Veterinary Perspectives on Hemoglobin-Based Oxygen Carriers in Experimental Hemorrhagic Shock: Insights from Rabbit Models
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Animals
2.2. Bioethics
2.3. Ovine Blood Collection
2.4. HBOC
2.5. Anesthesia and Preoperative Care
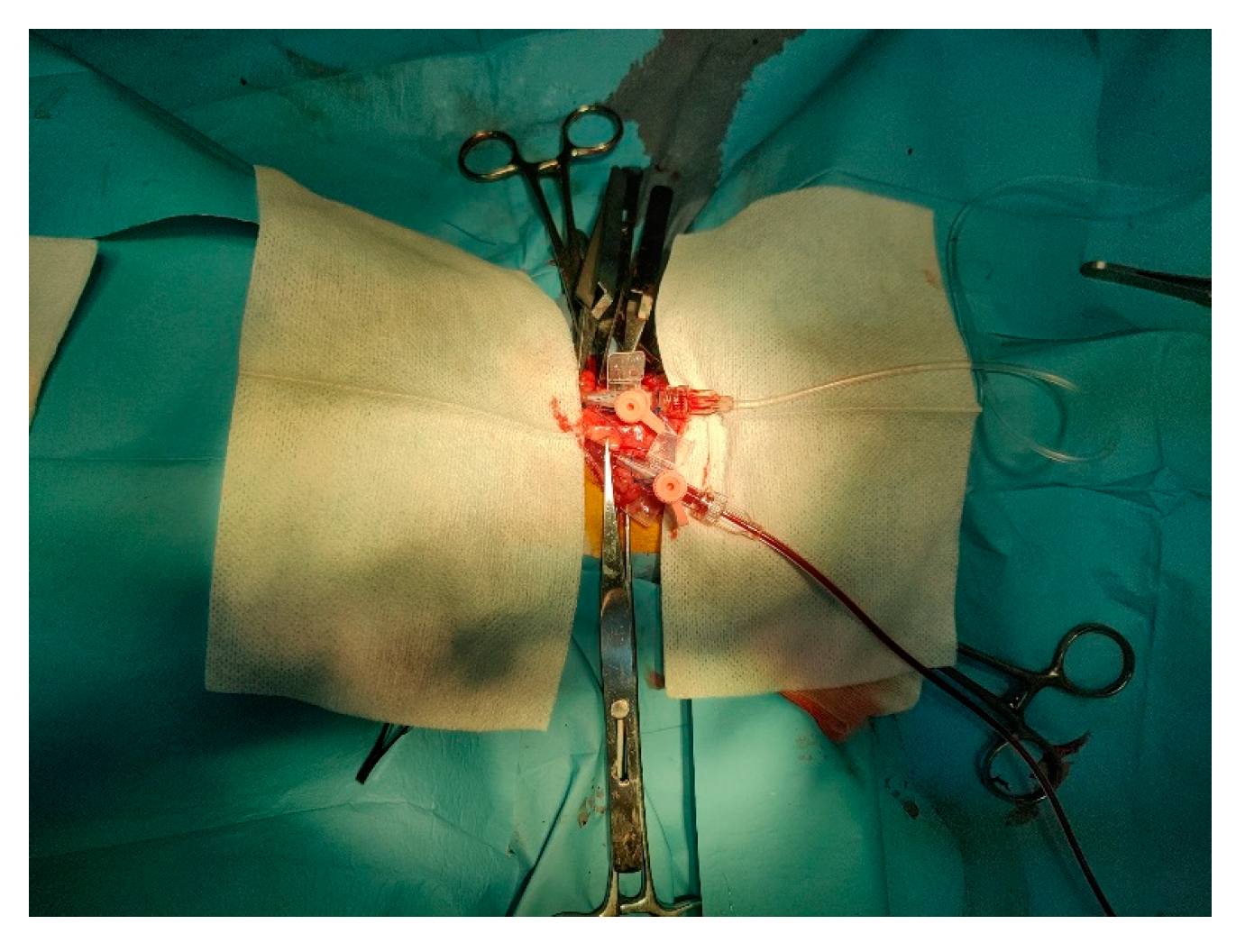
2.6. Induction of Hemorrhagic Shock
2.7. Blood Monitoring and Vitals
2.8. Statistics
3. Results and Discussion
3.1. Vitals During Experimental Procedures
3.2. Arterial Blood Gases Evolution
3.3. Arterial Blood Hemoglobin Parameters
3.4. Electrolyte Measurement in Arterial Blood
3.5. Metabolic Products Measurement in Arterial Blood
3.6. Respiratory Gas Evolution During Experimental Procedures
4. Discussion
5. Conclusions
6. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lichtenberger, M. Transfusion medicine in exotic pets. Clin. Tech. Small Anim. Pract. 2004, 19, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Farcas, A.D.; Toma, V.A.; Roman, I.; Sevastre, B.; Scurtu, F.; Silaghi-Dumitrescu, R. Glutaraldehyde-Polymerized Hemoglobin: In Search of Improved Performance as Oxygen Carrier in Hemorrhage Models. Bioinorg. Chem. Appl. 2020, 2020, 1096573. [Google Scholar] [CrossRef] [PubMed]
- Rice, J.; Philbin, N.; Handrigan, M.; Hall, C.; McGwin, G.; Ahlers, S.; Pearce, L.B.; Ar-naud, F.; McCarron, R.; Freilich, D. Vasoactivity of bovine polymerized hemoglobin (HBOC-201) in swine with traumatic hemorrhagic shock with and without brain injury. J. Trauma. Acute Care Surg. 2006, 61, 1085–1099. [Google Scholar] [CrossRef] [PubMed]
- Toma, V.; Lehen, M.; Sevastre, B.; Roman, I.; Dandea, S.; Moldoveanu, C.; Muntean, M.; Silaghi-Dumitrescu, R. Vascular homeostasis after exposure to sheep polymerized hemoglobin—Developments in semi-artificial oxygen carriers. In Posters FEBS Open Bio; FEBS Press: Cambridge, UK, 2024; Volume 14, pp. 92–516. [Google Scholar] [CrossRef]
- Marret, E.; Bonnin, P.; Mazoyer, E.; Riou, B.; Jacobs, T.; Coriat, P.; Samama, C.M. The effects of a polymerized bovine-derived hemoglobin solution in a rabbit model of arterial thrombosis and bleeding. Anesth. Analg. 2004, 98, 604–610. [Google Scholar] [CrossRef]
- Muller, C.R.; Williams, A.T.; Walser, C.; Eaker, A.M.; Sandoval, J.L.; Cuddington, C.T.; Wolfe, S.R.; Palmer, A.F.; Cabrales, P. Safety and efficacy of human polymerized hemoglobin on guinea pig resuscitation from hemorrhagic shock. Sci. Rep. 2022, 12, 20480. [Google Scholar] [CrossRef]
- Peruski, A.M.; Cooper, E.S.; Butler, A.L. Microcirculatory effects of a hyperviscous hemoglobin-based solution administered intravenously in dogs with experimentally induced hemorrhagic shock. Am. J. Vet. Res. 2014, 75, 77–84. [Google Scholar] [CrossRef]
- Kuang, L.; Hu, Y.; Wu, Y.; Tian, K.; Peng, X.; Xue, M.; Xiang, X.; Lau, B.; Tzang, F.C.; Liu, L.; et al. A Novel Cross-Linked Hemoglobin-Based Oxygen Carrier, YQ23, Extended the Golden Hour for Uncontrolled Hemorrhagic Shock in Rats and Miniature Pigs. Front. Pharmacol. 2021, 12, 652716. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, Y.; Peng, X.Y.; Li, Q.H.; Xiang, X.M.; Zhu, Y.; Li, T. The protective effect of a novel cross-linked hemoglobin-based oxygen carrier on hypoxia injury of acute mountain sickness in rabbits and goats. Front. Physiol. 2021, 12, 690190. [Google Scholar] [CrossRef]
- Okamoto, W.; Hiwatashi, Y.; Kobayashi, T.; Morita, Y.; Onozawa, H.; Iwazaki, M.; Kohno, M.; Tochinai, R.; Georgieva, R.; Bäumler, H.; et al. Poly (2-ethyl-2-oxazoline)-Conjugated Hemoglobins as a Red Blood Cell Substitute. ACS Appl. Bio Mater. 2023, 6, 3330–3340. [Google Scholar] [CrossRef]
- Gutierrez, G.; Reines, H.D.; Wulf-Gutierrez, M.E. Clinical review: Hemorrhagic shock. Crit. Care 2004, 8, 373–381. [Google Scholar] [CrossRef]
- Yoshizu, A.; Izumi, Y.; Park, S.; Sakai, H.; Takeoka, S.; Horinouchi, H.; Ikeda, E.; Tsuchida, E.; Kobayashi, K. Hemorrhagic Shock Resuscitation with an Artificial Oxygen Carrier, Hemoglobin Vesicle, Maintains Intestinal Perfusion and Suppresses the Increase in Plasma Tumor Necrosis Factor-α. ASAIO J. 2004, 50, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Rezende-Neto, J.B.; Moore, E.E.; Masuno, T.; Moore, P.T.; Johnson, J.L.; Sheppard, F.R.; Cunha-Melo, J.R.; Silliman, C.C. The abdominal compartment syndrome as a second insult during systemic neutrophil priming provokes multiple organ injury. Shock 2003, 20, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Sen Gupta, A. Hemoglobin-based Oxygen Carriers: Current State-of-the-art and Novel Molecules. Shock 2019, 52 (Suppl. S1), 70–83. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Toma, V.A.; Farcas, A.D.; Roman, I.; Sevastre, B.; Hathazi, D.; Scurtu, F.; Damian, G.; Silaghi-Dumitrescu, R. Comparative in vivo effects of hemoglobin-oxygen carriers (HBOC) with varying prooxidant and physiological reactivity. PLoS ONE 2016, 11, e0153909. [Google Scholar] [CrossRef]
- Yu, Y.H.; Gong, S.P.; Sheng, C.; Zhao, K.S.; Lodato, R.F.; Wang, C.H. Increased survival with hypotensive resuscitation in a rabbit model of uncontrolled hemorrhagic shock in pregnancy. Resuscitation 2009, 80, 1424–1430. [Google Scholar] [CrossRef]
- Horr, M.; Nunes, N.; Biteli, E.G.F.; Lopes, P.C.F.; Gering, A.P.; Moro, J.V.; Rocha, F.D.L. Effects of Inspired Oxygen Fractions in Rabbits Anesthetized with Isoflurane or Sevoflurane, Maintained On Spontaneous Ventilation. Arq. Bras. Med. Vet. Zootec. 2019, 71, 944–952. [Google Scholar] [CrossRef]
- Orr, H.E.; Roughan, J.V.; Flecknell, P.A. Assessment of ketamine and medetomidine anaesthesia in the domestic rabbit. Vet. Anaesth. Analg. 2005, 32, 271–279. [Google Scholar] [CrossRef]
- Sayce, L.J.; Powell, M.E.; Kimball, E.E.; Chen, P.; Gartling, G.J.; Rousseau, B. Continuous rate infusion of ketamine hydrochloride and dexmedetomidine for maintenance of anesthesia during laryngotracheal surgery in New Zealand White Rabbits (Oryctolagus cuniculus). J. Am. Assoc. Lab. Anim. Sci. 2020, 59, 176–185. [Google Scholar] [CrossRef]
- Su-Pei, S.; Wang, H.; Hui-Ming, C.; Pan, L.; Dai, T.J. The synergism of dexmedetomidine and ketamine. J. Anesth. Perioper. Med. (JAPM) 2015, 2, 183. [Google Scholar]
- Ardiaca, M.; Bonvehí, C.; Montesinos, A. Point-of-care blood gas and electrolyte analysis in rabbits. Vet. Clin. Exot. Anim. Pract. 2013, 16, 175–195. [Google Scholar] [CrossRef]
- Selleri, P.; Di Girolamo, N. Point-of-care blood gases, electrolytes, chemistries, hemoglobin, and hematocrit measurement in venous samples from pet rabbits. J. Am. Anim. Hosp. Assoc. 2014, 50, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Holzrichter, D.; Meiss, L.; Behrens, S.; Mickley, V. The rise of blood sugar as an additional parameter in traumatic shock. Arch. Orthop. Trauma. Surg. 1987, 106, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.B.; Christmas, A.B.; Heniford, B.T.; Sing, R.F.; Messick, J. Arterial vs. venous blood gas differences during hemorrhagic shock. World J. Crit. Care Med. 2014, 3, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Sun, L.; Ji, S.; Zhao, D.; Liu, J.; Su, Z.; Hu, T. Reversible protection of Cys-93(β) by PEG alters the structural and functional properties of the PEGylated hemoglobin. Biochim. Biophys. Acta 2014, 1844, 1201–1207. [Google Scholar] [CrossRef]
- Williams, A.T.; Lucas, A.; Muller, C.R.; Munoz, C.; Bolden-Rush, C.; Palmer, A.F.; Cabrales, P. Resuscitation from Hemorrhagic Shock with Fresh and Stored Blood and Polymerized Hemoglobin. Shock 2020, 54, 464–473. [Google Scholar] [CrossRef]
- Day, T.K. Current development and use of hemoglobin-based oxygen-carrying (HBOC) solutions. J. Vet. Emerg. Crit. Care 2003, 13, 77–93. [Google Scholar] [CrossRef]
- Li, K.; Xu, Y. Citrate metabolism in blood transfusions and its relationship to metabolic alkalosis and respiratory acidosis. Int. J. Clin. Exp. Med. 2015, 8, 6578–6584. [Google Scholar]
- Gu, X.; Bolden-Rush, C.; Cuddington, C.T.; Belcher, D.A.; Savla, C.; Pires, I.S.; Palmer, A.F. Comprehensive characterization of tense and relaxed quaternary state glutaraldehyde polymerized bovine hemoglobin as a function of cross-link density. Biotechnol. Bioeng. 2020, 117, 2362–2376. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, Y.; Massie, L.; Murata, G.H.; Tzamaloukas, A.H. Discrepancy between Measured Serum Total Carbon Dioxide Content and Bicarbonate Concentration Calculated from Arterial Blood Gases. Cureus 2015, 7, e398. [Google Scholar] [CrossRef]
- Olofsson, C.; Nygårds, E.B.; Ponzer, S.; Fagrell, B.; Przybelski, R.; Keipert, P.E.; Winslow, N.; Winslow, R.N. A randomized, single-blind, increasing dose safety trial of an oxygen-carrying plasma expander (Hemospan®) administered to orthopaedic surgery patients with spinal anaesthesia. Transfus. Med. 2008, 18, 28–39. [Google Scholar] [CrossRef]
- Cabrales, P. Examining and mitigating acellular hemoglobin vasoactivity. Antioxid. Redox Signal. 2013, 18, 2329–2341. [Google Scholar] [CrossRef] [PubMed]
- Elmer, J.; Alam, H.B.; Wilcox, S.R. Hemoglobin-based oxygen carriers for hemorrhagic shock. Resuscitation 2012, 83, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Schriner, J.B.; Van Gent, J.M.; Meledeo, M.A.; Olson, S.D.; Cotton, B.A.; Cox, C.S., Jr.; Gill, B.S. Impact of Transfused Citrate on Pathophysiology in Massive Transfusion. Crit. Care Explor. 2023, 5, e0925. [Google Scholar] [CrossRef] [PubMed]
- Roghani, K.; Holtby, R.J.; Jahr, J.S. Effects of Hemoglobin-Based Oxygen Carriers on Blood Coagulation. J. Funct. Biomater. 2014, 5, 288–295. [Google Scholar] [CrossRef]
- Stern, S.; Rice, J.; Philbin, N.; McGwin, G.; Arnaud, F.; Johnson, T.; Flournoy, W.S.; Ahlers, S.; Pearce, L.B.; McCarron, R.; et al. Resuscitation with the Hemoglobin-Based Oxygen Carrier HBOC-201 in a Swine Model of Severe Uncontrolled Hemorrhage and Traumatic Brain Injury. Shock 2009, 31, 64–79. [Google Scholar] [CrossRef]
- Prapan, A.; Suwannasom, N.; Kloypan, C.; Chaiwaree, S.; Steffen, A.; Xiong, Y.; Kao, I.; Pruß, A.; Georgieva, R.; Bäumler, H. Surface Modification of Hemoglobin-Based Ox-ygen Carriers Reduces Recognition by Haptoglobin, Immunoglobulin, and Hemoglo-bin Antibodies. Coatings 2019, 9, 454. [Google Scholar] [CrossRef]
- Stayner, S.; Ferguson, K. The anion gap and metabolic acidosis. In Advanced Anesthesia Review; Oxford University Press: Oxford, UK, 2023; p. 220. [Google Scholar]
- Lee, M.Y.; Yang, D.K.; Kim, S.J. Alterations of Mg2+ After Hemorrhagic Shock. Biol. Trace Elem. Res. 2017, 180, 120–126. [Google Scholar] [CrossRef]
- Cooper, C.E.; Silaghi-Dumitrescu, R.; Rukengwa, M.; Alayash, A.I.; Buehler, P.W. Peroxidase activity of hemoglobin towards ascorbate and urate: A synergistic protective strategy against toxicity of Hemoglobin-Based Oxygen Carriers (HBOC). Biochim. Biophys. Acta 2008, 1784, 1415–1420. [Google Scholar] [CrossRef] [PubMed]
- Faggiano, S.; Ronda, L.; Bruno, S.; Abbruzzetti, S.; Viappiani, C.; Bettati, S.; Mozzarelli, A. From hemoglobin allostery to hemoglobin-based oxygen carriers. Mol. Asp. Med. 2022, 84, 101050. [Google Scholar] [CrossRef]
- Jahr, J.S.; Osgood, S.; Rothenberg, S.J.; Li, Q.L.; Butch, A.W.; Gunther, R.; Cheung, A.; Driessen, B. Lactate measurement interference by hemoglobin-based oxygen carriers (Oxyglobin, Hemopure, and Hemolink). Anesth. Analg. 2005, 100, 431–436. [Google Scholar] [CrossRef]
- Alayash, A.I.; Summers, A.G.; Wood, F.; Jia, Y. Effects of glutaraldehyde polymerization on oxygen transport and redox properties of bovine hemoglobin. Arch. Biochem. Biophys. 2001, 391, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Chu, W.; Fan, D.; Dan, N.; Chen, C.; Wang, T.; Wang, F. Variations in dominant antigen determinants of glutaraldehyde polymerized human, bovine and porcine hemoglobin. Artif. Cells Blood Substit. Immobil. Biotechnol. 2007, 35, 518–532. [Google Scholar] [CrossRef]
- Gografe, S.I.; Wilson, J.S.; Johnson, B.L.; Rushing, G.; Bowser, A.; Parker, J.L.; Cornelius, C.E. Successful management of long-term general anesthesia in rabbits used as an animal model of human disease. Contemp. Top. Lab. Anim. Sci. 2003, 42, 16–19. [Google Scholar] [PubMed]
- Ghvaladze, M.; Kiria, P.; Dvalidze, N.; Arbolishvili, G.; Makharadze, N. Arterial and Venous Blood Gas Monitoring in Hemorrhagic Shock. Bull. Georg. Natl. Acad. Sci. 2011, 5, 107–115. [Google Scholar]
- Cao, M.; Yong, Z.; Hongli, H.; Ruiming, Y.; Lingai, P.; Huan, H.; Yingjie, R.; Qin, Q.; Xueliang, Y.; Tao, Y.; et al. New applications of HBOC-201: A 25-year review of the literature. Front. Med. 2021, 8, 794561. [Google Scholar] [CrossRef]
- de Vries, Y.; Matton, A.P.M.; Nijsten, M.W.N.; Werner, M.J.M.; van den Berg, A.P.; de Boer, M.T.; Buis, C.I.; Fujiyoshi, M.; de Kleine, R.H.J.; van Leeuwen, O.B.; et al. Pretransplant sequential hypo- and normothermic machine perfusion of suboptimal livers donated after circulatory death using a hemoglobin-based oxygen carrier perfusion solution. Am. J. Transplant. 2019, 19, 1202–1211. [Google Scholar] [CrossRef]
- Serruys, P.W.; Vranckx, P.; Slagboom, T.; Regar, E.; Meliga, E.; de Winter, R.J.; Heyndrickx, G.; Schuler, G.; van Remortel, E.A.; Dubé, G.P.; et al. Haemodynamic effects, safety, and tolerability of haemoglobin-based oxygen carrier-201 in patients undergoing PCI for CAD. Eurointervention 2008, 3, 600–609. [Google Scholar] [CrossRef]
- Yu, B.; Raher, M.J.; Volpato, G.P.; Bloch, K.D.; Ichinose, F.; Zapol, W.M. Inhaled nitric oxide enables artificial blood transfusion without hypertension. Circulation 2008, 117, 1982–1990. [Google Scholar] [CrossRef]
- Chen, L.; Yang, Z.; Liu, H. Hemoglobin-based oxygen carriers: Where are we now in 2023? Medicina 2023, 59, 396. [Google Scholar] [CrossRef]
- Zhang, Q.; Ma, Y.X.; Dai, Z.; Zhang, B.; Liu, S.S.; Li, W.X.; Fu, C.Q.; Wang, Q.M.; Yin, W. Tracking research on hemoglobin-based oxygen carriers: A scientometric analysis and in-depth review. Drug Des. Dev. Ther. 2023, 17, 2549–2571. [Google Scholar] [CrossRef]
- Varnado, C.L.; Mollan, T.L.; Birukou, I.; Smith, B.J.Z.; Henderson, D.P.; Olson, J.S. Development of recombinant hemoglobin-based oxygen carriers. Antioxid. Redox Signal. 2013, 18, 2314–2328. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Kassa, T.; Jana, S.; Wood, F.; Zhang, X.; Jia, Y.; D’Agnillo, F.; Alayash, A.I. Comprehensive biochemical and biophysical characterization of hemoglobin-based oxygen carrier therapeutics: All HBOCs are not created equally. Bioconjugate Chem. 2018, 29, 1560–1575. [Google Scholar] [CrossRef] [PubMed]
- Mohanto, N.; Monda, H.; Park, Y.J.; Jee, J.P. Therapeutic delivery of oxygen using artificial oxygen carriers demonstrates the possibility of treating a wide range of diseases. J. Nanobiotechnol. 2025, 23, 25. [Google Scholar] [CrossRef] [PubMed]
| Group | T1 | T2 | T3 | T4 | T5 | T6 | T7 | T8 |
|---|---|---|---|---|---|---|---|---|
| mHR (beats/min) | ||||||||
| Col | 206.66 ± 5.73 | 142.66 ± 2.49 | 165.60 ± 4.10 | 170.00 ± 7.07 | 186.60 ± 16.11 | 174.60 ± 8.37 | 166.60 ± 23.58 | 176.30 ± 13.07 |
| AT | 190.33 ± 1.24 | 176.66 ± 4.98 | 177.00 ± 1.63 | 183.33 ± 4.78 | 171.60 ± 27.62 | 173.66 ± 10.27 | 188.33 ± 6.23 | 240.66 ± 26.44 |
| HBOC | 194.66 ± 2.35 | 200.00 ± 1.41 | 265.00 ± 35.35 | 174.00 ± 1.41 | 208.33 ± 25.30 | 206.00 ± 4.24 | 232.00 ± 14.23 *,† | 239.00 ± 9.41 ** |
| RR (breaths/min) | ||||||||
| Col | 49.66 ± 6.84 | 41.00 ± 3.26 | 39.00 ± 2.16 | 38.33 ± 0.94 | 49.66 ± 4.49 | 46.66 ± 2.05 | 33.33 ± 5.43 | 48.33 ± 4.71 |
| AT | 31.66 ± 1.24 | 36.00 ± 1.63 | 39.00 ± 6.68 | 29.00 ± 2.16 | 38.66 ± 4.02 | 30.33 ± 1.24 | 31.33 ± 1.24 | 40.50 ± 3.5 |
| HBOC | 25.00 ± 6.48 | 24.00 ± 7.87 | 12.33 ± 3.68 | 25.33 ± 2.62 | 28.66 ± 6.12 | 36.66 ± 17.32 | 65.66 ± 14.29 | 55.66 ± 5.18 |
| T (°C) | ||||||||
| Col | 38.23 ± 0.12 | 38.20 ± 0.16 | 37.86 ± 0.26 | 37.53 ± 0.24 | 37.40 ± 0.14 | 37.36 ± 0.04 | 37.26 ± 0.32 | 37.20 ± 0.28 |
| AT | 38.96 ± 0.28 | 38.76 ± 0.12 | 38.13 ± 0.28 | 37.86 ± 0.36 | 37.76 ± 0.16 | 36.96 ± 0.09 | 38.03 ± 0.57 | 38.46 ± 0.36 ** |
| HBOC | 38.36 ± 0.68 | 38.46 ± 0.59 | 37.73 ± 0.24 | 38.06 ± 0.59 | 37.16 ± 0.61 | 37.20 ± 0.37 | 38.06 ± 0.47 | 38.36 ± 0.18 ** |
| Group | T1 | T2 | T3 | T4 | T5 | T6 | T7 | T8 |
|---|---|---|---|---|---|---|---|---|
| SAP | ||||||||
| Col | 109.33 ± 0.47 | 107.33 ± 1.69 | 84.00 ± 0.81 | 80.66 ± 1.24 | 70.33 ± 1.69 | 49.33 ± 4.92 | 55.66 ± 5.43 | 60.00 ± 10.23 |
| AT | 101.00 ± 6.97 | 86.33 ± 3.09 | 78.33 ± 3.09 | 60.66 ± 1.69 | 52.66 ± 1.69 | 50.00 ± 0.81 | 68.00 ± 1.63 | 65.00 ± 4.08 |
| HBOC | 94.66 ± 18.92 | 87.66 ± 3.85 | 74.66 ± 2.62 | 74.00 ± 16.26 | 66.00 ± 5.88 | 58.00 ± 9.09 | 80.33 ± 8.99 * | 93.66 ± 4.49 * |
| DAP | ||||||||
| Col | 84.33 ± 1.69 | 80.66 ± 0.47 | 64.00 ± 0.81 | 61.00 ± 1.63 | 58.33 ± 0.94 | 43.00 ± 1.63 | 54.66 ± 5.52 | 55.33 ± 11.61 |
| AT | 86.00 ± 0.81 | 76.00 ± 2.16 | 71.00 ± 2.94 | 55.00 ± 2.16 | 48.66 ± 0.47 | 45.33 ± 1.24 | 48.00 ± 8.83 | 48.66 ± 10.94 |
| HBOC | 89.33 ± 10.33 | 78.00 ± 12.02 | 69.00 ± 5.09 | 61.33 ± 2.49 | 50.33 ± 6.18 | 41.00 ± 1.41 | 61.00 ± 4.16 | 71.33 ± 11.48 * |
| MAP | ||||||||
| Col | 92.33 ± 1.24 | 89.00 ± 0.81 | 71.00 ± 0.81 | 67.33 ± 2.05 | 62.66 ± 1.24 | 45.66 ± 2.05 | 54.00 ± 5.71 | 57.66 ± 5.55 |
| AT | 91.00 ± 0.81 | 79.66 ± 2.05 | 73.33 ± 1.69 | 57.00 ± 0.81 | 49.33 ± 1.24 | 47.00 ± 0.81 | 55.00 ± 5.71 | 54.00 ± 10.19 |
| HBOC | 91.66 ± 13.29 | 81.00 ± 9.20 | 71.66 ± 0.47 | 65.66 ± 13.22 | 55.00 ± 4.54 | 47.00 ± 2.16 | 67.33 ± 5.83 | 78.00 ± 19.20 * |
| Group | T1 | T6 | T8 |
|---|---|---|---|
| pH | |||
| Col | 7.33 ± 0.14 | 7.12 ± 0.05 | 7.36 ± 0.14 |
| AT | 7.35 ± 0.03 | 7.15 ± 0.07 | 7.76 ± 0.15 ** |
| HBOC | 7.37 ± 0.04 | 7.11 ± 0.10 | 7.38 ± 0.07 †† |
| PCO2 (mmHg) | |||
| Col | 56.30 ± 40.87 | 48.45 ± 10.82 * | 43.05 ± 36.84 |
| AT | 54.75 ± 13.51 | 44.35 ± 12.23 * | 47.70 ± 88.67 |
| HBOC | 50.85 ± 18.88 | 43.00 ± 14.04 | 40.55 ± 27.37 |
| PO2 (mmHg) | |||
| Col | 98.20 ± 51.48 | 196.60 ± 39.03 | 112.25 ± 176.85 |
| AT | 100.25 ± 11.21 | 174.35 ± 114.76 | 110.75 ± 48.86 |
| HBOC | 95.65 ± 1.20 * | 167.75 ± 69.93 | 104.05 ± 3.45 |
| SO2 (%) | |||
| Col | 99.50 ± 3.54 | 99.50 ± 0.61 | 91.00 ± 1.41 |
| AT | 100.00 ± 0.10 | 99.50 ± 0.33 | 92.00 ± 1.41 |
| HBOC | 99.50 ± 0.71 | 99.50 ± 0.71 | 99.50 ± 0.71 †† |
| TotCO2 (mmol/L) | |||
| Col | 30.05 ± 7.71 | 49.40 ± 0.99 | 29.15 ± 5.40 |
| AT | 31.40 ± 5.52 | 48.90 ± 3.96 | 38.85 ± 0.92 ** |
| HBOC | 28.50 ± 4.42 | 46.20 ± 2.06 | 19.55 ± 3.65 †† |
| BE ecf (mmol/L) | |||
| Col | 3.65 ± 1.17 | −7.80 ± 0.14 | 1.25 ± 6.01 |
| AT | 3.00 ± 3.68 | −8.90 ± 0.57 | 7.70 ± 0.99 ** |
| HBOC | 2.05 ± 4.35 | −9.55 ± 3.12 | −1.90 ± 11.74 †† |
| Group | T1 | T6 | T8 |
|---|---|---|---|
| O2Hb (%) | |||
| Col | 94.23 ± 3.10 | 98.43 ± 1.08 | 92.63 ± 0.61 |
| AT | 99.36 ± 0.12 | 98.23 ± 0.80 | 93.30 ± 0.61 |
| HBOC | 99.16 ± 0.44 | 97.73 ± 0.38 | 97.93 ± 0.23 †† |
| COHb (%) | |||
| Col | 0.93 ± 0.68 | 0.96 ± 0.87 | 1.66 ± 0.88 |
| AT | 0.26 ± 0.04 | 0.50 ± 0.08 | 1.13 ± 0.12 |
| HBOC | 0.30 ± 0.08 | 0.63 ± 0.04 | 1.10 ± 0.08 |
| MetHb (%) | |||
| Col | 0.36 ± 0.04 | 0.33 ± 0.04 | 0.43 ± 0.04 |
| AT | 0.26 ± 0.04 | 0.20 ± 278 × 10−17 | 0.46 ± 0.04 |
| HBOC | 0.33 ± 0.04 | 0.30 ± 0.14 | 0.43 ± 0.12 |
| Hgb (g/dL) | |||
| Col | 11.50 ± 0.99 | 6.95 ± 0.35 | 5.40 ± 1.13 |
| AT | 11.05 ± 1.48 | 6.80 ± 2.26 | 8.20 ± 1.84 ** |
| HBOC | 11.25 ± 0.92 | 6.15 ± 0.21 | 6.00 ± 0.28 †† |
| HCT (%) | |||
| Col | 35.00 ± 1.41 | 25.00 ± 1.41 | 17.00 ± 5.66 |
| AT | 34.00 ± 4.24 | 20.00 ± 1.41 | 25.00 ± 1.41 ** |
| HBOC | 34.50 ± 2.12 | 24.00 ± 1.41 | 21.00 ± 0.00 †† |
| Group | T1 | T6 | T8 |
|---|---|---|---|
| Na (mmol/L) | |||
| Col | 146.10 ± 5.66 | 143.90 ± 1.27 | 143.40 ± 3.39 |
| AT | 143.55 ± 2.76 | 143.80 ± 2.83 | 147.10 ± 6.51 |
| HBOC | 138.80 ± 2.83 | 138.25 ± 4.45 | 139.85 ± 5.30 |
| K (mmol/L) | |||
| Col | 3.53 ± 0.42 | 4.18 ± 0.80 | 3.97 ± 0.30 |
| AT | 3.95 ± 0.33 | 3.96 ± 0.04 | 4.69 ± 0.79 |
| HBOC | 3.80 ± 0.15 | 4.24 ± 0.23 | 4.29 ± 0.08 |
| iCa (mmol/L) | |||
| Col | 1.62 ± 0.04 | 1.54 ± 0.14 | 1.43 ± 0.13 |
| AT | 1.63 ± 0.14 | 1.55 ± 0.02 | 1.40 ± 0.02 |
| HBOC | 1.59 ± 0.01 | 1.33 ± 0.04 | 1.22 ± 0.00 †† |
| iMg (mmol/L) | |||
| Col | 0.61 ± 0.03 | 0.64 ± 0.13 | 0.60 ± 0.01 |
| AT | 0.61 ± 0.01 | 0.73 ± 0.02 | 0.70 ± 0.01 ** |
| HBOC | 0.70 ± 0.04 | 0.81 ± 0.08 | 0.65 ± 0.17 |
| Glucose (mg/dL) | |||
| Col | 166.00 ± 80.61 | 167.50 ± 45.96 | 147.50 ± 79.9 |
| AT | 155.00 ± 26.87 | 153.00 ± 15.56 | 193.00 ± 2.83 |
| HBOC | 167.00 ± 93.34 | 164.00 ± 18.38 | 135.50 ± 33.23 |
| Cl (mmol/L) | |||
| Col | 105.05 ± 0.21 | 104.90 ± 0.85 | 107.60 ± 1.41 |
| AT | 107.45 ± 8.13 | 106.20 ± 0.71 | 110.20 ± 0.42 |
| HBOC | 105.45 ± 5.44 | 103.90 ± 4.38 | 105.55 ± 2.19 |
| AnGap (mmol/L) | |||
| Col | 11.25 ± 1.34 | 26.45 ± 2.33 | 13.22 ± 5.87 |
| AT | 11.50 ± 1.56 | 25.05 ± 1.34 | 14.15 ± 2.90 |
| HBOC | 12.50 ± 5.37 | 26.70 ± 12.30 | 20.35 ± 5.16 ††,** |
| Group | T1 | T6 | T8 |
|---|---|---|---|
| Creatinine (mg/dL) | |||
| Col | 0.90 ± 0.28 | 1.20 ± 0.28 | 1.05 ± 0.07 |
| AT | 0.90 ± 0.14 | 0.90 ± 0.28 | 0.85 ± 0.07 ** |
| HBOC | 1.00 ± 0.07 | 1.20 ± 0.07 | 1.25 ± 0.21 † |
| BUN (mg/dL) | |||
| Col | 22.50 ± 0.71 | 25.00 ± 4.24 | 25.50 ± 3.54 |
| AT | 24.00 ± 1.41 | 24.50 ± 0.71 | 28.50 ± 0.71 |
| HBOC | 24.00 ± 0 | 25.00 ± 1.41 | 27.00 ± 7.07 |
| Tot Bilirubin | |||
| Col | 1.20 ± 0.99 | 0.95 ± 0.49 | 0.50 ± 0.49 |
| AT | 0.65 ± 0.21 | 0.50 ± 0.14 | 0.85 ± 0.07 |
| HBOC | 0.95 ± 0.64 | 0.80 ± 0.42 | 1.10 ± 0.57 |
| Lactate (mmol/L) | |||
| Col | 0.90 ± 0.07 | 2.20 ± 1.56 | 2.05 ± 0.07 |
| AT | 1.00 ± 0.28 | 2.19 ± 0.57 | 2.15 ± 0.35 |
| HBOC | 0.70 ± 0.28 | 2.15 ± 0.49 | 3.00 ± 1.27 ** |
| Group | T1 | T2 | T3 | T4 | T5 | T6 | T7 | T8 |
|---|---|---|---|---|---|---|---|---|
| SO2% | ||||||||
| Col | 99.66 ± 1.24 | 100.00 ± 0.00 | 99.33 ± 0.94 | 99.33 ± 0.47 | 99.33 ± 0.47 | 98.33 ± 0.47 | 98.00 ± 2.82 | 98.00 ± 2.82 |
| AT | 99.00 ± 0.81 | 99.66 ± 1.24 | 98.00 ± 0.81 | 99.66 ± 0.47 | 98.33 ± 1.69 | 99.33 ± 0.47 | 98.00 ± 0.81 | 98.00 ± 4.32 |
| HBOC | 99.00 ± 0.00 | 99.66 ± 0.47 | 99.33 ± 0.47 | 99.66 ± 0.47 | 99.33 ± 0.47 | 96.00 ± 2.82 | 99.00 ± 0.81 | 98.66 ± 1.24 |
| ETCO2 | ||||||||
| Col | 31.33 ± 6.37 | 35.00 ± 0.47 | 30.33 ± 3.74 | 26.00 ± 2.62 | 26.33 ± 2.16 | 26.00 ± 2.62 | 38.33 ± 2.05 | 49.66 ± 9.53 |
| AT | 35.33 ± 6.62 | 32.33 ± 4.02 | 28.33 ± 2.05 | 24.66 ± 4.49 | 25.66 ± 3.39 | 26.33 ± 4.49 | 34.66 ± 1.69 | 52.66 ± 0.94 |
| HBOC | 34.33 ± 19.15 | 37.66 ± 3/39 | 30.33 ± 8.73 | 27.66 ± 8.04 | 26.00 ± 9.28 | 27.66 ± 3.69 | 34.33 ± 5.88 | 49.00 ± 4.54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dandea, Ș.-M.; Hașaș, A.-D.; Toma, V.-A.; Lehene, M.; Scurtu, F.; Peștean, C.P.; Codea, R.-A.; Bel, L.-V.; Melega, I.; Silaghi-Dumitrescu, R.; et al. Veterinary Perspectives on Hemoglobin-Based Oxygen Carriers in Experimental Hemorrhagic Shock: Insights from Rabbit Models. Vet. Sci. 2025, 12, 485. https://doi.org/10.3390/vetsci12050485
Dandea Ș-M, Hașaș A-D, Toma V-A, Lehene M, Scurtu F, Peștean CP, Codea R-A, Bel L-V, Melega I, Silaghi-Dumitrescu R, et al. Veterinary Perspectives on Hemoglobin-Based Oxygen Carriers in Experimental Hemorrhagic Shock: Insights from Rabbit Models. Veterinary Sciences. 2025; 12(5):485. https://doi.org/10.3390/vetsci12050485
Chicago/Turabian StyleDandea, Ștefania-Mădălina, Alina-Diana Hașaș, Vlad-Alexandru Toma, Maria Lehene, Florina Scurtu, Cosmin Petru Peștean, Răzvan-Andrei Codea, Lucia-Victoria Bel, Iulia Melega, Radu Silaghi-Dumitrescu, and et al. 2025. "Veterinary Perspectives on Hemoglobin-Based Oxygen Carriers in Experimental Hemorrhagic Shock: Insights from Rabbit Models" Veterinary Sciences 12, no. 5: 485. https://doi.org/10.3390/vetsci12050485
APA StyleDandea, Ș.-M., Hașaș, A.-D., Toma, V.-A., Lehene, M., Scurtu, F., Peștean, C. P., Codea, R.-A., Bel, L.-V., Melega, I., Silaghi-Dumitrescu, R., & Sevastre, B. (2025). Veterinary Perspectives on Hemoglobin-Based Oxygen Carriers in Experimental Hemorrhagic Shock: Insights from Rabbit Models. Veterinary Sciences, 12(5), 485. https://doi.org/10.3390/vetsci12050485









