The Application of the Food Insulin Index in the Prevention and Management of Insulin Resistance and Diabetes: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Selection of Sources of Evidence
2.4. Charting the Data
2.5. Summarizing and Reporting the Results
2.6. Quality Appraisal
3. Results
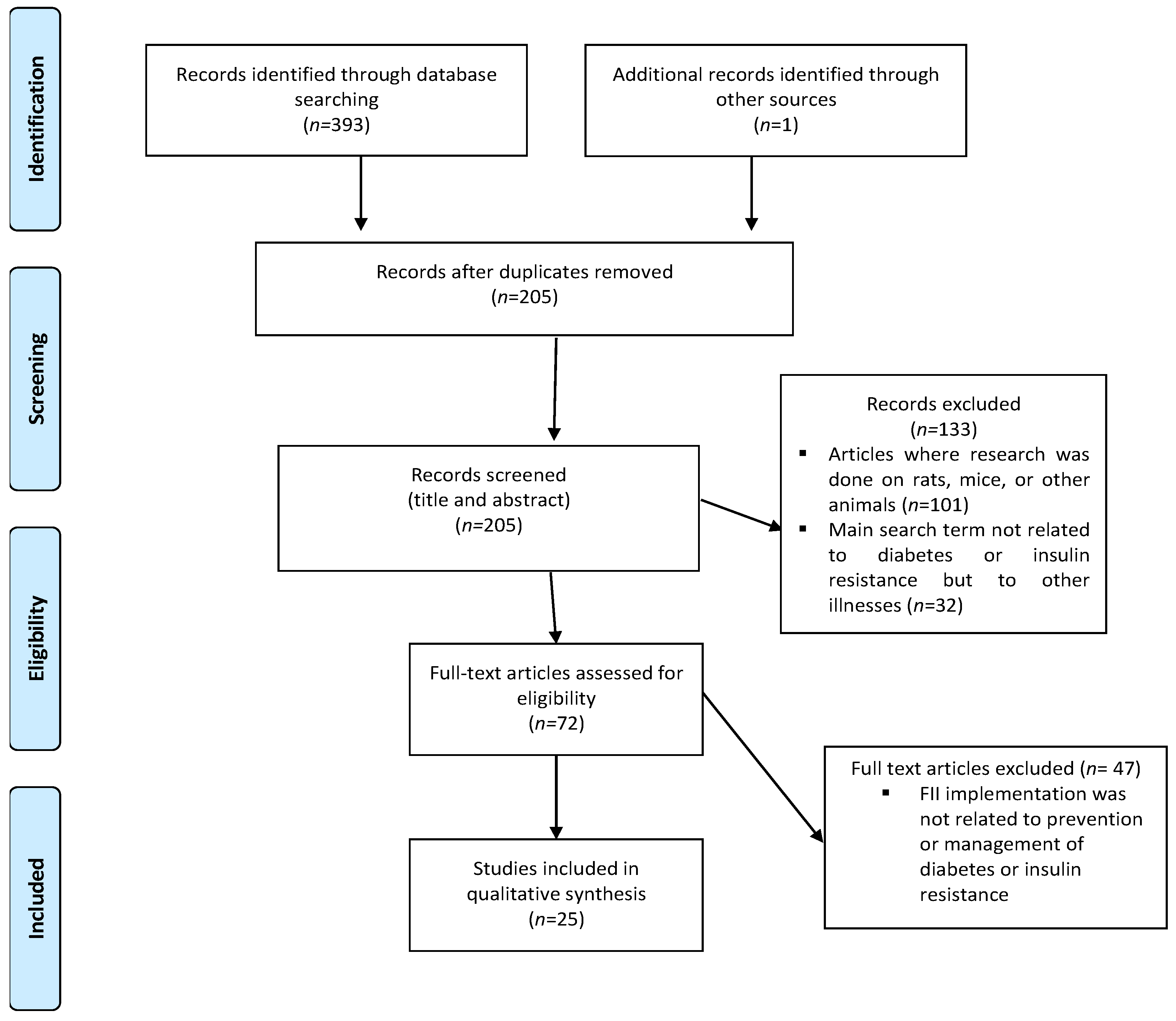
3.1. Selection of the Included Articles
3.2. Characteristics of the Included Articles
3.3. Quality of Evidence
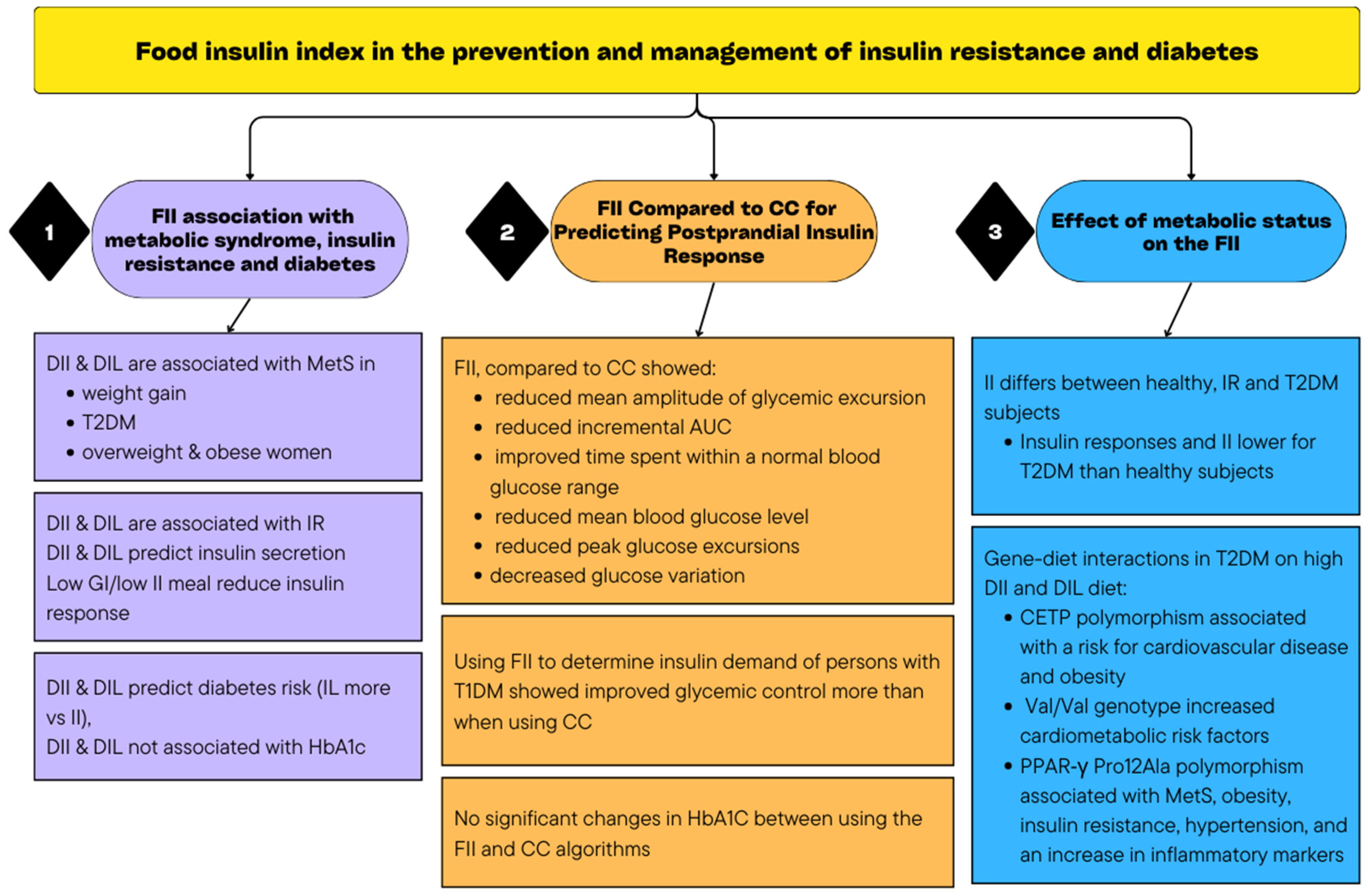
3.4. Main Findings
3.4.1. The Association of FII with the Development of Metabolic Syndrome, Insulin Resistance, and Diabetes
3.4.2. The FII Compared to CC for Predicting Postprandial Insulin Response
3.4.3. The Effect of Metabolic Status on the FII
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jeffery, A. Insulin resistance. Nurs. Stand. R. Coll. Nurs. Great Br. 1987 2003, 17, 47–53. [Google Scholar]
- Krentz, A. Insulin Resistance: A Clinical Handbook; John Wiley & Sons: Chichester, UK, 2002. [Google Scholar]
- LeRoith, D.; Taylor, S.I.; Olefsky, J.M. Diabetes Mellitus: A Fundamental and Clinical Text, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2004. [Google Scholar]
- Meade, L.T.; Rushton, W.E. Accuracy of Carbohydrate Counting in Adults. Clin. Diabetes A Publ. Am. Diabetes Assoc. 2016, 34, 142–147. [Google Scholar] [CrossRef]
- Gillespie, S.J.; Kulkarni, K.D.; Daly, A.E. Using carbohydrate counting in diabetes clinical practice. J. Am. Diet. Assoc. 1998, 98, 897–905. [Google Scholar] [CrossRef]
- Warshaw, H.S.; Bolderman, K.M. American Diabetes A. In Practical Carbohydrate Counting: A How-to-Teach Guide for Health Professionals, 2nd ed.; American Diabetes Association: Alexandria, VA, USA, 2008. Available online: http://catdir.loc.gov/catdir/toc/ecip0818/2008020554.html (accessed on 20 September 2023).
- Wolever, T.M.; Jenkins, D.J.; Jenkins, A.L.; Josse, R.G. The glycemic index: Methodology and clinical implications. Am. J. Clin. Nutr. 1991, 54, 846–854. [Google Scholar] [CrossRef]
- Villegas, R.; Liu, S.; Gao, Y.; Yang, G.; Li, H.; Zheng, W.; Shu, X.O. Prospective study of dietary carbohydrates, glycemic index, glycemic load, and incidence of type 2 diabetes mellitus in middle-aged Chinese women. Arch. Intern. Med. 2007, 167, 2310–2316. [Google Scholar] [CrossRef]
- Slabber, M.; Barnard, H.C. Effects of a low-insulin-response, energy-restricted diet on weight loss and plasma insulin. Am. J. Clin. Nutr. 1994, 60, 48–53. [Google Scholar] [CrossRef]
- Rizkalla, S.W.; Taghrid, L.; Laromiguiere, M.; Huet, D.; Boillot, J.; Rigoir, A.; Elgrably, F.; Slama, G. Improved plasma glucose control, whole-body glucose utilization, and lipid profile on a low-glycemic index diet in type 2 diabetic men: A randomized controlled trial. Diabetes Care 2004, 27, 1866–1872. [Google Scholar] [CrossRef]
- Liese, A.D.; Schulz, M.; Fang, F.; Wolever, T.M.; D’Agostino, R.B., Jr.; Sparks, K.C.; Mayer-Davis, E.J. Dietary glycemic index and glycemic load, carbohydrate and fiber intake, and measures of insulin sensitivity, secretion, and adiposity in the Insulin Resistance Atherosclerosis Study. Diabetes Care 2005, 28, 2832–2838. [Google Scholar] [CrossRef]
- Jenkins, D.J.; Wolever, T.M.; Taylor, R.H.; Barker, H.; Fielden, H.; Baldwin, J.M.; Bowling, A.C.; Newman, H.C.; Jenkins, A.L.; Goff, D.V. Glycemic index of foods: A physiological basis for carbohydrate exchange. Am. J. Clin. Nutr. 1981, 34, 362–366. [Google Scholar] [CrossRef]
- Bao, J.; Atkinson, F.; Petocz, P.; Willett, W.C.; Brand-Miller, J.C. Prediction of postprandial glycemia and insulinemia in lean, young, healthy adults: Glycemic load compared with carbohydrate content alone. Am. J. Clin. Nutr. 2011, 93, 984–996. [Google Scholar] [CrossRef]
- Brand-Miller, J.C.; Thomas, M.; Swan, V.; Ahmad, Z.I.; Petocz, P.; Colagiuri, S. Physiological validation of the concept of glycemic load in lean young adults. J. Nutr. 2003, 133, 2728–2732. [Google Scholar] [CrossRef]
- Augustin, L.S.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Björck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. 2015, 25, 795–815. [Google Scholar] [CrossRef]
- Steenkamp, G.; Delport, L. The Smart Carb Guide. In The South African GI and GL Guide; The Glycemic Index foundation of SA: Nelspruit, South Africa, 2016. [Google Scholar]
- Salmerón, J.; Ascherio, A.; Rimm, E.B.; Colditz, G.A.; Spiegelman, D.; Jenkins, D.J.; Stampfer, M.J.; Wing, A.L.; Willett, W.C. Dietary fiber, glycemic load, and risk of NIDDM in men. Diabetes Care 1997, 20, 545–550. [Google Scholar] [CrossRef]
- Jenkins, D.J.; Wolever, T.M.; Thorne, M.J.; Jenkins, A.L.; Wong, G.S.; Josse, R.G.; Csima, A. The relationship between glycemic response, digestibility, and factors influencing the dietary habits of diabetics. Am. J. Clin. Nutr. 1984, 40, 1175–1191. [Google Scholar] [CrossRef]
- Jenkins, D.J.; Wolever, T.M.; Jenkins, A.L. Starchy foods and glycemic index. Diabetes Care 1988, 11, 149–159. [Google Scholar] [CrossRef]
- Crapo, P.A.; Kolterman, O.G.; Waldeck, N.; Reaven, G.M.; Olefsky, J.M. Postprandial hormonal responses to different types of complex carbohydrate in individuals with impaired glucose tolerance. Am. J. Clin. Nutr. 1980, 33, 1723–1728. [Google Scholar] [CrossRef]
- Crapo, P.A.; Insel, J.; Sperling, M.; Kolterman, O.G. Comparison of serum glucose, insulin, and glucagon responses to different types of complex carbohydrate in noninsulin-dependent diabetic patients. Am. J. Clin. Nutr. 1981, 34, 184–190. [Google Scholar] [CrossRef]
- Salmeron, J. Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA J. Am. Med. Assoc. 1997, 277, 472–477. [Google Scholar] [CrossRef]
- Solomon, T.P.; Haus, J.M.; Kelly, K.R.; Rocco, M.; Kashyap, S.R.; Kirwan, J.P. Improved pancreatic beta-cell function in type 2 diabetic patients after lifestyle-induced weight loss is related to glucose-dependent insulinotropic polypeptide. Diabetes Care 2010, 33, 1561–1566. [Google Scholar] [CrossRef]
- Barclay, A.; Petocz, P.; McMillan-Price, J.; Flood, V.; Prvan, T.; Mitchell, P.; Brand-Miller, J.; Wellington New, Z. CD1-1 Glycemic index, glycemic load and diabetes risk: A meta-analysis. Diabetes Res. Clin. Pract. 2008, 79, S30–S31. [Google Scholar] [CrossRef]
- Livesey, G.; Taylor, R.; Livesey, H.; Liu, S. Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies. Am. J. Clin. Nutr. 2013, 97, 584–596. [Google Scholar] [CrossRef]
- Brownley, K.A.; Heymen, S.; Hinderliter, A.L.; Galanko, J.; Macintosh, B. Low-glycemic load decreases postprandial insulin and glucose and increases postprandial ghrelin in white but not black women. J. Nutr. 2012, 142, 1240–1245. [Google Scholar] [CrossRef]
- Holt, S.H.; Miller, J.C.; Petocz, P. An insulin index of foods: The insulin demand generated by 1000-kJ portions of common foods. Am. J. Clin. Nutr. 1997, 66, 1264–1276. [Google Scholar] [CrossRef]
- ISO. Determination of the Glycaemic Index (GI) and Recommendation for Food Classification. Available online: https://www.iso.org/standard/43633.html (accessed on 6 November 2023).
- Bao, J.; de Jong, V.; Atkinson, F.; Petocz, P.; Brand-Miller, J.C. Food insulin index: Physiologic basis for predicting insulin demand evoked by composite meals. Am. J. Clin. Nutr. 2009, 90, 986–992. [Google Scholar] [CrossRef]
- Bell, K.J.; Bao, J.; Petocz, P.; Colagiuri, S.; Brand-Miller, J.C. Validation of the food insulin index in lean, young, healthy individuals, and type 2 diabetes in the context of mixed meals: An acute randomized crossover trial. Am. J. Clin. Nutr. 2015, 102, 801–806. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Danielle, L.; Heather, C.; Kelly, K.O.B. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.; Godfrey, C.; McInerney, P.; Soares, C.; Khalil, H.; Parker, D. Methodology for JBI Scoping Reviews. In The Joanna Briggs Institute Reviewers’ Manual 2015; The Joanna Briggs Institute: Adelaide, South Australia, 2015; pp. 1–24. [Google Scholar]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) Version 2018 for Information Professionals and Researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Abaj, F.; Rafiee, M.; Koohdani, F. Interaction between CETP polymorphism and dietary insulin index and load in relation to cardiovascular risk factors in diabetic adults. Sci. Rep. 2021, 11, 15906. [Google Scholar] [CrossRef]
- Abaj, F.; Rafiee, M.; Koohdani, F. Interactions of dietary insulin index and dietary insulin load with brain-derived neurotrophic factor (BDNF) Val66Met polymorphism in relation to cardiometabolic markers in Iranian diabetic patients: A cross-sectional study. Br. J. Nutr. 2022, 128, 785–792. [Google Scholar] [CrossRef]
- Abaj, F.; Rafiee, M.; Koohdani, F. A personalised diet approach study: Interaction between PPAR-γ Pro12Ala and dietary insulin indices on metabolic markers in diabetic patients. J. Hum. Nutr. Diet. 2022, 35, 663–674. [Google Scholar] [CrossRef]
- Anjom-Shoae, J.; Namazi, N.; Ayati, M.H.; Darbandi, M.; Najafi, F.; Pasdar, Y. Dietary insulin index and load in relation to cardiometabolic risk factors in patients with type 2 diabetes mellitus: A cross-sectional study on the RaNCD cohort study. Nutrition 2023, 105, 111830. [Google Scholar] [CrossRef]
- Bao, J.; Gilbertson, H.R.; Gray, R.; Munns, D.; Howard, G.; Petocz, P.; Colagiuri, S.; Brand-Miller, J.C. Improving the estimation of mealtime insulin dose in adults with type 1 diabetes: The Normal Insulin Demand for Dose Adjustment (NIDDA) study. Diabetes Care 2011, 34, 2146–2151. [Google Scholar] [CrossRef]
- Bell, K.; Gray, R.; Munns, D.; Howard, G.; Petocz, P.; Brand-Miller, J.C.; Colagiuri, S. Estimating prandial insulin dose for single foods using the food insulin index improves post-prandial glycemic control in type 1 diabetes: A randomized controlled trial. Diabetes 2013, 62, A42. [Google Scholar] [CrossRef]
- Bell, K.J.; Gray, R.; Munns, D.; Howard, G.; Colagiuri, S.; Brand-Miller, J.C. Food Insulin Index (FII) vs. traditional carbohydrate counting for glycemic control in adults with type 1 diabetes: A 3-month pilot study. Diabetes 2014, 63, A189. [Google Scholar] [CrossRef]
- Bell, K.J.; Gray, R.; Munns, D.; Petocz, P.; Howard, G.; Colagiuri, S.; Brand-Miller, J.C. Estimating insulin demand for protein-containing foods using the food insulin index. Eur. J. Clin. Nutr. 2014, 68, 1055–1059. [Google Scholar] [CrossRef]
- Bell, K.J.; Gray, R.; Munns, D.; Petocz, P.; Steil, G.; Howard, G.; Colagiuri, S.; Brand-Miller, J.C. Clinical Application of the Food Insulin Index for Mealtime Insulin Dosing in Adults with Type 1 Diabetes: A Randomized Controlled Trial. Diabetes Technol. Ther. 2016, 18, 218–225. [Google Scholar] [CrossRef]
- Bell, K.J.; Petocz, P.; Colagiuri, S.; Brand-Miller, J.C. Algorithms to Improve the Prediction of Postprandial Insulinaemia in Response to Common Foods. Nutrients 2016, 8, 210. [Google Scholar] [CrossRef]
- Caferoglu, Z.; Hatipoglu, N.; Gokmen Ozel, H. Does food insulin index in the context of mixed meals affect postprandial metabolic responses and appetite in obese adolescents with insulin resistance? A randomised cross-over trial. Br. J. Nutr. 2019, 122, 942–950. [Google Scholar] [CrossRef]
- Erdal, B.; Caferoglu, Z.; Hatipoglu, N. The comparison of two mealtime insulin dosing algorithms for high and low glycaemic index meals in adolescents with type 1 diabetes. Diabet. Med. 2021, 38, e14444. [Google Scholar] [CrossRef]
- Ghorbaninejad, P.; Imani, H.; Sheikhhossein, F.; Tijani Jibril, A.; Mohammadpour, S.; Shab-Bidar, S. Higher dietary insulin load and index are not associated with the risk of metabolic syndrome and obesity in Iranian adults. Int. J. Clin. Pract. 2021, 75, e14229. [Google Scholar] [CrossRef]
- Khoshnoudi-Rad, B.; Hosseinpour-Niazi, S.; Javadi, M.; Mirmiran, P.; Azizi, F. Relation of dietary insulin index and dietary insulin load to metabolic syndrome depending on the lifestyle factors: Tehran lipid and glucose study. Diabetol. Metab. Syndr. 2022, 14, 198. [Google Scholar] [CrossRef]
- Lan-Pidhainy, X.; Wolever, T.M.S. Are the glycemic and insulinemic index values of carbohydrate foods similar in healthy control, hyperinsulinemic and type 2 diabetic patients. Eur. J. Clin. Nutr. 2011, 65, 727–734. [Google Scholar] [CrossRef]
- Lee, D.H.; Giovannucci, E.L.; Tabung, F.K. Insulin-related dietary indices predict 24-h urinary C-peptide in adult men. Br. J. Nutr. 2020, 1–8. [Google Scholar] [CrossRef]
- Lopez, P.E.; Evans, M.; King, B.R.; Jones, T.W.; Bell, K.; McElduff, P.; Davis, E.A.; Smart, C.E. A randomized comparison of three prandial insulin dosing algorithms for children and adolescents with Type 1 diabetes. Diabet. Med. 2018, 35, 1440–1447. [Google Scholar] [CrossRef] [PubMed]
- Mirmiran, P.; Esfandiari, S.; Bahadoran, Z.; Tohidi, M.; Azizi, F. Dietary insulin load and insulin index are associated with the risk of insulin resistance: A prospective approach in tehran lipid and glucose study. J. Diabetes Metab. Disord. 2015, 15, 23. [Google Scholar] [CrossRef]
- Nimptsch, K.; Brand-Miller, J.C.; Franz, M.; Sampson, L.; Willett, W.C.; Giovannucci, E. Dietary insulin index and insulin load in relation to biomarkers of glycemic control, plasma lipids, and inflammation markers. Am. J. Clin. Nutr. 2011, 94, 182–190. [Google Scholar] [CrossRef]
- Noori, S.; Mirzababaei, A.; Shiraseb, F.; Bagheri, R.; Clark, C.C.T.; Wong, A.; Suzuki, K.; Mirzaei, K. The Association of Inflammatory Markers, IL-1 α and TGF-β, with Dietary Insulin Load and Dietary Insulin Index in Overweight and Obese Women with Healthy and Unhealthy Metabolic Phenotypes: A Cross-Sectional Study. Int. J. Clin. Pract. 2022, 2022, 3407320. [Google Scholar] [CrossRef]
- Sadeghi, O.; Hasani, H.; Mozaffari-Khosravi, H.; Maleki, V.; Lotfi, M.H.; Mirzaei, M. Dietary Insulin Index and Dietary Insulin Load in Relation to Metabolic Syndrome: The Shahedieh Cohort Study. J. Acad. Nutr. Diet. 2020, 120, 1672–1686.e1674. [Google Scholar] [CrossRef]
- Teymoori, F.; Farhadnejad, H.; Moslehi, N.; Mirmiran, P.; Mokhtari, E.; Azizi, F. The association of dietary insulin and glycemic indices with the risk of type 2 diabetes. Clin. Nutr. 2021, 40, 2138–2144. [Google Scholar] [CrossRef] [PubMed]
| Author | City, Country | Aim | Study Design | Sample Size and Population | Main Findings |
|---|---|---|---|---|---|
| Theme 1: The association of FII with the development of metabolic syndrome, insulin resistance and diabetes | |||||
| Mirmiran et al., 2016 [53] | Tehran, Iran | To investigate the relationship between DII and DIL and the risk of development of insulin resistance in adults. | PS | 927 adults Mean age: 40.7 ± 12.4 year BMI: 27.3 ± 4.9 kg/m2 |
|
| Sadeghi et al., 2019 [56] | Yazd, Iran | To determine the association between DII and DIL and the development of MetS. | CS | 5954 adults 35–70 years | In men:
|
| Ghorbaninejad et al., 2021 [48] | Tehran, Iran | To examine the association between the insulinemic potential of a diet and MetS and obesity amongst Iranian adults. | CS | 850 healthy adults, 20–59 years |
|
| Teymoori et al., 2021 [57] | Tehran, Iran | To investigate the association between II, IL, GI and GL and the risk of developing diabetes among the Tehranian adults | Prospective study | 1149 healthy adults |
|
| Khoshnoudi-Rad et al., 2022 [49] | Tehran, Iran | To investigate: 1. The association between DII and DIL and the development of MetS. 2. The extent to which sex and lifestyle (physical activity, smoking status, and weight change) influence the relationship between DII, DIL, and MetS risk. | Prospective study | 1915 adults |
|
| Noori et al., 2022 [55] | Tehran, Iran | To investigate the relationship of inflammatory factors (IL-1αand TGF-α) with DII and DIL on healthy and unhealthy metabolic phenotypes in obese and overweight adult women. | CS | Healthy adults (women) 18–48 years |
|
| Anjom-Shoae et al., 2023 [39] | Kermanshah, Iran | To evaluate the link between the DII and DIL and cardiometabolic risk factors in patients with T2DM mellitus. | CS | 827 T2DM adults 40–70 years |
|
| Nimptsch et al., 2011 [54] | Boston, USA | To investigate the average dietary II and IL in relation to biomarkers of glycaemic control, plasma lipids, and inflammation markers. | CS | 4002 healthy adults |
|
| Lee et al., 2020 [51] | Boston, USA | To assess whether DII and empirical dietary index for hyperinsulinemia are predictive of insulin secretion. | CS | 293 healthy adult men Younger than 70 years |
|
| Caferoglu et al., 2019 [46] | Kayseri, Turkey | Comparing postprandial metabolic responses and appetite after ingestion of two meals with similar macronutrient content and GI with either high or low II in obese adolescents with insulin resistance. | RCOT | 15 obese adolescents with insulin resistance 12–18 years Weight ≥ 95th |
|
| Theme 2: The FII Compared to CC for Predicting Postprandial Insulin Response | |||||
| Holt et al., 1997 [27] | Sydney, Australia | To compare the postprandial insulin responses of isoenergetic food. | RCT | 41 healthy adults BMI: 22.7 ± 0.04 |
|
| Bao et al., 2009 [29] | Sidney, Australia | To determine whether using the FII was able to predict insulin responses to mixed meals compared to using GL or CC. | CS | 21 healthy adults Mean age: 24 ± 2.5 years BMI: 19–25 |
|
| Bao et al., 2011 [40] | Sidney, Australia | To determine whether using the FII algorithm to determine mealtime insulin demand will reduce the severity of blood glucose fluctuations (without causing hypoglycaemia) more than using CC. | RCT | 28 T1DM adults 18–70 years Diabetic diagnosis ≥1 year On insulin pump therapy |
|
| Bell et al., 2013 [41] | Sydney, Australia | To compare CC and the FII algorithm for estimating insulin dosage in adults with T1DM consuming six different single food. | TBR within-subject cross-over-controlled trial | 11 T1DM adults |
|
| Bell et al., 2014 [43] | Sidney, Australia | To compare postprandial glycaemic responses in adults with T1DM using CC and the FII algorithm to estimate the insulin dosage for protein-containing foods. | TBR within-subject cross-over design | 11 T1DM adults 18–70 years diabetic diagnosis ≥1 year On insulin pump therapy |
|
| Bell et al., 2014 [42] | Sydney, Australia | To compare if changes in HbA1c levels occurred when using CC versus the FII algorithm for estimating insulin dosages over 12 weeks in adults with type I diabetes using an insulin pump. | RCT | 26 adults with T1DM |
|
| Bell et al., 2016 [44] | Sidney, Australia and Boston, US | Comparing postprandial glycemia results over 12 weeks of using CC versus using the FII when estimating insulin dosage. | RCT | 26 T1DM adults 18–70 years old Diabetic diagnosis ≥1 year |
|
| Bell et al., 2016 [45] | Sydney, Australia | The aim was to generate mathematical algorithms to improve the prediction of postprandial insulin secretion for foods of known nutrient composition, GI and GL. | Regression analysis | - |
|
| Lopez et al., 2018 [52] | New-castle, Australia | To compare the impact of using Pankowska Equation and FII algorithms to CC on postprandial glucose excursions following a high fat and a high protein meal. | RCOT | 33 T1DM children and adolescents 7–14 years old Diabetic diagnosis ≥1 year Insulin pump therapy ≥6 months |
|
| Erdal et al., 2021 [47] | Kayseri, Turkey | Comparing the differences in the postprandial glycaemia when using CC and the food insulin index algorithms following the consumption of protein-rich, high-fat meals with different glycaemic index values. | RSBCT | 15 T1DM adolescents 14–18 years |
|
| Theme 3: The effect of metabolic status on the FII | |||||
| Lan-Pidhainy et al., 2011 [50] | Toronto, Canada | To investigate if GI and II values of carbohydrate-rich foods are similar in healthy, hyperinsulinemic and T2DM subjects, and whether metabolic status (insulin sensitivity, b-cell function, fasting-and postprandial-glucose, hepatic insulin extraction and plasma GLP-1 response) of the subjects influence the GI and II values. | CS | 31 Healthy, hyperinsulinemic, and T2DM adults |
|
| Bell et al., 2015 [30] | Sydney, Australia | To compare postprandial glucose and insulin responses to 3 consecutive meals of 2 nutrient-matched diets predicted to have either high or low insulin demand in healthy controls and participants with T2DM. | RCT | 20 Healthy adults and T2DM adults |
|
| Abaj et al., 2021 [36] | Tehran, Iran | To examine the interaction of CETP TaqB1 polymorphism with DII and DIL in altering cardiovascular risk factors among T2DM. | CS | 220 T2DM adults 134 female 86 male Mean age: 52.2 years | A significant interaction of CETP rs708272 polymorphism with DIL and DII in T2DM patients on:
|
| Abaj et al., 2022 [37] | Tehran, Iran | To investigate whether an interaction between BDNFVal66Met polymorphisms and DII and DIL can affect cardiometabolic markers among diabetic patients. | CS | 667 T2DM adults 407 female 260 male (35–65 years) |
|
| Abaj et al., 2022 [38] | Tehran, Iran | To examine the interaction of Pro12Ala polymorphism with DII and DIL in altering cardiovascular risk factors among T2DM. | CS | 393 T2DM adults |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strydom, H.; Delport, E.; Muchiri, J.; White, Z. The Application of the Food Insulin Index in the Prevention and Management of Insulin Resistance and Diabetes: A Scoping Review. Nutrients 2024, 16, 584. https://doi.org/10.3390/nu16050584
Strydom H, Delport E, Muchiri J, White Z. The Application of the Food Insulin Index in the Prevention and Management of Insulin Resistance and Diabetes: A Scoping Review. Nutrients. 2024; 16(5):584. https://doi.org/10.3390/nu16050584
Chicago/Turabian StyleStrydom, Hildegard, Elizabeth Delport, Jane Muchiri, and Zelda White. 2024. "The Application of the Food Insulin Index in the Prevention and Management of Insulin Resistance and Diabetes: A Scoping Review" Nutrients 16, no. 5: 584. https://doi.org/10.3390/nu16050584





