1. Introduction
Adhesive capsulitis (AC), or frozen shoulder, is a pathological glenohumeral (GH) joint condition, characterized by adhesions across the GH joint capsule and surrounding ligaments, which negatively affect active and passive GH mobility [
1,
2]. Movement restrictions generally occur in all movement planes, with more pain towards the end of the available joint motion and with more external rotation restrictions in elevated arm positions [
3]. Therefore, AC highly interferes with the independent performance of activities of daily living [
3]. A primary, idiopathic form of AC and a secondary form, following trauma or surgery, are described [
4]. The incidence of AC is 3% to 5% in the general population [
1], with 70% of persons with AC being women [
3]. Apart from pain and GH mobility deficits [
5,
6], AC leads to shoulder dysfunctions and reduces daily life autonomy and quality of life [
2]. Although AC is a self-limiting condition, it takes between one to three years to resolve [
7,
8]. However, mild symptoms may persist for several years in small groups of persons with AC [
8]. The treatment goals of medical and physiotherapy treatment in persons with AC are to increase glenohumeral mobility and to normalize scapulothoracic (ST) (mal)adaptive movement patterns, to increase shoulder function [
3]. Therefore, the objective assessment of GH motion and compensatory motion in the adjacent scapulothoracic (ST) and elbow joint is of interest to evaluate AC treatment effects and follow up progress [
5,
6].
The evaluation of active and passive shoulder movement in current clinical practice of AC patients is generally done by visual observation or goniometry [
3,
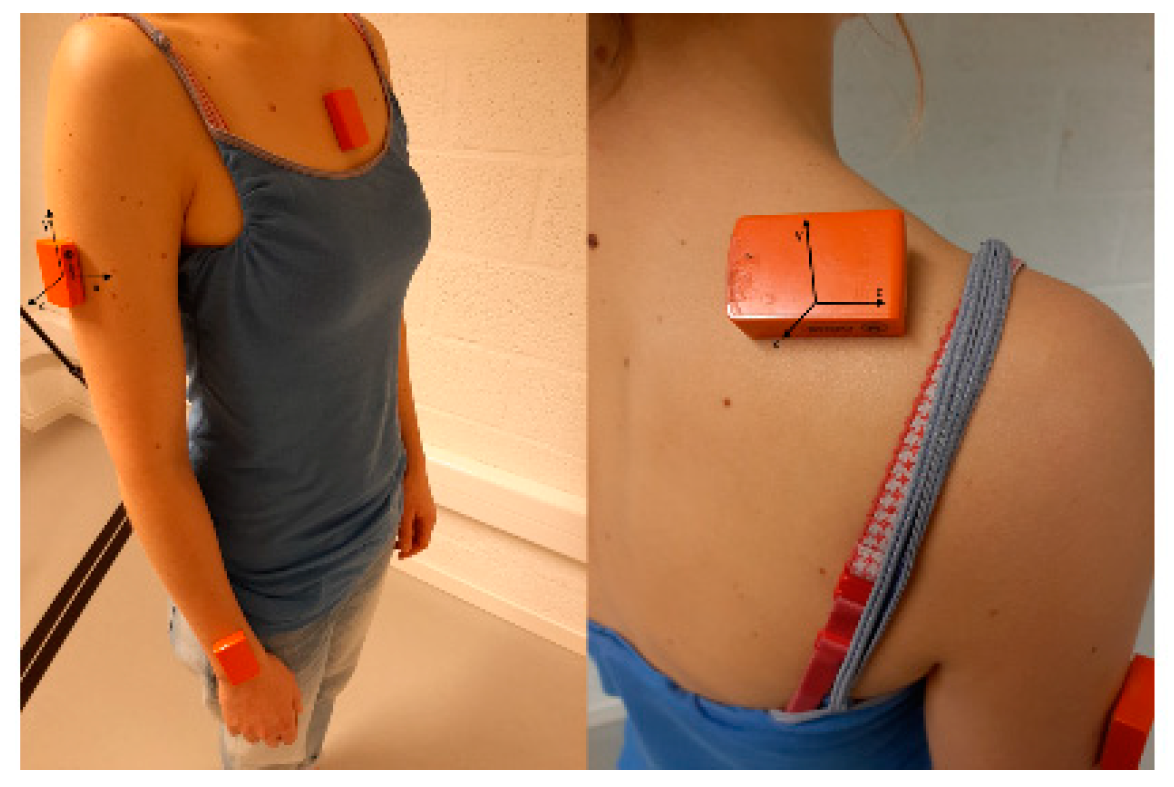
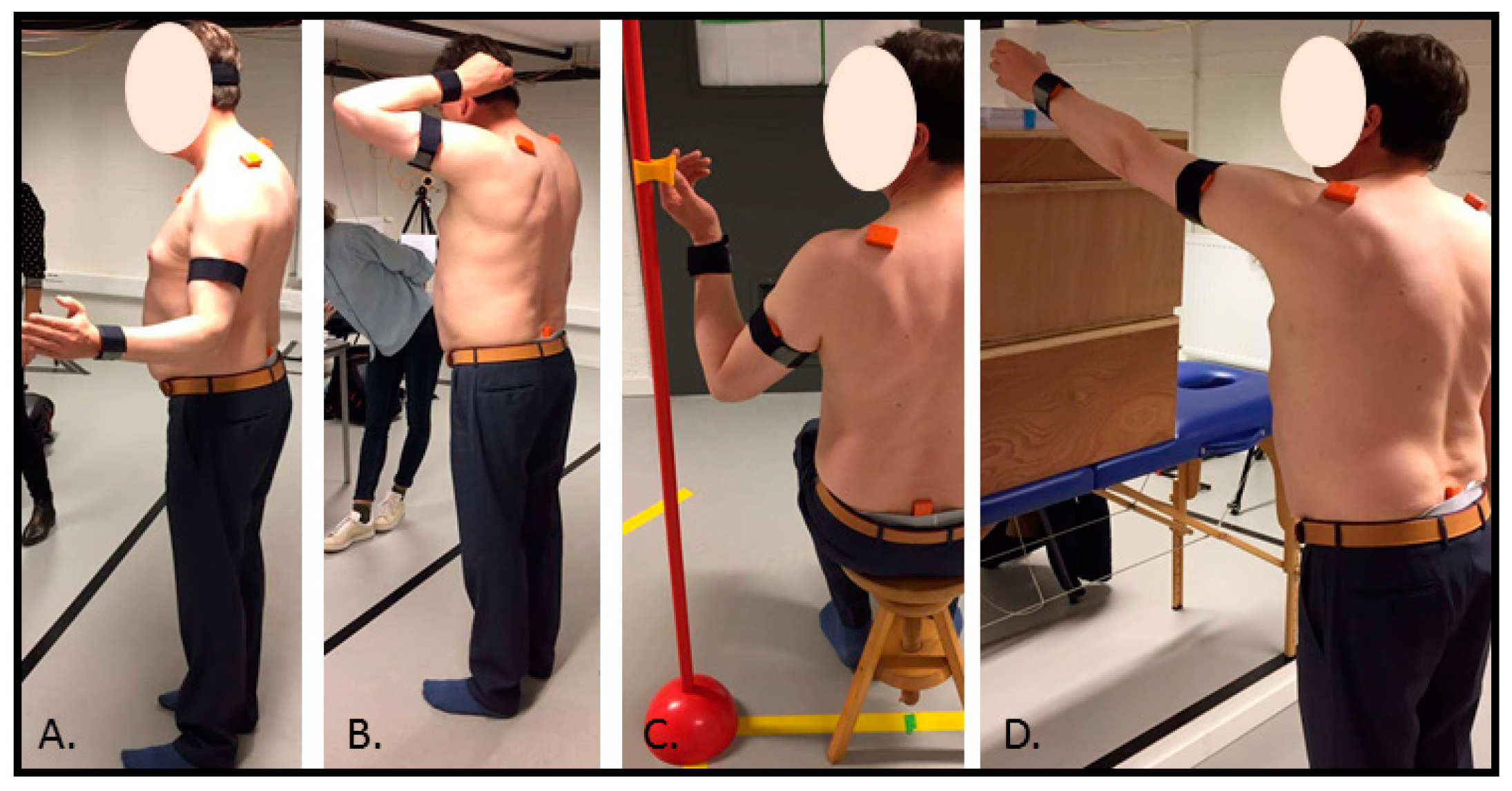
9]. Despite the easy-to-use character of these measurements, they have the disadvantage of not being able to measure isolated GH and scapulothoracic motion. Instead, they generally measure humerothoracic motion during active movement assessment. Furthermore, goniometry measurements are typically performed during uniplanar movement (e.g., arm elevation in the frontal plane), instead of during the performance of functional tasks resembling activities of daily life. However, in the last decade, the development of inertial sensor technologies for objective movement assessment of joint range of motion in clinical practice has emerged given their opportunity to measure range of motion during more complex, functional and multiplanar movements [
10,
11]. Inertial sensor systems are furthermore relatively inexpensive and do not require specific expertise to operate. Some of these systems are currently commercially available and provide, apart from the hardware (inertial motion sensors), software which is necessary to assess motion (i.e., calculate joint angles from the recorded signals of the inertial sensors). As such, these systems seem to be promising tools to use in clinical orthopedic and physiotherapy practice to investigate progression of GH motion in AC patients, and to investigate compensatory patterns in the elbow or ST joint during relevant functional activities.
However, before such a system is implemented in clinical settings, the assessment of the system’s reliability and agreement in calculating joint angles within and between assessors/clinicians should be assessed (i.e., the so-called within-session, intra-operator, and inter-operator reliability and agreement). Knowledge of a system’s measurement error makes interpretation of recorded motion data straightforward (i.e., measurement error can be distinguished from true differences/recovery) [
12]. A recent systematic review indicated that the main body of literature on the measurement properties of inertial sensors for the assessment of joint range of motion focused towards the assessment of lower limb joint angles during walking/running [
13]. Regarding shoulder complex joint angles, only three studies are currently available, which report appropriate reliability and agreement results for ST kinematic assessment by means of inertial sensors [
14,
15,
16]. However, they only describe the reliability and agreement of ST joint angles during analytical arm elevation tasks. Furthermore, with regard to the reliability of GH joint angles, no literature is available. Instead, two studies were found describing appropriate reliability results for humerothoracic range of movement assessment in persons without shoulder complaints [
17,
18]. However, in one of these studies, range of motion was assessed during passive arm movement, which does not resemble daily life movement [
18].
Apart from the assessment of GH and ST range of motion during analytical arm movement tasks, the assessment of GH and ST range of motion during functional movement tasks (i.e., tasks resembling the activities which are difficult to perform by persons with shoulder complaints), is essential in the evaluation of AC progression and in the evaluation of the effect of AC treatment [
3]. Given the lack on reliability and agreement data of GH and ST range of motion assessment by inertial sensors during functional movement tasks [
13], and given that AC patients have difficulties performing GH elevation and external rotation due to GH capsular restrictions [
3], the aim of this study was to assess within-session, intra-operator, and inter-operator reliability and agreement of a functional movement protocol with a special focus towards GH elevation and external rotation movement tasks, to assess GH, ST, and elbow motion in AC patients. We furthermore aim to formulate recommendations regarding parameter selection when using inertial sensor movement analysis to evaluate treatment efficacy and follow up progress. It is hypothesized that, in line with previous research [
14,
15,
16,
17,
18], in general good reliability and agreement results will be found for ST, GH, and elbow joint range of motion assessment, but that reliability and agreement results will depend on the complexity of the assessment movement task.
4. Discussion
Nowadays, commercially available inertial measurement systems for human movement analysis are emerging. This study assesses the reliability and agreement of ST, GH, and elbow joint ROM assessment in AC patients using a commercially available inertial measurement system. Such a system is of great value to evaluate treatment effects in persons with AC in daily practice. However, before such a system can be clinically implemented, the establishment of its reliability and knowledge of its measurement errors in the assessment of ST, GH, and elbow joint ROM is essential.
The reliability and agreement results, reported in this study, were not sufficient overall, indicating that that the clinical implementation of inertial sensor technology in the assessment of shoulder movement in persons with AC is not straightforward at this moment. The values of the SEMs/MDCs and of the ICCs (together with the width of their confidence intervals) were dependent on the assessed joint rotation and assessed task. Furthermore, task-specific differences in within-session, intra- and inter-operator reliability, and agreement were found.
However, results were comparable to reported reliability and agreement results of other studies assessing the reliability and agreement of ST or humerothoracic range of motion measurements by means of inertial sensors in healthy persons. Schiefer et al. [
18] reported a within-session ICC for humerothoracic abd-adduction of 0.96 in healthy persons which is in line with the reported within-session ICC-values in this study during functional task performance in persons with AC [
18]. Bouvier et al. [
17] described the performance of standardized analytical movements in healthy persons; there were lower intra-operator reliability results for humerothoracic abd-adduction and ext-internal rotation than for flexion-extension [
17]. This was not consistent with the results reported in this study, since a better reliability in GH flexion-extension than in GH abd-adduction or GH ext-internal during the performance of functional tasks was not consistently observed. Within-session agreement results (SEMs) for ST rotations, reported in healthy persons by Parel et al. [
15] (i.e., between 1.2°–3.9°, 1.8°–3.4°, and 1.4°–2.8° for scapulothoracic pro-retraction, med-lateral rotation and antr-posterior tilt) were generally higher than the reported within-session SEMs in this study [
15]. Furthermore, van den Noort et al. [
16] reported intra- and inter-operator SEMs for ST med-lateral rotation and ant-posterior tilt lower than 5°, which is generally in line with the reported intra- and inter-operator SEMs in this study [
16]. Reported intra- and inter-operator ICCs by van den Noort et al. [
16] during analytical arm elevation movements (pro-retraction ICC range 0.65–0.85 and med-lateral rotation ICC range 0.56–0.91) were slightly lower than the reported ICC in this study, indicating better slightly better reliability during functional task performance [
16].
In order to fully investigate the reliability and agreement of the inertial sensor system in the assessment of joint ROM in AC patients, within-session reliability and agreement was assessed together with intra- and inter-operator reliability and agreement. While within-session data provides information on reliability and measurement error caused by intra-subject movement variability (natural source of variability), intra-operator (between-session) and inter-operator reliability and agreement provide information on additional sources of error (e.g., task-standardization/explanation; manual handling during sensor placement/calibration). Specifically regarding the applied inertial sensor technology used in this study, following sources of errors must be considered: calibration inaccuracies when positioning the participant in the neutral calibration position; palpation inaccuracies when placing the sensors on the segments in alignment with the segment orientation; measurement errors when determining anthropometric dimensions which serve as necessary input for the upper body configuration/model; and inaccuracies in task-explanation. The fact that both intra- and inter-operator reliability and agreement are assessed, additionally provides information about the source of error which is seen between sessions: if the error is operator-dependent (e.g., personal manner of task explanation or placing sensors), better intra-operator than inter-operator reliability and agreement are expected. When intra-operator and inter-operator reliability/agreement are equal but worse than within-session data, natural variability in task-execution by testing on different occasions might be assumed.
Furthermore, it is known that the magnitude of the ICC is dependent on between-subject variability (i.e., high ICCs can hide poor trial-to-trial consistency in case of high between-subject variability) [
12]. Conversely, limited between-subject variability could result in poor ICCs even when trial-to-trial consistency is high. Therefore, ICCs should always be considered in conjunction with agreement parameters (SEMs, MDC, LOA). Since measurement errors have the same unit as the measurement of interest (in this case degrees), they are easily interpretable in clinical practice. Finally, the range of ICCs’ confidence intervals should be taken into account when interpreting the value of the reported ICC.
When interpreting the reported results based on the aforementioned information, recommendations for task selection can be made, in order to make specific guidelines on the appropriate use of inertial sensors systems for range of motion measurements in clinical practice. For the analytical GH external rotation, within-session and intra-operator agreement were similar for GH in-external rotation. In contrast, inter-operator agreement was remarkably lower for GH in-external rotation. In addition, for ST pro-retraction, inter-operator agreement was lower than intra-operator agreement. As this difference between intra- and inter-operator agreement is only notable during the analytical GH external rotation, differences in sensor placement between the operators are not expected. The agreement differences might rather be explained by the fact that the analytical external rotation task was the only task without a clear endpoint, making task standardization by thorough task explanation and clear task instructions crucial. As such, the lower inter-operator agreement results are expected to relate to inconsistent task explanation/instructions.
For the functional external rotation tasks (i.e., combing hair and grasping a seatbelt), different joint ROMs show different reliability and agreement results. For combing hair, better agreement results are reported for ST med-lateral rotation, GH flexion-extension, and elbow flexion-extension, indicating low intra-individual natural movement variability for these motions while combing hair. In contrast, given the lower agreement results for transversal plane motion during combing hair, this task is not recommended to assess ST pro-retraction and/or GH internal-external rotation. It seems a better choice to assess GH in-external rotation during the grasping the seatbelt task. For this task, best agreement results are reported for GH in-external rotation, GH ab-adduction, and elbow flexion-extension. On the other hand, grasping the seatbelt is not the optimal option when assessment of ST motion is of primarily interest, given the worse agreement results for ST medial-lateral rotation, ST tilting, and ST pro-retraction. Placing a cup on an overhead shelf is the task with the best agreement results across all ST and GH joint motions. Only for elbow flexion-extension, worse agreement results are reported. Probably the fact that this task is executed in one movement plane (i.e., the sagittal plane), in contrast to combing hair and grasping the seatbelt which are tasks consisting of movements in all movement planes, adds to the good agreement results for all ST and GH ROMs during placing a cup. Recommendations for parameter selection are summarized in
Table 6.
This protocol, consisting of four tasks during which ST, GH, and elbow kinematics are measured by means of a commercially available inertial sensor system, is only reliable and shows agreement within and between operators when specific recommendations for parameters selection (i.e., specific ROMs during specific tasks) are applied. Given that one measurement session only lasts for 15 minutes, this protocol seems usable in daily physiotherapy or orthopedic practice, when relying on these recommendations. However, when inspecting the magnitude of ST ROMs, one might question their validity. When comparing to literature, reported ST ROM seems underestimated for lateral rotation and overestimated for posterior tilting [
5,
6,
16,
24,
25,
26]. Parel et al. [
14,
15] and van den Noort et al. [
26] reported good validity results for inertial sensor-based ST joint motion during arm elevation tasks, when an YZX-sequence for ST joint angle calculation was used [
14,
15,
16,
26]. However, the software included in this commercially available package uses the ZXY-sequence for ST joint angle calculation, which might be the cause of over- or underestimation of ST tilting and lateral rotation ROM, respectively. Therefore, it is essential to further clarify these validity concerns on ST joint angle calculation during the proposed protocol before it is clinically applicable.
There are several limitations of this study. Given that the reported movement protocol was specifically designed for AC patients (i.e., persons with shoulder movement restrictions towards arm elevation and external rotation), one could argue that the reported SEM and MDC values are only applicable to persons with these shoulder movement restrictions, which decreases the generalizability of the results into different patient populations. However, the fact that arm abduction and external rotation movement restrictions often occur in other shoulder joint problems than AC, increases the relevance of the developed protocol for persons with other than AC shoulder joint conditions.
Only 10 persons with AC were included in this study which might be a limitation. For between-session reliability assessment, it is essential that all conditions are as similar as possible between the two assessment sessions, to exclude as much ‘noise’ as possible. An example of ‘noise’ is potential improvement in mobility between the two test sessions due to, for example, treatment or the performance of exercises. Given that mobility exercises and physiotherapy are the main treatment in persons with AC, participation in this study interfered with their normal rehabilitation. Therefore, only 10 participants were included.