An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver
Abstract
1. Introduction
2. Mathematical Model
3. Methodology
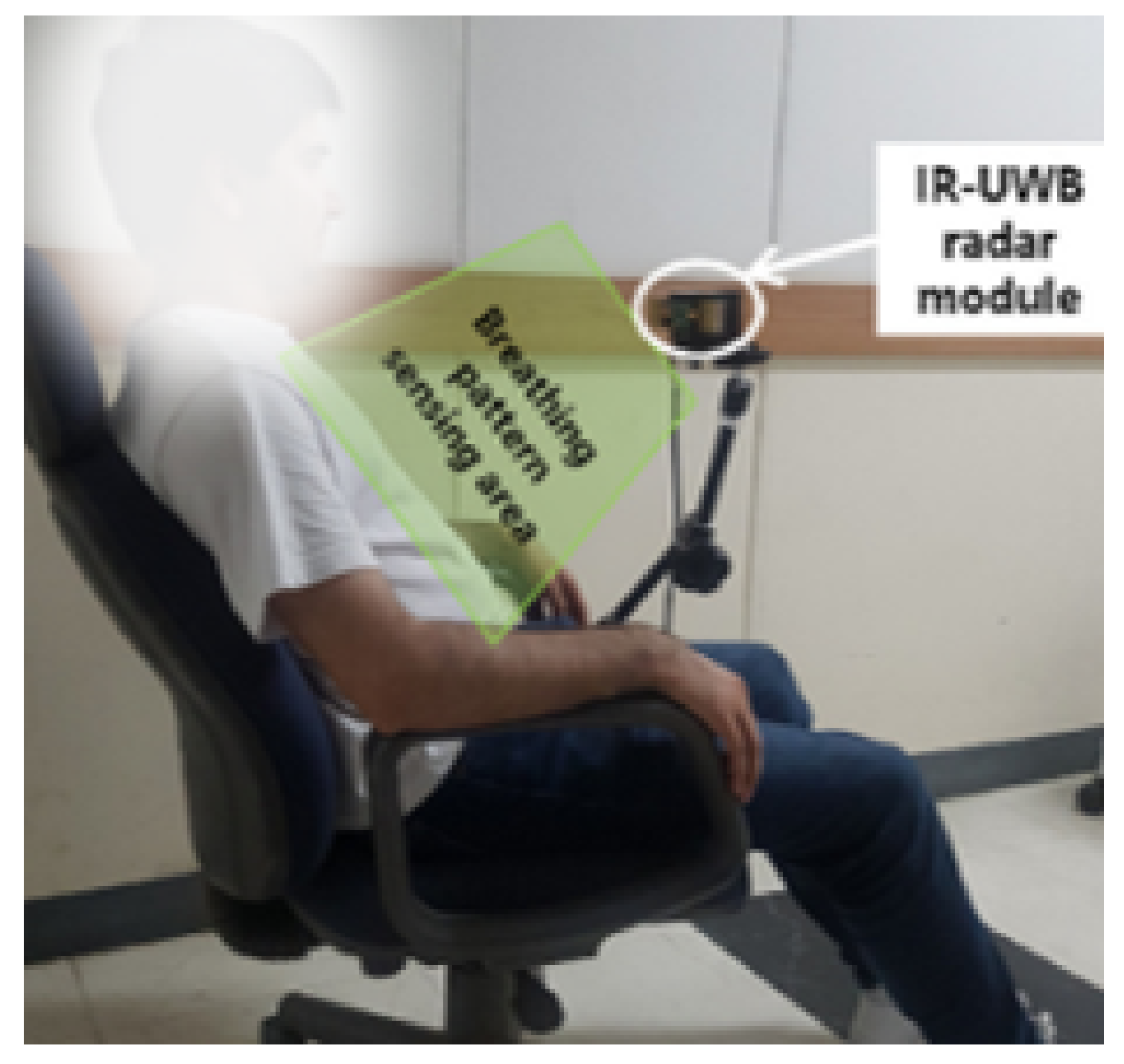
3.1. Hardware Setup
3.2. Pre-Processing of the Radar Signals before Vital Signs Extraction
3.2.1. Signal Model
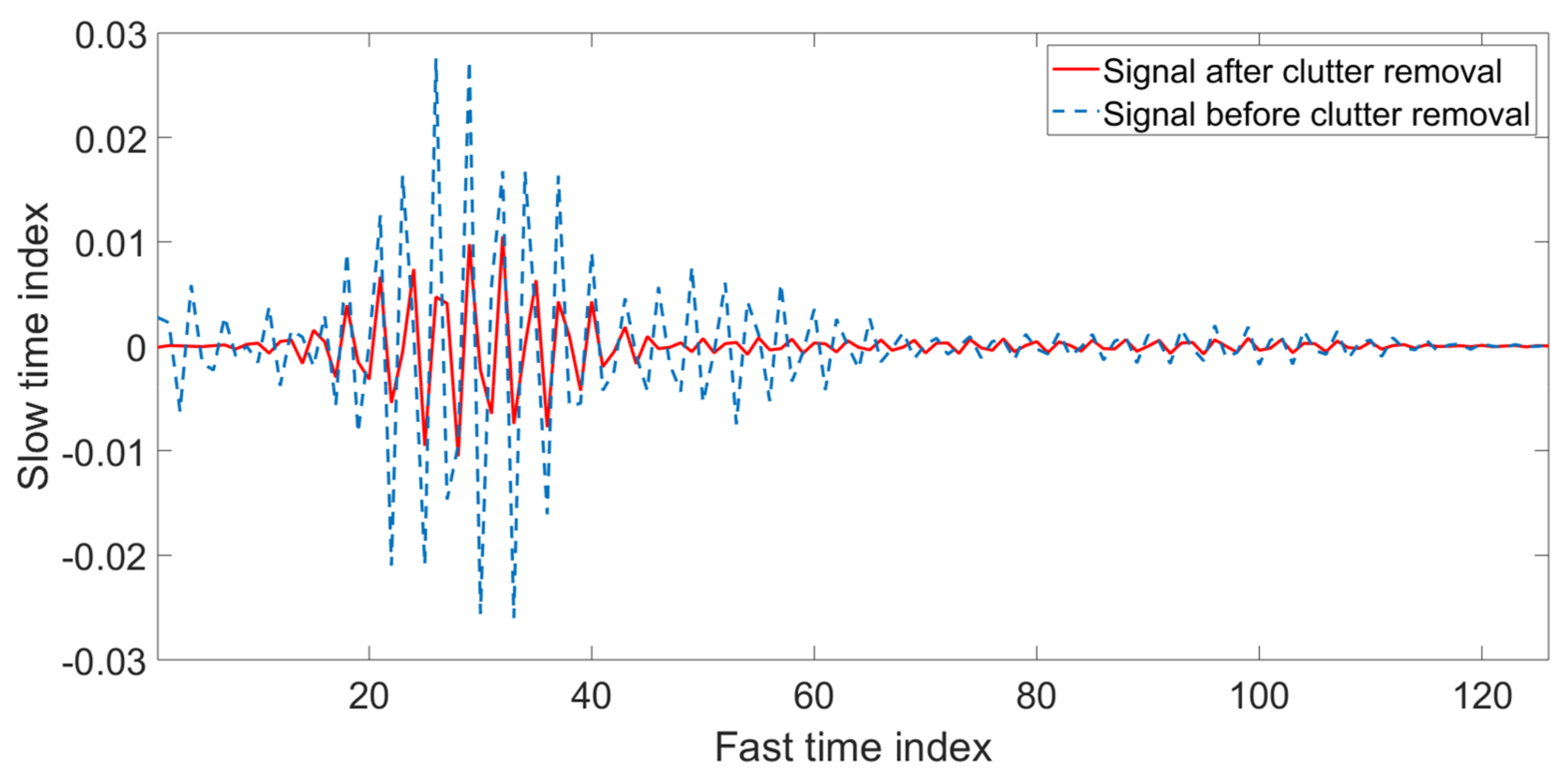
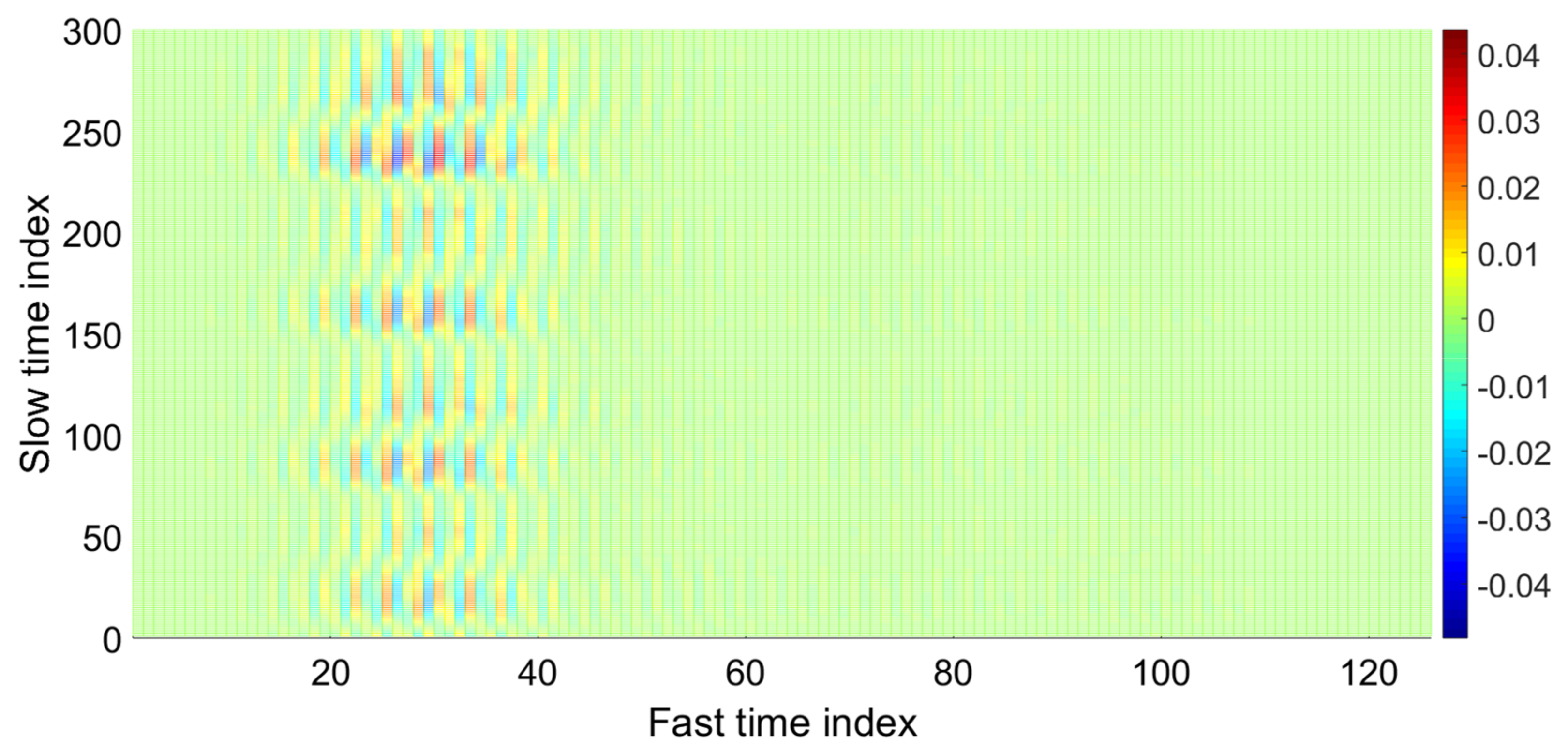
3.2.2. Clutter Removal
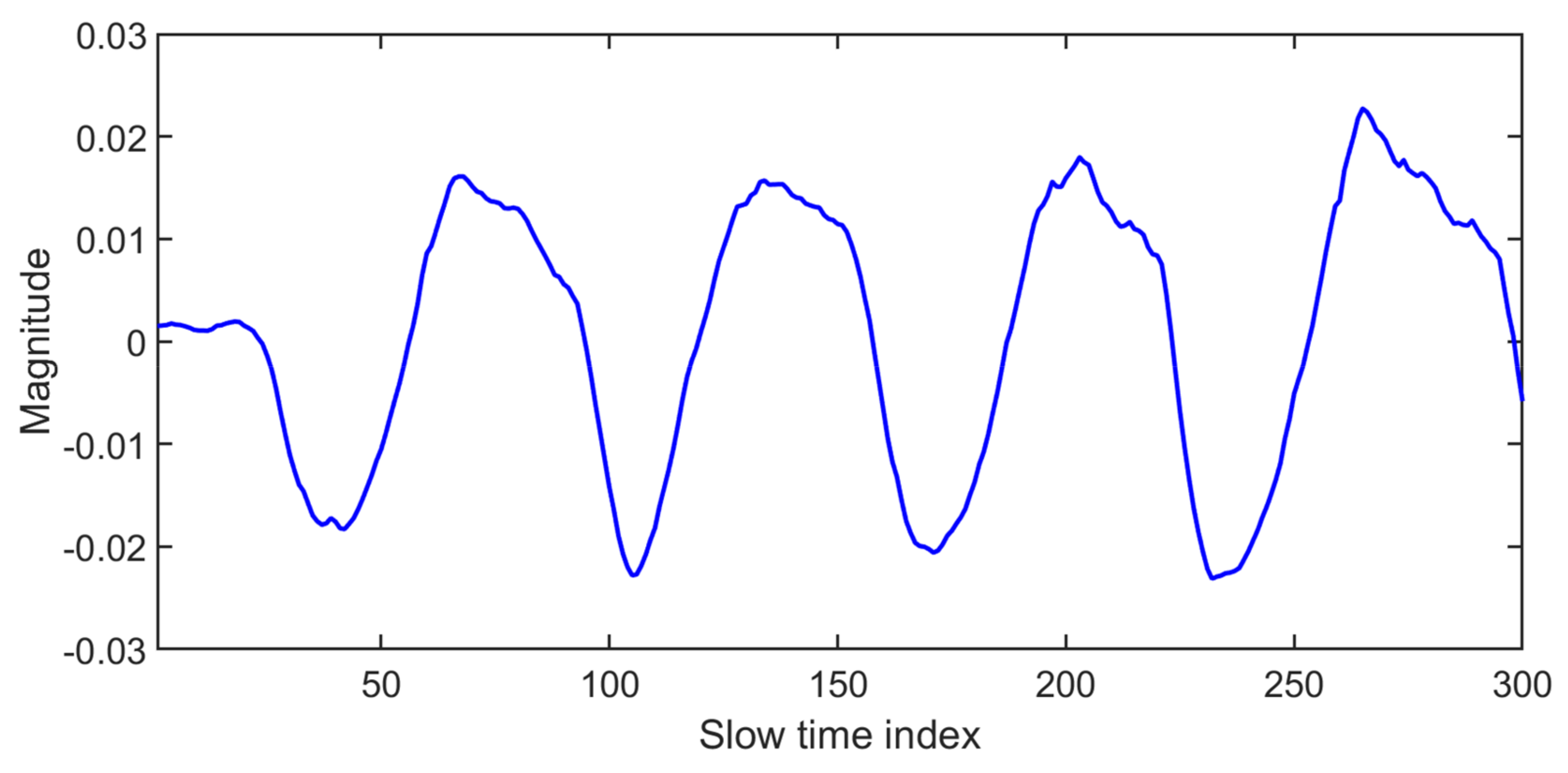
3.2.3. Vital Signal Detection in Time Domain
4. Respiration and Heart Rate Measurement
4.1. Vital Signs Detection Using Frequency Analysis
4.2. Previous Work Related to Vital Signs Extraction from Radar Data
5. Vital Signs of a Non-Stationary Subject
6. Vital Signs Inside Vehicles
7. Sleep Monitoring
8. Through the Wall Vital Signs
9. Vital Signs of Neonates
10. Other Medical Applications
10.1. Medical Imaging
10.2. Fall Detection
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fontana, R.J. Recent system applications of short-pulse ultra-wideband (UWB) technology. IEEE Trans. Microw. Theory Tech. 2004, 52, 2087–2104. [Google Scholar]
- Ghavami, M.; Michael, L.; Kohno, R. Ultra Wideband Signals and Systems in Communication Engineering; John Wiley & Sons: Hoboken, NJ, USA, 2007. [Google Scholar]
- Fernandes, J.R.; Wentzloff, D.D. >Recent advances in IR-UWB transceivers: An overview. In Proceedings of the 2010 IEEE International Symposium on Circuits and Systems, Paris, France, 30 May–2 June 2010. [Google Scholar]
- Lazaro, A.; Girbau, D.; Villarino, R. Analysis of vital signs monitoring using an IR-UWB radar. Prog. Electromagn. Res. 2010, 100, 265–284. [Google Scholar]
- Espes, D.; Pistea, A.M.; Canaff, C.; Iordache, I.; Parc, P.L.; Radoi, E. New method for localization and human being detection using UWB technology: Helpful solution for rescue robots. arXiv 2013, arXiv:1312.4162. [Google Scholar]
- Li, C.; Lin, J.; Boric-Lubecke, O.; Lubecke, V.M.; Host-Madsen, A.; Park, B.K. Development of non-contact physiological motion sensor on CMOS chip and its potential applications. In Proceedings of the IEEE 2007 7th International Conference on ASIC, Guilin, China, 22–25 October 2007. [Google Scholar]
- Yim, D.; Lee, W.H.; Kim, J.I.; Kim, K.; Ahn, D.H.; Lim, Y.H.; Cho, S.H.; Park, H.K.; Cho, S.H. Quantified Activity Measurement for Medical Use in Movement Disorders through IR-UWB Radar Sensor. Sensors 2019, 19, 688. [Google Scholar]
- Shikhsarmast, F.M.; Lyu, T.; Liang, X.; Zhang, H.; Gulliver, T.A. Random-Noise Denoising and Clutter Elimination of Human Respiration Movements Based on an Improved Time Window Selection Algorithm Using Wavelet Transform. Sensors 2019, 19, 95. [Google Scholar]
- Khan, F.; Cho, S. A detailed algorithm for vital sign monitoring of a stationary/non-stationary human through ir-uwb radar. Sensors 2017, 17, 290. [Google Scholar]
- Tariq, A.; Zahid, A.; Khan, U.; Khan, N.; Khan, F. Implementation of Wavelet transform for monitoring of vital signs through IR-UWB Radar. In Proceedings of the IEEE 2017 International Conference on Communication, Computing and Digital Systems (C-CODE), Islamabad, Pakistan, 8–9 March 2017. [Google Scholar]
- Khan, N.; Khan, K.; Khan, A.; Alam, I.; Khan, F.U.; Khan, S.U.; Ali, A. Accommodate Data Loss in Monitoring Vital Signs Through Autoregressive Model. J. Med. Imaging Health Inform. 2019, 9, 1205–1214. [Google Scholar]
- Yan, J.; Zhao, H.; Li, Y.; Sun, L.; Hong, H.; Zhu, X. Through-the-wall human respiration detection using impulse ultra-wide-band radar. In Proceedings of the 2016 IEEE Topical Conference on Biomedical Wireless Technologies, Networks, and Sensing Systems (BioWireleSS), Austin, TX, USA, 24–27 January 2016. [Google Scholar]
- Lin, J.C. Noninvasive microwave measurement of respiration. Proc. IEEE 1975, 63, 1530. [Google Scholar]
- Li, C.; Un, K.F.; Mak, P.I.; Chen, Y.; Muñoz-Ferreras, J.M.; Yang, Z.; Gómez-García, R. Overview of recent development on wireless sensing circuits and systems for healthcare and biomedical applications. IEEE J. Emerg. Sel. Top. Circuits Syst. 2018, 8, 165–177. [Google Scholar]
- Cho, H.-S.; Park, Y.-J.; Lyu, H.-K. Robust heart rate detection method using UWB impulse radar. In Proceedings of the IEEE 2016 International Conference on Information and Communication Technology Convergence (ICTC), Jeju, Korea, 19–21 October 2016. [Google Scholar]
- Leem, S.K.; Khan, F.; Cho, S.H. Vital sign monitoring and mobile phone usage detection using IR-UWB radar for intended use in car crash prevention. Sensors 2017, 17, 1240. [Google Scholar]
- Ren, L.; Wang, H.; Naishadham, K.; Kilic, O.; Fathy, A.E. Phase-based methods for heart rate detection using UWB impulse Doppler radar. IEEE Trans. Microw. Theory Tech. 2016, 64, 3319–3331. [Google Scholar]
- Tumalskis, M. Application of UWB radar for human respiration monitoring. Biomed. Eng. 2016, 19, 39–44. [Google Scholar]
- Wisland, D.T.; Granhaug, K.; Pleym, J.R.; Andersen, N.; Støa, S.; Hjortland, H.A. Remote monitoring of vital signs using a CMOS UWB radar transceiver. In Proceedings of the 2016 14th IEEE International New Circuits and Systems Conference (NEWCAS), Vancouver, BC, Canada, 26–29 June 2016. [Google Scholar]
- Zito, D.; Pepe, D.; Mincica, M.; Zito, F. A 90nm CMOS SoC UWB pulse radar for respiratory rate monitoring. In Proceedings of the 2011 IEEE International Solid-State Circuits Conference, San Francisco, CA, USA, 20–24 February 2011. [Google Scholar]
- Fear, E.C.; Li, X.; Hagness, S.C.; Stuchly, M.A. Confocal microwave imaging for breast cancer detection: Localization of tumors in three dimensions. IEEE Trans. Biomed. Eng. 2002, 49, 812–822. [Google Scholar] [PubMed]
- Hagness, S.C.; Taflove, A.; Bridges, J.E. Two-dimensional FDTD analysis of a pulsed microwave confocal system for breast cancer detection: Fixed-focus and antenna-array sensors. IEEE Trans. Biomed. Eng. 1998, 45, 1470–1479. [Google Scholar]
- Wang, P.; Qi, F.; Liu, M.; Liang, F.; Xue, H.; Zhang, Y.; Lv, H.; Wang, J. Noncontact Heart Rate Measurement Based on an Improved Convolutional Sparse Coding Method Using IR-UWB Radar. IEEE Access 2019, 7, 158492–158502. [Google Scholar]
- Kang, S.; Kim, D.K.; Lee, Y.; Lim, Y.H.; Park, H.K.; Cho, S.H.; Cho, S.H. Non-contact diagnosis of obstructive sleep apnea using impulse-radio ultra-wideband radar. Sci. Rep. 2020, 10, 1–7. [Google Scholar]
- Choi, J.W.; Nam, S.S.; Cho, S.H. Multi-human detection algorithm based on an impulse radio ultra-wideband radar system. IEEE Access 2016, 4, 10300–10309. [Google Scholar]
- Kota, J.S.; Papandreou-Suppappola, A. Joint Design of Transmit Waveforms for Object Tracking in Coexisting Multimodal Sensing Systems. Sensors 2019, 19, 1753. [Google Scholar]
- Ghaffar, A.; Khan, F.; Cho, S.H. Hand Pointing Gestures Based Digital Menu Board Implementation Using IR-UWB Transceivers. IEEE Access 2019, 7, 58148–58157. [Google Scholar]
- Ahmed, S.; Khan, F.; Ghaffar, A.; Hussain, F.; Cho, S.H. Finger-Counting-Based Gesture Recognition within Cars Using Impulse Radar with Convolutional Neural Network. Sensors 2019, 19, 1429. [Google Scholar]
- Leem, S.K.; Khan, F.; Cho, S.H. Detecting Mid-air Gestures for Digit Writing with Radio Sensors and a CNN. IEEE Trans. Instrum. Meas. 2019, 69, 1066–1081. [Google Scholar]
- Khan, F.; Leem, S.K.; Cho, S.H. Hand-based gesture recognition for vehicular applications using IR-UWB radar. Sensors 2017, 17, 833. [Google Scholar]
- Wang, D.; Leem, S.K.; Cho, S.H. 3D Shape Reconstruction Method for Multiple Aspects Using MIMO IR-UWB Radar System. In Proceedings of the IEEE 2018 9th International Conference on Ultrawideband and Ultrashort Impulse Signals (UWBUSIS), Odessa, Ukraine, 4–7 September 2018. [Google Scholar]
- Leem, S.K.; Wang, D.; Cho, S.H. An image quality improvement method under sparse array and small bandwidth in mimo ir-uwb imaging system. In Proceedings of the IEEE 2017 18th International Radar Symposium (IRS), Prague, Czech Republic, 28–30 June 2017. [Google Scholar]
- Williams, T.C.; Fear, E.C.; Westwick, D.T. Tissue sensing adaptive radar for breast cancer detection-investigations of an improved skin-sensing method. IEEE Trans. Microw. Theory Tech. 2006, 54, 1308–1314. [Google Scholar]
- Lazaro, A.; Girbau, D.; Villarino, R. Weighted centroid method for breast tumor localization using an UWB radar. Prog. Electromagn. Res. 2010, 24, 1–15. [Google Scholar]
- Fear, E.; Okoniewski, M.; Stuchly, M. Tissue Sensing Adaptive Radar Imaging for Breast Tumor Detection. U.S. Patent No. 7,454,242; Patent and Trademark Office, 18 November 2008. [Google Scholar]
- Li, X.; Bond, E.J.; Van Veen, B.D.; Hagness, S.C. An overview of ultra-wideband microwave imaging via space-time beamforming for early-stage breast-cancer detection. IEEE Antennas Propag. Mag. 2005, 47, 19–34. [Google Scholar]
- Hein, M.A. Ultra-wideband radar sensors for biomedical diagnostics and imaging. In Proceedings of the 2012 IEEE International Conference on Ultra-Wideband, Syracuse, NY, USA, 17–20 September 2012. [Google Scholar]
- Choi, J.W.; Yim, D.H.; Cho, S.H. People counting based on an IR-UWB radar sensor. IEEE Sens. J. 2017, 17, 5717–5727. [Google Scholar]
- Yue, W.; Zhang, Y.; Liu, Y.; Xie, J. Radar constant-modulus waveform design with prior information of the extended target and clutter. Sensors 2016, 16, 889. [Google Scholar]
- Leem, S.K.; Khan, F.; Cho, S.H. Remote Authentication Using an Ultra-Wideband Radio Frequency Transceiver. In Proceedings of the 2020 IEEE 17th Annual Consumer Communications & Networking Conference (CCNC), Las Vegas, NV, USA, 10–13 January 2020. [Google Scholar]
- Chiani, M.; Giorgetti, A.; Paolini, E. Sensor radar for object tracking. Proc. IEEE 2018, 106, 1022–1041. [Google Scholar]
- Praveen, S.; Raoul, O.; Bradley, P.; David, A.; Todd, L.; Daniel, S.; Jonathan, K. Miniature radar for mobile devices. In Proceedings of the 2013 IEEE High Performance Extreme Computing Conference (HPEC), Waltham, MA, USA, 10–12 September 2013. [Google Scholar]
- Skolnik, M.I. Radar Handbook; McGraw-Hill Publishing Company Professional: New York, NY, USA, 1970. [Google Scholar]
- Mcewan, T.E. Ultra-wideband Radar Motion Sensor. U.S. Patent No. 5,361,070, 1 November 1994. [Google Scholar]
- Lee, Y.; Park, J.Y.; Choi, Y.W.; Park, H.K.; Cho, S.H.; Cho, S.H.; Lim, Y.H. A Novel Non-contact Heart Rate Monitor Using Impulse-Radio Ultra-Wideband (IR-UWB) Radar Technology. Sci. Rep. 2018, 8, 13053. [Google Scholar]
- Creditor, M.C. Hazards of hospitalization of the elderly. Ann. Intern. Med. 1993, 118, 219–223. [Google Scholar]
- Sun, G.; Gotoh, S.; Zhao, Z.; Kim, S.; Suzuki, S.; Imamoglu, N.; Yu, W.; Matsui, T. Vital-CUBE: A non-contact vital sign monitoring system using medical radar for ubiquitous home healthcare. J. Med. Imaging Health Inform. 2014, 4, 863–867. [Google Scholar]
- Hamalainen, M.; Pirinen, P.; Iinatti, J.; Taparugssanagorn, A. UWB supporting medical ICT applications. In Proceedings of the 2008 IEEE International Conference on Ultra-Wideband, Hannover, Germany, 10–12 September 2008. [Google Scholar]
- Singh, M.; Ramachandran, G. Reconstruction of sequential cardiac in-plane displacement patterns on the chest wall by laser speckle interferometry. IEEE Trans. Biomed. Eng. 1991, 38, 483–489. [Google Scholar] [PubMed]
- Kondo, T.; Uhlig, T.; Pemberton, P.; Sly, P.D. Laser monitoring of chest wall displacement. Eur. Respir. J. 1997, 10, 1865–1869. [Google Scholar] [PubMed]
- Li, C.; Lin, J. Recent advances in Doppler radar sensors for pervasive healthcare monitoring. In Proceedings of the IEEE 2010 Asia-Pacific Microwave Conference, Yokohama, Japan, 7–10 December 2010. [Google Scholar]
- Venkatesh, S.; Anderson, C.R.; Rivera, N.V.; Buehrer, R.M. Implementation and analysis of respiration-rate estimation using impulse-based UWB. In Proceedings of the MILCOM 2005–2005 IEEE Military Communications Conference, Atlantic City, NJ, USA, 17–20 October 2005. [Google Scholar]
- Cramer, R.-M.; Scholtz, R.A.; Win, M.Z. Evaluation of an ultra-wide-band propagation channel. IEEE Trans. Antennas Propag. 2002, 50, 561–570. [Google Scholar]
- Yim, H.D.; Cho, H.S. An equidistance multi-human detection algorithm based on noise level using mono-static IR-UWB radar system. In Future Communication, Information and Computer Science, Proceedings of the 2014 International Conference on Future Communication, Information and Computer Science (FCICS 2014), Beijing, China, 22–23 May 2014; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Khan, F.; Choi, J.W.; Cho, S.H. Design issues in vital sign monitoring through IR UWB radar. In Proceedings of the 18th IEEE International Symposium on Consumer Electronics (ISCE 2014), JeJu Island, Korea, 22–25 June 2014. [Google Scholar]
- Khan, F.; Leem, S.K.; Cho, S.H. Human–computer interaction using radio sensor for people with severe disability. Sens. Actuators A Phys. 2018, 282, 39–54. [Google Scholar]
- Liang, X.; Zhang, H.; Ye, S.; Fang, G.; Gulliver, T.A. Improved denoising method for through-wall vital sign detection using UWB impulse radar. Digit. Signal Proc. 2018, 74, 72–93. [Google Scholar]
- Khan, F.; Cho, S.H. Hand based Gesture Recognition inside a car through IR-UWB Radar. In Proceedings of the International Conference on Electronics Information and Communication, Phuket, Thailand, 11–14 January 2017; pp. 154–157. [Google Scholar]
- Lazaro, A.; Girbau, D.; Villarino, R.; Ramos, A. Vital signs monitoring using impulse based UWB signal. In Proceedings of the IEEE 2011 41st European Microwave Conference, Manchester, UK, 10–13 October 2011. [Google Scholar]
- El-Bardan, R.; Malaviya, D.; di Rienzo, A. On the estimation of respiration and heart rates via an IR-UWB radar: An algorithmic perspective. In Proceedings of the 2017 IEEE International Conference on Microwaves, Antennas, Communications and Electronic Systems (COMCAS), Tel-Aviv, Israel, 13–15 November 2017. [Google Scholar]
- Shyu, K.K.; Chiu, L.J.; Lee, P.L.; Tung, T.H.; Yang, S.H. Detection of breathing and heart rates in UWB radar sensor data using FVPIEF-based two-layer EEMD. IEEE Sens. J. 2018, 19, 774–784. [Google Scholar]
- Baboli, M.; Ghorashi, S.A.; Saniei, N.; Ahmadian, A. A new wavelet based algorithm for estimating respiratory motion rate using UWB radar. In Proceedings of the IEEE 2009 International Conference on Biomedical and Pharmaceutical Engineering, Singapore, 2–4 December 2009. [Google Scholar]
- Conte, E.; Filippi, A.; Tomasin, S. ML period estimation with application to vital sign monitoring. IEEE Signal Proc. Lett. 2010, 17, 905–908. [Google Scholar]
- Lohman, B.; Boric-Lubecke, O.; Lubecke, V.M.; Ong, P.W.; Sondhi, M.M. A digital signal processor for Doppler radar sensing of vital signs. IEEE Eng. Med. Biol. Mag. 2002, 21, 161–164. [Google Scholar]
- Li, C.; Chen, F.; Jin, J.; Lv, H.; Li, S.; Lu, G.; Wang, J. A method for remotely sensing vital signs of human subjects outdoors. Sensors 2015, 15, 14830–14844. [Google Scholar]
- He, M.; Nian, Y.; Gong, Y. Novel signal processing method for vital sign monitoring using FMCW radar. Biomed. Signal Proc. Control 2017, 33, 335–345. [Google Scholar]
- Cavagnaro, M.; Pittella, E.; Pisa, S. UWB pulse propagation into human tissues. Phys. Med. Biol. 2013, 58, 8689. [Google Scholar] [PubMed]
- Leib, M.; Menzel, W.; Schleicher, B.; Schumacher, H. Vital signs monitoring with a UWB radar based on a correlation receiver. In Proceedings of the IEEE Fourth European Conference on Antennas and Propagation, Barcelona, Spain, 12–16 April 2010. [Google Scholar]
- Huang, J.Y.; Hsu, C.C.; Chang, C.H.; Hu, W.W. Non-Contact and Real-Time Pulse-Based Radar with Sensitivity Improvement for Vital-Sign Monitoring. In Proceedings of the IEEE 2018 Asia-Pacific Microwave Conference (APMC), Kyoto, Japan, 6–9 November 2018. [Google Scholar]
- Nguyen, V.; Javaid, A.Q.; Weitnauer, M.A. Harmonic Path (HAPA) algorithm for non-contact vital signs monitoring with IR-UWB radar. In Proceedings of the 2013 IEEE Biomedical Circuits and Systems Conference (BioCAS), Rotterdam, The Netherlands, 31 October–2 November 2013. [Google Scholar]
- Nguyen, V.; Javaid, A.Q.; Weitnauer, M.A. Spectrum-averaged Harmonic Path (SHAPA) algorithm for non-contact vital sign monitoring with ultra-wideband (UWB) radar. In Proceedings of the IEEE 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014. [Google Scholar]
- Xu, Y.; Dai, S.; Wu, S.; Chen, J.; Fang, G. Vital sign detection method based on multiple higher order cumulant for ultrawideband radar. IEEE Trans. Geosci. Remote Sens. 2011, 50, 1254–1265. [Google Scholar]
- Richards, J.L.; Fullerton, L.W.; Kelly, D.A.; Meigs, D.C.; Payment, T.T.; Finn, J.S.; Tucker, W.J.; Welch, W.D., Jr. System and Method Using Impulse Radio Technology to Track and Monitor People Needing Health Care. U.S. Patent No. 6,466,125, 15 October 2002. [Google Scholar]
- Zito, D.; Pepe, D.; Neri, B.; De Rossi, D.; Lanata, A.; Tognetti, A.; Scilingo, E.P. Wearable system-on-a-chip UWB radar for health care and its application to the safety improvement of emergency operators. In Proceedings of the IEEE 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007. [Google Scholar]
- Shen, H.; Xu, C.; Yang, Y.; Sun, L.; Cai, Z.; Bai, L.; Clancy, E.; Huang, X. Respiration and Heartbeat Rates Measurement Based on Autocorrelation Using IR-UWB Radar. IEEE Trans. Circuits Syst. II Express Briefs 2018, 65, 1470–1474. [Google Scholar]
- Liang, X.; Wang, Y.; Wu, S.; Gulliver, T.A. Experimental study of wireless monitoring of human respiratory movements using UWB impulse radar systems. Sensors 2018, 18, 3065. [Google Scholar]
- Zhang, Y.; Li, X.; Qi, R.; Qi, Z.; Zhu, H. Harmonic Multiple Loop Detection (HMLD) Algorithm for Not-Contact Vital Sign Monitoring Based on Ultra-Wideband (UWB) Radar. IEEE Access 2020, 8, 38786–38793. [Google Scholar]
- Khan, F.; Choi, J.W.; Cho, S.H. Vital sign monitoring of a non-stationary human through IR-UWB radar. In Proceedings of the 2014 4th IEEE International Conference on Network Infrastructure and Digital Content, Beijing, China, 19–21 September 2014. [Google Scholar]
- Adjrad, M.; Dudley, S.; Ghavami, M. Experimental vital signs estimation using commercially available IR-UWB radar. In Proceedings of the IEEE 2014 International Radar Conference, Lille, France, 13–17 October 2014. [Google Scholar]
- Yin, W.; Yang, X.; Li, L.; Zhang, L.; Kitsuwan, N.; Oki, E. Hear: Approach for heartbeat monitoring with body movement compensation by ir-uwb radar. Sensors 2018, 18, 3077. [Google Scholar]
- Eren, C.; Karamzadeh, S.; Kartal, M. The artifacts of human physical motions on vital signs monitoring. In Proceedings of the IEEE 2019 Scientific Meeting on Electrical-Electronics & Biomedical Engineering and Computer Science (EBBT), Istanbul, Turkey, 24–26 April 2019. [Google Scholar]
- Mercuri, M.; Lorato, I.R.; Liu, Y.H.; Wieringa, F.; Van Hoof, C.; Torfs, T. Vital-sign monitoring and spatial tracking of multiple people using a contactless radar-based sensor. Nat. Electron. 2019, 2, 252–262. [Google Scholar]
- Lazaro, A.; Girbau, D.; Villarino, R. Techniques for clutter suppression in the presence of body movements during the detection of respiratory activity through UWB radars. Sensors 2014, 14, 2595–2618. [Google Scholar]
- Yang, Z.; Bocca, M.; Jain, V.; Mohapatra, P. Contactless Breathing Rate Monitoring in Vehicle Using UWB Radar. In Proceedings of the 7th International Workshop on Real-World Embedded Wireless Systems and Networks, Shenzhen, China, 4 November 2018. [Google Scholar]
- Haramaki, T.; Nishino, H. A Study for Investigating Driver’s Condition by Radar. In Conference on Complex, Intelligent, and Software Intensive Systems; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Wang, G.R.; Han, H.G.; Kim, S.Y.; Kim, T.W. Wireless vital sign monitoring using penetrating impulses. IEEE Microw. Wirel. Compon. Lett. 2016, 27, 94–96. [Google Scholar]
- Schires, E.; Georgiou, P.; Lande, T.S. Vital sign monitoring through the back using an UWB impulse radar with body coupled antennas. IEEE Trans. Biomed. Circuits Syst. 2018, 12, 292–302. [Google Scholar] [PubMed]
- Leger, D.; Poursain, B.; Neubauer, D.; Uchiyama, M. An international survey of sleeping problems in the general population. Curr. Med. Res. Opin. 2008, 24.1, 307–317. [Google Scholar]
- Paalasmaa, J. Monitoring Sleep with Force Sensor Measurement; University of Helsinki: Helsinki, Finland, 7 February 2014. [Google Scholar]
- Ziganshin, E.; Numerov, M.; Vygolov, S. UWB baby monitor. In Proceedings of the IEEE 2010 5th International Confernce on Ultrawideband and Ultrashort Impulse Signals, Sevastopol, Ukraine, 6–10 September 2010. [Google Scholar]
- Tataraidze, A.; Anishchenko, L.; Alekhin, M.; Korostovtseva, L.; Sviryaev, Y. Estimation of respiratory rhythm during night sleep using a bio-radar. In Radar Sensor Technology XVIII; International Society for Optics and Photonics: Baltimore, MD, USA, 2014. [Google Scholar]
- Li, C.; Lin, J.; Xiao, Y. Robust overnight monitoring of human vital signs by a non-contact respiration and heartbeat detector. In Proceedings of the IEEE 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006. [Google Scholar]
- Kim, S.-H.; Geem, Z.W.; Han, G.-T. A Novel Human Respiration Pattern Recognition Using Signals of Ultra-Wideband Radar Sensor. Sensors 2019, 19, 3340. [Google Scholar]
- Javaid, A.Q.; Noble, C.M.; Rosenberg, R.; Weitnauer, M.A. Towards sleep apnea screening with an under-the-mattress IR-UWB radar using machine learning. In Proceedings of the 2015 IEEE 14th International Conference on Machine Learning and Applications (ICMLA), Miami, FL, USA, 9–11 December 2015. [Google Scholar]
- Pallesen, S.; Grønli, J.; Myhre, K.; Moen, F.; Bjorvatn, B.; Hanssen, I.; Heglum, H.S.A. A pilot study of impulse radio ultra wideband radar technology as a new tool for sleep assessment. J. Clin. Sleep Med. 2018, 14, 1249–1254. [Google Scholar] [PubMed]
- Hung, W.-P.; Chang, C.-H.; Lee, T.-H. Real-Time and Noncontact Impulse Radio Radar System for Movement Accuracy and Vital-Sign Monitoring Applications. IEEE Sens. J. 2017, 17, 2349–2358. [Google Scholar]
- Ossberger, G.; Buchegger, T.; Schimback, E.R.W.I.N.; Stelzer, A.; Weigel, R. Non-invasive respiratory movement detection and monitoring of hidden humans using ultra wideband pulse radar. In Proceedings of the IEEE 2004 International Workshop on Ultra Wideband Systems Joint with Conference on Ultra Wideband Systems and Technologies. Joint UWBST & IWUWBS 2004 (IEEE Cat. No. 04EX812), Kyoto, Japan, 18–21 May 2004. [Google Scholar]
- Ivashov, S.I.; Razevig, V.V.; Sheyko, A.P.; Vasilyev, I.A. Detection of human breathing and heartbeat by remote radar. In Proceedings of the Progress in Electromagnetic Research Symposium, Pisa, Italy, 28–31 March 2004. [Google Scholar]
- Levitas, B.; Matuzas, J. UWB radar for human being detection behind the wall. In Proceedings of the IEEE 2006 International Radar Symposium, Krakow, Poland, 24–26 May 2006. [Google Scholar]
- Greneker, E.F. RADAR flashlight for through-the-wall detection of humans. In Targets and Backgrounds: Characterization and Representation IV; International Society for Optics and Photonics: Baltimore, MD, USA, 7 July 1998. [Google Scholar]
- Wu, S.; Yao, S.; Liu, W.; Tan, K.; Xia, Z.; Meng, S.; Chen, J.; Fang, G.; Yin, H. Study on a novel UWB linear array human respiration model and detection method. IEEE J. Sel. Top. Appl. Earth Obs. Remote Sens. 2016, 9, 125–140. [Google Scholar]
- Yan, J.; Hong, H.; Zhao, H.; Li, Y.; Gu, C.; Zhu, X. Through-wall multiple targets vital signs tracking based on VMD algorithm. Sensors 2016, 16, 1293. [Google Scholar]
- Zito, D.; Pepe, D.; Mincica, M.; Zito, F.; Tognetti, A.; Lanata, A.; De Rossi, D. SoC CMOS UWB pulse radar sensor for contactless respiratory rate monitoring. IEEE Trans. Biomed. Circuits Syst. 2011, 5, 503–510. [Google Scholar]
- Kim, J.D.; Lee, W.H.; Lee, Y.; Lee, H.J.; Cha, T.; Kim, S.H.; Song, K.M.; Lim, Y.H.; Cho, S.H.; Cho, S.H.; et al. Non-contact respiration monitoring using impulse radio ultrawideband radar in neonates. R. Soc. Open Sci. 2019, 6, 190149. [Google Scholar]
- Mahbub, I.; Shamsir, S.; Pullano, S.A.; Islam, S.K. Low-power low-data-rate IR-UWB transmitter for paediatric apnoea monitoring system. IET Circuits Devices Syst. 2019, 13, 494–498. [Google Scholar]
- Huang, X.; Sun, L.; Tian, T.; Huang, Z.; Clancy, E. Real-time non-contact infant respiratory monitoring using UWB radar. In Proceedings of the 2015 IEEE 16th International Conference on Communication Technology (ICCT), Hangzhou, China, 18–20 October 2015. [Google Scholar]
- Schleicher, B.; Nasr, I.; Trasser, A.; Schumacher, H. IR-UWB radar demonstrator for ultra-fine movement detection and vital-sign monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2076–2085. [Google Scholar]
- Fiser, O.; Tesarik, J.; Pokorny, T.; Vrba, J. Non-contact Monitoring of Respiration and Heart Activity of Infants Using UWB Signals. In Proceedings of the IEEE 2019 PhotonIcs & Electromagnetics Research Symposium-Spring (PIERS-Spring), Rome, Italy, 17–20 June 2019. [Google Scholar]
- Staderini, E.M. UWB radars in medicine. IEEE Aerosp. Electron. Syst. Mag. 2002, 17, 13–18. [Google Scholar]
- Bond, E.J.; Li, X.; Hagness, S.C.; Van Veen, B.D. Microwave imaging via space-time beamforming for early detection of breast cancer. IEEE Trans. Antennas Propag. 2003, 51, 1690–1705. [Google Scholar]
- Lazaro, A.; Girbau, D.; Villarino, R. Wavelet-based breast tumor localization technique using a UWB radar. Prog. Electromagn. Res. 2009, 98, 75–95. [Google Scholar]
- Li, X.; Hagness, S.C. A confocal microwave imaging algorithm for breast cancer detection. IEEE Microw. Wirel. Compon. Lett. 2001, 11, 130–132. [Google Scholar]
- Kikkawa, T.; Toya, A.; Kubota, S.; Hafiz, M.; Azhari, A.; Sasaki, N. IR-UWB-CMOS circuits for breast cancer detection. In Proceedings of the IEEE 2012 6th European Conference on Antennas and Propagation (EUCAP), Prague, Czech Republic, 26–30 March 2012. [Google Scholar]
- McEwan, T.E. Body Monitoring and Imaging Apparatus and Method. U.S. Patent No. 5,573,012, 12 Novermber 1996. [Google Scholar]
- Thiel, F.; Kosch, O.; Seifert, F. Ultra-wideband sensors for improved magnetic resonance imaging, cardiovascular monitoring and tumour diagnostics. Sensors 2010, 10, 10778–10802. [Google Scholar]
- Saha, P.K.; Karim, M.N. A versatile pulse rate and low power CMOS IR UWB transmitter for medical imaging. In Proceedings of the 2015 IEEE International Wireless Symposium (IWS 2015), Shenzhen, China, 30 March–1 April 2015. [Google Scholar]
- Ota, K.; Ota, Y.; Otsu, M.; Kajiwara, A. Elderly-care motion sensor using UWB-IR. In Proceedings of the 2011 IEEE Sensors Applications Symposium, San Antonio, TX, USA, 22–24 February 2011. [Google Scholar]
- Diraco, G.; Leone, A.; Siciliano, P. A radar-based smart sensor for unobtrusive elderly monitoring in ambient assisted living applications. Biosensors 2017, 7, 55. [Google Scholar]
- Erol, B.; Amin, M.; Zhou, Z.; Zhang, J. Range information for reducing fall false alarms in assisted living. In Proceedings of the 2016 IEEE Radar Conference (RadarConf), Philadelphia, PA, USA, 2–6 May 2016. [Google Scholar]
- Mercuri, M.; Soh, P.J.; Pandey, G.; Karsmakers, P.; Vandenbosch, G.A.; Leroux, P.; Schreurs, D. Analysis of an indoor biomedical radar-based system for health monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2061–2068. [Google Scholar]


| Clutter & Noise Removal Algorithms | Research Articles |
|---|---|
| Loop Back Filter | [7,9,10,25,27,28,29,30,38,54,55,56] |
| Singular Value Decomposition (SVD) | [57] |
| Kalman Filter | [58] |
| Single Delay MTI Filter | [42] |
| Averaging Method | [4,17,18,52,59,60] |
| Pseudo-Bi-Dimensional Ensemble Empirical Mode Decomposition (PBDEEMD) | [61] |
| Vital Sign Assessed | Vital Sign Algorithms | Research Articles | Experimental Setup Range/Subjects/Reference Measurement Method | Results |
|---|---|---|---|---|
| HR, RR | Fast Fourier transform (FFT) | [47,52,60] | [47] 0.5–1 m/16/ECG [60]/9 human /fingertip pulse oximeter [52] 15 feet/7 humans/electronic heart-monitor | [47] Error rate: 5% [60] 1%–5% [52] Mean error for obstructed RR: 0.3 bpm Mean error for obstructed RR: 0.14 bpm Mean error for unobstructed HR: 8 bpm |
| HR, RR | Ensemble empirical mode decomposition (EEMD) and Continuous wavelet transforms (CWT) | [12] | 0.2–5m/3 human/ECG | SNR improvement for RR: 7.5 dB SNR improvement for HR: 4.8 dB |
| RR | Wavelet transform | [8,62] | [8] 6 –14 m/2 males, 2 females, 1 actuator/FFT method measurements [62] 1–2.5 m/-/manual measurement | [8] SNR: (−4.91dB–(−8.28 dB) Deviation: 0.66%–0.24% [62] Deviation: 0.19 per minute |
| HR, RR | MTI and Chirp Z-transform (CZT) | [4] | 1 m/3 human/ECG | Error rate BR/HR: 1%–2.4% |
| RR | Multiple Higher Order Cumulant (MHOC) | [72] | 2–7 m/1 human/manual | SNR improvement: 13.8 dB |
| HR, RR | HAPA (harmonic path) | [70] | 5–15 cm/1 male/pulse-oximeter | Error rate (MSE) for HR: 1.83% |
| HR, RR | Spectrum-Averaged Harmonic Path (SHAPA) | [71] | 5–15 cm/8 human/pulse-oximeter | Error rate: 16% improvement over [70] |
| RR | IIR filter | [18] | 1 m/--/respiration monitor belt (RPM) | Correlation co-efficient: 0.909 Absolute error: 0.5 mHz |
| HR | Time Domain Processing Algorithm | [16] | 0.25–1.25 m/5 human/ECG | Error rate: 1.01%–4.32% |
| HR | Time series analysis | [15] | 1m/apparatus/-- | Error rate: 1.26% |
| HR, RR | Pulse-Doppler signal processing technique | [19] | 5–15 cm/13 human/Polysomnography (PSG) | Deviation: 5% |
| HR | Maximum likelihood period estimation | [63] | 0.3 m/1 human/wearable sensor | Mean Square Error: < −8dB |
| RR, HR | Ensemble empirical mode decomposition (EEMD) | [57,61] | [57] 3 m–16 m/5 humans/-- [61] 50 cm/--/human tissue model | [57] Error rate: 1.5–3.75% [61] Error rate: 1.12% |
| RR, HR | Harmonic Multiple Loop Detection (HMLD) | [77] | 0.64 m/5 male, 5 female/pulse oximeter (HR), manual chest wall count (RR) | Error rate (RR): 4.95% Error rate (HR): 5.06% |
| Vital Sign Assessed | Vital Sign Algorithms | Research Articles | Experimental Setup Range/Subjects/Reference Measurement Method | Results |
|---|---|---|---|---|
| HR, RR | Fast Fourier transform (FFT), Autocorrelation | [58] | 1–2 m/5 humans /ECG | RMSE for RR: 0.006 HR: 0.372 |
| HR, RR | Wavelet, Kalman filter | [80] | 1–4.5 m/4 humans/ECG | Error rate: 2.25%–4.6% |
| RR | FFT | [81] | 70 cm/1 humans/manual | SNR (stationary): 20 dB SNR (speaking): 15 dB SNR (handwriting): 16 dB |
| RR, HR | FFT, Continuous Wavelet Transform (CWT) | [82] | 5.4 m/8 humans/ECG | Success rate: RR: 94% HR: 89% |
| RR | FFT, distance deviation threshold (for random body motion detection) | [83] | 1 m/22-year-old male/microphone | Normal breathing, apnea, macro-motion detection |
| Vital Sign Assessed | Vital Sign Algorithms | Research Articles | Experimental setup Range/Subjects/Reference Measurement Method | Results |
|---|---|---|---|---|
| HR, RR | Location based Variational Mode Decomposition (VMD) | [61] | Up to 1.5 m (inside car) /2 human/Oximeter | Error rate for only driver HR: 7.34% Error rate for two targets in car HR: 6.9%–11.5% |
| RR | FFT, band pass filter | [84] | Inside car/ 3 male, 1 female/manual push button based method | Mean error: 1.06 breathing rate per minute |
| RR, HR | FFT, Data fitting method | [16] | Inside car/5 humans/ECG, respiration belt | Mean RR error: 0.2–0.7 beats per minute Mean HR error: 0.6–2.5 beats per minute |
| RR, HR | FFT, band pass filter | [86] | Inside chamber/ 1 human/ECG | SNR: 8.6 dB |
| HR | FFT, FIR Kaiser filter of order 600, Correlation method | [87] | Inside car/3 humans/3 lead Olimex EKG (for ECG), a BioHarness 3 (RR) | Phase method: 13.1%–22.5% Correlation method: 14.4%–30.3% Slow time method: 24.3%–39.4% |
| Vital Sign Assessed | Vital Sign Algorithms | Research Articles | Experimental Setup Range/Subjects/ Wall Thickness | Results |
|---|---|---|---|---|
| HR, RR | CWT, background subtraction method | [97] | 1–5 m (non-obstructive), 0.8 through the wall/50 cm | SNR: 14 dB |
| Detection | Raw data, Frequency spectrum | [98] | 1 m/1 human/10 cm | Person detection: 100% |
| Detection | Time domain (slow time signal) analysis | [99] | 2.6 m/1 human/wall | Respiratory pattern |
| RR | Spectrum analysis | [12] | 0.7–2.5 m/1 human/20 cm reinforced concrete wall | Error rate: 0.6% |
| RR | IIR band pass, moving averaging filter, advanced normalization method, FFT | [101] | 5.5 m/3 humans/… | Detection of RR |
| RR | Variational mode decomposition (VMD) | [102] | 1.5 m/3 humans/15 cm thick concrete wall | Correlation: 97.6% |
| Vital Sign Assessed | Vital Sign Algorithms | Research Articles | Experimental Setup Range/Subjects (Age) | Results |
|---|---|---|---|---|
| RR | FFT | [103] | 30–45 cm/3 humans (1 man, 1 woman, 1 baby (5 months old) | Sub-centimeter chest moment detected successfully |
| RR | FFT | [104] | 35 cm/9 babies (age 2–27 days) | Mean bias: 1.7 bpm |
| RR, HR | Peak detection method | [108] | 60 cm/babies (1–3 years old) | Apnea detected |
| RR | FFT, band pass filter | [106] | 1 m/1 infant | 1 RR detected at 0.62 Hz |
| RR | Fourier Transform analysis | [107] | 20–25 cm/male human, 1 infant (7 weeks old) | Continuous breathing and arrhythmic breathing classification |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, F.; Ghaffar, A.; Khan, N.; Cho, S.H. An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver. Sensors 2020, 20, 2479. https://doi.org/10.3390/s20092479
Khan F, Ghaffar A, Khan N, Cho SH. An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver. Sensors. 2020; 20(9):2479. https://doi.org/10.3390/s20092479
Chicago/Turabian StyleKhan, Faheem, Asim Ghaffar, Naeem Khan, and Sung Ho Cho. 2020. "An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver" Sensors 20, no. 9: 2479. https://doi.org/10.3390/s20092479
APA StyleKhan, F., Ghaffar, A., Khan, N., & Cho, S. H. (2020). An Overview of Signal Processing Techniques for Remote Health Monitoring Using Impulse Radio UWB Transceiver. Sensors, 20(9), 2479. https://doi.org/10.3390/s20092479





