.; 6 times | Paw volume↓ a; gait score↓ a; histopathologic score↓ a; histopathological changes alleviated | [118] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, D.; Chen, Q.; Chen, H. Food-Derived Nanoscopic Drug Delivery Systems for Treatment of Rheumatoid Arthritis. Molecules 2020, 25, 3506. https://doi.org/10.3390/molecules25153506
Han D, Chen Q, Chen H. Food-Derived Nanoscopic Drug Delivery Systems for Treatment of Rheumatoid Arthritis. Molecules. 2020; 25(15):3506. https://doi.org/10.3390/molecules25153506
Chicago/Turabian StyleHan, Dong, Qilei Chen, and Hubiao Chen. 2020. "Food-Derived Nanoscopic Drug Delivery Systems for Treatment of Rheumatoid Arthritis" Molecules 25, no. 15: 3506. https://doi.org/10.3390/molecules25153506
APA StyleHan, D., Chen, Q., & Chen, H. (2020). Food-Derived Nanoscopic Drug Delivery Systems for Treatment of Rheumatoid Arthritis. Molecules, 25(15), 3506. https://doi.org/10.3390/molecules25153506







