Recombinant Human Adenovirus-p53 Therapy for the Treatment of Oral Leukoplakia and Oral Squamous Cell Carcinoma: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Method
2.2. Inclusion and Exclusion Criteria
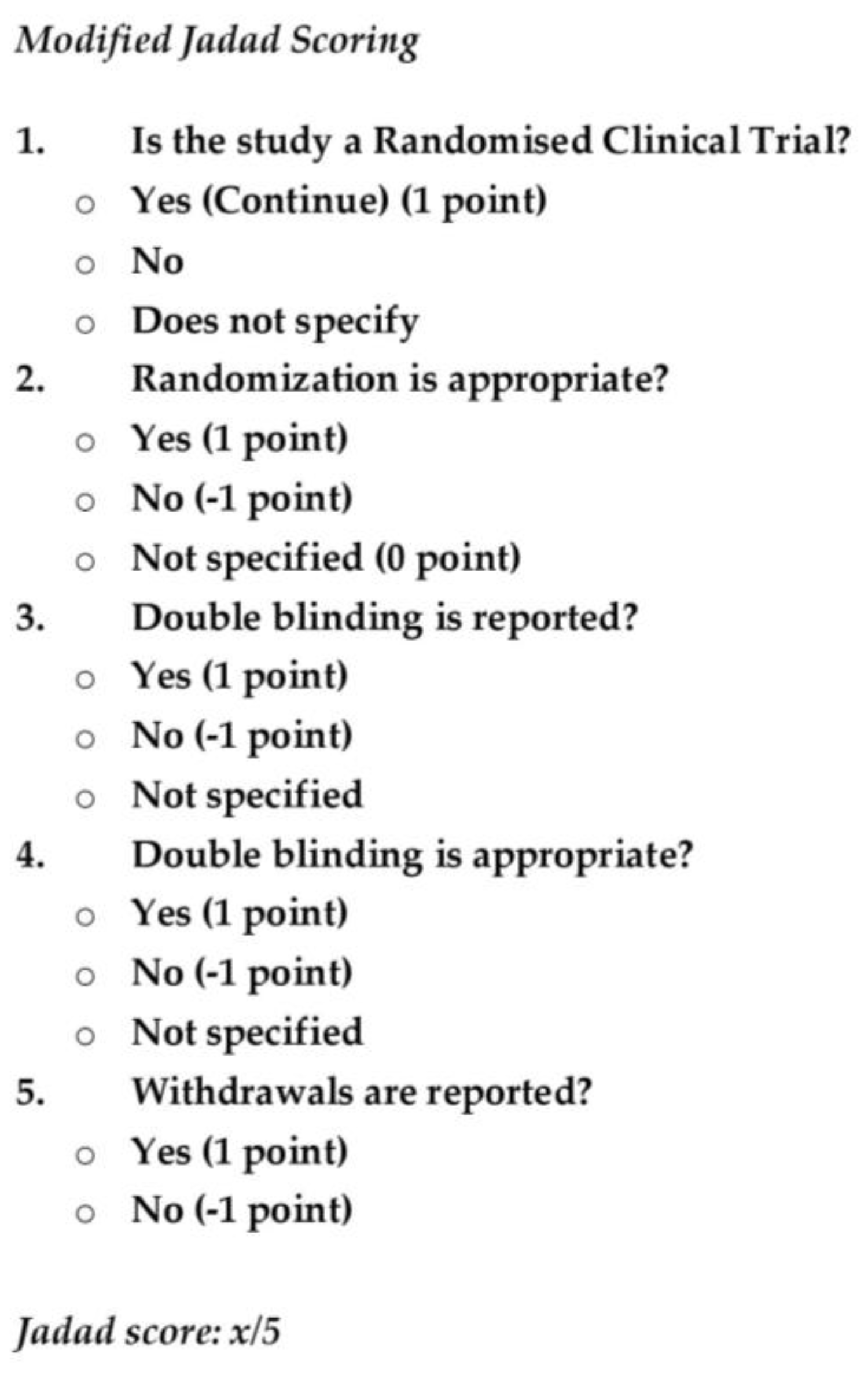
2.3. Jadad Scoring
Literature Search Summary
2.4. Outcome Measures
3. Results
3.1. Literature Search Summary
3.2. Synthesis of Evidence: Treatment, Follow-Up and the Outcome
4. Discussion
4.1. Oral Cancer, Oral Leukoplakia and rAD-p53 Therapy: Summary of the Studies
4.2. Mode of Action and Outcome of rAD-p53 Treatment
4.3. rAD-p53 Gene Therapy in US
4.4. p53 as Biosignature for Gene Therapy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Warnakulasuriya, S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009, 45, 309–316. [Google Scholar] [CrossRef]
- Van der Waal, I. Oral leukoplakia, the ongoing discussion on definition and terminology. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e685–e692. [Google Scholar] [CrossRef]
- Van der Waal, I.; Schepman, K.P.; van der Meij, E.H.; Smeele, L.E. Oral leukoplakia: A Clinicopathological review. Oral Oncol. 1997, 33, 291–301. [Google Scholar] [CrossRef]
- Warnakulasuriya, S.; Johnson, N.W.; Van der Waal, I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J. Oral Pathol. Med. 2007, 36, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Scully, C. Oral cancer aetiopathogenesis; past, present and future aspects. Med. Oral Patol. Oral Cir. Bucal 2011, 16, 306–311. [Google Scholar] [CrossRef]
- Speight, P.M.; Khurram, S.A.; Kujan, O. Oral potentially malignant disorders: Risk of progression to malignancy. Oral Surg. Oral Med. Oral Patol. Oral Radiol. 2018, 125, 612–627. [Google Scholar] [CrossRef] [PubMed]
- Feller, L.; Lemmer, J. Oral Squamous Cell Carcinoma: Epidemiology, Clinical Presentation and Treatment. J. Cancer Ther. 2012, 3, 263–268. [Google Scholar] [CrossRef]
- Lodi, G.; Franchini, R.; Warnakulasuriya, S.; Varoni, E.M.; Sardella, A.; Kerr, A.R.; Carrassi, A.; MacDonald, L.C.; Worthington, H.V. Interventions for treating oral leukoplakia to prevent oral cancer. Cochrane Database Syst. Rev. 2016, 7, CD001829. [Google Scholar] [CrossRef]
- Noguti, J.; De Moura, C.F.G.; De Jesus, G.P.P.; Da Silva, V.H.P.; Hossaka, T.A.; Oshima, C.T.F.; Ribeiro, D.A. Metastasis from Oral Cancer: An Overview. Cancer Genom. Proteom. 2012, 9, 329–335. [Google Scholar]
- Anguela, X.M.; High, K.A. Entering the Modern Era of Gene Therapy. Annu. Rev. Med. 2019, 70, 273–288. [Google Scholar] [CrossRef]
- Mollanoori, H.; Teimourian, S. Therapeutic applications of CRISPR/Cas9 system in gene therapy. Biotechnol. Lett. 2018, 40, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Ries, J.C.; Schreiner, D.; Steininger, H.; Girod, S.C. p53 mutation and detection of p53 protein expression in oral leukoplakia and oral squamous cell carcinoma. Anticancer Res. 1998, 18, 2031–2036. [Google Scholar] [PubMed]
- Goh, A.M.; Coffill, C.R.; Lane, D.P. The role of mutant p53 in human cancer. J. Pathol. 2011, 223, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Muller, P.A.; Vousden, K.H. p53 mutations in cancer. Nat. Cell Biol. 2013, 15, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Ventura, A.; Kirsch, D.G.; McLaughlin, M.E.; Tuveson, D.A.; Grimm, J.; Lintault, L. Restoration of p53 function leads to tumour regression in vivo. Nature 2007, 445, 661–665. [Google Scholar] [CrossRef]
- Xue, W.; Zender, L.; Miething, C.; Dickins, R.A.; Hernando, E.; Krizhanovsky, V.; Cordon-Cardo, C.; Lowe, S.W. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature 2007, 445, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Boulay, J.-L.; Perruchoud, A.P.; Reuter, J.; Bolliger, C.; Herrmann, R.; Rochlitz, C. P21 gene expression as an indicator for the activity of adenovirus-p53 gene therapy in non-small cell lung cancer patients. Cancer Gene Ther. 2000, 7, 1215–1219. [Google Scholar] [CrossRef][Green Version]
- Eastham, J.A.; Hall, S.J.; Sehgal, I.; Wang, J.; Timme, T.L.; Yang, G.; Connell-Crowley, L.; Elledge, S.J.; Zhang, W.W.; Harper, J.W. In vivo gene therapy with p53 or p21 adenovirus for prostate cancer. Cancer Res. 1995, 55, 5151–5155. [Google Scholar] [PubMed]
- Pearson, S.; Jia, H.; Kandachi, K. China approves first gene therapy. Nat. Biotechnol. 2004, 22, 3–4. [Google Scholar] [CrossRef]
- Ma, C.-C.; Wang, Z.-L.; Xu, T.; He, Z.-Y.; Wei, Y.-Q. The approved gene therapy drugs worldwide: From 1998 to 2019. Biotechnol. Adv. 2020, 40, 107502. [Google Scholar] [CrossRef]
- Pan, J.-J.; Zhang, S.-W.; Chen, C.-B.; Xiao, S.-W.; Sun, Y.; Liu, C.-Q.; Su, X.; Li, D.M.; Xu, G.; Xu, B.; et al. Effect of recombinant adenovirus-p53 combined with radiotherapy on long-term prognosis of advanced nasopharyngeal carcinoma. J. Clin. Oncol. 2009, 27, 799–804. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Xu, J.; Guo, W.; Kong, C. Therapeutic p53 gene agent in the treatment of NPC cases: Preliminary results. J. Clin. Oncol. 2015, 33, 15. [Google Scholar] [CrossRef]
- Li, L.; Huang, Y.; Wang, L.; Li, Y.; Wen, Y.; Han, B. A Combination Therapy of Selective Intraarterial Gendicine Infusion with Chemotherapy for Locally Advanced Head and Neck Carcinoma. Mol. Ther. 2006, 13, S20. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Zhang, S.; Li, Y.; Li, L.; Zhang, Y.; Gao, N.; Zhang, Z.; Zhao, H. Phase I study of repeated intraepithelial delivery of adenoviral p53 in patients with dysplastic oral leukoplakia. J. Oral Maxillofac. Surg. 2009, 7, 1074–1082. [Google Scholar] [CrossRef]
- Li, Y.; Li, L.-J.; Zhang, S.-T.; Wang, L.-J.; Zhang, Z.; Gao, N.; Zhang, Y.Y.; Chen, Q.M. In vitro and Clinical Studies of Gene Therapy with Recombinant Human Adenovirus-p53 Injection for Oral Leukoplakia. Clin. Cancer Res. 2009, 15, 6724–6731. [Google Scholar] [CrossRef]
- Liu, S.; Chen, P.; Hu, M.; Tao, Y.; Chen, L.; Liu, H.; Wang, J.; Luo, J.; Gao, G. Randomized, controlled phase II study of post-surgery radiotherapy combined with recombinant adenoviral human p53 gene therapy in treatment of oral cancer. Cancer Gene Ther. 2013, 20, 375–378. [Google Scholar] [CrossRef]
- Li, Y.; Li, L.-J.; Wang, L.-J.; Zhang, Z.; Gao, N.; Liang, C.-Y.; Huang, Y.D.; Han, B. Selective intra-arterial infusion of rAd-p53 with chemotherapy for advanced oral cancer: A randomized clinical trial. BMC Med. 2014, 12, 16. [Google Scholar] [CrossRef]
- Naldini, L. Gene therapy returns to centre stage. Nature 2015, 526, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Boycott, K.M.; Vanstone, M.R.; Bulman, D.E.; MacKenzie, A.E. Rare-disease genetics in the era of next-generation sequencing: Discovery to translation. Nat. Rev. Genet. 2013, 14, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Farkona, S.; Diamandis, E.P.; Blasutig, I.M. Cancer immunotherapy: The beginning of the end of cancer? BMC Med. 2016, 14, 73. [Google Scholar] [CrossRef] [PubMed]
- Biaoxue, R.; Hui, P.; Wenlong, G.; Shuanying, Y. Evaluation of efficacy and safety for recombinant human adenovirus-p53 in the control of the malignant pleural effusions via thoracic perfusion. Sci. Rep. 2016, 6, 39355. [Google Scholar] [CrossRef]
- Petti, S. Lifestyle risk factors for oral cancer. Oral Oncol. 2009, 45, 340–350. [Google Scholar] [CrossRef]
- Bieging, K.T.; Mello, S.S.; Attardi, L.D. Unravelling mechanisms of p53-mediated tumour suppression. Nat. Rev. Cancer 2014, 14, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Giono, L.E.; Manfredi, J.J. The p53 tumor suppressor participates in multiple cell cycle checkpoints. J. Cell Physiol. 2006, 209, 13–20. [Google Scholar] [CrossRef]
- Haupt, S.; Berger, M.; Goldberg, Z.; Haupt, Y. Apoptosis—The p53 network. J. Cell Sci. 2003, 116, 4077–4085. [Google Scholar] [CrossRef]
- Stegh, A.H. Targeting the p53 signaling pathway in cancer therapy—the promises, challenges and perils. Expert Opin. Ther. Targets 2012, 16, 67–83. [Google Scholar] [CrossRef]
- Tang, J.; Di, J.; Cao, H.; Bai, J.; Zheng, J. p53-mediated autophagic regulation: A prospective strategy for cancer therapy. Cancer Lett. 2015, 363, 101–107. [Google Scholar] [CrossRef]
- Zhang, W.W.; Alemany, R.; Wang, J.; Koch, P.E.; Ordonez, N.G.; Roth, J.A. Safety evaluation of Ad5CMV-p53 in vitro and in vivo. Hum. Gene Ther. 1995, 6, 155–164. [Google Scholar] [CrossRef]
- Crighton, D.; Wilkinson, S.; O’Prey, J.; Syed, N.; Smith, P.; Harrison, P.R.; Gasco, M.; Garrone, O.; Crook, T.; Ryan, K.M. DRAM, a p53-induced modulator of autophagy, is critical for apoptosis. Cell 2006, 126, 121–134. [Google Scholar] [CrossRef]
- Brady, C.A.; Attardi, L.D. p53 at a glance. J. Cell Sci. 2010, 123, 2527–2532. [Google Scholar] [CrossRef]
- Kaiser, A.M.; Attardi, L.D. Deconstructing networks of p53-mediated tumor suppression in vivo. Cell Death Differ. 2018, 25, 93–103. [Google Scholar] [CrossRef]
- Wu, M.; Ye, H.; Tang, Z.; Shao, C.; Lu, G.; Chen, B.; Yang, Y.; Wang, G.; Hao, H. p53 dynamics orchestrates with binding affinity to target genes for cell fate decision. Cell Death Dis. 2017, 8, e3130. [Google Scholar] [CrossRef]
- Levine, A.J.; Berger, S.L. The interplay between epigenetic changes and the p53 protein in stem cells. Genes Dev. 2017, 31, 1195–1201. [Google Scholar] [CrossRef]
- Scoumanne, A.; Chen, X. Protein methylation: A new mechanism of p53 tumor suppressor regulation. Histol. Histopathol. 2008, 23, 1143–1149. [Google Scholar] [CrossRef]
- Zhang, W.W.; Li, L.; Li, D.; Liu, J.; Li, X.; Li, W.; Xu, X.; Zhang, M.J.; Chandler, L.A.; Lin, H.; et al. The First Approved Gene Therapy Product for Cancer Ad-p53 (Gendicine): 12 Years in the Clinic. Hum. Gene Ther. 2018, 29, 160–179. [Google Scholar] [CrossRef]
- Jin, S.; Levine, A.J. The p53 functional circuit. J. Cell Sci. 2001, 114, 4139–4140. [Google Scholar]
- Liu, Y.; Zheng, X.; Liu, F. The mechanism and inhibitory effect of recombinant human P53 adenovirus injection combined with paclitaxel on human cervical cancer cell HeLa. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 1037–1042. [Google Scholar]
- Tu, K.; Zheng, X.; Zhou, Z.; Li, C.; Zhang, J.; Gao, J.; Yao, Y.; Liu, Q. Recombinant human adenovirus-p53 injection induced apoptosis in hepatocellular carcinoma cell lines mediated by p53-Fbxw7 pathway, which controls c-Myc and cyclin E. PLoS ONE 2013, 8, e68574. [Google Scholar]
- Chen, G.-X.; Zhang, S.; He, X.-H.; Liu, S.-Y.; Ma, C.; Zou, X.-P. Clinical utility of recombinant adenoviral human p53 gene therapy: Current perspectives. Onco Targets Ther. 2014, 7, 1901–1909. [Google Scholar] [CrossRef]
- Shahryari, A.; Saghaeian Jazi, M.; Mohammadi, S.; Razavi Nikoo, H.; Nazari, Z.; Hosseini, E.S.; Burtscher, I.; Mowla, S.J.; Lickert, H. Development and Clinical Translation of Approved Gene Therapy Products for Genetic Disorders. Front Genet. 2019, 10, 868. [Google Scholar] [CrossRef] [PubMed]
- Nemunaitis, J.; Clayman, G.; Agarwala, S.S.; Hrushesky, W.; Wells, J.R.; Moore, C.; Hamm, J.; Yoo, G.; Baselga, J.; Murphy, B.A.; et al. Biomarkers Predict p53 Gene Therapy Efficacy in Recurrent Squamous Cell Carcinoma of the Head and Neck. Clin. Cancer Res. 2009, 15, 7719–7725. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.; Liu, Z.; Myers, J.N. TP53 Mutations in Head and Neck Squamous Cell Carcinoma and Their Impact on Disease Progression and Treatment Response. J. Cell Biochem. 2016, 117, 2682–2692. [Google Scholar] [CrossRef] [PubMed]

| Author and Year | Study Type and Design | Sample Population; Age Range | rAD-p53 Alone or with Other |
|---|---|---|---|
| Li et al., 2009 [24] | Oral lichen planus (OLP), RCT, Phase I, Blinding not defined | 22; 35–74; Male (M) and Female (F) | rAD-p53 alone |
| Liu et al., 2013 [25] | Oral cancer, RCT, Phase II | 107; 27–80; M and F | radical resection followed by radiotherapy and rAD-p53 |
| Li et al., 2014 [26] | Oral cancer; RCT, double-blinded, Phase III | 99; mean age around 57; M and F | rAD-p53 and chemotherapy |
| Article and Year Published | Jadad Score |
|---|---|
| 1. Li et al., 2009 [24] | 2/5 (no blinding) |
| 2. Liu et al., 2013 [25] | 4/5 (unmasked) |
| 3. Li et al., 2014 [26] | 5/5 (double-blind) |
| Article and Year | Primary Outcomes (%) | p-Value | Adverse Events | p-Value | IHC Pre- vs. Post Treatment (%) |
|---|---|---|---|---|---|
| Li et al., 2009 [24] | Complete regression 22.7 Partial regression 50 No effect 18.2 Progress to cancer 9 | NA | Transient fever 31.8 Injection site pain 22.7 Flu-like symptoms 9.1 Increase in WBC 18.2 | NA | p-53 low or negative vs. high in all samples p-21CIP/WAF 22.7 vs. 86.4 Bcl-2 54.5 vs. 18.2 |
| Liu et al., 2013 [25] | TC recurrence: EG 7.4 CG 33.3 GC recurrence: EG 6.7 CG 30.8 3-year OS: EG 100 CG 94 3-year DFS EG 93 CG 68 | 0.0326 0.0332 0.0586 0.0002 | Transient Fever: EG 84 CG 12 Flu-like symtomps EG 64 CG 4 Oral Membrane EG 24.6 Burn and pain CG 30 | <0.0001 <0.0001 0.6634 | NA |
| Li et al., 2014 [26] | CR: G I 48.5 GII 16.7 GIII 17.2 PR: GI 33.3 GII 36.7 G III 34.5 SD or PD: GI 18.2 GII 46.7 GIII 48.3 Recurrence: GI 9.1 GII 20.0 GIII 24.1 | 0.006 0.961 0.020 0.267 | Flu-like symptoms GI 81.8 GII 76.7 GIII 55.2 Bone Marrow Suppression GI 36.4 GII 0.0 GIII 37.89 | 0.051 | Bax Increase GI 84.8 GII 90.0 GIII 3.4 Bcl-2 decrease GI 90.0 GII 80.0 GIII 27.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hosmani, J.; Mushtaq, S.; Abullais, S.S.; Almubarak, H.M.; Assiri, K.; Testarelli, L.; Mazzoni, A.; Patil, S. Recombinant Human Adenovirus-p53 Therapy for the Treatment of Oral Leukoplakia and Oral Squamous Cell Carcinoma: A Systematic Review. Medicina 2021, 57, 438. https://doi.org/10.3390/medicina57050438
Hosmani J, Mushtaq S, Abullais SS, Almubarak HM, Assiri K, Testarelli L, Mazzoni A, Patil S. Recombinant Human Adenovirus-p53 Therapy for the Treatment of Oral Leukoplakia and Oral Squamous Cell Carcinoma: A Systematic Review. Medicina. 2021; 57(5):438. https://doi.org/10.3390/medicina57050438
Chicago/Turabian StyleHosmani, Jagadish, Shazia Mushtaq, Shahabe Saquib Abullais, Hussain Mohammed Almubarak, Khalil Assiri, Luca Testarelli, Alessandro Mazzoni, and Shankargouda Patil. 2021. "Recombinant Human Adenovirus-p53 Therapy for the Treatment of Oral Leukoplakia and Oral Squamous Cell Carcinoma: A Systematic Review" Medicina 57, no. 5: 438. https://doi.org/10.3390/medicina57050438
APA StyleHosmani, J., Mushtaq, S., Abullais, S. S., Almubarak, H. M., Assiri, K., Testarelli, L., Mazzoni, A., & Patil, S. (2021). Recombinant Human Adenovirus-p53 Therapy for the Treatment of Oral Leukoplakia and Oral Squamous Cell Carcinoma: A Systematic Review. Medicina, 57(5), 438. https://doi.org/10.3390/medicina57050438









